Abstract
Objective
To investigate whether patients experienced improved functional outcomes as a result of their admission to rehabilitation and to identify whether the service provided effective, patient-centered and goal-directed rehabilitation.
Design
Retrospective chart review of admission and discharge data from patients accessing the service between 2011 and 2019.
Setting
Community-based interdisciplinary rehabilitation service.
Participants
Consecutive patients (N=612) admitted to the service.
Interventions
Routine care delivered with a median duration of 181 days and an interquartile range of 120-261 days.
Main Outcome Measures
The Canadian Occupational Performance Measure (COPM) administered on admission and discharge and an improvement ≥2 in the COPM subscales of performance and satisfaction.
Results
Of 612 participants, 96% had the COPM administered at admission (baseline) and 68% again at discharge. Performance and satisfaction were measured in 584 patients at admission, 406 at discharge, and 404 at both time points. For performance, 243 patients (60%) experienced an improvement (≥2), with an average of 2.2 points. For satisfaction, 268 patients (66%) experienced an improvement (≥2), with an average of 2.8 points. Factors influencing outcomes, differed. For each 10 year increase in patient age, the average improvement in satisfaction was 0.26 points lower (95% confidence interval, 0.07-0.45) after adjusting for sex, duration, completion, and health condition.
Conclusions
Irrespective of patient-related factors and regardless of age, sex, health condition, or discharge plan, the majority of patients reported a positive functional outcome in COPM Performance and satisfaction as a result of time spent in the community-based rehabilitation service. This service provided equitable care and patient-centered, goal-focused, and outcome-based therapy that enabled patients to improve their functional capacity.
KEYWORDS: COPM, Interdisciplinary, Patient-reported outcome measures, Rehabilitation, Stroke
List of abbreviations: CI, confidence interval; COPM, Canadian Occupational Performance Measure; WCRT, Westlakes Community Rehabilitation Team
In countries with an aging population, such as Australia, there is a concomitant, increasing economic and societal burden on the nation's health care system.1,2 Over the next few years, more and more Australians will experience the challenges associated with aging,1 frailty,2 comorbidities,3 chronic disease,4 and declining cognitive function.5 Many of these people may benefit from rehabilitation interventions6 with emerging evidence that community-based services have the potential to reduce the economic burden on both the health and social care systems.7,8
Interdisciplinary, community-based rehabilitation services strive to provide patient-centered, goal-focused, and outcome-based therapy that enables community dwelling patients to improve their functional capacity.9,10 Although some services are disease specific,9,11 many provide care to people with a range of health conditions.12,13 This diversity of patients, in combination with a diversity of disciplines, can challenge treatment, the routine collecting of outcome data, and the selection of tools that are fit for purpose and can be used with every patient.14 This can make it difficult to adequately demonstrate a health service's effectiveness, and in turn, the development and implementation of improved interdisciplinary models of care within this clinical context.15
Patient-reported outcome measures provide opportunities to routinely collect outcome focused data in clinical environments, and they are becoming increasingly important to health systems, including those targeting rehabilitation.10,16,17 They can be considered fit for purpose in the rehabilitation context because they enhance patient-centered care and facilitate the sharing of decision-making and goal setting between all stakeholders.17,18 In contrast to some disease-specific measures, patient-reported outcome measures can be used across diverse clinical populations and have the capacity to capture outcomes of person-centered therapy goals.14,19
In the rehabilitation context, a commonly used patient-reported outcome measure is the Canadian Occupational Performance Measure (COPM). This standardized, evidence-based, clinically proven measure captures outcomes over time from a uniquely person-centered perspective.20 The COPM has been used in more than 40 countries for more than 20 years and has high clinical validity and utility.21, 22, 23 Its efficacy has been demonstrated in interdisciplinary, community-based rehabilitation programs.13,24,25 It has also been shown to enhance patient-centered care,26 facilitate patient-centered goal setting,10,27, 28, 29 and measure outcomes from a patient's perspective.9,14,25
The Westlakes Community Rehabilitation Team (WCRT) is an interdisciplinary, community-based rehabilitation service based in regional New South Wales, Australia. It strives to improve health and well-being outcomes by restoring function and independence and providing ambulatory care in patients’ homes, in their community settings, or in the team's outpatient health care facility. The WCRT includes occupational therapists, nurses, a physiotherapist, a speech pathologist, and a social worker. Its interdisciplinary method of practice relies on each professional's expertise, in addition to high levels of team communication and the completion of shared tasks. To increase fidelity, all team members complete training in the COPM before administering the tool. A positive shift of ≥2 points on the performance or satisfaction scales indicates improvement that is clinically and functionally significant.21 Those who accessed this outpatient service live in the community, and most are older and live with chronic diseases, injuries, or disabilities.
This study aimed to investigate whether patients experienced clinically meaningful functional outcomes as measured by the COPM as a result of their admission to the service and to identify whether the WCRT provided an effective, patient-centered, and goal-directed rehabilitation service to people living in the community. In 2011, the WCRT implemented the COPM as a method of measuring outcomes in patients accessing its service. On the basis of the data collected since its implementation, the authors hypothesized that (1) irrespective of patient-related factors, the service will routinely collect outcome data as part of standard care in the majority of patients, and (2) irrespective of patient-related factors, between admission (baseline) and discharge, the majority of patients will report positive outcomes in COPM performance (∆≥2) and satisfaction (∆≥2).
Methods
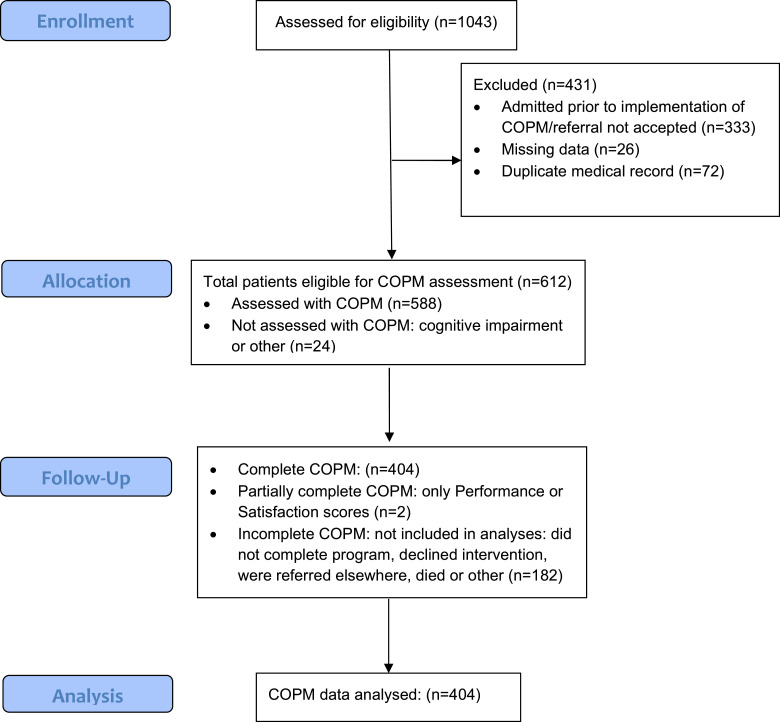
This retrospective chart review investigated routinely collected admission (baseline) and discharge data from all patients admitted to the WCRT service between 2011 and 2019. Ethics approval was granted by the local health district's human ethics committee. Informed consent was not required owing to the retrospective nature of the study exploring routine care. All data were manually extracted by the rehabilitation team into a deidentified Excela spreadsheet for analyses and securely stored and password protected. As figure 1 indicates, data from patients who declined rehabilitation before treatment, were discharged before assessment, had incomplete or missing data, or subsequent admissions for multiple care episodes in the study period were excluded from analyses.
Fig 1.
Flow chart of admissions to the WCRT between 2011 and 2019.
Categories and outcomes
Because the outpatient service treated a diverse patient cohort, prior to data collection a focus group of team members developed a number of categories including age, health condition, completion vs noncompletion, and discharge plan, which were each considered clinically relevant. They created a reference document describing these categories with practical examples to ensure consistency of classification by team members during data collection.
Patients were allocated to 1 of the 5 “health condition” categories. Referral subtypes included advanced disease, chronic rehabilitation, neurologic rehabilitation, subacute rehabilitation/neurologic, and subacute rehabilitation/other. Advanced disease included patients in the advanced stages of degenerative neurologic diseases such as motor neuron disease, which significantly affects multiple body systems and an individual's ability to participate in the community. Chronic rehabilitation included patients with multiple, chronic comorbidities primarily referred to the service because of their increased risk of falls. Participants in this group experienced functional problems but managed in the community with low levels of support. Neurologic rehabilitation included patients diagnosed with chronic neurologic diseases (eg, Parkinson disease). Subacute rehabilitation included patients who had experienced an acute event within the past 6 months. This group was divided into 2 subgroups: neurologic (eg, stroke) and nonneurologic (such as a fracture) diagnoses. Advanced disease was used as the reference cohort in the analysis because, when compared with the other cohorts, these patients were least likely to experience positive outcomes.
In addition to the health condition categories, patients were also grouped according to completion vs noncompletion and discharge plan. Completion referred to whether or not a patient remained in their rehabilitation program for the prescribed period. In patients who received some treatment, those designated as noncompletions included patients whose medical status changed, those who were admitted to social care facilities or hospitals, those who moved out of the service's area, and those who declined further interventions or were referred to another program. Completion was used as the reference cohort in this analysis.
The 5 discharge plan categories were: community exercise, onward referral, community support, admitted, and competing priorities. Community exercise included patients discharged to community-based programs that used physical activity to maintain the functional goals recently achieved. Onward referral included patients who exited the service for health-related reasons, such as patients diagnosed with stroke who were initially admitted to the WCRT service but were then referred on to the region's community-based stroke service. The admitted group included patients who exited the service because they were admitted to another health or social care facility. Community support included patients who were discharged with additional support from other health and social care services. Competing priorities included those who exited the program because of other commitments. Some patients who moved out of the area, who were unable to be contacted, or who were unable to complete the COPM because of cognitive or communication impairments were unable to be categorized. The community exercise cohort was used as the reference cohort in the analysis because this is a positive outcome for patients accessing the WCRT service.
Data collected from patients’ charts also included age (in years), sex, and duration of stay (in days). It should also be noted that the number of days in outpatient rehabilitation recorded as the duration of stay does not represent the number of days the patient received therapy, but rather the number of days from admission to the service to discharge from the service. To investigate the effect of increasing age on outcomes and to account for an age range potentially >80, patients were grouped based on 10-year ranges.
The COPM is a semistructured interview process that identifies deficits in occupational performance or problems with everyday activities that are most important to the patient. On admission to the service, patients identify deficits in occupational performance (goals) and rank them according to importance using a 10-point score card. Up to 5 most important goals are further assessed using 10-point score cards for performance and satisfaction. These 5 activities become the focus of the rehabilitation program.21 Performance and satisfaction are reassessed at discharge, and scores from admission are compared with scores at discharge. For example, if a patient identifies walking their dog as 1 of the 5 activities important to them at baseline, they may perceive their ability to perform that task at baseline as 3 out of 10, and their satisfaction with this level of performance as 2 out of 10. Only after being reassessed at discharge were patients able to view their baseline scores and discuss outcomes with team members. Those reassessing patients’ outcomes were not blinded to patients’ admission scores.
Data analysis
Patients were uniquely identified via their medical record number. When a medical record number was duplicated because a patient had multiple admissions during the study period, data corresponding to the earliest referral date were retained and the remainder were excluded from further analysis. Data from patients who had the COPM administered on admission to the service and again on discharge from the service were investigated, including those who did not complete their rehabilitation program but did complete their COPM assessment on discharge (eg, patients who left the service earlier than anticipated).
Continuous measures were summarized using means and SDs, and categorical measures were summarized as frequencies and percentages. The statistical significance level was set at 5% and adjusted for multiple comparisons using the Bonferroni method. This correction is likely to be conservative in this case because performance and satisfaction are likely to be correlated.30 The 95% confidence intervals (CIs) were calculated using normal approximations for means and using the exact binomial method for proportions. Linear regression was used to examine whether factors such as age, sex, duration of stay, completion, and categories were associated with better COPM outcomes. Logistic regression was used to examine the relationship between completion (vs noncompletion) age, sex, duration of stay, and categories.
Results
During the study period, 1043 patients referred to the WCRT were assessed for eligibility (see fig 1). There were 612 patients assessed using the COPM, from 684 admissions. For patients who were admitted to the service more than once, only the first admission was used in the analysis. Of these, 588 (96%) had the COPM administered at admission (baseline) and 404 (68%) at both baseline and discharge from the service. As hypothesized, irrespective of patient-related factors, the majority of patients had outcome data routinely collected as part of their admission to the WCRT service. Neither the descriptive data nor categories influenced whether the COPM was administered. Examples of activities identified by patients during the COPM administration included walking around the house and garden, getting into and out of bed, driving a car, accessing the community, and playing lawn bowls again.
Performance and satisfaction
Performance and satisfaction were measured on 584 patients at admission and in 406 patients at discharge. A total of 404 patients had performance and satisfaction data at both time points. Of these, 243 patients reported an improvement of ≥2 points in performance. The overall proportion of patients reporting a positive outcome in performance was 60.1% (95% CI, 55.2%-65.0%), with an average improvement of 2.2 points (95% CI, 2.0-2.4) (table 1). Of note, even the lower bound of the CI was above the clinically important threshold of 2.
Table 1.
Estimated increase in patient COPM performance and satisfaction scores
| Predictor | Performance Unadjusted |
Performance Adjusted (n=398) |
Satisfaction Unadjusted |
Satisfaction Adjusted (n=397) |
||||
|---|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | P Value | Estimate (95% CI) | P Value | Estimate (95% CI) | P Value | Estimate (95% CI) | P Value | |
| Age (10-year increase) | –0.056 (–0.216 to 0.104) |
.491 | –0.070 (–0.233 to 0.094) |
.402 | –0.191 (–0.378 to –0.004) |
.046 | –0.260 (–0.450 to –0.070) |
.007 |
| Duration (30-day increase) | 0.011 (–0.034 to 0.056) |
.636 | 0.003 (–0.043 to 0.049) |
.909 | 0.010 (–0.043 to 0.063) |
.721 | –0.010 (–0.063 to 0.044) |
.720 |
| Sex (male vs female) | 0.189 (–0.207 to 0.584) |
.349 | 0.062 (–0.328 to 0.452) |
.755 | 0.148 (–0.314 to 0.610) |
.529 | 0.066 (–0.387 to 0.518) |
.775 |
| Health condition: advanced disease reference cohort | ||||||||
| Chronic rehabilitation | 0.250 (–0.501 to 1.000) |
.514 | 0.209 (–0.529 to 0.948) |
.578 | 0.520 (–0.363 to 1.403) |
.248 | 0.442 (–0.415 to 1.298) |
.311 |
| Neurologic rehabilitation | 0.267 (–0.637 to 1.171) |
.562 | –0.208 (–1.096 to 0.679) |
.645 | 0.626 (–0.437 to 1.689) |
.247 | –0.101 (–1.131 to 0.929) |
.847 |
| Subacute rehabilitation: neurologic | 1.031 (0.207-1.854) |
.014 | 0.692 (–0.131 to 1.515) |
.099 | 1.182 (0.214-2.150) |
.017 | 0.751 (–0.203 to 1.706) |
.074 |
| Subacute rehabilitation: other | 1.108 (–0.269 to 2.485) |
.115 | 0.847 (–0.504 to 2.199) |
.219 | 0.535 (–1.084 to 2.153) |
.516 | 0.049 (–1.519 to 1.617) |
.951 |
| Completion: completed reference cohort | ||||||||
| Incomplete | –1.500 (–2.027 to –0.974) |
<.001 | –1.502 (–2.173 to –0.832) |
<.001 | –2.001 (–2.608 to –1.393) |
<.001 | –2.029 (–2.807 to –1.251) |
<.001 |
| Declined intervention | –0.712 (–1.614 to 0.189) |
.121 | –1.132 (–2.162 to –0.103) |
.031 | –0.938 (–1.978 to 0.102) |
.077 | –1.300 (–2.494 to –0.106) |
.033 |
| Alternate program | –1.604 (–3.325 to 0.116) |
.068 | –1.549 (–3.267 to 0.169) |
.077 | –1.954 (–3.939 to 0.031) |
.054 | –1.712 (–3.705 to 0.281) |
.092 |
| Discharge plan: community exercise reference cohort | ||||||||
| Medical management | –1.417 (–2.000 to –0.834) |
<.001 | –0.575 (–1.256 to 0.106) |
.098 | –1.887 (–2.566 to –1.208) |
<.001 | –0.811 (–1.601 to –0.021) |
.044 |
| Onward referral | 0.071 (–0.455 to 0.597) |
.791 | 0.070 (–0.469 to 0.608) |
.799 | –0.516 (–1.128 to 0.096) |
.098 | –0.497 (–1.122 to 0.128) |
.119 |
| Admitted | –0.985 (–1.994 to 0.024) |
.056 | –0.460 (–1.500 to 0.580) |
.385 | –1.546 (–2.720 to –0.371) |
.010 | –0.741 (–1.948 to 0.465) |
.228 |
| Community support | 0.097 (–0.493 to 0.687) |
.746 | 0.087 (–0.515 to 0.689) |
.776 | –0.066 (–0.753 to 0.622) |
.851 | –0.122 (–0.821 to 0.576) |
.731 |
| Competing priorities | 0.271 (–0.434 to 0.976) |
.450 | 1.079 (0.230-1.928) |
.013 | –0.273 (–1.094 to 0.547) |
.513 | 0.785 (–0.201 to 1.770) |
.118 |
The total number of patients who had an improvement in satisfaction ≥2 points was 268. The overall proportion of patients reporting a positive outcome in satisfaction was 66.3% (95% CI, 61.5%-70.9%), with an average improvement of 2.8 points (95% CI, 2.6-3.1) (see table 1). Of note, when compared with performance, the average improvement was greater for satisfaction, but the factors influencing the outcomes differ. For every 10-year increase in age, the improvement in satisfaction was 0.26 points lower (95% CI, 0.07-0.45) after adjusting for sex, duration, completion, and health condition. This means that for 2 patients of the same sex, duration of stay, completion status, and health condition who were 20 years apart in age, the average improvement in satisfaction would be 2×0.26=0.52 points lower for the older patient. Similarly, a patient 30 years older would expect a lower average improvement by 3×0.26=0.78 points. Despite this reduction in improvement with age, because the overall mean improvement in satisfaction was 2.81 points, we would still expect patients in every age category (with everything else being equal) to experience the clinically significant improvement in satisfaction of >2 points.
Completion and duration
Of the 612 patients, 345 (56.4%) completed the program, 182 (29.7%) did not complete the program, 44 (7.2%) declined intervention, 21 (3.4%) were assigned to an alternate program, and 20 (3.3%) died before they could complete the program (table 2). Of note, when compared with patients who did complete their programs, the average performance score in those who did not complete their programs was 1.5 points less (95% CI, 0.832-2.173; P<.001). In addition, after adjusting for other factors, those who did not complete their program had an average of 2 points less improvement on the satisfaction scale (95% CI, 1.251-2.807; P<.001) (table 3).
Table 2.
Sample demographics
| Characteristics | Reason for Referral |
||||
|---|---|---|---|---|---|
| Advanced Disease | Chronic Rehabilitation | Neurologic Rehabilitation | Subacute Rehabilitation | ||
| Neurological < 6 Months Post Acute Event | Other | ||||
| Female, n (%) | 26 (45) |
200 (56) |
36 (50) |
45 (42) |
4 (29) |
| Age (y), mean ± SD | 69.2±9.4 | 75.7±10.8 | 62.2±16.0 | 67.8±15.0 | 67.4±14.4 |
| Duration from referral date to discharge (d), median (minimum, maximum) | 245 (36, 946) |
172 (19, 1172) |
193 (49, 1007) |
167 (29, 697) |
145 (17, 335) |
| Rehabilitation program outcome | |||||
| Completion, n (%) | 28 (48) |
195 (54) |
44 (60) |
68 (64) |
10 (71) |
| Incomplete, n (%) | 18 (31) |
114 (32) |
23 (32) |
23 (22) |
4 (29) |
| Declined intervention, n (%) | 0 (0) |
27 (7.5) |
4 (5.5) |
13 (12) |
0 (0) |
| Alternate program, n (%) | 3 (5.2) |
15 (4.2) |
2 (2.7) |
1 (0.9) |
0 (0) |
| Deceased, n (%) | 9 (16) |
9 (2.5) |
0 (0) |
2 (1.9) |
0 (0) |
| Discharge plan | |||||
| Community exercise, n (%) | 5 (8.6) |
99 (28) |
17 (23) |
27 (25) |
5 (36) |
| Medical management, n (%) | 13 (22) |
72 (20) |
8 (11) |
8 (7.5) |
2 (14) |
| Onward referral, n (%) | 9 (16) |
47 (13) |
9 (12) |
27 (25) |
1 (7) |
| Admitted, n (%) | 12 (21) |
56 (16) |
9 (12) |
6 (5.6) |
2 (14) |
| Community support, n (%) | 9 (16) |
29 (8.1) |
14 (19) |
7 (6.5) |
0 (0) |
| Competing priorities, n (%) | 0 (0) |
24 (6.7) |
8 (11) |
21 (20) |
2 (14) |
| Missing / Unknown, n (%) | 10 (17) |
33 (9.2) |
8 (11) |
11 (10) |
2 (14) |
Table 3.
Estimated odds ratio of completion vs noncompletion
| Predictor | Unadjusted |
Adjusted (n=527) |
||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P Value | Odds Ratio (95% CI) | P Value | |
| Age (10-year increase) | 1.117 (0.972-1.284) |
.117 | 1.231 (0.981-1.544) |
.073 |
| Duration (30-day increase) | 1.015 (0.976-1.055) |
.469 | 1.047 (0.979-1.119) |
.180 |
| Sex (male vs female) | 0.931 (0.650-1.334) |
.697 | 0.987 (0.555-1.753) |
.963 |
| Health condition: advanced disease reference cohort | ||||
| Chronic rehabilitation | 1.100 (0.582-2.076) |
.770 | 0.762 (0.282-2.062) |
.593 |
| Neurologic rehabilitation | 1.230 (0.565-2.677) |
.602 | 0.849 (0.247-2.917) |
.795 |
| Subacute rehabilitation: neurologic | 1.901 (0.891-4.055) |
.097 | 1.015 (0.298-3.461) |
.980 |
| Subacute rehabilitation: other | 1.607 (0.437-5.909) |
.475 | 3.814 (0.589-24.70) |
.160 |
| Discharge plan: community exercise reference cohort | ||||
| Medical management | 61.97 (22.47-170.89) |
<.001 | 62.49 (22.47-170.89) |
<.001 |
| Onward referral | 53.44 (15.29-186.83) |
<.001 | 50.09 (13.88-180.82) |
<.001 |
| Admitted | 0.267 (0.115-0.622) |
.002 | 0.265 (0.110-0.639) |
.003 |
| Community support | 125.67 (16.42-961.71) |
<.001 | 126.18 (16.25-979.82) |
<.001 |
| Competing priorities | 0.747 (0.314-1.777) |
.510 | 0.743 (0.292-1.888) |
.532 |
The average program duration was 213.8 days, with a SD of 145.2 days. However, the distribution of duration has a distinct right skew with a minimum of 17 days and a maximum of 1172 days. The median duration was 181 days, with an interquartile range of 120 to 261 days (see table 2). As hypothesized, irrespective of patient-related factors, between admission (baseline) and discharge, the majority of patients reported a positive outcome in COPM performance (∆≥2) and satisfaction (∆≥2) (see table 1).
Discussion
The COPM successfully measured the effect of rehabilitation interventions across a broad range of patients, and a large percentage of patients experienced improvements in performance and satisfaction. These improvements were seen regardless of age, sex, health condition, or discharge plan, demonstrating equity in the service's health care delivery. Its achievements in relation to the team's purpose to provide patient-centered, goal-focused, and outcome-based therapy that enables community-dwelling patients to improve their functional capacity.9,10,31 The WCRT works on the premise all patients are offered care. Therefore, it is noteworthy that the patients who completed all aspects of their rehabilitation programs showed improvement of >2 points, when compared with those who did not complete their programs.
This study demonstrates that the COPM is an evidence-based tool13,24,25 that is “fit for purpose” in the community-based rehabilitation context. As anticipated, almost all patients who completed the program had outcome data routinely collected as part of their admission to the WCRT's service. One barrier potentially influencing the routine collecting of outcome data in clinical practice is a tool's clinical applicability and utility.15,32,33 The WCRT's success in routinely administrating the COPM once again demonstrates its feasibility and clinical utility in everyday, interdisciplinary, community-based rehabilitation team environments.13,24,25 It also affirms that patient-reported outcome measures such as the COPM present a unique opportunity for clinical services that provide care to diverse populations in terms of age and health conditions, to routinely capture outcomes from a patient perspective, and in turn demonstrate efficacy of service delivery.26
At the WCRT, the COPM appeared to have created uniformity of service delivery for every patient regardless of age, sex, duration of admission, health conditions, or discharge destination, but this would need further research to confirm. Patient-reported outcome measures such as the COPM enable the development of data frameworks for processes of care, providing a practical method for the WCRT to function as a patient-centered service that can demonstrate that its intake and assessment processes foster patient-centered care and shared decision-making between therapist and patient. In collaboration with patients, the WCRT can develop meaningful goals for therapy, promote engagement, evaluate outcomes from a patient perspective, and provide equitable care.25,26
Study limitations
This investigation was limited by the relatively small number of patients who accessed the WCRT service during the study period, the changes in staffing involved in the study over time, the absence of a control group, and the potential overlap between the classifications of the disease cohorts. Future investigations could consider using randomized or crossover methods to test the effect of community-based rehabilitation and by documenting the interventions that patients receive as a result of accessing such services. There is also potential to investigate the lived experiences of the staff involved in such studies and collect data on who administered the COPM and why. However, the investigation was also strengthened by the fact that data were retrospectively analyzed, reducing the potential bias toward positive outcomes, when outcomes are measured by those who are implementing the interventions. In addition, the findings were strengthened by the diversity of the study's cohort, as it is strongly reflective of the majority of community-based, rehabilitation populations in countries with aging populations that are experiencing high levels of chronic diseases.
Conclusions
Irrespective of patient-related factors and regardless of age, sex, health condition or discharge plan, the majority of the WCRT's patients who completed the COPM and the program reported a positive outcome in performance and satisfaction as a result of time spent in its community-based rehabilitation service. This service provided equitable health care delivery, and patient-centered, goal-focused, and outcome-based therapy that enabled patients to improve their functional capacity. Patient-reported outcome measures such as the COPM provide opportunities to collect outcome-focused data in clinical environments. This study found that the COPM can be used routinely by interdisciplinary teams providing community-based rehabilitation to diverse clinical populations.
Supplier
-
a.
Excel; Microsoft Corp.
Acknowledgments
We thank the members of the WCRT, including Sam Zok, BSocW, (Social Worker); Anna Reid, BAppSc (Speech Pathology) and Selena McCaig, BSc, BAppSci (Speech Pathology); Ingrid Fair, BOccThy, Kristie Innes, BHlthSc(OccThy), Eve Broadfoot, BOccThy, Joanne Anson-Smith, OMS, BHlthSc(OccThy), and Jodie McIvor, BHlthSc(OccThy) (Occupational Therapists); Allison Marler, ACEEN, Edlyn Thompson, ACEEN, and Kim Tobin, ACEN, (Enrolled Nurses); Danielle Hayden, BPhysio, Anitra Thomas, BAppSc (PT), PgC (CBT), Anjelica Carlos, (PT) (Hons), Heidi Janssen, PhD, MHSC, BPhysio, and Belinda Williamson, BPhysio (Physiotherapists); Andi Pramono, B(Dent), MQIHC, MHlthServMgt, (Quality Improvement Manager); and Christopher Catchpole, MAM (Health), BASc (Phys), (Allied Health Manager).
Footnotes
Supported by the Hunter New England Local Health District Allied Health Research Committee.
Disclosures: none.
References
- 1.World Health Organization . 2018. WHO country cooperation strategy at a glance: Australia.http://www.who.int/iris/handle/10665/272616 Available at: Accessed September 21, 2019. [Google Scholar]
- 2.Diouf I, Magliano DJ, Carrington MJ, Steward S, Shaw JE. Prevalence, incidence, risk factors and treatment of atrial fibrillation in Australia: the Australian Diabetes, Obesity and Lifestyle (AusDiab) longitudinal, population cohort study. Int J Cardiol. 2016;205:127–132. doi: 10.1016/j.ijcard.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Li E, Clark M, Heesch K, Vallmuur K. 94 Falls in middle-aged adults presenting to emergency departments in Queensland, Australia: risk factor exploration. Inj Prev. 2016;22:A35–A36. [Google Scholar]
- 4.Ullberg T, Zia E, Petersson J, Norrving B. Perceived unmet rehabilitation needs 1 year after stroke. An observational study from the Swedish Stroke Register. Stroke. 2016;47:539–541. doi: 10.1161/STROKEAHA.115.011670. [DOI] [PubMed] [Google Scholar]
- 5.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hillen JB, Vitry A, Caughey GE. Disease burden, comorbidity and geriatric syndromes in the Australian aged care population. Australas J Ageing. 2017;36:E14–E19. doi: 10.1111/ajag.12411. [DOI] [PubMed] [Google Scholar]
- 7.Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Arch Phys Med Rehabil. 2019;100:2205–2211. doi: 10.1016/j.apmr.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Lewin GF, Alfonso HS, Alan JJ. Evidence for the long term cost effectiveness of home care reablement programs. Clin Interv Aging. 2013;8:1273–1281. doi: 10.2147/CIA.S49164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kjerstad E, Tuntland HK. Reablement in community-dwelling older adults: a cost-effectiveness analysis alongside a randomized controlled trial. Health Econ Rev. 2016;6:15. doi: 10.1186/s13561-016-0092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurklinsky S, Perez RB, Lacayo ER, Sletten CD. The efficacy of interdisciplinary rehabilitation for improving function in people with chronic pain. Pain Res Treat. 2016;2016 doi: 10.1155/2016/7217684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lexell EM, Flansbjer UB, Lexell J. Self-perceived performance and satisfaction with performance of daily activities in persons with multiple sclerosis following interdisciplinary rehabilitation. Disabil Rehabil. 2014;36:373–378. doi: 10.3109/09638288.2013.797506. [DOI] [PubMed] [Google Scholar]
- 12.Nas K, Yazmalar L, Şah V, Aydın A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6:8–16. doi: 10.5312/wjo.v6.i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tuntland H, Aaslund MK, Langeland E, Espehaug B, Kjeken I. Psychometric properties of the Canadian Occupational Performance Measure in home-dwelling older adults. J Multidiscip Healthc. 2016;9:411–423. doi: 10.2147/JMDH.S113727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langeland E, Tuntland H, Folkestad B, Forland O, Jacobsen FF, Kjeken I. A multicenter investigation of reablement in Norway: a clinical controlled trial. BMC Geriatrics. 2019;19:29. doi: 10.1186/s12877-019-1038-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Öksüz Ç, Akel BS, Aran OT, Sığırtmaç İ, Leblebicioğlu AG. Do hand outcome measures reflect cultural influences? Acta Orthop Traumatol Turc. 2017;51:325–330. doi: 10.1016/j.aott.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duncan EA, Murray J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: a systematic review. BMC Health Serv Res. 2012;12:96. doi: 10.1186/1472-6963-12-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weldring T, Smith SM. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) Health Serv Insights. 2013;6:61–68. doi: 10.4137/HSI.S11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heinemann AW, Nitsch KP, Ehrlich-Jones L. Effects of an implementation intervention to promote use of patient-reported outcome measures on clinicians' perceptions of evidence-based practice, implementation leadership, and team functioning. J Contin Educ Health Prof. 2019;39:103–111. doi: 10.1097/CEH.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 19.Rotenstein LS, Agarwal A, O'Neil K. Implementing patient-reported outcome surveys as part of routine care: lessons from an academic radiation oncology department. J Am Med Inform Assoc. 2017;24:964–968. doi: 10.1093/jamia/ocx009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Disantis AY, Piva SR, Irrgang JJ. Standardized patient reported outcomes do not capture functional deficits of patients following contemporary total knee replacement: descriptive study. J Exerc Sports Orthop. 2018;5 doi: 10.15226/2374-6904/5/1/00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Law L, Baptise S, Carswell A, McColl MA, Polatajko H, Pollock N. Fourth ed. Canadian Association of Occupaitonal Therapists; Ottawa, Canada: 2005. Canadian Occupational Performance Measure; p. 89. [Google Scholar]
- 22.Roe D, Brown T, Thyer L. Validity, responsiveness, and perceptions of clinical utility of the Canadian Occupational Performance Measure when used in a sub-acute setting. Disabil Rehabil. 2020;42:2772–2789. doi: 10.1080/09638288.2019.1573934. [DOI] [PubMed] [Google Scholar]
- 23.Thyer L, Brown T, Roe D. The validity of the Canadian Occupational Performance Measure (COPM) when used in a sub-acute rehabilitation setting with older adults. Occup Ther Health Care. 2018;32:137–153. doi: 10.1080/07380577.2018.1446233. [DOI] [PubMed] [Google Scholar]
- 24.Yang SY, Lin CY, Lee YC, Chang JH. The Canadian Occupational Performance Measure for patients with stroke: a systematic review. J Phys Ther Sci. 2017;29:548–555. doi: 10.1589/jpts.29.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Enemark Larsen A, Carlsson G. Utility of the Canadian Occupational Performance Measure as an admission and outcome measure in interdisciplinary community-based geriatric rehabilitation. Scand J Occup Ther. 2012;19:204–213. doi: 10.3109/11038128.2011.574151. [DOI] [PubMed] [Google Scholar]
- 26.Tuntland H, Kjeken I, Folkestad B, Førland O, Langeland E. Everyday occupations prioritised by older adults participating in reablement. A cross-sectional study. Scand J Occup Ther. 2020;27:248–258. doi: 10.1080/11038128.2019.1604800. [DOI] [PubMed] [Google Scholar]
- 27.Enemark Larsen A, Rasmussen B, Christensen JR. Enhancing a client-centred practice with the Canadian Occupational Performance Measure. Occup Ther Int. 2018;2018 doi: 10.1155/2018/5956301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevens A, Koke A, van der Weijden T, Beurskens A. The development of a patient-specific method for physiotherapy goal setting: a user-centered design. Disabil Rehabil. 2018;40:2048–2055. doi: 10.1080/09638288.2017.1325943. [DOI] [PubMed] [Google Scholar]
- 29.Flink M, Bertilsson AS, Johansson U, Guidetti S, Tham K, von Koch L. Training in client-centeredness enhances occupational therapist documentation on goal setting and client participation in goal setting in the medical records of people with stroke. Clin Rehabil. 2016;30:1200–1210. doi: 10.1177/0269215515620256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eyssen IC, Steultjens MP, Oud TA, Bolt EM, Maasdam A, Dekker J. Responsiveness of the Canadian Occupational Performance Measure. J Rehabil Res Dev. 2011;48:517–528. doi: 10.1682/jrrd.2010.06.0110. [DOI] [PubMed] [Google Scholar]
- 31.Stevens A, Beurskens A, Köke A, van der Weijden T. The use of patient-specific measurement instruments in the process of goal-setting: a systematic review of available instruments and their feasibility. Clin Rehabil. 2013;27:1005–1019. doi: 10.1177/0269215513490178. [DOI] [PubMed] [Google Scholar]
- 32.Birkeland A, Tuntland H, Førland O, Jakobsen FF, Langeland E. Interdisciplinary collaboration in reablement: a qualitative study. J Multidiscip Healthc. 2017;10:195–203. doi: 10.2147/JMDH.S133417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Egdom LSE, Oemrawsingh A, Verweij LM. Implementing patient-reported outcome measures in clinical breast cancer care: a systematic review. Value Health. 2019;22:1197–1226. doi: 10.1016/j.jval.2019.04.1927. [DOI] [PubMed] [Google Scholar]