HIGHLIGHTS
-
•
People with diabetes may experience worse outcomes from frozen shoulder than those without diabetes; however, the certainty in evidence was moderate to low.
-
•
If high-quality studies can confirm the findings of this review, then clinicians should monitor patients with frozen shoulder with diabetes more closely and offer further treatment if pain or lack of function persists long-term.
KEYWORDS: Adhesive capsulitis, Diabetes, Frozen shoulder, Prognosis, Rehabilitation
Abstract
Objective
To summarize evidence from longitudinal observational studies to determine whether diabetes (types 1 and 2) is associated with the course of symptoms in people with frozen shoulder.
Data Sources
A systematic literature search of 11 bibliographic databases (published through June 2021), reference screening, and emailing professional contacts.
Study Selection
Studies were selected if they had a longitudinal observational design that included people diagnosed with frozen shoulder at baseline and compared outcomes at follow-up (>2wk) among those with and without diabetes at baseline.
Data Extraction
Data extraction was completed by 1 reviewer using a predefined extraction sheet and was checked by another reviewer. Two reviewers independently judged risk of bias using the Quality in Prognostic Factor Studies tool.
Data Synthesis
A narrative synthesis, including inspection of forest plots and use of the prognostic factor Grading of Recommendations, Assessment, Development and Evaluations framework. Twenty-eight studies satisfied the inclusion criteria. Seven studies were judged to be at a moderate risk of bias and 21 at a high risk of bias. Diabetes was associated with worse multidimensional clinical scores (moderate certainty in evidence), worse pain (low certainty in evidence), and worse range of motion (very low certainty in evidence).
Conclusions
This review provides preliminary evidence to suggest that people with diabetes may experience worse outcomes from frozen shoulder than those without diabetes. If high-quality studies can confirm the findings of this review, then clinicians should monitor patients with frozen shoulder with diabetes more closely and offer further treatment if pain or lack of function persists long-term.
Frozen shoulder, also known as adhesive capsulitis, is a painful condition that can cause prolonged disability.1 Stiffness of the capsule surrounding the glenohumeral joint reduces both active and passive range of motion (ROM), particularly external rotation.2 Frozen shoulder is commonly, but incorrectly, said to be a self-limiting condition (meaning that, in time, the condition will resolve without intervention).3, 4, 5 However, there is an abundance of evidence to suggest that many patients with frozen shoulder suffer from long-term pain and restricted movement.6, 7, 8, 9 Frozen shoulder is initially treated using conservative (nonsurgical) methods including analgesics, local corticosteroid injection, and gentle mobilization and exercise.5 Cases that are resistant to conservative management may be treated surgically with manipulation under anesthesia, arthroscopic capsular release, or arthrographic distention/hydrodilatation.10 Currently there is no clear consensus as to which management strategy is the most effective way to treat frozen shoulder.10, 11, 12
The onset of frozen shoulder most commonly occurs between 40 and 70 years of age, with patients rarely presenting before the age of 40.13 Fifty-eight percent of people with frozen shoulder are women.13 In 6%-17% of patients the contralateral shoulder is also affected, usually within 5 years of the first shoulder recovering.5,14 The prevalence of frozen shoulder in the general population has often been stated in the literature to be around 2%,14 although any estimates of the incidence or prevalence of frozen shoulder will be inconsistent owing to the variability in diagnostic criteria for frozen shoulder.15
People with diabetes are 5 times more likely to have frozen shoulder than people without diabetes, and the prevalence of frozen shoulder in people with diabetes has been estimated to be 13.4%.14 Although it is currently unclear why diabetes is associated with frozen shoulder, it has been hypothesized that glycation processes may cause changes in capsule tissues and consequently lead to the development of frozen shoulder.16 People with diabetes make up around 30% of the frozen shoulder population14; therefore, it is important to understand whether and how the outcomes of frozen shoulder may differ for people with diabetes compared with those without diabetes.
This review summarizes evidence from longitudinal observational studies to investigate whether diabetes is a prognostic factor in people with frozen shoulder.
Methods
Search strategy
The protocol for this systematic review was registered on PROSPERO (CRD42019122963), and the review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement.17 MEDLINE, EMBASE, AMED, PsycINFO, Web of Science core collection, Cumulative Index to Nursing and Allied Health Literature, Epistemonikos, Trip, PEDro, OpenGrey, and The Grey Literature Report were searched from inception to June 2021. Reference lists of included studies were screened and a professional contact of 1 author (D.vdW.) was contacted. The search for MEDLINE, using Medical Subject Headings and free-text words related to shoulder pain and diabetes, can be found in supplemental appendix S1 (available online only at http://www.archives-pmr.org/). The search strategy was constructed (with the help of a health information expert) to identify studies about shoulder pain in general, rather than frozen shoulder, to maximize the sensitivity of the search.
Study selection
Titles and abstracts were screened by 1 reviewer (B.P.D.) and a 20% random sample was independently checked by 2 reviewers (M.B-B., C.B.) using predefined inclusion and exclusion criteria. Disagreements were resolved by discussion with another reviewer (D.vdW.). Full-text articles were screened by B.P.D. and were independently checked by 3 reviewers (M.B-B., C.B., T.R-M.) using predefined inclusion and exclusion criteria. Any discrepancies were reviewed by and discussed with D.vdW.
To be eligible for inclusion, studies were required to have a longitudinal observational design (prospective or retrospective), include people diagnosed with frozen shoulder at baseline, establish self-reported or clinically diagnosed type 1 or type 2 diabetes at baseline, and compare outcomes between those with and without diabetes at follow-up (>2wk). Cross-sectional studies, case studies, and trials were excluded. We included population-based studies as well as clinical cohorts, with no limitations in terms of treatment received for frozen shoulder. When a full-text article could not be obtained, the study was excluded. All outcome variables related to frozen shoulder, including ROM, pain, and functionality, were eligible for inclusion. Non–English-language papers were assessed by a reviewer with appropriate language skills.
Data extraction and risk of bias assessment
Data were extracted using a predefined extraction sheet by 1 reviewer (B.P.D.) and independently checked by 3 reviewers (M.B-B., C.B., T.R-M.). Extracted data included details of study design, setting, sample characteristics, exposure/outcome/covariate measurement, sample size, treatment type, attrition, inclusion and exclusion criteria, statistical analysis, and association estimates and their corresponding raw data (if presented). Risk of bias for all studies was independently assessed by pairs of reviewers. The Quality In Prognosis Studies (QUIPS) tool18 was used to judge risk of bias. The QUIPS tool covers 6 domains: (1) study participation; (2) study attrition; (3) prognostic factor measurement; (4) outcome measurement; (5) study confounding; and (6) statistical analysis and reporting. Each domain is scored as either low, medium, or high risk of bias, and each domain contains numerous prompting items to help guide decision making. The bias scores for each domain and potential effect of biases on the overall study risk of bias were then used to judge the overall risk of bias. Disagreements regarding data extraction and risk of bias were resolved by discussion.
Analysis
There was a high level of variation between studies in terms of outcome measures and length of follow-up; therefore, pooled estimates of associations between diabetes and outcome were not calculated. Generally, results were reported as continuous data, so forest plots of mean differences in outcome scores between people with and without diabetes were plotted. This allowed for the results from the primary studies to be visualized and helped inspect the magnitude, direction, and consistency of possible associations. Where studies provided sufficient raw data, confidence intervals were calculated and included in the forest plot; otherwise, only the point estimate was used. Forest plots were plotted using R version 4.0.2.19,a
The synthesis and grading of evidence were conducted using an adapted version of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework, which is tailored specifically for the use of prognostic factor research.20 The GRADE framework scores prognostic evidence on 6 factors (phase of investigation, study limitations, inconsistency, indirectness, imprecision, publication bias) that may decrease the quality of evidence and 2 factors that may increase the certainty in evidence (effect size, exposure-response gradient). Evidence for the association of diabetes with outcomes in people with frozen shoulder was graded after considering all QUIPS scores, tallies of association direction, raw data, and forest plots.
Some studies reported results for the same outcome at multiple follow-up points. To ensure that these cohorts only contributed once to the results but were still incorporated into the evidence synthesis and GRADE assessment, the direction of association reported in the evidence synthesis for these studies was the direction of association observed most frequently throughout follow-up points. When multiple ROM movements were reported within a single article, the most common direction of association observed for those movements was used for the scoring of the GRADE direction of association between diabetes and ROM for that study. Additionally, some studies used multiple instruments to measure the same domain, so the measure that was used most frequently by papers in the review was included in the evidence synthesis.
Results
Search results
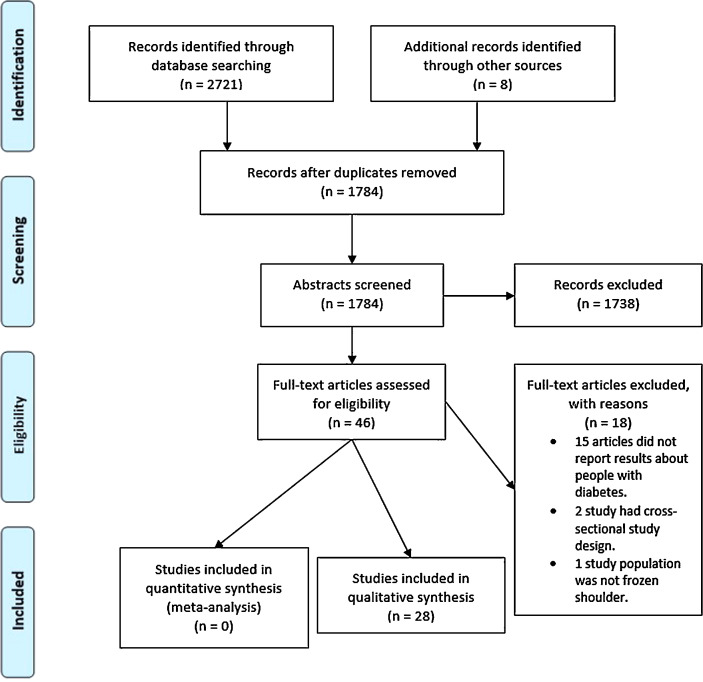
The searches identified 1784 unique citations; 46 studies were selected for full-text screening and 28 studies were selected for the final review (fig 1). Twenty-one studies reported results about the outcome domains ROM (abduction, forward flexion, external and internal rotation), pain (eg, 0-10 visual analog score21) and/or multidimensional clinical scores (eg, Constant score) and are summarized in this article, and 13 studies that reported less common (<5 studies) outcomes are reported in supplemental appendix S2, tables SB1 and SB2 (available online only at http://www.archives-pmr.org/). Thirteen studies investigated the association between diabetes and ROM, 10 with pain, and 19 with multidimensional clinical scores.
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram summarizing study identification and selection.
Study characteristics
The 21 articles reporting ROM, pain, or multidimensional clinical scores in this review were cohort studies. Patients received arthroscopic capsular release in 7 studies, hydrodilatation in 3, manipulation under anesthesia in 4, physiotherapy alone in 2, physiotherapy and ultrasound-guided intraarticular corticosteroid injection and exercise in 1, manipulation and arthroscopic capsular release in 1, manipulation under ultrasound-guided brachial plexus block in 1, and a mixture of surgical and conservative treatments in 3. Nine studies were from Europe, 9 from Asia, 3 from North America, and 1 from Oceania. Thirteen studies were hospital based, 2 were based in medical centers, 1 was based in a physiotherapy clinic, 1 was based in a sports medicine clinic, and the remaining 5 did not specify the setting. Sample size ranged from 15-295 shoulders, with a median sample size of 56 shoulders. The percentage of shoulders from people with diabetes ranged from 13%-57% with a mean of 25%±13%.
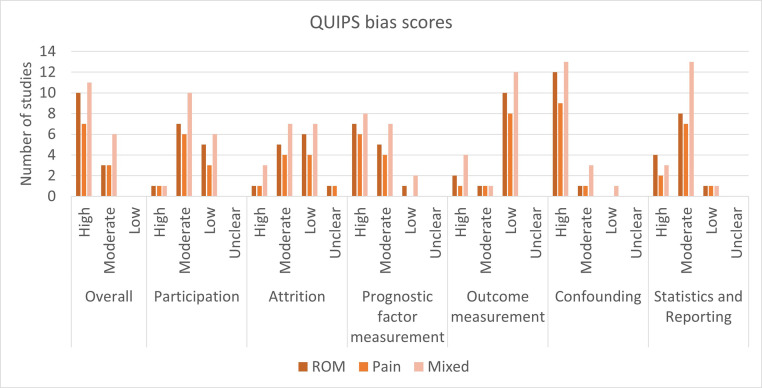
Risk of bias
QUIPS risk of bias assessments can be found in supplementarl table SC1 (available online only at http://www.archives-pmr.org/) and overall risk of bias scores for each study can be found in table 1. Across studies, the reviewers agreed on risk of bias scores for 82% of bias domains and agreed on 26 of the 28 overall risk of bias scores. Twenty-one studies were judged to be at a high risk of bias and 7 were judged to be at a moderate risk of bias. In general, the methods used to account for potential confounders, prognostic factors/diabetes measurements, and statistical analysis and reporting were poor (fig 2). Studies often used basic univariate tests to compare outcomes between the diabetes and non-diabetes groups and thus did not adjust for confounders and did not present or compare the characteristics of the 2 groups. Reporting of results was often incomplete and confidence intervals and measures of spread were not always reported (supplemental tables SB1-SB5, available online only at http://www.archives-pmr.org/). It was not clear whether the decision to compare outcomes between those with and without diabetes was based on a priori hypotheses or a posteriori hypotheses, meaning that there was potential reporting bias present. Studies rarely defined diabetes or reported how diabetes was established (self-reported, tested, or from medical records).
Table 1.
Summary of study characteristics for studies reporting ROM, pain, or multidimensional clinical scores
| Study | Study Design and Setting | Treatment Type | Outcomes Measured and Tools Used | Follow-Up Measurements Taken | Sample Size | QUIPS Risk of Bias Score |
|---|---|---|---|---|---|---|
| Nicholson22 | Cohort study Hospital, US |
Arthroscopic capsular release | ROM, pain (VAS), multidimensional score (ASES) | Mean 3 y post-capsular release (range, 2-8 y) | Diabetes: 8 shoulders; non-diabetes: 17 shoulders | High |
| Cvetanovich et al23 | Cohort study Medical center, US |
Arthroscopic capsular release | ROM | Mean 3.7 y post-capsular release (range, 2-6 y) | Diabetes: 8 shoulders; non-diabetes: 19 shoulders | High |
| Clement et al24 | Cohort study Hospital, UK |
Hydrodilatation. | ROM, pain (VAS), multidimensional score (OSS) | 1 mo post-hydrodilatation | Diabetes: 12 people; non-diabetes: 39 people | High |
| Bell et al25 | Cohort study Setting unclear, Australia |
Hydrodilatation | ROM, pain (VAS) scored as nil, mild, moderate, or severe | 2 mo post-hydrodilatation | Diabetes: 15 people; non-diabetes: 94 people | High |
| Vastamäki and Vastamäki26 | Cohort study Hospital, Finland |
MUA | ROM, pain (VAS) | Mean 23.1 y post-MUA (range, 19-30 y) | Diabetes: 4 people; non-diabetes: 11 people | High |
| Cho et al27 | Cohort study Setting unclear, Republic of Korea |
Arthroscopic capsular release | ROM, Pain (VAS), multidimensional score (ASES) | 3 mo, 6 mo, 12 mo post-capsular release and a final follow-up of mean 48.4±15.8 mo | Diabetes: 17 shoulders pre-capsular release and final follow-up, 15 at 3 mo, 9 at 6 mo, 13 at 12 mo; non-diabetes: 20 shoulders pre-capsular release, at 3 mo and final follow-up, 17 at 6 mo, 15 at 12 mo | Moderate |
| Ando et al28 | Cohort study Setting unclear, Japan |
Manipulation under ultrasound-guided brachial plexus block | ROM, pain (VAS), multidimensional score (Constant score) | Mean 4.8±3.5 y for the diabetes group; mean 5.1±2.4 y for the non-diabetes group | Diabetes: 10 shoulders; non-diabetes: 42 shoulders | High |
| Düzgün et al29 | Cohort study Physiotherapy center, Turkey |
Physiotherapy | ROM, multidimensional score (Constant score) | Following the treatment protocol averaging 8 wk duration | Diabetes: 12 people; non-diabetes: 38 people | Moderate |
| Vastamäki et al30 | Cohort study Hospital, Finland |
Diabetes group: 69% underwent MUA and 31% underwent conservative treatment; non-diabetes group: 53.3% underwent MUA and 37.3% underwent conservative treatment | ROM, pain (VAS), multidimensional score (Constant score) | Mean 10±8 y for the diabetes group and mean 9.7±7 y for the non-diabetes group | Diabetes: 29 shoulders; non-diabetes: 169 shoulders | High |
| Mehta et al31 | Cohort study Hospital, UK |
Arthroscopic capsular release | multidimensional score (Constant score) | 6 weeks, 6 mo, and 2 y post-capsular release | Diabetes: 21 people; non-diabetes: 21 people | High |
| Çınar et al32 | Cohort study Setting unclear, Turkey |
Arthroscopic capsular release | Multidimensional score (Constant score) | Mean 48.5 mo for the diabetes group and mean 60.2 mo for the non-diabetes group | Diabetes: 15 shoulders; non-diabetes: 13 shoulders | High |
| Wang et al33 | Cohort study Medical center, Taiwan |
MUA | Multidimensional score (Adjusted constant score, excluding the 25 points for assessment of muscle strength) | 3 wk post-MUA and an average of 95 mo (range, 18-189 mo) post-MUA | Diabetes: 21 shoulders; non-diabetes: 42 shoulders | High |
| Celik et al34 | Cohort study Setting unclear, Turkey |
Manipulation and arthroscopic capsular release | Multidimensional score (Constant score) | Mean 49.5 mo (range, 24-90 mo) | Diabetes: 12 shoulders; non-diabetes: 20 shoulders | High |
| Sinha et al35 | Cohort study Hospital, UK |
Hydrodilatation | Multidimensional score (OSS) | Improvement in OSS between pre-procedure and 4 wk post-procedure | Diabetes: 26 people; non-diabetes: 90 people | Moderate |
| Lyhne et al36 | Cohort study Hospital, Denmark |
Arthroscopic capsular release | Multidimensional score (OSS) | Improvement between pre-procedure and 6-mo post-op OSSs | Diabetes: 18 people; non-diabetes: 75 people | High |
| Theodorides et al37 | Cohort study Hospital, UK |
MUA | Multidimensional score (OSS) | Mean follow-up 28 d post-MUA and at mean follow-up 3.6 y post-MUA (IQR, 1.7-5.0 y) | Diabetes: 39 people; non-diabetes: 256 people | Moderate |
| Lamplot et al38 | Cohort study Sports medicine clinic, USA |
Conservative treatment | Multidimensional score (ASES) | Minimum 2-y follow-up (mean, 3.4 y) | Diabetes: 9 people; non-diabetes: 51 people | High |
| Cho et al39 | Cohort study Hospital, Republic of Korea |
Ultrasound-guided intraarticular corticosteroid injection | ROM, pain (VAS), multidimensional score (ASES) | 3 wk, 6 wk, 12 wk posttreatment | Diabetes group: 32 shoulders; non-diabetes group: 110 shoulders | High |
| Ko et al40 | Cohort study Hospital, Republic of Korea |
MUA | ROM, pain (VAS), multidimensional score (Constant score) | 6 wk, 3 mo posttreatment | Diabetes group: 32 shoulders; non-diabetes group: 203 shoulders | Moderate |
| Yanlei et al41 | Cohort study Hospital, Singapore |
Arthroscopic capsular release | ROM, pain (VAS), multidimensional scores (Constant score) | 12 mo posttreatment | Diabetes group: 32 shoulders; non-diabetes group: 24 shoulders | High |
| Barbosa et al42 | Cohort study Hospital, UK |
Mixture of conservative or surgical treatment | ROM, multidimensional score (OSS) | 3, 6, 12 mo follow-up | Diabetes group: 46 shoulders; non-diabetes group: 164 shoulders | High |
NOTE. Unless otherwise stated, ROM is measured in degrees, pain is measured on a 0-10 visual analog scale with 10 being the worst pain, Constant scores and ASES scores range from 0-100, OSS scores range from 0-48, and for each score reported, a higher score represents a better patient outcome.
Abbreviations: ASES, American Shoulder and Elbow Surgeons Shoulder Score; MUA, manipulation under anesthesia; OSS, Oxford Shoulder Score; UK, United Kingdom; US, United States; VAS, visual analog scale.
Fig 2.
Bar graph of QUIPS scores for each of the 6 bias domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting.
Results for diabetes as a prognostic factor in frozen shoulder
Studies that analyzed the relationship between the presence of diabetes at baseline with either range of motion, pain, or multidimensional clinical scores are summarized in table 1, and full results for these studies can be found in supplemental appendix S2, tables SB3-SB5 (available online only at http://www.archives-pmr.org/). For all 3 outcome domains, there was very little evidence to suggest that people with diabetes had worse baseline scores (see supplemental tables SB3-SB5, available online only at http://www.archives-pmr.org/).
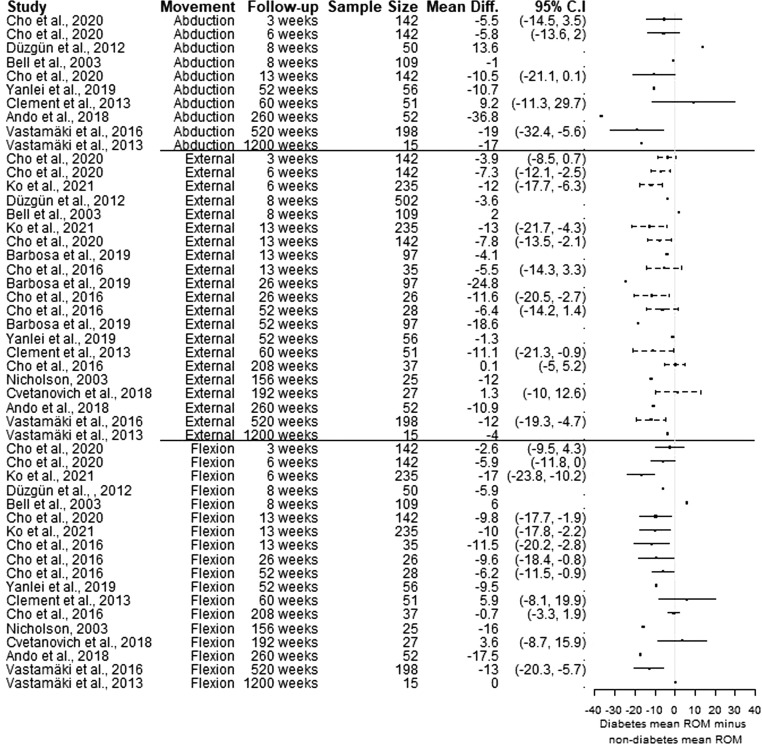
The forest plot of mean differences in ROM (fig 3) shows that generally people with diabetes had worse ROM at follow-up than those without diabetes, although association sizes were inconsistent. The strength of evidence was downgraded in the GRADE framework for the inconsistency in the direction of association because 3 of 13 studies suggested that diabetes is associated with better ROM (table 2). The forest plot contains results on abduction for 673 people from 8 studies, results on external rotation for 1581 people across 13 studies, and results on flexion for 997 people across 12 studies.
Fig 3.
Forest plots of mean differences in ROM scores (degrees) between those with diabetes vs those without diabetes.
Table 2.
Summary of GRADE results
| Direction of Association |
GRADE Factors | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Domain | Number of Participants | Number of Studies | Diabetes Group Generally Had Better Outcomes | Tie in Direction of Association | Diabetes Group Generally Had Worse Outcomes | Phase of Investigation | Study Limitations | Inconsistency | Indirectness | Imprecision | Publication Bias | Effect Size | Exposure-Response Gradient | Overall Certainty in Evidence |
| ROM | 2107 | 13 | 3 | 0 | 10 | Phase 2 | ✕ | ✕ | ✓ | ✕ | ✕ | ✕ | ✕ | Very low |
| Pain | 920 | 10 | 0 | 0 | 10 | Phase 2 | ✕ | ✓ | ✓ | ✕ | ✕ | ✕ | ✕ | Low |
| Multidimensional scores | 1785 | 18 | 2 | 1 | 15 | Phase 2 | ✕ | ✓ | ✓ | ✕ | ✕ | ✓ | ✕ | Moderate |
NOTE. GRADE factor scoring: ✓ = no serious limitations (or present for moderate/large association size, exposure-response gradient); ✕ = serious limitations (or absent for moderate/large effect size, exposure-response gradient). Within the GRADE framework, a study is classed as phase 2 if it is “a cohort study that seeks to confirm independent associations between the prognostic factor and the outcome.”20(p71)
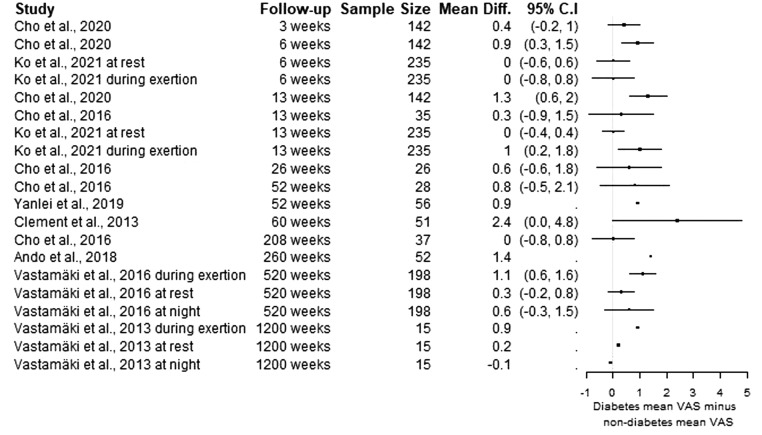
The forest plot of mean differences in pain/visual analog scale scored on a 0-10 scale (fig 4) includes 920 people across 10 studies. The plot suggests a possible association between diabetes and worse pain that is consistent across studies but small in magnitude (see fig 4; table 2). The differences often did not meet the statistical significance threshold defined in the respective article (see supplemental table SB4, available online only at http://www.archives-pmr.org/), which could be partly owing to small association sizes but also owing to small sample sizes.
Fig 4.
Forest plots of mean differences in visual analog scale scores (0-10 scale) between those with diabetes vs those without diabetes.
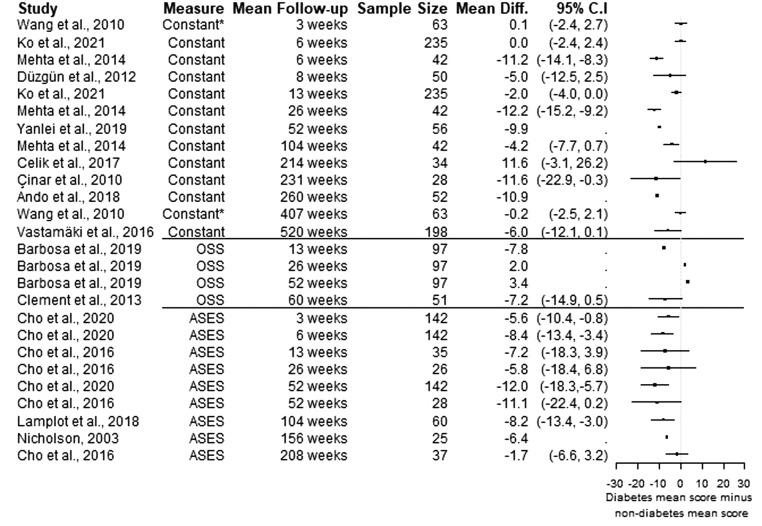
Articles reporting multidimensional clinical scores consistently demonstrated results suggesting that people with diabetes had worse outcomes from frozen shoulder (see supplemental table SB5, available online only at http://www.archives-pmr.org/; fig 5). The forest plot includes 2315 people, including 9 studies based on 758 people measured using Constant scores,43 2 studies of 148 people measured with Oxford Shoulder Scores,44 and 4 studies consisting of a total of 264 people measured with American Shoulder and Elbow Surgeons Shoulder Scores.45 In some smaller cohorts the difference did not meet statistical significance, but, in general, studies showed associations of similar magnitude and direction, in which people with diabetes had worse outcomes (see table 2).
Fig 5.
Forest plots of mean differences in multidimensional clinical scores between those with diabetes vs those without diabetes. Constant scores and American Shoulder and Elbow Surgeons Shoulder Scores are on a 0-100 scale; Oxford Shoulder Scores are scored from 0-48. For each measure, a higher score represents a better patient outcome. *Wang et al33 used an adjusted Constant score, excluding the 25 points for assessment of muscle strength.
For all 3 outcome domains (ROM, pain, multidimensional scores), certainty in evidence was downgraded/not upgraded on the GRADE factors limitations, imprecision, publication bias, and exposure-response gradient (see table 2) with respective reasoning being risk of bias was often high; no rationale for sample sizes was given and some studies produced imprecise estimates; some studies reported associations between diabetes and the outcome without corresponding hypotheses defined at the onset of the study; and diabetes was measured as a binary variable in all studies so there was no exposure-response gradient.
Final GRADE certainty in evidence for diabetes being associated with worse frozen shoulder outcomes was very low for ROM outcome scores, low for pain outcome scores, and moderate for multidimensional clinical outcome scores.
Results from articles reporting less common outcomes can be found in supplemental tables SB1 and SB2(available online only at http://www.archives-pmr.org/). These studies contained 11 results suggesting that people with diabetes had worse outcomes at follow-up, 1 result suggesting that people with diabetes had better outcomes at follow-up, and 3 results where there were no differences in outcomes between those with and without diabetes.
Discussion
This review demonstrates evidence of moderate to very low strength that people with diabetes are likely to experience poorer outcome after a diagnosis of frozen shoulder than those who do not have diabetes. The quality of evidence of diabetes as a prognostic factor in frozen shoulder was very low for ROM outcomes, low for pain outcomes, and moderate for mult-dimensional clinical scores. Through inspection of the forest plots it appears that many studies may have been underpowered, with wide confidence intervals including 0 despite an apparent association. Twenty-one of the 28 studies were at a high risk of bias, meaning that any conclusions based on the results need to be taken with caution. However, a general trend observed suggested that people with diabetes had worse outcomes at follow-up than people without diabetes.
The results of this systematic review are consistent with existing reviews on the topic. Whelton and Peach46 reported the results of 23 studies but lacked any evidence synthesis. The authors of the review concluded that people with diabetes had a more severe and intractable form of the condition. Boutefnouchet et al47 conducted a systematic review comparing the outcomes of patients with and without diabetes after arthroscopic capsular release. Again, the review lacked any evidence synthesis strategy, but after reporting the results of 6 studies, the authors concluded that patients with diabetes have more pain, reduced ROM, and inferior function compared with patients without diabetes. Boutefnouchet et al48 also suggested that the reason patients with diabetes have worse ROM and function could be because they experience more pain and the pain inhibits their ability to do the exercises that are recommended as treatment. The systematic review presented in this article provides a clear evidence synthesis approach using the GRADE framework, along with forest plots to assist data visualization and the use of the QUIPS tool to assess risk of bias.
Study Limitations
A transparent GRADE approach to evidence synthesis was used and raw data were analyzed, using forest plots to help visualize data from primary studies. High variation in definitions of outcome measures and length of follow-up meant that quantitative pooling of the results was not appropriate. The GRADE synthesis method uses vote counting of statistically significant associations in primary studies. A limitation of this approach is that, if interpreted alone, the vote counting of statistically significant associations does not take sample sizes, association sizes, and measures of spread into account.48,49 We attempted to overcome this issue by using forest plots to visualize association size and direction and the precision of estimates, alongside the presentation of raw data and tallies of association direction to score the GRADE factors. The tallies of association direction, along with presentation of raw data, were used to enable the summarization of results measured categorically that could not be included in the forest plot of mean differences, which uses continuously measured outcomes.
Another limitation of the review is that the GRADE synthesis approach relies on the judgment of the reviewer to score the GRADE factors. This approach is therefore less transparent than methods such as meta-analysis. Through the reporting of results in forest plots and supplemental tables, we have attempted to be transparent in showing the data that guided the scoring of GRADE factors and ultimately the conclusions drawn from this review.
A limitation of current available evidence is that many studies were judged to be at a high risk of bias. Few studies adjusted for confounders or compared baseline characteristics between diabetes and non-diabetes groups, and the type of diabetes that participants had was often not reported. Additionally, future research should clarify whether the decision to compare outcomes in people with and without diabetes is based on an a priori hypothesis or an a posteriori hypothesis. Furthermore, patients in most cohorts received treatments that are generally offered in secondary care settings to patients who have not responded to other treatments (pain relief, mobilization, exercise). This means that it is still unclear how diabetes may affect overall prognosis and treatment outcome in most patients with frozen shoulder managed in primary care, who may have a milder form or may be in an earlier phase of the condition.
Conclusions
To conclude, this review provides preliminary evidence to suggest that people with diabetes may have worse outcomes from frozen shoulder, but high-quality studies are required before more firm conclusions can be made. Nevertheless, given the evidence in this review, clinicians should monitor patients with frozen shoulder with diabetes and recommend further treatment if pain or lack of function persists long-term. Further work is warranted to determine whether patients with diabetes do indeed experience a less favorable outcome from frozen shoulder treated with conservative management in primary care, compared with patients who do not have diabetes. Additionally, further research may explore whether diabetes influences the effectiveness of specific treatments for frozen shoulder, which would need to be investigated in appropriately powered randomized controlled trials or using individual participant data from multiple smaller trials.
Supplier
a. R software, version 4.0.2; The R Foundation.
Acknowledgments
We thank the Keele University Research Institute Versus Arthritis systematic review team for their support throughout this project and Elaine Willmore, PhD, for taking time to check the results of our searches for this review. Further thanks are given to Linda Chesterton, PhD, who was involved in the initial conceptualization of this study.
Footnotes
List of abbreviations: GRADE, Grading of Recommendations, Assessment, Development and Evaluations; MUA, manipulation under anesthesia; QUIPS, Quality in Prognostic Factor Studies; ROM, range of motion; VAS, visual analog scale.
Supported by the Versus Arthritis PhD scholarship scheme (grant no. 21899). Claire Burton is funded by an NIHR (National Institute for Health Research) Clinical Lectureship. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care.
PROSPERO Registration No.: CRD42019122963.
Disclosures: None.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2021.100141.
Appendix. Supplementary materials
References
- 1.Bagheri F, Ebrahimzadeh MH, Moradi A, Bidgoli HF. Factors associated with pain, disability and quality of life in patients suffering from frozen shoulder. Arch Bone Jt Surg. 2016;4:243–247. [PMC free article] [PubMed] [Google Scholar]
- 2.Bunker T. Frozen shoulder. J Orthop Trauma. 2011;25:11–18. [Google Scholar]
- 3.Nagy MT, Macfarlane RJ, Khan Y, Waseem M. The frozen shoulder: myths and realities. Open Orthop J. 2013;7:352–355. doi: 10.2174/1874325001307010352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1:180–189. doi: 10.1007/s12178-008-9031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005;331:1453–1456. doi: 10.1136/bmj.331.7530.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manske RC, Prohaska D. Clinical commentary and literature review: diagnosis, conservative and surgical management of adhesive capsulitis. Shoulder Elbow. 2010;2:238–254. [Google Scholar]
- 7.Lewis J. Frozen shoulder contracture syndrome—aetiology, diagnosis and management. Man Ther. 2015;20:2–9. doi: 10.1016/j.math.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow. 2017;9:75–84. doi: 10.1177/1758573216676786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong CK, Levine WN, Deo K. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy. 2017;103:40–47. doi: 10.1016/j.physio.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Uppal HS, Evans JP, Smith C. Frozen shoulder: a systematic review of therapeutic options. World J Orthop. 2015;6:263–268. doi: 10.5312/wjo.v6.i2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maund E, Craig D, Suekarran S. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2012;16:1–264. doi: 10.3310/hta16110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rangan A, Brealey SD, Keding A. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicentre, pragmatic, three-arm, superiority randomised clinical trial. Lancet. 2020;396:977–989. doi: 10.1016/S0140-6736(20)31965-6. [DOI] [PubMed] [Google Scholar]
- 13.Cho C-H, Koo TW, Cho N-S. Demographic and clinical characteristics of primary frozen shoulder in a Korean population. Clin Shoulder Elbow. 2015;18:133–137. [Google Scholar]
- 14.Zreik NH, Malik RA. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6:26–34. doi: 10.11138/mltj/2016.6.1.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Windt DAWM, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hsu C-L, Sheu WH-H. Diabetes and shoulder disorders. J Diabetes Investig. 2016;7:649–651. doi: 10.1111/jdi.12491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158:280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 19.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Available at: https://www.R-project.org/. Accessed June 15, 2021.
- 20.Huguet A, Hayden JA, Stinson J. Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev. 2013;2:71. doi: 10.1186/2046-4053-2-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delgado DA, Lambert BS, Boutris N. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e088. doi: 10.5435/JAAOSGlobal-D-17-00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicholson GP. Arthroscopic capsular release for stiff shoulders: effect of etiology on outcomes. Arthroscopy. 2003;19:40–49. doi: 10.1053/jars.2003.50010. [DOI] [PubMed] [Google Scholar]
- 23.Cvetanovich GL, Leroux TS, Bernardoni ED. Clinical outcomes of arthroscopic 360° capsular release for idiopathic adhesive capsulitis in the lateral decubitus position. Arthroscopy. 2018;34:764–770. doi: 10.1016/j.arthro.2017.08.249. [DOI] [PubMed] [Google Scholar]
- 24.Clement RGE, Ray AG, Davidson C, Robinson CM, Perks FJ. Frozen shoulder: long-term outcome following arthrographic distension. Acta Orthop Belg. 2013;79:368–374. [PubMed] [Google Scholar]
- 25.Bell S, Coghlan J, Richardson M. Hydrodilatation in the management of shoulder capsulitis. Australas Radiol. 2003;47:247–251. doi: 10.1046/j.1440-1673.2003.01171.x. [DOI] [PubMed] [Google Scholar]
- 26.Vastamäki H, Vastamäki M. Motion and pain relief remain 23 years after manipulation under anesthesia for frozen shoulder. Clin Orthop Relat Res. 2013;471:1245–1250. doi: 10.1007/s11999-012-2542-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho C-H, Kim D-H, Lee Y-K. Serial comparison of clinical outcomes after arthroscopic capsular release for refractory frozen shoulder with and without diabetes. Arthroscopy. 2016;32:1515–1520. doi: 10.1016/j.arthro.2016.01.040. [DOI] [PubMed] [Google Scholar]
- 28.Ando A, Hamada J, Hagiwara Y, Sekiguchi T, Koide M, Itoi E. Short-term clinical results of manipulation under ultrasound-guided brachial plexus block in patients with idiopathic frozen shoulder and diabetic secondary frozen shoulder. Open Orthop J. 2018;12:99–104. doi: 10.2174/1874325001812010099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Düzgün İ, Baltacı G, Atay ÖA. Manual therapy is an effective treatment for frozen shoulder in diabetics: an observational study. Jt Dis Relat Surg. 2012;23:94–99. [PubMed] [Google Scholar]
- 30.Vastamäki H, Ristolainen L, Vastamäki M. Range of motion of diabetic frozen shoulder recovers to the contralateral level. J Int Med Res. 2016;44:1191–1199. doi: 10.1177/0300060516675112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehta SS, Singh HP, Pandey R. Comparative outcome of arthroscopic release for frozen shoulder in patients with and without diabetes. Bone Joint J. 2014 doi: 10.1302/0301-620X.96B10.34476. 96-B:1355-8. [DOI] [PubMed] [Google Scholar]
- 32.Çınar M, Akpınar S, Derincek A, Circi E, Uysal M. Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Arch Orthop Trauma Surg. 2010;130:401–406. doi: 10.1007/s00402-009-0900-2. [DOI] [PubMed] [Google Scholar]
- 33.Wang J-P, Huang T-F, Ma H-L, Hung S-C, Chen T-H, Liu C-L. Manipulation under anaesthesia for frozen shoulder in patients with and without non-insulin dependent diabetes mellitus. Int Orthop. 2010;34:1227–1232. doi: 10.1007/s00264-010-0968-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Celik H, Seckin MF, Akcal MA, Kara A, Kilinc BE, Akman S. Mid-long term results of manipulation and arthroscopic release in frozen shoulder. Acta Ortop Bras. 2017;25:270–274. doi: 10.1590/1413-785220172506174033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sinha R, Patel P, Rose N. Analysis of hydrodilatation as part of a combined service for stiff shoulder. Shoulder Elbow. 2017;9:169–177. doi: 10.1177/1758573216687273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lyhne JM, Jacobsen JR, Hansen SJ, Jensen CM, Deutch SR. Diabetic and non-diabetic patients report equal symptom relief after arthroscopic capsular release of frozen shoulder. J Clin Orthop Trauma. 2019;10:261–264. doi: 10.1016/j.jcot.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Theodorides AA, Owen JM, Sayers AE, Woods DA. Factors affecting short- and long-term outcomes of manipulation under anaesthesia in patients with adhesive capsulitis of the shoulder. Shoulder Elbow. 2014;6:245–256. doi: 10.1177/1758573214528155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lamplot JD, Lillegraven O, Brophy RH. Outcomes from conservative treatment of shoulder idiopathic adhesive capsulitis and factors associated with developing contralateral disease. Orthop J Sports Med. 2018;6:1–8. doi: 10.1177/2325967118785169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cho CH, Jin H-J, Kim D-H. Comparison of clinical outcomes between idiopathic frozen shoulder and diabetic frozen shoulder after a single ultrasound-guided intra-articular corticosteroid injection. Diagnostics. 2020;10:370. doi: 10.3390/diagnostics10060370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ko YW, Park JH, Youn S-M, Rhee YG, Rhee S-M. Effects of comorbidities on the outcomes of manipulation under anesthesia for primary stiff shoulder. J Shoulder Elbow Surg. 2021;30:e482–e492. doi: 10.1016/j.jse.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 41.Yanlei GL, Keong MW, Tjoen DLT. Do diabetic patients have different outcomes after arthroscopic capsular release for frozen shoulder? J Orthop. 2019;16:211–215. doi: 10.1016/j.jor.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barbosa F, Swamy G, Salem H. Chronic adhesive capsulitis (frozen shoulder): comparative outcomes of treatment in patients with diabetes and obesity. J Clin Orthop Trauma. 2019;10:265–268. doi: 10.1016/j.jcot.2018.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 44.Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford Shoulder Score revisited. Arch Orthop Trauma Surg. 2009;129:119–123. doi: 10.1007/s00402-007-0549-7. [DOI] [PubMed] [Google Scholar]
- 45.Richards RR, An K-N, Bigliani LU. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 46.Whelton C, Peach CA. Review of diabetic frozen shoulder. Eur J Orthop Surg Traumatol. 2018;28:363–371. doi: 10.1007/s00590-017-2068-8. [DOI] [PubMed] [Google Scholar]
- 47.Boutefnouchet T, Jordan R, Bhabra G, ModiC Saithna A. Comparison of outcomes following arthroscopic capsular release foridiopathic, diabetic and secondary shoulder adhesive capsulitis: a systematic review. Orthop Traumatol. 2019;105:839–846. doi: 10.1016/j.otsr.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 48.Wasserstein RL, Lazar NA. The ASA statement on P-values: context, process, and purpose. Am Stat. 2016;70:129–133. [Google Scholar]
- 49.Greenland S, Senn SJ, Rothman KJ. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31:337–350. doi: 10.1007/s10654-016-0149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.