Abstract
Background:
Integrated behavioral health models have been proposed as care delivery approaches to mitigate mental health disparities in primary care settings. However, these models have not yet been widely adopted or evaluated in pediatric oncology medical homes.
Methods:
We conducted a retrospective cohort study of 394 children with newly diagnosed cancer at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center (DF/BCH) from April 2013 to January 2017. Baseline sociodemographic characteristics and psychiatry utilization outcomes at 12-months following diagnosis were abstracted from the medical record. The severity of household material hardship (HMH), a concrete poverty exposure, at diagnosis and race/ethnicity were characterized by parent-report using the Psychosocial Assessment Tool 2.0 (PAT). Associations between sociodemographic characteristics and receipt of psychiatry consultation were assessed with multivariable logistic regression models.
Results:
Among 394 children, 29% received a psychiatric consultation within 12-months post-diagnosis. Of these, 88% received a new psychiatric diagnosis, 76% received a psychopharmacologic recommendation, and 62% received a new behavioral intervention recommendation. In multivariable logistic regression adjusting for age, cancer diagnosis, and PAT total score, there was no statistically significant association between HMH severity or household income and psychiatry utilization. Children who identified as racial/ethnic minorities were significantly less likely to receive a psychiatry consultation (OR=0.48, 95% CI: 0.27-0.84).
Conclusions:
In a pediatric oncology medical home with an integrated behavioral health model, socioeconomic status was not associated with disparate psychiatry utilization. However, there remained a profound racial/ethnic disparity in psychiatry utilization highlighting the need for additional research and care delivery intervention.
Keywords: Healthcare disparities, pediatric oncology, health services research, mental health, psychiatry, minority health
Introduction
Children and adolescents of lower socioeconomic status, as well as those of racial/ethnic minority backgrounds, experience worse mental health outcomes compared to wealthier White children.1, 2 These disparities are likely driven by interrelated mechanisms at the household (e.g. housing and food insecurity, chronic toxic stress for both the child and parent), neighborhood (e.g. increased exposure to violence and substance abuse), and societal (e.g. decreased access to well-funded school systems and mental health resources) levels.3-5 In the United States, structural racism has led to generations of systemic disadvantage in education, employment, and housing opportunities for families of racial and ethnic minority groups. The resulting profound racial and ethnic disparities in income, wealth, and poverty likely further predisposes minority families to increased psychiatric morbidity and decreased access to care.6 Primary care settings have led early efforts to mitigate these disparities through the implementation of integrated behavioral health models.7 These types of models can range in their care delivery from coordination (offering facilitated referral or collaborative consultation calls to patients and providers to off-site services) to co-location (located in the same physical space but largely operating as separate entities) to integration (generally on-site with close collaboration and communication as part of one treatment team).8-10 However, this integrated care delivery model has not been as rapidly expanded into pediatric oncology settings, which frequently function as the medical homes for children with cancer and where oncologists routinely assume primary care for these patients during active cancer treatment and early survivorship.
Innovations to address equity in this context are critical to consider in conjunction with widely accepted evidence-based standards for psychosocial care of children with cancer and their families, including a call for universal early and ongoing assessment of mental health needs and access to appropriate interventions.11 There are additionally broader implications for adult providers who will care for the >80% of these patients who become long-term survivors.12
In this study, we analyzed sociodemographic factors and psychiatry utilization in a large pediatric oncology referral center that includes an integrated behavioral health model with two child psychiatrists dedicated to pediatric cancer patients. Our objectives were to: (1) describe the psychiatry healthcare utilization in the first year of cancer treatment within this integrated model and (2) identify associations between sociodemographic factors and psychiatry utilization.
Methods
Study Population
The study population was derived from a previously published cohort of children with newly diagnosed cancer at Dana-Farber/Boston Children’s Cancer Center and Blood Disorders Center (DF/BCH).13 The analytic cohort included 394 children (<21 years of age) diagnosed with cancer from April 2013 – January 2017 with planned receipt of chemotherapy at DF/BCH and available baseline household material hardship (HMH) data. HMH is a concrete poverty exposure including domains of unmet basic needs like food, housing, utilities, and transportation.14 Detailed inclusion criteria and methodology regarding collection of these data were previously published.13 This study was approved by the Dana-Farber Cancer Institute Institutional Review Board.
Integrated Behavioral Health Model
DF/BCH serves as a subspecialty medical home for children with cancer with a fully integrated multidisciplinary psychosocial team. There are two child psychiatrists providing the equivalent of one full-time clinical position for all psychiatric care of DF/BCH pediatric oncology patients. Other integrated team members include 5 psychologists, and 6 social workers, and a child life specialist. These clinicians are co-located within the inpatient and outpatient oncology services. During the time period of this study, the standard of care was that every patient scheduled to receive chemotherapy in our center was assigned a psychologist or social worker as part of their disease-specific treatment team. Caregivers were given universal psychosocial risk screening (Psychosocial Assessment Tool 2.0 (PAT))15 and the psychosocial clinician followed patients and families based on clinical need. Psychiatry consultation could be initiated by the patient/family, oncology medical team or psychosocial clinician. Psychosocial and oncology clinicians shared the same electronic medical record and were in regular communication through inpatient rounds, outpatient clinic visits, email, and in-person liaison activities.
Data Source
Sociodemographic and medical characteristics for the cohort were previously abstracted from completed pencil-paper PAT surveys which had been scanned into the electronic medical record.13 For this analysis, additional structured medical chart abstraction from the electronic medical record was performed by a trained research assistant and duplicated by a second research assistant for every tenth subject for psychiatry utilization data elements at 12-months post-diagnosis and PAT total score. Inconsistencies were reconciled with the senior investigator (KB). These data were collected and stored in a secure REDCap database.
Study Endpoints
The primary outcome for this study was psychiatry utilization as measured by receipt of any psychiatric consultation (yes/no) within 12-months from cancer diagnosis. Among those patients who received a psychiatric consultation, secondary outcomes included new psychiatric Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnosis (yes/no), new behavioral intervention recommendation (yes/no), and new psychopharmacologic medication prescription (yes/no). Behavioral interventions were defined as discrete recommendations (e.g. cognitive behavioral therapy, behavioral reward chart for pill-taking, structured child life support for daily schedule and routine) beyond existing standard of care psychosocial support.
Covariates
HMH severity and race/ethnicity were the primary sociodemographic exposures of interest. Both of these variables were ascertained from the completed PAT surveys. Caregivers responded to the PAT question of self-identified combined race/ethnicity “Is your child (check all boxes that apply): Hispanic, Asian, Black/African American, White, Other.” Race/ethnicity was categorized as a binary variable (White, non-Hispanic vs. Other) given small numbers in individual categories that precluded analyses of individual racial or ethnic self-identified groups. If caregivers selected another race/ethnicity in addition to White, they were categorized as multi-racial and subsequently grouped with Other for the analysis. Children were characterized as living in a home with HMH if caregivers responded to the PAT question “In what areas are you having money problems (check all the boxes that apply)?” with affirmative responses in the domains of food (“buying food”), housing (“paying rent/mortgage”), utilities (“phone/heat/light bills”), or transportation (“car costs”). HMH was categorized as a binary variable by severity (0-1 domains vs. ≥2 domains) for all analyses. The assessment of HMH by severity in terms of domains affected is consistent with prior work in both general pediatrics and pediatric oncology.16, 17 Additional patient characteristics included sex, age at diagnosis in years, health insurance (Medicaid only vs. other), and cancer diagnosis (hematologic malignancy vs. solid/brain tumor). The PAT total score was utilized as a measure of psychosocial risk, with higher total scores indicating increased psychosocial risk.15 The PAT question used to assess HMH is not one of the questions that contributes to calculation of the total PAT score. As previously published, during this time period, it was standard of care to offer the PAT to all English- or Spanish-speaking families of a child with a new oncologic diagnosis at DF/BCH.13 Caregiver characteristics included highest level of educational attainment (bachelor’s or greater vs. high school or less). Finally, household characteristics included primary language (English vs. other), single parent household (yes/no), and household income as percent of federal poverty level (FPL) (>100% FPL vs. ≤100% FPL).18
Statistical Analysis
Patient, caregiver and household characteristics at time of diagnosis were summarized using descriptive statistics. Categorical variables were summarized using frequencies and proportions; continuous variables were summarized using means and standard deviations (SD), or medians and inter-quartile ranges (IQR). Psychiatry utilization outcomes 12-months from diagnosis were also summarized using descriptive statistics. The proportion of patients receiving psychiatry consultation was compared between families from racial/ethnic minority backgrounds vs. those who identified as non-Hispanic White with Fisher’s exact test. Univariate logistic regression models were used to test the association between sociodemographic variables and the primary outcome. A multivariable logistic regression model with backward elimination using p-value > 0.05 was performed including age at diagnosis, cancer diagnosis, PAT total score, race/ethnicity, and HMH severity. The multivariable analysis was restricted to the subset of patients with known race/ethnicity data. The Benjamani-Hochberg method19 was used to account for multiple hypothesis testing. Unadjusted p-values were reported; tests with a calculated false discovery rate (FDR) < 10% were considered statistically significant after adjustment for multiple hypothesis testing. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
Patient, caregiver, and household characteristics
Baseline characteristics for the analytic cohort (N=394) are displayed in Table 1. There were slightly more males (59.1%), and the median age of diagnosis was 7.5 years (IQR=3.4-4.5). More than half (51.5%) were diagnosed with a hematologic malignancy. Of the 368 patients with known race/ethnicity data, nearly 30% self-identified as belonging to a racial/ethnic minority group. More than 10% had Medicaid-only insurance (13.8%), belonged to a single-parent household (10.1%), and reported household income ≤100% FPL (13.8%). Over a fifth of the cohort (22.3%) reported HMH in 2 or more domains.
TABLE 1.
Patient, caregiver and household characteristics at time of diagnosis (N=394)
| Frequency (%) | |
|---|---|
| Patient characteristics | |
| Sex | |
| Male | 233/394 (59.1) |
| Female | 161/394 (40.9) |
| Age at diagnosis in years, median (IQR1) | 7.46 (3.41-4.51) |
| N=394 | |
| PAT Total score, Mean (SD) | 0.86 (0.68) |
| N=394 | |
| Race and Ethnicity | |
| African-American | 9/368 (2.4) |
| Asian | 25/368 (6.8) |
| Hispanic | 29/368 (7.9) |
| White | 259/368 (70.4) |
| Other | 11/368 (3.0) |
| Multiple race and/or ethnicities selected | 35/368 (9.5) |
| Cancer Diagnosis | |
| Hematologic Malignancy | 203/394 (51.5) |
| Solid/Brain Tumor | 191/394 (48.5) |
| Health Insurance | |
| Medicaid only | 53/385 (13.8) |
| Other | 332/385 (86.2) |
| Caregiver characteristics | |
| PAT Respondent’s Relationship to Child | |
| Mother | 284/394 (72.1) |
| Father | 103/394 (26.1) |
| Other | 7/394 (1.8) |
| Highest level of educational attainment | |
| High school or less | 115/389 (29.6) |
| Associate/Bachelors | 165/389 (42.4) |
| Masters/Doctorate | 109/389 (28.0) |
| Household characteristics | |
| Primary language | |
| English | 352/374 (94.1) |
| Other | 22/374 (5.9) |
| Single Parent Household | |
| Yes | 39/388 (10.1) |
| No | 349/388 (89.9) |
| Household income as percent of FPL | |
| ≤100% FPL | 49/354 (13.8) |
| >100% FPL | 305/354 (86.2) |
| HMH by severity | |
| 0-1 domain | 306/394 (77.7) |
| ≥2 domains | 88/394 (22.3) |
Abbreviations: IQR = interquartile range; PAT = Psychosocial Assessment Tool 2.0; SD = standard deviation; FPL = federal poverty level; HMH = household material hardship
Psychiatry utilization
At 12-months from diagnosis, 113 patients (29%) had received a psychiatric consultation. Among those who received a psychiatric consultation, 88% received a new DSM psychiatric diagnosis, 76% received a new psychopharmacologic prescription, and 62% received a recommendation for a new behavioral intervention.
Associations between sociodemographic factors and psychiatry utilization
In univariate analyses (Table 1), patients who identified as racial/ethnic minorities (odds ratio [OR] = 0.53; 95% confidence interval [CI] = 0.31-0.90; p=0.02) were significantly less likely to have a psychiatry consultation. Figure 1 displays the corresponding proportions with p-value from Fisher’s exact test comparison. HMH severity was not associated with psychiatry consultation. Older age at diagnosis, hematologic malignancy diagnosis, and higher PAT total score were associated with greater odds of psychiatry consultation.
Figure 1.
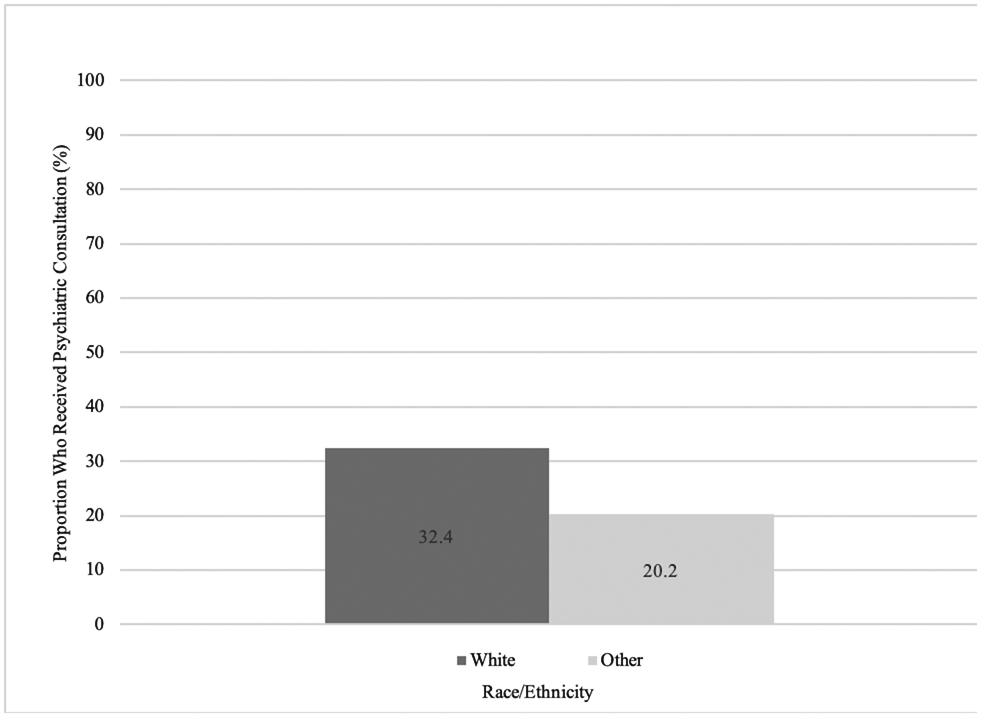
Proportion of patients who received psychiatric consultation stratified by race/ethnicity (N=368) and compared with Fisher’s exact test
In multivariable analysis (Table 2), patients who identified as racial/ethnic minorities (adjusted OR=0.48; 95% CI=0.27-0.84; p=0.01) were significantly less likely to receive a psychiatry consultation, adjusting for the effects of age, diagnosis, and PAT total score. Older age at diagnosis, higher PAT total score, and hematologic malignancy remained associated with a higher likelihood of psychiatry consultation in the multivariable model. HMH severity was not significantly associated with psychiatry consultation.
TABLE 2.
Multivariable model examining association of psychiatric consultation at 12-months from diagnosis with patient, household, and disease characteristics1
| Variable2 | Adjusted OR3 (95% CI)4 | Adjusted p-value |
|---|---|---|
| Race/Ethnicity | 0.01 | |
| White | 1 (Ref) | |
| Other | 0.48 (0.27-0.84) | |
| Age at diagnosis (per 1-year increase) | 1.06 (1.02-1.11) | 0.003 |
| Diagnosis | <0.001 | |
| Hematologic Malignancy | 1 (Ref) | |
| Solid/Brain Tumor | 0.35 (0.22-0.58) | |
| PAT total score (per 1-point increase) | 1.5 (1.06-2.11) | 0.02 |
N=368 as this analysis was restricted to the subset of patients with known race/ethnicity data
HMH by severity removed from model given p>0.05
Abbreviations: OR = odds ratio; PAT = Psychosocial Assessment Tool 2.0
Adjusted odds ratios (OR) and 95% confidence intervals of receiving psychiatric consultation at 12-months from diagnosis
Discussion
One-third of children with cancer receiving care at a large pediatric oncology referral center with an integrated behavioral health model received a psychiatry consultation during the first 12-months post-diagnosis. Despite this strikingly high utilization of psychiatry services overall, children who identified as racial/ethnic minorities were significantly less likely to receive a psychiatry consultation compared to non-Hispanic White children, even after adjusting for child and treatment factors. We notably did not find any clear associations between poverty exposures (including HMH severity and household income) and receipt of psychiatry consultation. The majority of patients who received a psychiatric consultation received a new DSM diagnosis, a new psychopharmacologic prescription, and/or a new behavioral health recommendation.
Our study interestingly did not find any significant association between household-level socioeconomic status, as measured by both parent-reported income and HMH severity, and psychiatry utilization. This cautiously suggests that an integrated behavioral health model with dedicated psychiatric care embedded within the medical home may help mitigate poverty-related barriers to accessing mental health care. Similar integrated care models have been advocated as promising strategies in the primary care setting for improving access and outcomes.7, 20 Our data provide evidence that these recommendations may in fact accomplish such aims and importantly need to be considered in oncology where subspecialists provide the primary medical home for children with cancer.
However, our data also suggest that these models by themselves are insufficient to overcome previously identified racial and ethnic disparities in mental health outcomes. Children who identified as racial and ethnic minorities in our cohort were less likely to access psychiatric care despite an overwhelming amount of literature demonstrating an increased prevalence of psychiatric morbidity in minority populations.2 This pattern of decreased access is worrisome for exacerbating existing disparities as psychiatric conditions are potentially left undiagnosed and unmanaged. Specifically, our data recapitulate identified trends in the literature including decreased treatment for major depression in minority adolescents, decreased Medicaid expenditures on psychotropic medications specifically for African-American and Latino maltreated children compared to their non-Hispanic White counterparts, and decreased use of outpatient mental health services by African-American and Asian American/Pacific Islander at-risk youths.21-23 Our data are also consistent with a smaller exploratory analysis of children with acute lymphoblastic leukemia treated at our center, which similarly demonstrated decreased psychiatry consultation for children of racial and ethnic minority groups.24 Possible explanations for the observed racial and ethnic disparity in psychiatry utilization within an integrated model of care include both provider and family-level factors. First, both unconscious bias and/or explicit discrimination at the provider level may result in misinterpretation of child symptoms or inferior communication with parents of racial/ethnic minority status leading to fewer psychiatry referrals.25 Second, families who identify as racial/ethnic minorities may fear increased stigma for seeking mental healthcare resulting in either a hesitancy to report worrisome symptoms or behaviors, or discomfort in accepting a recommendation for psychiatry referral.26, 27 Finally, the structural racism that has historically disenfranchised families who identify as racial/ethnic minorities may correspond with decreased comfort or success in advocating for psychiatry referral on behalf of their children as compared to non-Hispanic White parents. Systemic and standardized screening that occurs at multiple timepoints in the cancer trajectory as recommended in the Psychosocial Standards of Care for pediatric oncology may mitigate some of these barriers.11 However, next steps must include understanding referral patterns as well as patterns of caregiver/patient uptake of psychiatric referral to identify areas for multi-level interventions to address drivers of this disparity.
Patients with hematologic malignancy were significantly more likely to receive psychiatry consultation, an observation likely driven by differences in chemotherapy drug-exposures. Specifically, treatment for acute lymphoblastic leukemia—the most common hematologic malignancy—includes prolonged exposure to high-dose steroids with known psychiatric adverse effects.28 It is striking that a majority of children who received a psychiatry consult went on to receive DSM diagnoses, formal behavioral intervention recommendations, and psychopharmacologic prescriptions. These findings underscore the need for mental health expertise and collaboration in this population, particularly in light of prior literature suggesting suboptimal management practices when pediatric oncologists prescribe selective serotonin reuptake inhibitors without psychiatry consultation.29
Our results must be interpreted in the context of certain limitations. This is a single center study at a large urban referral center, thus our findings may not necessarily be representative on a national level. The availability of dedicated psychiatry is uncommon in pediatric oncology settings with only 19% of centers reporting access to a psychiatrist as part of their multidisciplinary psychosocial team.30 However, the fact that disparities exist even in our highly resourced setting should emphasize the magnitude of this association. It should also be noted that our primary outcome in this study was a documented visit with a consulting pediatric psychiatrist—not referral to pediatric psychiatry for which data were not available—thus we are unable to answer the question of where along the care continuum our observed racial/ethnic disparities arise. We do not have the specific reasons for consultation because these were not systematically documented in the EMR during this time period. It is additionally possible that patients received psychiatry consultations outside the DF/BCH system (e.g. from primary care referrals) although this seems less likely in the context of our integrated model. We were limited by small numbers within each racial and ethnic group and so a priori chose to use a combined binary race/ethnicity variable. This approach precludes more nuanced understanding of differences between self-identified racial and ethnic groups, which are likely to differ on the basis of culture, language and experiences of discrimination. Future investigations must leverage more diverse cohorts to investigate such potential differences.
Conclusion
A model of integrated behavioral and psychiatric care in a pediatric oncology medical home may help mitigate socioeconomic but not racial disparities in mental health utilization. The persistence of racial/ethnic disparities in this healthcare delivery model at a highly resourced center is striking and highlights the significant need to investigate drivers of racial and ethnic disparities in the context of universal access in pediatric oncology settings. Our study findings should prompt future research into both the specific barriers that prevent equitable care as well as potential interventions to proactively improve psychosocial support for underserved groups.
Supplementary Material
Acknowledgements:
We thank Giacomo Gotti for his assistance in chart abstraction of the data presented in this manuscript.
Study Funding:
This study was partially supported by the Academic Pediatric Association (APA) Resident Investigator Award awarded to Dr. Zheng. Dr. Bona is supported by the National Cancer Institute at the National Institutes of Health grant number K07CA211847. Dr. Van Litsenburg is supported by a Young Investigator Grant from the Dutch Cancer Society, grant number KWF10706.
Abbreviations
- DF/BCH
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center
- HMH
Household material hardship
- PAT
Psychosocial Assessment Tool 2.0
Footnotes
Conflict of interest disclosures (includes financial disclosures): Hasan Al-Sayegh received funding from GlaxoSmithKline, Agios, Rocket Pharma, Aileron Therapeutics, and Bristol-Myers Squibb. The other authors have no conflicts of interest relevant to the article to disclose.
Data Availability Statement:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. [DOI] [PubMed] [Google Scholar]
- 2.Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. 2010;19(4):759–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. [DOI] [PubMed] [Google Scholar]
- 4.Murali V, Oyebode F. Poverty, social inequality and mental health. Advances in psychiatric treatment. 2004;10(3):216–224. [Google Scholar]
- 5.Dashiff C, DiMicco W, Myers B, Sheppard K. Poverty and adolescent mental health. J Child Adolesc Psychiatr Nurs. 2009;22(1):23–32. [DOI] [PubMed] [Google Scholar]
- 6.McKernan S-M, Ratcliffe C, Steuerle CE, Zhang S. Less than equal: Racial disparities in wealth accumulation. Urban Institute; Washington, DC; 2013. [Google Scholar]
- 7.Hodgkinson S, Godoy L, Beers LS, Lewin A. Improving mental health access for low-income children and families in the primary care setting. Pediatrics. 2017;139(1):e20151175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Njoroge WF, Hostutler CA, Schwartz BS, Mautone JA. Integrated Behavioral Health in Pediatric Primary Care. Curr Psychiatry Rep. 2016;18(12):106. [DOI] [PubMed] [Google Scholar]
- 9.Lauerer JA, Marenakos KG, Gaffney K, Ketron C, Huncik K. Integrating behavioral health in the pediatric medical home. J Child Adolesc Psychiatr Nurs. 2018;31(1):39–42. [DOI] [PubMed] [Google Scholar]
- 10.Abuse S. Mental Health Services Administration (SAMHSA)-Health Resources and Services Administration (HRSA) Center for Integrated Health Solutions (CIHS).(2013). CIHS’Standard Framework for Levels of Integrated Healthcare. [Google Scholar]
- 11.Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the Psychosocial Care of Children With Cancer and Their Families: An Introduction to the Special Issue. Pediatr Blood Cancer. 2015;62 Suppl 5(Suppl 5):S419–S424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howlader N, Noone A, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2018, National Cancer Institute. Bethesda, MD. 2018. [Google Scholar]
- 13.Zheng DJ, Shyr D, Ma C, Muriel AC, Wolfe J, Bona K. Feasibility of systematic poverty screening in a pediatric oncology referral center. Pediatr Blood Cancer. 2018;65(12):e27380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beverly SG. Measures of material hardship: Rationale and recommendations. Journal of Poverty. 2001;5(1):23–41. [Google Scholar]
- 15.Pai AL, Patiño-Fernández AM, McSherry M, et al. The Psychosocial Assessment Tool (PAT2.0): psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. J Pediatr Psychol. 2008;33(1):50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics. 2010;125(5):e1115–e1123. [DOI] [PubMed] [Google Scholar]
- 17.Bona K, London WB, Guo D, Frank DA, Wolfe J. Trajectory of Material Hardship and Income Poverty in Families of Children Undergoing Chemotherapy: A Prospective Cohort Study. Pediatr Blood Cancer. 2016;63(1):105–111. [DOI] [PubMed] [Google Scholar]
- 18.Services USDoHH. Prior HHS Poverty Guidelines and Federal Register References. Accessed May 10, 2021. https://aspe.hhs.gov/prior-hhs-poverty-guidelines-and-federal-register-references
- 19.Benjamini YH, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B. 1995;57(1):289–300. [Google Scholar]
- 20.Wissow LS, van Ginneken N, Chandna J, Rahman A. Integrating Children's Mental Health into Primary Care. Pediatr Clin North Am. 2016;63(1):97–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. 2011;50(2):160–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. Am J Psychiatry. 2005;162(7):1336–1343. [DOI] [PubMed] [Google Scholar]
- 23.Raghavan R, Brown DS, Allaire BT, Garfield LD, Ross RE, Snowden LR. Racial/ethnic differences in Medicaid expenditures on psychotropic medications among maltreated children. Child Abuse Negl. 2014;38(6):1002–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muriel AC, Burgers DE, Treyball AN, Vrooman LM, Adolf E, Samsel C. Risk factors for steroid-induced affective disorder in children with leukemia. Pediatr Blood Cancer. 2021;68(5):e28847. [DOI] [PubMed] [Google Scholar]
- 25.Schnierle J, Christian-Brathwaite N, Louisias M. Implicit Bias: What Every Pediatrician Should Know About the Effect of Bias on Health and Future Directions. Curr Probl Pediatr Adolesc Health Care. 2019;49(2):34–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conner KO, Koeske G, Brown C. Racial differences in attitudes toward professional mental health treatment: the mediating effect of stigma. J Gerontol Soc Work. 2009;52(7):695–712. [DOI] [PubMed] [Google Scholar]
- 27.Rao D, Feinglass J, Corrigan P. Racial and ethnic disparities in mental illness stigma. J Nerv Ment Dis. 2007;195(12):1020–1023. [DOI] [PubMed] [Google Scholar]
- 28.Staub Y, Suga Y, Ikawa Y, et al. Detailed assessment and risk factor analysis of corticosteroid-induced psychiatric disorders in pediatric, adolescent, and young adult patients undergoing induction or consolidation therapy for hematologic malignancy. J Oncol Pharm Pract. 2020;26(5):1041–1051. [DOI] [PubMed] [Google Scholar]
- 29.Phipps S, Buckholdt KE, Fernandez L, et al. Pediatric oncologists' practices of prescribing selective serotonin reuptake inhibitors (SSRIs) for children and adolescents with cancer: a multi-site study. Pediatr Blood Cancer. 2012;58(2):210–215. [DOI] [PubMed] [Google Scholar]
- 30.Scialla MA, Canter KS, Chen FF, et al. Implementing the psychosocial standards in pediatric cancer: Current staffing and services available. Pediatr Blood Cancer. 2017;64(11): 10.1002/pbc.26634. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


