Abstract
Background
Empathy is the capacity to understand and resonate with the experiences of other people. Patient enablement is the degree to which a patient feels strengthened in terms of being able to deal with, understand and manage their disease.
Methods
Secondary cross-sectional analysis of existing data from 2 independent datasets (456 primary health care patients), with the application of two validated questionnaires, Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE) and Patient Enablement Instrument (PEI).
Objective
Evaluate medical empathy and patients’ enablement after consultation with their family doctors and to verify if there was an association between these two concepts.
Results
The median value of JSPPPE-VP score was 6.60 (interquartile range 1.00) and of PEI/ICC score was of 1.83 (interquartile range 0.67). Regarding empathy (JSPPPE-VP), patients taking chronic medication had a slight but significantly higher median score than patients not taking them (6.70 versus 6.60, P = 0.049), although regression modelling did not confirm any relevant predictor of JSPPPE-VP score. Regarding enablement (PEI/ICC), we found significantly higher scores on younger patients, as well as, on more educated and professionally active ones (P < 0.001). Multivariable linear regression and Poisson regression modelling confirmed such variables as statistically significant potential predictors.
Conclusions
A significant positive association was found between empathy score (JSPPPE-VP) and enablement score (PEI/ICC), when adjusted to sociodemographic cofactors. On this linear regression model, age category and educational level were also significantly associated with empathy score, with the same pattern found on bivariate analysis.
Keywords: Empathy, enabling factors, family practice, patient-centred medicine, physician–patient relationship, primary care
Key messages.
Positive association between empathy score and enablement score.
Age and educational level were also significantly associated with empathy score.
More research focussing on empathy and enablement in primary care is needed.
Introduction
Empathy is conceptually difficult to define given the inherent multidimensionality, but in this context, we can describe it as the capacity to understand and resonate with the experiences of other people (1), giving it a ‘predominantly cognitive attribute (rather than emotional) that involves understanding (rather than feeling) the patient’s experiences, concerns and perspectives, combined with the ability to communicate this understanding and the intention to help’ (2). Empathy is distinct from sympathy, which involves feeling the patient’s suffering and pain, and which in excess will lead to damage to the doctor–patient relationship and worse medical performance (3,4). The importance of empathy in the practice of medicine has been studied in recent years, and it was shown to have a positive impact for both patients and doctors, facilitating the effectiveness of treatments (4). To assess empathy, the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE) was developed, it is an instrument validated and used in international studies (2,5), translated and validated in Portugal (6,7).
Patient empowerment is a process of recognizing, promoting and enhancing patient’s abilities to meet their own needs, solve their own health problems and mobilize the necessary resources to feel in control of their health (8). For this paper, we consider patient enablement as the degree to which a patient feels strengthened, after a consultation, in terms of being able to deal with, understand and manage their disease (9,10). Higher enablement after the consultation has been linked to better clinical results, which may be influenced by several factors, such as empathy, and others inherent to the patient himself (age, gender, economic status and multimorbidity) or consultation (duration and continuity of care) (9,11). There are many empowerment measures, but the Patient Enablement Instrument (PEI) is a validated and internationally used instrument in primary care setting and measures the aspects of perceived control over illness (8,12,13). The PEI is translated and validated to Portuguese (14,15).
Patient’s capacity can be increased through proper enablement by the doctor, through empathy and familiarity with the person, with adequate communication during the consultation and increased time (2,16).
Due to the importance of the former mentioned concepts in GP/FM, the aim of this study is to describe medical empathy and enablement of the patients after a consultation with their family doctors and to verify if there is a correlation between doctor empathy and patient enablement.
Materials and methods
Study design, setting and sample
The current study is a secondary cross-sectional analysis of existing data from 2 independent datasets (456 primary health care patients). The first dataset was collected between July and August 2016 and consists of a representative sample of 172 patients from an urban academic primary health care unit located in the central region of Portugal that has enrolled 8730 patients (margin of error of ±7.39 percentage points at the 95% confidence level of 8000 different patients consulted on average in 1 year) (17). The second dataset was collected between September and December 2017 and consists of a representative sample of 284 patients from an urban academic primary health care unit located in the northern region of Portugal that has enrolled 10 013 patients (margin of error of ±4.93 percentage points at the 95% confidence level of 1010 consultations, on average per month) (18). In both samples, the most conservative scenario (a proportion of 50%) was considered.
The questionnaire
The same survey was used for the collection of both datasets, applied after the patient’s routine consultation with his/her family physician. It consisted of sociodemographic and clinical data (age group, gender, education and professional activity and the taking of chronic medication), JSPPPE-VP and PEI/ICC.
The JSPPPE-VP translated and validated to Portuguese language (6,7), with a reliability that varied between 0.737 and 1.000 and Cronbach’s alpha between 0.806 and 0.877 (7). It is a 5-item instrument answered on a 7-point Likert-type scale (7) (e.g. ‘My doctor can view things from my perspective (see things as I see them)’ (1 = Strongly Disagree, 7 = Strongly Agree)). It was used as a continuous scale.
The PEI/ICC, also translated and validated to Portuguese (14,15), presenting good internal consistency (Cronbach’s alpha >0.8) and reliability 0.85 (15). Consists of six questions designed to assess the enablement that the patient obtains for his health and life in general, after a consultation with the family physician (14). It was used as a continuous scale ranging from 1 point (worse case) to 3 points (best case) (e.g. ‘As a result of your visit with the doctor today, do you feel you are able to manage your illness much better (3 points), better (2 point), or the same or less (1 points)’).
Ethical approval
Ethical board approval was obtained for the collection of both datasets. For the first dataset from the University of Coimbra and from the Northern Region Health Administration for the second dataset. All research participants gave informed consent prior to their involvement in the study, and the anonymity of the information was assured.
Statistical analysis
All data were analysed with IBM SPSS Statistics (version 24.0)© and STATA Statistical Package© software and alpha level was set at 0.05. Methods of descriptive statistics and inferential analysis were used, and normality was accessed to allow the use of parametric approaches where necessary.
Linear regression models were used to determine the most relevant predictors of score at JSPPPE-VP and PEI/ICC questionnaires, according to sociodemographic variables, as well as to establish the association between JSPPPE-VP and PEI/ICC. To build the model we first performed bivariate associations to identify significant variables to be included at a 0.25 alpha level (19). Then, a step-up and step-down selection approach was used to set the best fit with a P value <0.05. Generalized linear models were performed with the same predictors, to confirm the best fitness of the linear regression (20).
Results
Data from 456 participants were collected. Most were female, aged between 36 and 65 years. More than 80% were on chronic medication. More than half had only a basic educational level and were professionally inactive.
Table 1 presents baseline characteristics collected according to sociodemographic variables and the scores obtained at JSPPPE-VP and PEI/ICC questionnaires. The median value of JSPPPE-VP score was 6.60 (interquartile range 1.00) and of PEI/ICC score was 1.83 (interquartile range 0.67). Regarding empathy (JSPPPE-VP), patients taking chronic medication had a slight but significantly higher median score than patients not taking any (6.70 versus 6.60; Mann–Whitney test, P = 0.049), although regression modelling did not confirm any relevant predictor of JSPPPE-VP score. Regarding enablement (PEI/ICC), we found significantly higher scores on younger patients, as well as on more educated and professionally active ones (Mann–Whitney and Kruskal–Wallis tests, P values under 0.001). Multivariable linear regression and Poisson regression modelling confirmed such variables as statistically significant potential predictors.
Table 1.
Full data from demographic and clinical variables collected from all participants and comparisons according to the major outcome variables (significant results highlighted)
| Baseline variable [median (±IQR) or %] | Total | JSPPPE-VP scorea | PEI/ICC scorea | ||
|---|---|---|---|---|---|
| Median | P value | Median | P value | ||
| No. of total participants | 456 | 6.60(±1.00) | — | 1.83(±0.67) | — |
| Age category | |||||
| Under 36 years | 22.6 | 6.60(±1.20) | 0.223‡ | 2.00(±0.50) | <0.001‡ |
| Between 36 and 65 years | 47.4 | 6.80(±1.00) | 1.83(±0.67) | ||
| Over 65 years | 30.0 | 6.60(±1.10) | 1.67(±0.83) | ||
| Men | 37.9 | 6.80(±1.00) | 0.198† | 1.83(±0.50) | 0.292† |
| Women | 62.1 | 6.60(±1.20) | 1.83(±0.67) | ||
| With chronic medication | 80.7 | 6.70(±1.00) | 0.049† | 1.83(±0.67) | 0.094† |
| Without chronic medication | 19.3 | 6.60(±1.35) | 2.00(±1.00) | ||
| Educational level | 0.330‡ | <0.001‡ | |||
| None (only reading/writing skills) | 3.5 | 6.60(±1.00) | 1.58(±0.92) | ||
| Basic | 50.2 | 6.80(±1.00) | 1.67(±0.75) | ||
| Highschool | 26.8 | 6.40(±1.20) | 2.00(±0.50) | ||
| Academic | 19.5 | 6.60(±1.20) | 2.00(±0.50) | ||
| Professionally active | 48.2 | 6.80(±1.00) | 0.105† | 2.00(±0.67) | 0.001† |
| Professionally inactiveb | 51.8 | 6.60(±1.20) | 1.83(±0.67) | ||
| Professional sector | 0.223‡ | <0.001‡ | |||
| Primary/Production | 7.0 | 7.00(±1.00) | 1.75(±0.96) | ||
| Secondary/Transformation | 5.3 | 6.70(±0.95) | 2.00(±0.33) | ||
| Tertiary/Services | 36.0 | 6.80(±1.00) | 2.00(±0.50) | ||
| Unemployed | 11.6 | 6.20(±1.90) | 1.83(±0.67) | ||
| Retired | 34.4 | 6.60(±1.00) | 1.67(±0.75) | ||
| Student | 5.7 | 6.70(±0.85) | 2.00(±0.33) | ||
IQR, interquartile range.
aOutcome data presented as values considering only the count of participants within each of the predictor variables.
bIncludes students, unemployed and retired.
†Mann–Whitney test.
‡Kruskal–Wallis test.
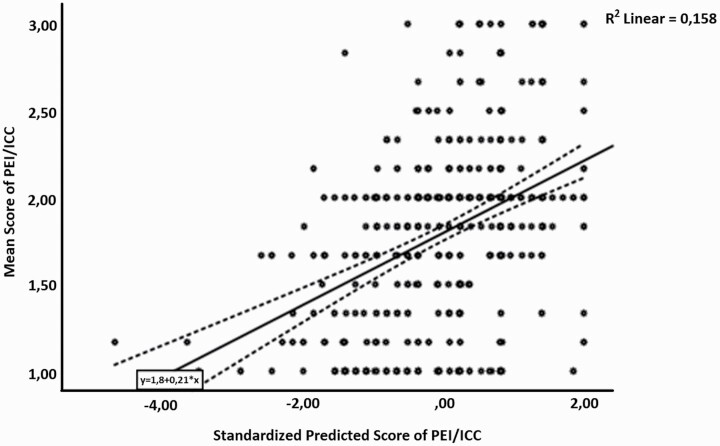
A significant positive association was found between empathy score (JSPPPE-VP) and enablement score (PEI/ICC), when adjusted to sociodemographic cofactors (with an increase of 0.155 point in PEI/ICC for each unit of increase in JSPPPE-VP score; P < 0.001; regression model R2: 0.158; adjusted to 0.153). On this linear regression model, age category and educational level were also significantly associated with empathy score, with the same pattern found on bivariate analysis (Table 2 and Fig. 1). A Poisson regression model confirmed the same findings. Figure 2 represents PEI/ICC values varying across JSPPPE-VP range.
Table 2.
Full data from predictors identified with statistical significance on multivariate analysis according to the outcome variable PEI/ICC score
| Outcome—PEI/ICC score (linear regression) | |||||
|---|---|---|---|---|---|
| Predictor variables in the model | Coef. | Std. error | P value | VIF | t value |
| JSPPPE-VP score | 0.155 | 0.023 | <0.001 | 1.005 | 6.679 |
| Age category | −0.124 | 0.033 | <0.001 | 1.126 | −3.718 |
| Educational level | 0.121 | 0.029 | <0.001 | 1.126 | 4.178 |
| (Constant) | 0.770 | 0.189 | <0.001 | — | 4.085 |
R2: 0.158 (adjusted to 0.153). A Poisson regression was performed with the same predictors, to confirm the best fitness of the linear regression (adapted from McCullagh and Nelder (20)). Excluded variables from this model (due to non-significance) were: gender, being professionally active and taking chronic medication. VIF, variance inflation factor for collinearity.
Figure 1.
Correlation between predicted values of multivariate regression model (that includes JSPPPE score) and PEI/ICC score. Dashed line—mean 95% confidence interval.
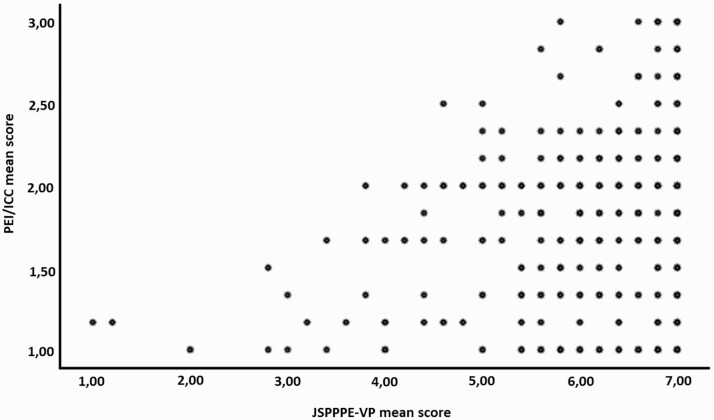
Figure 2.
PEI/ICC mean values according to JSPPPE-VP range.
Discussion
Strengths of the study
Multicentric original study using two adapted and validated scales for the Portuguese population. Assessment of an important area of the General Practice/Family Medicine environment such as empathy and enablement, two measurable characteristics of the patient–doctor relationship.
Statement of overall findings
The study results showed that most patients perceived a good empathy with the doctor and felt they had a medium-low level of enablement. No other study reporting the relation between global patients’ perceived empathy and enablement were yet found, for the Portuguese context, in the literature search. These results show that Portuguese GPs seem to be empathic, but that patients do not feel enough enabled.
Patient’s sociodemographic characteristic did not seem to significantly change their perceived medical empathy. To our knowledge, our study is the first Portuguese one to evaluate any differences in the patient perceived medical empathy with patients’ characteristics. On the other hand, some studies (21,22) found an association between patient perceived medical empathy and some physicians’ characteristics, namely exerting medical speciality and gender. Therefore, is patient’s perception of medical empathy more related to doctor-related factors than to patient-related ones? It is possible that factors related to the patient will influence the perception of medical empathy, namely feeling that problems have been solved.
According to patient’s enablement, we found that it decreases with ageing. A previous study (23) showed a decrease in enablement with age in male patients and no difference in female patients, but another one (24) showed an increase in enablement with ageing. A possible explanation for enablement’s decrease with age could be that physical and cognitive decline with ageing could turn patients more passive in consultation. Younger patients may wish a more active role in consultations having more control over their health care and demanding more information (25).
No difference in the patient enablement with the patient’s gender was found and this is in line with the literature (23,24) perhaps due to national and global effort to reduce gender inequality, which argues that doctors should give the same opportunities to both genders treating them just the same.
Patient’s enablement augments with the increase of educational level. Our findings are in line with the literature (23). As reason for this one can hypothesize that patients feel more able of controlling their health as they know more. On the other hand, GPs could be more likely to adopt a paternalistic posture towards patients with lower education and higher age does not enable them.
Professionally active patients demonstrated higher enablement levels than those not professionally active ones and this relationship has not yet been studied. Professionally active patients wish to participate on the decisions about their health care. Inactive patients may tend to rely more on their doctors’ decisions about health care.
Higher perceived empathy is associated with increased enablement. In the literature, there are other studies with a positive relationship between perceived medical empathy and patient enablement (16). However, there are also studies, in oncology setting, that did not find any relationship between both variables (26). Perhaps patients who realize their doctor is empathic are more likely to follow recommendations and feel more comfortable discussing with her/him about health and asking for more control over own health care, an ambience that the oncology one does not facilitate.
Our logistic regression had a low R2 and a wide dispersion. This suggests that there are other factors influencing the patient enablement level. Some proposed factors in the literature are emotional distress, quality of life, multimorbidity, the reason for encounter with the doctor and longer and better knowing of the doctor (9,23,24), even though the enablement characteristics in consultation could stand against what patients would expect. In fact, General Practitioner/Family Doctors tend to oppose what society wants.
Overall, empathy and enablement seem somehow linked and dissociated. In fact, empathy has to do with relationship and enablement with knowledge, ability and will to do.
Limitations of the study
There are some limitations that need to be considered for this study.
Firstly, this is a cross-sectional study and so no causal relationship can be proven.
Secondly, the short number of collected variables can have prevented the detection of more robust predictors for medical empathy and patient enablement.
Future studies must address other variables that may predict the relationship between empathy and enablement, like multimorbidity, chronic medications the patient is on, length of years of the patient–doctor relationship and doctor characteristics.
Conclusions
A significant positive association was found between empathy score (JSPPPE-VP) and enablement score (PEI/ICC), when adjusted to sociodemographic cofactors. On this linear regression model, age category and educational level were also significantly associated with empathy score, with the same pattern found on bivariate analysis. A Poisson regression model confirmed the same findings.
Declaration
Funding: this work was not funded.
Ethical approval: as this cohort study was based on existing data, being a secondary research-based analysis, ethical medical approval was not required. However, the original studies were approved by ethics committees.
Conflicts of interest: there are no conflicts of interests of any of the authors of this article.
References
- 1.Lockwood PL. The anatomy of empathy: vicarious experience and disorders of social cognition. Behav Brain Res 2016; 311: 255–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hojat M, Louis DZ, Maxwell Ket al. . Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ 2010; 1: 83–7. [Google Scholar]
- 3.Hojat M, Vergare MJ, Maxwell Ket al. . The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med 2009; 84(9): 1182–91. [DOI] [PubMed] [Google Scholar]
- 4.Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci 2014; 8: 457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hojat M, Mangione S, Kane GC, Gonnella JS. Relationships between scores of the Jefferson Scale of Physician Empathy (JSPE) and the Interpersonal Reactivity Index (IRI). Med Teach 2005; 27(7): 625–8. [DOI] [PubMed] [Google Scholar]
- 6.Loureiro J, Gonçalves-Pereira M, Trancas B, Caldas-de-Almeida JM, Castro-Caldas A. [Empathy in the doctor-patient relationship as viewed by first-year medical students: data on validity and sensibility to change of the Jefferson Measure in Portugal]. Acta Med Port 2011; 24 (suppl 2): 431–42. [PubMed] [Google Scholar]
- 7.Domingues AC, Santiago LM, Rodrigues ARet al. . Cross-cultural adaptation and validation of the Jefferson Scale of Patient’s Perceptions of Physician Empathy (JSPPPE) for the Portuguese population. Patient Prefer Adherence 2019; 13: 1145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerezo PG, Juvé-Udina ME, Delgado-Hito P. Concepts and measures of patient empowerment: a comprehensive review. Rev Esc Enferm USP 2016; 50(4): 667–74. [DOI] [PubMed] [Google Scholar]
- 9.Mercer SW, Jani BD, Maxwell M, Wong SY, Watt GC. Patient enablement requires physician empathy: a cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract 2012; 13: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reis AF, Santiago LM, Botas P. Patient-centered medicine and enablement in the general practice/family medicine setting. Rev ADSO 2015; 3(5): 19–32. [Google Scholar]
- 11.Mercer SW, Reilly D, Watt GC. The importance of empathy in the enablement of patients attending the Glasgow Homoeopathic Hospital. Br J Gen Pract 2002; 52(484): 901–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998; 15(2): 165–71. [DOI] [PubMed] [Google Scholar]
- 13.McKinstry B, Colthart I, Walker J. Can doctors predict patients’ satisfaction and enablement? A cross-sectional observational study. Fam Pract 2006; 23(2): 240–5. [DOI] [PubMed] [Google Scholar]
- 14.Pintalhão I, Botas P, Pereira C, Santiago LM. Portuguese translation of the patient enablement instrument. Rev ADSO 2013; 2: 18–22. [Google Scholar]
- 15.Remelhe M, Teixeira PM, Lopes I, Silva L, Correia de Sousa J. The modified patient enablement instrument: a Portuguese cross-cultural adaptation, validity and reliability study. NPJ Prim Care Respir Med 2017; 27: 16087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract 2013; 63(606): e76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romano JP, Santiago LM, Saraiva CB.. Medical empathy and patient training in consultation. Master’s Thesis [handle: 10316/82489]. Coimbra, Portugal: University of Coimbra, 2017. (in Portuguese). [Google Scholar]
- 18.Lourenço JA, Simões JA, Santiago LM.. Medical empathy and the training of consultants in General and Family Medicine. Master’s Thesis [handle: 10400.6/8634]. Covilhã, Portugal: University of Beira Interior, 2019. (in Portuguese). [Google Scholar]
- 19.Hosmer D, Lemeshow S.. Applied Logistic Regression. 2nd edn. New York, NY: John Wiley & Sons, Inc, 2000. [Google Scholar]
- 20.McCullagh P, Nelder JA.. Generalized Linear Models. 2nd edn. London, UK: Chapman and Hall, 1989. [Google Scholar]
- 21.Chaitoff A, Sun B, Windover Aet al.. Associations between physician empathy, physician characteristics, and standardized measures of patient experience. Acad Med 2017; 92(10): 1464–71. [DOI] [PubMed] [Google Scholar]
- 22.Kortlever JTP, Ottenhoff JSE, Vagner GA, Ring D, Reichel LM. Visit duration does not correlate with perceived physician empathy. J Bone Joint Surg Am 2019; 101(4): 296–301. [DOI] [PubMed] [Google Scholar]
- 23.Ozvacić Adzić Z, Katić M, Kern Jet al. . Patient, physician, and practice characteristics related to patient enablement in general practice in Croatia: cross-sectional survey study. Croat Med J 2008; 49: 813–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howie JG, Heaney DJ, Maxwell Met al. . Quality at general practice consultations: cross sectional survey. BMJ 1999; 319(7212): 738–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brom L, Hopmans W, Pasman HRet al. . Congruence between patients’ preferred and perceived participation in medical decision-making: a review of the literature. BMC Med Inform Decis Mak 2014; 14: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lelorain S, Brédart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology 2012; 21(12): 1255–64. [DOI] [PubMed] [Google Scholar]