Abstract
We use 7 waves of the Health and Retirement Study and construct a social vulnerability index (SVI) for elderly U.S. Americans (born 1913–1966). We show that the SVI is mildly larger for men than for women and increases in age from above age 60 onwards for both genders. Social vulnerability of men (but not of women) is lower in the West and Midwest than in other regions and higher income mildly reduces the SVI for men (but not for women). In cohort analysis we find an increase of the SVI for individuals born in the late 1940s or later, which is, however, statistically significant only for women. In order to investigate the nexus between social vulnerability and aging, we construct a frailty index from the same data. We find that socially vulnerable persons display more health deficits at any age. Using the initial SVI (at first interview) we find that social vulnerability exerts a significant impact on subsequent accumulation of health deficits, which is of about the same size for men and women. A one standard deviation increase in the initial SVI leads to a 20 percent increase of the frailty index at any age.
Keywords: Health, Aging, Social vulnerability, Social capital, Frailty index, United States
Highlights
-
•
Panel study of social vulnerability and aging in the U.S.
-
•
Social vulnerability index (SVI) increases for women born after 1940.
-
•
Strong impact of initial SVI on subsequent accumulation of health deficits.
1. Introduction
Humans are a social species. We evolved in an environment where social interaction and cooperation was essential for survival. While modes of production and cooperation changed tremendously from hunter gatherer times, social factors such as social networks, social capital, or social isolation continue to affect our wellbeing, health, and mortality (e.g. Andrew et al., 2008; Hawkley et al., 2010; House et al., 1988; Snyder-Macker et al., 2020; Wallace et al., 2015). The literature has identified three different pathways. Social networks and social control influence (un-) healthy behavior like exercising or food, alcohol, and drug consumption (e.g. Akerlind & Hoernquist, 1992; Christakis & Fowler, 2007; Hawkley et al., 2009; Umberson et al., 2010; Strulik, 2014, 2020). There is also mounting evidence for a direct physiological channel. In particular, perceived loneliness has been shown to affect health and aging through increasing stress, higher blood pressure, poorer sleep, higher cortisol response to awakening, and greater activation of the sympathetic adrenomedullary system (Hawkley and Cacioppo, 2007; Hawkley and Cacioppo, 2010). According to a frequently cited study, the odds ratio of all-cause mortality is higher for social isolation than for smoking (House, 1988). Moreover, for frail individuals, social support allows to maintain activities of daily living at home without use of professional care, it delays nursing home entry (Bonsang, 2009; Reeves et al., 2014; Van Houtven & Norton, 2004), and may through this channel be conducive to well-being and slower aging. For elderly and frail individuals there exists potentially a feedback mechanism from aging to the loss of social connections because existing relationships with peers and partners are increasingly eliminated by death and because health limitations constrain the maintenance of existing relationships and the creation of new ones (Rosso et al., 2013).
Many studies have documented a deleterious impact of loneliness on morbidity and mortality (for reviews see Hawkley & Cacioppo, 2010; Perissinotto et al., 2012, Holt-Lunstad et al., 2015). Loneliness, defined as perceived social isolation, has been found to increase in old age, at least from a certain age onwards (Hawkley et al., 2019) and a common belief is that, in rich individualistic societies, later born cohorts are more prone to loneliness such that there may be even a ‘loneliness epidemic’ (BBC, 2018; HRSA, 2019; The Economist, 2018). This belief is seemingly supported by the transition towards more individualistic societies (Santos et al., 2017), the erosion of social capital since the 1970s in all kinds of dimensions (Putnam, 2000), and the observation of an increasing trend of living alone in old age because of smaller family sizes, increased divorce rates, and greater geographical distance between family members (Dahlberg et al., 2018; Dykstra, 2009).
The existence of a loneliness epidemic, however, is not corroborated by scientific evidence. Longitudinal studies in rich individualistic societies typically find no trend of loneliness among the elderly (Dahlberg et al., 2018; Dykstra, 2009; Hackley et al., 2019). The disagreement between public perception and evidence could be explained by the difference between objective and subjective (i.e. perceived) social isolation. For example, a survey among elderly U.S. Americans found that the vast majority (85 percent of those age 75 and older) prefers to stay in their own home rather than to move in with family or a nursing home (AARP, 2005). The seemingly conflicting observations could thus be understood as a rising trend in objective isolation that is not expressed in subjective loneliness, perhaps because of adaptation of later born cohorts to a generally lower level of social contacts in old age. These observations, however, do not necessarily imply that there is no need for concern since a meta-analytic review reported similar odds ratio of mortality for subjective and objective measures of social isolation (Holt-Lunstad et al., 2015).
A related literature investigates the relationship between alternative measures of social capital (connections to other people) and health and mortality. Notably, Sirven and Debrand (2012) showed, for a panel of European countries, a negative association between participation in social activities and several health impairments with (Granger-) causality running in both directions (see also Leone & Hessel, 2016). Muennig et al. (2013) investigated the association between different measures of social capital and laboratory biomarkers and found that some measures (such as church attendance and belonging to clubs) were significantly associated with the combined expression of all biomarkers and predictive for subsequent death of all causes and diagnosed cardiovascular disease. Liu et al. (2016) used surname frequency as an instrument for family networks and argued in favor of a strong causal impact of this dimension of social capital on individual health status. For a recent review of the literature on social capital and health see Rodgers et al. (2019).
In this study, we focus on an encompassing measure of an individual's social environment, the social vulnerability index, and investigate its association with health and (biological) aging, measured by the frailty index. Both indices share a similar methodology but the frailty index is by far the more popular metric since it is well established in the gerontological literature (see e.g. Rockwood & Mitnitski, 2007, for a review). We thus first briefly introduce related literature on the frailty index before we turn to the introduction of the SVI.
The frailty index measures the number of health deficits of an individual at a given age relative to the number of potential health deficits that he or she may have. Health deficits include mild ones as well as serious disabilities. The exact choice of deficits is not crucial provided that sufficiently many indicators are present in the index (for methodological background see Rockwood & Mitnitski, 2006; Searle et al., 2008). An explanation for this remarkable feature is that health deficits are interdependent (Rutenberg et al., 2018). For example, hypertension is associated with the risk of stroke, heart diseases, kidney diseases, dementia, and problems of walking fast and sleeping well. This means that if a particular health deficit is missing from the list, its effect (on, for example, probability of death) is taken up by a combination of other health deficits. The quality of the deficit index is mostly demonstrated by its predictive power for death at the individual level, and for mortality at the group level (Rockwood & Mitnitski, 2007) as well as for the risk of institutionalization in nursing homes and becoming a disability insurance recipient (Blodgett et al., 2016; Hosseini et al., 2019).
It has been found that health deficits are accumulated exponentially with increasing age, akin to the Gompertz (1825) law of mortality. On average, the frailty index increases by 3–5 percent from one birthday to the next (Abeliansky et al., 2020; Abeliansky & Strulik, 2018a; Mitnitski et al, 2002a, 2016). The exponential association of health deficits with age implies that the development of new health deficits depends positively on the number of already present health deficits. It provides a formal expression of the generality of biological aging understood as “intrinsic, cumulative, progressive, and deleterious loss of function that eventually culminates in death” (Arking, 2006). The frailty index and its exponential increase with age has a micro-foundation in the reliability theory of human aging (Gavrilov and Gavrilova, 1991) and in network theories of human aging (Rutenberg et al., 2018). Several studies have shown that women, at given age, display more health deficits than men (see Gordon et al., 2017; for a review and meta study) and that men develop new health deficits faster than women (Abeliansky et al., 2020; Abeliansky and Strulik, 2018; Lachmann et al., 2019; Mitnitski et al., 2002). We therefore followed the literature and carried out the analysis separately for men and women.
The SVI takes up the idea of the frailty index by constructing a high-dimensional unweighted index that encompasses a wide range of factors that describe the complexity of a person's social situation. The methodology of the SVI has been developed in Andrew and Keefe (2015) and, in connection with the frailty index, in Andrew et al. (2008) and Wallace et al. (2015). Social vulnerability is understood as “the degree to which a person's overall social situation leaves them susceptible to health problems” (Andrew and Keefe, 2015). As mentioned above, there is an extensive literature on the relationship between health and instruments measuring social support, social capital, social networks, loneliness, and more. The SVI contributes to this literature by applying the frailty-index methodology; that is by constructing a holistic measure of social vulnerability that is generalizable between data sets (Wallace et al., 2015). An advantage of the SVI over one- or low dimensional measures of social circumstance is that the additive nature of the index takes the substitutability between items into account. Consider, for example, three elderly people living alone with no family support. The first person compensates with a rich network of friends and community engagement, the second person has few personal contacts but frequent exchanges with friends by phone and email, the third person is really separated from family and friends. The SVI allows us to assign different values of social vulnerability to these people. The high dimensionality of the index is the key feature that provides the robustness of results and the comparability of the index across studies. It implies that it does not really matter which items are exactly included in the index, as long as there are sufficiently many items. Individual items can be removed from the index without any significant impact on the estimated relationships (see below and Appendix Table A9-A10 and A.17) while at the same time the index as a whole is a powerful predictor of health and aging. Andrew and Keefe constructed several low-dimensional indicators of social circumstance (using principal component analysis), found them to be of relatively low explanatory power, and advocated a high-dimensional SVI as a suitable metric of social vulnerability. They conclude that “social vulnerability is a global construct that may be best understood as a whole, and that it may not lend itself well to being parsed into small numbers of defined bits for separate analysis of individual social factors, or dimensions, in isolation” (Andrew and Keefe, 2008, p. 11).1
A few studies have jointly used the SVI and the frailty index. These studies focused on the risk of mortality as the dependent variable and employed the frailty index as an independent variable, additional to the SVI, and other controls. It has been found that the SVI is positively associated with mortality in samples of elderly Canadians (Andrew et al., 2008; Andrew and Keefe, 2015) and Europeans (Wallace et al., 2015). The latter study also found a positive association of the SVI with disability. Additionally, Andrew et al. (2008) found the SVI to be higher for women than men at any age and Andrew et al. (2008) and Wallace et al. (2015) found the SVI to be increasing in chronological age.
In this study we compute the SVI and the frailty index for U.S. Americans and exploit the panel feature of the Health and Retirement Study (HRS) data. In the first part of the econometric analysis, we consider the SVI as the dependent variable. Here we expect new insights on the impact of (chronological) age on social vulnerability at the individual level and of year of birth on social vulnerability at the cohort level. In the second part of the analysis, we turn to the frailty index as the dependent variable. We expect to gain insights on the impact of social vulnerability on physiological aging at the individual level and at the cohort level.
2. Data description
For the analysis, we used the Health and Retirement Study RAND HRS Longitudinal File 2016 (V1), which contains information from the core and exit interviews of the HRS. The data were compiled by the RAND Center of the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration (HRS, 2019). Further information related to the sampling of the HRS is provided in Appendix Section A.1. In 2004 the HRS first introduced the questionnaire on psycho-social lifestyle statistics, from which we draw information to construct the Social Vulnerability Index. We merged the data retrieved from this questionnaire (“Psychosocial and Lifestyle Questionnaire 2006–2016”) with those from the Health and Retirement Study RAND HRS Longitudinal File 2016 (V1). Panel data are available at four year intervals for psycho-social information and at two-year intervals for health deficits. Since we have information from 2004 until 2016, the dataset contains 7 waves. We considered respondents aged 50 and above at the time of their first interview. Because a significant share of the oldest old individuals show “super healthy” characteristics, we focused on individuals aged 90 and below to avoid selection effects. Nevertheless, to assess the robustness of the results we changed the 90 cutoff to 85, we removed completely the cutoff, and we eliminated the first and last wave (in different instances).
A frailty index for each individual has been created, following the methodology developed by Mitnitski et al. (2001). We considered symptoms, signs, and disease classifications to construct the index. A summary of all 38 deficits considered is given in the Appendix Table A1. We coded multilevel deficits using a mapping to the Likert scale in the interval 0–1. In case of missing data for an individual, we constructed the respective index based on the available information on potential deficits (i.e. if for a particular individual data were not available for x potential deficits, the sum of the observed deficits was divided by 38 − x). From the surveyed individuals, we kept only those with information on at least 30 health deficits. Due to missing values in the creation of the indices or because of the lack of sufficient deficits to reach the 30-item minimum, we lost 20% of the observations of the initial dataset. We dropped observations where the region of residence and/or the place of birth was missing, as well as observations for individuals born outside the U.S. By excluding migrants we focus on a more homogenous group of individuals exposed to the U.S. American health environment for their whole life.2
Table 1.
Summary statistics.
| Mean | Std.Dev | Obs | Minimum | Maximum | |
|---|---|---|---|---|---|
| Frailty Index | 0.2182 | 0.1557 | 37,731 | 0 | 0.9341 |
| log Frailty Index | −1.8191 | 0.8643 | 37,669 | −6.4998 | −0.06814 |
| Social Vulnerability Index | 0.3092 | 0.1022 | 37,731 | 0.03285 | 0.8380 |
| Age | 68.338 | 9.7184 | 37,731 | 50 | 90 |
| Year of birth | 1941.5 | 10.131 | 37,731 | 1913 | 1966 |
| Household Income | 68,875 | 129733 | 37,731 | 0 | 13,569,370 |
| log income | 10.654 | 1.0053 | 37,529 | −1.8326 | 16.423 |
| Females | |||||
| Frailty Index | 0.2305 | 0.1604 | 21,977 | 0 | 0.9341 |
| log Frailty Index | −1.7621 | 0.8726 | 21,938 | −6.4998 | −0.06814 |
| Social Vulnerability Index | 0.3020 | 0.1037 | 21,977 | 0.03285 | 0.8369 |
| Age | 68.224 | 9.7956 | 21,977 | 50 | 90 |
| Year of birth | 1941.6 | 10.195 | 21,977 | 1913 | 1966 |
| Household Income | 61,902 | 102800 | 21,977 | 0 | 5,278,874 |
| log income | 10.530 | 1.0214 | 21,856 | −1.8326 | 15.479 |
| Males | |||||
| Frailty Index | 0.2011 | 0.1471 | 15,754 | 0 | 0.9306 |
| log Frailty Index | −1.8987 | 0.8461 | 15,731 | −5.3471 | −0.07197 |
| Social Vulnerability Index | 0.3192 | 0.09914 | 15,754 | 0.03536 | 0.8380 |
| Age | 68.497 | 9.6078 | 15,754 | 50 | 90 |
| Year of birth | 1941.3 | 10.038 | 15,754 | 1914 | 1966 |
| Household Income | 78,602 | 159392 | 15,754 | 0 | 13,569,370 |
| log income | 10.827 | 0.9562 | 15,673 | 1.3863 | 16.423 |
The construction of the SVI follows the methodology of the frailty index. The indices are calculated as the ratio of the number of social deficits a respondent suffers from to the number of potential social deficits. As items for the social deficits we considered variables that are in accordance with the seminal study of Andrew et al. (2008). The selection of items was guided by the objective to include a broad representation of factors that influence and describe an individual's social circumstances. These factors were based on previous studies which have suggested they are relevant, for example as indicators of social isolation (e.g. how much do you feel isolated from others?), social support (e.g. how often do you meet/speak on the phone with friends/relatives/children?), activities of the daily life (how often do you work on a hobby/project?), social engagement (e.g. how often do you go to a sport, social, or other club?), and subjective wellbeing (e.g. how satisfied are you with your life?). We collected objective measures of income and living circumstances (lives with a partner, number of household members) as separate control variables. Table A2 in the Appendix provides the list of all items considered in the SVI. As a sensitivity check, we also report results for a modified index created by removing one item at a time from the original index.
Table 2.
Social vulnerability.
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| Age | −0.0121∗∗∗ | −0.0123∗∗∗ | −0.0123∗∗∗ | −0.0125∗∗∗ | −0.0125∗∗∗ | −0.0125∗∗∗ | −0.0125∗∗∗ | −0.0125∗∗∗ |
| (0.00154) | (0.00154) | (0.00156) | (0.00157) | (0.00151) | (0.00151) | (0.00152) | (0.00150) | |
| Age2 | 0.000101∗∗∗ | 0.000102∗∗∗ | 0.000102∗∗∗ | 0.000103∗∗∗ | 0.000103∗∗∗ | 0.000102∗∗∗ | 0.000103∗∗∗ | 0.000103∗∗∗ |
| (0.0000115) | (0.0000115) | (0.0000117) | (0.0000117) | (0.0000109) | (0.0000109) | (0.0000109) | (0.0000108) | |
| log Income | −0.00126 | −0.00129 | −0.00187∗∗ | −0.00183∗∗ | ||||
| (0.000973) | (0.000967) | (0.000905) | (0.000903) | |||||
| Midwest | −0.0143 | −0.0137 | −0.0136 | −0.0134 | −0.0333∗∗∗ | −0.0356∗∗∗ | −0.0333∗∗∗ | −0.0359∗∗∗ |
| (0.0160) | (0.0159) | (0.0159) | (0.0160) | (0.0112) | (0.0115) | (0.0112) | (0.0115) | |
| South | −0.00735 | −0.00722 | −0.00693 | −0.00672 | −0.0132 | −0.0127 | −0.0132 | −0.0126 |
| (0.0113) | (0.0113) | (0.0113) | (0.0112) | (0.00879) | (0.00887) | (0.00879) | (0.00887) | |
| West | −0.0123 | −0.0121 | −0.0119 | −0.0118 | −0.0265∗∗ | −0.0267∗∗ | −0.0264∗∗ | −0.0268∗∗ |
| (0.0152) | (0.0152) | (0.0152) | (0.0152) | (0.0122) | (0.0123) | (0.0122) | (0.0123) | |
| Constant |
0.659∗∗∗ | 0.678∗∗∗ | 0.421∗∗∗ | 0.912∗∗∗ | 0.703∗∗∗ | 0.723∗∗∗ | 0.438∗∗∗ | 0.771∗∗∗ |
| (0.0520) |
(0.0493) |
(0.0916) |
(0.0808) |
(0.0532) |
(0.0547) |
(0.152) |
(0.145) |
|
| Sample | Women | Women | Women | Women | Men | Men | Men | Men |
| Method | FE | FE | Mundlak | Mundlak | FE | FE | Mundlak | Mundlak |
| N | 21977 | 21856 | 21977 | 21856 | 15754 | 15673 | 15754 | 15673 |
Standard errors clustered at the year of birth-level are in parentheses. ∗p < 0.10, ∗∗p < 0.05, ∗∗∗p < 0.01.
For regional effects we exploited the feature that the HRS data is categorized by four main U.S. American regions: Northeast, Midwest, South, and West. We also collected information on income. The variable “Household Income” reflects total income for the last calendar year and consists of the sum of respondent and spouse earnings, pensions and annuities, social security disability benefits, social security retirement benefits, unemployment and workers compensation, other government transfers, household capital income, and other income. If the individual does not live with a partner, household income is individual income. In the regressions we include the logarithm of income since income is approximately log-normally distributed and marginal returns of income on frailty and SVI are potentially declining with increasing income. We also report results for two alternative income measures, which include income from other household members.
Our dataset includes only those individuals who participated in the social survey. It contains information for 17,602 respondents, out of which 7526 are male and 10,076 are female. Aggregated over all seven waves this leads to 37,731 observations in total. Summary statistics are shown in Table 1. Men and women are on average 68 years old and born in mid 1941. Men are on average less frail, richer, and (mildly) more socially vulnerable than women.
3. Social vulnerability
In this section we analyze the potential drivers of the social vulnerability index (measured at the individual level) using the following model:
| (1) |
where i represents the individual, w the wave, age is chronological age at the time of the interview, and income is household income as defined above; yob is a set of dummy indicators, which take the value of one when t equals the year of birth of individual i, the β5s are the associated year-of-birth fixed effects, T is the last year of birth in the respective sample, b is the baseline year; region is a set of dummy indicators, which take the value of one when r equals the region of residence of individual i at the time of the interview, is the baseline region, and ε is the error term. We estimate Equation (1) separately for men and women, given that the subsequent aging analysis will be conducted by gender.3
We estimate Equation (1) firstly using a fixed effects model and then with the Mundlak approach. The first method accounts for unobserved heterogeneity at the individual level, while the second one allows to obtain cohort- and regional effects on social vulnerability. When using individual fixed effects (FE), we assume that the error term ϵiw is composed of μi and uiw, where the unobserved individual effects μi are correlated with the regressors (the age-invariant variables are now dropped since they are perfectly collinear with the fixed effects) and uiw is the idiosyncratic error term. The Mundlak (1978) approach assumes that the μi's (still unobserved) are not correlated with the regressors (i.e. the assumption in a random effects model) and we add the individual-time means of the time-changing variables. The Mundlak model is essentially a random effects estimator with the addition of the individual-means of the time-changing covariates. Mundlak (1978) has shown that the estimates of the time changing variables in this approach should be comparable to those of a fixed effects estimator.
Results are shown in Table 2. Columns (1)–(2) and (5)–(6) show the results from the fixed effects regressions. The positive coefficient on age and the negative coefficient for age squared are both statistically significantly different from zero for women and men, indicating that SVI is u-shaped in age. In order to better assess the quantitative importance of age, the age-SVI curve implied by the point estimates for women (represented by red solid lines) and men (represented by dashed blue lines) are shown in Fig. 1. For both genders, the SVI declines mildly until about age 61 and then it steeply increases in age. At any age, the SVI of men is somewhat larger with a mild convergence of the SVI as individuals grow older. For both genders, the SVI is about one standard deviation (0.1) larger at age 90 than at age 60.
Fig. 1.

Age and social vulnerability.
Red (solid) lines: women; blue (dashed) lines: men. Point estimates from fixed effects regression of columns (1) and (5) from Table 2. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
In columns (3)–(4) and (7)–(8) we provide results of the Mundlak regressions in order to assess regional and cohort effects. For more statistical power, we aggregate the year of birth in 3 year bins, i.e. we use yob dummies for births in 1916–1918, 1919–1921, etc., with baseline yob 1940–1942. Results for individual years of birth are similar and available upon request. In order to save space and increase readability we omit the cohort coefficients in Table 2 and present them instead graphically in Fig. 2 (the full Table is in the Appendix, Table A3). Confidence bands are represented by vertical lines. For both men and women, we observe an increase of the SVI for cohorts born after 1948, which is, however, statistically significant only for women. It is important to recall that these results are obtained controlling for age. For any given age, women born after 1948 face - on average-an SVI that is about 2 percentage points (i.e. about 1/3 of a standard deviation) higher.
Fig. 2.
Year of birth fixed effects.
Year of birth fixed effects retrieved from the Mundlak regressions (Table A3, columns (4) and (8)).Baseline: 1940–1942 cohort.
Table 3.
Aging and social vulnerability.
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| Age | 0.0403∗∗∗ | 0.0403∗∗∗ | 0.0413∗∗∗ | 0.0418∗∗∗ | 0.0486∗∗∗ | 0.0486∗∗∗ | 0.0495∗∗∗ | 0.0498∗∗∗ |
| (0.00117) | (0.00118) | (0.00127) | (0.00133) | (0.00135) | (0.00136) | (0.00135) | (0.00134) | |
| SVI | 0.558∗∗∗ | 0.556∗∗∗ | 0.531∗∗∗ | 0.530∗∗∗ | ||||
| (0.0657) | (0.0657) | (0.0875) | (0.0863) | |||||
| log Income | −0.00451 | −0.00494 | −0.00584 | −0.00805 | −0.0206∗∗ | −0.0209∗∗ | −0.0220∗∗∗ | −0.0231∗∗∗ |
| (0.00669) | (0.00675) | (0.00685) | (0.00680) | (0.00842) | (0.00839) | (0.00835) | (0.00825) | |
| Initial SVI | 2.079∗∗∗ | 2.072∗∗∗ | 1.779∗∗∗ | 1.818∗∗∗ | ||||
| (0.105) | (0.106) | (0.116) | (0.121) | |||||
| Lives with partner | 0.0192 | 0.0132 | ||||||
| (0.0141) | (0.0149) | |||||||
| No. persons in h. | 0.0128∗∗ | 0.0108∗ | ||||||
| (0.00527) | (0.00581) | |||||||
| Constant |
−4.537∗∗∗ | −0.715∗∗∗ | −0.340 | −0.420∗ | −5.159∗∗∗ | −1.386∗∗∗ | −1.130∗∗∗ | −1.139∗∗∗ |
| (0.119) |
(0.233) |
(0.221) |
(0.216) |
(0.151) |
(0.336) |
(0.331) |
(0.323) |
|
| Sample | Women | Women | Women | Women | Men | Men | Men | Men |
| Method | FE | Mundlak | Mundlak | Mundlak | FE | Mundlak | Mundlak | Mundlak |
| Obs. | 21817 | 21817 | 21817 | 21817 | 15650 | 15650 | 15650 | 15650 |
Robust standard errors clustered at the year of birth level in parenthesis. All columns include regional fixed effects, the baseline region is Northeast. Columns (2)–(4) and (6)–(8) further control for the year of birth and the means of the time changing variables. ∗p < 0.10, ∗∗p < 0.05, ∗∗∗p < 0.01.
The baseline of the regional effects is the Northeast. While the point estimates suggests that social vulnerability is greater there compared to all other regions, regional effects are only statistically significant for men from the West and Midwest. For men from these regions, SVI is about 1/4–1/3 of a standard a deviation lower (compared to those of Northeast). It should be noted that the regional effects here show the association between moving to each of these regions and social vulnerability.
In columns (2), (4), (6) and (8) we introduce log income as a potential confounder. Income reduces the SVI but in a statistically significant way only for men. Moreover, the protective effect of income is small. A 100 percent increase in log income decreases the SVI by about 0.0018, an effect that is more than one order of magnitude smaller than moving to the West or Midwest. In the Appendix, in Table A8 we check the sensitivity of results for alternative income measures including also income from other household members.4 We see, that the u-shaped age pattern of the SVI is hardly affected by income and that the size of the income coefficient varies insignificantly between the different specifications. The income coefficient, however, is less precisely estimated for the alternative income measures of income and becomes statistically insignificant from zero also for men. Summarizing, we find at best a small positive impact of income on the SVI of men.
Finally, we observe a great robustness of the age coefficients. The move from individual to cohort regressions including cohort fixed effects and the introduction of additional confounders leaves the size of the coefficients virtually unchanged. Additional results are provided in the Appendix (Tables A4.–A.7), where we have changed the maximum age to 85, removed the upper bound for age, and removed the first and the last wave. The overall picture remains the same.
As a final sensitivity check we re-computed the SVI by iteratively removing one item at a time. Results for the 49 thus compiled SVI's are shown in Appendix Tables A9 and A10. We see that the alternative composition of the index does not significantly change the coefficients on age and age squared and preserves the u-shaped age pattern.
4. Individual aging and social vulnerability
Based on numerous previous studies, we assume a log-linear association between chronological age and the frailty index (e.g. Abeliansky et al., 2020; Abeliansky & Strulik, 2018a; Mitnitski et al., 2016, 2002). This implies that, ceteris paribus, health deficits increase exponentially with age akin to the Gompertz (1825) law of mortality. The main innovation of this study is to introduce the social vulnerability index as an additional explanatory variable. For the benchmark regression we use the following model:
| (2) |
in which Diw is the frailty index of individual i in wave w and SVIiw is the social vulnerability index, as described above, and νiw is an error term. As before, we estimate the model separately for men and women, consider log income as a potential confounder, and introduce individual fixed effects (FE) or regional- and cohort effects (in Mundlak regressions).
Results are shown in Table 3. Columns (1) and (5) show results from the FE regressions. In line with previous research, we find that the age coefficient is larger for men than for women and the constant is lower for men. This means that men age faster but start out healthier than women. For the whole sample, the health deficit index for men increases by 4.9 percent and the one for women by 4.0 percent by each additional chronological year of age. Quantitatively these results are similar to those from our earlier study (Abeliansky et al., 2020). Income is insignificantly associated with the frailty index of women. For men, the coefficient on log income is significantly negative but small. Due to the log-log specification, the coefficient provides an elasticity. The point estimate implies that an increase in income of 100 percent is associated with a 2 percent decrease of the frailty index.
Being more socially vulnerable increases the frailty index of men and women in a statistically and economically significant way. The log-linear specification implies that the coefficient is a semi-elasticity. For women, a one standard deviation increase of the SVI (i.e. by 0.1 units) increases the frailty index by about 5.6 percent, i.e., evaluated at sample means, by 1.3 percentage points. Results for men are statically insignificantly different from those for women.
To test the robustness of these results we changed the age restrictions (upper-bound) and reduced the number of waves included in the sample. First, we lowered the maximum age of the individuals in the sample to 85 years. Next, we dropped the upper age restriction. We further tested the model without the first wave and lastly without the last one. The values of the estimated coefficients do not differ significantly from those in Table 3, see Tables A12–A15 in the Appendix.
We next turn to a cohort analysis by including year-of-birth-fixed effects in a regression using the Mundlak approach, as explained in conjunction with the SVI regressions in the previous section. A table with results for all included variables can be found in Appendix Table A11. The regression term “mean age” is statistically significant in all regressions, suggesting that there is indeed unobserved heterogeneity at the individual level correlated with the force of aging. Results for the year-of-birth effects (benchmark cohort 1940–1942) are visualized in Figure A1 in the Appendix. The yob-dummies are mostly significant and an almost linear trend is discernible. On average, each three-year step of later birth is associated with an improvement of the frailty index of about three percent, in line with our earlier result that the health of elderly Americans improves by about one percent per year of later birth (Abeliansky et al., 2020).
The main variables of interest in our present study are presented in columns (2)–(4) and (6)–(8) in Table 3. Comparing results from column (1) and (2) and (5) and (6), we conclude that the size of the coefficients for age, SVI, and income remain stable when we control for cohorts. The estimate for the coefficient on SVI, however, is potentially problematic. In the Introduction we argued that it is easily conceivable that increasing frailty leads to greater social isolation. This issue prevents a causal interpretation of the SVI coefficient. Moreover, we established in the previous section that (for individuals above 60) there is a strong positive association between SVI and age, which may cause a problem of multi-collinearity since age is necessarily included as a variable in regressions analyzing the frailty index. Both problems cannot not be addressed in fixed effects regressions, but they can be addressed with the Mundlak approach.
Columns (3)–(4) and (7)–(8) show results when Siw in model (2) is replaced by Si0, which is the initial value of the social vulnerability index in the first wave the respondents participated in the survey. Since Si0 is invariant to individual aging, the replacement takes care of issues of reverse causality and multicollinearity. Again, we observe that the coefficients of age and income are quite robust to the re-specification of the model. The coefficient of initial SVI is statistically significant and larger than the coefficient on age-dependent SVI from column (2) and (6). From the fact that individual SVI increases with age and thus from wave to wave we would expect that the size of the coefficient of initial SVI exceeds the coefficient of (wave-adjusted) SVI. The difference in size, however, is hard to interpret. The point estimate for women suggests that an initially higher SVI by one standard deviation leads to a 20 percent higher frailty index at any age. The estimated effect for men is mildly smaller with an almost 18 percent increase. This means that the frailty index is on average higher by about 3.5 percentage points.
Finally, we investigate to which extent the effect of the SVI on aging is explained by social relations within the household. For that purpose we added to model (2) a dummy variable that equals one if the individual lives together with a partner and a count variable that provides the number of people that live in the household. Results are shown in columns (4) and (8) of Table 3. The number of persons in the household is statistically significantly positive but small. Another person in the household is associated with an increase of the frailty index by about one percent. Living with a partner has no (additional) effect on frailty. Notice that these results are unlikely to be driven by nursing home inhabitants. In the sample there are only 186 observations where the respondents live in a nursing home (less than 0.5 percent of the sample). The size of the coefficient on SVI remains virtually unchanged when considering whether living together with a partner or other household members.
In Appendix Table A16 we show the results for the alternative income measures introduced in Section 3. The estimated coefficients for age, SVI, and income are robust to alternative income measurements and the finding that income is mildly protective for men but not for women is preserved. In Appendix Table A17 we examine robustness of the SVI–frailty nexus for the 49 alternative compositions of the SVI (dropping one item at a time). For men and women we observe only insignificant changes of the SVI coefficient compared to baseline results.
Finally in Appendix Tables A18 and A19 we estimate in two different ways the impact of the individual SVI items on aging. In columns (1), (3), and (5) we report results when in regression equation (2) the SVI is replaced iteratively by each of the 49 individual items of the SVI. In columns (2), (4), and (6) we report results when all 49 items enter the regression equation simultaneously. All regressions are based on the fixed effects specification. When all items enter as independent regressors, they jointly suffer from multicollinearity. The coefficients usually have the expected sign although most of them are not statistically significant. Some items turn out to be independently significant determinants of the frailty index. Some items show up significantly for both men and women, namely being active, going to meetings, doing gardening and cooking, being isolated, feelings of being left out, as well as indicators of life satisfaction. Items on contacts with friends, children, and family members, are not consistently found to be significant as stand-alone determinants of aging for both men and women. For men, being exposed to friends or children who get on their nerves is associated with increased frailty. For women, a lack of personal and written contact with children and relatives is a significant predictor of frailty.
5. Discussion and conclusion
Our study revealed that, controlling for individual heterogeneity, social circumstances of elderly U.S. Americans, measured by the SVI, deteriorated from about age 60 onwards. This result, obtained for men and women, is in line with earlier results considering Canadians and Europeans (Andrew et al., 2008; Wallace et al., 2015). The feature that the SVI mildly declines before age 60 and is thus u-shaped in age, relates to studies documenting a u-shaped age pattern of (perceived) loneliness (Hawkley & Cacioppo, 2010). The decline of SVI from age 50 to 60, however, is very mild compared to the subsequent increase. Additionally, we found a small protective effect of income on social vulnerability, which is statistically significant only for men. According to the point estimate, a twentyfold increase in income has about the same effect on SVI as moving from the Northeast to the Midwest. The finding that social vulnerability is lower in the West and Midwest is broadly consistent with Putnam’s (2000, Ch. 16) observation of higher social capital in these regions.
When analyzing the cohort fixed effects, we found that individuals born in the late 1940s or later displayed a greater SVI. The increase, however, is small and it is statistically significant only for women. We can only speculate on mechanisms behind this result. Women born after 1948 had access to the contraceptive pill during (most of) the fecundity period and had less children (Bailey, 2010). They were much better educated than previous generations, married later, stayed longer on the labor market, and were more likely to become divorced (Goldin, 2006). Life cycle behavior was more stable for men from different generations. Later born men supplied somewhat less labor to the market and spent somewhat more time on household work and with the family (Ramey, 2009; Ramey & Francis, 2009). They were also more likely to remarry than women (Livingston, 2014). The rapid change in many social dimensions for women of working age born after the late 1940s has been dubbed the “quiet revolution” (Goldin, 2006). The feature that the “quiet revolution” is apparently associated with (mildly) deteriorating SVI in old age, suggests that social connections outside the workplace are more protective against social isolation than friends and colleagues from work, perhaps because they are more easily maintained after retirement.
One way to rationalize the public perception of an increasing trend in loneliness (or social vulnerability) is by accounting for demographic change and compositional affects. Since the SVI is strongly increasing in age, there will be more socially vulnerable people at the population level when the population is aging. This was indeed the case for the U.S. In the decade 2010–2019, the 65-and-older population grew by over a third and the dependency ratio increased from 49 to 54 percent, driven by the aging baby-boomer cohorts (US Census, 2020).
In the regressions analyzing the frailty index we replicated earlier findings on the exponential rise of frailty with increasing age and found a statistically significant association of the SVI with health deficit accumulation at the individual- and cohort-level. Using the initial SVI (at first interview) in regressions on subsequent frailty, we established a causal effect of SVI on biological aging, which is statistically significant, large, and of about the same size for men and women. According to the point estimates, an increase of the initial SVI by one standard deviation leads to an increase of the frailty index of about 20 percent.
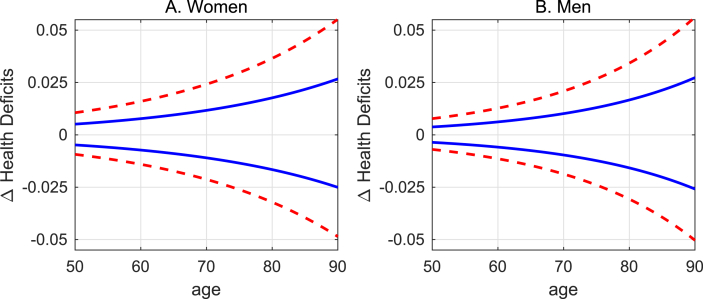
Since the frailty index is exponentially increasing in age, these results imply that a higher initial SVI leads not only to more health deficits but also to faster aging. In order to precisely obtain the aging effect, we take the anti-log of (2) and compute the difference in the frailty index (ΔD) for two individuals (i = 1, 2) of the same chronological age who differ only in their initial SVI (SVI10, SVI20):
We observe that the impact of the initial SVI on the frailty differential grows exponentially as individuals become older. Fig. 3 visualizes this result. It shows the frailty index differential using the point estimates from columns (3) and (7) of Table 3 and the associated sample means with exception of the initial SVI, which is by one standard deviation (blue solid lines) or two standard deviations higher or lower for person 2. A standard deviation is about 10 percentage points of the SVI. For example, as women grow older, the difference in frailty caused by the initial difference in SVI of one standard deviation grows from 5 percent at age 50 to 27 percent at age 90. For men it grows from 3.5 to 27 percent. Men catch-up in frailty difference to women due to their faster biological aging.
Fig. 3.
Social vulnerability and aging.
Difference in frailty index between average person and person with initial SVI by one (blue solid liens) and two (red dashed lines) standard deviation(s) higher. Point estimates from fixed effects regression of columns (3) and (7) from Table 3. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
The result highlights a general feature of the self-productive nature of health deficit accumulation (Dragone & Vanin, 2021): because health deficits increase exponentially (or, more, generally in a convex way) with age, initial differences are amplified as individuals grow older. This feature has been discussed in the context of developmental origins of health in old age (Dalgaard et al., 2021; Abeliansky and Strulik, 2018b, 2020a) and in the context of occupational health burden and retirement (Abeliansky & Strulik, 2020b). Here, it appears again in the context of social vulnerability. The result is intuitively plausible. Individuals with a greater initial SVI may have less incentive to leave the house, face less cognitive challenges, and experience more stress from perceived loneliness. As a result, initially mild health deficits (obesity, hypertension, declining cognitive function) may develop. The increase in health deficits then leads to a faster development of new health deficits due to the self-productive nature of health deficit accumulation, as predicted by reliability- and network-theories of biological aging (Gavrilov & Gavrilova, 1991; Rutenberg et al., 2018).
We also found that the impact of SVI on aging remains virtually unaffected when we add to the regression a dummy variable of living with a partner and a count variable of the number of household members and that the effect of the additional regressors on frailty is small and partially statistically insignificant. This – perhaps surprising – result sheds new light on the debate on objective vs. subjective social isolation (Hawkley et al., 2019). Individuals living with a partner or other family members are objectively not isolated. They may nevertheless be socially vulnerable and feel lonely and then the presence of other household members affects the impact of SVI on aging only insignificantly. The result suggests that the increasing trend of living alone in old age – due to changing demography, social welfare systems, and family culture – is not necessarily dangerous for the health of the elderly if they maintain social connections outside the household that protect against social isolation.
When we consider these results in light of the results from Section 3, showing that there is no significant trend increase in the SVI for men and only a relatively small increase for women, the observation that there is a strong trend of living alone in old age (Klinenberg et al., 2013) should not raise concerns, taken for itself. This does, of course, not imply that policy could disregard the social circumstances of the elderly. On the contrary, our analysis established a strong effect of social vulnerability on health and aging of elderly Americans. It should be also kept in mind that our panel data was collected in 2004–2016, i.e. in relatively calm times, in which social contacts were at least partially a choice variable and most individuals had the opportunity to actively respond to perceived loneliness and isolation by intensifying social interaction. In times of lockdown in a pandemic, in contrast, the means of social interaction are exogenously limited for everyone. We expect that enforced social distance, as recently experienced, does not only increase the average SVI but also its impact on health and aging of elderly Americans.
Data availability
The raw data of the study is from the Health and Retirement Study (RAND HRS 2014 Fat File (V2A)), which is a public use dataset. It was produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, (September 2019). RAND HRS 2014 Fat File (V2A) was produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA (September 2019). The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
Author contributions
AB, DE, and HS developed the design of the study, AB and DE performed the data analysis, AB, DE, and HS jointly wrote the manuscript text.
Declaration of competing interest
The authors declare no competing interests.
Acknowledgements
We thank two anonymous reviewers for helpful comments and suggestions.
Footnotes
The methodology of equal weighting of the items of the SVI follows the methodology of the frailty index. The developers of the frailty index argue that weighing health deficits in the index may somewhat improve the predictive power of the index but it destroys generalizability, which is regarded as the greatest value of the index (Rockwood & Mitnitski, 2007). Not weighting the frailty index was also defended on the grounds that the multiple dependencies of the variables on each other reflect an underlying biological redundancy (Rockwood et al., 2002). A similar redundancy argument can be made for the items of the SVI.
In the first core sample, the HRS includes three oversamples. The sample is designed to increase representation of African American and Hispanic individuals, and residents living in the state of Florida. The dataset includes compensatory weights. However, since the dataset is cleaned according to limitations described above, the original structure of the sample is not preserved. Thus, sample weights will be ignored for the main analysis. This approach is also supported by Yang and Lee (2009) who also used the HRS dataset to construct a health deficit index, refraining from using sample weights. They argue that it will not lead to significantly different results and they follow the recommendations of Winship and Radbill (1994).
Results remain essentially unchanged when we replace the log with the inverse hyperbolic sine in order to allow zeroes to be accounted for in the regressions.
In Table A8, the label bench indicates that income is measured as in the main text (benchmark). The label povhhi indicates that income includes total household income minus food stamps, plus Medicare Part B and/or Part D when these had been deducted from Social Security payments, income of non-core resident family members, minus income of any core HRS nursing home resident and all other household income. The label pvhhia indicates that income is measured as povhhi plus income from institutionalized family members who are part of the household. (RAND, 2021).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100924.
Contributor Information
Ana Lucia Abeliansky, Email: ana-lucia.abeliansky@wiwi.uni-goettingen.de.
Devin Erel, Email: devin.erel@uni-goettingen.de.
Holger Strulik, Email: holger.strulik@wiwi.uni-goettingen.de.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- AARP . American Association of Retired Persons; 2005. A report to the nation on livable communities: Creating environments for successful aging. [Google Scholar]
- Abeliansky A., Erel D., Strulik H. Aging in the USA. Scientific Reports. 2020;10:14309. doi: 10.1038/s41598-020-71269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abeliansky A., Strulik H. How we fall apart: Similarities of human aging in 10 European countries. Demography. 2018;55(1):341–359. doi: 10.1007/s13524-017-0641-8. [DOI] [PubMed] [Google Scholar]
- Abeliansky A., Strulik H. Hungry children age faster. Economics and Human Biology. 2018;29:211–222. doi: 10.1016/j.ehb.2018.03.005. [DOI] [PubMed] [Google Scholar]
- Abeliansky A., Strulik H. Season of birth, health and aging. Economics and Human Biology. 2020;36:100812. doi: 10.1016/j.ehb.2019.100812. [DOI] [PubMed] [Google Scholar]
- Abeliansky A., Strulik H. University of Goettingen; 2020. Health and aging before and after retirement. cege discussion paper 397. [Google Scholar]
- Akerlind I., Hoernquist J.O. Loneliness and alcohol abuse: A review of evidences of an interplay. Social Science & Medicine. 1992;34(4):405–414. doi: 10.1016/0277-9536(92)90300-f. [DOI] [PubMed] [Google Scholar]
- Andrew M.K., Keefe J.M. Social vulnerability from a social ecology perspective: A cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatrics. 2014;14(1):90. doi: 10.1186/1471-2318-14-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrew M.K., Mitnitski A.B., Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS One. 2008;3(5) doi: 10.1371/journal.pone.0002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arking R. Oxford University Press; Oxford: 2006. The biology of aging: Observations and principles. [Google Scholar]
- Bailey M.J. “Momma's got the pill”: How Anthony Comstock and Griswold v. Connecticut shaped US childbearing. The American Economic Review. 2010;100(1):98–129. doi: 10.1257/aer.100.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC . 2018. How should we tackle the loneliness epidemic?https://www.bbc.com/news/uk-42887932 11 February 2018. [Google Scholar]
- Blodgett J.M., Theou O., Howlett S.E., Wu F.C., Rockwood K. A frailty index based on laboratory deficits in community-dwelling men predicted their risk of adverse health outcomes. Age and Ageing. 2016;45(4):463–468. doi: 10.1093/ageing/afw054. [DOI] [PubMed] [Google Scholar]
- Bonsang E. Does informal care from children to their elderly parents substitute for formal care in Europe? Journal of Health Economics. 2009;28(1):143–154. doi: 10.1016/j.jhealeco.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Christakis N.A., Fowler J.H. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Dahlberg L., Agahi N., Lennartsson C. Lonelier than ever? Loneliness of older people over two decades. Archives of Gerontology and Geriatrics. 2018;75:96–103. doi: 10.1016/j.archger.2017.11.004. [DOI] [PubMed] [Google Scholar]
- Dalgaard C.-J., Hansen C., Strulik H. Fetal origins – a life cycle model of health and aging from conception to death. Health Economics. 2021;30(6):1276–1290. doi: 10.1002/hec.4231. [DOI] [PubMed] [Google Scholar]
- Dragone D., Vanin P. Substitution effects in intertemporal problems. American Economic Journal: Microeconomics. 2021 forthcoming. [Google Scholar]
- Dykstra P.A. Older adult loneliness: Myths and realities. European Journal of Ageing. 2009;6(2):91. doi: 10.1007/s10433-009-0110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavrilov L.A., Gavrilova N.S. Harwood Academic Publishers; London: 1991. The biology of human life span: A quantitative approach. [Google Scholar]
- Goldin C. The quiet revolution that transformed women's employment, education, and family. The American Economic Review. 2006;96(2):1–21. [Google Scholar]
- Gompertz B. On the nature of the function expressive of the law of human mortality, and on a new mode of determining the value of life contingencies. Philosophical Transactions of the Royal Society of London. 1825;115:513–583. doi: 10.1098/rstb.2014.0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon E.H., Peel N.M., Samanta M., Theou O., Howlett S.E., Hubbard R.E. Sex differences in frailty: a systematic review and meta-analysis. Experimental Gerontology. 2017;89:30–40. doi: 10.1016/j.exger.2016.12.021. [DOI] [PubMed] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Aging and loneliness: Downhill quickly? Current Directions in Psychological Science. 2007;16(4):187–191. [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L.C., Thisted R.A., Cacioppo J.T. Loneliness predicts reduced physical activity: Cross-sectional and longitudinal analyses. Health Psychology. 2009;28(3):354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L.C., Wroblewski K., Kaiser T., Luhmann M., Schumm L.P. Are US older adults getting lonelier? Age, period, and cohort differences. Psychology and Aging. 2019;34(8):1144. doi: 10.1037/pag0000365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Hosseini R., Kopecky K.A., Zhao K. 2019. The evolution of health over the life cycle. Discussion Paper. [Google Scholar]
- House J.S., Landis K.R., Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- HRSA . US Health Resources and Services Administration; 2019. The “loneliness epidemic”.https://www.hrsa.gov/enews/past-issues/2019/january-17/loneliness-epidemic [Google Scholar]
- Klinenberg E., Torres S., Portacolone E. Council on Contemporary Families; New York: 2013. Aging alone in America. Aging alone in America. [Google Scholar]
- Lachmann R., Stelmach-Mardas M., Bergmann M.M., Bernigau W., Weber D., Pischon T., Boeing H. The accumulation of deficits approach to describe frailty. PloS one. 2019;14(10) doi: 10.1371/journal.pone.0223449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone T., Hessel P. The effect of social participation on the subjective and objective health status of the over-fifties: Evidence from SHARE. Ageing and Society. 2016;36(5):968–987. [Google Scholar]
- Liu G.G., Xue X., Yu C., Wang Y. How does social capital matter to the health status of older adults? Evidence from the China health and retirement longitudinal Survey. Economics and Human Biology. 2016;22:177–189. doi: 10.1016/j.ehb.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Livingston G. Pew Research Center; Washington, D.C.: 2014. Four-in-Ten couples are saying ‘I do,’ again. November. [Google Scholar]
- Mitnitski A.B., Mogilner A.J., MacKnight C., Rockwood K. The accumulation of deficits with age and possible invariants of aging. Scientific World. 2002;2:1816–1822. doi: 10.1100/tsw.2002.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitnitski A., Rockwood K. The rate of aging: The rate of deficit accumulation does not change over the adult life span. Biogerontology. 2016;17(1):199–204. doi: 10.1007/s10522-015-9583-y. [DOI] [PubMed] [Google Scholar]
- Mitnitski A.B., Mogilner A.J., Rockwood K. Accumulation of deficits as a proxy measure of aging. Scientific World. 2001;1:323–336. doi: 10.1100/tsw.2001.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig P., Cohen A.K., Palmer A., Zhu W. The relationship between five different measures of structural social capital, medical examination outcomes, and mortality. Social Science & Medicine. 2013;85:18–26. doi: 10.1016/j.socscimed.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Mundlak Y. On the pooling of time series and cross section data. Econometrica. 1978;46(1):69–85. [Google Scholar]
- Perissinotto C.M., Cenzer I.S., Covinsky K.E. Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine. 2012;172(14):1078–1084. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R.D. Simon and Schuster; 2000. Bowling alone: The collapse and revival of American community. [Google Scholar]
- Ramey V.A. Time spent in home production in the twentieth-century United States: New estimates from old data. The Journal of Economic History. 2009;69(1):1–47. [Google Scholar]
- Ramey V.A., Francis N. A century of work and leisure. American Economic Journal: Macroeconomics. 2009;1(2):189–224. [Google Scholar]
- RAND HRS . 2021. Longitudinal file 2018 (V1) documentation.https://www.rand.org/content/dam/rand/www/external/labor/aging/dataprod/randhrs1992_2018v1.pdf accessed from. [Google Scholar]
- Reeves D., Blickem C., Vassilev I., Brooks H., Kennedy A., Richardson G., Rogers A. The contribution of social networks to the health and self-management of patients with long-term conditions: A longitudinal study. PLoS One. 2014;9(6) doi: 10.1371/journal.pone.0098340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwood K., Mitnitski A. Limits to deficit accumulation in elderly people. Mechanism of Ageing and Development. 2006;127(5):494–496. doi: 10.1016/j.mad.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Rockwood K., Mitnitski A.B. Frailty in relation to the accumulation of deficits. Journals of Gerontology Series A: Biological and Medical Sciences. 2007;62:722–727. doi: 10.1093/gerona/62.7.722. [DOI] [PubMed] [Google Scholar]
- Rockwood K., Mitnitski A.B., MacKnight C. Some mathematical models of frailty and their clinical implications. Reviews in Clinical Gerontology. 2002;12(2):109. [Google Scholar]
- Rodgers J., Valuev A.V., Hswen Y., Subramanian S.V. Social capital and physical health: An updated review of the literature for 2007–2018. Social Science & Medicine. 2019;236:112360. doi: 10.1016/j.socscimed.2019.112360. [DOI] [PubMed] [Google Scholar]
- Rosso A.L., Taylor J.A., Tabb L.P., Michael Y.L. Mobility, disability, and social engagement in older adults. Journal of Aging and Health. 2013;25(4):617–637. doi: 10.1177/0898264313482489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutenberg A.D., Mitnitski A.B., Farrell S.G., Rockwood K. Unifying aging and frailty through complex dynamical networks. Experimental Gerontology. 2018;107:126–129. doi: 10.1016/j.exger.2017.08.027. [DOI] [PubMed] [Google Scholar]
- Santos H.C., Varnum M.E., Grossmann I. Global increases in individualism. Psychological Science. 2017;28(9):1228–1239. doi: 10.1177/0956797617700622. [DOI] [PubMed] [Google Scholar]
- Searle S.D., Mitnitski A.B., Gahbauer E.A., Gill T.M., Rockwood K. A standard procedure for creating a frailty index. BMC Geriatrics. 2008;8(1):24. doi: 10.1186/1471-2318-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirven N., Debrand T. Social capital and health of older Europeans: Causal pathways and health inequalities. Social Science & Medicine. 2012;75(7):1288–1295. doi: 10.1016/j.socscimed.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Snyder-Mackler N., Burger J.R., Gaydosh L., Belsky D.W., Noppert G.A., Campos F.A., Harris K.M. Social determinants of health and survival in humans and other animals. Science. 2020;368(6493) doi: 10.1126/science.aax9553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strulik H. A mass phenomenon: The social evolution of obesity. Journal of Health Economics. 2014;33:113–125. doi: 10.1016/j.jhealeco.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Strulik H. Opioid epidemics. Economics and Human Biology. 2020;37:100835. doi: 10.1016/j.ehb.2019.100835. [DOI] [PubMed] [Google Scholar]
- The Economist . 2018. Loneliness is a serious public-health problem. 1 September 2018. [Google Scholar]
- Umberson D., Crosnoe R., Reczek C. Social relationships and health behavior across the life course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census . 2020. Annual estimates of the resident population for selected age groups.https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html [Google Scholar]
- Van Houtven C.H., Norton E.C. Informal care and health care use of older adults. Journal of Health Economics. 2004;23(6):1159–1180. doi: 10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Wallace L.M., Theou O., Pena F., Rockwood K., Andrew M.K. Social vulnerability as a predictor of mortality and disability: Cross-country differences in the survey of health, aging, and retirement in Europe (SHARE) Aging Clinical and Experimental Research. 2015;27(3):365–372. doi: 10.1007/s40520-014-0271-6. [DOI] [PubMed] [Google Scholar]
- Winship C., Radbill L. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–257. [Google Scholar]
- Yang Y., Lee L.C. Dynamics and heterogeneity in the process of human frailty and aging: Evidence from the US older adult population. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65(2):246–255. doi: 10.1093/geronb/gbp102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data of the study is from the Health and Retirement Study (RAND HRS 2014 Fat File (V2A)), which is a public use dataset. It was produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, (September 2019). RAND HRS 2014 Fat File (V2A) was produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA (September 2019). The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.