Abstract
Neuroinflammation and neurodegeneration are key components in the establishment and progression of neurodegenerative diseases including Alzheimer's Disease (AD). Over the past decade increasing evidence is emerging for the use of components of the canonical autophagy machinery in pathways that are characterized by LC3 lipidation yet are distinct from traditional macro-autophagy. One such pathway that utilizes components of the autophagy machinery to target LC3 to endosomes, a process termed LC3-associated endocytosis (LANDO), has recently been identified and regulates neuroinflammation. Abrogation of LANDO in microglia cells results in a propensity for elevated neuroinflammatory cytokine production. Using the well-established 5xFAD model of AD to interrogate neuroinflammatory regulation, impairment of LANDO through deletion of a key upstream regulator Rubicon or other downstream autophagy components, exacerbated disease onset and severity, while deletion of microglial autophagy alone had no measurable effect. Mice presented with robust deposition of the neurotoxic AD protein β-amyloid (Aβ), microglial activation and inflammatory cytokine production, tau phosphorylation, and aggressive neurodegeneration culminating in severe memory impairment. LANDO-deficiency impaired recycling of receptors that recognize Aβ, including TLR4 and TREM2. LANDO-deficiency alone through deletion of the WD-domain of the autophagy protein ATG16L, revealed a role for LANDO in the spontaneous establishment of age-associated AD. LANDO-deficient mice aged to 2 years presented with advanced AD-like disease and pathology correlative to that observed in human AD patients. Together, these studies illustrate an important role for microglial LANDO in regulating CNS immune activation and protection against neurodegeneration. New evidence is emerging that demonstrates a putative linkage between pathways such as LANDO and cell death regulation via apoptosis and possibly necroptosis. Herein, we provide a review of the use of the autophagy machinery in non-canonical mechanisms that alter immune regulation and could have significant impact in furthering our understanding of not only CNS diseases like AD, but likely beyond.
Key Words: aging, Alzheimer's disease, autophagy, inflammation, LC3-associated endocytosis, microglia, neurodegeneration, neuroinflammation
Introduction
Macro-autophagy (autophagy henceforth) has been shown to be a contributing pathway to the regulation of immune responses and inflammation with primary roles in modulating metabolic and cellular homeostasis. In this canonical form of autophagy, double-membraned vacuoles known as autophagosomes are responsible for the collection and deliverance of various intracellular materials to the lysosome for degradation as a response to stressors, such as starvation and nutrient deprivation (Dikic and Elazar, 2018). Additionally, autophagy has been shown to participate in the regulation of various immune pathways, including in the regulation of the type-I interferon response, which in turn helps combat viral infections more effectively (Martin et al., 2018; Jin, 2019; Tian et al., 2019). Likewise, autophagy has been implicated in regulating pro-inflammatory cytokine signaling including interleukin (IL)-1β secretion by targeting the IL-1β precursor, pro-IL-1β for degradation (Zhang et al., 2015; Claude-Taupin et al., 2018; Iula et al., 2018). Much investigation has led to the identification of multiple regulatory genes and proteins that govern the orchestrated processing and conjugation of the microtubule-associated protein light-chain 3 (LC3) to phosphatidylethanolamine residues within the developing autophagosome membrane following autophagic activation, newer evidence is revealing distinct roles for the autophagy machinery in alternate pathways including LC3-associated phagocytosis (LAP) (Kim et al., 2013; Martinez et al., 2015; Martinez et al., 2016; Heckmann et al., 2017; Heckmann and Green, 2019), and LC3-associated endocytosis (LANDO) (Heckmann et al., 2019; Birgisdottir and Johansen, 2020). We often described these, and similar pathways as “non-canonical functions of the autophagy machinery”.
Search Strategy and Selection Criteria
Studies cited in this review published from 2010 to 2020 were searched on the PudMed database using the following keywords: autophagy, neuroinflammation, Alzheimer's disease, neurodegeneration, neuronal cell death, LC3-associated endocytosis, LC3-associated phagocytosis, LAP, LANDO, inflammation, beta-amyloid, inflammasome, NLRP3, Parkinson's disease, amyotrophic lateral sclerosis, Huntington's disease, CNS pathologies, IL-1beta, TNF-alpha, tau pathology.
Role of the Autophagy Machinery outside of Autophagy
Interestingly, although quite similar at a genetic level; autophagy, LAP, and LANDO are distinct cellular entities. A large share of the machinery found in the canonical autophagy pathway is needed for both LAP and LANDO, however components of the autophagy initiation complex including FIP200 and ULK1 are dispensable for LAP and LANDO, whereas the run-domain containing protein Rubicon, long held as an autophagic inhibitor is obligatory for LAP and LANDO and as shown previously is expendable for autophagy (Martinez et al., 2015). In the context of the central nervous system (CNS), canonical autophagy has been shown to play significant roles in both neuronal development and homeostatic maintenance in adult organisms (Sumpter and Levine, 2011; Andres-Alonso et al., 2020; Fleming and Rubinsztein, 2020; Kuijpers et al., 2020). Moreover, autophagic dysregulation in neurons has been identified in a number of CNS diseases including Huntington's and Amyotrophic Lateral Sclerosis. Autophagic induction has therefore been proposed as a putative therapeutic avenue in these and other diseases of the brain (Cheon et al., 2019; Djajadikerta et al., 2020).
Similar to autophagy in neurons, the non-canonical functions of the autophagy machinery in LANDO have been shown to be key in preventing exacerbated β-amyloid accumulation and in mitigating β-amyloid induced neuroinflammation in a model of Alzheimer's disease (AD). AD is the leading form of dementia globally and is one of the most prevalent neurodegenerative disorders without viable therapy. β-Amyloid deposition is one of the earliest hallmark features of AD in humans and has long been thought to be the major driver of disease pathology (Murphy and LeVine, 2010). Over the past decade it has been well demonstrated that a primary component of AD pathology is robust and pervasive neuroinflammation. In particular, inflammatory cytokines including IL-1β and tumor necrosis factor alpha (TNFα) have been shown to be elevated in the brains of AD patients compared to healthy age-matched counterparts (Kinney et al., 2018). In the brain, cytokines such as IL-1β and TNFα are predominately produced by the resident innate macrophage-like immune cell, the microglia. In addition to localized cytokine production by microglia, peripheral cytokines have been shown to contribute in AD, especially as permeability of the blood-brain barrier increases concurrent with disease progression (Kinney et al., 2018).
Noncanonical Uses of the Autophagy Machinery in Neurodegeneration
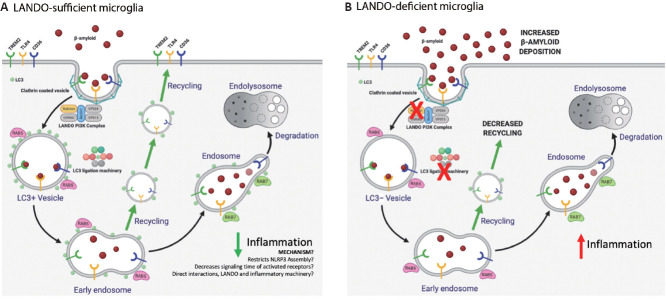
In a previous study, we identified a role for LANDO in the recognition and clearance of β-amyloid in a murine AD model (Heckmann et al., 2020a). We found that abrogation of LANDO in microglia, through genetic deletion of Rubicon led to an increase in extracellular β-amyloid deposition, a robust increase in microglial activation and neuroinflammation, as well as exacerbated tau pathology and neurodegeneration. In vitro analysis in cultured microglia clearly revealed that LANDO-deficiency alters the activation and inflammatory cytokine production following exposure to neurotoxic β-amyloid. In vivo studies were performed in mice on the 5xFAD background, a humanized transgenic model that leads to β-amyloid pathology (Heckmann et al., 2020a). Abrogation of LANDO greatly worsened the severity of disease and hastened the onset of pathology. Interestingly, we found that inhibition of canonical autophagy alone in microglia through deletion of FIP200 had little to no effect on the establishment of AD-like pathology when compared to autophagy-sufficient 5xFAD mice (Heckmann et al., 2019). Additionally, and as illustrated in Figure 1, we identified that a primary contributing factor to the decreased processing of internalized β-amyloid by LANDO-deficient microglia was not due to a defect in degradation, as is often seen in LAP-deficiency (Martinez et al., 2015; Martinez et al., 2016), but was rather caused by an impaired recycling of receptors that recognize β-amyloid, including TLR4 and TREM2 (Heckmann et al., 2019). Moreover, inflammatory cytokine production in response to β-amyloid paralleled the status of receptor recycling (Figure 1) (Heckmann et al., 2019). The role of the autophagy machinery in inflammatory pathways will be further described below.
Figure 1.
LANDO sufficiency or deficiency in microglia.
(A) LANDO-sufficient microglia internalize β-amyloid through a clathrin-associated endocytic process and the Rubicon containing PI3-kinase complex in LANDO initiates the downstream processing and lipidation of LC3 to the endosome. The LC3 ligation machinery is shared between canonical autophagy and LANDO, consisting of ATG5, ATG12, ATG16L, ATG7 and ATG4 as reviewed previously (Heckmann et al., 2017; Heckmann and Green, 2019), and no unique components that alter the function of the complex in LANDO compared to autophagy have yet to be identified. The Rab GTPases including Rab7 and Rab5 are required for endocytic trafficking and are present on LC3+ endosomes. LC3 conjugation facilitates the trafficking of the β-amyloid containing endosome towards recycling or degradation, by mechanisms which have not been fully elucidated. LANDO promotes the recycling of β-amyloid receptors including TREM2, TLR4, and CD36. LANDO suppresses inflammation following β-amyloid stimulation by currently unknown mechanisms, although putative hypotheses linking LANDO to inflammatory suppression include restriction of NLRP3 inflammasome assembly, decreases in signaling time of activated receptors by facilitating vesicle trafficking, and possible interactions between the LANDO machinery and inflammatory cytokines. B) LANDO-deficient microglia through deletion of Rubicon or ATG16L WD-domain fail to lipidate LC3 on endosomes and subsequently there is an impairment in the recycling of β-amyloid receptors leading to extracellular accumulation of β-amyloid, as continued uptake and degradation is decreased due to reduced receptor recycling. Consequently, there is an increase in inflammatory cytokine production from LANDO-deficient cells. ATG: Autophagy related genes; CD36: CLUSTER of differentiation 36; LANDO: LC3-associated endocytosis; LC3: microtubule-associated protein 1A/1B-light chain 3; NLRP3: NOD-, LRR- and pyrin domain-containing protein 3; Rab: Rab GTPase family; TLR4: Toll-like receptor 4; TREM2: triggering receptor expressed on myeloid cells 2.
Impaired Noncanonical Functions of the Autophagy Machinery is Enough to Drive Alzheimer's Disease
Since the AD phenotype associated with LANDO-deficiency was so greatly exacerbated, we decided to ask if LANDO-deficiency alone could drive AD-like pathology in mice in the absence of a humanized transgene(s). Elegant studies evaluating the WD-domain of the autophagy protein ATG16L and the binding regions required for interaction of ATG16L with the autophagy regulator WIPI2, led to the novel identification of a deletion mutant of ATG16L WD-domain that was sufficient for canonical autophagy but had an impairment of non-canonical pathways including LAP (Fletcher et al., 2018; Rai et al., 2019). We found that primary microglia lacking the WD-domain of ATG16L were likewise deficient in LANDO and presented with a severe impairment in the recycling of TREM2, TLR4, and CD36 (Heckmann et al., 2020b). Furthermore, those microglia had a decreased capacity for the continued uptake of extracellular β-amyloid (Heckmann et al., 2020b).
Evaluation of ATG16L WD-domain deficient mice that had been aged to 2 years revealed a deposition of endogenous murine β-amyloid in the hippocampus and cortex, consisting of neurotoxic β-amyloid 1–40 and 1–42 species (Heckmann et al., 2020b). When compared to β-amyloid deposits from LANDO-deficient mice on the 5xFAD background or human plaques, the deposits observed in the ATG16L WD-domain deficient mice were non-aggregated and more diffuse in morphology, consistent with the inherent biochemical and biophysical differences between mouse and human β-amyloid as reported previously (Lv et al., 2013). Nevertheless, these deposits of β-amyloid were neurotoxic and sufficient to drive downstream pathology including; tau hyperphosphorylation, reactive microgliosis and neuroinflammation, as well as active neurodegeneration (Heckmann et al., 2020b). Consistent with upstream markers of pathology, mice presented with severe memory and behavioral impairment.
Regulation of Inflammation by the Autophagy Machinery
While microglial LANDO suppresses neuroinflammation in response to β-amyloid, the role for other non-canonical uses of the autophagy machinery in the CNS in pathways such as LAP is less well defined. Currently, it is difficult to delineate LAP from LANDO at the genetic level (Martinez et al., 2015; Heckmann et al., 2017, 2019; Heckmann and Green, 2019). In pathologies characterized by neurodegeneration such as AD, LAP likely functions to prevent inflammation in response to the removal of dying neurons, a process called efferocytosis (Boada-Romero et al., 2020; Doran et al., 2020). Ongoing studies are directed at the genetic delineation of LAP, LANDO, and other non-canonical pathways. Having the ability to differentiate LAP and LANDO will allow for future studies that are directed at the contribution of each pathway to immune function and microglial responses to perturbations such as β-amyloid.
Peripheral to the CNS, non-canonical functions of the autophagy machinery have been shown to regulate inflammatory polarization of macrophages in response to a variety of cargoes (Heckmann et al., 2017; Heckmann and Green, 2019). A substantial amount of effort has been directed at understanding how the autophagy machinery in LAP suppresses inflammatory activation in response to dead or dying cells (Green et al., 2016; Asare et al., 2020; Boada-Romero et al., 2020). Signals that promote the identification of dead cells, often referred to as “Find-me” signals as well as signals promoting the engulfment of dead cells, “Eat-me” signals, have been shown to help shape the macrophage response to dead cell cargo as reviewed previously (Heckmann et al., 2017; Heckmann and Green, 2019; Boada-Romero et al., 2020). In addition, components of the autophagy machinery that are required for pathways like LAP and LANDO, such as ATG16L, have been shown to directly regulate anti-inflammatory signaling (Martinez et al., 2015; Heckmann et al., 2019, 2020b). The WD-domain of ATG16L interacts directly with cytokine receptors including IL-10RB and IL-2Rγ and exhibits WD-domain dependent LC3 lipidation (Serramito-Gomez et al., 2020). Cells deficient in the WD-domain of ATG16L have decreased anti-inflammatory signaling due to delayed endocytosis and insufficient trafficking of IL-10/IL-10R complexes leading to pro-inflammatory activation (Sorbara et al., 2013; Serramito-Gomez et al., 2020; Wang et al., 2021). Consistent with data on ATG16L, loss of Rubicon likewise alters IL-10 production and signaling (Martinez et al., 2016; Cunha et al., 2018). Whether Rubicon functions through downstream ATG16L or independently of the downstream components of LAP in regulating IL-10 biology remains unknown, although phenotypically, loss of either protein results in consistent changes to inflammatory polarization of macrophages. Moreover, stimuli that initiate these processes appear to be quite diverse, ranging from amyloids and extracellular aggregates to bacteria, viruses, and other pathogens (Heckmann et al., 2017; Heckmann and Green, 2019). In all scenarios the non-canonical use of the autophagy machinery is functioning to suppress inflammation. Once loss of components required for LAP and LANDO occurs, it seems cells subsequently are primed towards the production of inflammatory cytokines.
Exploiting Neuroinflammation as a Therapeutic Avenue in Alzheimer's Disease
One aspect we observed in the brains of the ATG16L WD-domain deficient aged mice was high levels of the inflammatory cytokine IL-1β in addition to TNFα, again paralleling human disease and consistent with inflammatory signaling described above. Over the past few years, there has been an accumulating interest in the possibility of targeting neuroinflammation as a therapeutic avenue for a variety of neurodegenerative conditions including AD. Targeting inflammatory cytokine production and/or signaling for mediators including IL-1β, TNFα, and IL-6 have been proposed (Camargo et al., 2015; Wu et al., 2015; Bronzuoli et al., 2016; Kinney et al., 2018; Lonnemann et al., 2020). In particular, IL-1β has proven to be an intriguing, albeit challenging target for putative therapy. Previous studies have demonstrated that compounds which modulate the activity of the NLRP3 inflammasome, the complex required for the production of IL-1β (Coll et al., 2019; Swanson et al., 2019; Jiang et al., 2020; Jiao et al., 2020), are efficacious and can readily cross the blood-brain barrier. Using our novel age-associated spontaneous AD model, we treated ATG16L WD-domain deficient mice with established AD-like disease for 8-weeks with the NLRP3 inhibitor MCC950 to reduce IL-1β production.
Following therapeutic intervention, MCC950 treated mice had comparable levels of β-amyloid to those observed in vehicle treated animals (Heckmann et al., 2020b). However, there were robust decreases in microglia activation, neuroinflammation, tau phosphorylation, and prominent decreases in activate neuronal apoptosis (Heckmann et al., 2020b). Although optimistic, we were surprised to find that MCC950 treatment led to an approximate 80–90% restoration in behavior and memory capacity as evaluated by Y-maze and novel object recognition analyses compared to mice treated with vehicle, which continued to have a decline in memory from the onset of therapy (Heckmann et al., 2020b). Together, these findings suggest that neuroinflammation is upstream of neurodegeneration and is leading to neuronal death by “fire” or as a consequence of inflammatory activation. Our results suggest that by alleviating inflammatory processes in the AD brain, there is the potential to overcome neuronal loss and have a positive impact on memory and reduction in disease progression. Moreover, these findings confirm that targeting neuroinflammatory mediators such as IL-1β in an established disease model is a promising therapeutic approach.
The Path Ahead
Superficially our findings reiterate the importance of neuroinflammation to disease processes in AD and that neuroinflammation is central to disease establishment and progression. As such, neuroinflammation is an attractive therapeutic target not only in AD but in a plethora of other CNS pathologies including Huntington's disease, Parkinson's disease (PD), and amyotrophic lateral sclerosis (Rizzo et al., 2014; Liu and Wang, 2017; Kwon and Koh, 2020). In particular, neuroinflammatory modulation has been proposed in amyotrophic lateral sclerosis and PD with promising efficacy (Lu and Hu, 2012; Guan and Han, 2020), The role of LANDO or other non-canonical pathways using the autophagy machinery in these diseases has to date not been evaluated, although changes in receptor recycling in diseases such as PD hint at a plausible role for LANDO (Kim et al., 2013; Ferguson and Green, 2014; Martinez et al., 2016; Muniz-Feliciano et al., 2017). Our results have further led to more in-depth biological questions, including how is LANDO-deficiency altering the neuroimmune architecture and by what mechanism(s)? Additionally, as hinted earlier, targeting IL-1β through inflammasome inhibition has proven more challenging in humans, with many compounds including MCC950 having deleterious side effects including hepatotoxicity. Similarly, targeting other inflammatory mediators such as TNFα which is also elevated in models of AD has proven less efficacious in human patients (Chang et al., 2017; Ekert et al., 2018). Would targeting non-canonical functions of the autophagy machinery in pathways such as LANDO prove less detrimental to peripheral systems while not sacrificing therapeutic efficacy? We can take hints from the role of pathways such as LAP in regulating inflammation in peripheral macrophages where the function appears to be fully independent of canonical autophagy (Martinez et al., 2015, 2016; Heckmann et al., 2017; Heckmann and Green, 2019), and as described above. A complete delineation from canonical autophagy would be ideal, as it allows for more targeted approaches to be applied to pathways such as LAP and LANDO. Previously, we have shown that abrogation of microglial autophagy in the 5xFAD model appears to have little to no effect on disease pathology and outcome (Heckmann et al., 2019). These data suggest that there is distinct regulation of LAP and LANDO compared to canonical autophagy and that each pathway likely is functioning independent of the others, although further investigation will be necessary to fully characterize these hypotheses.
Along those lines, we as well as others have shown that there is a consistent downregulation of components of the autophagy machinery and LANDO with age and further decreases in expression observed in the AD brain. Moreover, the suppression of pathways such as LANDO may prime the brain towards chronic neuroinflammatory activation, putatively “seeding” the brain for disease as one ages. With advances in genetic therapies and CRISPR technology, it is no longer unimaginable that we will soon have the capability of targeting these upstream regulators and associated pathways in human patients.
In summary, our prior work illustrates an important role for the autophagy machinery in non-canonical functions including LC3-associated endocytosis. Moreover, it is clear that LANDO is important for protection against neuroinflammation and downstream pathology in response to β-amyloid. Further studies are certainly required to unravel the exciting questions that are raised following the discovery of LANDO and its initial characterization in mitigating neuroinflammation and neurodegeneration, at both the cellular and molecular levels.
Additional file (78.6KB, pdf) : Open peer review report 1.
Footnotes
P-Reviewer: Jin S; C-Editors: Zhao M, Qiu Y; T-Editor: Jia Y
Conflicts of interest:BLH is a co-inventor on United States patent applications; 62/795,217, filed January 22, 2019, 62/797,564 filed January 28, 2019, and worldwide patent application PCT/IB2020/050504 filed January 22, 2020, through the United States Patent and Trademark Office. BLH consults for Ventus Therapeutics and USA Prime Biotech.
Financial support:This work was supported in part by the funding from the National Institute of Allergy and Infectious Disease and the National Cancer Institute under award numbers AI138492 and CA231423 to BLH. The content herein is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open peer reviewer:Shouheng Jin, Sun Yat-sen University, China.
References
- 1.Andres-Alonso M, Kreutz MR, Karpova A. Autophagy and the endolysosomal system in presynaptic function. Cell Mol Life Sci. 2020 doi: 10.1007/s00018-020-03722-5. doi: 10.1007/s00018-020-03722-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asare PF, Roscioli E, Hurtado PR, Tran HB, Mah CY, Hodge S. LC3-associated phagocytosis (LAP): a potentially influential mediator of efferocytosis-related tumor progression and aggressiveness. Front Oncol. 2020;10:1298. doi: 10.3389/fonc.2020.01298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birgisdottir AB, Johansen T. Autophagy and endocytosis - interconnections and interdependencies. J Cell Sci. 2020;133:jcs228114. doi: 10.1242/jcs.228114. [DOI] [PubMed] [Google Scholar]
- 4.Boada-Romero E, Martinez J, Heckmann BL, Green DR. The clearance of dead cells by efferocytosis. Nat Rev Mol Cell Biol. 2020;21:398–414. doi: 10.1038/s41580-020-0232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bronzuoli MR, Iacomino A, Steardo L, Scuderi C. Targeting neuroinflammation in Alzheimer's disease. J Inflamm Res. 2016;9:199–208. doi: 10.2147/JIR.S86958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Camargo CHF, Justus FF, Retzlaff G, Blood MRY, Schafranski MD. Action of anti-TNF-alpha drugs on the progression of Alzheimer's disease: a case report. Dement Neuropsychol. 2015;9:196–200. doi: 10.1590/1980-57642015DN92000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang R, Yee KL, Sumbria RK. Tumor necrosis factor alpha Inhibition for Alzheimer's Disease. J Cent Nerv Syst Dis. 2017;9:1179573517709278. doi: 10.1177/1179573517709278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheon SY, Kim H, Rubinsztein DC, Lee JE. Autophagy, cellular aging and age-related human diseases. Exp Neurobiol. 2019;28:643–657. doi: 10.5607/en.2019.28.6.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Claude-Taupin A, Bissa B, Jia J, Gu Y, Deretic V. Role of autophagy in IL-1beta export and release from cells. Semin Cell Dev Biol. 2018;83:36–41. doi: 10.1016/j.semcdb.2018.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coll RC, Hill JR, Day CJ, Zamoshnikova A, Boucher D, Massey NL, Chitty JL, Fraser JA, Jennings MP, Robertson AAB, Schroder K. MCC950 directly targets the NLRP3 ATP-hydrolysis motif for inflammasome inhibition. Nat Chem Biol. 2019;15:556–559. doi: 10.1038/s41589-019-0277-7. [DOI] [PubMed] [Google Scholar]
- 11.Cunha LD, Yang M, Carter R, Guy C, Harris L, Crawford JC, Quarato G, Boada-Romero E, Kalkavan H, Johnson MDL, Natarajan S, Turnis ME, Finkelstein D, Opferman JT, Gawad C, Green DR. LC3-associated phagocytosis in myeloid cells promotes tumor immune tolerance. Cell. 2018;175:429–441. doi: 10.1016/j.cell.2018.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dikic I, Elazar Z. Mechanism and medical implications of mammalian autophagy. Nat Rev Mol Cell Biol. 2018;19:349–364. doi: 10.1038/s41580-018-0003-4. [DOI] [PubMed] [Google Scholar]
- 13.Djajadikerta A, Keshri S, Pavel M, Prestil R, Ryan L, Rubinsztein DC. Autophagy induction as a therapeutic strategy for neurodegenerative diseases. J Mol Biol. 2020;432:2799–2821. doi: 10.1016/j.jmb.2019.12.035. [DOI] [PubMed] [Google Scholar]
- 14.Doran AC, Yurdagul A, Jr, Tabas I. Efferocytosis in health and disease. Nat Rev Immunol. 2020;20:254–267. doi: 10.1038/s41577-019-0240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekert JO, Gould RL, Reynolds G, Howard RJ. TNF alpha inhibitors in Alzheimer's disease: a systematic review. Int J Geriatr Psychiatry. 2018;33:688–694. doi: 10.1002/gps.4871. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson TA, Green DR. Autophagy and phagocytosis converge for better vision. Autophagy. 2014;10:165–167. doi: 10.4161/auto.26735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fleming A, Rubinsztein DC. Autophagy in neuronal development and plasticity. Trends Neurosci. 2020;43:767–779. doi: 10.1016/j.tins.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 18.Fletcher K, Ulferts R, Jacquin E, Veith T, Gammoh N, Arasteh JM, Mayer U, Carding SR, Wileman T, Beale R, Florey O. The WD40 domain of ATG16L1 is required for its non-canonical role in lipidation of LC3 at single membranes. EMBO J. 2018;37:e97840. doi: 10.15252/embj.201797840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green DR, Oguin TH, Martinez J. The clearance of dying cells: table for two. Cell Death Differ. 2016;23:915–926. doi: 10.1038/cdd.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guan Y, Han F. Key mechanisms and potential targets of the NLRP3 inflammasome in neurodegenerative diseases. Front Integr Neurosci. 2020;14:37. doi: 10.3389/fnint.2020.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heckmann BL, Green DR. LC3-associated phagocytosis at a glance. J Cell Sci. 2019;132:jcs222984. doi: 10.1242/jcs.222984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heckmann BL, Boada-Romero E, Cunha LD, Magne J, Green DR. LC3-associated phagocytosis and inflammation. J Mol Biol. 2017;429:3561–3576. doi: 10.1016/j.jmb.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heckmann BL, Teubner BJW, Tummers B, Boada-Romero E, Harris L, Yang M, Guy CS, Zakharenko SS, Green DR. LC3-associated endocytosis facilitates beta-amyloid clearance and mitigates neurodegeneration in murine Alzheimer's disease. Cell. 2019;178:536–551. doi: 10.1016/j.cell.2019.05.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heckmann BL, Teubner BJW, Tummers B, Boada-Romero E, Harris L, Yang M, Guy CS, Zakharenko SS, Green DR. LC3-associated endocytosis facilitates beta-amyloid clearance and mitigates neurodegeneration in murine Alzheimer's disease. Cell. 2020a;183:1733–1734. doi: 10.1016/j.cell.2020.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heckmann BL, Teubner BJW, Boada-Romero E, Tummers B, Guy C, Fitzgerald P, Mayer U, Carding S, Zakharenko SS, Wileman T, Green DR. Noncanonical function of an autophagy protein prevents spontaneous Alzheimer's disease. Sci Adv. 2020b;6:eabb9036. doi: 10.1126/sciadv.abb9036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iula L, Keitelman IA, Sabbione F, Fuentes F, Guzman M, Galletti JG, Gerber PP, Ostrowski M, Geffner JR, Jancic CC, Trevani AS. Autophagy mediates interleukin-1beta secretion in human neutrophils. Front Immunol. 2018;9:269. doi: 10.3389/fimmu.2018.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang M, Li R, Lyu J, Li X, Wang W, Wang Z, Sheng H, Zhang W, Karhausen J, Yang W. MCC950, a selective NLPR3 inflammasome inhibitor, improves neurologic function and survival after cardiac arrest and resuscitation. J Neuroinflammation. 2020;17:256. doi: 10.1186/s12974-020-01933-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiao J, Zhao G, Wang Y, Ren P, Wu M. MCC950, a selective inhibitor of NLRP3 inflammasome, reduces the inflammatory response and improves neurological outcomes in mice model of spinal cord injury. Front Mol Biosci. 2020;7:37. doi: 10.3389/fmolb.2020.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin S. The cross-regulation between autophagy and type I interferon signaling in host defense. Adv Exp Med Biol. 2019;1209:125–144. doi: 10.1007/978-981-15-0606-2_8. [DOI] [PubMed] [Google Scholar]
- 30.Kim JY, Zhao H, Martinez J, Doggett TA, Kolesnikov AV, Tang PH, Ablonczy Z, Chan CC, Zhou Z, Green DR, Ferguson TA. Noncanonical autophagy promotes the visual cycle. Cell. 2013;154:365–376. doi: 10.1016/j.cell.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT. Inflammation as a central mechanism in Alzheimer's disease. Alzheimers Dement (N Y) 2018;4:575–590. doi: 10.1016/j.trci.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuijpers M, Azarnia Tehran D, Haucke V, Soykan T. The axonal endo-lysosomal and autophagic systems. J Neurochem. 2020;31:7817–7830. doi: 10.1111/jnc.15287. [DOI] [PubMed] [Google Scholar]
- 33.Kwon HS, Koh SH. Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Transl Neurodegener. 2020;9:42. doi: 10.1186/s40035-020-00221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu J, Wang F. Role of neuroinflammation in amyotrophic lateral sclerosis: cellular mechanisms and therapeutic implications. Front Immunol. 2017;8:1005. doi: 10.3389/fimmu.2017.01005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lonnemann N, Hosseini S, Marchetti C, Skouras DB, Stefanoni D, D’Alessandro A, Dinarello CA, Korte M. The NLRP3 inflammasome inhibitor OLT1177 rescues cognitive impairment in a mouse model of Alzheimer's disease. Proc Natl Acad Sci U S A. 2020;117:32145–32154. doi: 10.1073/pnas.2009680117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu M, Hu G. Targeting metabolic inflammation in Parkinson's disease: implications for prospective therapeutic strategies. Clin Exp Pharmacol Physiol. 2012;39:577–585. doi: 10.1111/j.1440-1681.2011.05650.x. [DOI] [PubMed] [Google Scholar]
- 37.Lv X, Li W, Luo Y, Wang D, Zhu C, Huang ZX, Tan X. Exploring the differences between mouse mAbeta(1-42) and human hAbeta(1-42) for Alzheimer's disease related properties and neuronal cytotoxicity. Chem Commun (Camb) 2013;49:5865–5867. doi: 10.1039/c3cc40779a. [DOI] [PubMed] [Google Scholar]
- 38.Martin PK, Marchiando A, Xu R, Rudensky E, Yeung F, Schuster SL, Kernbauer E, Cadwell K. Autophagy proteins suppress protective type I interferon signalling in response to the murine gut microbiota. Nat Microbiol. 2018;3:1131–1141. doi: 10.1038/s41564-018-0229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martinez J, Malireddi RK, Lu Q, Cunha LD, Pelletier S, Gingras S, Orchard R, Guan JL, Tan H, Peng J, Kanneganti TD, Virgin HW, Green DR. Molecular characterization of LC3-associated phagocytosis reveals distinct roles for Rubicon, NOX2 and autophagy proteins. Nat Cell Biol. 2015;17:893–906. doi: 10.1038/ncb3192. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 40.Martinez J, Cunha LD, Park S, Yang M, Lu Q, Orchard R, Li QZ, Yan M, Janke L, Guy C, Linkermann A, Virgin HW, Green DR. Noncanonical autophagy inhibits the autoinflammatory, lupus-like response to dying cells. Nature. 2016;533:115–119. doi: 10.1038/nature17950. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 41.Muniz-Feliciano L, Doggett TA, Zhou Z, Ferguson TA. RUBCN/rubicon and EGFR regulate lysosomal degradative processes in the retinal pigment epithelium (RPE) of the eye. Autophagy. 2017;13:2072–2085. doi: 10.1080/15548627.2017.1380124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murphy MP, LeVine H., 3rd Alzheimer's disease and the amyloid-beta peptide. J Alzheimers Dis. 2010;19:311–323. doi: 10.3233/JAD-2010-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rai S, Arasteh M, Jefferson M, Pearson T, Wang Y, Zhang W, Bicsak B, Divekar D, Powell PP, Naumann R, Beraza N, Carding SR, Florey O, Mayer U, Wileman T. The ATG5-binding and coiled coil domains of ATG16L1 maintain autophagy and tissue homeostasis in mice independently of the WD domain required for LC3-associated phagocytosis. Autophagy. 2019;15:599–612. doi: 10.1080/15548627.2018.1534507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rizzo F, Riboldi G, Salani S, Nizzardo M, Simone C, Corti S, Hedlund E. Cellular therapy to target neuroinflammation in amyotrophic lateral sclerosis. Cell Mol Life Sci. 2014;71:999–1015. doi: 10.1007/s00018-013-1480-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Serramito-Gomez I, Boada-Romero E, Villamuera R, Fernandez-Cabrera A, Cedillo JL, Martin-Regalado A, Carding S, Mayer U, Powell PP, Wileman T, Garcia-Higuera I, Pimentel-Muinos FX. Regulation of cytokine signaling through direct interaction between cytokine receptors and the ATG16L1 WD40 domain. Nat Commun. 2020;11:5919. doi: 10.1038/s41467-020-19670-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sorbara MT, Ellison LK, Ramjeet M, Travassos LH, Jones NL, Girardin SE, Philpott DJ. The protein ATG16L1 suppresses inflammatory cytokines induced by the intracellular sensors Nod1 and Nod2 in an autophagy-independent manner. Immunity. 2013;39:858–873. doi: 10.1016/j.immuni.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 47.Sumpter R, Jr, Levine B. Selective autophagy and viruses. Autophagy. 2011;7:260–265. doi: 10.4161/auto.7.3.14281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477–489. doi: 10.1038/s41577-019-0165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tian Y, Wang ML, Zhao J. Crosstalk between autophagy and type I interferon responses in innate antiviral immunity. Viruses. 2019;11:132. doi: 10.3390/v11020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y, Sharma P, Jefferson M, Zhang W, Bone B, Kipar A, Bitto D, Coombes JL, Pearson T, Man A, Zhekova A, Bao Y, Tripp RA, Carding SR, Yamauchi Y, Mayer U, Powell PP, Stewart JP, Wileman T. Non-canonical autophagy functions of ATG16L1 in epithelial cells limit lethal infection by influenza A virus. EMBO. 2021;J:e105543. doi: 10.15252/embj.2020105543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu YY, Hsu JL, Wang HC, Wu SJ, Hong CJ, Cheng IH. Alterations of the neuroinflammatory markers IL-6 and TRAIL in Alzheimer's disease. Dement Geriatr Cogn Dis Extra. 2015;5:424–434. doi: 10.1159/000439214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang M, Kenny SJ, Ge L, Xu K, Schekman R. Translocation of interleukin-1beta into a vesicle intermediate in autophagy-mediated secretion. Elife. 2015;4:e11205. doi: 10.7554/eLife.11205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.