Abstract
Early findings suggest the COVID-19 pandemic and related containment measures negatively impact mental wellbeing. This study compared the contribution and relations of three factors to anxiety and wellbeing during the pandemic in June 2020. These factors were: i) Contextual factors (e.g. exposure to COVID-19, being a keyworker, feeling lonely); ii) Cognitive appraisals: perceived vulnerability to disease (PVD) and intolerance of uncertainty (IU); and iii) psychological flexibility (PF). 603 participants aged 18 or older completed an online survey of self-report measures. Hierarchical regression analyses demonstrated PVD, IU and PF predicted state anxiety, and IU and PF predicted mental wellbeing. Some, but not all of the contextual factors also predicted state anxiety and wellbeing. The findings support cognitive appraisal theories and the PF model, lending support to an acceptance and commitment therapy (ACT) approach to public health during pandemics.
Keywords: COVID-19, Psychological flexibility, Cognitive appraisals, Perceived vulnerability to disease, Intolerance of uncertainty
1. Introduction
The combined health-risk, mass disruption and isolation caused by the COVID-19 pandemic has the potential for substantial negative mental health outcomes (Holmes et al., 2020; Kelly, 2020; Mucci et al., 2020). A comparable event, the Severe Acute Respiratory Syndrome (SARS) outbreak of 2002–2003, had a lasting negative impact on the mental health of survivors, with elevated stress levels and psychological distress found one year after the outbreak (Lee et al., 2007) and depression and sleep disruption over 18 months post-infection (Moldofsky & Patcai, 2011). Cross-sectional studies have reported associations between the COVID-19 pandemic and negative psychological outcomes including anxiety, distress, depression, and post-traumatic stress (Moghanibashi-Mansourieh, 2020; Rossi et al., 2020; Shevlin et al., 2020; Wang et al., 2020). These findings are supported by longitudinal studies with pre- and during pandemic data showing decreases in wellbeing and increases in anxiety, mental distress and psychopathological symptoms (Kwong et al., 2020; Schäfer et al., 2020; Twenge & Joiner, 2020). However, a number of studies have found psychological flexibility to be associated with greater wellbeing during the pandemic and to be protective against the negative psychological impacts of the COVID-19 situation (e.g. Chong et al., 2021; Gloster, Lamnisos et al., 2020; McCracken et al., 2021).
Understanding how contextual features of the pandemic interact with psychological variables to influence wellbeing outcomes can help to identify mechanisms that interventions could target. This study aims to compare the contribution and relations between contextual factors, cognitive appraisals and psychological flexibility leading to state anxiety and mental wellbeing during the COVID-19 pandemic.
1.1. Contextual factors
At the time of data collection (June 2020), World Health Organization (WHO) transmission prevention recommendations included hand hygiene, face masks, physical distancing, travel restrictions, banning mass-gathering, infection tracing/quarantining, and school and workplace closure (WHO, 2020a; 2020b). These measures were largely adopted internationally, with further localized restrictions for outbreaks. At this time, the UK and Ireland (87% of participants) were past the peak of the first wave of infections with stay-at-home orders lifted the previous month and non-essential retail reopening throughout the month.
Research has identified a number of contextual factors associated with mental health in pandemics. Factors relating to COVID-19 symptoms and disease exposure are associated with negative psychological outcomes including depression, anxiety and stress (Moghanibashi-Mansourieh, 2020; Wang et al., 2020). Whereas, feeling well-informed about the COVID-19 pandemic is associated with lower anxiety (Jungmann & Witthöft, 2020). Disruption to daily routine and future plans were associated with lower mental wellbeing in previous health crises (Jeong et al., 2016; Mak et al., 2009; Mihashi et al., 2009) and during the COVID-19 pandemic (Williams et al., 2020). Additionally, pandemic-related experiences or ‘impact events’ impact mental wellbeing including trauma experienced by keyworkers (Lee et al., 2007; Wu et al., 2009), loss of income (Shevlin et al., 2020), and being bereaved or unable to care for a loved one who is unwell or dying (Vigo et al., 2020). Social isolation and self-quarantine have been associated with psychological distress (Boyraz et al., 2020; Brooks, 2020; Smith et al., 2020). Conversely, social support is positively associated with mental wellbeing during pandemics (Ko et al., 2006; Xiao et al., 2020).
1.2. Psychological factors
1.2.1. Cognitive appraisals
Cognitive theories of emotions, stress and coping (Clark & Beck, 2010; Smith & Lazarus, 1993), suggest that contextual factors alone will not account for the impact of the pandemic on mental wellbeing, individual differences in cognitive appraisals will also have an influence. Given COVID-19's high transmissibility and persistent uncertainties surrounding the pandemic, it is proposed that differences in threat appraisals relating to infectious disease and uncertainty are highly relevant.
1.2.1.1. Intolerance of uncertainty
Intolerance of uncertainty (IU) is “an individual's dispositional incapacity to endure the aversive response triggered by the perceived absence of salient, key, or sufficient information” (Carleton, 2016, p. 31). It is a biased cognitive appraisal that occurs when an ‘unknown/uncertain’ stimulus is interpreted as aversive, leading to a ‘fear of the unknown’ response (Carleton, 2016). Associations have been found between IU and a range of outcomes (Khawaja, 2011; Saulnier et al., 2019) leading to IU being recognized as a transdiagnostic cognitive vulnerability (Koerner & Dugas, 2008; Mahoney & McEvoy, 2012). Research indicates IU can magnify the negative impact of stressors on mental health, including stress, anxiety and depression (Chen & Hong, 2010; Ciarrochi et al., 2005).
COVID-19 has given rise to multiple stressors and a high degree of uncertainty. In the context of COVID-19, IU has been found to moderate the relationships between social isolation and anxiety and mental wellbeing (Smith et al., 2020), to positively correlate with depression, anxiety and stress (Seco Ferreira et al., 2020), and to have both direct and mediated relationships with anxiety and wellbeing (Rettie & Daniels, 2020; Satici et al., 2020).
1.2.1.2. Perceived vulnerability to disease
Perceived vulnerability to disease (PVD) refers to an appraisal of vulnerability to infectious disease. This study uses Duncan et al.’s (2009) model comprising two dimensions: perceived vulnerability to infectious disease; and germ aversion (emotional discomfort in the presence of perceived pathogens). PVD is concerned with how likely a person thinks they are to contract an infectious disease; how serious they believe the health outcomes would be and how comfortable they are in a perceived infection risk situation. An evolutionary understanding of PVD suggests it is part of the behavioral immune system to avoid pathogens (Park et al., 2003; Schaller & Park, 2011).
In the context of an H1N1 influenza outbreak, Wheaton et al. (2012) found that higher PVD, was associated with anxiety. During the COVID-19 pandemic research has found associations between PVD and general anxiety (Makhanova & Shepherd, 2020) and a relationship between PVD and traumatic stress was mediated by COVID-19 worries and social isolation (Boyraz et al., 2020). It is proposed that those with higher PVD appraisals will overinterpret the severity and likelihood of COVID-19 infection, triggering the behavioral immune system, leading to increased anxiety, avoidant behavior and social withdrawal (Asmundson & Taylor, 2020). It is proposed that this will result in lower mental wellbeing.
1.2.2. Psychological flexibility
Psychological flexibility (PF) is a person's ability to be aware of both external and internal influence factors, to adopt an open and non-defensive stance towards those stimuli, and to engage in actions that move them closer to their own freely chosen valued goals, even in the presence of aversive stimuli (Hayes et al., 2006). A large body of research supports the association of PF with mental wellbeing, and the association of psychological inflexibility with psychological difficulties including depression and anxiety (Doorley et al., 2020; Kashdan & Rottenberg, 2010). A meta-analysis of 63 studies found significant relationships between psychological inflexibility and anxiety (Bluett et al., 2014) and a protective moderating effect of PF has been found for psychological outcomes of daily stressors and threatening life events (Gloster et al., 2017).
It has been proposed that PF may be an antidote to anxiety-induced rigidity in response to COVID-19 related threats (Presti et al., 2020). Supporting this, PF was found to predict wellbeing, stress, depression and affect during the pandemic (Dawson & Golijani-Moghaddam, 2020; Gloster, Lamnisos et al., 2020). During the pandemic PF has also been found to moderate the relationships between social isolation and depression and anxiety (Smith et al., 2020), COVID-19 risk factors and mental health difficulties (Pakenham et al., 2020), COVID-19 stressors and suicide risk (Crasta et al., 2020) and psychological distress within family systems (Daks et al., 2020). Chong et al. (2021) found PF and prosociality mediated the relationship between illness perceptions toward COVID-19 and mental health with PF additionally exerting a direct effect on prosociality.
Empirical evidence supports PF as the mechanism of action of Acceptance and Commitment Therapy (ACT) (Doorley et al., 2020; Ruiz, 2010; Stockton et al., 2019; Trompetter et al., 2015). Addressing mechanisms for change in ACT, a review of 66 component studies found significant positive effect sizes for PF treatment elements and positive outcomes, with larger effect sizes for theoretically specified outcomes (Levin et al., 2012). Further, a review including 20 meta-analyses, 133 studies, and 12,477 participants found ACT to be efficacious for all conditions examined, including anxiety (Gloster et al., 2020). PF therefore presents a promising contender for both understanding how individuals deal with adversity as well as offering a potential focus for interventions to improve wellbeing.
1.3. Aims
The COVID-19 pandemic has heightened anxiety and reduced mental wellbeing and, to some extent, this can be attributed to contextual factors. Research shows PVD and IU are associated with higher anxiety and lower mental wellbeing during the pandemic, and that PF is associated with higher wellbeing and lower anxiety. To date, no study has brought together the full array of contextual factors being considered here alongside the three psychological factors IU, PVD and PF. The aim of this research is to explore the extent to which contextual factors, cognitive appraisals, and psychological flexibility are associated with state anxiety and mental wellbeing during COVID-19, and to identify how they interact in arriving at these outcomes. Understanding these interactions could indicate mechanisms that can be targeted in therapies and in public health campaigns.
1.4. Hypotheses
-
1.
Contextual factors relating to increased social isolation, loneliness, disruption to daily routines and future plans, being ill-informed about COVID-19, and higher COVID-19 exposure (e.g. having to self-isolate) will be associated with higher state anxiety and lower mental wellbeing
-
2.
Higher intolerance of uncertainty and perceived vulnerability to disease will be associated with higher state anxiety and lower mental wellbeing
-
3.
Higher psychological flexibility will be associated with lower state anxiety and higher mental wellbeing
-
4.
Perceived vulnerability to disease will predict higher state anxiety and lower wellbeing directly, and indirectly via intolerance of uncertainty. These pathways will also be moderated (attenuated) by psychological flexibility
2. Method
2.1. Procedure
Sponsorship and ethical approval were gained from The University of Edinburgh. Recruitment adverts were shared via social media, linking to an anonymous survey on the JISC Online Surveys platform (JISC online surveys, 2020). Participants provided informed consent. Participants were required to be 18 years or older and there was no restriction on participant location. The survey consisted of the following questionnaires: demographic information; contextual factors; mental wellbeing; state anxiety; situational loneliness; intolerance to uncertainty, perceived vulnerability to disease and psychological flexibility. On completion, participants were thanked and given information on accessing the summary of findings and how to access mental health support.
2.2. Sample
Using Green's (1991) guide to estimating required sample sizes for regression analysis, an expected medium effect size, 26 predictor variables and a power of .80 (α = .05) a minimum of 258 participants were required.
2.3. Measures
In addition to demographic variables (see Table 1 ), the following measures were completed:
Table 1.
Participant demographic data (n = 603).
| Characteristic | N | % |
|---|---|---|
| Gender | ||
| Male | 118 | 20 |
| Female | 483 | 80 |
| Other | 1a | <1 |
| Prefer not to say | 1 | <1 |
| Age | ||
| 18-24 | 135 | 22 |
| 25-34 | 194 | 32 |
| 35-44 | 82 | 14 |
| 45-55 | 66 | 11 |
| 55-64 | 86 | 14 |
| 65 -74 | 33 | 6 |
| 75+ | 7 | 1 |
| Occupation | ||
| Student (full-time) | 117 | 19 |
| Student (part-time) | 6 | 1 |
| Employed (full-time) | 290 | 48 |
| Employed (part-time) | 80 | 13 |
| Unemployed | 27 | 5 |
| Other | 83 | 14 |
| Country of residence | ||
| UK–England | 150 | 25 |
| UK–Northern Ireland | 178 | 30 |
| UK–Scotland | 136 | 22 |
| UK–Wales | 13 | 2 |
| Ireland | 47 | 8 |
| China | 28 | 5 |
| United States | 22 | 4 |
| Other European | 11 | 1 |
| Other Worldwide | 18 | 3 |
One participant recorded preferred gender as non-binary.
1. COVID-19 contextual factors
Self-report items were developed to capture COVID-19 contextual factors including: being a keyworker, disruption, financial security, infection status/exposure, family and friends' infection status and exposure, recent bereavement, adherence to public health measures, leaving the home and contact with others (see Table 2 ). Three items relating to leaving the home and contact with others were grouped together as ‘external contact’ for analysis.
Table 2.
COVID-19 contextual measures.
| Item | Response scale |
|---|---|
Situation
|
Yes/no Yes/no Yes/no |
Infection status
|
Yes/no Yes/no Yes/no |
Bereavement
|
Yes/no Yes/no |
Mental Health
|
Yes/no No-it's the same Yes-it has been worse Yes-it has been better |
External contact
|
|
Understanding and impact of COVID-19
|
|
Two measures relating to loneliness were included. The first measured situational loneliness using the social loneliness subscale of the Social and Emotional Loneliness Scale for Adults short-form (SELSA-S; DiTommaso et al., 2004). Although a psychological factor, in this study social loneliness is positioned as a contextual factor to measure meaningful social contact in the current situation. The second loneliness measure was a 1-item self-report measure of increased loneliness, answered on a five-point Likert scale of agreement: “I feel more lonely now than before the pandemic”.
2. Intolerance of uncertainty.
IU was measured using the short form Intolerance of Uncertainty Scale (IUS-12; Carleton et al., 2007). This 12-item version of the IUS (Freeston et al., 1994) measures reactions to ambiguous situations, uncertainty and future events. The IUS-12 has a two-factor structure: prospective anxiety and inhibitory anxiety (Carleton et al., 2007). All items are scored from 1 (not at all characteristic of me) to 5 (entirely characteristic of me). The IUS-12 has been found to have excellent internal consistency of α = 0.93 for the full scale and good internal consistency for subscale scores α = 0.89 (prospective IU) and α = 0.89 (inhibitory IU) (Carleton et al., 2013). For this sample the full scale had α = 0.92 and subscale scores α = 0.86 (prospective IU) and α = 0.88 (inhibitory IU).
3. Perceived vulnerability to disease.
Perceived vulnerability to infectious disease was measured using the Perceived Vulnerability to Disease Questionnaire (PVDQ; Duncan et al., 2009). The PVDQ is comprised of two subscales: Perceived Infectability and Germ Aversion. All items are scored from 1 (strongly disagree) to 7 (strongly agree) with higher scores indicating higher perceived vulnerability. The PVDQ has demonstrated good internal consistency α = 0.82 for all items and the subscale Perceived Infectability subscale (α = 0.87), and adequate internal consistency for the Germ Aversion subscale (α = 0.74) (Duncan et al., 2009). For this sample, all items had α = 0.80 and the subscales had α = 0.81 (Perceived Infectability) and α = 0.88 (Germ Aversion).
4. Psychological flexibility
The Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT; Francis et al., 2016) is a general measure of psychological flexibility processes. The CompACT has demonstrated a stable three factor model: openness to experience; behavioral awareness; and valued action (Francis et al., 2016). All 23 items are scored from 0 (strongly disagree) to 6 (strongly agree). Higher scores indicate higher psychological flexibility. The CompACT has demonstrated excellent internal consistency for all items α = 0.91, and good to excellent internal consistency for each of the subscales, openness to experience α = .90; behavioral awareness α = 0.87; and valued action α = 0.90 (Francis et al., 2016). For this sample, all items had α = 0.89 and the subscales had α = 0.82 (openness to experience), α = 0.82 (behavioral awareness) and α = 0.88 (valued action).
5. Anxiety.
The Current Anxiety Level Measure (CALM; Marris et al., 2017) was used to measure state anxiety. State anxiety was chosen over trait anxiety as trait measures of anxiety reflect more stable anxiety phenomena. In contrast, in the moment experiences of anxiety would be more likely to be context sensitive to the immediate anxiety producing features of the pandemic. CALM consists of 16 items asking participants to rate the extent each statement applies to them in the current moment from 0 (not at all) to 4 (extremely). Higher scores indicate a higher level of state anxiety. The CALM has strong concurrent validity (r = 0.90, p = .001) with the state dimension of the validated State-Trait Anxiety Inventory (STAI; Spielberger et al., 1983), suggesting CALM can accurately measure state anxiety. For this sample CALM showed excellent internal reliability with α = 0.96.
6. Mental wellbeing
The Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS) was used to measure mental wellbeing. It is a 7-item version of the 14-item Warwick-Edinburgh Mental Well-being Scale (WEMWBS; Stewart-Brown et al., 2009) for monitoring mental wellbeing in the general population. The scale covers feeling and functioning aspects of mental wellbeing and items are scored from 1 (none of the time) to 5 (all of the time). Higher scores indicate higher mental wellbeing. Internal validity of the SWEMWBS has been demonstrated as good to excellent (α = 0.84; Fat et al., 2017). For this sample the SWEMWBS had α = 0.84.
2.4. Recruitment
A convenience sample of 609 participants completed the survey between 22nd and 29th June 2020. One participant was excluded for selecting the lowest response to every item, suggestive of a non-attentive responder. Missing data for five participants was classed as missing completely at random (MCAR) using Little's MCAR test (χ2 = 109.608, df = 89, p = .068). Being MCAR and less than 1% of the sample from a large data set, exclusion of these cases was not seen to introduce bias (Tabachnick & Fidell, 2014). This resulted in a total sample of 603.
2.5. Data analyses
Data analyses were conducted using SPSS (Version 25; IBM Corp, 2017). Descriptive statistics were calculated for demographic variables, contextual factors and psychological scales. Correlation analyses were carried out to determine relationships between demographic and COVID-19 contextual variables with the outcome variables state anxiety and wellbeing. Dichotomous contextual variables (e.g. needing to self-isolate, being a keyworker) were used to test for differences in anxiety and wellbeing using t-tests. Demographic variables and COVID-19 contextual variables significantly associated with the outcome variables at p < .01 were carried forward to the regression analyses as control and predictor variables. Correlation analyses (Pearson's r) were run to identify relations between the six psychological measures (IUS-12, PVDQ, COMPACT, SELSA-S, CALM and SWEMWBM).
Two hierarchical multiple regression analyses were run for the outcome variables state anxiety and mental wellbeing to determine the total variance predicted by the models and the unique contribution of each predictor. Control variables were entered in the first step, followed by COVID-19 contextual factors, and finally cognitive appraisals and PF. Conditional Process Analysis (Hayes, 2017) was used to test the moderated mediation hypothesis that PVD would directly predict anxiety and wellbeing and indirectly via IU, and that these direct and indirect effects would be moderated (attenuated) by PF. The model was tested using bootstrapped confidence intervals with 10,000 resamples, using model 59 in PROCESS for SPSS (Version 3.5; Hayes, 2020).
3. Results
3.1. Sample characteristics
The 603 participants were aged 18 to 82, with the majority (54%) in the age bracket 18–34, 80% were female and 20% male. The majority (61%) were employed, and 20% were students. Most participants were from the United Kingdom (79%). Table 1 outlines the demographic data. Table 3, Table 4 present the contextual factor descriptive statistics and correlations with state anxiety and wellbeing. Table 5 presents descriptive statistics for the psychological measures.
Table 3.
COVID-19 contextual factors (n = 603).
| Yes (%) | No (%) | |
|---|---|---|
| Variable | ||
| Lives alone | 89 (15) | 514 (85) |
| Keyworkera | 186 (31) | 417 (69) |
| Responsibility for others | 256 (42) | 347 (58) |
| Required to self-isolate | 161 (27) | 442 (73) |
| Friends/family positive symptoms | 196 (32) | 407 (68) |
| Friends/family hospital treatment | 50 (8) | 553 (92) |
| Recently bereaved | 68b (11) | 535 (89) |
| Mental health treatment/support | 66 (13) | 526 (87) |
Keyworker: providing an essential service; b: 35% of participants recently bereaved stated bereavement was due to COVID-19.
Table 4.
Contextual factor correlations.
| Variable | Mean | SD | Correlation state anxiety | Correlation Wellbeing |
|---|---|---|---|---|
| External contacta | 9.08 | 2.08 | -.14** | .15** |
| To what extent do you agree with the follow statements:b | ||||
| I feel well informed about the Covid-19 situation in my country | 3.57 | 1.03 | -.19*** | .19*** |
| I have followed government advice for my country (e.g., social/physical distancing, shielding, handwashing) | 4.35 | .72 | .06, ns | .05, ns |
| My daily routine has been disrupted | 4.24 | .88 | .16*** | -.17*** |
| My plans for the future have been affected | 4.02 | 1.04 | .21*** | -.19*** |
| I have a good level of social support | 3.91 | .876 | -.25*** | .37*** |
| I feel more lonely now than before the pandemic | 2.95 | 1.21 | .37*** | -.41*** |
| I have lost income or will likely lose income as a result of the Covid-19 situation | 2.74 | 1.48 | .16*** | -.14** |
Total score from 3-items, ratings for each item ranged from 1 (not at all) to 5 (several times a day).
ratings ranged from 1 (strongly disagree) to 5 (strongly agree); all correlations are Pearson's r, *p < .05, **p < .01, ***p < .001.
Table 5.
Descriptive statistics for psychological measures.
| Variable | Possible range | Min | Max | Mean | SD | α |
|---|---|---|---|---|---|---|
| Predictor variables: | ||||||
| SELSA-S Soc. | 7–35 | 5 | 33 | 11.94 | 6.16 | .86 |
| IUS-12 – Total | 12–60 | 12 | 60 | 29.28 | 10.15 | .92 |
| Prospective anxiety | 7–35 | 7 | 35 | 18.34 | 6.03 | .86 |
| Inhibitory anxiety | 5–25 | 5 | 25 | 10.93 | 4.77 | .88 |
| PVDQ – Total | 15–105 | 20 | 99 | 58.76 | 14.53 | .80 |
| PVDSQ (item level) | 1–7 | 1 | 7 | 3.91 | 2.05 | |
| Perceived Infectability | 7–49 | 7 | 49 | 24.62 | 9.03 | .85 |
| Germ Aversion | 8–56 | 10 | 56 | 34.13 | 9.14 | .72 |
| CompACT total | 0–138 | 21 | 136 | 84.45 | 20.32 | .89 |
| Openness to Experience | 0–60 | 2 | 60 | 32.08 | 11.22 | .82 |
| Behavioural Awareness | 0–30 | 0 | 30 | 17.20 | 6.79 | .82 |
| Valued Action | 0–48 | 0 | 48 | 35.17 | 8.11 | .88 |
| Outcome variables: | ||||||
| SWEMWBS | 7–35 | 7.00 | 35.00 | 21.20 | 3.52 | .84 |
| CALM Anxiety | 0–64 | 0 | 60 | 15.05 | 12.80 | .96 |
SELSA-S Soc: Social and Emotional Loneliness Sale for Adults (short-form) Social subscale, IUS-12: Intolerance of Uncertainty Scale, PVDQ: Perceived Vulnerability to Disease Questionnaire, CompACT: Comprehensive assessment of Acceptance and Commitment Therapy Processes, SWEMWBS: Short Warwick-Edinburgh Mental Wellbeing Scale, CALM: Current Anxiety Level Measure.
3.2. Covariate analysis
Age had a moderate negative correlation with state anxiety (r = - 0.30 p < .001) and a small positive correlation with mental wellbeing (r = 0.26, p < .001). For mental wellbeing, male participants scored significantly higher (M: 22.12, SD: 3.78) than female participants (M: 20.97, SD: 3.42), t 599 = 3.20, p = .001. For state anxiety, female participants scored significantly higher (M: 16.24, SD: 13.14) than male participants (M: 10.36, SD: 10.12), t 599 = −5.31, p < .001. For those with an existing mental health difficulty, state anxiety scores were significantly higher (M: 25.03, SD: 15.00 vs' M: 13.59, SD: 0.513), t 601 = - 6.41, p < .001. Wellbeing scores were significantly lower for those with existing mental health difficulty (M: 19.10; SD: 2.64 vs’ M: 21.51, SD: 3.53), t 601 = 7.12, p < .001.
3.3. Hypothesis analyses
3.3.1. Contextual factors
A number of contextual variables were associated with state anxiety and wellbeing at statistically significant levels (Table 4). However, the overall magnitude of these correlations was relatively weak, with the exception of good social support and increased loneliness. Those who had been required to self-isolate had higher state anxiety (M:17.88, SD: 13.41) than those who had not (M: 14.02, SD: 12.43), t601 = −3.31, p = .001, d = .30). Contrary to hypothesis, keyworkers had significantly higher wellbeing (M: 22.01, SD: 3.61) than non-keyworkers (M: 20.84, SD: 3.42, t601 = - 3.81, p < .001, d = 0.33).
3.3.2. Correlation analysis
Table 6 shows a pattern of correlation between the psychological measures consistent with hypotheses.
Table 6.
Correlations between psychological measures.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. IUS-12 | 1 | |||||
| 2. PVDQ | .32** | 1 | ||||
| 3. SELSA-S Soc | .16** | .22** | 1 | |||
| 4. CompACT | -.58** | -.32** | .22** | 1 | ||
| 5. CALM | .53** | .37** | .33** | -.50** | 1 | |
| 6. SWEMWBS | -.41** | -.25** | -.39** | .52** | -.57** | 1 |
All correlations are Pearson's r: n = 603; ** Correlation is significant at the 0.01 level (2-tailed).
IUS-12: Intolerance of Uncertainty Scale, PVDQ: Perceived Vulnerability to Disease Questionnaire, SELSA-S Soc: Social and Emotional Loneliness Sale for Adults (short-form) Social subscale, CompACT: Comprehensive assessment of Acceptance and Commitment Therapy Processes, CALM: Current Anxiety Level Measure, SWEMWBS: Short Warwick-Edinburgh Mental Wellbeing Scale.
3.3.3. Regression analysis
3.3.3.1. Prediction of state anxiety
Hierarchical regression results are displayed in Table 7 . Gender, age and mental health difficulty were entered in Step 1 and accounted for 17.5% of the variance in state anxiety. The addition of COVID-19 contextual factors in Step 2 significantly improved the model, accounting for an additional 19.6% of the variance. After entry of the CompACT, PVDQ and IUS-12 measures in Step 3, the final model accounted for 48.7% of the variance in state anxiety, significantly improving the model and accounting for an additional 11.6% of the variance.
Table 7.
Hierarchical regression analysis for variables predicting state anxiety.
| Variable | Β | t | p | R | R2 | Δ R2 | F | p |
|---|---|---|---|---|---|---|---|---|
| Step 1 | .42 | .18 | .18 | 44.40 | <.001 | |||
| Gender | .11 | 2.870 | .004 | |||||
| Age | -.26 | −7.003 | <.001 | |||||
| Mental health difficulty | .27 | 7.135 | <.001 | |||||
| Step 2 | .61 | .37 | .20 | 28.97 | <.001 | |||
| Gender | .13 | 3.987 | <.001 | |||||
| Age | -.23 | −6.725 | <.001 | |||||
| Mental health difficulty | .18 | 5.359 | <.001 | |||||
| Self-isolated | .10 | 2.838 | .005 | |||||
| External contact | -.01 | -.341 | .733 | |||||
| Well-informed | -.09 | −2.772 | .006 | |||||
| Daily routine disruption | .06 | 1.669 | .096 | |||||
| Future plans impacted | .12 | 3.226 | .001 | |||||
| Good social support | -.03 | -.751 | .453 | |||||
| Increased loneliness | .19 | 5.253 | <.001 | |||||
| Lost income | .07 | 2.141 | .033 | |||||
| SELSA-S soc | .22 | 5.863 | <.001 | |||||
| Step 3 | .70 | .49 | .12 | 37.15 | <.001 | |||
| Gender | .12 | 3.819 | <.001 | |||||
| Age | -.12 | −3.531 | <.001 | |||||
| Mental health difficulty | .94 | 2.957 | .003 | |||||
| Self-isolated | .05 | 1.628 | .104 | |||||
| External contact | -.02 | -.752 | .452 | |||||
| Well-informed | -.08 | −2.452 | .014 | |||||
| Daily routine disruption | .07 | 2.006 | .045 | |||||
| Future plans impacted | .08 | 2.558 | .011 | |||||
| Good social support | -.02 | -.501 | .617 | |||||
| Increased loneliness | .13 | 3.798 | <.001 | |||||
| Lost income | .06 | 1.864 | .063 | |||||
| SELSA-S soc | .15 | 4.237 | <.001 | |||||
| CompACT | -.13 | −3.328 | .001 | |||||
| IUS-12 | .24 | 6.137 | <.001 | |||||
| PVDQ | .14 | 4.369 | <.001 |
SELSA-S Soc: Social and Emotional Loneliness Sale for Adults (short-form) Social subscale, CompACT: Comprehensive assessment of Acceptance and Commitment Therapy processes, IUS-12: Intolerance of Uncertainty Scale, PVDQ: Perceived Vulnerability to Disease Questionnaire.
Both situational loneliness (β = 0.148, p < .001) and increased loneliness (β = 0.128, p < .001) made significant contributions. Both disruption to daily routine (β = 0.068, p < .05) and impact on future plans (β = 0.084, p < .05) made smaller but significant positive contributions. As expected, being well-informed about the COVID-19 situation was a significant negative predictor of state anxiety (β = −0.075, p < .05). As hypothesized, both types of cognitive appraisals were significant predictors of state anxiety. IU (β = 0.237, p < .001) was found to make a larger contribution than PVD (β = 0.141, p < .001). Finally, PF was a significant negative predictor of state anxiety (β = −0.134, p < .001).
3.3.3.2. Prediction of wellbeing
Hierarchical regression results are displayed in Table 8 . Gender, age and mental health difficulty were entered in Step 1 and accounted for 11.5% of the variance in mental wellbeing. The addition of the COVID-19 contextual factors in Step 2 significantly improved the model, accounting for an additional 28% of the variance. After entry of CompACT, PVDQ and IUS-12 measures in Step 3, the final model accounted for 46.5% of the variance, significantly improving the model and accounting for an additional 7% of the variance in mental wellbeing.
Table 8.
Hierarchical regression analysis for variables predicting wellbeing.
| Variable | β | t | p | R | R2 | Δ R2 | F | p |
|---|---|---|---|---|---|---|---|---|
| Step 1 | .34 | .12 | .12 | 25.88 | <.001 | |||
| Gender | -.07 | −1.831 | .068 | |||||
| Age | .23 | 6.009 | <.001 | |||||
| Mental health difficulty | -.20 | −5.220 | <.001 | |||||
| Step 2 | .63 | .40 | .28 | 32.05 | <.001 | |||
| Gender | -.10 | −2.961 | .003 | |||||
| Age | .20 | 6.009 | <.001 | |||||
| Mental health difficulty | -.10 | −3.020 | .003 | |||||
| Key worker | .13 | 3.840 | <.001 | |||||
| External contact | -.01 | -.432 | .666 | |||||
| Well-informed | .09 | 2.610 | .009 | |||||
| Daily routine disruption | -.10 | −2.680 | .008 | |||||
| Future plans impacted | -.09 | −2.526 | .012 | |||||
| Good social support | .14 | 3.784 | <.001 | |||||
| Increased loneliness | -.21 | −5.968 | <.001 | |||||
| Lost income | -.02 | -.436 | .663 | |||||
| SELSA-S soc. | -.25 | −6.867 | <.001 | |||||
| Step 3 | .68 | .47 | .07 | 34.01 | <.001 | |||
| Gender | -.10 | −3.087 | .002 | |||||
| Age | .11 | 3.230 | .001 | |||||
| Mental health difficulty | -.02 | -.626 | .532 | |||||
| Keyworker | .10 | 3.234 | .001 | |||||
| External contact | .01 | .112 | .911 | |||||
| Well-informed | .07 | 2.316 | .021 | |||||
| Daily routine disruption | -.11 | −3.118 | .002 | |||||
| Future plans impacted | -.07 | −2.027 | .043 | |||||
| Good social support | .12 | 3.293 | .001 | |||||
| Increased loneliness | -.17 | −5.003 | <.001 | |||||
| Lost income | -.01 | -.105 | .916 | |||||
| SELSA-S soc | -.18 | −5.139 | <.001 | |||||
| CompACT | .26 | 6.250 | <.001 | |||||
| IUS-12 | -.08 | −2.097 | .036 | |||||
| PVDQ | -.03 | -.799 | .425 |
SELSA-S Soc: Social and Emotional Loneliness Sale for Adults (short-form) Social subscale, CompACT: Comprehensive assessment of Acceptance and Commitment Therapy processes, IUS-12: Intolerance of Uncertainty Scale, PVDQ: Perceived Vulnerability to Disease Questionnaire.
Situational loneliness (β = −0.183, p < .001) and increased loneliness (β = −0.172, p < .001) both made significant contributions to the model. For factors relating to social interaction, only good social support made a significant contribution (β = 0.474, p < .01). Disruption to daily routine (β = - 0.108, p < .01) and impact on future plans (β = - 0.068, p < .05) both made significant contributions to the model. Loss of income did not make a significant contribution and being a keyworker had the opposite to expected effect (being a key worker was associated with greater rather than poorer wellbeing). As expected, being well-informed about the COVID-19 situation made a significant positive contribution to the model (β = 0.073, p < .05). From the cognitive appraisals, only IU was a significant negative predictor of mental wellbeing (β = −0.083, p < .05). Finally, as expected, PF was associated with higher mental wellbeing as a significant positive predictor (β = 0.257, p < .001), and made the largest unique contribution to the final model.
All assumptions of normality, linearity, multicollinearity and homoscedasticity were met. The data met the assumption of independent errors with Durbin-Watson values of 1.96 (anxiety) and 2.00 (wellbeing). Variance inflation factor (VIF) and tolerance statistics were within accepted ranges (Field, 2018). All cases had Cook's distance less than 1 and leverage values and Mahalanobis distances within the acceptable range (Field, 2018).
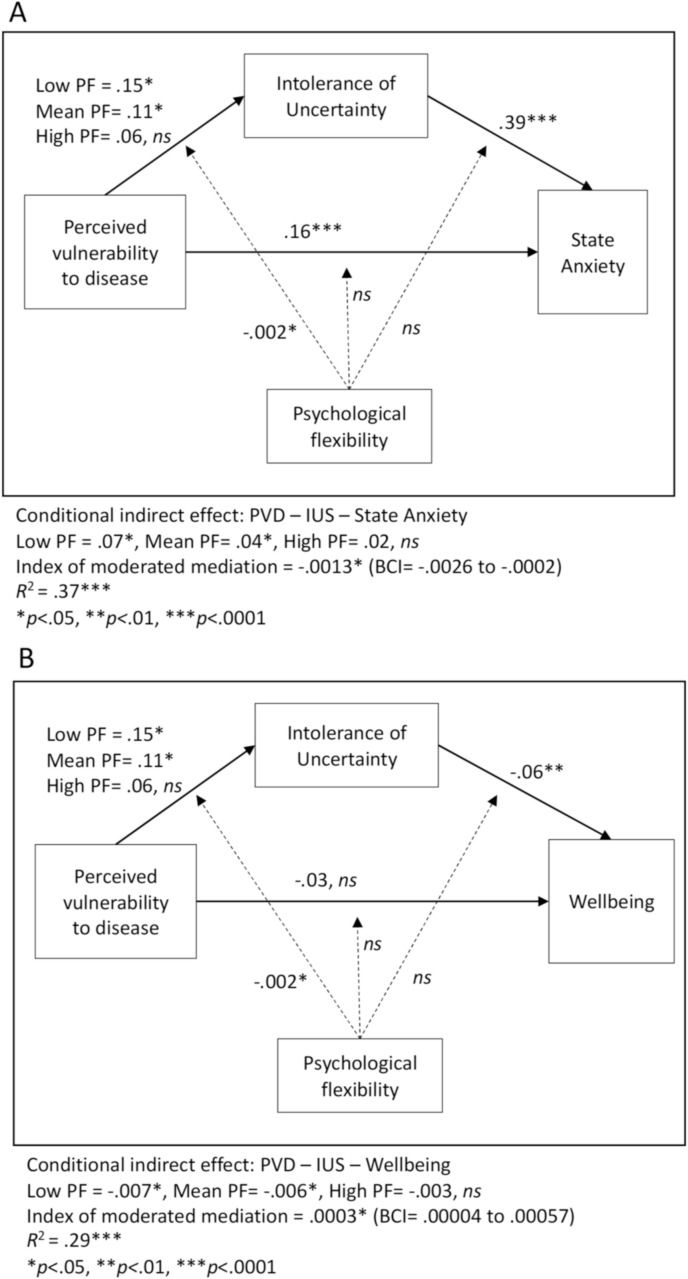
Fig. 1 shows the conditional process models. Panel A shows that PVD had both direct influences on state anxiety, and indirect influences via IU. The indirect path was moderated by PF, such that at high levels of flexibility the indirect path was no longer significant. Panel B shows the same pattern of moderated mediation for the outcome of wellbeing, though the direct path from PVD to wellbeing was not significant in this model. These models account for significant portions of variance in the dependent variables. The mediation effects are relatively strong, based on the beta values shown on the paths. The moderation of those effects by PF was significant, but was a relatively weak effect.
Fig. 1.
Conditional Process Model predicting state anxiety (Panel A) and wellbeing (Panel B).
4. Discussion
This research explored the extent to which contextual factors, cognitive appraisals (IU and PVD) and PF were associated with state anxiety and mental wellbeing during the COVID-19 pandemic. Some, but not all of the contextual factors had the hypothesized associations with state anxiety and wellbeing. Having to self-isolate was not a significant predictor. This is surprising given research on self-quarantine in previous non-COVID infection outbreaks (Brooks, 2020) and is perhaps indicative of an absence or minimising of stressors associated with previous situations requiring self-quarantine. For example, as COVID-19 self-isolation mainly takes place in the individual's home, typically with access to communication technologies, there may have been less loneliness, boredom and frustration than found in studies of previous pandemics and epidemics reviewed by Brooks (2020). Finding a similar disparity with the findings of Brooks (2020), Gloster, Lamnisos et al. (2020) suggest the difference may stem from the largescale lockdowns during the COVID-19 pandemic creating a sense of unity not present in previous infection outbreaks.
The finding that age had a significant moderate negative correlation with state anxiety is interesting given the health threat from COVID-19 increases with age (Docherty et al., 2020). Other studies have also found higher anxiety in younger age groups during the pandemic (Fancourt et al., 2020; Rossi et al., 2020). We suggest these findings provide evidence for stressors beyond a threat to health, suggesting containment measures themselves are also associated with increased anxiety. Kwong et al. (2020) suggest the threat of rapid change in society during the pandemic has led to higher anxiety levels in younger people, who may feel more vulnerable to this change as typically have less housing and financial security. Further, the finding is consistent with studies of ageing, that show older people experience better emotion regulation than younger adults (e.g. Carstensen et al., 2011).
Cognitive appraisals were found to be significantly associated with state anxiety and to some extent mental wellbeing. As hypothesized higher levels of PVD predicted higher state anxiety. Unexpectedly, PVD was not found to be a significant predictor of wellbeing. It had been proposed that higher PVD would lead to avoidant behavior and social withdrawal, resulting in lower mental wellbeing. Perhaps not enough time passed for avoidant behavior to impact wellbeing. Also, in the context of COVID-19, where avoidant behavior is encouraged and opportunities to socialize out of the home are diminished, these behaviors may not negatively impact mental wellbeing in the way they would in another context. As hypothesized, higher IU was associated with both higher state anxiety and lower mental wellbeing. This is consistent with findings that IU is both directly related to anxiety (Rettie & Daniels, 2020) and can moderate the impact of social isolation and stressors on anxiety (Chen & Hong, 2010; Ciarrochi et al., 2005; Smith et al., 2020). That PVD predicted only state anxiety, and IU predicted both anxiety and wellbeing suggests IU has broader psychological implications than PVD.
As hypothesized, PF predicted lower state anxiety and higher mental wellbeing. This is consistent with previous findings that higher PF is associated with positive psychological outcomes (Hayes et al., 2006) and a protective factor moderating the impact of daily stressors and threatening life events for depression, anxiety and life satisfaction (Gloster et al., 2017). This finding is also consistent with COVID-19 related findings that PF has direct effects on wellbeing (Dawson & Golijani-Moghaddam, 2020; Gloster, Lamnisos et al., 2020; McCracken et al., 2021) and a moderating role between the psychological impacts of COVID-19 and mental health outcomes and wellbeing (Chong et al., 2021; Crasta et al., 2020; Daks et al., 2020; Pakenham et al., 2020; Smith et al., 2020). The current study supports these findings through replication and extends them by contrasting these variables with other predictors to establish their relative associations with anxiety and wellbeing.
The conditional process models supported the hypotheses that the impact of PVD on state anxiety and wellbeing would be mediated by IU, and that this would be buffered at high levels of PF. Whilst significant, this moderating effect was relatively weak, in comparison to the direct influence that PF had on state anxiety and wellbeing as shown in the regression analyses.
4.1. Theoretical implications
Cognitive accounts describe how anxiety is the outcome of a threat appraisal where threat is perceived alongside an inability to cope with it (Clark & Beck, 2010; Smith & Lazarus, 1993). The findings that PVD and IU predict anxiety are consistent with these models as PVD and IU are threat appraisals based on biased assumptions and beliefs about perceived infectability and outcomes of infection (Duncan et al., 2009) and the threat of experiencing uncertainty (Carleton, 2016).
Supporting theories of PF (Kashdan & Rottenberg, 2010), we found increased PF negatively predicted state anxiety and positively predicted mental wellbeing. The negative contribution of PF to anxiety does not contradict cognitive accounts of anxiety. Arch and Craske (2008) describe how PF processes (cognitive defusion, acceptance) are applied to coping with threat-related thoughts. It is proposed that these processes are likely to be applied to secondary appraisals and reappraisals, moderating feedback into the cognitive system that would otherwise perpetuate maladaptive anxiety (Clark & Beck, 2010). PF's ability to predict mental wellbeing may also explain its association with lower anxiety as negative affectivity is recognized as a vulnerability to anxiety (Clark & Beck, 2010). Therefore, higher mental wellbeing may provide a better mode for dealing with threats during the pandemic.
PF did buffer the impact of PVD and IU on state anxiety and wellbeing, and PF and IU were strongly correlated. The relationship between them is of interest due to the strength of findings of IU as an explanatory mechanism in anxiety (e.g. Shihata et al., 2016), and the strength of association between IU and PF. Previous studies have found a similar magnitude of correlation between PF and IU as reported in this study (r = 0.55 - 0.65, Smith et al., 2020; Stevens et al., 2018). Furthermore, an RCT of ACT versus CBT for GAD found that IU improved in both conditions, with the ACT group performing slightly better (Avdagic et al., 2014).
Smith et al. (2020) conceptualised IU as a specific manifestation of PF (difficulty accepting thoughts and feelings related to uncertainty and a behavioral orientation towards emotional control). Merwin et al. (2011) further described intolerance of the uncertainty of bodily functions and appetite as a core feature in their PF conceptualization of Anorexia Nervosa. These features drive rigid rule following and behaviors oriented at control, characteristic of psychological inflexibility.
Whilst IU is considered to be principally a cognitive construct, coming from a cognitive approach to emotional disorders, it also has emotional, physiological and behavioral facets. PF on the other hand has roots within a behavioral approach to language and cognition. These philosophical and ontological differences are not easily resolved by appeal to the empirical data. Furthermore, these distinctions are not likely to be meaningful to participants responding to self-report items that measure IU and PF, and the data shows substantial shared variance in those responses. Looking at the items themselves shows considerable overlap. Some items from the IUS (e.g. “When it's time to act, uncertainty paralyses me” and “When I am uncertain I can't function very well”) suggest a process of behavioral inhibition due to cognitive events, conceptually similar to psychological inflexibility. Furthermore, some items from the CompACT such as “I find it difficult to stay focussed on what's happening in the present” are suggestive of the prospective anxiety construct in IU. Where the items share the greatest overlap is in behavioral inhibition by cognitive events, with items from both scales appearing to measure this kind of process. Factor analytic studies could explore if common factors underlie responding to these items, though that analysis is beyond the scope of the current paper.
From an ACT perspective, intervention using these constructs would seek to enhance a person's awareness of the function of their behavior, that is, attempting to reduce anxiety. The effectiveness and the costs of such behaviors would be explored, and if greater tolerance of uncertainty appeared to be a functional goal for effective living, that could be pursued using openness skills such as willingness and defusion strategies. If greater tolerance of uncertainty occurred as a result of those contextual influences, it would be regarded as a by-product of altering the functional relations between appraisals, behaviors and valued outcomes, rather than as a core cognitive driver of such change, which would be the interpretation from a cognitive perspective. From within this perspective, greater tolerance of uncertainty would be seen as a manifestation of increased PF.
A cognitive perspective, in contrast, would be likely to view the various ACT strategies described above as behavioral experiments that alter the appraisal of the ‘awfulness’ of not being certain. Where the two models share common ground is in conceptualising the importance of increasing behavioral action, in the presence of the repertoire narrowing stimulus of uncertainty, and in increasing awareness of the tendency of people who experience a high degree of IU to anxiously live in the future. Ultimately, both IU and PF are clinical heuristics that orient therapists towards potential treatment targets. They are not precise descriptions of functionally-defined and manipulable processes; they are ways of talking about clinical phenomena that serve a purpose. They must therefore be judged (from a contextual behavioral science perspective) not according to which account is more accurate, but instead according to the scientific goals of prediction and influence, within a specific context. The context of discussion in a journal article is different for example than the context of a therapy room, or of recommending psychological tools for public health intervention in the time of pandemics. Which of these accounts leads to greater prediction and influence may well differ across these contexts.
4.2. Clinical implications
Ongoing risk of infection and containment measures make it difficult to target most contextual factors for change. One exception is feeling well-informed about the situation, which could be targeted with clear public messaging. Psychological factors, on the other hand, can be targeted for change. Our findings support cognitive appraisal theories typically associated with CBT. Interventions based on this framework should help people to more accurately appraise the likelihood of contracting the virus while framing susceptibility as influenced by an ability to engage in public health behaviors (e.g. hand washing, limiting contact with others). In an uncertain context, focussing on what is certain, that is our capacity to control our own behavior in the service of protecting ourselves and those around us, may also reduce uncertainty.
The transdiagnostic nature of ACT makes it highly suitable for individual interventions for COVID-19 related anxiety, and also society-wide public-health interventions. Discussing approaches to increasing PF in an entire population, Levin et al. (2016) consider the use of the internet, mass-media, tip lists and education programmes, suggesting the Triple P programme as an exemplar delivery approach. Mobile phone apps are another contender for society-wide ACT delivery (Levin, Pierce, & Schoendorff, 2017). No study to date has evaluated a society-wide ACT intervention, however, empirical support can be found in studies using non-clinical populations. For example, ACT workshops for staff in a special education setting were found to influence factors affecting depression, stress, and burnout (Biglan et al., 2013) and a web-based self-help programme for college students was found to have positive outcomes on a range of psychological difficulties and positive mental health (Levin, Haeger, et al., 2017). Further, ACT training for people with mild-to-moderate depression and anxiety in a non-clinical sample had positive outcomes for mental health and wellbeing (Fledderus et al., 2012, 2013). Future research could evaluate a pilot public health ACT intervention following Levin et al.’s (2016) suggestions of replicating the Triple P model and incorporating web-based and mobile app delivery.
4.3. Limitations
The cross-sectional study design prevented causal inferences being made and self-report measures may have introduced subjective bias affecting accuracy and reliability. However, anonymity may have mitigated against perceived social desirability bias. The use of social media for recruitment of a convenience sample means it is unlikely to be representative of the public more widely. Therefore, the findings remain tentative and need replication in a more randomly selected sample. Additionally, few participants were recruited from outside the UK and Ireland, limiting conclusions about country of residence. Another potential weakness may come from the use of a current-state anxiety measure. A state measure of anxiety was chosen to capture sensitivity to context, in comparison to trait-based measures, this sensitivity may however have been gained at the expense of stability. For example, people may be less likely to complete an online survey when feeling highly anxious or alternatively complete the survey when experiencing uncharacteristically elevated anxiety symptoms. This may lead to either an over or under estimate of the level of anxiety in the sample.
Given the uniqueness of the COVID-19 situation, selection of predictor and outcome variables relied on logical and theoretical reasoning as well as previous research. Therefore, observed relationships may in practice be reversed or bidirectional. The contextual factors were not standardized measures, but were face valid, designed to capture aspects of the context that were considered likely to influence wellbeing and anxiety. Despite these limitations, the model predicting state anxiety and the model predicting wellbeing were both significant and a broad range of predictor variables covering both contextual and psychological factors were investigated.
5. Conclusion
The findings of this study suggest contextual factors, cognitive appraisals and psychological flexibility are associated with state anxiety and mental wellbeing during the COVID-19 pandemic. Contextual factors related to loneliness and disruption made the largest contributions to state anxiety and mental wellbeing. Biased cognitive appraisals of uncertainty predicted both anxiety and wellbeing, whereas biased cognitive appraisals relating to the threat of infection predicted only state anxiety. As many of the pandemic-related contextual factors are outside of our control and stressors are present across multiple domains of life, the transdiagnostic approach of ACT and its emphasis on psychological flexibility suggest it could be a useful lens to develop large-scale interventions to support mental wellbeing during public health crises. This is supported by our finding that psychological flexibility was a negative predictor of state anxiety and the largest unique predictor of mental wellbeing. Further research could build on existing evaluations of web-based and mobile app ACT interventions by developing and evaluating an intervention to increase psychological flexibility in the general population.
Declaration of competing interest
The authors have no financial relationships to declare. Given his role as an Editorial Board member, Gillanders, D.T. had no involvement in the peer-review of this article and had no access to information regarding its peer-review. All other authors have declared no conflicts of interest.
Acknowledgements
We would like to thank the participants who took time to support this research by completing our survey.
References
- Arch J.J., Craske M.G. Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice. 2008;15(4):263–279. doi: 10.1111/j.1468-2850.2008.00137.x. [DOI] [Google Scholar]
- Asmundson G.J., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71:102211. doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avdagic E., Morrissey S.A., Boschen M.J. A randomised controlled trial of acceptance and commitment therapy and cognitive-behaviour therapy for generalised anxiety disorder. Behaviour Change. 2014;31(2):110–130. doi: 10.1017/bec.2014.5. [DOI] [Google Scholar]
- Biglan A., Layton G.L., Jones L.B., Hankins M., Rusby J.C. The value of workshops on psychological flexibility for early childhood special education staff. Topics in Early Childhood Special Education. 2013;32(4):196–210. doi: 10.1177/0271121411425191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluett E.J., Homan K.J., Morrison K.L., Levin M.E., Twohig M.P. Acceptance and commitment therapy for anxiety and OCD spectrum disorders: An empirical review. Journal of Anxiety Disorders. 2014;28(6):612–624. doi: 10.1016/j.janxdis.2014.06.008. [DOI] [PubMed] [Google Scholar]
- Boyraz G., Legros D.N., Tigershtrom A. COVID-19 and traumatic stress: The role of perceived vulnerability, COVID-19-related worries, and social isolation. Journal of Anxiety Disorders. 2020;76:102307. doi: 10.1016/j.janxdis.2020.102307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton R.N. Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders. 2016;39:30–43. doi: 10.1016/j.janxdis.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Fetzner M.G., Hackl J.L., McEvoy P. Intolerance of uncertainty as a contributor to fear and avoidance symptoms of panic attacks. Cognitive Behaviour Therapy. 2013;42(4):328–341. doi: 10.1080/16506073.2013.792100. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Norton M.P.J., Asmundson G.J. Fearing the unknown: A short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders. 2007;21(1):105117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Carstensen L.L., Turan B., Scheibe S., Ram N., Ersner-Hershfield H., Samanez-Larkin G.R., Brooks K.P., Nesselroade J.R. Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging. 2011;26(1):21. doi: 10.1037/a0021285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C.Y., Hong R.Y. Intolerance of uncertainty moderates the relation between negative life events and anxiety. Personality and Individual Differences. 2010;49(1):49–53. doi: 10.1016/j.paid.2010.03.006. [DOI] [Google Scholar]
- Chong Y.Y., Chien W.T., Cheng H.Y., Kassianos A.P., Gloster A.T., Karekla M. Can psychological flexibility and prosociality mitigate illness perceptions toward COVID-19 on mental health? A cross-sectional study among Hong Kong adults. Globalization and Health. 2021;17(1):1–13. doi: 10.1186/s12992-021-00692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciarrochi J., Said T., Deane F.P. When simplifying life is not so bad: The link between rigidity, stressful life events, and mental health in an undergraduate population. British Journal of Guidance and Counselling. 2005;33(2):185–197. doi: 10.1080/03069880500132540. [DOI] [Google Scholar]
- Clark D.A., Beck A.T. Guilford Press; 2010. Cognitive therapy of anxiety disorders: Science and practice. [Google Scholar]
- Crasta D., Daks J.S., Rogge R.D. Modeling suicide risk among parents during the COVID-19 pandemic: Psychological inflexibility exacerbates the impact of COVID-19 stressors on interpersonal risk factors for suicide. Journal of contextual behavioral science. 2020;18:117–127. doi: 10.1016/j.jcbs.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daks J.S., Peltz J.S., Rogge R.D. Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID-19 stress on family systems with a contextual behavioral science lens. Journal of Contextual Behavioral Science. 2020;18:16–27. doi: 10.1016/j.jcbs.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.L., Golijani-Moghaddam N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of contextual behavioral science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiTommaso E., Brannen C., Best L.A. Measurement and validity characteristics of the short version of the social and emotional loneliness scale for adults. Educational and Psychological Measurement. 2004;64(1):99–119. doi: 10.1177/0013164403258450. [DOI] [Google Scholar]
- Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., Holden K.A., Read J.M., Dondelinger F., Carson G., Merson L., Lee J., Plotkin D., Sigfrid L., Jackson C., Gamble C., Horby P.W., Nguyen-Van-Tam J.S., Ho A., Semple M.G. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: Prospective observational cohort study. Bmj. 2020;369 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doorley J.D., Goodman F.R., Kelso K.C., Kashdan T.B. Psychological flexibility: What we know, what we do not know, and what we think we know. Social and Personality Psychology Compass. 2020;14(12):1–11. doi: 10.1111/spc3.12566. [DOI] [Google Scholar]
- Duncan L.A., Schaller M., Park J.H. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Personality and Individual Differences. 2009;47(6):541–546. doi: 10.1016/j.paid.2009.05.001. [DOI] [Google Scholar]
- Fancourt D., Bu F., Mak H.W., Steptoe A. 2020. COVID-19 social study - results release 15.https://www.covidsocialstudy.org/results (Week 15) [Google Scholar]
- Fat L.N., Scholes S., Boniface S., Mindell J., Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short warwick–edinburgh mental well-being scale (SWEMWBS): Findings from the health survey for england. Quality of Life Research. 2017;26(5):1129–1144. doi: 10.1007/s11136-016-1454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. 5th ed. 2018. Discovering statistics using IBM SPSS statistics. [Google Scholar]
- Fledderus M., Bohlmeijer E.T., Fox J.P., Schreurs K.M., Spinhoven P. The role of psychological flexibility in a self-help acceptance and commitment therapy intervention for psychological distress in a randomized controlled trial. Behaviour Research and Therapy. 2013;51(3):142–151. doi: 10.1016/j.brat.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Fledderus M., Bohlmeijer E.T., Pieterse M.E., Schreurs K.M.G. Acceptance and commitment therapy as guided self-help for psychological distress and positive mental health: A randomized controlled trial. Psychological Medicine. 2012;42(3):485. doi: 10.1017/S0033291711001206. [DOI] [PubMed] [Google Scholar]
- Francis A.W., Dawson D.L., Golijani-Moghaddam N. The development and validation of the comprehensive assessment of acceptance and commitment therapy processes (CompACT) Journal of Contextual Behavioral Science. 2016;5(3):134–145. doi: 10.1016/j.jcbs.2016.05.003. [DOI] [Google Scholar]
- Freeston M.H., Rhéaume J., Letarte H., Dugas M.J., Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17(6):791–802. doi: 10.1016/0191-8869(94)90048-5. [DOI] [Google Scholar]
- Gloster A.T., Lamnisos D., Lubenko J., Presti G., Squatrito V., Constantinou M., Nicolaou C., Papacostas S., Aydin G., Chong Y.Y., Chien W.T., Cheng H.Y., Ruiz F.J., Garcia-Martin M.B., Obando-Posada D.P., Segura-Vargas M.A., Vasilou V.S., McHugh L., Höfer S.…Karekla M. Impact of COVID-19 pandemic on mental health: An international study. PloS One. 2020;15(12) doi: 10.1371/journal.pone.0244809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloster A.T., Meyer A.H., Lieb R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6(2):166–171. doi: 10.1016/j.jcbs.2017.02.003. [DOI] [Google Scholar]
- Gloster A.T., Walder N., Levin M., Twohig M., Karekla M. The empirical status of acceptance and commitment therapy: A review of meta-analyses. Journal of Contextual Behavioral Science. 2020 doi: 10.1016/j.jcbs.2020.09.009. [DOI] [Google Scholar]
- Green S.B. How many subjects does it take to do a regression analysis. Multivariate Behavioral Research. 1991;26(3):499–510. doi: 10.1207/s15327906mbr2603_7. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. 2nd ed. The Guilford Press; New York, NY: 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hayes A.F. Computer software; 2020. PROCESS macro. Version 3.5. [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A.…Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp Released . IBM Corp; Armonk, NY: 2017. IBM SPSS statistics for macintosh, version 25.0. [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JISC online surveys . June 2020. [Computer software]https://www.onlinesurveys.ac.uk Retrieved from. [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders. 2020;102239 doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B.D. Covid-19 (coronavirus): Challenges for psychiatry. British Journal of Psychiatry. 2020:1–6. doi: 10.1192/bjp.2020.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khawaja N.G., McMahon J. The relationship of meta-worry and intolerance of uncertainty with pathological worry, anxiety, and depression. Behaviour Change. 2011;28(4):165–180. doi: 10.1375/bech.28.4.165. [DOI] [Google Scholar]
- Koerner N., Dugas M.J. An investigation of appraisals in individuals vulnerable to excessive worry: The role of intolerance of uncertainty. Cognitive Therapy and Research. 2008;32(5):619–638. doi: 10.1007/s10608-007-9125-2. [DOI] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry and Clinical Neurosciences. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Kwong A.S.F., Pearson R.M., Adams M.J., Northstone K., Tilling K., Smith D., FawnsRitchie C., Bould H., Warne N., Zammit S., Gunnell D.J., Moran P., Micali N., Reichenberg A., Hickman M., Rai D., Haworth S., Campbell A., Altschul D., Timpson N.J. 2020. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chu C., Wong P., Tsang K.W.T., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry. 2007;52(4):233240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Levin M.E., Haeger J.A., Pierce B.G., Twohig M.P. Web-based acceptance and commitment therapy for mental health problems in college students: A randomized controlled trial. Behavior Modification. 2017;41(1):141–162. doi: 10.1177/0145445516659645. [DOI] [PubMed] [Google Scholar]
- Levin M.E., Hildebrandt M.J., Lillis J., Hayes S.C. The impact of treatment components suggested by the psychological flexibility model: A meta-analysis of laboratory-based component studies. Behavior Therapy. 2012;43(4):741–756. doi: 10.1016/j.beth.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Levin M.E., Lillis J., Biglan A. The potential of community-wide strategies for promoting psychological flexibility. The Wiley Handbook of Contextual Behavioral Science. 2016:483–495. [Google Scholar]
- Levin M.E., Pierce B., Schoendorff B. The acceptance and commitment therapy matrix mobile app: A pilot randomized trial on health behaviors. Journal of Contextual Behavioral Science. 2017;6(3):268–275. doi: 10.1016/j.jcbs.2017.05.003. [DOI] [Google Scholar]
- Mahoney A.E., McEvoy P.M. A transdiagnostic examination of intolerance of uncertainty across anxiety and depressive disorders. Cognitive Behaviour Therapy. 2012;41(3):212–222. doi: 10.1080/16506073.2011.622130. [DOI] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makhanova A., Shepherd M.A. Behavioral immune system linked to responses to the threat of COVID-19. Personality and Individual Differences. 2020;167:110221. doi: 10.1016/j.paid.2020.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marris M., Sladyk K., St Pierre B., Coverly Dey E. Reliability and validity of the current anxiety level measure. Occupational Therapy in Mental Health. 2017;33(4):386–393. doi: 10.1080/0164212X.2017.1312662. [DOI] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. Journal of Contextual Behavioral Science. 2021;19:28–35. doi: 10.1016/j.jcbs.2020.11.003. [DOI] [Google Scholar]
- Merwin R.M., Timko C.A., Moskovich A.A., Ingle K.K., Bulik C.M., Zucker N.L. Psychological inflexibility and symptom expression in Anorexia nervosa. Eating Disorders. 2011;19(1):62–82. doi: 10.1080/10640266.2011.533606. [DOI] [PubMed] [Google Scholar]
- Mihashi M., Otsubo Y., Yinjuan X., Nagatomi K., Hoshiko M., Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychology. 2009;28(1):91. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian journal of psychiatry. 2020:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moldofsky H., Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurology. 2011;11(1):37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucci F., Mucci N., Diolaiuti F. Lockdown and isolation: Psychological aspects of COVID-19 pandemic in the general population. Clinical Neuropsychiatry: Journal of Treatment Evaluation. 2020;17(2):63–64. doi: 10.36131/CN20200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakenham K.I., Landi G., Boccolini G., Furlani A., Grandi S., Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of contextual behavioral science. 2020;17:109–118. doi: 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J.H., Faulkner J., Schaller M. Evolved disease-avoidance processes and contemporary anti-social behavior: Prejudicial attitudes and avoidance of people with physical disabilities. Journal of Nonverbal Behavior. 2003;27(2):65–87. doi: 10.1023/A:1023910408854. [DOI] [Google Scholar]
- Presti G., Mchugh L., Gloster A., Karekla M., Hayes S.C. The dynamics of fear at the time of COVID-19: A contextual behavioral science perspective. Clinical Neuropsychiatry. 2020;17(2) doi: 10.36131/CN20200206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rettie H., Daniels J. Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. American Psychologist. Advance online publication. 2020 doi: 10.1037/amp0000710. [DOI] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di MArco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz F.J. A review of Acceptance and Commitment Therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of Psychology and Psychological Therapy. 2010;10(1):125–162. [Google Scholar]
- Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. International Journal of Mental Health and Addiction. 2020;1 doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulnier K.G., Allan N.P., Raines A.M., Schmidt N.B. Depression and intolerance of uncertainty: Relations between uncertainty subfactors and depression dimensions. Psychiatry. 2019;82(1):72–79. doi: 10.1080/00332747.2018.1560583. [DOI] [PubMed] [Google Scholar]
- Schäfer S., Sopp R., Schanz C., Staginnus M., Göritz A.S., Michael T. Impact of COVID-19 on public mental health and the buffering effect of sense of coherence. OSF Preprints. 2020 doi: 10.31219/osf.io/4ptfz. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller M., Park J.H. The behavioral immune system (and why it matters) Current Directions in Psychological Science. 2011;20(2):99–103. doi: 10.1177/0963721411402596. [DOI] [Google Scholar]
- Seco Ferreira D.C., Oliveira W.L., Costa Delabrida Z.N., Faro A., Cerqueira-Santos E. Intolerance of uncertainty and mental health in Brazil during the Covid-19 pandemic. Suma Psicológica. 2020;27(1):62–69. doi: 10.14349/sumapsi.2020.v27.n1.8. [DOI] [Google Scholar]
- Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L., Mason L., Martinez A., McKay R., Stocks T.V.A., Bennett K.M., Hyland P., Karatzias T., Bentall R.P. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6):E125. doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shihata S., McEvoy P.M., Mullan B.A., Carleton R.N. Intolerance of uncertainty in emotional disorders: What uncertainties remain? Journal of Anxiety Disorders. 2016;41:115–124. doi: 10.1016/j.janxdis.2016.05.001. [DOI] [PubMed] [Google Scholar]
- Smith C.A., Lazarus R.S. Appraisal components, core relational themes, and the emotions. Cognition & Emotion. 1993;7(3–4):233–269. doi: 10.1080/02699939308409189. [DOI] [Google Scholar]
- Smith B.M., Twohy A.J., Smith G.S. Psychological inflexibility and intolerance of uncertainty moderate the relationship between social isolation and mental health outcomes during COVID-19. Journal of Contextual Behavioral Science. 2020;18:162–174. doi: 10.1016/j.jcbs.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D. 1983. Manual for the state-trait anxiety inventory STAI (form Y) (" self evaluation questionnaire") [Google Scholar]
- Stevens K., Rogers T., Campbell M., Björgvinsson T., Kertz S. A transdiagnostic examination of decreased intolerance of uncertainty and treatment outcome. Cognitive Behaviour Therapy. 2018;47(1):19–33. doi: 10.1080/16506073.2017.133831. [DOI] [PubMed] [Google Scholar]
- Stewart-Brown S., Tennant A., Tennant R., Platt S., Parkinson J., Weich S. Internal construct validity of the warwick-edinburgh mental well-being scale (WEMWBS): A rasch analysis using data from the scottish health education population survey. Health and Quality of Life Outcomes. 2009;7(1):15. doi: 10.1186/1477-7525-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockton D., Kellett S., Berrios R., Sirois F., Wilkinson N., Miles G. Identifying the underlying mechanisms of change during acceptance and commitment therapy (ACT): A systematic review of contemporary mediation studies. Behavioural and Cognitive Psychotherapy. 2019;47(3):332–362. doi: 10.1017/S1352465818000553. [DOI] [PubMed] [Google Scholar]
- Tabachnick B., Fidell L. Pearson Education Limited; Harlow, Essex: 2014. Using multivariate statistics (International edition of sixth ed., Pearson custom library. [Google Scholar]
- Trompetter H.R., Bohlmeijer E.T., Fox J.P., Schreurs K.M.G. Psychological flexibility and catastrophizing as associated change mechanisms during online Acceptance & Commitment Therapy for chronic pain. Behaviour Research and Therapy. 2015;74:50–59. doi: 10.1016/j.brat.2015.09.001. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. Mental distress among U.S. adults during the COVID-19 pandemic. Journal of Clinical Psychology. 2020;76(12):2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D., Patten S.B., Pajer K., Krausz M., Taylor S., Rush B., Raviola G., Saxena S., Thornicroft G., Yatham L.N. Mental health of communities during the COVID‐19 pandemic. Canadian Journal of Psychiatry. 2020;65 doi: 10.1177/0706743720926676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.J., Ho C. 2020. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, behavior, and immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36(3):210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Williams S.N., Armitage C.J., Tampe T., Dienes K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK based focus group study. BMJ Open 2020. 2020;10 doi: 10.1101/2020.04.10.20061267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. COVID-19 – strategy update; p. 14.https://www.who.int/publications/m/item/covid-19-strategy-update April 2020. [Google Scholar]
- World Health Organization . 2020. Advice on the use of masks in the context of COVID-19:interim guidance, 5 June 2020.https://apps.who.int/iris/handle/10665/332293 [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. The Canadian Journal of Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 Days during the coronavirus disease 2019 (COVID19) outbreak in january 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]