Abstract
Background:
The aim of this study was to determine the association between neutrophil-lymphocyte ratio (NLR) and severity of lower extremity peripheral artery disease (PAD).
Methods:
A retrospective chart review identified 928 patients referred for peripheral angiography. NLR was assessed from routine pre-procedural hemograms with automated differentials and available in 733 patients. Outcomes of interest were extent of disease on peripheral angiography and target vessel revascularization. Median follow-up was 10.4 months. Odds ratio (OR) [95% confidence intervals] was assessed using a logistic regression model.
Results:
There was a significant association between elevated NLR and presence of severe multi-level PAD versus isolated suprapopliteal or isolated infrapopliteal disease (OR 1.11 [1.03–1.19], p = 0.007). This association remained significant even after adjustment for age (OR 1.09 [1.01–1.17], p = 0.02); age, sex, race, and body mass index (OR 1.08 [1.00–1.16], p = 0.046); and age, sex, race, body mass index, hypertension, diabetes mellitus, coronary artery disease, and creatinine (OR 1.07 [1.00–1.15], p = 0.049). After additional adjustment for clinical presentation, there was a trend towards association between NLR and severe multi-level PAD (OR 1.07 [1.00–1.15], p = 0.056), likely limited by sample size. In patients who underwent endovascular intervention (n = 523), there was no significant difference in rate of target vessel revascularization across tertiles of NLR (1st tertile 14.8%, 2nd tertile 14.1%, 3rd tertile 20.1%; p = 0.32).
Conclusion:
In a contemporary cohort of patients undergoing peripheral angiography with possible endovascular intervention, elevated NLR was independently associated with severe multi-level PAD. Larger studies evaluating the association between this inexpensive biomarker and clinical outcomes are warranted.
Keywords: Neutrophil, Lymphocyte, Peripheral artery disease, Peripheral angiography
1. Introduction
Lower extremity peripheral artery disease (PAD) affects more than 8 million people in the United States, and more than 1 million people undergo peripheral artery revascularization in the United States each year [1–2]. Inflammation is central to atherogenesis, a common cause of PAD [3]. Neutrophils, the most abundant white blood cell in the circulation, interact with atherosclerotic endothelium to promote disease progression. Neutrophil-lymphocyte ratio (NLR) is a marker measured on routine pre-procedural hemogram and correlates with both disease severity and prognosis in patients with coronary artery disease [4–5]. There is limited data, however, examining this association in PAD, particularly in an all-comers population.
The aim of this study was to evaluate the association between NLR and severity of PAD in patients undergoing peripheral angiography. A secondary aim was to evaluate the association between NLR and target vessel revascularizations in patients undergoing endovascular intervention.
2. Methods
2.1. Study population
This retrospective observational study identified 928 consecutive patients referred for peripheral angiography with possible endovascular intervention for symptomatic PAD at a tertiary care center between December 2012 and June 2015. If multiple peripheral angiograms/endovascular interventions were performed within the study period, the first to occur temporally was defined as the index procedure. Of the 928 patients, 195 (21%) patients were excluded due to lack of available data on pre-procedural neutrophil or lymphocyte count. The study was approved by the NYU School of Medicine Institutional Review Board.
2.2. Variables of interest
Demographic, clinical, laboratory, and procedural variables were recorded from review of the electronic medical record. Tobacco use was defined as self-reported activity within one year of the index procedure. Hemograms with automated differentials were obtained within 30 days prior to peripheral angiography per the cardiac catheterization laboratory policy, and those closest to the procedure date were recorded. The NLR was calculated as the ratio of neutrophil to lymphocyte counts. Tertiles of NLR were defined as follows: 1st tertile 0.04–1.87, 2nd tertile 1.88–3.0, and 3rd tertile 3.01–34.38.
2.3. Outcomes
PAD was defined in the lower extremity contralateral to the site of retrograde access or ipsilateral to the site of antegrade access. The primary outcome was defined as severe multi-level disease. Severe disease was defined as ≥70% diameter stenosis by visual estimate on peripheral angiography or site of endovascular intervention. Level of disease was categorized as suprapoliteal (iliac, femoral, and popliteal arteries), infrapopliteal (anterior tibial, peroneal, and posterior tibial arteries), and multi-level disease (severe disease in both the supra and infrapopliteal regions). The secondary outcome was defined as target vessel revascularization.
2.4. Statistical analysis
Distributions of continuous variables were examined using the Shapiro-Wilkes test. Normally distributed continuous variables are presented as mean ± standard deviation and evaluated across tertiles of NLR using one-way ANOVA, while skewed continuous variables are presented as median [interquartile range] and evaluated across tertiles of NLR using the Kruskal Wallis test. Categorical variables are presented as n (proportions) and analyzed across tertiles of NLR using the chi square test. The strength of association between NLR and outcomes was determined using a logistic regression model and presented as odds ratios (OR) [95% Confidence Interval (CI)]. Variables were chosen for the model based on significance level of <0.01 in univariate analysis and a priori choice of baseline demographics and presence of diabetes mellitus. Significance was tested using a 2-sided alpha level of 0.05. Statistical analysis was conducted using the IBM Statistical Package for Social Sciences software, version 20 (IBM Corporation, Armonk, New York) and Statistical Analysis System 9.3 (SAS Institute Inc., Cary, North Carolina).
3. Results
A total of 733 patients met inclusion/exclusion criteria. Baseline demographic, clinical, and laboratory characteristics across tertiles of NLR are presented in Table 1. Age, the proportion of hypertension, proportion of coronary artery disease, and serum creatinine increased, while the proportion of Black non Hispanic race decreased, with increasing tertiles of NLR.
Table 1.
Baseline demographic, clinical, and laboratory characteristics across tertiles of neutrophil-lymphocyte ratio (NLR) in patients undergoing peripheral angiography with possible endovascular intervention.
| Tertile 1 (n = 244) | Tertile 2 (n = 250) | Tertile 3 (n = 239) | p-Value | |
|---|---|---|---|---|
| Age (years) | 68 [60–76] | 72 [65–78] | 74 [67–80] | <0.001 |
| Men | 133 (55%) | 152 (61%) | 152 (64%) | 0.113 |
| White, not Hispanic | 104 (25%) | 163 (65%) | 164 (69%) | <0.001 |
| Black, not Hispanic | 58 (24%) | 33 (13%) | 15 (6%) | |
| Hispanic | 67 (27%) | 47 (19%) | 50 (21%) | |
| Asian | 10 (4%) | 4 (2%) | 5 (2%) | |
| Other | 5 (2%) | 3 (1%) | 2 (1%) | |
| Body mass index (kg/m2) | 28.2 [25.2–31.2] | 28.6 [25.5–31.6] | 27.6 [24.4–30.8] | 0.047 |
| Hypertension | 209 (86%) | 219 (88%) | 227 (96%) | 0.002 |
| Dyslipidemia | 192 (79%) | 219 (88%) | 196 (82%) | 0.03 |
| Diabetes mellitus | 132 (54%) | 142 (57%) | 135 (57%) | 0.83 |
| Coronary artery disease | 123 (51%) | 165 (66%) | 150 (66%) | 0.001 |
| Smoker | 147 (65%) | 161 (69%) | 138 (62%) | 0.33 |
| Aspirin | 145 (70%) | 152 (70%) | 144 (65%) | 0.47 |
| Clopidogrel | 111 (54%) | 126 (58%) | 126 (57%) | 0.68 |
| Cilostazol | 22 (11%) | 22 (10%) | 22 (10%) | 0.97 |
| Statin | 136 (67%) | 163 (75%) | 161 (73%) | 0.15 |
| Creatinine (mg/dL) | 1.2 [1.0–1.4] | 1.3 [1.1–1.5] | 1.5 [1.3–1.8] | <0.001 |
| Glucose (mg/dL) | 125 [99–151] | 130 [102–159] | 141 [110–172] | 0.42 |
| Presentation | <0.001 | |||
| Stable claudication | 224 (92%) | 224 (90%) | 178 (74%) | |
| Critical limb ischemia | 18 (8%) | 26 (10%) | 61 (26%) |
Continuous variables are presented as median [interquartile range] and compared using Kruskal Wallis test. Categorical variables are presented as n (proportion) and compared using the chi square test.
Baseline peripheral artery anatomy across tertiles of NLR are presented in Table 2. The proportion of severe disease increased in all suprapopliteal vascular territories, as did the proportion of severe multi-level PAD, with increasing tertiles of NLR. Strength of association between NLR and severe multi-level PAD is shown in Fig. 1.
Table 2.
Baseline peripheral artery anatomy across tertiles of neutrophil-lymphocyte ratio (NLR) in patients undergoing peripheral angiography with possible endovascular intervention.
| Tertile 1 (n = 244) | Tertile 2 (n = 250) | Tertile 3 (n = 239) | p-Value | |
|---|---|---|---|---|
| Severe iliac artery disease | 16 (17%) | 44 (18%) | 61 (25%) | 0.03 |
| Severe femoral artery disease | 135 (55%) | 150 (60%) | 167 (70%) | 0.004 |
| Severe popliteal artery disease | 47 (19%) | 56 (22%) | 91 (38%) | <0.001 |
| Severe anterior tibial artery disease | 95 (39%) | 134 (54%) | 117 (49%) | 0.004 |
| Severe peroneal artery disease | 66 (27%) | 93 (37%) | 94 (39%) | 0.01 |
| Severe posterior tibial artery disease | 106 (43%) | 120 (48%) | 122 (51%) | 0.24 |
| Severe suprapopliteal disease | 164 (67%) | 180 (72%) | 195 (82%) | 0.001 |
| Severe infrapopliteal disease | 139 (57%) | 166 (66%) | 162 (68%) | 0.03 |
| Severe multilevel disease | 92 (38%) | 119 (48%) | 131 (55%) | 0.001 |
| Presence of suprapopliteal chronic total occlusion | 82 (34%) | 91 (36%) | 118 (49%) | 0.001 |
| Presence of infrapopliteal chronic total occlusion | 117 (48%) | 129 (52%) | 126 (53%) | 0.55 |
| Presence of multilevel chronic total occlusion | 42 (17%) | 56 (22%) | 75 (31%) | 0.001 |
Variables are presented as n (proportion) and compared using the chi square test.
Fig. 1.
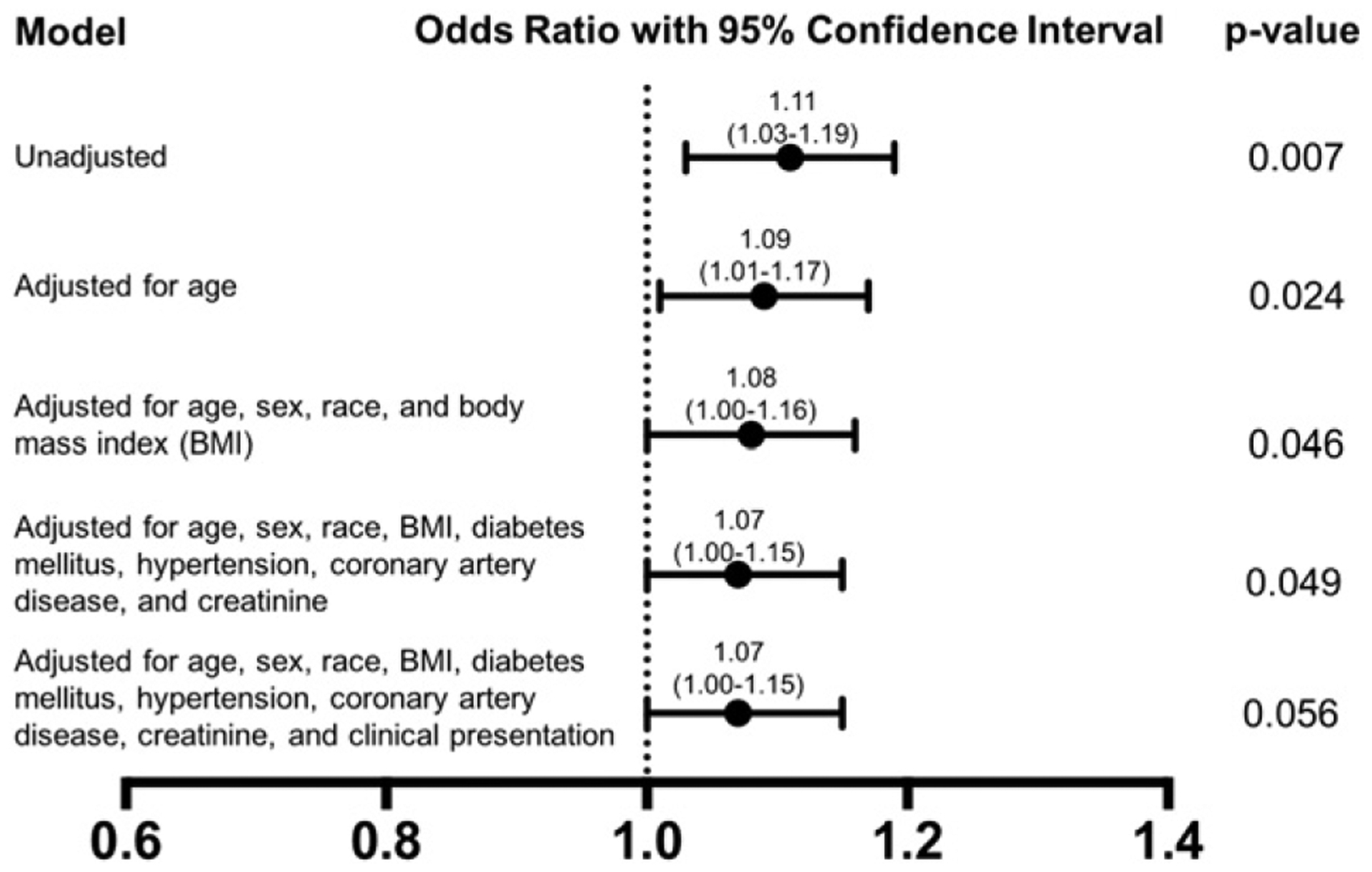
Association between neutrophil-lymphocyte ratio and severe multi-level peripheral artery disease in patients undergoing peripheral angiography with possible endovascular intervention.
Of the 733 patients undergoing peripheral angiography, 523 (71.4%) underwent endovascular intervention. Of these patients, follow-up was available in 424 (81.1%) patients, and median follow-up was 10.4 months. There was no significant difference in the rate of target vessel revascularization on follow-up across tertiles of NLR (1st tertile 14.8%, 2nd tertile 14.1%, 3rd tertile 20.1%; p = 0.32). Numerically, the rate of target vessel revascularization was highest in the third tertile of NLR (1st and 2nd tertile vs 3rd tertile p = 0.09).
4. Discussion
This observational study demonstrates a significant association between NLR, a rapidly assessable and inexpensive marker measured on routine hemogram, and the presence of multi-level lower extremity PAD in an all-comers population even after adjustment for traditional atherosclerosis risk factors.
NLR has previously been shown to be a marker for extent of atherosclerotic disease in the coronary arteries. One retrospective observational study of 396 patients presenting with a non-ST segment elevation myocardial infarction who underwent coronary angiography demonstrated a NLR as an independent predictor of left main or severe triple vessel disease [4]. Another study evaluated 3738 consecutive patients undergoing elective and urgent coronary angiography and demonstrated a significant independent association between NLR and the presence and severity of coronary artery disease [6]. Our study also shows an increased incidence of coronary artery disease with increasing tertiles of NLR, and similar to other reports in populations with and without vascular disease shows a lower NLR in Black non Hispanic individuals [7–8]. The current report is one of the very few studies to evaluate an all-comers population of patients with PAD undergoing delineation of peripheral arterial anatomy on angiography. One center in Austria did report NLR to be significantly associated with the presence of critical limb ischemia on clinical presentation in 2121 patients with lower extremity PAD even after adjustment with age > 75 years, sex, diabetes, congestive heart failure, stroke/transient ischemia attack, and CHA2DS2-VASC score [9].
NLR is also associated with clinical outcomes in patients with atherosclerotic disease. This is extensively studied across the spectrum of patients with coronary artery disease. In patients presenting with ST segment elevation myocardial infarction, NLR has been shown to be associated with a higher rate of no-reflow percutaneous coronary intervention, in-hospital major adverse cardiovascular events, and long-term all-cause mortality [10–12]. Similarly, in patients with non-ST segment elevation acute coronary syndrome, NLR is an independent predictor of both short- and long-term major adverse cardiovascular events, and in an all-comers population of patients undergoing coronary angiography or coronary artery bypass grafting, NLR is an independent predictor of long-term mortality [5,13–15]. NLR has also been shown to independently predict symptomatic cerebrovascular disease in patients with intermediate carotid artery stenosis [16].
Several studies have shown the association between NLR and outcomes in patients with critical limb ischemia. A single center study of 149 patients with critical limb ischemia in South Australia demonstrated a significant association between NLR and all-cause mortality on medium follow-up of 8.7 months [17]. A similar independent association between NLR and 5-year mortality was noted in a study of 561 patients with critical limb ischemia who underwent infrainguinal revascularization at a single center in Spain [18]. However, only a few studies evaluated solely patients who underwent percutaneous peripheral intervention. An analysis of the 83 patients who underwent tibial angioplasty for critical limb ischemia in the Bypass vs Angioplasty in Severe Ischaemia of the Leg (BASIL) trial, NLR was associated with 12-month mortality [19]. In addition, there are even more limited data on clinical outcomes in an all-comers population of patients with lower extremity PAD. A retrospective analysis of 593 inpatients at a tertiary medical center in Turkey demonstrated a significant association between NLR and long-term cardiovascular mortality in patients with PAD [20]. In the current study’s population, the majority of patients presented with stable claudication rather than critical limb ischemia. After additional adjustment for clinical presentation, there remains only a trend towards an association between NLR and severe multi-level PAD. However, this is likely due to the sample size evaluated given that point estimates remain the same, and the data suggest that even a chronic level of inflammation may be associated with adverse effects. Although there was no significant difference in the rate of target vessel revascularization on follow-up across NLR tertiles, there was a trend towards a higher rate of target vessel revascularization in the highest NLR tertile.
While elevated baseline markers of systemic inflammation are known to be associated with poor long-term outcomes in patients with PAD, the role of neutrophils in patients with PAD is not completely elucidated. Furthermore, disruption of the vascular endothelium occurs during percutaneous peripheral artery revascularization, which may result in recruitment of neutrophils. With vascular injury, neutrophils first loosely associate with the endothelium via selectins and then adhere more tightly to the endothelium via β2-integrins and cellular adhesion molecules, followed by migration into the tissue and a resultant activation of neutrophils. In addition, systemic inflammation may be evident with elevated C-reactive protein and other cytokines. However, unlike other markers of inflammation, a hemogram with an automated differential is routinely measured, inexpensive, and standardly assessed making it easily applicable to different populations and clinical settings. Future studies of outcomes in patients with PAD should consider adjustment for baseline NLR, and neutrophils specifically may be considered as a target of therapy.
This study does carry some limitations, including those inherent to a retrospective cohort design. Second, the clinical status of the patient at the time of the baseline hemogram is unknown (e.g. active infection or an inflammatory condition that may alter the patient’s baseline NLR). Third, there are no other inflammatory markers, such as C-reactive protein, available for correlation. However, the aim of the study is to demonstrate the utility of a routinely measured, inexpensive marker of inflammation validated in other atherosclerotic vascular diseases. Third, the study is underpowered for the clinical outcome of target vessel revascularization. Finally, approximately one-fifth of the study population were excluded due to lack of data on hemogram differentials, and may be a source of potential selection bias. Nonetheless, this is one of the larger studies of patients with PAD and delineated peripheral anatomy in an all-comers population.
5. Conclusion
In conclusion, NLR, a valid marker of inflammation measured on routine hemograms, is independently associated with severity of lower extremity PAD in an all-comers population.
Acknowledgments
Binita Shah was supported in part by the National Center for Advancing Translational Sciences (NYU CTSA UL1TR000038) and New York State (Empire Clinical Research Investigator Program) in 2015 and the Biomedical Laboratory Research and Development, VA Office of Research and Development (I01BX007080) in 2016. Statistical support was provided in part by the New York University School of Medicine Cardiovascular Outcomes Group.
Footnotes
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
References
- [1].Allison M, Ho E, Denenberg J, Langer R, Newman A, Fabsitz R, Criqui M, Ethnic-specific prevalence of peripheral arterial disease in the United States, Am. J. Prev. Med 32 (2007) 328–333. [DOI] [PubMed] [Google Scholar]
- [2].Jim J, Owens PL, Sanchez LA, Rubin BG, Population-based analysis of inpatient vascular procedures and predicting future workload and implications for training, J. Vasc. Surg 55 (2012) 1394–1399. [DOI] [PubMed] [Google Scholar]
- [3].Packard RR, Libby P, Inflammation in atherosclerosis: from vascular biology to biomarker discovery and risk prediction, Clin. Chem 54 (2008) 24–38. [DOI] [PubMed] [Google Scholar]
- [4].Misumida N, Kobayashi A, Saeed M, Fox JT, Kanei Y, Neutrophil-to-lymphocyte ratio as an independent predictor of left main and/or three-vessel disease in patients with non-ST-segment elevation myocardial infarction, Cardiovasc. Revasc. Med 16 (2015) 331–335. [DOI] [PubMed] [Google Scholar]
- [5].Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS, Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome, Am. J. Cardiol 102 (2008) 653–657. [DOI] [PubMed] [Google Scholar]
- [6].Verdoia M, Barbieri L, Di Giovine G, Marino P, Suryapranata H, De Luca G, Novara Atherosclerosis Study group (NAS), neutrophil to lymphocyte ratio and the extent of coronary artery disease: results from a large cohort study, Angiology 67 (2016) 75–82. [DOI] [PubMed] [Google Scholar]
- [7].Misumida N, Kobayashi A, Kanei Y, Racial differences in the neutrophil-to-lymphocyte ratio in patients with non-ST-segment elevation myocardial infarction, Coron. Artery Dis 26 (2015) 381–385. [DOI] [PubMed] [Google Scholar]
- [8].Azab B, Camacho-Rivera M, Taioli E, Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects, PLoS One 9 (2014), e112361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gary T, Pichler M, Belaj K, Hafner F, Gerger A, Froehlich H, Eller P, Pilger E, Brodmann M, Neutrophil-to-lymphocyte ratio and its association with critical limb ischemia in PAOD patients, PLoS One 8 (2013), e56745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Akpek M, Kaya MG, Lam YY, Sahin O, Elcik D, Celik T, Ergin A, Gibson CM, Relation of neutrophil/lymphocyte ratio to coronary flow to in-hospital major adverse cardiac events in patients with ST-elevated myocardial infarction undergoing primary coronary intervention, Am. J. Cardiol 110 (2012) 621–627. [DOI] [PubMed] [Google Scholar]
- [11].Park JJ, Jang HJ, Oh IY, Yoon CH, Suh JW, Cho YS, Youn TJ, Cho GY, Chae IH, Choi DJ, Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention, Am. J. Cardiol 111 (2013) 636–642. [DOI] [PubMed] [Google Scholar]
- [12].Núñez J, Núñez E, Bodí V, Sanchis J, Miñana G, Mainar L, Santas E, Merlos P, Rumiz E, Darmofal H, Heatta AM, Llàcer A, Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction, Am. J. Cardiol 101 (2008) 747–752. [DOI] [PubMed] [Google Scholar]
- [13].Azab B, Zaher M, Weiserbs KF, Torbey E, Lacossiere K, Gaddam S, Gobunsuy R, Jadonath S, Baldari D, McCord D, Lafferty J, Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction, Am. J. Cardiol 106 (2010) 470–476. [DOI] [PubMed] [Google Scholar]
- [14].Arbel Y, Finkelstein A, Halkin A, Birati EY, Revivo M, Zuzut M, Shevach A, Berliner S, Herz I, Keren G, Banai S, Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography, Atherosclerosis 225 (2012) 456–460. [DOI] [PubMed] [Google Scholar]
- [15].Gibson PH, Croal BL, Cuthbertson BH, Small GR, Ifezulike AI, Gibson G, Jeffrey RR, Buchan KG, El-Shafei H, Hillis GS, Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting, Am. Heart J 154 (2007) 995–1002. [DOI] [PubMed] [Google Scholar]
- [16].Köklü E, Yüksel İÖ, Arslan Ş, Bayar N, Çağırcı G, Gencer ES, Alparslan AŞ, Çay S, Kuş G, Is elevated neutrophil-to-lymphocyte ratio a predictor of stroke in patients with intermediate carotid artery stenosis, J. Stroke. Cerebrovasc. Dis 25 (2015) 578–584. [DOI] [PubMed] [Google Scholar]
- [17].Spark JI, Sarveswaran J, Blest N, Charalabidis P, Asthana S, An elevated neutrophil-lymphocyte ratio independently predicts mortality in chronic critical limb ischemia, J. Vasc. Surg 52 (2010) 632–636. [DOI] [PubMed] [Google Scholar]
- [18].González-Fajardo JA, Brizuela-Sanz JA, Aguirre-Gervás B, Merino-Díaz B, Del Río-Solá L, Martín-Pedrosa M, Vaquero-Puerta C, Prognostic significance of an elevated neutrophil-lymphocyte ratio in the amputation-free survival of patients with chronic critical limb ischemia, Ann. Vasc. Surg 28 (2014) 999–1004. [DOI] [PubMed] [Google Scholar]
- [19].Chan C, Puckridge P, Ullah S, Delaney C, Spark JI, Neutrophil-lymphocyte ratio as a prognostic marker of outcome in infrapopliteal percutaneous interventions for critical limb ischemia, J. Vasc. Surg 60 (2014) 661–668. [DOI] [PubMed] [Google Scholar]
- [20].Erturk M, Cakmak HA, Surgit O, Celik O, Aksu HU, Akgul O, Gurdogan M, Bulut U, Ozalp B, Akbay E, Yildirim A, Predictive value of elevated neutrophil to lymphocyte ratio for long-term cardiovascular mortality in peripheral arterial occlusive disease, J. Cardiol 64 (2014) 371–376. [DOI] [PubMed] [Google Scholar]


