Abstract
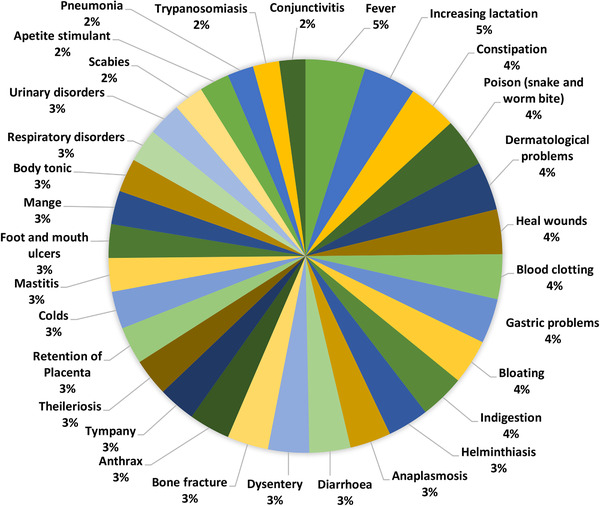
Medicinal plants are highly used in the ethnoveterinary practice as considerable livestock resources in remote areas. The aim of the present study is to explore the ethnoveterinary medicinal practices in three different communities and discuss the cross‐cultural consensus on the usage of medicinal plants for the treatment of animals. The field survey was conducted by the animal healers of the area during the different seasons of plant growth. A total of 83 informants were interviewed through Semi‐structured interview involving experts of traditional knowledge in 21 localities of the three regions (Zhob, D. I. Khan and Mianwali) were conducted. Findings of the study were quantitatively analyzed through the informant consensus factors to identify the homogeneity information provided by the informants. Furthermore, cross‐culture consensuses were analyzed and recorded data were represented in a tabulated and Venn diagrams. In particularly, 59 species of plants were documented in the comparative analysis. Among them, 32 plant species were recorded in Pashto community, while Punjabi and Sarakai communities exhibited nine and four plant species, respectively. Whereas cross‐cultural analysis showed 14 medicinal plants that were commonly utilized by three different ethnic communities, that indicated low interregional consensus in regard to ethnoveterinary practices of medicinal plants. The current study showed that different communities and ethnic groups sharing some traditional knowledge and cross‐culturally approaches have been reported from traditional uses of plants against livestock's diseases. Therefore, current findings are the opportunities to scrutinize the plants for the discovery of new drug sources for humans and animals.
Keywords: ethnic communities, ethnoveterinary, medicinal plants, traditional knowledge
This research work provides the cross‐cultural information about medicinal plants in different communities of three different regions in the Southwest Pakistan. Cross‐cultural analysis showed medicinal plants was commonly used among three ethnic communities that indicates a low interregional consensus with regard to the ethnoveterinary practices of medicinal plants.
1. INTRODUCTION
Since the mankind's existence, natural systems of plant‐based products have offered a continuous viable source of medicine and their applications have been preserved through the usage of traditional medicines (Lev, 2003; Phillipson and Anderson, 1989). Traditional human populations have access to a vast natural wealth of plant and animal species (Alves and Rosa, 2005; Alves and Rosa, 2007). Medicinal plants have been used as a source of medicine in all ethnic cultures (Agra et al., 2007; Alves et al., 2009; Yineger et al., 2007). The plant‐based products are not only used for medical purposes to cure human diseases, but these products can also be used for the treatment of livestock diseases (Barboza et al., 2007; Pradhan and Badola, 2008). This is a comprehensive field that involves the knowledge, skills, practices and people's beliefs about veterinary health care (Tamboura et al., 2000). It employs diverse elements including animals, minerals, plants and folk medicine in various communities (McCorkle and Mathias‐Mundy, 1992).
In recent times, herbal medications got more attention worldwide due to minimum/low‐risk factors caused by the synthetic drugs. Moreover, plant‐based veterinary medicines or formulations are much cheaper (Raza et al., 2014). Although, some communities in modern society are unable to access veterinary practices. In such situation/cases ethnoveterinary medicine (EVM) plays an important role in various communities and areas of the world. The modern drugs derived from plant‐based materials have been used traditionally for the treatment of humans and animals. Further investigation, on the other hand, may lead to the identification of new possible EVM results (Ali‐Shtayeh et al., 2016; Getachew et al., 2012; Rates, 2001; Zorloni et al., 2010). Despite this, the traditional knowledge of ethnoveterinary remediation has been practiced all over the world, although the process of researching, recording and commercialization of this knowledge is still hidden behind the ethnomedicine. However, current documentation process of the ethnomedicine has shown progression in the worldwide (Aziz et al., 2020). Thus, several studies have been conducted on the ethnoveterinary investigations and use of plants in livestock from other regions of Pakistan (Abbasi et al., 2013; Aziz et al., 2018; Mussarat et al., 2014). The plant‐based ethnoveterinary herbal medicine is one of the alternatives and most sustainable approaches that easily adapted to rural livestock for the treatment of animal diseases in Pakistan. It has been serving as a treatment purpose for several years in the lack of modern veterinary practices (Ashall et al., 2018). Community members gave traditional knowledge of herbal medication services to their community with minimum cost or some time free of charge. However, communication and exchange of traditional knowledge between various ethnic communities are stumpy and sometimes traditional healers can only transfer knowledge to one son or pass away without transmitting their knowledge to anyone else. This condition is coupled with the fact that the awareness of ethnomedicine is at risk because no resources are available for younger generations. The key explanation is that local people, especially those of younger generations, are not interested in the traditional knowledge of ethnomedicinal plants (Amjad et al., 2020; Aziz et al., 2018; Smylie et al., 2014). For that reason, ethnoveterinary medicinal knowledge may be lost soon unless researchers organize the information and pass it from one generation to other generation (Aziz et al., 2018). The country's livestock population is very extensive, consisting of a variety of native varieties that are well adapted to local conditions. In particular, there are an estimated 30 million cattle, 54 million goats, 27 million sheep, 01 million camels, 27 million buffaloes, 0.3 million horses, 0.2 million mules, 4 million asses and 74 million poultry in Pakistan (Hasnain and Usmani, 2006). The research region in South West Pakistan includes the provinces of Khyber Pakhtunkhw (Dera Ismail Khan), Balochistan (Zhob) and Punjab (Mianwali). Three main cultures, that is, Pashtun, Saraiki and Punjabi, occupy these areas. Due to the remote areas, the majority of the local people of ethnic communities using medicinal plants residing in these areas due to the unavailability of allopathic medicine and having no or little schooling. The two main reasons discussed outside of people that are native, relying on plants established materials for healthcare for livestock. Therefore, the people mainly relied on past curing for diseases of their livestock. As a result, the people depended heavily on historical curing for cattle ailments.
These reasons trigger us to conduct field surveys on the cross‐sectional study of medicinal uses of plants in the health care system of livestock of cross‐cultural ethnic communities. Therefore, the current study was designed with the goal of documenting and reporting traditional veterinary usage of medicinal herbs in three ethnic tribes in Southwest Pakistan. Moreover, a discussion was done on the cross‐cultural unity and practicing of medicinal plants. In addition, we elaborate traditional acuity of plants rooted cure as the best solution for animal's health. Therefore, the current study prominent the preservation values of ethnoveterinary knowledge in three regions and provides the basic exploration of new phytochemicals.
2. MATERIALS AND METHODS
2.1. Southwest Pakistan: A study area
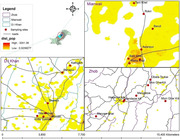
Pakistan, which covers a territory of 881,913 km2 and stretches 1600 kilometers north to south and 885 kilometers east to west, has a diverse cultural and linguistic landscape. A very rich variety of flora and fauna occur in different parts of the country. Figure 1 depicts the areas of Dera Ismail Khan, Zhob and Mianwali in South West Pakistan. Three main cultures, that is, Pashtun, Saraiki and Punjabi are the residence of these areas. Dera Ismail Khan is one of Khyber Pakhtunkhwa's major cities, located between 310 49´ N and 700 55´ E at an elevation of around 150 m on the western bank of the Indus River. D.I. Khan, with a population of about 15 million extends its boundaries to the North to Tank and Lakki Marwat districts (Khyber Pakhtunkhwa Province), East to Mianwali and Bhakkar districts (Punjab Province), South to Dera Ghazi Khan District (Punjab) and West to the Tribal Areas of Pakistan. Mianwali is situated on the North‐West side of Punjab between 320 58´ N and 540 36´ E at an elevation of 690. Zhob is the largest district of Baluchistan Province, which lies between 30°26′ N 67°48′ E at an elevation of 1525 m. This district is famous for its pleasant climate, beautiful mountains and famous varieties of fruits (Ahmad, 2007).
FIGURE 1.
Maps of the three districts along with their sub‐localities where data on medicinal plants used for gastropathic applications were collected
The major vegetation in the D.I. Khan is “tropical thorn forests.” It is characterized by an open low forest in which thorny, usually hardwood species predominate, Acacia nilotica being particularly characteristic. Along with Pathan tribes (Koh‐e‐surkh) a big mixed Baloch population and Jat tribes of the south and trans‐Indus areas migrated to Dera Ismail Khan. The city has many families referred to in the earlier documents Mootani‐Pathans, these are Alizai, Sadozai, Khawjakzai and Barakzai. The predominant population of the district speaks Saraiki almost 72.47% of the total population. The 22.02% of the population speaks Pashto and other languages such as Urdu, Balochi and Sindhi contribute about 4.28% of the total population in the district.
The most common plants of the Mianwali District are Acacia modesta, Acacia nilotica, Dalbergia sissoo, Olea feruginea, Melia azadarach, Morus alba and Morus nigra. Niazi tribes are the majority in the area, followed by Awan (Malik), Baloch and Syed, Jutts, Sheikh and Mughals. The mother tongue of 90% families is Saraiki while 10% had other languages such as Urdu, Hindko and Pashto.
The soil of Zhob is very fertile and having rich cultural biodiversity. The most common plant taxa of the area such as Ephedra intermedia, Ephedra procera, Pistacia atlantica, Pistacia khinjuk, Tamarix aphyla, Solanum nigrum, Calotropis procera, Pegnum hermala and Withania coagulans. Zhob is inhabited by inhabitants of Afghan origin. Dominant tribes of the district are Kakar, Mandokhel, Sherani, Harifal, Babar and lawoon. The majority of the population in district Zhob is Pashtoon. Therefore, Pashto is used as the mother language (96%) in the district Zhob while fewer people are found in that area who speak Saraiki (1.8%) and Punjabi (1.77%).
2.2. Documentation of indigenous ethnobotanical knowledge
The study was conducted from August 2017 to March 2019 using the protocol for the gathering of ethnobotanical data (Alexiades and Sheldon, 1996). Ethnobotanical surveys were conducted in 21 different localities of Southwest Pakistan, that is, Mianwali (Kotla Syedan, Muryali, Zafara Abad, Wazir Abad, Shorkot, Pahapur and Kathgarh), Zhob (Hasanzai kili, Mandazai kili, Maryam Ghar, Obata Tsukai, Shin Ghar Kili, Mizri Ghar Kili and Mangalzai) and D. I. Khan (Balo Khel, Awanpur, Watta Khel, Wandhi Ghund Wali, Beruli, Tarri Khel and Rokri. Data on traditional ethnobotanical use were collected from three different ethnic communities (Saraiki, Punjabi and Pashtun). The surveys followed the pattern structured with semi‐structure interviews (Martin, 1995). The project objectives and procedures were clearly explained in the local language. A total of 83 interviews were conducted in the indigenous languages of Pashto, Saraiki and Punjabi because the studied area consists of three regions such as Zhob where native people spoke Pashto, D. I. Khan Saraiki and in Mianwali mostly people speak Punjabi language. We maintained a relationship with the native people of ethnic communities regarding to develop a sense of trust and allowed to stay within the foothill village squares. After that, we accompanied the inhabitants during their day‐to‐day activities and to contribute to their ceremonies.
2.3. Plant collection, identification and submission to the herbarium
Plant species were collected, photographed and essential data were documented on the spot. Medicinal plants were collected during the flowering and fruiting stages in triplicate. All the plants were dried, pressed, preserved and mounted on the standard herbarium sheets and vouchers were allocated in the herbarium. The plant species were duly identified by the plant taxonomist Dr. Mir Ajab Khan and compared with the specimen in Herbarium of Pakistan (ISL). In addition, the names of medicinal plant species were verified by the Medicinal Plant Name Services (MPNS), International Plant Name Index (IPNI) and flora of Pakistan (Nasir and Ali, 1970). The specimens were deposited in Herbarium (ISL) for future reference.
2.4. Ethnoveterinary data for livestock diseases
Eighty‐three informants (67 males and 16 females) were selected from Southwest Pakistan. The informants included farmers, herders and housewives. We have interviewed 23 experienced herders, 49 farmers and 11 housewives from three ethnic communities of Southwest Pakistan. The male candidates were usually done herding; therefore, the people keep knowledge on traditional therapies to treat livestock diseases using the medicinal plants of the surrounding areas.
2.5. Data analysis
2.5.1. Fidelity level
The fidelity level (FL) is useful in identifying the most common key informant species used to treat specific conditions. The FL value of medicinal plants used in the area is higher than that of less popular plants. The proportion of informants who claim to use the same plant species in the same way is represented by the level of fidelity. The goal is to quantify the species' significance for a particular purpose. All reported complaints are classified into main classes before the FL values are calculated (Alexiades and Sheldon, 1996; Friedman et al., 1986), The fidelity level index was calculated using the following formula:
where Np is the number of people who said they used a specific plant for a specific illness category and N is the total number of people who said they used the plant for any ailment category. A higher FL value implies that the plant species is important and used frequently by the informants in the study area to treat a certain condition.
2.5.2. Informant consensus factor
The informant consensus factor (FIC) was utilized to identify plants of specific cultural importance and agreement in the usage of plants for the examination of general plant use. The FIC was used to assess the level of agreement between respondents from the study area and the use of plant species for various disease categories (Vitalini et al., 2009) and was calculated by the following formula(Heinrich et al., 1998; Singh et al., 2012).
where Nur is the number of use citations for a certain disease category and Nt is the total number of botanical species utilized by all informants for a specific use category.
3. RESULTS AND DISCUSSION
3.1. Demographic data of informants
In the current study, 83 people were interviewed in 21 different locations in Southwest Pakistan. The informants were selected based on their knowledge about the traditional plants and their uses. The informants, 47 were men (27 traditional healers, 9 religious scholars and 11 herdsmen) and 36 were women (15 traditional healers and 21 experienced housewives). Thirteen informants were literate while the rest of the informants had not attended school. In addition, most of the informants were illiterate, while some of them have primary and matric level education, which imitates a lack of awareness and unavailability of the standard educational system in these areas. Whereas, we found that illiterate people were found to be more familiar regarding the traditional knowledge of veterinary compared to educated people. Similarly, compared to other professions, traditional health practitioners possessed a broad traditional knowledge of medicinal plant usage. Highly educated informants tended to rely on allopathic drugs for emergency medical care and had little knowledge of herbal medicines and preparation procedures (Amjad et al., 2020)
3.2. Cross‐cultural consensus on ethnoveterinary uses of medicinal plants
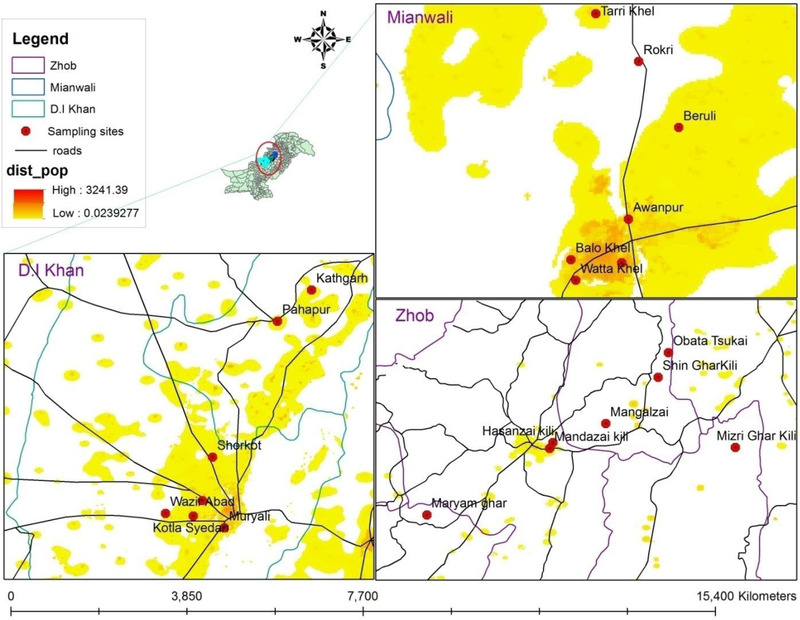
A total of 59 plant species were documented for ethnoveterinary use in traditional medicine for curing 31 animal ailments (Table 1) such as helminthiasis, pneumonia, trypanosomiasis, mastitis, foot and mouth ulcers, tympany, mange, fever, colds, constipation, poison (snake and worm bite), heal wounds, dysentery, increasing lactation, bone fracture, blood clotting, body tonic, gastric problems, scabies, appetite, stimulant, dermatological problems, bloating, anthrax, indigestion, respiratory disorders and urinary disorders in the three ethnic communities of the study areas (Figure 2). A comparison of cross‐cultural use plants for ethnoveterinary practices in Pashto, Punjabi and Sarakai communities are given in Figure 3. According to our results, we found that Saraiki community used less medicinal plants compared to other communities for animal healthcare practices. These results do not mean that Pashto community flora is more diverse and more prominent than Punjab and Saraiki communities. All these might be due to the knowledge and familiar about medicinal plant uses as compared to other communities. The folk knowledge of medicinal plants is usually exclusive to the communities. Previously, several studies on the traditional knowledge of medicinal plants in one or two ethnic groups and neglected the Holo cultural studies of such knowledge (Heinrich et al., 1998). Current studies have shown an increasing tendency of intracultural and intercultural assessments of traditional knowledge on medicinal plants. The intercultural comparative studies have applied applications as they address both the consensus and differences among the different communities. Most frequently used plant species were recorded from three ethnic communities, Cichorium intybus with 56 use reports, Morus nigra (34 URs) followed by Ziziphus oxyphylla (33 URs) and Calotropis procera (30 URs). In Pashto community, the most frequently used species were Acorus calamus with 37 use reports followed by Jurinea berardioides (27 URs) and Convolvulus arvensis (27 URs), while in Punjabi community the highest use reports were documented with the following species: Acacia modesta (21 URs), Ziziphus jujuba (20 URs), Malcolmia cabulica (18 URs) and in Saraiki community Celtis australis (15 URs), Ziziphus nummularia (14 URs) and Dicliptera bupleuroides (11 URs; Table 1). According to the findings of this study, people in the area use these medicinal herbs for animal health care. Furthermore, similar research have been reported in Pakistan's other provinces (Azam Khan et al., 2012; Ul Hassan et al., 2014)
TABLE 1.
Cross‐cultural ethnoveterinary traditional practices of medicinal plants usage among three ethnic communities in Southwest Pakistan
| Vernacular name | Use in community | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Botanical Name | Family | Voucher Number | Pashto | Saraiki | Punjabi | Parts used | Mode of preparation | Pashto | Punjabi | Saraiki | Veterinary Uses & (UR) | FL (%) | Types of animal treated |
| Dicliptera bupleuroides Nees | Acanthaceae | ISI‐H‐78562 | – | Somni | – | Whole plant | Juice, Extract, Decoction | – | – | × | P neumonia (6), Retention of Placenta (2), Appetite stimulant (3) | 54.55 | Buffaloes, Cows |
| Acorus calamus L. | Acoraceae | ISI‐H‐78964 | Bach | – | – | Rhizome | Juice | × | – | – | Anaplasmosis (2), Mastitis(4), Constipation (6), Heal wounds (7), Dysentery (3), Body tonic (4), Gastric problems (5), Bloating (2), Indigestion (2), Urinary disorders (2) | 24.32 | Cows, Sheeps, Goats, Donkeys, Camels, Buffaloes |
| Aerva javanica (Burm.f.) Juss. ex Schult. | Amaranthaceae | ISI‐H‐78965 | Bui Booti | Bui | bhuii | Aerial parts | Juice, infusion | × | × | × | C onstipation (5),Gastric problems (9), Dermatological problems (5), Indigestion (3) | 40.91 | Sheeps, Goats, Donkeys |
| Atriplex lasiantha Boiss. | Amaranthaceae | ISI‐H‐78552 | Zumai | – | – | leaves | powdered, decoction | × | – | – | Pneumonia (3), Conjunctivitis (2), Gastric problems (7), Bloating (1) | 53.85 | Cows, Sheeps, Camels, Buffaloes |
| Chenopodium foliosum Asch. | Amaranthaceae | ISI‐H‐78558 | joasag | – | – | leaves | Powdered | × | – | – | Increasing lactation (4), Fever (3), Foot and mouth ulcers (6), Pneumonia (4) | 35.29 | Goats, Buffaloes |
| Ferula oopoda (Boiss. & Buhse) Boiss. | Apiaceae | ISI‐H‐78566 | hing | – | – | Aerial parts | Paste, powdered | × | – | – | Theileriosis (4), Fever (2), Constipation (3), Gastric problems (2), Appetite stimulant (1), Indigestion (3) | 26.67 | Sheeps, Goats, Donkeys |
| Trachyspermum ammi (L.) Sprague | Apiaceae | ISI‐H‐79013 | .سپرکئ | سپرئ | اجوائن | Fruits | Eaten raw form | × | × | × | M ange (4), Dysentery (3), Gastric problems (7), Appetite stimulant (4), Bloating (3), Indigestion (2) | 30.43 | Donkeys, Camels, Buffaloes |
| Calotropis procera (Aiton) Dryand. | Apocynaceae | ISI‐H‐78971 | spalmai | Akh | Akh | Flowers, leaves, latex | Juice, Decoction | × | × | × | R espiratory disorders (4), Anthrax (3), Scabies (2), Bone fracture (6), Poison (snake and worm bite) (2), Retention of Placenta (4), Anaplasmosis (3), Mastitis (3), Helminthiasis (3) | 20.00 | Buffaloes, Goats |
| Asparagus capitatus Baker | Asparagaceae | ISI‐H‐78436 | Satawar | – | – | young shootts | Paste | × | × | × | T ympany (1),Mastitis (2), Diarrhoea (4), Colds (6), Increasing lactation (3), Body tonic (7) | 30.43 | Cows, Sheeps |
| Asparagus officinalis L. | Asparagaceae | ISI‐H‐78969 | Teen doni | – | – | Young Leaves bud | Juice | × | × | × | T rypanosomiasis (2), Theileriosis (1), Diarrhoea (1), Fever (1), Heal wounds (4), Increasing lactation (6), Scabies (2), Anthrax (2), Respiratory disorders (2), Urinary disorders (4) | 24.00 | Goats, Donkeys, Camels |
| Jurinea berardioides (Boiss.) O.Hoffm. | Asteraceae | ISI‐H‐78576 | Not known | – | – | Leaves | Paste | × | – | – | Anthrax (4), Dermatological problems (4), Heal wounds (3),Poison (snake and worm bite) (2), Colds (5), Conjunctivitis (3), Mange (3), Trypanosomiasis (3) | 18.52 | Cows, Sheeps, Goats, Camels |
| Artemisia biennis Willd | Asteraceae | ISI‐H‐78437 | Tharkha | – | – | Aerial parts | Powdered, extract | × | – | – | Helminthiasis (5), Trypanosomiasis (2), Anaplasmosis (1), Diarrhoea (3), Bloating (4), Respiratory disorders (3) | 27.78 | Goats, Donkeys, Camels, Buffaloes |
| Artemisia scoparia Waldst. & Kitam. | Asteraceae | ISI‐H‐78438 | Gajar | – | – | Aerial parts | Paste, extract | × | – | – | Foot and mouth ulcers (3), Mastitis(2), Pneumonia (4), Appetite stimulant (3), Respiratory disorders (3), Urinary disorders (2) | 23.53 | Buffaloes, Camels |
| Cichorium intybus L | Asteraceae | ISI‐H‐78978 | Kasni | – | – | Aerial parts | Juice, Powdered, Decoction | × | × | × | G astric problems (5), Body tonic (2), Blood clotting (1), Bone fracture (4), Heal wounds (3), Constipation (5), Fever (2), Diarrhoea (4), Retention of Placenta (6), Anaplasmosis (3), Conjunctivitis (3), Foot and mouth ulcers (4), Mastitis (4), Trypanosomiasis (1), Pneumonia (3), Helminthiasis (6) | 10.71 | Cows, Camels, Buffaloes |
| Echinops echinatus Roxb | Asteraceae | ISI‐H‐78529 | Kundiari | – | – | Root | Decoction | × | – | – | Tympany (3), Bone fracture (7), Dermatological problems (2) | 58.33 | Sheeps, Goats |
| Launaea spinosa (Forssk.) Kuntze | Asteraceae | ISI‐H‐78440 | Bubar Aghzai/ZOZ | – | – | Whole plant | Powdered, Infusion | × | – | – | Tympany (6) | 100.00 | Cows, Sheeps |
| Varthemia persica DC. | Asteraceae | ISI‐H‐78439 | Not known | – | – | Whole plant | powdered, decoction, paste | × | – | – | Body tonic (3), Scabies (4), Trypanosomiasis (2) | 44.44 | Goats, Donkeys, Camels |
| Launaea oligocephala (Bornm.) Bornm | Asteraceae | ISI‐H‐78441 | Markharai | – | – | Flowers | Extract | × | – | – | Diarrhoea (4), Increasing lactation (5), Helminthiasis (2) | 45.45 | Camels, Cows, Sheeps |
| Buglossoides arvensis (L.) I.M.Johnst. | Boraginaceae | ISI‐H‐78555 | Not known | – | – | leaves | Juice, Powdered,infusion | – | × | – | Tympany (3), Bloating (5) | 62.50 | Cows, Sheeps, Goats, Buffaloes |
| Mattiastrum asperum (Stocks) Brand | Boraginaceae | ISI‐H‐78442 | Not known | – | – | Whole plant | Powdered | × | – | – | Anthrax (9) | 100.00 | Donkeys, Camels |
| Conringia orientalis (L.) Dumort. | Brassicaceae | ISI‐H‐78443 | Not known | – | – | Aerial parts | Extract, paste | × | – | – | Increasing lactation (11) | 100.00 | Camels, Buffaloes |
| Diplotaxis griffithii (Hook.f. & Thomson) Boiss | Brassicaceae | ISI‐H‐78580 | Janbo, تریخ ساگ | – | – | Whole plant | Juice, Extract, Infusion | × | – | – | Bone fracture (8) | 100.00 | Cows, Sheeps, Camels |
| Malcolmia cabulica (Boiss.) Hook. f. & Thomson | Brassicaceae | ISI‐H‐78582 | – | – | khatol | Leaves | Decoction, Infusion | – | × | – | Respiratory disorders (4), Indigestion (5), Dermatological problems (4), Increasing lactation (5) | 27.78 | Buffaloes, Cows, Goats |
| Buxus papillosa C.K.Schneid. | Buxaceae | ISI‐H‐78556 | Shamshad/Angaroo | – | – | leaves | Decoction | × | – | – | Foot and mouth ulcers (6), Fever (6) | 50.00 | Cows, Sheeps, Goats, Buffaloes |
| Celtis australis L | Cannabaceae | ISI‐HS‐41 | – | Batkarar | – | Leaves, Fruit | Decoction | – | – | × | I ndigestion (3), Bloating (4), Blood clotting (2), Dysentery (3), Poison (snake and worm bite) (3) | 26.67 | Sheeps, Buffaloes |
| Acanthophyllum squarrosum Boiss | Caryophyllaceae | ISI‐H‐78444 | Shah‐verdar, Kucha‐ghazi, کنڈہ باغ | – | – | Roots, flowers | Powder, Decoction | × | – | – | Respiratory disorders (7) | 100.00 | Goats, Buffaloes |
| Dianthus crinitus Sm | Caryophyllaceae | ISI‐H‐78445 | – | – | – | Aerial parts | Powdered, extract | × | – | – | Dysentery (10) | 100.00 | Goats, Cows, Sheeps |
| Cleome brachycarpa (Forssk.) Vahl ex DC | Cleomaceae | ISI‐H‐78560 | – | – | Gandi booti | Whole plant | Powdered | – | × | – | Fever (3), Blood clotting (2), Scabies (9) | 64.29 | Cows, Buffaloes |
| Convolvulus arvensis L. | Convolvulaceae | ISI‐H‐78981 | Prewaty | – | – | Root | Juice | × | – | – | Urinary disorders (4), Anthrax (3), Appetite stimulant (3), Blood clotting (3), Bone fracture (5), Poison (snake and worm bite) (1), Fever (2), Theileriosis (1), Mastitis(2), Helminthiasis (3) | 18.52 | Goats, Cows, Camels, Buffaloes |
| Elaeagnus angustifolia L. | Elaeagnaceae | ISI‐HS‐I | Kankoli | – | – | Fruit | Decoction | × | – | – | Blood clotting (4), Body tonic (7) | 63.64 | Cows, Sheeps, Goats, Buffaloes |
| Elaeagnus umbellata Thunb. | Elaeagnaceae | ISI‐HS‐26 | Kanrkoli | – | – | Fruit | Eaten raw form | × | – | – | Diarrhoea (9) | 100.00 | Sheeps, Buffaloes, Cows, Camels |
| Ephedra intermedia Schrenk & C.A.Mey | Ephedraceae | ISI‐H‐78446 | غٹ اومان | – | – | Stem | Juice, Powder, Paste, Poultice | × | – | – | Respiratory disorders (5), Colds (4), Retention of Placenta (2), Anaplasmosis (1), Pneumonia (4) | 31.25 | Buffaloes, Cows, Donkeys, Camels, Sheeps, Goats |
| Ephedra major subsp. procera (C.A.Mey.) Bornm. | Ephedraceae | ISI‐H‐78447 | نرئ اومان | – | – | Stem | Juice, Powder, Paste, Poultice | × | – | – | Colds (6), Bloating (4), Urinary disorders (3) | 46.15 | Cows, Sheeps, Goats, Donkeys, Camels, Buffaloes |
| Euphorbia serpens Kunth | Euphorbiaceae | ISI‐H‐78448 | Bunai | Buni | – | leaves | Paste | × | – | – | Poison (snake and worm bite) (5), Tympany (3) | 62.50 | Donkeys, Camels, Cows, Sheep, Buffaloes, Goats |
| Ricinus communis L. | Euphorbiaceae | ISI‐H‐79006 | Hernoli | Arand | Arand | Fruit, Leaves | As food | × | × | × | R etention of Placenta (11), Poison (snake and worm bite) (7) | 61.11 | Cows, Camels, Buffaloes |
| Centaurium tenuiflorum (Hoffmanns. & Link) Fritsch | Gentianaceae | ISI‐H‐78557 | – | kanderi | – | flowers | juice, extract | – | – | × | A naplasmosis (3), Colds (4) | 57.14 | Goats, Sheeps, Cows, Donkeys, Camels, Buffaloes |
| Lycopus europaeus L. | Lamiaceae | ISI‐H‐78449 | Not known | – | – | Aerial parts | Paste, extract | × | – | – | Conjunctivitis (8) | 100.00 | Cows, Sheeps, Goats |
| Acacia modesta Wall. | Fabaceae | ISI‐H‐78534 | – | – | Palosa | Leaves | Infusion | – | × | – | Urinary disorders (7), Bloating (2), Scabies (3), Colds (4), Mange (5) | 33.33 | Sheeps, Cows, Buffaloes, Goats, Donkeys, Camels |
| Acacia nilotica (L.) Delile | Fabaceae | ISI‐H‐78962 | babul | Kikar | Kikar | Seeds, gum | Decoction, juice | × | × | × | H elminthiasis (2), Foot and mouth ulcers (3), Anaplasmosis (1), Constipation (8), Dysentery (6), Gastric problems (7), Indigestion (2) | 27.59 | Goats, Sheeps, Cows, Donkeys, Camels, Buffaloes |
| Albizia lebbeck (L.) Benth | Fabaceae | ISI‐H‐78549 | – | Sirin, Siris | Bark, Leaves | Powdered, Paste | – | × | – | Dermatological problems (6), Colds (3) | 66.67 | Cows, Sheeps, Goats, Buffaloes | |
| Astragalus stocksii Bunge | Fabaceae | ISI‐H‐78450 | Shenallo | – | – | Leaves | powdered | × | – | – | Heal wounds (7), Dermatological problems (6) | 58.33 | Sheeps, Goats, Donkeys |
| Astragalus anisacanthus Boiss | Fabaceae | ISI‐H‐78451 | Kunda Zarga, سسئ | – | – | Leaves | Extract, Juice, Infusion | × | – | – | Constipation (7) | 100.00 | Cows, Sheeps, Goats, Camels, Buffaloes |
| Caragana ambigua Stocks | Fabaceae | ISI‐H‐78535 | Makhi, ماخئ | – | – | Leaves, Flower | Eaten raw, Powder, Juice | × | – | – | Heal wounds (4), Scabies (9) | 69.23 | Cows, Goats, Buffaloes |
| Ebenus stellata Boiss | Fabaceae | ISI‐H‐78564 | Sambal, بخال | – | – | Leaves, Stem | Powder, Paste, Decoction | × | – | – | Indigestion (14) | 100.00 | Sheeps, Goats, Donkeys |
| Lathyrus aphaca L. | Fabaceae | ISI‐HS‐35 | Jangali matter | chota matar | matar | Pods | Eaten raw form | × | × | × | M ange (6), Fever(3), Increasing lactation (8) | 47.06 | Donkeys, Camels, Buffaloes |
| Grewia asiatica L | Malvaceae | ISI‐H‐78519 | Phalsa | falsa | falsa | Leaves | Eaten raw, Paste | × | × | × | A ppetite stimulant (2), Urinary disorders (4), Heal wounds (9) | 60.00 | Sheeps, Goats, Buffaloes |
| Morus nigra L. | Moraceae | ISI‐H‐78998 | Toor toot | Black toot | Kala toot | Fruit | Juice, Infusion | × | × | × | T rypanosomiasis (2), Foot and mouth ulcers (3), Anaplasmosis (2), Fever (4), Dysentery (5), Increasing lactation(6), Blood clotting (4), Bloating (5), Respiratory disorders (3) | 17.65 | Cows, Sheeps, Goats, Camels, Buffaloes |
| Morus alba L. | Moraceae | ISI‐HS‐59 | Safeed toot | White toot | Chita toot | Leaves | Decoction | – | × | – | Heal wounds (5), Respiratory disorders (2) | 71.43 | Goats, Cows, Sheeps |
| Fraxinus xanthoxyloides (G.Don) Wall. ex A.DC. | Oleaceae | ISI‐H‐78424 | – | – | Shang | Leaves | Decoction | – | × | – | Heal wounds (5), Colds (2), Conjunctivitis (4) | 45.45 | Goats, Buffaloes, Cows, Sheeps |
| Limonium cabulicum (Boiss.) Kuntze | Plumbaginaceae | ISI‐H‐78541 | ghwagai, Mashnawaro, غواگئ | – | – | Whole plant | Juice, powder, infusion | × | – | – | Tympany (5),Theileriosis (3) | 62.50 | Cows, Sheeps, Buffaloes |
| Cymbopogon jwarancusa (Jones) Schult | Poaceae | ISI‐H‐78984 | Sargary | Kavi | Khavi | Leaves | Decoction | × | × | × | F ever (8), Poison (snake and worm bite) (6), Blood clotting (4), Gastric problems (9) | 34.62 | Sheeps, Goats, Cows, Buffaloes |
| Atraphaxis spinosa L. | Polygonaceae | ISI‐H‐78551 | Karwankush | – | – | Leaves | Extract, powdered | × | – | – | Conjunctivitis (9), Scabies (5) | 64.29 | Goats, Cows, Sheeps |
| Adonis aestivalis L. | Ranunculaceae | ISI‐H‐78544 | unknown | – | – | Whole plant | Decoction | × | – | – | Trypanosomiasis (2), Mange (12) | 85.71 | Cows, Sheeps, Buffaloes |
| Clematis graveolens Lindl. | Ranunculaceae | ISI‐H‐78552 | Malaghonai | – | – | leaves | Decoction | × | – | – | Appetite stimulant (3), Anthrax (4) | 57.14 | Sheeps, Buffaloes, Goats, Camels |
| Ziziphus jujuba Mill | Rhamnaceae | ISI‐HS‐6 | – | – | Ber | Leaves, Fruit | Eaten raw, Paste, Powdered | – | × | – | Mastitis (5), Tympany (2), Diarrhoea (6), Anthrax (7) | 35.00 | Cows, Sheeps, Goats, Buffaloes |
| Ziziphus nummularia (Burm.f.) Wight & Arn. | Rhamnaceae | ISI‐H‐78545 | Beeri | Fruit | Decoction | – | – | × | D ermatological problems (9), Blood clotting (5) | 64.29 | Camels, Buffaloes | ||
| Ziziphus oxyphylla Edgew. | Rhamnaceae | ISI‐H‐78453 | Phitni | Jhar ber | Jhar ber | Fruit, Root | Eaten raw, powdered | × | × | × | U rinary disorders (3), Dermatological problems (9), Blood clotting (4), Colds (7), Retention of Placenta (3), Mange (4), Helminthiasis (3) | 27.27 | Camels, Buffaloes, Donkeys, Sheeps, Goats, Cows |
| Withania somnifera (L.) Dunal | Solanaceae | ISI‐H‐78548 | – | – | lakri | Leaves, Stem | Juice | – | × | – | Bone fracture (6), Constipation (3), Diarrhoea (3), Anaplasmosis (1), Conjunctivitis (3) | 37.50 | Goats, Camels, Buffaloes |
| Withania coagulans (Stocks) Dunal | Solanaceae | ISI‐H‐78435 | خمازورہ | Panir | Panirbad | Leaves, roots, Fruits | Eaten raw form | × | × | × | I ndigestion (3), Dermatological problems (5), Gastric problems (7), Bone fracture (7), (snake and worm bite) (2), Fever (3), Retention of Placenta (2) | 24.14 | Sheep, Camels, Buffaloes |
FIGURE 2.
Proportion of veterinary diseases treated among three ethnic communities
FIGURE 3.
Plant utilization patterns among the three ethnic communities for veterinary diseases
3.3. Diversity of ethnoveterinary medicinal plants and cross‐cultural uses
These three communities (Pashto, Mianwali, D. I. Khan) residing in three regions such as Zhob, Mianwali, D. I. Khan and are parts of Southwest Pakistan, however they are isolated on the basis of phytogeography, climatic conditions, linguistics status and other cultural aspects. A total of 59 plant species, among them 14 plant taxa were commonly used in the three communities for the ethnoveterinary practices such as Aerva javanica (Burm.f.) Juss. ex Schult., Trachyspermum ammi (L.) Sprague, Calotropis procera (Aiton) Dryand., Asparagus capitatus Baker, Asparagus officinalis L., Cichorium intybus L, Ricinus communis L., Acacia nilotica (L.) Delile, Lathyrus aphaca L., Grewia asiatica L, Morus nigra L., Cymbopogon jwarancusa (Jones) Schult, Ziziphus oxyphylla Edgew and Withania coagulans (Stocks) Dunal. These certain differences in the utilization of plants and their parts were noticed in both regions of Southwest Pakistan. For instance, aerial part of Cichorium intybus was used for gastric problems, body tonic, blood clotting in Saraiki community, while in the Punjabi community, for bone fracture, healing wounds, constipation and in Pashto community, it is used to treat fever, diarrhoea, retention of anaplasmosis, conjunctivitis, placenta, foot and mouth ulcers, mastitis, trypanosomiasis, pneumonia and helminthiasis. M. nigra is utilized for foot and mouth ulcers, Anaplasmosis, fever, dysentery in Saraiki community, while in the Punjabi community it is recorded for increasing lactation and in Pashto community used for blood clotting, bloating, respiratory disorders and trypanosomiasis. Several other studies have been reported that M. nigra is used for throat inflammation cough, cold and constipation in other regions of Pakistan (Aziz et al., 2018; Tariq et al., 2014). Fruit and root of Z. oxyphylla were extensively used as urinary disorders in Punjabi community, in Saraiki community used for dermatological problems, blood clotting and colds; while in Pashto community its use was recorded against retention of placenta, mange and helminthiasis. The ethnic Pashto community considers the leaves of C. procera useful in respiratory disorders, anthrax, bone fractures and in Punjabi community it is used for scabies, poison (snake and worm bites), anaplasmosis, mastitis, helminthiasis, while in the residents of Saraiki community used for retention of Placenta. A. nilotica is used for helminthiasis, foot and mouth ulcers in Saraiki community and Punjabi community used for anaplasmosis while in Pashto communities used for constipation, dysentery, gastric problems and indigestion. W. coagulans is given for the retention of placenta, indigestion, dermatological problems in Pashto community and Punjabi community is used for gastric problems, bone fracture, while in Saraiki community it is reported for the treatment of fever. C. jwarancusa is widely used in Pashto community for fever, poison (snake and worm bite) and in Punjabi community, it is used for blood clotting while it is used only for gastric problems in Saraiki community as shown in Table 1. This is probably because of the lack of agreement between three ethnic communities in ethno‐veterinary medicinal plants or because of unique vegetation and different socio‐cultural values. Similar research have found that ethnic communities employ different plants due to differences in cultural/ ethnicity and ecology/geography (Aziz et al., 2020).
3.4. Dominant plant families used as ethnoveterinary medicine
Asteraceae and Fabaceae families have been reported at first rank from three ethnic communities while Poaceae and Polygonaceae as the least utilized families recorded as depicted. Similar results have also been reported by previous studies that Asteraceae was the second dominant family. The Asteraceae were the predominant family due to the wildly distributed species in the area (Fortini et al., 2016; Güzel et al., 2015; Islam et al., 2014; Sadat‐Hosseini et al., 2017). Other remaining ethnoveterinary plant families in three ethnic communities include Amaranthaceae, Brassicaceae and Rhamnaceae with three species, Apiaceae, Asparagaceae, Boraginaceae, Caryophyllaceae, Elaeagnaceae, Ephedraceae, Euphorbiaceae, Moraceae, Ranunculaceae, Solanaceae and Poaceae with two species each and remaining fourteen families belonging to one species each (Figure 4). Based on the obtained results for each family in terms of use reports, it is possible to deduce that the plants in these families may contain some specific pharmacologically active chemicals/secondary metabolites that make them useful for treating a variety of disorders. Therefore, members of all these plant families, especially Asteraceae and Fabaceae as well as other families have worth to investigate the chemical constituents and pharmacologically for the discovery of new ethnoveterinary drugs (Abdalla and Zidorn, 2020; Koc et al., 2015; Obakiro et al., 2021; Surendran et al., 2021)
FIGURE 4.
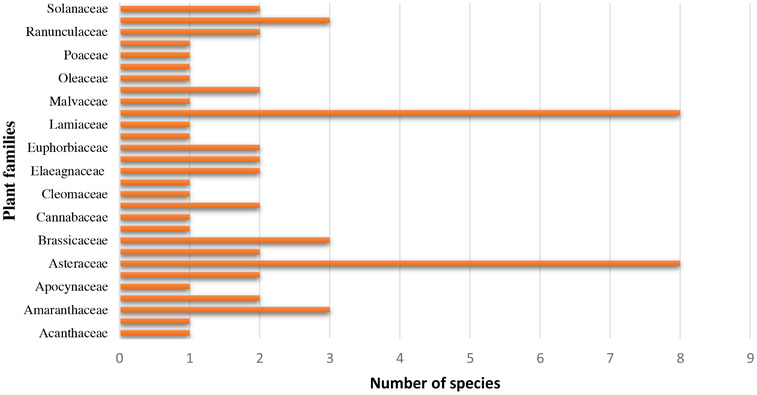
Dominant ethnoveterinary plant families used cross‐culturally
3.5. Plant parts used and modes of preparation
Herbal recipes were prepared using various plant parts in the study area. As shown in Figure 5, leaves were the most preferred plant parts used in the preparation of traditional veterinary medicine followed by fruits, whole plant, aerial parts, roots, flower and the stem. The rhizome, latex shoots, seeds, gum, bark and pods were the least parts used in the preparation (Figure 5). The key process of herbal remedy preparation for the cure of malaria was decoction (79%). These findings were consistent with previously reported studies from Pakistan and other countries (Asase et al., 2010; Kankara et al., 2015; Koudouvo et al., 2011; Nguta et al., 2010). Additionally, the usage of leaves is considered as less hazardous for the plants in comparison to the use of other parts (bark) and whole plants. Similar results were also reported by a previous study (Yetein et al., 2013). The most common method of traditional remedies in preparation for veterinary practice was used in the form of powdered (22) that is consistent with the previously reported literature indicating that most remedies were prepared in the form of powder (Aziz et al., 2020). In addition, the respondents also employed preparation of decoction (19), juice (18), paste (14), extract (11), infusion (9), eaten raw form (8), poultice (2), as food (1) (Figure 6).
FIGURE 5.
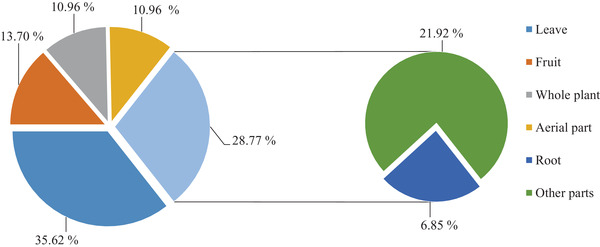
Plant parts used to prepare medicinal regimes
FIGURE 6.
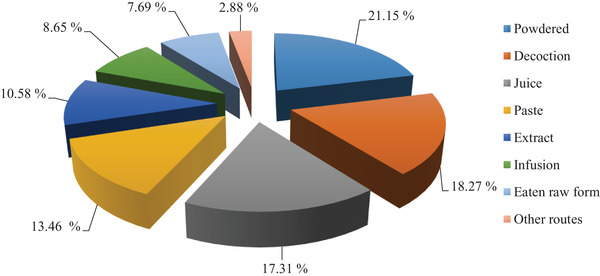
Route of administration of medicinal plant preparations
3.6. Ethnoveterinary practices of medicinal plants
Most frequently used plants in veterinary practices among three ethnic communities were A. javanica, T. ammi, A. capitatus, C. procera, A. officinalis, R. communis, C. intybus, A. nilotica, L. aphaca, G. asiatica, C. jwarancusa, M. nigra, Z. oxyphylla, W. coagulans and C. intybus is most frequently used in the treatment of ethnoveterinary services such as gastric problems, body tonic, blood clotting, bone fracture, healing wounds, constipation, fever, diarrhoea, retention of Placenta, anaplasmosis, conjunctivitis, foot and mouth ulcers, mastitis, trypanosomiasis, pneumonia and helminthiasis. A. javanica is used for the treatment of gastric problems, constipation, dermatological problems and indigestion. M. nigra is used in various veterinary practices like trypanosomiasis, foot and mouth ulcers, anaplasmosis, fever, dysentery, increased lactation, blood clotting, bloating and respiratory disorders. T. ammi is used in the treatment of mange. A. capitatus is used against diarrhoea, colds and increasing lactation. Similarly, C. procera is effective in mastitis treatment, retention of placenta, bone fractures, anthrax and respiratory disorders. Seeds of W. coagulans were used for gastric problems, fever and retention of placenta (Table 1).
A literature survey has revealed similar and different ethnoveterinary uses of medicinal plants by indigenous communities. The C. intybus was used to increase milk production (Nwafor et al., 2017; Waugh et al., 1998). In addition, aerial parts of C. intybus were also traditionally used for the treatment of stomach problems and used to maintain body heat (Lans et al., 2006; Lans et al., 2007). A. javanica was used for skin infection (Abbasi et al., 2013). The leaves of M. nigra were used for anti‐inflammatory (Manganelli et al., 2001). T. ammi was reported for cold and cough (Yadav et al., 2014), blot, anorexia, pneumonia, abdominal pain (Phondani et al., 2010), appetite stimulant, galactagogue (Abbasi et al., 2013). The latex of Calotropis procera is used to treat with inflammation (Kumar and Roy, 2007), dermal problems and poison (snake bite) (Jain et al., 1996). Withania coagulans is used as carminative, eliminate flatulence (Khattak et al., 2015), body coolness, abdominal pain, external wounds, sunstroke, jaundice, skeleton‐muscular pain aliments (Ahmad et al., 2015), trypanosomiasis (Raziq et al., 2010), digestive disorders (Muhammad et al., 2005), diarrhoea (Mussarat et al., 2014). Xiong & Long (2020) also reported that indigenous communities of Southwest Guizhou, China has rich use of medicinal plants and traditional remedies for ethnoveterinary practices. The comparison of current results with earlier studies shows multiple uses of medicinal plants in different parts of the country.
3.7. Veterinary disease categories and plant usage
The reported 59 plant taxa were used for 31 different veterinary diseases. 13 species were used for fever with a total of 39 reports. C. intybus was the most frequently used plant species with the highest use report 56 among all three ethnic groups. To heal wounds, blood clotting, dermatological problems, bloating (10 species each) were recorded, most commonly G. asiatica with nine reports. Nine plant species were cited for each disease with different reports such as gastric problems (58 URs), increased lactation (52 URs), bone fracture (54 URs), constipation (45 URs), anthrax (42 URs), diarrhea (39 URs), indigestion (37 URs), respiratory disorders (33 URs), urinary disorders (33 URs), colds (30 URs) and anaplasmosis (17 URs). Similarly, eight plant species were cited for scabies (38 URs), helminthiasis (29 URs), mastitis (26 URs) and appetite stimulant (21 URs). For trypanosomiasis (14 URs), foot and mouth ulcers (28), tympany (23 URs), Mange (37 URs), Conjunctivitis (32 URs), theileriosis (15 URs), retention of placenta (30 URs), poison (snake and worm bite) (26 URs), Dysentery (31 URs), nine species are named. Six plant species were reported for body tonic (26 URs) and pneumonia (24 URs). Previously, 36 ethnoveterinary disease categories had been reported (Verma, 2014). Similar uses of some plants were also supported by other studies from Pakistan and other countries (Abbasi et al., 2013; Antonio et al., 2015; Assefa and Bahiru, 2018; Aziz et al., ; Bahmani and Eftekhari, 2013; Benítez et al., 2012; Gabalebatse et al., 2013; Parthiban et al., 2016; Sharma and Manhas, 2015; Tariq et al., 2014).
Culture and ethnicity have a strong impact on traditional ethnoveterinary medicine systems (Aziz et al., 2018). By comparing the medicinal plant species used nowadays in Sardinia and Sicily with those reported in old texts and found that 74% of the uses were similar to those reported previously (Leonti et al., 2009). Exploring the cross‐cultural analysis of medicinal plants traditionally used among two regions (Bajaur agency and Waziristan agency) in federally administrated tribal areas of Pakistan reported 94 plant taxa used in the ethnoveterinary practices (Aziz et al., 2018). Similarly, investigated the traditional use of medicinal plants among three ethnic groups (Kalasha, Ismaeli and Sunni) in Chitral District, Khyber Pakhtunkhwa province, Pakistan and reported 76 plant species used for the treatment of various diseases (Sher et al., 2016). The cross‐cultural studies are very significant to determine and enlist the traditional ethnobotanical knowledge, similarities and variation among different ethnic groups in plant utilization.
3.8. Quantitative analysis of the data
The collected data was quantitatively analysed by informant consensus factor and fidelity level. The maximum FL values were observed for L. spinosa, M. asperum, C. orientalis, D. griffithii, A. squarrosum, D. crinitus, E. umbellata, L. europaeus, A. anisacanthus and E. s stellata has 100% FL values represented in the Table 1. The high values indicate that these species are culturally important medicinal species and valued by the local inhabitants to treat a particular disease (Uddin and Hassan, 2014). The informant consensus index values varied between 0.84 (reproductive disorders) and 0.70 (Infection). Reproductive disorders had the highest FIC values with 284 use reports, followed by skin diseases and injuries (0.80) with 293 citations are reported (Table 2). The highest FIC values indicate that either the disease was very prevalent in the area, or that reported plant species are commonly used for the treatment of that particular disease. The FIC determines the plants, which are inter‐culturally important and used to treat similar diseases, as a result FIC determines cross culturally important species (Aziz et al., 2018; Muhammad et al., 2005).
TABLE 2.
Informant Consensus Factor (ICF) by category of ailment within the present study
| Ailment Category | Number of use‐Report | Number of species | ICF |
|---|---|---|---|
| Abdominal disorders | 218 | 52 | 0.76 |
| Skin diseases and injuries | 293 | 60 | 0.80 |
| Breast diseases and milk production | 78 | 17 | 0.79 |
| Inflammatory diseases | 56 | 13 | 0.78 |
| Infection (with virus, bacteria or parasite) | 284 | 85 | 0.70 |
| Reproductive disorders | 93 | 16 | 0.84 |
| Respiratory disorders | 33 | 9 | 0.75 |
| Toxic chemicals | 26 | 7 | 0.76 |
4. CONCLUSIONS
According to our best knowledge, this study revealed for the first time a cross‐cultural use of medicinal plants among three main ethnic communities in Southwest Pakistan. These ethnicities typically rely on indigenous flora for basic health care and traditional healers, shepherds, religious scholars and elder people of the area hold the traditional knowledge. In this cross‐cultural and comparative study, 59 medicinal plants have been reported, with 14 plant species being widely used by all three ethnic communities, followed by 32 species in Pashto, nine species in Punjabi and five species in Saraiki. The lack of interregional agreement and wide disparities in medicinal plants used in different areas may be related to cultural differences and ecological diversity. This study will serve as a foundation for future pharmacological, phytochemical and scientific validation, therefore assisting in the development of new, low‐cost medicines. The current study highlights the importance of traditional medicinal plant uses in different cultures. Elders and health practitioners mostly hold the traditional knowledge, while the younger generation is uninterested in herbal formulas. The lack of attention contributes to deforestation and reduction of medicinal flora in the area. The study recommends further investigation of these plants for phytochemical, toxicological and clinical studies to develop an improved and clear understanding of the dosage safety and effectiveness of this precious treasure. To maintain and preserve indigenous folk knowledge of medicinal plants and its applications, people must be the educated about the significance of these plants in order to be motivated to conserve and sustainably use of the local flora for ethnobotanical and pharmacological research.
COMPETING INTEREST
The authors have no competing interests.
AUTHOR CONTRIBUTIONS
SZA and AM designed and conducted the experimental work. RK, GSB interpreted the results. MA, AS, AAK and MZ guided the project and coordinated the survey work. AA and MZB analyzed the data and manuscript writing and literature collection HFH, MHM, AM, SZA and AS manuscript writing. The manuscript was finalized by all authors.
ACKNOWLEDGEMENTS
The authors would like to thanks King Saud University (Riyadh, Saudi Arabia) for supporting this study under researchers supporting project number (RSP‐2021/406). We are grateful to the three ethnic communities for their logical assistance and contributions in the documentation of indigenous ethnomedicinal knowledge. Muhammad Zeeshan Bhatti: Conceptualization; Writing‐original draft
Abidin, S.Z.U., Munem, A., Khan, R., Batiha, G.E.‐S., Amhad, M., Zafar, M., Khalil, A.A.K., Hetta, H.F., Mahmoud, M.H., Sami A., & Bhatti, M.Z. (2021). Ethnoveterinary botanical survey of medicinal plants used in Pashto, Punjabi and Saraiki Communities of Southwest Pakistan. Veterinary Medicine and Science, 7, 2068–2085. 10.1002/vms3.582
Sheikh Zain Ul Abidin and Afifa Munem contributed equally to this work.
REFERENCES
- Abbasi, A.M., Khan, S.M., Ahmad, M., Khan, M.A., Quave, C.L., & Pieroni, A. (2013). Botanical ethnoveterinary therapies in three districts of the Lesser Himalayas of Pakistan. Journal of Ethnobiology and Ethnomedicine, 9, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdalla, M.A., & Zidorn, C. (2020). The genus Tragopogon (Asteraceae): A review of its traditional uses, phytochemistry and pharmacological properties. Journal of Ethnopharmacology, 250, 112466. [DOI] [PubMed] [Google Scholar]
- Agra, M.F., Baracho, G.S., Nurit, K., Basílio, I.J.L.D., & Coelho, V.P.M. (2007). Medicinal and poisonous diversity of the flora of “Cariri Paraibano”, Brazil. Journal of Ethnopharmacology, 111(2), 383–395. [DOI] [PubMed] [Google Scholar]
- Ahmad, K., Ahmad, M., & Weckerle, C. (2015). Ethnoveterinary medicinal plant knowledge and practice among the tribal communities of Thakht‐e‐Sulaiman hills, west Pakistan. Journal of Ethnopharmacology, 170, 275–283. [DOI] [PubMed] [Google Scholar]
- Ahmad, S.S. (2007). Medicinal wild plants from Lahore‐Islamabad motorway (M‐2). Pakistan Journal of Botany, 39(2), 355–375. [Google Scholar]
- Alexiades, M.N., & Sheldon, J.W. (1996). Selected Guidelines for Ethnobotanical Research: A Field Manual. New York Botanical Garden. [Google Scholar]
- Ali‐Shtayeh, M.S., Jamous, R.M., & Jamous, R.M. (2016). Traditional Arabic Palestinian ethnoveterinary practices in animal health care: a field survey in the West Bank (Palestine). Journal of Ethnopharmacology, 182, 35–49. [DOI] [PubMed] [Google Scholar]
- Alves, R. R. N., Barbosa, J.A. A., Santos, S.L. D. X., Souto, W. M. S., & Barboza, R. R. D. (2011). Animal‐Based Remedies as Complementary Medicines in the Semi‐Arid Region of Northeastern Brazil. Evidence‐Based Complementary and Alternative Medicine, 2011, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves, R.R., & Rosa, I.L. (2005). Why study the use of animal products in traditional medicines? Journal of Ethnobiology and Ethnomedicine, 1, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves, R.R., & Rosa, I.M. (2007). Biodiversity, traditional medicine and public health: where do they meet? Journal of Ethnobiology and ethnomedicine, 3, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amjad, M.S., Zahoor, U., Bussmann, R.W., Altaf, M., Gardazi, S.M.H., & Abbasi, A.M. (2020). Ethnobotanical survey of the medicinal flora of Harighal, Azad Jammu & Kashmir, Pakistan. Journal of Ethnobiology and Ethnomedicine, 16, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonio, R., Souza, R., Furlan, M., Pedro, C., Cassas, F., Honda, S., & Rodrigues, E. (2015). Investigation of urban ethnoveterinary in three veterinary clinics at east zone of São Paulo city, Brazil. Journal of Ethnopharmacology, 173, 183–190. [DOI] [PubMed] [Google Scholar]
- Asase, A., Akwetey, G.A., & Achel, D.G. (2010). Ethnopharmacological use of herbal remedies for the treatment of malaria in the Dangme West District of Ghana. Journal of Ethnopharmacology, 129, 367–376. [DOI] [PubMed] [Google Scholar]
- Ashall, V., Millar, K.M., & Hobson‐West, P. (2018). Informed Consent in Veterinary Medicine: Ethical Implications for the Profession and the Animal ‘Patient’. Food Ethics, 1, 247–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assefa, A., & Bahiru, A. (2018). Ethnoveterinary botanical survey of medicinal plants in Abergelle, Sekota and Lalibela districts of Amhara region, Northern Ethiopia. Journal of Ethnopharmacology, 213, 340–349. [DOI] [PubMed] [Google Scholar]
- Aziz, M.A., Adnan, M., Khan, A.H., Sufyan, M., & Khan, S.N., (2018). Cross‐Cultural Analysis of Medicinal Plants commonly used in Ethnoveterinary Practices at South Waziristan Agency and Bajaur Agency, Federally Administrated Tribal Areas (FATA), Pakistan. Journal of Ethnopharmacology, 210, 443–468. [DOI] [PubMed] [Google Scholar]
- Aziz, M.A., Khan, A.H., & Pieroni, A. (2020). Ethnoveterinary plants of Pakistan: a review. Journal of Ethnobiology and Ethnomedicine, 16, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahmani, M., & Eftekhari, Z. (2013). An ethnoveterinary study of medicinal plants in treatment of diseases and syndromes of herd dog in southern regions of Ilam province, Iran. Comparative clinical pathology, 22, 403–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barboza, R.R.D., de Souto, W.de.M.S., & Mourão, J.da.S. (2007). The use of zootherapeutics in folk veterinary medicine in the district of Cubati, Paraíba State, Brazil. Journal of Ethnobiology and Ethnomedicine, 3(32), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benítez, G., González‐Tejero, M.R., & Molero‐Mesa, J. (2012). Knowledge of ethnoveterinary medicine in the Province of Granada andalusia, Spain. Journal of Ethnopharmacology, 31(139), 429–439. [DOI] [PubMed] [Google Scholar]
- Fortini, P., Di Marzio, P., Guarrera, P., & Iorizzi, M. (2016). Ethnobotanical study on the medicinal plants in the Mainarde Mountains (central‐southern Apennine, Italy). Journal of Ethnopharmacology, 184, 208–218. [DOI] [PubMed] [Google Scholar]
- Friedman, J., Yaniv, Z., Dafni, A., & Palewitch, D. (1986). A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. Journal of Ethnopharmacology, 16, 275–287. [DOI] [PubMed] [Google Scholar]
- Gabalebatse, M., Ngwenya, B.N., Teketay, D., & Kolawole, O.D. (2013). Ethno‐veterinary practices amongst livestock farmers in Ngamiland District, Botswana. African Journal of Traditional, Complementary and Alternative Medicines, 10, 490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew, S., Ibrahim, N., Abebe, B., & Eguale, T. (2012). In vitro evaluation of Anthelmintic activities of crude extracts of selected medicinal plants against Haemonchus contortus in AlemgenaWereda, Ethiopia. Acta Parasitologica Globalis, 3(2), 20–27. [Google Scholar]
- Güzel, Y., Güzelşemme, M., & Miski, M. (2015). Ethnobotany of medicinal plants used in Antakya: a multicultural district in Hatay Province of Turkey. Journal of Ethnopharmacology, 174, 118–152. [DOI] [PubMed] [Google Scholar]
- Hasnain, H., & Usmani, R. (2006). Livestock of Pakistan. Livestock Foundation, Islamabad, Pakistan. [Google Scholar]
- Heinrich, M., Ankli, A., Frei, B., Weimann, C., & Sticher, O. (1998). Medicinal plants in Mexico: healers' consensus and cultural importance. Social Science & Medicine, 47, 1859–1871. [DOI] [PubMed] [Google Scholar]
- Islam, M.K., Saha, S., Mahmud, I., Mohamad, K., Awang, K., Uddin, S.J., Rahman, M.M., & Shilpi, J.A. (2014). An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area, Bangladesh. Journal of Ethnopharmacology, 151, 921–930. [DOI] [PubMed] [Google Scholar]
- Jain, S.C., Sharma, R., Jain, R., & Sharma, R.A. (1996). Antimicrobial activity of Calotropis procera. Fitoterapia, 67(3), 275–277. [Google Scholar]
- Kankara, S.S., Ibrahim, M.H., Mustafa, M., & Go, R. (2015). Ethnobotanical survey of medicinal plants used for traditional maternal healthcare in Katsina state, Nigeria. South African Journal of Botany, 97, 165–175. [Google Scholar]
- Khan, M.A., Khan, M. A., & Hussain, M. (2012). Ethno veterinary medicinal uses of plants of Poonch valley Azad Kashmir. Pakistan Journal of Weed Science Research, 18(4), 495–507. [Google Scholar]
- Khattak, N.S., Nouroz, F., Rahman, I.U., & Noreen, S. (2015). Ethno veterinary uses of medicinal plants of district Karak, Pakistan. Journal of Ethnopharmacology, 171, 273–279. [DOI] [PubMed] [Google Scholar]
- Koc, S., Isgor, B.S., Isgor, Y.G., Shomali Moghaddam, N., & Yildirim, O. (2015). The potential medicinal value of plants from Asteraceae family with antioxidant defense enzymes as biological targets. Pharmaceutical Biology, 53, 746–751. [DOI] [PubMed] [Google Scholar]
- Koudouvo, K., Karou, D., Kokou, K., Essien, K., Aklikokou, K., Glitho, I., Simpore, J., Sanogo, R., De Souza, C., & Gbeassor, M. (2011). An ethnobotanical study of antimalarial plants in Togo Maritime Region. Journal of Ethnopharmacology, 134, 183–190. [DOI] [PubMed] [Google Scholar]
- Kumar, V.L., & Roy, S. (2007). Calotropis procera latex extract affords protection against inflammation and oxidative stress in Freund's complete adjuvant‐induced monoarthritis in rats. Mediators of Inflammation, 47523.1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lans, C., Turner, N., Brauer, G., Lourenco, G., & Georges, K. (2006). Ethnoveterinary medicines used for horses in Trinidad and in British Columbia, Canada. Journal of Ethnobiology and Ethnomedicine, 2, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lans, C., Turner, N., Khan, T., Brauer, G., & Boepple, W. (2007). Ethnoveterinary medicines used for ruminants in British Columbia, Canada. Journal of Ethnobiology and Ethnomedicine, 3, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonti, M., Casu, L., Sanna, F., & Bonsignore, L. (2009). A comparison of medicinal plant use in Sardinia and Sicily—De Materia Medica revisited? Journal of Ethnopharmacology, 121, 255–267. [DOI] [PubMed] [Google Scholar]
- Lev, E. (2003). Traditional healing with animals (zootherapy): medieval to present‐day Levantine practice. Journal of Ethnopharmacology, 85, 107–118. [DOI] [PubMed] [Google Scholar]
- Manganelli, R.U., Camangi, F., & Tomei, P. (2001). Curing animals with plants: traditional usage in Tuscany (Italy). Journal of Ethnopharmacology, 78, 171–191. [DOI] [PubMed] [Google Scholar]
- Martin, G.J. (1995). Ethnobotany, conservation and community development. In Ethnobotany. Springer, Boston, MA, pp. 223–251. [Google Scholar]
- McCorkle, C.M., & Mathias‐Mundy, E. (1992). Ethnoveterinary medicine in Africa. Journal of the International African, 62(1), 59–93. [Google Scholar]
- Muhammad, G., Khan, M.Z., Hussain, M.H., Iqbal, Z., Iqbal, M., & Athar, M. (2005). Ethnoveterinary practices of owners of pneumatic‐cart pulling camels in Faisalabad City (Pakistan). Journal of Ethnopharmacology, 97, 241–246. [DOI] [PubMed] [Google Scholar]
- Mussarat, S., Amber, R., Tariq, A., Adnan, M., AbdElsalam, N.M., Ullah, R., & Bibi, R. (2014). Ethnopharmacological assessment of medicinal plants used against livestock infections by the people living around indus river. BioMed Research International, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasir, E.,& Ali, S.I. “Flora of Pakistan,” National Herbarium, NARC, Islamabad, Department of Botany, University of Karachi, Karachi, (Fascicles), 1972‐1994.
- Nguta, J., Mbaria, J., Gakuya, D., Gathumbi, P., & Kiama, S. (2010). Traditional antimalarial phytotherapy remedies used by the South Coast community, Kenya. Journal of Ethnopharmacology, 131, 256–267. [DOI] [PubMed] [Google Scholar]
- Nwafor, I.C., Shale, K., & Achilonu, M.C. (2017). Chemical Composition and Nutritive Benefits of Chicory (Cichorium intybus) as an Ideal Complementary and/or Alternative Livestock Feed Supplement. The Scientific World Journal, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obakiro, S.B., Kiprop, A., Kigondu, E., K'Owino, I., Odero, M.P., Manyim, S., Omara, T., Namukobe, J., Owor, R.O., & Gavamukulya, Y. (2021). Traditional medicinal Uses, phytoconstituents, bioactivities and toxicities of Erythrina abyssinica Lam. ex DC.(fabaceae): a systematic review. Evidence‐Based Complementary Alternative Medicine, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthiban, R., Vijayakumar, S., Prabhu, S., & Yabesh, J.G.E.M. (2016). Quantitative traditional knowledge of medicinal plants used to treat livestock diseases from Kudavasal taluk of Thiruvarur district, Tamil Nadu, India. Revista Brasileira de Farmacognosia, 26, 109–121. [Google Scholar]
- Phillipson, J.D., & Anderson, L.A. (1989). Ethnopharmacology and western medicine. Journal of Ethnopharmacology, 25, 61–72. [DOI] [PubMed] [Google Scholar]
- Phondani, P.C., Maikhuri, R., & Kala, C. (2010). Ethnoveterinary uses of medicinal plants among traditional herbal healers in Alaknanda catchment of Uttarakhand, India. African Journal of Traditional, Complementary and Alternative Medicines, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan, B.K., & Badola, H.K. (2008). Ethnomedicinal plant use by Lepcha tribe of Dzongu valley, bordering Khangchendzonga biosphere reserve, in north Sikkim, India. Journal of Ethnobiology and Ethnomedicine, 4, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rates, S.M.K. (2001). Plants as source of drugs. Toxicon, 39, 603–613. [DOI] [PubMed] [Google Scholar]
- Raza, M.A., Younas, M., Buerkert, A., & Schlecht, E. (2014). Ethno‐botanical remedies used by pastoralists for the treatment of livestock diseases in Cholistan desert, Pakistan. Journal of Ethnopharmacology, 151, 333–342. [DOI] [PubMed] [Google Scholar]
- Raziq, A., de Verdier, K., & Younas, M. (2010). Ethnoveterinary treatments by dromedary camel herders in the Suleiman Mountainous Region in Pakistan: an observation and questionnaire study. Journal of Ethnobiology and Ethnomedicine, 6, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadat‐Hosseini, M., Farajpour, M., Boroomand, N., & Solaimani‐Sardou, F. (2017). Ethnopharmacological studies of indigenous medicinal plants in the south of Kerman, Iran. Journal of Ethnopharmacology, 199, 194–204. [DOI] [PubMed] [Google Scholar]
- Sharma, R., & Manhas, R. (2015). Ethnoveterinary plants for the treatment of camels in Shiwalik regions of Kathua district of Jammu & Kashmir, India. Journal of Ethnopharmacology, 169, 170–175. [DOI] [PubMed] [Google Scholar]
- Sher, H., Bussmann, R.W., Hart, R., & de Boer, H.J. (2016). Traditional use of medicinal plants among Kalasha, Ismaeli and Sunni groups in Chitral District, Khyber Pakhtunkhwa province, Pakistan. Journal of Ethnopharmacology, 188, 57–69. [DOI] [PubMed] [Google Scholar]
- Singh, A.G., Kumar, A., & Tewari, D.D. (2012). An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. Journal of Ethnobiology and Ethnomedicine, 8, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smylie, J., Olding, M., & Ziegler, C. (2014). Sharing What We Know about Living a Good Life: Indigenous Approaches to Knowledge Translation. Journal of the Canadian Health Libraries Association, 35, 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surendran, S., Prabha, A.C., Ramasubbu, R., & Krishnaraj, M.V. (2021). Humboldtia Vahl (Fabaceae): A Review on Ethnobotany, Phytochemistry and Pharmacology. Phytomedicine Plus, 100080. [Google Scholar]
- Tamboura, H.H., Sawadogo, L., KaborÉ, H., & Yameogo, S.M. (2000). Ethnoveterinary medicine and indigenous pharmacopoeia of Passoré Province in Burkina Faso. Annals of the New York Academy of Sciences, 916, 259–264. [DOI] [PubMed] [Google Scholar]
- Tariq, A., Mussarat, S., Adnan, M., AbdElsalam, N.M., Ullah, R., & Khan, A.L. (2014). Ethnoveterinary study of medicinal plants in a tribal society of Sulaiman range. Scientific World Journal, 2014, 127526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin, M., & Hassan, M. (2014). Determination of informant consensus factor of ethnomedicinal plants used in Kalenga forest, Bangladesh. Bangladesh Journal of Plant Taxonomy, 21, 83–91. [Google Scholar]
- Ul Hassan, H., Murad, W., Tariq, A., & Ahmad, A. (2014). Ethnoveterinary study of medicinal plants in Malakand Valley, District Dir (Lower), Khyber Pakhtunkhwa, Pakistan. Irish Veterinary Journal, 67, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma, R.K. (2014). An ethnobotanical study of plants used for the treatment of livestock diseases in Tikamgarh District of Bundelkhand, Central India. Asian Pacific Journal of Tropical Biomedicine, 4, S460‐S467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitalini, S., Tome, F., & Fico, G. (2009). Traditional uses of medicinal plants in Valvestino (Italy). Journal of Ethnopharmacology, 121, 106–116. [DOI] [PubMed] [Google Scholar]
- Waugh, C.D., Clark, D.A., Harris, S.L., Thom, E.R., Copeman, P.J.A., & Napper, A.R. 1998. Chicory for milk production. In: Proceedings of the Conference‐New Zealand Grassland Association, pp. 33–38.
- Yadav, S.S., Bhukal, R.K., Bhandoria, M.S., Ganie, S.A., Gulia, S.K., & Raghav, T.B.S. (2014). Ethnoveterinary Medicinal plants of Tosham block of district Bhiwani (Haryana) India. Journal of Applied Pharmaceutical Science, 4(6), 040–048. [Google Scholar]
- Yetein, M.H., Houessou, L.G., Lougbégnon, T.O., Teka, O., & Tente, B. (2013). Ethnobotanical study of medicinal plants used for the treatment of malaria in plateau of Allada, Benin (West Africa). Journal of Ethnopharmacology, 146, 154–163. [DOI] [PubMed] [Google Scholar]
- Yineger, H., Kelbessa, E., Bekele, T., & Lulekal, E. (2007). Ethnoveterinary medicinal plants at bale mountains national park, Ethiopia. Journal of Ethnopharmacology, 112, 55–70. [DOI] [PubMed] [Google Scholar]
- Zorloni, A., Penzhorn, B.L., & Eloff, J.N. (2010). Extracts of Calpurnia aurea leaves from southern Ethiopia attract and immobilise or kill ticks. Veterinary Parasitology, 168, 160–164. [DOI] [PubMed] [Google Scholar]


