Abstract
The COVID-19 pandemic has accelerated the transition to virtual healthcare while also prompting an abundance of new literature highlighting telemedicine’s capabilities and limitations for various medical applications, notably musculoskeletal examinations. Telemedicine provides an opportunity to deliver timely patient- and family-centred care while maintaining physical distancing and improving access to remote communities. This review aims to narrate the current state of the literature on telemedicine applied in the context of a musculoskeletal examination for children aged 3 to 18 years. The PubMed and ScienceDirect databases were searched for relevant articles from January 2015 to August 2021 using a combination of keywords and nested searches. The general examination components relevant to the back and lumbosacral spine, hip, knee, ankle/foot, and gait are described. These components include inspection, palpation, range of motion, motor, and sensory examination as well as special testing. There is general feasibility, validity, and substantial reliability in performing most examination components, and primary diagnoses established virtually were found to be either the same or similar in the vast majority of cases. Despite the current literature focusing mainly on adult populations, we describe how each aspect of the exam can be reliably incorporated into a virtual appointment specific to the pediatric population. Currently available smartphone-based applications that measure joint range of motion were generally found to have high reliability and validity. Caregivers are needed for most of the consultation, especially in younger children, but select physical exam maneuvers can be self-performed by older children and adolescents alone. By providing an overview of the available smartphone tools as well as the reliability and validity of remote assessments, this review not only establishes a foundation for a structured pediatric musculoskeletal examination, but also aims to increase providers’ confidence in incorporating telemedicine into their practice.
Keywords: telehealth, telemedicine, eHealth, pediatric, musculoskeletal, evaluation
Introduction
Telemedicine is an evolving platform of healthcare delivery that has gained a lot of momentum during the COVID-19 pandemic. It is broadly defined as the real-time delivery of health services at a distance via means of digital technology.1 The lockdown measures associated with the pandemic have led to a hasty shift away from in-office visits, leading to rapid adoption of telemedicine technologies.2 Face-to-face consultations for pediatric patients are being replaced by videoconference meetings or telephone encounters, carrying their own set of advantages and limitations.3,4 For one, videoconference-based orthopedic consultations have been shown to be cost-effective and do not result in serious adverse events.5,6 Additionally, telemedicine appointments have been shown to provide convenience to the patient and provider, leading to increased satisfaction, as well as increased access to specialized care in rural/remote areas.7,8 Given that musculoskeletal pathologies are a common reason for primary care visits,9 it is important to have a framework and standardized approach to evaluate and diagnose these issues via telemedicine. This will be of importance not only in the current pandemic climate, but as telemedicine continues to evolve even after physical distancing restrictions are lifted.
While many resources exist to guide aspects of a virtual musculoskeletal examination, specific recommendations for the pediatric population are lacking.4 Therefore, the aim of this narrative review was to provide the clinician with a summary of written guidelines to facilitate specific physical examination techniques on children aged 3–18 years, with or without the help of a caregiver. Most of these techniques are based on validated physical exam maneuvers performed during in-person encounters which have been modified to enable the child and caregiver to self-perform the maneuvers. Pictures and detailed descriptions for the patient and caregiver on how to perform these maneuvers are in the Supplemental Materials. In addition, we provide our own recommendations on performing certain examination components. Another neglected area addressed by this review is the feasibility, reliability, and validity of performing remote exams as well as tools clinicians can incorporate in their consultations. Given this, we discuss assessment scores amenable to the virtual platform as well as validated and reliable smartphone applications for measuring joint range of motion (ROM). Additionally, the overall reliability and validity of individual examination components are assessed as well as their impact on diagnosis and subsequent clinical management when performed remotely.
Methods
The PubMed and ScienceDirect databases were searched for available journal articles from January 2015 to August 2021 published in the English language. Our search was limited to this period to include primarily new telemedicine technology. A research question in the population, intervention, comparison, and outcome (PICO) format was generated to guide the literature search and develop a screening process for relevant articles. The question was:
In pediatric patients with musculoskeletal pathology of the back and lower limbs, are consultations delivered via telemedicine feasible and comparable to in-person appointments in terms of clinical outcomes?
The following keywords were used: Telehealth, telemedicine, tele-assessment, teleconsultation, mHealth, eHealth, pediatric, adolescent, child, back, spine, hip, knee, ankle foot, gait, and balance.
Two distinct set of searches were performed. The first search screened for articles with the broader scope of remote physical examination in the pediatric population. The nested search used in PubMed was: (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” OR “mHealth”) AND (“pediatric” OR “adolescent” OR “child*”) AND (“remote exam*” OR “physical exam*” OR “virtual exam*”). A total of 47 citations were found for which titles and abstracts were screened for relevance and consideration for thorough review. We excluded 45 articles due to lack of relevance to our topic. Similarly, ScienceDirect was searched using the terms: (“telemedicine” OR “telehealth”) AND (“pediatric” OR “child” OR “adolescent”) AND “musculoskeletal”. A total of 251 citations were found of which 246 were excluded. Publications on smartphone applications for range of motion measurement were also screened for on PubMed and ScienceDirect using the following nested search: “smartphone” AND “range of motion”. The searches yielded 626 total citations of which 574 were excluded due to irrelevance or not pertaining to the joints covered in our review.
Given that the first search yielded minimal pediatric-specific articles, a second search was performed to identify articles describing the physical examination of the back, spine, hips, knee, ankle, foot, and gait, regardless of the patient population. The intention was to screen for articles that can be applied to the pediatric population. The keywords mentioned previously were combined into nested searches used in PubMed, which are described in Table 1 along with the citations the searches yielded, and the number of citations ultimately included in our review. A similar approach was used for the ScienceDirect database. Duplicates from both searches were removed and reference lists were screened for other relevant articles which escaped our initial search. Finally, some additional references were individually selected during manuscript preparation to provide clarification on certain topics.
Table 1.
Nested Searches Used in Second PubMed Iteration
| Section | Nested Search | Citations Yielded | Citations Included |
|---|---|---|---|
| Back and lumbosacral spine | (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” OR “mHealth”) AND (“back” OR “spine” OR “low* back” OR “lumbar” OR “lumbosacral”) | 456 | 12 |
| Hips | (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” or “mHealth”) AND “hip” | 136 | 5 |
| Knee | (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” or “mHealth”) AND “knee” | 176 | 7 |
| Ankle and foot | (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” or “mHealth”) AND (“ankle” OR “foot”) | 138 | 4 |
| Gait, balance, movement assessment | (“telemedicine”[MeSH] OR “telehealth” OR “tele-assessment” OR “teleconsultation” OR “eHealth” or “mHealth”) AND “gait” | 124 | 5 |
Patient/Caregiver Preparation for Virtual Visit
In order to achieve an efficient, productive, and child-centred virtual visit, there are a few considerations for the patient and caregiver. Given that the vast majority of pediatric telemedicine encounters will be performed in the patient’s home, caregivers should consider the environment of the virtual exam room, items that may be required during the visit, the readiness of the child for the exam, as well as proper functioning of technical equipment.4,10 These are summarized below. Lastly, clinicians should be mindful of the legal implications of parental presence during a virtual visit.
Preparing the Virtual Exam Room
The environment of the virtual exam room can be optimized by allowing for adequate floor space for the child to demonstrate different aspects of the motor examination such as walking, running, jumping, and crawling, among others. It is also helpful to have a flat surface on which the child can lie for evaluation of ROM, strength, and for certain special tests. Caregivers should minimize background noise and other possible distractions during the visit, which may include ensuring that other young children in the home are occupied. The caregiver will be responsible for assisting with portions of the physical examination as well as proper camera placement. A second caregiver, if present, may also assist with either one of the previous tasks.
Items Which May Be Required
Caregivers should prepare items that the child can use to demonstrate some gross and fine motor skills. This can include favourite toys which can be physically manipulated by the child, books for turning pages or paper and crayons for writing. For older children and adolescents for which certain activities are a challenge, such as combing their hair, having a hairbrush available to demonstrate these challenges can be helpful.
Preparing the Child
To promote a quick transition to the physical examination portion of the visit, dressing toddlers in easily removable clothing and older children in shorts, T-shirt, tank top, or sports bra prior to the visit are recommended. We suggest that young children be rested, fed, and freshly diapered prior to the visit. Children can also be encouraged to bring a favourite toy and present it to the provider as a “show and tell” which may help build the child’s excitement and willingness to demonstrate what they can do during the visit. Lastly, children should be briefed on what to expect during their visit.
Parental/Legal Representative Presence
As denoted in the American Telemedicine Association’s Operating Procedures for Pediatric Telehealth, providers must have a mechanism in place to communicate with the parent or legal representative of a minor patient before a telehealth encounter, except when telehealth is provided as a means of managing certain limited pediatric emergencies.10 In addition, a parent or legal representative may participate in the virtual encounter unless the patient is legally authorized to consent to their own care. Lastly, if the parent or legal representative is present during the visit, providers must have provisions in place (eg, breakout rooms on Zoom), to confirm that the parents can leave the room during confidential parts of the history and physical exam. We also remind providers that all existing laws and regulations regarding patient privacy and confidentiality, including laws pertaining to the protection of privacy when minors consent to their own care, apply to telehealth encounters just as they do for face-to-face encounters.
Back and Lumbosacral Spine
In preparation for their appointment, patients should be dressed in shorts and a loose-fitting shirt while younger children can be dressed in their undergarments. We also stress that a hip examination is an integral part of the lower back exam and should not be excluded. Similarly, gait inspection and dynamic functional testing should be included in the examination of the spine, hips, and lower limbs.11
Inspection and Palpation
Inspection of the spine is particularly important in a growing child. Clinicians can begin with examination of the overlying dorsal skin, noting any tufts of hair, birthmarks, or lipomas on the lower back. The patient’s posture should be assessed in the coronal and sagittal planes, noting any asymmetry of the torso, pelvis and shoulders, lack of or increase in normal lordosis or kyphosis as well as signs of scoliosis.4 Patients with adolescent scoliosis require additional exam components including evaluation of cranial nerves, facial asymmetry, neurologic abnormalities of the feet, leg-length discrepancy and presence of a rib hump.12 If the patient has focal pain, the provider can ask them to point to its location. For instance, if sacroiliac joint (SIJ) dysfunction is suspected, a Fortin’s finger test can be performed by asking the patient to point to the painful area on two separate occasions.12 If the pain is localized within 1 cm inferomedial to the posterior superior iliac spine (PSIS) both times, the test is positive.
Clinicians can guide the patient or caregiver to palpate the PSIS, ischial tuberosities, greater trochanter, paraspinal musculature and spinal processes for any tenderness. The child can also lay in the prone position and a caregiver can palpate for SIJ tenderness.13 Given that proper palpation requires sufficient anatomical knowledge and graded pressure, untrained assistants may produce false positive findings or render palpation potentially unsafe if they palpate too vigorously. Therefore, we recommend that guided palpation be used at the provider’s discretion.
ROM Assessment
Active lumbar ROM can be assessed by having the patient stand and reproduce movements that either precipitate or alleviate pain. An Adams test can be performed in which the child is asked to face away from the camera, bend forward and touch their toes with the knees locked to assess for forward flexion as well as presence of scoliosis.13 Similarly, extension, lateral bending and rotation can be examined, with an assistant holding the patient’s hips from behind to prevent hip compensation when the patient attempts trunk rotation.
Inclinometer-based applications can be downloaded and used with the help of a caregiver to acquire ROM measurements under the guidance of a clinician. Quantification of lumbar spine flexion and extension has been studied in adults using two inclinometer-based applications: “iHandy Level” (iHandy Ltd; AppStore, Google Play) and “TiltMeter” (Carlos Hernandez; AppStore). A summary of currently available applications and the different joint ROM they measure can be found in Table 2. Both iHandy and TiltMeter are simple to use, requiring an assistant to position the smartphone on the T12-L1 spinal level followed by flexion and extension. This is repeated at the S1-S2 spinal level, and the total lumbar spine flexion and extension ROM is calculated by subtracting the T12-L1 value from the S1-S2 value for iHandy and vice versa for the TiltMeter. Despite its reliability and validity in measuring ankle ROM,14 the iHandy app has inconsistent intra- and inter-rater reliability in measuring lumbar ROM. Additionally, it has not been shown to have sufficient concurrent validity in measuring active lumbar flexion when compared to a gravity-based inclinometer, but may be moderately valid in measuring extension.15 In a similar comparison, the TiltMeter app has been shown to possess good-to-excellent intra- and inter-rater reliability and concurrent validity in lumbar flexion and extension.16 While clinicians may be more inclined to use the TiltMeter app due to its superior reliability and validity, they must remain cautious when using these tools as they have not been validated in pediatric populations.
Table 2.
Available Smartphone Apps and Their Studied Reliability and Validity in Measuring Various Joint ROMa
| Application | Technology | Platform | Demonstrated Validity and Reliability in Joint ROM |
|---|---|---|---|
| TiltMeter (Carlos Hernandez) | Inclinometer | AppStore | Lumbar spine flexion/extension16 Ankle dorsiflexion34 |
| Compass (Apple) | Compass | AppStore | Hip internal rotation35 |
| Accurate Compass (Ngo Na; PVDApps) | Compass | AppStore Google Play |
Hip internal/external rotation36 |
| Clinometer + Bubble Level (Peter Breitling; Plaincode) | Inclinometer | AppStore Google Play |
Hip flexion/extension, internal/external rotation36,37,39,40,42 Ankle dorsiflexion/plantar flexion69 |
| Measure (Apple) | Inclinometer | AppStore | Hip flexion/extension, internal/external rotation37 |
| PT Goniometer (Mark Busman) | Inclinometer | AppStore | Hip flexion, internal/external rotation, abduction38 |
| Angle Meter 360 (Aleksey Kozlov) | Photo-capture | AppStore Google Play |
Knee flexion/extension26 |
| Dr. Goniometer (CDM S.r.L) | Photo-capture | AppStore | Knee flexion/extension34,55 Ankle dorsiflexion/plantar flexion69 |
| Goniometer Pro (5fuf5) | Inclinometer | AppStore | Knee flexion/extension34 Ankle dorsiflexion/plantar flexion69 |
| iHandy Level (iHandy Ltd.) | Inclinometer | AppStore Google Play |
Ankle dorsiflexion14 |
Note:aAvailable as of July 2021.
Abbreviation: ROM, range of motion.
Sensory Examination
Patients can be prompted to localize areas of paresthesia, numbness or where they feel “funny”. A caregiver or the patients themselves can screen for light touch sensation of the L1-S2 dermatomes with a paper tissue or cotton ball.11 If a caregiver is assisting, the clinician may ask the patient to keep their eyes closed to better concentrate on subtle sensory differences. If a more subtle sensory loss is suspected or if the patient’s description is unclear, the clinician can direct the patient or assistant to assess pinprick sensation with a paperclip, pin, toothpick, pencil tip, or hairbrush.17 Temperature sensation can also be assessed with assistance from the caregiver, using an icepack.11
Motor Examination
Lower extremity motor strength can be assessed either by manual muscle testing (eg, knee extension) or by functional testing, as described in Table 3. It is worth noting that the inability of the clinician to provide resistance with manual testing makes it difficult to detail anything beyond 3/5 strength (against gravity) and therefore functional testing may be more useful in the telemedicine setting.12 Also of note is that no reliable method of eliciting reflexes over telemedicine has been identified, with the exception of clonus at the ankles and the Babinski reflex,4,11,18 although the latter has questionable applicability.17,19 Despite this, it has been suggested that a caregiver can attempt the patellar knee reflex and Achilles tendon reflex with a spatula, edge of a smartphone or their knuckles in the case of a younger child, but we urge caution when interpreting findings.4,11
Table 3.
Examining Strength of the Lower Limbs in a Virtual Spine Assessment
| Component Examined | How to Examine via Telemedicine |
|---|---|
| Hip flexor/iliopsoas (L1-L2) | Patient is seated or standing and is asked to flex their hip and maintain this position. Holding with no perceived difficulty can suggest 5/5 strength while lifting without being able to hold denotes 3/5 strength.17,18,21 |
| Quadriceps (L3-4) | Patient is asked to perform single sit-to-stand from chair. No difficulty suggests 5/5 strength while only being able to fully extend the knee while sitting denotes 3/5 strength.17,18 Patient is asked to perform a timed five repetition sit-to-stand (5R-STS) test,2 shown to be highly reliable when performed at home without supervision.86 Child is asked to squat and “frog jump”.11 Child is asked to sit cross-legged and stand up (pay attention for Gower sign).13 |
| Hip abductors (L5) | Patient is asked to perform a standing Trendelenburg test12,20,21 and lateral leg raise. |
| Ankle dorsiflexion/tibialis anterior (L4-5) | Patient is asked to perform heel-walking or standing metatarsal raises. The ability to walk on the heels for 10 paces while clearing the metatarsal heads suggests 5/5 strength.17,18 |
| Ankle plantarflexion/gastrocnemius-soleus (S1) | Patient can perform unipodal heel raises where the ability to perform 10 repetitions indicates 5/5 strength.17,18 Patient can also be asked to perform toe-walking and the ability to do so indicates at least 4/5 strength.67,68 |
| Ankle inversion (L5-S1) | Patient is asked to perform a lateral foot walk. |
| Ankle eversion (L4-S1) | Patient is asked to perform a medial foot walk. |
Special Testing
If there is suspicion of juvenile ankylosing spondylitis, a modified Schober test can be performed remotely.11 The straight leg raise (SLR) can be performed in patients with suspected disc herniation affecting the L4-S1 nerve roots where the reproduction of sciatic pain is a positive test.4,11,17,18,20–22 A caregiver should be assigned to passively raise the patient’s leg, ensuring that it is kept straight (Figure S1). Initially, a seated SLR may be done and if it is negative, a standard supine SLR is suggested.11 Similarly, a contralateral SLR and reverse SLR can be performed remotely to evaluate for the possibility of central disc herniation or L2-L4 radiculopathy, respectively.11 Another useful test for lumbar radiculopathy that can be performed remotely without an assistant is the slump test (Figures 1A and S2).11,21 In younger athletic patients in which spondylolysis is suspected, the stork/Gillet test for facet joint and posterior element pain can be performed without the need of a caregiver (Figure S3).11 For lumbar segmental instability, the cluster of Rehorst can be performed with the help of a caregiver (Figure S4). It consists of a lumbar thrust, prone instability test, Beighton score as well as an assessment of pain and other abnormal signs on active trunk flexion/extension. The Beighton score can be used to remotely assess joint hypermobility of the trunk, knee, elbow, thumb, and small finger, and has been validated in children ages 6 to 12.23 The prone instability test may be more difficult to perform but can be accomplished with the help of a reliable caregiver. Although patients are unable to perform a lumbar thrust independently, an untrained assisstant may attempt it with graded pressure, making sure not to elicit excess pain.
Figure 1.
Special testing with caregiver assistance. (A) Slump test: Caregiver may assist by supporting neck flexion and adding passive ankle dorsiflexion. (B) Gaenslen’s test: Caregiver can apply pressure on the lowered leg and opposite leg at the knee. (C) FADER + isometric IR: Caregiver performs movements passively then provides resistance against IR. (D) Lever sign/Lelli’s test: with patient lying supine, caregiver positions their fist beneath one calf and then applies downward force on the distal femur.
Several special tests for SIJ dysfunction have been deemed suitable to perform over telemedicine. These include the flexion, abduction and external rotation (FABER) test,4,11,12,20,21 Gaenslen’s test11 as well as the lateral iliac crest compression test,11 for which only the latter requires an assistant. During a remote FABER test, the patient or caregiver can stabilize the opposite pelvis with one hand while applying downward pressure on the contralateral medial knee (Figure S8). Performing a virtual Gaenslen's test involves having the patient lie on a bed and lower one leg off the side. They are then instructed to attempt pulling the opposite knee to the chest, increasing shearing at the SIJ If present, an assistant can apply pressure on the lowered leg and the opposite leg at the knee (Figures 1B and S6). Providers should be aware that patients being close to the edge of the bed when performing this test may introduce the risk of falls. Given that the Gaenslen’s test has little diagnostic value on its own,24 we recommend using a cluster of tests with the help of a caregiver such as the Laslett SIJ cluster (distraction, compression, thigh thrust, sacral thrust; Figure S5) or Van der Wurff SIJ cluster (distraction, compression, thigh thrust, Gaenslen’s and FABER).
While we do not believe that patients can perform a sacral thrust independently, they can attempt performing a thigh thrust on their own by bringing their knees up towards their chest and pulling down, assessing for pain reproduction. SIJ compression can also be attempted independently by asking the patient to place their palms on their waist and squeeze their hands together. We do not recommend patients attempting the distraction test as it will be too difficult for them to generate the force required for proper interpretation of the test. Limitations of these self-applied SIJ provocation maneuvers include unwanted muscle activation, which may falsify results, as well as the inability to generate the necessary force to properly stress the SIJ and reproduce pain. We recommend that a caregiver assists in performing all the aforementioned tests with the patient relaxed, advising them to begin with light pressure followed by graded pressure.
Reliability and Validity
A systematic review assessed the reliability of the virtual spine examination in adults when compared to an in-person exam.25 While all studies used different reliability measures, the concensus was that some portions of the lower back exam had acceptable reliability with poor reliability and disagreement in others. Lumbar flexion, extension and finger-floor distance were found to have relatively high reliability in comparison to lateral flexion. While the SLR was found to have good inter-rater reliability in one study, another found it to have significant disagreement in regards to the ROM achieved as well as presence of pain when compared to an in-person assessment. Judgement of centralization/peripheralization was also shown to have significant disagreement. Clinicians should take this information with some scrutiny as these studies only included small portions of the lumbar spine examination, which primarily pertained to the physical therapy literature. A recent study examined the intra-rater reliability of the virtual spine exam compared to videoconference-based appointments and concluded that there was good to very good agreement in pain location, dorsal and lateral spine inspection, sensory deficits and active ROM of the hip, knee and foot.26 Only moderate intra-rater reliability was found for the Adam’s test, SLR and reverse SLR, consistent with the mixed results from the aforementioned studies.
A global survey of spine surgeons was recently performed to elucidate the overall provider confidence in the telemdicine evaluation of the spine. Providers felt that physical exam-based tasks (eg provocative testing, assessing neurologic deficits and myelopathy) were inferior to in-person exams while communication-based components (eg history taking, imaging review) were equivalent.27 Another study using an adult population examined the agreement between telehealth and in-person assessment of chronic lumbar spine conditions in terms of clinical management decisions.28 After performing a virtual musculoskeletal exam, there was an 85.7% agreement in the selected management pathway, 76–93% agreement in referral to specific allied health professionals and 93% agreement that the clinical diagnosis was either the same or similar. There was also 100% agreement on request for further pathology and 64.3% agreement on request for further radiological investigations. A final study added that 94% of surgical plans established in virtual visits did not change after in-person evaluation of adults with spinal pathology.29
Although the preceding literature is not specific to the pediatric population, it highlights two important conclusions about the virtual lumbar spine exam. First, some components of the physical exam may be reliably conducted over telemedicine despite physicians’ overall sentiment that it is inferior to the in-person exam.25,27 Second, the clinical management decisions made by physicians, including surgical plans, strongly agree with decisions made based on in-person encounters.28,29
Hips
Prior to the encounter, there should be enough room to permit a full-body view of the patient walking towards and away from the camera as well as a flat surface where a small child can lie on.11,21 A thorough spine exam and gait assessment may be needed to evaluate concomitant or primary lumbar spine pathology.
Inspection and Palpation
The exam begins with inspection of the frontal, sagittal and posterior views of the patient to assess for asymmetry of the iliac crests, pelvic tilt and PSIS imbalance, respectively.11,30 The examiner can instruct the patient to perform a double leg squat and if possible, single leg squat to assess for dynamic medial knee valgus or medial movement of the knee during the squat. In addition, climbing up and down stairs, running, jumping, hopping on one-foot, single leg stance and rising from sitting on the floor can be assessed in younger children. In very young children, the examiner can observe for asymmetry of skin folds at the gluteal region, thighs and knees.11 To assess for leg length discrepancy, providers can use a virtual ruler to measure the distance from the ASIS to the floor.31
Providers can guide the patient or caregiver through palpation of the anterior groin, greater trochanter, iliac crest, ASIS and ischial tuberosity, asking them to note any points of tenderness.32 Trochanteric palpation can be performed with the patient standing21 or in the lateral decubitus position with the symptomatic leg facing upwards.11 Patients can be asked to localize their pain which may produce a C-sign around the hip, raising suspicion for intra-articular pathology.30–32
ROM Assessment
Hip ROM can be examined with the patient in the supine, seated and prone positions. The supine patient should perform active internal and external rotation with the hips flexed at 90°, noting the furthest position which does not cause any discomfort.4,11,30,31 If a caregiver is present, they can perform the same maneuvers passively as well as a leg roll to assess for internal and external rotation.13 In a seated position, the provider can assess for the same motions using a seated FABER test21 or with a towel wrapped around the patient’s ankle to assist in pulling the lower leg inwards or outwards.11 The prone examination involves the child lying with the knees flexed to 90° and having the caregiver place the patient’s legs in a “W” to assess external rotation and an “X” position to assess internal rotation.13 Active and passive hip extension can also be assessed in the prone position as well as the thigh-foot angle if there is suspicion of tibial torsion.11
If quantification of hip ROM is desired, clinicians can use digital photography or inclinometer-based smartphone applications. Digital photography followed by joint angle quantification through an image manipulation software has been shown to have equivalent accuracy and near-equivalent precision compared to visual estimation and goniometry of hip ROM.33
Several smartphone applications display good-to-excellent inter- and intra-rater reliability in the majority of hip movements as well as good-to-excellent validity when compared to a universal goniometer, digital inclinometer, and motion tracking system.34–42 Among the apps currently available for download are “Clinometer + Bubble Level” (Peter Breitling, Plaincode; AppStore, Google Play), “Accurate Compass” (Ngo Na, PVD Apps; AppStore, Google Play), “PT Goniometer” (Mark Busman; AppStore) as well as “Compass” (Apple; AppStore) and “Measure” (Apple; AppStore). For each app, the smartphone is relatively simple to place, being either in the patient’s pocket or held up against different parts of the leg by an assistant or via a strap, with the most studied application being “Clinometer + Bubble Level”.
Special Testing
Special testing of the hip is summarized in Table 4 and in Figures S7–S16. In addition to performing resisted hip adduction for athletic pubalgia (Figure S16), we suggest that clinicians guide patients to perform a cluster. This includes an external rotation Stinchfield test as well as resisted cross-body sit-up and single-leg sit-up tests, all of which, except the latter, require caregiver assistance.
Table 4.
Special Testing for the Hip via Telemedicine
| Test (Clinical Correlate) | Assistance Required? | How to Examine via Telemedicine |
|---|---|---|
| FADIR (intra-articular impingement) | No* | Patient is asked to perform flexion, adduction and internal rotation of the hip while seated or supine.4,11,21,32 Caregivers may assist by performing these movements passively. Can also be accomplished with the patient’s foot on a chair with the knee and hip flexed while the contralateral hand draws the knee across the midline, resulting in a relative adduction and internal rotation of the hip21,87 (87% sensitivity, 79% specificity).55 |
| FABER (intra-articular hip pathology) | No* | Patient is asked to perform flexion, abduction and external rotation of the hip while seated or supine.4,11,20,21,30–32 Patient or caregiver can stabilize the opposite pelvis with one hand while applying downward pressure on the contralateral medial knee. |
| FADER + isometric IR (greater trochanteric pain syndrome) | Yes | Patient lies supine and caregiver passively flexes the hip to 90º, followed by adduction and ER. In this position, patient is asked to perform isometric IR against caregiver’s resistance. Reproduction of lateral hip pain is a positive test. |
| Stinchfield test (intra-articular hip pathology) | Yes | Patient lies supine and undergoes resisted hip flexion with the knee extended.4,11,20 Pain in the anterior groin is a positive test. |
| Trendelenburg (hip abductor strength) | No | Patient is asked to stand on each leg. Contralateral dipping of the hemipelvis should be noted. |
| Long Stride Walk (ischiofemoral impingement) | No | Patient is asked to take long strides towards or away from the camera. Deep posterior hip pain on terminal extension indicates a positive test.30 |
| Anterior Labral Tear test (anterior labral tear, anterior-superior impingement syndrome, iliopsoas tendonitis) | Yes | Patient lies supine and caregiver brings hip into flexion, ER and abduction. Then, hip is slowly moved into IR, adduction, and extension. Reproduction of patient’s symptoms with or without a click is a positive test. |
| Posterior Labral Tear test (posterior labral tear, posterior-inferior impingement syndrome, anterior hip instability) | Yes | Patient is supine and caregiver brings hip into flexion, IR, and adduction. Then, hip is slowly moved into ER, abduction, and extension. Reproduction of patient’s symptoms with or without a click is a positive test. |
| Modified Thomas test (iliopsoas, ITB and rectus femoris tightness) | No | Patient is supine and is asked to pull the opposite leg into full hip flexion while the observer notes whether the contralateral hip lifts off the surface, which would be indicative of a positive test.11,20 |
| Ely test (rectus femoris tightness) | Yes | While patient lies prone, the caregiver flexes the knee to bring heel to buttock. Examiner assesses heel-to-buttock distance to test flexibility of rectus femoris. Test is positive if patient’s hip spontaneously flexes with knee flexion on that side. |
| Modified Ober test (ITB tightness) | Yes | Patient lies in lateral decubitus position with the affected side up. The bottom knee and hip should be flexed. Examiner grasps the upper leg, extends the hip then lets the leg fall. This leg remaining in an abducted position accompanied with lateral knee pain indicates a positive test.4,11,20,30 |
| Galeazzi test (developmental dysplasia of the hip) | No | Patient lies supine with their feet flat on the ground, close to the buttocks. Examiner observes relative knee height to assess for leg-length discrepancy.4,11 |
| Drehmann sign (SCFE, FAIS, OA) | Yes | Positive if unavoidable external rotation of the hip occurs when performing passive hip flexion. Additionally, internal rotation is either not possible or associated with pain when forcefully induced. |
| Single hip adduction (athletic pubalgia) | No | Patient is asked to palpate their pubic region for tenderness followed by performing hip adduction in the supine position with a rolled-up towel between the legs and knees bent at 90°.30 |
Note: *Test can be facilitated by a caregiver.
Abbreviations: FADIR, flexion adduction internal rotation; FABER, flexion abductions external rotation; FADER, flexion adduction external rotation; IR, internal rotation; ER, external rotation; ITB, iliotibial band; SCFE, slipped capital femoral epiphysis; FAIS, femoroacetabular impingement syndrome; OA, osteoarthritis.
Assessment Measures
The following assessment measures were used as outcomes in a study evaluating the effectiveness of technology-assisted rehabilitation following total hip or knee arthroplasty.43 We suggest their possible incorporation by clinicians into a telemedicine appointment.
Western Ontario and McMaster Universities Arthritis Index (WOMAC) score. Providers can use the WOMAC score to objectively assess for pain, stiffness, and physical function at the start of the appointment. Nonetheless, it is important to note that pediatric OA is uncommon and thus efforts have only been rarely undertaken to validate adult WOMAC scores in children and adolescents.44
Timed up-and go (TUG) test. Modified protocols of the TUG have been made for the pediatric population (ages 3–18 years); however, the choice of protocol and the use of a motivational aspect all affect the test times and the consistency between sessions.45 When compared to in-person assessments, virtual administration of the TUG test in adults post-total knee arthroplasty was found to have near perfect inter-rater reliability.46
6-minute walk test (6MWT). A systematic review on reference values for the 6MWT in children and adolescents has revealed that values varied substantially between studies in different countries and depended on variables such as exercise performance, height, heart rate, age and weight.47 There is ongoing research evaluating the best way to incorporate the 6MWT into the physical examination of children with rheumatic conditions.48
The WOMAC can either be completed at home prior to the consultation or by clinicians during the telemedicine appointment. While both the TUG and 6MWT can be performed at home without clinician supervision, the latter may be less convenient as it requires more equipment and setup time.
Reliability and Validity
The feasibility of a clinical examination of the hip joint and pelvis via telemedicine has been previously examined. In one study, virtual inspection and strength testing showed substantial agreement when compared to an in-office assessment. In contrast, palpation, ROM, and special testing (including Apley, Drehmann, Trendelenburg, FADIR and Thomas tests) only showed slight agreement.49 Despite not being statistically significant, the validity and execution of the examination were inferior in patients who were elderly, obese or had multiple comorbidities. This suggests a possible need for targeted patient selection prior to the appointment. Another study sought to compare a physician-guided self-administered examination to one directly performed by a physician in the diagnosis of femoroacetabular impingement syndrome.50 It revealed that the self-performed examination had a slightly higher mean diagnostic accuracy, although the difference may not be clinically relevant. While this study was not conducted in a virtual setting, its findings imply that both methods are comparable and offer support for self-administered exams over videoconference. Although both these studies used adult populations, they shed light on the limitations of the remote hip exam, particularly in palpation, ROM, and special testing.
Knee
For the virtual examination of the knee, patients should be dressed in shorts and remove their shoes and socks. Given that knee pain may be indicative of hip pathology, providers may want to examine the hip as well.11 If the provider is performing a follow-up assessment in a post-operative patient, they can use a condensed version of the knee exam with emphasis on wound healing, surrounding erythema, ecchymosis, rashes and ROM.51 In a patient reporting recent trauma, the Ottawa Knee Rule can be used to determine whether imaging is necessary to evaluate for a possible fracture.32
Inspection and Palpation
The exam begins with observation of gait.31,32 Next, the child’s knee is inspected in the frontal, sagittal and posterior planes. Presence of genu valgus/varus and patella alta/baja can be appreciated in the frontal plane while genu recurvatum can be assessed in the sagittal plane.4,11 The posterior plane can help visualize popliteal or calf swelling. Erythema, bruising, scarring, warmth, and muscle atrophy should also be assessed and compared with the contralateral knee.13,21,31,32,51 Patients can be asked to point to the area of maximal tenderness. Clinicians can then guide patients or a caregiver to palpate the following areas: quadriceps and patellar tendons, hamstring tendons, patella, iliotibial band insertion, tibial tubercle, pes anserinus and joint lines.11,21,32 Lastly, the patellofemoral joint can be assessed with the patient lying supine with the knee extended and quadriceps relaxed. The patient is then asked to gently push their kneecaps medially and laterally, assessing for femoral condyle or patellar facet tenderness.11
ROM Assessment
Providers can assess knee ROM by visual estimation with the patient standing, supine or seated. Throughout flexion and extension, patients can be asked to put their hand over the ipsilateral patella and feel for crepitus with movement.51 With the patient standing, the provider can ask them to pull their foot up to the ipsilateral buttock to assess for knee flexion. Hyperextension of the knee can also be assessed with the patient standing on the affected leg while pushing the knee posteriorly.31,32 Flexibility of the gastrocnemius muscle can be assessed by a knee-to-wall test. In the supine position, patients’ ability to fully extend and flex the knee can be evaluated as well as the presence of any extension or flexion lag,52 which may be associated with swelling or meniscal involvement.11 Seated ROM can be assessed by the patient’s ability to fully extend and fully flex the knee towards the chest.21,32
Knee ROM can be quantified with the use of simple web-based goniometers, digital photography, or inclinometer-based smartphone applications. Some web-based goniometers are available as browser extensions compatible with telemedicine applications such as InTouch Health, Doxy.me and Zoom.31 Digital photography for knee flexion/extension with subsequent image analysis has been shown to have equivalent accuracy and near-equivalent precision when compared to universal goniometry and visual estimation.33 Additionally, several studies have demonstrated that smartphone applications, when compared with a universal goniometer, demonstrate good-to-excellent inter- and intra-rater reliability as well as excellent concurrent validity in knee flexion and extension.26,34,53–55 Of these, three apps are currently available for download: “Dr. Goniometer” (CDM S.r.L.; AppStore), “Goniometer Pro” (5fuf5; AppStore) and “Angle Meter 360” (Aleksey Kozlov; AppStore, Google Play). Dr. Goniometer and Angle Meter 360 are photo-capture based applications, allowing parents to take a picture in the sagittal plane with the leg, foot, and ankle in the frame, and then position moveable markers to calculate the knee angle.26,55 Goniometer Pro is an accelerometer-based application which requires a smartphone to be placed on the anterior surface of the thigh and then on the anterior surface of the distal tibia. The knee flexion angle is subsequently calculated based on these two measurements.34 Despite their high reliability and validity, none of these applications were studied in the pediatric population. Providers should thus remain critical of the applicability of these smartphone tools, especially in younger children. If they deem their use appropriate, they should familiarize themselves with how to properly position the smartphone by referring to the original studies and complement their use with virtual estimation for additional reliability.56,57
Motor Examination
Strength can be assessed by asking the patient to perform a single sit-to-stand. No difficulty suggests 5/5 quadriceps strength, and only being able to extend the knee while seated suggests 3/5 strength.17,18 Additionally, single-leg stance and single-leg squat assessed from the frontal view can serve as a measure of overall quadriceps, hip, and core function.21,31,51 Lastly, given that the gastrocnemius crosses the knee joint, manual muscle testing of ankle plantar flexion strength via unipodal heel raises should not be omitted as part of the knee exam.
Special Testing
Special testing of the knee with modifications for the telemedicine platform is detailed in Table 5 and in Figures S17–S25.
Table 5.
Special Testing for the Knee via Telemedicine
| Test (Clinical Correlate) | Assistance Required? | How to Examine via Telemedicine |
|---|---|---|
| Thessaly test (meniscal pathology) | No | Patient is asked to stand on one leg with that knee slightly bent at 5º, using support as needed. Patient then internally and externally rotates the knee while pain along the joint line in either direction is assessed. The test is repeated at 20º of knee flexion.11,20,21,31,32,51,70 |
| Apley grind test (meniscal pathology) | Yes | Patient lies prone with involved knee flexed at 90º. Assistant rotates the tibia medially and laterally while applying an axial/downwards force. Repeat using a distraction/upwards force. Pain, clicking and/or restriction indicates a positive test with compression while an increase and/or change in location of pain is a positive test with distraction. |
| Posterior sag sign + quadriceps active test (PCL injury) | No* | Patient lies supine with affected knee flexed to 90º and feet flat on surface. Clinician observes for tibia to “sag” compared to the position of the femur. The patient is then asked to actively contract their quadriceps muscle by sliding their foot forward, against caregiver’s resistance if present. Forward translation of the tibia indicates a positive test.4,11,51 |
| Posterior drawer test (PCL injury) | Yes | Patient lies supine with the symptomatic knee in 90º of flexion and feet flat on surface. Caregiver pushes lower leg posteriorly, just below knee joint. The tibia translating posteriorly more than normal is a positive test. |
| Anterior drawer test (ACL injury) | Yes | Patient lies supine with the symptomatic knee in 90º of flexion and feet flat on surface. Caregiver pulls lower leg anteriorly, just below knee joint. The tibia translating anteriorly more than normal is a positive test. |
| Lever sign/Lelli’s test (ACL injury) | Yes | Patient lies supine with both knees extended while assistant positions their fist beneath one calf and then applies downward force on the distal femur. A positive test is noted when the patient’s heel does not rise off the table.51 |
| MCL/LCL stress test (collateral ligament injury) | No* | Patient is seated with affected knee in 30º of flexion. Instruct them to apply a varus (LCL) or valgus (MCL) stress at the knee with their hands, assessing for pain and joint opening.11,21 If present, a caregiver can assist with the patient supine. |
| Fairbanks patellar apprehension test (patellar subluxation) | No* | Patient is seated with the knee slightly flexed at 30º and asked to put laterally directed stress on the patella with the thumbs of both hands, while clinician notes any apprehension or pain.21,51 If present, caregiver can apply pressure. |
| J-sign (patellar maltracking) | No | Patient is in seated position and is asked to flex and extend the knee. Clinician observes for patella subluxing laterally at terminal knee extension.4,31,32,51 |
| Patellar grind test (patellofemoral pain syndrome) | Yes | Patient lies supine with both knees extended while assistant grasps the patella with thumb and index finger. Patient is instructed to flex their quadriceps (as in knee extension) while assistant applies downward pressure on patella.20,70 Pain on contraction is a positive finding. |
Note: *Test can be facilitated by a caregiver.
Abbreviations: PCL, posterior cruciate ligament; ACL, anterior cruciate ligament; MCL, medial collateral ligament; LCL, lateral collateral ligament.
Assessment Measures
We identified three modified and validated patient-reported outcome measures for the knee in children: Knee Injury and Osteoarthritis Outcome Score for Children (KOOS-Child), International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form in Children, as well as the Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS).58
KOOS-Child. The KOOS-child is a patient-reported outcome measure employing a 5-item Likert scale covering pain, symptoms, difficulty during daily activities, function in sport and play as well as knee-related quality of life. Overall, it shows excellent psychometric properties as well as good validity and reliability in children aged 7–16 years with various knee disorders.59,60
IKDC Subjective Knee Evaluation Form in Children. The IKDC is an adult knee-specific measure that was found to be difficult to interpret and answer for children, specifically in the domains of current and prior knee function assessment. Iversen et al presented modifications to directions, item formatting and definitions in order to ensure comprehensibility and validity in children and adolescents.61 This version measures pain, symptoms and physical functioning during daily sport activities in children and adolescents with knee-related problems. It has been shown to be a valid, reliable, and responsive questionnaire in children aged 9–18 years with a broad range of knee disorders.62,63
HSS Pedi-FABS. Designed for athletically active children aged 10–18 years, it consists of an 8-item scale to assess activity in the fields of sports medicine, rehabilitation and orthopedic surgery.58 Although the scale is not sport or joint-specific, it has been shown to be a reliable and valid metric to assess activity in children and adolescents within that age group.64
Reliability and Validity
The studied reliability and validity of performing a virtual knee exam can increase providers’ confidence in integrating telemedicine into their practice. First, visual estimation of knee ROM performed over videoconference has been shown to have high inter- and intra-rater reliability as well as high validity when compared to in-office visual estimation and manual goniometry.56,57 Similarly, the use of a virtual goniometer has also been shown to have high inter-rater reliability when compared to universal in-office goniometry.46 While the latter studies all included adult populations, only one also examined the reliability of remote, visual estimation of knee flexion and extension in adolescent patients.65 As in adults, there were no clinically significant differences when compared to in-person estimations.
Remote evaluation of effusion size and incision colour were found to have identical results when compared to in-office visits in adolescents post-knee arthroscopy.65 Another study in adults reported near perfect inter-rater reliability in evaluation of knee effusion.46 Moreover, MCL stress testing was found to have substantial agreement and high inter- and intra-rater reliability56 while the Apley grind test was found to have only slight agreement when compared to an in-person examination.49
In comparison to a traditional visit, telemedicine appointments in adults with chronic knee conditions demonstrated high levels of agreement with respect to clinical diagnosis and subsequent management decisions. Two studies revealed that the pathoanatomical diagnosis was either the same or similar in 78% and 89% of the cases.28,56 There was 93% agreement in the selected management pathway, 93% agreement on request for further pathology and 86% agreement on request for further radiological investigations.28 Lastly, in adults indicated for knee surgery who underwent a telemedicine interview followed by an in-person evaluation, the final pre-operative plans were only changed in 4% of the cases. This highlights telemedicine’s potential in the development of accurate surgical plans for orthopedic patients.66
Ankle and Foot
Like in the knee exam, patients should be instructed to wear shorts and to be barefoot in preparation for their virtual appointment. The camera should be positioned at the level of the patient’s shins when sitting, and on the ground angled towards their feet when standing.67,68 A mobile device rather than a desktop can facilitate camera positioning. In the case of traumatic injuries, clinicians can use the Ottawa Ankle Rule over videoconference to determine whether imaging is needed to evaluate for a foot or ankle fracture.32
Inspection and Palpation
When observing the ankle and foot, the clinician should look for misalignment, atrophy, deformity, incision, scarring, rash, swelling, ecchymosis and erythema in the frontal, sagittal and posterior planes.11,67,68 The plantar aspect of the foot should not be neglected. Special attention should be paid to the Achilles tendon, plantar fascia, and the possible presence of pes planus, pes cavus and bunions. We recommend that the arches of the feet be examined with and without weight-bearing to differentiate between muscle insufficiency and structural causes. The number of toes visible lateral to each ankle should also be assessed as it is an indicator of over-pronation.11 Gait assessment includes standard walking, toe walking and heel walking. The caregiver can be asked to position the camera on the ground to get a better view of the feet. In an ambulatory child, the clinician can also assess running, jumping, hopping on one foot or single leg stance.11 Patients should be asked to point to the area of maximal tenderness which is easily identifiable as many structures causing pathology in this area are located superficially.67
Although distal pulses cannot be reliably palpated by the patient or caregiver, circulation can be assessed first by noting any colour incongruencies between both soles of the feet.67 The clinician can then assess for temperature differences between their feet in response to the patient’s touch or ideally, the caregiver’s touch.68 Capillary refill can be tested by asking the patient to press on the big toe until it blanches and allowing it to return to pink while on camera, noting how long this takes.68
ROM Assessment
The ROM can be visually estimated or quantified with the assistance of smartphone goniometers. Dorsiflexion, plantar flexion, eversion, and inversion can be observed with the patient seated with their feet hanging above the floor.67,68 When testing active ROM, providers can consider having the patient plantar flex against a caregiver’s hand which may elicit pain in the case of an ankle sprain.4
Three smartphone apps can be used to measure both dorsiflexion and plantar flexion in adults: “Goniometer Pro”, “Clinometer + Bubble Level” and “Dr. Goniometer”.69 Goniometer Pro and Clinometer + Bubble Level are accelerometer-based applications which require a smartphone to be held against the patient’s lateral malleolus, with the side edge of the phone parallel to the longitudinal axis of the fifth metatarsal. As mentioned previously, Dr. Goniometer is photo-capture based. All three apps were found to have good to excellent inter-rater reliability and moderate correlation when compared to a manual goniometer, with Dr. Goniometer having the highest correlation.69 Similarly, two other apps were studied only for dorsiflexion in adults: “iHandy Level”14 and “TiltMeter”.34 Both accelerometer-based applications measure ankle dorsiflexion with the patient performing a weight-bearing lunge and the smartphone placed either distal to the tibial tuberosity (iHandy) or against the flat surface of the Achilles tendon (TiltMeter). TiltMeter and iHandy were found to have good to excellent inter- and intra-rater reliability, and they satisfied criterion validity when compared to a digital inclinometer and motion tracker, respectively.14,34 Although these tools prove to be reliable and/or valid in the clinic, none were studied in pediatric populations and the reliability of the measurements may vary with user experience.34 Moreover, placement of the smartphone device as well as performing a weight-bearing lunge may be challenging in young children.
Sensory Examination
As described in the Back and Lumbosacral Spine section, clinicians can screen for touch, pinprick, and temperature sensation of the dermatomes supplied by the superficial fibular, deep fibular, tibial, sural, and saphenous nerves.
Motor Examination
Strength testing has been described as one of the largest challenges of the virtual foot and ankle examination.14,34 Nevertheless, the clinician can assess for ankle dorsiflexion, plantar flexion, eversion, inversion, and big toe extensor strength by having the patient or caregiver resist the patient’s movements while communicating perceived strength.68 In addition, a patient’s ability to walk on their tip toes indicates at least 4/5 strength in plantar flexion67,68 but asymmetries may be difficult to appreciate virtually. Having the patient walk on their heels can assess for dorsiflexion strength while lateral and medial foot walks can assess for ankle inversion and eversion, respectively.
Special Testing
Several studies have adapted special testing of the foot and ankle to virtual consultations.4,11,20,67,68,70 Clinicians can guide the patient to test for pes planus by performing heel raises, and pes cavus by performing the Coleman block test (Figure S26). It is also possible to test for hallux rigidus by assessing the ROM of the big toe and for Achilles rupture by guiding the patient through a Thompson test (Figure S27). If a Morton’s neuroma is suspected, the clinician can ask the patient to perform a self-applied metatarsal squeeze and assess for tenderness between the metatarsal heads, pain reproduction or the presence of a clicking sound (Figure S28).
Reliability and Validity
A systematic review identified a study demonstrating criterion validity and reliability in performing a virtual examination of the ankle in adults compared to face-to-face consultations.46 Out of 15 patients presenting with ankle pain, 14 received either the same (53%) or a similar (40%) pathoanatomical diagnosis from the in-person versus online examiners, with high inter- and intra-rater reliability. Clinical observations of ankle ROM, calcaneofibular ligament stress testing, gait analysis and neurodynamic testing (eg leg squat) were found to have significant agreement between examiners, with high inter- and intra-rater reliability. Additionally, standardized virtual management of acute Achilles’ tendon rupture has been shown to be safe and reproducible, with re-rupture rates comparable to those managed in person.71 Despite not being specific to the pediatric population, the evidence highlighted above can increase providers’ confidence when performing a virtual foot and ankle exam.
Gait, Balance and Movement Assessment
To ensure proper evaluation of gait, there should be adequate room to permit a full-body view of the patient walking both towards and away from the camera. A caregiver can be helpful in controlling camera placement as well as assisting the child if there are concerns regarding gait unsteadiness. When inspecting the child’s gait, the clinician should observe the child walking towards and away from the camera, assessing for symmetry and possible joint malalignment such as knee varus and valgus.4 Attention should be paid to indications of weakness, sensory loss, incoordination, spasticity as well as an antalgic gait, and feelings of instability or mechanical block.11 In addition, we suggest that single leg stance, tandem gait, toe-walking, heel-walking, running, jumping or hopping on one foot should be observed. A Romberg test should be considered if tandem gait is abnormal.
Special Testing
The Tinetti test and Berg Balance Scale have been shown to have high inter-rater reliability when performed over videoconference.46 There exists modified, pediatric versions of both tests which are described below.
Modified Performance-Oriented Mobility Assessment (mPOMA). Also known as the Tinetti test, the POMA has been originally validated for evaluating gait and balance disorders in the elderly population.72 The gait subtest evaluates initiation of gait, step characteristics, path and trunk sway and has recently been modified and validated for use in children with ambulatory difficulties.73 The balance subtest evaluates sitting and standing balance. To our knowledge, a modified version of the balance subtest does not exist, although the original has been used in studies on pediatric populations.74
Pediatric Balance Scale (PBS). The PBS is a modified version of the Berg Balance Scale used to assess functional balance in school-aged children. Items on the scale include, among others, sit-to-stand, various sitting and standing positions as well as retrieving objects from the floor.75 It has been demonstrated to have good test-retest and inter-rater reliability when used in children of ages 5–15 with mild-to-moderate motor impairments.75
Reliability and Validity
When compared to in-person examination of gait, videoconference assessments have been shown to exhibit excellent inter-rater49 and intra-rater reliability26 in patients without hip pathology and patients with spinal pathologies, respectively.
Assessment Scores
At the present time, we are unaware of any validated assessment scores for pediatric gait assessment in the telemedicine context. Nonetheless, the following observational gait tools have been identified as relatively simple and quick to use, making them amenable to the virtual platform. We believe they can be applied to children with gait abnormalities, regardless of if they have cerebral palsy.
Physician Ratings Scale (PRS). This is an observational tool for clinical gait evaluation originally proposed to assess gait in children with cerebral palsy. It has undergone several modifications and typically has high intra-observer but poor inter-observer reliability in children with cerebral palsy.76 If clinicians choose to implement this tool, they should observe the child’s gait in both sagittal and coronal planes, scoring each side and documenting scores for future comparison.
Edinburgh Visual Gait Score (EVGS). While developed specifically for children with cerebral palsy, the EVGS is similar to the PRS but has stronger psychometric properties to enhance reliability.77 It also has a similar reliability profile to the PRS.76,77
Pediatric version of the Wisconsin Gait Scale (WGS). The WGS is a valuable observational tool originally destined for adult stroke patients which has been modified for children with hemiplegic cerebral palsy given that both gaits are very similar.78 The authors have reported very high inter- and intra-observer reliability.
Lastly, gait and balance assessment can be followed by a general evaluation of the child’s movement capabilities. The Movement Assessment Battery for Children 2nd Edition (MABC-2) is a tool providers can use to assess a child’s upper and lower limb functioning which was shown to be valid when applied over videoconference.79 The MABC-2 is a standardized motor assessment which includes 3 subsets of tests: manual dexterity, aiming and catching as well as balance. If the child scores less than 1.5 standard deviations below the mean, it is suggestive of significant movement difficulty. It has been demonstrated that there was no statistical difference in the agreement between face-to-face and telemedicine appointments administering the test, suggesting completion of the MABC-2 is feasible over videoconference.
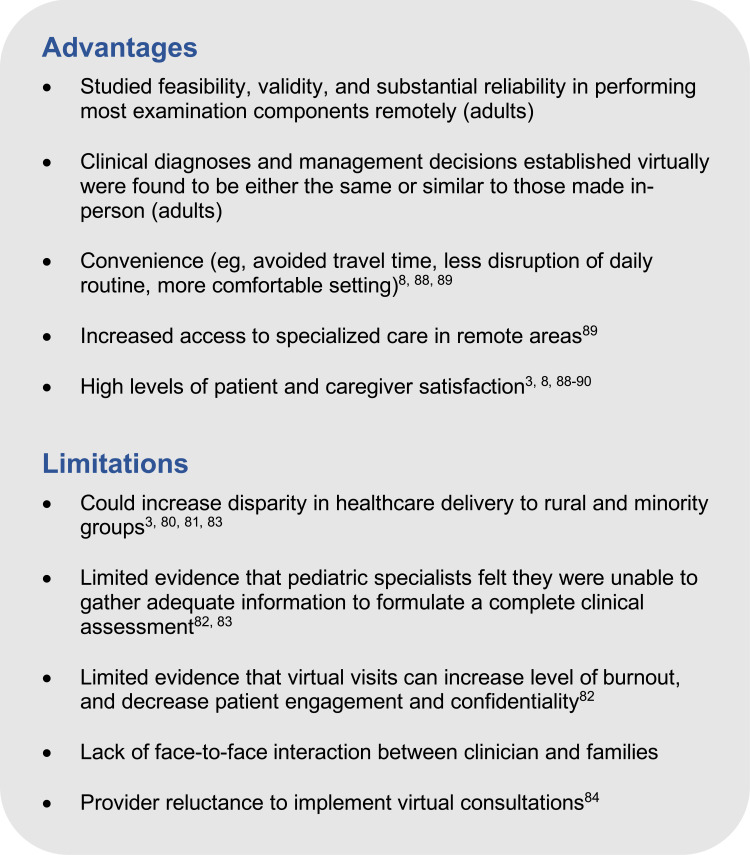
Limitations of Telemedicine
Providers must also be cognizant of the limitations of telemedicine and challenges it can introduce, both from a clinician and patient perspective. These are summarized in Figure 2 alongside the many advantages of telemedicine. First, due to telemedicine’s reliance on technology, it could further increase disparity in the delivery of healthcare, primarily impacting rural populations, racial and ethnic minorities, as well as low-income populations. For instance, some rural communities may not have access to mobile technologies (smartphones, tablets) or to a reliable internet connection due to lack of infrastructure.80 Racial and ethnic minority groups have also been shown to have more telephone than video consultations, suggesting a lack of access.3 In addition, groups with lower household income tend to be less likely to attend telemedicine appointments.81
Figure 2.
Advantages and limitations of telemedicine for pediatric musculoskeletal examinations.
Second, there is evidence that pediatric specialists sometimes feel unable to gather the necessary information from their remote consultations in order to formulate a complete clinical assessment of their patients.82,83 Furthermore, some feel that virtual consultations increased level of burnout and decreased patient engagement and confidentiality.82 Concomitantly, adult studies have shown that there is general feasibility, validity, and substantial reliability in performing most components of the lower limbs examination remotely. Clinical diagnoses established virtually were also found to be either the same or similar to those made in-person in the majority of cases, and management decisions had high agreement. This discordance may suggest a discrepancy between the reliability of virtual examinations in the context of a research study and in real-world clinical practice, especially in the setting of a pediatric virtual visit. These examinations require creativity depending on the location of the patient and family, knowledge of how to navigate technical issues, consideration of the examination sequence, and of how to cue the child and caregiver to gain optimal views of the areas of interest. All of these are added challenges providers must consider. Research efforts should therefore be focused on validating various components of musculoskeletal examinations in children, including agreement on clinical diagnosis and management plan. Efforts should also be made to identify barriers to conducting a thorough remote musculoskeletal examination as well as training clinicians on how to effectively provide virtual patient care. Until such research is available, we recommend that clinicians maintain a low threshold for undertaking further in-person evaluation for their pediatric patients. In addition, new patient referrals can be first screened by a physician who would automatically direct the most urgent cases to a dedicated clinic. Most new and established patients can then be scheduled for a videoconference or phone appointment. This triaging process at a dedicated pediatric neurologic clinic has been demonstrated as effective in transitioning to virtual patient care,3 and may reduce the burnout physicians may feel from handling emergent cases remotely.
As a final point, patients and families are typically amenable to participating in virtual encounters with some preferring remote visits over face-to-face.8 However, they may be reluctant to adopt this service over conventional appointments due to lack of direct interaction with their provider which may figuratively distance both parties even further. Providers may also be resistant to implementing telemedicine into their practice due to the necessary technological infrastructure and savviness, uncertainty regarding reimbursement for remote encounters, subjective resistance to change, and lack of training on providing patient care remotely.84 Furthermore, physicians’ medicolegal liability is the same as with in-person visits, which can be perceived as a disadvantage for those who are unable to fully examine their patients in person.85
Conclusion
Telemedicine for pediatric musculoskeletal consultations provides an opportunity to deliver convenient patient and family-centered care while minimizing potential COVID-19 exposure and providing remote communities with access to specialized care. This review presented clinicians with foundational guidelines in performing a virtual musculoskeletal examination of the back, spine, and lower limbs, serving as a starting point for standardizing the pediatric physical exam using telemedicine. It also highlighted currently available smartphone applications for their ability to measure joint ROM reliably, serving as a tool that clinicians can adopt into their practice.
Studies in adults have demonstrated that there is general feasibility, validity, and substantial reliability in performing most examination components remotely. Primary diagnoses established virtually were found to be either the same or similar in the vast majority of cases and management decisions were also shown to have high agreement. Despite this, some pediatric specialists felt that they were unable to gather the necessary information to formulate a complete clinical assessment of their patients. Clinicians should therefore retain a low threshold for undertaking further in-person evaluation if said diagnosis or initial management is unclear. This also presents an area in which future research efforts should be dedicated, namely in validating musculoskeletal examinations in pediatric populations, identifying barriers to conducting such examinations successfully, and training physicians on providing virtual care.
Upon setting a triaging system to identify patients appropriate for remote consultations and those for face-to-face visits, a well-structured virtual consultation presents many advantages to patients and clinicians. These include high satisfaction, convenience, and increased access to specialized care in remote areas. At the same time, providers must also be aware of the potential barriers to implementing telemedicine into their practice and be willing to adopt this technology. Overall, with clinician guidance and acceptance as well as caregiver assistance, telemedicine examinations are efficient and effective tools which can be integrated in our standard of care for pediatric patients and their families.
Acknowledgments
Informed consent has been provided by all parties, including parents or legal guardians of any minors, for their photographs to be published in this review. The research activities of the Edwards Family Interdisciplinary Centre for Complex Pain of the Montreal Children’s Hospital are supported by unrestricted grants of the Montreal Children’s Hospital Foundation and of the Louise and Alan Edwards Foundation. We would also like to acknowledge the efforts of Émilie Groulx-Boivin from McGill University’s Faculty of Medicine in helping structure and edit this review.
Abbreviations
ROM, range of motion; SIJ, sacroiliac joint; PSIS, posterior superior iliac spine; 5R-STS, five repetition sit-to-stand; SLR, straight leg raise; DTR, deep tendon reflexes; ASIS, anterior superior iliac spine; FABER, flexion abduction external rotation; RCT, randomized control trial; FADIR, flexion adduction internal rotation; WOMAC, Western Ontario and McMaster Universities Arthritis Index; TUG, timed up-and-go; 6MWT, 6 minute walk test; OA, osteoarthritis; JIA, juvenile idiopathic arthritis; PT, physiotherapy; KOOS-Child, Knee Injury and Osteoarthritis Outcome Score for Children; IKDC, International Knee Documentation Committee; HSS Pedi-FABS, Hospital for Special Surgery Pediatric Functional Activity Brief Scale; PRS, Physician Rating Scale; EVGS, Edinburgh Visual Gait Scale; WGS, Wisconsin Gait Scale.
Disclosure
Dr. Ingelmo received unrestricted support from the Louise and Alan Edwards Foundation and from the Montreal Children’s Hospital Foundation. The authors report no other conflicts of interest in this work.
References
- 1.Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018;58(4):475–485. doi: 10.1002/mus.26115 [DOI] [PubMed] [Google Scholar]
- 2.Bhaskar S, Nurtazina A, Mittoo S, Banach M, Weissert R. Editorial: telemedicine during and beyond COVID-19. Front Public Health. 2021;9:233. doi: 10.3389/fpubh.2021.662617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rametta SC, Fridinger SE, Gonzalez AK, et al. Analyzing 2589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020;95(9):e1257–e1266. doi: 10.1212/WNL.0000000000010010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rabatin AE, Lynch ME, Severson MC, Brandenburg JE, Driscoll SW. Pediatric telerehabilitation medicine: making your virtual visits efficient, effective and fun. J Pediatr Rehabil Med. 2020;13(3):355–370. doi: 10.3233/prm-200748 [DOI] [PubMed] [Google Scholar]
- 5.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16(1):1–11. doi: 10.1186/s12913-016-1717-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2):e11330. doi: 10.2196/11330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. 2019;14(8):e0221848. doi: 10.1371/journal.pone.0221848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–02. Vital Health Stat 13. 2006;159:1–66. [PubMed] [Google Scholar]
- 10.Operating procedures for pediatric telehealth. American Telemedicine Association; 2021. Available from:https://www.americantelemed.org/resources/operating-procedures-for-pediatric-telehealth/. Accessed September11, 2021. [DOI] [PubMed] [Google Scholar]
- 11.Laskowski ER, Johnson SE, Shelerud RA, et al. The telemedicine musculoskeletal examination. Mayo Clinic Proc. 2020;95(8):1715–1731. doi: 10.1016/j.mayocp.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satin AM, Lieberman IH. The virtual spine examination: telemedicine in the era of COVID-19 and beyond. Global Spine J. 2020;11:2192568220947744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International PMM. Virtual or video-pGALS (V-pGALS). Pediatric musculoskeletal matters international. Available from:http://www.pmmonline.org/doctor/approach-to-clinical-assessment/examination/v-pgals. Accessed March4, 2021.
- 14.Vohralik SL, Bowen AR, Burns J, Hiller CE, Nightingale EJ. Reliability and validity of a smartphone app to measure joint range. Am J Phys Med Rehabil. 2015;94(4):325–330. doi: 10.1097/PHM.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 15.Pourahmadi M, Momeni E, Mohseni N, Hesarikia H, Ghanjal A, Shamsoddini A. The reliability and concurrent validity of a new iPhone® application for measuring active lumbar spine flexion and extension range of motion in patients with low back pain. Physiother Theory Pract. 2021;37(1):204–217. doi: 10.1080/09593985.2019.1616017 [DOI] [PubMed] [Google Scholar]
- 16.Pourahmadi MR, Taghipour M, Jannati E, Mohseni-Bandpei MA, Takamjani IE, Rajabzadeh F. Reliability and validity of an iPhone® application for the measurement of lumbar spine flexion and extension range of motion. PeerJ. 2016;4:e2355. doi: 10.7717/peerj.2355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iyer S, Shafi K, Lovecchio F, et al. The spine physical examination using telemedicine: strategies and best practices. Global Spine J. 2020;10:2192568220944129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoon JW, Welch RL, Alamin T, et al. Remote virtual spinal evaluation in the era of COVID-19. Int J Spine Surg. 2020;14(3):433–440. doi: 10.14444/7057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robblee J. Conducting a telemedicine neurologic examination. American Headache Society; 2020. Available from:https://americanheadachesociety.org/news/telemedicine-neurologic-examination/. Accessed February23, 2021. [Google Scholar]
- 20.Verduzco‐Gutierrez M, Bean AC, Tenforde AS, Tapia RN, Silver JK. How to conduct an outpatient telemedicine rehabilitation or prehabilitation visit. PM&R. 2020;12(7):714–720. doi: 10.1002/pmrj.12380 [DOI] [PubMed] [Google Scholar]
- 21.Wahezi SE, Duarte RA, Yerra S, et al. Telemedicine during COVID-19 and beyond: a practical guide and best practices multidisciplinary approach for the orthopedic and neurologic pain physical examination. Pain Phy. 2020;23(4s):S205–s238. [PubMed] [Google Scholar]
- 22.Sardar ZM, Coury JR, Luzzi AJ, Weidenbaum M, Riew KD. The telehealth spine physical examination: a practical approach learned during the COVID-19 pandemic. World Neurosurg. 2021. doi: 10.1016/j.wneu.2021.06.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158(1):119–123.e4. doi: 10.1016/j.jpeds.2010.07.021 [DOI] [PubMed] [Google Scholar]
- 24.Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207–218. doi: 10.1016/j.math.2005.01.003 [DOI] [PubMed] [Google Scholar]
- 25.Piche J, Butt BB, Ahmady A, Patel R, Aleem I. Physical examination of the spine using telemedicine: a systematic review. Global Spine J. 2020;10:2192568220960423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jansen T, Gathen M, Touet A, et al. [Spine examination during COVID-19 pandemic via video consultation] Telemedizinische Wirbelsäulenuntersuchung während der COVID-19-Pandemie. Z Orthop Unfall. 2021;159(2):193–201. doi: 10.1055/a-1283-7160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lovecchio F, Riew GJ, Samartzis D, et al. Provider confidence in the telemedicine spine evaluation: results from a global study. Eur Spine J. 2020;30:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cottrell MA, O’Leary SP, Swete-Kelly P, et al. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskeletal Sci Practice. 2018;38:99–105. doi: 10.1016/j.msksp.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 29.Lightsey IVHM, Crawford AM, Xiong GX, Schoenfeld AJ, Simpson AK. Surgical plans generated from telemedicine visits are rarely changed after in person evaluation in spine patients. Spine J. 2020;21:359–398. [DOI] [PubMed] [Google Scholar]
- 30.Swensen Buza S, Lawton CD, Lamplot JD, et al. The hip physical examination for telemedicine encounters. HSS J. 2021;17(1):75–79. doi: 10.1177/1556331620975708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102(12):e57–e57. doi: 10.2106/JBJS.20.00609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yedlinsky NT, Peebles RL. Telemedicine management of musculoskeletal issues. Am Fam Physician. 2021;103(3):147–154. [PubMed] [Google Scholar]
- 33.Russo RR, Burn MB, Ismaily SK, et al. Is digital photography an accurate and precise method for measuring range of motion of the hip and knee? J Exp Orthopaed. 2017;4(1):1–8. doi: 10.1186/s40634-017-0103-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi W, Zheng H, Franklin P, Tulu B. mHealth technologies for osteoarthritis self-management and treatment: a systematic review. Health Info J. 2019;25(3):984–1003. doi: 10.1177/1460458217735676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.St-Pierre M-O, Sobczak S, Fontaine N, Saadé N, Boivin K. Quantification and reliability of hip internal rotation and the FADIR test in supine position using a smartphone application in an asymptomatic population. J Manipulative Physiol Ther. 2020;43(6):620–626. doi: 10.1016/j.jmpt.2019.10.009 [DOI] [PubMed] [Google Scholar]
- 36.Ganokroj P, Sompornpanich N, Kerdsomnuek P, Vanadurongwan B, Lertwanich P. Validity and reliability of smartphone applications for measurement of hip rotation, compared with three‐dimensional motion analysis. BMC Musculoskelet Disord. 2021;22(1):166. doi: 10.1186/s12891-021-03995-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ceballos-Laita L, Mingo-Gómez T, Mar Latorre-Balsa M, Jiménez-del-Barrio S. Reliability of two smartphone applications to measure the hip range of motion in asymptomatic patients. Archiv Physiother Global Researches. 2019;23(1):21–27. [Google Scholar]
- 38.Sarac D, Yalcinkaya G, Unver B. AB1197-HPR Validity and reliability of a smartphone goniometer application for measuring hip range of motion in patients with hip osteoarthritis: a pilot study. Ann Rheum Dis. 2017;76(Suppl2):1531. doi: 10.1136/annrheumdis-2017-eular.5710 [DOI] [Google Scholar]
- 39.Miley E, May J, Albertin E, Takahashi E, Goodman C, Pettaway A. Reliability and validity for measuring active hip rotation with the clinometer smartphone application™. J Rehabil Sci Res. 2019;6(4):193–199. doi: 10.30476/jrsr.2019.82397.1031 [DOI] [Google Scholar]
- 40.Mohammad WS, Elattar FF, Elsais WM, AlDajah SO. Validity and reliability of a smartphone and digital inclinometer in measuring the lower extremity joints range of motion. Montenegrin J Sports Sci Med. 2021;10(2):47–52. doi: 10.26773/mjssm.210907 [DOI] [Google Scholar]
- 41.Charlton PC, Mentiplay BF, Pua Y-H, Clark RA. Reliability and concurrent validity of a smartphone, bubble inclinometer and motion analysis system for measurement of hip joint range of motion. J Sci Med Sport. 2015;18(3):262–267. doi: 10.1016/j.jsams.2014.04.008 [DOI] [PubMed] [Google Scholar]
- 42.Whyte E, Doinn TO, Downey M, O’Connor S. Reliability of a smartphone goniometric application in the measurement of hip range of motion among experienced and novice clinicians. J Sport Rehabil. 2021;1(aop):1–4. [DOI] [PubMed] [Google Scholar]
- 43.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):506. doi: 10.1186/s12891-019-2900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mecklenburg G, Smittenaar P, Erhart-Hledik JC, Perez DA, Hunter S. Effects of a 12-week digital care program for chronic knee pain on pain, mobility, and surgery risk: randomized controlled trial. J Med Internet Res. 2018;20(4):e156–e156. doi: 10.2196/jmir.9667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verbecque E, Schepens K, Theré J, Schepens B, Klingels K, Hallemans A. The timed up and go test in children: does protocol choice matter? A systematic review. Pediatr Phy Ther. 2019;31(1):22–31. doi: 10.1097/PEP.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 46.Mani S, Sharma S, Omar B, Paungmali A, Joseph L. Validity and reliability of internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. 2017;23(3):379–391. doi: 10.1177/1357633X16642369 [DOI] [PubMed] [Google Scholar]
- 47.Cacau L, Santana-Filho V, Maynard LG, Gomes Neto M, Fernandes M, Carvalho VO. Reference values for the six-minute walk test in healthy children and adolescents: a systematic review. Braz J Cardiovasc Surg. 2016;31(5):381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vambheim SM, Lyby PS, Aslaksen PM, Flaten MA, Åsli O, Martinussen LM. The fear of pain questionnaire-III and the fear of pain questionnaire-short form: a confirmatory factor analysis. J Pain Res. 2017;10:1871–1878. doi: 10.2147/JPR.S133032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jaenisch M, Kohlhof H, Touet A, et al. [Evaluation of the feasibility of a telemedical examination of the hip and pelvis - early lessons from the COVID-19 pandemic] Evaluation der Durchführbarkeit einer telemedizinischen Untersuchung des Hüftgelenks und des Beckens – frühe Lehren aus der COVID-19-Pandemie. Z Orthop Unfall. 2021;159(1):39–46. doi: 10.1055/a-1289-0779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Owusu-Akyaw KA, Hutyra CA, Evanson RJ, Cook CE, Reiman M, Mather RC. Concurrent validity of a patient self-administered examination and a clinical examination for femoroacetabular impingement syndrome. BMJ Open Sport Exerc Med. 2019;5(1):e000574. doi: 10.1136/bmjsem-2019-000574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lamplot JD, Pinnamaneni S, Swensen-Buza S, et al. The virtual shoulder and knee physical examination. Orthopaed J Sports Med. 2020;8(10):2325967120962869. doi: 10.1177/2325967120962869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Atanda A, Shah SA. Virtual musculoskeletal examination using telemedicine. In Telemedicine in Orthopedic Surgery and Sports Medicine. Springer; 2021:81–84. [Google Scholar]
- 53.Pereira LC, Rwakabayiza S, Lécureux E, Jolles BM. Reliability of the knee smartphone-application goniometer in the acute orthopedic setting. J Knee Surg. 2017;30(03):223–230. [DOI] [PubMed] [Google Scholar]
- 54.Dos Santos RA, Derhon V, Brandalize M, Brandalize D, Rossi LP. Evaluation of knee range of motion: correlation between measurements using a universal goniometer and a smartphone goniometric application. J Bodyw Mov Ther. 2017;21(3):699–703. doi: 10.1016/j.jbmt.2016.11.008 [DOI] [PubMed] [Google Scholar]
- 55.Castle H, Kozak K, Sidhu A, et al. Smartphone technology: a reliable and valid measure of knee movement in knee replacement. Int J Rehabil Res. 2018;41(2):152–158. doi: 10.1097/MRR.0000000000000276 [DOI] [PubMed] [Google Scholar]
- 56.Richardson BR, Truter P, Blumke R, Russell TG. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J Telemed Telecare. 2017;23(1):88–95. doi: 10.1177/1357633X15627237 [DOI] [PubMed] [Google Scholar]
- 57.Mehta SP, Kendall KM, Reasor CM. Virtual assessments of knee and wrist joint range motion have comparable reliability with face‐to‐face assessments. Musculoskeletal Care. 2020;19:208–216. [DOI] [PubMed] [Google Scholar]
- 58.van Meer B, Meuffels D, Reijman M. A comparison of the standardized rating forms for evaluation of anterior cruciate ligament injured or reconstructed patients; 2017.
- 59.Örtqvist M, Iversen MD, Janarv P-M, Broström EW, Roos EM. Psychometric properties of the knee injury and osteoarthritis outcome score for children (KOOS-child) in children with knee disorders. Br J Sports Med. 2014;48(19):1437–1446. doi: 10.1136/bjsports-2013-093164 [DOI] [PubMed] [Google Scholar]
- 60.Örtqvist M, Roos EM, Broström EW, Janarv P-M, Iversen MD. Development of the knee injury and osteoarthritis outcome score for children (KOOS-child) comprehensibility and content validity. Acta orthopaedica. 2012;83(6):666–673. doi: 10.3109/17453674.2012.747921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iversen M, Lee B, Connell P, Andersen J, Anderson A, Kocher M. Validity and comprehensibility of the international knee documentation committee subjective knee evaluation form in children. Scand J Med Sci Sports. 2010;20(1):e87–e95. doi: 10.1111/j.1600-0838.2009.00917.x [DOI] [PubMed] [Google Scholar]
- 62.Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified international knee documentation committee subjective knee form (pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39(5):933–939. doi: 10.1177/0363546510383002 [DOI] [PubMed] [Google Scholar]
- 63.Jacobsen JS, Knudsen P, Fynbo C, Rolving N, Warming S. Reproducibility and responsiveness of a D anish P edi‐IKDC subjective knee form for children with knee disorders. Scand J Med Sci Sports. 2016;26(12):1408–1414. doi: 10.1111/sms.12589 [DOI] [PubMed] [Google Scholar]
- 64.Fabricant PD, Robles A, Downey-Zayas T, et al. Development and validation of a pediatric sports activity rating scale: the hospital for special surgery pediatric functional activity brief scale (HSS pedi-FABS). Am J Sports Med. 2013;41(10):2421–2429. doi: 10.1177/0363546513496548 [DOI] [PubMed] [Google Scholar]
- 65.Abel KC, Baldwin K, Chuo J, et al. Can telemedicine be used for adolescent postoperative knee arthroscopy follow-up? JBJS J Orthopaed Phy Assist. 2017;5(4):e26. doi: 10.2106/JBJS.JOPA.17.00014 [DOI] [Google Scholar]
- 66.Crawford AM, Lightsey HM, Xiong GX, Striano BM, Schoenfeld AJ, Simpson AK. Telemedicine visits generate accurate surgical plans across orthopaedic subspecialties. Arch Orthop Trauma Surg. 2021;21:1–8. doi: 10.1007/s00402-021-03903-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eble SK, Hansen OB, Ellis SJ, Drakos MC. The virtual foot and ankle physical examination[formula: see text]. Foot Ankle Int. 2020;41(8):1017–1026. doi: 10.1177/1071100720941020 [DOI] [PubMed] [Google Scholar]
- 68.Hansen OB, Eble SK, Ellis SJ, Drakos MC. Adaptation of the foot and ankle physical exam for telehealth. HSS J. 2021;17(1):85–90. doi: 10.1177/1556331620974675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang KY, Hussaini SH, Teasdall RD, Gwam CU, Scott AT. Smartphone applications for assessing ankle range of motion in clinical practice. Foot Ankle Orthopaed. 2019;4(3):2473011419874779. doi: 10.1177/2473011419874779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Phuphanich ME, Sinha KR, Truong M, Pham QG. Telemedicine for musculoskeletal rehabilitation and orthopedic postoperative rehabilitation. Phys Med Rehabil Clin N Am. 2021;32(2):319–353. doi: 10.1016/j.pmr.2020.12.004 [DOI] [PubMed] [Google Scholar]
- 71.Robertson A, Godavitarne C, Bellringer S, et al. Standardised virtual fracture clinic management of achilles tendon ruptures is safe and reproducible. Foot Ankle Surg. 2019;25(6):782–784. doi: 10.1016/j.fas.2018.10.010 [DOI] [PubMed] [Google Scholar]
- 72.Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80(3):429–434. doi: 10.1016/0002-9343(86)90717-5 [DOI] [PubMed] [Google Scholar]
- 73.Phillips D, Griffin D, Przybylski T, et al. Development and validation of a modified performance-oriented mobility assessment tool for assessing mobility in children with hypophosphatasia. J Pediatr Rehabil Med. 2018;11:187–192. doi: 10.3233/PRM-170523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Niiler TA. Assessing dynamic balance in children with cerebral palsy. In: Miller F, Bachrach S, Lennon N, O’Neil M, editors. Cerebral Palsy. Springer International Publishing; 2018:1–32. [Google Scholar]
- 75.Franjoine MR, Gunther JS, Taylor MJ. Pediatric balance scale: a modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatr Phy Ther. 2003;15(2):114–128. doi: 10.1097/01.PEP.0000068117.48023.18 [DOI] [PubMed] [Google Scholar]
- 76.Maathuis KGB, van der Schans CP, van Iperen A, Rietman HS, Geertzen JHB. Gait in children with cerebral palsy: observer reliability of physician rating scale and Edinburgh visual gait analysis interval testing scale. J Pediatr Orthopaed. 2005;25(3):268–272. doi: 10.1097/01.bpo.0000151061.92850.74 [DOI] [PubMed] [Google Scholar]
- 77.Read HS, Hazlewood ME, Hillman SJ, Prescott RJ, Robb JE. Edinburgh visual gait score for use in cerebral palsy. J Pediatr Orthopaed. 2003;23(3):296–301. doi: 10.1097/01241398-200305000-00005 [DOI] [PubMed] [Google Scholar]
- 78.Guzik A, Drużbicki M, Kwolek A, et al. The paediatric version of Wisconsin gait scale, adaptation for children with hemiplegic cerebral palsy: a prospective observational study. BMC Pediatr. 2018;18(1):301. doi: 10.1186/s12887-018-1273-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nicola K, Waugh J, Charles E, Russell T. The feasibility and concurrent validity of performing the movement assessment battery for children–2nd edition via telerehabilitation technology. Res Dev Disabil. 2018;77:40–48. doi: 10.1016/j.ridd.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 80.Davis LE, Harnar J, LaChey-Barbee LA, Pirio RS, Fraser A, King MK. Using teleneurology to deliver chronic neurologic care to rural veterans: analysis of the first 1100 patient visits. Telemed e-Health. 2019;25(4):274–278. doi: 10.1089/tmj.2018.0067 [DOI] [PubMed] [Google Scholar]
- 81.Nolen L, Mejia NI. Inequities in neurology amplified by the COVID-19 pandemic. Nat Rev Neurol. 2021;17(2):67–68. doi: 10.1038/s41582-020-00452-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pooni R, Ronis T, Lee T. Telemedicine use by pediatric rheumatologists during the COVID-19 pandemic. Pediatr Rheumatol Online J. 2021;19(1):93. doi: 10.1186/s12969-021-00565-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Killackey T, Noel M, Birnie KA, et al. COVID-19 pandemic impact and response in Canadian pediatric chronic pain care: a national survey of medical directors and pain professionals. Canadian J Pain. 2021;5(1):139–150. doi: 10.1080/24740527.2021.1931069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lo MD, Gospe SM Jr. Telemedicine and child neurology. J Child Neurol. 2019;34(1):22–26. [DOI] [PubMed] [Google Scholar]
- 86.Staartjes VE, Beusekamp F, Schröder ML. Can objective functional impairment in lumbar degenerative disease be reliably assessed at home using the five-repetition sit-to-stand test? A prospective study. Eur Spine J. 2019;28(4):665–673. doi: 10.1007/s00586-019-05897-3 [DOI] [PubMed] [Google Scholar]
- 87.Weinrauch P, Quach L, Smith I. The e-quadrant test for telemedicine assessment of symptomatic articular hip pathology. Int J Adv Joint Reconstr. 2015;1:1–15. [Google Scholar]
- 88.Qubty W, Patniyot I, Gelfand A. Telemedicine in a pediatric headache clinic: a prospective survey. Neurology. 2018;90(19):e1702–e1705. doi: 10.1212/WNL.0000000000005482 [DOI] [PubMed] [Google Scholar]
- 89.Shah AC, Badawy SM. Telemedicine in pediatrics: systematic review of randomized controlled trials. JMIR Pediatr Parenting. 2021;4(1):e22696. doi: 10.2196/22696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vyas S, Murren-Boezem J, Solo-Josephson P. Analysis of a pediatric telemedicine program. Telemed e-Health. 2018;24(12):993–997. doi: 10.1089/tmj.2017.0281 [DOI] [PubMed] [Google Scholar]