Abstract
Background
Migrants are one of the most vulnerable populations facing many health issues. Inadequate health care access and unequal insurance are the most challenging. This study aimed to construct a nomogram to predict the risk of hospitalization forgone among internal migrants in China.
Methods
We analyzed the 2014 Mobile Population Social Integration and Mental Health Survey (MPSIMHS) launched by National Health and Family Planning Commission. Using the Probability Proportionate to Size Sampling method (PPS), MPSIMHS sampled from eight cities (districts) with a total sample size of 15,999. Of total 589 patients who were diagnosed with hospitalization requirement, 116 forwent their hospitalization, 473 had no forgone. Demographics, socioeconomic status, and health conditions were analyzed using univariate analysis and multivariate logistic regression. A nomogram was built and validated by applying bootstrap resampling.
Results
After model selection, gender, age group, marital status, migration range, insurance (having NRMI), and self-evaluated health were chosen into the nomogram to predict the risk of hospitalization forgone. The nomogram that predicted the risk of hospitalization forgone was validated for discrimination and calibration using bootstrap resampling. The calibration curves illustrated optimal agreement between the actual and predicted probabilities of the nomogram. The value of C-index from bootstrap was 0.80 (95% CI: 0.76–0.85).
Conclusion
This study identified some possible factors contributing to migrant’s hospitalization forgone: being single, male and middle-aged, having fixed health insurance, and having bad or great self-evaluated health. By integrating significant and easy-to-get prognostic factors, a nomogram was developed to estimate an individual patient’s risk of hospitalization forgone, which might have practical utility and the potential to assist clinicians in making hospitalization recommendations.
Keywords: urbanization, internal migrant, hospitalization forgone, nomogram, China
Background
China is initiating a new round of urbanization on an unprecedented scale boosted by significant reform on household registration. If migrants from rural areas own or rent a house or apartment in an urban area, they and their direct relatives can apply for the urban household registration.1 The proportion of urban population increased to 56% in 2015, and more than 30%, roughly 247 million living in urban areas, are migrants.2 According to statistics issued by the Development Research Center of the State Council, it is expected that the urban population will increase by 350 million by 2025. Thus, 1 billion people will live in cities by the year 2030.
There were mainly three primary health insurance schemes in China: the new rural cooperative medical insurance (NRMI; started since 2003), urban resident basic medical insurance (URBMI; begun since 2007), and urban employee basic medical insurance (UEBMI; launched in 1998), which currently covered over 1.35 billion people (95% of the total population).3 Premium subsidies for the NRMI and URBMI schemes increased to ¥360 RMB per capita by 2014 (up from ¥80 in 2009). Higher NRMI and URBMI reimbursement rates cover at least 75% and 50% of inpatient and outpatient services expenditures, respectively.4
NRMI funds are concentrated at the county level (2854 rural counties in 2014), urban (prefecture) level (333 municipalities directly under the central government in 2014) control the URBMI and UEBMI. About 70% of the rural laborers in urban areas are self-employed or work in private and small enterprises, commonly in high-risk jobs with low pay. In most counties, migrant workers seeking medical services must pay the full service cost and can only be reimbursed when returning to their hometowns.5 NRMI is not transferable from one province to another.
People choose health insurance schemes according to their employment status, Hukou (household registration), and residency.6 The benefits and financial protection are not identical within and across the different insurance, which hinders health insurance reform in China. The capita annual fund for UEBMI is approximately 6 and 7 times higher than that for the NRMI and URBMI, respectively.7 The separated urban-rural health insurance has led to the financial burden for the vulnerable population such as rural-to-urban migrants.
The health consequences followed by urbanization are mixed. In general, migrants work with lower payment, fewer benefits, and public welfare compared to urban residents.8 In China, urbanization has been co-occurred by high living standards and prolonged life expectancy. Still, the prevalence of chronic diseases and the rising number of unhealthy people may imply a health penalty.9
For migrants facing many health issues, inadequate health care access and unequal insurance are the most challenging.10 Migration caused by urbanization has been a significant demographic stimulus of NCDs, such as cardiovascular disease. Based on China’s Coronary Heart Disease (CHD) Policy Model, the future impact of urbanization was predicted using a nationwide cardiovascular disease computer simulation model. Taking 2010 as the base year, the population in 2030 was predicted with high and low urbanization rate scenarios. The incidence rate of cardiovascular disease in urban areas will increase more than twice, and the possibility of having cardiovascular disease in rural areas will increase by 27.0–45.6%. The incidence rate of age-standardized coronary heart disease is estimated to be raised by 73–81/100,00 because of urbanization, and the incidence rate of stroke is only slightly increased.11
Understanding migrants’ socio-demographic contexts is the key to figure out the possible reasons of hospitalization forgone. Previous studies have found that original culture beliefs and insufficient knowledge of health services contribute to migrants’ delayed health-seeking behavior. No study has investigated how different factors, such as socioeconomic status (SES) and medical insurance, might work in conjunction to result in hospitalization forgone among migrants in China.
If the migrant population cannot bear the relevant medical expenses or is affected by the limited reimbursement policy, it may hinder their timely hospital visit. In March 2020, the CPC Central Committee and the State Council issued “the Opinions of the CPC Central Committee and the State Council on Deepening the Reform of the Medical Security System,” which is an essential top-level design for the medical security system. The migrant population is the critical group that this regulation points to help. It is of great significance to study and predict the medical treatment of the migrant population to improve the medical security design under the new round of medical reform in China.
In this study, we show the prevalence of hospitalization forgone among migrants in China. This study also aims to identify the factors that could predict hospitalization forgone, including gender, age group, marital status, migration range, insurance (having NRMI), and self-evaluated health.
Methods
Conceptual Framework
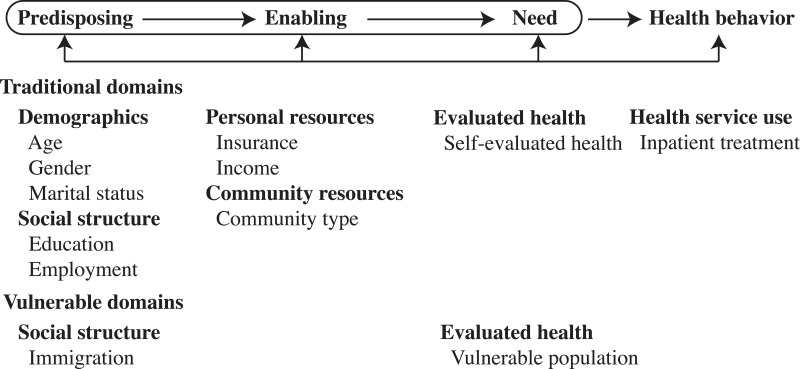
The conceptual framework of this study is developed from the revised and expanded Behavior Model for Vulnerable Populations originated from the well-known Andersen Health Service Utilization Model.12,13 Andersen introduced the model in 1968 and had undergone several phases of updates.14,15 According to the model for vulnerable populations, the factors that make some populations vulnerable might also affect health services utilization and health status. We assumed that migrants, as a vulnerable population, their use of service might be affected by three sequential clusters of factors: predisposing, enabling and need factors in two domains (traditional and vulnerable domain) (see Figure 1). In this study, predisposing factors (predisposition to use health services) include demographic characteristics (age, gender, marital status), social structures (education, employment), and vulnerable social structure (immigration). The enabling factors (impede the use of health services) include personal resources (insurance and income), community resources (community type). Need factors include self-evaluated health and vulnerable population (migration range). The outcome variable is whether patients use inpatient treatment or not.
Figure 1.
The conceptual framework based on the Andersen Health Service Utilization Model including the selected variables in this study.
Introduction of the Mobile Population Social Integration and Mental Health Survey
In 2014, the Mobile Population Social Integration and Mental Health Survey (MPSIMHS) was launched by the National Health and Family Planning Commission. The implementation plan is as follows.
Participants and Survey Content
Participants include the mobile population, which refers to the influx population aged 18–59 who has lived in the surveyed region (county, city) for over a month without registered permanent residency. The survey was conducted by using both individual and community questionnaires. The individual questionnaire includes personal and family demographics and employment information, health service use, social integration, and mental health status. Community questionnaire mainly includes demographics, community management and service, and the primary public services equalization status of mobile population health and family planning.
Sampling Method and Sample Size
Based on the sample points of the 2014 national mobile population dynamic monitoring survey (“Big Survey”), MPSIMHS sampled from eight cities (districts), including Chaoyang District of Beijing, Shenzhen and Zhongshan City (Guangdong province), Chengdu City (Sichuan province), Qingdao City (Shandong province), Jiaxing City (Zhejiang province), Xiamen City (Fujian province), Zhengzhou City (Henan province).
The Probability Proportionate to Size Sampling method (PPS) was applied for stratified, multi-stage sampling. The sampling framework was constructed among migrants reported by village or community. Twenty participants were randomly chosen from a randomly selected village or community. Migrants were defined as individuals who had lived in the residency place for over a month without “Hukou” (household registration). All migrants aged between 15 and 59 years old. The total sample size was 15,999 (2000 for each city (district), 1999 for Chengdu).
In the questionnaire, there is a variable indicated whether the subject was using inpatient service during the past 12 months and another variable showed how many people forwent hospitalization, which was used for sample selection.
Data Analysis
Both descriptive and analytical statistics were employed. Generalized linear models (GLMs) were used to test the relationship between hospitalization forgone and migration, along with other independent variables, such as age group, gender, marital status, education, community type, employment, income, health insurance (have New Rural Medical insurance or not) and self-evaluated health. GLMs are the most commonly used to model binary data and handle mixtures of categorical and continuous variables. Univariate analysis was performed based on the chi-square test. A significant difference was identified when P-value was less than 0.05.
The potential factors were screened according to the results of previous studies and univariate analysis of this study. Then stepwise model selection was applied to optimize the model. Last, based on the Akaike information criterion (AIC), the optimal model was determined using statistical model selection and suggestions from other studies. The Wald’s test and likelihood ratio test were applied to test the statistical significance of the variable in the logistic regression model. A p-value less than 0.05 indicates that a variable has statistical significance in the model. The 95% confidence interval (95% CI) was calculated. R software (version 3.5.2) was used for all statistical analyses. R packages “tidyverse” was used for data cleaning, “rms” and “forestplot” was used for creating the nomogram and forest plot graphs.
Ethical Consideration
This study is confined to the principles of the World Medical Association Declaration of Helsinki. The whole process followed the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. Permission to use the dataset was approved by the Migrant Population Service Center, National Health Commission P.R. China for this research. Ethical approval was obtained from the Ethics Committee of Jiujiang University (REC: JJU20160116). Because this study only involved identity-removed secondary data, ethical approval was not necessary. Data from the hospital information system was disaggregated.
Results
Univariate analysis was performed to explore possible factors related to hospitalization forgone (Table 1). Of total 589 patients who were diagnosed with hospitalization requirement, 116 forwent their hospitalization, 473 had no forgone. There were statistically significant differences between forgone and no forgone groups in terms of gender, age group, marital status, migration range, employment, insurance (having NRMI or not), and self-evaluated health (P<0.05). Results showed that 60 (41.38%) male patient forwent hospitalization, as well as 30 (41.67%) patient aged from 41–50 years old, 56 (27.45%) patient moving across city, 27 (26.21%) patient who was self-employed, 76 (25.00%) patient having NRMI, 7 (53.85%) patient with bad self-evaluated health and 39 (35.14%) patient with great self-evaluated health, 23 (30.67%) patient who only went to primary or lower school, 9 (29.03%) patient with family monthly income less than 2500 Yuan.
Table 1.
Univariate Analysis of Possible Factors Related to Hospitalization Forgone
| No Forgone | Forgone | Total | Chisq. Test | P value | |
|---|---|---|---|---|---|
| Total | 473 (80.31) | 116 (19.69) | 589 (100) | ||
| Gender | 55.39 | < 0.001 | |||
| Male | 85 (58.62) | 60 (41.38) | 145 (100) | ||
| Female | 388 (87.39) | 56 (12.61) | 444 (100) | ||
| Age group | 28.71 | < 0.001 | |||
| (15,30] | 262 (85.90) | 43 (14.10) | 305 (100) | ||
| (30,40] | 159 (80.30) | 39 (19.70) | 198 (100) | ||
| (40,50] | 42 (58.33) | 30 (41.67) | 72 (100) | ||
| (50,60] | 10 (71.43) | 4 (28.57) | 14 (100) | ||
| Marital status | 12.28 | 0.0045 | |||
| Married | 450 (81.82) | 100 (18.18) | 550 (100) | ||
| Not married | 20 (60.61) | 13 (39.39) | 33 (100) | ||
| Divorced or Widowed | 3 (50.00) | 3 (50.00) | 6 (100) | ||
| Education | 8.40 | 0.0778 | |||
| Undergraduate and higher | 32 (84.21) | 6 (15.79) | 38 (100) | ||
| Vocational | 64 (86.49) | 10 (13.51) | 74 (100) | ||
| High school | 113 (79.02) | 30 (20.98) | 143 (100) | ||
| Middle school | 212 (81.85) | 47 (18.15) | 259 (100) | ||
| Primary school and lower | 52 (69.33) | 23 (30.67) | 75 (100) | ||
| Migration range | 13.37 | 0.0013 | |||
| Cross county | 306 (83.84) | 59 (16.16) | 365 (100) | ||
| Cross city | 148 (72.55) | 56 (27.45) | 204 (100) | ||
| Cross province | 19 (95.00) | 1 (5.00) | 20 (100) | ||
| Community type | 5.65 | 0.0592 | |||
| Commercial or institution apartment | 133 (86.36) | 21 (13.64) | 154 (100) | ||
| Shanty town or Suburb | 203 (79.61) | 52 (20.39) | 255 (100) | ||
| Rural community | 137 (76.11) | 43 (23.89) | 180 (100) | ||
| Employment | 14.91 | 0.0019 | |||
| No job | 186 (88.57) | 24 (11.43) | 210 (100) | ||
| Employee | 189 (75.90) | 60 (24.10) | 249 (100) | ||
| Employer | 22 (81.48) | 5 (18.52) | 27 (100) | ||
| Self employed | 76 (73.79) | 27 (26.21) | 103 (100) | ||
| Family monthly income | 9.45 | 0.0924 | |||
| [0, 2500] | 22 (70.97) | 9 (29.03) | 31 (100) | ||
| (2500, 3500] | 48 (76.19) | 15 (23.81) | 63 (100) | ||
| (3500, 5000] | 105 (75.00) | 35 (25.00) | 140 (100) | ||
| (5000, 7000] | 119 (80.95) | 28 (19.05) | 147 (100) | ||
| (7000, 10,000] | 115 (85.19) | 20 (14.81) | 135 (100) | ||
| (10,000, 300,000] | 64 (87.67) | 9 (12.33) | 73 (100) | ||
| Having NRMI | 10.50 | 0.0012 | |||
| Yes | 228 (75.00) | 76 (25.00) | 304 (100) | ||
| No | 245 (85.96) | 40 (14.04) | 285 (100) | ||
| Self-evaluated health | 40.30 | < 0.001 | |||
| Bad | 6 (46.15) | 7 (53.85) | 13 (100) | ||
| Ordinary | 95 (84.82) | 17 (15.18) | 112 (100) | ||
| Good | 165 (90.66) | 17 (9.34) | 182 (100) | ||
| Very good | 135 (78.95) | 36 (21.05) | 171 (100) | ||
| Great | 72 (64.86) | 39 (35.14) | 111 (100) |
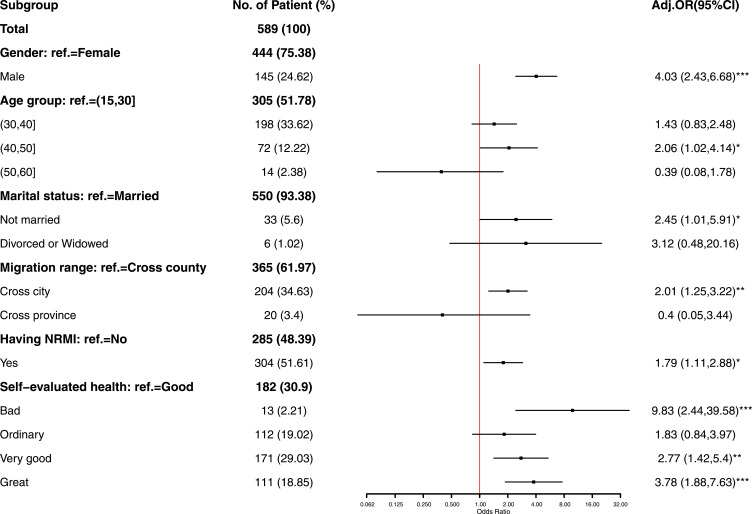
Odds ratios (ORs) for hospitalization forgone was firstly adjusted for gender, age group, marital status, education, migration range, community type, family monthly income, insurance (having NRMI), and self-evaluated health using multiple logistic regression. Through model screening, the optimized model includes six variables, including gender, age group, marital status, migration range, insurance (having NRMI), and self-evaluated health (Figure 2).
Figure 2.
Logistic regression and forest plot for hospitalization forgone among migrants.
Notes: *p<0.05; **p<0.01; ***p<0.001.
Gender, age group, marital status, migration range, insurance (having NRMI), and self-evaluated health were the variables significantly associated with hospitalization forgone in multiple logistic regression. Compared to the female, the male had higher odds of hospitalization forgone (adjusted OR=4.03; 95% CI: 2.43–6.68; P<0.001). Patients aged from 41 to 50 years old had higher odds of hospitalization forgone (adjusted OR=2.06; 95% CI: 1.02–4.14; P<0.05) compared with those aged from 16 to 30 years old. For the patient who was not married, there was a trend toward increased hospitalization forgone that was statistically significant (adjusted OR=2.45; 95% CI: 1.01–5.91; P<0.05). Compared to patients moving across county, those moving across city had higher odds of hospitalization forgone (adjusted OR=2.01; 95% CI: 1.25–3.22; P<0.01). Among patients having NRMI, there was a trend toward increased odds of hospitalization forgone that was statistically significant (adjusted OR=1.79; 95% CI: 1.11–2.88; P<0.05). Compared to patients who had good self-evaluated health, those having bad self-evaluated health (adjusted OR=9.83; 95% CI: 2.44–39.58; P<0.001), those having very good self-evaluated health (adjusted OR=2.77; 95% CI: 1.42–5.4; P<0.01) and those having great self-evaluated health (adjusted OR=3.78; 95% CI: 1.88–7.63; P<0.001) had higher odds of hospitalization forgone.
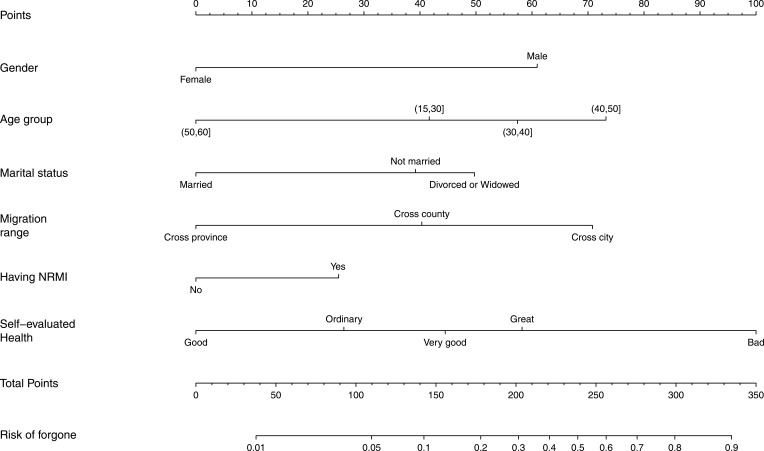
Nomogram
A nomogram of hospitalization forgone was built based on significant prognostic variables, including gender, age group, marital status, migration range, insurance (having NRMI), and self-evaluated health (Figure 3). Outcomes were reported as the risk of hospitalization forgone.
Figure 3.
Nomogram for migrants having hospitalization forgone.
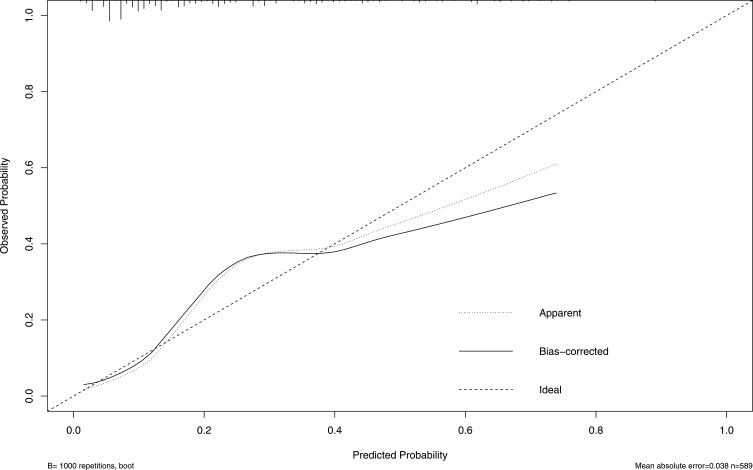
Nomograms Validation
The nomogram that predicted the risk of hospitalization forgone was validated for discrimination and calibration using bootstrap resampling. The calibration curves illustrated optimal agreement between the actual and predicted probabilities of the nomogram (Figure 4). The value of C-index from bootstrap was 0.80 (95% CI: 0.76–0.85).
Figure 4.
The calibration curves of the actual and predicted probabilities of the nomogram.
Discussion
Migrants usually work in a relatively difficult environment with higher risks, such as the construction and service industry. Studies showed that migrants had poor local health service access.16,17 A study identified that the proportion of medical return for hospitalization was 15.3%, significantly related to nontransferable health insurance.18 The result in this study presented that the proportion of having hospitalization forgone was nearly 20% among migrants, and migrants who had new rural medical insurance (NRMI) are more likely to forgo hospitalization, which might result from the fixed medical insurance across different regions. Because NRMI is not a portable health insurance, patient has to go back to their hometown to claim the reimbursement. So many patients covered by NRMI might choose to give up the hospitalization and use health service in their hometown instead. The Hukou system (household registration) in China contributed to migrants’ limited health services access.19 Our study also showed that with the increasing range of migration, especially moving across city, patients tended to forgo hospitalization, which indicated that the limited pooling level of NRMI had been an obstacle for the migrant to access necessary hospitalization. Enlarging the pooling of health insurance is helpful to increase the equity and efficiency of health insurance.
Previous studies showed a gap between local people and migrants, the latter had less inpatient care utilization.20 The result of our study showed that male migrants and those aged 41–50 were more likely to face the risk of having hospitalization forgone. The middle-aged male migrants are usually the main income provider for their family, being hospitalized can put an extra burden on patients and their families, who not only have to tolerate medical treatment costs but also suffer from the income loss due to absenteeism to work.21 Under this circumstance, they will take more time to decide whether to use inpatient care or major treatment that can lead to hospitalization forgone.
It was also noticeable that patients who had bad, or very good, or great self-evaluated health were more likely to forgo hospitalization. People with bad self-evaluated health might have relatively lower socioeconomic status, so they had limited resources for hospitalization. On the other hand, people with great self-evaluated health might have overconfident about their physical health, resulting in skip necessary hospitalization. Targeted health education should be provided to increase health service utilization.
Between the forgone and no forgone group, there were many differences in education, marital status, and employment, which were consistent with other studies: being single, having less education, and being self-employed were more likely to have hospitalization forgone.22–26 Patients being single, having less education, and self-employed may face insufficient family support, poor knowledge about health insurance, and lower income, leading to less inpatient service utilization.
A nomogram of predicting the risk of hospitalization forgone was developed by integrating significant and easy-to-get prognostic factors. Currently, there are no scoring systems for the risk of hospitalization forgone. Our nomogram is a practical tool to predict the risk of hospitalization forgone for individual patients. For example, we can use this nomogram to screen the migrants who have a greater chance to skip the initial hospital visit. Furthermore, the nomogram might be applied to the estimation of risk in policy intervention. In addition, the nomogram was assessed carefully. In this study, the calibration curve and the C-index (0.80) reflect the good discrimination power and predictive accuracy.
Limitations
Our study had some limitations. First, social-economic determinants related to hospitalization forgone were dynamic factors, which might be different overtimes and from country to country. Our findings may not be generalized to all migrants in China and other countries. Second, social capital and social support were also related to health-seeking behavior, but we could not collect the above information. Third, only the internal validation was conducted for the nomogram, lack of external validation decreased the reliability. However, this is the first study to explore predictable factors for hospitalization forgone.
Conclusion
This study identified some possible factors contributing to migrant’s hospitalization forgone: being single, male and middle-aged, having fixed health insurance, and having bad or great self-evaluated health. A nomogram was developed to estimate an individual patient’s risk of hospitalization forgone by integrating significant and easy-to-get prognostic factors. Transferable health insurance and health education should be provided for migrants to increase their health service utilization.
Acknowledgments
We would like to thank the National Health Commission of the People’s Republic of China for providing the mobile population dynamic monitoring data.
Funding Statement
We disclosed receipt of the following financial support for the research, authorship, and publication of this article: This work was supported by the National Natural Science Foundation of China [grant numbers 71864020] and China Medical Board [grant number 16-261].
Data Sharing Statement
The data that support the findings of this study are available from the National Health Commission of the People’s Republic of China upon reasonable request.
Ethics Approval and Consent to Participate
Permission to use the dataset was approved by the Migrant Population Service Center, National Health Commission P.R. China for this research. The analysis of public access data was exempt from the informed consent requirement by the Ethics Committee of Jiujiang University (REC: JJU20160116). Ethical approval was not required because this study only involved de-identified secondary data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.State Council Issued Opinions on Further Promoting Reform of Household Registration System. China Population Today. 2014;31(05):3–5.
- 2.NBSC. Statistical bulletin of the national economic and social development. Beijing: National Bureau of Statistics of China; 2015. [Google Scholar]
- 3.Liu P, Guo W, Liu H, Hua W, Xiong L. The integration of urban and rural medical insurance to reduce the rural medical burden in China: a case study of a county in Baoji City. BMC Health Serv Res. 2018;18(1):796. doi: 10.1186/s12913-018-3611-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yip W, Hsiao W. Harnessing the privatisation of China’s fragmented health-care delivery. Lancet. 2014;384(9945):805–818. doi: 10.1016/S0140-6736(14)61120-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meng Q, Xu K. Progress and challenges of the rural cooperative medical scheme in China. Bull World Health Organ. 2014;92(6):447–451. doi: 10.2471/BLT.13.131532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiu P, Yang Y, Zhang J, Ma X. Rural-to-urban migration and its implication for new cooperative medical scheme coverage and utilization in China. BMC Public Health. 2011;11(1):1. doi: 10.1186/1471-2458-11-520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang L, Langenbrunner JC. The Long March to Universal Coverage : Lessons from China. World Bank Washington Dc. 2013(UNICO Study Series 9). Available from: https://openknowledge.worldbank.org/handle/10986/13303. Accessed September 16, 2021.
- 8.Huang ZJ, Yu SM, Liu XW, Young D, Wong FY. Beyond medical insurance: delayed or forgone care among children in Chinese immigrant families. J Health Care Poor Underserved. 2009;20(2):364–377. doi: 10.1353/hpu.0.0137 [DOI] [PubMed] [Google Scholar]
- 9.Miao J, Wu X. Urbanization, socioeconomic status and health disparity in China. Health Place. 2016;42:87–95. doi: 10.1016/j.healthplace.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 10.Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet. 2012;379(9818):843–852. doi: 10.1016/S0140-6736(11)61878-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan F, Adamo S, Coxson P, et al. Projected impact of urbanization on cardiovascular disease in China. Int J Public Health. 2012;57(5):849–854. doi: 10.1007/s00038-012-0400-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen's Behavioral Model of Health Services Use: a systematic review of studies from 1998-2011. Psychosoc Med. 2012;9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273. [PMC free article] [PubMed] [Google Scholar]
- 14.Andersen R. A behavioral model of families' use of health services. [Chicago]: Center for Health Administration Studies, University of Chicago; 1968. Available from: https://www.worldcat.org/title/behavioral-model-of-families-use-of-health-services/oclc/475040. Accessed September 16, 2021. [Google Scholar]
- 15.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi: 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- 16.Zhang A, Nikoloski Z, Mossialos E. Does health insurance reduce out-of-pocket expenditure? Heterogeneity among China’s middle-aged and elderly. Soc Sci Med. 2017;190:11–19. doi: 10.1016/j.socscimed.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 17.Mucci N, Traversini V, Giorgi G, et al. Migrant workers and physical health: an umbrella review. Sustainability. 2019;11(1):232. doi: 10.3390/su11010232 [DOI] [Google Scholar]
- 18.Peng BL, Ling L. Association between rural-to-urban migrants’ social medical insurance, social integration and their medical return in China: a nationally representative cross-sectional data analysis. BMC Public Health. 2019;19(1):86. doi: 10.1186/s12889-019-6416-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X, Yu B, He T, Wang P. Status and determinants of health services utilization among elderly migrants in China. Global Health Res Policy. 2018;3:8. doi: 10.1186/s41256-018-0064-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xi S, Song Y, Li X, et al. Local-migrant gaps in healthcare utilization between older migrants and local residents in China. J Am Geriatr Soc. 2020;68(7):1560–1567. doi: 10.1111/jgs.16421 [DOI] [PubMed] [Google Scholar]
- 21.Leive A, Xu K. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86(11):849–856C. doi: 10.2471/BLT.07.049403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Facione NC, Miaskowski C, Dodd MJ, Paul SM. The self-reported likelihood of patient delay in breast cancer: new thoughts for early detection. Prev Med. 2002;34(4):397–407. doi: 10.1006/pmed.2001.0998 [DOI] [PubMed] [Google Scholar]
- 23.Lefler LL, Bondy KN. Women’s delay in seeking treatment with myocardial infarction: a meta-synthesis. J Cardiovasc Nurs. 2004;19(4):251–268. doi: 10.1097/00005082-200407000-00005 [DOI] [PubMed] [Google Scholar]
- 24.Betti R, Vergani R, Tolomio E, Santambrogio R, Crosti C. Factors of delay in the diagnosis of melanoma. Eur J Dermatol. 2003;13(2):183–188. [PubMed] [Google Scholar]
- 25.Montella M, Crispo A, Botti G, et al. An assessment of delays in obtaining definitive breast cancer treatment in Southern Italy. Breast Cancer Res Treat. 2001;66(3):209–215. doi: 10.1023/A:1010622909643 [DOI] [PubMed] [Google Scholar]
- 26.Cai X, Yang F, Bian Y. Gap analysis on hospitalized health service utilization in floating population covered by different medical insurances —– case study from Jiangsu Province, China. Int J Equity Health. 2019;18(1):84. doi: 10.1186/s12939-019-0992-4 [DOI] [PMC free article] [PubMed] [Google Scholar]