To the Editor
More than two thirds of global cancer deaths occur in LMICs due in part to delayed diagnosis and lack of access to specialized staff, chemotherapy and radiation.(Livingston, 2013) Cutaneous malignancies are common and morbid in LMICs, particularly for people living with HIV.(Bray et al., 2018, McMahon et al., 2020) People living with HIV develop more AIDS-defining and non-AIDS defining skin cancers compared to the general population, including Kaposi sarcoma (KS), human papillomavirus (HPV)-associated squamous cell carcinomas, cutaneous lymphoma, keratinocyte carcinomas and melanoma.(Chelidze et al., 2019, Jaquet et al., 2015, WHO, 2014) KS in particular continues to be the leading cause of cancer incidence and mortality across the general population of Malawi, Mozambique, Uganda, and Zambia.(Bray et al., 2018) Although the majority of people living with HIV reside in LMICs – including 25.6 million people in sub-Saharan Africa – little is known about LMIC capacity to diagnose and manage skin cancers.(Kingham et al., 2013)
To address this question, we conducted a cross-sectional study using The International epidemiology Databases to Evaluate AIDS (IeDEA) non-communicable diseases (NCD) site assessment survey to identify gaps in skin cancer diagnostic and therapeutic services at HIV treatment centers across LMICs. We distributed the survey to a stratified random sample of HIV treatment centers participating in IeDEA from 2016–2017. For this analysis, we report the availability of diagnostics, therapeutics, and staffing required to diagnose and treat most cutaneous malignancies (Supplementary Appendix).
Of 162 HIV treatment sites approached to participate, 86 completed the survey (53%). The most common reasons for survey non-completion included sites no longer participating in IeDEA (56%) and sites which suspended operations or closed (26%). Nine replacement sites were selected from the original sampling frame based on sample size calculations for the parent study, resulting in 95 sites included for analysis.(Parcesepe et al., 2018) Sites were distributed across six geographic regions representing 29 countries. Sites were primarily urban (80%), public (88%), and in sub-Saharan Africa (62%) (Supplemental Table 1).
Using a care cascade model, we found that 18% of sites in low and lower-middle income countries and 64% of sites in upper-middle income countries had the requisite diagnostics and therapeutics to offer diagnosis and treatment for an advanced skin malignancy (Figure 1). Differences in availability of skin cancer services were noted across level of health facility and country income level (Table 1). For example, combined skin biopsy and histopathology availability was 27% for HIV centers and associated health facilities in low and lower-middle income countries, contrasted with 82% in upper-middle income countries.
Figure 1:
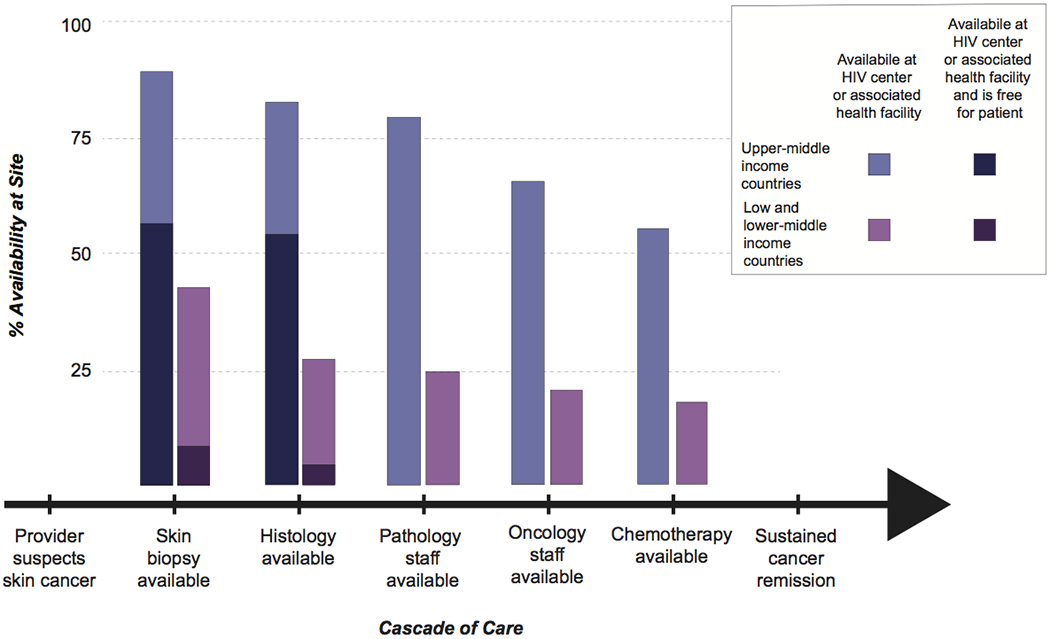
Cascade of care for patients with skin cancer in low and middle income countries, depicting potential losses of patients over time from provider first suspecting skin cancer to the patient achieving sustained cancer remission. For diagnostic tests only, the cost to the patient is depicted.
Table 1.
Availability diagnostic, therapeutic and staffing resources for HIV treatment sites stratified by level of healthcare facility and World Bank classified country income level.
| Overall | Level of Health Facility | Country Income Level | Free for Patient¶ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| % Availability§, (95% CI) | n=95 | Health Center (n=32) | District Hospital (n=10) | Tertiary Hospital* (n=53) | P Value† | Low Income (n=25) | Lower Middle Income (n=42) | Upper Middle Income (n=28) | P Value† | |
| Diagnostics | ||||||||||
|
| ||||||||||
| Skin Biopsy | 57% (46-70) | 19% (7.2-36) | 50% (19-81) | 81% (68-91) | <.001 | 48% (28-69) | 40% (26-57) | 89% (72-98) | <.001 | 37% (24-51) |
| Histopathology | 45% (35-56) | 16% (5.3-33) | 20% (5.3-33) | 68% (54-80) | <.001 | 20% (6.8-41) | 36% (22-52) | 82% (63-94) | <.001 | 33% (19-49) |
| Biobank | 47% (37-58) | 34% (19-53) | 20% (2.5-56) | 60% (46-74) | .01 | 56% (35-76) | 31% (18-47) | 64% (44-81) | .014 | 40% (25-57) |
| Endoscopy/ Colonoscopy | 42% (32-53) | 13% (3.5-29) | 10% (0.25-45) | 66% (52-78) | <.001 | 24% (9.4-45) | 24% (12-39) | 86% (67-96) | <.001 | 44% (30-58) |
| Fine needle aspiration/ Lymph node biopsy | 58% (47-68) | 22% (9.3-40) | 40% (12-74) | 83% (70-92) | <.001 | 52% (31-72) | 40% (26-57) | 89% (72-98) | <.001 | 45% (30-58) |
| Abdominal ultrasound | 79% (69-87) | 50% (32-68) | 80% (44-97) | 96% (87-100) | <.001 | 72% (51-88) | 73% (58-86) | 93% (76-99) | .08 | 40% (29-52) |
| Chest X-Ray | 82% (73-89) | 59% (41-76) | 80% (44-97) | 96% (87-100) | <.001 | 76% (55-91) | 76% (61-88) | 96% (82-100) | .05 | 50% (38-62) |
| Other X-Ray | 76% (66-84) | 50% (32-68) | 70% (35-93) | 92% (82-98) | <.001 | 68% (47-85) | 67% (50-80) | 96% (82-100) | .004 | 37% (26-49) |
| CT Scan‡ | 54% (43-64) | 25% (11-43) | 20% (2.5-56) | 77% (64-88) | <.001 | 36% (18-57) | 38% (24-54) | 93% (76-99) | <.001 | 39% (26-54) |
| MRI | 47% (37-58) | 19% (7.2-36) | 20% (2.5-56) | 70% (56-82) | <.001 | 24% (9.3-45) | 33% (20-50) | 89% (72-98) | <.001 | 36% (22-51) |
|
| ||||||||||
| Therapeutics | ||||||||||
|
| ||||||||||
| Chemotherapy | 36% (26-46) | 16% (5.3-33) | 10% (0.25-45) | 53% (39-67) | <.001 | 24% (9.4-45) | 19% (8.6-34) | 71% (51-87) | <.001 | - |
| Radiation | 20% (12-29) | 9.4% (2.0-25) | 10% (0.25-45) | 28% (17-42) | <.001 | 4% (0.1-20) | 14% (5.4-29) | 43% (24-63) | .001 | - |
| Morphine | 51% (40-61) | 19% (7.2-36) | 60% (26-88) | 68% (54-80) | <.001 | 48% (28-69) | 38% (24-54) | 71% (51-87) | .02 | - |
|
| ||||||||||
| Staffing | ||||||||||
|
| ||||||||||
| Oncology staff | 43% (33-54) | 16% (5.3-33) | 30% (6.7-65) | 62% (48-75) | <.001 | 28% (12-49) | 31% (18-47) | 75% (55-89) | <.001 | - |
| Pathology staff | 44% (34-55) | 13% (3.5-29) | 10% (56-82) | 70% (56-82) | <.001 | 24% (9.4-45) | 31% (18-47) | 82% (63-94) | <.001 | - |
Availability defined as presence at the HIV treatment site itself or within the associated health facility
Tertiary hospital defined as regional, provincial, or university hospital
Chi square tests or Fisher exact tests used to calculate all P values
CT scan either with or without contrast
Only calculated if diagnostic test was available at the HIV treatment site itself or within the same health facility. Value was not available for therapeutics or staffing.
Skin biopsy was free of charge at 25% of public and 9% of private sites; histopathology was free at 21% of public and no private sites. Disparities in diagnostic capacity extended to additional skin cancer tests and tended to be more extreme for costly diagnostics; for example, ultrasound had greater availability compared to MRI. Pathology and oncology staff were available at 44% and 43% of sites respectively, with 36% of sites having chemotherapy available and 20% of sites radiation.
Our results may partially explain the advanced stage at diagnosis and poor outcomes reported for people living with HIV diagnosed with cutaneous malignancies in LMICs.(Kingham et al., 2013, McMahon et al., 2020) Lack of biopsy availability for skin cancer diagnosis means that i) cancer diagnosis can be missed and ii) patients who are diagnosed with skin cancer on clinical grounds alone may be given chemotherapy and radiation inappropriately.(Freeman et al., 2020) Furthermore, even when skin biopsy and histopathology were available, few centers in LMICs offered these services free of charge, especially in the private sector.
Prior studies have similarly demonstrated limited oncology and pathology staff in LMICs (Adesina et al., 2013) Less is known about the number of dermatologists practicing in LMICs, but is likely to be even scarcer given the limited number of dermatology specialty training programs especially across sub-Saharan Africa.(Seth et al., 2020)
Lack of non-communicable disease care is a continued challenge in global health, where the majority of funding is infectious diseases driven.(Rajbhandari et al., 2020) Because many LMICs already have a robust network of HIV facilities, these vertical service delivery models could be harnessed to improve non-communicable disease control both for people living with HIV and the broader population.(Hyle et al., 2014)
While this study is most generalizable to sites treating people living with HIV, we also believe that this survey may approximate skin cancer service availability for the general population in LMICs. The majority of our HIV treatment sites were based at tertiary hospitals (56% of sites) and district hospitals (11% of sites), so survey responses characterize the health services available to the population at that site generally, not just in the HIV clinic.(Rajbhandari et al., 2020) Therefore, our results also suggest limited access to skin cancer diagnostics and therapeutics for the general population.(Hyle et al., 2014)
Study limitations include limited sample size of 95 HIV treatment sites and selection bias for HIV treatment centers participating in IeDEA, which requires clinics to have robust data collection abilities and therefore represents highly functional clinics.(Parcesepe et al., 2018) Additionally, our survey response rate was low at 53%, often due to HIV treatment sites no longer participating in IeDEA, reflecting broader challenges in longitudinally collecting HIV data in resource-limited settings. All sites were asked whether services were “available” rather than whether or not they were actually being performed. The modality of skin biopsy was not specified, which has important implications for feasibility and cost. For example, an “available” skin biopsy could mean sporadic excisional biopsies performed by a surgeon at high cost.(Laker-Oketta et al., 2015, Seth et al., 2020). Due to these limitations, our results likely depict the best-case scenario for skin cancer service availability in LMICs.
This study highlights disparities in skin cancer supplies and staffing across country income levels and levels of health facility. Investment in cancer diagnostics at health facilities will be an important step in reducing the burden of advanced stage cancers in LMICs.
Supplementary Material
Acknowledgments
Funding: National Institutes of Health (U01AI069911, K23 AI136579, U54 CA190153) and the Dermatology Foundation. The International Epidemiology Databases to Evaluate AIDS (IeDEA) is supported by the U.S. National Institutes of Health’s National Institute of Allergy and Infectious Diseases, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Cancer Institute, the National Institute of Mental Health, the National Institute on Drug Abuse, the National Heart, Lung, and Blood Institute, the National Institute on Alcohol Abuse and Alcoholism, the National Institute of Diabetes and Digestive and Kidney Diseases, the Fogarty International Center, and the National Library of Medicine: Asia-Pacific, U01AI069907; CCASAnet, U01AI069923; Central Africa, U01AI096299; East Africa, U01AI069911; NA-ACCORD, U01AI069918; Southern Africa, U01AI069924; West Africa, U01AI069919. Informatics resources are supported by the Harmonist project, R24AI124872. This work is solely the responsibility of the authors and does not necessarily represent the official views of any of the institutions mentioned above.
Footnotes
Conflicts of Interest: The authors state they have no conflicts of interest.
Ethical Considerations: All study sites and their respective IeDEA coordinating centers had Institutional Review Board approvals that permitted collection of site-level data for the study. The Partners Healthcare human research committee/IRB determined this site-level data did not meet the definition of human subjects research.
Data Availability Statement: The data that support the findings of this study are available from the International epidemiology Databases to Evaluate AIDS (IeDEA) which follows the National Institutes of Health data sharing policy. Data can be requested through IeDEA (www.iedea.org).
References
- Regional factsheets 2018. UNAIDS. https://aidsinfo.unaids.org/ (accessed February 23, 2020). [accessed. [Google Scholar]
- Adesina A, Chumba D, Nelson AM, Orem J, Roberts DJ, Wabinga H, et al. Improvement of pathology in sub-Saharan Africa. Lancet Oncol 2013;14(4):e152–7. [DOI] [PubMed] [Google Scholar]
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018. [DOI] [PubMed] [Google Scholar]
- Chelidze K, Thomas C, Chang AY, Freeman EE. HIV-Related Skin Disease in the Era of Antiretroviral Therapy: Recognition and Management. Am J Clin Dermatol 2019;20(3):423–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman EE, McMahon DE, Laker-Oketta M. Time to address disparities in the standard of care for Kaposi sarcoma. Lancet 2020;395(10231):1169–70. [DOI] [PubMed] [Google Scholar]
- Hyle EP, Naidoo K, Su AE, El-Sadr WM, Freedberg KA. HIV, tuberculosis, and noncommunicable diseases: what is known about the costs, effects, and cost-effectiveness of integrated care? J Acquir Immune Defic Syndr 2014;67Suppl 1:S87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaquet A, Odutola M, Ekouevi DK, Tanon A, Oga E, Akakpo J, et al. Cancer and HIV infection in referral hospitals from four West African countries. Cancer Epidemiol 2015;39(6):1060–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingham TP, Alatise OI, Vanderpuye V, Casper C, Abantanga FA, Kamara TB, et al. Treatment of cancer in sub-Saharan Africa. Lancet Oncol 2013;14(4):e158–67. [DOI] [PubMed] [Google Scholar]
- Laker-Oketta MO, Wenger M, Semeere A, Castelnuovo B, Kambugu A, Lukande R, et al. Task Shifting and Skin Punch for the Histologic Diagnosis of Kaposi’s Sarcoma in Sub-Saharan Africa: A Public Health Solution to a Public Health Problem. Oncology 2015;89(1):60–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston J Cancer in the shadow of the AIDS epidemic in southern Africa. Oncologist 2013;18(7):783–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon DE, Maurer T, Freeman EE. 25 Years of Kaposi Sarcoma Herpesvirus: Discoveries, Disparities, and Diagnostics. JCO Glob Oncol 2020;6:505–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parcesepe AM, Mugglin C, Nalugoda F, Bernard C, Yunihastuti E, Althoff K, et al. Screening and management of mental health and substance use disorders in HIV treatment settings in low- and middle-income countries within the global IeDEA consortium. Journal of the International AIDS Society 2018;21(3):e25101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajbhandari R, McMahon DE, Rhatigan JJ, Farmer PE. The Neglected Hospital - The District Hospital’s Central Role in Global Health Care Delivery. N Engl J Med 2020;382(5):397–400. [DOI] [PubMed] [Google Scholar]
- Seth D, Williams VL, McMahon DE, Regan S, Busakhala N, Wools-Kaloustian K, et al. The role of dermatology in Kaposi sarcoma diagnosis across three regions in sub-Saharan Africa. J Am Acad Dermatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Guidelines on the treatment of skin and oral HIV-associated conditions in children and adults, https://www.who.int/maternal_child_adolescent/documents/skin-mucosal-and-hiv/en/2014. [accessed January 9.2021]. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


