Abstract
Purpose:
To estimate the prevalence, patterns, and correlates of self-reported nicotine dependence symptoms among U.S. youth who use JUUL - a widely-sold e-cigarette brand - in 2019 and compare findings to nicotine dependence symptoms in youth who smoke cigarettes.
Methods:
Data were from a nationally-representative subsample of 8th, 10th, and 12th grade students in the Monitoring the Future Study who had used JUUL or cigarettes in the past 30 days. Participants self-reported presence/absence of 9 different nicotine dependence symptoms for JUUL or cigarettes. Weighted percentages for JUUL or cigarette nicotine dependence symptom status (≥1 vs. 0 symptoms) and severity (count, range: 0–9) were calculated. Among JUUL users, we estimated associations of sociodemographic characteristics and other substance use with nicotine dependence and severity.
Results:
Among 1,748 past 30-day JUUL users, 41.3% screened positive for ≥1 nicotine dependence symptoms; the mean symptom count was 1.6 (SD=2.6). Non-nicotine substance use and more frequent JUUL use was associated with significantly greater odds of dependence and more severe dependence symptoms in multivariable models. The severity distribution of most (craving) and least (inability to quit) dependence symptom types observed in JUUL dependence paralleled those observed in analysis of combustible cigarette dependence symptoms in past 30-day smokers.
Conclusion:
A substantial proportion of U.S. adolescent JUUL users reported symptoms of nicotine dependence, which is greater for those who vape more frequently and use other substances. Nicotine dependence screening, prevention, and regulatory policies addressing use of JUUL or similar e-cigarette products should be considered to protect U.S. youth.
Keywords: adolescent, e-cigarette, JUUL use, nicotine dependence
INTRODUCTION
E-cigarette use (i.e., nicotine vaping) among U.S. youth has been declared a public health crisis (Walley et al., 2019). In 2019, 6.9% and 11.7% of 10th and 12th grade U.S. students, respectively, currently vaped nicotine on a daily basis, raising concerns about whether nicotine dependence is widespread in adolescents (Miech et al., 2019)
JUUL—the most commonly used e-cigarette brand among U.S. youth in 2019—was the first company to market pod-style e-cigarettes. Pod-style e-cigarettes are characterized by their small size, resemblance of a computer USB drive, and compatibility with cartridges (i.e., “pods”) that contain solutions with high concentrations of nicotine in a protonated salt chemical form (i.e., “nicotine salt” formulations; Barrington-Trimis & Leventhal, 2018). Compared to standard free-base nicotine e-cigarettes, e-cigarettes with nicotine salt formulations are believed to emit aerosol that is less harsh and easier to inhale (Duell et al., 2018; Goniewicz et al., 2019; Jackler & Ramamurthi, 2019), which could increase the risk of nicotine dependence (Jackler & Ramamurthi, 2019).
Prior research of regional samples of adolescent e-cigarette users suggest that nicotine dependence is higher among subsets of youth who use JUUL or other e-cigarettes with high nicotine concentrations or pod-based systems (Boykan et al., 2019; Case et al., 2020; Morean et al., 2018). Recent nationally-representative estimates of the prevalence and severity of nicotine dependence among youth who use JUUL are lacking. Such evidence may provide insight regarding the potential for nicotine dependence among users of JUUL or other e-cigarettes with high concentrations of nicotine in nicotine salt formulations. The types of symptoms and key correlates (e.g., sociodemographic characteristics and other substance use) of nicotine dependence in youth JUUL users are unknown, which is important for characterizing nicotine dependence syndrome and subpopulations at greatest risk.
The current study estimated the prevalence, severity, and correlates of self-reported nicotine dependence symptoms in JUUL users among U.S. youth in 2019. The association of JUUL use frequency with nicotine dependence and severity was also examined to determine whether a characteristic association was observed for dose of exposure with dependence risk, as has been observed for other drugs of abuse. To further place the findings in context, a comparison analysis was used to estimate the prevalence and correlates of nicotine dependence among youth who used combustible cigarettes, a tobacco product with high dependence potential (Rose, 2006).
METHODS
Participants and Procedures
Data are from the 2019 Monitoring the Future (MTF) study, which uses self-administered questionnaires to annually survey a nationally representative sample of U.S. 8th-grade, 10th-grade, and 12th-grade students (Miech et al., 2020). By design, one-third of students from each grade were randomly selected for the JUUL module. The analytic sample included those administered the module who reported past 30-day JUUL use with nicotine dependence data (N=1,748). A randomly-assigned one-third of students were also selected to receive a cigarette smoking module, among whom past 30-day cigarette smokers with cigarette nicotine dependence data constituted the sample for the comparison analysis (N=437); this sample was partially overlapping with the youth receiving the JUUL module. Students provided assent; active written or passive parental informed consent was collected per each school’s policies. Surveys were self-administered in classrooms via tablets, yielding response rates of 89.5%, 87.4%, and 82.5% for 8th, 10th, and 12th grade students, respectively. The University of Michigan Institutional Review Board approved this study.
Measures
Past 30-day JUUL or Cigarette Use.
Participants who reported vaping in the past 30 days completed a survey item asking how many days in the past 30 days they used a JUUL: 0, 1–2, 3–5, 6–9, 10–19, or ≥20 days. Participants reporting smoking cigarettes in the past 30 days were asked how many cigarettes they smoked in the past 30-days on smoking days: none, ≤1 cigarette per day, 1–5 cigarettes per day, ½ pack per day, 1 pack per day, 1.5 packs per day, or ≥2 packs per day.
Nicotine Dependence Symptoms.
Two parallel 9-item adapted versions of the Hooked on Nicotine Checklist (HONC; Wheeler et al., 2004) were administered to assess nicotine dependence symptoms. One version measured symptoms experienced from use of JUUL, whereas the other measured symptoms from combustible cigarette smoking. In both versions, the following 9 symptoms (yes/no) were identically worded expect for the substitution of "JUUL” and “cigarette” terms: “Have you ever tried to quit using (JUUL/cigarettes), but couldn’t?”; “Do you use (JUUL/cigarettes) now because it is really hard to quit?”; “Have you ever felt like you were addicted to (JUUL/cigarettes)?”; “Do you ever have strong cravings to use (JUUL/cigarettes)?”; “Is it hard to keep from using (JUUL/cigarettes) in places where you are not supposed to?”; “Did you find it hard to concentrate because you couldn’t use (JUUL/cigarettes)?”; “Did you feel more irritable because you couldn’t use (JUUL/cigarettes)?”; “Did you feel a strong need or urge to use (JUUL/cigarettes)?”; “Did you feel nervous, restless or anxious because you couldn’t use (JUUL/cigarettes)?” As in prior research (Vogel, Cho, et al., 2020; Wheeler et al., 2004). participants who indicated ≥1 symptoms were classified as screening positive for dependence symptoms; total number of symptoms were tallied as a severity estimate (range: 0–9). Previous research of youth e-cigarette users has demonstrated that the HONC evidences adequate convergent and predictive validity (Vogel, Cho, et al., 2020).
Demographic Characteristics and Substance Use.
Sociodemographic information was collected for gender (male/female), grade (8th, 10th, 12th), race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Other), parental education (no college degree/college degree) via self-report; population density (rural, suburban, large city), and region (Northeast, Midwest, South, West) of school location were collected via census data. Participants reported past 30-day use of any other nicotine substances (smokeless tobacco, cigars/cigarillos, or hookah tobacco; yes/no) and other non-nicotine substances (alcohol, cannabis, or other drugs [inhalants, hallucinogen, LSD, cocaine, crack, heroin, opioids, barbiturates, tranquilizers, methamphetamine]; range: 0 – 3).
Statistical Analyses
After descriptive analyses, we calculated the prevalence (unweighted n, and weighted %± 95% CI) of nicotine dependence symptom positive screens (yes/no), symptom severity (Range=0–9), and individually for each of the 9 different dependence symptoms for JUUL users. We also report prevalence of those screening positive for JUUL dependence in the larger overall sample of MTF students to provide base rate estimates in the general population. For comparative purposes, parallel analyses were performed with responses to the HONC for cigarette smoking, among past-30-day cigarette smokers. Multivariable regression models were used to evaluate the association of sociodemographic and substance use variables with nicotine dependence (logistic regression) and severity (negative binomial regression), including all items as simultaneous regressors. Results are reported as odds ratios (ORs) or rate ratios (RRs) with 95% confidence intervals (95% CIs). All analyses were conducted in Mplus version 8 (Muthén & Muthén, 1998–2017). Full information maximum likelihood estimating to account for missing data, and complex analyses were conducted using the cluster variable (astrat: Stratum for single or multiple year analysis). Benjamini-Hochberg multiple-testing corrections (Benjamini & Hochberg, 1995) were applied to regression estimates to control the false-discovery rate at 0.05 (based on two-tailed corrected p-value).
RESULTS
Study Sample
Among all 42,531 MTF respondents, a randomly-selected 14,191(33.4%) were eligible to receive the JUUL module, of whom 1,779 (12.5%) reported past 30-day use of JUUL. After eliminating 31 students who did not complete JUUL dependence symptom items, the analytic sample included 1,748 past 30-day JUUL users with valid nicotine dependence symptom data (n=333 8th graders; n=722 10th graders; n=693 12th graders). Sample characteristics (50.1% female; 64.3% Non-Hispanic White; 11.1% Hispanic; 4.8% Non-Hispanic Black; 19.8% Other race/ethnicity) are depicted in the left column of Table 1. Descriptive data on the comparison sample of past 30-day cigarette smokers (N=437) are reported in Supplementary Table 1.
Table 1.
Sample Descriptive Statistics and Nicotine Dependence Symptoms in JUUL Users, by Participant Characteristicsa
| Variable | Sample Characteristics N, Column %b | Any dependence symptoms | Total no. of dependence symptoms | ||
|---|---|---|---|---|---|
| Row % (95% CI)b | P-Valuec | Row Mean (95% CI)b | P-Valuec | ||
| Overall Sample | 1748, 100% | 41.3% (39.0, 43.7) | N/A | 1.61 (1.49, 1.74) | N/A |
| Sociodemographics | |||||
| Grade | |||||
| 8th | 333, 18.2% | 44.7% (39.1, 50.2)1 | .37 | 1.77 (1.46, 2.07)1 | .42 |
| 10th | 722, 40.9% | 40.0% (36.3, 43.6)1 | 1.54 (1.34, 1.73)1 | ||
| 12th | 693, 40.9% | 41.2% (37.6, 44.9)1 | 1.62 (1.43, 1.82)1 | ||
| Gender | |||||
| Female | 880, 50.1% | 39.6% (36.3, 42.9) | .21 | 1.67 (1.49, 1.85) | .39 |
| Male | 849, 49.9% | 42.6% (39.3, 45.9) | 1.56 (1.39, 1.74) | ||
| Race/Ethnicity | |||||
| Non-Hispanic White | 1092, 64.3% | 42.6% (39.6, 45.5)1 | .42 | 1.68 (1.52, 1.84)1 | .22 |
| Non-Hispanic Black | 89, 4.8% | 39.7% (28.8, 50.5)1 | 1.45 (0.87, 2.03)1,2 | ||
| Hispanic | 185, 11.1% | 36.8% (29.8, 43.9)1 | 1.26 (0.93, 1.59)2 | ||
| Othersd | 344, 19.8% | 39.4% (34.1, 44.7)1 | 1.63 (1.34, 1.91)1,2 | ||
| Population Density | |||||
| Rural | 487, 26.7% | 38.7% (24.2, 43.1)2 | .06 | 1.54 (1.30, 1.78)1 | .66 |
| Suburban | 723, 51.0% | 40.5% (37.2, 43.7)2 | 1.67 (1.49, 1.85)1 | ||
| Large city | 538, 22.3% | 46.5% (41.5, 51.5)1 | 1.57 (1.33, 1.81)1 | ||
| Region | |||||
| Northeast | 285, 14.4% | 41.2% (35.0, 47.4)1,2 | .11 | 1.71 (1.37, 2.06)12 | .03 |
| Midwest | 497, 30.7% | 40.8% (36.5, 45.0)1,2 | 1.60 (1.37, 1.82)12 | ||
| South | 719, 36.5% | 38.9% (35.1, 42.8)2 | 1.42 (1.23, 1.61)2 | ||
| West | 247, 18.4% | 47.2% (41.6, 52.7)1 | 1.95 (1.64, 2.26)1 | ||
| Parental education level | |||||
| No college degree | 655, 40.6% | 39.4% (35.7, 43.2) | .15 | 1.46 (1.27, 1.65) | .03 |
| College degree | 1001, 56.1% | 43.0% (39.9, 46.2) | 1.74 (1.57, 1.92) | ||
| Nicotine dependence | |||||
| Combustible cigarette dependence symptoms | |||||
| None | 100, 41.4% | 36.2% (26.9, 45.5) | .003 | 1.40 (0.93, 1.86) | <.001 |
| 1 or more symptoms | 116, 58.6% | 55.0% (46.8, 62.9) | 3.15 (2.56, 3.73) | ||
| Past 30-day substance use | |||||
| Combustible cigarettes | |||||
| No | 1529, 84.9% | 40.3% (37.8, 42.8) | .04 | 1.47 (1.35, 1/j) | <.001 |
| Yes | 216, 14.9% | 47.1% (40.9, 53.3) | 2.42 (2.02, 2.83 ) | ||
| Other tobacco productse | |||||
| No | 1140, 82.2% | 39.0% (36.1, 41.9) | .04 | 1.40 (1.26, 1.54) | <.001 |
| Yes | 245, 17.8% | 46.1% (39.8, 52.5) | 2.38 (1.96, 2.80) | ||
| No. alcohol/cannabis/other drugsf | |||||
| 0 | 384, 23.3% | 29.0 (24.5, 33.5)4 | <.001 | 0.94 (0.75, 1.14)3 | <.001 |
| 1 | 669, 37.4% | 38.5 (34.7, 42.2)3 | 1.46 (1.26, 1.65)2 | ||
| 2 | 548, 30.4% | 49.1 (44.7, 53.4)2 | 2.6 (1.81, 2.30)1 | ||
| 3 | 147, 9.0% | 59.3 (51.4, 67.2)1 | 2.52 (2.03, 3.01)1 | ||
| JUUL | |||||
| 1–2 days | 579, 32.8% | 23.0% (19.5, 26.5)4 | <.001 | 0.76 (0.61, 0.91)3 | <.001 |
| 3–5 days | 302, 17.4% | 38.3% (32.7, 43.8)3 | 1.19 (0.94, 1.43)2 | ||
| 6–9 days | 211, 11.8% | 38.3% (31.5, 45.0)3 | 1.23 (0.93, 1.52)2 | ||
| 10–19 days | 175, 9.3% | 52.5% (44.6, 60.4)2 | 1.45 (1.12, 1.78)2 | ||
| 20 or more days | 481, 28.6% | 61.9% (57.6, 66.2)1 | 3.07 (2.78, 3.36)1 | ||
Note. Overall sample N=1748; participants ≥1 Juul dependence symptoms: Unweighted N = 735 / Weighted % = 41.3%
Past 30-day JUUL users. Available data ranges across variables (NS=1385–1748).
Unweighted frequency (N) and weighted percentage (%) are reported.
Calculated using one-way Analysis of Variance (ANOVA). Groups not sharing superscript numerals are significantly different in estimated prevalence from ANOVA Least Significant Difference tests.
Other race/ethnicity includes Asian and multiracial groups.
Indudes smokeless tobacco, cigars/cigarillos, and hookah tobacco.
Total number of substance classes used (alcohol, cannabis, or other drugs [inhalants, hallucinogen, LSD, cocaine, crack, heroin, opioids, barbiturate drugs, tranquilizer drugs, methamphetamine]).
Prevalence and Severity of Nicotine Dependence Symptoms in JUUL Users and Comparison Sample of Combustible Cigarette Users
Among past 30-day JUUL users, 41.3% (95% CI: 39.0, 43.7) of students screened positive for nicotine dependence (i.e., ≥1 symptoms), amounting to 5.2% of all MTF students eligible for the JUUL module. The prevalence of any nicotine dependence among JUUL past-30-day users did not vary appreciably by grade; among 8th, 10th, and 12th grade past 30-day JUUL users, the prevalence of dependence was 44.7%, 40.0%, and 41.2%, respectively. The distribution of JUUL dependence symptom scores (range: 0–9) was positively skewed (Figure 1) and the mean symptom count was 1.61 (SD=2.62). Craving (29.0%) and feeling addicted (26.5%) were the most commonly reported symptoms, while inability to concentrate while abstinent (12.3%) and difficulty quitting (10.9%) were the least common (Figure 2).
Figure 1.
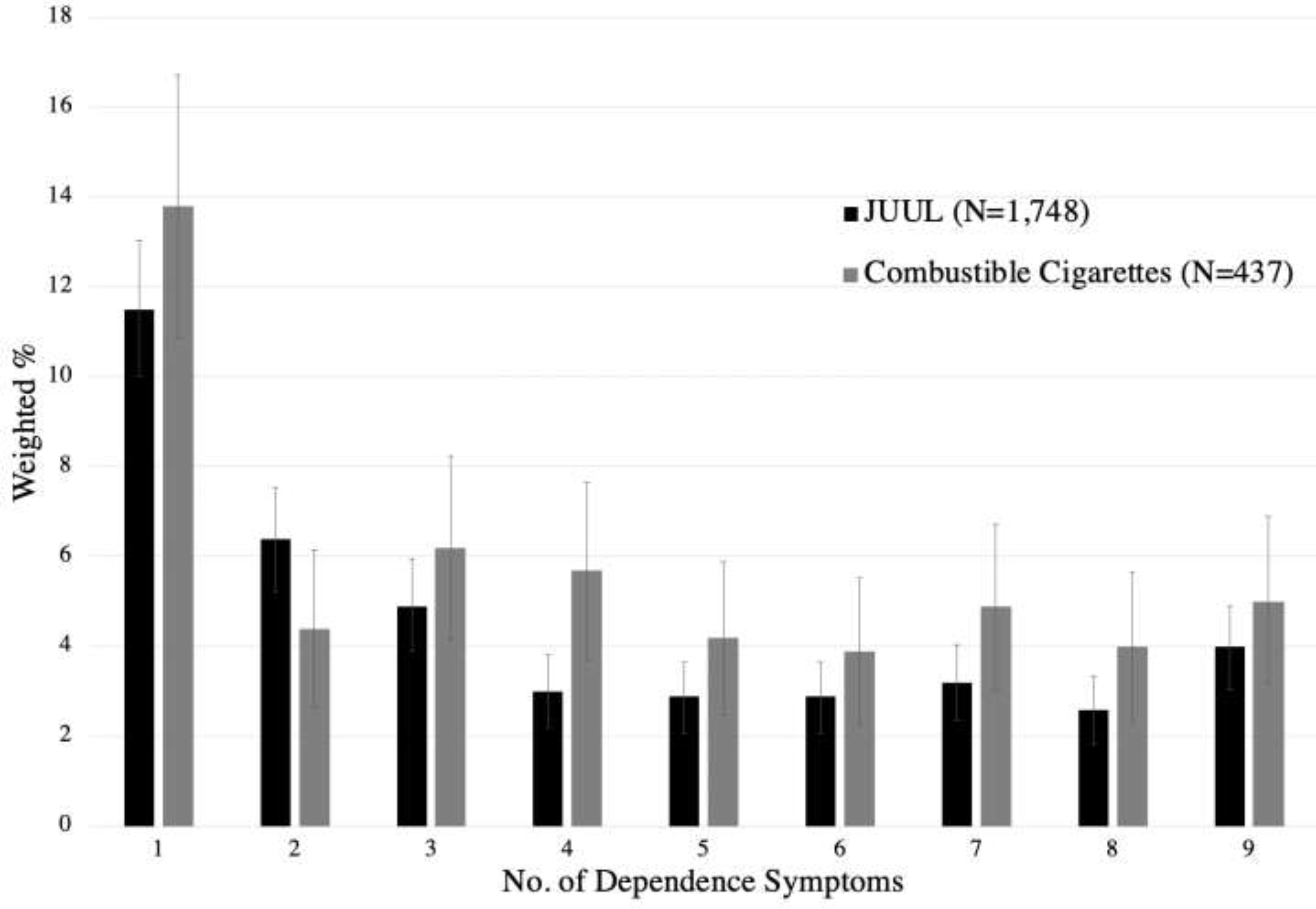
Distribution of JUUL and Cigarette Dependence Symptom Severity Scores
Note. Unweighted Ns for JUUL, stratified by number of symptoms: 0=1013, 1=206, 2=113, 3=87, 4=57, 5=54, 6=53, 7=49, 8=39, 9=77
Unweighted Ns for Combustible Cigarettes: 0=217, 1=60, 2=27, 3=23, 4=21, 5=19, 6=15, 7=19, 8=15, 9=21
Error bars indicate 95% confidence intervals calculated using the estimated prevalence of one-sample t-test.
Figure 2.
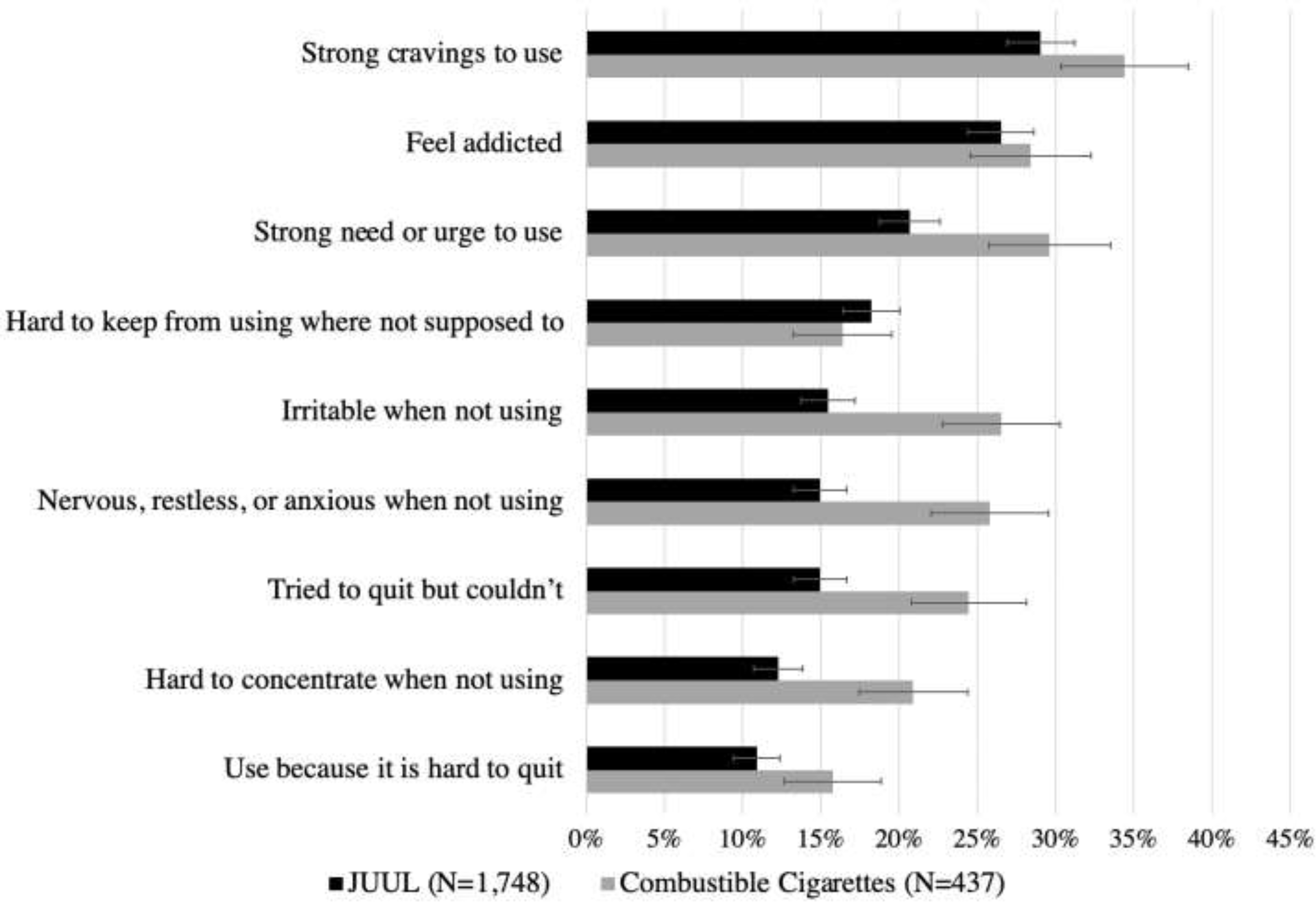
Prevalence of Types of Nicotine Dependence Symptoms Experienced among JUUL and Combustible Cigarette Users
Note. Error bars indicate 95% confidence intervals calculated using the estimated prevalence of one-sample t-test.
In the comparison sample of past 30-day cigarette smokers, 52.1% (95% CI: 47.8, 56.3) screened positive for nicotine dependence symptoms and the mean symptom count was 2.20 (SD=2.91). The symptom count distribution and ordering of the prevalence of symptom types followed similar patterns observed with JUUL; however, several prevalence estimates were higher for cigarettes than JUUL (see Figures 1–2).
Correlates of Nicotine Dependence Symptoms from JUUL Use
Sociodemographics.
Among past 30-day JUUL users, lower JUUL prevalence and severity was observed among past 30-day users who were in 10th or 12th (vs. 8th) grade; JUUL prevalence and severity was higher in females vs. males (Table 2). No other associations were statistically significant.
Table 2.
Association of Sociodemogra phic and substance Use with Nicotine Dependence Symptoms in JUUL Users
| Regressors | Any dependence symptoms | Total no. of dependence symptoms | ||
|---|---|---|---|---|
| Odds Ratio (95% CI)a,c | P-Value | Risk Ratio (95% CI)b,c | P-Value | |
| Sociodemographics | ||||
| Grade | ||||
| 8th | REF | -- | REF | -- |
| 10th | 0.55 (0.37, 0.81) | .002* | 0.64 (0.47, 0.87) | .004* |
| 12th | 0.57 (0.39, 0.83) | .003* | 0.60 (0.45, 0.80) | <.001* |
| Female (male REF) | 1.29 (1.05, 1.59) | .02* | 1.11 (0.93, 1.32) | .26 |
| Race/Ethnicity | ||||
| Non-Hispanic White | REF | -- | REF | -- |
| Non-Hispanic Black | 1.01 (0.56, 1.83) | .98 | 0.83 (0.56, 1.24) | .37 |
| Hispanic | 0.77 (0.52, 1.13) | .18 | 0.86 (0.63, 1.16) | .33 |
| Othersd | 0.74 (0.52, 1.06) | .10 | 0.89 (0.66, 1.19) | .42 |
| Population Density | ||||
| Rural | REF | -- | REF | -- |
| Suburban | 0.98 (0.78, 1.24) | .87 | 1.02 (0.82, 1.27) | .85 |
| Large city | 1.42 (1.03, 1.96) | .03 | 1.07 (0.83, 1.38) | .61 |
| Region | ||||
| Northeast | REF | -- | REF | -- |
| Midwest | 0.86 (0.71, 1.05) | .13 | 0.84 (0.65, 1.10) | .21 |
| South | 0.90 (0.74, 1.09) | .28 | 0.80 (0.63, 1.02) | .07 |
| West | 1.10 (0.82, 1.46) | .53 | 1.02 (0.76, 1.38) | .89 |
| Parent with (vs. without) college degree | 1.13 (0.85, 1.50) | .42 | 1.14 (0.92, 1.40) | .23 |
| Nicotine dependence | ||||
| Combustible cigarette dependence symptoms (Any vs. None) | 2.46 (1.22, 4.93) | .01* | 1.70 (1.27, 2.26) | <.001* |
| Past 30-day substance use | ||||
| Combustible cigarettes | 0.95 (0.65, 1.39) | .80 | 1.20 (0.95, 1.52) | .13 |
| Other tobacco productse | 0.76 (0.53, 1.10) | .14 | 1.10 (0.86, 1.39) | .45 |
| No. alcohol/cannabis/other drugsf | ||||
| 0 | REF | -- | REF | -- |
| 1 | 1.36 (0.98, 1.89) | .07 | 1.47 (1.09, 1.98) | .01* |
| 2 | 1.92 (1.32, 2.81) | .001* | 1.67 (1.29, 2.16) | <.001* |
| 3 | 2.65 (1.57, 4.47) | <.001* | 1.90 (1.37, 2.64) | <.001* |
| JUUL | ||||
| 1–2 days | REF | -- | REF | -- |
| 3–5 days | 2.13 (1.45, 3.11) | <.001* | 1.46 (1.07, 1.98) | .02* |
| 6–9 days | 1.98 (1.44, 2.72) | <.001* | 1.46 (1.05, 2.03) | .02* |
| 10–19 days | 4.19 (2.60, 6.77) | <.001* | 1.97 (1.34, 2.90) | .001* |
| 20 or more days | 5.86 (4.10, 8.37) | <.001* | 3.80 (2.86, 5.05) | <.001* |
Note. Past 30-day JUUL users N=1748.
Multivariable logistic regression model for binary outcome of JUUL dependence status (any symptoms vs. none).
Multivariable negative binomial regression model for count outcome of JUUL dependence symptom score (Range=0–9).
Sampling weight was considered. Complex analyses were conducted using the cluster variable (astrat: Stratum for single or multiple year analysis).
Other race/ethnicity includes Asian and multiracial groups.
Includes smokeless tobacco, cigars/cigarillos, and hookah tobacco.
Total number of substance classes used (alcohol, cannabis, or other drugs [inhalants, hallucinogen, LSD, cocaine, crack, heroin, opioids, barbiturate drugs, tranquilizer drugs, methamphetamine]).
Statistically significant after Benjamini-Hochberg correction for multiple tests to maintain study-wise false discovery rate of .05.
Tobacco and Other Substance Use.
Among past 30-day JUUL users, the prevalence of JUUL dependence symptoms was successively higher among youth who reported using 0 (29 0%), 1 (38.5%), 2 (49.1%), or 3 or more (59.3%) non-nicotine substances in the past 30-days; similar results were found with the nicotine severity score, with greater dependence severity for every additional product used (Table 1); differences in prevalence and severity were statistically significant (ps<0.05)
JUUL Use Frequency.
The prevalence and severity of nicotine dependence symptoms was successively higher with each increasing response category of past 30-day JUUL use frequency. For example, the prevalence of nicotine dependence symptoms was 23.0% among participants who reported 1–2 days of past 30-day JUUL use, 38.3% among 6–9 days, 52.5% among 10–19 days, and 61.9% among 20 or more days (Table 1). The total number of nicotine dependence symptoms increased with each response category of past 30-day JUUL use in a similar fashion. In comparison to students reporting using JUUL on 1–2 of the past 30 days, students that used JUUL on 3–5 days, 6–9 days, 10–19 days, and 20 or more days reported 1.46 (95% CI: 1.07, 1.98), 1.46 (95% CI: 1.05, 2.03), 1.97 (1.34, 2.90), and 3.80 (95% CI: 2.86, 5.05) more JUUL dependence symptoms, respectively (Table 2). See supplemental materials for JUUL, cigarette, and dual user comparisons.
DISCUSSION
This study provides new evidence on nationally representative estimates of the prevalence, patterns, and correlates of JUUL dependence among U.S. youth in 2019. Among past 30-day JUUL users - which represented 12.5% of 8th, 10th, and 12th graders - 42.1% screened positive for nicotine dependence symptoms. These findings depart from the 17.6% prevalence estimate of dependence using the same measure in the current study among a Southern California sample of 12th grade students in 2016 (Vogel, Cho, et al., 2020), but concord with a 44% estimate of perceived addiction to JUUL in a small national sample of JUUL users (n=44) in 2017 (Hammond et al., 2018) - prior to the widespread use of high-nicotine pod-style e-cigarette brands. Regional studies conducted more recently with less comprehensive measures of nicotine dependence have also found a high prevalence of e-cigarette dependence symptoms in users of pod-style, high nicotine brands (Boykan et al., 2019; Morean et al., 2018).
Parallels between nicotine dependence in JUUL users and combustible cigarette dependence were observed. Similar to previous evidence in combustible cigarettes (Storr, 2008), we found a characteristic dose dependent relation between increasing frequency of JUUL use and risk and severity of dependence symptoms, after adjustment for multiple covariates. The qualitative shape of the nicotine dependence symptom severity distribution (i.e., positive skew) and rank ordering of symptom types that were most (e.g., cravings, urges) and least (e.g., inability to quit) were similar between JUUL users and the comparison sample of past 30-day combustible cigarette smokers, consistent with prior work (Vogel, Cho, et al., 2020). This pattern suggests that the way in which the nicotine dependence syndrome manifests may be similar across youth who use either tobacco product.
The prevalence and severity of nicotine dependence appeared to be higher in the comparison sample of cigarette smokers than in JUUL asers in this study. While these two samples are each nationally representative samples of the respective populations of JUUL users and combustible cigarette smokers, direct comparisons are complicated by the fact they are different groups (only 11.1% of sample overlapped). The comparison sample of smokers (vs. the JUUL user sample) appeared to include greater proportion of poly-substance users, parents with less education, and other characteristics, which are known to increase risk of nicotine dependence (Racicot et al., 2012). Whether differences in nicotine dependence prevalence across the two samples are explained by these risk factors or that dependence risk is inherently higher for combustible cigarettes than JUUL across populations warrants further research. Regardless, the nicotine dependence symptom positivity rate was high in both samples (JUUL: 41.3%, cigarettes: 52.1%) and the population health impact of e-cigarette dependence is of particular concern given the high prevalence of past-30-day nicotine vaping in youth (Miech et al., 2019).
Poly-use of alcohol and other non-nicotine substances was highly associated with JUUL dependence, above and beyond use of other tobacco products, and after adjustment for frequency of JUUL use. Previous studies have shown that other drug use and mental health issues can increase the odds and severity of cigarette dependence even after holding constant the frequency of smoking, suggesting diathesis between other drugs and nicotine dependence risk (Cross et al., 2016; Dierker et al., 2015). Previous research has also found pharmacological interactions between nicotine and other substances that may enhance the dependence potential of tobacco products (Adams, 2017). While under the influence of non-nicotine substances, the reinforcing effects of cigarettes are enhanced (Glautier et al., 1996; Tidey et al., 2000), which may in turn increase risk for progression to nicotine dependence (Buchmann et al., 2013).
Based on the results from the current study and previous studies (Boykan et al., 2019; Nardone et al., 2019), JUUL and other high-nicotine pod-style e-cigarette brands may substantively increase risk of nicotine dependence. As of 2018, 39 small pod-based devices that emulate JUUL both in their design and high nicotine salt e-liquid have been identified in addition to 14 brands marketing JUUL compatible pods with even higher nicotine content than JUUL (Jackler & Ramamurthi, 2019). Thus, even if there are future reductions in the prevalence of adolescent use of JUUL brand e-cigarettes, per se, and youth begin to adopt use of other similar products, it is reasonable to expect that current findings may generalize to other nicotine-salt based products (Boykan et al., 2019). This is a concern because nicotine dependence has become distressing to teens. Youth who use e-cigarettes report unease over mental health problems (e.g., depression), difficulty concentrating, reduction in academic success, and distress related to their use of e-cigarettes but an inability to stop vaping (Amato et al., 2020). Nicotine dependence may also prolong vaping and increase risk to progression to heavier patterns of vaping (Boykan et al., 2019; Nardone et al., 2019), thereby increasing to extent of exposure to e-cigarette aerosol. Since e-cigarette aerosol contains cardiovascular and respiratory toxins (National Academies of Sciences, Engineering, and Medicine, 2018) and nicotine exposure may interfere with the adolescent developing brain and increase risk of attention and mood problems (U.S. Department of Health and Human Services, 2016), the health consequences of nicotine dependence in youth e-cigarette users may be substantial.
Limitations
First, the current study is limited by its cross-sectional observational design. Thus, it cannot be definitively concluded whether the correlates studied here are risk factors, consequences, or epiphenomena associated with JUUL dependence. Second, all measures were self-reported and did not include a clinical diagnosis of tobacco use disorder. While the measure of dependence used here has shown high sensitivity and parallel validity across combustible and e-cigarette versions of the scale (Vogel, Cho, et al., 2020; Wheeler et al., 2004), the measure’s specificity for identifying tobacco use disorder may be modest (Vogel, Prochaska, & Rubinstein, 2020). There may also be slight underestimations of JUUL and cigarette dependence symptoms as we used a modified 9-item version to the original 10-item HONC. Furthermore, by design, the instructions are simple for adolescent populations and do not instruct youth to report their experience over a specific time frame, leaving unclear whether the symptoms reported are current symptoms. Given that this study was limited to past 30-day users, the likelihood that symptoms youth reported on were recently experienced is high. Finally, although a comparative analysis was conducted for dependence symptoms in combustible cigarette smokers, nicotine dependence symptoms among users of e-cigarette brands other than JUUL were not assessed. Future work comparing the prevalence and correlates of e-cigarette dependence symptoms across a variety of e-cigarette brands, product characteristics, and user behaviors would be fruitful.
Conclusions
In this nationally representative sample of U.S. youth, nicotine dependence symptoms were of appreciable prevalence and severity in JUUL users and more common among youth who vaped more frequently and used multiple other non-nicotine substances. These findings contribute further evidence that e-cigarette dependence is likely a genuine expression of tobacco use disorder among U.S. youth (Vogel, Cho, et al., 2020; Walley et al., 2019). This holds important implications for nicotine dependence screening as the HONC may be an easy and reliable way to assess youth nicotine dependence symptoms as well as risk for other drug use. They also suggest that nicotine dependence screening may warrant prioritization in pediatric health service settings, particularly in youth that use pod-style e-cigarette products and use other substances. Given the assumption that nicotine dependence may make quitting use difficult and evidence a substantial portion of U.S. youth e-cigarette users are interested in quitting (Smith et al., 2020), evidence-based e-cigarette use prevention and cessation treatments are needed (Sargent et al., 2020). The prevalence and health consequences of nicotine dependence in adolescent users of JUUL and other pod-style e-cigarette products should be considered in regulatory policies that aim to protect pediatric population health. Ideally, such policies would align with FDA’s Youth Tobacco Prevention Plan (U.S. Food & Drug Administration, 2020) to focus on limiting youth access to and marketing of JUUL as well as educating on the dangers of any tobacco use.
Supplementary Material
Highlights.
Forty-two percent of JUUL users reported symptoms of nicotine dependence.
Frequent JUUL and other substance use associated with greater dependence severity.
The profile of JUUL dependence symptoms paralleled cigarette dependence symptoms.
Funding
Research reported in this publication was supported by NIH (grant numbers R01-DA001411S1 [Miech, P.I.], K24 DA048160 and U54 CA180905 [Leventhal]).
Role of Funder
The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest Disclosures
The authors have no conflicts of interest relevant to this article ro disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams S, 2017. Psychopharmacology of Tobacco and Alcohol Comorbidity: a Review of Current Evidence. Curr. Addict. Rep. 4(1), 25–34. 10.1007/s40429-017-0129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Food & Drug Administration, 2020. FDA's Youth Tobacco Prevention Plan. Retrieved from https://www.fda.gov/tobacco-products/youth-and-tobacco/fdas-youth-tobacco-prevention-plan.
- Amato M, Bottcher M, Cha S, Jacobs M, Pearson J, Graham A, 2020. “It’s really addictive and I’m trapped:” A qualitative analysis of the reasons for quitting vaping among treatment-seeking young people. Addictive Behaviors, 112, 106599–106599. 10.1016/j.addbeh.2020.106599. [DOI] [PubMed] [Google Scholar]
- Barrington-Trimis JB, Leventhal AM, 2018. Adolescents’ Use of “Pod Mod” E-Cigarettes — Urgent Concerns. N. Engl. J. Med. 379(12), 1099–1102. 10.1056/NEJMp1805758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y, 1995. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal statistical society: Series B (Methodological), 57(1), 289–300. 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- Boykan R, Goniewicz ML, Messina CR, 2019. Evidence of Nicotine Dependence in Adolescents Who Use Juul and Similar Pod Devices. Int. J. Environ. Res. Public Health, 16(12). 10.3390/ijerph16122135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann AF, Blomeyer D, Jennen-Steinmetz C, Schmidt MH, Esser G, Banaschewski T, Laucht M, 2013. Early smoking onset may promise initial pleasurable sensations and later addiction. Addict. Biol. 18(6), 947–954. 10.1111/j.1369-1600.2011,00377.x. [DOI] [PubMed] [Google Scholar]
- Case KR, Hinds JT, Creamer MR, Loukas A, Perry CL, 2020. Who is JUULing and Why? An Examination of Young Adult Electronic Nicotine Delivery Systems Users. J. Adolesc. Health, 66(1), 48–55.. 10.1016/j.jadohealth.2019.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross S, Lotfipour S, Leslie F, 2016. Mechanisms and genetic factors underlying co-use of nicotine and alcohol or other drugs of abuse. The American Journal of Drug and Alcohol Abuse, 43(2), 171–185. 10.1080/00952990.2016.1209512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierker L, Rose J, Selya A, Piasecki TM, Hedeker D, Mermelstein R/2015. Depression and nicotine dependence from adolescence to young adulthood. Addict. Behav. 41, 124–128. 10.1016/j.addbeh.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duell AK, Pankow JF, Peyton DH, 2018. Free-Base Nicotine Determination in Electronic Cigarette Liquids by (1)H NMR Spectroscopy. Chem. Res. Toxicol, 31(6), 431–434. 10.1021/acs.chemrestox.8b00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glautier S, Clements K, White JA, Taylor C, Stolerinan IP, 1996. Alcohol and the reward value of cigarette smoking. Behav. Pharmacol, 7(2), 144–154. 10.1097/00008877-19960300000005. [DOI] [PubMed] [Google Scholar]
- Goniewicz M, Boykan R, Messina C, Eliscu A, Tolentino J, 2019. High exposure to nicotine among adolescents who use Juul and other vape pod systems (“pods”). Tob. Control, 28(6), 676–677. 10.1136/tobaccocontrol-2018-054565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Wackowski O, Reid J, O’Connor R, 2018. Use of JUUL E-cigarettes Among Youth in the United States. Nicotine & Tobacco Research, 22(5), 827–832. 10.1093/ntr/nty237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackler RK, Ramamurthi D, 2019. Nicotine arms race: JUUL and the high-nicotine product market. Tob. Control, 28(6), 623–628. 10.1136/tobaccocontrol-2018-054796. [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O Malley PM, Bachman JG, Patrick ME, 2019. Trends in Adolescent Vaping, 2017–2019. N. Engl. J. Med. 381(15), 1490–1491. 10.1056/NEJMc1910739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME, 2020. Monitoring the Future national survey results on drug use, 1975–2019: Volume I, Secondary school students. Retrieved from Available at http://monitoringthefuture.org/pubs.html#monographs. [Google Scholar]
- Morean ME, Krishnan-Sarin S, O' Malley S, 2018. Assessing nicotine dependence in adolescent E-cigarette users: The 4-item Patient-Reported Outcomes Measurement Information System (PROMIS) Nicotine Dependence Item Bank for electronic cigarettes. Drug. Alcohol Depend. 188, 60–63. 10.1016/j.drugalcdep.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (Eds.), 1998-2017. Mplus User’s Guide. Eighth Edition: Muthén & Muthén. [Google Scholar]
- Nardone N, Helen G, Addo N, Meighan S, Benowitz N, 2019. JUUL electronic cigarettes: Nicotine exposure and the user experience. Drug. Alcohol Depend. 203, 83–87. 10.1016/j.drugalcdep.2019.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2018. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press, 10.17226/24952. [DOI] [PubMed] [Google Scholar]
- Racicot S, McGrath J, Karp I, O’Loughlin J, 2012. Predictors of nicotine dependence symptoms among never-smoking adolescents: A longitudinal analysis from the Nicotine Dependence in Teens Study. Drug. Alcohol Depend 130(1), 38–44. 10.1016/j.drugalcdep.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JE, 2006. Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl), 184(3–4), 274–285. 10.1007/s00213-005-0250-x. [DOI] [PubMed] [Google Scholar]
- Sargent JD, Unger J, Leventhal AM, 2020. Recommendations From the USPSTF for Prevention and Cessation of Tobacco Use in Children and Adolescents. JAMA Netw. Open, 323, 1563–1564. 10.1001/jama.2019.22312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2016. E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. Atlanta, GA: U.S.Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- Smith TT, Nahhas GJ, Carpenter MJ, Squeglia LM, Diaz VA, Leventhal AM, Dahne J, 2020. Intention to Quit Vaping Among United States Adolescents. JAMA Pediatr. 175(1), 97–99. 10.1001/jamapediatrics.2020.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storr CL, 2008. Characteristics associated with rapid transition to tobacco dependence in youth. Nicotine Tob. Res. 10(6), 1099–1104. 10.1080/14622200802087556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, O'Neill SC, Higgins ST, 2000. d-amphetamine increases choice of cigarette smoking over monetary reinforcement. Psychopharmacology (Berl), 153(1), 85–92. 10.1007/s002130000600. [DOI] [PubMed] [Google Scholar]
- Vogel EA, Cho J, McConnell RS, Barrington-Trimis JL, Leventhal AM, 2020. Prevalence of Electronic Cigarette Dependence Among Youth and Its Association With Future Use. JAMA Netw. Open, 3(2), e1921513. 10.1001/jamanetworkopen.2019.21513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Prochaska JJ, Rubinstein ML, 2020. Measuring e-cigarette addiction among adolescents. Tob. Control, 29(3), 258–262. 10.1136/tobaccocontrol-2018-054900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley SC, Wilson KM, Winickoff JP, Groner J, 2019. A Public Health Crisis: Electronic Cigarettes, Vape, and JUUL. Pediatrics, 143(6). 10.1542/peds.2018-2741. [DOI] [PubMed] [Google Scholar]
- Wheeler KC, Fletcher KE, Wellman RJ, Difranza JR, 2004. Screening adolescents for nicotine dependence: the Hooked On Nicotine Checklist. J. Adolesc. Health, 35(3), 225–230. 10.1016/S1054-139X(03)00531-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


