Abstract
Background:
Evidence for use of electronic cigarettes (e-cigs) as a potential aid in quitting or reducing combustible cigarette (c-cig) use is mixed. This study examined the extent to which e-cig initiation among smokers in their 30s predicted quitting or reducing smoking or nicotine dependence symptoms by age 39, and whether the role of e-cigs in quitting differed by prospectively assessed moderators.
Methods:
Data were from the Seattle Social Development Project (SSDP), a panel study of 808 diverse participants with high retention. A subsample of 221 smokers at age 33 was selected for analysis. Self-reports of c-cig use and dependence were assessed longitudinally at ages 33 and 39. Sixteen potential moderators were examined, including social demographics, smoking attitudes and desire to quit, other health behaviors and status, and adolescent and early adult assessments of smoking history.
Results:
The use of e-cigs was consistently associated with a lower likelihood of quitting c-cigs by age 39, after accounting for frequency of prior c-cig use at age 33. This negative association persisted across all moderators examined, although it was nonsignificant among those with a definite desire to cut down. Among those who did not quit smoking, e-cig use had no association with decreases in either quantity of c-cigs used or dependence symptoms.
Conclusions:
Results indicate that e-cigarette use was not helpful for quitting or reducing combustible cigarette use in the 30s. Rather, across extensive tests of moderation, e-cig initiation consistently predicted less quitting during this important age period for successful cessation.
Keywords: Electronic cigarettes, Smoking, Smoking cessation, Longitudinal research, Moderators, Adulthood
1. Introduction
Electronic cigarettes (e-cigs) entered the market in the United States in 2007 and their sales and use increased dramatically over the next several years (Marynak et al., 2017; McMillen et al., 2015). Although the prevalence of adult use has varied somewhat in recent years, e-cig use reached 3.2% of the adult U.S. population in 2018 and was 10% among current smokers (i.e., dual users) (Bao et al., 2020; Dai and Leventhal, 2019b). E-cigarettes are typically battery-powered devices that heat a nicotine-containing liquid producing an aerosol that is inhaled by the user (Orellana-Barrios et al., 2015). Despite a number of unsafe constituents, e-cigs expose the user to significantly fewer toxic substances than use of combustible cigarettes (c-cigs) and are likely to be less harmful overall (National Academies of Sciences, Engineering, and Medicine, 2018). Many adult smokers have turned to e-cigarettes in efforts to quit smoking c-cigs, preferring them over some other cessation approaches such as nicotine patch, gum, or inhalers (Hajek et al., 2019; Steinberg et al., 2014). Nearly 6% of former smokers in 2018 reported using e-cigarettes, suggesting that e-cigs may have replaced their prior combustible cigarette use (Bao et al., 2020).
Understanding the potential for use of e-cigarettes as an aid in quitting or reducing combustible cigarette use is important for determining their overall public health impact. The research literature, however, is mixed (National Academies of Sciences, Engineering, and Medicine, 2018). In a meta-analysis of 38 real-world and clinical studies, Kalkhoran and Glantz (2016) found that e-cig use was associated with significantly less quitting among smokers. Other observational studies buttress this conclusion (Kulik et al., 2018; Rigotti et al., 2018 ). But using data from the large US Current Population Study-Tobacco Use Supplement, Zhu et al. (2017) concluded that e-cig use was associated with significantly more quitting and likely contributed to an increase in smoking cessation at the population level. Some randomized trials also indicated positive effects of prescribing e-cig use for cessation under certain conditions (Hajek et al., 2019; Halpern et al., 2018), and Jorenby et al. (2017) reported that e-cig use helped to maintain reductions in c-cig use among dual users. Studies by Berry et al. (2019) and Kalkhoran et al. (2019) found that daily e-cig users were more likely to report prolonged smoking abstinence than smokers who did not use e-cigs, but there was no significant association with quitting for those who used e-cigs less than daily. In their review, Bhatnagar et al. (2019) summarized current findings on the association between e-cig use and smoking cessation as mostly negative in real-world scenarios, but possibly helpful in a small percentage of individuals motivated to quit.
Some limitations of existing studies are important to address. Many relied on retrospective reports of prior smoking behavior, which could be influenced by current behaviors or other factors affecting recall and accurate reporting (National Academies of Sciences, Engineering, and Medicine, 2018). Most studies that did include prospective reports examined a relatively brief history of prior smoking behavior and a short timeframe for e-cig use to have occurred (El Dib et al., 2017; Kalkhoran and Glantz, 2016). There is also limited understanding of potential moderators. Because of varying rates of e-cig use across groups and observed relationships with social and behavioral factors (Kalkhoran et al., 2020), it is plausible that the role of e-cigs differs by gender, socioeconomic status, smoking environment or norms, desire and attempts to quit smoking, or other health behaviors or status. Interactions with one’s prior smoking and dependence history are particularly important to investigate. Lack of key measures of user characteristics—and examination of these characteristics as moderators of e-cig use as a smoking cessation aid—has been noted as a major limitation in the research base (National Academies of Sciences, Engineering, and Medicine, 2018).
The developmental period during which e-cigarettes became available is also important to consider. Smokers in their 30s may be an important but underexamined cohort to investigate because adults who quit successfully often do so in their 30s (Babb et al., 2017; Gilman et al., 2002; Kalkhoran et al., 2020; Schauer et al., 2015). Typical life transitions during the 30s (e.g., growing recognition of health risks, career development, parenting) may help reinforce efforts to change health habits (Ostbye et al., 2011; Settersten, 2003; Settersten and Ray, 2010). To the extent e-cigarettes are effective quit aids, those who were in their 30s when e-cigs became commercially available and rapidly grew in popularity may have been the most likely candidates to successfully utilize this new technology for smoking cessation.
To address these research gaps, the current study used prospective, longitudinal data to examine four key questions. First, did e-cig use predict smoking cessation? We examined whether e-cig initiation among those who were smokers at age 33 was associated with quitting c-cigs by age 39. Second, among smokers who did not quit, did e-cig use predict reduced smoking or dependence? We examined whether e-cig initiation was associated with longitudinal changes in the quantity of c-cigs used or number of nicotine dependence symptoms by age 39. Third, were the effects of e-cig use moderated by current social or behavioral factors? We investigated individuals’ social settings, attitudes, and health behaviors as potential moderators of the role of e-cigs for quitting c-cigs by age 39. Finally, were the effects of e-cig use moderated by prior smoking history? We examined prospectively assessed smoking history to understand the role of smoking and dependence onset and intensity over time for the relationship between e-cig and c-cig use in the 30s.
2. Materials and methods
2.1. Sample
Data were from the Seattle Social Development Project, a longitudinal panel study established in 1985 from a population of all students (N = 1053) entering Grade 5 in 18 public schools serving higher crime neighborhoods in Seattle, Washington. Of these students, 808 (77%) youth and their parents consented to participate in the longitudinal study. Main analyses reported here were based on surveys conducted at ages 33 and 39 (M = 39.51, SD = .55) in 2008 and 2014, respectively. Other prospective survey waves beginning at age 13 were used to assess smoking history, and an abbreviated survey (excluding most moderator variables) at age 35 was used for sensitivity analyses. Retention of still-living participants from the original panel averaged 92% across waves, and was 92% and 88% at ages 33 and 39, respectively (37 participants were deceased by age 39). Over the course of the study, retention was not consistently related to gender, ethnicity, childhood poverty, or adolescent substance use. The analysis sample was limited to those who reported smoking any amount at age 33 (N = 221). This sample was similar to the original full sample and was 56% male (compared with 51% in the full sample); 47% were European American, 29% African American, 15% Asian American, and 9% Native American—across race, 5% were Hispanic ethnicity (47%, 26%, 22%, 5%, and 5%, respectively, in the full sample); 54% had participated in the National School Lunch/Breakfast Program between the ages of 10 and 12, an indicator of childhood poverty (52% in the full sample). The study was approved by the Human Subjects Review Committee at the University of Washington and participants provided informed consent.
2.2. Measures
2.2.1. Combustible cigarette use
Use of combustible cigarettes at ages 33 and 39 was assessed with the item, “In the last 12 months, how many cigarettes did you usually smoke in a day?” (coded to a maximum of 20 to limit the effect of outliers—98% reported 20 or fewer; “less than one” was coded to .5). A dichotomous measure of quitting c-cig use by age 39 was computed for those who smoked any amount at age 33 but reported no c-cig use at age 39 (coded 1, or coded 0 if c-cig use continued).
2.2.2. Electronic cigarette use
Use of electronic cigarettes was assessed at age 39 with the item, “Have you ever used smokeless or electronic cigarettes (‘e-cigarettes,’ ‘vaping,’ or ‘ENDS’)?” Note that e-cigs were not available on the U.S. market until 2007 and still rare for 3 or 4 years thereafter, so it is unlikely that e-cig initiation occurred prior to the age 33 (2008) survey (Khan et al., 2014; Marynak et al., 2017; McMillen et al., 2015). Some sensitivity analyses used the measure, “How many times in the past month have you used smokeless or electronic cigarettes?” asked at age 39 (coded to a maximum of 30 to limit outliers).
2.2.3. Nicotine dependence
Nicotine dependence corresponding to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) was assessed using the Diagnostic Interview Schedule (DIS) (American Psychiatric Association, 1994; Robins et al., 1999). Past-year symptom counts ranged from 0 to 7. Dichotomous measures of dependence were computed for those with three or more symptoms (coded 1, or 0 if less than three symptoms).
2.2.4. Moderators
Dichotomous moderators were based on self-reports of the past year at age 33 unless noted otherwise. Moderators examined included the following: gender (all identified as female or male); race/ethnicity (European American and African American; other groups included too few smokers for moderation analyses); 2-year college degree (or beyond); partner who smokes (if a cohabitating partner or spouse); friends approve of one’s own smoking (at least a “pretty good chance” friends would approve); participant approves of adult smoking (agreed that it is “okay for adults to smoke”); definitely wishes to cut down (answered "yes" to “wished you cut down, or had more control over when and how much you smoked”; responses of “no” and “maybe/sometimes” coded as “does not definitely wish to cut down”); tried to quit or cut down (attempted in past year); alcohol, marijuana, depressive, and anxiety disorder (for each, met DSM-IV diagnostic criteria assessed with the DIS); onset of one or more cigarettes per day by age 21 (assessed prospectively at ages 13 through 16 annually, and at ages 18 and 21); onset of nicotine dependence by age 30 (assessed at ages 24, 27 and 30); average use of a half-pack of cigarettes or more per day from ages 21 to 33 (assessed at ages 21, 24, 27, 30, and 33); average of 3 or more nicotine dependence symptoms from ages 24 to 33 (assessed at ages 24, 27, 30, and 33).
2.3. Analyses
Tests of moderation used multiple-group analysis procedures in Mplus 8.4, calculating the χ2 difference between unconstrained models and those with pathways constrained to be equal between groups. Full-information maximum likelihood missing data estimation was used (Muthén and Muthén, 1998-2017). Part of the sample was assigned to a preventive intervention in the elementary grades, consisting of teacher workshops, parenting classes, and social competence instruction for children (Hawkins et al., 2005). It is possible that the intervention led to differences in the covariances among the c-cig use, nicotine dependence, and e-cig use variables examined in the study. To investigate this, we conducted multiple-group model tests (corresponding to the results reported) where covariances were constrained to be equal versus freely estimated across the control and full intervention groups (the “full” group received all intervention components, where intervention effects have been found to be strongest in prior reports). These tests showed no significant reduction in the overall fit of the constrained models (Δχ2(3) = .84 to 4.77, p-values .84 to .19), suggesting no substantial group differences and supporting full-sample analyses.
3. Results
3.1. E-cig use and quitting smoking
Of 671 participants providing data at ages 33 and 39, 221 (33%) reported smoking in the past year at age 33. Among smokers, Figure 1 shows that 62% reported no e-cigarette use and 38% reported having used e-cigs by age 39. Figure 1 also indicates the portion of those who quit smoking by age 39 within each group. Among smokers who had not tried e-cigs, 44% quit smoking c-cigs within the next 6 years, whereas only 8% of those who had tried e-cigs went on to quit (χ2[1] = 31.88, p < .001).
Figure 1.
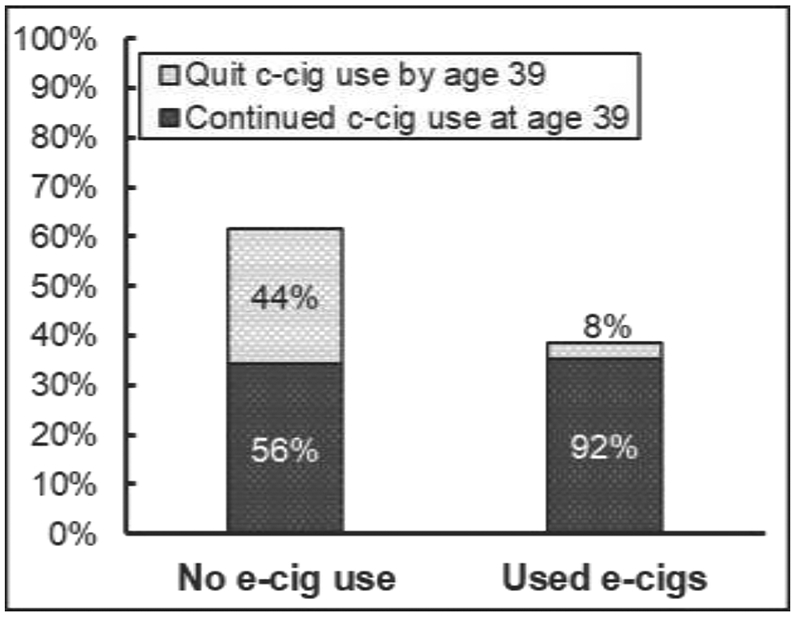
Prevalence of electronic cigarette use and quitting combustible cigarettes by age 39, among those who smoked at age 33 (N = 221). c-cig = combustible cigarette; e-cig = electronic cigarette.
3.2. E-cig use and changes in c-cig use and nicotine dependence symptoms
Next, we examined the role of e-cig use in changes, from age 33 to age 39, in the number of c-cigs usually used per day and the number of nicotine dependence symptoms reported, among those who did not quit smoking (n = 154). The upper plot in Figure 2 indicates that those who initiated e-cig use were significantly heavier smokers at age 33 (11.17 c-cigs per day, SD = 6.24) compared with those who never used e-cigs (9.13 c-cigs per day, SD = 5.98; F = 4.32, p = .04). By age 39, however, the difference in smoking quantity between e-cig users and nonusers was no longer significant (10.51 [SD = 5.94] vs. 9.05 [SD = 5.52] c-cigs per day, respectively; F = 2.52, p = .11). Overall, after accounting for different levels of use at age 33, the association of e-cig use with quantity of c-cigs used at age 39 did not approach significance (β = .05, p = .54).
Figure 2.
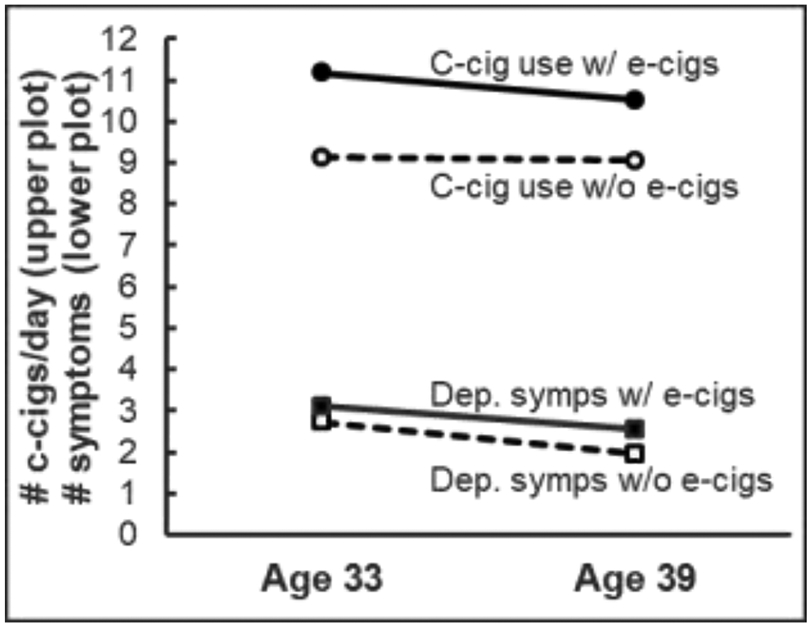
Changes in combustible cigarette use and nicotine dependence symptoms by electronic cigarette use, among smokers who did not quit by age 39 (n = 154). c-cig = combustible cigarette; e-cig = electronic cigarette; dep. symps = dependence symptoms.
Nicotine dependence symptoms at age 33 were also significantly different for those who did and did not use e-cigs (given relatively small standard deviations for these measures: 3.11 [SD = .90] vs. 2.73 [SD = 1.11] symptoms, respectively, F = 5.17, p = .02) (lower plot of Figure 2). Symptoms declined for both groups by age 39, but there was somewhat less decline for e-cig users (2.55 [SD = 1.61] symptoms, vs. 1.96 [SD = 1.46] symptoms for nonusers, F = 5.55, p = .02). The association of e-cig use with number of nicotine dependence symptoms at age 39, however, only approached significance after accounting for symptoms at age 33 (β = .17, p = .10).
3.3. Potential moderation of the role of e-cig use for quitting smoking
As shown in Table 1, we investigated possible moderation of the role of e-cigarette use for quitting c-cigs by age 39 among those who smoked at age 33. These analyses sought to identify if there were any groups or types of individuals for whom e-cig use played a positive role in quitting smoking, even though it was negatively associated with quitting at the aggregate level (Figure 1). We examined a series of multiple-group mediated models that included paths from quantity of c-cig use at age 33 to e-cig initiation, and from both of these to quitting c-cig use by age 39. In this way, these models estimated the relationship between e-cig use and quitting smoking, accounting for the effect of prior smoking at age 33 on each. Standardized coefficients for each pathway are reported in columns (a), (b), and (c) in Table 1, showing group pairs tested in each model. The final column reports the χ2 difference test comparing models where the e-cig → quitting path was constrained to be equal across groups to an unconstrained model.
Table 1.
Potential Moderators of the Role of E-cigarette Use in Quitting Combustible Cigarettes Between Ages 33 and 39
| Model paths |
|||||
|---|---|---|---|---|---|
| N | (a) Quant. c-cigs at 33 →Quit by age 39 |
(b) Quant. c-cigs at 33 →E-cig initiation |
(c) E-cig initiation →Quit by age 39 |
Diff. χ2 † |
|
| Full analysis sample (smokers at age 33) | 221 | −.30*** | .29*** | −.56*** | |
| Moderation by social position, setting | |||||
| Female | 98 | −.45*** | .07 | −.54*** | .08 |
| Male | 123 | −.18 | .43*** | −.66*** | |
| European American | 104 | −.31** | .34** | −.64*** | .00 |
| African American | 63 | −.32* | .19 | −.64*** | |
| Without 2-yr college degree | 168 | −.21* | .30** | −.64*** | .15 |
| With 2-yr college degree | 53 | −.70*** | .21 | −.37* | |
| Partner who does not smoke | 80 | −.34** | −.06 | −.70*** | 2.41 |
| Partner who smokes | 91 | −.33* | .55*** | −.37+ | |
| Moderation by attitudes, desire to quit | |||||
| Friends disapprove if you smoke | 124 | −.33** | .05 | −.57*** | .04 |
| Friends approve if you smoke | 80 | −.29 | .59*** | −.61*** | |
| Self disapproves of adult smoking | 57 | −.15 | .10 | −.70*** | .61 |
| Self approves of adult smoking | 157 | −.40*** | .31*** | −.49*** | |
| Does not definitely wish to cut down | 136 | −.26** | .13 | −.74*** | 5.60* |
| Definitely wishes to cut down | 77 | −.50*** | .47*** | −.21 | |
| Has not tried to quit or cut down | 67 | −.50*** | .44*** | −.37* | .80 |
| Has tried to quit or cut down | 147 | −.25* | .19+ | −.62*** | |
| Moderation by health behavior, status | |||||
| Without alcohol use disorder | 155 | −.34*** | .30** | −.59*** | .50 |
| With alcohol use disorder | 59 | −.22 | .23 | −.50** | |
| Without marijuana use disorder | 183 | −.34*** | .29** | −.54*** | .18 |
| With marijuana use disorder | 30 | −.16 | .21 | −.67** | |
| Without depressive disorder | 185 | −.27** | .32*** | −.53*** | .46 |
| With depressive disorder | 33 | −.66** | .07 | −.52* | |
| Without anxiety disorder | 185 | −.29** | .30*** | −.53*** | 1.87 |
| With anxiety disorder | 33 | −.47+ | .24 | −.67** | |
| Moderation by smoking history: Prospective longitudinal assessment | |||||
| Onset 1+ cig. per day < age 21 | 115 | −.21 | .28** | −.52*** | .84 |
| Onset 1+ cig. per day ≥ age 21 | 86 | −.20 | .23+ | −.68*** | |
| Onset dependence < age 30 | 104 | −.05 | .24* | −.56** | 1.12 |
| Onset dependence ≥ age 30 | 49 | −.28+ | .21 | −.75*** | |
| Avg. < .5 packs per day ages 21-33 | 151 | −.24* | .13 | −.56*** | .16 |
| Avg. ≥ .5 packs per day ages 21-33 | 70 | .01 | .37** | −.69*** | |
| Avg. < 3 dep. symps ages 24-33 | 163 | −.34*** | .23* | −.59*** | .20 |
| Avg. ≥ 3 dep. symps ages 24-33 | 58 | .46 | .19 | −.48+ | |
Notes. c-cig = combustible cigarette; e-cig = electronic cigarette; quant. = quantity; diff. = difference; dep. symps = dependence symptoms.
Difference χ2 tests the difference between groups in the model path from e-cig initiation to quitting c-cigs by age 39, using multiple-group modeling procedures.
P < .10, p < .05.
p < .05
p < .01
p < .001.
We first examined demographics and moderators assessed concurrently with c-cig use at age 33, relatively proximal to but also prior to common e-cig availability. Columns (a) and (b) indicate that more smoking at age 33 was associated with significantly less quitting by age 39 and more e-cig initiation across nearly all groups, and nonsignificant associations showed the same direction of effects (with the exception of one small −.06 coefficient in column (b)). Column (c) indicates that e-cig initiation was negatively associated with quitting smoking across all groups, and these associations were highly significant in all but a small number of cases. There was also little evidence for moderation, with one exception: E-cig use had a large and highly significant negative association with quitting smoking among those who did not definitely wish to quit or cut down, but this association was not significant among those who did definitely wish to quit or cut down (illustrated in Figure 3).
Figure 3.
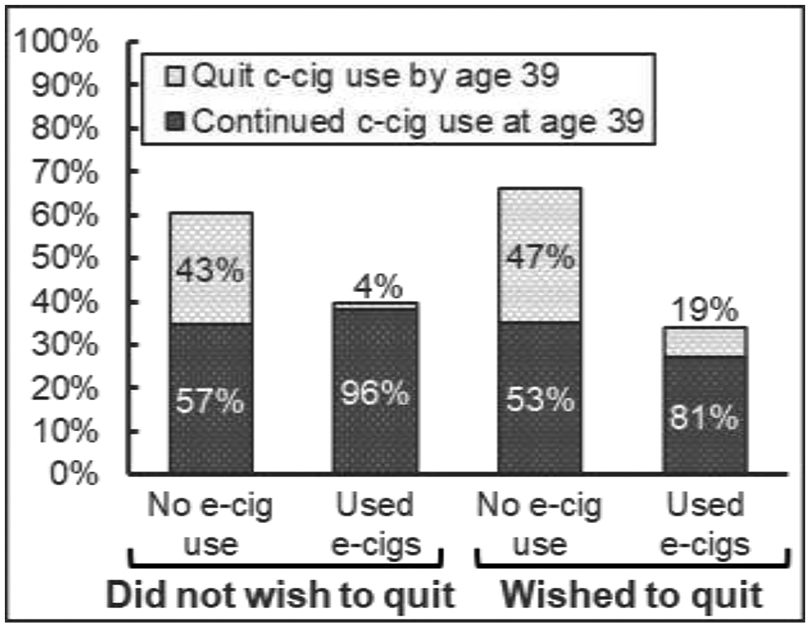
Prevalence of electronic cigarette use and quitting combustible cigarettes by age 39, for those who did and did not definitely wish to quit or cut down (n = 77 and n = 136, respectively). c-cig = combustible cigarette; e-cig = electronic cigarette.
3.4. Smoking history and the role of e-cig use for quitting smoking
Next, we examined potential moderation by smoking and dependence history using prospective, longitudinal assessments. As shown in the bottom of Table 1, initiation of e-cigarette use continued to have a negative association with quitting smoking by age 39 whether or not smoking onset occurred prior to age 21, dependence onset occurred prior to age 30, smokers averaged less than a half a pack a day since age 21, or averaged fewer than 3 dependence symptoms since age 24. No tests of moderation approached significance.
3.5. Sensitivity analyses
It is important to consider the possibility that the frequency of e-cig use could have effects on quitting smoking that are different from the effects of initiation or not (Kalkhoran et al., 2020; National Academies of Sciences, Engineering, and Medicine, 2018). To examine this, we duplicated the models reported in Table 1 but replaced e-cig initiation with a continuous measure of past-month e-cigarette use frequency assessed at age 39. Results were similar to the prior models, however, with a significant negative association between e-cig use and quitting smoking (β = −.56 for both e-cig measures), and no significant association between e-cig use and reduced smoking or dependence symptoms, regardless of whether e-cig initiation or frequency of use was included in the models. The results of moderation analyses were also similar: e-cig use frequency was negatively associated with quitting smoking for all groups.
Another possibility is that some smokers may have quit prior to the wide availability of e-cigs, were subsequently less likely to try e-cigs, and remained nonsmokers at age 39. To the extent this occurred, prior quitting may provide an alternative explanation for the negative association observed between e-cig use and cessation at age 39. To test this, we examined smokers at age 30 and compared those who continued to smoke at ages 33 and 35 with those who desisted at these ages, labeled “early desisters” (i.e., those reporting not smoking at age 35 or who were missing and not smoking at age 33; data were available for a smaller portion of the sample at age 35). Among early desisters (n = 66), 17% went on to try e-cigs, and over half of those (55%) who tried e-cigs relapsed to smoking combustible cigarettes by age 39. Of the early desisters who did not try e-cigs, only 18% relapsed by age 39. These findings are consistent with other studies (Dai and Leventhal, 2019a; Everard et al., 2020) that also found a positive association between e-cig use and relapse among desisters. Among those who did not desist early (n = 182), findings were similar to main results shown in Figure 1: age 39 quit rates were 7% and 34% for those who did and did not use e-cigs, respectively. Thus, although e-cig use was relatively rare among early desisters, it was negatively associated with quitting by age 39 for both those who did and did not desist early (β = −.55 and −.54, respectively, both p < .05, accounting for quantity of c-cig use at age 30 parallel to analyses in Table 1).
A final sensitivity check replicated main analyses but used a measure of not smoking in the past month at age 39 in order to provide a wider window of time for e-cig use to potentially aid quitting and to identify as quitters some participants who may have quit more recently. Results using this measure were similar to prior analyses, however, with past-month quit rates of 19% and 47% for those who did and did not use e-cigs, respectively (β = −.37, p < .001, corresponding to the first row, column (c), in Table 1).
4. Discussion
This study found that the use of electronic cigarettes among smokers in their 30s was consistently related to a lower likelihood of quitting combustible cigarettes, compared with those who did not initiate e-cig use. This was true regardless of gender, ethnicity, education, whether one’s partner smoked, smoking attitudes, prior attempts to quit, other substance use disorders, or mental health status. Even smoking history and nicotine dependence, assessed prospectively over several years, had no notable effect on the negative association between e-cigarette use and smoking cessation. Only among those who expressed a definite desire to cut down on their smoking was the relationship between e-cig use and quitting not significant or approaching significance. Other studies have shown some support for e-cig use aiding smoking cessation particularly among those wanting to quit (Berry et al., 2019; Bhatnagar et al., 2019; Martínez et al., 2020). Our findings suggest only that e-cig use did not significantly interfere with quit attempts for some individuals—though the association remained negative overall. The consistent negative association with cessation held whether e-cig use was assessed as initiation or frequency of use, whether cessation was measured in the past year or past month, and held among those who did and did not desist early.
Among those who continued to smoke to age 39 and also used e-cigs, there was somewhat steeper decline in the quantity of combustible cigarettes used per day, but they were also significantly heavier smokers to begin with at age 33 compared with those who did not use e-cigs. After accounting for initial differences, we found no significant association between e-cig use and quantity of c-cigs used or nicotine dependence symptoms at age 39.
The data for this study were limited in some important respects. A community sample was utilized, originating from Seattle, potentially limiting its generalizability. Many had dispersed across diverse communities throughout the U.S., however, with only 30% residing in Seattle by age 39. And the prevalence of cigarette use at age 33 (33% in the past year) was comparable to the national prevalence for the corresponding age and year (Substance Abuse and Mental Health Services Administration, 2008). The sample size was somewhat limited for moderation analyses, though the multiple-group modeling procedures used helped to maximize power (Bollen, 1989). Also, because all associations between e-cig use and cessation were negative for all subgroups, the significance level of interactions pertains only to variations in the degree of negative association. The study did not include an ongoing assessment of e-cigarette use, but relied on self-reports of e-cig initiation and past-month use at age 39. The data also predate the introduction of JUUL, the largest retail brand by 2017, so may not reflect more recent changes in the retail landscape and increased nicotine delivery of e-cig devices (Huang et al., 2019; National Academies of Sciences,, Engineering, and Medicine, 2018). Like nearly all studies predicting smoking cessation, it was not possible to precisely identify the degree to which prior cessation drove lack of e-cig use, rather than the reverse. However, analyses of early desisters—and of desire and attempts to quit, and duration and extent of dependence, which are likely correlates of early desistence—sought to address this concern. Studies with initiation and quit dates are needed to fully untangle temporal order.
The study also included key strengths that help to address important outstanding questions regarding e-cigarette use and quitting smoking. We prospectively examined change in smoking behavior over a 6-year period corresponding to the initial availability of e-cigs and growth in their popularity. The study cohort was likely young enough to be open to new technologies, was at an advantageous age to succeed at quitting, and had ample opportunity to try e-cigs for this purpose (e-cigs were widely available for 2 or 3 years prior to the outcome assessment at age 39) (Khan et al., 2014; Schauer et al., 2015; Vogels, 2019). We are aware of no other studies broadly investigating potential moderators of the association between e-cigs and smoking cessation, including smoking and smoking attitudes of partners and friends, personal smoking norms, and other substance use and mental health disorders, in addition to sociodemographics and prior desire and attempts to quit or cut down. Nor are we aware of other studies that have incorporated prospective assessments of smoking onset and adult history of dependence symptoms.
4.1. Conclusions
In the current literature on the efficacy of e-cigarette use for smoking cessation, our data are consistent with studies indicating that e-cigs are not helpful, and may instead be a hinderance to quitting smoking. We recognize that different studies with different strengths and weaknesses are reaching divergent conclusions. The present results underscore the need for more research and, in the meantime, an abundance of caution with respect to the use of electronic cigarettes as a potential aid to quitting tobacco smoking.
Highlights.
Understanding the role of e-cigarettes in quitting smoking is important for public health.
This longitudinal study examined potential moderators of the effects of e-cigarette use.
The study cohort experienced the introduction and growth of e-cigarettes during their 30s.
E-cigarette use was associated with less smoking cessation in all study analyses.
Acknowledgments
We thank our funders, the study participants, and the staff of the Social Development Research Group.
Role of Funding Source
This research was supported by the National Cancer Institute [NCI; grant number R37CA225690] and the National Institute on Drug Abuse [NIDA; grant numbers R01DA033956 and 1R01DA09679]. Content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. NCI and NIDA played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Footnotes
Conflict of Interest
No conflict declared.
Declaration of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association, Washington, DC. [Google Scholar]
- Babb S, Malarcher A, Schauer G, Asman K, Jamal A, 2017. Quitting smoking among adults - United States, 2000-2015. MMWR Morb. Mortal. Wkly. Rep 65, 1457–1464. 10.15585/mmwr.mm6552a1.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Bao W, Liu B, Du Y, Snetselaar LG, Wallace RB, 2020. Electronic cigarette use among young, middle-aged, and older adults in the United States in 2017 and 2018. JAMA Intern. Med 180, 313–314. 10.1001/jamainternmed.2019.4957.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Reynolds LM, Collins JM, Siegel MB, Fetterman JL, Hamburg NM, Bhatnagar A, Benjamin EJ, Stokes A, 2019. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013-2015. Tob. Control 28, 42–49. 10.1136/tobaccocontrol-2017-054108.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar A, Payne TJ, Robertson RM, 2019. Is there a role for electronic cigarettes in tobacco cessation? J. Am. Heart Assoc 8, e012742. 10.1161/JAHA.119.012742.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, 1989. Structural Equations with Latent Variables. John Wiley & Sons, Oxford. [Google Scholar]
- Dai H, Leventhal AM, 2019a. Association of electronic cigarette vaping and subsequent smoking relapse among former smokers. Drug Alcohol Depend. 199, 10–17. 10.1016/j.drugalcdep.2019.01.043.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Leventhal AM, 2019b. Prevalence of e-cigarette use among adults in the United States, 2014-2018. JAMA 322, 1824–1827. 10.1001/jama.2019.15331.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Dib R, Suzumura EA, Akl EA, Gomaa H, Agarwal A, Chang Y, Prasad M, Ashoorion V, Heels-Ansdell D, Maziak W, Guyatt G, 2017. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis. BMJ Open 7, e012680. 10.1136/bmjopen-2016-012680.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everard CD, Silveira ML, Kimmel HL, Marshall D, Blanco C, Compton WM, 2020. Association of electronic nicotine delivery system use with cigarette smoking relapse among former smokers in the United States. JAMA Network Open 3, e204813. 10.1001/jamanetworkopen.2020.4813.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Abrams DB, Buka SL, 2002. Life course socioeconomic status and transitions of tobacco use: event-history analyses of the age at first cigarette, daily smoking, and smoking cessation (meeting abstract). Am. J. Epidemiol 155(11), S71. [Google Scholar]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross L, Goniewicz M, Wu Q, McRobbie HJ, 2019. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N. Engl. J. Med 380, 629–637. 10.1056/NEJMoa1808779.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Halpern SD, Harhay MO, Saulsgiver K, Brophy C, Troxel AB, Volpp KG, 2018. A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. N. Engl. J. Med 378, 2302–2310. 10.1056/NEJMsa1715757.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD, 2005. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch. Pediatr. Adolesc. Med 159, 25–31. 10.1001/archpedi.159.1.25.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Huang J, Duan Z, Kwok J, Binns S, Vera LE, Kim Y, Szczypka G, Emery SL, 2019. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob. Control 28, 146–151. 10.1136/tobaccocontrol-2018-054382.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorenby DE, Smith SS, Fiore MC, Baker TB, 2017. Nicotine levels, withdrawal symptoms, and smoking reduction success in real world use: a comparison of cigarette smokers and dual users of both cigarettes and e-cigarettes. Drug Alcohol Depend. 170, 93–101. 10.1016/j.drugalcdep.2016.10.041.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S, Chang Y, Rigotti NA, 2019. Electronic cigarette use and cigarette abstinence over 2 years among U.S. smokers in the Population Assessment of Tobacco and Health Study. Nicotine Tob. Res 22, 728–733. 10.1093/ntr/ntz114.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S, Chang Y, Rigotti NA, 2020. Electronic cigarette use and cigarette abstinence over 2 years among U.S. smokers in the Population Assessment of Tobacco and Health Study. Nicotine Tob. Res 22, 728–733. 10.1093/ntr/ntz114.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S, Glantz SA, 2016. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir. Med 4, 116–128. 10.1016/S2213-2600(15)00521-4.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan T, Barker DC, Quinn CM, Huang J, Chaloupka FJ, 2014. Changes in E-cigarette Availability Over Time in the United States: 2010-2012 -A BTG Research Brief. Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago, Chicago, IL. [Google Scholar]
- Kulik MC, Lisha NE, Glantz SA, 2018. E-cigarettes associated with depressed smoking cessation: a cross-sectional study of 28 European Union countries. Am. J. Prev. Med 54, 603–609. 10.1016/j.amepre.2017.12.017.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez Ú, Martínez-Loredo V, Simmons VN, Meltzer LR, Drobes DJ, Brandon KO, Palmer AM, Eissenberg T, Bullen CR, Harrell PT, Brandon TH, 2020. How does smoking and nicotine dependence change after onset of vaping? a retrospective analysis of dual users. Nicotine Tob. Res 22, 764–770. 10.1093/ntr/ntz043.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marynak KL, Gammon DG, King BA, Loomis BR, Fulmer EB, Wang TW, Rogers T, 2017. National and state trends in sales of cigarettes and e-cigarettes, U.S., 2011–2015. Am. J. Prev. Med 53, 96–101. 10.1016/j.amepre.2017.01.016.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, Klein JD, 2015. Trends in electronic cigarette use among US adults: use is increasing in both smokers and nonsmokers. Nicotine Tob. Res 17, 1195–1202. 10.1093/ntr/ntu213.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998-2017. Mplus User's Guide. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2018. Public Health Consequences of E-cigarettes. The National Academies Press, Washington, DC. [PubMed] [Google Scholar]
- Orellana-Barrios MA, Payne D, Mulkey Z, Nugent K, 2015. Electronic cigarettes—a narrative review for clinicians. Am. J. Med 128, 674–681. https://doi.org/https://doi.org/10.1016/j.amjmed.2015.01.033.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Ostbye T, Malhotra R, Landerman LR, 2011. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981-2006). Int. J. Epidemiol 40, 240–250. 10.1093/ije/dyq142.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Rigotti NA, Chang Y, Tindle HA, Kalkhoran SM, Levy DE, Regan S, Kelley JHK, Davis EM, Singer DE, 2018. Association of e-cigarette use with smoking cessation among smokers who plan to quit after a hospitalization: a prospective study. Ann. Intern. Med 168, 613–620. 10.7326/m17-2048.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North C, Rourke K, 1999. The Diagnostic Interview Schedule for DSM-IV (DIS-IV). Washington University, St. Louis, MO. [Google Scholar]
- Schauer GL, Malarcher AM, Asman KJ, 2015. Trends in the average age of quitting among U.S. adult cigarette smokers. Am. J. Prev. Med 49, 939–944. 10.1016/j.amepre.2015.06.028.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Settersten RA, 2003. Age structuring and the rhythm of the life course. In: Mortimer JT, Shanahan MJ (Eds.), Handbook of the Life Course. Springer US, Boston, MA, pp. 81–98. [Google Scholar]
- Settersten RA Jr., Ray B, 2010. What's going on with young people today? The long and twisting path to adulthood. Future Child. 20, 19–41. 10.1353/foc.0.0044.Accessed May 10, 2021. [DOI] [PubMed] [Google Scholar]
- Steinberg MB, Zimmermann MH, Delnevo CD, Lewis MJ, Shukla P, Coups EJ, Foulds J, 2014. E-cigarette versus nicotine inhaler: comparing the perceptions and experiences of inhaled nicotine devices. J. Gen. Intern. Med 29, 1444–1450. 10.1007/s11606-014-2889-7.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2008. National Survey on Drug Use and Health, 2008. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Vogels EA, 2019. Millennials Stand Out for Their Technology Use, But Older Generations Also Embrace Digital Life. https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/.Accessed May 10, 2021. [Google Scholar]
- Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ, 2017. E-cigarette use and associated changes in population smoking cessation: evidence from US Current Population Surveys. BMJ 358, j3262. 10.1136/bmj.j3262.Accessed May 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]


