Abstract
The causes and mechanisms of increased cardiac troponin T and I (cTnT and cTnI) concentrations are numerous and are not limited to acute myocardial infarction (AMI) (ischemic necrosis of cardiac myocytes). Any type of reversible or irreversible cardiomyocyte injury can result in elevated serum cTnT and cTnI levels. Researchers and practitioners involved in the diagnosis and treatment of cardiovascular disease, including AMI, should know the key causes and mechanisms of elevated serum cTnT and cTnI levels. This will allow to reduce or completely avoid diagnostic errors and help to choose the most correct tactics for further patient management. The purpose of this article is to discuss the main causes and mechanisms of increase in cardiac troponins concentrations in frequently occurring physiological (physical exertion, psycho-emotional stress) and pathological conditions (inflammatory heart disease, pulmonary embolism, chronic renal failure and sepsis (systemic inflammatory response)) not related to myocardial infarction.
Keywords: diagnostics, differential diagnosis, causes of increased concentration, mechanisms of increase, cardiac troponins, troponin T, troponin I, acute myocardial infarction, physical activity, psycho-emotional stress, myocarditis, endocarditis, pericarditis, sepsis, pulmonary embolism, chronic renal failure
Introduction
Cardiac troponin T and I isoforms (cTnT and cTnI) are expressed in cardiac muscle tissue and are by far the most specific and sensitive indicators for the diagnosis of acute myocardial infarction (AMI).1–4 There are only a few studies that have reported the expression of cTnT and cTnI outside the myocardium, particularly in skeletal muscle,5–7 but the results of these studies are contradictory and have not been confirmed in other research studies.8,9
Methods for determining cTnT and cTnI, which were first developed in the late 90s of the 20th century,10,11 have been continuously improved, increasing analytical sensitivity and specificity. This allowed to accelerate the early diagnosis of AMI and reduce the number of false-positive results due to the interaction of anti-cTnT and anti-cTnI antibodies with skeletal troponins released from muscle fibers in skeletal myopathies and rhabdomyolysis.12–14 Nowadays, there are highly sensitive immunoassays available for determining the hs-cTnT and hs-cTnI concentrations; they allow detecting very low (at the level of several ng/L), but diagnostically significant concentrations of cardiac troponin molecules in blood serum.15,16 This has significantly accelerated the diagnosis of AMI, making it possible to speed up the decision-making on the choice of optimal management tactics for patients arriving with chest pain. For instance, the official edition of the Fourth Universal Definition of Myocardial Infarction (2018) regulates the use of hs-cTnT and hs-cTnI in 1h and 3h diagnostic algorithms.1
Despite the high specificity of cTnT and cTnI, they are not ideal biomarkers for the diagnosis of AMI, since they elevate in blood serum not only in ischemic necrosis of myocardial cells, but also in a number of other pathologies that lead to damage or death of myocardial cells caused by non-ischemic factors.17–19 Also, the improvement in analytical sensitivity of methods for determining cardiac troponins has led to a decrease in specificity, which is expressed by more frequent cases of elevated troponin levels in the absence of myocardial infarction.15,20 On the one hand, it has a great clinical importance due to the opportunity to better assess the degree of myocardial damage in a number of pathological conditions, such as sepsis, pulmonary embolism (PE), inflammatory myocardial diseases, but on the other hand, it can make differential diagnosis more difficult and contribute to incorrect diagnoses. This is especially true in cases where clinicians excessively rely only on the results of patients’ laboratory examinations.
It is very important to understand that an increase in the concentration of cardiac troponins in biological fluids, in particular in blood serum, indicates reversible or irreversible damage to cardiomyocytes, but does not explain the etiopathogenesis of such damage, which may occur in a number of other pathological processes not associated with myocardial infarction.1,14,21–23 And in some cases (impaired renal filtration, false positive results), elevation of cardiac troponins can occur even in the absence of cardiomyocytes damage.12,13,24–26 For this reason, practitioners and researchers should not disregard the data on the possibility of cardiac troponins elevation in other diseases.
Elucidation of the key causes and mechanisms of cardiac troponin elevation is of theoretical value and practical importance.27 This is necessary to improve the differential diagnosis of myocardial infarction from other conditions accompanied by non-ischemic alteration of cardiomyocytes.
The purpose of this article is to discuss the main causes and mechanisms of increase in cardiac troponins concentrations in frequently occurring physiological (physical exertion, psycho-emotional stress) and pathological conditions (inflammatory heart disease, pulmonary embolism, chronic renal failure and sepsis (systemic inflammatory response)) not related to myocardial infarction.
Classification of Major Causes of Elevated Serum Cardiac Troponins Levels Other Than Acute Myocardial Infarction
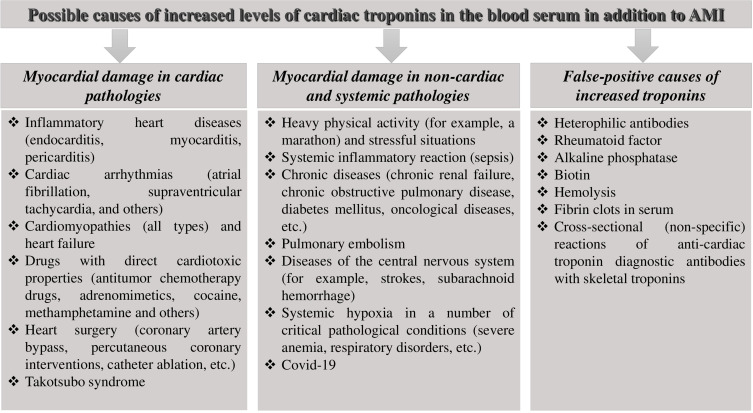
Based on the literature, the most significant causes of cTnT and cTnI elevation, that may complicate differential diagnosis and lead to diagnostic errors, are: severe and/or prolonged physical exertion, inflammatory diseases of cardiac membranes (pericarditis, endocarditis and myocarditis), hereditary and acquired cardiomyopathies, heart failure, Takotsubo syndrome, pulmonary embolism (PE), systemic inflammation (sepsis), acute and chronic renal failure, cardiotoxicity of some therapeutic agents and manipulations, and a number of others. Conventionally, all these conditions can be classified into two groups: 1) myocardial damage in cardiac pathologies, and 2) myocardial damage in non-cardiac and systemic pathologies. False-positive factors (interference) contributing to incorrect (false) overestimation of troponin levels in particular heterophile antibodies, alkaline phosphatase, cross-reactions of anti-cTnT and anti-cTnI antibodies with skeletal troponin isoforms in skeletal myopathies and rhabdomyolysis are considered no less important problems in laboratory diagnosis. These causes of cTnT and cTnI elevation can be conventionally grouped into a third group: false-positive causes of cardiac troponin elevation (Figure 1).
Figure 1.
Classification of the main causes of troponins elevation not associated with myocardial infarction.1,14
Cardiac Troponins During Physical Exertion and Psycho-Emotional Stress: Mechanisms of Elevation and Diagnostic Value
Increased troponins during heavy and/or prolonged physical exertion have been noted in numerous studies almost immediately after the first troponin immunoassays were created.28–30 However, due to the fact that these immunoassays had low specificity and often gave false positive results (diagnostic antibodies against cardiac troponins reacted nonspecifically and cross-reacted with skeletal troponin isoforms).30,31 Nevertheless, some studies have revealed very interesting data, which indicated the adverse effects of some heavy and prolonged loads on the cardiovascular system of athletes.28,32 For example, N. Rifai et (1999) found an increase in troponin T in 26% of athletes after triathlon (swimming 3.9 km → cycling 180.2 km → running 42.2 km), with the highest concentrations recorded in the prize-winners. There was a significant correlation between finishing time and cTnT values (r = −0.65; p < 0.01). There was also a 24% reduction in ejection fraction (measured by echocardiography) when compared with pre-start values (p < 0.002). Based on the results obtained, the researchers concluded that such a load leads to damage to myocardial cells.28
As the sensitivity of immunoassays improved, the number of athletes with positive (elevated) cardiac troponins levels increased. And the highly sensitive methods introduced in 2007–2010 revealed elevated levels in almost all people after prolonged and/or heavy exertion.33–37 A study by Mingels et al (2009) clearly demonstrated that high-sensitivity troponin assays reveal increased concentrations in higher percentage of athletes after physical exertion. Thus, immediately after the marathon, hs-cTnT levels were increased in 81% of marathon runners, while moderately sensitive troponins cTnT and cTnI increased in only 45 and 61% of runners, respectively. Moreover, in some athletes hs-cTnT increased more than 10-fold after the race compared to the values before the start of the marathon. Statistical processing of the results using multiple regression analysis showed that higher troponin concentrations were detected in marathon runners who were older and had less sporting experience. When troponin concentrations in the serum of marathon runners were determined again after 24 hours, troponin levels decreased significantly, but were still about 3–4 times higher than initial values.33
In another study by Scherr et al (2011)36 the dynamic changes in many biomarkers of inflammation and myocardial damage, including hs-cTnT in marathon runners (n=102) were analyzed. In addition to determining indicators before the start, immediately after the finish, and 24 hours after the finish, as examined in a previous study,33 the authors also investigated the hs-cTnT levels 72 hours after the race. The concentrations of hs-cTnT after the marathon were increased about 10-fold compared with the values before the start (from 0.00361 ng/mL to 0.031 ng/mL), but returned to the initial values 72 hours after the finish.36
Richardson et al (2018) in their study also noted a significant increase in hs-cTnT levels (more than 10-fold) in 52 marathon runners in Brighton, UK. The researchers also found that the degree of increase in hs-сTnT was related to the intensity of physical exertion.37
Besides physical activity, psycho-emotional stress can also lead to an increase in levels of high-sensitivity troponins.38–40 For example, Lazzarino et al (2013) were first to discover that the concentration of the cortisol hormone (one of the key biomarkers of psycho-emotional stress) is associated with serum levels of high-sensitivity troponin T (hs-cTnT) (Roche Diagnostics). This relationship was traced on a fairly large sample of patients (n = 508) with no signs of cardiovascular disease.38 The authors emphasize the need for further study of the role of stress in the pathophysiology of myocardial cell damage and the mechanisms underlying the increase in serum hs-cTnT levels.38
The mechanisms of elevation and the diagnostic value of troponins during physical exertion are controversial and their further discussion still continues.40–43 Some researchers think that prolonged/heavy physical exertion leads to cardiomyocytes death through small-scale (subclinical) necrotic and apoptotic processes. Damage and gradual death of cardiomyocytes causes hypertrophy of the remaining contractile cardiomyocytes, but its capabilities are limited and excessive myocardial hypertrophy is considered an extremely dangerous and undesirable sign. Thus, frequent and excessive physical exertion can increase the likelihood of heart failure due to decompensation (cardiosclerosis) in athletes during their lifetime. On this basis, cardiac troponins hold promise for use in sports medicine/cardiology for regulation of acceptable physical exertion levels. In this case, highly sensitive immunoassays are of the greatest value due to their significantly higher detecting ability allowing to detect even the smallest damage to myocytes. Some researchers are of the opinion that heavy exertion cause only transient myocardial ischemia. This opinion is based on the fact that the kinetics of the cardiac troponins levels in the blood serum during physical exertion and AMI differ. Thus, in AMI, the duration of circulation of cardiac troponin molecules in increased concentrations is approximately 1–2 weeks, while during physical exertion, the duration of circulation of troponin molecules in the blood serum does not exceed 1–3 days.33,36 Another argument in favor of the reversibility of myocardial damage is the data of magnetic resonance imaging (MRI) with gadolinium-based contrasts. This MRI method allows detecting inflammatory and sclerotic changes in myocardial tissue. In their study O’Hanlon et al (2010) examined cardiac muscle tissue of athletes using MRI and did not reveal signs of necrosis and cardiosclerosis.41
Transient ischemia under heavy and/or prolonged physical exertion develops because of the imbalance between cellular oxygen demand and its delivery through the coronary arteries. Under conditions of increased physical exertion, myocardial oxygen demand may increase so much that even intact coronary arteries cannot fully meet these needs. At the same time, cardiac muscle tissue is very sensitive to oxygen deficiency, due to a number of factors: high metabolic activity to maintain contractile activity, small reserves of myoglobin, glycogen and other energy substrates. In addition, some biologically active substances and hormones, in particular catecholamines and cortisol, can contribute to the narrowing of the coronary vessels, and as a consequence, a decrease in the supply of the myocardium, impairment of their metabolism and reversible damage.42–44
Another hypothetical mechanism underlying the release of cardiac troponin molecules from cardiomyocytes is the formation of «blebbing vesicles» (membrane vesicles) on the surface of cardiomyocytes. These vesicles on the surface of myocardium and liver cells were first discovered by Schwartz et al (1984) in an in vitro experiment using electron microscopy. The researchers noted that when ischemia is induced, the number of vesicles on the surface of cardiomyocytes increases, and when ischemia is eliminated, the vesicles are reabsorbed back into the cytoplasm.45 Presumably vesicles may contain cytoplasmic proteins of cardiomyocytes, including cardiac troponins. However, this mechanism has been described only in an experimental study in vitro and there is still no reliable evidence in favor of the existence of this mechanism in vivo.
Some existing diagnostic methods are based on the use of physical or psycho-emotional stress. Stress electrocardiography (stress ECG) and stress echocardiography (stress ECHO) with physical and pharmacological load are considered the most important tools for diagnosis of early coronary atherosclerosis (latent coronary heart disease (CHD)), and also allows to predict the unfavorable course of coronary heart disease (CHD).46–48 However, the sensitivity of these functional diagnostic methods (ECG, ECHO) is significantly inferior to the sensitivity of myocardial damage biomarkers, especially high-sensitivity cardiac troponins. Thus, these biomarkers can provide certain advantages. Several researchers have studied the kinetics of serum levels of highly sensitive troponins after stress tests. For example, Samaha et al (2019) examined the kinetics of hs-cTnT concentration (Roche Diagnostics Elecsys 2010) in patients (n = 48) after stress echo in a prospective study. Thirty-three patients underwent stress echo with exercise and 15 patients underwent pharmacological (dobutamine) stress echo. The maximum increase in hs-cTnT levels was observed 4–6 hours after the stress tests, with a more significant increase in concentration (∆hs-cTnT + 9.7 ng/L) after pharmacological stress (dobutamine) than after physical stress (∆hs-cTnT + 2.3 ng/L).49 Other researchers noted a direct correlation between the severity of CHD and the concentration of cardiac troponins both in serum and oral fluid. There was a correlation between the values of troponin I in blood serum and saliva.50–52 Considering the correlations between CHD severity and exercise intensity with troponin concentration in biological fluids,37,49–52 it can be suggested that troponin determination using highly sensitive immunoassays can detect latent myocardial ischemia more precisely and reliably than stress echo and stress ECG or become an important additional criterion for diagnosis and stratification of CHD after stress tests. Besides, there are prospects of using oral fluid as biomaterial for these purposes. However, the works in this area are still few and the number of examined patients is relatively small. Further studies using larger samples are needed to refine the findings.
In some cases, troponin elevation during physical exertion can complicate the differential diagnosis and lead to overdiagnosis of AMI. For example, Manjunath et al (2018) described a case of elevated troponin I (0.123 ng/mL with a norm < 0.055 ng/mL) in a young patient admitted to the emergency department with chest pain characteristic of AMI. Based on these data, clinicians suspected AMI. Additionally, unfavorable family history and lipid profile (significant increase of total cholesterol and low-density lipoproteins) were indicative of AMI. At the same time, ECG, ECHO and coronarography showed no signs of ischemia. Subsequently, careful history taking revealed that the young man is actively engaged in sports and ran several miles on the eve of admission.53
Thus, elevated troponins are often observed during physical exertion, which has been shown by moderately sensitive and highly sensitive methods of cardiac troponin determination. Highly sensitive methods report a much higher percentage of troponin-positive athletes than moderately sensitive methods. Also, highly sensitive assays made it possible to detect troponins after psycho-emotional stress. Due to the frequent elevation of troponins during physical exertion, it may be difficult to make a differential diagnosis. However, a thorough medical history (in particular, sports history), as well as the use of additional diagnostic methods (ECG, ECHO) help to avoid overdiagnosis and, subsequently, unnecessary invasive diagnostic methods (coronarography), incorrect treatment and unnecessary costs for hospitalization. It should also be noted that the use of highly sensitive methods of troponin determination after stress tests (physical, psycho-emotional, pharmacological) has certain prospects for diagnosis and prognosis of latent forms of CHD, and needs further study.
Cardiac Troponins in Inflammatory Heart Diseases (Endo-, Peri-, and Myocarditis): Mechanisms of Elevation and Diagnostic Value
The main mechanism of increasing cardiac markers in myocarditis, particularly troponins, is associated with the direct cytotoxic effect of infectious agents (viruses, bacteria, etc.), toxins, and autoantibodies on cardiomyocytes. The concentration of cardiac troponins in myocarditis, their sensitivity and specificity vary widely. According to several studies, troponins determined by moderately sensitive methods for the diagnosis of myocarditis had a sensitivity of 34–71% and specificity of 86–94%.54–56
Due to the high mortality rate of newborn infants and children from myocarditis, averaging 75 and 25%, respectively, timely diagnosis and optimal therapy in the early stages is of vital importance.57 The clinical picture of infantile myocarditis is often asymptomatic or paucisymptomatic under the guise of other diseases, most often acute respiratory viral infections. In this regard, the search for biomarkers for early diagnosis of myocarditis and assessment of prognosis is considered a priority.57–59
Soongswang et al (2005) report a moderate diagnostic value of cardiac troponins in myocarditis in children. For example, serum troponin T levels > 0.052 ng/L have an analytical sensitivity of 71% and a specificity of 86% for the diagnosis of acute myocarditis in pediatric patients.56 A large retrospective analysis of medical records of Chang et al (2019), which included 94 pediatric patients with acute myocarditis, found that fatal cases were much more common in children with elevated levels of cardiac troponin I, creatine kinase MB isoform; however, elevated concentrations of these biomarkers were associated with arrhythmia, hypotension, acidosis and reduced LVEF. The vast majority of these patients died within the first 72 h. In multivariate analysis, very high cTnI levels (>45 ng/mL) and reduced LVEF were associated with a high risk of death, especially in the first 24 hours. According to the authors, the appointment of more intensive therapy is justified for pediatric patients with elevated concentrations of troponin I.60 In an observational study conducted by Abrar et al (2016), cTnI concentrations and echocardiography data had the greatest diagnostic efficiency, contributing to the correct diagnosis. Troponin I levels also had high prognostic value. In the subgroup of deceased patients, mean serum cTnI concentrations (0.958±1.13 ng/mL) were significantly higher than in the subgroup of surviving patients (p=0.0074). Along with troponins, levels of brain natriuretic peptide (BNP), hypotension and reduced ejection fraction were also associated with adverse outcome.61
High-sensitivity troponins have advantages over moderately sensitive troponins, as well as several other biomarkers and methods of myocarditis diagnosis. Thus, in a study by Ukena et al (2014) measured the concentration of hs-TnT, copeptin and N-terminal N-terminal proBNP (NT-proBNP) in patients with suspected myocarditis (n=70). All admitted patients were divided into 3 groups on the basis of endomyocardial biopsy data (“gold standard” for myocarditis diagnosis): a) acute myocarditis, b) chronic myocarditis, c) no inflammatory process in myocardium. The highest mean levels and concentrations range of hs-cTnT (262.9 [61.4–884.2] pg/mL) were observed in patients with acute myocarditis, and they exceeded hs-cTnT levels both in patients with chronic myocarditis (20.4 [15.6–20.4] pg/mL; p<0.0001) and in patients without myocardial inflammation (19.5 [13.8–50.7] pg/mL; p<0.0001). Serum hs-cTnT levels ≥50 pg/mL had the highest analytical sensitivity and specificity for the diagnosis of acute myocarditis. At the same time, serum levels of other biomarkers (copeptin and NT-proBNP) did not differ significantly in patients of all three subgroups, and thus were not effective for the diagnosis of acute myocarditis.62
The pathogenetic significance of viral persistence in striated cardiac muscle tissue is not definitively known. In many cases it is accompanied by asymptomatic chronic myocarditis which is extremely difficult to diagnose. It is possible to confirm this diagnosis and the presence of viral agents in myocardial cells using polymerase chain reaction (PCR), while endomyocardial biopsy is ineffective. Thus, Ukena et al (2014) examined the viral genome (enteroviruses, adenovirus, herpes viruses and others) in the myocardium by PCR in patients with clinical symptoms of myocarditis. It is quite remarkable that in patients with positive PCR results indicating persistence of viral agents in myocardial tissue, serum hs-cTnT concentration was significantly higher than in patients with negative PCR results [(37.4 (21.9–163.6) pg/mL) versus (20 (14–44.4) pg/mL), p=0.042]. At the same time, endomyocardial biopsy revealed no signs of inflammation in many patients with positive PCR results.62 Thus, elevated levels of hs-cTnT may indicate the damaging effect of these viruses on myocardial cells and allow to detect signs of chronic myocarditis and persistence of viral particles in cardiac muscle tissue. So, the laboratory determination of hs-cTnT is a more effective method than the determination of other biomarkers (copeptin, natriuretic peptides, moderately sensitive troponins) and endomyocardial biopsy, which “does not see” latent (weakly active) inflammatory processes in the myocardium.
However, in some research works in many patients with myocarditis no increase of cardiac troponins concentration in blood serum was registered.54,63 On a basis of these data, an important question arises: Why do cardiac troponins have high sensitivity (90–100%) for ischemic myocardial damage (in AMI), but at the same time are less effective for diagnosis of inflammatory cardiomyocyte damage (in myocarditis)? This circumstance can be explained by several factors. Firstly, analytical characteristics of troponin immunoassays (sensitivity and specificity) significantly differ, and in serum of the same patient troponin concentrations when using different immunochemical test systems will also differ greatly. This is due to the fact that test systems from different manufacturers may contain antibodies to different epitopes (antigenic determinants) of cardiac troponin molecules, while the cardiac troponin molecules in blood are in the form of a heterogeneous fraction (fragments of troponin molecules, free molecules, oligomeric complexes, and their oxidized and phosphorylated derivatives) and the ratio of individual components is constantly changing under the influence of various factors.14,40 Secondly, autoantibodies to cardiac troponins may play a role in false-negative reduction of serum troponin levels in myocarditis. According to Matsumori et al (2011), there is a significant increase in titers of autoantibodies to troponins in the blood of patients with myocarditis.64 Autoantibodies to troponins play a role in the pathophysiology of cardiomyocyte damage and, also, are sources of analytical interference in the determination of troponins, binding epitopes of circulating troponin molecules, which makes them inaccessible for diagnostic antibodies included in immunoassays and leads to false-negative results.64–66
Endocardial and epicardial cells do not contain molecules of cardiac troponins, but endocarditis and pericarditis are often accompanied by an increase in their serum levels, which is probably due to the involvement of myocardial tissue in the inflammatory process.67,68 Thus, Tsenovoy et al (2009) recorded an increase in troponin levels above normal values (>0.4 ng/mL) in 57% of patients with infective endocarditis. It is noteworthy that in-hospital mortality was higher among troponin-positive patients than in troponin-negative patients. In addition, the need for valve replacement surgery in patients with elevated levels of cardiac troponin I occurred significantly more often than in troponin-negative patients (51% versus 15%; p<0.005).69 According to another retrospective study, troponin I was elevated in 65% of patients with infective endocarditis. Elevated levels of troponin I were also associated with a poor prognosis (combination of adverse events): death, myocardial abscess and CNS injury (p<0.001).70
According to a study by Imazio et al (2003) troponin I exceeded the upper reference limit (1.5 ng/mL) in 32% of patients with acute viral or idiopathic pericarditis. The authors note that in some patients the kinetics of serum troponin levels in pericarditis corresponded to the kinetics of troponins in myocardial infarction. There was also an increase in the concentration of creatine kinase MB and left ventricular regional wall motion abnormality (LVWMAs) according to echocardiography. These features led to incorrect preliminary diagnoses in some patients at the admission stage. Elevated troponin I levels in patients with acute pericarditis were significantly associated with younger age, gender (male), ST-segment elevation, and pericardial effusion (p=0.007). At the same time, in this study, positive cTnI was not associated with poor prognosis in acute pericarditis,71 in contrast to the above studies on the prognostic value of cardiac troponins in myocarditis and endocarditis.
Gamaza-Chulian et al (2014) in their study revealed a higher prevalence of elevated levels of cardiac troponins in patients with pericarditis. Troponin T levels were elevated in 61% of patients with pericarditis. At the same time, there were no deaths during hospital stay in troponin-positive patients with pericarditis.72
Thus, cardiac troponin levels can be elevated in quite a significant number of patients (according to many studies, more than 50%) with inflammatory myocardial diseases (endocarditis, myocarditis, pericarditis). This should be taken into account by physicians in differential diagnosis to prevent misdiagnosis. Significant differences in the prevalence of elevated serum troponin levels in these nosologies are associated with the analytical characteristics of the immunoassays used. Autoantibodies to cardiac troponin molecules in case of myocarditis, are also a very interesting cause of false negative results requiring further study. Cardiac troponins in endocarditis and myocarditis, but not in pericarditis, are very valuable prognostic biomarkers.
Cardiac Troponins in Pulmonary Embolism: Diagnostic Value and Mechanisms of Elevation
Pulmonary embolism (PE) is a frequent cause of troponin elevation. Approximately 50% of patients feel “coronary-like” pain, which leads to difficulties and errors in differential diagnosis.73,74
Results of a study by Giannitis et al (2000) led to the conclusion that prevalence of cardiac troponin concentration increase in PE depends on the volume of pulmonary vascular bed damage. Thus, in massive pulmonary embolism, elevated troponin levels were recorded in 50% of patients, in submassive PE - 35%, and in nonmassive PE - just isolated cases. In addition, elevated cTnT levels in PE were associated with increased hospital mortality, cardiogenic shock, and the need for resuscitation. Patients with PE and elevated cTnT levels were also much more likely to require inotropic support and mechanical ventilation compared with troponin-negative PE patients.75
A study conducted by Kilinc et al (2012) found that elevated cTnI levels (Beckman Coulter) were much more frequent in patients with a confirmed PE diagnosis (50.8% versus 11.6%; p<0.001), which indicates a moderate diagnostic value of cardiac troponins in case of PE.76 At the same time, by analogy with the research outcomes of Giannitis et al (2000)75 the troponin level also depended on the volume of pulmonary vascular bed damage. For instance, elevated cTnI levels were found in 80% of patients with massive PE, 56% of patients with submassive PE, and 38% of patients with nonmassive PE. The researchers found that elevated cTnI levels for the diagnosis of PE had the following analytical parameters: sensitivity, 51%; specificity, 88%. When analyzing the diagnostic efficiency of a combination of elevated levels of cTnI and D-dimer, the sensitivity indicator reached 93%, but the specificity decreased to 54%.76
According to a large meta-analysis that included 20 clinical trials and involved 1985 patients, cardiac troponins have high prognostic value in PE. For example, among 618 patients with elevated cardiac troponin levels, 122 died [(19.7%; 95% confidence interval (CI) 16.6–22.8)]. Whereas, among 1367 subjects with reference troponin values, mortality was much lower - 51 (3.7%; 95% CI 2.7–4.7). At the same time, the prognostic value of cardiac troponin I and cardiac troponin T was almost the same. According to the results of meta-analysis, high serum levels of cardiac troponins are significantly associated with short-term mortality in patients with PE [odds ratio (OR) 5.24; 95% CI 3.28–8.38]. Even in the subgroup of hemodynamically stable PE patients, elevated serum troponin concentrations were also associated with a high risk of death (OR 5.90; 95% CI 2.68–12.95).77 Thus, focusing on the elevated concentrations of cardiac troponins in case of PE, it is possible to identify patients with a high risk of adverse outcomes. Many leading experts came to the conclusion that cardiac troponins have a high prognostic value in PE, which is reflected in clinical guidelines. In accordance with the Clinical Guidelines of the European Society of Cardiology (ESC) for the diagnosis and treatment of acute PE, cardiac troponins are recommended for predicting and stratification of risk in patients with PE.78,79
The kinetics of cardiac troponin concentration in PE differs from the kinetics of troponin concentration in AMI, and this may indicate different mechanisms of cardiomyocyte damage and troponin levels elevation. According to the results of the study, positive cTnT levels were noted in 56% of patients admitted with acute PE. After 10 hours, serum cTnT levels reached peak values (median 0.48 μg/L), after which gradually decreased, and the duration of elevated values of troponin molecules circulation in the bloodstream was 30–40 hours. In myocardial infarction, troponin levels elevated to median concentrations (0.22–0.41 μg/L on average) much more slowly, with the curves characterizing the kinetics of cTnT concentration having several sharp up and down slopes and the duration of elevated values of troponin molecules circulation of more than 120 hours.80
High-sensitivity cardiac troponins have an advantage over standard moderately sensitive troponins, which was shown by Lankeit et al (2010). In this prospective study, the authors examined the prognostic value of moderate- and high-sensitivity troponin T (hs-cTnT) in patients with a confirmed PE (n=156). Hs-cTnT concentrations exceeded the 99th percentile (14 ng/mL) in about 65% of patients. Hs-cTnT levels above 99th percentile had excellent negative and positive predictive values (NPV= 100%, PPV = 100%). Elevated serum hs-cTnT levels (>14 ng/L) were associated with a decreased probability of long-term survival in patients with PE (p=0.029). According to Cox regression analysis, hs-cTnT was the only biomarker predicting an increased mortality risk in the long term. However, in 50% of patients with poor prognosis, the concentration of moderately sensitive troponin T was within the normal range, and when using this marker for risk stratification, many patients could be mistakenly assigned to the group of patients with a favorable prognosis. Thus, the results of this study emphasize the significant advantage of high-sensitivity troponin T over moderately sensitive troponin T for risk stratification of patients with PE.81
Right ventricular (RV) dysfunction is one of the key indicators that determines the prognosis of patients with PE. Patients with PE and developed RV dysfunction have higher (2–5 times) probability of death, than patients with PE, but with no RV dysfunction. Since the concentration of cardiac troponins in the blood serum is associated with the degree of RV dysfunction, they can complement the data of echocardiographic examination or be used as an alternative to echocardiography to detect RV dysfunction in patients with PE.82 The association of serum troponin levels with the degree of RV dysfunction may indicate that cardiac troponin molecules are released predominantly from cardiac myocytes of the right ventricle as a result of reversible damage (nonmassive PE) or cell death (massive PE). Thus, the determination of the cardiac troponins concentration in PE is of great clinical importance. For instance, in a study by Cotugno et al (2017) it was discovered that serum levels of cTnT and NT-proBNP were significantly higher in patients with acute PE and RV dysfunction than in patients with PE but no RV dysfunction. At the same time, NT-proBNP showed higher analytical sensitivity in detecting RV dysfunction than moderately sensitive troponin T.83
Establishing a short-term and long-term prognosis in patients with PE is important for optimizing the treatment and diagnostic process.84 For example, patients with favorable prognosis (lower or negative serum cardiac troponins levels) can receive less aggressive therapy and the duration of their hospital stay can be shortened. Although high-sensitivity cardiac troponins are much better suited for risk stratification in PE patients than moderately sensitive troponins, their use may further complicate the differential diagnosis of PE and myocardial infarction. This is due to a number of similar clinical symptoms, more frequent elevation of troponin concentrations, and some similarities in kinetics of troponin concentrations in PE and myocardial infarction.
As an additional method to solve the problem of differential diagnosis of PE and myocardial infarction, researchers Kim et al (2017) suggested to use D-dimer/troponin I concentration ratio. In a prospective study including 771 patients with AMI and 233 patients with acute PE, researchers examined the diagnostic value of D-dimers, troponin I, and their ratio. An increase in D-dimer concentration was observed in half of the patients with AMI while increase in cTnI concentration was observed in 38% of the patients with PE. The upper threshold laboratory values for the differential diagnosis of PE and AMI were as follows: 1.12 mg/L for D-dimer (analytical sensitivity and specificity were 81.1% and 70.2%, respectively) and 0.72 ng/mL for cTnI (analytical sensitivity and specificity were 80.6% and 78.9%, respectively). When the D-dimer/cTnI ratio was used, the analytical sensitivity and specificity in the diagnosis of these diseases were higher than when separate D-dimer and cTnI concentrations were used. Thus, the authors calculated that with a D-dimer/cTnI ratio >1.82, the analytical sensitivity and specificity for the differential diagnosis of PE and AMI were 93% and 86%. On the basis of these results, the researchers believe that invasive coronarography for differential diagnosis and clarification of the diagnosis could have been avoided in the majority of admitted patients.85
The mechanisms of elevated serum cardiac troponin levels in PE appear to depend on the severity of PE. It is assumed that in nonmassive PE, reversible damage of RV cardiomyocytes and release of cytosolic troponins pool through the cell membrane due to increased afterload occur.86,87 In submassive and massive PE, RV overload is much more pronounced and cardiomyocyte necrosis develops. Probably the cause of cardiac myocyte necrosis in PE are sharp overload and expansion of RV, which might lead to compression of small branches of coronary arteries, passing in myocardial tissue thickness, causing disruption of hemoperfusion and delivery of oxygen and metabolic substrates to myocardial cells.88 The existence of this mechanism is confirmed by the results of pathological studies, which revealed small foci of necrosis in the RV myocardium with intact coronary vessels.82,88,89
Cardiac Troponins in Chronic Renal Failure: Mechanisms of Elevation and Diagnostic Value
According to modern concepts, cardiac troponins can be considered as products of normal myocardial metabolism, and “there are no more troponin-negative patients”.40,90 These concepts were formed due to the creation of the latest (highly sensitive and ultrasensitive) immunoassays for the detection of cardiac troponin molecules.91,92 For instance, ultrasensitive test systems, can detect cardiac troponin molecules in all healthy patients at concentrations below the threshold level (99th percentile). However, if this threshold is exceeded, troponin concentrations are considered abnormal and physicians should carefully review the possible causes of elevation.
The detection of cardiac troponins in healthy patients has led researchers to think about the possible causes of their release from cardiomyocytes under normal conditions.40 Also, the mechanism of elimination of troponin molecules from the bloodstream is a very significant factor that may affect the serum troponin concentration. Currently, the following methods have been established for elimination of troponins from blood serum:
1) In cells of the reticuloendothelial system (intracellular cleavage by specific proteases);93,94
2) In serum (extracellular cleavage by proteolytic enzymes). It has now been proven that an enzyme of the hemostasis system (thrombin) causes specific cleavage of the troponin T molecule into two fragments;95–98
3) Renal (glomerular) filtration.99–101
Glomerular filtration is considered to be the most discussed and perhaps the key mechanism of cardiac troponin elimination in terms of clinical significance. According to some researchers, the involvement of the kidneys in cardiac troponin elimination is highly controversial and doubtful, since cardiac troponin molecules were not detected in urine of most patients.99 Nevertheless, elevated cardiac troponin concentrations in patients with chronic renal failure without any signs of cardiovascular disease have often been observed in clinical practice.100 These findings provide indirect evidence of renal involvement in the elimination of troponins from serum.
One of the most significant pieces of evidence for the role of renal filtration in elevating serum troponins is the CRIC (Chronic Renal Insufficiency Cohort) study, which included 2464 patients with chronic renal failure but without overt signs of cardiovascular disease. Elevated hs-cTnT values were found in 81% of patients participating in this study. Lower glomerular filtration rate (GFR) was associated with higher troponin T concentrations: patients with GFR <30 mL/min had 3-fold higher troponin levels than patients with GFR >60 mL/min. The correlation between lower GFR values and higher troponin T levels is partly explained by the decreased renal clearance of troponin T. However, intact protein molecules of cardiac troponins are relatively large and must obviously be pre-fragmented into smaller molecules by proteolytic enzymes in order to pass through the glomerular filter. Small fragments of troponin T are small enough and, presumably, can be filtered by the kidneys, and if renal filtration is impaired, these fragments will accumulate and make an important contribution to the elevation of serum troponin levels in CRF. Nevertheless, some patients with low GFR in the CRIC study had normal troponin T concentration, which indicates that impaired renal clearance is not the only reason for the rise in troponins in patients with CRF.100
Another confirmation of the dependence of serum troponin levels on GFR is the study by Wilhelm et al (2013)102 and Rosjo et al (2011),103 in which serum troponin and creatinine levels correlate: r=0.554; p<0.001 and r=0.32, p<0.001, respectively. These data prove the relationship of elevated serum cardiac troponin levels with impaired renal elimination (decreased GFR) in patients with renal failure. However, these data provided just indirect evidence for the role of kidneys in troponin elimination.
The first direct evidence was recently presented by Croatian researchers Pervan et al (2017). hs-cTnI (troponin I, high-sensitivity) was detected in the urine of all patients using a highly sensitive immunoanalyzer Abbott Architect i1000SR (USA), and in the morning urine portion of normotensive patients, the average concentration of hs-cTnI was significantly lower than in patients with high blood pressure (14.95 pg/mL vs 26.59 pg/mL; p<0.05). The researchers also noted that hs-cTnI levels decreased when blood pressure was lowered with antihypertensive drugs. Thus, according to the authors, the determination of hs-cTnI concentration in urine can be used as an additional method for the diagnosis and monitoring of arterial hypertension.104 Since blood pressure is one of the key factors in increasing GFR, this study can be considered as an additional reliable confirmation of the dependence of serum levels of cardiac troponins on GFR. Also, according to several clinical studies,102,103 serum cardiac troponins correlate with the levels of creatinine, an endogenous metabolite that used to calculate GFR as well.
The most likely reason why some researchers have failed to detect troponin in urine and thereby question the mechanism of renal elimination is the analytical sensitivity of immunoassays.104,105 Thus, the levels of troponins in urine are small and range from only a few ng/L to several tens of ng/L - these concentrations can be detected only by highly sensitive and ultrasensitive immunoassays, while in conventional moderately sensitive methods used previously, the minimum detectable concentration was, as a rule, not less than 100 ng/l. Therefore, this low concentration of troponin molecules in the urine remained as insignificant and “invisible” to standard moderately sensitive immunoassays.
Other putative mechanisms responsible for the increase in cardiac troponins in chronic renal failure are 1) the “skeletal hypothesis”,6,106,107 2) the direct damaging effect on cardiomyocytes of toxins accumulated in CRF,108,109 3) myocardial volume overload and its hypertrophy.110,111
The skeletal hypothesis was proposed by several scientists who discovered the expression of cardiac troponin isoforms in striated skeletal muscle. Researchers believe that in CRF, skeletal muscle fibers are altered (uremic skeletal myopathy), followed by reparative regeneration processes, during which the expression of cardiac troponin isoforms occurs. Some studies have also shown that the expression of cardiac-specific troponins in skeletal muscle is normal for the embryonic period of human development. V. Ricchiutti and F. Apple (1999) reported the detection of cardiac troponin T messenger RNA in skeletal muscle biopsy specimen in 50% of patients with end-stage CRF.6 However, a study by Haller et al (1998) did not find cardiac troponin T isoforms in biopsy specimen of the anterior abdominal wall muscles in patients with CRF.106 A recent study also showed no traces of cardiac troponin expression in skeletal muscle.9 It can be assumed that earlier studies noting the expression of cardiac-specific troponins in striated skeletal muscle obtained false-positive results because of the low specificity of the methods used. Therefore, the “skeletal hypothesis” is a dubious and unlikely mechanism for increasing cardiac troponins in patients with CRF.
Considering the presence of a correlation between the level of cardiac troponins and toxic products of nitrogen metabolism, including creatinine,102,103 it can be assumed that there is a direct damaging effect of these compounds on cardiomyocytes.
Also, with a prolonged course of CRF due to an increase in the volume of circulating blood, myocardial overload and gradually increasing hypertrophy of the heart muscle take place. With a sharp hypertrophy of myocardium, narrowing of subepicardial branches of the coronary arteries may occur due to their mechanical compression, with subsequent damage and death of cardiomyocytes, which increases the release of troponin molecules. The existence of this mechanism is confirmed by pathological studies, in which foci of microinfarction and cardiosclerosis were identified in people who died from CRF.110,111 Moreover, the volume of the myocardium determines the levels of highly sensitive troponins in healthy people, which is confirmed by the existence of gender characteristics of the 99th percentile, according to which the concentration of cardiac troponins in men is approximately 1.5–2.5 times higher than in women.14,112
According to the results of several large meta-analyses,113–115 cardiac troponins in chronic renal failure have a high prognostic value, allowing to identify patients with an increased risk of general and cardiovascular death.
Therefore, CRF is a common cause of elevated cardiac troponins in clinical practice. The main mechanisms of increased cardiac troponins in СКА are considered to be impaired elimination of molecules from serum due to decreased GFR, direct damaging effect of toxic products of nitrogen metabolism, and increased myocardial hypertrophy. Another described mechanism (“skeletal hypothesis”) is contradictory and unlikely. Cardiac troponins can be used in the management of patients with CRF to stratify risk.
Cardiac Troponins in Systemic Inflammatory Response (Sepsis): Mechanisms of Elevation and Diagnostic Value
Sepsis leads to damage to almost all organs and systems of the body, including the cardiovascular system, and causes the development of severe multiple organ failure.116 The mechanisms of cardiomyocyte damage and increasing serum cardiac troponin concentrations are very diverse. Myocardial ischemia can be considered as one of the mechanisms of increasing serum cardiac troponin levels in sepsis, which develops due to the imbalance between myocardial cell oxygen demand and its delivery. In contrast to the most common type 1 myocardial infarction (associated with atherothrombosis), myocardial ischemia in sepsis develops with no signs of acute atherothrombosis, ie with intact coronary arteries. So, this mechanism of ischemia development is almost similar to the formation of ischemia in type 2 myocardial infarction. The imbalance between myocardial oxygen demand and its delivery is caused by a number of pathophysiological pathways, of which the most significant are fever, arterial hypotension, respiratory failure (respiratory hypoxia), disorders of acid-base and fluid and electrolyte balance, as well as microcirculatory disorders, which are accompanied by a decrease in hemoperfusion of all organs, including cardiac muscle tissue. While the latter is one of the most vulnerable to a deficiency of oxygen and metabolic substrates. Against the background of fever and arterial hypotension, tachycardia intensifies, which in turn increases cardiomyocyte demand for oxygen and metabolic substrates, while their delivery through coronary arteries may be reduced due to arterial hypotension. Under conditions of oxygen deficiency, myocardial cells are forced to switch to anaerobic metabolism (glycolysis), which is accompanied by an increase in lactate formation and a shift of acid-base balance toward acidosis. Acidosis, in turn, causes additional disruption of enzyme proteins involved in energy (metabolic) pathways (Krebs cycle, Cori cycle, fatty acid oxidation, etc.) in myocardial cells. These mechanisms form a vicious pathogenetic circle that aggravates myocardial ischemia and, depending on the severity of such disorders, might lead to reversible or irreversible damage (necrosis) of cardiomyocytes and release of cardiac troponin molecules into the bloodstream.117–119
There are also other opinions concerning the mechanisms of cardiomyocyte damage in sepsis. For instance, some researchers suggest that the leading role in myocardial cell alteration during systemic inflammatory response is played by inflammatory mediators, in particular tumor necrosis factor-alpha (TNF-α), interleukins-1, 6 (IL-1, IL-6) and others, as well as bacterial toxins (exotoxins and endotoxins), which have direct negative (cytotoxic) effect on cardiac muscle tissue cells.120,121 The evidence for the existence of such a mechanism is presented in an experimental study conducted by Kumar et al (2007). For instance, with the introduction of blood serum obtained from patients with sepsis and containing increased levels of the major mediators of inflammation (TNF-α, IL-1, IL-6, and others), a decrease in the amplitude and rate of cardiomyocytes contraction was observed.121
Microthrombosis of small branches of coronary arteries due to disorders of the hemostatic system and increased cardiomyocyte death by apoptosis caused by inflammatory cytokines and bacterial toxins can be additional mechanisms of troponin levels increase in sepsis patients.119,122 Also, in some cases severe sepsis (septic shock) can be accompanied by severe multiple organ pathologies, including renal failure,102,123 which, as described above, can lead to increased levels of cardiac troponins in blood due to their reduced elimination through the glomerular filter, as well as direct damage to cardiomyocytes by products of nitrogen metabolism.
Considering the above, it is obvious that the mechanisms of cardiac troponin elevation in systemic inflammatory response are diverse and their complex contribution with predominance of a particular mechanism in a particular situation (for example, the cause of sepsis and/or the severity of sepsis) is very likely.
The diagnostic value of cardiac troponins in sepsis is clearly demonstrated by the results of meta-analysis124,125 and several clinical studies.102,103 According to these studies, cardiac troponins are valuable prognostic markers. A large meta-analysis conducted by Bessiere et al (2013) with 13 clinical trials and 1227 patients with sepsis involved, showed that elevated serum cardiac troponin concentrations were significantly associated with a higher risk of death (OR 1.91; CI 1.62–2.24). Moreover, elevated serum levels of cardiac troponins were noted on average in 61% (95% CI 58–64%) of patients with sepsis.124
In several studies, cardiac troponin levels of patients with sepsis were determined using high-sensitivity methods, and then diagnostic value was compared with troponin results determined using moderately sensitive methods. In a study by Rosjo et al (2011) the concentration of troponin T in 207 patients was assessed by the moderately sensitive method (cTnT) and the highly sensitive method (hs-cTnT). Serum hs-cTnT levels were elevated in 166 (80%) patients, whereas cTnT concentration was elevated in only 86 (42%) patients.102 Thereby, high-sensitivity methods detect myocardial damage in a larger number of patients with sepsis compared to moderately sensitive immunoassays. Also, the research by Rosjo et al (2011) revealed a correlation of serum hs-cTnT levels with patients’ SAPS II score (r=0.27, p<0.001), severity of multiple organ dysfunction on SOFA scale (r=0.30, p<0.001) and serum creatinine levels (r=0.32, p<0.001) indicative of renal failure. In the subgroup of deceased patients, the median hs-cTnT values [0.054 (0.022–0.227) μg/L] were significantly higher (p=0.047) than the median hs-cTnT levels in the subgroup of surviving patients [0.035 (0.015–0.111) μg/L], which indicates the high prognostic value of hs-cTnT. However, the levels of moderately sensitive hs-cTnT did not differ significantly (p=0.14) in the subgroups of surviving and deceased patients. Quite remarkably, serum hs-cTnT levels in patients with severe sepsis (septic shock) were significantly higher than in patients without septic shock [0.044 (0.024–0.171) µg/L versus 0.033 (0.012–0.103) µg/L; p=0.03], which indicates that hs-cTnT levels can be used to determine sepsis severity. At the same time, serum levels of moderately sensitive cTnT in patients with septic shock and patients without septic shock did not differ significantly.102
According to Wilhelm et al (2014) elevated hs-TnT levels were recorded in 63% of patients admitted to the emergency department with sepsis. And higher concentrations of hs-TnT were noted in those patients who had more severe sepsis (52.6 pg/mL) and septic shock (65.1 pg/mL), compared with patients who had uncomplicated sepsis (14.5 pg/mL; p<0.001). It should also be noted that hs-cTnT was elevated in 34.5% of patients with sepsis, but without renal insufficiency, which further suggests the role of other mechanisms (besides weakened elimination of cardiac troponins from the blood serum through the glomerular filter) in increasing serum hs-TnT levels in the systemic inflammatory response. It is also quite remarkable that serum hs-cTnT concentrations were significantly correlated with several inflammatory markers, such as IL-6 (r=0.193; p<0.005), procalcitonin (r=0.265; p<0.001). This may indicate that inflammatory cytokines make a certain contribution to the increase in serum hs-TnT levels due to the mechanisms of direct cytotoxic action and enhanced apoptosis. The correlation between hs-TnT and serum creatinine (r=0.554; p<0.001) noted by the authors confirms the important role of impaired renal function as a mechanism for increasing cardiac troponins in sepsis. Besides that, hs-cTnT levels closely correlated with the APACHE II severity of disease classification system scale (r=0.654; p <0.001) and in deceased patients serum hs-TnT concentrations were significantly higher than in surviving patients (AUC 0.72; p<0.001), which also confirms the high prognostic value of hs-TnT in patients with sepsis.103
This means that cardiac troponin levels can increase quite often in patients with, and the prevalence and degree of troponin elevation depends on the severity of sepsis and the presence of concomitant multiple organ pathologies, particularly renal failure. The increase in concentration of cardiac troponins in sepsis is based on the following mechanisms: ischemia of cardiomyocytes, apoptosis, cytotoxic action of inflammatory cytokines and impaired elimination of troponin molecules from blood serum into urine through a glomerular filter. At the same time, the results of clinical studies show that it is better to use high-sensitivity cardiac troponins to assess the severity and prognosis of patients. However, due to the higher frequency of hs-cTnT elevation in sepsis, additional difficulties and doubts may arise in the differential diagnosis from other nosologies accompanied by elevated cardiac troponin concentrations.
Conclusion
On the basis of the conducted literature review, it can be concluded that there are a significant number of causes for cardiac troponin concentration elevation. The physiological (heavy and intensive physical exertion, stress) and pathological (pulmonary embolism, inflammatory myocardial disease, chronic renal failure and sepsis) conditions discussed in the article are quite common causes of increased cardiac troponin concentration. At the same time, modern highly sensitive methods for cardiac troponins determination detect troponin molecules more often and in a larger number of individuals engaged in heavy physical exertion or suffer from the aforementioned pathologies. Thus, for the sake of increasing one important criterion of laboratory diagnostics (sensitivity of immunoassays), the developers sacrificed another important criterion for diagnostics (specificity of immunoassays). This circumstance should be taken into account by clinicians when interpreting the results of laboratory examination of patients admitted with suspected acute myocardial infarction. Otherwise, the likelihood of a misdiagnosis and the subsequent appointment of incorrect treatment will increase significantly. The mechanisms of elevating the concentration of cardiac troponins in the blood serum under these conditions are quite numerous and differ from the mechanism of elevating cardiac troponins in acute myocardial infarction. Understanding the specific mechanisms of high-sensitivity cardiac troponin concentration elevation will not only improve the differential diagnosis of acute myocardial infarction from the above conditions, but also bring in additional diagnostic methods. For example, high-sensitivity troponins can be determined in serum or other biological fluids after physical or pharmacological exercise, and thus cardiac troponins can be used as markers of latent ischemic heart disease. Determination of serum cardiac troponin molecule concentrations can be used to detect cardiomyocyte damage in pulmonary embolism, inflammatory heart disease (endocarditis, myocarditis, pericarditis), sepsis, and chronic renal failure. Due to the fact that elevated levels of cardiac troponins reflect the degree of myocardial damage in these nosologies and have prognostic value, this additional diagnostic method will help to improve existing algorithms for the management of patients suffering from pulmonary embolism, inflammatory heart diseases (endocarditis, myocarditis, pericarditis), sepsis and chronic renal failure.
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Thygesen K, Alpert JS, Jaffe AS, et al.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618–e651. doi: 10.1161/CIR.0000000000000617 [DOI] [PubMed] [Google Scholar]
- 2.Chaulin AM, Duplyakov DV. Biomarkers of acute myocardial infarction: diagnostic and prognostic value. Part 1. J Clin Pract. 2020;11(3):75–84. In Russian. doi: 10.17816/clinpract34284 [DOI] [Google Scholar]
- 3.Mair J, Lindahl B, Hammarsten O, et al. How is cardiac troponin released from injured myocardium? Eur Heart J Acute Cardiovasc Care. 2018;7(6):553–560. doi: 10.1177/2048872617748553 [DOI] [PubMed] [Google Scholar]
- 4.Chaulin AM, Duplyakov DV. Biomarkers of acute myocardial infarction: diagnostic and prognostic value. Part 2. J Clin Pract. 2020;11(4):70–82. In Russian. doi: 10.17816/clinpract48893 [DOI] [Google Scholar]
- 5.Messner B, Baum H, Fischer P, et al. Expression of messenger RNA of the cardiac isoforms of troponin T and I in myopathic skeletal muscle. Am J Clin Pathol. 2000;114(4):544–549. doi: 10.1309/8KCL-UQRF-6EEL-36XK [DOI] [PubMed] [Google Scholar]
- 6.Ricchiutti V, Apple FS. RNA expression of cardiac troponin T isoforms in diseased human skeletal muscle. Clin Chem. 1999;45(12):2129–2135. doi: 10.1093/clinchem/45.12.2129 [DOI] [PubMed] [Google Scholar]
- 7.Apple FS, Ricchiuti V, Voss EM, Anderson PA, Ney A, Odland M. Expression of cardiac troponin T isoforms in skeletal muscle of renal disease patients will not cause false-positive serum results by the second generation cardiac troponin T assay. Eur Heart J. 1998;19(Suppl N):N30–N33. [PubMed] [Google Scholar]
- 8.Hammerer-Lercher A, Erlacher P, Bittner R, et al. Clinical and experimental results on cardiac troponin expression in Duchenne muscular dystrophy. Clin Chem. 2001;47(3):451–458. doi: 10.1093/clinchem/47.3.451 [DOI] [PubMed] [Google Scholar]
- 9.Schmid J, Liesinger L, Birner-Gruenberger R, et al. Elevated cardiac troponin T in patients with skeletal myopathies. J Am Coll Cardiol. 2018;71(14):1540–1549. doi: 10.1016/j.jacc.2018.01.070 [DOI] [PubMed] [Google Scholar]
- 10.Cummins B, Auckland ML, Cummins P. Cardiac-specific troponin-I radioimmunoassay in the diagnosis of acute myocardial infarction. Am Heart J. 1987;113(6):1333–1344. doi: 10.1016/0002-8703(87)90645-4 [DOI] [PubMed] [Google Scholar]
- 11.Katus HA, Looser S, Hallermayer K, et al. Development and in vitro characterization of a new immunoassay of cardiac troponin T. Clin Chem. 1992;38(3):386–393. doi: 10.1093/clinchem/38.3.386 [DOI] [PubMed] [Google Scholar]
- 12.Li SF, Zapata J, Tillem E. The prevalence of false-positive cardiac troponin I in ED patients with rhabdomyolysis. Am J Emerg Med. 2005;23(7):860–863. doi: 10.1016/j.ajem.2005.05.008 [DOI] [PubMed] [Google Scholar]
- 13.Du Fay de Lavallaz J, Zehntner T, Puelacher C, et al. Rhabdomyolysis: a noncardiac source of increased circulating concentrations of cardiac troponin T? J Am Coll Cardiol. 2018;72(23):2936–2937. doi: 10.1016/j.jacc.2018.09.050 [DOI] [PubMed] [Google Scholar]
- 14.Chaulin A. Cardiac troponins: contemporary biological data and new methods of determination. Vasc Health Risk Manag. 2021;17:299–316. doi: 10.2147/VHRM.S300002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaulin AM, Karslyan LS, Bazyuk EV, et al. [Clinical and diagnostic value of cardiac markers in human biological fluids]. Kardiologiia. 2019;59(11):66–75. In Russian. doi: 10.18087/cardio.2019.11.n414 [DOI] [PubMed] [Google Scholar]
- 16.Chaulin A. Clinical and diagnostic value of highly sensitive cardiac troponins in arterial hypertension. Vasc Health Risk Manag. 2021;17:431–443. doi: 10.2147/VHRM.S315376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindner G, Pfortmueller CA, Braun CT, Exadaktylos AK. Non-acute myocardial infarction-related causes of elevated high-sensitive troponin T in the emergency room: a cross-sectional analysis. Intern Emerg Med. 2014;9(3):335–339. doi: 10.1007/s11739-013-1030-y [DOI] [PubMed] [Google Scholar]
- 18.Long B, Long DA, Tannenbaum L, Koyfman A. An emergency medicine approach to troponin elevation due to causes other than occlusion myocardial infarction. Am J Emerg Med. 2020;38(5):998–1006. doi: 10.1016/j.ajem.2019.12.007 [DOI] [PubMed] [Google Scholar]
- 19.Chaulin AM, Abashina OE, Duplyakov DV. Pathophysiological mechanisms of cardiotoxicity in chemotherapeutic agents. Russ Open Med J. 2020;9:e0305. doi: 10.15275/rusomj.2020.0305 [DOI] [Google Scholar]
- 20.Jarolim P. High sensitivity cardiac troponin assays in the clinical laboratories. Clin Chem Lab Med. 2015;53(5):635–652. doi: 10.1515/cclm-2014-0565 [DOI] [PubMed] [Google Scholar]
- 21.Chaulin AM, Svechkov NA, Volkova SL, Grigoreva YV. Diagnostic value of cardiac troponins in elderly patients without myocardial infarction. Modern Prob Sci Educ. 2020;6. In Russian. doi: 10.17513/spno.30302 [DOI] [Google Scholar]
- 22.Chaulin AM, Duplyakov DV. MicroRNAs in atrial fibrillation: pathophysiological aspects and potential biomarkers. Int J Biomed. 2020;10(3):198–205. doi: 10.21103/Article10(3)_RA3 [DOI] [Google Scholar]
- 23.Chaulin AM, Duplyakov DV. Arrhythmogenic effects of doxorubicin. Complex Issues Cardiovasc Dis. 2020;9(3):69–80. In Russ. doi: 10.17802/2306-1278-2020-9-3-69-80 [DOI] [Google Scholar]
- 24.Kanderian AS, Francis GS. Cardiac troponins and chronic kidney disease. Kidney Int. 2006;69(7):1112–1114. doi: 10.1038/sj.ki.5000174 [DOI] [PubMed] [Google Scholar]
- 25.Nørlund H, Bovin A. [False positive troponin I due to heterophile antibodies]. Ugeskr Laeger. 2017;179(49):V05170412. Danish. [PubMed] [Google Scholar]
- 26.Kaplan A, Orhan N, Ilhan’ E. False positive troponin levels due to heterophil antibodies in a pregnant woman. Turk J Emerg Med. 2016;15(1):47–50. doi: 10.5505/1304.7361.2014.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chaulin AM, Karslyan LS, Nurbaltaeva DA, et al. Cardial troponins metabolism under normal and pathological conditions. Siberian Med Rev. 2019;6:5–14. doi: 10.20333/2500136-2019-6-5-14 [DOI] [Google Scholar]
- 28.Rifai N, Douglas PS, O’Toole M, et al. Cardiac troponin T and I, echocardiographic [correction of electrocardiographic] wall motion analyses, and ejection fractions in athletes participating in the Hawaii Ironman Triathlon. Am J Cardiol. 1999;83(7):1085–1089. doi: 10.1016/s0002-9149(99)00020-x [DOI] [PubMed] [Google Scholar]
- 29.Tulloh L, Robinson D, Patel A, et al. Raised troponin T and echocardiographic abnormalities after prolonged strenuous exercise–the Australian Ironman Triathlon. Br J Sports Med. 2006;40(7):605–609. doi: 10.1136/bjsm.2005.022319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.La Gerche A, Boyle A, Wilson AM, Prior DL. No evidence of sustained myocardial injury following an Ironman distance triathlon. Int J Sports Med. 2004;25(1):45–49. doi: 10.1055/s-2003-45236 [DOI] [PubMed] [Google Scholar]
- 31.Body R, Carlton E. Understanding cardiac troponin part 1: avoiding troponinitis. Emerg Med J. 2018;35(2):120–125. doi: 10.1136/emermed-2017-206812 [DOI] [PubMed] [Google Scholar]
- 32.Shave RE, Dawson E, Whyte G, et al. Evidence of exercise-induced cardiac dysfunction and elevated cTnT in separate cohorts competing in an ultra-endurance mountain marathon race. Int J Sports Med. 2002;23(7):489–494. doi: 10.1055/s-2002-35069 [DOI] [PubMed] [Google Scholar]
- 33.Mingels A, Jacobs L, Michielsen E, et al. Reference population and marathon runner sera assessed by highly sensitive cardiac troponin T and commercial cardiac troponin T and I assays. Clin Chem. 2009;55(1):101–108. doi: 10.1373/clinchem.2008.106427 [DOI] [PubMed] [Google Scholar]
- 34.Broz P, Rajdl D, Novak J, et al. High-sensitivity troponins after a standardized 2-hour treadmill run. J Med Biochem. 2018;37(3):364–372. doi: 10.1515/jomb-2017-0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li F, Yi L, Yan H, et al. High-sensitivity cardiac troponin T release after a single bout of high-intensity interval exercise in experienced marathon runners. J Exerc Sci Fit. 2017;15(2):49–54. doi: 10.1016/j.jesf.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scherr J, Braun S, Schuster T, et al. 72-h kinetics of high-sensitive troponin T and inflammatory markers after marathon. Med Sci Sports Exerc. 2011;43(10):1819–1827. doi: 10.1249/MSS.0b013e31821b12eb [DOI] [PubMed] [Google Scholar]
- 37.Richardson AJ, Leckie T, Watkins ER, et al. Post marathon cardiac troponin T is associated with relative exercise intensity. J Sci Med Sport. 2018;21(9):880–884. doi: 10.1016/j.jsams.2018.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Lazzarino AI, Hamer M, Gaze D, et al. The association between cortisol response to mental stress and high sensitivity cardiac troponin T plasma concentration in healthy adults. J Am Coll Cardiol. 2013;62(18):1694–1701. doi: 10.1016/j.jacc.2013.05.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chaulin AM, Duplyakov DV. On the potential effect of circadian rhythms of cardiac troponins on the diagnosis of acute myocardial infarction. Signa Vitae. 2021;17(3):79–84. doi: 10.22514/sv.2021.050 [DOI] [Google Scholar]
- 40.Chaulin AM, Karslyan LS, Grigorieva EV, et al. Metabolism of cardiac troponins (literature review). Complex Issues Cardiovasc Dis. 2019;8(4):103–115. In Russ. doi: 10.17802/2306-1278-2019-8-4-103-115 [DOI] [Google Scholar]
- 41.O’Hanlon R, Wilson M, Wage R, et al. Troponin release following endurance exercise: is inflammation the cause? A cardiovascular magnetic resonance study. J Cardiovasc Magn Resonan. 2010;12(1):38. doi: 10.1186/1532-429X-12-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lippi G, Cervellin G, Banfi G, et al. Cardiac troponins and physical exercise. It’s time to make a point. Biochemia Medica (Zagreb). 2011;21(1):55–62. doi: 10.11613/BM.2011.012 [DOI] [PubMed] [Google Scholar]
- 43.Hickman PE, Potter JM, Aroney C, et al. Cardiac troponin may be released by ischemia alone, without necrosis. Clin Chim Acta. 2010;411(5–6):318–323. doi: 10.1016/j.cca.2009.12.009 [DOI] [PubMed] [Google Scholar]
- 44.Lavie CJ, O’Keefe JH, Sallis RE. Exercise and the heart–the harm of too little and too much. Curr Sports Med Rep. 2015;14(2):104–109. doi: 10.1249/JSR.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 45.Schwartz P, Piper HM, Spahr R, et al. Ultrastructure of cultured adult myocardial cells during anoxia and reoxygenation. Am J Pathol. 1984;115(3):349–361. [PMC free article] [PubMed] [Google Scholar]
- 46.Sicari R, Nihoyannopoulos P, Evangelista A, et al. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr. 2008;9(4):415–437. doi: 10.1093/ejechocard/jen175 [DOI] [PubMed] [Google Scholar]
- 47.Picano E, Pellikka PA. Stress echo applications beyond coronary artery disease. Eur Heart J. 2014;35(16):1033–1040. doi: 10.1093/eurheartj/eht350 [DOI] [PubMed] [Google Scholar]
- 48.Sicari R, Cortigiani L. The clinical use of stress echocardiography in ischemic heart disease. Cardiovasc Ultrasound. 2017;15(1):7. doi: 10.1186/s12947-017-0099-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Samaha E, Brown J, Brown F, et al. High-sensitive cardiac troponin T increases after stress echocardiography. Clin Biochem. 2019;63:18–23. doi: 10.1016/j.clinbiochem.2018.11.013 [DOI] [PubMed] [Google Scholar]
- 50.Bunin VA, Kozlov KL, Linkova NS, et al. An increase in troponin-I concentration in the saliva of patients with coronary heart disease correlates with the stage of disease development. Kompleksnye Problemy Serdecno-Sosudistyh Zabolevanij. 2017;6(S4):13–14. in Russ. [Google Scholar]
- 51.Chaulin AM, Duplyakova PD, Bikbaeva GR, Tukhbatova AA, Grigorieva EV, Duplyakov DV. Concentration of high-sensitivity cardiac troponin I in the oral fluid in patients with acute myocardial infarction: a pilot study. Russ J Cardiol. 2020;25(12):3814. doi: 10.15829/1560-4071-2020-3814 [DOI] [Google Scholar]
- 52.Mirzaii-Dizgah I, Riahi E. Salivary troponin I as an indicator of myocardial infarction. Indian J Med Res. 2013;138(6):861–865. [PMC free article] [PubMed] [Google Scholar]
- 53.Manjunath L, Yeluru A, Rodriguez F. 27-year-old man with a positive troponin: a case report. Cardiol Ther. 2018;7(2):197–204. doi: 10.1007/s40119-018-0120-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lauer B, Niederau C, Kuhl U, et al. Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol. 1997;30(5):1354–1359. doi: 10.1016/S0735-1097(97)00317-3 [DOI] [PubMed] [Google Scholar]
- 55.Soongswang J, Durongpisitkul K, Ratanarapee S, et al. Cardiac troponin T: a marker in the diagnosis of clinically suspected acute myocarditis and chronic dilated cardiomyopathy in children. Pediatr Cardiol. 2002;23(5):531–535. doi: 10.1007/PL00021005 [DOI] [PubMed] [Google Scholar]
- 56.Soongswang J, Durongpisitkul K, Nana A, et al. Cardiac troponin T: a marker in the diagnosis of acute myocarditis in children. Pediatr Cardiol. 2005;26(1):45–49. doi: 10.1007/s00246-004-0677-6 [DOI] [PubMed] [Google Scholar]
- 57.Dancea AB. Myocarditis in infants and children: a review for the paediatrician. Paediatr Child Health. 2001;6(8):543–545. doi: 10.1093/pch/6.8.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yozgat CY, Yesilbas O, Uzuner S, et al. Recurrent elevation of troponin levels in acute myocarditis: is it a sign of ventricular tachycardia? Indian J Pediatr. 2020;87(12):1076–1077. doi: 10.1007/s12098-020-03272-5 [DOI] [PubMed] [Google Scholar]
- 59.Putschoegl A, Auerbach S. Diagnosis, evaluation, and treatment of myocarditis in children. Pediatr Clin North Am. 2020;67(5):855–874. doi: 10.1016/j.pcl.2020.06.013 [DOI] [PubMed] [Google Scholar]
- 60.Chang YJ, Hsiao HJ, Hsia SH, et al. Analysis of clinical parameters and echocardiography as predictors of fatal pediatric myocarditis. PLoS One. 2019;14(3):e0214087. doi: 10.1371/journal.pone.0214087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Abrar S, Ansari MJ, Mittal M, et al. Predictors of mortality in paediatric myocarditis. J Clin Diagn Res. 2016;10(6):SC12–SC16. doi: 10.7860/JCDR/2016/19856.7967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ukena C, Kindermann M, Mahfoud F, et al. Diagnostic and prognostic validity of different biomarkers in patients with suspected myocarditis. Clin Res Cardiol. 2014;103(9):743–751. doi: 10.1007/s00392-014-0709-z [DOI] [PubMed] [Google Scholar]
- 63.Smith SC, Ladenson JH, Mason JW, Jaffe AS. Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates. Circulation. 1997;95(1):163–168. doi: 10.1161/01.CIR.95.1.163 [DOI] [PubMed] [Google Scholar]
- 64.Matsumori A, Shimada T, Hattori H, et al. Autoantibodies against cardiac troponin I in patients presenting with myocarditis. CVD Prev Control. 2011;6(2):41–46. doi: 10.1016/j.cvdpc.2011.02.004 [DOI] [Google Scholar]
- 65.Bohner J, von Pape KW, Hannes W, Stegmann T. False-negative immunoassay results for cardiac troponin I probably due to circulating troponin I autoantibodies. Clin Chem. 1996;42(12):2046. doi: 10.1093/clinchem/42.12.2046 [DOI] [PubMed] [Google Scholar]
- 66.Nussinovitch U, Shoenfeld Y. Anti-troponin autoantibodies and the cardiovascular system. Heart. 2010;96(19):1518–1524. doi: 10.1136/hrt.2010.195255 [DOI] [PubMed] [Google Scholar]
- 67.Watkin RW, Lang S, Smith JM, et al. Role of troponin I in active infective Endocarditis. Am J Cardiol. 2004;94(9):1198–1199. doi: 10.1016/j.amjcard.2004.07.096 [DOI] [PubMed] [Google Scholar]
- 68.Brandt RR, Filzmaier K, Hanrath P. Circulating cardiac troponin I in acute pericarditis. Am J Cardiol. 2001;87(11):1326–1328. doi: 10.1016/s0002-9149(01)01536-3 [DOI] [PubMed] [Google Scholar]
- 69.Tsenovoy P, Aronow WS, Joseph J, et al. Patients with infective endocarditis and increased cardiac troponin I levels have a higher incidence of in-hospital mortality and valve replacement than those with normal cardiac troponin I levels. Cardiology. 2009;112(3):202–204. doi: 10.1159/000149573 [DOI] [PubMed] [Google Scholar]
- 70.Purcell JB, Patel M, Khera A, et al. Relation of troponin elevation to outcome in patients with infective endocarditis. Am J Cardiol. 2006;101(10):1479–1481. doi: 10.1016/j.amjcard.2008.01.031 [DOI] [PubMed] [Google Scholar]
- 71.Imazio M, Demichelis B, Cecchi E, et al. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144–2148. doi: 10.1016/j.jacc.2003.02.001 [DOI] [PubMed] [Google Scholar]
- 72.Gamaza-Chulian S, Leon-Jimenez J, Recuerda-Nunez M, et al. Cardiac troponin-T in acute pericarditis. J Cardiovasc Med (Hagerstown). 2014;15(1):68–72. doi: 10.2459/JCM.0b013e3283641161 [DOI] [PubMed] [Google Scholar]
- 73.Razin VA, Sapozhnikov AN, Mazurova OV, Gimaev RH. Pulmonary embolism: features diagnosis and treatment in the office of acute coronary syndrome. Ulyanovsk Medico Biol J. 2012;(1):13–16. In Russ. [Google Scholar]
- 74.Chaulin AM, Svechkov NA, Grigoreva YUV. Laboratory biomarkers of right ventricular dysfunction. Modern Prob Sci Educ. 2021;1. In Russian. doi: 10.17513/spno.30462 [DOI] [Google Scholar]
- 75.Giannitsis E, Muller-Bardorff M, Kurowski V, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism. Circulation. 2000;102:211–217. doi: 10.1161/01.CIR.102.2.211 [DOI] [PubMed] [Google Scholar]
- 76.Kilinc G, Dogan OT, Berk S, et al. Significance of serum cardiac troponin I levels in pulmonary embolism. J Thorac Dis. 2012;4(6):588–593. doi: 10.3978/j.issn.2072-1439.2012.10.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Becattini C, Vedovati MC, Agnelli G. Prognostic value of troponins in acute pulmonary embolism. A meta-analysis. Circulation. 2007;116:427–433. doi: 10.1161/CIRCULATIONAHA.106.680421 [DOI] [PubMed] [Google Scholar]
- 78.Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008;29(18):2276–2315. doi: 10.1093/eurheartj/ehn310 [DOI] [PubMed] [Google Scholar]
- 79.Lippi G, Favaloro EJ, Kavsak P. Measurement of high-sensitivity cardiac troponin in pulmonary embolism: useful test or a clinical distraction. Semin Thromb Hemost. 2019;45(8):784–792. doi: 10.1055/s-0039-1698762 [DOI] [PubMed] [Google Scholar]
- 80.Muller-Bardorff M, Weidtmann B, Giannitsis E, et al. Release kinetics of cardiac troponin T in survivors of confirmed severe pulmonary embolism. Clin Chem. 2002;48:673–675. doi: 10.1093/clinchem/48.4.673 [DOI] [PubMed] [Google Scholar]
- 81.Lankeit M, Friesen D, Aschoff J, et al. Highly sensitive troponin T assay in normotensive patients with acute pulmonary embolism. Eur Heart J. 2010;31(15):1836–1844. doi: 10.1093/eurheartj/ehq234 [DOI] [PubMed] [Google Scholar]
- 82.Meyer T, Binder L, Hruska N, et al. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632–1636. doi: 10.1016/S0735-1097(00)00905-0 [DOI] [PubMed] [Google Scholar]
- 83.Cotungo M, Orgaz-Molina J, Rosa-Salazar V, et al. Right ventricular dysfunction in acute pulmonary embolism: NT-proBNP vs. troponin T. Med Clin (Barc). 2017;148(8):339–344. doi: 10.1016/j.medcli.2016.11.023 [DOI] [PubMed] [Google Scholar]
- 84.Chaulin AM, Grigorieva Yu V, Pavlova TV, Duplyakov DV. Diagnostic significance of complete blood count in cardiovascular patients. Russ J Cardiol. 2020;25(12):3923. doi: 10.15829/1560-4071-2020-3923 [DOI] [Google Scholar]
- 85.Kim JY, Kim KH, Cho JY, et al. D-dimer/troponin ratio in the differential diagnosis of acute pulmonary embolism from non-ST elevation myocardial infarction. Korean J Intern Med. 2019;34(6):1263. doi: 10.3904/kjim.2018.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chaulin AM, Abashina OE, Duplyakov DV. High-sensitivity cardiac troponins: detection and central analytical characteristics. Cardiovasc Ther Prev. 2021;20(2):2590. In Russian. doi: 10.15829/1728-8800-2021-2590 [DOI] [Google Scholar]
- 87.Chaulin AM, Duplyakov DV. Comorbidity in chronic obstructive pulmonary disease and cardiovascular disease. Cardiovasc Ther Prev. 2021;20(3):2539. In Russ. doi: 10.15829/1728-8800-2021-2539 [DOI] [Google Scholar]
- 88.Rahimtoola A, Bergin JD. Acute pulmonary embolism: an update on diagnosis and management. Curr Probl Cardiol. 2005;30(2):61–114. doi: 10.1016/j.cpcardiol.2004.06.001 [DOI] [PubMed] [Google Scholar]
- 89.Punukollu G, Khan IA, Gowda RM, Lakhanpal G, Vasavada BC, Sacchi TJ. Cardiac troponin I release in acute pulmonary embolism in relation to the duration of symptoms. Int J Cardiol. 2005;99(2):207–211. doi: 10.1016/j.ijcard.2004.01.012 [DOI] [PubMed] [Google Scholar]
- 90.Chaulin AM, Duplyakov DV. High-sensitivity cardiac troponins: circadian rhythms. Cardiovasc Ther Prev. 2021;20(1):2639. In Russian. doi: 10.15829/1728-8800-2021-2639 [DOI] [Google Scholar]
- 91.Chaulin AM, Duplyakova PD, Duplyakov DV. Circadian rhythms of cardiac troponins: mechanisms and clinical significance. Russ J Cardiol. 2020;25(3):4061. doi: 10.15829/1560-4071-2020-4061 [DOI] [Google Scholar]
- 92.Garcia-Osuna A, Gaze D, Grau-Agramunt M, et al. Ultrasensitive quantification of cardiac troponin I by a single molecule counting method: analytical validation and biological features. Clin Chim Acta. 2018;486:224–231. doi: 10.1016/j.cca.2018.08.015 [DOI] [PubMed] [Google Scholar]
- 93.Muslimovic A, Fridén V, Tenstad O, et al. The Liver and Kidneys mediate clearance of cardiac troponin in the rat. Sci Rep. 2020;10(1):6791. doi: 10.1038/s41598-020-63744-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fridén V, Starnberg K, Muslimovic A, et al. Clearance of cardiac troponin T with and without kidney function. Clin Biochem. 2017;50(9):468–474. doi: 10.1016/j.clinbiochem.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 95.Katrukha IA, Kogan AE, Vylegzhanina AV, et al. Thrombin-mediated degradation of human cardiac troponin T. Clin Chem. 2017;63(6):1094–1100. doi: 10.1373/clinchem.2016.266635 [DOI] [PubMed] [Google Scholar]
- 96.Streng AS, de Boer D, van Doorn WP, Kocken JM, Bekers O, Wodzig WK. Cardiac troponin T degradation in serum is catalysed by human thrombin. Biochem Biophys Res Commun. 2016;481(1–2):165–168. doi: 10.1016/j.bbrc.2016.10.149 [DOI] [PubMed] [Google Scholar]
- 97.Chaulin AM. Phosphorylation and fragmentation of the cardiac troponin T: mechanisms, role in pathophysiology and laboratory diagnosis. Int J Biomed. 2021;11(3). http://ijbm.org/v11i3_2.htm DOI: 10.21103/Article11(3)_RA2 [DOI] [Google Scholar]
- 98.Chaulin AM, Duplyakov DV. Cardiac troponins: current data on the diagnostic value and analytical characteristics of new determination methods. Cor Vasa. 2021;63:486–493. doi: 10.33678/cor.2021.041 [DOI] [Google Scholar]
- 99.Ziebig R, Lun A, Hocher B, et al. Renal elimination of troponin T and troponin I. Clin Chem. 2003;49(7):1191–1193. doi: 10.1373/49.7.1191 [DOI] [PubMed] [Google Scholar]
- 100.Dubin RF, Li Y, He J, et al. Predictors of high sensitivity cardiac troponin T in chronic kidney disease patients: a cross-sectional study in the chronic renal insufficiency cohort (CRIC). BMC Nephrol. 2013;14:229. doi: 10.1186/1471-2369-14-229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chaulin AM, Duplyakov DV. Cardiac troponins: analytical characteristics and diagnostic capabilities of modern (high-sensitive) determination methods. J Clin Diagn Res. 2021;15(6):BE01–BE06. doi: 10.7860/JCDR/2021/47764.15025 [DOI] [Google Scholar]
- 102.Wilhelm J, Hettwer S, Schuermann M, et al. Elevated troponin in septic patients in the emergency department: frequency, causes, and prognostic implications. Clin Res Cardiol. 2014;103(7):561–567. doi: 10.1007/s00392-014-0684-4 [DOI] [PubMed] [Google Scholar]
- 103.Rosjo H, Varpula M, Hagve TA, et al. Circulating high-sensitive troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Int Care Med. 2011;37(1):77–85. doi: 10.1007/s00134-010-2051-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pervan P, Svagusa T, Prkacin I, et al. Urine high-sensitive troponin I measuring in patients with hypertension. Signa Vitae. 2017;13(3):62–64. doi: 10.22514/SV133.062017.13 [DOI] [Google Scholar]
- 105.Chen JY, Lee SY, Li YH, Lin CY, Shieh MD, Ciou DS. Urine high-sensitivity troponin I predict incident cardiovascular events in patients with diabetes mellitus. J Clin Med. 2020;9(12):3917. doi: 10.3390/jcm9123917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Haller C, Zehelein J, Remppis A, et al. Cardiac troponin T in patients with end stage renal disease: absence of expression in truncal skeletal muscle. Clin Chem. 1998;44:930–938. doi: 10.1093/clinchem/44.5.930 [DOI] [PubMed] [Google Scholar]
- 107.Arroyo D, Quiroga B, Panizo N, et al. High-sensitivity troponin T levels in kidney transplant recipients. Transplant Proc. 2012;44(9):2545–2547. doi: 10.1016/j.transproceed.2012.09.073 [DOI] [PubMed] [Google Scholar]
- 108.de Filippi CR, Herzog CA. Herzog CA Interpreting cardiac biomarkers in the setting of chronic kidney disease. Clin Chem. 2016;63:59–65. doi: 10.1373/clinchem.2016.254748 [DOI] [PubMed] [Google Scholar]
- 109.Chaulin AM, Duplyakov DV. Increased natriuretic peptides not associated with heart failure. Russ J Cardiol. 2020;25:4140. doi: 10.15829/1560-4071-2020-4140 [DOI] [Google Scholar]
- 110.Ooi DS, Isolato PA, Veinot JP. Correlation of antemortem serum creatine kinase, creatine kinase-MB, troponin I, and troponin T with cardiac pathology. Clin Chem. 2000;46(3):338–344. doi: 10.1093/clinchem/46.3.338 [DOI] [PubMed] [Google Scholar]
- 111.Ali SA, Kazmi S, Jalal-Ud-Din M, Qasim MI, Jadoon ZG. Frequency of elevated troponin T in patients of chronic renal failure without clinically suspected acute myocardial infarction. J Ayub Med Coll Abbottabad. 2019;31(3):364–367. [PubMed] [Google Scholar]
- 112.Rocco E, La Rosa G, Liuzzo G, Biasucci LM. High-sensitivity cardiac troponin assays and acute coronary syndrome: a matter of sex? J Cardiovasc Med (Hagerstown). 2019;20(8):504–509. doi: 10.2459/JCM.0000000000000811 [DOI] [PubMed] [Google Scholar]
- 113.Khan NA, Hemmelgarn BR, Tonelli M, Thompson CR, Levin A. Prognostic value of troponin T and I among asymptomatic patients with end-stage renal disease: a meta-analysis. Circulation. 2005;112(20):3088–3096. doi: 10.1161/CIRCULATIONAHA.105.560128 [DOI] [PubMed] [Google Scholar]
- 114.Aimo A, Januzzi JL, Vergaro G, et al. Prognostic value of high-sensitivity troponin T in chronic heart failure: an individual patient data meta-analysis. Circulation. 2018;137(3):286–297. doi: 10.1161/CIRCULATIONAHA.117.031560 [DOI] [PubMed] [Google Scholar]
- 115.Aimo A, Januzzi JL, Vergaro G, et al. High-sensitivity troponin T, NT-proBNP and glomerular filtration rate: a multimarker strategy for risk stratification in chronic heart failure. Int J Cardiol. 2019;277:166–172. doi: 10.1016/j.ijcard.2018.10.079 [DOI] [PubMed] [Google Scholar]
- 116.Jozwiak M, Persichini R, Monnet X, et al. Management of myocardial dysfunction in severe sepsis. Semin Respir Crit Care Med. 2011;32(2):206–214. doi: 10.1055/s-0031-1275533 [DOI] [PubMed] [Google Scholar]
- 117.Kolwicz SC, Purohit S, Tian R. Cardiac metabolism and its interactions with contraction, growth, and survival of cardiomyocytes. Circ Res. 2013;113(5):603–616. doi: 10.1161/CIRCRESAHA.113.302095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Guest TM, Ramanathan AV, Tuteur PG, et al. Myocardial injury in critically ill patients. A frequently unrecognized complication. JAMA. 1995;273(24):1945–1949. doi: 10.1001/jama.1995.03520480065042 [DOI] [PubMed] [Google Scholar]
- 119.Rosano GM, Fini M, Caminiti G, Barbaro G. Cardiac metabolism in myocardial ischemia. Curr Pharm Des. 2008;14(25):2551–2562. doi: 10.2174/138161208786071317 [DOI] [PubMed] [Google Scholar]
- 120.Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183(3):949–958. doi: 10.1084/jem.183.3.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kumar A, Kumar A, Paladugu B, et al. Transforming growth factor-beta 1 blocks in vitro cardiac myocyte depression induced by tumour necrosis factor-alpha, interleukin-1 beta, and human septic shock serum. Crit Care Med. 2007;35(2):358–364. doi: 10.1097/01.CCM.0000254341.87098.A4 [DOI] [PubMed] [Google Scholar]
- 122.Aberegg SK, Kaufman DA. Troponin in Sepsis. Ann Am Thorac Soc. 2019;16(10):1335–1336. doi: 10.1513/AnnalsATS.201905-412LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chaulin AM. Diagnostic value of highly sensitive cardiac troponins and mechanisms of their increase in serum and urine in arterial hypertension. Rivista Italiana della Medicina di Laboratorio. 2021;17(2):99–107. doi: 10.23736/S1825-859X.21.00107-9 [DOI] [Google Scholar]
- 124.Bessiere F, Khenifer S, Dubourg J, et al. Prognostic value of troponins in sepsis: a meta-analysis. Intensive Care Med. 2013;39(7):1181–1189. doi: 10.1007/s00134-013-2902-3 [DOI] [PubMed] [Google Scholar]
- 125.Sheyin O, Davies O, Duan W, Perez X. The prognostic significance of troponin elevation in patients with sepsis: a meta-analysis. Heart Lung. 2015;44(1):75–81. doi: 10.1016/j.hrtlng.2014.10.002 [DOI] [PubMed] [Google Scholar]