Abstract
Listeria monocytogenes is the etiological agent of listeriosis, a foodborne illness associated with high hospitalizations and mortality rates. This bacterium can persist in food associated environments for years with isolates being increasingly linked to outbreaks. This review presents a discussion of genomes of Listeria monocytogenes which are commonly regarded as persisters within food production environments, as well as genes which are involved in mechanisms aiding this phenotype. Although criteria for the detection of persistence remain undefined, the advent of whole genome sequencing (WGS) and the development of bioinformatic tools have revolutionized the ability to find closely related strains. These advancements will facilitate the identification of mechanisms responsible for persistence among indistinguishable genomes. In turn, this will lead to improved assessments of the importance of biofilm formation, adaptation to stressful conditions and tolerance to sterilizers in relation to the persistence of this bacterium, all of which have been previously associated with this phenotype. Despite much research being published around the topic of persistence, more insights are required to further elucidate the nature of true persistence and its implications for public health.
Keywords: Listeria monocytogenes, virulence, persistence, whole genome sequencing, genotypes, biocide resistance, taxonomy
1. Introduction
The genus Listeria belongs to the Listeriaceae family. This family belongs to the phylum Firmicutes, which is composed of Gram-positive bacteria that possess a low GC-content (36–42%) [1]. Listeria monocytogenes is a Gram-positive, facultatively anaerobic, non-sporulating, rod-shaped bacterium [2]. The size of these rods varies from 0.4- to 0.5-µm in diameter and from 0.5- to 2.0-µm in length. The genus Listeria currently consists of 21 species [3], with L. monocytogenes being the most significant pathogen in this genus and L. ivanovii being the only other pathogenic member reported [4], which rarely infects humans [5,6] but frequently causes listeriosis in ruminants [7,8]. Together with L. marthii [9], L. innocua, L. welshimeri, and L. seeligeri, these two species form the Listeria sensu stricto group [10], clade I, being one of two distinct clades within the genus.
All members of clade I are cultured from feces or the gastrointestinal tract (GIT) of asymptomatic animals, as well as from foods of animal origin [11,12,13,14,15], suggesting a specific interaction with mammalian hosts. Clade II, the Listeria sensu lato group, contains the remaining species of Listeria which are cultured from food-processing surfaces or the production environment. This clade includes the novel species, L. valentina, which was isolated from an animal farm environment in Valencia, Spain [3].
L. monocytogenes is a heterogenous group of bacteria. This bacterium can be differentiated into 14 different serotypes, with serovar 4 h being recently described [16,17]. These serotypes are divided into four lineages (denoted as I-IV) [18]. From the four lineages, most L. monocytogenes fall into lineages-I and -II [19]. Serotypes 1/2a (lineage II), 1/2b and 4b (both lineage I) cause 95% of human cases of listeriosis [20]. These categories can be further subdivided into clonal complexes (CCs), where sequence types are grouped based on their similarity to a central allelic profile [21].
Despite the low incidence of listeriosis, the mortality rate is high (20–30%) and, consequently, the burden of the disease is high [2]. This disease may manifest as a blood stream infection (BSI), meningitis, or maternal-neonatal infection following transplacental transmission [2,22]. The populations which are most at risk include the elderly, pregnant women and immunocompromised individuals. Listeriosis in humans is mostly associated with the consumption of contaminated food. Many studies reported that the contamination of food-processing facilities and associated environments is often the route by which foods become contaminated [23,24,25,26,27,28].
Cases of listeriosis are mainly sporadic. However, outbreaks have also been described [29]. Globalization of the food supply chain is likely to contribute to an increased occurrence of outbreaks. This development can be understood in terms of the wider international distribution of food. Outbreak situations may also arise due to vulnerable populations consuming contaminated food, as in the case of the documented listeriosis outbreak linked to pasteurized ice cream involving hospitalized patients who became ill [30], among other factors. The application of WGS will facilitate detection of these outbreaks. In 2019, 21 European food-borne outbreak situations were described, which was 50% higher than the previous year [31]. On an international level, the largest ever detected outbreak of listeriosis took place in South Africa from January 2017 until July 2018. During this time 1060 laboratory-confirmed cases of listeriosis were recorded, including 216 deaths [28]. Multi-locus sequence typing (MLST) revealed that 91% cases were caused by ST6, a sequence type commonly implicated in listeriosis outbreaks. The source of the outbreak was a large ready-to-eat processed meat production facility, wherein L. monocytogenes ST6 was isolated from environmental samples and ready-to-eat processed meat produced by the facility [28]. The advent of whole genome sequencing (WGS) has revolutionized bacterial characterization and, in turn, outbreak investigation [32,33], aiding in the global surveillance of food-borne pathogens. With many food production systems operating within a globalized supply chain, effective (global) surveillance is crucial in limiting the dissemination of food-associated microbial contaminants and protecting public health. WGS has facilitated the detection of international outbreaks of listeriosis, including an outbreak in Australia caused by contaminated rockmelons, which were linked to two cases in Singapore [34] and a US outbreak that was connected to cases in Australia, which implicated contaminated stone fruit [35].
In addition to bacterial characterization, the development of WGS technologies allows for the description of antimicrobial resistance (AMR) and virulence genes. The pathogenesis and virulence of L. monocytogenes is well documented [2,22,36,37,38,39,40,41,42]. Previously all L. monocytogenes were regarded as equally virulent. However, there is new evidence to suggest that some strains are less virulent than others, being attributed to a premature stop codon mutation in the internalin A gene, leading to the production of a truncated and inactive protein [43]. WGS is utilized to detect these truncations, allowing an assessment of the virulence potential of L. monocytogenes. Furthermore, hypervirulent strains which pose a greater threat to public health can also be described using WGS. These strains contain putative virulence factor-encoding genes, often mapped within gene clusters. Four virulence gene clusters have been identified, which are known as Listeria pathogenicity islands (LIPIs). The recognized LIPIs include LIPI-1, LIPI-2, LIPI-3 and LIPI-4, all of which have been associated with L. monocytogenes (Table 1). Until recently, LIPI-2 had only been associated with L. ivanovii. However, a partial LIPI-2 locus has been detected in atypical CC33 L. monocytogenes (Table 1) [42]. In a recent review by Disson, Moura and Lecuit [42], the heterogeneity in virulence is suggested to be associated with differences in host adaptation. As lineage I isolates are usually more tolerant to low pH [44], they are more likely to survive in the acidic gastric environment of a host. This observation is concordant with findings that CCs associated with hypervirulence are more effective colonizers of the gut [45]. As indicated in this review, more research is required to fully elucidate the process by which L. monocytogenes adapt to different environments. WGS will play an important role in this, as transcriptomic studies of different CCs are likely to clarify the phenotypes of L. monocytogenes in various environments.
Table 1.
Pathogenicity islands found in Listeria monocytogenes.
| Island | Gene | Product | Function |
|---|---|---|---|
| LIPI-1 | actA | Actin assembly-inducing protein |
|
| mpI | Metalloprotease | Process the PC-PLC into its mature and active form [49] | |
| plcA | Phosphatidylinositol-specific Phospholipase C | ||
| plcB | phosphatidylcholine-specific Phospholipase C or lecithinase | ||
| prfA | PrfA (Pleiotropic regulatory factor) | Belongs to CAP (for catabolite gene activator protein)/FNR family, Dimeric protein and bindis binds to its DNA target sequences in dimeric form [54] | |
| hly | Listeriolysin O |
|
|
| LIPI-2 |
i-inlB2
i-inlL i-inlK i-inlB1 i-inlJ i-inlI i-inlH i-inlG smcL i-inlF i-inlE surF3 |
Inernalins and SMase | |
| LIPI-3 | llsAGHXBYDP | Listeriolysin S | Haemolysin that is post-translationally modified and belongs to a family of modified virulence peptides, including streptolysin S and several as-yet uncharacterized members of the same family in other pathogens. LLS demonstrated to play a role in the survival of L. monocytogenes in PMNs and also contributes to its virulence in the mouse model [60] |
| LIPI-4 | lm4b_02324 | Maltose-6′-P-glucosidase | Putative 6-phospho-beta-glucosidase [61] |
| lm4b_02325 | Transcriptional antiterminator | Putative transcription antiterminator BglG family [61] | |
| lm4b_02326 | Uncharacterized protein associated to PTS systems | Unknown [61] | |
| lm4b_02327 | Membrane permease EIIA | Putative PTS system, cellobiose-specific enzyme component [61] | |
| lm4b_02328 | Membrane permease EIIB | Putative PTS system, cellobiose-specific enzyme component [61] | |
| lm4b_02329 | Membrane permease EIIC | Putative PTS system, cellobiose-specific enzyme component [61] |
WGS technologies have made a significant impact on the characterization of L. monocytogenes and have allowed for the prediction of the virulence potential of this pathogen. The remainder of this review will focus on the contribution of WGS to the assessment of the persistence of L. monocytogenes in food production environments and how these methodologies may advance our understanding of the persister phenotype.
2. Persistent Strains of L. monocytogenes
Persistent L. monocytogenes are described as isolates that are repeatedly cultured from the same source or ecological niche over time. Criteria used to define persistence have varied and this lack of a standardized definition makes it difficult to determine true persistence (Table 2). It can also be difficult to distinguish true persistence in a food production facility and reintroduction from an external source, such as a supplier of raw materials. In general, persistent Listeria have indistinguishable pulsotypes when repeatedly isolated from the same source at different dates over a defined period, for example, at intervals of six or more months apart [62]. Persistent strains of L. monocytogenes are indistinguishable when characterized using genomic epidemiological sub-typing methods. However, it is important to consider the discriminatory power of these sub-typing methods. In recent years, sub-typing methods have come a long way from the earlier multilocus enzyme electrophoresis (MEE) and restriction length polymorphism (RFLP) methods as applied by Harvey and Gilmour [63]; one of the first studies to hypothesize the persistence of L. monocytogenes sub-types in food production environments. Nowadays there are several molecular-based epidemiological typing methods available, including MLST and pulsed-field gel electrophoresis (PFGE), that can be applied. These methods have advantages and disadvantages which can be addressed with the application of Next Generation Sequencing (NGS) technologies which provide the best possible resolution to modern strain typing.
Table 2.
Criteria used to define persistence of Listeria monocytogenes in literature.
| Persistence Definition | Time Frame | Sample Number | Persisters Identified | Reference |
|---|---|---|---|---|
| PFGE type detected repeatedly for longer than 6 months | 1 year | |||
| 319 | ST9, ST121 | [64] | ||
| PFGE type isolated at least 3 occasions over the 16-month sampling period | 16 months | 2496 | LS1, LS2, LS4, LS5, LS7, LS25, LS35, LS45 | [65] |
| Genotypes isolated at least on 3 occasions with a minimum interval of 6 months between first and last isolation | 3 years | 1702 | Serogroup IIa | [66] |
| PFGE type isolated at least six months apart | 3 years | 5869 | P59, P6, P10, P32, P44 | [67] |
| PFGE type isolated repeatedly, at least 4 times | 2 years | 1801 | 26 pulsotypes | [68] |
| CTs isolated at least 3 times with a minimum of 1 year between the first and last isolation | 4 years | 100 | CT1526, CT1828, CT1833, CT1834, CT1836, CT1839 | [69] |
L. monocytogenes is ubiquitous in nature and can persist in food processing environments for extended periods of time. Persistent isolates may prevail for years and even decades in these food processing environments [70]. Certain phenotypes allow L. monocytogenes to survive and multiply in food. The bacterium’s psychrophilic nature allows it to survive and thrive at refrigeration temperatures. L. monocytogenes also tolerates high salt concentrations and low pH levels, which are strategies used in food preservation to limit the growth of bacterial pathogens [71]. This phenotype allows L. monocytogenes to contaminate a variety of foods, such as soft or hard cheese, meat and vegetables [29]. Ready-to-eat (RTE) foods (certain meats, fish or cheeses) are a particular cause for concern. These food products are often identified in outbreak situations as vehicles of infection [72]. RTE products do not require cooking prior to consumption and L. monocytogenes will survive and multiply during refrigeration. Therefore, prevention of cross-contamination within the food processing environment to food is imperative.
RTE products have been the primary focus of sampling for the presence of L. monocytogenes. However, other unusual sources have recently been described. Frozen corn was implicated in an EU-wide outbreak [73]. Ice-cream [74], pre-packaged caramel apples [75] and sprouts [76] were all implicated in US outbreaks. Although the number of samples tested for fruit and vegetables has increased since 2016, in 2019 less than 2% of all samples studied belonged to the fruit and vegetable categories [31]. This number is significantly lower compared to the number of RTE foods of animal origin sampled [31]. An increase in the sampling of fruit and vegetables has been suggested, as these matrices are increasingly implicated in cases of listeriosis.
Contamination by L. monocytogenes can also occur at the retail level. This bacterium has been isolated from environmental samples in commercial retail establishments, however, the transmission in these environments is not well understood and further studies are required. The majority of human listeriosis cases result from the consumption of contaminated RTE foods [77]. Interestingly, a higher risk is associated with products that are sliced or prepared at retail delicatessens, as they are contaminated more often and more heavily than products which do not require further processing in retail establishments.
As mentioned previously, the discriminatory power of WGS is unparalleled. Many researchers have utilized this technology in order to reduce the ambiguity of the persister phenotype, described above [78,79,80,81]. This method is useful for the detection of persistent isolates as well as outbreak investigations. Typing tools used to characterize sequence data such as cgMLST and SNP analysis can facilitate the detection of very closely related isolates that may be persisting in food production environments. Several functional concepts have been suggested to describe persistence, such as stress resistance, biofilm formation and an increased tolerance to disinfecting agents, all of which will be discussed further in the subsequent sections.
3. Stress Resistance
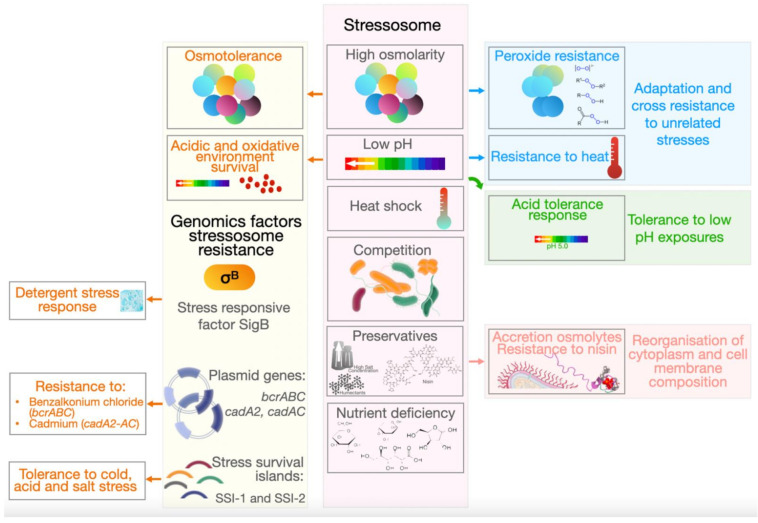
Most of the time, environmental conditions in food processing facilities are not conducive to the growth of bacteria of importance to human health. Moreover, L. monocytogenes in these niches, are often exposed to nutrient deficiency, heat shock, high osmolarity, low pH and competition with other microorganisms. Nonetheless, L. monocytogenes can adapt to a wide range of environmental stresses, including sublethal levels when later exposed to other types of stress/lethal conditions [82]. Furthermore, cross resistance to unrelated stresses resulting from previous exposure to other sublethal levels has been described [82]. Examples include resistance to peroxide following the exposure to osmotic stress [83] and resistance to heat from the exposure to low pH (Figure 1) [84]. This may be described by the vast number of mechanisms of stress resistance applied by L. monocytogenes, as this increases the likelihood of cross-resistance [85]. The diverse mechanisms employed by L. monocytogenes to survive in unfavorable conditions allows this bacterium to deploy mechanisms in response to the same stress or the same mechanism for different stresses, as is the case with heat-shock genes which are activated in response to heat stress, high hydrostatic pressure (HHP) and pulsed-electric fields (PEF) [85].
Figure 1.
L. monocytogenes adaptation to stress conditions (stressosome) involves various genomic factors and causes different adaption phenomena.
L. monocytogenes’ ability to survive at temperatures between −0.4 to 45 °C allows it to overcome the thermal interventional strategies that are often deployed in food preservation and production [86,87]. It is more tolerant to high temperatures when compared to other food-borne pathogens, such as Salmonella species and E. coli [88,89]. Survival at temperatures as low as −0.4 °C results in the frequent isolation of L. monocytogenes from refrigerated food products [90]. Another traditional method of food preservation is acidification, normally applied to dairy, meat and vegetables. The production of weak organic acids by bacteria found in the raw food or added as starter cultures have antimicrobial activity and can inhibit microbial growth through the generation of a low pH environment [91,92]. L. monocytogenes exhibits an adaptive acid tolerance response (ATR) whereby exposure to mild acid stress (pH 5.0) leads to tolerance to subsequent exposures at an even lower pH (3.0) [93,94]. Bacteria experience osmotic stress in the presence of increased concentrations of salt or sugar, humectants that are added to foods such as cheese, seafood, pickles, jams and syrups as preserving agents [95]. The concentrations of these additives alter the osmotic balance between the cytoplasm of a bacterium and its external environment [96]. Furthermore, L. monocytogenes can reduce osmotic pressure and water loss through the accumulation of osmolytes within the cytoplasm in the presence of high salt concentrations [97]. Nisin a bacteriocin with a broad activity against Gram-positive bacteria can be used as a preserving agent [98]. This antibiotic has two modes of action against bacteria; inhibition of cell wall synthesis and formation of pores in the cell membrane, resulting in permeabilization [99]. Not surprisingly, L. monocytogenes has developed resistance to nisin, mediated through changes in the cell membrane composition [100,101].
A recent study by Hingston et al. [44] revealed that L. monocytogenes’ survival in stressful conditions can be linked to its serotype, clonal complex, full length inlA profile and plasmid harborage. In this latter study, a full length inlA gene contributed to an increased tolerance to cold temperatures, while the presence of plasmids resulted in an increased acid tolerance. There are two phylogenetic groups of L. monocytogenes plasmids which are distinguished by their repA sequences [102]. Although plasmid harborage can result in a reduced bacterial growth rate due to increased metabolic demand [103], certain genes mapped on plasmids can, in contrast, provide L. monocytogenes with a growth advantage. Genes mapped on L. monocytogenes plasmids include benzalkonium chloride resistance genes (encoded by bcrABC) [104,105,106] and cadmium resistance genes (encoded by cadA2, cadAC) [105,106,107]. Oxidative stress response genes such as peroxidases and reductases have also been found to be located on these plasmids [102]. More research is needed to elucidate the function of other genes also located on L. monocytogenes plasmids and how they contribute to stress tolerance (i.e., acid and salt) and persistence. As a full length inlA gene was more prevalent among isolates that are tolerant to cold, salt and acid, it can be suggested that the presence of surface proteins such as InlA can contribute to protection against certain stresses. In contrast to this, a study by Franciosa et al. [108], found that truncations in inlA contributed to increased biofilm formation, while a study by Piercey et al. [109] reported isolates with truncations in inlA, inlB and inlH to be better biofilm formers. These results suggest that internalins may have a function in processes other than virulence.
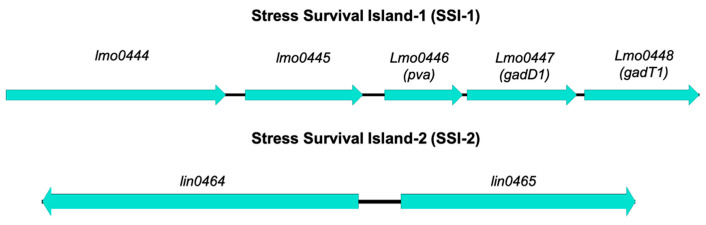
Listeria stress survival islands include SSI-1 and SSI-2 (Figure 2) (Table 3). SSI-1 contains 5 genes which contribute to L. monocytogenes tolerance to cold, acid and salt [110]. Some studies have found no significant variations in responses to cold, acid or salt between isolates which contain SSI-1 and those which do not [44,111,112]. However, this may be the case when comparing large numbers of isolates, rather than a mutant and its isogenic wildtype. A study by Ryan, Begley [110] which compared a SSI-1 harboring strain with its isogenic mutant reported that loss of SSI-1 significantly compromised L. monocytogenes’ ability to grow and survive in frankfurters, which have previously been implicated in outbreaks of listeriosis [113,114,115], as well as growth at 4- and 15-degrees C. These data, along with the absence of SSI-1 from the genomes of L. monocytogenes which are not commonly associated with foods, suggest that genes found in SSI-1 may be involved in the bacteriums’ ability to survive in food [116,117,118,119,120]. SSI-1 is located in a hypervariable hot spot, wherein homologues of L. innocua genes lin0464 and lin0465 can also be found [121]. It has been demonstrated that these genes can also be found in strains which belong to sequence type (ST) 121 [1,121,122]. These strains are often found to be persisting in food processing environments [123,124]. Therefore, it is possible that these loci have a function in adaptation to stress.
Figure 2.
Scheme of the genetic organization of genes mapping to stress survival islands. Created using Easyfig [33]. (see also Table 2).
Table 3.
Stress survival islands detected in Listeria monocytogenes.
| Island | Acronym | Gene | Product | Function | Reference |
|---|---|---|---|---|---|
| Stress Survival Island-1 | SSI-1 | lmo0444 | Hypothetical protein | Unknown | Ryan et al. [110] |
| lmo0445 | Transcriptional regulator | Regulation of transcription | |||
| lmo0446 (pva) | Penicillin acylase | Conversion of penicillin to 6-amino-penicillinate and phenylacetate—reduced susceptibility to penicillin V Survival in bile salts |
Begley et al. [125] | ||
| lmo0447 (gadD1) | Glutamate decarboxylase | Growth in mildly acidic pHs | Cotter et al. [126] | ||
| lmo0448 (gadT1) | Amino acid antiporter | ||||
| Stress Survival Island-2 | SSI-2 | lin0464 | Transcriptional factor | Involvement in alkaline and oxidative stress responses | Harter et al. [127] |
| lin0465 | Pfpl protease |
A more recent study by Harter, Wagner [127] investigated the role of these stress islands by creating a lin0465 deletion mutant using a persistent L. monocytogenes belonging to ST121 which was repeatedly isolated from an Irish cheese production facility over a 12-year period [128]. The isolate was exposed to a variety of stress conditions, including acid, gastric juice, cold, heat, osmotic, alkaline, oxidative and antibiotic stresses. This study characterized this gene insertion as SSI-2 and phenotypic characterization of strains possessing SSI-2 have conferred resistance to stresses different to those encoded by genes mapped to SSI-1 (Figure 2) (Table 3). SSI-2 is believed to be involved in the response to oxidative stress which occurs as a result of a high concentration of oxygen radicals leading to cell death due to irreversible damage to proteins, lipids and nucleic acids [129]. The resistance of L. monocytogenes to oxidative stress is suggested to be associated with biofilm formation [129]. Harter and Wagner [127] also reported that, unlike SSI-1, the regulation of SSI-2 is independent of the alternative stress sigma factor (sigB). Although SSI-2 does not confer resistance to QACs, the novel transposon Tn6188 involved in QAC resistance is harbored by ST121 strains [122,130,131].
It has also been shown that although isolates are very closely related and belong to the same clonal complex, they can still exhibit significant differences in stress tolerance patterns [44,132]. These variations can be attributed to small genetic differences which result in a significant effect on the phenotype. Small genetic variations can be detected through genome-wide association studies (GWAS). Although these studies have been hugely effective, they can be of limited value when it comes to bacterial genomes due to the high frequency of mutations encountered [44,133,134]. Hingston, Chen [44] applied GWAS to their collection of Listeria in order to detect SNVs responsible for stress tolerance. Their results showed no common SNVs in the stress tolerant isolates. However, unique SNVs were recorded in up to four stress susceptible isolates. The gene sigB facilitates L. monocytogenes to survive in unfavorable conditions and this has been well documented [99,135]. Notably, common SNVs found among the collection of stress sensitive isolates resulted in PMSCs in several regulatory networks controlled by sigB. These included PMSCs in rsbS and rsbV [136] in the cold sensitive group; PMSCs in rsbS among three desiccation sensitive isolates; and PMSCs in rsbU, a post transcriptional regulator of sigB in two other desiccation sensitive isolates. In another GWAS study reported by Fritsch et al., [137] a slow growth phenotype was established among the isolates when grown at two degrees for two months. A SNP based GWAS revealed 184 significant SNPs and a gene based GWAS found 114 significant associated genes. Some of these SNPs/genes were known to be associated with L. monocytogenes’ tolerance of cold temperatures and others were linked to hypothetical proteins. There have been few GWAS studies performed to assess phenotypes relevant to food safety, however these methods have the potential to further our understanding of the persistence of L. monocytogenes in food environments.
The continuous emergence of stress resistance among isolates of L. monocytogenes cultured from food matrices and/or their associated production environments led to the establishment of novel methods for food preservation. These include high pressure processing (HPP), the application of UV-light, pulsed-electric field processing and oxidative stress. L. monocytogenes have also evolved to adapt to these novel technologies. HPP is an alternative processing technology to thermal treatment and is designed to increase the permeability of the bacterial cell membrane by disrupting structural proteins, therein ultimately leading to the inhibition of metabolism, replication and transcription [138]. Resistance to HPP, expressed by L. monocytogenes, appears to be strain specific [139]. Pulsed-electric field processing is also an alternative to thermal treatment. This strategy is mostly used in the processing of liquid foods, and it acts to irreversibly damage the cell membrane, leading to leakage of cytoplasmic contents [140]. Gram-positive bacteria are more resistant to this treatment when compared to Gram-negative bacteria; an observation which may be attributed to their thicker cell wall [141]. Exposure to UV-light eradicates surface microorganisms that have contaminated food products during processing stages [142]. UV-light acts on bacteria in a number of ways, including by damaging DNA along with exerting photophysical and photothermal effects which lead to leakage of cellular contents [142,143]. Although specific L. monocytogenes mechanisms of resistance to UV-light are unknown, it has been demonstrated to be more resistant to UV-light than other pathogens such as E. coli [144].
4. Biofilm Formation
One of the main sources of repeated contaminations in food production is the growth of biofilms [145,146,147]. Biofilms are an accumulation of bacterial cells, encased in a self-produced exopolysaccharide matrix which have an enhanced ability to attach to surfaces [148]. Bacteria enclosed within this matrix are protected from stresses arising from the external environment, such as desiccation, nutrient deprivation and disinfection procedures [149,150]. Previous research findings into biofilm formation by L. monocytogenes have been inconsistent and contradictory. However, many recent studies have shown that this is a significant strategy deployed for the survival and persistence of some L. monocytogenes [147,151,152,153]. L. monocytogenes can produce biofilms on a variety of materials found in food production facilities, such as buna-N rubber, cast iron, stainless steel, nylon, teflon, polyester floor sealant and glass [154,155,156,157].
Earlier studies explored the relationship between biofilms and the persistence of L. monocytogenes. Some authors reported persistent strains to be better biofilm formers when compared to sporadic strains. Manso and Melero [158] studied biofilm formation by L. monocytogenes on plastic surfaces and on stainless steel. Here it was found that L. monocytogenes only formed biofilms on polyvinyl chloride (PVC), however, the strongest biofilm formers were identified as persistent strains. Lee and Cole [159] found no association between persistence and biofilm formation. Other researchers investigating the ability of L. monocytogenes to form biofilms utilized a simple microtiter plate method, followed by crystal violet staining, as described by Stepanovic and Cirkovic [160] (Table 4). Using this approach, researchers reported L. monocytogenes to be weak/intermediate biofilm formers [158,161,162]. A major disadvantage of this method is that crystal violet stains both the bacterial cells and the extracellular matrix and, thus, only measures the biofilm mass, not its viability. Metabolic assays have been suggested to overcome this limitation, as they quantify the viability of the biofilm itself. An example of this is the use of the resazurin assay, wherein a blue dye is reduced to pink resorufin by metabolically active cells, embedded in the biofilm.
Table 4.
Comparison of results obtained from crystal violet staining of biofilms in literature.
| Method | Duration | Temp. | Substrate | Strains | Summary | Reference |
|---|---|---|---|---|---|---|
| MPA stained with crystal violet | 24 h | 37 °C and 10 °C | Bacterial biomass | 19 persistent, 20 prevalent, 19 rare (27 genotypes) | Persistence/prevalence did not correspond to a higher biofilm formation, supplementation with NaCl in nutrient deprived cells improved biofilms, production ~5 times greater at 37 °C than at 10 °C | [159] |
| MPA/stainless steel sheets stained with crystal violet | 24 h | 37 °C | Bacterial biomass | ST1, ST2, ST5, ST8, ST9, ST87, ST121, ST199, ST321, ST388 | All strains formed moderate biofilms on microtiter plates but not on stainless steel | [158] |
| MPA stained with crystal violet | 16, 24 and 36 h | 30 °C | Bacterial biomass | Range of serotypes from food/clinical samples | Lineage I isolates produced more biofilm, no significant difference in biofilm formation found between food/clinical isolates | [163] |
| MPA stained with crystal violet | 224 h | 37 °C | Bacterial biomass | Range of serotypes | Lineage II (persistent) isolates produced more biofilms, biofilm formation correlated with phylogenetic division but not serotype | [164] |
| MPA stained with crystal violet | 24 h (37C) and 5 days (4C) | 37 °C and 4 °C | Bacterial biomass | Range of serotypes from food/clinical samples | Higher biofilm formation at 37 °C with food isolates producing slightly more biofilm at both temperatures | [165] |
The relationship between biofilm formation and serotype/lineage has been commented upon, but with conflicting results. Takahashi and Miya [163] observed significantly higher biofilm-forming ability among isolates of lineage I using the CV assay. Likewise, Djordjevic and Wiedmann [166] reported a higher biofilm-forming ability for lineage I (serovars l/2b and 4b) than for lineages-II (serovars 1/2a and l/2c) and -III, using the same method. Contradictory to these findings, Borucki and Peppin [164] found a higher biofilm-forming ability for isolates of lineage II. Barbosa and Borges [165] compared the biofilm forming ability of food and clinical isolates, and reported a significant difference. The majority of clinical isolates in this study were weak biofilm formers, while 40% of food isolates were moderate formers. Serogroups IIa and IIb (and IIc for food isolates) included the highest percentage of isolates showing the strongest ability to form biofilms at 37 °C. This study also compared biofilm formation at 4- and 37-degrees C, with increased biofilm formation being recorded at the latter temperature. It has also been suggested that serotype-specific differences in biofilm formation patterns of L. monocytogenes can be linked to the presence of SSI-1 [167]. In a study by Keeney and Trmcic [167], strains of serotype 1/2b were the strongest biofilm formers; the majority of which contained SSI-1. The weakest biofilm formers belonged to serotype 4b, the majority of which did not harbor SSI-1. The conflicting results in investigations of biofilm formation being related to persistence could also be a result of the varying criteria used to determine persistence or the discriminatory power of the methods used to detect persistence. In addition, the serotypes of these presumptive persistent strains varied across studies. As different serotypes are associated with infection and the food environment, they may be adapted to form biofilms at different temperatures, (i.e., clinical strains favoring the body temperature and food strains favoring lower temperatures). Another reason for conflicting results in studies attempting to explore the association of the biofilm phenotype with lineage, serotypes and origin may be caused by the differences in methods applied and the strains selected for study.
As the majority of attempts to link biofilm formation to serotype or persistence have been conducted using phenotypic investigations, genomic methods may have the potential to overcome these conflicting results. An example of this is a study by Lee and Cole [159] who utilized GWAS, wherein large numbers of genetic variants were tested with a given phenotype. Although there were definite differences in the biofilm formation by strains belonging to different serotypes, they were inconsistent when all the growth conditions were taken into account. In fact, associations based on lineage, yielded conflicting results, as two serogroups (IIb and IVb) belonging to lineage I presented significant variations in biofilm formation under some selected conditions. These authors suggest that instead of using these criteria to determine the intraspecific differences in biofilm formation, other genetic markers, such as strain types or clonal complexes, may prove to be more reliable. In this study, CC26 produced more biofilm at 10 degrees C, which indicates that core genes are involved in survival under cold temperatures. This hypothesis has also been explored by other authors. For example, Maury and Bracq-Dieye [45] recorded that the genomes of certain clonal complexes may present advantages when exposed to environmental stress, as they have shown that hypovirulent clonal complexes (CC9 and CC121) were better biofilm formers when exposed to sub-inhibitory concentrations of benzalkonium chloride. Hingston and Chen [44] reported similar associations in relation to stress tolerance traits. Most studies implementing GWAS focused on clinical phenotypes. Nevertheless, GWAS is emerging as a tool that can be applied to address food safety questions—as in the case of investigating L. monocytogenes traits associated with cold, salt, acid and desiccation stresses [44,137].
To date, many genetic determinants have been linked to biofilm formation in L. monocytogenes a feature that demonstrates the complexity of the phenotype being studied. Transposon mutagenesis is a method often utilized to investigate the functionality of genetic determinants responsible for biofilm formation and several studies focused on examining the effect of knockouts of individual genes involved in biofilm formation. The genes involved in biofilm formation include the degU (virulence) orphan response [168] and flaA [169] both of which control motility [170,171]. The agrBDCA operon is involved in quorum sensing [172,173]. The L. monocytogenes Biofilm-Associated Protein (BapL) contributes to the surface adherence of strains that possess it, however it is not essential for all strains [174]. Similarly, the transcriptional regulator of stress response genes, SigB, has been shown to exert an effect on biofilm formation by van der Veen and Abee [175]. Although these studies are useful, identification of functionally relevant biofilm genes on a genome-wide level would be of value. Chang, Gu [176] conducted one of the first GWAS studies using the mariner-based transposon mutagenesis approach. This study identified 24 genes involved in biofilm formation. Alonso and Perry [177] identified 38 genetic loci believed to be involved in L. monocytogenes biofilm formation when grown at 35 degrees C. Among these loci were the D-alanylation pathway genes dltABCD and the phosphate-sensing two component system phoPR, the significance of which was explored by the creation of deletion mutants. The result of this was a significant reduction in biofilm formation by the mutants. These results are indicative of the significance of the D-alanylation of lipoteichoic acids mediated by the gene products of the dltABCD operon and the phosphate-sensing phoPR two-component system in L. monocytogenes’ ability to form biofilms. A list of genes involved in biofilm formation by L. monocytogenes is found in Table 5.
Table 5.
Genes involved in biofilm production by L. monocytogenes.
| Gene | Product | Function | Reference |
|---|---|---|---|
| degU | Putative response regulator | degU is essential for flagellar synthesis and motility in L. monocytogenes. It is required for growth at high temperature, adherence to plastic surfaces and formation of efficient biofilms. It also functions in virulence of L. monocytogenes. | [168,170] |
| flaA | Flagellin A | Involved in initial attachment of L. monocytogenes in biofilm formation. | [169,171] |
| agrBDCA | Peptide-sensing system | Peptide-sensing system involved in quorum-sensing. Involved in early stages of biofilm formation. Also involved in virulence. | [172,173] |
| bapL | Putative cell wall-anchored protein | Surface adherence of L. monocytogenes in L. monocytogenes. | [174] |
| sigB | Major transcriptional regulator of stress response genes | Required to obtain wild-type levels of static and continuous-flow biofilms. Also involved in resistance of planktonic/biofilm cells to benzalkonium chloride and peracetic acid. | [175] |
| dltABCD | D-alanylation pathway | Further work needed to find specific function. | [177] |
| phoPR | Phosphate-sensing two component system | Further work needed to find specific function. | [177] |
A study by Piercey and Hingston [109] identified genes that are involved in biofilm formation at 15 degrees C, a temperature more commonly encountered in food production environments. It is likely that these genes may differ, as the environmental temperature affects cell surface hydrophobicity [178], motility [179] and the expression of other genetic factors [180,181]. This study also utilized transposon-mediated mutagenesis to create mutant libraries. Nine loci associated with biofilm formation were identified that were not previously described to be linked to biofilm formation at higher temperatures. A Pan Genome Wide Association Study conducted by Lee and Cole [159] compared sets of genes identified to be related to biofilm formation at 37- and at 10-degrees C and which included four different conditions. The conditions tested included BHI, distilled BHI, BHI + NaCl and distilled BHI + NaCl. At 37-degrees C some 1360 genes were identified with only 50 genes (3.68%) found in three or more conditions. At 10-degrees C, some 1050 genes were identified, with 59 genes (5.62%) common in more than three conditions. The products of the identified genes were found to encode cell surface proteins and transformation/competence-related functions.
To fully elucidate the process of biofilm formation, further genetic investigations are required such as examining unknown gene functions and transcriptomics/proteomics approaches. Furthermore, it would be interesting to explore the effects of the relationship between biofilm formation and biocide resistance on the persistence of L. monocytogenes in food production environments (FPEs), which is discussed further in the following section.
5. Biocide Susceptibility
Susceptibility to biocides used to eradicate L. monocytogenes has been described as a potential mechanism for persistence due to the survival of certain strains post-cleaning/disinfecting procedures. This tolerance may be caused by the presence of niches within food processing environments which are inaccessible to disinfectants, resistance to biocides arising from the acquisition of genetic markers, and/or formation of biofilms which inhibit the penetration of biocides. Biocides are extensively applied in food production environments to prevent bacterial contamination, and common examples include: quaternary ammonium compounds (QACs), aldehydes, alcohols, chlorine-releasing compounds and peracids. The modes of action of biocides are similar to that of antimicrobial agents, involving targets such as cellular constituents, cell membranes and thiol groups [182]. Resistance to biocides among L. monocytogenes has been recognized for decades and is on the rise, posing a challenge in the elimination of L. monocytogenes from the food processing environment [183,184]. The extensive use of biocides and exposure to sub-inhibitory concentrations can create a selective pressure which can then cause resistance through mutation or horizontal gene transfer [182]. Sub-inhibitory concentrations of biocides in the environment may stem from inadequate cleaning prior to disinfection, disinfection of wet surfaces, and incorrect dosing [185,186].
Benzalkonium chloride (BC) is a common QAC applied in food production which has a broad spectrum of activity [187]. BC targets cytoplasmic membrane permeability functions [182]. Reduced susceptibility to BC, expressed by some isolates of L. monocytogenes, has been documented since 1998 and several genetic determinants have been linked to this phenotype. In particular, small multidrug resistance (SMR) protein family-encoding genes are associated with reduced susceptibility to BC. In L. monocytogenes these genes include qacH mapped to the transposon Tn6188 [122], emrE located on the genomic island LGI1 [188], emrC [182] and the bcrABC cassette [104]. This latter cassette consists of a transcriptional regulator gene (bcrA) along with two SMR efflux pump genes (bcrB and bcrC) [104,189]. Along with SMR efflux pumps, major facilitator superfamily (MFS) efflux pump-encoding genes such as mdrL and lde have also been described in L. monocytogenes [190,191,192]. These pumps are acquired from recombinant elements and mobile genetic elements (MGE) through horizontal gene transfer. The acquisition of resistance mechanisms to QACs can result in persistence of L. monocytogenes in FPEs, as the concentration of remaining QAC may be inhibitory for susceptible strains, yet subinhibitory for resistant strains, as demonstrated by Ortiz and Lopez [193]. In their study, certain resistant strains of L. monocytogenes were able to form biofilms at 5 mg L−1 BAC, an inhibitory concentration for the majority of strains.
Many studies reported the presence of L. monocytogenes resistant to QACs in different food processing facilities [65,124,194,195]. Several have also linked QAC resistance to persistence of L. monocytogenes in food production environments [65,195,196,197]. BC resistance in L. monocytogenes is considered low-level and is unlikely to lead to resistance to the concentrations of these compounds usually applied in the food industry (generally 200–1000 mg L−1) [70,194]. This low-level resistance, expressed by these efflux pumps, can lead to the reduction of intracellular biocides to sub-inhibitory levels, leading to prolonged survival [198]. The correlations between low-level resistance to QACs and persistence of L. monocytogenes in FPEs are scarce [124,193,199,200,201]. This can also occur in the environment. In domestic wastewater, for example, the average concentration of QACs is around 0.5 mg L−1, decreasing to 0.05 mg L−1 in wastewater treatment plant effluents [194]. This can lead to environmental persistence of L. monocytogenes which express low-level resistance to QACs.
However, it is often a challenge to interpret data describing the biocide resistance of bacteria. This is due to the lack of standardized criteria defining resistance to disinfectants and, often, L. monocytogenes isolates are characterized as resistant based on survival at concentrations which inhibit most strains [202]. There is also a need for standardized protocols to study biocide susceptibility, as MICs may vary when different methods are applied. Additional investigations are also required into biocide resistance patterns of planktonic versus sessile cells, as the increased resistance expressed by biofilms to biocides is believed to be reduced once bacterial cells return to their planktonic state [149,203]. The ability to form biofilms can vary among strains which are equally resistant to BAC, but have different genetic determinants of BC resistance. This is evident in a study by Ortiz and Lopez-Alonso [201] wherein L. monocytogenes belonging to ST121, containing the gene qacH, formed biofilms at 5 mg L−1. Meanwhile s ST31 isolate which was also resistant, formed no biofilm at the same concentration. Nakamura and Takakura [204] have also shown that QAC resistant L. monocytogenes are quicker to form biofilms than sensitive strains. It is possible that the selection of resistant L. monocytogenes due to exposure to subinhibitory concentrations of QACs may allow for biofilm formation and subsequent persistence in FPEs. As BC tolerance and stress resistance genes are often found on MGEs, susceptible isolates can readily become resistant in the presence of resistant isolates [102,104,130,205,206]. To combat the spread of BC resistance genes and subsequent persistence in FPEs, the use of non-chemical or combined antimicrobial approaches has been suggested [207,208,209]. CC1 and CC4 are commonly associated with infection, while CC9 and CC121 are related to food [61]. CC2 and CC6 that usually harbor BC resistance-encoding genes are associated with infection to a lesser extent than CC1 and CC4 [45]. However, a recent outbreak in Switzerland was attributed to L. monocytogenes CC6 that was found to be persisting in a cheese production facility [210]. Furthermore, L. monocytogenes CC6 is progressively implicated in outbreaks, such as the European-wide outbreak linked to five countries between 2015 and 2018 [73], an outbreak in Switzerland in 2016 [208], the largest global outbreak which occurred between 2017 and 2018 in South Africa [211] and the largest European outbreak in the last 25 years that occurred in Germany [212]. These results may indicate that virulent strains could be simultaneously resistant and persistent within food production environments, having detrimental effects on the food production industry and public health.
6. Conclusions
Many studies have failed to clarify the association between L. monocytogenes persistence and biofilm formation and biocide resistance. As a result, it has been argued that long-term persistence of L. monocytogenes may simply be due to the survival and growth in specific ecological niches found within the food processing environment, rather than adaptation of the bacterium itself. These specific niches may include cracks and crevices of surfaces along with seals and gaskets that can be difficult to clean and disinfect. However, with the advent of novel genome characterization methods, better comparisons among isolates of L. monocytogenes can now be made. These strategies have allowed researchers to determine the specific distribution of L. monocytogenes CCs identified in different environments, as well as to discover unique characteristics associated with them. Epidemiological links between persistence, resistance to disinfectants and biofilm formation have been made in numerous studies, however evolution studies of biofilm formation in response to subinhibitory levels of disinfectants could prove more insightful to describe this relationship. With the emergence of standardized protocols for the measurement of biocide MICs, it is likely that results among different studies will now be more concordant. With the continuous advancement of molecular- and phenotypic-based methods, the ambiguity surrounding our understanding the persistent nature of L. monocytogenes in food production environments will be clarified.
Author Contributions
Conceptualization, S.F., E.M., N.U.; writing—original draft preparation, N.U., E.M., G.M., S.F.; writing—review and visualization, S.F., N.U., G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Department of Agriculture, Food and the Marine.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Buchrieser C., Rusniok C., Kunst F., Cossart P., Glaser P., Listeria C. Comparison of the genome sequences of Listeria monocytogenes and Listeria innocua: Clues for evolution and pathogenicity. FEMS Immunol. Med. Microbiol. 2003;35:207–213. doi: 10.1016/S0928-8244(02)00448-0. [DOI] [PubMed] [Google Scholar]
- 2.Farber J.M., Peterkin P.I. Listeria monocytogenes, a food-borne pathogen. Microbiol. Rev. 1991;55:476–511. doi: 10.1128/mr.55.3.476-511.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quereda J.J., Leclercq A., Moura A., Vales G., Gomez-Martin A., Garcia-Munoz A., Thouvenot P., Tessaud-Rita N., Bracq-Dieye H., Lecuit M. Listeria valentina sp. nov., isolated from a water trough and the faeces of healthy sheep. Int. J. Syst. Evol. Microbiol. 2020;70:5868–5879. doi: 10.1099/ijsem.0.004494. [DOI] [PubMed] [Google Scholar]
- 4.Seeliger H.P. Modern taxonomy of the Listeria group relationship to its pathogenicity. Clin. Investig. Med. 1984;7:217–221. [PubMed] [Google Scholar]
- 5.Guillet C., Join-Lambert O., Le Monnier A., Leclercq A., Mechai F., Mamzer-Bruneel M.F., Bielecka M.K., Scortti M., Disson O., Berche P., et al. Human listeriosis caused by Listeria ivanovii. Emerg. Infect. Dis. 2010;16:136–138. doi: 10.3201/eid1601.091155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cummins J., Casey P.G., Joyce S.A., Gahan C.G. A mariner transposon-based signature-tagged mutagenesis system for the analysis of oral infection by Listeria monocytogenes. PLoS ONE. 2013;8:e75437. doi: 10.1371/journal.pone.0075437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexander A.V., Walker R.L., Johnson B.J., Charlton B.R., Woods L.W. Bovine abortions attributable to Listeria ivanovii: Four cases (1988–1990) J. Am. Vet. Med. Assoc. 1992;200:711–714. [PubMed] [Google Scholar]
- 8.Chand P., Sadana J.R. Outbreak of Listeria ivanovii abortion in sheep in India. Vet. Rec. 1999;145:83–84. doi: 10.1136/vr.145.3.83. [DOI] [PubMed] [Google Scholar]
- 9.Graves L.M., Helsel L.O., Steigerwalt A.G., Morey R.E., Daneshvar M.I., Roof S.E., Orsi R.H., Fortes E.D., Milillo S.R., den Bakker H.C., et al. Listeria marthii sp. nov., isolated from the natural environment, Finger Lakes National Forest. Int. J. Syst. Evol. Microbiol. 2010;60:1280–1288. doi: 10.1099/ijs.0.014118-0. [DOI] [PubMed] [Google Scholar]
- 10.Chiara M., Caruso M., D’Erchia A.M., Manzari C., Fraccalvieri R., Goffredo E., Latorre L., Miccolupo A., Padalino I., Santagada G., et al. Comparative Genomics of Listeria sensu lato: Genus-wide differences in evolutionary dynamics and the progressive gain of complex, potentially pathogenicity-related traits through lateral gene transfer. Genome Biol. Evol. 2015;7:2154–2172. doi: 10.1093/gbe/evv131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rocourt J., Seeliger H.P. Distribution of species of the genus Listeria. Zentralbl. Bakteriol. Mikrobiol. Hyg. A. 1985;259:317–330. [PubMed] [Google Scholar]
- 12.Huang B., Eglezos S., Heron B.A., Smith H., Graham T., Bates J., Savill J. Comparison of multiplex PCR with conventional biochemical methods for the identification of Listeria spp. isolates from food and clinical samples in Queensland, Australia. J. Food Prot. 2007;70:1874–1880. doi: 10.4315/0362-028X-70.8.1874. [DOI] [PubMed] [Google Scholar]
- 13.Nayak D.N., Savalia C.V., Kalyani I.H., Kumar R., Kshirsagar D.P. Isolation, identification, and characterization of Listeria spp. from various animal origin foods. Vet. World. 2015;8:695–701. doi: 10.14202/vetworld.2015.695-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dahshan H., Merwad A.M., Mohamed T.S. Listeria species in broiler poultry farms: Potential public health hazards. J. Microbiol. Biotechnol. 2016;26:1551–1556. doi: 10.4014/jmb.1603.03075. [DOI] [PubMed] [Google Scholar]
- 15.Husu J.R. Epidemiological studies on the occurrence of Listeria monocytogenes in the feces of dairy cattle. J. Vet. Med. B. 1990;37:276–282. doi: 10.1111/j.1439-0450.1990.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 16.Yin Y., Yao H., Doijad S., Kong S., Shen Y., Cai X., Tan W., Wang Y., Feng Y., Ling Z., et al. A hybrid sub-lineage of Listeria monocytogenes comprising hypervirulent isolates. Nat. Commun. 2019;10:4283. doi: 10.1038/s41467-019-12072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feng Y., Yao H., Chen S., Sun X., Yin Y., Jiao X. Rapid detection of hypervirulent serovar 4h Listeria monocytogenes by multiplex PCR. Front. Microbiol. 2020;11:1309. doi: 10.3389/fmicb.2020.01309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doumith M., Buchrieser C., Glaser P., Jacquet C., Martin P. Differentiation of the major Listeria monocytogenes serovars by multiplex PCR. J. Clin. Microbiol. 2004;42:3819–3822. doi: 10.1128/JCM.42.8.3819-3822.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piffaretti J.C., Kressebuch H., Aeschbacher M., Bille J., Bannerman E., Musser J.M., Selander R.K., Rocourt J. Genetic characterization of clones of the bacterium Listeria monocytogenes causing epidemic disease. Proc. Natl. Acad. Sci. USA. 1989;86:3818–3822. doi: 10.1073/pnas.86.10.3818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vines A., Swaminathan B. Identification and characterization of nucleotide sequence differences in three virulence-associated genes of Listeria monocytogenes strains representing clinically important serotypes. Curr. Microbiol. 1998;36:309–318. doi: 10.1007/s002849900315. [DOI] [PubMed] [Google Scholar]
- 21.Ragon M., Wirth T., Hollandt F., Lavenir R., Lecuit M., Le Monnier A., Brisse S. A new perspective on Listeria monocytogenes evolution. PLoS Pathog. 2008;4:e1000146. doi: 10.1371/journal.ppat.1000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vazquez-Boland J.A., Dominguez-Bernal G., Gonzalez-Zorn B., Kreft J., Goebel W. Pathogenicity islands and virulence evolution in Listeria. Microbes Infect. 2001;3:571–584. doi: 10.1016/S1286-4579(01)01413-7. [DOI] [PubMed] [Google Scholar]
- 23.Gudmundsdottir S., Gudbjornsdottir B., Lauzon H.L., Einarsson H., Kristinsson K.G., Kristjansson M. Tracing Listeria monocytogenes isolates from cold-smoked salmon and its processing environment in Iceland using pulsed-field gel electrophoresis. Int. J. Food Microbiol. 2005;101:41–51. doi: 10.1016/j.ijfoodmicro.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 24.Guerini M.N., Brichta-Harhay D.M., Shackelford T.S., Arthur T.M., Bosilevac J.M., Kalchayanand N., Wheeler T.L., Koohmaraie M. Listeria prevalence and Listeria monocytogenes serovar diversity at cull cow and bull processing plants in the United States. J. Food Prot. 2007;70:2578–2582. doi: 10.4315/0362-028X-70.11.2578. [DOI] [PubMed] [Google Scholar]
- 25.Zhu L., Feng X., Zhang L., Zhu R., Luo X. Prevalence and serotypes of Listeria monocytogenes contamination in Chinese beef processing plants. Foodborne Pathog. Dis. 2012;9:556–560. doi: 10.1089/fpd.2011.1088. [DOI] [PubMed] [Google Scholar]
- 26.Almeida G., Magalhaes R., Carneiro L., Santos I., Silva J., Ferreira V., Hogg T., Teixeira P. Foci of contamination of Listeria monocytogenes in different cheese processing plants. Int. J. Food Microbiol. 2013;167:303–309. doi: 10.1016/j.ijfoodmicro.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Camargo A.C., Dias M.R., Cossi M.V., Lanna F.G., Cavicchioli V.Q., Vallim D.C., Pinto P.S., Hofer E., Nero L.A. Serotypes and pulsotypes diversity of Listeria monocytogenes in a beef-processing environment. Foodborne Pathog. Dis. 2015;12:323–326. doi: 10.1089/fpd.2014.1875. [DOI] [PubMed] [Google Scholar]
- 28.Smith A.M., Tau N.P., Smouse S.L., Allam M., Ismail A., Ramalwa N.R., Disenyeng B., Ngomane M., Thomas J. Outbreak of Listeria monocytogenes in South Africa, 2017–2018: Laboratory activities and experiences associated with whole-genome sequencing analysis of isolates. Foodborne Pathog. Dis. 2019;16:524–530. doi: 10.1089/fpd.2018.2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Painset A., Bjorkman J.T., Kiil K., Guillier L., Mariet J.F., Felix B., Amar C., Rotariu O., Roussel S., Perez-Reche F., et al. LiSEQ—Whole-genome sequencing of a cross-sectional survey of Listeria monocytogenes in ready-to-eat foods and human clinical cases in Europe. Microb. Genom. 2019;5 doi: 10.1099/mgen.0.000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rietberg K., Lloyd J., Melius B., Wyman P., Treadwell R., Olson G., Kang M.G., Duchin J.S. Outbreak of Listeria monocytogenes infections linked to a pasteurized ice cream product served to hospitalized patients. Epidemiol. Infect. 2016;144:2728–2731. doi: 10.1017/S0950268815003039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.EFSA. ECDC The European Union One Health 2019 Zoonosesn Report. EFSA J. 2021;19:286. doi: 10.2903/j.efsa.2021.6406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deurenberg R.H., Bathoorn E., Chlebowicz M.A., Couto N., Ferdous M., Garcia-Cobos S., Kooistra-Smid A.M.D., Raangs E.C., Rosema S., Veloo A.C.M., et al. Reprint of “Application of next generation sequencing in clinical microbiology and infection prevention”. J. Biotechnol. 2017;250:2–10. doi: 10.1016/j.jbiotec.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 33.Moran-Gilad J. Whole genome sequencing (WGS) for food-borne pathogen surveillance and control—Taking the pulse. Eurosurveillance. 2017;22:30547. doi: 10.2807/1560-7917.ES.2017.22.23.30547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Das A. Listeriosis in Australia—January to july 2018. Global Biosecurity. 2019;1:1. doi: 10.31646/gbio.9. [DOI] [Google Scholar]
- 35.Kwong J.C., Mercoulia K., Tomita T., Easton M., Li H.Y., Bulach D.M., Stinear T.P., Seemann T., Howden B.P. Prospective whole-genome sequencing enhances national surveillance of Listeria monocytogenes. J. Clin. Microbiol. 2016;54:333–342. doi: 10.1128/JCM.02344-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kathariou S. Listeria monocytogenes virulence and pathogenicity, a food safety perspective. J. Food Prot. 2002;65:1811–1829. doi: 10.4315/0362-028X-65.11.1811. [DOI] [PubMed] [Google Scholar]
- 37.Reddy S., Lawrence M.L. Virulence characterization of Listeria monocytogenes. Methods Mol. Biol. 2014;1157:157–165. doi: 10.1007/978-1-4939-0703-8_13. [DOI] [PubMed] [Google Scholar]
- 38.Rolhion N., Cossart P. How the study of Listeria monocytogenes has led to new concepts in biology. Future Microbiol. 2017;12:621–638. doi: 10.2217/fmb-2016-0221. [DOI] [PubMed] [Google Scholar]
- 39.Pizarro-Cerda J., Cossart P. Listeria monocytogenes: Cell biology of invasion and intracellular growth. Microbiol. Spectr. 2018;6 doi: 10.1128/microbiolspec.GPP3-0013-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matereke L.T., Okoh A.I. Listeria monocytogenes virulence, antimicrobial resistance and environmental persistence: A review. Pathogens. 2020;9:528. doi: 10.3390/pathogens9070528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lecuit M. Listeria monocytogenes, a model in infection biology. Cell Microbiol. 2020;22:e13186. doi: 10.1111/cmi.13186. [DOI] [PubMed] [Google Scholar]
- 42.Disson O., Moura A., Lecuit M. Making sense of the biodiversity and virulence of Listeria monocytogenes. Trends Microbiol. 2021;29:811–822. doi: 10.1016/j.tim.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 43.Nightingale K.K., Windham K., Martin K.E., Yeung M., Wiedmann M. Select Listeria monocytogenes subtypes commonly found in foods carry distinct nonsense mutations in inlA, leading to expression of truncated and secreted internalin A, and are associated with a reduced invasion phenotype for human intestinal epithelial cells. Appl. Environ. Microbiol. 2005;71:8764–8772. doi: 10.1128/AEM.71.12.8764-8772.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hingston P., Chen J., Dhillon B.K., Laing C., Bertelli C., Gannon V., Tasara T., Allen K., Brinkman F.S., Truelstrup Hansen L., et al. Genotypes associated with Listeria monocytogenes isolates displaying impaired or enhanced tolerances to cold, salt, acid, or desiccation stress. Front. Microbiol. 2017;8:369. doi: 10.3389/fmicb.2017.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maury M.M., Bracq-Dieye H., Huang L., Vales G., Lavina M., Thouvenot P., Disson O., Leclercq A., Brisse S., Lecuit M. Author correction: Hypervirulent Listeria monocytogenes clones’ adaptation to mammalian gut accounts for their association with dairy products. Nat. Commun. 2019;10:3619. doi: 10.1038/s41467-019-11625-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pistor S., Chakraborty T., Niebuhr K., Domann E., Wehland J. The ActA protein of Listeria monocytogenes acts as a nucleator inducing reorganization of the actin cytoskeleton. EMBO J. 1994;13:758–763. doi: 10.1002/j.1460-2075.1994.tb06318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng M.I., Chen C., Engstrom P., Portnoy D.A., Mitchell G. Actin-based motility allows Listeria monocytogenes to avoid autophagy in the macrophage cytosol. Cell Microbiol. 2018;20:e12854. doi: 10.1111/cmi.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Travier L., Lecuit M. Listeria monocytogenes ActA: A new function for a ‘classic’ virulence factor. Curr. Opin. Microbiol. 2014;17:53–60. doi: 10.1016/j.mib.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Alvarez-Dominguez C., Vazquez-Boland J.A., Carrasco-Marin E., Lopez-Mato P., Leyva-Cobian F. Host cell heparan sulfate proteoglycans mediate attachment and entry of Listeria monocytogenes, and the listerial surface protein ActA is involved in heparan sulfate receptor recognition. Infect. Immun. 1997;65:78–88. doi: 10.1128/iai.65.1.78-88.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marquis H., Goldfine H., Portnoy D.A. Proteolytic pathways of activation and degradation of a bacterial phospholipase C during intracellular infection by Listeria monocytogenes. J. Cell Biol. 1997;137:1381–1392. doi: 10.1083/jcb.137.6.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gandhi A.J., Perussia B., Goldfine H. Listeria monocytogenes phosphatidylinositol (PI)-specific phospholipase C has low activity on glycosyl-PI-anchored proteins. J. Bacteriol. 1993;175:8014–8017. doi: 10.1128/jb.175.24.8014-8017.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Camilli A., Tilney L.G., Portnoy D.A. Dual roles of plcA in Listeria monocytogenes pathogenesis. Mol. Microbiol. 1993;8:143–157. doi: 10.1111/j.1365-2958.1993.tb01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marquis H., Doshi V., Portnoy D.A. The broad-range phospholipase C and a metalloprotease mediate listeriolysin O-independent escape of Listeria monocytogenes from a primary vacuole in human epithelial cells. Infect. Immun. 1995;63:4531–4534. doi: 10.1128/iai.63.11.4531-4534.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scortti M., Monzo H.J., Lacharme-Lora L., Lewis D.A., Vazquez-Boland J.A. The PrfA virulence regulon. Microbes Infect. 2007;9:1196–1207. doi: 10.1016/j.micinf.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 55.Gedde M.M., Higgins D.E., Tilney L.G., Portnoy D.A. Role of listeriolysin O in cell-to-cell spread of Listeria monocytogenes. Infect. Immun. 2000;68:999–1003. doi: 10.1128/IAI.68.2.999-1003.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dramsi S., Cossart P. Listeriolysin O-mediated calcium influx potentiates entry of Listeria monocytogenes into the human Hep-2 epithelial cell line. Infect. Immun. 2003;71:3614–3618. doi: 10.1128/IAI.71.6.3614-3618.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hamon M.A., Cossart P. K+ efflux is required for histone H3 dephosphorylation by Listeria monocytogenes listeriolysin O and other pore-forming toxins. Infect. Immun. 2011;79:2839–2846. doi: 10.1128/IAI.01243-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stavru F., Cossart P. Listeria infection modulates mitochondrial dynamics. Commun. Integr. Biol. 2011;4:364–366. doi: 10.4161/cib.4.3.15506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dominguez-Bernal G., Muller-Altrock S., Gonzalez-Zorn B., Scortti M., Herrmann P., Monzo H.J., Lacharme L., Kreft J., Vazquez-Boland J.A. A spontaneous genomic deletion in Listeria ivanovii identifies LIPI-2, a species-specific pathogenicity island encoding sphingomyelinase and numerous internalins. Mol. Microbiol. 2006;59:415–432. doi: 10.1111/j.1365-2958.2005.04955.x. [DOI] [PubMed] [Google Scholar]
- 60.Cotter P.D., Draper L.A., Lawton E.M., Daly K.M., Groeger D.S., Casey P.G., Ross R.P., Hill C. Listeriolysin S, a novel peptide haemolysin associated with a subset of lineage I Listeria monocytogenes. PLoS Pathog. 2008;4:e1000144. doi: 10.1371/journal.ppat.1000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maury M.M., Tsai Y.H., Charlier C., Touchon M., Chenal-Francisque V., Leclercq A., Criscuolo A., Gaultier C., Roussel S., Brisabois A., et al. Uncovering Listeria monocytogenes hypervirulence by harnessing its biodiversity. Nat. Genet. 2016;48:308–313. doi: 10.1038/ng.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leong D., Alvarez-Ordonez A., Jordan K. Monitoring occurrence and persistence of Listeria monocytogenes in foods and food processing environments in the Republic of Ireland. Front. Microbiol. 2014;5:436. doi: 10.3389/fmicb.2014.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Harvey J., Gilmour A. Application of multilocus enzyme electrophoresis and restriction fragment length polymorphism analysis to the typing of Listeria monocytogenes strains isolated from raw milk, nondairy foods, and clinical and veterinary sources. Appl. Environ. Microbiol. 1994;60:1547–1553. doi: 10.1128/aem.60.5.1547-1553.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Melero B., Manso B., Stessl B., Hernandez M., Wagner M., Rovira J., Rodriguez-Lazaro D. Distribution and persistence of Listeria monocytogenes in a heavily contaminated poultry processing facility. J. Food Prot. 2019;82:1524–1531. doi: 10.4315/0362-028X.JFP-19-087. [DOI] [PubMed] [Google Scholar]
- 65.Cherifi T., Arsenault J., Pagotto F., Quessy S., Cote J.C., Neira K., Fournaise S., Bekal S., Fravalo P. Distribution, diversity and persistence of Listeria monocytogenes in swine slaughterhouses and their association with food and human listeriosis strains. PLoS ONE. 2020;15:e0236807. doi: 10.1371/journal.pone.0236807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Castro H., Jaakkonen A., Hakkinen M., Korkeala H., Lindstrom M. Occurrence, persistence, and contamination routes of Listeria monocytogenes genotypes on three finnish dairy cattle farms: A longitudinal study. Appl. Environ. Microbiol. 2018;84:e02000-17. doi: 10.1128/AEM.02000-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Leong D., NicAogain K., Luque-Sastre L., McManamon O., Hunt K., Alvarez-Ordonez A., Scollard J., Schmalenberger A., Fanning S., O’Byrne C., et al. A 3-year multi-food study of the presence and persistence of Listeria monocytogenes in 54 small food businesses in Ireland. Int. J. Food Microbiol. 2017;249:18–26. doi: 10.1016/j.ijfoodmicro.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 68.D’Arrigo M., Mateo-Vivaracho L., Guillamon E., Fernandez-Leon M.F., Bravo D., Peiroten A., Medina M., Garcia-Lafuente A. Characterization of persistent Listeria monocytogenes strains from ten dry-cured ham processing facilities. Food Microbiol. 2020;92:103581. doi: 10.1016/j.fm.2020.103581. [DOI] [PubMed] [Google Scholar]
- 69.Hurley D., Luque-Sastre L., Parker C.T., Huynh S., Eshwar A.K., Nguyen S.V., Andrews N., Moura A., Fox E.M., Jordan K., et al. Whole-genome sequencing-based characterization of 100 Listeria monocytogenes isolates collected from food processing environments over a four-year period. mSphere. 2019;4:e00252-19. doi: 10.1128/mSphere.00252-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ferreira V., Wiedmann M., Teixeira P., Stasiewicz M.J. Listeria monocytogenes persistence in food-associated environments: Epidemiology, strain characteristics, and implications for public health. J. Food Prot. 2014;77:150–170. doi: 10.4315/0362-028X.JFP-13-150. [DOI] [PubMed] [Google Scholar]
- 71.Ryan S., Hill C., Gahan C.G. Acid stress responses in Listeria monocytogenes. Adv. Appl. Microbiol. 2008;65:67–91. doi: 10.1016/S0065-2164(08)00603-5. [DOI] [PubMed] [Google Scholar]
- 72.Ricci A., Allende A., Bolton D., Chemaly M., Davies R., Fernandez Escamez P.S., Girones R., Herman L., Koutsoumanis K., Norrung B., et al. Listeria monocytogenes contamination of ready-to-eat foods and the risk for human health in the EU. EFSA J. 2018;16:e05134. doi: 10.2903/j.efsa.2018.5134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.EFSA. ECDC Multi-country outbreak of Listeria monocytogenes serogroup IVb, multi-locus sequence type 6, infections probably linked to frozen corn. EFSA Support. Publ. 2018;15 doi: 10.2903/sp.efsa.2018.EN-1402. [DOI] [Google Scholar]
- 74.Pouillot R., Klontz K.C., Chen Y., Burall L.S., Macarisin D., Doyle M., Bally K.M., Strain E., Datta A.R., Hammack T.S., et al. Infectious dose of Listeria monocytogenes in outbreak linked to ice cream, United States, 2015. Emerg. Infect. Dis. 2016;22:2113–2119. doi: 10.3201/eid2212.160165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Angelo K.M., Conrad A.R., Saupe A., Dragoo H., West N., Sorenson A., Barnes A., Doyle M., Beal J., Jackson K.A., et al. Multistate outbreak of Listeria monocytogenes infections linked to whole apples used in commercially produced, prepackaged caramel apples: United States, 2014–2015. Epidemiol. Infect. 2017;145:848–856. doi: 10.1017/S0950268816003083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.CDC Sprouts and Investigation of Human Listeriosis Cases (Final Update) [(accessed on 15 April 2021)]; Available online: https://www.cdc.gov/listeria/outbreaks/bean-sprouts-11-14/key-resources.html.
- 77.U.S. Department of Agriculture . FSIS Comparative Risk Assessment for Listeria monocytogenes in Ready-to-Eat Meat and Poultry Deli meats. U.S. Department of Agriculture; Washington, DC, USA: 2010. [Google Scholar]
- 78.Stoller A., Stevens M.J.A., Stephan R., Guldimann C. Characteristics of Listeria monocytogenes strains persisting in a meat processing facility over a 4-year period. Pathogens. 2019;8:32. doi: 10.3390/pathogens8010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guidi F., Orsini M., Chiaverini A., Torresi M., Centorame P., Acciari V.A., Salini R., Palombo B., Brandi G., Amagliani G., et al. Hypo- and hyper-virulent Listeria monocytogenes clones persisting in two different food processing plants of central Italy. Microorganisms. 2021;9:376. doi: 10.3390/microorganisms9020376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wieczorek K., Bomba A., Osek J. Whole-genome sequencing-based characterization of Listeria monocytogenes from fish and fish production environments in Poland. Int. J. Mol. Sci. 2020;21:9419. doi: 10.3390/ijms21249419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cherifi T., Carrillo C., Lambert D., Miniai I., Quessy S., Lariviere-Gauthier G., Blais B., Fravalo P. Genomic characterization of Listeria monocytogenes isolates reveals that their persistence in a pig slaughterhouse is linked to the presence of benzalkonium chloride resistance genes. BMC Microbiol. 2018;18:220. doi: 10.1186/s12866-018-1363-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hill C., Cotter P.D., Sleator R.D., Gahan C.G. Bacterial stress response in Listeria monocytogenes: Jumping the hurdles imposed by minimal processing. Int. Dairy J. 2002;12:273–283. doi: 10.1016/S0958-6946(01)00125-X. [DOI] [Google Scholar]
- 83.Bergholz T.M., Bowen B., Wiedmann M., Boor K.J. Listeria monocytogenes shows temperature-dependent and -independent responses to salt stress, including responses that induce cross-protection against other stresses. Appl. Environ. Microbiol. 2012;78:2602–2612. doi: 10.1128/AEM.07658-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lou Y., Yousef A.E. Resistance of Listeria monocytogenes to heat after adaptation to environmental stresses. J. Food Prot. 1996;59:465–471. doi: 10.4315/0362-028X-59.5.465. [DOI] [PubMed] [Google Scholar]
- 85.Bucur F.I., Grigore-Gurgu L., Crauwels P., Riedel C.U., Nicolau A.I. Resistance of Listeria monocytogenes to stress conditions encountered in food and food processing environments. Front. Microbiol. 2018;9:2700. doi: 10.3389/fmicb.2018.02700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chaturongakul S., Raengpradub S., Wiedmann M., Boor K.J. Modulation of stress and virulence in Listeria monocytogenes. Trends Microbiol. 2008;16:388–396. doi: 10.1016/j.tim.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chan Y.C., Wiedmann M. Physiology and genetics of Listeria monocytogenes survival and growth at cold temperatures. Crit. Rev. Food Sci. Nutr. 2009;49:237–253. doi: 10.1080/10408390701856272. [DOI] [PubMed] [Google Scholar]
- 88.Abdel Karem H., Mattar Z. Heat resistance and growth of Salmonella enteritidis, Listeria monocytogenes and Aeromonas hydrophila in whole liquid egg. Acta Microbiol. Pol. 2001;50:27–35. [PubMed] [Google Scholar]
- 89.Huang L. Thermal resistance of Listeria monocytogenes, Salmonella heidelberg, and Escherichia coli O157:H7 at elevated temperatures. J. Food Prot. 2004;67:1666–1670. doi: 10.4315/0362-028X-67.8.1666. [DOI] [PubMed] [Google Scholar]
- 90.Sallami L., Marcotte M., Naim F., Ouattara B., Leblanc C., Saucier L. Heat inactivation of Listeria monocytogenes and Salmonella enterica serovar Typhi in a typical bologna matrix during an industrial cooking-cooling cycle. J. Food Prot. 2006;69:3025–3030. doi: 10.4315/0362-028X-69.12.3025. [DOI] [PubMed] [Google Scholar]
- 91.Hill D., Sugrue I., Arendt E., Hill C., Stanton C., Ross R.P. Recent advances in microbial fermentation for dairy and health. F1000Research. 2017;6:751. doi: 10.12688/f1000research.10896.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Caplice E., Fitzgerald G.F. Food fermentations: Role of microorganisms in food production and preservation. Int. J. Food Microbiol. 1999;50:131–149. doi: 10.1016/S0168-1605(99)00082-3. [DOI] [PubMed] [Google Scholar]
- 93.Davis M.J., Coote P.J., O’Byrne C.P. Acid tolerance in Listeria monocytogenes: The adaptive acid tolerance response (ATR) and growth-phase-dependent acid resistance. Microbiology. 1996;142:2975–2982. doi: 10.1099/13500872-142-10-2975. [DOI] [PubMed] [Google Scholar]
- 94.Chorianopoulos N., Giaouris E., Grigoraki I., Skandamis P., Nychas G.J. Effect of acid tolerance response (ATR) on attachment of Listeria monocytogenes Scott A to stainless steel under extended exposure to acid or/and salt stress and resistance of sessile cells to subsequent strong acid challenge. Int. J. Food Microbiol. 2011;145:400–406. doi: 10.1016/j.ijfoodmicro.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 95.Burgess C.M., Gianotti A., Gruzdev N., Holah J., Knochel S., Lehner A., Margas E., Esser S.S., Sela Saldinger S., Tresse O. The response of foodborne pathogens to osmotic and desiccation stresses in the food chain. Int. J. Food Microbiol. 2016;221:37–53. doi: 10.1016/j.ijfoodmicro.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 96.Bae D., Liu C., Zhang T., Jones M., Peterson S.N., Wang C. Global gene expression of Listeria monocytogenes to salt stress. J. Food Prot. 2012;75:906–912. doi: 10.4315/0362-028X.JFP-11-282. [DOI] [PubMed] [Google Scholar]
- 97.Duche O., Tremoulet F., Glaser P., Labadie J. Salt stress proteins induced in Listeria monocytogenes. Appl. Environ. Microbiol. 2002;68:1491–1498. doi: 10.1128/AEM.68.4.1491-1498.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cleveland J., Montville T.J., Nes I.F., Chikindas M.L. Bacteriocins: Safe, natural antimicrobials for food preservation. Int. J. Food Microbiol. 2001;71:1–20. doi: 10.1016/S0168-1605(01)00560-8. [DOI] [PubMed] [Google Scholar]
- 99.Wiedemann I., Breukink E., van Kraaij C., Kuipers O.P., Bierbaum G., de Kruijff B., Sahl H.G. Specific binding of nisin to the peptidoglycan precursor lipid II combines pore formation and inhibition of cell wall biosynthesis for potent antibiotic activity. J. Biol. Chem. 2001;276:1772–1779. doi: 10.1074/jbc.M006770200. [DOI] [PubMed] [Google Scholar]
- 100.Ming X., Daeschel M.A. Correlation of cellular phospholipid content with nisin resistance of Listeria monocytogenes Scott A. J. Food Prot. 1995;58:416–420. doi: 10.4315/0362-028X-58.4.416. [DOI] [PubMed] [Google Scholar]
- 101.Verheul A., Russell N.J., Van T.H.R., Rombouts F.M., Abee T. Modifications of membrane phospholipid composition in nisin-resistant Listeria monocytogenes Scott A. Appl. Environ. Microbiol. 1997;63:3451–3457. doi: 10.1128/aem.63.9.3451-3457.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuenne C., Voget S., Pischimarov J., Oehm S., Goesmann A., Daniel R., Hain T., Chakraborty T. Comparative analysis of plasmids in the genus Listeria. PLoS ONE. 2010;5:e0012511. doi: 10.1371/journal.pone.0012511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Diaz Ricci J.C., Hernandez M.E. Plasmid effects on Escherichia coli metabolism. Crit. Rev. Biotechnol. 2000;20:79–108. doi: 10.1080/07388550008984167. [DOI] [PubMed] [Google Scholar]
- 104.Elhanafi D., Dutta V., Kathariou S. Genetic characterization of plasmid-associated benzalkonium chloride resistance determinants in a Listeria monocytogenes strain from the 1998–1999 outbreak. Appl. Environ. Microbiol. 2010;76:8231–8238. doi: 10.1128/AEM.02056-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rakic-Martinez M., Drevets D.A., Dutta V., Katic V., Kathariou S. Listeria monocytogenes strains selected on ciprofloxacin or the disinfectant benzalkonium chloride exhibit reduced susceptibility to ciprofloxacin, gentamicin, benzalkonium chloride, and other toxic compounds. Appl. Environ. Microbiol. 2011;77:8714–8721. doi: 10.1128/AEM.05941-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Katharios-Lanwermeyer S., Rakic-Martinez M., Elhanafi D., Ratani S., Tiedje J.M., Kathariou S. Coselection of cadmium and benzalkonium chloride resistance in conjugative transfers from nonpathogenic Listeria spp. to other Listeriae. Appl. Environ. Microbiol. 2012;78:7549–7556. doi: 10.1128/AEM.02245-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lebrun M., Loulergue J., Chaslus-Dancla E., Audurier A. Plasmids in Listeria monocytogenes in relation to cadmium resistance. Appl. Environ. Microbiol. 1992;58:3183–3186. doi: 10.1128/aem.58.9.3183-3186.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Franciosa G., Maugliani A., Scalfaro C., Floridi F., Aureli P. Expression of internalin A and biofilm formation among Listeria monocytogenes clinical isolates. Int. J. Immunopathol. Pharmacol. 2009;22:183–193. doi: 10.1177/039463200902200121. [DOI] [PubMed] [Google Scholar]
- 109.Piercey M.J., Hingston P.A., Truelstrup Hansen L. Genes involved in Listeria monocytogenes biofilm formation at a simulated food processing plant temperature of 15 degrees C. Int. J. Food Microbiol. 2016;223:63–74. doi: 10.1016/j.ijfoodmicro.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 110.Ryan S., Begley M., Hill C., Gahan C.G. A five-gene stress survival islet (SSI-1) that contributes to the growth of Listeria monocytogenes in suboptimal conditions. J. Appl. Microbiol. 2010;109:984–995. doi: 10.1111/j.1365-2672.2010.04726.x. [DOI] [PubMed] [Google Scholar]
- 111.Arguedas-Villa C., Kovacevic J., Allen K.J., Stephan R., Tasara T. Cold growth behaviour and genetic comparison of Canadian and Swiss Listeria monocytogenes strains associated with the food supply chain and human listeriosis cases. Food Microbiol. 2014;40:81–87. doi: 10.1016/j.fm.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 112.Karatzas K.A., Wouters J.A., Gahan C.G., Hill C., Abee T., Bennik M.H. The CtsR regulator of Listeria monocytogenes contains a variant glycine repeat region that affects piezotolerance, stress resistance, motility and virulence. Mol. Microbiol. 2003;49:1227–1238. doi: 10.1046/j.1365-2958.2003.03636.x. [DOI] [PubMed] [Google Scholar]
- 113.Schwartz B., Ciesielski C.A., Broome C.V., Gaventa S., Brown G.R., Gellin B.G., Hightower A.W., Mascola L. Association of sporadic listeriosis with consumption of uncooked hot dogs and undercooked chicken. Lancet. 1998;2:779–782. doi: 10.1016/s0140-6736(88)92425-7. [DOI] [PubMed] [Google Scholar]
- 114.Graves L.M., Hunter S.B., Ong A.R., Schoonmaker-Bopp D., Hise K., Kornstein L., DeWitt W.E., Hayes P.S., Dunne E., Mead P., et al. Microbiological aspects of the investigation that traced the 1998 outbreak of listeriosis in the United States to contaminated hot dogs and establishment of molecular subtyping-based surveillance for Listeria monocytogenes in the PulseNet network. J. Clin. Microbiol. 2005;43:2350–2355. doi: 10.1128/JCM.43.5.2350-2355.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mead P.S., Dunne E.F., Graves L., Wiedmann M., Patrick M., Hunter S., Salehi E., Mostashari F., Craig A., Mshar P., et al. Nationwide outbreak of listeriosis due to contaminated meat. Epidemiol. Infect. 2006;134:744–751. doi: 10.1017/S0950268805005376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gilot P., Genicot A., Andre P. Serotyping and esterase typing for analysis of Listeria monocytogenes populations recovered from foodstuffs and from human patients with listeriosis in Belgium. J. Clin. Microbiol. 1996;34:1007–1010. doi: 10.1128/jcm.34.4.1007-1010.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Baek S.Y., Lim S.Y., Lee D.H., Min K.H., Kim C.M. Incidence and characterization of Listeria monocytogenes from domestic and imported foods in Korea. J. Food Prot. 2000;63:186–189. doi: 10.4315/0362-028X-63.2.186. [DOI] [PubMed] [Google Scholar]
- 118.Choi Y.C., Cho S.Y., Park B.K., Chung D.H., Oh D.H. Incidence and characterization of Listeria spp. from foods available in Korea. J. Food Prot. 2001;64:554–558. doi: 10.4315/0362-028X-64.4.554. [DOI] [PubMed] [Google Scholar]
- 119.Gilbreth S.E., Call J.E., Wallace F.M., Scott V.N., Chen Y., Luchansky J.B. Relatedness of Listeria monocytogenes Isolates recovered from selected ready-to-eat foods and listeriosis patients in the United States. Appl. Environ. Microbiol. 2005;71:8115–8122. doi: 10.1128/AEM.71.12.8115-8122.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thevenot D., Delignette-Muller M.L., Christieans S., Vernozy-Rozand C. Prevalence of Listeria monocytogenes in 13 dried sausage processing plants and their products. Int. J. Food Microbiol. 2005;102:85–94. doi: 10.1016/j.ijfoodmicro.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 121.Hein I., Klinger S., Dooms M., Flekna G., Stessl B., Leclercq A., Hill C., Allerberger F., Wagner M. Stress survival islet 1 (SSI-1) survey in Listeria monocytogenes reveals an insert common to Listeria innocua in sequence type 121 L. monocytogenes strains. Appl. Environ. Microbiol. 2011;77:2169–2173. doi: 10.1128/AEM.02159-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Schmitz-Esser S., Muller A., Stessl B., Wagner M. Genomes of sequence type 121 Listeria monocytogenes strains harbor highly conserved plasmids and prophages. Front. Microbiol. 2015;6:380. doi: 10.3389/fmicb.2015.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Holch A., Webb K., Lukjancenko O., Ussery D., Rosenthal B.M., Gram L. Genome sequencing identifies two nearly unchanged strains of persistent Listeria monocytogenes isolated at two different fish processing plants sampled 6 years apart. Appl. Environ. Microbiol. 2013;79:2944–2951. doi: 10.1128/AEM.03715-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fox E.M., Leonard N., Jordan K. Physiological and transcriptional characterization of persistent and nonpersistent Listeria monocytogenes isolates. Appl. Environ. Microbiol. 2011;77:6559–6569. doi: 10.1128/AEM.05529-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Begley M., Sleator R.D., Gahan C.G., Hill C. Contribution of three bile-associated loci, bsh, pva, and btlB, to gastrointestinal persistence and bile tolerance of Listeria monocytogenes. Infect. Immun. 2005;73:894–904. doi: 10.1128/IAI.73.2.894-904.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cotter P.D., Ryan S., Gahan C.G., Hill C. Presence of GadD1 glutamate decarboxylase in selected Listeria monocytogenes strains is associated with an ability to grow at low pH. Appl. Environ. Microbiol. 2005;71:2832–2839. doi: 10.1128/AEM.71.6.2832-2839.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Harter E., Wagner E.M., Zaiser A., Halecker S., Wagner M., Rychli K. Stress survival islet 2, predominantly present in Listeria monocytogenes strains of sequence type 121, is involved in the alkaline and oxidative stress responses. Appl. Environ. Microbiol. 2017;83:e00827-17. doi: 10.1128/AEM.00827-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Casey A., Fox E.M., Schmitz-Esser S., Coffey A., McAuliffe O., Jordan K. Transcriptome analysis of Listeria monocytogenes exposed to biocide stress reveals a multi-system response involving cell wall synthesis, sugar uptake, and motility. Front. Microbiol. 2014;5:68. doi: 10.3389/fmicb.2014.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Suo Y., Liu Y., Zhou X., Huang Y., Shi C., Matthews K., Shi X. Impact of Sod on the expression of stress-related genes in Listeria monocytogenes 4b G with/without paraquat treatment. J. Food Sci. 2014;79:M1745–M1749. doi: 10.1111/1750-3841.12545. [DOI] [PubMed] [Google Scholar]
- 130.Muller A., Rychli K., Zaiser A., Wieser C., Wagner M., Schmitz-Esser S. The Listeria monocytogenes transposon Tn6188 provides increased tolerance to various quaternary ammonium compounds and ethidium bromide. FEMS Microbiol. Lett. 2014;361:166–173. doi: 10.1111/1574-6968.12626. [DOI] [PubMed] [Google Scholar]
- 131.Muller A., Rychli K., Muhterem-Uyar M., Zaiser A., Stessl B., Guinane C.M., Cotter P.D., Wagner M., Schmitz-Esser S. Tn6188—A novel transposon in Listeria monocytogenes responsible for tolerance to benzalkonium chloride. PLoS ONE. 2013;8:e76835. doi: 10.1371/journal.pone.0076835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hoffmann R.F., McLernon S., Feeney A., Hill C., Sleator R.D. A single point mutation in the listerial betL sigma(A)-dependent promoter leads to improved osmo- and chill-tolerance and a morphological shift at elevated osmolarity. Bioengineered. 2013;4:401–407. doi: 10.4161/bioe.24094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Read T.D., Massey R.C. Characterizing the genetic basis of bacterial phenotypes using genome-wide association studies: A new direction for bacteriology. Genome Med. 2014;6:109. doi: 10.1186/s13073-014-0109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Falush D. Bacterial genomics: Microbial GWAS coming of age. Nat. Microbiol. 2016;1:16059. doi: 10.1038/nmicrobiol.2016.59. [DOI] [PubMed] [Google Scholar]
- 135.Kazmierczak M.J., Mithoe S.C., Boor K.J., Wiedmann M. Listeria monocytogenes sigma B regulates stress response and virulence functions. J. Bacteriol. 2003;185:5722–5734. doi: 10.1128/JB.185.19.5722-5734.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Voelker U., Dufour A., Haldenwang W.G. The Bacillus subtilis rsbU gene product is necessary for RsbX-dependent regulation of sigma B. J. Bacteriol. 1995;177:114–122. doi: 10.1128/jb.177.1.114-122.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fritsch L., Felten A., Palma F., Mariet J.F., Radomski N., Mistou M.Y., Augustin J.C., Guillier L. Insights from genome-wide approaches to identify variants associated to phenotypes at pan-genome scale: Application to L. monocytogenes’ ability to grow in cold conditions. Int. J. Food Microbiol. 2019;291:181–188. doi: 10.1016/j.ijfoodmicro.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 138.Huang H.W., Hsu C.P., Yang B.B., Wang C.Y. Potential utility of high-pressure processing to address the risk of food allergen concerns. Compr. Rev. Food Sci. Food Saf. 2014;13:78–90. doi: 10.1111/1541-4337.12045. [DOI] [PubMed] [Google Scholar]
- 139.Van Boeijen I.K., Moezelaar R., Abee T., Zwietering M.H. Inactivation kinetics of three Listeria monocytogenes strains under high hydrostatic pressure. J. Food Prot. 2008;71:2007–2013. doi: 10.4315/0362-028X-71.10.2007. [DOI] [PubMed] [Google Scholar]
- 140.Góngora-Nieto M.M., Sepúlveda D.R., Pedrow P., Barbosa-Cánovas G.V., Swanson B.G. Food processing by pulsed electric fields: Treatment delivery, inactivation level, and regulatory aspects. LWT Food Sci. Technol. 2002;35:375–388. doi: 10.1006/fstl.2001.0880. [DOI] [Google Scholar]
- 141.Lado B.H., Yousef A.E. Alternative food-preservation technologies: Efficacy and mechanisms. Microbes Infect. 2002;4:433–440. doi: 10.1016/S1286-4579(02)01557-5. [DOI] [PubMed] [Google Scholar]
- 142.Gómez-López V.M., Ragaert P., Debevere J., Devlieghere F. Pulsed light for food decontamination: A review. Trends Food Sci. Technol. 2007;18:464–473. doi: 10.1016/j.tifs.2007.03.010. [DOI] [Google Scholar]
- 143.Rastogi R.P., Richa , Kumar A., Tyagi M.B., Sinha R.P. Molecular mechanisms of ultraviolet radiation-induced DNA damage and repair. J. Nucleic Acids. 2010;2010:592980. doi: 10.4061/2010/592980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Beauchamp S., Lacroix M. Resistance of the genome of Escherichia coli and Listeria monocytogenes to irradiation evaluated by the induction of cyclobutane pyrimidine dimers and 6-4 photoproducts using gamma and UV-C radiations. Radiat. Phys. Chem. 2012;81:1193–1197. doi: 10.1016/j.radphyschem.2011.11.007. [DOI] [Google Scholar]
- 145.Chmielewski R., Frank J. Biofilm formation and control in food processing facilities. Compr. Rev. Food Sci. Food Saf. 2003;2:22–32. doi: 10.1111/j.1541-4337.2003.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 146.Giaouris E., Heir E., Hebraud M., Chorianopoulos N., Langsrud S., Moretro T., Habimana O., Desvaux M., Renier S., Nychas G.J. Attachment and biofilm formation by foodborne bacteria in meat processing environments: Causes, implications, role of bacterial interactions and control by alternative novel methods. Meat Sci. 2014;97:298–309. doi: 10.1016/j.meatsci.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 147.Colagiorgi A., Bruini I., Di Ciccio P.A., Zanardi E., Ghidini S., Ianieri A. Listeria monocytogenes biofilms in the wonderland of food industry. Pathogens. 2017;6:41. doi: 10.3390/pathogens6030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Costerton J.W., Lewandowski Z., Caldwell D.E., Korber D.R., Lappin-Scott H.M. Microbial biofilms. Annu Rev. Microbiol. 1995;49:711–745. doi: 10.1146/annurev.mi.49.100195.003431. [DOI] [PubMed] [Google Scholar]
- 149.Bridier A., Briandet R., Thomas V., Dubois-Brissonnet F. Resistance of bacterial biofilms to disinfectants: A review. Biofouling. 2011;27:1017–1032. doi: 10.1080/08927014.2011.626899. [DOI] [PubMed] [Google Scholar]
- 150.Esbelin J., Santos T., Hebraud M. Desiccation: An environmental and food industry stress that bacteria commonly face. Food Microbiol. 2018;69:82–88. doi: 10.1016/j.fm.2017.07.017. [DOI] [PubMed] [Google Scholar]
- 151.Price R., Jayeola V., Niedermeyer J., Parsons C., Kathariou S. The Listeria monocytogenes key virulence determinants hly and prfA are involved in biofilm formation and aggregation but not colonization of fresh produce. Pathogens. 2018;7:18. doi: 10.3390/pathogens7010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rodriguez-Lopez P., Rodriguez-Herrera J.J., Vazquez-Sanchez D., Lopez Cabo M. Current knowledge on Listeria monocytogenes biofilms in food-related environments: Incidence, resistance to biocides, ecology and biocontrol. Foods. 2018;7:85. doi: 10.3390/foods7060085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wagner E.M., Pracser N., Thalguter S., Fischel K., Rammer N., Pospisilova L., Alispahic M., Wagner M., Rychli K. Identification of biofilm hotspots in a meat processing environment: Detection of spoilage bacteria in multi-species biofilms. Int. J. Food Microbiol. 2020;328:108668. doi: 10.1016/j.ijfoodmicro.2020.108668. [DOI] [PubMed] [Google Scholar]
- 154.Blackman I.C., Frank J.F. Growth of Listeria monocytogenes as a biofilm on various food-processing surfaces. J. Food Prot. 1996;59:827–831. doi: 10.4315/0362-028X-59.8.827. [DOI] [PubMed] [Google Scholar]
- 155.Chae M.S., Schraft H., Truelstrup Hansen L., Mackereth R. Effects of physicochemical surface characteristics of Listeria monocytogenes strains on attachment to glass. Food Microbiol. 2006;23:250–259. doi: 10.1016/j.fm.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 156.Chavant P., Martinie B., Meylheuc T., Bellon-Fontaine M.N., Hebraud M. Listeria monocytogenes LO28: Surface physicochemical properties and ability to form biofilms at different temperatures and growth phases. Appl. Environ. Microbiol. 2002;68:728–737. doi: 10.1128/AEM.68.2.728-737.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Spurlock A.T., Zottola E.A. Growth and attachment of Listeria monocytogenes to cast iron. J. Food Prot. 1991;54:925–929. doi: 10.4315/0362-028X-54.12.925. [DOI] [PubMed] [Google Scholar]
- 158.Manso B., Melero B., Stessl B., Fernandez-Natal I., Jaime I., Hernandez M., Wagner M., Rovira J., Rodriguez-Lazaro D. Characterization of virulence and persistence abilities of Listeria monocytogenes strains isolated from food processing premises. J. Food Prot. 2019;82:1922–1930. doi: 10.4315/0362-028X.JFP-19-109. [DOI] [PubMed] [Google Scholar]
- 159.Lee B.H., Cole S., Badel-Berchoux S., Guillier L., Felix B., Krezdorn N., Hebraud M., Bernardi T., Sultan I., Piveteau P. Biofilm formation of Listeria monocytogenes strains under food processing environments and pan-genome-wide association study. Front. Microbiol. 2019;10:2698. doi: 10.3389/fmicb.2019.02698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Stepanovic S., Cirkovic I., Ranin L., Svabic-Vlahovic M. Biofilm formation by Salmonella spp. and Listeria monocytogenes on plastic surface. Lett. Appl. Microbiol. 2004;38:428–432. doi: 10.1111/j.1472-765X.2004.01513.x. [DOI] [PubMed] [Google Scholar]
- 161.Mureddu A., Mazza R., Fois F., Meloni D., Bacciu R., Piras F., Mazzette R. Listeria monocytogenes persistence in ready-to-eat sausages and in processing plants. Ital. J. Food Saf. 2014;3:1697. doi: 10.4081/ijfs.2014.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Pasquali F., Palma F., Guillier L., Lucchi A., De Cesare A., Manfreda G. Listeria monocytogenes sequence types 121 and 14 repeatedly isolated within one year of sampling in a rabbit meat processing plant: Persistence and ecophysiology. Front. Microbiol. 2018;9:596. doi: 10.3389/fmicb.2018.00596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Takahashi H., Miya S., Igarashi K., Suda T., Kuramoto S., Kimura B. Biofilm formation ability of Listeria monocytogenes isolates from raw ready-to-eat seafood. J. Food Prot. 2009;72:1476–1480. doi: 10.4315/0362-028X-72.7.1476. [DOI] [PubMed] [Google Scholar]
- 164.Borucki M.K., Peppin J.D., White D., Loge F., Call D.R. Variation in biofilm formation among strains of Listeria monocytogenes. Appl. Environ. Microbiol. 2003;69:7336–7342. doi: 10.1128/AEM.69.12.7336-7342.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Barbosa J., Borges S., Camilo R., Magalhaes R., Ferreira V., Santos I., Silva J., Almeida G., Teixeira P. Biofilm formation among clinical and food isolates of Listeria monocytogenes. Int. J. Microbiol. 2013;2013:524975. doi: 10.1155/2013/524975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Djordjevic D., Wiedmann M., McLandsborough L.A. Microtiter plate assay for assessment of Listeria monocytogenes biofilm formation. Appl. Environ. Microbiol. 2002;68:2950–2958. doi: 10.1128/AEM.68.6.2950-2958.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Keeney K., Trmcic A., Zhu Z., Delaquis P., Wang S. Stress survival islet 1 contributes to serotype-specific differences in biofilm formation in Listeria monocytogenes. Lett. Appl. Microbiol. 2018;67:530–536. doi: 10.1111/lam.13072. [DOI] [PubMed] [Google Scholar]
- 168.Gueriri I., Cyncynatus C., Dubrac S., Arana A.T., Dussurget O., Msadek T. The DegU orphan response regulator of Listeria monocytogenes autorepresses its own synthesis and is required for bacterial motility, virulence and biofilm formation. Microbiology. 2008;154:2251–2264. doi: 10.1099/mic.0.2008/017590-0. [DOI] [PubMed] [Google Scholar]
- 169.Kumar S., Parvathi A., George J., Krohne G., Karunasagar I., Karunasagar I. A study on the effects of some laboratory derived genetic mutations on biofilm formation by Listeria monocytogenes. World J. Microbiol. Biotechnol. 2009;25:527–531. doi: 10.1007/s11274-008-9919-8. [DOI] [Google Scholar]
- 170.Knudsen G.M., Olsen J.E., Dons L. characterization of DegU, a response regulator in Listeria monocytogenes, involved in regulation of motility and contributes to virulence. FEMS Microbiol. Lett. 2006;240:171–179. doi: 10.1016/j.femsle.2004.09.039. [DOI] [PubMed] [Google Scholar]
- 171.Williams T., Bauer S., Beier D., Kuhn M. Construction and characterisation of Listeria monocytogenes mutants with in-frame deletions in the response regulator genes identified in the genome sequence. Infect. Immun. 2005;73:3152–3159. doi: 10.1128/IAI.73.5.3152-3159.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Riedel C.U., Monk I.R., Casey P.G., Waidmann M.S., Gahan C.G., Hill C. AgrD-dependent quorum sensing affects biofilm formation, invasion, virulence and global gene expression profiles in Listeria monocytogenes. Mol. Microbiol. 2009;71:1177–1189. doi: 10.1111/j.1365-2958.2008.06589.x. [DOI] [PubMed] [Google Scholar]
- 173.Rieu A., Weidmann S., Garmyn D., Piveteau P., Guzzo J. Agr system of Listeria monocytogenes EGD-e: Role in adherence and differential expression pattern. Appl. Environ. Microbiol. 2007;73:6125–6133. doi: 10.1128/AEM.00608-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Jordan S.J., Perni S., Glenn S., Fernandes I., Barbosa M., Sol M., Tenreiro R.P., Chambel L., Barata B., Zilhao I., et al. Listeria monocytogenes biofilm-associated protein (BapL) may contribute to surface attachment of L. monocytogenes but is absent from many field isolates. Appl. Environ. Microbiol. 2008;74:5451–5456. doi: 10.1128/AEM.02419-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.van der Veen S., Abee T. Importance of SigB for Listeria monocytogenes static and continuous-flow biofilm formation and disinfectant resistance. Appl. Environ. Microbiol. 2010;76:7854–7860. doi: 10.1128/AEM.01519-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chang Y., Gu W., Fischer N., McLandsborough L. Identification of genes involved in Listeria monocytogenes biofilm formation by mariner-based transposon mutagenesis. Appl. Microbiol. Biotechnol. 2012;93:2051–2062. doi: 10.1007/s00253-011-3719-z. [DOI] [PubMed] [Google Scholar]
- 177.Alonso A.N., Perry K.J., Regeimbal J.M., Regan P.M., Higgins D.E. Identification of Listeria monocytogenes determinants required for biofilm formation. PLoS ONE. 2014;9:e113696. doi: 10.1371/journal.pone.0113696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Di Bonaventura G., Piccolomini R., Paludi D., D’Orio V., Vergara A., Conter M., Ianieri A. Influence of temperature on biofilm formation by Listeria monocytogenes on various food-contact surfaces: Relationship with motility and cell surface hydrophobicity. J. Appl. Microbiol. 2008;104:1552–1561. doi: 10.1111/j.1365-2672.2007.03688.x. [DOI] [PubMed] [Google Scholar]
- 179.Mauder N., Williams T., Fritsch F., Kuhn M., Beier D. Response regulator DegU of Listeria monocytogenes controls temperature-responsive flagellar gene expression in its unphosphorylated state. J. Bacteriol. 2008;190:4777–4781. doi: 10.1128/JB.00258-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.McGann P., Wiedmann M., Boor K.J. The alternative sigma factor sigma B and the virulence gene regulator PrfA both regulate transcription of Listeria monocytogenes internalins. Appl. Environ. Microbiol. 2007;73:2919–2930. doi: 10.1128/AEM.02664-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Liu S., Graham J.E., Bigelow L., Morse P.D., 2nd, Wilkinson B.J. Identification of Listeria monocytogenes genes expressed in response to growth at low temperature. Appl. Environ. Microbiol. 2002;68:1697–1705. doi: 10.1128/AEM.68.4.1697-1705.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.McDonnell G., Russell A.D. Antiseptics and disinfectants: Activity, action, and resistance. Clin. Microbiol. Rev. 1999;12:147–179. doi: 10.1128/CMR.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Harbarth S., Tuan Soh S., Horner C., Wilcox M.H. Is reduced susceptibility to disinfectants and antiseptics a risk in healthcare settings? A point/counterpoint review. J. Hosp. Infect. 2014;87:194–202. doi: 10.1016/j.jhin.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 184.Ortega M., Fernández-Fuentes M.A., Grande Burgos M.J., Abriouel H., Pérez Pulido R., Gálvez A. Biocide tolerance in bacteria. Int. J. Food Microbiol. 2013;162:13–25. doi: 10.1016/j.ijfoodmicro.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 185.Cramer M.M. Food Plant. Sanitation. Design, Maintenance, and Good Manufacturing Practices. CRC Press; Boca Raton, FL, USA: 2006. [Google Scholar]
- 186.Carpentier B., Cerf O. Review—Persistence of Listeria monocytogenes in food industry equipment and premises. Int. J. Food Microbiol. 2011;145:1–8. doi: 10.1016/j.ijfoodmicro.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 187.McBain A.J., Ledder R.G., Moore L.E., Catrenich C.E., Gilbert P. Effects of quaternary-ammonium-based formulations on bacterial community dynamics and antimicrobial susceptibility. Appl. Environ. Microbiol. 2004;70:3449–3456. doi: 10.1128/AEM.70.6.3449-3456.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kovacevic J., Ziegler J., Walecka-Zacharska E., Reimer A., Kitts D.D., Gilmour M.W. Tolerance of Listeria monocytogenes to quaternary ammonium sanitizers is mediated by a novel efflux pump encoded by emrE. Appl. Environ. Microbiol. 2016;82:939–953. doi: 10.1128/AEM.03741-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Dutta V., Elhanafi D., Kathariou S. Conservation and distribution of the benzalkonium chloride resistance cassette bcrABC in Listeria monocytogenes. Appl. Environ. Microbiol. 2013;79:6067–6074. doi: 10.1128/AEM.01751-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tamburro M., Ripabelli G., Vitullo M., Dallman T.J., Pontello M., Amar C.F., Sammarco M.L. Gene expression in Listeria monocytogenes exposed to sublethal concentration of benzalkonium chloride. Comp. Immunol. Microbiol. Infect. Dis. 2015;40:31–39. doi: 10.1016/j.cimid.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 191.Mereghetti L., Quentin R., Marquet-Van Der Mee N., Audurier A. Low sensitivity of Listeria monocytogenes to quaternary ammonium compounds. Appl. Environ. Microbiol. 2000;66:5083–5086. doi: 10.1128/AEM.66.11.5083-5086.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Romanova N.A., Wolffs P.F., Brovko L.Y., Griffiths M.W. Role of efflux pumps in adaptation and resistance of Listeria monocytogenes to benzalkonium chloride. Appl. Environ. Microbiol. 2006;72:3498–3503. doi: 10.1128/AEM.72.5.3498-3503.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Ortiz S., Lopez V., Martinez-Suarez J.V. The influence of subminimal inhibitory concentrations of benzalkonium chloride on biofilm formation by Listeria monocytogenes. Int. J. Food Microbiol. 2014;189:106–112. doi: 10.1016/j.ijfoodmicro.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 194.Tezel U., Pavlostathis S.G. Quaternary ammonium disinfectants: Microbial adaptation, degradation and ecology. Curr. Opin. Biotechnol. 2015;33:296–304. doi: 10.1016/j.copbio.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 195.Moretro T., Schirmer B.C.T., Heir E., Fagerlund A., Hjemli P., Langsrud S. Tolerance to quaternary ammonium compound disinfectants may enhance growth of Listeria monocytogenes in the food industry. Int. J. Food Microbiol. 2017;241:215–224. doi: 10.1016/j.ijfoodmicro.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 196.Martinez-Suarez J.V., Ortiz S., Lopez-Alonso V. Potential impact of the resistance to quaternary ammonium disinfectants on the persistence of Listeria monocytogenes in food processing environments. Front. Microbiol. 2016;7:638. doi: 10.3389/fmicb.2016.00638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Cooper A.L., Carrillo C.D., DeschEnes M., Blais B.W. Genomic markers for quaternary ammonium compound resistance as a persistence indicator for Listeria monocytogenes contamination in food manufacturing environments. J. Food Prot. 2021;84:389–398. doi: 10.4315/JFP-20-328. [DOI] [PubMed] [Google Scholar]
- 198.Piddock L.J. Clinically relevant chromosomally encoded multidrug resistance efflux pumps in bacteria. Clin. Microbiol. Rev. 2006;19:382–402. doi: 10.1128/CMR.19.2.382-402.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Aase B., Sundheim G., Langsrud S., Rorvik L.M. Occurrence of and a possible mechanism for resistance to a quaternary ammonium compound in Listeria monocytogenes. Int. J. Food Microbiol. 2000;62:57–63. doi: 10.1016/S0168-1605(00)00357-3. [DOI] [PubMed] [Google Scholar]
- 200.Lunden J.M., Autio T.J., Sjoberg A.M., Korkeala H.J. Persistent and nonpersistent Listeria monocytogenes contamination in meat and poultry processing plants. J. Food Prot. 2003;66:2062–2069. doi: 10.4315/0362-028X-66.11.2062. [DOI] [PubMed] [Google Scholar]
- 201.Ortiz S., Lopez-Alonso V., Rodriguez P., Martinez-Suarez J.V. The connection between persistent, disinfectant-resistant Listeria monocytogenes strains from two geographically separate iberian pork processing plants: Evidence from comparative genome analysis. Appl. Environ. Microbiol. 2016;82:308–317. doi: 10.1128/AEM.02824-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.EFSA Assessment of the possible effect of the four antimicrobial treatment substances on the emergence of antimicrobial resistance, Scientific Opinion of the Panel on Biological Hazards. EFSA J. 2008;6:659. doi: 10.2903/j.efsa.2008.659. [DOI] [Google Scholar]
- 203.Pan Y., Breidt F., Jr., Kathariou S. Resistance of Listeria monocytogenes biofilms to sanitizing agents in a simulated food processing environment. Appl. Environ. Microbiol. 2006;72:7711–7717. doi: 10.1128/AEM.01065-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Nakamura H., Takakura K., Sone Y., Itano Y., Nishikawa Y. Biofilm formation and resistance to benzalkonium chloride in Listeria monocytogenes isolated from a fish processing plant. J. Food Prot. 2013;76:1179–1186. doi: 10.4315/0362-028X.JFP-12-225. [DOI] [PubMed] [Google Scholar]
- 205.Kremer P.H., Lees J.A., Koopmans M.M., Ferwerda B., Arends A.W., Feller M.M., Schipper K., Valls Seron M., van der Ende A., Brouwer M.C., et al. Benzalkonium tolerance genes and outcome in Listeria monocytogenes meningitis. Clin. Microbiol. Infect. 2017;23:265.e1–265.e7. doi: 10.1016/j.cmi.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Xu D., Nie Q., Wang W., Shi L., Yan H. Characterization of a transferable bcrABC and cadAC genes-harboring plasmid in Listeria monocytogenes strain isolated from food products of animal origin. Int. J. Food Microbiol. 2016;217:117–122. doi: 10.1016/j.ijfoodmicro.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 207.Nguyen U.T., Burrows L.L. DNase I and proteinase K impair Listeria monocytogenes biofilm formation and induce dispersal of pre-existing biofilms. Int. J. Food Microbiol. 2014;187:26–32. doi: 10.1016/j.ijfoodmicro.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 208.Gray J.A., Chandry P.S., Kaur M., Kocharunchitt C., Bowman J.P., Fox E.M. Novel biocontrol methods for Listeria monocytogenes biofilms in food production facilities. Front. Microbiol. 2018;9:605. doi: 10.3389/fmicb.2018.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rodriguez-Lopez P., Carballo-Justo A., Draper L.A., Cabo M.L. Removal of Listeria monocytogenes dual-species biofilms using combined enzyme-benzalkonium chloride treatments. Biofouling. 2017;33:45–58. doi: 10.1080/08927014.2016.1261847. [DOI] [PubMed] [Google Scholar]
- 210.Nuesch-Inderbinen M., Bloemberg G.V., Muller A., Stevens M.J.A., Cernela N., Kolloffel B., Stephan R. Listeriosis caused by persistence of Listeria monocytogenes serotype 4b sequence type 6 in cheese production environment. Emerg. Infect. Dis. 2021;27:284–288. doi: 10.3201/eid2701.203266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Thomas J., Govender N., McCarthy K.M., Erasmus L.K., Doyle T.J., Allam M., Ismail A., Ramalwa N., Sekwadi P., Ntshoe G., et al. Outbreak of Listeriosis in South Africa associated with processed meat. N. Engl. J. Med. 2020;382:632–643. doi: 10.1056/NEJMoa1907462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Halbedel S., Wilking H., Holzer A., Kleta S., Fischer M.A., Luth S., Pietzka A., Huhulescu S., Lachmann R., Krings A., et al. Large nationwide outbreak of invasive Listeriosis associated with blood sausage, Germany, 2018–2019. Emerg. Infect. Dis. 2020;26:1456–1464. doi: 10.3201/eid2607.200225. [DOI] [PMC free article] [PubMed] [Google Scholar]