Abstract
Annexin A1 is a 37 kDa phospholipid-binding protein that is expressed in many tissues and cell types, including leukocytes, lymphocytes and epithelial cells. Although Annexin A1 has been extensively studied for its anti-inflammatory activity, it has been shown that, in the cancer context, its activity switches from anti-inflammatory to pro-inflammatory. Remarkably, Annexin A1 shows pro-invasive and pro-tumoral properties in several cancers either by eliciting autocrine signaling in cancer cells or by inducing a favorable tumor microenvironment. Indeed, the signaling of the N-terminal peptide of AnxA1 has been described to promote the switching of macrophages to the pro-tumoral M2 phenotype. Moreover, AnxA1 has been described to prevent the induction of antigen-specific cytotoxic T cell response and to play an essential role in the induction of regulatory T lymphocytes. In this way, Annexin A1 inhibits the anti-tumor immunity and supports the formation of an immunosuppressed tumor microenvironment that promotes tumor growth and metastasis. For these reasons, in this review we aim to describe the role of Annexin A1 in the establishment of the tumor microenvironment, focusing on the immunosuppressive and immunomodulatory activities of Annexin A1 and on its interaction with the epidermal growth factor receptor.
Keywords: Annexin A1, tumor microenvironment, immune-suppression, cancer aggressiveness
1. Introduction
Neoplastic transformation and progression encompass multiple unknown or poorly described events. In this context, Hanahan and Weinberg proposed different hallmarks that, despite being interrelated, define the principles of tumorigenesis. These hallmarks include the resistance to cell death mechanisms, uncontrolled proliferation, induction of angiogenesis, invasion potential, metastasis formation and immune escape [1]. Cancer cells acquire these hallmarks by modifying the extracellular matrix (ECM) and modulating the behavior of different cell types that surround the tumor. In this way, cancer cells create a unique environment, called the tumor microenvironment (TME), that strongly favors malignancy and cancer dissemination [2]. Unfortunately, the appearance of metastasis profoundly worsens the prognoses of patients, since no efficient therapies are available [3]. It is therefore essential to study the factors that are involved in the establishment of the TME in order to design new therapeutic strategies that could help to avoid cancer spreading and manage metastatic cancer patients. Of particular interest is the understanding of how cancer cells create a TME that favors immune evasion. In this context, it is important to unravel the immunomodulatory role of the protein Annexin A1 (AnxA1), which is the purpose of this review.
2. Anticancer Immune Response and Cancer Immune Escape
The immune system recognizes antigens expressed on the surface of transformed cells, leading to their destruction, thus hampering tumor progression. Remarkably, both standard therapies and targeted therapies induce an anti-tumor immune response, while immunotherapies modulate the immune system of cancer patients. However, the success of these therapies relies on the immunogenicity of the tumor antigens expressed by transformed cells [4]. Hence, those tumors that are strongly immunogenic easily elicit an immune response, while recognition by the immune system is greatly impaired when cancer cells are of low immunogenicity [5]. Interestingly, tumor cells can also develop the immune escape hallmark that takes place either by the capacity of cancer cells of hiding or inhibiting the attack by immune cells. In fact, cancer cells can modulate gene expression and signaling pathways of the immune system, inducing an immune-suppressive phenotype that supports tumor growth and metastasis [6]. In this regard, cancer cells also produce several factors that trigger a persistent inflammation that contributes to suppressing anti-tumor immunity [7]. Indeed, while an acute pro-inflammatory response can exert an anti-tumoral effect, chronic inflammation seems to be always detrimental in the cancer context [8]. A proper anti-tumor immune response relies on the optimal function of both the innate and adaptive immunities [9]. Conforming to this, a balance between a pro-inflammatory response, mediated by eicosanoids and cytokines such as IL-1β, tumor necrosis factor-α (TNF-α) and IL-6, and an anti-inflammatory response mediated by pro-resolving mediators, is also crucial [10].
In order to activate the adaptive immune response, the activity of the antigen-presenting cells (APCs), which are represented by macrophages, dendritic cells (DCs) and B cells, is crucial [11]. In this sense, the T cell receptor (TCR) expressed on naïve T lymphocytes must recognize MHC class II molecules loaded with tumoral peptides on the cell surface of APCs. Besides this, the interaction between the CD28 molecule expressed on T cells and the B7 molecule expressed on APCs, represent a costimulatory signal that is essential for the activation of naïve T cells. Upon these interactions, naïve T cells clonally expand and differentiate into effector or memory cells. Effector T cells are subdivided into (i) three types of CD4+ T helper cells (TH1, TH2 and TH17) with different cytokine expression profiles, (ii) regulatory T cells (Tregs) and (iii) cytotoxic T lymphocytes (CTLs) [12]. TH1 cells produce interferon-gamma (IFN-γ) and are necessary for an effective response against intracellular infectious agents and cancer cells. Indeed, TH1 cells are essential for CTLs activation, therefore for the destruction of infected or cancerous cells [13]. For this purpose, TH1 cells produce cytokines that activate the expression of death receptors on cancer cells [14]. On the other side, when TH1 cells are activated erroneously by self-antigens, they are responsible for the development of autoimmune diseases [15]. TH2 cells express IL-4, IL-5, IL-10 and IL-13, which are related to the humoral response [16]. They are involved in immune reactions against allergens and parasitic infections, while, in the cancer context, TH2 cells can favor tumor growth by enhancing angiogenesis and by inhibiting tumor cell killing [17,18]. TH17 cells are characterized by the production of IL-17 and their pro-inflammatory profile that is implicated in autoimmune and inflammatory disorders [19]. The role of TH17 cells in the cancer context is controversial, since some reports indicate a suppressive role on anti-tumor immunity, while other reports describe their role in enhancing recognition of cancer cells [20,21]. However, there is the possibility for TH17 cells recruited to the tumor site to differentiate into the highly immunosuppressive Tregs [22]. Tregs play an outstanding role in maintaining self-tolerance, thus in avoiding autoimmunity and allergies [23,24]. They are characterized by a CD4+CD25high phenotype and express the transcriptional factor forkhead box P3 (FOXP3). Tregs favor cancer immune evasion by producing the immune-suppressive cytokines IL-10 and IL-35 and transforming growth factor-β (TGF-β) [25], which hamper APC functions or induce apoptosis of APCs [26]. Finally, CTLs are involved in the elimination of virus-infected or neoplastic cells and exert their cytotoxic activity through the Fas receptor pathway or the release of perforins. The cytotoxicity of CTLs can also be indirect through the release of cytokines such as IFN-γ and TNF-α [27].
Different types of APCs drive differentiation toward a specific type of effector T cell. Macrophages are released from the bone marrow as immature monocytes and, after circulating in the blood vessels, migrate to the target tissues to undergo final differentiation into M1 or M2 mature macrophages. M1 macrophages produce pro-inflammatory factors such as IL-12 and TNF-α and promote TH1 response, with potent microbicidal activity [28]. On the other side, M2 macrophages control inflammation, remove apoptotic cells and sustain tissue repair and are induced by IL-4. M2 macrophages enhance immune suppression by producing the cytokines, IL-10 and TGF-β [29,30], and expressing arginase-1 (Arg-1) [31]. Moreover, they also stimulate tumor growth and progression by producing the vascular endothelial growth factor (VEGF), thus supporting the angiogenesis process [32,33,34].
When the TME is enriched in IL-6, IL-1β and TNF-α, DCs achieve a maturation state that activates the adaptive immune system in order to destroy infected or cancer cells [35]. On the other side, two types of DCs are involved in the maintenance of self-tolerance in physiological conditions, the tolerogenic DCs (tDCs) and immature DCs (iDCs). Both hamper the immune response by expressing low levels of co-stimulatory molecules and producing IL-10 and TGF-β [36,37]. Remarkably, cancer cells enrich the environment with immune suppressive factors and cytokines, such as VEGF, IL-10 and TGF-β, which can either induce tDCs or hamper the maturation of DCs [38,39,40]. Immature DCs (iDCs) are found in peripheral tissues where they recognize and phagocyte pathogens or antigens and reduce the production of pro-inflammatory cytokines. When T cells are stimulated either by iDCs or tDCs, a Treg phenotype or an anergic state are triggered [40,41]. Anergic lymphocytes do not respond to their specific antigens; hence, their effector functions and proliferation are inhibited, resulting in immunological tolerance [42]. B cells are also important for the anti-cancer immune response, because, beside producing IgGs that stimulate the T cell response, they can also directly kill cancer cells [43,44]. However, B cells can also acquire a regulatory phenotype (Bregs) that negatively regulates the immune response by producing IL-10, IL-35 and TGF-β [45].
Another class of immune cells that have been implicated in the negative regulation of the immune system is represented by the myeloid-derived suppressor cells (MDSCs). MDSCs are a heterogeneous population of immature myeloid cells that are important for keeping inflammation and autoimmunity at bay [46,47]. Nevertheless, MDSCs contribute to cancer immune escape by producing reactive oxygen species (ROS) [48] that promote the function of Tregs, leading to a decreased activity of effector cells [49]. Notwithstanding, for eliciting an efficient anti-tumor immunity, a cellular component of the innate immune system, the natural killer cells (NK), deserves special attention. Thanks to the expression of perforins, NK cells permeabilize infected or cancer cells and release granzymes, thus exerting cytotoxic activity [50,51]. The absence of MHC class I molecules that characterize certain cancers represents an activation signal for NK cells [52]. Once activated in this manner, NK cells exert their cytotoxic activity on cancer cells. The absence of MHC class I molecules in certain cancer cells represents an activation signal for NK cells. Once activated in this manner, NK cells exert their cytotoxic activity. In addition, NK cells can kill cancer cells by antibody-dependent cellular cytotoxicity. In this case, the receptor CD16 of NK cells binds to tumor-specific antibodies enabling the recognition of membrane-associated tumoral antigens and ultimately leading to the destruction of cancer cells [53].
In order to mount a proper anti-tumor immune response, it is essential that APCs, T, B and NK cells function properly. However, cancer cells take advantage of several tolerance mechanisms modulating the phenotype of tumor-surrounding cells to create an immune-suppressive TME [54,55]. Understanding the mechanisms and the molecules involved in this microenvironment, including immune cells, is essential in controlling the evolution of the tumor and its impact on the outcomes of patients.
3. The Immunosuppressive Properties of the TME
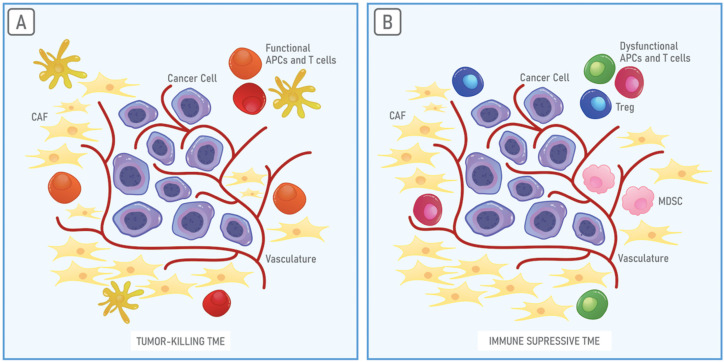
The tumor and the surrounding environment are in a constant relationship in order to establish and maintain the TME. The TME is a dynamic environment that strongly influences cancer cells and is essential for tumor progression, metastasis and resistance to therapies [56,57]. The TME is characterized by metabolic reprogramming, angiogenesis and dysfunction of the immune system that enables the immune escape [58,59,60]. The TME comprises extracellular matrix (ECM) components, signaling molecules, endothelial cells, cancer-associated fibroblasts (CAFs), immune cells and inflammatory cells [61]. Cancer cells control the functions of the cellular and non-cellular components of the TME through the establishment of signaling networks by releasing soluble factors or extracellular vesicles (EVs), or by cell–cell interactions [62,63]. ECM is composed of water and macromolecules, including glycoproteins, collagens and enzymes that, in physiological conditions, guarantee structural and biochemical support. Collagen is the main component of ECM, functioning as a physical barrier to prevent cell migration; thus, it is responsible to maintain the tissue morphology and organization [64,65]. Hence, in the TME, ECM influences cell adhesion, cell proliferation and cell communication [2]. Metalloproteinases released by cancer cells in the TME assist in the degradation of ECM barriers and allow the release of growth factors that can, in this way, act on endothelial cells, stimulating angiogenesis. Angiogenesis is essential to supply cancer cells with nutrients and supports tumor development and progression [66]. The TME is enriched in CAFs that support the migration of cancer cells from the primary tumor into the bloodstream to colonize distal tissue and organs for metastasis establishment [67,68]. Immune cells, in turn, are the second most abundant in the TME and are prevalently represented by granulocytes, lymphocytes and macrophages [69]. Notably, the immune system of the TME has attracted much attention in the last years to better understand one of the most crucial hallmarks of cancer [1]. The TME can either promote tumor killing by the immune system (Figure 1A) or immune evasion and tumor progression. An immune suppressive TME is characterized by the presence of not functional T cells and APCs that lead to a lack of recognition of tumor antigens. In this case, anti-tumor immunity is further hampered by the presence of several immune suppressive cells, such as Tregs and MDSCs [1,70,71,72] (Figure 1B).
Figure 1.
The tumor microenvironment (TME). Cancer cells are surrounded by a complex and heterogeneous environment composed of cancer-associated fibroblasts (CAFs), blood vessel cells and immune system cells, the TME. (A) Whether enriched in functional antigen-presenting cells (APCs) or T cells, the TME can promote the recognition of cancer cells by the immune system. (B) On the contrary, the TME can be enriched in dysfunctional APCs and T cells, myeloid-derived suppressor cells (MDSCs) and Tregs, creating a highly immune suppressive environment that favors tumor growth and progression.
The abundance of tDCs [73,74] and the constant communication between DCs and Tregs are important features of the TME. When contacted by Tregs, DCs suffer changes in their cytoskeleton and enter a lethargic state that impedes T cell priming [75]. Activation of T cells is additionally compromised by the downregulation of co-stimulatory molecules on DCs mediated by Tregs [76]. Moreover, Tregs express the immune checkpoint molecules, CTLA4 and PD-L1, that hamper DCs activity by inhibiting B7. While these molecules are essential to maintain immune response homeostasis, in the cancer context, they prevent the activation of a T-cell mediated anti-cancer immune response [77].
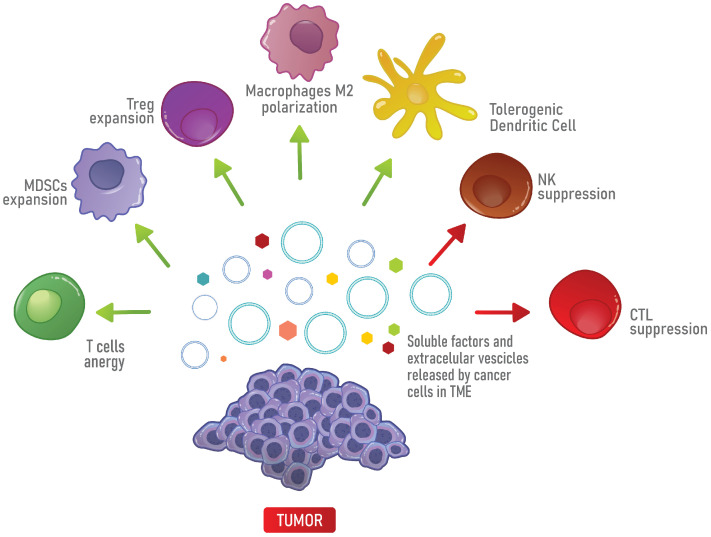
Macrophages also contribute to the immunological status of the TME. Monocytes are recruited to the TME and differentiate into tumor-associated macrophages (TAMs), a particular cell type that expresses TGF-β, iNOS and Arg-1 [31,78] and resembles the M2 phenotype [79,80,81]. Interestingly, by secreting TGF-β, TAMs can impair NK cell functions [78]. Moreover, through the secretion of IL-6, TGF-β cancer cells promote the accumulation of MDSCs [82,83], that, in turn, promote the expansion of Tregs [84]. MDSCs also upregulate iNOS and Arg-1 and, in this way, suppress T cell-mediated anti-tumor immunity [73]. Finally, the TME is also characterized by a deficiency in the activity of NK cells and by the recruitment of TH17 that, in turn, attract MDSCs through the production of IL-17 [85]. In addition, TGF-β present in the TME can induce TH17 to differentiate into Tregs [22,86,87] (Figure 2).
Figure 2.
Immune suppression in the TME. In the TME, soluble factors and extracellular vesicles (EVs) released by cancer cells promote the differentiation into immune suppressive cells, such as Tregs, MDSCs, M2 macrophages and tolerogenic DCs, which in turn, inhibit the anti-tumor immune response mediated by T cells, CTLs and NK cells.
In summary, the TME is a complex and specialized environment that is finely tuned by cancer cells and has a great impact on patients’ prognoses. A highly immune suppressive TME is characterized by the presence of tDCs, M2 macrophages, MDSCs and Tregs that avoid the mounting of a proper anti-tumor T cell response. However, other molecules are actively involved, in an intricate pro-tumor signaling network. A protein that has attracted much attention, for its immunomodulatory functions in cancer, is the phospholipid and calcium-binding protein, Annexin A1 [88]. Different studies have been dedicated to discovering its intricate functioning to better establish phenotypic patterns and assist in the design of new therapeutic strategies.
4. Structure and Functions of Annexin A1
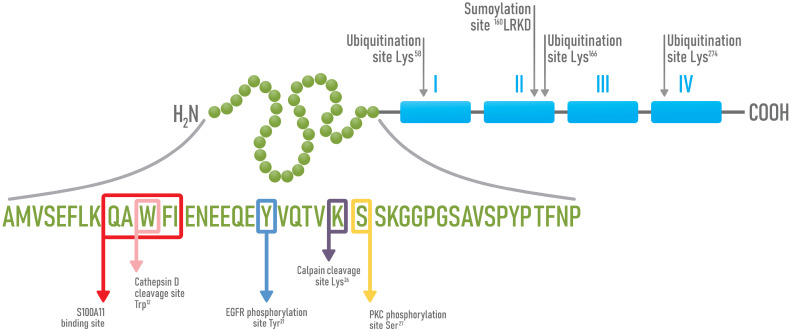
Discovered in the 1980s, Annexin A1 (AnxA1) is a member of the Annexins superfamily, a group of proteins that share high homology and are characterized by the ability of binding phospholipids in a calcium-dependent manner [89,90,91,92]. AnxA1 is an anti-inflammatory protein that acts on innate immune cell response and is one of the downstream mediators of glucocorticoids [93,94,95]. Besides being highly expressed in neutrophils, monocytes and macrophages [96], AnxA1 is also expressed in several tissues and organs, including the heart, liver, spleen, colon, pancreas, brain, adipose tissue, prostatic tissue and arteries [97,98]. AnxA1 is composed of 346 amino acids (aa) and displays a molecular weight of 37 kDa [99,100]. Structurally, it is composed of a C-terminal portion (from Pro44 to Gly344) and an N-terminal region (from Ala2 to Asp43) that is specific to AnxA1 [101]. The C-terminal portion is highly conserved among Annexins and contains four domains of approximately 70 aa in length each, which are rearranged in 5 helixes responsible for the binding to calcium. These four domains are organized in a compact configuration that is maintained stable by hydrophobic interactions with resistance to proteolysis [102,103,104,105] (Figure 3). Domains 2 and 3 guarantee the binding to calcium and, in this way, mediate the association to membrane phospholipids, while the N-terminal region stays away from the membrane and is susceptible to specific interactions with cellular components [106,107]. On the contrary, the N-terminal region is extremely variable in length and sequence and confers biological specific activities to the different members of the family [108,109]. A crystallographic analysis showed that the N-terminal domain organizes in two alpha helixes (from Ala2 to Asn16 and from Glu18 to Lys26) that spatially arrange with a 60° inclination [81]. In the absence of Ca2+ ions, the N-terminal domain stays close to domain 3, while, in the presence of Ca2+ ions, AnxA1 suffers a conformational change that enables its binding to phospholipids through the C-terminal region and the exposition of the N-terminal domain [101,102,104]. This conformational change allows the amphipathic helix of the N-terminal domain to interact with a second phospholipid site that promotes membrane aggregation or allows the interaction with cellular mediators [101].
Figure 3.
Schematic representation of AnxA1 structure and its sites of post-translational modifications. AnxA1 is composed of an N-terminal peptide (green) and a C-terminal region, composed of four repetitive domains of about 70 aa each (blue). In the N-terminal domain, AnxA1 display sites for EGFR (Y, Tyr21) and PKC dependent phosphorylation (S, Ser27), sites for Cathepsin D (W, Trp12) and Calpain I dependent cleavages (K, Lys26) and a peptide motif (QAWFI), responsible for the binding to S100A11. In the C-terminal portion, three sites of ubiquitination (Lys58, Lys166 and Lys276) and a site of sumoylation (160 LRKD) are present.
About the cellular localization, previous studies described AnxA1 expression in the nucleus, cytoplasm and cell membrane [110,111,112,113], which justifies its participation in different processes, such as proliferation, apoptosis, survival, differentiation and migration [109,114]. Regarding the nuclear localization, AnxA1 displays DNA and/or RNA binding sequences and structural motifs and can bind either to double-stranded or single-stranded DNA, in an Mg2+ and Ca2+ dependent manner, respectively. Furthermore, the helicase activity of AnxA1 has been reported [105,115,116]. In the presence of ATP and Mg2+, nuclear AnxA1 binds to DNA and unwinds the double-strand by hydrolysis of ATP. In the presence of Ca2+ ions, nuclear AnxA1 binds to two single-stranded DNA molecules, mediating their annealing [115].
Cytoplasmic AnxA1 is distributed throughout the entire intracellular environment, including the inner face of the plasma membrane, linked to vesicular structures, such as early and multivesicular endosomes, phagosomes and, under certain circumstances, to the endoplasmic reticulum [113,117]. In the cytoplasm, by inhibiting the phospholipase A2 (PLA2), AnxA1 impedes the release of arachidonic acid and its pro-inflammatory metabolites derivatives, such as thromboxane A2 and prostaglandins E2, I2, D2 and F2α [92,118,119,120,121,122]. By acting on this lipid metabolism pathway, AnxA1 regulates tissue repair and controls the migration of leukocytes through the endothelium [89,123,124]. Furthermore, the action of AnxA1 in decreasing iNOS levels and in inhibiting the synthesis of prostaglandins, by blocking the expression of cyclooxygenase-2 (COX2), has been demonstrated in macrophages [89,125]. To inhibit PLA2, AnxA1 needs to interact with a member of the S100 protein family, S100A11, which is a Ca2+ binding protein [126]. The biological functions of this family of proteins are related to the processes of endocytosis, exocytosis, inflammation, cell growth, apoptosis and enzymatic activity regulation [127]. Activation of S100A11, through binding to the Ca2+ ion, promotes the recognition of different biological targets, among them, the N-terminal domain of AnxA1 [126,128,129].
AnxA1 can also be cleaved at the N-terminal domain by elastases [117], metalloproteases [130,131], proteinase 3 [132], by the cysteine protease, Calpain I [133], or by the aspartyl protease Cathepsin D [126,134]. Calpain I cleaves AnxA1 at Lys26, generating a C-terminal fragment that displays pro-inflammatory effects through the activation of the ERK1/2 pathway in endothelial cells and the accumulation of the intracellular adhesion molecule 1 (ICAM1). ICAM1 expression leads to the immobilization of neutrophils on endothelial cells and, in this way, increases the transendothelial migration capacity of neutrophils [135]. Furthermore, the cleavage at Trp12 by Cathepsin D also contributes to inflammation, since the fragment of AnxA1 generated has no PLA2 inhibitory activity [126]. AnxA1 is also translocated to the cell membrane and externalized or secreted into the extracellular fluid to exert its anti-inflammatory properties [136]. The process of externalization of AnxA1 occurs by three basic mechanisms: (i) through ATP A1 binding cassette transport system (ABCA1), (ii) through phosphorylation of AnxA1 at the Ser27 residue and (iii) through the release of polymorphonucleate gelatinase granules during the degranulation process [93,98,137]. Several groups reported that ABCA1 is a mediator of AnxA1 externalization in cytoplasmic lipid structures, such as microvesicles (MVs). Moreover, ABCA1 also contributes to AnxA1 externalization through lipidation and phosphorylation at Ser27 [98,138,139,140]. In pituitary cell lines, this type of phosphorylation is induced by protein kinase C (PKC) and promotes AnxA1 translocation to the cell surface. However, in order to traffic across the cell membrane, AnxA1 needs to be modified by myristoylation [136]. In fact, AnxA1 contains in its aa sequence potential myristoylation sites localized within the following peptides: Gly30–Ala35, Gly59–Ile65, Gly215–Asn222 and Gly320–Gln325 [136]. Finally, AnxA1 externalization can take place through degranulation, a process that occurs along with chemotaxis and adhesion of polymorphonucleate cells to the endothelial cell monolayer [100,141,142]. Since AnxA1 activation occurs in a calcium-dependent manner, all the processes mentioned above are regulated by the concentrations of Ca2+ ions [101].
Once externalized, AnxA1 can interact with formylated peptide receptors (FPR1, 2 and 3) that belong to the G protein-coupled receptors family [143,144]. The main receptor responsible for the anti-inflammatory effects of AnxA1 is FPR2, which is expressed in several cell types, including endothelial cells and stromal cells, being more abundantly expressed in leukocytes [145]. Once activated by AnxA1, FPR2 elicits signaling pathways that inhibit leukocytes migration and adhesion, thus leading to the resolution of inflammation [127,145,146]. FPR2 interacts with a variety of ligands, including the N-terminal domain of AnxA1 [147,148]. It is noteworthy that recent studies have shown that FPR2 can be found as a monomer or homo/heterodimer (associated with FPR1 or FPR3). In this context, according to the FPR complex formed, FPR2 ligands can activate multiple pathways, which partially explains the multiple functions exerted by AnxA1 [148,149]. FPR1 was also originally identified for its ability to recognize the N-formylated peptides of bacterial origin and, in this way, to activate phagocytic leukocytes chemotaxis towards the site of infection. This receptor is mainly expressed on leukocytes, such as neutrophils, monocytes/macrophages, NKs and DCs, and has specific endogenous agonists, such as AnxA1 [144,150,151,152,153,154].
AnxA1 displays anti-inflammatory activities by activating apoptosis of neutrophils. Indeed, AnxA1 activates apoptosis by increasing the cytosolic calcium flux that leads to dephosphorylation of the death promoter associated with Bcl-2 (Bad) [137]. Furthermore, apoptotic neutrophils release AnxA1 in order to stimulate their phagocytosis through the recruitment of monocytes. Such a process avoids inflammation, thus ensuring the integrity of the adjacent healthy tissue [155]. AnxA1 also acts in resolving inflammation by decreasing the expression of the intracellular adhesion molecule (ICAM) and of the vascular cell adhesion molecule 1 (VCAM1) that results in the detachment of leukocytes from the endothelium and migration inhibition [156]. Finally, AnxA1 is associated with the process of differentiation of bone and muscle tissue and with the activation and differentiation of T cells into T helper cells [157,158]. Indeed, in T cells, the activation of FPR1 by AnxA1 activates ERK and Akt and increases the TCR signaling pathway. Therefore, the activation of downstream transcription factors, such as the nuclear factor of activated T-cells (NFAT), NF-κB and the activating protein-1 (AP-1), is enhanced [159].
Notably, AnxA1 integrates several signaling pathways that are involved in health and disease. AnxA1 exerts important anti-inflammatory and pro-resolution properties by eliciting signaling pathways through FPRs that inhibit adhesion and migration of leukocytes and by directly inhibiting PLA2. However, AnxA1 can also be pro-inflammatory, when cleaved by proteases. Due to its pleiotropic behavior, its role in cancer has been extensively studied in the last years and its expression has been frequently correlated with cancer aggressiveness and resistance to therapies [160,161].
4.1. AnxA1 in Cancer
Besides AnxA1 being widely described for its anti-inflammatory activities, its role in cancer development and progression stands out [105]. In this context, it has been suggested that AnxA1 plays a role in malignant transformation, activation of oncogenes, inactivation of tumor suppressor genes, induction of proliferation and cellular invasion [162,163,164,165]. However, AnxA1 can act either as an anti-tumor or as a pro-tumoral factor, depending on the tumor origin and stage [166]. High AnxA1 expression levels have been found in breast cancer [167,168], melanomas [169], hepatocellular carcinomas [170], colorectal cancers [171], gliomas [172], lung adenocarcinomas [173,174] and prostate cancer [175], correlating with worse prognosis, lower disease-free survival rates and lower overall survival [170,174,176]. On the contrary, low expression levels of AnxA1 have been observed in squamous head and neck cancer [177] and thyroid cancer [178] and associate with a worse prognosis, poor differentiation, lower overall survival and higher relapse rates [177,178,179].
Cao and collaborators showed that, despite that breast cancers frequently display downregulation of AnxA1, this protein is upregulated in the triple-negative subtype [180]. Furthermore, AnxA1 has been associated with poorly differentiated breast cancers [167], correlating with lower survival rates [181]. In line with these findings, our group has previously demonstrated that AnxA1 is overexpressed in the triple-negative subtype and lymph node metastasis, when compared to the corresponding primary tumors [168]. Moreover, De Graauw and collaborators demonstrated the crucial role of AnxA1 in supporting the epithelial–mesenchymal transition (EMT) event, promoting migration, invasion and metastasis formation in breast cancer. By using the triple-negative cell line, MDA-MB-231, the authors showed that AnxA1 is essential for the TGF-β signaling, resulting in increased phosphorylation of the small mothers against decapentaplegic homolog 2 (Smad2) and EMT activation [182]. Another study also showed that AnxA1 displays pro-angiogenic functions in breast cancer by supporting the activation of the nuclear factor-kappa B (NF-kB) transcriptional factor [183].
In gastric cancer, AnxA1 up-regulation correlates with advanced stages of the disease and peritoneal dissemination [184], while, in nasopharyngeal cancer, AnxA1 has also been described for promoting migration, invasion and metastasis formation, by mediating autophagy suppression [185]. In lung cancer, a high expression of AnxA1 correlated with the proliferation, invasion, migration and appearance of bone metastasis [157,186].
AnxA1 also exerts important pro-tumoral activities by triggering an FPR1-dependent signaling pathway. In glioblastoma multiforme cells, several studies demonstrated that FPR1 activation mediates tumor cells’ chemotaxis, invasion, proliferation and angiogenesis [187,188,189,190,191]. Huang’s and Zhou’s groups showed that AnxA1 or other ligands released by glioblastoma multiforme necrotic cells would mediate FPR1 activation [189,192]. Beside this, Huang and collaborators also described that FPR1 signaling pathway is responsible for the transactivation of the epidermal growth factor receptor (EGFR) that would result in cancer progression [191]. In colon cancer and hepatocellular carcinoma cells, FPR1 elicits signaling pathways related to chronic inflammation that activate ERK, MAPK and the transcriptional factors, NF-kB and the signal transducer and activator of transcription 3 (STAT3) [158,193,194,195,196]. FPR1 expression was also reported in breast cancer [197,198] and it can be activated, in an autocrine manner, by the N-terminal peptide of AnxA1, which is secreted by the triple-negative breast cancer cell line, MDA-MB-231. In these cells, AnxA1/FPR1 autocrine signaling promotes proliferation, migration, invasion and metastatic potential [168]. Nevertheless, it is worth noting that different studies suggest that the role played by FPR1 in carcinogenesis is context-specific. In gastric cancer, FPR1 overexpression was associated with disease progression, as well as lower survival rates [199]. However, other results pointed to FPR1 as a tumor suppressor in this same cancer type [200]. Since the role of FPR1 in carcinogenesis is not fully elucidated, it is crucial to carry on new research in order to elucidate its contribution in different tumors.
In addition to AnxA1 expression and signaling pathways, its cellular localization has been demonstrated to be relevant in the cancer context. Indeed, nuclear AnxA1 has been suggested as a negative prognostic factor of oral squamous cell carcinoma and esophageal squamous cell carcinoma, being associated with lower overall survival [112,201]. In gastric cancer, the nuclear expression of AnxA1 is associated with advanced stages of the disease and with peritoneal dissemination [202]. The involvement of nuclear AnxA1 in tumorigenesis seems to be mediated by a monoubiquitinated form of AnxA1 that is able to introduce DNA mutations [105,203,204,205]. In this sense, insertional mutations can be catalyzed by error-prone DNA polymerases, which are recruited by ubiquitinated nuclear proteins [204,206]. Upon treating cells with mutagenic agents, it was possible to observe an increase in the translocation of cytoplasmic AnxA1 to nuclei, which is likely occurring in response to DNA damage [207]. Another study also demonstrated that upon treatment with mutagenic agents, monoubiquitinated AnxA1 increased in nuclei, indicating the relevance of this type of post-translational modifications during DNA damage response [208].
One of the main causes of cancer lethality relies on the capacity of cancer cells to develop multiple drug resistance [209]. In this context, some studies are indicating the role of AnxA1 in inducing resistance of cancer cells toward chemotherapies. The upregulation of AnxA1 has been correlated with the resistance to adriamycin, melphalan and etoposide. In order to confirm this finding, the authors induced the expression of AnxA1 in an AnxA1-negative breast cancer cell line, MCF-7 and showed that such expression results in resistance to several chemotherapeutic agents. In this same study, the inhibition of AnxA1 expression in an ovarian cancer cell line, SKOV-3, led to increased sensitivity to anti-tumoral drugs [161]. On the other side, in chronic myeloid leukemia, resistance toward chemotherapeutic agents has been associated with a lower expression of AnxA1. Indeed, by suppressing AnxA1 expression in K562 cells, the authors showed that the resistance to anti-tumoral drugs was significantly increased [210].
Worthy of mention, AnxA1 can be differentially phosphorylated in different tumors by EGFR or by the hepatocyte growth factor receptor (HGFR) [211,212,213,214]. Intriguingly, the phosphorylation mediated by EGFR has been described for inducing AnxA1 cleavage, keeping PLA2 active in squamous carcinomas [126]. Hence, the differential phosphorylation and the possible subsequent cleavage could explain the effect of AnxA1 on the growth, proliferation, metastasis formation and drug resistance of different tumors and stages of progression [211].
Collectively, the information presented in this section emphasizes the essential role of AnxA1 and its signaling pathway through FPRs in the aggressiveness of several cancers. Indeed, its role in tumor growth, angiogenesis, DNA damage response and migration and invasion of cancer cells have been reported. Besides its anti-inflammatory effect, AnxA1 is profoundly involved in the modulation of the immune system and in the promotion of immune suppression, either in physiological or pathological conditions [148]. Indeed, recently, its role in cancer immune escape has been described [215].
4.2. Immunosuppressive Functions of AnxA1 in Physiological and Cancer Contexts
In physiological conditions, it has been shown that AnxA1 promotes immune suppression and resolves the inflammatory process. In this context, AnxA1 enhances the differentiation into M2 macrophages and supports the expression of IL-10 by these cells [216]. When liver cells extracted from mice were treated with exogenous AnxA1, the macrophage M1 phenotype was abolished and an increase in IL-10 expression was observed [217]. Accordingly, other studies demonstrated that treatment of macrophages with a recombinant AnxA1 led to inhibition of iNOS expression, which is accompanied by increased IL-10 levels and decreased IL-12 mRNA levels [218]. The increase in IL-10 expression seems to be due to the FPRs downstream signaling activation of ERK mediated by AnxA1 [192] and may be responsible for the decreased expression of IL-12 in macrophages [218]. Moreover, it has been demonstrated that the tolerogenic nature of cells undergoing apoptosis depends on AnxA1 translocation on the cell surface of these cells. Weyd and collaborators co-cultured apoptotic primary human thymocyte, T cell and neutrophils with DC cells. They showed that AnxA1 expressed on the cell surface of apoptotic cells prevented the activation of toll-like receptors (TLRs) expressed on DCs. The resulting DCs displayed a tolerogenic phenotype that, when it came in contact with CTLs, inhibited their activation, producing IFN-γ and TNF-α [219]. On the other hand, it has been reported that the action of AnxA1 on T cells can vary, according to the environmental conditions and to the state of T cell activation. Gold and others pointed that exogenous AnxA1 can suppress T cell proliferation and limits T cell response [220], but when T cells are stimulated with CD3 and CD28, AnxA1 leads to proliferation and activation of T cells and prolonged activation of Akt, ERK, AP1, NFAT and NF-kB [221]. Furthermore, in activated T cells, the absence of AnxA1 reduces the activation of the TCR downstream signaling pathway [222] and promotes the differentiation into TH2 cells, while inhibiting TH1 response [221]. In another study, Kamal and collaborators described that the mimetic peptide of the N-terminal domain of AnxA1 (Acetylated-AMVSEFLKQACYIEKQEQEYVQAVK; Ac2-26) inhibits the proliferation and cytokine production of both TH1 and TH2 [223].
The immune-suppressive activities of AnxA1 can also depend on its presence in EVs. Indeed, AnxA1 can either be secreted or released from the cell within MVs [224]. It is well known that EVs contain cargo molecules such as lipids, proteins and nucleic acids and promote intercellular communication either by binding to the cell surface or by fusing with a specific cellular type [225,226]. Indeed, MVs containing AnxA1 of both normal and cancer cells can alter immune cells’ phenotype [227]. Previously, it was demonstrated that neutrophils produce MVs that, at least in part, due to their AnxA1 content, are capable of stimulating TGF-β expression [228,229]. In agreement with this study, another work demonstrated the immunosuppressive function of neutrophils MVs enriched in AnxA1 and TGF-β. Moreover, these MVs interact with NK cells, decreasing the expression of IFN-γ and TNF-α [230], and with macrophages, increasing TGF-β expression [231].
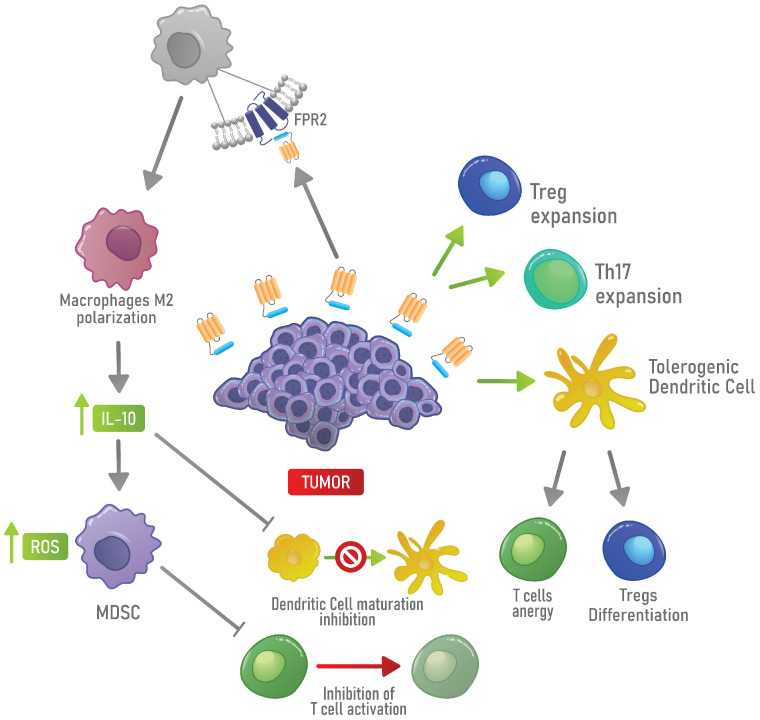
In the tumor landscape, one of the first indications that AnxA1 could promote immune escape came from experiments in which AnxA1 was knocked down in a glioblastoma multiforme animal model and caused decreased tumor growth and myeloid infiltration. In this work, the authors suggested that AnxA1 acts in highly malignant and actively growing glioblastomas as a chemoattractant for tumor-promoting myeloid cells, especially granulocytes and macrophages [232]. Link and collaborators also described the activity of AnxA1-coated particles in inducing antigen-specific immunosuppression. Indeed, DCs treated with AnxA1-coated particles displayed a tolerogenic phenotype that, in co-culture experiments, promotes an anergic phenotype in T cells, inducing a decrease in proliferation and cytokine secretion [233]. Moraes and collaborators demonstrated, in breast cancer, that, in the absence of AnxA1, macrophages were less sensitive to the polarization toward an M2 phenotype induced by IL-4. Moreover, they showed that macrophages treated with the N-terminal peptide of AnxA1 increased the expression of Arg-1, while they decreased the expression of IL-12 [188]. The decrease in IL-12 correlates with cancer progression and metastasis and is probably dependent on the upregulation of IL-10 induced by AnxA1 [215,216,217,218,234]. The role of AnxA1 in polarizing macrophages towards the M2 phenotype in hepatocellular carcinoma has also been described. In this type of cancer, the N-terminal peptide of AnxA1 induces a signaling cascade through FPR2 that activates ERK, Akt and NF-kB. Accordingly, a deficiency in FPR2 has been related to a sustained polarization toward an M1 phenotype in hepatocellular carcinoma [216]. Moreover, the role of AnxA1 in inducing TH2 cells infiltration in pancreatic cancer [235] and in inducing the differentiation and expansion of Tregs in the TME of triple-negative breast cancer models has also been described [100]. Bai and collaborators showed that the proliferation of effector T cells, when treated with Ac2-26, was lower and that the function of Tregs was impaired when these cells were treated with the FPR inhibitor Boc1. Boc1 decreased the expression of markers of Tregs, including Granzyme A, IL-2 receptor (CD25) and CCR8. The authors concluded that the AnxA1 signaling regulates the function of Tregs [100]; hence, this could be an ideal target for innovative therapies against breast cancer. A summary of these finding is provided in Figure 4.
Figure 4.
Mechanism of immune escape induced by AnxA1 in the TME. AnxA1 expressed by cancer cells promotes the expansion of Tregs, tDCs and TH17. Moreover, AnxA1 can activate FPR2 on the cell surface of macrophages, supporting the polarization toward an M2 phenotype. In turn, M2 macrophages induce MDSC activity and inhibit the maturation of DCs by producing IL-10.
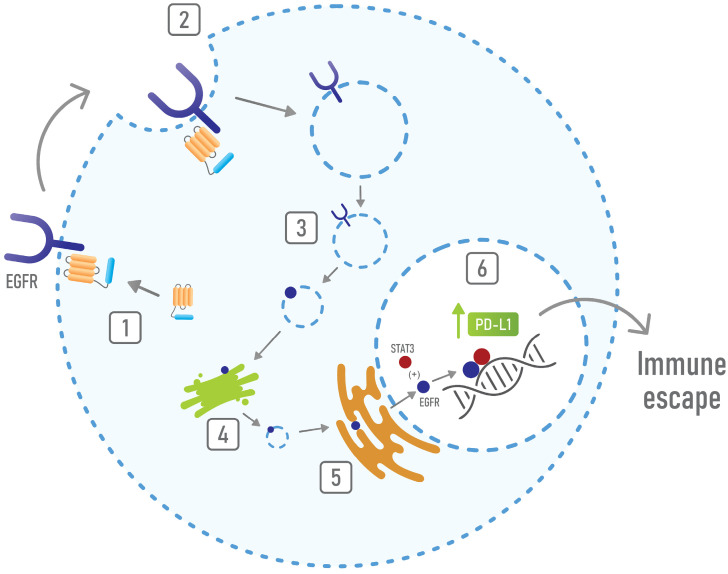
Finally, the activity of AnxA1 in promoting immune suppression in the TME could be related to its interaction with the EGFR [236]. Existing evidence showed that EGFR activation upregulates PD-L1 in lung cancer [237,238], that, in turn, induces the apoptosis of T cells [239]. Confirming this finding, another work showed that the increased expression of PD-L1 is activated by the EGFR through its interaction with STAT3 in nuclei [240]. Moreover, another work described that the EGFR/STAT3 interaction in nuclei is responsible for the expression of iNOS, whose levels correlate with poor overall survival [241]. The role of iNOS expression in cancer cells had been already associated with reduced tumor-infiltrating lymphocytes and with the suppression of anti-tumor immune response [242]. Hence, current evidence suggests that the EGFR/STAT3 interaction induces immune suppression by regulating either PD-L1 or iNOS expression. Indeed, it has been shown that EGFR at the nuclear level functions as a co-transcriptional factor that favors disease progression and resistance to therapies [243]. In the cancer context, it has been shown that AnxA1 promotes the stabilization and the constitutive activation of EGFR [105], as well as the nuclear localization of this receptor [175]. Furthermore, reports showed that, in head and neck cancers, AnxA1 regulates the formation of exosomes and the release of EGFR in these EVs [236,244]. Interestingly, Huang and collaborators demonstrated that, in lung cancer, EGFR-enriched exosomes induce tDCs; tDCs, in turn, induce tumor specific Tregs, which inhibit the specific anti-tumor CTL response. They showed that exosomes containing EGFR are formed thanks to the activity of AnxA1, inducing tumor specific Tregs [236,244]. Based on this, the AnxA1/EGFR interaction seems to play a relevant role in immune suppression in the cancer context. In addition, it has been described that AnxA1 induces STAT3 activation in cancer [245]. Hence, the immune-suppressive properties of AnxA1 also rely on its activities in supporting EGFR signaling and nuclear localization and in promoting STAT3 activation. In this scenario, by inducing the nuclear localization of EGFR, AnxA1 can promote the interaction of this receptor with STAT3 and, subsequently, can induce immune suppression (Figure 5).
Figure 5.
Mechanisms of immune escape mediated by the AnxA1/EGFR interaction. AnxA1 interacts with EGFR (1) and promotes its internalization (2 and 3) and its retrograde transport to nuclei (4 and 5). Once in nuclei, EGFR interacts with STAT3 and induces the expression of PD-L1 (6), thus resulting in immune suppression.
Taken together, these findings point towards an important role of AnxA1 in the induction of immune suppression in the cancer context. Therefore, it is possible to draw some future perspectives for cancer treatment that involve the inhibition of AnxA1 signaling. In this scenario, the inhibition of FPRs achieved by Boc1, Boc2, or Cyclosporin H [245] could represent an interesting strategy to induce an anti-tumor immune response. This approach could be used as an isolated therapy, or in association with gold standard immunotherapies, in order to improve the clinical outcome of refractory patients.
5. Concluding Remarks
AnxA1 has attracted much attention due to its pleiotropic functions and its involvement in tumor growth and progression. Indeed, its expression and signaling through FPRs are tightly involved in the aggressive behavior of some types of cancer. Recently, the role of AnxA1 in the TME has also emerged and particular effort has been devoted to the description of its immunomodulatory and immune suppressive properties. In this review, we focused on the immune response regulated by AnxA1, which favors M2 macrophages polarization, by increasing the function and proliferation of MDSCs and Tregs and by promoting the enrichment in tDCs and TH17. Therefore, AnxA1 manipulates the TME. Moreover, it is known that AnxA1 regulates the nuclear localization of EGFR and, as a consequence, it can promote immune evasion by favoring the EGFR/STAT3 transcriptional activities in cancer cells. Through these mechanisms, AnxA1 would significantly promote T cell dysfunction and, as a consequence, would enhance immune evasion and tumor progression.
Unraveling the mechanisms by which cancer cells evade the immune system is crucial for the development of new possible therapeutic approaches. Based on the information presented in this review, it is possible to suggest that the inhibition of the AnxA1/FPRs signaling could represent an important and innovative immunotherapy strategy.
Abbreviations
| ABC A1 | ATP A1 binding cassette transport system |
| Ala | alanine |
| AnxA1 | Annexin A1 |
| APC | antigen-presenting cell |
| Asn | asparagine |
| Bad | death promoter associated with Bcl-2 |
| Bcl2 | B cell lymphoma 2 |
| Bregs | regulatory B lymphocytes |
| AP-1 | activating protein-1 |
| APC | antigen presenting cell |
| Arg-1 | arginase-1 |
| CAF | cancer-associated fibroblast |
| CCR8 | C-C motif chemokine receptor 8 |
| CD | cluster of differentiation |
| CTL | cytotoxic T lymphocytes |
| CTLA4 | cytotoxic T-lymphocyte antigen 4 |
| DC | dendritic cell |
| ECM | extracellular matrix |
| EGFR | epidermal growth factor receptor |
| EMT | epithelial–mesenchymal transition |
| ERK | extracellular signal-regulated kinases |
| EV | extracellular vesicle |
| FOXP3 | factor forkhead box P3 |
| FPR | formylated peptide receptor |
| Gly | glycine |
| HGFR | hepatocyte growth factor receptor |
| ICAM | intracellular adhesion molecule |
| iDC | immature DC |
| IFN-γ | interferon-gamma |
| IL | interleukin Ile, isoleucine |
| iNOS | inducible nitric oxide synthase |
| Lys | lysine |
| MDSC | myeloid-derived suppressor cells |
| MHC | major histocompatibility complex |
| MV | microvesicle |
| NFAT | nuclear factor of activated T-cells |
| NF-kB | nuclear factor kappa B |
| NK | natural killer cell |
| NO | nitric oxide |
| PD-L1 | programmed death-ligand 1 |
| PLA2 | phospholipase A2 |
| ROS | reactive oxygen species |
| Ser | serine |
| Smad2 | small mothers against decapentaplegic homolog 2 |
| STAT3 | signal transducer and activator of transcription 3 |
| TAM | tumor-associated macrophages |
| TCR | T cell receptor |
| tDC | tolerogenic DC |
| TGF-β | transforming growth factor-β |
| TH | T helper cell |
| TME | tumor microenvironment |
| TNF-α | tumor necrosis factor α |
| Treg | regulatory T cell |
| Trp | tryptophane |
| VCAM 1 | vascular cell adhesion molecule 1 |
| VEGF | vascular endothelial growth factor |
Author Contributions
L.V., conceptualization, writing and revision of the manuscript; T.G.A., H.S.V.F., S.T.S.M., M.A.R. and L.R.G., writing and revision of the manuscript, designing of figures. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the following institutions: FAPEMIG, CNPq and CAPES (23038007281201161).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Brassart-Pasco S., Brezillon S., Brassart B., Ramont L., Oudart J.B., Monboisse J.C. Tumor Microenvironment: Extracellular Matrix Alterations Influence Tumor Progression. Front. Oncol. 2020;10:397. doi: 10.3389/fonc.2020.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaffer C.L., Weinberg R.A. A perspective on cancer cell metastasis. Science. 2011;331:1559–1564. doi: 10.1126/science.1203543. [DOI] [PubMed] [Google Scholar]
- 4.Blankenstein T., Coulie P.G., Gilboa E., Jaffee E.M. The determinants of tumour immunogenicity. Nat. Rev. Cancer. 2012;12:307–313. doi: 10.1038/nrc3246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pradeu T., Carosella E.D. On the definition of a criterion of immunogenicity. Proc. Natl. Acad. Sci. USA. 2006;103:17858–17861. doi: 10.1073/pnas.0608683103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kitamura T., Qian B.Z., Pollard J.W. Immune cell promotion of metastasis. Nat. Rev. Immunol. 2015;15:73–86. doi: 10.1038/nri3789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crusz S.M., Balkwill F.R. Inflammation and cancer: Advances and new agents. Nat. Rev. Clin. Oncol. 2015;12:584–596. doi: 10.1038/nrclinonc.2015.105. [DOI] [PubMed] [Google Scholar]
- 8.Colotta F., Allavena P., Sica A., Garlanda C., Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: Links to genetic instability. Carcinogenesis. 2009;30:1073–1081. doi: 10.1093/carcin/bgp127. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez H., Hagerling C., Werb Z. Roles of the immune system in cancer: From tumor initiation to metastatic progression. Genes Dev. 2018;32:1267–1284. doi: 10.1101/gad.314617.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim R., Emi M., Tanabe K. Cancer cell immune escape and tumor progression by exploitation of anti-inflammatory and pro-inflammatory responses. Cancer Biol. Ther. 2005;4:924–933. doi: 10.4161/cbt.4.9.2101. [DOI] [PubMed] [Google Scholar]
- 11.Gaudino S.J., Kumar P. Cross-Talk Between Antigen Presenting Cells and T Cells Impacts Intestinal Homeostasis, Bacterial Infections, and Tumorigenesis. Front. Immunol. 2019;10:360. doi: 10.3389/fimmu.2019.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waldman A.D., Fritz J.M., Lenardo M.J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuzaki J., Tsuji T., Luescher I., Old L.J., Shrikant P., Gnjatic S., Odunsi K. Nonclassical antigen-processing pathways are required for MHC class II-restricted direct tumor recognition by NY-ESO-1-specific CD4(+) T cells. Cancer Immunol. Res. 2014;2:341–350. doi: 10.1158/2326-6066.CIR-13-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knutson K.L., Disis M.L., Salazar L.G. CD4 regulatory T cells in human cancer pathogenesis. Cancer Immunol. Immunother. 2007;56:271–285. doi: 10.1007/s00262-006-0194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dardalhon V., Korn T., Kuchroo V.K., Anderson A.C. Role of Th1 and Th17 cells in organ-specific autoimmunity. J. Autoimmun. 2008;31:252–256. doi: 10.1016/j.jaut.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bretscher P. On Analyzing How the Th1/Th2 Phenotype of an Immune Response Is Determined: Classical Observations Must Not Be Ignored. Front. Immunol. 2019;10:1234. doi: 10.3389/fimmu.2019.01234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Emens L.A. Breast cancer immunobiology driving immunotherapy: Vaccines and immune checkpoint blockade. Expert Rev. Anticancer Ther. 2012;12:1597–1611. doi: 10.1586/era.12.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burkholder B., Huang R.Y., Burgess R., Luo S., Jones V.S., Zhang W., Lv Z.Q., Gao C.Y., Wang B.L., Zhang Y.M., et al. Tumor-induced perturbations of cytokines and immune cell networks. Biochim. Biophys. Acta. 2014;1845:182–201. doi: 10.1016/j.bbcan.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Zambrano-Zaragoza J.F., Romo-Martinez E.J., Duran-Avelar Mde J., Garcia-Magallanes N., Vibanco-Perez N. Th17 cells in autoimmune and infectious diseases. Int. J. Inflam. 2014;2014:651503. doi: 10.1155/2014/651503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kryczek I., Wei S., Szeliga W., Vatan L., Zou W. Endogenous IL-17 contributes to reduced tumor growth and metastasis. Blood. 2009;114:357–359. doi: 10.1182/blood-2008-09-177360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zou W., Restifo N.P. T(H)17 cells in tumour immunity and immunotherapy. Nat. Rev. Immunol. 2010;10:248–256. doi: 10.1038/nri2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guery L., Hugues S. Th17 Cell Plasticity and Functions in Cancer Immunity. Biomed. Res. Int. 2015;2015:314620. doi: 10.1155/2015/314620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cvetanovich G.L., Hafler D.A. Human regulatory T cells in autoimmune diseases. Curr. Opin. Immunol. 2010;22:753–760. doi: 10.1016/j.coi.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin-Orozco E., Norte-Munoz M., Martinez-Garcia J. Regulatory T Cells in Allergy and Asthma. Front. Pediatr. 2017;5:117. doi: 10.3389/fped.2017.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu H., Li P., Shao N., Ma J., Ji M., Sun X., Ma D., Ji C. Aberrant expression of Treg-associated cytokine IL-35 along with IL-10 and TGF-beta in acute myeloid leukemia. Oncol. Lett. 2012;3:1119–1123. doi: 10.3892/ol.2012.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohue Y., Nishikawa H. Regulatory T (Treg) cells in cancer: Can Treg cells be a new therapeutic target? Cancer Sci. 2019;110:2080–2089. doi: 10.1111/cas.14069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andersen M.H., Schrama D., Thor Straten P., Becker J.C. Cytotoxic T cells. J. Investig. Dermatol. 2006;126:32–41. doi: 10.1038/sj.jid.5700001. [DOI] [PubMed] [Google Scholar]
- 28.Mills C.D. M1 and M2 Macrophages: Oracles of Health and Disease. Crit. Rev. Immunol. 2012;32:463–488. doi: 10.1615/CritRevImmunol.v32.i6.10. [DOI] [PubMed] [Google Scholar]
- 29.Cai J., Zhang W., Yang P., Wang Y., Li M., Zhang C., Wang Z., Hu H., Liu Y., Li Q., et al. Identification of a 6-cytokine prognostic signature in patients with primary glioblastoma harboring M2 microglia/macrophage phenotype relevance. PLoS ONE. 2015;10:e0126022. doi: 10.1371/journal.pone.0126022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qi L., Yu H., Zhang Y., Zhao D., Lv P., Zhong Y., Xu Y. IL-10 secreted by M2 macrophage promoted tumorigenesis through interaction with JAK2 in glioma. Oncotarget. 2016;7:71673–71685. doi: 10.18632/oncotarget.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arlauckas S.P., Garren S.B., Garris C.S., Kohler R.H., Oh J., Pittet M.J., Weissleder R. Arg1 expression defines immunosuppressive subsets of tumor-associated macrophages. Theranostics. 2018;8:5842–5854. doi: 10.7150/thno.26888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hao N.B., Lu M.H., Fan Y.H., Cao Y.L., Zhang Z.R., Yang S.M. Macrophages in tumor microenvironments and the progression of tumors. Clin. Dev. Immunol. 2012;2012:948098. doi: 10.1155/2012/948098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Solinas G., Germano G., Mantovani A., Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J. Leukoc. Biol. 2009;86:1065–1073. doi: 10.1189/jlb.0609385. [DOI] [PubMed] [Google Scholar]
- 34.Leek R.D., Lewis C.E., Whitehouse R., Greenall M., Clarke J., Harris A.L. Association of macrophage infiltration with angiogenesis and prognosis in invasive breast carcinoma. Cancer Res. 1996;56:4625–4629. [PubMed] [Google Scholar]
- 35.Cruvinel Wde M., Mesquita D., Jr., Araujo J.A., Catelan T.T., de Souza A.W., da Silva N.P., Andrade L.E. Immune system—Part I. Fundamentals of innate immunity with emphasis on molecular and cellular mechanisms of inflammatory response. Rev. Bras. Reumatol. 2010;50:434–461. [PubMed] [Google Scholar]
- 36.Hubo M., Trinschek B., Kryczanowsky F., Tuettenberg A., Steinbrink K., Jonuleit H. Costimulatory molecules on immunogenic versus tolerogenic human dendritic cells. Front. Immunol. 2013;4:82. doi: 10.3389/fimmu.2013.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Domogalla M.P., Rostan P.V., Raker V.K., Steinbrink K. Tolerance through Education: How Tolerogenic Dendritic Cells Shape Immunity. Front. Immunol. 2017;8:1764. doi: 10.3389/fimmu.2017.01764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bharadwaj U., Li M., Chen C., Yao Q. Mesothelin-induced pancreatic cancer cell proliferation involves alteration of cyclin E via activation of signal transducer and activator of transcription protein 3. Mol. Cancer Res. 2008;6:1755–1765. doi: 10.1158/1541-7786.MCR-08-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jarnicki A.G., Lysaght J., Todryk S., Mills K.H. Suppression of antitumor immunity by IL-10 and TGF-beta-producing T cells infiltrating the growing tumor: Influence of tumor environment on the induction of CD4+ and CD8+ regulatory T cells. J. Immunol. 2006;177:896–904. doi: 10.4049/jimmunol.177.2.896. [DOI] [PubMed] [Google Scholar]
- 40.Wiguna A.P., Walden P. Role of IL-10 and TGF-beta in melanoma. Exp. Dermatol. 2015;24:209–214. doi: 10.1111/exd.12629. [DOI] [PubMed] [Google Scholar]
- 41.Bonetti M.I., Pieri L., Domenici L., Urbani S., Romano G., Aldinucci A., Ballerini C., Monici M., Saccardi R., Basile V., et al. Dendritic cells with lymphocyte-stimulating activity differentiate from human CD133 positive precursors. Blood. 2011;117:3983–3995. doi: 10.1182/blood-2010-08-299735. [DOI] [PubMed] [Google Scholar]
- 42.Saibil S.D., Deenick E.K., Ohashi P.S. The sound of silence: Modulating anergy in T lymphocytes. Curr. Opin. Immunol. 2007;19:658–664. doi: 10.1016/j.coi.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 43.Candolfi M., Yagiz K., Foulad D., Alzadeh G.E., Tesarfreund M., Muhammad A.K., Puntel M., Kroeger K.M., Liu C., Lee S., et al. Release of HMGB1 in response to proapoptotic glioma killing strategies: Efficacy and neurotoxicity. Clin. Cancer Res. 2009;15:4401–4414. doi: 10.1158/1078-0432.CCR-09-0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olkhanud P.B., Damdinsuren B., Bodogai M., Gress R.E., Sen R., Wejksza K., Malchinkhuu E., Wersto R.P., Biragyn A. Tumor-evoked regulatory B cells promote breast cancer metastasis by converting resting CD4(+) T cells to T-regulatory cells. Cancer Res. 2011;71:3505–3515. doi: 10.1158/0008-5472.CAN-10-4316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matsushita T. Regulatory and effector B cells: Friends or foes? J. Dermatol. Sci. 2019;93:2–7. doi: 10.1016/j.jdermsci.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 46.Veglia F., Perego M., Gabrilovich D. Myeloid-derived suppressor cells coming of age. Nat. Immunol. 2018;19:108–119. doi: 10.1038/s41590-017-0022-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sendo S., Saegusa J., Morinobu A. Myeloid-derived suppressor cells in non-neoplastic inflamed organs. Inflamm. Regen. 2018;38:19. doi: 10.1186/s41232-018-0076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beury D.W., Carter K.A., Nelson C., Sinha P., Hanson E., Nyandjo M., Fitzgerald P.J., Majeed A., Wali N., Ostrand-Rosenberg S. Myeloid-Derived Suppressor Cell Survival and Function Are Regulated by the Transcription Factor Nrf2. J. Immunol. 2016;196:3470–3478. doi: 10.4049/jimmunol.1501785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anani W., Shurin M.R. Targeting Myeloid-Derived Suppressor Cells in Cancer. In: Kalinski P., editor. Tumor Immune Microenvironment in Cancer Progression and Cancer Therapy. Springer International Publishing; Cham, Switzerland: 2017. pp. 105–128. [DOI] [PubMed] [Google Scholar]
- 50.Purdy A.K., Campbell K.S. Natural killer cells and cancer: Regulation by the killer cell Ig-like receptors (KIR) Cancer Biol. Ther. 2009;8:2211–2220. doi: 10.4161/cbt.8.23.10455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jost S., Altfeld M. Control of human viral infections by natural killer cells. Annu. Rev. Immunol. 2013;31:163–194. doi: 10.1146/annurev-immunol-032712-100001. [DOI] [PubMed] [Google Scholar]
- 52.Vivier E., Raulet D.H., Moretta A., Caligiuri M.A., Zitvogel L., Lanier L.L., Yokoyama W.M., Ugolini S. Innate or adaptive immunity? The example of natural killer cells. Science. 2011;331:44–49. doi: 10.1126/science.1198687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morvan M.G., Lanier L.L. NK cells and cancer: You can teach innate cells new tricks. Nat. Rev. Cancer. 2016;16:7–19. doi: 10.1038/nrc.2015.5. [DOI] [PubMed] [Google Scholar]
- 54.Zhang Z., Liu S., Zhang B., Qiao L., Zhang Y., Zhang Y. T Cell Dysfunction and Exhaustion in Cancer. Front. Cell Dev. Biol. 2020;8:17. doi: 10.3389/fcell.2020.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DeVito N.C., Plebanek M.P., Theivanthiran B., Hanks B.A. Role of Tumor-Mediated Dendritic Cell Tolerization in Immune Evasion. Front. Immunol. 2019;10:2876. doi: 10.3389/fimmu.2019.02876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Correia A.L., Bissell M.J. The tumor microenvironment is a dominant force in multidrug resistance. Drug Resist. Updates. 2012;15:39–49. doi: 10.1016/j.drup.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yuan Y., Jiang Y.C., Sun C.K., Chen Q.M. Role of the tumor microenvironment in tumor progression and the clinical applications (Review) Oncol. Rep. 2016;35:2499–2515. doi: 10.3892/or.2016.4660. [DOI] [PubMed] [Google Scholar]
- 58.Spill F., Reynolds D.S., Kamm R.D., Zaman M.H. Impact of the physical microenvironment on tumor progression and metastasis. Curr. Opin. Biotechnol. 2016;40:41–48. doi: 10.1016/j.copbio.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reina-Campos M., Moscat J., Diaz-Meco M. Metabolism shapes the tumor microenvironment. Curr. Opin. Cell Biol. 2017;48:47–53. doi: 10.1016/j.ceb.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kashyap A.S., Schmittnaegel M., Rigamonti N., Pais-Ferreira D., Mueller P., Buchi M., Ooi C.H., Kreuzaler M., Hirschmann P., Guichard A., et al. Optimized antiangiogenic reprogramming of the tumor microenvironment potentiates CD40 immunotherapy. Proc. Natl. Acad. Sci. USA. 2020;117:541–551. doi: 10.1073/pnas.1902145116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anderson N.M., Simon M.C. The tumor microenvironment. Curr. Biol. 2020;30:R921–R925. doi: 10.1016/j.cub.2020.06.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang M., Zhao J., Zhang L., Wei F., Lian Y., Wu Y., Gong Z., Zhang S., Zhou J., Cao K., et al. Role of tumor microenvironment in tumorigenesis. J. Cancer. 2017;8:761–773. doi: 10.7150/jca.17648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Huang W., Luo S., Burgess R., Yi Y.H., Huang G.F., Huang R.P. New Insights into the Tumor Microenvironment Utilizing Protein Array Technology. Int. J. Mol. Sci. 2018;19:559. doi: 10.3390/ijms19020559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Frantz C., Stewart K.M., Weaver V.M. The extracellular matrix at a glance. J. Cell Sci. 2010;123:4195–4200. doi: 10.1242/jcs.023820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Theocharis A.D., Skandalis S.S., Gialeli C., Karamanos N.K. Extracellular matrix structure. Adv. Drug Deliv. Rev. 2016;97:4–27. doi: 10.1016/j.addr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 66.Deryugina E.I., Quigley J.P. Tumor angiogenesis: MMP-mediated induction of intravasation- and metastasis-sustaining neovasculature. Matrix Biol. 2015;44–46:94–112. doi: 10.1016/j.matbio.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shiga K., Hara M., Nagasaki T., Sato T., Takahashi H., Takeyama H. Cancer-Associated Fibroblasts: Their Characteristics and Their Roles in Tumor Growth. Cancers. 2015;7:2443–2458. doi: 10.3390/cancers7040902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X., Zhang W., Sun X., Lin Y., Chen W. Cancer-associated fibroblasts induce epithelial-mesenchymal transition through secreted cytokines in endometrial cancer cells. Oncol. Lett. 2018;15:5694–5702. doi: 10.3892/ol.2018.8000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lei X., Lei Y., Li J.K., Du W.X., Li R.G., Yang J., Li J., Li F., Tan H.B. Immune cells within the tumor microenvironment: Biological functions and roles in cancer immunotherapy. Cancer Lett. 2020;470:126–133. doi: 10.1016/j.canlet.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 70.Mayer A., Haist M., Loquai C., Grabbe S., Rapp M., Roth W., Vaupel P., Schmidberger H. Role of Hypoxia and the Adenosine System in Immune Evasion and Prognosis of Patients with Brain Metastases of Melanoma: A Multiplex Whole Slide Immunofluorescence Study. Cancers. 2020;12:3753. doi: 10.3390/cancers12123753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nachmany I., Bogoch Y., Friedlander-Malik G., Amar O., Bondar E., Zohar N., Hantisteanu S., Fainaru O., Lubezky N., Klausner J.M., et al. The transcriptional profile of circulating myeloid derived suppressor cells correlates with tumor development and progression in mouse. Genes Immun. 2019;20:589–598. doi: 10.1038/s41435-019-0062-3. [DOI] [PubMed] [Google Scholar]
- 72.Magnuson A.M., Kiner E., Ergun A., Park J.S., Asinovski N., Ortiz-Lopez A., Kilcoyne A., Paoluzzi-Tomada E., Weissleder R., Mathis D., et al. Identification and validation of a tumor-infiltrating Treg transcriptional signature conserved across species and tumor types. Proc. Natl. Acad. Sci. USA. 2018;115:E10672–E10681. doi: 10.1073/pnas.1810580115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gabrilovich D. Mechanisms and functional significance of tumour-induced dendritic-cell defects. Nat. Rev. Immunol. 2004;4:941–952. doi: 10.1038/nri1498. [DOI] [PubMed] [Google Scholar]
- 74.Melief C.J. Cancer immunotherapy by dendritic cells. Immunity. 2008;29:372–383. doi: 10.1016/j.immuni.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 75.Chen J., Ganguly A., Mucsi A.D., Meng J., Yan J., Detampel P., Munro F., Zhang Z., Wu M., Hari A., et al. Strong adhesion by regulatory T cells induces dendritic cell cytoskeletal polarization and contact-dependent lethargy. J. Exp. Med. 2017;214:327–338. doi: 10.1084/jem.20160620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wing K., Onishi Y., Prieto-Martin P., Yamaguchi T., Miyara M., Fehervari Z., Nomura T., Sakaguchi S. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 77.Fife B.T., Bluestone J.A. Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol. Rev. 2008;224:166–182. doi: 10.1111/j.1600-065X.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 78.Peng L.S., Zhang J.Y., Teng Y.S., Zhao Y.L., Wang T.T., Mao F.Y., Lv Y.P., Cheng P., Li W.H., Chen N., et al. Tumor-Associated Monocytes/Macrophages Impair NK-Cell Function via TGFbeta1 in Human Gastric Cancer. Cancer Immunol. Res. 2017;5:248–256. doi: 10.1158/2326-6066.CIR-16-0152. [DOI] [PubMed] [Google Scholar]
- 79.Gordon S., Taylor P.R. Monocyte and macrophage heterogeneity. Nat. Rev. Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 80.Ruffell B., Affara N.I., Coussens L.M. Differential macrophage programming in the tumor microenvironment. Trends Immunol. 2012;33:119–126. doi: 10.1016/j.it.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen J.J., Lin Y.C., Yao P.L., Yuan A., Chen H.Y., Shun C.T., Tsai M.F., Chen C.H., Yang P.C. Tumor-associated macrophages: The double-edged sword in cancer progression. J. Clin. Oncol. 2005;23:953–964. doi: 10.1200/JCO.2005.12.172. [DOI] [PubMed] [Google Scholar]
- 82.Jiang M., Chen J., Zhang W., Zhang R., Ye Y., Liu P., Yu W., Wei F., Ren X., Yu J. Interleukin-6 Trans-Signaling Pathway Promotes Immunosuppressive Myeloid-Derived Suppressor Cells via Suppression of Suppressor of Cytokine Signaling 3 in Breast Cancer. Front. Immunol. 2017;8:1840. doi: 10.3389/fimmu.2017.01840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shvedova A.A., Kisin E.R., Yanamala N., Tkach A.V., Gutkin D.W., Star A., Shurin G.V., Kagan V.E., Shurin M.R. MDSC and TGFbeta Are Required for Facilitation of Tumor Growth in the Lungs of Mice Exposed to Carbon Nanotubes. Cancer Res. 2015;75:1615–1623. doi: 10.1158/0008-5472.CAN-14-2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huang B., Pan P.Y., Li Q., Sato A.I., Levy D.E., Bromberg J., Divino C.M., Chen S.H. Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res. 2006;66:1123–1131. doi: 10.1158/0008-5472.CAN-05-1299. [DOI] [PubMed] [Google Scholar]
- 85.Armstrong D., Chang C.Y., Lazarus D.R., Corry D., Kheradmand F. Lung Cancer Heterogeneity in Modulation of Th17/IL17A Responses. Front. Oncol. 2019;9:1384. doi: 10.3389/fonc.2019.01384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mucida D., Park Y., Kim G., Turovskaya O., Scott I., Kronenberg M., Cheroutre H. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317:256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- 87.Garrido-Mesa N., Algieri F., Rodriguez Nogales A., Galvez J. Functional plasticity of Th17 cells: Implications in gastrointestinal tract function. Int. Rev. Immunol. 2013;32:493–510. doi: 10.3109/08830185.2013.834899. [DOI] [PubMed] [Google Scholar]
- 88.Vecchi L., Araújo T.G., Azevedo F.V.P.D.V., Mota S.T.S., Ávila V.D.M.R., Ribeiro M.A., Goulart L.R. Phospholipase A2 Drives Tumorigenesis and Cancer Aggressiveness through Its Interaction with Annexin A1. Cells. 2021;10:1472. doi: 10.3390/cells10061472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Parente L., Solito E. Annexin 1: More than an anti-phospholipase protein. Inflamm. Res. 2004;53:125–132. doi: 10.1007/s00011-003-1235-z. [DOI] [PubMed] [Google Scholar]
- 90.Gerke V., Creutz C.E., Moss S.E. Annexins: Linking Ca2+ signalling to membrane dynamics. Nat. Rev. Mol. Cell Biol. 2005;6:449–461. doi: 10.1038/nrm1661. [DOI] [PubMed] [Google Scholar]
- 91.Sheikh M.H., Solito E. Annexin A1: Uncovering the Many Talents of an Old Protein. Int. J. Mol. Sci. 2018;19:1045. doi: 10.3390/ijms19041045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pepinsky R.B., Sinclair L.K., Browning J.L., Mattaliano R.J., Smart J.E., Chow E.P., Falbel T., Ribolini A., Garwin J.L., Wallner B.P. Purification and partial sequence analysis of a 37-kDa protein that inhibits phospholipase A2 activity from rat peritoneal exudates. J. Biol. Chem. 1986;261:4239–4246. doi: 10.1016/S0021-9258(17)35653-3. [DOI] [PubMed] [Google Scholar]
- 93.Perretti M., D’Acquisto F. Annexin A1 and glucocorticoids as effectors of the resolution of inflammation. Nat. Rev. Immunol. 2009;9:62–70. doi: 10.1038/nri2470. [DOI] [PubMed] [Google Scholar]
- 94.Arcone R., Arpaia G., Ruoppolo M., Malorni A., Pucci P., Marino G., Ialenti A., Di Rosa M., Ciliberto G. Structural characterization of a biologically active human lipocortin 1 expressed in Escherichia coli. Eur. J. Biochem. 1993;211:347–355. doi: 10.1111/j.1432-1033.1993.tb19904.x. [DOI] [PubMed] [Google Scholar]
- 95.Flower R.J. Eleventh Gaddum memorial lecture. Lipocortin and the mechanism of action of the glucocorticoids. Br. J. Pharmacol. 1988;94:987–1015. doi: 10.1111/j.1476-5381.1988.tb11614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sugimoto M.A., Vago J.P., Teixeira M.M., Sousa L.P. Annexin A1 and the Resolution of Inflammation: Modulation of Neutrophil Recruitment, Apoptosis, and Clearance. J. Immunol. Res. 2016;2016:8239258. doi: 10.1155/2016/8239258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Purvis G.S.D., Solito E., Thiemermann C. Annexin-A1: Therapeutic Potential in Microvascular Disease. Front. Immunol. 2019;10:938. doi: 10.3389/fimmu.2019.00938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shen X., Zhang S., Guo Z., Xing D., Chen W. The crosstalk of ABCA1 and ANXA1: A potential mechanism for protection against atherosclerosis. Mol. Med. 2020;26:84. doi: 10.1186/s10020-020-00213-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hall S.C., Smith D.M., Masiarz F.R., Soo V.W., Tran H.M., Epstein L.B., Burlingame A.L. Mass spectrometric and Edman sequencing of lipocortin I isolated by two-dimensional SDS/PAGE of human melanoma lysates. Proc. Natl. Acad. Sci. USA. 1993;90:1927–1931. doi: 10.1073/pnas.90.5.1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bai F., Zhang P., Fu Y., Chen H., Zhang M., Huang Q., Li D., Li B., Wu K. Targeting ANXA1 abrogates Treg-mediated immune suppression in triple-negative breast cancer. J. Immunother. Cancer. 2020;8:e000169. doi: 10.1136/jitc-2019-000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rosengarth A., Luecke H. A calcium-driven conformational switch of the N-terminal and core domains of Annexin A1. J. Mol. Biol. 2003;326:1317–1325. doi: 10.1016/S0022-2836(03)00027-5. [DOI] [PubMed] [Google Scholar]
- 102.Rosengarth A., Gerke V., Luecke H. X-ray structure of full-length Annexin 1 and implications for membrane aggregation. J. Mol. Biol. 2001;306:489–498. doi: 10.1006/jmbi.2000.4423. [DOI] [PubMed] [Google Scholar]
- 103.Glenney J.R., Jr., Tack B.F. Amino-terminal sequence of p36 and associated p10: Identification of the site of tyrosine phosphorylation and homology with S-100. Proc. Natl. Acad. Sci. USA. 1985;82:7884–7888. doi: 10.1073/pnas.82.23.7884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Donnelly S.R., Moss S.E. Functional analysis of the human Annexin I and VI gene promoters. Pt 3Biochem. J. 1998;332:681–687. doi: 10.1042/bj3320681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Boudhraa Z., Bouchon B., Viallard C., D’Incan M., Degoul F. Annexin A1 localization and its relevance to cancer. Clin. Sci. 2016;130:205–220. doi: 10.1042/CS20150415. [DOI] [PubMed] [Google Scholar]
- 106.Gerke V., Moss S.E. Annexins: From structure to function. Physiol. Rev. 2002;82:331–371. doi: 10.1152/physrev.00030.2001. [DOI] [PubMed] [Google Scholar]
- 107.Moss S.E., Morgan R.O. The annexins. Genome Biol. 2004;5:219. doi: 10.1186/gb-2004-5-4-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Weyd H. More than just innate affairs—On the role of annexins in adaptive immunity. Biol. Chem. 2016;397:1017–1029. doi: 10.1515/hsz-2016-0191. [DOI] [PubMed] [Google Scholar]
- 109.Grewal T., Hoque M., Conway J.R.W., Reverter M., Wahba M., Beevi S.S., Timpson P., Enrich C., Rentero C. Annexin A6-A multifunctional scaffold in cell motility. Cell Adhes. Migr. 2017;11:288–304. doi: 10.1080/19336918.2016.1268318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Boudhraa Z., Merle C., Mazzocut D., Chezal J.M., Chambon C., Miot-Noirault E., Theisen M., Bouchon B., Degoul F. Characterization of pro-invasive mechanisms and N-terminal cleavage of ANXA1 in melanoma. Arch. Dermatol. Res. 2014;306:903–914. doi: 10.1007/s00403-014-1517-z. [DOI] [PubMed] [Google Scholar]
- 111.Gerdes H.H. Membrane traffic in the secretory pathway. Cell. Mol. Life Sci. 2008;65:2779–2780. doi: 10.1007/s00018-008-8348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Han G., Tian Y., Duan B., Sheng H., Gao H., Huang J. Association of nuclear Annexin A1 with prognosis of patients with esophageal squamous cell carcinoma. Int. J. Clin. Exp. Pathol. 2014;7:751–759. [PMC free article] [PubMed] [Google Scholar]
- 113.Futter C.E., White I.J. Annexins and endocytosis. Traffic. 2007;8:951–958. doi: 10.1111/j.1600-0854.2007.00590.x. [DOI] [PubMed] [Google Scholar]
- 114.Lim L.H., Pervaiz S. Annexin 1: The new face of an old molecule. FASEB J. 2007;21:968–975. doi: 10.1096/fj.06-7464rev. [DOI] [PubMed] [Google Scholar]
- 115.Hirata A., Hirata F. DNA chain unwinding and annealing reactions of lipocortin (Annexin) I heterotetramer: Regulation by Ca(2+) and Mg(2+) Biochem. Biophys. Res. Commun. 2002;291:205–209. doi: 10.1006/bbrc.2002.6422. [DOI] [PubMed] [Google Scholar]
- 116.Lin S., Hickey R., Malkas L. The biochemical status of the DNA synthesome can distinguish between permanent and temporary cell growth arrest. Cell Growth Differ. 1997;8:1359–1369. [PubMed] [Google Scholar]
- 117.Rescher U., Zobiack N., Gerke V. Intact Ca(2+)-binding sites are required for targeting of Annexin 1 to endosomal membranes in living HeLa cells. Pt 22J. Cell Sci. 2000;113:3931–3938. doi: 10.1242/jcs.113.22.3931. [DOI] [PubMed] [Google Scholar]
- 118.Sudlow A.W., Carey F., Forder R., Rothwell N.J. The role of lipocortin-1 in dexamethasone-induced suppression of PGE2 and TNF alpha release from human peripheral blood mononuclear cells. Br. J. Pharmacol. 1996;117:1449–1456. doi: 10.1111/j.1476-5381.1996.tb15305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sanches J.M., Branco L.M., Duarte G.H.B., Oliani S.M., Bortoluci K.R., Moreira V., Gil C.D. Annexin A1 Regulates NLRP3 Inflammasome Activation and Modifies Lipid Release Profile in Isolated Peritoneal Macrophages. Cells. 2020;9:926. doi: 10.3390/cells9040926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Seidel S., Neymeyer H., Kahl T., Röschel T., Mutig K., Flower R., Schnermann J., Bachmann S., Paliege A. Annexin A1 modulates macula densa function by inhibiting cyclooxygenase 2. Am. J. Physiol. Renal. Physiol. 2012;303:F845–F854. doi: 10.1152/ajprenal.00704.2011. [DOI] [PubMed] [Google Scholar]
- 121.Flower R.J., Rothwell N.J. Lipocortin-1: Cellular mechanisms and clinical relevance. Trends Pharmacol. Sci. 1994;15:71–76. doi: 10.1016/0165-6147(94)90281-X. [DOI] [PubMed] [Google Scholar]
- 122.Flower R.J., Blackwell G.J. Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Nature. 1979;278:456–459. doi: 10.1038/278456a0. [DOI] [PubMed] [Google Scholar]
- 123.Leoni G., Nusrat A. Annexin A1: Shifting the balance towards resolution and repair. Biol. Chem. 2016;397:971–979. doi: 10.1515/hsz-2016-0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chatterjee B.E., Yona S., Rosignoli G., Young R.E., Nourshargh S., Flower R.J., Perretti M. Annexin 1-deficient neutrophils exhibit enhanced transmigration in vivo and increased responsiveness in vitro. J. Leukoc. Biol. 2005;78:639–646. doi: 10.1189/jlb.0405206. [DOI] [PubMed] [Google Scholar]
- 125.Kiani-Esfahani A., Kazemi Sheykhshabani S., Peymani M., Hashemi M.S., Ghaedi K., Nasr-Esfahani M.H. Overexpression of Annexin A1 Suppresses Pro-Inflammatory Factors in PC12 Cells Induced by 1-Methyl-4-Phenylpyridinium. Cell J. 2016;18:197–204. doi: 10.22074/cellj.2016.4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sakaguchi M., Murata H., Sonegawa H., Sakaguchi Y., Futami J., Kitazoe M., Yamada H., Huh N.H. Truncation of Annexin A1 is a regulatory lever for linking epidermal growth factor signaling with cytosolic phospholipase A2 in normal and malignant squamous epithelial cells. J. Biol. Chem. 2007;282:35679–35686. doi: 10.1074/jbc.M707538200. [DOI] [PubMed] [Google Scholar]
- 127.Sakaguchi M., Huh N.H. S100A11, a dual growth regulator of epidermal keratinocytes. Amino. Acids. 2011;41:797–807. doi: 10.1007/s00726-010-0747-4. [DOI] [PubMed] [Google Scholar]
- 128.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Santamaria-Kisiel L., Rintala-Dempsey A.C., Shaw G.S. Calcium-dependent and -independent interactions of the S100 protein family. Biochem. J. 2006;396:201–214. doi: 10.1042/BJ20060195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Blume K.E., Soeroes S., Keppeler H., Stevanovic S., Kretschmer D., Rautenberg M., Wesselborg S., Lauber K. Cleavage of Annexin A1 by ADAM10 during secondary necrosis generates a monocytic “find-me” signal. J. Immunol. 2012;188:135–145. doi: 10.4049/jimmunol.1004073. [DOI] [PubMed] [Google Scholar]
- 131.Movitz C., Sjolin C., Dahlgren C. Cleavage of Annexin I in human neutrophils is mediated by a membrane-localized metalloprotease. Biochim. Biophys. Acta. 1999;1416:101–108. doi: 10.1016/S0005-2736(98)00212-0. [DOI] [PubMed] [Google Scholar]
- 132.Vong L., D’Acquisto F., Pederzoli-Ribeil M., Lavagno L., Flower R.J., Witko-Sarsat V., Perretti M. Annexin 1 cleavage in activated neutrophils: A pivotal role for proteinase 3. J. Biol. Chem. 2007;282:29998–30004. doi: 10.1074/jbc.M702876200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang W., Creutz C.E. Role of the amino-terminal domain in regulating interactions of Annexin I with membranes: Effects of amino-terminal truncation and mutagenesis of the phosphorylation sites. Biochemistry. 1994;33:275–282. doi: 10.1021/bi00167a036. [DOI] [PubMed] [Google Scholar]
- 134.Zoia M.A.P., Azevedo F.V.P., Vecchi L., Mota S.T.S., Rodovalho V.R., Cordeiro A.O., Correia L.I.V., Silva A.C.A., Avila V.M.R., Araujo T.G., et al. Inhibition of Triple-Negative Breast Cancer Cell Aggressiveness by Cathepsin D Blockage: Role of Annexin A1. Int. J. Mol. Sci. 2019;20:1337. doi: 10.3390/ijms20061337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Williams S.L., Milne I.R., Bagley C.J., Gamble J.R., Vadas M.A., Pitson S.M., Khew-Goodall Y. A proinflammatory role for proteolytically cleaved Annexin A1 in neutrophil transendothelial migration. J. Immunol. 2010;185:3057–3063. doi: 10.4049/jimmunol.1000119. [DOI] [PubMed] [Google Scholar]
- 136.Solito E., Christian H.C., Festa M., Mulla A., Tierney T., Flower R.J., Buckingham J.C. Post-translational modification plays an essential role in the translocation of Annexin A1 from the cytoplasm to the cell surface. FASEB J. 2006;20:1498–1500. doi: 10.1096/fj.05-5319fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Solito E., Kamal A., Russo-Marie F., Buckingham J.C., Marullo S., Perretti M. A novel calcium-dependent proapoptotic effect of Annexin 1 on human neutrophils. FASEB J. 2003;17:1544–1546. doi: 10.1096/fj.02-0941fje. [DOI] [PubMed] [Google Scholar]
- 138.Frambach S., de Haas R., Smeitink J.A.M., Rongen G.A., Russel F.G.M., Schirris T.J.J. Brothers in Arms: ABCA1- and ABCG1-Mediated Cholesterol Efflux as Promising Targets in Cardiovascular Disease Treatment. Pharmacol. Rev. 2020;72:152–190. doi: 10.1124/pr.119.017897. [DOI] [PubMed] [Google Scholar]
- 139.Hafiane A., Genest J. ATP binding cassette A1 (ABCA1) mediates microparticle formation during high-density lipoprotein (HDL) biogenesis. Atherosclerosis. 2017;257:90–99. doi: 10.1016/j.atherosclerosis.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 140.Nandi S., Ma L., Denis M., Karwatsky J., Li Z., Jiang X.C., Zha X. ABCA1-mediated cholesterol efflux generates microparticles in addition to HDL through processes governed by membrane rigidity. J. Lipid Res. 2009;50:456–466. doi: 10.1194/jlr.M800345-JLR200. [DOI] [PubMed] [Google Scholar]
- 141.Brancaleone V., Mitidieri E., Flower R.J., Cirino G., Perretti M. Annexin A1 mediates hydrogen sulfide properties in the control of inflammation. J. Pharmacol. Exp. Ther. 2014;351:96–104. doi: 10.1124/jpet.114.217034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Perretti M., Christian H., Wheller S.K., Aiello I., Mugridge K.G., Morris J.F., Flower R.J., Goulding N.J. Annexin I is stored within gelatinase granules of human neutrophil and mobilized on the cell surface upon adhesion but not phagocytosis. Cell Biol. Int. 2000;24:163–174. doi: 10.1006/cbir.1999.0468. [DOI] [PubMed] [Google Scholar]
- 143.Li Y., Ye D. Molecular biology for formyl peptide receptors in human diseases. J. Mol. Med. 2013;91:781–789. doi: 10.1007/s00109-013-1005-5. [DOI] [PubMed] [Google Scholar]
- 144.Ye R.D., Boulay F., Wang J.M., Dahlgren C., Gerard C., Parmentier M., Serhan C.N., Murphy P.M. International Union of Basic and Clinical Pharmacology. LXXIII. Nomenclature for the formyl peptide receptor (FPR) family. Pharmacol. Rev. 2009;61:119–161. doi: 10.1124/pr.109.001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Migeotte I., Communi D., Parmentier M. Formyl peptide receptors: A promiscuous subfamily of G protein-coupled receptors controlling immune responses. Cytokine Growth Factor Rev. 2006;17:501–519. doi: 10.1016/j.cytogfr.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 146.Perretti M., Chiang N., La M., Fierro I.M., Marullo S., Getting S.J., Solito E., Serhan C.N. Endogenous lipid- and peptide-derived anti-inflammatory pathways generated with glucocorticoid and aspirin treatment activate the lipoxin A4 receptor. Nat. Med. 2002;8:1296–1302. doi: 10.1038/nm786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dalpiaz A., Spisani S., Biondi C., Fabbri E., Nalli M., Ferretti M.E. Studies on human neutrophil biological functions by means of formyl-peptide receptor agonists and antagonists. Curr. Drug Targets Immune Endocr. Metab. Disord. 2003;3:33–42. doi: 10.2174/1568008033340333. [DOI] [PubMed] [Google Scholar]
- 148.Gavins F.N., Hickey M.J. Annexin A1 and the regulation of innate and adaptive immunity. Front. Immunol. 2012;3:354. doi: 10.3389/fimmu.2012.00354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cooray S.N., Gobbetti T., Montero-Melendez T., McArthur S., Thompson D., Clark A.J., Flower R.J., Perretti M. Ligand-specific conformational change of the G-protein-coupled receptor ALX/FPR2 determines proresolving functional responses. Proc. Natl. Acad. Sci. USA. 2013;110:18232–18237. doi: 10.1073/pnas.1308253110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Li L., Chen K., Xiang Y., Yoshimura T., Su S., Zhu J., Bian X.W., Wang J.M. New development in studies of formyl-peptide receptors: Critical roles in host defense. J. Leukoc. Biol. 2016;99:425–435. doi: 10.1189/jlb.2RI0815-354RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Vacchelli E., Ma Y., Baracco E.E., Sistigu A., Enot D.P., Pietrocola F., Yang H., Adjemian S., Chaba K., Semeraro M., et al. Chemotherapy-induced antitumor immunity requires formyl peptide receptor 1. Science. 2015;350:972–978. doi: 10.1126/science.aad0779. [DOI] [PubMed] [Google Scholar]
- 152.Nagaya T., Kawata K., Kamekura R., Jitsukawa S., Kubo T., Kamei M., Ogasawara N., Takano K.I., Himi T., Ichimiya S. Lipid mediators foster the differentiation of T follicular helper cells. Immunol. Lett. 2017;181:51–57. doi: 10.1016/j.imlet.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 153.Chen K., Xiang Y., Huang J., Gong W., Yoshimura T., Jiang Q., Tessarollo L., Le Y., Wang J.M. The formylpeptide receptor 2 (Fpr2) and its endogenous ligand cathelin-related antimicrobial peptide (CRAMP) promote dendritic cell maturation. J. Biol. Chem. 2014;289:17553–17563. doi: 10.1074/jbc.M113.535674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kim S.D., Kim J.M., Jo S.H., Lee H.Y., Lee S.Y., Shim J.W., Seo S.K., Yun J., Bae Y.S. Functional expression of formyl peptide receptor family in human NK cells. J. Immunol. 2009;183:5511–5517. doi: 10.4049/jimmunol.0802986. [DOI] [PubMed] [Google Scholar]
- 155.McArthur S., Gobbetti T., Kusters D.H., Reutelingsperger C.P., Flower R.J., Perretti M. Definition of a Novel Pathway Centered on Lysophosphatidic Acid To Recruit Monocytes during the Resolution Phase of Tissue Inflammation. J. Immunol. 2015;195:1139–1151. doi: 10.4049/jimmunol.1500733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Peshavariya H.M., Taylor C.J., Goh C., Liu G.S., Jiang F., Chan E.C., Dusting G.J. Annexin peptide Ac2-26 suppresses TNFalpha-induced inflammatory responses via inhibition of Rac1-dependent NADPH oxidase in human endothelial cells. PLoS ONE. 2013;8:e60790. doi: 10.1371/journal.pone.0060790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Miki T., Yano S., Hanibuchi M., Sone S. Bone metastasis model with multiorgan dissemination of human small-cell lung cancer (SBC-5) cells in natural killer cell-depleted SCID mice. Oncol. Res. 2000;12:209–217. doi: 10.3727/096504001108747701. [DOI] [PubMed] [Google Scholar]
- 158.Huang S., Chen L.Y., Zuraw B.L., Ye R.D., Pan Z.K. Chemoattractant-stimulated NF-kappaB activation is dependent on the low molecular weight GTPase RhoA. J. Biol. Chem. 2001;276:40977–40981. doi: 10.1074/jbc.M105242200. [DOI] [PubMed] [Google Scholar]
- 159.Han P.F., Che X.D., Li H.Z., Gao Y.Y., Wei X.C., Li P.C. Annexin A1 involved in the regulation of inflammation and cell signaling pathways. Chin. J. Traumatol. 2020;23:96–101. doi: 10.1016/j.cjtee.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Biaoxue R., Xiguang C., Shuanying Y. Annexin A1 in malignant tumors: Current opinions and controversies. Int. J. Biol. Markers. 2014;29:e8–e20. doi: 10.5301/jbm.5000046. [DOI] [PubMed] [Google Scholar]
- 161.Wang Y., Serfass L., Roy M.O., Wong J., Bonneau A.M., Georges E. Annexin-I expression modulates drug resistance in tumor cells. Biochem. Biophys. Res. Commun. 2004;314:565–570. doi: 10.1016/j.bbrc.2003.12.117. [DOI] [PubMed] [Google Scholar]
- 162.Liu Y., Hu X., Han C., Wang L., Zhang X., He X., Lu X. Targeting tumor suppressor genes for cancer therapy. BioEssays. 2015;37:1277–1286. doi: 10.1002/bies.201500093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Cao Y., Li Y., Edelweiss M., Arun B., Rosen D., Resetkova E., Wu Y., Liu J., Sahin A., Albarracin C.T. Loss of Annexin A1 expression in breast cancer progression. Appl. Immunohistochem. Mol. Morphol. 2008;16:530–534. doi: 10.1097/PAI.0b013e31817432c3. [DOI] [PubMed] [Google Scholar]
- 164.Hnisz D., Weintraub A.S., Day D.S., Valton A.L., Bak R.O., Li C.H., Goldmann J., Lajoie B.R., Fan Z.P., Sigova A.A., et al. Activation of proto-oncogenes by disruption of chromosome neighborhoods. Science. 2016;351:1454–1458. doi: 10.1126/science.aad9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Anderson M.W., Reynolds S.H., You M., Maronpot R.M. Role of proto-oncogene activation in carcinogenesis. Environ. Health Perspect. 1992;98:13–24. doi: 10.1289/ehp.929813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Foo S.L., Yap G., Cui J., Lim L.H.K. Annexin-A1—A Blessing or a Curse in Cancer? Trends Mol. Med. 2019;25:315–327. doi: 10.1016/j.molmed.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 167.Sobral-Leite M., Wesseling J., Smit V.T., Nevanlinna H., van Miltenburg M.H., Sanders J., Hofland I., Blows F.M., Coulson P., Patrycja G., et al. Annexin A1 expression in a pooled breast cancer series: Association with tumor subtypes and prognosis. BMC Med. 2015;13:156. doi: 10.1186/s12916-015-0392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Vecchi L., Alves Pereira Zoia M., Goss Santos T., de Oliveira Beserra A., Colaco Ramos C.M., Franca Matias Colombo B., Paiva Maia Y.C., Piana de Andrade V., Teixeira Soares Mota S., Goncalves de Araujo T., et al. Inhibition of the AnxA1/FPR1 autocrine axis reduces MDA-MB-231 breast cancer cell growth and aggressiveness in vitro and in vivo. Biochim. Biophys. Acta Mol. Cell Res. 2018;1865:1368–1382. doi: 10.1016/j.bbamcr.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 169.Boudhraa Z., Rondepierre F., Ouchchane L., Kintossou R., Trzeciakiewicz A., Franck F., Kanitakis J., Labeille B., Joubert-Zakeyh J., Bouchon B., et al. Annexin A1 in primary tumors promotes melanoma dissemination. Clin. Exp. Metastasis. 2014;31:749–760. doi: 10.1007/s10585-014-9665-2. [DOI] [PubMed] [Google Scholar]
- 170.Lin Y., Lin G., Fang W., Zhu H., Chu K. Increased expression of Annexin A1 predicts poor prognosis in human hepatocellular carcinoma and enhances cell malignant phenotype. Med Oncol. 2014;31:327. doi: 10.1007/s12032-014-0327-7. [DOI] [PubMed] [Google Scholar]
- 171.Su N., Xu X.Y., Chen H., Gao W.C., Ruan C.P., Wang Q., Sun Y.P. Increased expression of Annexin A1 is correlated with K-ras mutation in colorectal cancer. Tohoku J. Exp. Med. 2010;222:243–250. doi: 10.1620/tjem.222.243. [DOI] [PubMed] [Google Scholar]
- 172.Cheng S.X., Tu Y., Zhang S. FoxM1 promotes glioma cells progression by up-regulating Anxa1 expression. PLoS ONE. 2013;8:e72376. doi: 10.1371/journal.pone.0072376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu Y.F., Zhang P.F., Li M.Y., Li Q.Q., Chen Z.C. Identification of Annexin A1 as a proinvasive and prognostic factor for lung adenocarcinoma. Clin. Exp. Metastasis. 2011;28:413–425. doi: 10.1007/s10585-011-9380-1. [DOI] [PubMed] [Google Scholar]
- 174.Biaoxue R., Xiling J., Shuanying Y., Wei Z., Xiguang C., Jinsui W., Min Z. Upregulation of Hsp90-beta and Annexin A1 correlates with poor survival and lymphatic metastasis in lung cancer patients. J. Exp. Clin. Cancer Res. 2012;31:70. doi: 10.1186/1756-9966-31-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Mota S.T.S., Vecchi L., Alves D.A., Cordeiro A.O., Guimaraes G.S., Campos-Fernandez E., Maia Y.C.P., Dornelas B.C., Bezerra S.M., de Andrade V.P., et al. Annexin A1 promotes the nuclear localization of the epidermal growth factor receptor in castration-resistant prostate cancer. Int. J. Biochem. Cell Biol. 2020;127:105838. doi: 10.1016/j.biocel.2020.105838. [DOI] [PubMed] [Google Scholar]
- 176.Sato Y., Kumamoto K., Saito K., Okayama H., Hayase S., Kofunato Y., Miyamoto K., Nakamura I., Ohki S., Koyama Y., et al. Up-regulated Annexin A1 expression in gastrointestinal cancer is associated with cancer invasion and lymph node metastasis. Exp. Ther. Med. 2011;2:239–243. doi: 10.3892/etm.2011.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rodrigo J.P., Garcia-Pedrero J.M., Fernandez M.P., Morgan R.O., Suárez C., Herrero A. Annexin A1 expression in nasopharyngeal carcinoma correlates with squamous differentiation. Am. J. Rhinol. 2005;19:483–487. doi: 10.1177/194589240501900511. [DOI] [PubMed] [Google Scholar]
- 178.Petrella A., Festa M., Ercolino S.F., Zerilli M., Stassi G., Solito E., Parente L. Annexin-1 downregulation in thyroid cancer correlates to the degree of tumor differentiation. Cancer Biol. Ther. 2006;5:643–647. doi: 10.4161/cbt.5.6.2700. [DOI] [PubMed] [Google Scholar]
- 179.Garcia Pedrero J.M., Fernandez M.P., Morgan R.O., Herrero Zapatero A., Gonzalez M.V., Suarez Nieto C., Rodrigo J.P. Annexin A1 down-regulation in head and neck cancer is associated with epithelial differentiation status. Am. J. Pathol. 2004;164:73–79. doi: 10.1016/S0002-9440(10)63098-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Shen D., Nooraie F., Elshimali Y., Lonsberry V., He J., Bose S., Chia D., Seligson D., Chang H.R., Goodglick L. Decreased expression of Annexin A1 is correlated with breast cancer development and progression as determined by a tissue microarray analysis. Hum. Pathol. 2006;37:1583–1591. doi: 10.1016/j.humpath.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 181.Yom C.K., Han W., Kim S.W., Kim H.S., Shin H.C., Chang J.N., Koo M., Noh D.Y., Moon B.I. Clinical significance of Annexin A1 expression in breast cancer. J. Breast Cancer. 2011;14:262–268. doi: 10.4048/jbc.2011.14.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.de Graauw M., van Miltenburg M.H., Schmidt M.K., Pont C., Lalai R., Kartopawiro J., Pardali E., Le Devedec S.E., Smit V.T., van der Wal A., et al. Annexin A1 regulates TGF-beta signaling and promotes metastasis formation of basal-like breast cancer cells. Proc. Natl. Acad. Sci. USA. 2010;107:6340–6345. doi: 10.1073/pnas.0913360107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Anbalagan D., Yap G., Yuan Y., Pandey V.K., Lau W.H., Arora S., Bist P., Wong J.S., Sethi G., Nissom P.M., et al. Annexin-A1 regulates microRNA-26b* and microRNA-562 to directly target NF-kappaB and angiogenesis in breast cancer cells. PLoS ONE. 2014;9:e114507. doi: 10.1371/journal.pone.0114507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cheng T.Y., Wu M.S., Lin J.T., Lin M.T., Shun C.T., Huang H.Y., Hua K.T., Kuo M.L. Annexin A1 is associated with gastric cancer survival and promotes gastric cancer cell invasiveness through the formyl peptide receptor/extracellular signal-regulated kinase/integrin beta-1-binding protein 1 pathway. Cancer. 2012;118:5757–5767. doi: 10.1002/cncr.27565. [DOI] [PubMed] [Google Scholar]
- 185.Zhu J.F., Huang W., Yi H.M., Xiao T., Li J.Y., Feng J., Yi H., Lu S.S., Li X.H., Lu R.H., et al. Annexin A1-suppressed autophagy promotes nasopharyngeal carcinoma cell invasion and metastasis by PI3K/AKT signaling activation. Cell Death Dis. 2018;9:1154. doi: 10.1038/s41419-018-1204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen P., Min J., Wu H., Zhang H., Wang C., Tan G., Zhang F. Annexin A1 is a potential biomarker of bone metastasis in small cell lung cancer. Oncol. Lett. 2021;21:141. doi: 10.3892/ol.2020.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yao X.H., Ping Y.F., Chen J.H., Chen D.L., Xu C.P., Zheng J., Wang J.M., Bian X.W. Production of angiogenic factors by human glioblastoma cells following activation of the G-protein coupled formylpeptide receptor FPR. J. Neurooncol. 2008;86:47–53. doi: 10.1007/s11060-007-9443-y. [DOI] [PubMed] [Google Scholar]
- 188.Huang J., Chen K., Chen J., Gong W., Dunlop N.M., Howard O.M., Gao Y., Bian X.W., Wang J.M. The G-protein-coupled formylpeptide receptor FPR confers a more invasive phenotype on human glioblastoma cells. Br. J. Cancer. 2010;102:1052–1060. doi: 10.1038/sj.bjc.6605591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Zhou Y., Bian X., Le Y., Gong W., Hu J., Zhang X., Wang L., Iribarren P., Salcedo R., Howard O.M., et al. Formylpeptide receptor FPR and the rapid growth of malignant human gliomas. J. Natl. Cancer Inst. 2005;97:823–835. doi: 10.1093/jnci/dji142. [DOI] [PubMed] [Google Scholar]
- 190.Chen D.L., Ping Y.F., Yu S.C., Chen J.H., Yao X.H., Jiang X.F., Zhang H.R., Wang Q.L., Bian X.W. Downregulating FPR restrains xenograft tumors by impairing the angiogenic potential and invasive capability of malignant glioma cells. Biochem. Biophys. Res. Commun. 2009;381:448–452. doi: 10.1016/j.bbrc.2009.02.065. [DOI] [PubMed] [Google Scholar]
- 191.Snapkov I., Oqvist C.O., Figenschau Y., Kogner P., Johnsen J.I., Sveinbjornsson B. The role of formyl peptide receptor 1 (FPR1) in neuroblastoma tumorigenesis. BMC Cancer. 2016;16:490. doi: 10.1186/s12885-016-2545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Alldridge L.C., Harris H.J., Plevin R., Hannon R., Bryant C.E. The annexin protein lipocortin 1 regulates the MAPK/ERK pathway. J. Biol. Chem. 1999;274:37620–37628. doi: 10.1074/jbc.274.53.37620. [DOI] [PubMed] [Google Scholar]
- 193.Jo E.J., Lee H.Y., Kim J.I., Kang H.K., Lee Y.N., Kwak J.Y., Bae Y.S. Activation of formyl peptide receptor-like 1 by WKYMVm induces serine phosphorylation of STAT3, which inhibits its tyrosine phosphorylation and nuclear translocation induced by hydrogen peroxide. Life Sci. 2004;75:2217–2232. doi: 10.1016/j.lfs.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 194.Shi Y., Lai X., Ye L., Chen K., Cao Z., Gong W., Jin L., Wang C., Liu M., Liao Y., et al. Activated niacin receptor HCA2 inhibits chemoattractant-mediated macrophage migration via Gβγ/PKC/ERK1/2 pathway and heterologous receptor desensitization. Sci. Rep. 2017;7:42279. doi: 10.1038/srep42279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wang X., Qin W., Song M., Zhang Y., Sun B. Exogenous carbon monoxide inhibits neutrophil infiltration in LPS-induced sepsis by interfering with FPR1 via p38 MAPK but not GRK2. Oncotarget. 2016;7:34250–34265. doi: 10.18632/oncotarget.9084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Cao G., Zhang Z. FPR1 mediates the tumorigenicity of human cervical cancer cells. Cancer Manag. Res. 2018;10:5855–5865. doi: 10.2147/CMAR.S182795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Khau T., Langenbach S.Y., Schuliga M., Harris T., Johnstone C.N., Anderson R.L., Stewart A.G. Annexin-1 signals mitogen-stimulated breast tumor cell proliferation by activation of the formyl peptide receptors (FPRs) 1 and 2. FASEB J. 2011;25:483–496. doi: 10.1096/fj.09-154096. [DOI] [PubMed] [Google Scholar]
- 198.Chen K., Bao Z., Gong W., Tang P., Yoshimura T., Wang J.M. Regulation of inflammation by members of the formyl-peptide receptor family. J. Autoimmun. 2017;85:64–77. doi: 10.1016/j.jaut.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Cheng T.Y., Wu M.S., Lin J.T., Lin M.T., Shun C.T., Hua K.T., Kuo M.L. Formyl Peptide receptor 1 expression is associated with tumor progression and survival in gastric cancer. Anticancer. Res. 2014;34:2223–2229. [PubMed] [Google Scholar]
- 200.Prevete N., Liotti F., Visciano C., Marone G., Melillo R.M., de Paulis A. The formyl peptide receptor 1 exerts a tumor suppressor function in human gastric cancer by inhibiting angiogenesis. Oncogene. 2015;34:3826–3838. doi: 10.1038/onc.2014.309. [DOI] [PubMed] [Google Scholar]
- 201.Lin C.Y., Jeng Y.M., Chou H.Y., Hsu H.C., Yuan R.H., Chiang C.P., Kuo M.Y. Nuclear localization of Annexin A1 is a prognostic factor in oral squamous cell carcinoma. J. Surg. Oncol. 2008;97:544–550. doi: 10.1002/jso.20992. [DOI] [PubMed] [Google Scholar]
- 202.Zhu F., Xu C., Jiang Z., Jin M., Wang L., Zeng S., Teng L., Cao J. Nuclear localization of Annexin A1 correlates with advanced disease and peritoneal dissemination in patients with gastric carcinoma. Anat. Rec. 2010;293:1310–1314. doi: 10.1002/ar.21176. [DOI] [PubMed] [Google Scholar]
- 203.Kunkel T.A. The high cost of living. American Association for Cancer Research Special Conference: Endogenous sources of mutations, Fort Myers, Florida, USA, 11–15 November 1998. Trends Genet. 1999;15:93–94. doi: 10.1016/S0168-9525(98)01664-3. [DOI] [PubMed] [Google Scholar]
- 204.Kunz B.A., Straffon A.F., Vonarx E.J. DNA damage-induced mutation: Tolerance via translesion synthesis. Mutat. Res. 2000;451:169–185. doi: 10.1016/S0027-5107(00)00048-8. [DOI] [PubMed] [Google Scholar]
- 205.Makridakis N.M., Reichardt J.K. Translesion DNA Polymerases and Cancer. Front. Genet. 2012;3:174. doi: 10.3389/fgene.2012.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Dieckman L.M., Freudenthal B.D., Washington M.T. PCNA structure and function: Insights from structures of PCNA complexes and post-translationally modified PCNA. Sub Cell. Biochem. 2012;62:281–299. doi: 10.1007/978-94-007-4572-8_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Choi S., Srivas R., Fu K.Y., Hood B.L., Dost B., Gibson G.A., Watkins S.C., Van Houten B., Bandeira N., Conrads T.P., et al. Quantitative proteomics reveal ATM kinase-dependent exchange in DNA damage response complexes. J. Proteome Res. 2012;11:4983–4991. doi: 10.1021/pr3005524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hirata F., Thibodeau L.M., Hirata A. Ubiquitination and SUMOylation of Annexin A1 and helicase activity. Biochim. Biophys. Acta. 2010;1800:899–905. doi: 10.1016/j.bbagen.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 209.Ganesan T., Sinniah A., Ibrahim Z.A., Chik Z., Alshawsh M.A. Annexin A1: A Bane or a Boon in Cancer? A Systematic Review. Molecules. 2020;25:3700. doi: 10.3390/molecules25163700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhu F., Wang Y., Zeng S., Fu X., Wang L., Cao J. Involvement of Annexin A1 in multidrug resistance of K562/ADR cells identified by the proteomic study. Omics. 2009;13:467–476. doi: 10.1089/omi.2009.0046. [DOI] [PubMed] [Google Scholar]
- 211.D’Acunto C.W., Gbelcova H., Festa M., Ruml T. The complex understanding of Annexin A1 phosphorylation. Cell. Signal. 2014;26:173–178. doi: 10.1016/j.cellsig.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 212.Pepinsky R.B., Sinclair L.K. Epidermal growth factor-dependent phosphorylation of lipocortin. Nature. 1986;321:81–84. doi: 10.1038/321081a0. [DOI] [PubMed] [Google Scholar]
- 213.Skouteris G.G., Schröder C.H. The hepatocyte growth factor receptor kinase-mediated phosphorylation of lipocortin-1 transduces the proliferating signal of the hepatocyte growth factor. J. Biol. Chem. 1996;271:27266–27273. doi: 10.1074/jbc.271.44.27266. [DOI] [PubMed] [Google Scholar]
- 214.Shao G., Zhou H., Zhang Q., Jin Y., Fu C. Advancements of Annexin A1 in inflammation and tumorigenesis. OncoTargets Ther. 2019;12:3245–3254. doi: 10.2147/OTT.S202271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Moraes L.A., Kar S., Foo S.L., Gu T., Toh Y.Q., Ampomah P.B., Sachaphibulkij K., Yap G., Zharkova O., Lukman H.M., et al. Annexin-A1 enhances breast cancer growth and migration by promoting alternative macrophage polarization in the tumour microenvironment. Sci. Rep. 2017;7:17925. doi: 10.1038/s41598-017-17622-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Li Y., Cai L., Wang H., Wu P., Gu W., Chen Y., Hao H., Tang K., Yi P., Liu M., et al. Pleiotropic regulation of macrophage polarization and tumorigenesis by formyl peptide receptor-2. Oncogene. 2011;30:3887–3899. doi: 10.1038/onc.2011.112. [DOI] [PubMed] [Google Scholar]
- 217.Locatelli I., Sutti S., Jindal A., Vacchiano M., Bozzola C., Reutelingsperger C., Kusters D., Bena S., Parola M., Paternostro C., et al. Endogenous Annexin A1 is a novel protective determinant in nonalcoholic steatohepatitis in mice. Hepatology. 2014;60:531–544. doi: 10.1002/hep.27141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ferlazzo V., D’Agostino P., Milano S., Caruso R., Feo S., Cillari E., Parente L. Anti-inflammatory effects of Annexin-1: Stimulation of IL-10 release and inhibition of nitric oxide synthesis. Int. Immunopharmacol. 2003;3:1363–1369. doi: 10.1016/S1567-5769(03)00133-4. [DOI] [PubMed] [Google Scholar]
- 219.Weyd H., Abeler-Dorner L., Linke B., Mahr A., Jahndel V., Pfrang S., Schnolzer M., Falk C.S., Krammer P.H. Annexin A1 on the surface of early apoptotic cells suppresses CD8+ T cell immunity. PLoS ONE. 2013;8:e62449. doi: 10.1371/journal.pone.0062449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Gold R., Schmied M., Tontsch U., Hartung H.P., Wekerle H., Toyka K.V., Lassmann H. Antigen presentation by astrocytes primes rat T lymphocytes for apoptotic cell death. A model for T-cell apoptosis in vivo. Pt 2Brain. 1996;119:651–659. doi: 10.1093/brain/119.2.651. [DOI] [PubMed] [Google Scholar]
- 221.D’Acquisto F., Merghani A., Lecona E., Rosignoli G., Raza K., Buckley C.D., Flower R.J., Perretti M. Annexin-1 modulates T-cell activation and differentiation. Blood. 2007;109:1095–1102. doi: 10.1182/blood-2006-05-022798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Ng F.S., Wong K.Y., Guan S.P., Mustafa F.B., Kajiji T.S., Bist P., Biswas S.K., Wong W.S., Lim L.H. Annexin-1-deficient mice exhibit spontaneous airway hyperresponsiveness and exacerbated allergen-specific antibody responses in a mouse model of asthma. Clin. Exp. Allergy. 2011;41:1793–1803. doi: 10.1111/j.1365-2222.2011.03855.x. [DOI] [PubMed] [Google Scholar]
- 223.Kamal A.M., Flower R.J., Perretti M. An overview of the effects of Annexin 1 on cells involved in the inflammatory process. Memórias Inst. Oswaldo Cruz. 2005;100((Suppl. 1)):39–47. doi: 10.1590/S0074-02762005000900008. [DOI] [PubMed] [Google Scholar]
- 224.Jeppesen D.K., Fenix A.M., Franklin J.L., Higginbotham J.N., Zhang Q., Zimmerman L.J., Liebler D.C., Ping J., Liu Q., Evans R., et al. Reassessment of Exosome Composition. Cell. 2019;177:428–445.e418. doi: 10.1016/j.cell.2019.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Lo Cicero A., Stahl P.D., Raposo G. Extracellular vesicles shuffling intercellular messages: For good or for bad. Curr. Opin. Cell Biol. 2015;35:69–77. doi: 10.1016/j.ceb.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 226.van Niel G., D’Angelo G., Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell. Biol. 2018;19:213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 227.Aalberts M., van Dissel-Emiliani F.M., van Adrichem N.P., van Wijnen M., Wauben M.H., Stout T.A., Stoorvogel W. Identification of distinct populations of prostasomes that differentially express prostate stem cell antigen, Annexin A1, and GLIPR2 in humans. Biol. Reprod. 2012;86:82. doi: 10.1095/biolreprod.111.095760. [DOI] [PubMed] [Google Scholar]
- 228.Perretti M., Cooper D., Dalli J., Norling L.V. Immune resolution mechanisms in inflammatory arthritis. Nat. Rev. Rheumatol. 2017;13:87–99. doi: 10.1038/nrrheum.2016.193. [DOI] [PubMed] [Google Scholar]
- 229.Headland S.E., Norling L.V. The resolution of inflammation: Principles and challenges. Semin. Immunol. 2015;27:149–160. doi: 10.1016/j.smim.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 230.Gasser O., Schifferli J.A. Activated polymorphonuclear neutrophils disseminate anti-inflammatory microparticles by ectocytosis. Blood. 2004;104:2543–2548. doi: 10.1182/blood-2004-01-0361. [DOI] [PubMed] [Google Scholar]
- 231.Rhys H.I., Dell’Accio F., Pitzalis C., Moore A., Norling L.V., Perretti M. Neutrophil Microvesicles from Healthy Control and Rheumatoid Arthritis Patients Prevent the Inflammatory Activation of Macrophages. EBioMedicine. 2018;29:60–69. doi: 10.1016/j.ebiom.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yang Y., Liu Y., Yao X., Ping Y., Jiang T., Liu Q., Xu S., Huang J., Mou H., Gong W., et al. Annexin 1 released by necrotic human glioblastoma cells stimulates tumor cell growth through the formyl peptide receptor 1. Am. J. Pathol. 2011;179:1504–1512. doi: 10.1016/j.ajpath.2011.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Link C., Bujupi F., Krammer P.H., Weyd H. Annexin-coated particles induce antigen-specific immunosuppression. Autoimmunity. 2020;53:86–94. doi: 10.1080/08916934.2019.1710134. [DOI] [PubMed] [Google Scholar]
- 234.Ampomah P.B., Moraes L.A., Lukman H.M., Lim L.H.K. Formyl peptide receptor 2 is regulated by RNA mimics and viruses through an IFN-β-STAT3-dependent pathway. FASEB J. 2018;32:1468–1478. doi: 10.1096/fj.201700584RR. [DOI] [PubMed] [Google Scholar]
- 235.Oshi M., Tokumaru Y., Mukhopadhyay S., Yan L., Matsuyama R., Endo I., Takabe K. Annexin A1 Expression Is Associated with Epithelial-Mesenchymal Transition (EMT), Cell Proliferation, Prognosis, and Drug Response in Pancreatic Cancer. Cells. 2021;10:653. doi: 10.3390/cells10030653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Huang S.H., Li Y., Zhang J., Rong J., Ye S. Epidermal growth factor receptor-containing exosomes induce tumor-specific regulatory T cells. Cancer Investig. 2013;31:330–335. doi: 10.3109/07357907.2013.789905. [DOI] [PubMed] [Google Scholar]
- 237.Azuma K., Ota K., Kawahara A., Hattori S., Iwama E., Harada T., Matsumoto K., Takayama K., Takamori S., Kage M., et al. Association of PD-L1 overexpression with activating EGFR mutations in surgically resected nonsmall-cell lung cancer. Ann. Oncol. 2014;25:1935–1940. doi: 10.1093/annonc/mdu242. [DOI] [PubMed] [Google Scholar]
- 238.Akbay E.A., Koyama S., Carretero J., Altabef A., Tchaicha J.H., Christensen C.L., Mikse O.R., Cherniack A.D., Beauchamp E.M., Pugh T.J., et al. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov. 2013;3:1355–1363. doi: 10.1158/2159-8290.CD-13-0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Chen N., Fang W., Zhan J., Hong S., Tang Y., Kang S., Zhang Y., He X., Zhou T., Qin T., et al. Upregulation of PD-L1 by EGFR Activation Mediates the Immune Escape in EGFR-Driven NSCLC: Implication for Optional Immune Targeted Therapy for NSCLC Patients with EGFR Mutation. J. Thorac. Oncol. 2015;10:910–923. doi: 10.1097/JTO.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 240.Li T., Zhang C., Zhao G., Zhang X., Hao M., Hassan S., Zhang M., Zheng H., Yang D., Liu L., et al. IGFBP2 regulates PD-L1 expression by activating the EGFR-STAT3 signaling pathway in malignant melanoma. Cancer Lett. 2020;477:19–30. doi: 10.1016/j.canlet.2020.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Lo H.W., Hsu S.C., Ali-Seyed M., Gunduz M., Xia W., Wei Y., Bartholomeusz G., Shih J.Y., Hung M.C. Nuclear interaction of EGFR and STAT3 in the activation of the iNOS/NO pathway. Cancer Cell. 2005;7:575–589. doi: 10.1016/j.ccr.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 242.Bronte V., Kasic T., Gri G., Gallana K., Borsellino G., Marigo I., Battistini L., Iafrate M., Prayer-Galetti T., Pagano F., et al. Boosting antitumor responses of T lymphocytes infiltrating human prostate cancers. J. Exp. Med. 2005;201:1257–1268. doi: 10.1084/jem.20042028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Brand T.M., Iida M., Luthar N., Starr M.M., Huppert E.J., Wheeler D.L. Nuclear EGFR as a molecular target in cancer. Radiother. Oncol. 2013;108:370–377. doi: 10.1016/j.radonc.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 244.Eden E.R., Sanchez-Heras E., Tsapara A., Sobota A., Levine T.P., Futter C.E. Annexin A1 Tethers Membrane Contact Sites that Mediate ER to Endosome Cholesterol Transport. Dev. Cell. 2016;37:473–483. doi: 10.1016/j.devcel.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Zhao X., Ma W., Li X., Li H., Li J., Li H., He F. ANXA1 enhances tumor proliferation and migration by regulating epithelial-mesenchymal transition and IL-6/JAK2/STAT3 pathway in papillary thyroid carcinoma. J. Cancer. 2021;12:1295–1306. doi: 10.7150/jca.52171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.