Abstract
The psychosocial impact of the work environment during the COVID-19 pandemic on health professionals is a growing issue. The present study examined specific psychosocial work environment indicators during the COVID-19 pandemic, through a multiple regression model of a self-administered cross-sectional online survey in a cohort of physical therapists from a region of Southern Italy from March 2020 to May 2021. The questionnaire contained items on work and healthcare issues related to COVID-19. Eighty physical therapists (29 male and 51 female), mean age 32.5 ± 10.1 years, were involved in this survey. The multiple regression analysis showed that “management activity” was significantly correlated to “therapist frustration” during the COVID-19 pandemic (ΔR2 = 0.16; p < 0.03). Findings of this study underline the importance of a healthy psychosocial work environment to enhance job satisfaction of all health professionals and to avoid role conflict and burnout syndrome during the COVID-19 pandemic.
Keywords: COVID-19, psychology, physical therapy, rehabilitation, work environment, healthcare, burnout, depression, healthcare workers
1. Introduction
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which started in late December 2019 in Hubei Province in China, caused millions of cases of coronavirus disease (COVID-19) worldwide in just a few months and evolved into a pandemic [1]. In Italy, from 3 January 2020 to 11 June 2021, there have been 4,239,868 confirmed cases of COVID-19 with 126,855 deaths, as reported by the World Health Organization [2].
Overall, in October 2020, the research on this topic progressively shifted from the description of COVID-19 related disability in the acute phase (almost half of papers published in 2020) to complications in the sub-acute (33.9%) and chronic phase (4.8%). In early 2021, the research shed light on putative predictive factors for unfavorable outcomes and severe consequences of COVID-19 infection on long-lasting activity limitations and participation restrictions [2]. To date, large numbers of COVID-19 patients require outpatient and home rehabilitation care and the negative impact of the pandemic on Rehabilitation Units’ performance and organization still causes deficiencies in meeting patient needs [3]. In this scenario, the remodeling of hospitals and territorial rehabilitation services would still be necessary, while recommendations on telerehabilitation approaches still do not seem to be established [4].
Early rehabilitation treatment begins immediately after discharge from intensive care and clinically stable COVID-19 patients in the post-acute phase have undergone a rehabilitation protocol aimed at reducing dyspnea and improving gas exchange, muscle function and autonomy in activities of daily living (ADL) [5].
The dramatic spread of the current COVID-19 pandemic in Italy has spurred the establishment of multidisciplinary operators to address the complex and multifaceted disabling sequelae affecting these patients and to set up comprehensive and effective rehabilitative interventions. The so-called “respiratory rehabilitators” (pulmonologists and physical therapists), who have been involved for years in the treatment of patients with disabilities secondary to pathological respiratory conditions, are the health professionals most involved in this complex rehabilitative framework. Their experience gained in the management of chronic and acute respiratory failure is proving to be a fundamental reference point for the management of patients needing rehabilitative interventions during the COVID-19 epidemic, although the disabling sequelae of COVID-19 are not only related to the respiratory system but also include neuromuscular and cognitive impairments [6,7,8]. Hence, the reorganization involved in taking care of this scenario is not likely to be a short-term issue [9]. In short, previous research has provided insight into the relationships between personality, age, gender, coping styles, social support, and emotional distress during the COVID-19 pandemic [10,11].
A recent study performed in 12 different countries found that the COVID-19 pandemic disrupted the usual rehabilitation services, with the negative consequence that many patients are not receiving the correct rehabilitative care. In this context, infection control procedures posed significant barriers to providing effective rehabilitative interventions [12]. Moreover, hospitals have also requested greater support from physical and rehabilitative medicine (PRM) physicians due to the high amount of COVID-19 patient admittances. Thus, their usual clinical activities have been dramatically reduced. Moreover, the decisions of the Italian government aimed at slowing down the pandemic phenomenon and reduce the burden on the emergency departments reduced outpatient access and hospital admissions for chronic patients [13]. Taken together, all these issues have strongly limited access to treatment for rehabilitative patients.
Koffman et al. reported that uncertainty is pervasive in healthcare with overlapping sources including ethical and systems uncertainty for health systems, providers, patients, and families in addressing doubts and concerns during the COVID19 epidemic. In this context, it is recommended to set up new management workflows tailored for the pandemic, rehearsing and exploring imaginative ways to show empathy and collaborate with patients/families in order to assist physical therapists in coping with a “new normal” [14,15].
Shechter et al. suggested that severe COVID-19-related psychological distress is expected to have downstream impacts on healthcare workers’ physical health, in light of the well-known association between clinical workplace environmental stressors and long -term cardiometabolic risk, exerted by both direct (systemic inflammation, arterial damage, increased blood pressure) and indirect (maladaptive coping such as substance use, poor sleep) factors [16]. In this context, considering the basic psychological needs in terms of frustration, rather than a lack of satisfaction, it is crucial to provide a more adequate understanding of the damaging effects that psychological distress might have in the workplace [17].
As a whole, learning of new protocols and procedures at work, dealing with an exceedingly large number of patients and sustaining long shifts with protective equipment along with the fear of getting infected, has led healthcare workers to perceive a lower quality work environment relationships with colleagues [18]. This has often resulted in developing emotional and behavioral symptoms such as excessive worries, mood swings, sleep difficulties and eating disorders [19,20]. Given this background, key protective factors have been identified to help healthcare workers to cope with the work situation in a more resilient way, limiting distress [21]. These latter have included both individual characteristics (e.g., resilient coping style and self-esteem) [22], and perceived characteristics of the work environment (e.g., sense of work group cohesion and coherence) that have been shown to be protective measures against distress [23,24].
In this scenario, a better understanding of the relationships between clinical and emotional outcomes would increase our knowledge of these protective or vulnerability factors associated with the development of negative emotions in healthcare workers [25]. Moreover, in addition to the personal experiences of trauma, several reports have underlined many operational difficulties stemming from power hierarchies, inequality and a perceived disconnection between senior management and front-line staff [26,27].
Therefore, the aim of the present study is to assess the correlation between work environmental factors and psychological distress in a cohort of physical therapists working in hospitals in Southern Italy during the COVID-19 pandemic.
2. Materials and Methods
2.1. Participants
In this local cross-sectional survey, entitled “COVID-19: A Long And Brief Rehabilitative Interdisciplinary Approach (C.A.L.A.B.R.I.A) study”, we enrolled a cohort of Italian physical therapists involved in the management of patients with post-acute COVID-19 in Calabria, a Region of Southern Italy. All study participants were recruited from March 2020 to May 2021 through an online recruitment strategy and were asked to fill in a questionnaire, after a detailed description of the survey and previous authorization by the participants to be contacted for survey purposes.
Inclusion criteria were: (a) physical therapists working in COVID-19 clinics; (b) physical therapists involved in the management of patients with COVID-19; (c) consent to share their data with the researchers (which guaranteed privacy protection and permission for distribution of the survey). The exclusion criteria were previous diagnosis of psychiatric disorder or a history of confirmed infection with COVID-19. This study was approved by the Institutional Review Board and was performed in accordance with pertinent national regulatory requirements. All the participants were asked to carefully read and sign an informed consent before collecting the data and privacy protection was guaranteed by the study investigators.
2.2. Survey Questionnaire
All participants were asked to complete a nine-item questionnaire built for the C.A.L.A.B.R.I.A study to evaluate the correlation among work environmental determinants and psychological distress in a cohort of physical therapists in hospitals in Southern Italy during the second wave of the COVID-19 pandemic. The survey questionnaire was created by a group of technical experts, composed of 6 PRM physicians, 2 cognitive psychologists, 1 physical therapist, and 1 healthcare director. This investigation was in agreement with previous studies already published in the literature focusing on occupational environmental factors [28].
The questionnaire started with a brief description (including aim) of the C.A.L.A.B.R.I.A study, also reporting the online informed consent agreement via the following statement: “I have read the consent and agree to participate”. We performed an online recruitment strategy through E-mails, Facebook, and WhatsApp, to administer the link to the present survey.
Before starting the online survey, all study participants were asked to provide information on personal data (e.g., age, gender, work experience, etc.). The questionnaire consisted of two different domains: domain A) consisted of open-ended questions describing epidemiologic and job information during the COVID-19 pandemic; domain B) consisted of questions on psychological distress and work environmental factors, assessed by a 7-point Likert scale [29] (ranging from 1 = never to 7 = always). The questionnaire is shown in detail in Table 1.
Table 1.
Online questionnaire aimed at evaluating epidemiological data, psychological distress and work environmental factors in physical therapists involved in the C.A.L.A.B.R.I.A. study.
| Domain A: Epidemiologic questions |
| (Q1) How long have you been working in this Region and in which sector do you work? |
| (Q2) What has significantly changed in your work duties during COVID-19 pandemic? |
| (Q3) Have you performed a specific course/training to manage COVID-19 issues in your workplace? |
| Domain B: Questions on psychological distress and work environment (7-point Likert scale) |
| (Q4) How much do you feel sure of your working skills during COVID-19 pandemic? |
| (Q5) How much does your superior actively work to ensure an optimal organization of the activities? |
| (Q6) How much does your superior actively work to ensure good conditions of well-being and employee development? |
| (Q7) How much do you feel frustrated in relation to your work? |
| (Q8) How much do you feel exposed to the risk of being affected by COVID-19? |
| (Q9) How much do you fear your colleagues being affected by COVID-19? |
2.3. Statistical Analysis
The statistical analysis was performed using JASP 0.14 (JASP Team, Amsterdam, The Netherlands). Data are presented as means ± standard deviations (SD) for continuous variables, and counts and percentages for dichotomous, nominal, and ordinal variables. Kendall’s correlations τ were conducted to investigate the extent of association between two sets of ranked order data, with range of values from −1 to 1 [30,31]. In more detail, we performed a sequential multiple regression considering Q7 (“How much do you feel frustrated in relation to your work?”) as criterion value (CV) and inserting a fixed number of predictive variables (PV) (Q4, Q5, Q6, Q8, and Q9). Hence, the objective of this sequential multiple regression is to estimate the individual contribution of each PV in changing the CV (Q7) variance, reported as change in R2 (denoted as delta R2 or ΔR2) [32]. ΔR2 resulted from entering each PV into the above-mentioned regression mode, emerging from entering each PV into a regression design [32], and consists of physical therapists’ frustration change according to the other variables [32]. Moreover, we also estimated the Root Mean Square Error (RMSE) as the standard deviation of the residuals (prediction errors) to enrich the quality of the model. Residuals are considered as a distance measure from data points of the regression line; thus, the lower the RMSE, the better the model [33]. Finally, we performed the F-statistic giving the overall significance of the model, evaluating if at least one predictor variable has a non-zero coefficient [34].
3. Results
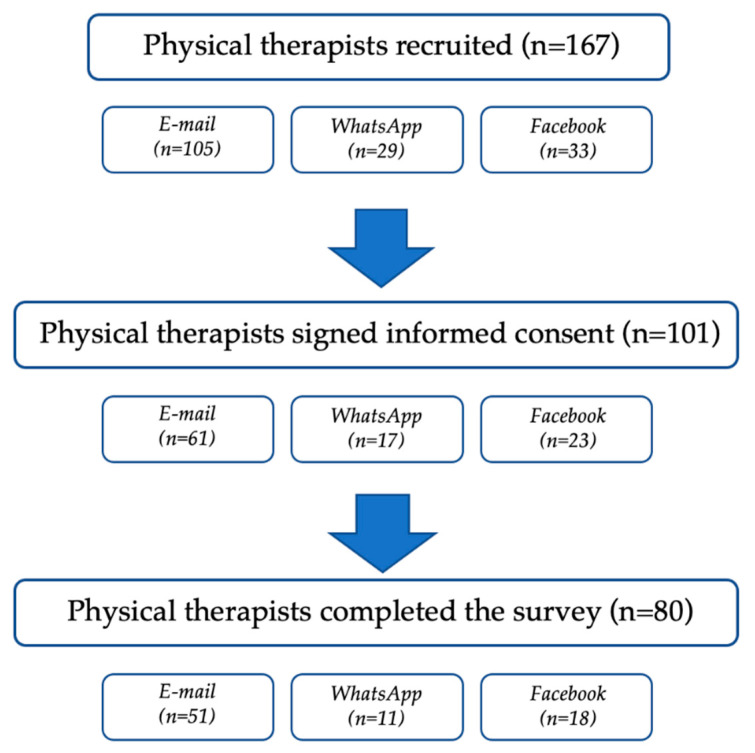
Out of 167 physical therapists recruited through an online recruitment strategy, 101 physical therapists adequately signed the informed consent. However, 18 forgot to answer at least one psychological impact-related question, and three did not send the form, thus being excluded from the analysis (see Figure 1 for further details).
Figure 1.
Survey response flow chart.
Therefore, 80 physical therapists (29 male and 51 female), mean aged 32.5 ± 10.1 years, were involved in this survey, as depicted in Table 2.
Table 2.
Demographic characteristics of participants.
| Total (n = 80) | |
|---|---|
| Male/female | 29/51 |
| Age (years) | 32.5 ± 10.1 |
| Physical therapists working in the private sector (%) | 49 (61.3) |
| Physical therapists working in the National Health System (%) | 31 (38.7) |
Data are presented as mean and standard deviation for continuous variables; counts and percentages for categorical variables; x/y for ratios.
Regarding the first question (Q1), 42 (52.5%) participants had worked in the Calabria Region for less than 5 years, 23 (28.8%) for more than 5 years, and 21 (26.2%) for less than a year. Forty-nine (61.3%) physical therapists were hired by private facilities affiliated with the Italian National Health System, while 31 (38.7%) were hired by the NHS. Regarding question Q2, 64 (80.0%), participants stated that their job duties had totally changed, 14 (17.5%) considered their job had partially changed, while only 2 (2.5%) replied that their job duties had not changed at all. Regarding question Q3, 75% of participants revealed that they had not followed an adequate training course for the rehabilitation of patients with COVID-19.
Concerning the questions on psychological distress and work environmental factors, the physical therapists involved in the study reported the following mean values using the 7-point Likert scale:
-
-
Question 4 (Q4—“How much do you feel sure of your working skills during COVID-19 pandemic?”) = 4.3 ± 1.4;
-
-
Question 5 (Q5—“How much does your superior actively work to ensure an optimal organization of the activities?”) = 4.6 ± 1.2;
-
-
Question 6 (Q6—“How much does your superior actively work to ensure good conditions of well-being and employee development?”) = 4.5 ± 1.2;
-
-
Question 7 (Q7—“How much do you feel frustrated in relation to your work?”) = 3.9 ± 1.2;
-
-
Question 8 (Q8—“How much do you feel exposed to the risk of being affected by COVID-19”) = 4.8 ± 1.3;
-
-
Question 9 (Q9—“How much do you fear your colleagues being affected by COVID-19?”) = 4.9 ± 1.1.
As shown in Table 3, we performed Kendall’s τ correlation based on the working sector (private = 0; public = 1) and the gender (male = 0; female = 1), obtaining a significant negative Kendall’s τ correlation between the question of the public or private nature of the physiotherapist’s work with a τ = −0.32; (p < 0.01) for Q4, and a τ = −0.48 (p < 0.001) for Q6. The physiotherapists that work in the public sector reported a higher confidence in their skills and their direct superiors worked more to ensure good conditions of well-being.
Table 3.
Kendall’s τ correlations concerning demographical data of physical therapists involved in the C.A.L.A.B.R.I.A. study (n = 80).
| Variable | In Which Sector Do You Work? | Age | Gender |
|---|---|---|---|
| In which sector do you work? | — | ||
| Age | 0.04 | — | |
| Gender | 0.14 | 0.03 | — |
| Q4 | −0.32 * | 0.13 | −0.04 |
| Q5 | −0.02 | −0.06 | −0.06 |
| Q6 | −0.48 ** | 0.01 | −0.16 |
| Q7 | 0.16 | 0.18 | −0.09 |
| Q8 | 0.06 | −0.03 | 0.09 |
| Q9 | 0.16 | 0.08 | 0.05 |
* = p < 0.01, ** = p < 0.001.
Furthermore, a significant positive Kendall’s τ correlation was found between Q4 and Q5 (τ = 0.52; p < 0.001); τ = 0.36 in Q4:Q6 (p = 0.03); τ = 0.50 in Q5:Q6 (p < 0.001), τ = 0.39 in Q5:Q7 (p = 0.03); τ = 0.50 in Q7:Q9 (p < 0.004); τ = 0.69 in Q8:Q9 (p < 0.001) (see Table 4 for further details).
Table 4.
Kendall’s τ correlations concerning the answers to the questions on psychological distress and work environmental factors by physical therapists involved in the C.A.L.A.B.R.I.A. study (n = 80).
| Variable | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|
| 1. Q4 | — | |||||
| 2. Q5 | 0.52 *** | — | ||||
| 3. Q6 | 0.36 * | 0.50 *** | — | |||
| 4. Q7 | −0.24 | −0.30 * | −0.27 | — | ||
| 5. Q8 | −0.03 | −0.26 | 0.01 | 0.31 | — | |
| 6. Q9 | −0.04 | −0.06 | −0.24 * | 0.50 ** | 0.69 *** | — |
* = p < 0.05; ** = p <0.01; *** = p < 0.001.
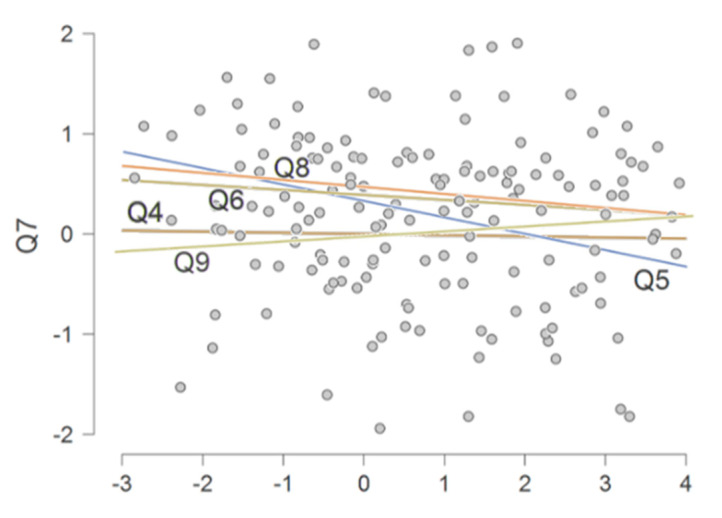
Moreover, by performing a sequential multiple regression, we evaluated each question in relation to the variation made to the frustration perceived by each participant (Q7) (see Figure 2).
Figure 2.
Multiple regression scatterplot, estimating the individual contribution of each predictive variable (Q4, Q5, Q6, Q8, and Q9) in changing the variance of the criterion value (Q7: “To what extent did you feel frustrated in relation to your work?”), to estimate the individual contribution of each answer by physical therapists to the other specific questions on psychological distress and work environmental factors.
Therefore, after the multiple regression analysis, we reported a significant ΔR2 of 0.16 (p = 0.03) of Q5 regarding Q7, with a RMSE = 1.12.
4. Discussion
Other recent studies have showed a high prevalence of rehabilitative healthcare professionals’ burnout during the COVID-19 pandemic [35,36]. However, to the best of our knowledge, this is the first study investigating the impact that the psychosocial work environment might have on frustration perceived by physical therapists.
Indeed, this cross-sectional survey interestingly highlighted that the 16% incremental variance of the frustration related to the work of the physical therapists involved might be explained by the question “How much does your superior actively work to ensure an optimal organization of the activities? (Q5)”. More in detail, the variation in the therapist’s frustration depended on activity by their superiors in ensuring optimal working conditions during the COVID-19 pandemic.
Recommendations have been addressed to support the implementation of a multidisciplinary rehabilitative pathway for those COVID-19 patients in need of functional recovery [37]. In this context, early post-acute rehabilitation including mobilization and respiratory physiotherapy measures may have a significant impact on patient recovery after COVID-19 and may be especially important for patients who needed critical care medicine with or without mechanical ventilation and are at risk for the development of post-intensive care syndrome [38]. Recent studies reported that a significant percentage of healthcare workers, including physical therapists, suffer from psychological problems such as depression, insomnia, obsessive-compulsive symptoms and anxiety related to the workplace and general issues related to the COVID-19 pandemic [39,40]. Indeed, manual and direct contact with patients increases fear and worries of contracting and transmitting the virus to family members, leading to the promotion of partially effective treatment strategies including not touching the patient unless necessary, necessitating patients to use face masks, excessive use of sanitizers and the provision of instructions to patients from a distance [41]. Thus, considering that healthcare workers are vulnerable to psychological symptoms, and that such symptoms lasting for long periods lead to allostatic overload [42], the mental health of physical therapists should be constantly and cautiously monitored [39].
The reorganization of the rehabilitation services exploited the professional and clinical skills of the physiotherapists [43]. It is well known that physiotherapists consider clinical supervision to be effective, especially if it favors the development of their professional skills. Indeed, the physical therapists preferred a direct supervision model, in which their supervisor directly observed and guided the development of their professional expertise [44]. Additionally, physical therapists recognized the importance of informal supervision in which guidance is provided from supervisors who appreciate the supervision process [45].
The analysis of the demographic data correlations showed two significant associations between the private or public employment relationship and these two questions: “Q4—How much do you feel sure of your working skills during COVID-19 pandemic?” and “Q6—How much does your superior actively work to ensure good conditions of well-being and employee development?”. In more detail, the relationship between private and public employment and self-reported working skills might be partly related to the different reallocation rates in different units. On the other hand, a recent study [46] underlined that one out five physiotherapists were reallocated in different wards (such as infective wards, pulmonology wards, or intensive care units) during COVID-19 pandemic as a result of clinical PRM departments’ reorganization. Therefore, changes in tasks might significantly affect the operator’s perceived job skills.
Similarly, the positive relation between direct superior care of workers’ well-being and work setting might be strictly linked to the difference in infection risk in physiotherapists called to face the COVID-19 pandemic. It might not be surprising to understand how anxiety and depression might be associated with direct superior commitment to ensure good working conditions. The suggestions and ideas proposed by frontline healthcare workers contribute to the maintenance of appropriate equipment and optimal hygiene protocols in high-risk departments such as intensive care units [47], and generate a feeling of security and motivation that boost the work efficiency and motivation of all the team [48,49]. Therefore, these data highlighted the need for further research focusing on the type of work environment and not just the physiotherapist’s relationship with the work environment [50]. Moreover, the multiple regression showed a consistent correlation of frustration with all of the domains analyzed. However, a total of 16% of the variation in frustration could be explained by the active work of the superior perceived by the therapist. Beyond the degree of raw association of the single predictive values obtained through a sequential multiple regression analysis, we are able to weigh how much a predictor explains a variation of a dependent criterion. In this scenario, the need for continuous improvement of qualifications is essential for the medical professions, and the perception of the usefulness and effectiveness of one’s work is one of the main factors in combating burnout [36].
Physical therapists and all health care workers are among individuals with the highest risk of contracting the virus, considering that they are under an overwhelming psychological pressure, requiring manual contact with patients [35,41,43,48]. It has been proposed that focusing on lack of basic need satisfaction alone may be ineffective in adequately describing how negative work-related social factors impact employees’ psychological needs [17,41]. Indeed, many operational difficulties stemmed from inequalities of role between management and front-line workers. The work frustration by healthcare workers might be more clinically relevant than their work satisfaction in explaining how the COVID-19 pandemic has negatively affected the rehabilitation field. We are aware that learning from this experience could reduce staff distress and improve patient care in case of further waves of this pandemic.
Thus, in the context of the ongoing pandemic, social support could be dominantly viewed as a useful option for an individual to rely on and use as emotional support to cope with traumatic stress [3,4]. Evidence shows that social support is associated with resilience to stress and the reduction of depression and anxiety. Therefore, social support could play a key role in maintaining mental and physical health, not only in health workers but also in the general population [51].
We are aware that the present study is not free from limitations. First, a multiple regression approach would require a larger sample, but a low RMSE ensured the validity of the analysis. Second, the study was unable to distinguish pre-existing mental health symptoms from new symptoms, albeit the different sense of frustration felt in the various waves remains difficult to resolve. Third, it would have been useful to use widespread, standardized, and validated scales, despite that a panel of experts had formulated the online questionnaire that should be reliable for all physiotherapists involved in counteracting this COVID-19 pandemic. Thus, future research is needed to address the above limitations, including the comparison of the presence of anxiety and depression between physical therapists and a control group.
5. Conclusions
Taken together, findings of the C.A.L.A.B.R.I.A. suggest the need to constantly monitor the needs of rehabilitative healthcare workers and to implement tailored psychological intervention programs during the COVID-19 pandemic. In more detail, the variation in the therapist’s frustration seems to be strictly related to the role of medical directors in ensuring a safe environment to reduce burnout in healthcare worker in the rehabilitation field.
Author Contributions
Conceptualization, A.d.S., N.M. and A.A.; Methodology, A.d.S., N.M. and S.R.; Investigation: M.T.I. and A.T.; Formal Analysis: A.d.S., N.M. and A.G.; Writing—Original Draft Preparation, A.d.S. and N.M.; Writing—Review and Editing: L.P., M.I. and A.A.; Visualization, S.R., L.L., M.T.I., A.T., A.G. and A.A. Supervision: A.d.S., M.I. and A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Institutional Review Board.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Attia Y.A., El-Saadony M.T., Swelum A.A., Qattan S.Y., Al-Qurashi A.D., Asiry K.A., Shafi M.E., Elbestawy A.R., Gado A.R., Khafaga A.F., et al. COVID-19: Pathogenesis, advances in treatment and vaccine development and environmental impact—an updated review. Environ. Sci. Pollut. Res. 2021;28:22241–22264. doi: 10.1007/s11356-021-13018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Sire A., Andrenelli E., Negrini F., Patrini M., Lazzarini S.G., Ceravolo M.G., Kiekens C., Arienti C., Ceravolo M.G., Côté P., et al. Rehabilitation and COVID-19: A rapid living systematic review by cochrane rehabilitation field updated as of December 31st, 2020 and synthesis of the scientific literature of 2020. Eur. J. Phys. Rehabil. Med. 2021;57:181–188. doi: 10.23736/S1973-9087.21.06870-2. [DOI] [PubMed] [Google Scholar]
- 3.Demeco A., Marotta N., Barletta M., Pino I., Marinaro C., Petraroli A., Moggio L., Ammendolia A. Rehabilitation of patients post-COVID-19 infection: A literature review. J. Int. Med. Res. 2020;48 doi: 10.1177/0300060520948382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marotta N., Demeco A., Moggio L., Ammendolia A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation. J. Enabling Technol. 2021 doi: 10.1108/JET-11-2020-0047. [DOI] [Google Scholar]
- 5.Curci C., Negrini F., Ferrillo M., Bergonzi R., Bonacci E., Camozzi D.M., Ceravolo C., De Franceschi S., Guarnieri R., Moro P., et al. Functional outcome after inpatient rehabilitation in post-intensive care unit COVID-19 patients: Findings and clinical implications from a real-practice retrospective study. Eur. J. Phys. Rehabil. Med. 2021 doi: 10.23736/S1973-9087.20.06660-5. [DOI] [PubMed] [Google Scholar]
- 6.Carda S., Invernizzi M., Bavikatte G., Bensmaïl D., Bianchi F., Deltombe T., Draulans N., Esquenazi A., Francisco G.E., Gross R., et al. COVID-19 pandemic. What should Physical and Rehabilitation Medicine specialists do? A clinician’s perspective. Eur. J. Phys. Rehabilitation Med. 2020;56:515–524. doi: 10.23736/S1973-9087.20.06317-0. [DOI] [PubMed] [Google Scholar]
- 7.Negrini F., Ferrario I., Mazziotti D., Berchicci M., Bonazzi M., de Sire A., Negrini S., Zapparoli L. Neuropsychological Features of Severe Hospitalized Coronavirus Disease 2019 Patients at Clinical Stability and Clues for Postacute Rehabilitation. Arch. Phys. Med. Rehabil. 2021;102:155–158. doi: 10.1016/j.apmr.2020.09.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferraro F., Calafiore D., Dambruoso F., Guidarini S., de Sire A. COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series. J. Med. Virol. 2021;93:1896–1899. doi: 10.1002/jmv.26717. [DOI] [PubMed] [Google Scholar]
- 9.Vitacca M., Carone M., Clini E.M., Paneroni M., Lazzeri M., Lanza A., Privitera E., Pasqua F., Gigliotti F., Castellana G., et al. Joint Statement on the Role of Respiratory Rehabilitation in the COVID-19 Crisis: The Italian Position Paper. Respiration. 2020;99:493–499. doi: 10.1159/000508399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Margetić B., Peraica T., Stojanović K., Ivanec D. Predictors of emotional distress during the COVID-19 pandemic; a Croatian study. Pers. Individ. Dif. 2021;175:110691. doi: 10.1016/j.paid.2021.110691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minahan J., Falzarano F., Yazdani N., Siedlecki K.L. The COVID-19 Pandemic and Psychosocial Outcomes Across Age Through the Stress and Coping Framework. Gerontologist. 2021;61:228–239. doi: 10.1093/geront/gnaa205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bettger J.P., Thoumi A., Marquevich V., De Groote W., Rizzo Battistella L., Imamura M., Delgado Ramos V., Wang N., Dreinhoefer K.E., Mangar A., et al. COVID-19: Maintaining essential rehabilitation services across the care continuum. BMJ Glob. Heal. 2020;5:e002670. doi: 10.1136/bmjgh-2020-002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Penati R., Begenisic T., Zeni F., DE Sire A., Bernetti A., Fiore P., Nardone A. Impact of COVID-19 pandemic on Physical Medicine and Rehabilitation residency: An Italian nationwide epidemiologic survey. Eur. J. Phys. Rehabil. Med. 2021 doi: 10.23736/S1973-9087.21.06844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koffman J., Gross J., Etkind S.N., Selman L. Uncertainty and COVID-19: How are we to respond? J. R. Soc. Med. 2020;113:211–216. doi: 10.1177/0141076820930665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ditwiler R.E., Swisher L.L., Hardwick D.D. Professional and Ethical Issues in United States Acute Care Physical Therapists Treating Patients With COVID-19: Stress, Walls, and Uncertainty. Phys. Ther. 2021;101 doi: 10.1093/ptj/pzab122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trépanier S.-G., Fernet C., Austin S. Longitudinal relationships between workplace bullying, basic psychological needs, and employee functioning: A simultaneous investigation of psychological need satisfaction and frustration. Eur. J. Work. Organ. Psychol. 2016;25:690–706. doi: 10.1080/1359432X.2015.1132200. [DOI] [Google Scholar]
- 18.Collantoni E., Saieva A., Meregalli V., Girotto C., Carretta G., Boemo D., Bordignon G., Capizzi A., Contessa C., Nesoti M., et al. Psychological Distress, Fear of COVID-19, and Resilient Coping Abilities among Healthcare Workers in a Tertiary First-Line Hospital during the Coronavirus Pandemic. J. Clin. Med. 2021;10:1465. doi: 10.3390/jcm10071465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic Stress in Healthcare Workers During COVID-19 Pandemic: A Review of the Immediate Impact. Front. Psychol. 2020;11:569935. doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spoorthy M.S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panzeri A., Rossi Ferrario S., Cerutti P. Psychological Differences Among Healthcare Workers of a Rehabilitation Institute During the COVID-19 Pandemic: A Two-Step Study. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.636129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rieckert A., Schuit E., Bleijenberg N., Ten Cate D., De Lange W., De Man-Van Ginkel J.M., Mathijssen E., Smit L.C., Stalpers D., Schoonhoven L., et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-043718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gómez-Salgado J., Domínguez-Salas S., Romero-Martín M., Ortega-Moreno M., García-Iglesias J.J., Ruiz-Frutos C. Sense of coherence and psychological distress among healthcare workers during the COVID-19 pandemic in Spain. Sustainability. 2020;12:6855. doi: 10.3390/su12176855. [DOI] [Google Scholar]
- 24.Weaver M.S., Rosenberg A.R., Fry A., Shostrom V., Wiener L. The Impact of the Coronavirus Pandemic on Pediatric Palliative Care Team Structures, Services, and Care Delivery. J. Palliat. Med. 2020;24:1213–1220. doi: 10.1089/jpm.2020.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nikčević A.V., Marino C., Kolubinski D.C., Leach D., Spada M.M. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J. Affect. Disord. 2021;279:578–584. doi: 10.1016/j.jad.2020.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bennett P., Noble S., Johnston S., Jones D., Hunter R. COVID-19 confessions: A qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open. 2020;10:e043949. doi: 10.1136/bmjopen-2020-043949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duarte H., Daros Vieira R., Cardozo Rocon P., Andrade A.C.D.S., Wittmer V.L., Capellini V.K., Soares S.C.S., Paro F.M. Factors associated with Brazilian physical therapists’ perception of stress during the COVID-19 pandemic: A cross-sectional survey. Psychol. Heal. Med. 2021;25:1–12. doi: 10.1080/13548506.2021.1875133. [DOI] [PubMed] [Google Scholar]
- 28.Baert S., Lippens L., Moens E., Sterkens P., Weytjens J. The COVID-19 Crisis and Telework: A Research Survey on Experiences, Expectations and Hopes. [(accessed on 23 July 2021)];IZA Discuss. Pap. 2005 doi: 10.1007/s10198-021-01392-z. Available online: https://www.iza.org/publications/dp/13229/the-covid-19-crisis-and-telework-a-research-survey-on-experiences-expectations-and-hopes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Likert R. A technique for the measurement of attitudes. Arch. Psychol. 1932;140:55. [Google Scholar]
- 30.Choi J., Peters M., Mueller R.O. Correlational analysis of ordinal data: From Pearson’s r to Bayesian polychoric correlation. Asia Pacific Educ. Rev. 2010;11:459–466. doi: 10.1007/s12564-010-9096-y. [DOI] [Google Scholar]
- 31.Croux C., Dehon C. Influence functions of the Spearman and Kendall correlation measures. Stat. Methods Appl. 2010;19:497–515. doi: 10.1007/s10260-010-0142-z. [DOI] [Google Scholar]
- 32.Plonsky L., Ghanbar H. Multiple Regression in L2 Research: A Methodological Synthesis and Guide to Interpreting R2 Values. Mod. Lang. J. 2018;102:713–731. doi: 10.1111/modl.12509. [DOI] [Google Scholar]
- 33.Jeong Y., Jung M.J. Application and interpretation of hierarchical multiple regression. Orthop. Nurs. 2016;35:338–341. doi: 10.1097/NOR.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 34.Serrão C., Duarte I., Castro L., Teixeira A. Burnout and depression in portuguese healthcare workers during the covid-19 pandemic—the mediating role of psychological resilience. Int. J. Environ. Res. Public Health. 2021;18:636. doi: 10.3390/ijerph18020636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farì G., de Sire A., Giorgio V., Rizzo L., Bruni A., Bianchi F.P., Zonno A., Pierucci P., Ranieri M., Megna M. Impact of COVID-19 on the mental health in a cohort of Italian rehabilitation healthcare workers. J Med. Virol. 2021 doi: 10.1002/jmv.27272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pniak B., Leszczak J., Adamczyk M., Rusek W., Matosz P., Guzik A. Occupational burnout among active physiotherapists working in clinical hospitals during the COVID-19 pandemic in south-eastern Poland. Work. 2021;68:285–295. doi: 10.3233/WOR-203375. [DOI] [PubMed] [Google Scholar]
- 37.Alemanno F., Houdayer E., Parma A., Spina A., Del Forno A., Scatolini A., Angelone S., Brugliera L., Tettamanti A., Beretta L., et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID rehabilitation unit experience. PLoS ONE. 2021;16:e0246590. doi: 10.1371/journal.pone.0246590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Puchner B., Sahanic S., Kirchmair R., Pizzini A., Sonnweber B., Wöll E., Mühlbacher A., Garimorth K., Dareb B., Ehling R., et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: An observational cohort study. Eur. J. Phys. Rehabil. Med. 2021;57 doi: 10.23736/S1973-9087.21.06549-7. [DOI] [PubMed] [Google Scholar]
- 39.Yang S., Kwak S.G., Ko E.J., Chang M.C. The mental health burden of the covid-19 pandemic on physical therapists. Int. J. Environ. Res. Public Health. 2020;17:3723. doi: 10.3390/ijerph17103723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muhammad D.G., Musa J.S. Impact of the corona virus disease 2019 pandemic on physiotherapy services in Nigeria. J. Heal. Res. 2021;35:369–373. doi: 10.1108/JHR-09-2020-0433. [DOI] [Google Scholar]
- 42.Fava G.A., McEwen B.S., Guidi J., Gostoli S., Offidani E., Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 43.Simonelli C., Paneroni M., Fokom A.G., Saleri M., Speltoni I., Favero I., Garofali F., Scalvini S., Vitacca M. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: An experience from Northern Italy. Monaldi Arch. Chest Dis. 2020;90:292–298. doi: 10.4081/monaldi.2020.1085. [DOI] [PubMed] [Google Scholar]
- 44.Snowdon D.A., Cooke S., Lawler K., Scroggie G., Williams K., Taylor N.F. Physiotherapists prefer clinical supervision to focus on professional skill development: A qualitative study. Physiother. Canada. 2020;72:249–257. doi: 10.3138/ptc-2019-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Snowdon D.A., Leggat S.G., Harding K.E., Scroggie G., Hau R., Darzins P., Taylor N.F. Direct supervision of physiotherapists improves compliance with clinical practice guidelines for patients with hip fracture: A controlled before-and-after study. Disabil. Rehabil. 2020;42:3825–3832. doi: 10.1080/09638288.2019.1610805. [DOI] [PubMed] [Google Scholar]
- 46.Gianola S., Bargeri S., Campanini I., Corbetta D., Gambazza S., Innocenti T., Meroni R., Castellini G., Turolla A. The Spread of COVID-19 Among 15,000 Physical Therapists in Italy: A Cross-Sectional Study. Phys. Ther. 2021;101 doi: 10.1093/ptj/pzab123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Varona J.F., Madurga R., Peñalver F., Abarca E., Almirall C., Cruz M., Ramos E., Castellano Vázquez J.M. Seroprevalence of SARS-CoV-2 antibodies in over 6000 healthcare workers in Spain. Int. J. Epidemiol. 2021;50:400–409. doi: 10.1093/ije/dyaa277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Theorell T. COVID-19 and Working Conditions in Health Care. Psychother. Psychosom. 2020;89:193–194. doi: 10.1159/000507765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cao J., Wei J., Zhu H., Duan Y., Geng W., Hong X., Jiang J., Zhao X., Zhu B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020;89:252–254. doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alkassabi O.Y., Al-Sobayel H., Al-Eisa E.S., Buragadda S., Alghadir A.H., Iqbal A. Job satisfaction among physiotherapists in Saudi Arabia: Does the leadership style matter? BMC Health Serv. Res. 2018;18:422. doi: 10.1186/s12913-018-3184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hou T., Zhang T., Cai W., Song X., Chen A., Deng G., Ni C. Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS ONE. 2020;15:e0233831. doi: 10.1371/journal.pone.0233831. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.