Abstract
Previously, we demonstrated an 81% reduction in pediatric Emergency Room (ER) visits in Italy during the strict lockdown due to the SARS-CoV-2 pandemic. Since May 2020, lockdown measures were relaxed until 6 November 2020, when a strict lockdown was patchily reintroduced. Our aim was to evaluate the impact of the relaxed lockdown on pediatric ER visits in Italy. We performed a retrospective multicenter study involving 14 Italian pediatric ERs. We compared total ER visits from 24 September 2020 to 6 November 2020 with those during the corresponding timeframe in 2019. We evaluated 17 ER specific diagnoses grouped in air communicable and non-air communicable diseases. We recognized four different triage categories: white, green, yellow and red. In 2020 total ER visits were reduced by 51% compared to 2019 (16,088 vs. 32,568, respectively). The decrease in air communicable diseases was significantly higher if compared to non-air communicable diseases (−64% vs. −42%, respectively). ER visits in each triage category decreased in 2020 compared to 2019, but in percentage, white and red codes remained stable, while yellow codes slightly increased and green codes slightly decreased. Our results suggest that preventive measures drastically reduced the circulation of air communicable diseases even during the reopening of social activities but to a lesser extent with regard to the strict lockdown period (March–May 2020).
Keywords: air communicable infections, emergency rooms, social activities reopening, lockdown measures, pediatric, pandemic, SARS-CoV-2, COVID-19
1. Introduction
The first cases of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) were described in China in December 2019 and the WHO declared a pandemic on 11 March 2020 [1]. The first Italian case was described in February 2020. Since that date, a total of 4,515,967 cases and 128,362 deaths (2.8%) were reported in Italy, with a median age of 46 years [2]. Until 25 August 2021, 711,898 (15.9%) pediatric cases were reported in Italy, with 31 fatalities [2].
In order to face this pandemic spread, the Italian Prime Minister declared a strict lockdown on 9 March 2020 [3]. Bans of mass gatherings, social distancing and the obligation of wearing face masks starting at six years of age were introduced. Moreover, simple hygiene measures, such as hand washing, were implemented. Mass closures followed, including schools, factories, pubs, shopping centers and restaurants. Only supermarkets remained open, providing daily necessities. Workers were encouraged to use smart-working. Breaking the quarantine was allowed only in case of extreme necessities. These preventive measures were operative until 3 May 2020, when they were relaxed [4]: factories, shopping malls, pubs and restaurants were reopened, while schools remained closed. People were allowed to leave their home and take summer holidays. From 14 September 2020 to 24 September 2020, schools were reopened in Italy [5], implementing the environmental and surveillance measures in order to face the in-school transmission. The obligation to wear face masks, handwashing and bans of mass gatherings were highlighted as cornerstones in order to prevent the spread of SARS-CoV-2 in children and, consequently, from children to adults [5].
In a previous Italian epidemiologic study including 15 hospitals over eight Italian regions, we showed an 81% decrease in pediatric Emergency Room (ER) visits during March–May 2020 compared to the corresponding timeframes in 2019, with the largest drop affecting air communicable diseases [6]. The drastic preventive measures applied during the strict lockdown can explain these results [6]. It would be useful to know what happened when more permissive measures were applied.
In this multicentric study, our aim was the evaluation of how the SARS-CoV-2 preventive strategies, such as social distancing, face masks and hygiene measures, affected pediatric ER visits when lockdown measures were relaxed, allowing the reopening of social activities in Italy. We compared ER visit rates, specific ER diagnoses and triage categories from 24 September 2020 to 6 November 2020 with the corresponding timeframe in 2019.
2. Materials and Methods
We performed a retrospective multicentric study involving 14 Italian pediatric ERs, from northern to southern Italy (Figure 1). We randomly selected 14 public hospitals throughout Italy, thus providing a representative sample of the entire Italian population. We collected data from ERs located in Ancona, Bergamo, Bologna, Catania, Foligno, Frosinone, Latina, Milan, Naples, Rome and Trieste, which represented about 10% of the total pediatric ERs visits per year in Italy [6].
Figure 1.
Pediatric Emergency Rooms (ERs) included in the study.
We compared two corresponding timeframes in 2019 and 2020, starting from 24 September. In Italy, schools were opened patchily in the different regions, because each region itself decided the dates in which they should be reopened. The reopenings started from the first days of September and continued until 24 September. In order to avoid confounding factors, we decided to start our analysis on 24 September 2020, when schools were opened throughout the national territory. For the same reason, we decided to stop our analysis on 6 November 2020 because, since that date, a new legislation was adopted in Italy, establishing a further differentiation between Italian regions based on their pandemic critical features. The classification assigned different colors to each region, indicating its SARS-CoV-2 pandemic background, from the least to the most severe: white, yellow, orange and red. These different features determined different strict lockdown measures, such as different curfew times, obligation to wear face masks outdoors, the opening of restaurants and shopping centers and different social activities proceedings, from their complete closure to their opening.
Firstly, we compared these two reference periods in terms of total visits in the 14 pediatric ERs participating in the study. Subsequently, consistent with our previous study [6], we evaluated 17 ER specific diagnoses, based on the primary discharge diagnoses ruled out in ER according to the ICD9-CM codes. These diagnoses were grouped into air communicable and non-air communicable diseases [6]. In the group of air communicable diseases, we included upper and lower respiratory infections, gastroenterological infections and exanthematous diseases, and we assumed that these conditions were related to airborne transmission. Non-air communicable diseases included accidents, cardiovascular, dermatological diseases, endocrinological disorders, fever and surgical pathologies, as well as hematological, nephrological, neurological, neuropsychiatric, oncological, ophthalmological and rheumatological diseases, because we assumed that these conditions were not related to airborne transmission. Fever was included in this second category because, if it occurs without any other signs or symptoms, it is more likely related to non-airborne infections, such as urinary tract infections. In order to better understand our analysis, we also investigated the trend in respiratory diseases alone compared to the other 16 specific diagnoses evaluated in this study.
Similarly, we recognized four different triage categories, from the least to the most severe: white, green, yellow, and red, which were standardized combining the orange and blue codes as yellow codes, as previously described [6]. In fact, since 2019 some regions, including Lazio, adopted new triage colors and defined five new triage categories with different priority codes: red (immediate access), orange (access in 15 min), blue (access in 60 min), green (access in 120 min) and white (access in 240 min). To standardize our data, we combined the orange and blue codes as yellow codes.
We performed our statistical analysis using IBM SPSS Statistics v.25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). We compared the ER visits rates, ER specific diagnoses in terms of air communicable diseases and non-air communicable diseases and triage categories in 2019 vs. 2020 by chi-square tests. A p-value < 0.05 was considered statistically significant.
3. Results
We collected data from 14 Italian pediatric ERs, from 24 September to 6 November, 2019 and 2020: Umberto I hospital, Rome (2901 vs. 1338); San Camillo de Lellis hospital, Rome (1587 vs. 711); Sant’Eugenio hospital, Rome (591 vs. 222); Santa Maria Goretti hospital, Latina (643 vs. 283); Vittorio Emanuele hospital, Catania (874 vs. 374); San Paolo hospital, Milan (1489 vs. 720); Burlo Garofalo hospital, Trieste (3041 vs. 1894); Ponte San Pietro hospital, Bergamo (1297 vs. 481); Papa Giovanni XXIII hospital, Bergamo (1952 vs. 864); Santobono-Pausilipon hospital, Naples (11,062 vs. 5032); Sant’Orsola hospital, Bologna (2709 vs. 1941); Fabrizio Spaziani hospital, Frosinone (1323 vs. 527); San Giovanni Battista hospital, Foligno (625 vs. 253); and Gaspare Salesi hospital, Ancona (2474 vs. 1448).
Comparing total ER visits from 24 September to 6 November 2020, with those from 24 September to 6 November 2019, we observed a reduction rate of 51% (32,568 vs. 16,088 visits, respectively) (p < 0.001) (Table 1).
Table 1.
ER visits registered in September–November, 2019 and 2020.
| Hospital | 2019 | 2020 | p-Value | |
|---|---|---|---|---|
| Umberto I–Rome | 2901 | 1338 | −54% | p < 0.001 |
| San Camillo de Lellis–Rome | 1587 | 711 | −55% | |
| Sant’Eugenio–Rome | 591 | 222 | −52% | |
| Santa Maria Goretti–Latina | 643 | 283 | −56% | |
| Vittorio Emanuele–Catania | 874 | 374 | −57% | |
| San Paolo–Milan | 1489 | 720 | −52% | |
| Burlo Garofalo–Trieste | 3041 | 1894 | −38% | |
| Ponte San Pietro–Bergamo | 1297 | 481 | −63% | |
| Papa Giovanni XXIII–Bergamo | 1952 | 864 | −56% | |
| Santobono-Pausilipon–Naples | 11,062 | 5032 | −54% | |
| Sant’Orsola–Bologna | 2709 | 1941 | −28% | |
| Fabrizio Spaziani–Frosinone | 1323 | 527 | −60% | |
| San Giovanni Battista–Foligno | 625 | 253 | −60% | |
| Gaspare Salesi–Ancona | 2474 | 1448 | −41% | |
| TOTAL | 32,568 | 16,088 | −51% |
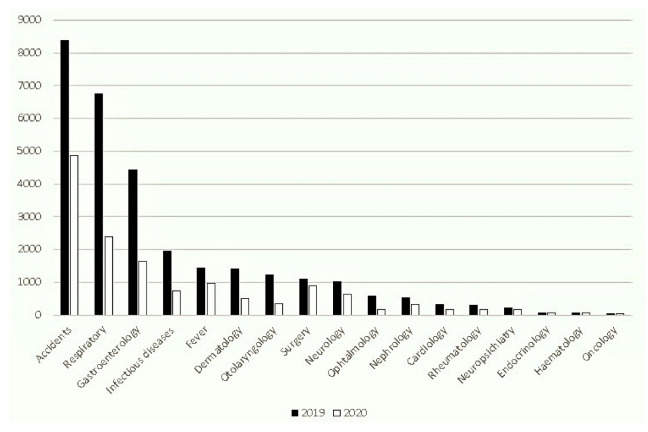
We encountered a significant reduction in visits for all 17 clinical categories evaluated in the 2020 period compared to 2019 (Figure 2).
Figure 2.
Pediatric ER diagnoses in September–November, 2019 and 2020.
Nevertheless, for some categories, such as accidents, we observed a relative increase in percentage when compared to the total number of visits per reference period (Figure 3).
Figure 3.
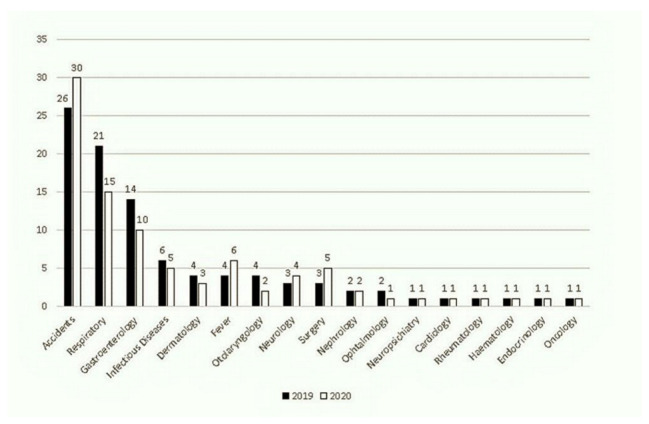
Proportion of pediatric ER diagnoses in September–November, 2019 and 2020.
The decrease in air communicable diseases (13,134 vs. 4754: −63.8%) was significantly higher compared to non-air communicable diseases (19,434 vs. 11,334: −41.7%) (p < 0.001). Analyzing respiratory diseases alone, we found a statistical significantly decrease in respiratory diseases (6743 vs. 2393, −4%) compared to the total amount of the others 16 specific diagnoses evaluated in this study (25,296 vs. 11,667, +4%) (p < 0.001).
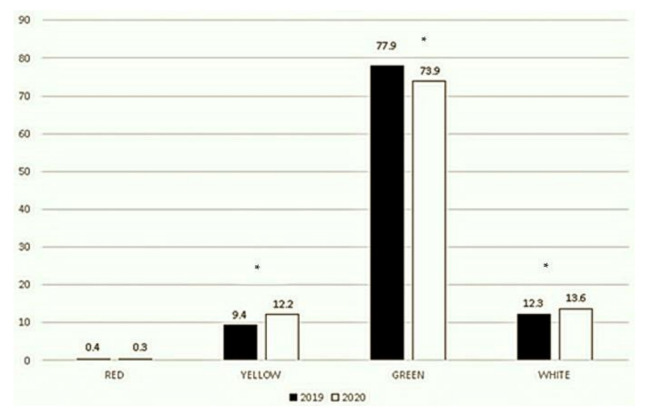
ER visits in each triage category decreased in 2020. Our data showed 118 vs. 43 red codes, 3083 vs. 1954 yellow codes, 25,369 vs. 11,898 green codes, and 3998 vs. 2189 white codes in 2019 vs. 2020, respectively. By contrast, considering the proportion of each category over the total number of visits per reference period, the red codes remained almost similar (0.4% vs. 0.3%, p = 0.85), while the yellow codes increased (9.4% vs. 12.2%, p < 0.001), green codes decreased (77.9% vs. 73.9%, p < 0.001), and white codes slightly increased (12.3% vs. 13.6%, p < 0.001) (Figure 4).
Figure 4.
Triage categories in September–November, 2019 and 2020. This figure shows the breakdown of 100% of ER visits into 4 codes. * p < 0.001.
4. Discussion
In our study, evaluating 14 Italian hospitals that are a representative sample of the whole Italian population, the most important result is that total pediatric ER visits dropped by 51% from 24 September to 6 November 2020, compared to the corresponding timeframe in 2019. After demonstrating a significant reduction of ER visits during the strict lockdown (9 March to 3 May 2020) in our previous manuscript [6], we rolled out this study in order to assess the effect of relaxed preventing restrictions, such as social activities reopening. We found a significantly lower drop in ER visits in September–November 2020 compared to March–May 2020 (−51% vs. −81%, respectively). Our results are supported by other studies that have demonstrated a drastic fall in ER visits both in children and in adults [6,7,8,9,10,11,12,13]. This drop can be explained by the preventive measures adopted in Italy, such as social-distancing measures, the use of face masks, hand washing and bans of mass gatherings, which may have contributed to the reduction of the spread of both SARS-CoV-2 and other acute communicable diseases, the most common ER presentations in children along with accidents [6,7]. Moreover, in the present study, we confirmed the reduction in all 17 clinical categories, regarding both air communicable and non-air communicable diseases, but similarly to above, the reduction of air communicable diseases was significantly lower in September–November 2020 when compared to March–May 2020 (−64% vs. −88.5%, respectively). We can speculate that the reopening of social activities, with the mitigation of lockdown measures in May 2020 and in particular the reopening of schools in September 2020, at least partially allowed the circulation of air communicable diseases. Our speculations are supported by other studies that have demonstrated an increase in air communicable diseases’ diffusion after the mitigation of lockdown, both in children and in adults [14,15,16]. By contrast, during the strict lockdown, air communicable diseases’ diffusion was really reduced [6,16,17,18,19,20], leading to a drastic drop in ER visits [9,10,11,13], as we have already demonstrated in our previous study [6]. These results highlight the importance of preventive measures in order to face acute communicable diseases’ diffusion, in particular in pediatric age, because several studies have shown that children are at higher risk of infections [17,18,21] and are pivotal in air communicable diseases’ transmission [22]. Our preliminary data, analyzing a one year surveillance period from March 2020 to February 2021, showed that RSV and other viruses (including influenza virus A and B, human coronavirus OC43, 229E, NL-63 and HUK1, adenovirus, parainfluenza virus 1-3, human bocavirus and human metapneumovirus) almost disappeared, while human rhinovirus (hRV) was the only detected virus. In fact, evaluating 86 hospitalized children, we found hRV in 41, RSV in 4 and other viruses in 1. Interestingly, hRV did not show a peak in spring 2020 as the other epidemic seasons, but in autumn–winter 2020, it was the one detected in hospitalized children, showing a spread trend comparable to other epidemic seasons. Thus, the relatively low efficacy of surgical masks, along with hRV features and the reduced social distancing in social activities, allowed the circulation of the virus.
Every year in Italy, approximately 3 million children are admitted to ERs [23]. Approximately 0.5–1% are classified as red codes and 10–12% as yellow codes, meaning that approximately 20,000–30,000 children seek medical advice for life-threatening clinical conditions and about 300,000 children present with serious conditions each year. Nevertheless, approximately 70–80% of ER visits are categorized as green codes. This considerable number of non-urgent patients with acute clinical conditions, which could be used to treat with in an outpatient setting, has necessarily led to the well-known and harmful overcrowding of ER departments [23]. Evaluating triage categories, we demonstrated a consistent reduction in all ER visits. This reduction goes along with the reduction in the spread of air communicable diseases [6,7] and in outdoor accidents [6], which represent the most frequent clinical presentations in pediatric ERs. Moreover, we cannot rule out that parents’ fear of SARS-CoV-2 [6,8,9,24,25] and the strict measures adopted in Italy [6,8,26] have contributed to this reduction. Another interesting result that came out comparing our two studies was that in both reference periods, yellow codes increased, and green codes decreased compared to their corresponding timeframes in 2019 but, in September–November 2020, yellow codes increased, and green codes decreased to a lesser extent than March–May 2020, when lockdown measures were more stringent (yellow codes: +11.1% vs. +2.8%; green codes: −10.8% vs. −4%, respectively) [6]. These results may highlight that a lesser sense of fear concerning SARS-CoV-2 [27] and more organized primary cares have limited the number of patients that delayed their ER visits, in contrast to what happened during the first wave of pandemic [28,29,30,31,32]. In particular, a more intense sense of fear was demonstrated in people living in high-death-rate countries with strict lockdown measures [26]. Thus, the mitigation of lockdown measures could have led people to have a lesser sense of fear in respect to SARS-CoV-2, avoiding delayed ER visits.
An interesting result came out analyzing the trend in ER visits for accidents considering the strict and the relaxed lockdown period. Accidents, together with air communicable diseases, typically represent the main clinical presentation in pediatric ERs [6,7]. In our previous work, comparing the strict lockdown period (March–May 2020) with the same period in 2019, we demonstrated 11148 ER visits for accidents in 2019 compared to 3380 in 2020 (−70%) [6]. Our results were superimposable on other studies that reported reductions in injuries in pediatric age in UK, Germany, Belgium, France, Italy, USA, South Africa and Singapore [13,17,33,34,35,36,37]. Along this hypothesis, several studies demonstrated a drastic drop in pediatric ER visits for accidents during the lockdown period [6,38,39]. This decreasing trend is confirmed also by more recent published works that analyzed different timeframes, in particular until June [40] and August [41] 2020, when strict lockdown measures were patchily reintroduced. In the present work, analyzing ER visits in September–November 2020, we confirm this decreasing trend in accidents even when lockdown measures were relaxed, allowing several social activities reopening, such as schools. In fact, we found 8384 ER visits for accidents in September–November 2019 compared to 4871 in the same timeframe in 2020 (−42%). We can compare accident visits during the strict lockdown and relaxed lockdown period. Interestingly, we found 3380 vs. 4871 accident visits (+31%) [6]. We can speculate that, during the strict lockdown, the increased parental supervision and the school, sport activities and playground closures may have played a pivotal role in the reduction of accidental injuries [42]. However, when strict measures were relaxed, the increase in opportunities for trauma led to an increase in accidents visits. On the other hand, we cannot forget that the home environment remains a frequent place for accidents in children [43,44]. In fact, we found a marked increase in the proportion of injuries both during the strict [6] and relaxed lockdown periods.
An important decision that was made during the relaxed lockdown was the reopening of schools. In fact, an important effect of the SARS-CoV-2 pandemic was school closure that affected thousands of children worldwide for about one year. By 26 April 2020, the United Nations Education, Scientific and Cultural Organization (UNESCO) estimated that 1,451,874,449 learners were affected globally. Thus, is school closure beneficial? It is known that the SARS-CoV-2 infection in children is mostly a mild disease [45]. However, we cannot forget that children are susceptible in any case to the infection and then they can spread the virus [46,47]. The mild clinical presentation arises concerns about in-school transmission, as children are seen as super spreaders. Several studies highlighted that child contribute minimally to SARS-CoV-2 growth rates [48,49,50,51,52,53,54]. The opening of schools may be considered safe where there is low SARS-CoV-2 background prevalence. In fact, several data indicate that adults play a crucial role in spreading the virus to their households [55,56] and that in-school SARS-CoV-2 transmission depends on local background prevalence [57,58]. Thus, improving preventing measures (such as decreasing class sizes, organizing different timetables, holding lessons outdoors, physical distancing, hygiene measures, face masks and the obligation to stay at home when sick) are crucial to minimizing the risk of in-class transmission [46,47,59,60]. It is important to remember that social activities closures can lead to potential harmful consequences for the school-aged population and their families, concerning obesity and malnutrition, immunization rates, domestic violence and child abuse [57], delays or precocity in cognitive, physical or social growth, later diagnoses of developmental conditions and overall health inequity [61,62,63,64,65,66]. Thus, school closures should be correctly assessed balancing the risk/benefit ratio, protecting, on the one side, the child health and, on the other side, their crucial growth milestones.
This study has some limitations. Social distancing or other preventive strategies were not directly measured in order to evaluate their contribution in reducing the spread of SARS-CoV-2 and other air communicable infections. We did not investigate the parents’ feelings about keeping their children at home in spite of medical problems due to the fear of the pandemic. We focused the analysis on a period in which lockdown measures were relaxed, and we assumed that these measures, such as social distancing, face masks and hand washing, were followed.
5. Conclusions
Our results suggest that preventive measures, such as face masks, social distancing and simple hygiene measures, were associated with a reduction in air communicable diseases’ spread even during the reopening of social activities and schools in particular but to a lesser extent with respect to the lockdown period (March–May 2020).
The slight percentage increase in yellow codes and the slight percentage decrease in green codes in September–November 2020 compared to lockdown period may indicate an improvement in primary cares and, consequently, a reduction of delayed visits at pediatric ERs.
Acknowledgments
CICERO Group: Angela Amoroso, Teresa Agovino, Silvia Bloise, Stefania Bolognini, Giulia Cantiello, Ilaria Corsini, Luisa Cortellazzo Wiel, Carolina D’Anna, Fabiana De Stasio, Cristina Di Lillo, Francesco Maria Di Ubaldo, Chiara Gianfelici, Marzia Mandelli, Alessia Marcellino, Maria Claudia Meli, Iolanda Parente, Claudia Pellegrinelli, Laura Petrarca, Federica Roccabella, Sara Santarelli, Paola Silvestri and Stranges Anna. All members of the CICERO group declare no conflict of interest.
Author Contributions
Conceptualization, L.M., R.N. and F.M.; data curation, L.M., F.A.M., G.B., M.C. (Mauro Calvani), M.C. (Matteo Calvi), G.C., R.F., R.G., A.K., M.L., R.L., B.M., A.A.N. and V.T.; formal analysis, L.M. and R.N.; methodology, L.M., R.N. and F.M.; project administration, L.M. and F.M.; supervision, L.M., R.N. and F.M.; writing—original draft, L.M.; writing—review and editing, L.M., R.N., F.A.M., G.B., M.C. (Mauro Calvani), M.C. (Matteo Calvi), G.C., R.F., R.G., A.K., M.L., R.L., B.M., A.A.N., V.T. and F.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO Director—General’s Openings Remarks at the Media Briefing on COVID-19. Mar 11, 2020. [(accessed on 29 August 2021)]. Available online: https://www.who.int/director-general/speeches/detail/whodirector-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Istituto Superiore di Sanità. Epicentro. Epidemia COVID-19. [(accessed on 29 August 2021)]. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard.
- 3.Decreto del Presidente del Consiglio dei Ministri. Mar 9, 2020. [(accessed on 29 August 2021)]. Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg.
- 4.Decreto del Presidente del Consiglio dei Ministri. Apr 26, 2020. [(accessed on 29 August 2021)]. Available online: https://www.gazzettaufficiale.it/eli/id/2020/04/27/20A02352/sg.
- 5.Decreto del Presidente del Consiglio dei Ministri. Aug 7, 2020. [(accessed on 29 August 2021)]. Available online: https://www.gazzettaufficiale.it/eli/id/2020/08/08/20A04399/sg.
- 6.Matera L., Nenna R., Rizzo V., Ardenti Morini F., Banderali G., Calvani M., Calvi M., Cozzi G., Fabiani E., Falsaperla R., et al. SARS-CoV-2 Pandemic Impact on Pediatric Emergency Rooms: A Multicenter Study. Int. J. Environ. Res. Public Health. 2020;17:8753. doi: 10.3390/ijerph17238753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H., Yu G., Duan H., Fu J., Shu Q. Changes in Children’s Healthcare Visits During Coronavirus Disease-2019 Pandemic in Hangzhou, China. J. Pediatr. 2020;224:146–149. doi: 10.1016/j.jpeds.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ojetti V., Covino M., Brigida M., Petruzziello C., Saviano A., Migneco A., Candelli M., Franceschi F. Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone? Medicina. 2020;56:512. doi: 10.3390/medicina56100512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casalino E., Choquet C., Bouzid D., Peyrony O., Curac S., Fontaine J.P., Plaisance P., Chauvin A., Ghazali D.A. Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study. Int. J. Environ. Res. Public Health. 2020;17:8302. doi: 10.3390/ijerph17228302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baum A., Schwartz M.D. Admissions to Veterans Affairs Hospitals for Emergency Conditions During the COVID-19 Pandemic. JAMA. 2020;324:96. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS England A&E Attendances and Emergency Admissions 2019–2020: Adjusted Monthly. A&E Time Series. 2020. [(accessed on 12 April 2021)]. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-andactivity/ae-attendances-and-emergency-admissions-2019-20/
- 12.Castagneto-Gissey L., Casella G., Russo M.F., Del Corpo G., Iodice A., Lattina I., Ferrari P., Iannone I., Mingoli A., La Torre F. Impact of COVID-19 outbreak on emergency surgery and emergency department admissions: An Italian level 2 emergency department experience. BJS. 2020;107:e374–e375. doi: 10.1002/bjs.11813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dopfer C., Wetzke M., Scharff A.Z., Mueller F., Dressler F., Baumann U., Sasse M., Hansen G., Jablonka A., Happle C. COVID-19 related reduction in pediatric emergency healthcare utilization—A concerning trend. BMC Pediatr. 2020;20:427. doi: 10.1186/s12887-020-02303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poole S., Brendish N.J., Tanner A.R., Clark T.W. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir. Med. 2020;8:e92–e93. doi: 10.1016/S2213-2600(20)30502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh C.C., Lin C.H., Wang W.Y.C., Pauleen D.J., Chen J.V. The outcome and implications of public precautionary measures in Taiwan—Declining respiratory disease cases in the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17:4877. doi: 10.3390/ijerph17134877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haapanen M., Renko M., Artama M., Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children—A nationwide register study in Finland. EClinicalMedicine. 2021;34:100807. doi: 10.1016/j.eclinm.2021.100807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Angoulvant F., Ouldali N., Yang D.D., Filser M., Gajdos V., Rybak A., Guedj R., Soussan-Banini V., Basmaci R., Lefevre-Utile A., et al. Coronavirus disease 2019 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections—A time series analysis. Clin. Infect. Dis. 2021;72:319. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McBride J.A., Eickhoff J., Wald E.R. Impact of COVID-19 quarantine and school cancelation on other common infectious diseases. Pediatr. Infect. Dis. J. 2020;39:e449–e452. doi: 10.1097/INF.0000000000002883. [DOI] [PubMed] [Google Scholar]
- 19.Olsen S.J., Azziz-Baumgartner E., Budd A.P., Brammer L., Sullivan S., Pineda R.F., Cohen C., Fry A.M. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. Morb. Mortal. Wkly. Rep. 2020;69:1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuitunen I., Haapanen M., Artama M., Renko M. Closing Finnish schools and day care centres had a greater impact on primary care than secondary care emergency department visits. Acta Paediatr. 2020;110:937–938. doi: 10.1111/apa.15646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Louhiala P.J., Jaakkola N., Ruotsalainen R., Jaakkola J.J. Form of day care and respiratory infections among Finnish children. Am. J. Public Health. 1995;85:1109–2212. doi: 10.2105/AJPH.85.8_Pt_1.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cauchemez S., Ferguson N.M., Wachtel C., Tegnell A., Saour G., Duncan B., Nicoll A. Closure of schools during an influenza pandemic. Lancet Infect. Dis. 2009;9:473–481. doi: 10.1016/S1473-3099(09)70176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panuccio A., Pinto L., Urbino A., Lubrano R., Guidi B., Zampogna S., Cantoni B. I Nuovi Modelli di Triage; Proceedings of the XII National Congress, Società Italiana di Medicina di Emergenza ed Urgenza Pediatrica (SIMEUP); Padova, Italy. 27–29 October 2016. [Google Scholar]
- 24.Mauro V., Lorenzo M., Paolo C., Sergio H. Correction to: Treat all COVID 19-positive patients, but do not forget those negative with chronic diseases. Intern. Emerg. Med. 2020;15:787–790. doi: 10.1007/s11739-020-02395-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hautz W.E., Sauter T.C., Exadakytlos A.K., Krummrey G., Schauber S., Müller M. Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality—A retrospective study from a Swiss university hospital. Swiss Med. Wkly. 2020;150:20331. doi: 10.4414/smw.2020.20331. [DOI] [PubMed] [Google Scholar]
- 26.Remuzzi A., Remuzzi G. COVID-19 and Italy: What next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo Coco G., Gentile A., Bosnar K., Milovanoviic I., Bianco A., Drid P., Pišot S. A Cross-Country Examination on the Fear of COVID-19 and the Sense of Loneliness during the First Wave of COVID-19 Outbreak. Int. J. Environ. Res. Public Health. 2021;18:2586. doi: 10.3390/ijerph18052586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lynn R.M., Avis J.L., Lenton S., Amin-Chowdhury Z., Ladhani S.N. Delayed access to care and late presentations in children during the COVID-19 pandemic: A snapshot survey of 4075 paediatricians in the UK and Ireland. Arch. Dis. Child. 2020;106:e8. doi: 10.1136/archdischild-2020-319848. [DOI] [PubMed] [Google Scholar]
- 30.Jeffery M.M., D’Onofrio G., Paek H., Platts-Mills T.F., Soares W.E., Hoppe J.A., Genes N., Nath B., Melnick E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401. doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 32.Isba R., Edge R., Jenner R., Broughton E., Francis N., Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020;105:704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 33.Akuaake L.M., Hendrikse C., Spittal G., Evans K., Van Hoving D.J. Cross-sectional study of paediatric case mix presenting to an emergency centre in Cape Town, South Africa, during COVID-19. BMJ Paediatr. Open. 2020;4:e000801. doi: 10.1136/bmjpo-2020-000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ciofi Degli Atti M.L., Campana A., Muda A.O., Concato C., Ravà L., Ricotta L., Reale A., Barbieri M., D’Argenio P., Lancella L., et al. Facing SARS-CoV-2 Pandemic at a COVID-19 Regional Children’s Hospital in Italy. Pediatr. Infect. Dis. J. 2020;39:e221–e225. doi: 10.1097/INF.0000000000002811. [DOI] [PubMed] [Google Scholar]
- 35.Chaiyachati B.H., Agawu A., Zorc J.J., Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J. Pediatr. 2020;226:274–277.e1. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chong S.L., Soo J.S.L., Allen J.C., Ganapathy S., Lee K.P., Tyebally A., Yung C.F., Thoon K.C., Ng Y.H., Oh J.Y., et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020;20:562. doi: 10.1186/s12887-020-02469-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Brusselen D., De Troeyer K., Ter Haar E., Vander Auwera A., Poschet K., Van Nuijs S., Bael A., Stobbelaar K., Verhulst S., Van Herendael B., et al. Bronchiolitis in COVID-19 times: A nearly absent disease? Eur. J. Pediatr. 2021;180:1969–1973. doi: 10.1007/s00431-021-03968-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scaramuzza A., Tagliaferri F., Bonetti L., Soliani M., Morotti F., Bellone S., Cavalli C., Rabbone I. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch. Dis. Child. 2020;105:704–706. doi: 10.1136/archdischild-2020-319397. [DOI] [PubMed] [Google Scholar]
- 39.Silvagni D., Baggio L., Lo Tartaro Meragliotta P., Soloni P., La Fauci G., Bovo C., Ielo S., Biban P. Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy. Pediatr. Rep. 2021;13:168–176. doi: 10.3390/pediatric13020023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jaehn P., Holmberg C., Uhlenbrock G., Pohl A., Finkenzeller T., Pawlik M.T., Quack I., Ernstberger A., Rockmann F., Schreyer A.G. Differential trends of admissions in accident and emergency departments during the COVID-19 pandemic in Germany. BMC Emerg. Med. 2021;21:42. doi: 10.1186/s12873-021-00436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nourazari S., Davis S.R., Granovsky R., Austin R., Straff D.J., Joseph J.W., Sanchez L.D. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am. J. Emerg. Med. 2021;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Charlesworth J.E.G., Bold R., Pal R. Using ICD-10 diagnostic codes to identify ‘missing’ paediatric patients during nationwide COVID-19 lockdown in Oxfordshire, UK. Eur. J. Pediatr. 2021;26:1–15. doi: 10.1007/s00431-021-04123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dann L., Fitzsimons J., Gorman K.M., Hourihane J., Okafor I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch. Dis. Child. 2020;105:810–811. doi: 10.1136/archdischild-2020-319654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hon K.L., Leung A.K. Childhood accidents: Injuries and poisoning. Adv. Pediatr. 2010;57:33–62. doi: 10.1016/j.yapd.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 45.Mehta N.S., Mytton O.T., Mullins E.W.S., Fowler T.A., Falconer C.L., Murphy O.B., Langenberg C., Jayatunga W.J.P., Eddy D.H., Nguyen-Van-Tam J.S. SARS-CoV-2 (COVID-19): What Do We Know About Children? A Systematic Review. Clin. Infect. Dis. 2020;71:2469–2479. doi: 10.1093/cid/ciaa556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Viner R.M., Bonell C., Drake L., Jourdan D., Davies N., Baltag V., Jerrim J., Proimos J., Darzi A. Reopening schools during the COVID-19 pandemic: Governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch. Dis. Child. 2021;106:111–113. doi: 10.1136/archdischild-2020-319963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fontanet A., Grant R., Greve-Isdahl M., Sridhar D. Covid-19: Keeping schools as safe as possible. BMJ. 2021;372:n524. doi: 10.1136/bmj.n524. [DOI] [PubMed] [Google Scholar]
- 48.Munro A.P.S., Faust S.N. Children are not COVID-19 super spreaders: Time to go back to school. Arch. Dis. Child. 2020;105:618–619. doi: 10.1136/archdischild-2020-319474. [DOI] [PubMed] [Google Scholar]
- 49.Gandini S., Rainisio M., Iannuzzo M.L., Bellerba F., Cecconi F., Scorrano L. A cross-sectional and prospective cohort study of the role of schools in the SARS-CoV-2 second wave in Italy. Lancet Reg. Health-Eur. 2021;5:100092. doi: 10.1016/j.lanepe.2021.100092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heavey L., Casey G., Kelly C., Kelly D., McDarby G. No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Eurosurveillance. 2020;25:2000903. doi: 10.2807/1560-7917.ES.2020.25.21.2000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Macartney K., Quinn H.E., Pillsbury A.J., Koirala A., Deng L., Winkler N., Katelaris A.L., O’Sullivan M.V., Dalton C., Wood N., et al. Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health. 2020;4:807–816. doi: 10.1016/S2352-4642(20)30251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ehrhardt J., Ekinci A., Krehl H., Meincke M., Finci I., Klein J., Geisel B., Wagner-Wiening C., Eichner M., Brockmann S.O. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Württemberg, Germany. Eurosurveillance. 2020;25:2001587. doi: 10.2807/1560-7917.ES.2020.25.36.2001587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Theuring S., Thielecke M., van Loon W., Hommes F., Huelso C., von der Haar A., Koerner J., Schmidt M., Boehringer F., Mall M.A., et al. SARS-CoV-2 infection and transmission in school settings during the second wave in Berlin, Germany: A cross-sectional study. medRxiv. 2021 doi: 10.1101/2021.01.27.21250517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Villani A., Coltella L., Ranno S., di Castelbianco F.B., Murru P.M., Sonnino R., Mazzone T., Piccioni L., Linardos G., Chiavelli S., et al. School in Italy: A safe place for children and adolescents. Ital. J. Pediatr. 2021;47:23. doi: 10.1186/s13052-021-00978-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maltezou H.C., Magaziotou I., Dedoukou X., Eleftheriou E., Raftopoulos V., Michos A., Lourida A., Panopoulou M., Stamoulis K., Papaevangelou V., et al. Children and Adolescents With SARS-CoV-2 Infection: Epidemiology, Clinical Course and Viral Loads. Pediatr. Infect. Dis. J. 2020;39:e388–e392. doi: 10.1097/INF.0000000000002899. [DOI] [PubMed] [Google Scholar]
- 56.Van den Berg P., Schechter-Perkins E.M., Jack R.S., Epshtein I., Nelson R., Oster E., Branch-Elliman W. Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: A retrospective, state-wide cohort study. Clin. Infect. Dis. 2021;2021:ciab230. doi: 10.1093/cid/ciab230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ismail S.A., Saliba V., Lopez Bernal J., Ramsay M.E., Ladhani S.N. SARS-CoV-2 infection and transmission in educational settings: A prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect. Dis. 2021;21:344–353. doi: 10.1016/S1473-3099(20)30882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Willeit P., Krause R., Lamprecht B., Berghold A., Hanson B., Stelzl E., Stoiber H., Zuber J., Heinen R., Köhler A., et al. Prevalence of RT-qPCR-detected SARS-CoV-2 infection at schools: First results from the Austrian School-SARS-CoV-2 prospective cohort study. Lancet Reg. Health-Eur. 2021;5:100086. doi: 10.1016/j.lanepe.2021.100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krishnaratne S., Pfadenhauer L.M., Coenen M., Geffert K., Jung-Sievers C., Klinger C., Kratzer S., Littlecott H., Movsisyan A., Rabe J.E., et al. Measures implemented in the school setting to contain the COVID-19 pandemic: A scoping review. Cochrane Database Syst. Rev. 2020;12:CD013812. doi: 10.1002/14651858.CD013812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Couzin-Frankel J., Vogel G., Weiland M. School Openings Across Globe Suggest Ways to Keep Coronavirus at Bay, Despite Outbreaks. American Association for the Advancement of Science; Washington, DC, USA: 2020. [Google Scholar]
- 61.Araújo L.A., Veloso C.F., Souza M.C., Azevedo J.M.C., Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J. Pediatr. 2020;97:369–377. doi: 10.1016/j.jped.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Figueiredo C.S., Sandre P.C., Portugal L.C.L., Mázala-de-Oliveira T., da Silva Chagas L., Raony Í., Ferreira E.S., Giestal-de-Araujo E., Dos Santos A.A., Bomfim P.O.S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;106:110171. doi: 10.1016/j.pnpbp.2020.110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020;293:113429. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim E.S., Kwon Y., Choe Y.H., Kim M.J. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci. Rep. 2021;11:5494. doi: 10.1038/s41598-021-84766-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chanchlani N., Buchanan F., Gill P.J. Addressing the indirect effects of COVID-19 on the health of children and young people. CMAJ. 2020;192:E921–E927. doi: 10.1503/cmaj.201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lachman P. Where to make a difference: Research and the social determinants in pediatrics and child health in the COVID-19 era. Pediatr. Res. 2021;89:259–262. doi: 10.1038/s41390-020-01253-0. [DOI] [PMC free article] [PubMed] [Google Scholar]