Abstract
Hypoxia-inducible factor-1 alpha (HIF-1α) is overexpressed in cancer, leading to a poor prognosis in patients. Diverse cellular factors are able to regulate HIF-1α expression in hypoxia and even in non-hypoxic conditions, affecting its progression and malignant characteristics by regulating the expression of the HIF-1α target genes that are involved in cell survival, angiogenesis, metabolism, therapeutic resistance, et cetera. Numerous studies have exhibited the anti-cancer effect of HIF-1α inhibition itself and the augmentation of anti-cancer treatment efficacy by interfering with HIF-1α-mediated signaling. The anti-cancer effect of plant-derived phytochemicals has been evaluated, and they have been found to possess significant therapeutic potentials against numerous cancer types. A better understanding of phytochemicals is indispensable for establishing advanced strategies for cancer therapy. This article reviews the anti-cancer effect of phytochemicals in connection with HIF-1α regulation.
Keywords: naturally derived compounds, phytochemical, hypoxia, normoxia, HIF, cancer
1. Introduction
Hypoxia-inducible factors (HIFs) are transcription factors that contain α and β subunits. HIF-1α and HIF-1β subunits form HIF-1 heterodimers. In addition, HIF-2 complexes are made up of HIF-2α and HIF-1β subunits [1]. A beta subunit shows a constitutively expressed pattern, whereas the expression of alpha subunits is oxygen-dependently regulated. In normoxic conditions, HIF-1α and HIF-2α can be hydroxylated by prolyl hydroxylases (PHDs). Hydroxylated α subunits are ubiquitinated by von Hippel Lindau E3 ubiquitin ligase (VHL) and consequently degraded by proteasomes [2]. Under hypoxic conditions, PHDs are inactivated due to the deficiency of oxygen. Therefore, the transcriptional activities of HIFs are promoted [2].
In addition to this, the level of α subunits can be modulated by several different factors. For instance, phosphatase and tensin homolog (PTEN) is able to promote HIF-1α degradation by mouse double min 2 homolog (MDM2) in hypoxic conditions. Accumulation of HIF-1α is interrupted by the inhibition of phosphoinositide 3-kinase (PI3K)/AKT [3]. Besides, PI3K/AKT/mechanistic target of rapamycin (mTOR) signaling activates HIF-1α expression in both normoxic and hypoxic conditions. Specifically, the translation of HIF-1α messenger RNA (mRNA) is enhanced by the PI3K/AKT/mTOR pathway [4]. Moreover, HIF-1α can be upregulated via nitric oxide and signal transducer and activator of transcription 1 (STAT1) in response to doxorubicin under normoxia [5]. In the case of HIF-2α, it was demonstrated that OTU deubiquitinase 7B (OTUD7B) can positively regulate the transcription of HIF-2α by stabilizing an E2F transcription factor 1 (E2F1) independently of hypoxia [6].
HIFs exert influence on diverse cellular events by transcriptionally controlling a broad range of genes [7,8]. HIF-1α and HIF-2α suppress apoptotic cell death induced by the tumor protein p53 (TP53) [9,10]. HIFs can promote stemness and epithelial-to-mesenchymal transition (EMT), thus supporting cancer aggressiveness and metastasis [11,12]. HIFs also contribute to angiogenesis and energy metabolism via transcriptionally regulating target genes, such as vascular endothelial growth factor (VEGF) and glucose transporter 1 (GLUT1) [13,14,15]. Other cellular events controlled by HIFs include therapeutic resistance and anti-cancer immunity. For example, HIFs aggravate resistance to paclitaxel and gemcitabine via inducing the expression of interleukin 6 (IL-6), IL-8, and ATP-binding cassette subfamily B member 1 (ABCB1, also known as multidrug resistance protein 1 (MDR1)) [16]. HIF-1α and HIF-2α can lead to the induction of programmed death-ligand 1 (PD-L1) and the infiltration of tumor-associated macrophages (TAMs), respectively, thereby limiting anti-cancer immunity [17,18].
It has been noticed that the expression of HIF-1a and HIF-2a is stronger in cancer than in normal tissues [19,20,21]. Therefore, targeting HIFs has been suggested as an effective strategy for cancer therapy. The silencing of HIF-1α can compensatorily upmodulate HIF-2α and vice versa [22,23]. In addition, HIF-1α and HIF-2α have target gene divergency, so they can differently regulate the transcription of downstream targets [24,25,26]. Therefore, it is desirable to dually inhibit HIF-1α and HIF-2α. Phytochemicals and their derivatives have exhibited potent anti-cancer activities by restraining progression and malignancy, such as cell proliferation and metastasis [27,28,29]. Advanced knowledge on the functional aspects of phytochemicals is invaluable to establishing better therapeutic options against cancer. This review article presents the effects of compounds derived from plants on HIF-1α in conjunction with their efficacy in cancer. The structure, source, and clinical trial status of phytochemicals stated in this review are summarized in supplementary Table S1.
2. Alkaloid and Organosulfur Compounds from Natural Sources
2.1. Alkaloids
2.1.1. Berberine
A clinical trial found that berberine effectively reduces the recurrence of colorectal cancer after polypectomy [30] (clinical Study Identifier: NCT02226185, Table S1). Moreover, preclinical studies have shown that berberine reverses therapeutic resistance in multiple cancers. Berberine can downmodulate the level of microRNA-93 (miR-93) that directly targets PTEN, thus sensitizing drug-resistant ovarian cancer cells to cisplatin [31]. In addition, treatment with berberine downregulates the expression of ABC transporters, including ABCB1 and ABCC1 (also known as multidrug resistance protein 1 (MRP1)), thereby improving anti-growth effects of doxorubicin on breast cancer in vivo [32]. Recently, it was reported that the level of both HIF-1α and AMP-activated protein kinase (AMPK) is reduced by berberine, alleviating hypoxia-mediated doxorubicin resistance. Co-treatment with berberine and doxorubicin significantly retards the growth of breast cancer in vivo [33]. Berberine may destabilize HIF-1α by increasing PTEN levels. In addition, AMPK is known to potentiate doxorubicin resistance in breast cancer [34], and HIF-1α can be stabilized by AMPKα2, one of the catalytic subunits of AMPK [35]. Therefore, berberine may sensitize cancer cells to doxorubicin by regulating the AMPKα2-HIF-1α axis (Figure 1 and Table 1).
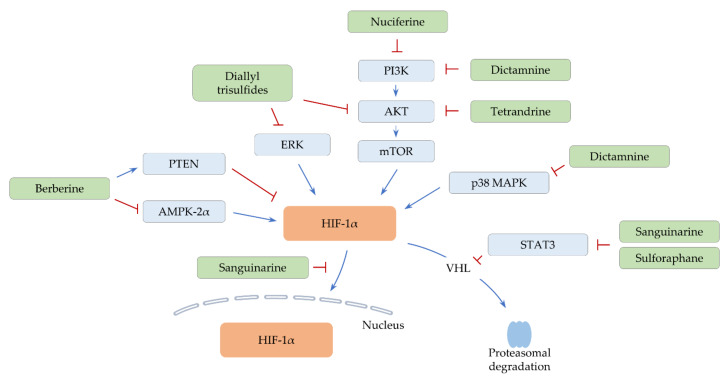
Figure 1.
Proposed signaling pathways of HIF-1α regulation by alkaloids and organosulfurs. Positive regulation is indicated by arrow lines (blue). A negative effect is shown by perpendicular lines (red).
Table 1.
The list of alkaloid and organosulfur compounds that suppress HIF-1α in cancer (alphabetical order).
| Compound | Compound Class | Type of Cancer | In Vitro Testing (Effective Concentrations, Cell Line, Culture Condition (Normoxia/Hypoxia)) |
In Vivo Experiment Model (Dose and Administration Route) |
Ref. |
|---|---|---|---|---|---|
| Alkaloids | |||||
| Berberine | Benzylisoquinoline | Breast cancer | 10–160 μM (human MCF-7 cell line), hypoxia (1% O2) | Subcutaneous injection of MCF-7 cells (5–200 mg/kg, oral) | [33] |
| Cyclopamine tartrate | Derivative of cyclopamine (veratrum alkaloid) | Lung cancer | 15–25 μM (human H1299 cell line), normoxia | Subcutaneous injection of H1299 cells (7.5 mg/kg, intravenous) | [36] |
| Dictamnine | Furanoquinoline alkaloid | Colorectal cancer | 10–100 μM (human HCT-116 cell line), hypoxia (1% O2) | Subcutaneous injection of HCT-116 cells (50–100 mg/kg, oral) | [37] |
| Nuciferine | Aporphine alkaloid | Colorectal cancer, Lung cancer | 4–48 μM (drug-sensitive or -resistant human HCT-8 and A549 cell lines), normoxia | Subcutaneous injection of drug-resistant A549 cells (7.5 mg/kg, intraperitoneal) | [38] |
| Sanguinarine | Benzophenanthridine alkaloid | Breast cancer | 2–4 μM (human MDA-MB-231 cell line), hypoxia (1% O2, cobalt (II) chloride (CoCl2)) | - | [39] |
| Breast cancer | 0.5–1 μM (human T47D and MDA-MB-231 cell lines), hypoxia (1% O2, CoCl2) | Subcutaneous injection of MDA-MB-231 cells (1.25–5 mg/kg, oral) | [40] | ||
| Hepatocellular carcinoma | 0.5–2 μM (human HepG2 and SMMC-7721 cell lines), hypoxia (1% O2, CoCl2) | Subcutaneous injection of HepG2 and SMMC-7721 cells (1.25–5 mg/kg, oral) | [41] | ||
| Tetrandrine | Benzylisoquinoline | Lung cancer | 5–10 μM (human A549 cell line), normoxia | - | [42] |
| Organosulfurs | |||||
| Diallyl trisulfide | Organic trisulfide | Breast cancer | 2.5–10 μM (human MDA-MB-231 cell line), hypoxia (1% O2) | Microinjection of MDA-MB-231 cells into perivitelline space of zebrafish embryos (2.5–10 μM), Tail vein or orthotopic injections of MDA-MB-231 cells (25–50 mg/kg, oral) | [43] |
| Sulforaphane | Isothiocyanate | Bladder cancer | 5–20 μM (human RT112 and RT4 cell lines), hypoxia (2% O2) | - | [44] |
| Hepatocellular carcinoma | 5–20 μM (human HepG2 cell line), hypoxia (CoCl2) | HepG2-bearing chick chorioallantoic membrane (CAM) assay (20 μM) | [45] | ||
2.1.2. Dictamnine
Dictamnine was reported to suppress the activity of mTOR and various mitogen-activated protein kinases (MAPKs), such as p38 MAPK and c-Jun N-terminal kinase (JNK). Moreover, dictamnine downregulates HIF-1α levels under hypoxia in vitro [37]. Treatment with dictamnine restrains cell proliferation, survival, and EMT in vitro. In addition, dictamnine hinders colorectal cancer growth in conjunction with the downregulation of HIF-1α and snail family transcriptional repressor 2 (SNAI2) expression in vivo [37]. Since p38 MAPK can stabilize and upregulate HIF-1α proteins [46,47], both p38 MAPK and PI3K/AKT/mTOR signaling may contribute to the regulation of HIF-1α in dictamnine-treated cells (Figure 1 and Table 1). Another study showed that dictamnine induces cell cycle arrest and that apoptotic cell death is elevated by dictamnine in combination with dihydroartemisinin [48]. These results suggest that dictamnine has multiple anti-cancer effects and that dictamnine-based combinatorial therapy may be useful to overcome hypoxia.
2.1.3. Nuciferine
Several studies denoted that nuciferine inhibits diverse cellular events, such as proliferation, invasion, and EMT via suppressing the PI3K/AKT and Wnt/β-catenin signaling pathways [49,50,51]. Another study noted that nuciferine treatment results in the suppression of PI3K/AKT signaling, which in turn downmodulates the level of NF-E2-related factor 2 (NRF2) and HIF-1α under normoxic conditions [38] (Figure 1 and Table 1). Both NRF2 and HIF-1α can confer drug resistance via upregulating ABCB1 and ABCG2 (also known as breast cancer resistance protein, BCRP) [52,53,54,55]. Indeed, nuciferine abates the expression of ABCB1 and ABCG2, improving the anti-cancer activity of paclitaxel in vitro and in vivo [38]. Further investigation is required to investigate the effect of nuciferine on the expression of other ABC transporters and the efficacy of other anti-cancer treatments.
2.1.4. Sanguinarine
STAT3 is activated by hypoxia and stabilizes HIF-1α by blocking HIF-1α binding to VHL. Therefore, HIF-1α target genes are cooperatively regulated by STAT3 [56,57]. Sanguinarine was found to disrupt the interaction between HIF-1α and STAT3 in hypoxic conditions [39]. Similarly, sanguinarine promotes proteasomal degradation of HIF-1α via inactivating STAT3 under hypoxia and impedes the growth of breast cancer in vivo [40]. In addition, sanguinarine suppresses the nuclear translocation of HIF-1α under hypoxia and restrains the HIF-1α/transforming growth factor-beta (TGF-β) feedback loop. Thus, sanguinarine significantly retards the growth and EMT progress of hepatocellular carcinoma in vivo [41]. Since TGF-β is able to activate STAT3, sanguinarine may regulate the HIF-1α/TGF-β/STAT3 axis to negatively control hypoxia-induced signaling (Figure 1 and Table 1).
2.1.5. Tetrandrine
Accumulating evidence showed that tetrandrine possesses various anti-cancer activities, including the induction of apoptosis, the restraint of migration, invasion, and metastasis, and the reversal of drug resistance [58,59,60]. Moreover, tetrandrine can inactivate AKT and downregulate HIF-1α under normoxic conditions [42], suggesting that AKT signaling is partly responsible for HIF-1α regulation (Figure 1 and Table 1). Tetrandrine consequently reduces and increases the level of VEGF and BCL2-associated X protein (BAX), respectively [42], denoting the involvement of HIF-1α in the anti-angiogenic and apoptosis effects of tetrandrine in lung cancer.
2.2. Organosulfurs
2.2.1. Diallyl Trisulfides
The metastatic potential of cancer can be enhanced by HIF-1α target genes, such as angiopoietin-like 4 (ANGPTL4), lysyl oxidase (LOX), and lysyl oxidase-like 4 (LOXL4) [61,62,63]. ANGPTL4 facilitates the extravasation of cancer cells [61], and LOX increases the migratory and invasive capacities of cells by activating the focal adhesion kinase (FAK)/AKT pathway [62]. In addition, LOXL4 is involved in the establishment of a metastatic niche [63]. A recent study presented that diallyl trisulfide attenuates the expression of HIF-1α, together with a decrease in ANGPTL4, LOX, and LOXL4 levels under hypoxia. Diallyl trisulfide also inhibits the expression of VEGF and EMT-associated genes such as SNAI2 [43]. They further observed that diallyl trisulfide diminishes the motility of hypoxic cancer cells in vitro and the lung metastasis of breast cancer in vivo [43]. Diallyl trisulfide inactivates AKT and extracellular signal-regulated kinase (ERK) [64,65]. ERK can stabilize HIF-1α by preventing PHD2-mediated hydroxylation of HIF-1α [66]. Therefore, diallyl trisulfide may modulate the level of HIF-1α and its target genes via both AKT-HIF-1α and ERK-HIF-1α axes (Figure 1 and Table 1).
2.2.2. Sulforaphane
Sulforaphane has multitudinous anti-cancer effects. For example, sulforaphane activates caspase-3, inducing apoptotic cell death [67]. Besides, sulforaphane upregulates and downregulates miR-200c and teratocarcinoma-derived growth factor 1 (TDGF1), respectively, thus impeding cancer stemness [68,69]. Moreover, sulforaphane represses both expression and nuclear translocation of HIF-1α, thereby negatively regulating cell proliferation and glycolysis in bladder cancer [44]. By reducing STAT3 and HIF-1α levels, sulforaphane also diminishes VEGF expression, exerting anti-angiogenic effects in hepatocellular carcinoma [45] (Figure 1 and Table 1). STAT3 can epigenetically repress miR-200c that directly targets HIF-1α [70,71]. Thus, sulforaphane may additionally control HIF-1α expression and hypoxia-mediated signaling via the STAT3/miR-200c axis. Other miRNAs that are regulated by STAT3 may have a possibility to directly or indirectly change HIF-1α levels.
3. Natural Polyphenolic Compounds
3.1. Flavonoids
3.1.1. Apigenin
The anti-cancer activity of apigenin has been evaluated in different cancer types. In osteosarcoma, apigenin diminishes the level of mitochondria membrane potential and activates caspase-3 [72]. Likewise, apigenin induces caspase-dependent apoptotic cell death and cell cycle arrest in bladder cancer cells [73]. Apigenin was observed to suppress cell migration and invasion in vitro and metastasis in vivo via downregulating the level of neural precursor cell expressed developmentally down-regulated protein 9 (NEDD9) in colorectal cancer [74]. It was also observed that apigenin can induce the level of inositol polyphosphate-5-phosphatase D (INPP5D), thus reducing the population of M2-like TAMs and eventually promoting anti-cancer immune responses in murine pancreatic cancer models [75]. In addition, the expression of HIF-1α and VEGF is downregulated by apigenin in both normoxic and hypoxic conditions. Consistently, in vivo administration of apigenin blocks angiogenesis [76]. Another study further exhibited that the levels of hypoxia-induced stemness markers such as Nanog homeobox (NANOG) are attenuated by apigenin in head and neck cancer [77]. It was suggested that nuclear factor-kappa B (NF-κB) transcriptionally induces HIF-1α and also stimulates HIF-1α translation [78,79]. Considering that AKT and NF-κB are inactivated by apigenin [80,81], apigenin may regulate HIF-1α levels, at least partly, through the AKT and NF-κB pathways (Figure 2 and Table 2).
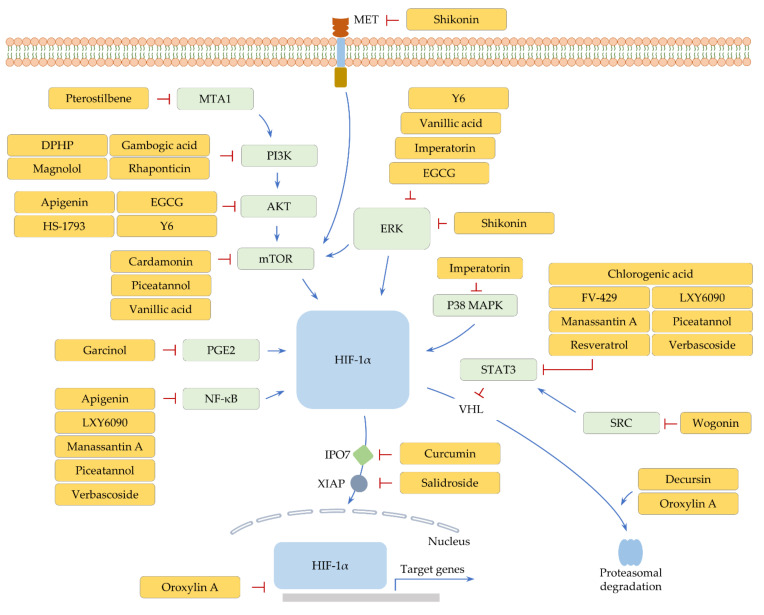
Figure 2.
Polyphenol-mediated cellular signaling pathways that are anticipated to regulate HIF-1α. Positive regulation is pointed out by arrow lines (blue). A restrictive action is indicated by perpendicular lines (red).
Table 2.
The list of polyphenolic compounds that inhibit HIF-1α in cancer (alphabetical order).
| Compound | Compound Class | Type of Cancer | In Vitro Testing (Effective Concentrations, Cell Line, Culture Condition (Normoxia/Hypoxia)) |
In Vivo Experiment Model (Dose and Administration Route) |
Ref. |
|---|---|---|---|---|---|
| Polyphenols (Flavonoids) | |||||
| Apigenin | Trihydroxyflavone | Prostate, Ovarian, Colon, and Breast cancer | 10–40 μM (human PC-3, DU145, MCF-7, HCT-8, LNCaP cell lines), hypoxia (1% O2) | PC-3 and OVCAR-3-bearing CAM assay (7.5–20 μM), Matrigel plug assays (15–20 μM) | [76] |
| Head and Neck cancer | 20–40 μM (human HN-30 cell line), hypoxia (0.5–1% O2) | - | [77] | ||
| Cardamonin | Chalcone | Breast cancer | 20–40 μM (human MDA-MB-231 cell line), hypoxia (CoCl2) | Subcutaneous injection of MDA-MB-231 cells (3 mg/kg, intra-peritoneal) | [82] |
| Epigallocatechin-3-gallate (EGCG) | Flavanol | Breast cancer | 5–20 μM (human MCF-7 cell line), normoxia | - | [83] |
| FV-429 | Wogonin derivative | Ovarian cancer | 5–20 μM (human SK-OV-3 and A2780 cell lines), hypoxia (1% O2) | Subcutaneous injection of A2780 cells (10 mg/kg) | [84] |
| Oroxylin A | Dihydroxyflavone | Glioblastoma | 25–20 μM (human U251 cell line), 10–20 μM (rat C6 cell line), hypoxia (1% O2) | Intracranial transplantations of U251 cells or subcutaneous injections of mouse GL261 cell line (300 mg/kg, oral) | [85] |
| Lung cancer | 50 μM (human H460, A549, 95D, PC9, HCC827 and H1975 cell lines), hypoxia (1% O2) | Subcutaneous injections of H460 cells (50 mg/kg, oral) | [86] | ||
| Wogonin | Hydroxyflavone | Gastric cancer | 20–100 μM (human SGC-7901 cell line), normoxia | - | [87] |
| Y6 | EGCG derivative | Hepatocellular carcinoma | 10–15 μM (doxorubicin-resistant human BEL-7404 cell line), normoxia | - | [88] |
| Hepatocellular carcinoma | 10 μg/mL (human SMMC-7721 cell line), hypoxia (1% O2) | CAM model for angiogenesis assay (200–500 μg/mL), Subcutaneous injections of HepG2 cells (55 mg/kg, oral) | [89] | ||
| Polyphenols (Lignans, Phenolic Acids, and Stilbenes) | |||||
| HS-1793 | Resveratrol analogue | Breast cancer | 12.5–50 μM (human MCF-7 and MDA-MB-231 cell lines), hypoxia (1% O2) | Subcutaneous injections of MDA-MB-231 cells (5–10 mg/kg, intraperitoneal) | [90] |
| LXY6090 | Manassantin A derivative | Breast cancer | 0.4–10 nM (human T47D, MCF-7, and MX-1 cell lines), hypoxia (1% O2) | Subcutaneous injections of MX-1 cells (25–100 mg/kg, oral) | [91] |
| Magnolol | Lignan | Bladder cancer | 1–10 μM (human T24 cell line), hypoxia (1% O2) | CAM model of T24 cells (1–10 μM), Matrigel plug assays (25–75 μg), Subcutaneous injections of T24 cells (2–10 mg/kg, intraperitoneal) | [92] |
| Manassantin A | Lignan | Lung cancer | 0.01–10 μM (luciferase-reporter assay using human embryonic kidney 293T cells), hypoxia (1% O2) | Lewis lung carcinoma allografts (5 mg/kg, intraperitoneal) | [93] |
| Piceatannol | Stilbene | Colorectal cancer | 7.5 μg/mL of piceatannol-loaded nanoparticles (PNs) (human CaCo-2 and HT-29 cell lines), normoxia | Colitis-associated colorectal cancer mouse model (40 mg/kg) | [94] |
| Pterostilbene | Stilbene | Prostate cancer | 50 μM (human LNCaP and PC3M cell lines), normoxia | Pten-null mouse model (10 mg/kg, intraperitoneal) | [95] |
| Resveratrol | Stilbene | Lung cancer | - | Orthotopic injections of A549 cells (250 mg/kg, intragastric) | [96] |
| Gastric cancer | 12.5–100 μM (human SGC-7901 cell line), hypoxia (3% O2) | - | [97] | ||
| Pancreatic cancer | 50 μM (human pancreatic stellate cells from normal tissues), hypoxia (3% O2) | KPC mouse model of pancreatic cancer (50 mg/kg) | [98] | ||
| Rhaponticin | Stilbene | Fibrosarcoma | 25–100 μM (human HT1080 cell line), hypoxia (CoCl2) | - | [99] |
| Vanillic acid | Phenolic acid | Colorectal cancer | 3–30 μM (human HCT-116 cell line), hypoxia (1% O2, CoCl2) | Subcutaneous injections of HCT-116 cells (10–30 mg/kg, oral) | [100] |
| Other Polyphenols | |||||
| Chlorogenic acid | Tannin | Lung cancer | 2–10 μM (human A549 cell line), hypoxia (1% O2, CoCl2) | Matrigel plug assays (10 μM) | [101] |
| Curcumin | Diarylheptanoid | Chronic myelogenous leukemia | 20 μM (human K526 cell line), normoxia | - | [102] |
| Decursin | Pyranocoumarin | Lung and Colorectal cancer | 10–50 μM (human A549 and HCT-116 cell lines), hypoxia (1% O2, CoCl2) | Lewis lung carcinoma allografts (10 mg/kg, intraperitoneal) | [103] |
| DPHP | Alpinoid c (diarylheptanoid) derivative | Colorectal cancer | 3.5–14 μM (human COLO205 cell line), hypoxia (CoCl2) | CAM model for angiogenesis assay (3.5–14 μM) | [104] |
| Gambogic acid | Xanthone | Multiple myeloma | 0.1–0.2 μM (human U266 cell line), hypoxia (1% O2) | Subcutaneous injections of U266 cells (2–4 mg/kg, intravenous) | [105] |
| Garcinol | Polyisoprenylated benzophenone | Colorectal cancer | 20–60 μM (human HT-29 cell line), normoxia | - | [106] |
| Imperatorin | Furanocoumarin | Colorectal cancer | 50–150 μM (human HCT-116 cell line), hypoxia (1% O2, CoCl2) | Subcutaneous injections of HCT-116 cells (50–100 mg/kg, oral) | [107] |
| Salidroside | Phenylethanoid | Hepatocellular carcinoma | 100 μM (human PLC/PRF/5, SMMC-7721, and HepG2 cell lines), hypoxia (1% O2) | Subcutaneous or orthotopic injections of PLC/PRF/5 cells (60 mg/kg, intragastric) | [108] |
| Shikonin | Naphthoquinone | Colorectal cancer | 1–10 μM (human SW-620 and HCT-116 cell lines), hypoxia (1% O2) | Subcutaneous injections of HCT-116 cells (2–10 mg/kg, oral) | [109] |
| Verbascoside | Phenylethanoid glycoside | Colorectal cancer | 50–150 μM (human HT-29 cell line), normoxia | - | [110] |
3.1.2. Cardamonin, Epigallocatechin-3-Gallate, and Y6
In breast cancer, cardamonin and epigallocatechin-3-gallate (EGCG) induce cell cycle arrest and apoptotic cell death [111,112]. Activation of JNK and forkhead box O3 (FOXO3) contributes to the upregulation of cyclin-dependent kinase inhibitor 1A (CDKN1A, also called p21), CDKN1B (also named as p27), and Bcl-2-like protein 11 (BCL2L11) following cardamonin treatment [111]. EGCG induces G2/M cell cycle arrest and inhibits cell survival by downregulating miR-25 [112]. In addition, cardamonin and EGCG can reverse the EMT process by suppressing Wnt/β-catenin signaling and DNA methyltransferase levels in breast cancer [113,114].
Moreover, both phytochemicals negatively regulate HIF-1α expression in breast cancer. Cardamonin was revealed to regulate HIF-1α expression via the mTOR pathway and repress glycolysis process by reducing the uptake of glucose and the production of lactic acid [82]. Cardamonin impedes the growth of breast cancer, along with a decrease in HIF-1α and its target genes, such as lactate dehydrogenase A (LDHA), in vivo [82]. EGCG diminishes HIF-1α and VEGF levels in breast cancer cells [83]. EGCG inactivates a number of cellular factors, such as AKT and ERK [115,116]. EGCG may, therefore, transcriptionally and post-transcriptionally regulate HIF-1α (Figure 2 and Table 2). It should be pointed out that EGCG can trigger autophagy-dependent survival, delaying apoptosis in consequence [117].
Further, Y6, a derivative of EGCG, downmodulates HIF-1α and ABCB1 levels in doxorubicin-resistant hepatocellular carcinoma cells. Therefore, resistant cells treated with Y6 exhibits an increase in apoptosis and sensitivity to doxorubicin [88]. Another study also demonstrated that Y6 reduces the activity of ERK and AKT and the level of HIF-1α and VEGF in hypoxic cancer cells (Figure 2 and Table 2). It was further verified that Y6 constrains the growth of hepatocellular carcinoma and angiogenesis in vivo [89].
3.1.3. FV-429 and Wogonin
Therapeutic resistance and the EMT process can be suppressed by wogonin-mediated inactivation of STAT3 [118,119]. Further, it was noted that wogonin downmodulates HIF-1α levels under normoxia in gastric cancer cells (Figure 2 and Table 2). Wogonin, owing to this ability, significantly decreases several glycolysis-related genes, including LDH, succinate dehydrogenase (SDH), and monocarboxylate transporter 4 (MCT4) [87]. In their study, wogonin was shown to inhibit the proliferation of A549 lung cancer cells. However, HIF-1α expression is unaffected by wogonin in A549 cells [87]. These findings suggest that the control of HIF-1α expression by wogonin may be context-dependent. Besides, FV-429, a derivative of wogonin, diminishes the level of HIF-1α by inhibiting SRC proto-oncogene (SRC)/STAT3 signaling under hypoxia [84] (Figure 2 and Table 2). Therefore, FV-429 can potentiate the effectiveness of paclitaxel against ovarian cancer in vitro and in vivo [84].
3.1.4. Oroxylin A
Hedgehog (Hh) signaling is activated by hypoxia and controls multiple events, such as stemness, invasion, and EMT [120]. Moreover, there is evidence that Hh signaling induces the expression of ABC transporters and DNA repair genes, triggering therapeutic resistance to several anti-cancer drugs, such as 5-fluorouracil, cisplatin, and temozolomide [121,122,123]. In glioblastoma, oroxylin A was observed to promote VHL-mediated HIF-1α degradation and limit the HIF-1α-Hh signaling pathway, thus sensitizing glioma cells to temozolomide in vitro and in vivo [85]. Interestingly, another study revealed that oroxylin A directly interacts with HIF-1α and inhibits the DNA binding property of HIF-1α, decreasing the transcription of xeroderma pigmentosum group C (XPC), a DNA repair gene [86] (Figure 2 and Table 2). Both oroxylin A treatment and XPC knockdown augment anti-cancer efficacy of cisplatin in vitro, indicating that oroxylin A alleviates hypoxia-induced cisplatin resistance at least partly through downregulating XPC. Indeed, oroxylin A combined with cisplatin significantly increases apoptotic cell death and inhibits the growth of lung cancer in vivo [86].
3.2. Lignans, Phenolic Acids, and Stilbenes
3.2.1. HS-1793 and Resveratrol
STAT3 is downregulated by resveratrol administration concomitantly with an attenuation of HIF-1α as well as VEGF levels in xenograft models of lung cancer [96], indicating the inhibitory function of resveratrol in hypoxia-mediated angiogenesis. In gastric cancer, resveratrol suppresses the HIF-1α/Hh signaling axis, reversing hypoxia-driven cell invasion and the EMT process [97].
Additionally, resveratrol abates the level of HIF-1α in pancreatic stellate cells (PSCs) under hypoxia, restraining PSC activation and the secretion of various cellular factors, such as IL-6 and VEGF from PSCs [98]. The invasive capacities of pancreatic cancer cells are weakened following treatment with conditioned media (CM) from resveratrol-exposed PSCs compared to CM from hypoxia-activated PSCs [98]. These findings demonstrate that resveratrol may impair the crosstalk between cancer cells and other cellular components in the microenvironment, hence decelerating the malignant progression of cancer.
HS-1793, a resveratrol derivative, was investigated to arrest cells at the G2/M phase and induce apoptotic cell death via suppressing AKT activity [124]. Moreover, HS-1793 can exert potent anti-breast cancer effects via hindering HIF-1α-mediated transcriptional activation of VEGF expression in vitro and in vivo [90] (Figure 2 and Table 2).
3.2.2. LXY6090 and Manassantin A
Manassantin A has an inhibitory role in HIF-1 transactivation activity in a dose-dependent manner [93]. In this study, evaluation of the combined effect of manassantin A and gefitinib (an epidermal growth factor receptor (EGFR) inhibitor) shows cooperative therapeutic effects on lung cancer in vivo [93]. This finding suggests that manassantin A sensitizes cancer cells to gefitinib, at least in part, via HIF-1α inhibition.
Besides, LXY6090, a manassantin A derivative, downregulates the expression of HIF-1α proteins via both inhibiting mRNA levels and promoting VHL-mediated degradation under hypoxia [91]. LXY6090 reduces the level of HIF-1α target genes, such as VEGF and insulin-like growth factor 2 (IGF2), in vitro and the growth of cancer in vivo [91]. Considering that manassantin A can inhibit NF-κB signaling and STAT3 activation [125,126], manassantin A and its derivative may transcriptionally as well as post-transcriptionally block HIF-1α expression via the NF-κB and STAT3 signaling pathways (Figure 2 and Table 2). Further investigation is desired to unveil the mechanisms of anti-cancer action of these phytochemicals.
3.2.3. Magnolol
Magnolol can negatively control HIF-1α expression by interfering with the PI3K/AKT/mTOR pathway under hypoxia, hence suppressing angiogenesis and cancer growth in vivo [92]. In addition to this, functional characterization of magnolol shows that this compound can exert anti-cancer activity by inactivating MAPKs such as p38 MAPK [127]. These pieces of evidence suggest that magnolol may intricately control HIF-1α levels by affecting diverse cellular signaling pathways (Figure 2 and Table 2).
3.2.4. Piceatannol and Vanillic Acid
Piceatannol shows an anti-cancer activity by exerting repressive effects on multiple cellular factors, such as mTOR and STAT3 [128]. Moreover, piceatannol can upregulate PMA-induced protein 1 (PMAIP1), thus strengthening cisplatin-induced apoptosis [129]. Further exploration of piceatannol revealed that NF-κB and HIF-1α levels are downregulated in colorectal cancer cells exposed to piceatannol-loaded nanoparticles (PNs) [94]. Not only do PNs inhibit colony formation and invasion activities of cancer cells in vitro, but PNs suppress the growth of colorectal cancer in vivo [94], suggesting that the NF-κB/HIF-1α axis partly mediates the anti-cancer effects of piceatannol (Figure 2 and Table 2). However, ABCB1 levels can be elevated by piceatannol exposure [130], suggesting the possibility of the incidence of multidrug resistance.
In colorectal cancer, vanillic acid also limits HIF-1α expression. Mechanistically, it was confirmed that HIF-1α is regulated by both mTOR and ERK pathways in hypoxic cancer cells following vanillic acid treatment [100] (Figure 2 and Table 2). Vanillic acid is capable of attenuating the synthesis of angiogenic factors, such as VEGF and erythropoietin (EPO). The anti-cancer properties of vanillic acid were determined by a decrease in cell proliferation in vitro and the growth of cancer in vivo as well [100].
3.2.5. Pterostilbene
Metastasis-associated 1 (MTA1) is able to transcriptionally repress PTEN expression and consequently stimulate PI3K/AKT signaling [131]. Moreover, it was explored that MTA1 is induced by hypoxia and stabilizes HIF-1α proteins [132]. Recently, pterostilbene was demonstrated to abolish MTA1-mediated PTEN suppression, hence stimulating apoptosis and hindering cell invasion in vitro and cancer growth in vivo [133] (Figure 2 and Table 2). What is more, pterostilbene leads to a reduction of HIF-1α levels in conjunction with MTA1 downregulation [95]. In this study, pterostilbene was determined to enhance the efficacy of suberoylanilide hydroxamic acid (SAHA) [95]. This evidence suggests the feasibility of utilizing pterostilbene as an adjuvant to reduce the dose and toxic side effects of SAHA.
3.2.6. Rhaponticin
Rhaponticin exhibits cytotoxic effects in both drug-sensitive and -resistant leukemia cells by stimulating apoptotic cell death [134]. Rhaponticin was also validated to inhibit the expression of fatty acid synthase in breast cancer and the PI3K/AKT/mTOR pathway in osteosarcoma [135,136]. Another study denoted that the nuclear expression of HIF-1α is suppressed by rhaponticin in fibrosarcoma cells exposed to hypoxic conditions and that rhaponticin reduces EMT-associated markers (e.g., SNAI2) and pro-angiogenic factors (e.g., VEGF) [99] (Figure 2 and Table 2).
3.3. Other Polyphenols
3.3.1. Chlorogenic Acid
HIF-1α protein levels are notably downregulated by chlorogenic acid without changes in mRNA amounts in lung cancer cells exposed to cobalt (II) chloride (CoCl2), a hypoxia-mimetic agent [101]. This observation demonstrates post-transcriptional modulation of HIF-1α expression in response to chlorogenic acid. Such downregulation of HIF-1α is accompanied by VEGF decrement in vitro. It was then confirmed that chlorogenic acid subdues VEGF-induced angiogenesis in vivo [101]. Chlorogenic acid can interfere with the STAT3 pathway [137]. It is, therefore, feasible that HIF-1α proteins may be destabilized by VHL after chlorogenic acid exposure (Figure 2 and Table 2).
3.3.2. Curcumin
Importin 7 (IPO7) performs a role in nuclear protein import and is overexpressed in cancers, including lung and colorectal cancer [138,139]. IPO7 knockdown reduces survival advantages of cancer cells by downregulating and upregulating AKT and BAX levels, respectively [138]. The depletion of IPO7 downregulates the nuclear import of ribosomal protein L4 and elicits ribosomal biogenesis stress. Tumor protein p53 (TP53) is activated by ribosomal biogenesis stress, ultimately inhibiting the colony formation of cancer cells [140]. Moreover, nuclear localization of glioma-associated oncogene homolog 1 (GLI1) is driven by IPO7, advancing cell proliferation and invasion in glioblastoma cells [141]. Of note, the nuclear translocation of HIF-1α can be mediated by IPO7 [142]. Nuclear accumulation of HIF-1α is impaired by curcumin, in company with an abatement of cellular factors associated with glucose metabolism under non-hypoxic conditions [102], suggesting the therapeutic potential of curcumin for chronic myelogenous leukemia. In addition, curcumin increases miR-22 that directly targets IPO7 in chronic myelogenous leukemia cells [102], indicating that curcumin modulates HIF-1α activity via the miR-22/IPO7 axis (Figure 2 and Table 2).
3.3.3. Decursin
Proteasomal degradation of HIF-1α is prompted by decursin in lung and colorectal cancer cells under hypoxia [103] (Figure 2 and Table 2). Decursin downregulates the mRNA level of several genes, including C-X-C motif chemokine receptor 4 (CXCR4) and VEGF, indicating the transcriptional suppression of HIF-1α target genes. In vitro experiments showed that the treatment of lung cancer cells with decursin increases and decreases apoptosis and cell invasion, respectively. Further in vivo investigation noticeably demonstrated decursin-induced enhancement of anti-cancer immune response in the murine allograft model [103].
3.3.4. DPHP, Garcinol, Imperatorin, Shikonin, and Verbascoside
DPHP can restrain the expression of PI3K and an activated form of AKT in colorectal cancer cells treated with CoCl2. HIF-1α levels are also reduced by DPHP, suggesting that PI3K/AKT signaling may influence the expression of HIF-1α in DPHP-treated conditions [104] (Figure 2 and Table 2). By altering HIF-1α expression levels, DPHP can cause a drop in VEGF and matrix metallopeptidase 2 (MMP2) levels [104], indicating anti-angiogenic and anti-invasive potencies of DPHP.
Prostaglandin E2 (PGE2) stabilizes HIF-1α proteins and facilitates their nuclear translocation [143]. In this study, pharmacological inhibition of the ERK pathway using PD98059 abolishes the effect of PGE2 on HIF-1α. ERK signaling has been identified to mediate PGE2 induction [144]. Therefore, HIF-1α can be stabilized and translocated to the nucleus via the ERK/PGE2 axis. In colorectal cancer, garcinol was noticed to target prostaglandin E synthase (PTGES) and thus decrease PGE2 productions [106]. Garcinol showed anti-migration and anti-angiogenesis effects, along with a reduction in HIF-1α and VEGF levels [106]. These results suggest that garcinol exerts anti-cancer activity via the PTGES/PGE2/HIF-1α axis in colorectal cancer (Figure 2 and Table 2).
Imperatorin was recognized to suppress cancer by halting cell cycle progression [145]. Moreover, imperatorin can augment the cytotoxicity of gamma-delta T cells against CD133-positive cancer via targeting myeloid cell leukemia 1 (MCL1), an endogenous apoptosis inhibitor [146]. It was further shown that imperatorin inhibits TGF-β-mediated ERK activation, thus hindering metastasis [147]. In colorectal cancer, imperatorin shows a repressive activity on HIF-1α in hypoxic conditions [107]. Imperatorin inhibits ERK and p38 MAPK, preventing the induction of HIF-1α target genes such as VEGF and EPO (Figure 2 and Table 2). Not surprisingly, imperatorin decreases the growth of colorectal cancer and the tissue expression of HIF-1α and VEGF in vivo [107].
Furthermore, shikonin causes the suppression of HIF-1α under hypoxia, resulting in efficient restraint of in vitro proliferation and in vivo growth of colorectal cancer cells [109]. Investigation of the level and activity of signaling molecules showed that shikonin inactivates mTOR independently of AKT, indicating that shikonin has an effect on other cellular factors to suppress mTOR-mediated HIF-1α regulation. Although the underlying mechanisms of such events remain elusive, ERK and MET proto-oncogene (MET) can be implicated in the control of HIF-1α levels, since both ERK and MET are rendered inactive by shikonin [148,149], and they can promote AKT-independent mTOR activation [150,151] (Figure 2 and Table 2).
The anti-cancer properties of verbascoside can be due to its suppressive effects on multiple cellular signaling pathways, such as NF-κB, STAT3, and TGF-β signaling [152,153,154]. Verbascoside adversely affects HIF-1α expression under normoxic conditions in colorectal cancer and downregulates EMT-related factors such as zinc finger E-box-binding homeobox 1 (ZEB1) [110]. NF-κB and STAT3 may be involved in verbascoside-induced HIF-1α inhibition (Figure 2 and Table 2). In addition, TGF-β can increase the nuclear expression of HIF-2α, activating VEGF transcription under normoxic conditions [155]. Therefore, verbascoside may also abrogate HIF-2α signaling in non-hypoxic cells.
3.3.5. Gambogic Acid
The therapeutic potential of gambogic acid against cancer has been determined by its abrogative effects on NF-κB and STAT3 signaling, leading to apoptosis and anti-angiogenesis [156,157]. In addition, PI3K/AKT/mTOR signaling is deactivated in gambogic acid-treated cancer cells [158]. In multiple myeloma, gambogic acid restrains hypoxia signaling [105]. Under hypoxia, the induction of HIF-1α and VEGF is significantly attenuated by gambogic acid, and PI3K/AKT/mTOR signaling is engaged in HIF-1α regulation (Figure 2 and Table 2). Further, it was presented that the growth of multiple myeloma is impaired in the gambogic acid-treated xenografts [105]. However, it is noteworthy that caspase activation can be detained by gambogic acid-induced autophagy [156].
3.3.6. Salidroside
Oxaliplatin resistance can be advanced by a number of cellular factors and events, such as XIAP and EMT. Knockdown of XIAP restores the sensitivity of resistant cancer cells to oxaliplatin. ZEB1 is upregulated in oxaliplatin-resistant cells, and its silencing increases oxaliplatin-induced apoptotic cell death [159,160]. Besides, pharmacological inhibition of HIF-1α enhances the anti-cancer potency of oxaliplatin, demonstrating the association of hypoxia with oxaliplatin resistance [161]. Recent research showed that salidroside decreases HIF-1α and EMT factors such as ZEB1 under hypoxia. Thus, salidroside can enhance the oxaliplatin sensitivity of hepatocellular carcinoma cells in vitro and in vivo [108]. Salidroside was reported to downregulate XIAP, and XIAP was interestingly discerned to promote the nuclear retention of HIF-1α and subsequently escalate the level of HIF-1α responsive genes [162,163]. Therefore, the XIAP/HIF-1α axis may be one of the signaling axes accountable for the resistance-alleviating effect of salidroside (Figure 2 and Table 2).
4. Terpene Phytochemicals
4.1. Monoterpenes
4.1.1. Perillyl Alcohol
In vitro reporter assays showed that perillyl alcohol efficiently blocks the transcriptional activity of HIF-1α in several types of cancer cells treated with CoCl2 [164]. Moreover, perillyl alcohol efficiently reduces mTOR activation and the level of HIF-1α and VEGF proteins under CoCl2-mediated hypoxic conditions [164], suggesting that perillyl alcohol negatively regulates angiogenic signaling via the mTOR/HIF-1α pathway (Figure 3 and Table 3). In vivo administration of perillyl alcohol remarkably arrests the growth of colorectal cancer with a decrease in VEGF levels in the serum [164].
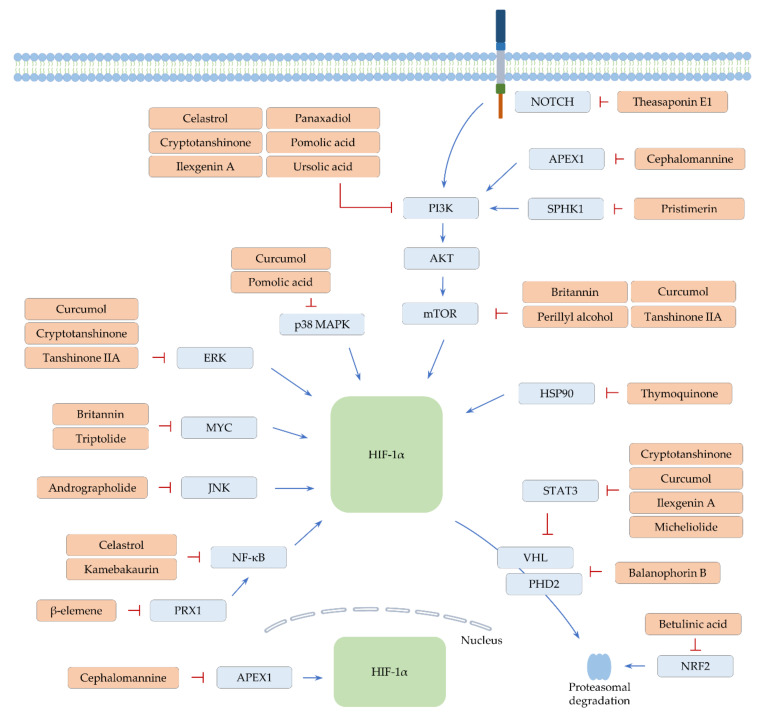
Figure 3.
Proposed mechanisms by which terpenes regulate HIF-1α. Positive modulation is denoted by arrow lines (blue). Perpendicular lines designate an inhibitory effect (red).
Table 3.
The list of terpene compounds restricting HIF-1α in cancer (alphabetical order).
| Compound | Compound Class | Type of Cancer | In Vitro Testing (Effective Concentrations, Cell Line, Culture Condition (Normoxia/Hypoxia) |
In Vivo Experiment Model (Dose and Administration Route) |
Ref. |
|---|---|---|---|---|---|
| β-elemene | Sesquiterpene | Lung cancer | - | Subcutaneous injections of A549 cells (45 mg/kg) | [165] |
| Lung cancer | - | Lewis lung carcinoma allografts (45 mg/kg, intraperitoneal) | [166] | ||
| Andrographolide | Diterpene | Hepatocellular carcinoma | 25–50 μM (human Hep3B and HepG2 cell lines), normoxia | Subcutaneous injections of Hep3B cells (10 mg/kg, intraperitoneal) | [167] |
| Balanophorin B | Triterpene | Hepatocellular carcinoma | 25–50 μM (human Huh-7 and HepG2 cell lines), hypoxia (1% O2) | Subcutaneous injections of HepG2 cells (50–100 mg/kg, oral) | [168] |
| Betulinic acid | Triterpene | Cervical cancer | 3–30 μM (human HeLa cell line), hypoxia (1% O2) | - | [169] |
| Britannin | Sesquiterpene | Colorectal cancer | 1–10 μM (human HCT-116 cell line), normoxia | Subcutaneous injections of HCT-116 cells (5–15 mg/kg, oral) | [170] |
| Celastrol | Triterpene | Glioblastoma | 0.25–1 μM (human U87 and U251 cell lines), normoxia | Orthotopic injections of U87 cells (0.5–2 mg/kg, intraperitoneal) | [171] |
| Cephalomannine | Diterpene | Lung cancer | 0.025–0.1 μM (human A549 and H460 cell lines), hypoxia (1% O2) | Subcutaneous injections of H460 cells (0.4 mg/kg, intraperitoneal) | [172] |
| Cryptotanshinone | Diterpene | Colorectal cancer | 5–20 μM (mouse CT26 cell line), normoxia | Subcutaneous injections of CT26 cells (20–80 mg/kg, oral) | [173] |
| Curcumol | Sesquiterpene | Hepatocellular carcinoma | 3–30 μM (human Hep3B cell line), hypoxia (1% O2) | Subcutaneous injections of Hep3B cells (3–30 mg/kg, oral) | [174] |
| Ilexgenin A | Triterpene | Colorectal cancer | 25–50 μM (human HT-29 and HCT-116 cell lines), hypoxia (1% O2) | Colitis-associated colorectal cancer mouse model (20 mg/kg) | [175] |
| Kamebakaurin | Diterpene | Colorectal cancer | 10–30 μM (human HCT-116 cell line), hypoxia (CoCl2) | Subcutaneous injections of HCT-116 cells (15–50 mg/kg, oral) | [176] |
| Micheliolide | Sesquiterpene | Lung cancer | 5–20 μM (human H1299 and Calu-1 cell lines), hypoxia (1% O2) | - | [177] |
| Panaxadiol | Triterpene | Colorectal cancer | 10 μM (human HCT-116 cell line), hypoxia (1% O2) | Subcutaneous injections of HCT-116 cells (10–30 mg/kg, oral) | [178] |
| Perillyl alcohol | Monoterpene | Cervical and Colorectal cancer, Hepatocellular carcinoma | 50–200 μM (human HCT-116, HeLa, and SK-Hep1 cell lines), hypoxia (1% O2, CoCl2) | Subcutaneous injections of HCT-116 cells (50–100 mg/kg, oral) | [164] |
| Pomolic acid | Triterpene | Breast cancer | 1–10 μM (human MCF-7 and MDA-MB-231 cell lines), hypoxia (CoCl2) | - | [179] |
| Pristimerin | Triterpene | Prostate cancer | 1 μM (human PC-3, DU145, and LNCaP cell lines), hypoxia (1% O2) | - | [180] |
| Tanshinone IIA | Diterpene | Breast cancer | 2.5–20 μM (human MCF-7 and MDA-MB-231 cell lines), hypoxia (1% O2) | Subcutaneous injections of MDA-MB-231 cells (50 mg/kg, intraperitoneal) | [181] |
| Theasaponin E1 | Triterpene | Ovarian cancer | 1–5 μM (human OVCAR-3 and A2780/CP70 cell lines), normoxia | CAM model of OVCAR-3 cells (4 μM) | [182] |
| Thymoquinone | Monoterpene | Renal cancer | 5–10 μM (human Caki-1, Caki-2, and A498 cell lines), hypoxia (1% O2) | - | [183] |
| Triptolide | Diterpene | Pancreatic cancer | 55–140 μM (human SW1990 cell line), normoxia | Subcutaneous injections of SW1990 cells (0.2–0.8 mg/kg, intraperitoneal) | [184] |
| Ursolic acid | Triterpene | Colorectal cancer | 20–40 μM (human RKO, LoVo, and SW480 cell lines), hypoxia (1% O2) | - | [185] |
| Lung cancer | 50–80 μM (human H1299 cell line), normoxia | - | [186] | ||
| Ovarian cancer | 6.5–65 μM (spheroid cultures of human SKOV3 cell line), hypoxia (1% O2) | - | [187] |
4.1.2. Thymoquinone
The screening of 502 natural compounds identified thymoquinone as one of the HIF-1α inhibitors [183]. Treatment with thymoquinone represses HIF-1α expression under hypoxia in renal cancer cells. Thus, thymoquinone downregulates various HIF-1α target genes involved in glycolysis, angiogenesis, and metastasis [183]. Heat shock protein 90 (HSP90) has been known to physically interact with and protect HIF-1α from proteasome-mediated degradation independently of VHL [188]. Thymoquinone was observed to destabilize HIF-1α by hindering the interaction of HIF-1α with HSP90, ultimately promoting the apoptosis of hypoxic cancer cells [183] (Figure 3 and Table 3).
4.2. Sesquiterpenes
4.2.1. β-Elemene and Micheliolide
A decrease in HIF-1α and GLUT1 expression was detected in lung cancer xenografts treated with β-elemene [165]. The administration of β-elemene sensitizes lung cancer to radiotherapy, demonstrating that β-elemene can improve radiotherapy efficiency by impeding hypoxia-mediated glycolysis. Another study demonstrated that the treatment of hypoxic cancer cells with β-elemene downregulates the expression of peroxiredoxin 1 (PRX1), a mediator of NF-κB activation [166]. Restraint of the PRX1/NF-κB pathway contributes to an attenuation of HIF-1α levels in lung cancer (Figure 3 and Table 3). Such HIF-1α inhibition further suppresses hypoxia-mediated induction of monocyte chemoattractant protein-1 (MCP1), ultimately restricting the infiltration of TAMs into the tumor microenvironment and enhancing the effect of radiotherapy [166].
Micheliolide also sensitizes lung cancer cells to irradiation, owing to its prohibitory action on HIF-1α. Notably, micheliolide was confirmed to facilitate HIF-1α degradation [177]. Although it is required to uncover molecular mechanisms accounting for micheliolide-mediated HIF-1α degradation, STAT3 can be involved in HIF-1α regulation, since its activity is inhibited by micheliolide [189] (Figure 3 and Table 3).
4.2.2. Britannin
Tumor necrosis factor (TNF) can induce and stabilize PD-L1, driving cancer immune evasion [190,191]. PD-L1 is also known as one of the HIF-1α targets [17], and TNF has been shown to induce HIF-1α [192]. These findings suggest that the TNF-HIF-1α pathway plays a part in controlling PD-L1 expression. More recently, britannin was recognized to exhibit anti-colorectal cancer effects via downmodulating TNF-induced PD-L1 expression [170]. Britannin interrupts mTOR signaling and inhibits MYC proto-oncogene (MYC), as well as HIF-1α expression in TNF-treated colorectal cancer cells [170]. Since MYC is able to post-transcriptionally induce HIF-1α proteins [193], britannin may abrogate the effect of TNF on HIF-1α via affecting mTOR and MYC, thus leading to a decline in PD-L1 (Figure 3 and Table 3). The growth of cancer is inhibited by britannin, together with a reduction of PD-L1 and VEGF in vivo [170], proposing the therapeutic potential of britannin towards colorectal cancer.
4.2.3. Curcumol
Similarly, curcumol downregulates HIF-1α and PD-L1 expression under hypoxia in hepatocellular carcinoma cells [174]. Curcumol adversely affects the activity of STAT3, mTOR, and MAPKs (e.g., ERK and p38 MAPK), implying the feasibility of involvement of these signaling factors in HIF-1α regulation [174] (Figure 3 and Table 3). Curcumol enhances T cell-mediated lysis of hepatocellular carcinoma cells in vitro and retards the growth of cancer in vivo [174]. Combination therapy with PD-L1 inhibitors and other therapeutic approaches (e.g., chemotherapy and immunotherapy) has been suggested to reinforce anti-cancer responses [194]. Therefore, the development of effective curcumol-based combination strategies may enhance therapeutic responses.
4.3. Diterpenes
4.3.1. Andrographolide
The anti-cancer action of andrographolide is through multiple mechanisms, including the suppression of ERK activity and cyclooxygenase 2 (COX2) expression [195,196]. In hepatocellular carcinoma, andrographolide diminishes the level of HIF-1α and VEGF in vitro and in vivo [167]. In this study, it was additionally noticed that inhibition of JNK using a pharmacological inhibitor, SP600125, nullifies the effect of andrographolide on HIF-1α expression [167] (Figure 3 and Table 3). The role of JNK in regulating HIF-1α expression is inconclusive, because JNK has been reported to repress or advance HIF-1α levels [197,198], proposing the requirement of more investigation on the relationship between JNK and HIF-1α.
4.3.2. Cephalomannine
Apurinic/apyrimidinic endodeoxyribonuclease 1 (APEX1) advances malignant properties, such as proliferation, invasion, and angiogenesis through activating, for example, PI3K/AKT and Notch signaling [199,200]. In addition, APEX1 interacts with HIF-1α and positively affects the transcription activity of HIF-1α under hypoxia [201]. Recently, it was demonstrated that cephalomannine inhibits the interaction of APEX1 and HIF-1α, resulting in the attenuation of cell viability and migration of lung cancer cells under hypoxic conditions [172] (Figure 3 and Table 3). In their study, cephalomannine was also confirmed to impede the growth of lung cancer with a reduction of several HIF target genes such as MMP2 in xenograft models [172].
4.3.3. Cryptotanshinone and Kamebakaurin
The anti-colorectal cancer effects of cryptotanshinone can be caused by the downregulation of HIF-1α and VEGF levels in vivo [173]. Cryptotanshinone exerts a negative influence on the PI3K/AKT/mTOR signaling in vitro [173], implying the participation of this signaling pathway in HIF-1α regulation. Apart from this, cryptotanshinone can exert its anti-cancer activity via inactivating STAT3 and ERK [202,203]. Thus, it can be speculated that multiple cellular factors affected by cryptotanshinone coordinately modulate HIF-1α signaling (Figure 3 and Table 3).
Kamebakaurin is capable of inhibiting the activity of NF-κB and blocks the induction of anti-apoptotic genes controlled by NF-κB. Thus, cancer cells treated with kamebakaurin become susceptible to apoptosis [204]. Further, kamebakaurin causes downregulation of HIF-1α and its target gene levels, impairing cancer progression in vitro and in vivo [176]. Reduction of HIF-1α proteins took place without an alteration of mRNA levels and protein stability in CoCl2-treated colorectal cancer cells [176], suggesting the ability of kamebakaurin to inhibit translation of HIF-1α mRNA. The molecular mechanisms behind HIF-1 regulation are unknown. However, it is conceivable that NF-κB can be one of the critical mediators in kamebakaurin-mediated downregulation of HIF-1 (Figure 3 and Table 3).
4.3.4. Tanshinone IIA
Accumulating evidence has demonstrated the efficacy of tanshinone IIA against cancer. For instance, lipid peroxidation and ferroptotic cell death can be induced by tanshinone IIA in gastric cancer [205]. In addition, tanshinone IIA can trigger caspase activation and cell cycle arrest in breast cancer cells, along with a forceful inhibition of ERK, mTOR, and protein kinase C activities [206]. Evidence from another study showed that tanshinone IIA negatively modulates both HIF-1α and VEGF levels via hampering the mTOR signaling pathway under normoxic and hypoxic conditions in vitro [181] (Figure 3 and Table 3). Tanshinone IIA indeed showed anti-angiogenesis and cancer growth suppression potency in vivo [181].
4.3.5. Triptolide
Diverse cellular events, including apoptosis, cellular senescence, and EMT, are influenced by triptolide [207,208,209], connoting its therapeutic benefit against cancer. Further, triptolide can attain its anti-pancreatic cancer activity via imposing limits on HIF-1α expression in vitro and in vivo [184]. MYC is downregulated by triptolide at the transcription level [184], suggesting the high likelihood of MYC involvement in HIF-1α regulation (Figure 3 and Table 3).
4.4. Triterpenes
4.4.1. Balanophorin B
In hepatocellular carcinoma, the expression of HIF-1α and its target genes LDHA and hexokinase 2 (HK2) is inhibited by balanophorin B under hypoxia, resulting in the suppression of glycolysis in vitro. Moreover, balanophorin B retards cancer growth without inducing normal tissue toxicity in vivo [168]. In their study, balanophorin B was noticed to augment the expression of VHL and PHD2 without a change in HIF-1α mRNA levels, suggesting post-transcriptional regulation of HIF-1α [168] (Figure 3 and Table 3). Balanophorin B deserves further investigation to explore signaling pathways associated with HIF-1α regulation and to uncover other mechanisms by which balanophorin B exerts anti-cancer activity.
4.4.2. Betulinic Acid
The anti-cancer activity of betulinic acid occurs through the regulation of several events, such as apoptosis and metastasis [210,211]. Of note, betulinic acid can control stemness and drug resistance [212,213], suggesting that betulinic acid is one of the potential candidate agents for cancer treatments. Moreover, it was presented that HIF-1α accumulation is weakened by betulinic acid, leading to a diminution of HIF-1α responsive genes such as VEGF and GLUT1 in hypoxic cervical cancer cells [169]. In this study, it was suggested that betulinic acid inhibits HIF-1α accumulation by activating proteasome. Such proteasome activation may be mediated by NRF2, which can upregulate the level of several proteasome genes and is activated by betulinic acid [214,215] (Figure 3 and Table 3). Further investigation is required to disclose the mechanisms of proteasome activation by betulinic acid.
4.4.3. Celastrol
Celastrol has been determined to adversely affect cancer progression and metastasis in multiple types of cancer [216]. The findings from mechanism studies revealed that celastrol is able to inhibit VEGF expression, PI3K/AKT/mTOR, and NF-κB signaling [217]. In glioblastoma, celastrol inhibits cell viability as well as the migratory and invasive capacities of cancer cells in vitro [171]. The findings from in vivo experiments showed that celastrol limits glioblastoma infiltration. Celastrol suppresses angiogenesis, vasculogenic mimicry formation (VMF), and the level of angiogenesis- and VMF-promoting factors, such as VEGF, EPH receptor A2 (EPHA2), and cadherin 5 (CDH5, also called VE-cadherin). Mechanistically, celastrol blocks the PI3K/AKT/mTOR pathway and reduces the expression of HIF-1α [171]. Both EPHA2 and CDH5 can be positively regulated by HIF-1α [218,219]. Therefore, celastrol may downregulate angiogenesis and VMF via the PI3K/AKT/mTOR/HIF-1α pathway in glioblastoma (Figure 3 and Table 3).
4.4.4. Ilexgenin A and Panaxadiol
Ilexgenin A has been shown to repress melanoma via inducing cell cycle arrest and exerting anti-hepatocellular carcinoma activity by inhibiting the PI3K and STAT3 pathways [220,221]. Of note, the combination of ilexgenin A and sorafenib has synergistic effects on hepatocellular carcinoma growth [221]. This finding can provide a possibility to develop a novel treatment strategy against hepatocellular carcinoma. Moreover, ilexgenin A inhibits HIF-1α expression, consequently downregulating sterol regulatory element-binding transcription factor 1 (SREBF1) expression and lipid accumulation in colorectal cancer cells [175] (Figure 3 and Table 3). Treatment of cancer cells with ilexgenin A reduces cell viability and mRNA levels of β-catenin and TNF, suggesting that ilexgenin A acts by disturbing multiple signaling events. Ilexgenin A attenuates colitis-induced carcinogenesis in conjunction with a reduction of HIF-1α and SREBF1 levels in vivo [175]. These findings demonstrate that ilexgenin A possesses an anti-carcinogenic activity and impedes the progression of cancer.
In colorectal cancer cells, panaxadiol suppresses HIF-1α expression via the PI3K/AKT pathway under hypoxia [178] (Figure 3 and Table 3). In addition, panaxadiol was noticed to inhibit PD-L1, thereby restoring the cytotoxic activity of T cells against cancer cells in vitro. As expected, the growth of colorectal cancer is effectively hampered by panaxadiol in vivo [178]. Findings from this study may provide the basis for developing panaxadiol as a HIF-1α/PD-L1 inhibitor to treat colorectal cancer.
4.4.5. Pomolic Acid
Increasing evidence demonstrated that pomolic acid exerts anti-cancer activity by inducing apoptotic cell death and inhibiting invasion and metastasis [222,223,224]. Pomolic acid also mitigates multidrug resistance via inhibiting ABCB1 activity [225]. In breast cancer, pomolic acid was discerned to abolish the stimulatory effect of EGF on HIF-1α and VEGF expression [179]. It was additionally indicated that the negative effects of pomolic acid on EGF-induced HIF-1α and VEGF accumulation is due to its repressive action on PI3K/AKT/mTOR signaling and p38 MAPK activity [179] (Figure 3 and Table 3).
4.4.6. Pristimerin
In cancer cells, sphingosine kinase 1 (SPHK1) is activated by reactive oxygen species (ROS) and increases AKT activity under hypoxia, eventually stabilizing HIF-1α proteins [226]. Lately, hypoxia-induced SPHK1 was noticed to be significantly suppressed by pristimerin in prostate cancer cells, resulting in a downregulation of AKT activity and HIF-1α expression [180] (Figure 3 and Table 3). Unsurprisingly, cell viability and VEGF levels are restrained by pristimerin under hypoxia [180]. SPHK1 is also known to upmodulate HIF-2α expression under hypoxia [227]. Thus, it seems probable that pristimerin controls hypoxia signaling via limiting both HIF-1α and HIF-2α.
4.4.7. Theasaponin E1
The Notch pathway generally prevents apoptotic cell death through activating AKT [228]. Inhibition of this pathway leads to the enhancement of anti-cancer drug efficacy by promoting growth inhibition, cell cycle arrest, and apoptotic cell death [229]. Theasaponin E1 showed effective growth inhibition in several types of cancer, including breast, uterus, and gastric cancer [230]. Moreover, theasaponin E1 depresses Notch signaling, AKT activation, and HIF-1α levels, suggesting that HIF-1α can be partly regulated by the Notch/AKT axis in theasaponin E1-treated cells [182] (Figure 3 and Table 3). Theasaponin E1 can inhibit angiogenesis and cause apoptosis via activating caspases, cell cycle arrest, and migration in cisplatin-resistant ovarian cancer cells. In contrast, low cytotoxicity of theasaponin E1 was observed in normal cells [182], indicating its selective cytotoxicity towards ovarian cancer cells.
4.4.8. Ursolic Acid
Multiple studies have shown that ursolic acid effectively alleviates therapeutic resistance in cancer. Oxaliplatin-induced apoptosis is enhanced by ursolic acid in colorectal cancer cells [231]. Ursolic acid reverses paclitaxel resistance by upregulating miR-149–5p, a tumor-suppressive miRNA, in breast cancer cells [232]. In addition, ursolic acid can counter therapeutic resistance, owing to its capability to inhibit HIF-1α levels. The expression of both HIF-1α and ABCB1 is reduced by ursolic acid in hypoxic colorectal cancer cells. Ursolic acid thereby sensitizes hypoxic cells to 5-fluorouracil and augments 5-fluorouracil-induced apoptosis [185]. Another study demonstrated that radio-resistance of HIF-1α-overexpressing lung cancer cells is weakened by ursolic acid treatment [186]. Moreover, ursolic acid can deactivate PI3K/Akt signaling, bringing about downregulation of HIF-1α and ABCG2 levels in hypoxic ovarian cancer stem cells [187] (Figure 3 and Table 3). Further, ursolic acid downmodulates the expression of stemness factors, such as NANOG, CD44, octamer-binding protein 4 (OCT4), and prominin-like protein 1 (PROM1, also named CD133), and enhances the efficacy of cisplatin under hypoxia [187]. These results imply that ursolic acid may strengthen the anti-cancer effect of other therapeutic agents by altering drug efflux and cancer stemness.
5. Conclusions
Accumulated evidence introduced here showed that phytochemicals can be used as potent HIF-1α inhibitors and that the suppression of HIF-1α can reinforce the efficiency of cancer treatments, such as chemotherapy and radiation therapy. These findings suggest that phytochemicals are substantial sources of new HIF-1α inhibitors. Since Y6 and ursolic acid can restrict HIF-1α expression in both normoxic and hypoxic conditions, they may potentially block HIF-1α-related signaling in cancer. Furthermore, verbascoside and pristimerin can act as dual HIF-1α and HIF-2α inhibitors. In this regard, the development of phytochemical-based treatment has a considerable potentiality to improve therapeutic benefits.
Even though phytochemicals possess anti-cancer properties, cellular protection mechanisms, such as autophagy and the induction of efflux pumps, can be actuated by them. These findings imply the inevitable emergence of resistance towards phytochemicals. Accordingly, the development of an optimal combination of phytochemicals with other autophagy inhibitors can be one of the beneficial strategies against cancer. A deep understanding of molecular mechanisms is necessary to move phytochemicals from preclinical tests to clinical trials and then clinical practice in the future.
Supplementary Materials
Supplementary Materials can be found at https://www.mdpi.com/article/10.3390/ijms22189819/s1. Table S1. The structure, source, and clinical trial status of phytochemicals.
Author Contributions
Conceptualization, B.D.Y. and J.K.P.; literature review and visualization, B.D.Y., S.W.S., S.Y.C., H.J.K., T.-J.O. and J.K.P.; writing—original draft preparation, B.D.Y. and J.K.P.; writing—review and editing, J.K.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the National Research Foundation of Korea (NRF). This grant was funded by the Korean government (MSIT) (2019R1A2C1089710) (J.K.P.) (2019R1A2B5B02070524) (H.J.K.) and the Basic Science Research Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Education (2019R1A6A1A11036849) (S.Y.C.).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tirpe A.A., Gulei D., Ciortea S.M., Crivii C., Berindan-Neagoe I. Hypoxia: Overview on hypoxia-mediated mechanisms with a focus on the role of hif genes. Int. J. Mol. Sci. 2019;20:6140. doi: 10.3390/ijms20246140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liao C., Zhang Q. Understanding the oxygen-sensing pathway and its therapeutic implications in diseases. Am. J. Pathol. 2020;190:1584–1595. doi: 10.1016/j.ajpath.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joshi S., Singh A.R., Durden D.L. Mdm2 regulates hypoxic hypoxia-inducible factor 1alpha stability in an e3 ligase, proteasome, and pten-phosphatidylinositol 3-kinase-akt-dependent manner. J. Biol. Chem. 2014;289:22785–22797. doi: 10.1074/jbc.M114.587493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pore N., Jiang Z., Shu H.K., Bernhard E., Kao G.D., Maity A. Akt1 activation can augment hypoxia-inducible factor-1alpha expression by increasing protein translation through a mammalian target of rapamycin-independent pathway. Mol. Cancer Res. 2006;4:471–479. doi: 10.1158/1541-7786.MCR-05-0234. [DOI] [PubMed] [Google Scholar]
- 5.Cao Y., Eble J.M., Moon E., Yuan H., Weitzel D.H., Landon C.D., Nien C.Y., Hanna G., Rich J.N., Provenzale J.M., et al. Tumor cells upregulate normoxic hif-1alpha in response to doxorubicin. Cancer Res. 2013;73:6230–6242. doi: 10.1158/0008-5472.CAN-12-1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moniz S., Bandarra D., Biddlestone J., Campbell K.J., Komander D., Bremm A., Rocha S. Cezanne regulates e2f1-dependent hif2alpha expression. J. Cell Sci. 2015;128:3082–3093. doi: 10.1242/jcs.168864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Son S.W., Yun B.D., Song M.G., Lee J.K., Choi S.Y., Kuh H.J., Park J.K. The hypoxia-long noncoding rna interaction in solid cancers. Int. J. Mol. Sci. 2021;22:7261. doi: 10.3390/ijms22147261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poon E., Harris A.L., Ashcroft M. Targeting the hypoxia-inducible factor (hif) pathway in cancer. Expert Rev. Mol. Med. 2009;11:e26. doi: 10.1017/S1462399409001173. [DOI] [PubMed] [Google Scholar]
- 9.Bertout J.A., Majmundar A.J., Gordan J.D., Lam J.C., Ditsworth D., Keith B., Brown E.J., Nathanson K.L., Simon M.C. Hif2alpha inhibition promotes p53 pathway activity, tumor cell death, and radiation responses. Proc. Natl. Acad. Sci. USA. 2009;106:14391–14396. doi: 10.1073/pnas.0907357106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nardinocchi L., Puca R., D’Orazi G. Hif-1alpha antagonizes p53-mediated apoptosis by triggering hipk2 degradation. Aging. 2011;3:33–43. doi: 10.18632/aging.100254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X., Dong J., Jia L., Zhao T., Lang M., Li Z., Lan C., Li X., Hao J., Wang H., et al. Hif-2-dependent expression of stem cell factor promotes metastasis in hepatocellular carcinoma. Cancer Lett. 2017;393:113–124. doi: 10.1016/j.canlet.2017.01.032. [DOI] [PubMed] [Google Scholar]
- 12.Zhang L., Huang G., Li X., Zhang Y., Jiang Y., Shen J., Liu J., Wang Q., Zhu J., Feng X., et al. Hypoxia induces epithelial-mesenchymal transition via activation of snai1 by hypoxia-inducible factor -1alpha in hepatocellular carcinoma. BMC Cancer. 2013;13:108. doi: 10.1186/1471-2407-13-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choueiri T.K., Kaelin W.G., Jr. Targeting the hif2-vegf axis in renal cell carcinoma. Nat. Med. 2020;26:1519–1530. doi: 10.1038/s41591-020-1093-z. [DOI] [PubMed] [Google Scholar]
- 14.Ravi R., Mookerjee B., Bhujwalla Z.M., Sutter C.H., Artemov D., Zeng Q., Dillehay L.E., Madan A., Semenza G.L., Bedi A. Regulation of tumor angiogenesis by p53-induced degradation of hypoxia-inducible factor 1alpha. Genes Dev. 2000;14:34–44. [PMC free article] [PubMed] [Google Scholar]
- 15.Meijer T.W., Kaanders J.H., Span P.N., Bussink J. Targeting hypoxia, hif-1, and tumor glucose metabolism to improve radiotherapy efficacy. Clin. Cancer Res. 2012;18:5585–5594. doi: 10.1158/1078-0432.CCR-12-0858. [DOI] [PubMed] [Google Scholar]
- 16.Samanta D., Gilkes D.M., Chaturvedi P., Xiang L., Semenza G.L. Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cells. Proc. Natl. Acad. Sci. USA. 2014;111:E5429–E5438. doi: 10.1073/pnas.1421438111. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Noman M.Z., Desantis G., Janji B., Hasmim M., Karray S., Dessen P., Bronte V., Chouaib S. Pd-l1 is a novel direct target of hif-1alpha, and its blockade under hypoxia enhanced mdsc-mediated t cell activation. J. Exp. Med. 2014;211:781–790. doi: 10.1084/jem.20131916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imtiyaz H.Z., Williams E.P., Hickey M.M., Patel S.A., Durham A.C., Yuan L.J., Hammond R., Gimotty P.A., Keith B., Simon M.C. Hypoxia-inducible factor 2alpha regulates macrophage function in mouse models of acute and tumor inflammation. J. Clin. Investig. 2010;120:2699–2714. doi: 10.1172/JCI39506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talks K.L., Turley H., Gatter K.C., Maxwell P.H., Pugh C.W., Ratcliffe P.J., Harris A.L. The expression and distribution of the hypoxia-inducible factors hif-1alpha and hif-2alpha in normal human tissues, cancers, and tumor-associated macrophages. Am. J. Pathol. 2000;157:411–421. doi: 10.1016/S0002-9440(10)64554-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y.M., Ying S.P., Huang Y.R., Pan Y., Chen W.J., Ni L.Q., Xu J.Y., Shen Q.Y., Liang Y. Expression of hif-1alpha and hif-2alpha correlates to biological and clinical significance in papillary thyroid carcinoma. World J. Surg. Oncol. 2016;14:30. doi: 10.1186/s12957-016-0785-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L., Chen Q., Hu J., Chen Y., Liu C., Xu C. Expression of hif-2alpha and vegf in cervical squamous cell carcinoma and its clinical significance. Biomed. Res. Int. 2016;2016:5631935. doi: 10.1155/2016/5631935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreno Roig E., Groot A.J., Yaromina A., Hendrickx T.C., Barbeau L.M.O., Giuranno L., Dams G., Ient J., Olivo Pimentel V., Van Gisbergen M.W., et al. Hif-1alpha and hif-2alpha differently regulate the radiation sensitivity of nsclc cells. Cells. 2019;8:45. doi: 10.3390/cells8010045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isono T., Chano T., Yoshida T., Kageyama S., Kawauchi A., Suzaki M., Yuasa T. Hydroxyl-hif2-alpha is potential therapeutic target for renal cell carcinomas. Am. J. Cancer Res. 2016;6:2263–2276. [PMC free article] [PubMed] [Google Scholar]
- 24.Downes N.L., Laham-Karam N., Kaikkonen M.U., Yla-Herttuala S. Differential but complementary hif1alpha and hif2alpha transcriptional regulation. Mol. Ther. 2018;26:1735–1745. doi: 10.1016/j.ymthe.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loboda A., Jozkowicz A., Dulak J. Hif-1 and hif-2 transcription factors--similar but not identical. Mol. Cells. 2010;29:435–442. doi: 10.1007/s10059-010-0067-2. [DOI] [PubMed] [Google Scholar]
- 26.Hoefflin R., Harlander S., Schafer S., Metzger P., Kuo F., Schonenberger D., Adlesic M., Peighambari A., Seidel P., Chen C.Y., et al. Hif-1alpha and hif-2alpha differently regulate tumour development and inflammation of clear cell renal cell carcinoma in mice. Nat. Commun. 2020;11:4111. doi: 10.1038/s41467-020-17873-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Son S.W., Lee H.Y., Moeng S., Kuh H.J., Choi S.Y., Park J.K. Participation of micrornas in the treatment of cancer with phytochemicals. Molecules. 2020;25:4701. doi: 10.3390/molecules25204701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montane X., Kowalczyk O., Reig-Vano B., Bajek A., Roszkowski K., Tomczyk R., Pawliszak W., Giamberini M., Mocek-Plociniak A., Tylkowski B. Current perspectives of the applications of polyphenols and flavonoids in cancer therapy. Molecules. 2020;25:3342. doi: 10.3390/molecules25153342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitra T., Bhattacharya R. Phytochemicals modulate cancer aggressiveness: A review depicting the anticancer efficacy of dietary polyphenols and their combinations. J. Cell Physiol. 2020;235:7696–7708. doi: 10.1002/jcp.29703. [DOI] [PubMed] [Google Scholar]
- 30.Chen Y.X., Gao Q.Y., Zou T.H., Wang B.M., Liu S.D., Sheng J.Q., Ren J.L., Zou X.P., Liu Z.J., Song Y.Y., et al. Berberine versus placebo for the prevention of recurrence of colorectal adenoma: A multicentre, double-blinded, randomised controlled study. Lancet Gastroenterol. Hepatol. 2020;5:267–275. doi: 10.1016/S2468-1253(19)30409-1. [DOI] [PubMed] [Google Scholar]
- 31.Chen Q., Qin R., Fang Y., Li H. Berberine sensitizes human ovarian cancer cells to cisplatin through mir-93/pten/akt signaling pathway. Cell Physiol. Biochem. 2015;36:956–965. doi: 10.1159/000430270. [DOI] [PubMed] [Google Scholar]
- 32.Qian K., Tang C.Y., Chen L.Y., Zheng S., Zhao Y., Ma L.S., Xu L., Fan L.H., Yu J.D., Tan H.S., et al. Berberine reverses breast cancer multidrug resistance based on fluorescence pharmacokinetics in vitro and in vivo. ACS Omega. 2021;6:10645–10654. doi: 10.1021/acsomega.0c06288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan Y., Shao D., Zhao Y., Zhang F., Zheng X., Tan Y., He K., Li J., Chen L. Berberine reverses hypoxia-induced chemoresistance in breast cancer through the inhibition of ampk- hif-1alpha. Int. J. Biol. Sci. 2017;13:794–803. doi: 10.7150/ijbs.18969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu L., Shi Q., Jin Y., Liu Z., Li J., Sun W. Blockage of ampk-ulk1 pathway mediated autophagy promotes cell apoptosis to increase doxorubicin sensitivity in breast cancer (bc) cells: An in vitro study. BMC Cancer. 2021;21:195. doi: 10.1186/s12885-021-07901-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Satoh K. Ampkalpha2 regulates hypoxia-inducible factor-1alpha stability and neutrophil survival to promote vascular repair after ischemia. Circ. Res. 2017;120:8–10. doi: 10.1161/CIRCRESAHA.116.310217. [DOI] [PubMed] [Google Scholar]
- 36.Kalainayakan S.P., Ghosh P., Dey S., Fitzgerald K.E., Sohoni S., Konduri P.C., Garrossian M., Liu L., Zhang L. Cyclopamine tartrate, a modulator of hedgehog signaling and mitochondrial respiration, effectively arrests lung tumor growth and progression. Sci. Rep. 2019;9:1405. doi: 10.1038/s41598-018-38345-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J.Y., Wang Z., Li M.Y., Zhang Z., Mi C., Zuo H.X., Xing Y., Wu Y.L., Lian L.H., Xu G.H., et al. Dictamnine promotes apoptosis and inhibits epithelial-mesenchymal transition, migration, invasion and proliferation by downregulating the hif-1alpha and slug signaling pathways. Chem. Biol. Interact. 2018;296:134–144. doi: 10.1016/j.cbi.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 38.Liu R.M., Xu P., Chen Q., Feng S.L., Xie Y. A multiple-targets alkaloid nuciferine overcomes paclitaxel-induced drug resistance in vitro and in vivo. Phytomedicine. 2020;79:153342. doi: 10.1016/j.phymed.2020.153342. [DOI] [PubMed] [Google Scholar]
- 39.Su Q., Wang J., Fan M., Ghauri M.A., Ullah A., Wang B., Dai B., Zhan Y., Zhang D., Zhang Y. Sanguinarine disrupts the colocalization and interaction of hif-1alpha with tyrosine and serine phosphorylated-stat3 in breast cancer. J. Cell Mol. Med. 2020;24:3756–3761. doi: 10.1111/jcmm.15056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Su Q., Wang J., Wu Q., Ullah A., Ghauri M.A., Sarwar A., Chen L., Liu F., Zhang Y. Sanguinarine combats hypoxia-induced activation of ephb4 and hif-1alpha pathways in breast cancer. Phytomedicine. 2021;84:153503. doi: 10.1016/j.phymed.2021.153503. [DOI] [PubMed] [Google Scholar]
- 41.Su Q., Fan M., Wang J., Ullah A., Ghauri M.A., Dai B., Zhan Y., Zhang D., Zhang Y. Sanguinarine inhibits epithelial-mesenchymal transition via targeting hif-1alpha/tgf-beta feed-forward loop in hepatocellular carcinoma. Cell Death Dis. 2019;10:939. doi: 10.1038/s41419-019-2173-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Z., Zhao L., Zhao F., Yang G., Wang J.J. Tetrandrine suppresses lung cancer growth and induces apoptosis, potentially via the vegf/hif-1alpha/icam-1 signaling pathway. Oncol. Lett. 2018;15:7433–7437. doi: 10.3892/ol.2018.8190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wei Z., Shan Y., Tao L., Liu Y., Zhu Z., Liu Z., Wu Y., Chen W., Wang A., Lu Y. Diallyl trisulfides, a natural histone deacetylase inhibitor, attenuate hif-1alpha synthesis, and decreases breast cancer metastasis. Mol. Carcinog. 2017;56:2317–2331. doi: 10.1002/mc.22686. [DOI] [PubMed] [Google Scholar]
- 44.Xia Y., Kang T.W., Jung Y.D., Zhang C., Lian S. Sulforaphane inhibits nonmuscle invasive bladder cancer cells proliferation through suppression of hif-1alpha-mediated glycolysis in hypoxia. J. Agric. Food Chem. 2019;67:7844–7854. doi: 10.1021/acs.jafc.9b03027. [DOI] [PubMed] [Google Scholar]
- 45.Liu P., Atkinson S.J., Akbareian S.E., Zhou Z., Munsterberg A., Robinson S.D., Bao Y. Sulforaphane exerts anti-angiogenesis effects against hepatocellular carcinoma through inhibition of stat3/hif-1alpha/vegf signalling. Sci. Rep. 2017;7:12651. doi: 10.1038/s41598-017-12855-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nys K., Van Laethem A., Michiels C., Rubio N., Piette J.G., Garmyn M., Agostinis P. A p38(mapk)/hif-1 pathway initiated by uvb irradiation is required to induce noxa and apoptosis of human keratinocytes. J. Investig. Dermatol. 2010;130:2269–2276. doi: 10.1038/jid.2010.93. [DOI] [PubMed] [Google Scholar]
- 47.Khandrika L., Lieberman R., Koul S., Kumar B., Maroni P., Chandhoke R., Meacham R.B., Koul H.K. Hypoxia-associated p38 mitogen-activated protein kinase-mediated androgen receptor activation and increased hif-1alpha levels contribute to emergence of an aggressive phenotype in prostate cancer. Oncogene. 2009;28:1248–1260. doi: 10.1038/onc.2008.476. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 48.An F.F., Liu Y.C., Zhang W.W., Liang L. Dihydroartemisinine enhances dictamnine-induced apoptosis via a caspase dependent pathway in human lung adenocarcinoma a549 cells. Asian Pac. J. Cancer Prev. 2013;14:5895–5900. doi: 10.7314/APJCP.2013.14.10.5895. [DOI] [PubMed] [Google Scholar]
- 49.Li Z., Chen Y., An T., Liu P., Zhu J., Yang H., Zhang W., Dong T., Jiang J., Zhang Y., et al. Nuciferine inhibits the progression of glioblastoma by suppressing the sox2-akt/stat3-slug signaling pathway. J. Exp. Clin. Cancer Res. 2019;38:139. doi: 10.1186/s13046-019-1134-y. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 50.Qi Q., Li R., Li H.Y., Cao Y.B., Bai M., Fan X.J., Wang S.Y., Zhang B., Li S. Identification of the anti-tumor activity and mechanisms of nuciferine through a network pharmacology approach. Acta Pharmacol. Sin. 2016;37:963–972. doi: 10.1038/aps.2016.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu W., Yi D.D., Guo J.L., Xiang Z.X., Deng L.F., He L. Nuciferine, extracted from nelumbo nucifera gaertn, inhibits tumor-promoting effect of nicotine involving wnt/beta-catenin signaling in non-small cell lung cancer. J. Ethnopharmacol. 2015;165:83–93. doi: 10.1016/j.jep.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 52.Xia X., Wang Q., Ye T., Liu Y., Liu D., Song S., Zheng C. Nrf2/abcb1-mediated efflux and parp1-mediated dampening of DNA damage contribute to doxorubicin resistance in chronic hypoxic hepg2 cells. Fundam Clin. Pharmacol. 2020;34:41–50. doi: 10.1111/fcp.12505. [DOI] [PubMed] [Google Scholar]
- 53.Singh A., Wu H., Zhang P., Happel C., Ma J., Biswal S. Expression of abcg2 (bcrp) is regulated by nrf2 in cancer cells that confers side population and chemoresistance phenotype. Mol. Cancer Ther. 2010;9:2365–2376. doi: 10.1158/1535-7163.MCT-10-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He X., Wang J., Wei W., Shi M., Xin B., Zhang T., Shen X. Hypoxia regulates abcg2 activity through the activivation of erk1/2/hif-1alpha and contributes to chemoresistance in pancreatic cancer cells. Cancer Biol. Ther. 2016;17:188–198. doi: 10.1080/15384047.2016.1139228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wartenberg M., Ling F.C., Muschen M., Klein F., Acker H., Gassmann M., Petrat K., Putz V., Hescheler J., Sauer H. Regulation of the multidrug resistance transporter p-glycoprotein in multicellular tumor spheroids by hypoxia-inducible factor (hif-1) and reactive oxygen species. FASEB J. 2003;17:503–505. doi: 10.1096/fj.02-0358fje. [DOI] [PubMed] [Google Scholar]
- 56.Jung J.E., Kim H.S., Lee C.S., Shin Y.J., Kim Y.N., Kang G.H., Kim T.Y., Juhnn Y.S., Kim S.J., Park J.W., et al. Stat3 inhibits the degradation of hif-1alpha by pvhl-mediated ubiquitination. Exp. Mol. Med. 2008;40:479–485. doi: 10.3858/emm.2008.40.5.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pawlus M.R., Wang L., Hu C.J. Stat3 and hif1alpha cooperatively activate hif1 target genes in mda-mb-231 and rcc4 cells. Oncogene. 2014;33:1670–1679. doi: 10.1038/onc.2013.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bai X.Y., Liu Y.G., Song W., Li Y.Y., Hou D.S., Luo H.M., Liu P. Anticancer activity of tetrandrine by inducing pro-death apoptosis and autophagy in human gastric cancer cells. J. Pharm. Pharmacol. 2018;70:1048–1058. doi: 10.1111/jphp.12935. [DOI] [PubMed] [Google Scholar]
- 59.Zhang Z., Liu T., Yu M., Li K., Li W. The plant alkaloid tetrandrine inhibits metastasis via autophagy-dependent wnt/beta-catenin and metastatic tumor antigen 1 signaling in human liver cancer cells. J. Exp. Clin. Cancer Res. 2018;37:7. doi: 10.1186/s13046-018-0678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ye L.Y., Hu S., Xu H.E., Xu R.R., Kong H., Zeng X.N., Xie W.P., Wang H. The effect of tetrandrine combined with cisplatin on proliferation and apoptosis of a549/ddp cells and a549 cells. Cancer Cell Int. 2017;17:40. doi: 10.1186/s12935-017-0410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang H., Wong C.C., Wei H., Gilkes D.M., Korangath P., Chaturvedi P., Schito L., Chen J., Krishnamachary B., Winnard P.T., Jr., et al. Hif-1-dependent expression of angiopoietin-like 4 and l1cam mediates vascular metastasis of hypoxic breast cancer cells to the lungs. Oncogene. 2012;31:1757–1770. doi: 10.1038/onc.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 62.Ji F., Wang Y., Qiu L., Li S., Zhu J., Liang Z., Wan Y., Di W. Hypoxia inducible factor 1alpha-mediated lox expression correlates with migration and invasion in epithelial ovarian cancer. Int. J. Oncol. 2013;42:1578–1588. doi: 10.3892/ijo.2013.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wong C.C., Gilkes D.M., Zhang H., Chen J., Wei H., Chaturvedi P., Fraley S.I., Wong C.M., Khoo U.S., Ng I.O., et al. Hypoxia-inducible factor 1 is a master regulator of breast cancer metastatic niche formation. Proc. Natl. Acad. Sci. USA. 2011;108:16369–16374. doi: 10.1073/pnas.1113483108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xiao D., Singh S.V. Diallyl trisulfide, a constituent of processed garlic, inactivates akt to trigger mitochondrial translocation of bad and caspase-mediated apoptosis in human prostate cancer cells. Carcinogenesis. 2006;27:533–540. doi: 10.1093/carcin/bgi228. [DOI] [PubMed] [Google Scholar]
- 65.Xiao X., Chen B., Liu X., Liu P., Zheng G., Ye F., Tang H., Xie X. Diallyl disulfide suppresses src/ras/erk signaling-mediated proliferation and metastasis in human breast cancer by up-regulating mir-34a. PLoS ONE. 2014;9:e112720. doi: 10.1371/journal.pone.0112720. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 66.Li Z., Zhou W., Zhang Y., Sun W., Yung M.M.H., Sun J., Li J., Chen C.W., Li Z., Meng Y., et al. Erk regulates hif1alpha-mediated platinum resistance by directly targeting phd2 in ovarian cancer. Clin. Cancer Res. 2019;25:5947–5960. doi: 10.1158/1078-0432.CCR-18-4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singh A.V., Xiao D., Lew K.L., Dhir R., Singh S.V. Sulforaphane induces caspase-mediated apoptosis in cultured pc-3 human prostate cancer cells and retards growth of pc-3 xenografts in vivo. Carcinogenesis. 2004;25:83–90. doi: 10.1093/carcin/bgg178. [DOI] [PubMed] [Google Scholar]
- 68.Castro N.P., Rangel M.C., Merchant A.S., MacKinnon G., Cuttitta F., Salomon D.S., Kim Y.S. Sulforaphane suppresses the growth of triple-negative breast cancer stem-like cells in vitro and in vivo. Cancer Prev Res. 2019;12:147–158. doi: 10.1158/1940-6207.CAPR-18-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu C.M., Peng C.Y., Liao Y.W., Lu M.Y., Tsai M.L., Yeh J.C., Yu C.H., Yu C.C. Sulforaphane targets cancer stemness and tumor initiating properties in oral squamous cell carcinomas via mir-200c induction. J. Formos. Med. Assoc. 2017;116:41–48. doi: 10.1016/j.jfma.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 70.Chang C.C., Wu M.J., Yang J.Y., Camarillo I.G., Chang C.J. Leptin-stat3-g9a signaling promotes obesity-mediated breast cancer progression. Cancer Res. 2015;75:2375–2386. doi: 10.1158/0008-5472.CAN-14-3076. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 71.Byun Y., Choi Y.C., Jeong Y., Lee G., Yoon S., Jeong Y., Yoon J., Baek K. Mir-200c downregulates hif-1alpha and inhibits migration of lung cancer cells. Cell Mol. Biol. Lett. 2019;24:28. doi: 10.1186/s11658-019-0152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin C.C., Chuang Y.J., Yu C.C., Yang J.S., Lu C.C., Chiang J.H., Lin J.P., Tang N.Y., Huang A.C., Chung J.G. Apigenin induces apoptosis through mitochondrial dysfunction in u-2 os human osteosarcoma cells and inhibits osteosarcoma xenograft tumor growth in vivo. J. Agric. Food Chem. 2012;60:11395–11402. doi: 10.1021/jf303446x. [DOI] [PubMed] [Google Scholar]
- 73.Zhu Y., Mao Y., Chen H., Lin Y., Hu Z., Wu J., Xu X., Xu X., Qin J., Xie L. Apigenin promotes apoptosis, inhibits invasion and induces cell cycle arrest of t24 human bladder cancer cells. Cancer Cell Int. 2013;13:54. doi: 10.1186/1475-2867-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dai J., Van Wie P.G., Fai L.Y., Kim D., Wang L., Poyil P., Luo J., Zhang Z. Downregulation of nedd9 by apigenin suppresses migration, invasion, and metastasis of colorectal cancer cells. Toxicol. Appl. Pharmacol. 2016;311:106–112. doi: 10.1016/j.taap.2016.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Villalobos-Ayala K., Ortiz Rivera I., Alvarez C., Husain K., DeLoach D., Krystal G., Hibbs M.L., Jiang K., Ghansah T. Apigenin increases ship-1 expression, promotes tumoricidal macrophages and anti-tumor immune responses in murine pancreatic cancer. Cancers. 2020;12:3631. doi: 10.3390/cancers12123631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fang J., Zhou Q., Liu L.Z., Xia C., Hu X., Shi X., Jiang B.H. Apigenin inhibits tumor angiogenesis through decreasing hif-1alpha and vegf expression. Carcinogenesis. 2007;28:858–864. doi: 10.1093/carcin/bgl205. [DOI] [PubMed] [Google Scholar]
- 77.Ketkaew Y., Osathanon T., Pavasant P., Sooampon S. Apigenin inhibited hypoxia induced stem cell marker expression in a head and neck squamous cell carcinoma cell line. Arch. Oral Biol. 2017;74:69–74. doi: 10.1016/j.archoralbio.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 78.Yoshida T., Hashimura M., Mastumoto T., Tazo Y., Inoue H., Kuwata T., Saegusa M. Transcriptional upregulation of hif-1alpha by nf-kappab/p65 and its associations with beta-catenin/p300 complexes in endometrial carcinoma cells. Lab. Investig. 2013;93:1184–1193. doi: 10.1038/labinvest.2013.111. [DOI] [PubMed] [Google Scholar]
- 79.Zhou J., Callapina M., Goodall G.J., Brune B. Functional integrity of nuclear factor kappab, phosphatidylinositol 3’-kinase, and mitogen-activated protein kinase signaling allows tumor necrosis factor alpha-evoked bcl-2 expression to provoke internal ribosome entry site-dependent translation of hypoxia-inducible factor 1alpha. Cancer Res. 2004;64:9041–9048. doi: 10.1158/0008-5472.CAN-04-1437. [DOI] [PubMed] [Google Scholar]
- 80.Tong X., Pelling J.C. Targeting the pi3k/akt/mtor axis by apigenin for cancer prevention. Anticancer Agents Med. Chem. 2013;13:971–978. doi: 10.2174/18715206113139990119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Qin Y., Zhao D., Zhou H.G., Wang X.H., Zhong W.L., Chen S., Gu W.G., Wang W., Zhang C.H., Liu Y.R., et al. Apigenin inhibits nf-kappab and snail signaling, emt and metastasis in human hepatocellular carcinoma. Oncotarget. 2016;7:41421–41431. doi: 10.18632/oncotarget.9404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jin J., Qiu S., Wang P., Liang X., Huang F., Wu H., Zhang B., Zhang W., Tian X., Xu R., et al. Cardamonin inhibits breast cancer growth by repressing hif-1alpha-dependent metabolic reprogramming. J. Exp. Clin. Cancer Res. 2019;38:377. doi: 10.1186/s13046-019-1351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luo H.Q., Xu M., Zhong W.T., Cui Z.Y., Liu F.M., Zhou K.Y., Li X.Y. Egcg decreases the expression of hif-1alpha and vegf and cell growth in mcf-7 breast cancer cells. J. BUON. 2014;19:435–439. [PubMed] [Google Scholar]
- 84.Guo Q., Lu L., Liao Y., Wang X., Zhang Y., Liu Y., Huang S., Sun H., Li Z., Zhao L. Influence of c-src on hypoxic resistance to paclitaxel in human ovarian cancer cells and reversal of fv-429. Cell Death Dis. 2018;8:e3178. doi: 10.1038/cddis.2017.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wei M., Ma R., Huang S., Liao Y., Ding Y., Li Z., Guo Q., Tan R., Zhang L., Zhao L. Oroxylin a increases the sensitivity of temozolomide on glioma cells by hypoxia-inducible factor 1alpha/hedgehog pathway under hypoxia. J. Cell Physiol. 2019;234:17392–17404. doi: 10.1002/jcp.28361. [DOI] [PubMed] [Google Scholar]
- 86.Liu Y., Wang X., Li W., Xu Y., Zhuo Y., Li M., He Y., Wang X., Guo Q., Zhao L., et al. Oroxylin a reverses hypoxia-induced cisplatin resistance through inhibiting hif-1alpha mediated xpc transcription. Oncogene. 2020;39:6893–6905. doi: 10.1038/s41388-020-01474-x. [DOI] [PubMed] [Google Scholar]
- 87.Wang S.J., Zhao J.K., Ren S., Sun W.W., Zhang W.J., Zhang J.N. Wogonin affects proliferation and the energy metabolism of sgc-7901 and a549 cells. Exp. Ther. Med. 2019;17:911–918. doi: 10.3892/etm.2018.7023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wen Y., Zhao R.Q., Zhang Y.K., Gupta P., Fu L.X., Tang A.Z., Liu B.M., Chen Z.S., Yang D.H., Liang G. Effect of y6, an epigallocatechin gallate derivative, on reversing doxorubicin drug resistance in human hepatocellular carcinoma cells. Oncotarget. 2017;8:29760–29770. doi: 10.18632/oncotarget.15964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liao Z.H., Zhu H.Q., Chen Y.Y., Chen R.L., Fu L.X., Li L., Zhou H., Zhou J.L., Liang G. The epigallocatechin gallate derivative y6 inhibits human hepatocellular carcinoma by inhibiting angiogenesis in mapk/erk1/2 and pi3k/akt/ hif-1alpha/vegf dependent pathways. J. Ethnopharmacol. 2020;259:112852. doi: 10.1016/j.jep.2020.112852. [DOI] [PubMed] [Google Scholar]
- 90.Kim D.H., Sung B., Kim J.A., Kang Y.J., Hwang S.Y., Hwang N.L., Suh H., Choi Y.H., Im E., Chung H.Y., et al. Hs-1793, a resveratrol analogue, downregulates the expression of hypoxia-induced hif-1 and vegf and inhibits tumor growth of human breast cancer cells in a nude mouse xenograft model. Int. J. Oncol. 2017;51:715–723. doi: 10.3892/ijo.2017.4058. [DOI] [PubMed] [Google Scholar]
- 91.Lai F., Liu Q., Liu X., Ji M., Xie P., Chen X. Lxy6090—A novel manassantin a derivative-limits breast cancer growth through hypoxia-inducible factor-1 inhibition. Onco. Targets Ther. 2016;9:3829–3840. doi: 10.2147/OTT.S106925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen M.C., Lee C.F., Huang W.H., Chou T.C. Magnolol suppresses hypoxia-induced angiogenesis via inhibition of hif-1alpha/vegf signaling pathway in human bladder cancer cells. Biochem. Pharmacol. 2013;85:1278–1287. doi: 10.1016/j.bcp.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 93.Kwak S.H., Stephenson T.N., Lee H.E., Ge Y., Lee H., Min S.M., Kim J.H., Kwon D.Y., Lee Y.M., Hong J. Evaluation of manassantin a tetrahydrofuran core region analogues and cooperative therapeutic effects with egfr inhibition. J. Med. Chem. 2020;63:6821–6833. doi: 10.1021/acs.jmedchem.0c00151. [DOI] [PubMed] [Google Scholar]
- 94.Aljabali A.A.A., Bakshi H.A., Hakkim F.L., Haggag Y.A., Al-Batanyeh K.M., Al Zoubi M.S., Al-Trad B., Nasef M.M., Satija S., Mehta M., et al. Albumin nano-encapsulation of piceatannol enhances its anticancer potential in colon cancer via downregulation of nuclear p65 and hif-1alpha. Cancers. 2020;12:113. doi: 10.3390/cancers12010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Butt N.A., Kumar A., Dhar S., Rimando A.M., Akhtar I., Hancock J.C., Lage J.M., Pound C.R., Lewin J.R., Gomez C.R., et al. Targeting mta1/hif-1alpha signaling by pterostilbene in combination with histone deacetylase inhibitor attenuates prostate cancer progression. Cancer Med. 2017;6:2673–2685. doi: 10.1002/cam4.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang H., Jia R., Lv T., Wang M., He S., Zhang X. Resveratrol suppresses tumor progression via inhibiting stat3/hif-1alpha/vegf pathway in an orthotopic rat model of non-small-cell lung cancer (nsclc) Onco. Targets Ther. 2020;13:7057–7063. doi: 10.2147/OTT.S259016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xu Q.H., Xiao Y., Li X.Q., Fan L., Zhou C.C., Cheng L., Jiang Z.D., Wang G.H. Resveratrol counteracts hypoxia-induced gastric cancer invasion and emt through hedgehog pathway suppression. Anticancer Agents Med. Chem. 2020;20:1105–1114. doi: 10.2174/1871520620666200402080034. [DOI] [PubMed] [Google Scholar]
- 98.Xiao Y., Qin T., Sun L., Qian W., Li J., Duan W., Lei J., Wang Z., Ma J., Li X., et al. Resveratrol ameliorates the malignant progression of pancreatic cancer by inhibiting hypoxia-induced pancreatic stellate cell activation. Cell Transplant. 2020;29:963689720929987. doi: 10.1177/0963689720929987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kim A., Ma J.Y. Rhaponticin decreases the metastatic and angiogenic abilities of cancer cells via suppression of the hif1alpha pathway. Int J. Oncol. 2018;53:1160–1170. doi: 10.3892/ijo.2018.4479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gong J., Zhou S., Yang S. Vanillic acid suppresses hif-1alpha expression via inhibition of mtor/p70s6k/4e-bp1 and raf/mek/erk pathways in human colon cancer hct116 cells. Int. J. Mol. Sci. 2019;20:465. doi: 10.3390/ijms20030465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Park J.J., Hwang S.J., Park J.H., Lee H.J. Chlorogenic acid inhibits hypoxia-induced angiogenesis via down-regulation of the hif-1alpha/akt pathway. Cell Oncol. 2015;38:111–118. doi: 10.1007/s13402-014-0216-2. [DOI] [PubMed] [Google Scholar]
- 102.Monteleone F., Taverna S., Alessandro R., Fontana S. Swath-ms based quantitative proteomics analysis reveals that curcumin alters the metabolic enzyme profile of cml cells by affecting the activity of mir-22/ipo7/hif-1alpha axis. J. Exp. Clin. Cancer Res. 2018;37:170. doi: 10.1186/s13046-018-0843-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ge Y., Yoon S.H., Jang H., Jeong J.H., Lee Y.M. Decursin promotes hif-1alpha proteasomal degradation and immune responses in hypoxic tumour microenvironment. Phytomedicine. 2020;78:153318. doi: 10.1016/j.phymed.2020.153318. [DOI] [PubMed] [Google Scholar]
- 104.Velatooru L.R., Vakamullu S., Penugurti V. Alpinoid c analog inhibits angiogenesis and induces apoptosis in colo205cell line. Chem. Biol. Interact. 2019;308:1–10. doi: 10.1016/j.cbi.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 105.Wang F., Zhang W., Guo L., Bao W., Jin N., Liu R., Liu P., Wang Y., Guo Q., Chen B. Gambogic acid suppresses hypoxia-induced hypoxia-inducible factor-1alpha/vascular endothelial growth factor expression via inhibiting phosphatidylinositol 3-kinase/akt/mammalian target protein of rapamycin pathway in multiple myeloma cells. Cancer Sci. 2014;105:1063–1070. doi: 10.1111/cas.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ranjbarnejad T., Saidijam M., Tafakh M.S., Pourjafar M., Talebzadeh F., Najafi R. Garcinol exhibits anti-proliferative activities by targeting microsomal prostaglandin e synthase-1 in human colon cancer cells. Hum. Exp. Toxicol. 2017;36:692–700. doi: 10.1177/0960327116660865. [DOI] [PubMed] [Google Scholar]
- 107.Mi C., Ma J., Wang K.S., Zuo H.X., Wang Z., Li M.Y., Piao L.X., Xu G.H., Li X., Quan Z.S., et al. Imperatorin suppresses proliferation and angiogenesis of human colon cancer cell by targeting hif-1alpha via the mtor/p70s6k/4e-bp1 and mapk pathways. J. Ethnopharmacol. 2017;203:27–38. doi: 10.1016/j.jep.2017.03.033. [DOI] [PubMed] [Google Scholar]
- 108.Qin Y., Liu H.J., Li M., Zhai D.H., Tang Y.H., Yang L., Qiao K.L., Yang J.H., Zhong W.L., Zhang Q., et al. Salidroside improves the hypoxic tumor microenvironment and reverses the drug resistance of platinum drugs via hif-1alpha signaling pathway. EBioMedicine. 2018;38:25–36. doi: 10.1016/j.ebiom.2018.10.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li M.Y., Mi C., Wang K.S., Wang Z., Zuo H.X., Piao L.X., Xu G.H., Li X., Ma J., Jin X. Shikonin suppresses proliferation and induces cell cycle arrest through the inhibition of hypoxia-inducible factor-1alpha signaling. Chem. Biol. Interact. 2017;274:58–67. doi: 10.1016/j.cbi.2017.06.029. [DOI] [PubMed] [Google Scholar]
- 110.Seyfi D., Behzad S.B., Nabiuni M., Parivar K., Tahmaseb M., Amini E. Verbascoside attenuates rac-1 and hif-1alpha signaling cascade in colorectal cancer cells. Anticancer Agents Med. Chem. 2018;18:2149–2155. doi: 10.2174/1871520618666180611112125. [DOI] [PubMed] [Google Scholar]
- 111.Kong W., Li C., Qi Q., Shen J., Chang K. Cardamonin induces g2/m arrest and apoptosis via activation of the jnk-foxo3a pathway in breast cancer cells. Cell Biol. Int. 2019;44:177–188. doi: 10.1002/cbin.11217. [DOI] [PubMed] [Google Scholar]
- 112.Zan L., Chen Q., Zhang L., Li X. Epigallocatechin gallate (egcg) suppresses growth and tumorigenicity in breast cancer cells by downregulation of mir-25. Bioengineered. 2019;10:374–382. doi: 10.1080/21655979.2019.1657327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shrivastava S., Jeengar M.K., Thummuri D., Koval A., Katanaev V.L., Marepally S., Naidu V.G.M. Cardamonin, a chalcone, inhibits human triple negative breast cancer cell invasiveness by downregulation of wnt/beta-catenin signaling cascades and reversal of epithelial-mesenchymal transition. Biofactors. 2017;43:152–169. doi: 10.1002/biof.1315. [DOI] [PubMed] [Google Scholar]
- 114.Sheng J., Shi W., Guo H., Long W., Wang Y., Qi J., Liu J., Xu Y. The inhibitory effect of (-)-epigallocatechin-3-gallate on breast cancer progression via reducing scube2 methylation and dnmt activity. Molecules. 2019;24:2899. doi: 10.3390/molecules24162899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yuan C.H., Horng C.T., Lee C.F., Chiang N.N., Tsai F.J., Lu C.C., Chiang J.H., Hsu Y.M., Yang J.S., Chen F.A. Epigallocatechin gallate sensitizes cisplatin-resistant oral cancer car cell apoptosis and autophagy through stimulating akt/stat3 pathway and suppressing multidrug resistance 1 signaling. Environ. Toxicol. 2017;32:845–855. doi: 10.1002/tox.22284. [DOI] [PubMed] [Google Scholar]
- 116.Wu D., Liu Z., Li J., Zhang Q., Zhong P., Teng T., Chen M., Xie Z., Ji A., Li Y. Epigallocatechin-3-gallate inhibits the growth and increases the apoptosis of human thyroid carcinoma cells through suppression of egfr/ras/raf/mek/erk signaling pathway. Cancer Cell Int. 2019;19:43. doi: 10.1186/s12935-019-0762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Holczer M., Besze B., Zambo V., Csala M., Banhegyi G., Kapuy O. Epigallocatechin-3-gallate (egcg) promotes autophagy-dependent survival via influencing the balance of mtor-ampk pathways upon endoplasmic reticulum stress. Oxid. Med. Cell Longev. 2018;2018:6721530. doi: 10.1155/2018/6721530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xu X., Zhang X., Zhang Y., Yang L., Liu Y., Huang S., Lu L., Kong L., Li Z., Guo Q., et al. Wogonin reversed resistant human myelogenous leukemia cells via inhibiting nrf2 signaling by stat3/nf-kappab inactivation. Sci. Rep. 2017;7:39950. doi: 10.1038/srep39950. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 119.Zhao Y., Yao J., Wu X.P., Zhao L., Zhou Y.X., Zhang Y., You Q.D., Guo Q.L., Lu N. Wogonin suppresses human alveolar adenocarcinoma cell a549 migration in inflammatory microenvironment by modulating the il-6/stat3 signaling pathway. Mol. Carcinog. 2015;54((Suppl. S1)):E81–E93. doi: 10.1002/mc.22182. [DOI] [PubMed] [Google Scholar]
- 120.Bhuria V., Xing J., Scholta T., Bui K.C., Nguyen M.L.T., Malek N.P., Bozko P., Plentz R.R. Hypoxia induced sonic hedgehog signaling regulates cancer stemness, epithelial-to-mesenchymal transition and invasion in cholangiocarcinoma. Exp. Cell Res. 2019;385:111671. doi: 10.1016/j.yexcr.2019.111671. [DOI] [PubMed] [Google Scholar]
- 121.Po A., Citarella A., Catanzaro G., Besharat Z.M., Trocchianesi S., Gianno F., Sabato C., Moretti M., De Smaele E., Vacca A., et al. Hedgehog-gli signalling promotes chemoresistance through the regulation of abc transporters in colorectal cancer cells. Sci. Rep. 2020;10:13988. doi: 10.1038/s41598-020-70871-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Munoz J.L., Rodriguez-Cruz V., Walker N.D., Greco S.J., Rameshwar P. Temozolomide resistance and tumor recurrence: Halting the hedgehog. Cancer Cell Microenviron. 2015;2:e747. doi: 10.14800/ccm.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kudo K., Gavin E., Das S., Amable L., Shevde L.A., Reed E. Inhibition of gli1 results in altered c-jun activation, inhibition of cisplatin-induced upregulation of ercc1, xpd and xrcc1, and inhibition of platinum-DNA adduct repair. Oncogene. 2012;31:4718–4724. doi: 10.1038/onc.2011.610. [DOI] [PubMed] [Google Scholar]
- 124.Kim D.H., Kim M.J., Sung B., Suh H., Jung J.H., Chung H.Y., Kim N.D. Resveratrol analogue, hs-1793, induces apoptotic cell death and cell cycle arrest through downregulation of akt in human colon cancer cells. Oncol. Rep. 2017;37:281–288. doi: 10.3892/or.2016.5219. [DOI] [PubMed] [Google Scholar]
- 125.Lee J.H., Hwang B.Y., Kim K.S., Nam J.B., Hong Y.S., Lee J.J. Suppression of rela/p65 transactivation activity by a lignoid manassantin isolated from saururus chinensis. Biochem. Pharmacol. 2003;66:1925–1933. doi: 10.1016/S0006-2952(03)00553-7. [DOI] [PubMed] [Google Scholar]
- 126.Chang J.S., Lee S.W., Kim M.S., Yun B.R., Park M.H., Lee S.G., Park S.J., Lee W.S., Rho M.C. Manassantin a and b from saururus chinensis inhibit interleukin-6-induced signal transducer and activator of transcription 3 activation in hep3b cells. J. Pharmacol. Sci. 2011;115:84–88. doi: 10.1254/jphs.10239SC. [DOI] [PubMed] [Google Scholar]
- 127.Kim G.D., Oh J., Park H.J., Bae K., Lee S.K. Magnolol inhibits angiogenesis by regulating ros-mediated apoptosis and the pi3k/akt/mtor signaling pathway in mes/eb-derived endothelial-like cells. Int. J. Oncol. 2013;43:600–610. doi: 10.3892/ijo.2013.1959. [DOI] [PubMed] [Google Scholar]
- 128.Seyed M.A., Jantan I., Bukhari S.N., Vijayaraghavan K. A comprehensive review on the chemotherapeutic potential of piceatannol for cancer treatment, with mechanistic insights. J. Agric. Food Chem. 2016;64:725–737. doi: 10.1021/acs.jafc.5b05993. [DOI] [PubMed] [Google Scholar]
- 129.Farrand L., Byun S., Kim J.Y., Im-Aram A., Lee J., Lim S., Lee K.W., Suh J.Y., Lee H.J., Tsang B.K. Piceatannol enhances cisplatin sensitivity in ovarian cancer via modulation of p53, x-linked inhibitor of apoptosis protein (xiap), and mitochondrial fission. J. Biol. Chem. 2013;288:23740–23750. doi: 10.1074/jbc.M113.487686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Siedlecka-Kroplewska K., Slebioda T., Kmiec Z. Induction of autophagy, apoptosis and aquisition of resistance in response to piceatannol toxicity in molt-4 human leukemia cells. Toxicol. Vitro. 2019;59:12–25. doi: 10.1016/j.tiv.2019.03.040. [DOI] [PubMed] [Google Scholar]
- 131.Reddy S.D., Pakala S.B., Molli P.R., Sahni N., Karanam N.K., Mudvari P., Kumar R. Metastasis-associated protein 1/histone deacetylase 4-nucleosome remodeling and deacetylase complex regulates phosphatase and tensin homolog gene expression and function. J. Biol. Chem. 2012;287:27843–27850. doi: 10.1074/jbc.M112.348474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yoo Y.G., Kong G., Lee M.O. Metastasis-associated protein 1 enhances stability of hypoxia-inducible factor-1alpha protein by recruiting histone deacetylase 1. EMBO J. 2006;25:1231–1241. doi: 10.1038/sj.emboj.7601025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Qian Y.Y., Liu Z.S., Yan H.J., Yuan Y.F., Levenson A.S., Li K. Pterostilbene inhibits mta1/hdac1 complex leading to pten acetylation in hepatocellular carcinoma. Biomed. Pharmacother. 2018;101:852–859. doi: 10.1016/j.biopha.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 134.Czop M., Bogucka-Kocka A., Kubrak T., Knap-Czop K., Makuch-Kocka A., Galkowski D., Wawer J., Kocki T., Kocki J. Imaging flow cytometric analysis of stilbene-dependent apoptosis in drug resistant human leukemic cell lines. Molecules. 2019;24:1896. doi: 10.3390/molecules24101896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Li P., Tian W., Wang X., Ma X. Inhibitory effect of desoxyrhaponticin and rhaponticin, two natural stilbene glycosides from the tibetan nutritional food rheum tanguticum maxim. Ex balf., on fatty acid synthase and human breast cancer cells. Food Funct. 2014;5:251–256. doi: 10.1039/C3FO60484E. [DOI] [PubMed] [Google Scholar]
- 136.Mickymaray S., Alfaiz F.A., Paramasivam A., Veeraraghavan V.P., Periadurai N.D., Surapaneni K.M., Niu G. Rhaponticin suppresses osteosarcoma through the inhibition of pi3k-akt-mtor pathway. Saudi J. Biol. Sci. 2021;28:3641–3649. doi: 10.1016/j.sjbs.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang F., Yin G., Han X., Jiang X., Bao Z. Chlorogenic acid inhibits osteosarcoma carcinogenesis via suppressing the stat3/snail pathway. J. Cell Biochem. 2019;120:10342–10350. doi: 10.1002/jcb.28318. [DOI] [PubMed] [Google Scholar]
- 138.Lee A.Y., Kim S., Lee S., Jiang H.L., Kim S.B., Hong S.H., Cho M.H. Knockdown of importin 7 inhibits lung tumorigenesis in k-ras(la1) lung cancer mice. Anticancer Res. 2017;37:2381–2386. doi: 10.21873/anticanres.11576. [DOI] [PubMed] [Google Scholar]
- 139.Li S.R., Gyselman V.G., Dorudi S., Bustin S.A. Elevated levels of ranbp7 mrna in colorectal carcinoma are associated with increased proliferation and are similar to the transcription pattern of the proto-oncogene c-myc. Biochem. Biophys. Res. Commun. 2000;271:537–543. doi: 10.1006/bbrc.2000.2666. [DOI] [PubMed] [Google Scholar]
- 140.Golomb L., Bublik D.R., Wilder S., Nevo R., Kiss V., Grabusic K., Volarevic S., Oren M. Importin 7 and exportin 1 link c-myc and p53 to regulation of ribosomal biogenesis. Mol. Cell. 2012;45:222–232. doi: 10.1016/j.molcel.2011.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xue J., Zhou A., Tan C., Wu Y., Lee H.T., Li W., Xie K., Huang S. Forkhead box m1 is essential for nuclear localization of glioma-associated oncogene homolog 1 in glioblastoma multiforme cells by promoting importin-7 expression. J. Biol. Chem. 2015;290:18662–18670. doi: 10.1074/jbc.M115.662882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chachami G., Paraskeva E., Mingot J.M., Braliou G.G., Gorlich D., Simos G. Transport of hypoxia-inducible factor hif-1alpha into the nucleus involves importins 4 and 7. Biochem. Biophys. Res. Commun. 2009;390:235–240. doi: 10.1016/j.bbrc.2009.09.093. [DOI] [PubMed] [Google Scholar]
- 143.Liu X.H., Kirschenbaum A., Lu M., Yao S., Dosoretz A., Holland J.F., Levine A.C. Prostaglandin e2 induces hypoxia-inducible factor-1alpha stabilization and nuclear localization in a human prostate cancer cell line. J. Biol. Chem. 2002;277:50081–50086. doi: 10.1074/jbc.M201095200. [DOI] [PubMed] [Google Scholar]
- 144.Rodriguez-Barbero A., Dorado F., Velasco S., Pandiella A., Banas B., Lopez-Novoa J.M. Tgf-beta1 induces cox-2 expression and pge2 synthesis through mapk and pi3k pathways in human mesangial cells. Kidney Int. 2006;70:901–909. doi: 10.1038/sj.ki.5001626. [DOI] [PubMed] [Google Scholar]
- 145.Grabarska A., Skalicka-Wozniak K., Kielbus M., Dmoszynska-Graniczka M., Miziak P., Szumilo J., Nowosadzka E., Kowalczuk K., Khalifa S., Smok-Kalwat J., et al. Imperatorin as a promising chemotherapeutic agent against human larynx cancer and rhabdomyosarcoma cells. Molecules. 2020;25:2046. doi: 10.3390/molecules25092046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.You C., Yang Y., Gao B. Imperatorin targets mcl-1 to sensitize cd133+ lung cancer cells to gammadelta-t cell-mediated cytotoxicity. Cell Physiol. Biochem. 2018;49:235–244. doi: 10.1159/000492874. [DOI] [PubMed] [Google Scholar]
- 147.Xu W.W., Huang Z.H., Liao L., Zhang Q.H., Li J.Q., Zheng C.C., He Y., Luo T.T., Wang Y., Hu H.F., et al. Direct targeting of creb1 with imperatorin inhibits tgfbeta2-erk signaling to suppress esophageal cancer metastasis. Adv. Sci. 2020;7:2000925. doi: 10.1002/advs.202000925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gwon S.Y., Ahn J.Y., Jung C.H., Moon B.K., Ha T.Y. Shikonin suppresses erk 1/2 phosphorylation during the early stages of adipocyte differentiation in 3t3-l1 cells. BMC Complement. Altern. Med. 2013;13:207. doi: 10.1186/1472-6882-13-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hsieh Y.S., Liao C.H., Chen W.S., Pai J.T., Weng M.S. Shikonin inhibited migration and invasion of human lung cancer cells via suppression of c-met-mediated epithelial-to-mesenchymal transition. J. Cell Biochem. 2017;118:4639–4651. doi: 10.1002/jcb.26128. [DOI] [PubMed] [Google Scholar]
- 150.Memmott R.M., Dennis P.A. Akt-dependent and -independent mechanisms of mtor regulation in cancer. Cell Signal. 2009;21:656–664. doi: 10.1016/j.cellsig.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Huang X., Xu X., Wang X., Tang T., Li E., Zhang X., Xu J., Shen H., Guo C., Xu T., et al. The akt-independent met-v-atpase-mtor axis suppresses liver cancer vaccination. Signal. Transduct. Target. Ther. 2020;5:122. doi: 10.1038/s41392-020-0179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang Y., Yuan Y., Wu H., Xie Z., Wu Y., Song X., Wang J., Shu W., Xu J., Liu B., et al. Effect of verbascoside on apoptosis and metastasis in human oral squamous cell carcinoma. Int. J. Cancer. 2018;143:980–991. doi: 10.1002/ijc.31378. [DOI] [PubMed] [Google Scholar]
- 153.Jia W.Q., Wang Z.T., Zou M.M., Lin J.H., Li Y.H., Zhang L., Xu R.X. Verbascoside inhibits glioblastoma cell proliferation, migration and invasion while promoting apoptosis through upregulation of protein tyrosine phosphatase shp-1 and inhibition of stat3 phosphorylation. Cell Physiol. Biochem. 2018;47:1871–1882. doi: 10.1159/000491067. [DOI] [PubMed] [Google Scholar]
- 154.Wu C.H., Chen C.H., Hsieh P.F., Lee Y.H., Kuo W.W., Wu R.C., Hung C.H., Yang Y.L., Lin V.C. Verbascoside inhibits the epithelial-mesenchymal transition of prostate cancer cells through high-mobility group box 1/receptor for advanced glycation end-products/tgf-beta pathway. Environ. Toxicol. 2021;36:1080–1089. doi: 10.1002/tox.23107. [DOI] [PubMed] [Google Scholar]
- 155.Chae K.S., Kang M.J., Lee J.H., Ryu B.K., Lee M.G., Her N.G., Ha T.K., Han J., Kim Y.K., Chi S.G. Opposite functions of hif-alpha isoforms in vegf induction by tgf-beta1 under non-hypoxic conditions. Oncogene. 2011;30:1213–1228. doi: 10.1038/onc.2010.498. [DOI] [PubMed] [Google Scholar]
- 156.Ishaq M., Khan M.A., Sharma K., Sharma G., Dutta R.K., Majumdar S. Gambogic acid induced oxidative stress dependent caspase activation regulates both apoptosis and autophagy by targeting various key molecules (nf-kappab, beclin-1, p62 and nbr1) in human bladder cancer cells. Biochim. Biophys. Acta. 2014;1840:3374–3384. doi: 10.1016/j.bbagen.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 157.Wan L., Zhang Q., Wang S., Gao Y., Chen X., Zhao Y., Qian X. Gambogic acid impairs tumor angiogenesis by targeting yap/stat3 signaling axis. Phytother. Res. 2019;33:1579–1591. doi: 10.1002/ptr.6350. [DOI] [PubMed] [Google Scholar]
- 158.Yu J., Wang W., Yao W., Yang Z., Gao P., Liu M., Wang H., Chen S., Wang D., Wang W., et al. Gambogic acid affects escc progression through regulation of pi3k/akt/mtor signal pathway. J. Cancer. 2020;11:5568–5577. doi: 10.7150/jca.41115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hua Y., Zhu Y., Zhang J., Zhu Z., Ning Z., Chen H., Liu L., Chen Z., Meng Z. Mir-122 targets x-linked inhibitor of apoptosis protein to sensitize oxaliplatin-resistant colorectal cancer cells to oxaliplatin-mediated cytotoxicity. Cell Physiol. Biochem. 2018;51:2148–2159. doi: 10.1159/000495832. [DOI] [PubMed] [Google Scholar]
- 160.Guo C., Ma J., Deng G., Qu Y., Yin L., Li Y., Han Y., Cai C., Shen H., Zeng S. Zeb1 promotes oxaliplatin resistance through the induction of epithelial-mesenchymal transition in colon cancer cells. J. Cancer. 2017;8:3555–3566. doi: 10.7150/jca.20952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Xu K., Zhan Y., Yuan Z., Qiu Y., Wang H., Fan G., Wang J., Li W., Cao Y., Shen X., et al. Hypoxia induces drug resistance in colorectal cancer through the hif-1alpha/mir-338-5p/il-6 feedback loop. Mol. Ther. 2019;27:1810–1824. doi: 10.1016/j.ymthe.2019.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Park C.V., Ivanova I.G., Kenneth N.S. Xiap upregulates expression of hif target genes by targeting hif1alpha for lys63-linked polyubiquitination. Nucleic Acids Res. 2017;45:9336–9347. doi: 10.1093/nar/gkx549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Yu G., Li N., Zhao Y., Wang W., Feng X.L. Salidroside induces apoptosis in human ovarian cancer skov3 and a2780 cells through the p53 signaling pathway. Oncol. Lett. 2018;15:6513–6518. doi: 10.3892/ol.2018.8090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ma J., Li J., Wang K.S., Mi C., Piao L.X., Xu G.H., Li X., Lee J.J., Jin X. Perillyl alcohol efficiently scavenges activity of cellular ros and inhibits the translational expression of hypoxia-inducible factor-1alpha via mtor/4e-bp1 signaling pathways. Int. Immunopharmacol. 2016;39:1–9. doi: 10.1016/j.intimp.2016.06.034. [DOI] [PubMed] [Google Scholar]
- 165.Wu W., Hu Z., Zhao Q., Zhang X., Zhang H., Wang H., Xue W., Yu L., Duan G. Down-regulation of hypoxia-inducible factor-1alpha and downstream glucose transporter protein-1 gene by beta-elemene enhancing the radiosensitivity of lung adenocarcinoma transplanted tumor. Onco. Targets Ther. 2020;13:11627–11635. doi: 10.2147/OTT.S275956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yu X., Li Z., Zhang Y., Xu M., Che Y., Tian X., Wang R., Zou K., Zou L. Beta-elemene inhibits radiation and hypoxia-induced macrophages infiltration via prx-1/nf-kappab/hif-1alpha signaling pathway. Onco. Targets Ther. 2019;12:4203–4211. doi: 10.2147/OTT.S196910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shi L., Zhang G., Zheng Z., Lu B., Ji L. Andrographolide reduced vegfa expression in hepatoma cancer cells by inactivating hif-1alpha: The involvement of jnk and mta1/hdca. Chem. Biol. Interact. 2017;273:228–236. doi: 10.1016/j.cbi.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 168.Dai T., Li L., Qi W., Liu B., Jiang Z., Song J., Hua H. Balanophorin b inhibited glycolysis with the involvement of hif-1alpha. Life Sci. 2021;267:118910. doi: 10.1016/j.lfs.2020.118910. [DOI] [PubMed] [Google Scholar]
- 169.Kim H.J., Cho H.S., Ban H.S., Nakamura H. Suppression of hif-1alpha accumulation by betulinic acid through proteasome activation in hypoxic cervical cancer. Biochem. Biophys. Res. Commun. 2020;523:726–732. doi: 10.1016/j.bbrc.2020.01.031. [DOI] [PubMed] [Google Scholar]
- 170.Zhang Y.F., Zhang Z.H., Li M.Y., Wang J.Y., Xing Y., Ri M., Jin C.H., Xu G.H., Piao L.X., Zuo H.X., et al. Britannin stabilizes t cell activity and inhibits proliferation and angiogenesis by targeting pd-l1 via abrogation of the crosstalk between myc and hif-1alpha in cancer. Phytomedicine. 2021;81:153425. doi: 10.1016/j.phymed.2020.153425. [DOI] [PubMed] [Google Scholar]
- 171.Zhu Y., Liu X., Zhao P., Zhao H., Gao W., Wang L. Celastrol suppresses glioma vasculogenic mimicry formation and angiogenesis by blocking the pi3k/akt/mtor signaling pathway. Front. Pharmacol. 2020;11:25. doi: 10.3389/fphar.2020.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ullah A., Leong S.W., Wang J., Wu Q., Ghauri M.A., Sarwar A., Su Q., Zhang Y. Cephalomannine inhibits hypoxia-induced cellular function via the suppression of apex1/hif-1alpha interaction in lung cancer. Cell Death Dis. 2021;12:490. doi: 10.1038/s41419-021-03771-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zhang L., Chen C., Duanmu J., Wu Y., Tao J., Yang A., Yin X., Xiong B., Gu J., Li C., et al. Cryptotanshinone inhibits the growth and invasion of colon cancer by suppressing inflammation and tumor angiogenesis through modulating mmp/timp system, pi3k/akt/mtor signaling and hif-1alpha nuclear translocation. Int. Immunopharmacol. 2018;65:429–437. doi: 10.1016/j.intimp.2018.10.035. [DOI] [PubMed] [Google Scholar]
- 174.Zuo H.X., Jin Y., Wang Z., Li M.Y., Zhang Z.H., Wang J.Y., Xing Y., Ri M.H., Jin C.H., Xu G.H., et al. Curcumol inhibits the expression of programmed cell death-ligand 1 through crosstalk between hypoxia-inducible factor-1alpha and stat3 (t705) signaling pathways in hepatic cancer. J. Ethnopharmacol. 2020;257:112835. doi: 10.1016/j.jep.2020.112835. [DOI] [PubMed] [Google Scholar]
- 175.Zhang L., Qiao X., Chen M., Li P., Wen X., Sun M., Ma X., Hou Y., Yang J. Ilexgenin a prevents early colonic carcinogenesis and reprogramed lipid metabolism through hif1alpha/srebp-1. Phytomedicine. 2019;63:153011. doi: 10.1016/j.phymed.2019.153011. [DOI] [PubMed] [Google Scholar]
- 176.Wang K.S., Ma J., Mi C., Li J., Lee J.J., Jin X. Kamebakaurin inhibits the expression of hypoxia-inducible factor-1alpha and its target genes to confer antitumor activity. Oncol. Rep. 2016;35:2045–2052. doi: 10.3892/or.2016.4576. [DOI] [PubMed] [Google Scholar]
- 177.Kong P., Yu K.N., Yang M., Almahi W.A., Nie L., Chen G., Han W. Micheliolide enhances radiosensitivities of p53-deficient non-small-cell lung cancer via promoting hif-1alpha degradation. Int. J. Mol. Sci. 2020;21:3392. doi: 10.3390/ijms21093392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wang Z., Li M.Y., Zhang Z.H., Zuo H.X., Wang J.Y., Xing Y., Ri M., Jin H.L., Jin C.H., Xu G.H., et al. Panaxadiol inhibits programmed cell death-ligand 1 expression and tumour proliferation via hypoxia-inducible factor (hif)-1alpha and stat3 in human colon cancer cells. Pharmacol. Res. 2020;155:104727. doi: 10.1016/j.phrs.2020.104727. [DOI] [PubMed] [Google Scholar]
- 179.Park J.H., Yoon J., Park B. Pomolic acid suppresses hif1alpha/vegf-mediated angiogenesis by targeting p38-mapk and mtor signaling cascades. Phytomedicine. 2016;23:1716–1726. doi: 10.1016/j.phymed.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 180.Lee S.O., Kim J.S., Lee M.S., Lee H.J. Anti-cancer effect of pristimerin by inhibition of hif-1alpha involves the sphk-1 pathway in hypoxic prostate cancer cells. BMC Cancer. 2016;16:701. doi: 10.1186/s12885-016-2730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Li G., Shan C., Liu L., Zhou T., Zhou J., Hu X., Chen Y., Cui H., Gao N. Tanshinone iia inhibits hif-1alpha and vegf expression in breast cancer cells via mtor/p70s6k/rps6/4e-bp1 signaling pathway. PLoS ONE. 2015;10:e0117440. doi: 10.1371/journal.pone.0117440. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 182.Li B., Tong T., Ren N., Rankin G.O., Rojanasakul Y., Tu Y., Chen Y.C. Theasaponin e1 inhibits platinum-resistant ovarian cancer cells through activating apoptosis and suppressing angiogenesis. Molecules. 2021;26:1681. doi: 10.3390/molecules26061681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lee Y.M., Kim G.H., Park E.J., Oh T.I., Lee S., Kan S.Y., Kang H., Kim B.M., Kim J.H., Lim J.H. Thymoquinone selectively kills hypoxic renal cancer cells by suppressing hif-1alpha-mediated glycolysis. Int. J. Mol. Sci. 2019;20:1092. doi: 10.3390/ijms20051092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Ding X., Zhou X., Jiang B., Zhao Q., Zhou G. Triptolide suppresses proliferation, hypoxia-inducible factor-1alpha and c-myc expression in pancreatic cancer cells. Mol. Med. Rep. 2015;12:4508–4513. doi: 10.3892/mmr.2015.3960. [DOI] [PubMed] [Google Scholar]
- 185.Shan J.Z., Xuan Y.Y., Zhang Q., Huang J.J. Ursolic acid sensitized colon cancer cells to chemotherapy under hypoxia by inhibiting mdr1 through hif-1alpha. J. Zhejiang Univ. Sci. B. 2016;17:672–682. doi: 10.1631/jzus.B1600266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Song B., Zhang Q., Yu M., Qi X., Wang G., Xiao L., Yi Q., Jin W. Ursolic acid sensitizes radioresistant nsclc cells expressing hif-1alpha through reducing endogenous gsh and inhibiting hif-1alpha. Oncol. Lett. 2017;13:754–762. doi: 10.3892/ol.2016.5468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wang W.J., Sui H., Qi C., Li Q., Zhang J., Wu S.F., Mei M.Z., Lu Y.Y., Wan Y.T., Chang H., et al. Ursolic acid inhibits proliferation and reverses drug resistance of ovarian cancer stem cells by downregulating abcg2 through suppressing the expression of hypoxia-inducible factor-1alpha in vitro. Oncol. Rep. 2016;36:428–440. doi: 10.3892/or.2016.4813. [DOI] [PubMed] [Google Scholar]
- 188.Isaacs J.S., Jung Y.J., Mimnaugh E.G., Martinez A., Cuttitta F., Neckers L.M. Hsp90 regulates a von hippel lindau-independent hypoxia-inducible factor-1 alpha-degradative pathway. J. Biol. Chem. 2002;277:29936–29944. doi: 10.1074/jbc.M204733200. [DOI] [PubMed] [Google Scholar]
- 189.Tang X., Ding Q., Chen C., Chen F., Zhou X., Hong C.J., Pan W. Micheliolide inhibits gastric cancer growth in vitro and in vivo via blockade of the il-6/stat3 pathway. Pharmazie. 2019;74:175–178. doi: 10.1691/ph.2019.8816. [DOI] [PubMed] [Google Scholar]
- 190.Antonangeli F., Natalini A., Garassino M.C., Sica A., Santoni A., Di Rosa F. Regulation of pd-l1 expression by nf-kappab in cancer. Front. Immunol. 2020;11:584626. doi: 10.3389/fimmu.2020.584626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lim S.O., Li C.W., Xia W., Cha J.H., Chan L.C., Wu Y., Chang S.S., Lin W.C., Hsu J.M., Hsu Y.H., et al. Deubiquitination and stabilization of pd-l1 by csn5. Cancer Cell. 2016;30:925–939. doi: 10.1016/j.ccell.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Jung Y., Isaacs J.S., Lee S., Trepel J., Liu Z.G., Neckers L. Hypoxia-inducible factor induction by tumour necrosis factor in normoxic cells requires receptor-interacting protein-dependent nuclear factor kappa b activation. Biochem. J. 2003;370:1011–1017. doi: 10.1042/bj20021279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Doe M.R., Ascano J.M., Kaur M., Cole M.D. Myc posttranscriptionally induces hif1 protein and target gene expression in normal and cancer cells. Cancer Res. 2012;72:949–957. doi: 10.1158/0008-5472.CAN-11-2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Wang D., Lin J., Yang X., Long J., Bai Y., Yang X., Mao Y., Sang X., Seery S., Zhao H. Combination regimens with pd-1/pd-l1 immune checkpoint inhibitors for gastrointestinal malignancies. J. Hematol. Oncol. 2019;12:42. doi: 10.1186/s13045-019-0730-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Yu C.C., Chen C.A., Fu S.L., Lin H.Y., Lee M.S., Chiou W.Y., Su Y.C., Hung S.K. Andrographolide enhances the anti-metastatic effect of radiation in ras-transformed cells via suppression of erk-mediated mmp-2 activity. PLoS ONE. 2018;13:e0205666. doi: 10.1371/journal.pone.0205666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Peng Y., Wang Y., Tang N., Sun D., Lan Y., Yu Z., Zhao X., Feng L., Zhang B., Jin L., et al. Andrographolide inhibits breast cancer through suppressing cox-2 expression and angiogenesis via inactivation of p300 signaling and vegf pathway. J. Exp. Clin. Cancer Res. 2018;37:248. doi: 10.1186/s13046-018-0926-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wu C.A., Huang D.Y., Lin W.W. Beclin-1-independent autophagy positively regulates internal ribosomal entry site-dependent translation of hypoxia-inducible factor 1alpha under nutrient deprivation. Oncotarget. 2014;5:7525–7539. doi: 10.18632/oncotarget.2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang D., Li J., Costa M., Gao J., Huang C. Jnk1 mediates degradation hif-1alpha by a vhl-independent mechanism that involves the chaperones hsp90/hsp70. Cancer Res. 2010;70:813–823. doi: 10.1158/0008-5472.CAN-09-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kim M.H., Kim H.B., Yoon S.P., Lim S.C., Cha M.J., Jeon Y.J., Park S.G., Chang I.Y., You H.J. Colon cancer progression is driven by apex1-mediated upregulation of jagged. J. Clin. Investig. 2013;123:3211–3230. doi: 10.1172/JCI65521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Deng X., Zhen P., Niu X., Dai Y., Wang Y., Zhou M. Ape1 promotes proliferation and migration of cutaneous squamous cell carcinoma. J. Dermatol. Sci. 2020;100:67–74. doi: 10.1016/j.jdermsci.2020.08.012. [DOI] [PubMed] [Google Scholar]
- 201.Logsdon D.P., Grimard M., Luo M., Shahda S., Jiang Y., Tong Y., Yu Z., Zyromski N., Schipani E., Carta F., et al. Regulation of hif1alpha under hypoxia by ape1/ref-1 impacts ca9 expression: Dual targeting in patient-derived 3d pancreatic cancer models. Mol. Cancer Ther. 2016;15:2722–2732. doi: 10.1158/1535-7163.MCT-16-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Shin D.S., Kim H.N., Shin K.D., Yoon Y.J., Kim S.J., Han D.C., Kwon B.M. Cryptotanshinone inhibits constitutive signal transducer and activator of transcription 3 function through blocking the dimerization in du145 prostate cancer cells. Cancer Res. 2009;69:193–202. doi: 10.1158/0008-5472.CAN-08-2575. [DOI] [PubMed] [Google Scholar]
- 203.Chen W., Liu L., Luo Y., Odaka Y., Awate S., Zhou H., Shen T., Zheng S., Lu Y., Huang S. Cryptotanshinone activates p38/jnk and inhibits erk1/2 leading to caspase-independent cell death in tumor cells. Cancer Prev. Res. 2012;5:778–787. doi: 10.1158/1940-6207.CAPR-11-0551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Lee J.H., Koo T.H., Hwang B.Y., Lee J.J. Kaurane diterpene, kamebakaurin, inhibits nf-kappa b by directly targeting the DNA-binding activity of p50 and blocks the expression of antiapoptotic nf-kappa b target genes. J. Biol. Chem. 2002;277:18411–18420. doi: 10.1074/jbc.M201368200. [DOI] [PubMed] [Google Scholar]
- 205.Guan Z., Chen J., Li X., Dong N. Tanshinone iia induces ferroptosis in gastric cancer cells through p53-mediated slc7a11 down-regulation. Biosci. Rep. 2020;40:BSR20201807. doi: 10.1042/BSR20201807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lv C., Zeng H.W., Wang J.X., Yuan X., Zhang C., Fang T., Yang P.M., Wu T., Zhou Y.D., Nagle D.G., et al. The antitumor natural product tanshinone iia inhibits protein kinase c and acts synergistically with 17-aag. Cell Death Dis. 2018;9:165. doi: 10.1038/s41419-017-0247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Phillips P.A., Dudeja V., McCarroll J.A., Borja-Cacho D., Dawra R.K., Grizzle W.E., Vickers S.M., Saluja A.K. Triptolide induces pancreatic cancer cell death via inhibition of heat shock protein 70. Cancer Res. 2007;67:9407–9416. doi: 10.1158/0008-5472.CAN-07-1077. [DOI] [PubMed] [Google Scholar]
- 208.Li R., Zhang X., Tian X., Shen C., Zhang Q., Zhang Y., Wang Z., Wang F., Tao Y. Triptolide inhibits tumor growth by induction of cellular senescence. Oncol. Rep. 2017;37:442–448. doi: 10.3892/or.2016.5258. [DOI] [PubMed] [Google Scholar]
- 209.Deng Q.D., Lei X.P., Zhong Y.H., Chen M.S., Ke Y.Y., Li Z., Chen J., Huang L.J., Zhang Y., Liang L., et al. Triptolide suppresses the growth and metastasis of non-small cell lung cancer by inhibiting beta-catenin-mediated epithelial-mesenchymal transition. Acta Pharmacol. Sin. 2021;42:1486–1497. doi: 10.1038/s41401-021-00657-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zeng A., Hua H., Liu L., Zhao J. Betulinic acid induces apoptosis and inhibits metastasis of human colorectal cancer cells in vitro and in vivo. Bioorg. Med. Chem. 2019;27:2546–2552. doi: 10.1016/j.bmc.2019.03.033. [DOI] [PubMed] [Google Scholar]
- 211.Kim S.Y., Hwangbo H., Kim M.Y., Ji S.Y., Kim D.H., Lee H., Kim G.Y., Moon S.K., Leem S.H., Yun S.J., et al. Betulinic acid restricts human bladder cancer cell proliferation in vitro by inducing caspase-dependent cell death and cell cycle arrest, and decreasing metastatic potential. Molecules. 2021;26:1381. doi: 10.3390/molecules26051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Sun L., Cao J., Chen K., Cheng L., Zhou C., Yan B., Qian W., Li J., Duan W., Ma J., et al. Betulinic acid inhibits stemness and emt of pancreatic cancer cells via activation of ampk signaling. Int. J. Oncol. 2019;54:98–110. doi: 10.3892/ijo.2018.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Zhan X.K., Li J.L., Zhang S., Xing P.Y., Xia M.F. Betulinic acid exerts potent antitumor effects on paclitaxel-resistant human lung carcinoma cells (h460) via g2/m phase cell cycle arrest and induction of mitochondrial apoptosis. Oncol. Lett. 2018;16:3628–3634. doi: 10.3892/ol.2018.9097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ci X., Zhou J., Lv H., Yu Q., Peng L., Hua S. Betulin exhibits anti-inflammatory activity in lps-stimulated macrophages and endotoxin-shocked mice through an ampk/akt/nrf2-dependent mechanism. Cell Death Dis. 2017;8:e2798. doi: 10.1038/cddis.2017.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Aiken C.T., Kaake R.M., Wang X., Huang L. Oxidative stress-mediated regulation of proteasome complexes. Mol. Cell Proteom. 2011;10:R110.006924. doi: 10.1074/mcp.M110.006924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kannaiyan R., Shanmugam M.K., Sethi G. Molecular targets of celastrol derived from thunder of god vine: Potential role in the treatment of inflammatory disorders and cancer. Cancer Lett. 2011;303:9–20. doi: 10.1016/j.canlet.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 217.Shi J., Li J., Xu Z., Chen L., Luo R., Zhang C., Gao F., Zhang J., Fu C. Celastrol: A review of useful strategies overcoming its limitation in anticancer application. Front. Pharmacol. 2020;11:558741. doi: 10.3389/fphar.2020.558741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Vihanto M.M., Plock J., Erni D., Frey B.M., Frey F.J., Huynh-Do U. Hypoxia up-regulates expression of eph receptors and ephrins in mouse skin. FASEB J. 2005;19:1689–1691. doi: 10.1096/fj.04-3647fje. [DOI] [PubMed] [Google Scholar]
- 219.Tang N.N., Zhu H., Zhang H.J., Zhang W.F., Jin H.L., Wang L., Wang P., He G.J., Hao B., Shi R.H. Hif-1alpha induces ve-cadherin expression and modulates vasculogenic mimicry in esophageal carcinoma cells. World J. Gastroenterol. 2014;20:17894–17904. doi: 10.3748/wjg.v20.i47.17894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Yang H., Liu C., Zhang Y.Q., Ge L.T., Chen J., Jia X.Q., Gu R.X., Sun Y., Sun W.D. Ilexgenin a induces b16-f10 melanoma cell g1/s arrest in vitro and reduces tumor growth in vivo. Int. Immunopharmacol. 2015;24:423–431. doi: 10.1016/j.intimp.2014.12.040. [DOI] [PubMed] [Google Scholar]
- 221.Yang H., Wang J., Fan J.H., Zhang Y.Q., Zhao J.X., Dai X.J., Liu Q., Shen Y.J., Liu C., Sun W.D., et al. Ilexgenin a exerts anti-inflammation and anti-angiogenesis effects through inhibition of stat3 and pi3k pathways and exhibits synergistic effects with sorafenib on hepatoma growth. Toxicol. Appl. Pharmacol. 2017;315:90–101. doi: 10.1016/j.taap.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 222.Guimaraes L., Rocha G.D.G., Queiroz R.M., Martins C.A., Takiya C.M., Gattass C.R. Pomolic acid induces apoptosis and inhibits multidrug resistance protein mrp1 and migration in glioblastoma cells. Oncol. Rep. 2017;38:2525–2534. doi: 10.3892/or.2017.5895. [DOI] [PubMed] [Google Scholar]
- 223.Kim B., Kim Y.C., Park B. Pomolic acid inhibits metastasis of her2 overexpressing breast cancer cells through inactivation of the erk pathway. Int. J. Oncol. 2016;49:744–752. doi: 10.3892/ijo.2016.3568. [DOI] [PubMed] [Google Scholar]
- 224.Kim B., Kim J.H., Park B. Pomolic acid inhibits invasion of breast cancer cells through the suppression of cxc chemokine receptor type 4 expression. J. Cell Biochem. 2016;117:1296–1307. doi: 10.1002/jcb.25417. [DOI] [PubMed] [Google Scholar]
- 225.Martins C.A., Rocha G.D.G., Gattass C.R., Takiya C.M. Pomolic acid exhibits anticancer potential against a docetaxelresistant pc3 prostate cell line. Oncol. Rep. 2019;42:328–338. doi: 10.3892/or.2019.7132. [DOI] [PubMed] [Google Scholar]
- 226.Ader I., Brizuela L., Bouquerel P., Malavaud B., Cuvillier O. Sphingosine kinase 1: A new modulator of hypoxia inducible factor 1alpha during hypoxia in human cancer cells. Cancer Res. 2008;68:8635–8642. doi: 10.1158/0008-5472.CAN-08-0917. [DOI] [PubMed] [Google Scholar]
- 227.Bouquerel P., Gstalder C., Muller D., Laurent J., Brizuela L., Sabbadini R.A., Malavaud B., Pyronnet S., Martineau Y., Ader I., et al. Essential role for sphk1/s1p signaling to regulate hypoxia-inducible factor 2alpha expression and activity in cancer. Oncogenesis. 2016;5:e209. doi: 10.1038/oncsis.2016.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Meurette O., Stylianou S., Rock R., Collu G.M., Gilmore A.P., Brennan K. Notch activation induces akt signaling via an autocrine loop to prevent apoptosis in breast epithelial cells. Cancer Res. 2009;69:5015–5022. doi: 10.1158/0008-5472.CAN-08-3478. [DOI] [PubMed] [Google Scholar]
- 229.Wang L., Zi H., Luo Y., Liu T., Zheng H., Xie C., Wang X., Huang X. Inhibition of notch pathway enhances the anti-tumor effect of docetaxel in prostate cancer stem-like cells. Stem Cell Res. Ther. 2020;11:258. doi: 10.1186/s13287-020-01773-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Kim J.D., Chaudhary N., Seo H.J., Kim M.Y., Shin T.S. Theasaponin e(1) as an effective ingredient for anti-angiogenesis and anti-obesity effects. Biosci. Biotechnol. Biochem. 2014;78:279–287. doi: 10.1080/09168451.2014.893183. [DOI] [PubMed] [Google Scholar]
- 231.Zhang Y., Huang L., Shi H., Chen H., Tao J., Shen R., Wang T. Ursolic acid enhances the therapeutic effects of oxaliplatin in colorectal cancer by inhibition of drug resistance. Cancer Sci. 2018;109:94–102. doi: 10.1111/cas.13425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Xiang F., Fan Y., Ni Z., Liu Q., Zhu Z., Chen Z., Hao W., Yue H., Wu R., Kang X. Ursolic acid reverses the chemoresistance of breast cancer cells to paclitaxel by targeting mirna-149-5p/myd88. Front. Oncol. 2019;9:501. doi: 10.3389/fonc.2019.00501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.