Abstract
Breast cancer (BC) is the most commonly diagnosed cancer among women worldwide and the most common cause of cancer-related death. To date, it is still a challenge to estimate the magnitude of the clinical impact of physical activity (PA) on those parameters producing significative changes in future BC risk and disease progression. However, studies conducted in recent years highlight the role of PA not only as a protective factor for the development of ER+ breast cancer but, more generally, as a useful tool in the management of BC treatment as an adjuvant to traditional therapies. In this review, we focused our attention on data obtained from human studies analyzing, at each level of disease prevention (i.e., primary, secondary, tertiary and quaternary), the positive impact of PA/exercise in ER+ BC, a subtype representing approximately 70% of all BC diagnoses. Moreover, given the importance of estrogen receptors and body composition (i.e., adipose tissue) in this subtype of BC, an overview of their role will also be made throughout this review.
Keywords: breast cancer, physical activity, body composition, risk factors, cancer prevention
1. Introduction
Breast cancer (BC) is the most commonly diagnosed cancer among women in 140 of 184 countries worldwide, and it is the most common cause of cancer-related death in 103 countries [1]. To date, it is considered curable in ~70–80% of patients with early-stage, non-metastatic disease [2].
BC is known to be a hormone-dependent disease characterized by molecular mechanisms involving activation of human epidermal growth factor receptor 2 (HER2, encoded by ERBB2), hormone receptors (estrogen receptor and progesterone receptor) and/or BRCA mutations [2]. Most BCs (70–80%) express a significant amount of estrogen receptors (ER) and/or progesterone receptors (PR), which are considered biomarkers of a favourable prognosis [3].
Although BC is defined as a malignant tumor that affects the breast, there are recognizable different types on the base of specific breast cells involved. The following classification is made according to the stage of the tumor and where it takes place. In particular, it is possible to distinguish the ductal carcinoma in situ (DCIS), which is considered non-invasive or pre-invasive, whose cells have become cancerous but have not yet invaded the surrounding tissues, and nonobligate precursors of invasive BC (20% of screen detected), as well as the invasive BC whose cancerous cells have reached the surrounding tissues [1,4]. It is estimated that about 50% of DCIS patients will progress to invasive cancer [4].
Another classification is made according to the molecular subtype, determined by the analysis of the gene expression of HER2, and by quantitative hormone receptor (HR) analysis [5], which so far has identified four main subtypes: (1) Luminal A (HR+/HER2−), the most common type that tends to be slower growing and less aggressive with the most favourable prognosis; (2) Luminal B (HR+/HER2+), which results in HR+ and is highly positive for Ki97 and/or HER2 protein with poorer outcomes; (3) Basal-like (HR−/HER2−), also called triple-negative because of ER−, PR− and HER2−, with the worst prognosis of all other subtypes and a very low survival expectancy; (4) the HER2-enriched (HR−/HER2+) [6] (Table 1).
Table 1.
Molecular subtypes of breast cancer.
| Subtypes | Molecular Signatures | % Incidence |
|---|---|---|
| Luminal A | ER+, PR±, HER2−, Low Ki67 | ≈70% |
| Luminal B | ER+, PR±, HER2±, High Ki67 | 10–20% |
| Triple Negative | ER−, PR−, HER2− | 15–20% |
| HER2 | ER−, PR−, HER+ | 5–15% |
To date, women with a history of BC represent the largest group of cancer survivors in high-income countries [7]; thus, it becomes a category of patients who require an increasingly demanding management.
The implementation of an effective intervention plan is necessary at each level, from the origins of the cause to the management of disease; therefore, it is a priority to understand the risk factors leading to the development of disease and possible interventional approaches.
In this narrative review, we focused our attention on data obtained from human studies analyzing, at each level of disease prevention (i.e., primary, secondary, tertiary and quaternary), the positive impact of physical activity (PA)/exercise in sedentary/non-active subjects (<2 h × week) with ER+ BC, a subtype representing approximately 70% of all BC diagnoses. Moreover, given the importance of ER and body composition (i.e., adipose tissue) in this subtype of BC [8], throughout this review an overview of their role will also be made.
2. Estrogen Receptors in Breast Cancer and Their Clinical Implications
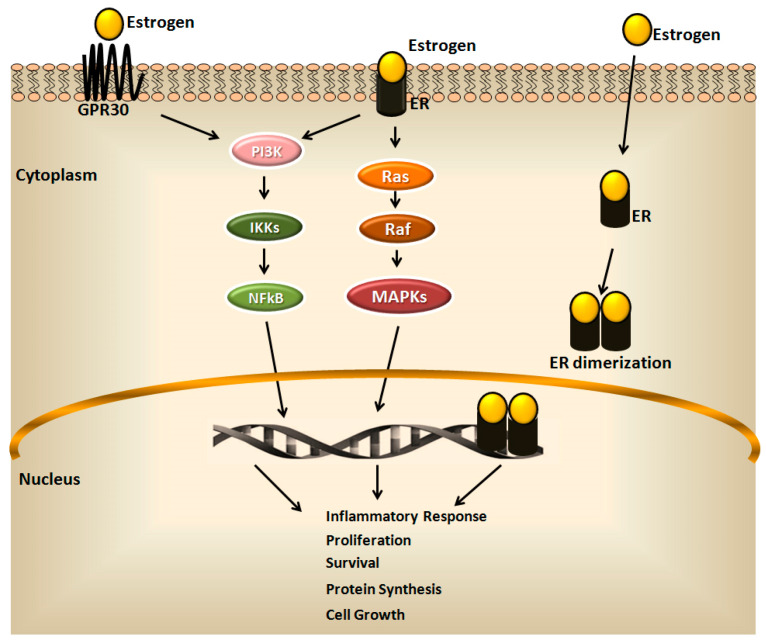
Some of the features of human BC (e.g., initiation and progression) are derived from a deregulation of estrogen-dependent and ER signaling pathways [9] (Figure 1).
Figure 1.
The estrogen signaling pathway. The estrogen signaling mainly includes activation of intracellular estrogen receptor (ER) that, upon ligand binding and dimerization, translocates to the nucleus, where it directly binds responsive elements of target genes involved in the cell growth, inflammation, proliferation, survival, and protein synthesis. Differently, estrogens mediate non-genomic effects and activate intracellular signaling through the binding of the plasma membrane receptors, ER variants and the G protein-coupled receptor (GPR30). This binding induces the rapid activation of protein kinases, phosphatidylinositol-3-kinase (PI3K), renin-angiotensin system (Ras) and rapidly accelerated fibrosarcoma (Raf), as well as the transcription factors nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) and mitogen-activated protein kinase (MAPK), which regulate the gene expression of estrogen target genes.
It is known that the effects of estrogen are mediated by three different ERs: (1) the nuclear receptor ERα, which drives almost ∼75% of BCs [10]; (2) nuclear receptor ERβ; (3) the cytoplasmic G protein-coupled estrogen receptor 1 (GPER) [11,12,13,14].
ERα and ERβ share common structural characteristics with five different domains, named A/B, C, D, E and F, with similar mechanism of action [14,15]. Generally, estrogens move the cell passively by diffusion through the cellular membrane, bind ERs in the cytoplasm and are transported to the nucleus [16]. The interaction receptor-ligand induces conformational change of the receptors, whereby the ERs form dimers, bind DNA and initiate gene transcription [14]. In this case, ERs regulate transcriptional processes by nuclear translocation and binding to specific response elements, which act on the regulation of gene expression [17].
Three ERα isoforms have been identified in mammals: full-length ERα, and two truncated isoforms, ERα36 and ERα46, respectively. ERα36 expression has been particularly detected in BC, as well as in endometrial, colorectal, gastric and hepatic cancers [14,18].
ERα and ERβ are distributed differently in human breast tissues: ERα expression is mainly limited to the nuclei of epithelial cells present in the lobules and ducts of the healthy breast. Differently, ERβ is also expressed in normal breast tissue, where it is detectable in myoepithelial cells as well as in surrounding stromal and endothelial cells [14,19,20].
BCs not expressing ERα were tested positively for ERβ expression. It has been demonstrated that ERβ possesses a weaker activity than ERα, able to repress the transcriptional activity of ERα, although this mechanism remains to be investigated [14,19,21]. A comprehensive clarification about the role of ERβ in BC is hampered by the presence of five different isoforms of ERβ (ERβ, β2, β3, β4, and β5). However, although more investigations are needed, the general consensus is its suppressor role in BC, since it is able to reduce growth, proliferation and cancer cell migration and invasion mediated by ERα, [14,22,23,24]. Besides its genomic actions, ER mediates non-genomic effects towards the transmembrane protein, GPER, commonly accepted as being responsible for the extra-nuclear, non-genomic effects of estrogens [14,25].
Multiple ER-targeting drugs are used routinely in the clinical practice to treat ER+ BC patients; however, initial or acquired resistance to these therapies frequently occurs, with recurrence of metastatic tumors [9]. Therefore, understanding the mechanisms leading to drug resistance becomes extremely important. In normal conditions, the activity of ER is controlled mainly by the availability of estrogens, which bind the ER-ligand-binding domain and mediate receptor dimerization, nuclear translocation and the binding to estrogen response elements (EREs), located close the promoters of target genes [21]. Different studies demonstrate that growth factors, hormones and cytokines produced by the tumor microenvironment play pivotal roles in the progression of ER+ BC, and many of these signaling pathways can directly affect the transcriptional activity and function of ER, independently by the classical estrogenic ligands. In particular, the ER phosphorylation may have a key role in the receptor activation in a ligand-independent manner [26].
Phosphorylation of Ser118 (S118) is one of the most well-characterized systems of ER activation independently of estrogens and can be induced by epidermal growth factor (EGF) and mitogen-activated protein kinase (MAPK) [27,28,29]. This EGF-induced phosphorylation has been demonstrated to be involved in increasing cell proliferation in tumorigenic cells, favouring the binding of ER to chromatin through cooperation with several transcription factor complexes, such as AP-1 transcription factors and early B-cell leukaemia transcription factor 1 (PBX1) [30,31]. To be noted, the Y537 and D538 ER BC mutants are constitutively phosphorylated on S118 in an estrogen-independent manner [32,33], highlighting the importance of this phosphorylation event for ER activity and suggesting the S118 as a fundamental regulatory site in the drug-resistant metastatic disease. Phosphorylation of S305 appears to be important for this estrogen-independent activation of ER as well. This event is mediated by the protein kinase-A (PKA) [34] and Pak1 [35] in the absence of estradiol and drives receptor activity that is refractory to tamoxifen inhibition [34].
Particularly, PKA-mediated ER phosphorylation induces receptor binding to non-classic regulatory sites that differ from those typically bound by ER after estradiol-induced activation. It was suggested that this mechanism induces the expression of the oncogene c-MYC responsible of tamoxifen resistance [36]. The phosphorylation on S305 can also be induced by inflammatory molecules and adypokines as leptin, TNF-alpha, IL6 and IL1-beta, produced by different cell types involved in cancer progression [37]. The cytokine-induced phosphorylation is mediated by the inhibition of nuclear factor κB kinase subunit β (IKKβ), rather than PKA or Pak1, and it is involved in cell extravasation, an important part of the metastatic process [37]. Once ER binds chromatin, other transcription factors can redirect the binding on DNA, reprogramming the transcriptional activity of ER to other target genes. These factors include FOXA1 [38], PBX1 [31], the transcription factor AP-2γ [39], and GATA-binding protein 3 (GATA3) [40]. Therefore, different pathways triggered by molecules, produced by the tumor microenvironment, can impact ER function and influence endocrine resistance. This highlights the need to understand as much as possible the molecular mechanisms related to factors involved in ER+ BC.
To date, few studies performed in rat models following physical training analyzed the expression of ER in BC cells. In these studies, authors demonstrated an effect of PA in increasing the ratio of ERβ/ERα, and a reduction in the sensitivity of BC cells to the pro-proliferative and antiapoptotic effects of estrogen, leading to apoptotic cell death [41].
However, further studies in human and in disease-applicable preclinical models could be useful to validate these mechanisms and determine if these pathways may provide molecular tools for therapeutic application.
3. The Role of Adipose Tissue
According to the anatomical location and to the main cell component, adipose tissue can be divided in three different types: white adipose tissue (WAT), which represents more than 95% of the fat mass, brown adipose tissue (BAT), which constitutes 1% to 2% of fat, and the most recently discovered beige adipose tissue [42].
This tissue derives from WAT by a conversion process called the browning of adipose tissue but resembles BAT in morphology and role. The formation of beige adipocytes is reversible and is generally a consequence of adrenergic stimulation, cold exposure, diet and exercise [43,44,45].
The WAT is the main storage site for energy deposition, and it is composed of mature adipocytes capable of storing energy in the form of triacylglycerol (TAGs) in lipid droplets. Only 20–30% of adipose tissue is made up of mature adipocytes; the remaining 70–80% is composed of the stromal vascular fraction (SVF) [46,47], connective tissue matrix, as well as vascular and neural tissues. The non-adipocyte cellular component includes various types of immune cells such as macrophages, neutrophils, eosinophils, mast cells, lymphocyte T cells and B cells, as well as preadipocytes and fibroblasts [48,49].
This cellular heterogeneity clearly demonstrates that adipose tissue is a complex organ with different functions, regulating the metabolism of the whole body [47]. In particular, it is considered an endocrine organ releasing numerous substances, such as adipokines (i.e., adiponectin, leptin and resistin), hormones, as well as cytokines (i.e., TNF-α, IL-6, IL-1, IL-8) [50]. This explains the excess adipose tissue in the body, which contributes to the onset of a pathological state of many organs and systems [51]. Among the different types of adipose tissue, WAT is responsible for the inflammation process. This means that the inflammation grade increases with the progression of obesity, and the results strongly associated with an increase in adipocytes size and a systemic insulin resistance (IR) state.
Numerous preclinical and clinical studies demonstrated that chronic low-grade inflammation of adipose tissue, also called “metaflammation”, is strongly and consistently associated with excess body fat mass and metabolic disease onset and progression. This mechanism is initiated and sustained over time by adipocyte dysfunction, which releases inflammatory adipokines, and by the infiltration/activation of numerous immune cells (i.e., pro-inflammatory M1 macrophages, dendritic cells, mast cells, neutrophils, B cells, and T cells), which amplify the inflammatory response through the production/secretion of proinflammatory cytokines and chemokines [52,53]. Differently from the acute inflammation, metaflammtation is characterized by chronic low-grade inflammation, since cytokine release and immune cell infiltration come out gradually and remain unresolved over time [52,53].
Besides adipokines and inflammatory mediators, adipose tissue is responsible for estrogen production. Especially in postmenopausal woman, the increase in BMI is associated with a high release of estrone, estradiol and free estradiol, as well as a high expression of the enzyme aromatase. These abnormal changes lead to excessive, 10-fold estrogen secretion in the breast and therefore to a higher risk of developing BC [54,55].
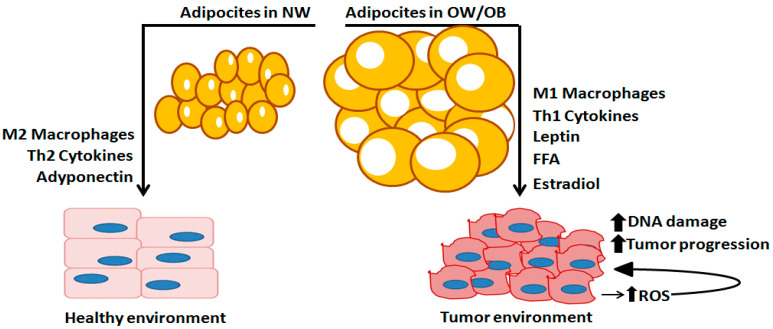
As shown in Figure 2 adipocyte hypertrophy leads to “unhealthy” adipocytes characterized by mitochondria dysfunction, which produces reactive oxygen species (ROS), lipolysis and insulin resistance. The inability of insulin to suppress lipolysis increases free fatty acid (FFA) mobilization. In the absence of FFA utilization, they can trigger adipocyte inflammation and increase inflammatory macrophages (M1), which also produce TNF-α, a cytokine able to induce a supra-physiological production of ROS through the inhibition of insulin signaling and mitochondrial function.
Figure 2.
Adipose-related factors engaged to the initiation and progression of breast cancer. Normal adipose tissue, generally existing in “normal weight” (NW) subjects (%BF cutoff values between 8 and 20% for men and 14 and 23% for women), is characterized by smaller and less adipocyte cells and M2-polarized macrophages that release anti-inflammatory cytokines and adiponectin that contribute to normal breast cell development. In overweight (OW) and obese condition (OB), adipose tissue is characterized by larger size and more abundant adipocytes, releasing pro-inflammatory cytokines, M1-polarized macrophages, leptin, free fatty acids (FFAs), and estrogens, synthesized by aromatase enzyme. These factors act as mutagens stimulating the growth of tumor cells. A tumor environment produces more reactive oxygen species (ROS), which generate DNA damage, amplify and induce mutagenesis, tumor growth and progression. Therefore, the OW/OB condition provides a favorable microenvironment for adipose tissue to induce tumor establishment and progression.
Exercise training has been shown to have a multitude of health benefits, including those at a metabolic, antioxidant, and anti-inflammatory level [56,57,58,59,60]. For instance, resistance training positively affects WAT metabolism. Indeed, exercise decreases blood glucose levels and increases the activity of different hormones, including glucagon, catecholamines (epinephrine and norepinephrine), growth hormone (GH), atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP) and cortisol. These molecules act as lipolytic hormones and regulate the release of FFA and glucagone, providing energy substrates for skeletal muscle cells [61,62,63]. By creating a negative energy balance, fat loss is facilitated, which occurs as a first adaptation with the reduction in the adipocytes size, which becomes more insulin-sensitive, a mechanism by which the inflammation of the WAT and the dysregulated lipolysis are reduced. Moreover, the stimulation of lipolysis and insulin sensitivity following exercise training is correlated with increased FFA oxidation and lower lipid storage in WAT.
Other important effects related to training concern inflammation of the adipose tissue and mitochondrial function. In fact, the adaptation process involves not only the mitochondria in skeletal muscle, but also those present in adipose tissue. A higher density of mitochondria is characteristic within BAT, but mitochondrial biogenesis can be induced by exercise training, improving the brown adipocyte-specific gene expression and the phenotypic switching from WAT to BAT. This framework of training-induced adaptation clarifies not only the importance of weight loss, but also better adipose tissue function through increased mitochondrial activity and a reduced inflammation level. This makes the fat cells “fit”, which can be used in favour of a healthy body [64].
4. Physical Activity and Physical Exercise in Breast Cancer Prevention
Since the interchangeable use of exercise and PA in research literature, Dasso [65] tried to clarify the differences. The author reported the Center for Disease Control and Prevention definition of exercise, which is a subcategory of PA, intended as a planned, structured, repetitive, and purposive activity so that the improvement or maintenance of one or more functional parameters can be objectively quantified. Instead, as reported by the World Health Organization [66], PA consists in any bodily movement produced by skeletal muscles that result in energy expenditure. According to the author, a clear definition of exercise allows health care providers to speak to patients about improving their PA.
However, regardless of the definitions, it is known that both PA and exercise play a pivotal role on health status, helping to prevent different diseases, including cancer [56,57,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81].
To date, five levels of disease prevention are recognized [82]:
Primordial prevention—It consists in programs and campaigns, usually addressed to the younger population, aimed at promoting a healthy lifestyle and avoiding the incurrence of risk factors;
Primary prevention—It consists in measures, addressed to a susceptible but healthy population, aimed at preventing a disease through specific activities that limit risk exposure or increase the immunity;
Secondary prevention—It consists in procedures that increase the early disease detection, and its target is healthy-appearing individuals with subclinical forms of the disease, and often occurs in the form of screenings. The objective is the early identification of sick or high-risk subjects to achieve healing or prevent the onset and progression of the disease;
Tertiary prevention—It targets both clinical and outcome stages of a disease, with the aim to reduce the severity of the disease as well as of any associated consequences, and to reduce the effects of the disease once established in an individual, through a tailored rehabilitation program;
Quaternary prevention—It consist in practice able to protect patients from medical interventions that cause more harm than benefits, due to the over-treatment condition or final-stage of the disease.
Epidemiological studies have highlighted a variety of modifiable and non-modifiable BC risk factors [83], also known as host and environmental factors [84,85].
Among the non-modifiable risk factors, there are: family history of the cancer, BRCA1 and/or BRCA2 mutations, reproductive factors that influence endogenous estrogen exposure (nulliparity, early age at menarche, later menopause, and later age at first full-term pregnancy), race and ethnicity.
Differently, the modifiable risk factors include alcohol drinking, physical inactivity, excess body weight, as well as the use of exogenous hormones (oral contraceptives and menopausal hormone replacement therapy), and smoking [83].
BC is considered a heterogeneous disease with 30% of cases recognized as familial BC (which reveals the association with number of high-, moderate-, and low-penetrance susceptibility genes) compared to 70% of cases of BC presenting as sporadic [86]. These data highlight the importance to modify those risk factors correlated with the lifestyle to potentially reduce the disease incidence [87].
Particularly interesting are the results of several studies, which found a strong correlation between adipose inflammation and an alteration in estrogen biosynthesis/signaling pathways in obese patients. The excessive chronic exposure to estrogens increases the risk of developing BC [11,88,89]. This led to the recognition of obesity as a risk factor for the hormone-dependent subtype of BC, especially in postmenopausal women [15].
PA has been demonstrated to positively impact specific biomarkers related to physiological and pathological condition [56,57,75,76,90,91,92,93,94,95,96,97] or to reduce the incidence of cardiovascular and metabolic diseases in broad populations of individuals, including women, older individuals, patients with coronary heart diseases [98], as well as those with diabetes [77,97,99] and heart failure [98]. Moreover, numerous research studies have identified the PA as an important factor in the primary prevention of BC able to ameliorate the patient conditions in the different stages of the disease, either after the diagnosis of BC or in the early post-surgery steps improving survival outcomes [67,68,70,71,72,73,100]. Indeed, the authors have been demonstrated positive effects of well-structured aerobic or strength training protocols on Quality of Life (QoL), fatigue, aerobic fitness, and muscular strength in BC survivors during and after treatments [101,102,103]. Moreover, it is known that the beneficial association between PA and BC survival are partially related to biological and biochemical changes capable of influencing several hormones (i.e., sex hormones, insulin, IGF-1) and DNA methylation levels of specific tumor suppressor genes, which appear to be directly involved in the progression of this disease [104].
5. Physical Activity and Exercise as Fundamental Approaches within ER-Positive Breast Cancer at Each Disease Prevention Level
The strong association between PA/exercise and BC risk is widely recognized, reporting beneficial effects on tumor number sites, growth, metastasis and incidence [105,106]. The mechanisms involved in these processes are complex and multifaceted and may be mediated, at least in part, by a reduction in inflammation markers, particularly MCP-1 and IL-6 [105], and the reduced expression of the transcription factor NF-κB [107]. To date, most of the main findings regarding the molecular mechanisms involving physical exercise and tumorigenesis were obtained in preclinical models available elsewhere [108,109,110,111,112].
In the next paragraphs, we have reported data from human studies related to the impact of PA on BC at each level of disease prevention: primary, secondary, tertiary and quaternary. In particular, we focused on studies analyzing whether or not the amount of exercise prescribed influences BC biomarker levels in patients with a sedentary lifestyle (<120 min/week of moderate-to-vigorous PA) [113].
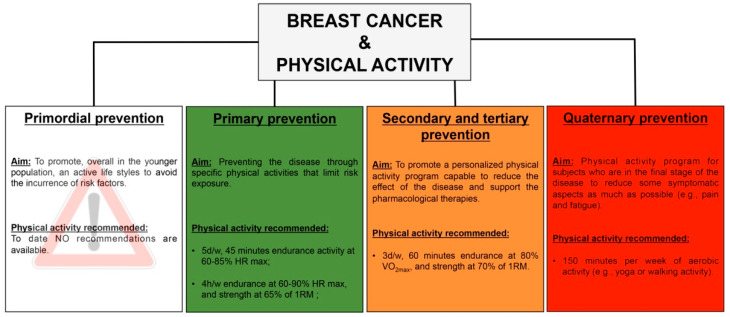
Unfortunately, no studies are still conducted on the possible role of physical exercise as “primordial” BC intervention.
5.1. Primary Prevention
The American Cancer Society (ACS) and the American Institute for Cancer Research/World Research Fund (AICR/WCRF) publish PA guidelines for cancer prevention. For an adult, the ACS guideline recommended 150 min/week of moderate activity or 75 min/week of vigorous activity throughout the week [114]. The AICR/WCRF recommends 30 min/day of moderate activity increasing to 60 min/day of moderate activity or 30 min/day of vigorous activity as fitness improves [115]. However, to date, questions remain about the applicability of these guidelines with respect to reductions in BC risk.
Furthermore, even if an exercise intervention achieves these targets, it is unknown what the long-term implications are for postmenopausal BC risk.
Previous randomized controlled trials [116,117,118,119,120,121,122,123,124,125,126,127,128,129] have highlighted several plausible biological mechanisms whereby PA can reduce postmenopausal BC risk (Table 2).
Table 2.
Exercise and physical activity in primary prevention of breast cancer in overweight/obese postmenopausal women.
| REF. | GROUPS | EXERCISE CHARACTERISTICS | MAIN OUTCOMES |
|---|---|---|---|
| [128] | (n = 173) age 50 to 79 years BMI ≥ 25 kg/m2 (mean 30.4 ± 4.1) Groups: AG (n = 84) CG (n = 86) |
12 months AG: endurance exercise, 5 d/w progressively increase to 45 min at 60–75% HRmax; CG: no interventions |
↓Fat mass ↓ Testosterone and free testosterone = DHEA, DHEA-S =androstenedione |
| [129] | (n = 169) age 50 to 75 years BMI ≥ 25 kg/m2 (mean 30.4 ± 4.1) Groups: AG (n = 84) CG (n = 85) |
12 months AG: endurance exercise, 5 d/w progressively increase to 45 min at 60–75% HRmax; CG: no interventions |
↓Fat mass ↓ Estrone ↓ Estradiol and free estradiol 🡹 SHBG |
| [127] | (n = 189) age 50 to 69 years BMI 22–40 kg/m2 (mean 27.3 ± 3.6) Groups: AG (n = 96) CG (n = 93) |
12 months AG: 3 d/w of combined endurance + strength program (from 60–85% HRmax) (2.5 h/w) CG: no interventions |
↓Fat mass =estrogen levels =androgen levels =SHBG |
| [116] | (n = 320) age 50–74 years BMI 22–40 kg/m2 (mean 29.1 ± 4.5) Groups: AG (n = 160) CG (n = 160) |
12 months AG: 225 min/w (average of 3.6 d/w for 178 min/w) at 70% to 80% HRR CG: no interventions |
↓ Estradiol and free estradiol 🡹 SHBG ↓ Body weight = estrone, androstenedione and testosterone |
| [119] | (n = 439) age 50–75 years BMI ≥ 25 kg/m2 (mean 30.9) Groups: DG (n = 118) AG (n = 117) DAG (n = 117) CG (n = 87) |
12 months; DG: daily energy intake of 1200 to 2000 kcal/d based on baseline weight; AG: ≥45 min MVPA (70% to 85% heart rate max), 5 d/w; DAG: both interventions; CG: no interventions |
↓Fat mass in all groups vs. CG ↓ Insulin in DG and DAG ↓ hs-CRP in DG and DAG ↓ Leptin in all groups vs. CG 🡹 Adiponectin in DG and DAG ↓ Estron, estradiol, free estradiol, and free testosterone in all in all intervention groups vs. CG ↓ Total testosterone in DAG 🡹 SHBG in DG and DAG |
| [126] | (n = 439) aged 50–75 years BMI ≥ 25 kg/m2 (mean 30.9) Groups: DG (n = 118) AG (n = 117) DAG (n = 117) CG (n = 87) |
12 months; DG: daily energy intake of 1200–2000 kcal/d based on baseline weight; AG: ≥45 min of MVPA (70–85% heart rate max), 5 d/w (225 min/w). DAG: both interventions (diet + exercise) CG: no interventions |
↓Fat mass in all intervention groups vs. CG; ↓ Waist circumference in all intervention groups vs. CG; |
| [117] | (n = 382) age 50–74 years BMI 22–40 kg/m2 (mean 29.4 ± 4.4) Groups: COG (n = 193) MVG (n = 189) |
12 months of endurance activity (5 d/w, 3 supervised, 2 unsupervised); COG: 60 min/session, 60–80% HRR MVG: 30 min/session, 60–80% HRR |
↓Fat mass depending on exercise volume (high or moderate); =sex hormone levels between groups |
| [120] | (n = 243) age 50–69 years BMI 25–35 kg/m2 (mean 29.5 ± 2.6) Groups: DG (n = 97) COG (n = 98) CG (n = 48) |
16 weeks; DG: caloric deficit of 3500 kcal/w with habitual physical activity level; COG: 4 h/w of combined endurance (from 60% to 90% HRR) and strength program with an average energy expenditure of 2530 kcal/week; CG: habitual physical activity level + standardized diet |
↓Fat mass in DG and COG ↓ hs-CRP in DG and COG; =IL6 in all groups; ↓ Adiponectin in COG; ↓ Leptin in DG and COG |
| [121] | (n = 41) age 50–74 years BMI 23.8–32.9 kg/m2 (mean 28.2 ± 3.4) Groups: AG (n = 22) CG (n = 19) |
6 months; AG: 3 d/w progressively increase to 50 min at 70–80% HRmax; CG: no interventions |
=Leptin =Resistin =Fat mass 🡹 Aerobic Fitness level ↓ BMI |
| [122] | (n = 306) age 50–74 years BMI 22–40 kg/m2 (mean 29.0) Groups: AG (n = 153) CG (n = 154) |
12 months; AG: 45 min/d, 5 d/w (70% to 80% HRR); CG: no interventions |
↓ Total estradiol =estrogen metabolites and metabolic pathways |
| [123] |
(n = 439) age 50–75 years BMI ≥ 25 kg/m2 (mean 30.0 ± 3.7) Groups: DG (n = 118) AG (n = 117) DAG (n = 117) CG (n = 87) |
12 months + 18 months follow-up (FU); DG: daily energy intake of 1200–2000 kcal/d based on baseline weight; AG: ≥45 min of MVPA (70–85% heart rate max), 5 d/w (225 min/w); DAG: both interventions (diet + exercise); CG: no interventions |
🡹SHBG in DAG; =SHBG in DG and AG; Participants who reported weight loss had statistically greater decreases in free estradiol, free testosterone, and increases in SHBG |
| [118] | (n = 333) age 50–74 years BMI 22–40 kg/m2 (mean 28.9 ± 4.4) Groups: COG (n = 168) MVG (n = 165) |
12 months of endurance activity (5 d/w, 3 supervised, 2 unsupervised) + 12 months follow-up (FU); COG: 60 min/session, 65% to 75% HRR; MVG: 30 min/session, 65% to 75% HRR |
↓Fat mass depending on exercise volume (high or moderate); ↓ hs-CRP, insulin, glucose, HOMA-IR, estrone, estradiol, free estradiol at 12 months; SHBG at 12 months; ↓ Glucose, insulin, HOMA-IR, estrone at FU; 🡹 hs-CRP, free estradiol, estradiol at FU; ↓ SHBG at FU =biomarker changes over the time between groups. |
| [124] | (n = 35) age 50–65 years BMI ≥ 25 kg/m2 (mean 33.2 ± 1.4) Groups: AG (n = 10) COG (n = 13) CG (n = 12) |
12 weeks, 3 d/w; AG: 60 min/session of endurance exercise, 55–75% of HRR; COG: 40 mn resistance (6 exercises, 3 sets of 8–12 repetition at 65% of 1RM) + 20 min endurance exercise; CG: no interventions |
↓Fat mass in AG and COG; ↓ Lean body mass in the COG; ↓ DHEA-S (−13%), total (−40%) and free testosterone (−41%) in AG; ↓ Total (25%) and free testosterone (21%) in COG; =estrogen levels in both groups. The decrease in fat mass and DHEA-S correlates with an increase in circulating SHBG. |
Legend: AG, aerobic group; DG, diet group; DAG, diet + aerobic group; CG, control group; COG, combined group (diet + exercise); HVG, high volume group; MVG, moderate volume group; MVPA, moderate to vigorous physical activity; HRR, heart rate reserve; HRmax, maximal heart rate; FU, follow-up; w, week; d, days, HOMA-IR, fasting glucose (mmol/L) x fasting insulin (mIU/mL)/22.5; hs-CRP, high-sensitivity C-reactive protein; SHBG, sex-hormone-binding globulin; DHEA-S, dehydroepiandrosterone sulfate; 1RM, one-rep maximum; BMI, body mass index. The Red color indicates reported parameters worsened during experimental trails.
These studies presented in Table 2 highlight how PA/exercise interventions contribute to the modulation of adiposity, endogenous sex and metabolic hormones, and inflammatory markers. A careful analysis of the research papers showed that these effects, especially those on sex hormones, were dependent on the characteristics of exercise (i.e., type, intensity, duration and frequency) and on the homogeneity of the subjects recruited in terms of BMI. In particular, it was evident that 12 months of training (5 d/w, 45 min at 60–85% HRmax), mainly of endurance activity, in subjects with a narrow range of BMI between overweight and obesity, showed a significant decrease in fat mass, free and total testosterone, estrone, free and total estradiol, as well as an increase in SHBG [117,119,126,129].
These results seem to be achieved when people also followed a healthy dietary lifestyle combined with training, evidencing a decrease in insulin, adiponectin, leptin and hsCRCP levels, likely associated with a lower BC risk [119,120,121,123]. A change of exercise characteristics such as type and frequency, as well as the choice of a non-homogeneous sample, was sufficient to determine a lower impact of PA [116,122,127]. A minor impact of PA was observed when the training period was shortened, and the subjects recruited had a wider range of BMI [121].
Interestingly, in 2019, both Duggan et al. [123] and Friedenrich et al. [118] demonstrated that most of the beneficial effects of PA were maintained even after 18 months of follow-up. Still, the caloric restriction combined with exercise seems to be most beneficial for lowering sex hormone levels [119,123]. Comparing the combination of exercise and caloric restriction with caloric restriction only, all results favored the combination, even when weight loss between the groups was comparable. An additional important advantage of combining caloric restriction with adequate protein intake and regular physical activity is the preservation of as much muscle mass, and thereby muscle strength, physical function and cardiovascular fitness, as possible [130,131,132].
Finally, Gonzalo-Encabo et al. [124] and van Gemert et al. [120] demonstrated that a combined exercise (i.e., resistance and endurance activity), adapted from the American College of Sports Medicine’s guidelines [133], improves body composition and sex hormone profile in postmenopausal women, known to be important risk factors for ER+ BC.
5.2. Secondary and Tertiary Prevention
The latest evidence supports the role of exercise prescription to reduce morbidity, improves function and quality of life, and potentially improves survival, with very low risk of harm [67,134,135]. As suggested by Schmitz [136], on the basis of other diseases’ rehabilitation programs, a model to integrate exercise prescription into cancer clinical care is needed to reduce the risk of mortality and recurrence, through improvements in functional capacity, body composition and other several factors [137].
To date, numerous side effects related to adjuvant hormone therapy were reported, such as biological (dyslipidemia), physical (weight gain, hot flashes, vaginal dryness, sexual disorders with low libido, musculoskeletal alterations), and psychosocial (anxious-depressive disorders, poor body image, difficulties of professional reintegration) [138,139].
More specifically, the aromatase inhibitor, a drug commonly prescribed for postmenopausal ER+ BC, has been shown to induce an increase in body fat and a reduction in insulin sensitivity [140,141,142], as well as long-term cardiotoxicity [143,144,145], osteoporosis [146,147,148], and arthralgia [149,150,151].
In this section, we included trials proposing exercise and PA protocols for BC patients (from I to III stage) before, during, or after the classic pharmacological treatments, when they reported the ER + or the aromatase inhibitors in the patient characteristics (Table 3).
Table 3.
Exercise and physical activity as secondary and tertiary prevention among ER+ breast cancer survivors before and during pharmacological treatments.
| REF. | GROUPS | EXERCISE CHARACTERISTICS | MAIN OUTCOMES |
| [152] |
(n = 85) age 52–62 years IRG (n = 42) DRG (n = 42) |
6 months (after treatment) 2 d/w IRG and DRG: 3 set 12 repetition (13 w supervised + 13 w no-supervised) |
↓ Body fat and IGF-II in IRG 🡹 IGFBP-3 in IRG |
| [153] | (n = 66) age 46–58 years HAG (n = 22) HRG (n = 21) CG (n = 23) |
6 months (before and during adjuvant CH) 4 d/w HAG: 15–30 min HRG: 2 sets 10 repetitions CG: no intervention |
🡹 Aerobic capacity (25%) in HAG and (4%) in HRG ↓ BMD (6.2%) in CG, (4.9%) in HRG and (0.7%) in HAG ↓ Aerobic capacity (10%) in CG |
| [154] | (n = 101) Age HARG (n = 51) CG (n = 50) |
16 weeks (after CH, RT, during HT) 2 d/w HARG: 50-min supervised strength + 90 min unsupervised aerobic CG: no intervention |
↓ Fast insulin and hip circumference in HARG = insulin resistance, fasting glucose and BMI |
| [155] | (n = 90) age 41–48 years DG (n = 29) DHARG (n = 29) DHARG + FVLF (32) |
6 months 5 d/w DG: Calcium reach Diet DHARG: Calcium Diet + 150 min of MVPA AT + RT DHARG + FVLF: Calcium Diet + exercise + FVLF |
↓ Waist circumference and % body fat in DHARG + FVLF = insulin, proinsulin, IGF-1, CRP, cholesterol, SHBG, IL-1B, and TNFR2 in all groups 🡹 In QoL in all groups |
| [156] | (n = 75) age 55–64 years AG + HAG (n = 37) CG (n = 38) |
6 months (after CH) 5 d/w AG + HAG: 3 d/w 150 min/week of supervised gym- and 2 d/w home-based moderate-intensity aerobic exercise CG: no intervention |
↓ FAT in AG + HAG 🡹 LM in AG + HAG ↓ FAT, LM and BMD in CG |
| [157] | (n = 26) Age 40–60 years AG (n = 16) CG (n = 10) |
8 weeks AG: moderate intensity CG: no intervention |
↓ Waist circumference in AG 🡹 PA level = blood pressure, HDL, insulin resistance and CRP |
| [158] | (n = 90) age 55–65 years DARG (n = 47) CG (n = 43) |
6 months (duirng and after CH) 3 d/w DARG: 30 min 65–80% predicted HRmax + 10–15 min resistance band exercise + total daily caloric intake 600 kcal below their requirements CG: no intervenation |
↓ Central adiposity, WHR, total cholesterol and leptin in DARG 🡹 Predicted VO2max in DARG |
| [159] | (n = 28) age 56–66 years ARG (n = 15) CG (n = 13) |
12 weeks, supervised 6 wks, unsupervised 6 wks ARG:, 150 min/wk aerobic moderate intensity + resistance exercise, 2 d/wk CG: no intervention |
🡹 IL6 and predicted O2 in ARG ↓ IL-10, adiponectin, fatigue and sleep disturbance in ARG |
| [160] | (n = 46) age 30–70 years ARG (n = 22) CG (n = 24) |
12 weeks 5 d/w ARG: 160 min/wk at 48–52% of heart rate reserve +resistance exercise CG: no intervention |
↓ %BF, IL10, anxiety, sleep dysfunction, exercise social support in ARG 🡹 VO2max in ARG |
| [161] | (n = 242) age ≥ 18 years AG (n = 78) RG (n = 82) CG (n = 82) |
3 d/w during CH AG: 45 min at 80% VO2max RG: two sets of 8–12 at 60–70% of estimated 1-RM GC: no intervention |
🡹DFS and RFI in AG and RG |
| [162] | (n = 165) DG (n = 83) DRG (n = 82) |
12 months (after CH, during antiestrogenic treatment) 7 d/w DG: food naturally high in proteins, calcium, probiotics and prebiotics DRG: diet + 4 reps of 1 isometric exercise |
↓ Weight and fat in DG and DRG
↓ Visceral fat in DRG |
| [163] |
(n = 36) age 63–75 years ARG (n = 18) CG (n = 18) |
9 months (during AI) 3 d/w ARG: 30 min at 75/80% HRmax + 3 sets 8–10 reps at 75% 1RM CG: no intervention |
🡹 Osteocalcin in ARG ↓ Total mass, total fat and HDL in ARG |
| [164] | (n = 240) age 52–64 years ARG-HIIT (n = 79) AG-HIIT (n = 80) CG (n = 81) |
16 weeks 2 d/w + 12 months FU (during and after CH) ARG-HIIT: 3 sets 10 rep at 70–80% 1RM + 3 × 3-min bouts on cycle ergometer, 1 min of recovery AG-HIIT: from 20 min MACT to aerobic part of ARG-HIIT CG: no intervention |
🡹 Role functioning in RG-HIIT and AG-HIIT ↓ Total cancer-related fatigue in RG-HIIT and AG-HIIT 🡹 Pain in CG |
| [69] | (n = 23) age 51–63 years ARG-HIIT (n = 8) AG-HIIT (n = 9) CG (n = 13) |
16 weeks 2 d/w + 12 months FU (during and after CH) ARG-HIIT: 3 sets 10 rep at 70–80% 1RM + 3 × 3-min bouts on cycle ergometer, 1 min of recovery AG-HIIT: from 20 min MACT to aerobic part of ARG-HIIT CG: no intervention |
🡹 Muscle fiber CSA and SC count per fiber in ARG-HIIT ↓ Symptoms and displayed gains in lower limb in ARG-HIIT and AG-HIIT 🡹 Number of capillaries per fiber in AG-HIIT ↓ MHC isoform type I and protein levels of PINK1 in CG 🡹 SOD2 level in CG |
Legend: CH, chemotherapy; RT, radiotherapy; HT, hormonal therapy; AI, aromatase inhibitor; AG, aerobic group; RG, resistance group; HAG, home-based aerobic group; ARG, aerobic + resistance group; HARG, home-based aerobic + resistance group; DG, diet group; DRG, diet + resistance group; DARG, diet + aerobic + resistance group; IRG, immediate resistance group; DRG, delayed resistance group; CG, control group; FVLF, fruit and vegetable, low-fat diet; MVPA, moderate to vigorous physical activity; MACT = moderate aerobic continuous training; VO2max, maximal oxygen consumption; 1RM, one-rep maximum BMI, body mass index; Fat, body fat mass; LM, lean mass; ACSM, American College of Sport Medicine; HRmax, maximal heart rate; FU, follow-up; min, minutes; DFS, disease-free survival; RFI, recurrence-free interval; IGFBP-3, insulin-like growth-factor-binding protein 3; IGF-1, insulin-like growth factor; CRP = C-reactive protein; SHBG, sex-hormone-binding globulin; SOD, superoxide dismutase; MHC, myosin heavy chain; CSA, cross-sectional area; SC, satellite cells; FACT-B, the functional assessment of cancer therapy—breast; FACT-G, the functional assessment of cancer therapy—general; SF-36, short form health survey; TNFR2, tumor necrosis factor receptor 2; IL-1B, interleukin 1 beta; HDL, high-density lipoprotein; BSAP, bone-specific alkaline phosphatase; PA, physical activity.
Shmitz et al. [152] evidenced that weight exercise protocols can be performed safely and without contraindications immediately after the traditional cancer treatments, increasing muscle mass, as well as decreasing body fat % and IGF-II levels. During recent years, literature showed the effectiveness of training, not only after the treatment, but also during radiotherapy and chemotherapy [157,165,166]. One of the first studies on ER+ patients compared aerobic and strength protocols performed at home [167], with a no intervention group; data reported a most evident increase in aerobic capacity and a reduction in body mineral density (BDM) decline in the aerobic group compared to the others, suggesting that home-based aerobic protocol may prevent or at least minimize bone loss observed during chemotherapy, counteracting the long-term side effects. Similarly, Ligibel and colleagues [154] highlighted, in BC patients undergoing hormonal therapy (HT), the effects of a combined protocol, unsupervised aerobic and supervised strength training, on fast insulin levels and hip circumference, despite no insulin resistance, fasting glucose or body mass index (BMI) modification being reported. These results support the relationship between PA and BC prognosis through the modulation of insulin levels and/or body fat or fat deposition. A similar type of protocol, supervised + unsupervised aerobic activity, was proposed to BC after CH [156], and the results confirm that a moderate-intensity aerobic exercise can induce favorable changes in body composition improving the disease prognosis. Moreover, in recent years, studies have focused their attention on the effect of exercise on C-reactive protein (CRP) and interleukins in BC patients [157,159,160,167]. The aerobic protocol proposed by Guinan et al. [157] showed a decrease in waist circumference, but no changes were evidenced in CRP, blood pressure, high-density lipoprotein (HDL), and insulin resistance, probably because 8 weeks are not enough to produce these types of modulations. On the other hand, Rogers et al. [160] proposed a combined protocol, unsupervised aerobic and supervised strength, to 15 BC patients to evaluate the effects on the inflammatory system. The results showed an improvement in predicted oxygen consumption and sleep latency, but, contrary to the hypothesis, an increase in IL-6 and a decrease in IL-10 and adiponectin, probably due to the small sample size or to the differences between the group baseline characteristics. The following year, the same authors [159] confirmed the previous results on IL-10, sleep dysfunction and VO2max, showing a decrease in % of body fat in the active group. They also revealed that the increase in fatigue intensity seems to be mediated by interleukin IL-6 and IL-10; instead, the decrease in fatigue interference could be mediated by sleep dysfunction. Moreover, the reduction in general fatigue could be mediated by minutes of PA, sleep dysfunction, and PA enjoyment. These results add significant data about the importance of biobehavioral factors as mediators of fatigue management in BC patients. According to de Paulo et al. [163], 9 months of supervised high-intensity combined training performed three times per week can increase those parameters, such as total and fat mass, HDL and osteocalcin levels, decreasing the side effects of aromatase inhibitors in old BC patients. In 2018 and 2019, Mijwel et al. [69,100] proposed two different types of high-intensity interval training (HIIT), as well as a combined and aerobic protocol, to BC patients during and after treatment. The first study evidenced a decrease in fatigue sensation in both active groups and a decrease in pain perception in the control group [164]. The second study [69] confirmed those results and showed an increase in muscle fiber cross-sectional area and satellite cell count per fiber in the combined HIIT group, an increase in the number of capillaries per fiber in the aerobic HIIT group and a decrease in MHC isoform type I and protein levels of PINK1 in the control group. These results illustrate the importance of exercise in patients undergoing chemotherapy to prevent the negative side effects of treatment and inactivity through preserving skeletal muscle mass and function. In conclusion, supervised aerobic and strength training performed during chemotherapy seems to be one of the best adjuvant treatments able to improve survivorship in ER+ BC patients [161]. Moreover, the combination between exercise and diet seems to be a new effective strategy to counteract the treatment side effect of the disease and treatments [155,158,162]. According to Demark-Wahnefried et al. [155], the combination of a calcium diet, 6 months of exercise and a fruit and vegetable, low-fat diet can decrease waist circumference and % body fat despite no change in insulin, proinsulin, IGF-1, CRP, cholesterol, SHBG, IL-1B, and TNFR2 levels being detected. As reported by Scott et al. [158], an aerobic and strength protocol combined with a daily caloric reduction of 600 kcal below the patient’s requirement produces a decrease in central adiposity, waist to hip ratio (WHR), total cholesterol and leptin levels as well as an increase in predicted VO2max. These findings suggest that a well-tailored protocol combined with a hypocaloric diet positively impact on long-term prognosis in overweight BC patients undergoing treatments. Indeed, as reported by Artene et al. [162], diet is effective for ER+/PR±/HER2- BC patients on anti-estrogenic medication, but adding at least a minimal exercise protocol improves patients’ chances of counteracting sarcopenic obesity, fatigue, and other negative cancer-related effects.
5.3. Quaternary Prevention
The role of physical exercise is as essential in the quaternary prevention phase as it is in the secondary and tertiary prevention phases. It seems that, in patients with advanced cancer, exercise provides the maintenance and improvement of fitness and physical function and may diminish fatigue sensation, improving quality of life (QoL). It should be considered as an intervention to prevent further health complications [168,169]. Few studies investigated these effects related to specific types of cancer, which are often poorly described. Thus, in this section, the feasibility and the effect of exercise in patients at the terminal stage of BC are evidenced in the presence of metastases, under treatment, with a life expectancy of at least 4 months (Table 4).
Table 4.
Exercise and physical activity as quaternary prevention in advanced-stage breast cancer patients.
| REF. | GROUPS | EXERCISE CHARACTERISTICS | MAIN OUTCOMES |
|---|---|---|---|
| [170] |
(n = 13) Life expectancy ≥ 6 months age 44–75 years YG (n = 13) |
YG: 8 weekly group session (during CH) |
↓ Pain, fatigue distress 🡹 Relaxation, invigoration |
| [171] | (n = 101) Life expectancy ≥ 12 months age 59–59 years AG (n = 48) CG (n = 53) |
16 weeks (during CH) AG: 150 min MVPA per week CG: no intervention |
=min/w exercise and physical functioning in AG |
| [172] | (n = 65) age 62–72 years AG (n = 33) CG (n = 32) |
12 weeks 3 d/w (during CH) AG: 55–80 % VO2peak on treadmill CG: no intervention |
🡹VO2peak and functional capacity in AG. Attendance rate 63%, permanent discontinuation 27%, dose modification 49%, acceptable tolerability 42% in AG. |
| [173] | (n = 14) Life expectancy at least 4 months age ≥ 18 years HARG (n = 8) CG (n = 6) |
8 weeks 2 d/w (during CH and HT) HARG: supervised RT 2 sets of 12 repetitions 1 min recovery, intensity 6–7 Adult OMNI Scale + unsupervised 10–15 min walking CG: no intervention |
🡹FACIT-F score, VO2max and six-minute walking test in HARG. Adherence 100% in RT and 25% in walking. |
| [174] | (n = 48) Life expectancy ≥ 9 months age 56–67 years YG (n = 30) CG (n = 18) |
8 week 5–6 d/w (undergoing treatments) YG: meditation, gentle postures, breathing techniques, presentations on yogic principles for optimal coping. 15–30 min/d CG: Discussion about several topic related to the disease concerns |
↓ Pain levels in YG and CG Dose–response relationship between YG, duration and daily pain. |
| [175] | (n = 49) age 55–65 years HPA (n = 49) |
6 months (during CH, RT, HT, TT) HPA: reach 10,000 steps per day. |
🡹HPA increases 6-MWT, quadriceps strength ↓ BMI =muscle CSA, skeletal muscle radiodensity, LM. |
Legend: CH, chemotherapy; RT, radiotherapy; HT, hormonal therapy; TT, targeted therapy; AG, aerobic group; HARG, home-based aerobic + resistance group; YG, yoga group; HPA, home physical activity; CG, control group; MVPA, moderate to vigorous physical activity; BMI, body mass index; VO2peak, peak oxygen uptake; FACIT-F, functional assessment of chronic illness therapy—fatigue; CSA, cross-sectional area; LM, lean body mass; 6MWT, 6 min walking test; min = minutes.
According to the studies, the training protocols feasibility and effect on the metastatic BC patient undergoing treatments are still controversial [171,172,173,175]. It seems that an aerobic exercise, supervised or unsupervised, that reaches 150 min of moderate-intensity aerobic training per week is safe but not feasible [170], and it did not show significant improvements in physical functioning in a heterogeneous group of women living with advanced BC [171]. On the contrary, 8-week home-based supervised resistance training combined with an unsupervised walking program seems to be feasible, improving fatigue sensation, VO2max and functional capacity [173]. These data suggest that further studies are needed to explore alternative interventions to determine whether exercise could help women with metastatic disease to live more fully with fewer symptoms from disease and treatment. As highlighted by Carson et al. [170,174], PA such as yoga could be useful for the treatment of side effects. In particular, 8 weeks of meditation, gentle postures and breathing techniques seems to reduce the daily pain and fatigue distress, increasing relaxation and invigorating the patients.
Our analysis of the literature is synthesized in Figure 3, highlighting that the most beneficial effects of exercise for primary prevention of ER+ BC were found with both an endurance activity (e.g., 5 d/w, 45 min at 60–85% HR max) and a combined activity (i.e., 4 h/w endurance at 60–90% HR max, and strength at 65% of 1RM); regarding secondary and tertiary prevention, the combination between endurance and strength training (i.e., 3 d/w, 60 min endurance at 80% VO2max, and strength at 70% of 1RM) can affect the tumor development and progression during and after treatments; finally, for the quaternary prevention, 150 min per week of aerobic activity (e.g., yoga or walking activity) seems feasible and increases QoL in BC patients.
Figure 3.
Physical activity recommendations based on scientific evidence and stratified for each prevention level of breast cancer. d, day; w, week; HR max, heart rate max; 1RM, one-repetition maximum.
6. Conclusions
BC is one of the most common cancers in the world, but cancer survivors in high-income countries have also grown thanks to medical advances. Most BCs express ER and/or PR. Among the modifiable risk factors involved in excessive estrogen exposure, body fat was identified to be responsible for estrogen biosynthesis and their signaling pathways. Indeed, during the last decade, an increased prevalence of female obesity characterized by an unhealthy body composition was reported worldwide. It is precisely this group of women who are considered to be at a high risk of developing this BC subgroup.
To date, it is still a challenge to estimate the magnitude of the clinical impact of PA on the observed levels of sex hormones, since there are no absolute cut-off values defined that correspond with a certain change in future BC risk and disease progression. However, besides an important effect on circulating sex hormone levels, it should also be considered that different studies on pre-clinical BC animal models demonstrate an important effect of PA to increase the ERβ/ERα ratio, as well as an increase in mammary gland cell apoptosis [41,176,177].
Furthermore, studies conducted in recent years highlight the role of PA not only as a protective factor for the development of ER+ BC but also as a useful tool in the management of BC treatment as an adjuvant to traditional therapies.
In the future, it is a priority to introduce PA in health care paths as well as to improve our knowledge with studies based on exercise-related health promotion. We also hope to focus on the primordial prevention of BC to avoid, where possible, the development of risk factors in the first place.
Author Contributions
Conceptualization, I.D., C.A. and E.G.; literature review, I.D., C.A., E.G. and A.A.; writing-original draft preparation, I.D., C.A. and E.G.; writing-review and editing, I.D., C.A., E.G., G.D., E.A.G., D.C., A.A., A.M., A.P. and L.D.L.; supervision, I.D., A.P. and L.D.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the University of Rome Foro Italico (Research Grant 2017 Prot. 18/002168-GEN) to A.P.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Torre L.A., Islami F., Siegel R.L., Ward E.M., Jemal A. Global Cancer in Women: Burden and Trends. Cancer Epidemiol. Biomark. Prev. 2017;26:444–457. doi: 10.1158/1055-9965.EPI-16-0858. [DOI] [PubMed] [Google Scholar]
- 2.Harbeck N., Penault-Llorca F., Cortes J., Gnant M., Houssami N., Poortmans P., Ruddy K., Tsang J., Cardoso F. Breast cancer. Nat. Rev. Dis. Primers. 2019;5:66. doi: 10.1038/s41572-019-0111-2. [DOI] [PubMed] [Google Scholar]
- 3.Harbeck N. Advances in targeting HER2-positive breast cancer. Curr. Opin. Obs. Gynecol. 2018;30:55–59. doi: 10.1097/GCO.0000000000000431. [DOI] [PubMed] [Google Scholar]
- 4.Van Bockstal M.R., Agahozo M.C., Koppert L.B., van Deurzen C.H.M. A retrospective alternative for active surveillance trials for ductal carcinoma in situ of the breast. Int. J. Cancer. 2020;146:1189–1197. doi: 10.1002/ijc.32362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheang M.C., Martin M., Nielsen T.O., Prat A., Voduc D., Rodriguez-Lescure A., Ruiz A., Chia S., Shepherd L., Ruiz-Borrego M., et al. Defining breast cancer intrinsic subtypes by quantitative receptor expression. Oncologist. 2015;20:474–482. doi: 10.1634/theoncologist.2014-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Cancer Society . Breast Cancer Facts & Figures 2019–2020. American Cancer Society, Inc.; Atlanta, GA, USA: 2019. [Google Scholar]
- 7.Carreira H., Williams R., Funston G., Stanway S., Bhaskaran K. Associations between breast cancer survivorship and adverse mental health outcomes: A matched population-based cohort study in the United Kingdom. PLoS Med. 2021;18:e1003504. doi: 10.1371/journal.pmed.1003504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Picon-Ruiz M., Morata-Tarifa C., Valle-Goffin J.J., Friedman E.R., Slingerland J.M. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J. Clin. 2017;67:378–397. doi: 10.3322/caac.21405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roy R., Moses M.A. ADAM12 induces estrogen-independence in breast cancer cells. Breast Cancer Res. Treat. 2012;131:731–741. doi: 10.1007/s10549-011-1431-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siersbæk R., Kumar S., Carroll J.S. Signaling pathways and steroid receptors modulating estrogen receptor α function in breast cancer. Genes Dev. 2018;32:1141–1154. doi: 10.1101/gad.316646.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang B., Warner M., Gustafsson J.Å. Estrogen receptors in breast carcinogenesis and endocrine therapy. Mol. Cell Endocrinol. 2015;15:240–244. doi: 10.1016/j.mce.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 12.Zekas E., Prossnitz E.R. Estrogen-mediated inactivation of FOXO3a by the G protein-coupled estrogen receptor GPER. BMC Cancer. 2015;15:702. doi: 10.1186/s12885-015-1699-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eyster K.M. The Estrogen Receptors: An Overview from Different Perspectives. Methods Mol. Biol. 2016;1366:1–10. doi: 10.1007/978-1-4939-3127-9_1. [DOI] [PubMed] [Google Scholar]
- 14.Girgert R., Emons G., Gründker C. Estrogen Signaling in ERα-Negative Breast Cancer: ERβ and GPER. Front. Endocrinol. 2019;9:781. doi: 10.3389/fendo.2018.00781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gérard C., Brown K.A. Obesity and breast cancer—Role of estrogens and the molecular underpinnings of aromatase regulation in breast adipose tissue. Mol. Cell Endocrinol. 2018;466:15–30. doi: 10.1016/j.mce.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 16.NIH Common Fund . Molecular Imaging and Contrast Agent Database (MICAD) National Center for Biotechnology Information; Bethesda, MD, USA: 2013. pp. 2004–2013. [PubMed] [Google Scholar]
- 17.Saczko J., Michel O., Chwiłkowska A., Sawicka E., Mączyńska J., Kulbacka J. Estrogen Receptors in Cell Membranes: Regulation and Signaling. Adv. Anat. Embryol. Cell Biol. 2017;227:93–105. doi: 10.1007/978-3-319-56895-9_6. [DOI] [PubMed] [Google Scholar]
- 18.Hua H., Zhang H., Kong Q., Jiang Y. Mechanisms for estrogen receptor expression in human cancer. Exp. Hematol. Oncol. 2018;7:24. doi: 10.1186/s40164-018-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmieri C., Cheng G.J., Saji S., Zelada-Hedman M., Wärri A., Weihua Z., Van Noorden S., Wahlstrom T., Coombes R.C., Warner M., et al. Estrogen receptor beta in breast cancer. Endocr. Relat. Cancer. 2002;9:1–13. doi: 10.1677/erc.0.0090001. [DOI] [PubMed] [Google Scholar]
- 20.Speirs V., Skliris G.P., Burdall S.E., Carder P.J. Distinct expression patterns of ER alpha and ER beta in normal human mammary gland. J. Clin. Pathol. 2002;55:371–374. doi: 10.1136/jcp.55.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou Y., Liu X. The role of estrogen receptor beta in breast cancer. Biomark Res. 2020;8:39. doi: 10.1186/s40364-020-00223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng Y., Miki Y., Nakanishi A. Estradiol/GPER affects the integrity of mammary duct-like structures in vitro. Sci. Rep. 2020;10:1386. doi: 10.1038/s41598-020-57819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox E.M., Davis R.J., Shupnik M.A. ERbeta in breast cancer--onlooker, passive player, or active protector? Steroids. 2008;11:1039–1051. doi: 10.1016/j.steroids.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song P., Li Y., Dong Y., Liang Y., Qu H., Qi D., Lu Y., Jin X., Guo Y., Jia Y., et al. Estrogen receptor β inhibits breast cancer cells migration and invasion through CLDN6-mediated autophagy. J. Exp. Clin. Cancer Res. 2019;38:354. doi: 10.1186/s13046-019-1359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pupo M., Maggiolini M., Musti A.M. GPER Mediates Non-Genomic Effects of Estrogen. Methods Mol. Biol. 2016;1366:471–488. doi: 10.1007/978-1-4939-3127-9_37. [DOI] [PubMed] [Google Scholar]
- 26.Anbalagan M., Rowan B.G. Estrogen receptor alpha phosphorylation and its functional impact in human breast cancer. Mol. Cell Endocrinol. 2015;418:264–272. doi: 10.1016/j.mce.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 27.Kato S., Endoh H., Masuhiro Y., Kitamoto T., Uchiyama S., Sasaki H., Masushige S., Gotoh Y., Nishida E., Kawashima H., et al. Activation of the estrogen receptor through phosphorylation by mitogen-activated protein kinase. Science. 1995;270:1491–1494. doi: 10.1126/science.270.5241.1491. [DOI] [PubMed] [Google Scholar]
- 28.Bunone G., Briand P.A., Miksicek R.J., Picard D. Activation of the unliganded estrogen receptor by EGF involves the MAP kinase pathway and direct phosphorylation. EMBO J. 1996;15:2174–2183. doi: 10.1002/j.1460-2075.1996.tb00571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen J., Stavro P.M., Thompson L.U. Dietary flaxseed inhibits human breast cancer growth and metastasis and downregulates expression of insulin-like growth factor and epidermal growth factor receptor. Nutr. Cancer. 2002;43:187–192. doi: 10.1207/S15327914NC432_9. [DOI] [PubMed] [Google Scholar]
- 30.Lupien M., Meyer C.A., Bailey S.T., Eeckhoute J., Cook J., Westerling T., Zhang X., Carroll J.S., Rhodes D.R., Liu X.S., et al. Growth factor stimulation induces a distinct ER(alpha) cistrome underlying breast cancer endocrine resistance. Genes Dev. 2010;24:2219–2227. doi: 10.1101/gad.1944810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Magnani L., Patten D.K., Nguyen V.T., Hong S.P., Steel J.H., Patel N., Lombardo Y., Faronato M., Gomes A.R., Woodley L., et al. The pioneer factor PBX1 is a novel driver of metastatic progression in ERα-positive breast cancer. Oncotarget. 2015;6:21878–21891. doi: 10.18632/oncotarget.4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harrod A., Fulton J., Nguyen V.T.M., Periyasamy M., Ramos-Garcia L., Lai C.F., Metodieva G., de Giorgio A., Williams R.L., Santos D.B., et al. Genomic modelling of the ESR1 Y537S mutation for evaluating function and new therapeutic approaches for metastatic breast cancer. Oncogene. 2017;36:2286–2296. doi: 10.1038/onc.2016.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jeselsohn R., Bergholz J.S., Pun M., Cornwell M., Liu W., Nardone A., Xiao T., Li W., Qiu X., Buchwalter G., et al. Allele-Specific Chromatin Recruitment and Therapeutic Vulnerabilities of ESR1 Activating Mutations. Cancer Cell. 2018;33:173–186. doi: 10.1016/j.ccell.2018.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michalides R., Griekspoor A., Balkenende A., Verwoerd D., Janssen L., Jalink K., Floore A., Velds A., van’t Veer L., Neefjes J. Tamoxifen resistance by a conformational arrest of the estrogen receptor alpha after PKA activation in breast cancer. Cancer Cell. 2004;5:597–605. doi: 10.1016/j.ccr.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 35.Wang R.A., Mazumdar A., Vadlamudi R.K., Kumar R. P21-activated kinase-1 phosphorylates and transactivates estrogen receptor-alpha and promotes hyperplasia in mammary epithelium. EMBO J. 2002;21:5437–5447. doi: 10.1093/emboj/cdf543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Leeuw R., Flach K., Bentin Toaldo C., Alexi X., Canisius S., Neefjes J., Michalides R., Zwart W. PKA phosphorylation redirects ERα to promoters of a unique gene set to induce tamoxifen resistance. Oncogene. 2013;32:3543–3551. doi: 10.1038/onc.2012.361. [DOI] [PubMed] [Google Scholar]
- 37.Stender J.D., Nwachukwu J.C., Kastrati I., Kim Y., Strid T., Yakir M., Srinivasan S., Nowak J., Izard T., Rangarajan E.S., et al. Structural and Molecular Mechanisms of Cytokine-Mediated Endocrine Resistance in Human Breast Cancer Cells. Mol. Cell. 2017;65:1122–1135. doi: 10.1016/j.molcel.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hurtado A., Holmes K.A., Ross-Innes C.S., Schmidt D., Carroll J.S. FOXA1 is a key determinant of estrogen receptor function and endocrine response. Nat. Genet. 2011;43:27–33. doi: 10.1038/ng.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tan S.K., Lin Z.H., Chang C.W., Varang V., Chng K.R., Pan Y.F., Yong E.L., Sung W.K., Cheung E. AP-2γ regulates oestrogen receptor-mediated long-range chromatin interaction and gene transcription. EMBO J. 2011;30:2569–2581. doi: 10.1038/emboj.2011.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Theodorou V., Stark R., Menon S., Carroll J.S. GATA3 acts upstream of FOXA1 in mediating ESR1 binding by shaping enhancer accessibility. Genome Res. 2013;23:12–22. doi: 10.1101/gr.139469.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siewierska K., Malicka I., Kobierzycki C., Grzegrzolka J., Piotrowska A., Paslawska U., Cegielski M., Podhorska-Okolow M., Dziegiel P., Wozniewski M. Effect of Physical Training on the Levels of Sex Hormones and the Expression of Their Receptors in Rats With Induced Mammary Cancer in Secondary Prevention Model—Preliminary Study. In Vivo. 2020;2:495–501. doi: 10.21873/invivo.11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kahn C.R., Wang G., Lee K.Y. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J. Clin. Investig. 2019;129:3990–4000. doi: 10.1172/JCI129187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zorena K., Jachimowicz-Duda O., Ślęzak D., Robakowska M., Mrugacz M. Adipokines and Obesity. Potential Link to Metabolic Disorders and Chronic Complications. Int. J. Mol. Sci. 2020;21:3570. doi: 10.3390/ijms21103570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaisanlahti A., Glumoff T. Browning of white fat: Agents and implications for beige adipose tissue to type 2 diabetes. J. Physiol. Biochem. 2019;1:1–10. doi: 10.1007/s13105-018-0658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mulya A., Kirwan J.P. Brown and Beige Adipose Tissue: Therapy for Obesity and Its Comorbidities? Endocrinol. Metab. Clin. N. Am. 2016;3:605–621. doi: 10.1016/j.ecl.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muller S., Ader I., Creff J., Leménager H., Achard P., Casteilla L., Sensebé L., Carrière A., Deschaseaux F. Human adipose stromal-vascular fraction self-organizes to form vascularized adipose tissue in 3D cultures. Sci. Rep. 2019;1:7250. doi: 10.1038/s41598-019-43624-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Müller S., Kulenkampff E., Wolfrum C. Adipose Tissue Stem Cells. Handb. Exp. Pharm. 2016;233:251–263. doi: 10.1007/164_2015_13. [DOI] [PubMed] [Google Scholar]
- 48.Ibrahim M.M. Subcutaneous and visceral adipose tissue: Structural and functional differences. Obes. Rev. 2010;11:11–18. doi: 10.1111/j.1467-789X.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 49.Huh J.Y., Park Y.J., Ham M., Kim J.B. Crosstalk between adipocytes and immune cells in adipose tissue inflammation and metabolic dysregulation in obesity. Mol. Cells. 2014;5:365–371. doi: 10.14348/molcells.2014.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu F., Wang A., Li Y., Liang R., Li D., Li B. Adipose Tissue-Resident Regulatory T Cells. Adv. Exp. Med. Biol. 2017;1011:153–162. doi: 10.1007/978-94-024-1170-6_4. [DOI] [PubMed] [Google Scholar]
- 51.Murawska-Ciałowicz E. Adipose tissue—Morphological and biochemical characteristic of different depots. Postepy Hig. Med. Dosw. 2017;71:466–484. doi: 10.5604/01.3001.0010.3829. [DOI] [PubMed] [Google Scholar]
- 52.Chawla A., Nguyen K.D., Goh Y.P. Macrophage-mediated inflammation in metabolic disease. Nat. Rev. Immunol. 2011;11:738–749. doi: 10.1038/nri3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burhans M.S., Hagman D.K., Kuzma J.N., Schmidt K.A., Kratz M. Contribution of Adipose Tissue Inflammation to the Development of Type 2 Diabetes Mellitus. Compr. Physiol. 2018;1:1–58. doi: 10.1002/cphy.c170040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cleary M.P., Grossmann M.E. Obesity and Breast Cancer: The Estrogen Connection. Endocrinology. 2009;150:2537–2542. doi: 10.1210/en.2009-0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kothari C., Diorio C., Durocher F. The Importance of Breast Adipose Tissue in Breast Cancer. Int. J. Mol. Sci. 2020;21:5760. doi: 10.3390/ijms21165760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paronetto M.P., Dimauro I., Grazioli E., Palombo R., Guidotti F., Fantini C., Sgrò P., De Francesco D., Di Luigi L., Capranica L., et al. Exercise-mediated downregulation of MALAT1 expression and implications in primary and secondary cancer prevention. Free Radic. Biol. Med. 2020;160:28–39. doi: 10.1016/j.freeradbiomed.2020.06.037. [DOI] [PubMed] [Google Scholar]
- 57.Dimauro I., Paronetto M.P., Caporossi D. Exercise, redox homeostasis and the epigenetic landscape. Redox Biol. 2020;35:101477. doi: 10.1016/j.redox.2020.101477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grazioli E., Dimauro I., Mercatelli N., Wang G., Pitsiladis Y., Di Luigi L., Caporossi D. Physical activity in the prevention of human diseases: Role of epigenetic modifications. BMC Genom. 2017;18:802. doi: 10.1186/s12864-017-4193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khalafi M., Malandish A., Rosenkranz S.K. The impact of exercise training on inflammatory markers in postmenopausal women: A systemic review and meta-analysis. Exp. Gerontol. 2021;150:111398. doi: 10.1016/j.exger.2021.111398. [DOI] [PubMed] [Google Scholar]
- 60.Sgrò P., Emerenziani G.P., Antinozzi C., Sacchetti M., Di Luigi L. Exercise as a drug for glucose management and prevention in type 2 diabetes mellitus. Curr. Opin. Pharm. 2021;59:95–102. doi: 10.1016/j.coph.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 61.Birbrair A., Zhang T., Wang Z.M., Messi M.L., Enikolopov G.N., Mintz A., Delbono O. Role of pericytes in skeletal muscle regeneration and fat accumulation. Stem Cells Dev. 2013;16:2298–2314. doi: 10.1089/scd.2012.0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lafontan M., Langin D. Lipolysis and lipid mobilization in human adipose tissue. Prog. Lipid Res. 2009;5:275–297. doi: 10.1016/j.plipres.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 63.Jaworski K., Sarkadi-Nagy E., Duncan R.E., Ahmadian M., Sul H.S. Regulation of triglyceride metabolism. IV. Hormonal regulation of lipolysis in adipose tissue. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;1:G1–G4. doi: 10.1152/ajpgi.00554.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vieira-Potter V.J., Zidon T.M., Padilla J. Exercise and Estrogen Make Fat Cells “Fit”. Exerc. Sport Sci. Rev. 2015;43:172–178. doi: 10.1249/JES.0000000000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dasso N.A. How is exercise different from physical activity? A concept analysis. Nurs. Forum. 2019;54:45–52. doi: 10.1111/nuf.12296. [DOI] [PubMed] [Google Scholar]
- 66.WHO . WHO Guidelines on Physical Activity and Sedentary Behaviour. World Health Organization; Geneva, Switzerland: 2020. [PubMed] [Google Scholar]
- 67.van Waart H., Stuiver M.M., van Harten W.H., Geleijn E., Kieffer J.M., Buffart L.M., de Maaker-Berkhof M., Boven E., Schrama J., Geenen M.M., et al. Effect of Low-Intensity Physical Activity and Moderate- to High-Intensity Physical Exercise During Adjuvant Chemotherapy on Physical Fitness, Fatigue, and Chemotherapy Completion Rates: Results of the PACES Randomized Clinical Trial. J. Clin. Oncol. 2015;33:1918–1927. doi: 10.1200/JCO.2014.59.1081. [DOI] [PubMed] [Google Scholar]
- 68.Travier N., Velthuis M.J., Steins Bisschop C.N., van den Buijs B., Monninkhof E.M., Backx F., Los M., Erdkamp F., Bloemendal H.J., Rodenhuis C., et al. Effects of an 18-week exercise programme started early during breast cancer treatment: A randomised controlled trial. BMC Med. 2015;13:121. doi: 10.1186/s12916-015-0362-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mijwel S., Cardinale D.A., Norrbom J., Chapman M., Ivarsson N., Wengström Y., Sundberg C.J., Rundqvist H. Exercise training during chemotherapy preserves skeletal muscle fiber area, capillarization, and mitochondrial content in patients with breast cancer. FASEB J. 2018;32:5495–5505. doi: 10.1096/fj.201700968R. [DOI] [PubMed] [Google Scholar]
- 70.Thorsen L., Skovlund E., Strømme S.B., Hornslien K., Dahl A.A., Fosså S.D. Effectiveness of physical activity on cardiorespiratory fitness and health-related quality of life in young and middle-aged cancer patients shortly after chemotherapy. J. Clin. Oncol. 2005;23:2378–2388. doi: 10.1200/JCO.2005.04.106. [DOI] [PubMed] [Google Scholar]
- 71.Rezende L.F.M., Sá T.H., Markozannes G., Rey-López J.P., Lee I.M., Tsilidis K.K., Ioannidis J.P.A., Eluf-Neto J. Physical activity and cancer: An umbrella review of the literature including 22 major anatomical sites and 770,000 cancer cases. Br. J. Sports Med. 2018;52:826–833. doi: 10.1136/bjsports-2017-098391. [DOI] [PubMed] [Google Scholar]
- 72.Chen X., Wang Q., Zhang Y., Xie Q., Tan X. Physical Activity and Risk of Breast Cancer: A Meta-Analysis of 38 Cohort Studies in 45 Study Reports. Value Health. 2019;22:104–128. doi: 10.1016/j.jval.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 73.Grazioli E., Cerulli C., Dimauro I., Moretti E., Murri A., Parisi A. New Strategy of Home-Based Exercise during Pandemic COVID-19 in Breast Cancer Patients: A Case Study. Sustainability. 2020;12:6940. doi: 10.3390/su12176940. [DOI] [Google Scholar]
- 74.Natalucci V., Marini C.F., Flori M., Pietropaolo F., Lucertini F., Annibalini G., Vallorani L., Sisti D., Saltarelli R., Villarini A., et al. Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. J. Clin. Med. 2021;10:2678. doi: 10.3390/jcm10122678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ceci R., Duranti G., Di Filippo E.S., Bondi D., Verratti V., Doria C., Caporossi D., Sabatini S., Dimauro I., Pietrangelo T. Corrigendum to “Endurance training improves plasma superoxide dismutase activity in healthy elderly”. Mech. Ageing Dev. 2020;186:111214. doi: 10.1016/j.mad.2020.111214. [DOI] [PubMed] [Google Scholar]
- 76.Dimauro I., Sgura A., Pittaluga M., Magi F., Fantini C., Mancinelli R., Sgadari A., Fulle S., Caporossi D. Regular exercise participation improves genomic stability in diabetic patients: An exploratory study to analyse telomere length and DNA damage. Sci. Rep. 2017;23:4137. doi: 10.1038/s41598-017-04448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pittaluga M., Sgadari A., Dimauro I., Tavazzi B., Parisi P., Caporossi D. Physical exercise and redox balance in type 2 diabetics: Effects of moderate training on biomarkers of oxidative stress and DNA damage evaluated through comet assay. Oxidative Med. Cell Longev. 2015;2015:981242. doi: 10.1155/2015/981242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Warburton D.E., Nicol C.W., Bredin S.S. Health benefits of physical activity: The evidence. CMAJ. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Capodaglio E.M. Attività fisica, strumento di prevenzione e gestione delle malattie croniche [Physical activity, tool for the prevention and management of chronic diseases] G Ital. Med. Lav. Erg. 2018;40:106–119. [PubMed] [Google Scholar]
- 80.Anderson E., Durstine J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019;1:3–10. doi: 10.1016/j.smhs.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Boshnjaku A., Dimauro I., Krasniqi E., Grazioli E., Tschan H., Migliaccio S., Di Luigi L., Caporossi D. Effect of sport training on forearm bone sites in female handball and soccer players. J. Sports Med. Phys. Fit. 2016;56:1503–1510. [PubMed] [Google Scholar]
- 82.Kisling L.A., Das J.M. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Prevention Strategies. [PubMed] [Google Scholar]
- 83.Coughlin S.S. Epidemiology of Breast Cancer in Women. Adv. Exp. Med. Biol. 2019;1152:9–29. doi: 10.1007/978-3-030-20301-6_2. [DOI] [PubMed] [Google Scholar]
- 84.Nomura S.J., Inoue-Choi M., Lazovich D., Robien K. WCRF/AICR recommendation adherence and breast cancer incidence among postmenopausal women with and without non-modifiable risk factors. Int. J. Cancer. 2016;138:2602–2615. doi: 10.1002/ijc.29994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Midha S., Chawla S., Garg P.K. Modifiable and non-modifiable risk factors for pancreatic cancer: A review. Cancer Lett. 2016;381:269–277. doi: 10.1016/j.canlet.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 86.Filippini S.E., Vega A. Breast cancer genes: Beyond BRCA1 and BRCA2. Front. Biosci. 2013;18:1358–1372. doi: 10.2741/4185. [DOI] [PubMed] [Google Scholar]
- 87.Walter K.R., Ford M.E., Gregoski M.J., Kramer R.M., Knight K.D., Spruill L., Nogueira L.M., Krisanits B.A., Phan V., La Rue A.C., et al. Advanced glycation end products are elevated in estrogen receptor-positive breast cancer patients, alter response to therapy, and can be targeted by lifestyle intervention. Breast Cancer Res. Treat. 2019;173:559–571. doi: 10.1007/s10549-018-4992-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Younes M., Honma N. Estrogen receptor β. Arch. Pathol. Lab. Med. 2011;135:63–66. doi: 10.5858/2010-0448-RAR.1. [DOI] [PubMed] [Google Scholar]
- 89.Linowiecka K., Urbanowska-Domańska O., Guz J., Foksiński M. The potential influence of breast cancer estrogen receptors’ distribution on active DNA demethylation. Contemp. Oncol. 2019;23:74–80. doi: 10.5114/wo.2019.85200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ahmed H.M., Blaha M.J., Nasir K., Rivera J.J., Blumenthal R.S. Effects of physical activity on cardiovascular disease. Am. J. Cardiol. 2012;109:288–295. doi: 10.1016/j.amjcard.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 91.Cartee G.D., Hepple R.T., Bamman M.M., Zierath J.R. Exercise Promotes Healthy Aging of Skeletal Muscle. Cell Metab. 2016;23:1034–1047. doi: 10.1016/j.cmet.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T., Lancet Physical Activity Series Working Group Effect of physical inactivity on major noncommunicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gleeson M., Bishop N.C., Stensel D.J., Lindley M.R., Mastana S.S., Nimmo M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011;11:607–615. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 94.Ceci R., Beltran Valls M.R., Duranti G., Dimauro I., Quaranta F., Pittaluga M., Sabatini S., Caserotti P., Parisi P., Parisi A., et al. Oxidative stress responses to a graded maximal exercise test in older adults following explosive-type resistance training. Redox Biol. 2014;2:65–72. doi: 10.1016/j.redox.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dimauro I., Scalabrin M., Fantini C., Grazioli E., Beltran Valls M.R., Mercatelli N., Parisi A., Sabatini S., Di Luigi L., Caporossi D. Resistance training and redox homeostasis: Correlation with age-associated genomic changes. Redox Biol. 2016;10:34–44. doi: 10.1016/j.redox.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Magi F., Dimauro I., Margheritini F., Duranti G., Mercatelli N., Fantini C., Ripani F.R., Sabatini S., Caporossi D. Telomere length is independently associated with age, oxidative biomarkers, and sport training in skeletal muscle of healthy adult males. Free Radic. Res. 2018;52:639–647. doi: 10.1080/10715762.2018.1459043. [DOI] [PubMed] [Google Scholar]
- 97.Lee E.C., Fragala M.S., Kavouras S.A., Queen R.M., Pryor J.L., Casa D.J. Biomarkers in Sports and Exercise: Tracking Health, Performance, and Recovery in Athletes. J. Strength Cond. Res. 2017;10:2920–2937. doi: 10.1519/JSC.0000000000002122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Matelot D., Schnell F., Kervio G., Ridard C., Thillaye du Boullay N., Wilson M., Carre F. Cardiovascular benefits of endurance training in seniors: 40 is not too late to start. Int. J. Sports Med. 2016;37:625–632. doi: 10.1055/s-0035-1565237. [DOI] [PubMed] [Google Scholar]
- 99.Sigal R.J., Kenny G.P., Boulé N.G., Wells G.A., Prud’homme D., Fortier M., Reid R.D., Tulloch H., Coyle D., Phillips P., et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: A randomized trial. Ann. Intern. Med. 2007;147:357–369. doi: 10.7326/0003-4819-147-6-200709180-00005. [DOI] [PubMed] [Google Scholar]
- 100.Mijwel S., Jervaeus A., Bolam K.A., Norrbom J., Bergh J., Rundqvist H., Wengström Y. High-intensity exercise during chemotherapy induces beneficial effects 12 months into breast cancer survivorship. J. Cancer Surviv. Res. Pract. 2019;13:244–256. doi: 10.1007/s11764-019-00747-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.De Luca V., Minganti C., Borrione P., Grazioli E., Cerulli C., Guerra E., Bonifacino A., Parisi A. Effects of concurrent aerobic and strength training on breast cancer survivors: A pilot study. Public Health. 2016;136:126–132. doi: 10.1016/j.puhe.2016.03.028. [DOI] [PubMed] [Google Scholar]
- 102.Milne H.M., Wallman K.E., Gordon S., Courneya K.S. Effects of a combined aerobic and resistance exercise program in breast cancer survivors: A randomized controlled trial. Breast Cancer Res. Treat. 2008;108:279–288. doi: 10.1007/s10549-007-9602-z. [DOI] [PubMed] [Google Scholar]
- 103.Courneya K.S., Segal R.J., Mackey J.R., Gelmon K., Reid R.D., Friedenreich C.M., Ladha A.B., Proulx C., Vallance J.K., Lane K., et al. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: A multicenter randomized controlled trial. J. Clin. Oncol. 2007;25:4396–4404. doi: 10.1200/JCO.2006.08.2024. [DOI] [PubMed] [Google Scholar]
- 104.Coyle Y.M., Xie X.J., Lewis C.M., Bu D., Milchgrub S., Euhus D.M. Role of physical activity in modulating breast cancer risk as defined by APC and RASSF1A promoter hypermethylation in nonmalignant breast tissue. Cancer Epidemiol. Biomark. Prev. 2007;16:192–196. doi: 10.1158/1055-9965.EPI-06-0700. [DOI] [PubMed] [Google Scholar]
- 105.Murphy E.A., Davis J.M., Barrilleaux T.L., McClellan J.L., Steiner J.L., Carmichael M.D., Pena M.M., Hebert J.R., Green J.E. Benefits of exercise training on breast cancer progression and inflammation in C3(1)SV40Tag mice. Cytokine. 2011;55:274–279. doi: 10.1016/j.cyto.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rao R., Cruz V., Peng Y., Harker-Murray A., Haley B.B., Zhao H., Xie X.J., Euhus D. Bootcamp during neoadjuvant chemotherapy for breast cancer: A randomized pilot trial. Breast Cancer. 2012;6:39–46. doi: 10.4137/BCBCR.S9221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Buss L.A., Dachs G.U. Voluntary exercise slows breast tumor establishment and reduces tumor hypoxia in ApoE-/- mice. J. Appl. Physiol. 2018;124:938–949. doi: 10.1152/japplphysiol.00738.2017. [DOI] [PubMed] [Google Scholar]
- 108.Spencer A., Sligar A.D., Chavarria D., Lee J., Choksi D., Patil N.P., Lee H., Veith A.P., Riley W.J., Desai S., et al. Biomechanical regulation of breast cancer metastasis and progression. Sci. Rep. 2021;11:9838. doi: 10.1038/s41598-021-89288-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jafari A., Sheikholeslami-Vatani D., Khosrobakhsh F., Khaledi N. Synergistic Effects of Exercise Training and Vitamin D Supplementation on Mitochondrial Function of Cardiac Tissue, Antioxidant Capacity, and Tumor Growth in Breast Cancer in Bearing-4T1 Mice. Front. Physiol. 2021;12:640237. doi: 10.3389/fphys.2021.640237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gomes-Santos I.L., Amoozgar Z., Kumar A.S., Ho W.W., Roh K., Talele N.P., Curtis H., Kawaguchi K., Jain R.K., Fukumura D. Exercise training improves tumor control by increasing CD8+ T-cell infiltration via CXCR3 signaling and sensitizes breast cancer to immune checkpoint blockade. Cancer Immunol. Res. 2021;10 doi: 10.1158/2326-6066.CIR-20-0499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Eschke R.K., Lampit A., Schenk A., Javelle F., Steindorf K., Diel P., Bloch W., Zimmer P. Impact of Physical Exercise on Growth and Progression of Cancer in Rodents-A Systematic Review and Meta-Analysis. Front Oncol. 2019;5:35. doi: 10.3389/fonc.2019.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Khori V., Amani Shalamzari S., Isanejad A., Alizadeh A.M., Alizadeh S., Khodayari S., Khodayari H., Shahbazi S., Zahedi A., Sohanaki H., et al. Effects of exercise training together with tamoxifen in reducing mammary tumor burden in mice: Possible underlying pathway of miR-21. Eur. J. Pharm. 2015;765:179–187. doi: 10.1016/j.ejphar.2015.08.031. [DOI] [PubMed] [Google Scholar]
- 113.Ainsworth B.E., Haskell W.L., Herrmann S.D., Meckes N., Bassett D.R., Jr., Tudor-Locke C., Greer J.L., Vezina J., Whitt-Glover M.C., Leon A.S. Compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 114.Kushi L.H., Doyle C., McCullough M., Rock C.L., Demark-Wahnefried W., Bandera E.V., McCullough M., McTiernan A., Gansler T., Andrews K.S., et al. American cancer society guidelines on nutrition and physical activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 2012;62:30–67. doi: 10.3322/caac.20140. [DOI] [PubMed] [Google Scholar]
- 115.World Cancer Research Fund/American Institute for Cancer Research . Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. World Cancer Research Fund; London, UK: 2018. Continuous Update Project External Report. [Google Scholar]
- 116.Friedenreich C.M., Woolcott C.G., McTiernan A., Ballard-Barbash R., Brant R.F., Stanczyk F.Z., Terry T., Boyd N.F., Yaffe M.J., Irwin M.L., et al. Alberta physical activity and breast cancer prevention trial: Sex hormone changes in a year-long exercise intervention among postmenopausal women. J. Clin. Oncol. 2010;28:1458–1466. doi: 10.1200/JCO.2009.24.9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Friedenreich C.M., Neilson H.K., O’Reilly R., Duha A., Yasui Y., Morielli A.R., Adams S.C., Courneya K.S. Effects of a high vs moderate volume of aerobic exercise on adiposity outcomes in postmenopausal women: A randomized clinical trial. JAMA Oncol. 2015;1:766–776. doi: 10.1001/jamaoncol.2015.2239. [DOI] [PubMed] [Google Scholar]
- 118.Friedenreich C.M., Wang Q., Yasui Y., Stanczyk F.Z., Duha A., Brenner D.R., Courneya K.S. Long-term Effects of Moderate versus High Durations of Aerobic Exercise on Biomarkers of Breast Cancer Risk: Follow-up to a Randomized Controlled Trial. Cancer Epidemiol. Biomark. Prev. 2019;28:1725–1734. doi: 10.1158/1055-9965.EPI-19-0523. [DOI] [PubMed] [Google Scholar]
- 119.Campbell K.L., Foster-Schubert K.E., Alfano C.M., Wang C.C., Wang C.Y., Duggan C.R., Mason C., Imayama I., Kong A., Xiao L., et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: Randomized controlled trial. J. Clin. Oncol. 2012;30:2314–2326. doi: 10.1200/JCO.2011.37.9792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.van Gemert W.A., May A.M., Schuit A.J., Oosterhof B.Y., Peeters P.H., Monninkhof E.M. Effect of Weight Loss with or without Exercise on Inflammatory Markers and Adipokines in Postmenopausal Women: The SHAPE-2 Trial, A Randomized Controlled Trial. Cancer Epidemiol. Biomark. Prev. 2016;25:799–806. doi: 10.1158/1055-9965.EPI-15-1065. [DOI] [PubMed] [Google Scholar]
- 121.Khosravi N., Eskandari Z., Farajivafa V., Hanson E.D., Agha-Alinejad H., Abdollah-Pour A., Haghighat S. Effect of 6 months of aerobic training on adipokines as breast cancer risk factors in postmenopausal women: A randomized controlled trial. J. Cancer Res. 2018;14:1336–1340. doi: 10.4103/jcrt.JCRT_684_16. [DOI] [PubMed] [Google Scholar]
- 122.Matthews C.E., Sampson J.N., Brenner D.R., Moore S.C., Courneya K.S., Ziegler R.G., Friedenreich C.M. Effects of Exercise and Cardiorespiratory Fitness on Estrogen Metabolism in Postmenopausal Women. Cancer Epidemiol. Biomark. Prev. 2018;27:1480–1482. doi: 10.1158/1055-9965.EPI-17-0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Duggan C., Tapsoba J.D., Stanczyk F., Wang C.Y., Schubert K.F., McTiernan A. Long-term weight loss maintenance, sex steroid hormones, and sex hormone-binding globulin. Menopause. 2019;26:417–422. doi: 10.1097/GME.0000000000001250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gonzalo-Encabo P., Valadés D., García-Honduvilla N., de Cos Blanco A., Friedenreich C.M., Pérez-López A. Exercise type and fat mass loss regulate breast cancer-related sex hormones in obese and overweight postmenopausal women. Eur. J. Appl. Physiol. 2020;120:1277–1287. doi: 10.1007/s00421-020-04361-1. [DOI] [PubMed] [Google Scholar]
- 125.de Roon M., van Gemert W.A., Peeters P.H., Schuit A.J., Monninkhof E.M. Long-term effects of a weight loss intervention with or without exercise component in postmenopausal women: A randomized trial. Prev. Med. Rep. 2016;5:118–123. doi: 10.1016/j.pmedr.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Foster-Schubert K.E., Alfano C.M., Duggan C.R., Xiao L., Campbell K.L., Kong A., Bain C.E., Wang C.Y., Blackburn G.L., McTiernan A. Effect of diet and exercise, alone or combined, on weight and body composition in overweight-to-obese postmenopausal women. Obesity (Silver Spring) 2012;20:1628–1638. doi: 10.1038/oby.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Monninkhof E.M., Velthuis M.J., Peeters P.H., Twisk J.W., Schuit A.J. Effect of exercise on postmenopausal sex hormone levels and role of body fat: A randomized controlled trial. J. Clin. Oncol. 2009;27:4492–4499. doi: 10.1200/JCO.2008.19.7459. [DOI] [PubMed] [Google Scholar]
- 128.McTiernan A., Tworoger S.S., Rajan K.B., Yasui Y., Sorenson B., Ulrich C.M., Chubak J., Stanczyk F.Z., Bowen D., Irwin M.L., et al. Effect of exercise on serum androgens in postmenopausal women: A 12-month randomized clinical trial. Cancer Epidemiol. Biomark. Prev. 2004;13:1099–1105. [PubMed] [Google Scholar]
- 129.McTiernan A., Tworoger S.S., Ulrich C.M., Yasui Y., Irwin M.L., Rajan K.B., Sorenson B., Rudolph R.E., Bowen D., Stanczyk F.Z., et al. Effect of exercise on serum estrogens in postmenopausal women: A 12-month randomized clinical trial. Cancer Res. 2004;64:2923–2928. doi: 10.1158/0008-5472.CAN-03-3393. [DOI] [PubMed] [Google Scholar]
- 130.Thomas D.T., Erdman K.A., Burke L.M. American College of Sports Medicine Joint Position Statement. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016;3:543–568. doi: 10.1249/MSS.0000000000000852. [DOI] [PubMed] [Google Scholar]
- 131.Wycherley T.P., Moran L.J., Clifton P.M., Noakes M., Brinkworth G.D. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2012;6:1281–1298. doi: 10.3945/ajcn.112.044321. [DOI] [PubMed] [Google Scholar]
- 132.Leidy H.J., Clifton P.M., Astrup A., Wycherley T.P., Westerterp-Plantenga M.S., Luscombe-Marsh N.D., Woods S.C., Mattes R.D. The role of protein in weight loss and maintenance. Am. J. Clin. Nutr. 2015;6:1320S–1329S. doi: 10.3945/ajcn.114.084038. [DOI] [PubMed] [Google Scholar]
- 133.Patel A.V., Friedenreich C.M., Moore S.C., Hayes S.C., Silver J.K., Campbell K.L., Winters-Stone K., Gerber L.H., George S.M., Fulton J.E., et al. American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Med. Sci. Sports Exerc. 2019;51:2391–2402. doi: 10.1249/MSS.0000000000002117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Basen-Engquist K., Carmack C., Brown J., Jhingran A., Baum G., Song J., Scruggs S., Swartz M.C., Cox M.G., Lu K.H. Response to an exercise intervention after endometrial cancer: Differences between obese and non-obese survivors. Gynecol. Oncol. 2014;133:48–55. doi: 10.1016/j.ygyno.2014.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yoh K., Nishikawa H., Enomoto H., Ishii N., Iwata Y., Ishii A., Yuri Y., Miyamoto Y., Hasegawa K., Nakano C., et al. Effect of exercise therapy on sarcopenia in pancreatic cancer: A study protocol for a randomised controlled trial. BMJ Open Gastroenterol. 2018;5:e000194. doi: 10.1136/bmjgast-2017-000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Schmitz K.H., Campbell A.M., Stuiver M.M., Pinto B.M., Schwartz A.L., Morris G.S., Ligibel J.A., Cheville A., Galvão D.A., Alfano C.M., et al. Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA Cancer J. Clin. 2019;69:468–484. doi: 10.3322/caac.21579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Leclerc A.F., Foidart-Dessalle M., Tomasella M., Coucke P., Devos M., Bruyère O., Bury T., Deflandre D., Jerusalem G., Lifrange E., et al. Multidisciplinary rehabilitation program after breast cancer: Benefits on physical function, anthropometry and quality of life. Eur. J. Phys. Rehabil. Med. 2017;53:633–642. doi: 10.23736/S1973-9087.17.04551-8. [DOI] [PubMed] [Google Scholar]
- 138.Cella D., Fallowfield L.J. Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res. Treat. 2008;107:167–180. doi: 10.1007/s10549-007-9548-1. [DOI] [PubMed] [Google Scholar]
- 139.Saghatchian M., Lesur A. Gestion des effets secondaires de l’hormonothérapie du cancer du sein chez la femme jeune [Management of side effects related to adjuvant hormone therapy in young women with breast cancer] Bull Cancer. 2019;106:S37–S42. doi: 10.1016/S0007-4551(20)30046-1. [DOI] [PubMed] [Google Scholar]
- 140.Bundred N.J. The effects of aromatase inhibitors on lipids and thrombosis. Br. J. Cancer. 2005;93:S23–S27. doi: 10.1038/sj.bjc.6602692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fredslund S.O., Gravholt C.H., Laursen B.E., Jensen A.B. Key metabolic parameters change significantly in early breast cancer survivors: An explorative PILOT study. J. Transl. Med. 2019;17:105. doi: 10.1186/s12967-019-1850-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gibb F.W., Dixon J.M., Clarke C., Homer N.Z., Faqehi A.M.M., Andrew R., Walker B.R. Higher Insulin Resistance and Adiposity in Postmenopausal Women With Breast Cancer Treated With Aromatase Inhibitors. J. Clin. Endocrinol. Metab. 2019;104:3670–3678. doi: 10.1210/jc.2018-02339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Foglietta J., Inno A., de Iuliis F., Sini V., Duranti S., Turazza M., Tarantini L., Gori S. Cardiotoxicity of Aromatase Inhibitors in Breast Cancer Patients. Clin. Breast Cancer. 2017;17:11–17. doi: 10.1016/j.clbc.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 144.Zhao F., Ren D., Shen G., Ahmad R., Dong L., Du F., Zhao J. Toxicity of extended adjuvant endocrine with aromatase inhibitors in patients with postmenopausal breast cancer: A Systemtic review and Meta-analysis. Crit. Rev. Oncol. Hematol. 2020;156:103114. doi: 10.1016/j.critrevonc.2020.103114. [DOI] [PubMed] [Google Scholar]
- 145.Jacobse J.N., Schaapveld M., Boekel N.B., Hooning M.J., Jager A., Baaijens M.H.A., Hauptmann M., Russell N.S., Rutgers E.J.T., Aleman B.M.P., et al. Risk of heart failure after systemic treatment for early breast cancer: Results of a cohort study. Breast Cancer Res. Treat. 2021;185:205–214. doi: 10.1007/s10549-020-05930-w. [DOI] [PubMed] [Google Scholar]
- 146.Cheung A.M., Heisey R., Srighanthan J. Breast cancer and osteoporosis. Curr. Opin. Endocrinol. Diabetes Obes. 2013;20:532–538. doi: 10.1097/01.med.0000436195.10599.dd. [DOI] [PubMed] [Google Scholar]
- 147.Imanishi Y. Secondary osteoporosis. Cancer treatment-induced bone loss. Clin. Calcium. 2018;28:1665–1670. [PubMed] [Google Scholar]
- 148.Leslie W.D., Morin S.N., Lix L.M., Niraula S., McCloskey E.V., Johansson H., Harvey N.C., Kanis J.A. Fracture Risk in Women with Breast Cancer Initiating Aromatase Inhibitor Therapy: A Registry-Based Cohort Study. Oncologist. 2019;24:1432–1438. doi: 10.1634/theoncologist.2019-0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nagykálnai T., Landherr L., Mészáros E. Aromatázgátlók és artralgia [Aromatase inhibitors and arthralgia] Magy. Onkol. 2011;55:32–39. [PubMed] [Google Scholar]
- 150.Niravath P. Aromatase inhibitor-induced arthralgia: A review. Ann. Oncol. 2013;24:1443–1449. doi: 10.1093/annonc/mdt037. [DOI] [PubMed] [Google Scholar]
- 151.Romero S.A.D., Su H.I., Satagopan J., Li Q.S., Seluzicki C.M., Dries A., DeMichele A.M., Mao J.J. Clinical and genetic risk factors for aromatase inhibitor-associated arthralgia in breast cancer survivors. Breast. 2020;49:48–54. doi: 10.1016/j.breast.2019.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Schmitz K.H., Ahmed R.L., Hannan P.J., Yee D. Safety and efficacy of weight training in recent breast cancer survivors to alter body composition, insulin, and insulin-like growth factor axis proteins. Cancer Epidemiol. Biomark. Prev. 2005;14:1672–1680. doi: 10.1158/1055-9965.EPI-04-0736. [DOI] [PubMed] [Google Scholar]
- 153.Schwartz A.L., Winters-Stone K. Effects of a 12-month randomized controlled trial of aerobic or resistance exercise during and following cancer treatment in women. Phys. Sportsmed. 2009;37:62–67. doi: 10.3810/psm.2009.10.1730. [DOI] [PubMed] [Google Scholar]
- 154.Ligibel J.A., Campbell N., Chen H., Salinardi T., Chen W., Partridge A., Mantzoros C., Winer E. Impact of physical activity on insulin levels in breast cancer survivors. J. Clin. Oncol. 2008;26:907–912. doi: 10.1200/JCO.2007.12.7357. [DOI] [PubMed] [Google Scholar]
- 155.Demark-Wahnefried W., George S.L., Switzer B.R., Snyder D.C., Madden J.F., Polascik T.J., Ruffin M.T., Vollmer R.T. Overcoming challenges in designing and implementing a phase II randomized controlled trial using a presurgical model to test a dietary intervention in prostate cancer. Clin. Trials. 2008;5:262–272. doi: 10.1177/1740774508091676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Irwin M.L., Alvarez-Reeves M., Cadmus L., Mierzejewski E., Mayne S.T., Yu H., Chung G.G., Jones B., Knobf M.T., DiPietro L. Exercise improves body fat, lean mass, and bone mass in breast cancer survivors. Obesity (Silver Spring) 2009;17:1534–1541. doi: 10.1038/oby.2009.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Guinan E., Hussey J., Broderick J.M., Lithander F.E., O’Donnell D., Kennedy M.J., Connolly E.M. The effect of aerobic exercise on metabolic and inflammatory markers in breast cancer survivors—A pilot study. Support. Care Cancer. 2013;21:1983–1992. doi: 10.1007/s00520-013-1743-5. [DOI] [PubMed] [Google Scholar]
- 158.Scott E., Daley A.J., Doll H., Woodroofe N., Coleman R.E., Mutrie N., Crank H., Powers H.J., Saxton J.M. Effects of an exercise and hypocaloric healthy eating program on biomarkers associated with long-term prognosis after early-stage breast cancer: A randomized controlled trial. Cancer Causes Control. 2013;24:181–191. doi: 10.1007/s10552-012-0104-x. [DOI] [PubMed] [Google Scholar]
- 159.Rogers L.Q., Fogleman A., Trammell R., Hopkins-Price P., Spenner A., Vicari S., Rao K., Courneya K.S., Hoelzer K., Robbs R., et al. Inflammation and psychosocial factors mediate exercise effects on sleep quality in breast cancer survivors: Pilot randomized controlled trial. Psychooncology. 2015;24:302–310. doi: 10.1002/pon.3594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rogers L.Q., Vicari S., Trammell R., Hopkins-Price P., Fogleman A., Spenner A., Rao K., Courneya K.S., Hoelzer K., Robbs R., et al. Biobehavioral factors mediate exercise effects on fatigue in breast cancer survivors. Med. Sci. Sports Exerc. 2014;46:1077–1088. doi: 10.1249/MSS.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Courneya K.S., Segal R.J., McKenzie D.C., Dong H., Gelmon K., Friedenreich C.M., Yasui Y., Reid R.D., Crawford J.J., Mackey J.R. Effects of exercise during adjuvant chemotherapy on breast cancer outcomes. Med. Sci. Sports Exerc. 2014;46:1744–1751. doi: 10.1249/MSS.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 162.Artene D., Blidaru A. Factors that influence oncology nutrition efficacy in breast cancer patients under antiestrogenic treatment. Ann. Oncol. 2018;29:603–640. doi: 10.1093/annonc/mdy300.001. [DOI] [Google Scholar]
- 163.de Paulo T.R.S., Winters-Stone K.M., Viezel J., Rossi F.E., Simões R.R., Tosello G., Freitas I.F. Junior. Effects of resistance plus aerobic training on body composition and metabolic markers in older breast cancer survivors undergoing aromatase inhibitor therapy. Exp. Gerontol. 2018;111:210–217. doi: 10.1016/j.exger.2018.07.022. [DOI] [PubMed] [Google Scholar]
- 164.Mijwel S., Backman M., Bolam K.A., Jervaeus A., Sundberg C.J., Margolin S., Browall M., Rundqvist H., Wengström Y. Adding high-intensity interval training to conventional training modalities: Optimizing health-related outcomes during chemotherapy for breast cancer: The OptiTrain randomized controlled trial. Breast Cancer Res. Treat. 2018;168:79–93. doi: 10.1007/s10549-017-4571-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nuri R., Kordi M.R., Moghaddasi M., Rahnama N., Damirchi A., Rahmani-Nia F., Emami H. Effect of combination exercise training on metabolic syndrome parameters in postmenopausal women with breast cancer. J. Cancer Res. Ther. 2012;8:238–242. doi: 10.4103/0973-1482.98977. [DOI] [PubMed] [Google Scholar]
- 166.Karimi N., Roshan V.D. Change in adiponectin and oxidative stress after modifiable lifestyle interventions in breast cancer cases. Asian Pac. J. Cancer Prev. 2013;14:2845–2850. doi: 10.7314/APJCP.2013.14.5.2845. [DOI] [PubMed] [Google Scholar]
- 167.Kang D.W., Lee J., Suh S.H., Ligibel J., Courneya K.S., Jeon J.Y. Effects of Exercise on Insulin, IGF Axis, Adipocytokines, and Inflammatory Markers in Breast Cancer Survivors: A Systematic Review and Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2017;26:355–365. doi: 10.1158/1055-9965.EPI-16-0602. [DOI] [PubMed] [Google Scholar]
- 168.Dittus K.L., Gramling R.E., Ades P.A. Exercise interventions for individuals with advanced cancer: A systematic review. Prev. Med. 2017;104:124–132. doi: 10.1016/j.ypmed.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 169.Heywood R., McCarthy A.L., Skinner T.L. Safety and feasibility of exercise interventions in patients with advanced cancer: A systematic review. Support. Care Cancer. 2017;25:3031–3050. doi: 10.1007/s00520-017-3827-0. [DOI] [PubMed] [Google Scholar]
- 170.Carson J.W., Carson K.M., Olsen M., Sanders L., Westbrook K., Keefe F.J., Porter L.S. Yoga Practice Predicts Improvements in Day-to-Day Pain in Women with Metastatic Breast Cancer. J. Pain Symptom Manag. 2020;14:30804–30806. doi: 10.1016/j.jpainsymman.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ligibel J.A., Giobbie-Hurder A., Shockro L., Campbell N., Partridge A.H., Tolaney S.M., Lin N.U., Winer E.P. Randomized trial of a physical activity intervention in women with metastatic breast cancer. Cancer. 2016;122:1169–1177. doi: 10.1002/cncr.29899. [DOI] [PubMed] [Google Scholar]
- 172.Scott J.M., Iyengar N.M., Nilsen T.S., Michalski M., Thomas S.M., Herndon J., Sasso J., Yu A., Chandarlapaty S., Dang C.T., et al. Feasibility, safety, and efficacy of aerobic training in pretreated patients with metastatic breast cancer: A randomized controlled trial. Cancer. 2018;124:2552–2560. doi: 10.1002/cncr.31368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Yee J., Davis G.M., Hackett D., Beith J.M., Wilcken N., Currow D., Emery J., Phillips J., Martin A., Hui R., et al. Physical Activity for Symptom Management in Women With Metastatic Breast Cancer: A Randomized Feasibility Trial on Physical Activity and Breast Metastases. J. Pain Symptom Manag. 2019;58:929–939. doi: 10.1016/j.jpainsymman.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 174.Carson J.W., Carson K.M., Porter L.S., Keefe F.J., Shaw H., Miller J.M. Yoga for women with metastatic breast cancer: Results from a pilot study. J. Pain Symptom Manag. 2007;33:331–341. doi: 10.1016/j.jpainsymman.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 175.Delrieu L., Pialoux V., Pérol O., Morelle M., Martin A., Friedenreich C., Febvey-Combes O., Pérol D., Belladame E., Clémençon M., et al. Feasibility and Health Benefits of an Individualized Physical Activity Intervention in Women With Metastatic Breast Cancer: Intervention Study. JMIR mHealth uHealth. 2020;8:e12306. doi: 10.2196/12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang M., Yu B., Westerlind K., Strange R., Khan G., Patil D., Boeneman K., Hilakivi-Clarke L. Prepubertal physical activity up-regulates estrogen receptor beta, BRCA1 and p53 mRNA expression in the rat mammary gland. Breast Cancer Res. Treat. 2009;1:213–220. doi: 10.1007/s10549-008-0062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Enger S.M., Ross R.K., Paganini-Hill A., Carpenter C.L., Bernstein L. Carpenter and Leslie Bernstein Body Size, Physical Activity, and Breast Cancer Hormone Receptor Status: Results from Two Case-Control Studies Cancer Epidemiol. Biomark. Prev. 2000;9:681–687. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.