Abstract
Cellular iron homeostasis and mitochondrial iron homeostasis are interdependent. Mitochondria must import iron to form iron–sulfur clusters and heme, and to incorporate these cofactors along with iron ions into mitochondrial proteins that support essential functions, including cellular respiration. In turn, mitochondria supply the cell with heme and enable the biogenesis of cytosolic and nuclear proteins containing iron–sulfur clusters. Impairment in cellular or mitochondrial iron homeostasis is deleterious and can result in numerous human diseases. Due to its reactivity, iron is stored and trafficked through the body, intracellularly, and within mitochondria via carefully orchestrated processes. Here, we focus on describing the processes of and components involved in mitochondrial iron trafficking and storage, as well as mitochondrial iron–sulfur cluster biogenesis and heme biosynthesis. Recent findings and the most pressing topics for future research are highlighted.
Keywords: iron homeostasis, mitochondrial iron–sulfur clusters, heme biosynthesis, iron trafficking
1. Introduction
Most iron in vertebrates is used to make heme b cofactors for hemoglobin in red blood cells; however, the essential nature of iron derives from more than this role in oxygen transport through the bloodstream. Iron functions in a variety of cellular processes, including enzyme catalysis, DNA synthesis, gas sensing, electron transport, and mitochondrial respiration [1,2]. Iron is critical to the function of mitochondria, including the organelles’ energy-producing capabilities, which have earned them the nickname the “powerhouses of the cell” [3,4,5].
To generate ATP, mitochondria—and, more specifically, mitochondrial enzymes composing the citric acid cycle (TCA cycle) and oxidative phosphorylation system (OXPHOS)—require the iron-containing cofactors iron–sulfur clusters (ISCs) and heme [4,6,7,8]. These two types of cofactors are produced via highly conserved processes through multistep synthetic pathways that occur in part in the mitochondrial matrix [7,8]. Both ISC biogenesis and heme biosynthesis require proper iron homeostasis, which begins with environmental iron acquisition and its efficient translocation to the mitochondrial matrix.
1.1. Clinical Significance of Iron Homeostasis
Perturbations in iron homeostasis manifest in a vast spectrum of disorders. Oftentimes, these maladies result from mutations, which can occur in any one of a large number of genes. The most common iron-related clinical manifestations result from iron deficiency and, in the most severe cases, are diagnosed as one of numerous anemias [1,9,10]. Some iron-related diseases result from iron accumulation or overload, such as hemochromatosis and iron-loading anemias—thalassemias, congenital dyserythropoietic anemias, sideroblastic anemias, and myelodysplastic syndromes [11,12,13,14,15]. Both iron overload and deficiency are associated with adverse patient outcomes, including cardiovascular disease, cognitive impairment and neurodegeneration, organ failure, diabetes mellitus, and various cancers [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. Defects in heme biosynthesis cause hereditary porphyria diseases, and mutations in many of the genes involved in ISC biosynthesis also result in human disease [34,35].
At a molecular level, disruptions to mitochondrial iron homeostasis may lead to ferroptosis—a recently identified form of non-apoptotic cell death. Ferroptosis is primarily initiated by iron-dependent lipid peroxidation, which can be caused by aberrant mitochondrial iron storage, defective ISC biogenesis, or disturbed heme homeostasis (as reviewed in [36]).
1.2. Iron Transport and Cellular Uptake
Due to the reactivity of iron through Fenton-chemistry-like reactions, iron metabolism and transport are meticulously orchestrated by transport molecules [37]. Iron acquired through the diet is taken up by enterocytes via the plasma-membrane-bound divalent metal transporter (DMT1) or, in the case of heme, one of the plasma membrane heme importers. Feline leukemia virus subgroup C receptor-related (FLVCR) protein 2 and heme carrier protein 1 (HCP1) have been identified as heme importers in mammals, but their roles in heme transport and heme transporting mechanisms are debated [7,38,39]. Iron not used by those enterocytes is exported into bodily fluids by the transporter ferroportin or stored in ferritin.
In vertebrates, circulating ferric iron (Fe3+) in the bloodstream is bound to the plasma iron-transport protein transferrin (Tf). To deliver iron to tissues, Tf binds to transferrin receptor 1 (TfR1) on the cellular membrane of the target cell. The iron-loaded Tf–TfR1 assembly is endocytosed, and iron is released into the endosome, where it is reduced to the ferrous (Fe2+) state [40,41,42,43]. The plasma membrane metal ion transporter ZIP14 has been shown to participate in the uptake of both transferrin-bound and non-transferrin-bound iron [44,45]. Plasma heme and hemoglobin serve as alternative iron sources, since they too can be endocytosed from blood plasma following their sequestration by hemopexin and haptoglobin. From the endosome, iron relocates to the cytosol via DMT1 [46].
In unicellular eukaryotes such as the budding yeast Saccharomyces cerevisiae, iron is imported through several pathways. Iron import can be mediated by the Fet3/Ftr1 complex on the plasma membrane, which functions with high affinity for iron [47,48], or by a low-affinity iron import pathway, which involves the plasma membrane proteins Smf1 and Fet4 [49,50]. Similar to some prokaryotes, budding yeast can also take up iron that is siderophore-bound, in a process mediated by the ARN family transporters [51]. Unlike in metazoans, exogenous heme uptake pathways in S. cerevisiae are not efficient, so heme supplies a negligible amount of iron. Once within the cell, iron is stored in the vacuole until needed in the cytosol or other cellular compartments [52].
Iron in the cytosol forms the dynamic reservoir known as the cytosolic labile iron pool (CLIP). The CLIP consists of ferrous iron either stored within the protein ferritin (particularly in the liver in mammals) or chelated by low-molecular-mass ligands to form complexes. In S. cerevisiae and higher order eukaryotes, small molecules such as citrate, cysteine, and reduced glutathione have been proposed to serve as these ligands. To date, glutathione appears to be a strong candidate as an iron ligand, based on in vitro studies and studies in S. cerevisiae [53]. Iron from the CLIP can be utilized in the cytosol to metalate proteins or form ISCs, but most iron is directed to mitochondria [10,54,55].
For further discussion of cellular iron uptake and distribution, readers are referred to comprehensive reviews on this topic [56,57,58,59,60,61,62].
2. Mitochondrial Iron Trafficking
From the CLIP or from storage in either vacuoles (S. cerevisiae) or ferritin (mammals), iron is readily available to each compartment of the cell, with mitochondria being among the primary targets. In some cases, mitochondria contain more iron than the cytosol [63,64], and this iron is found within mitochondrial proteins as metal ions, ISCs, and different types of heme cofactors. Mitochondrial iron in heme and ISCs is essential for the organelles’ energy production, as it is required for electron-transfer flavoproteins, NADH:ubiquinone oxidoreductase (respiratory complex I of the ETC), succinate:ubiquinone oxidoreductase (respiratory complex II of the ETC), ubiquinol:cytochrome c oxidoreductase (respiratory complex III of the ETC), cytochrome c, cytochrome c oxidase (respiratory complex IV of the ETC), aconitase, lipoic acid synthase, and other proteins [10]. Mitochondria also have several diiron monooxygenases and dioxygenases involved in mitochondrial tRNA modification and cell necrosis regulation [65,66].
As with the cellular import and movement of iron, mitochondrial iron import and transport are highly regulated, meticulous processes designed to limit unwanted reactivity of the metal ions. In mitochondria, iron import and utilization involve several conserved and clinically relevant factors facilitating the efficient targeting of iron for ISC biogenesis, heme biosynthesis, and metalation of other iron-containing mitochondrial proteins (Table 1), as discussed below. For further discussion of non-mitochondrial iron metabolism, readers are referred to reviews on that topic [60,67,68,69].
Table 1.
Conservation of proteins involved in maintaining mitochondrial iron homeostasis. (SA = sideroblastic anemia; MMDS = multiple mitochondrial dysfunctions syndrome).
| Pathway | S. cerevisiae | Mammalian | Function | Pathology |
|---|---|---|---|---|
| Mitochondrial Fe Import | Por1/Por2 | VDAC | Mitochondrial Fe import? | - |
| - | DMT1 | Mitochondrial Fe import | Hypochromic microcytic anemia [70,71,72] | |
| - | PCBP2 | Fe transporter | - | |
| Mrs3/Mrs4 | MFRN1/ MFRN2 |
IMM Fe importer | - | |
| Rim2 | - | IMM low-affinity Fe importer | - | |
| Mdl1 (peptide transporter) | ABCB10 | Stabilization of MFRN1/IMM biliverdin transporter in mammals? | - | |
| - | MCU | IMM Ca (Fe?) import | - | |
| - | SFXN1-5 | Similar and differing functions in serine transport and Fe transport across IMM | Mitochondriopathy; macrocytic anemia [73] |
|
| Mitochondrial Iron Storage | - | FTMT | Mitochondrial Fe storage | - |
| ISC Biogenesis and Maturation of ISC Proteins | Nfs1 | NFS1 | Cysteine desulfurase/sulfur donation | Combined oxidative phosphorylation deficiency [74,75] |
| Isd11 | ISD11 | Nfs1 stabilization/regulation | Combined oxidative phosphorylation deficiency [76] | |
| Acp1 | ACP1 | Nfs1 stabilization/regulation | - | |
| Yfh1 | FXN | Iron donation?/ISC biogenesis regulator | Friedreich’s ataxia [77,78,79,80,81,82,83] | |
| Isu1/Isu2 | ISCU | Core ISC biogenesis scaffold | Hereditary myopathy with lactic acidosis [84,85,86,87] |
|
| Yah1 | FDX2 | Electrons for ISC synthesis | Episodic mitochondrial myopathy [88,89] | |
| Arh1 | FDXR | Electrons for ISC synthesis | Auditory neuropathy; optic atrophy [90] |
|
| Ssq1 | HSPA9 | ISC transfer | SA [91,92] | |
| Jac1 | HSC20 | ISC transfer | - | |
| Mge1 | GRPEL1 | Nucleotide release factor for Ssq1/HSPA9 | - | |
| Grx5 | GLRX5 | ISC transfer | SA [93,94,95] | |
| Isa1 | ISCA1 | 4Fe-4S synthesis | MMDS [96,97] | |
| Isa2 | ISCA2 | 4Fe-4S synthesis | MMDS [98,99,100,101] | |
| Iba57 | IBA57 | 4Fe-4S synthesis | MMDS [102,103,104,105,106,107] | |
| Nfu1 | NFU1 | Maturation of ISC proteins | MMDS [108,109] | |
| - | NUBPL | Maturation of ISC proteins | Mitochondrial complex I deficiency [110,111,112,113] | |
| Bol3 | BOLA3 | Maturation of ISC proteins | MMDS 2 [108,114,115] | |
| Bol1 | BOLA1 | Maturation of ISC proteins | - | |
| Atm1 | ABCB7 | Fe or ISC intermediate export | SA with ataxia [116,117,118] | |
| - | ABCB8 | Fe or ISC intermediate export? | - | |
| Heme Biosynthesis and Modification | Hem15 | FECH | Final step in formation of heme b | Erythropoietic protoporphyria [119,120,121,122,123,124,125] |
| Cox10 | COX10 | Formation of heme o intermediate from heme b | Mitochondrial complex IV deficiency [126,127,128] | |
| Cox15 | COX15 | Formation of heme a from heme o intermediate | Mitochondrial complex IV deficiency [129,130,131,132] | |
| Cyc3/Cyt2 | HCCS | Heme installation in cytochrome c and cytochrome c1 | - | |
| Mitochondrial Fe Export | Mmt1/Mmt2 | - | Mitochondrial Fe export | - |
| Mtm1 | Slc25a39 | IMM Fe export | - | |
| - | FLVCR1b | Mitochondrial heme export? | - | |
| Dap1 | PGRMC1 | Cytosolic acceptor of mitochondrial heme? | - | |
| - | HBP-1 | Cytosolic acceptor of mitochondrial heme? | - |
2.1. Iron Delivery to Mitochondria
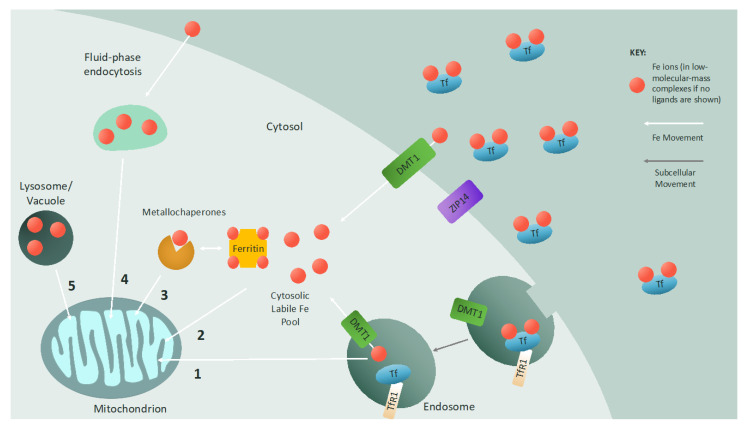
Mitochondrial function is entirely dependent on proper iron homeostasis, and in turn, mitochondria are imperative for proper cellular iron homeostasis. Even with the importance of this mitochondria–iron relationship and the large body of research on this topic, the delivery of iron to mitochondria remains only partially understood. In mammalian cells, there is evidence for several paths of mitochondrial iron import, including endosome–mitochondria “kiss and run”, fluid-phase endocytosis, interorganellar contact sites with the lysosome, transport from the CLIP, and metallochaperone transport (Figure 1).
Figure 1.
Iron delivery to the mitochondrion: Iron is imported into cells by either endocytosis (transferrin-bound iron) or plasma membrane channels (non-transferrin-bound iron). The metal transporter ZIP14 has been shown to aid in the cellular uptake of both transferrin-bound and non-transferrin-bound iron. When iron-loaded transferrin binds to the transferrin receptor on the cell surface, the protein–receptor complex is endocytosed, and iron is released into the endosome and reduced. This iron can be exported via the endosomal divalent metal transporter (DMT1) to the cytosolic labile iron pool, which consists of iron ions in low-molecular-mass complexes or stored in ferritin. Alternatively, if the endosome contacts the mitochondrion, iron is transferred to the mitochondrion via a “kiss and run” mechanism (1). Non-transferrin-bound iron imported by DMT1 on the cell membrane directly enters the cytosolic labile iron pool as iron chelated by low-molecular-mass molecules or ferritin and can then be imported into mitochondria (2). Metallochaperones such as glutaredoxin can also deliver iron to mitochondria (3). Fluid-phase endocytosis is an additional mechanism to deliver non-transferrin-bound iron to mitochondria (4). In some cases, interactions between mitochondria and lysosomes or vacuoles mediate iron transfer between organelles (5), and there may be a synergistic effect between lysosome/vacuole homeostasis and mitochondrial iron homeostasis. (Tf = transferrin; TfR1 = transferrin receptor 1).
One pathway for the delivery of iron to mitochondria that has been studied extensively is the endosome–mitochondria “kiss and run” interaction. Primarily found in developing erythrocytes, but also demonstrated in epithelial cells, this method utilizes a direct, transient, interorganellar interaction between iron-loaded Tf-containing endosomes and mitochondria. The direct and transient nature of this interaction provides mitochondria with the excessive amounts of iron required for hemoglobin and heme synthesis during erythropoiesis [133,134,135]. This direct transfer of iron from one organelle to another bypasses the cytosolic diffusion of iron, preventing the production of reactive oxygen species via Fenton chemistry.
Another method of iron transfer to mitochondria that bypasses the cytosol and the CLIP is fluid-phase endocytosis. This pathway, proposed to occur in cardiac cells, occludes solvents from iron to directly deliver non-Tf-bound iron to mitochondria. The limited effect of chelating cytosolic iron on mitochondrial iron uptake supports this fluid-phase endocytosis model [136,137,138].
The lysosome (and lysosome-like vacuole in yeast) has recently been implicated in mitochondrial iron import and homeostasis. In erythrocytes, it appears that iron is directly conveyed to mitochondria at lysosome–mitochondria membrane contact sites to promote heme biosynthesis during erythropoiesis [139]. In yeast and mammalian cell cultures, disruptions to vacuolar and lysosomal homeostasis via an increase in alkalinity impair mitochondrial iron uptake, solidifying the roles of the lysosome and the vacuole in mitochondrial iron import and homeostasis [140,141,142,143].
Mitochondria also obtain iron from the CLIP. Low-molecular-mass iron complexes such as Fe(ATP)2, iron–citrate, iron–glutathione, and iron chelated by the mammalian siderophore 2,5-dihydroxybenzoic acid [144,145,146] may be imported into mitochondria, although the impact of glutathione and 2,5-dihydroxybenzoic acid on mitochondrial iron import has been contested [75]. The process of transferring iron from the CLIP to mitochondria is dependent on the mitochondrial membrane potential [147,148].
Iron trafficking is proposed to involve the coordination of iron to chaperone proteins. This mode of transportation is not unprecedented, since metallochaperones for copper (CCS and Atox1) have long been identified [149], as have several iron-specific metallochaperones. Two classes of chaperones—poly(rC)-binding proteins (specifically, PCBP1 and PCBP2) and monothiol glutaredoxins—which have been extensively studied for their roles outside of iron metabolism, have recently been the focus of iron trafficking research. PCBP1 and PCBP2 were initially identified as RNA-binding proteins required for splicing, transcript stabilization, and translational regulation. More recently, they have been shown to act as iron chaperones to deliver iron to ferritin, and for metalation of cytosolic proteins [150,151]. Glutaredoxins are glutathione (GSH)-dependent redox enzymes necessary for DNA synthesis, protein folding, signal transduction, and reactive oxygen species defense. In yeast, deletion of glutaredoxin 3 and glutaredoxin 4 results in mitochondrial iron deficiencies and impairments in both ISC and heme biogenesis. Additionally, the interaction between glutaredoxin and bovine lymphocyte antigen-like protein is required for iron delivery to mitochondria [152,153].
2.2. Iron Transport at the Outer Mitochondrial Membrane
Once iron is delivered to mitochondria by one of the aforementioned pathways, it must cross both the outer (OMM) and inner (IMM) mitochondrial membranes. The exact mechanism of iron transport across the OMM remains undetermined, but some factors have been speculated. Voltage-dependent anion channels (VDACs) are widely hypothesized as mitochondrial iron channels throughout eukaryotes; however, their proposed role in mitochondrial iron import relies entirely on their prevalence, involvement in other energy-related metabolite channeling, and role in the transport of other divalent cations [154]. Recent studies show that mitochondrial isoforms of DMT1 facilitate iron influx to mitochondria in several cell types, expanding the role of DMT1 in iron homeostasis beyond enterocyte iron uptake and endosomal iron export [155,156]. The aforementioned iron chaperone PCBP2, which interacts with DMT1 and with ferritin, may transport iron to other cellular compartments, such as the mitochondrion [151].
2.3. Iron Transport at the Inner Mitochondrial Membrane
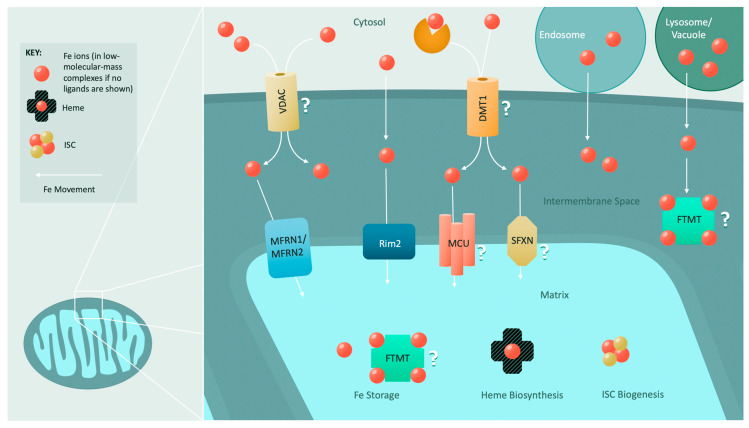
Unlike iron import across the OMM, iron import at the IMM is relatively well studied (Figure 2).
Figure 2.
Mitochondrial iron import and utilization: The mechanism for iron import through the outer mitochondrial membrane is poorly understood. However, it is speculated that ion channels such as VDACs and a recently identified mitochondrial divalent metal transporter (DMT1) facilitate the import of iron. Interorganellar contacts with endosomes, lysosomes, and vacuoles can also convey iron to mitochondria. Transport across the inner mitochondrial membrane is primarily driven by the conserved mitoferrins (MFRN1 and MFRN2). In yeast, a low-affinity iron transporter (Rim2) assists the mitoferrins. Roles in inner mitochondrial membrane iron import have also been hypothesized for the mitochondrial calcium uniporter (MCU) and several members of the sideroflexin (SFXN) family. Once iron is imported into the mitochondrion, it is utilized for heme biosynthesis or ISC biogenesis, or it is stored in mitochondrial ferritin (FTMT) or within low-molecular-mass complexes.
Iron transport across the IMM into the matrix is dependent on proper mitochondrial membrane potential [147]. Initial discoveries of the mechanism of iron transport across the IMM were completed in yeast, where the mitochondrial solute carrier proteins—mitoferrins Mrs3 and Mrs4—are directly involved in mitochondrial IMM and matrix iron supply [157,158]. Mrs3 and Mrs4 are highly conserved from fungi to mammals and are members of a family of proteins required for IMM metabolite transport [159,160,161,162,163,164,165,166,167,168]. Mitochondrial iron levels and heme and ISC biogenesis are directly dependent on Mrs3 and Mrs4 expression [157,158,169,170]. Furthermore, genetic expression of Mrs4 is dependent on iron concentration and ISC synthesis [171,172]. However, the mechanism by which these two proteins transport iron across the IMM is presently unknown. Interestingly, it has been posited that Mrs3 and Mrs4 may also transport Cu2+ into the mitochondrial matrix [173,174].
Mrs3 and Mrs4 are nonessential proteins, with their deletion only being lethal in low-iron conditions, suggesting that compensatory iron uptake mechanisms must exist for the IMM [157,175]. Genetic screens in yeast mutants with defective mitochondrial iron homeostasis identified the known pyrimidine transporter Rim2 as a low-affinity mitochondrial iron transporter [175,176,177]. Overexpression of Rim2 recovers heme and ISC biosynthesis deficiencies and growth defects exhibited in mrs3∆ mrs4∆ double mutants [175,177,178,179]. Whether Rim2 follows the trend of other mitochondrial carrier proteins by co-transporting substrates remains to be determined [175,177,180,181]. Deletion of RIM2 minimally affects mitochondrial iron homeostasis, but deletion of RIM2 in parallel with MRS3 and MRS4 deletion exacerbates ISC maturation defects [176,177]. Additional genetic screens were performed to identify other IMM iron transporters; however, no candidates suppressed the phenotypes of Mrs3-/Mrs4-deficient yeast like Rim2 does; thus, it was postulated that low levels of iron nonspecifically enter mitochondria, allowing triple-deletion mutants to survive [182].
In mammalian cells, the proteins mitoferrin 1 (MFRN1) and mitoferrin 2 (MFRN2), which are functionally complementary to and homologous to Mrs3 and Mrs4 (~35% identity with Mrs4) [52,160], are responsible for iron transport across the IMM [164]. MFRN1 is the primary IMM iron transporter in differentiating erythrocytes, partly due to its extended half-life [164]. Clinically, the loss of MFRN1 causes erythropoietic protoporphyria due to defects in heme biosynthesis [160,183,184]. While the exact mechanism it employs to transport iron across the IMM remains elusive, MFRN1 is stabilized by an interaction with the IMM ATP-binding cassette (ABC) transporter ABCB10, which is likewise highly expressed in erythroid cells. This interaction also enhances mitochondrial iron import [185]. These two proteins are associated with the final heme b biosynthetic enzyme ferrochelatase (FECH), likely bolstering heme synthesis during erythropoiesis by stabilizing MFRN1 and funneling iron directly to FECH for integration into protoporphyrin IX to produce heme b [186]. Interestingly, in hepatocytes, ABCB10 has a very different role as a mitochondrial biliverdin exporter to promote the regeneration of the antioxidant bilirubin [187].
In contrast to MFRN1, MFRN2 is expressed in all vertebrate tissues (with the highest expression in the heart, skeletal muscle, liver, and kidney) and is the primary IMM iron importer of non-erythroid cells [52,160]. MFRN2 levels are increased in murine models for Friedreich’s ataxia—the iron dysregulation disease associated with mutations in the mitochondrial protein frataxin (FXN)—and in patients with muscle-specific mitochondrial iron accumulation in ISC-deficiency-related human diseases [188,189,190,191,192,193].
In conjunction with the mitoferrins, the mitochondrial calcium uniporter (MCU) may play a role in IMM iron transport as well. Several studies have provided evidence that the inhibition of MCU-mediated calcium entry prevents mitochondrial iron uptake [32,148,194].
Another group of mitochondrial proteins required for proper mitochondrial iron homeostasis has recently been uncovered: the sideroflexins (SFXN). This family of five IMM proteins is hypothesized to act either as channels or as carrier proteins [195,196]. Reduced sideroflexin expression (of SFXN4) or loss of sideroflexin function (of SFXN1) results in impaired erythropoiesis [73,196], but the precise roles of the sideroflexins in erythropoiesis remain to be determined. While SFXN1 was initially identified as a serine transporter, further analyses have revealed that it also participates in mitochondrial respiratory complex III biogenesis, activity, and assembly [197,198]. SFXN4 deficiency impairs respiration in zebrafish, and its role has been predicted to be related to mitochondrial respiratory complex I assembly, with recent studies suggesting that it is required for ISC biogenesis [73,199].
3. Sites of Mitochondrial Iron Utilization
Upon import into the mitochondrion, there are three primary destinations for iron: (1) iron storage, (2) ISC biogenesis and incorporation into ISC proteins, and (3) heme biosynthesis and use to form hemoproteins.
3.1. Mitochondrial Iron Storage
Iron can be stored in mitochondrial ferritin (FTMT)—a ferritin variant with high sequence homology to the heavy chain ferritin subunit H-ferritin [200]. In humans, FTMT is primarily expressed in the testes, and in sideroblasts of patients with sideroblastic anemia, but immunohistochemical experiments have identified FTMT in the heart, spinal cord, kidney, pancreas, and smooth muscle [200,201,202,203]. Similar to H-ferritin, FTMT also has ferroxidase activity, but this occurs much more slowly than in its cytosolic paralog [204]. The expression of FTMT significantly impacts cellular iron homeostasis; increased FTMT expression correlates with increased iron localization to mitochondria, causing mitochondrial iron accumulation [64,205]. Iron sequestration by FTMT appears to be protective against oxidative stress, since it protects mitochondria from hydrogen peroxide, antimycin A, and glucose-free conditions [206]. Further experiments are needed to determine the localization, mechanism of action, regulation, and role of FTMT in iron homeostasis.
In addition to storage in FTMT, iron can be sequestered in the mitochondrial matrix within low-molecular-mass complexes to form the mitochondrial labile iron pool [207]. GSH might serve as a ligand for mitochondrial iron since it is highly concentrated in mitochondria, is capable of chelating cytosolic ferrous iron, and has been proposed to coordinate 2Fe-2S clusters within mitochondria [208,209,210,211,212]. Citrate—another highly concentrated metabolite in the mitochondrial matrix—has also been hypothesized to function in mitochondrial iron coordination and sequestration [209,213].
3.2. Mitochondrial Iron–Sulfur Cluster Biogenesis and Transport
In eukaryotes, mitochondria are essential for the synthesis of all cellular ISC-containing proteins and are the site for the biogenesis of ISCs needed for mitochondrial proteins. Composed of iron and sulfide ions, ISCs are commonly found with rhomboid (2Fe-2S) or cubane (4Fe-4S) (and more rarely cuboidal, 3Fe-4S) geometries within ISC-containing proteins, where the iron atoms are ligated to cysteine thiolates or nitrogen atoms from residues such as histidine. The formation of this cofactor is critical for mitochondrial and cellular homeostasis. ISCs are involved in electron transport (e.g., ISC-containing subunits of the mitochondrial respiratory complexes I, II, and III), substrate binding and enzymatic catalysis (e.g., aconitase), nucleic acid processing and repair (e.g., ISC-containing enzymes required for DNA replication and mRNA translation), and metabolite sensing (e.g., cytosolic regulation of iron metabolism) [62,214,215,216,217,218,219,220].
The formation of ISCs in eukaryotes occurs via two pathways: one responsible for forming mitochondrial ISCs and the other responsible for forming ISCs in the cytosol. Both pathways are necessary for overall cellular health. Mitochondrial ISC biogenesis is discussed below, while the cytosolic ISC assembly (CIA) biogenesis pathway is discussed elsewhere [221,222,223].
Mitochondrial ISC biogenesis entails synthesis of the ISC on a scaffold composed of assembly proteins followed by transfer of the ISC to target apoproteins [224]. The ISC assembly factor cysteine desulfurase (NFS1) abstracts sulfur from free cysteine in a pyridoxal phosphate-dependent process that is activated by the binding of the protein ISD11 [76,225,226,227]. This sulfur, held on a catalytic cysteine as a persulfide, is transferred to the ISC scaffold protein ISCU, which directly interacts with NFS1, ISD11, and the mitochondrial acyl carrier protein (ACP1) to form the ISC biogenesis scaffold [228,229]. Electrons for the persulfide reduction, permitting formation of the ISC, are supplied by ferredoxin (which is, in turn, reduced by ferredoxin reductase) [230,231,232], while iron is supplied via an unknown mechanism [221,233]. The molecular mechanism of ISC formation remains debated, but recent work suggests the mechanism may require iron to bind to the scaffold before the sulfur is supplied [234,235].
The most probable sources of the necessary iron are the mitochondrial labile iron pool and frataxin, which can bind iron through acidic regions within the protein. Frataxin interacts with the ISCU–NSF1–ISD11 complex, and has been hypothesized to mediate iron’s entry into the ISC biogenesis scaffold and/or act as a modulator for NFS1 that might facilitate persulfide transfer to ISCU [208,221,236,237,238,239,240,241,242,243]. Decreased expression of frataxin impairs ISC biogenesis and iron metabolism, as seen in Friedreich’s ataxia [77,244].
Studies in yeast and bacteria have suggested additional roles for frataxin, including as an iron chaperone, an iron sensor and allosteric regulator of ISC biogenesis, or a metabolic switch between ISC and heme synthesis. As an iron sensor for ISC biogenesis, frataxin acts as either a negative or positive regulator of ISC biogenesis, depending on the organism. Iron binding to frataxin in bacteria decreases the rate of ISC formation, while eukaryotic frataxin enhances ISC formation via several mechanisms [238,245,246,247,248,249,250]. In eukaryotes, frataxin also interacts with ferrochelatase and regulates heme biosynthesis [251,252]. Evidence that frataxin may be acting as a metabolic switch between the formation of ISCs and heme cofactors includes its role in modulating both heme synthesis and ISC biogenesis, its ability to bind to ferrochelatase and the yeast homolog of ISCU with significantly different affinities, and its regulation by levels of protoporphyrin IX—the precursor to heme b [56].
Following the coordinated assembly of the ISC, the cofactor is transferred from the ISC biogenesis scaffold to target apoproteins via a mechanism that entails a chaperone–co-chaperone system. In higher eukaryotes, a member of the mitochondrial HSP70 family (HSPA9), its J-type co-chaperone HSC20, and the glutaredoxin GLRX5 mediate the transfer of ISCs to their targets. As an ATPase, HSPA9 utilizes the energy from ATP hydrolysis to induce conformational changes in the ISC-loaded ISCU, allowing ISC release from ISCU [214,253,254]. The ISC is transferred to GLRX5 which, in turn, transfers it to a recipient apoprotein, though in some cases apoproteins may receive ISCs without the intervention of GLRX5 [8,255]. Nucleotide exchange at the active site of HSPA9 is facilitated by GRPEL1 to permit future catalytic cycles [256].
How the HSPA9–HSC20 system properly determines the targets for ISC delivery remains to be determined. In some cases, a conserved leucine–tyrosine–arginine (LYR) motif in the recipient apoprotein or an accessory protein is recognized by HSC20 prior to ISC loading. This appears to be the case for many of the ISC-containing electron transport chain components [214,255,257,258]. The role of HSAP9 in ISC transport is still debated, but HSC20 has been shown to directly interact with ISCU and FXN. Depletion of this protein induces severe ISC deficits in both mitochondria and the cytosol [254,259].
In addition to their use in the maturation of 2Fe-2S cluster-containing proteins, 2Fe-2S clusters can be used to produce 4Fe-4S clusters. A dedicated complex composed of ISCA1, ISCA2, and IBA57 is required to fuse two 2Fe-2S clusters delivered by GLRX5 to form a 4Fe-4S cluster in a process that requires ferredoxin and its reductase [260,261,262,263,264]. The proteins BOLA3, NFU1, and NUBPL have all been identified as ISC targeting factors that assist in loading 4Fe-4S clusters into particular mitochondrial proteins [102,115,256,257,263,265,266,267]. GLRX5 physically interacts with BOLA3 and BOLA1, and the yeast homologs of both these BOLA family proteins have been shown to play a role in the maturation of 4Fe-4S cluster proteins [268,269].
In addition to producing ISCs for mitochondrial proteins, this mitochondrial ISC biogenesis pathway directly enables its cytosolic counterpart—the CIA—which is required to produce cytosolic and nuclear ISCs. The mitochondrial ISC pathway does this by donating a sulfur-containing (and perhaps iron-containing) intermediate from the mitochondrial matrix to the cytosol [270]. Although the exact mechanism for the transport of this intermediate is not fully understood, several studies in yeast have provided insight into the factors involved. The ABC transporter Atm1 is postulated as the IMM transporter of the sulfur-containing intermediate, and the intermembrane space (IMS) sulfhydryl oxidase Erv1 facilitates Atm1-mediated transport [271,272]. In Atm1-deficient yeast, cytosolic ISC biogenesis is disrupted, iron accumulates in mitochondria, and cellular iron uptake is enhanced [270,273]. While the involvement of the human ortholog of Atm1 (ABCB7) in transporting the intermediate to the cytosol remains to be clarified, ABCB7 has been implicated in several iron-related disorders, such as X-linked sideroblastic anemia and ataxia [272,274,275]. ABCB7 appears to be assisted in transporting the ISC intermediate by another ABC transporter (ABCB8), though the exact nature of its involvement is presently unknown. Deletion of ABCB8 in murine hearts severely impairs cardiac function due to significant mitochondrial damage, mitochondrial iron accumulation, and cytosolic ISC and heme deficiencies, which is a phenotype similar to that caused by the absence of ABCB7 [16,274,276,277]. These ABC transporters share similarity with the yeast mitochondrial peptide exporter Mdl1. Overexpression of Mdl1 partially rescues the phenotype of Atm1 deletion but, overall, Mdl1 is not implicated in iron homeostasis [278,279,280]. These data suggest that ABCB8, alongside ABCB7, may be mediating the transfer of a sulfur-containing intermediate for cytosolic ISC biogenesis.
3.3. Heme Biosynthesis and Transport
Heme b, which is an iron ion ligated by the protoporphyrin IX tetrapyrrole, and its biosynthetic derivatives heme c and heme a, are the other vital iron-containing cofactors produced by mitochondria and necessitating mitochondrial iron import. Heme is required for a plethora of processes, including oxygen transport and storage (e.g., hemoglobin and myoglobin), electron transfer (e.g., cytochrome c, respiratory complex III, and respiratory complex IV), signal transduction (e.g., nitric oxide synthase), ligand binding (e.g., horseradish peroxidase), transcriptional regulation (e.g., Rev-erbβ), and xenobiotic detoxification (e.g., cytochrome P450) [281,282].
The biosynthesis of heme b differs greatly from ISC biogenesis. In ISC biogenesis, iron is present throughout much of the process, whereas in heme biosynthesis, iron is only utilized in the final step, wherein it is incorporated into protoporphyrin IX by ferrochelatase. The process of heme biosynthesis has been studied extensively, and its details are beyond the scope of the present review; the reader is directed to reviews focused on this topic [7,283,284,285,286]. Briefly, heme biosynthesis begins with the condensation of succinyl–CoA and glycine by aminolevulinic acid (ALA) synthase to produce ALA in the mitochondrial matrix. ALA is exported to the cytosol and sequentially modified to create a cytosolic porphyrin. This porphyrin (coproporphyrinogen III) is transported back into the mitochondrion, where it is converted to protoporphyrin IX. Protoporphyrin IX and ferrous iron are combined by ferrochelatase to produce heme b in the mitochondrial matrix [7]. Iron is proposed to be delivered directly to ferrochelatase via protein–protein interactions with the mitoferrins [94,95,97,106,107,123]. Several enzymes in the heme biosynthetic pathway have recently been shown to interact with one another and with ABCB7, ABCB10, the protoporphyrinogen transporter TMEM14c, and the transferrin receptor to form a complex termed the heme metabolon [287].
Once synthesized, heme b is used to form hemoproteins required for various functions throughout mitochondria and other cellular compartments. The mechanism for the trafficking of heme to these other locales remains unknown and is the subject of ongoing research. Recent studies using ratiometric heme sensors to study heme distribution kinetics between cellular compartments in yeast revealed that the mitochondrial GTPases Gem1, Mgm1, and Dnm1 modulate heme transport to the nucleus by regulating mitochondrial architecture and endoplasmic reticulum–mitochondria contact sites [288].
Heme b destined for use within mitochondria is either added non-covalently to form hemoproteins or covalently modified to produce heme c or heme a for use in the hemoproteins of the electron transport chain. Heme b is utilized by several mitochondria-localized proteins, including the matrix protein neuroglobin (flavohemoglobin Yhb1 in yeast), respiratory complex II, respiratory complex III, and yeast-specific proteins (respiratory complex IV assembly factor Mss51, cytochrome c peroxidase Ccp1, and L-lactate cytochrome c oxidoreductase Cyb2) (reviewed in [7]). To date, the mechanism of heme b translocation to these proteins is unknown.
To form the covalently bound c-type heme found in cytochrome c (human CYCS or yeast paralogs Cyc1/Cyc7) and the respiratory complex III subunit cytochrome c1 (human CYC1 or yeast Cyt1), heme b is covalently bound to the hemoprotein via thioether bonds with highly conserved cysteine residues [6,289,290]. The process by which heme b is transported to these heme-c-containing proteins is partially understood. The mammalian holocytochrome c synthase (HCCS) and the yeast cytochrome c heme lyases (Cyc3 and Cyt2) are responsible for directly delivering and covalently attaching heme b to cysteines in cytochrome c and cytochrome c1. However, the factors that mediate heme b transfer to HCCS, Cyc3, and Cyt2 remain elusive [289,291,292].
In the heme a modification pathway, heme b is extensively modified via the addition of a hydroxyfarnesyl group to one of its vinyl carbons by heme o synthase (COX10) and the conversion of a methyl group to an aldehyde by heme a synthase (COX15). Heme a is exclusively found in the COX1 subunit of respiratory complex IV, and heme chaperones for delivering and installing the cofactor have not been identified. The complex IV assembly factors SURF1 (Shy1 in yeast) and Coa2 have been posited as heme chaperones for this pathway, but each protein appears to only be involved in the hemylation of COX1 rather than trafficking heme to the site of complex assembly [293,294,295,296,297,298,299,300,301,302].
4. Iron Export from Mitochondria
The role of mitochondria in iron homeostasis is not limited to utilization in ISC biogenesis and heme synthesis; the labile iron pool in mitochondria can also act as an iron depot to supply the rest of the cell. This iron is in the form of “free” iron (a term for iron ions with various low-molecular-mass ligands), heme iron, and ISC intermediates.
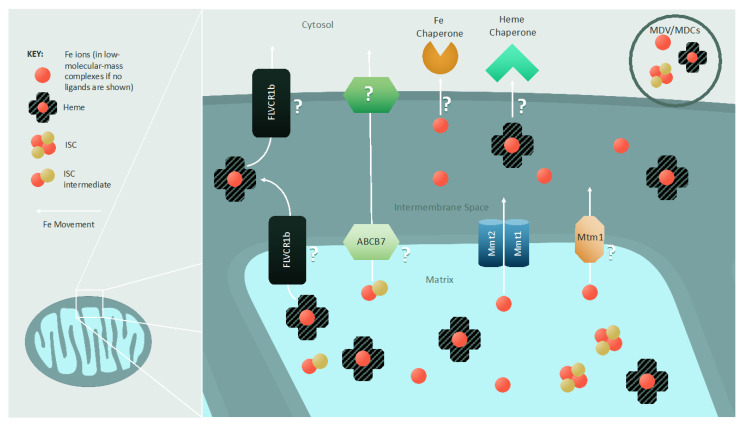
Several proteins have been hypothesized to export “free” iron (Figure 3), with most studies carried out in S. cerevisiae. The mitochondrial metal transporters Mmt1 and Mmt2 conserved in fungi and plants have been identified as exporters of mitochondrial iron [303,304]; their overexpression results in cytosolic iron accumulation, while their deletion decreases cytosolic iron load [304]. Another protein postulated to be involved in mitochondrial iron export in yeast is Mtm1. Deletion of Mtm1 in S. cerevisiae results in mitochondrial iron accumulation and enhanced cellular iron uptake, while also inducing the misincorporation of iron into the mitochondrial manganese-containing superoxide dismutase [305,306,307]. The vertebrate functional ortholog of Mtm1 (Slc25a39) is required for iron’s integration into protoporphyrin IX to produce heme b in murine erythroid cells; its deletion induces anemia in zebrafish, cementing its role in mitochondrial iron homeostasis, while suggesting that further studies are needed to completely elucidate the role of Mtm1-related proteins [308]. As discussed earlier, a sulfur- (and possibly iron-) containing intermediate is exported from the mitochondrion to enable cytosolic ISC biogenesis, and its export may involve proteins such as Atm1 and Mdl1 (in yeast) and ABCB7 and ABCB8 (in mammals) [270,271,272,273,274,275].
Figure 3.
Export of mitochondrial iron and iron-containing cofactors: Iron is exported from mitochondria as heme or metal ions in low-molecular-mass complexes. Additionally, a presently unidentified intermediate required for cytosolic ISC biogenesis is also exported from mitochondria. In yeast, three inner mitochondrial membrane iron exporters have been identified: Mmt1, Mmt2, and Mtm1. In the case of heme export, FLVCR1b is postulated to play a role, but it is unclear where FLVCR1b localizes within the mitochondrion or to what extent it facilitates heme export. The ISC intermediate necessary for cytosolic ISC biogenesis is trafficked across the inner mitochondrial membrane by Atm1 in yeast and ABCB7 in mammals. Methods of export across the outer mitochondrial membrane remain unknown. It is hypothesized that various protein channels allow for the flow of these iron species, and that iron and cofactor chaperones directly accept or extract their cargo from the mitochondrion. A non-protein-based mechanism for iron, heme, and ISC intermediate export is also possible via mitochondria-derived vesicles (MDVs) and compartments (MDCs).
Non-protein pathways—specifically, mitochondria-derived compartments (MDCs) and mitochondria-derived vesicles (MDVs)—are also hypothesized to participate in the efflux of “free” iron, along with ISCs and heme. MDCs and MDVs are single- and double-membrane-bound vesicles with an approximate diameter of 70–100 nm that can interact with other subcellular compartments, such as the ER, lysosome, and peroxisome [309,310,311,312,313,314]. MDVs have been shown to contain various cargo loads, including metabolites and proteins [312,315], and proteomic analysis of purified MDVs has uncovered high levels of mitochondrial ISC biogenesis proteins and proteins capable of binding iron [316]. The strategy of mobilizing “free” iron, ISCs, and heme through MDCs and MDVs would be advantageous in terms of minimizing their cytotoxic effects and enhancing their availability.
The mechanism of heme export from mitochondria remains elusive and debated, but several factors have been implicated. To date, only one protein—a mitochondrial isoform of FLVCR protein 1b—has been identified as a potential heme exporter. Erythropoiesis is terminated and heme is accumulated in mitochondria following FLVCR1b depletion, while overexpression of this transporter increases cytosolic heme levels. FLVCR1b lacks a defined heme-binding/transport segment akin to that found in its isozyme FLVCR1a [317,318]. Significantly, FLVCR1a and FLVCR1b appear to be specific to erythroid cells. Moreover, they are not found in lower eukaryotes, suggesting that other, more conserved mechanisms of heme export should exist.
Once heme is trafficked to the mitochondrial outer membrane, a cytosolic chaperone is required to accept heme from the mitochondrion. Progesterone receptor membrane component 1 (PGRMC1) and heme-binding protein 1 (HBP-1) are candidates for this function, but further studies are required to delineate their role in heme extraction from mitochondria.
Some of the iron exported from mitochondria may ultimately be exported from the cell. Mechanisms of cellular iron export are poorly understood; however, ferroportin has been identified as an exporter of non-heme iron, and multidrug resistance protein 5 (MRP-5) and FLVCR1a both export heme [10,319,320,321,322]. In macrophages, heme-responsive gene 1 (HRG-1), which is homologous to a heme plasma membrane transporter in Caenorhabditis elegans, exports heme from the phagolysosome to the cytosol during erythrophagocytosis [323,324].
5. Concluding Remarks
Iron is essential for cellular physiology and life. Since this metal obtained from the environment is redox-active, cellular iron import and transport are highly regulated processes. Much is known about how iron is trafficked extracellularly, as well as cytosolically, and how it is delivered to various organelles, but there remain many gaps in the information known about mitochondrial iron transport and the movement of iron-containing cofactors. One currently elusive topic that requires further elucidation is the coordination of iron’s delivery to mitochondria and transport across the OMM and IMM, as well as how those pathways cooperate to maintain cellular iron homeostasis. Regarding IMM transport, mechanistic studies of both yeast and mammalian mitoferrins will provide insight into how iron import is mediated and regulated at the molecular level.
Even though a breadth of knowledge has been generated regarding the trafficking of iron to the mitochondrial ISC biogenesis machinery and the transport of the sulfur- (and possibly iron-) containing intermediate to the cytosol for ISC biogenesis via the CIA, many outstanding questions about this process remain. For example, a defined role of frataxin has not been delineated, despite extensive analysis of this protein. If frataxin does not directly provide iron to the ISC biogenesis scaffold, then the involvement of the mitochondrial labile iron pool or additional factors would need to be identified. The molecular mechanism for transporting the sulfur-containing intermediate to the cytosol and its precise identity remain elusive. Unraveling the roles of ABCB7 and ABCB8 in mitochondrial iron homeostasis, and whether these two proteins mediate the transfer of this intermediate, could lead to therapies for diseases where mitochondrial iron homeostasis is implicated. Determining the mechanism of ISC transfer from the ISC biogenesis scaffold to apoproteins is another important goal. The LYR motif being commonly found in some, but not all, ISC proteins suggests that the mechanisms of substrate recognition by the HSPA9–HSC20 system and GLRX5 for the delivery of 2Fe-2S clusters to target proteins require further elucidation. Likewise, the molecular mechanisms involved in delivery of 4Fe-4S clusters by specialized ISC trafficking proteins are still under study. The mechanism by which the sideroflexins support iron homeostasis and ISC biogenesis will also be enlightening, and may answer some of the above questions.
Further research is necessary to determine the factors involved in mitochondrial heme trafficking and export. Similarly, limited information is known about how heme b, heme c, and heme a are trafficked to their sites of utilization within mitochondria. Defining these processes and mechanisms will provide answers to a plethora of fundamental biological questions, and contribute to a more expansive understanding of mitochondrial iron homeostasis and mitochondrial iron-related disease pathologies, which have been extensively reviewed [1,9,10,325] Finally, it will be important to place many of these fundamental mechanisms into physiological context by addressing their tissue and/or organ specificity, which may hold clues to understanding the molecular bases of iron management-related disorders in humans.
Acknowledgments
We thank the members of Khalimonchuk lab for critical reading of the manuscript, and Carey Goddard for her expert help with the illustrations.
Author Contributions
Conceptualization, J.V.D., J.L.F. and O.K.; writing—original draft preparation, J.V.D., J.L.F. and O.K.; writing—review and editing, J.V.D., J.L.F. and O.K.; funding acquisition, O.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Institutes of Health grants GM131701-01 (O.K.) and T32-GM107001 (J.V.D.).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the interpretation of data or in the writing of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gao J., Zhou Q., Wu D., Chen L. Mitochondrial iron metabolism and its role in diseases. Clin. Chim. Acta. 2020;513:6–12. doi: 10.1016/j.cca.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Puig S., Askeland E., Thiele D.J. Coordinated remodeling of cellular metabolism during iron deficiency through targeted mRNA degradation. Cell. 2005;120:99–110. doi: 10.1016/j.cell.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Siekevitz P. Powerhouse of the cell. Sci. Am. 1957;197:131–144. doi: 10.1038/scientificamerican0757-131. [DOI] [Google Scholar]
- 4.Van der Bliek A., Sedensky M.M., Morgan P.G. Cell biology of the mitochondrion. Genetics. 2017;207:843–871. doi: 10.1534/genetics.117.300262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng Z., Ristow M. Mitochondria and metabolic homeostasis. Antioxid. Redox Signal. 2013;19:240–242. doi: 10.1089/ars.2013.5255. [DOI] [PubMed] [Google Scholar]
- 6.Kim H.J., Khalimonchuk O., Smith P.M., Winge D.R. Structure, function, and assembly of heme centers in mitochondrial respiratory complexes. Biochim. Biophys. Acta (BBA) Bioenerg. 2012;1823:1604–1616. doi: 10.1016/j.bbamcr.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swenson S., Moore C.M., Marcero J.R., Medlock A.E., Reddi A.R., Khalimonchuk O. From synthesis to utilization: The ins and outs of mitochondrial heme. Cells. 2020;9:579. doi: 10.3390/cells9030579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braymer J.J., Lill R. Iron–sulfur cluster biogenesis and trafficking in mitochondria. J. Biol. Chem. 2017;292:12754–12763. doi: 10.1074/jbc.R117.787101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward D.M., Cloonan S.M. Mitochondrial iron in human health and disease. Annu. Rev. Physiol. 2019;81:453–482. doi: 10.1146/annurev-physiol-020518-114742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paul B.T., Manz D.H., Torti F.M., Torti S.V. Mitochondria and iron: Current questions. Expert Rev. Hematol. 2016;10:65–79. doi: 10.1080/17474086.2016.1268047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker E.M., Walker S.M. Review: Effects of iron overload on the immune system. Ann. Clin. Labr. Sci. 2000;30:354–365. [PubMed] [Google Scholar]
- 12.Rivella S. Iron metabolism under conditions of ineffective erythropoiesis in beta-Thalassemia. Blood. 2019;133:51–58. doi: 10.1182/blood-2018-07-815928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gambale A., Iolascon A., Andolfo I., Russo R. Diagnosis and management of congenital dyserythropoietic anemias. Expert Rev. Hematol. 2016;9:283–296. doi: 10.1586/17474086.2016.1131608. [DOI] [PubMed] [Google Scholar]
- 14.Ducamp S., Fleming M.D. The molecular genetics of sideroblastic anemia. Blood. 2019;133:59–69. doi: 10.1182/blood-2018-08-815951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shenoy N., Vallumsetla N., Rachmilewitz E., Verma A., Ginzburg Y. Impact of iron overload and potential benefit from iron chelation in low-risk myelodysplastic syndrome. Blood. 2014;124:873–881. doi: 10.1182/blood-2014-03-563221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ichikawa Y., Ghanefar M., Bayeva M., Wu R., Khechaduri A., Prasad S.V.N., Mutharasan R.K., Naik T.J., Ardehali H. Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation. J. Clin. Investig. 2014;124:617–630. doi: 10.1172/JCI72931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawicki K.T., Shang M., Wu R., Chang H., Khechaduri A., Sato T., Kamide C., Liu T., Prasad S.V.N., Ardehali H. Increased heme levels in the heart lead to exacerbated ischemic injury. J. Am. Heart Assoc. 2015;4:e002272. doi: 10.1161/JAHA.115.002272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang H.-C., Wu R., Shang M., Sato T., Chen C., Shapiro J.S., Liu T., Thakur A., Sawicki K.T., Prasad S.V.N., et al. Reduction in mitochondrial iron alleviates cardiac damage during injury. EMBO Mol. Med. 2016;8:247–267. doi: 10.15252/emmm.201505748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang M., Chen Z., Wu D., Chen L. Ferritinophagy/ferroptosis: Iron-related newcomers in human diseases. J. Cell. Physiol. 2018;233:9179–9190. doi: 10.1002/jcp.26954. [DOI] [PubMed] [Google Scholar]
- 20.Horowitz M.P., Greenamyre J.T. Mitochondrial iron metabolism and its role in neurodegeneration. J. Alzheimer’s Dis. 2010;20:S551–S568. doi: 10.3233/JAD-2010-100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richardson D.R., Huang M.L., Whitnall M., Becker E.M., Ponka P., Rahmanto Y.S. The ins and outs of mitochondrial iron-loading: The metabolic defect in Friedreich’s ataxia. J. Mol. Med. 2009;88:323–329. doi: 10.1007/s00109-009-0565-x. [DOI] [PubMed] [Google Scholar]
- 22.Bagheri H., Ghasemi F., Barreto G.E., Rafiee R., Sathyapalan T., Sahebkar A. Effects of curcumin on mitochondria in neurodegenerative diseases. BioFactors. 2019;46:5–20. doi: 10.1002/biof.1566. [DOI] [PubMed] [Google Scholar]
- 23.Anzovino A., Lane D.J.R., Huang M.L.-H., Richardson D.R. Fixing frataxin: ‘Ironing out’ the metabolic defect in Friedreich’s ataxia. Br. J. Pharmac. 2014;171:2174–2190. doi: 10.1111/bph.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muñoz Y., Carrasco C.M., Campos J.D., Aguirre P., Núñez M.T. Parkinson’s disease: The mitochondria-iron link. Parkinson’s Dis. 2016;2016:7049108. doi: 10.1155/2016/7049108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kohgo Y., Ikuta K., Ohtake T., Torimoto Y., Kato J. Body iron metabolism and pathophysiology of iron overload. Int. J. Hematol. 2008;88:7–15. doi: 10.1007/s12185-008-0120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simcox J., McClain D.A. Iron and diabetes risk. Cell Metab. 2013;17:329–341. doi: 10.1016/j.cmet.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.González-Domínguez A., Visiedo-García F.M., Domínguez-Riscart J., González-Domínguez R., Mateos R.M., Lechuga-Sancho A.M. Iron metabolism in obesity and metabolic syndrome. Int. J. Mol. Sci. 2020;21:5529. doi: 10.3390/ijms21155529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manz D.H., Blanchette N.L., Paul B.T., Torti F.M., Torti S.V. Iron and cancer: Recent insights. Ann. N. Y. Acad. Sci. 2016;1368:149–161. doi: 10.1111/nyas.13008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bystrom L.M., Rivella S. Cancer cells with irons in the fire. Free Radic. Biol. Med. 2014;79:337–342. doi: 10.1016/j.freeradbiomed.2014.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan L.B., Chandel N.S. Mitochondrial reactive oxygen species and cancer. Cancer Metab. 2014;2:17. doi: 10.1186/2049-3002-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Favaro E., Ramachandran A., McCormick R., Gee H., Blancher C., Crosby M., Devlin C., Blick C., Buffa F., Li J.-L., et al. MicroRNA-210 regulates mitochondrial free radical response to hypoxia and krebs cycle in cancer cells by targeting iron sulfur cluster protein ISCU. PLoS ONE. 2010;5:e10345. doi: 10.1371/journal.pone.0010345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hung H.-I., Schwartz J.M., Maldonado E.N., Lemasters J.J., Nieminen A.-L. Mitoferrin-2-dependent mitochondrial iron uptake sensitizes human head and neck squamous carcinoma cells to photodynamic therapy. J. Biol. Chem. 2013;288:677–686. doi: 10.1074/jbc.M112.422667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hooda J., Cadinu D., Alam M., Shah A., Cao T.M., Sullivan L.A., Brekken R., Zhang L. Enhanced heme function and mitochondrial respiration promote the progression of lung cancer cells. PLoS ONE. 2013;8:e63402. doi: 10.1371/journal.pone.0063402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Puy H., Gouya L., Deybach J.-C. Porphyrias. Lancet. 2010;375:924–937. doi: 10.1016/S0140-6736(09)61925-5. [DOI] [PubMed] [Google Scholar]
- 35.Rouault T.A., Tong W.H. Iron-sulfur cluster biogenesis and human disease. Trends Genet. 2008;24:398–407. doi: 10.1016/j.tig.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu H., Wang F., Ta N., Zhang T., Gao W. The multifaceted regulation of mitochondria in ferroptosis. Life. 2021;11:222. doi: 10.3390/life11030222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chevion M. A site-specific mechanism for free radical induced biological damage: The essential role of redox-active transition metals. Free Radic. Biol. Med. 1988;5:27–37. doi: 10.1016/0891-5849(88)90059-7. [DOI] [PubMed] [Google Scholar]
- 38.Reddi A.R., Hamza I. Heme mobilization in animals: A metallolipid’s journey. Acc. Chem. Res. 2016;49:1104–1110. doi: 10.1021/acs.accounts.5b00553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duffy S.P., Shing J., Saraon P., Berger L.C., Eiden M.V., Wilde A., Tailor C.S. The fowler syndrome-associated protein FLVCR2 is an importer of heme. Mol. Cell. Biol. 2010;30:5318–5324. doi: 10.1128/MCB.00690-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hentze M.W., Muckenthaler M., Andrews N. Balancing acts: Molecular control of mammalian iron metabolism. Cell. 2004;117:285–297. doi: 10.1016/S0092-8674(04)00343-5. [DOI] [PubMed] [Google Scholar]
- 41.Kawabata H. Transferrin and transferrin receptors update. Free Radic. Biol. Med. 2019;133:46–54. doi: 10.1016/j.freeradbiomed.2018.06.037. [DOI] [PubMed] [Google Scholar]
- 42.Lawen A., Lane D.J. Mammalian iron homeostasis in health and disease: Uptake, storage, transport, and molecular mechanisms of action. Antioxid. Redox Signal. 2013;18:2473–2507. doi: 10.1089/ars.2011.4271. [DOI] [PubMed] [Google Scholar]
- 43.Richardson D.R., Ponka P. The molecular mechanisms of the metabolism and transport of iron in normal and neoplastic cells. Biochim. Biophys. Acta (BBA) Rev. Biomembr. 1997;1331:1–40. doi: 10.1016/S0304-4157(96)00014-7. [DOI] [PubMed] [Google Scholar]
- 44.Liuzzi J.P., Aydemir F., Nam H., Knutson M.D., Cousins R.J. Zip14 (Slc39a14) mediates non-transferrin-bound iron uptake into cells. Proc. Natl. Acad. Sci. USA. 2006;103:13612–13617. doi: 10.1073/pnas.0606424103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao N., Gao J., Enns C.A., Knutson M.D. ZRT/IRT-like protein 14 (ZIP14) promotes the cellular assimilation of iron from transferrin. J. Biol. Chem. 2010;285:32141–32150. doi: 10.1074/jbc.m110.143248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gunshin H., Mackenzie B., Berger U.V., Gunshin Y., Romero M.F., Boron W.F., Nussberger S., Gollan J.L., Hediger M.A. Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature. 1997;388:482–488. doi: 10.1038/41343. [DOI] [PubMed] [Google Scholar]
- 47.Kwok E.Y., Severance S., Kosman D.J. Evidence for iron channeling in the Fet3p−Ftr1p high-affinity iron uptake complex in the yeast plasma membrane. Biochemistry. 2006;45:6317–6327. doi: 10.1021/bi052173c. [DOI] [PubMed] [Google Scholar]
- 48.Singh A., Severance S., Kaur N., Wiltsie W., Kosman D.J. Assembly, activation, and trafficking of the Fet3p-Ftr1p high affinity iron permease complex in Saccharomyces cerevisiae. J. Biol. Chem. 2006;281:13355–13364. doi: 10.1074/jbc.M512042200. [DOI] [PubMed] [Google Scholar]
- 49.Chen X.-Z., Peng J.-B., Cohen A., Nelson H., Nelson N., Hediger M.A. Yeast SMF1 mediates H+-coupled iron uptake with concomitant uncoupled cation currents. J. Biol. Chem. 1999;274:35089–35094. doi: 10.1074/jbc.274.49.35089. [DOI] [PubMed] [Google Scholar]
- 50.Dix D., Bridgham J., Broderius M., Wide D. Characterization of the FET4 protein of yeast: Evidence for a direct role in the transport of iron. J. Biol. Chem. 1997;272:11770–11777. doi: 10.1074/jbc.272.18.11770. [DOI] [PubMed] [Google Scholar]
- 51.Moore R.E., Kim Y., Philpott C.C. The mechanism of ferrichrome transport through Arn1p and its metabolism in Saccharomyces cerevisiae. Proc. Natl. Acad. Sci. USA. 2003;100:5664–5669. doi: 10.1073/pnas.1030323100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li F.-Y., Nikali K., Gregan J., Leibiger I., Leibiger B., Schweyen R., Larsson C., Suomalainen-Wartiovaara A. Characterization of a novel human putative mitochondrial transporter homologous to the yeast mitochondrial RNA splicing proteins 3 and 4. FEBS Lett. 2001;494:79–84. doi: 10.1016/S0014-5793(01)02319-5. [DOI] [PubMed] [Google Scholar]
- 53.Philpott C.C., Ryu M.-S. Special delivery: Distributing iron in the cytosol of mammalian cells. Front. Pharmacol. 2014;5:173. doi: 10.3389/fphar.2014.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arosio P., Levi S. Cytosolic and mitochondrial ferritins in the regulation of cellular iron homeostasis and oxidative damage. Biochim. Biophys. Acta (BBA) Gen. Subj. 2010;1800:783–792. doi: 10.1016/j.bbagen.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 55.Ferreira C., Bucchini D., Martin M.-E., Levi S., Arosio P., Grandchamp B., Beaumont C. Early embryonic lethality of H ferritin gene deletion in mice. J. Biol. Chem. 2000;275:3021–3024. doi: 10.1074/jbc.275.5.3021. [DOI] [PubMed] [Google Scholar]
- 56.Lane D.J.R., Merlot A.M., Huang M.H.-L., Bae D.-H., Jansson P.J., Sahni S., Kalinowski D.S., Richardson D.R. Cellular iron uptake, trafficking, and metabolism: Key molecules and mechanisms and their roles in disease. Biochim. Biophys. Acta. 2015;1853:1130–1144. doi: 10.1016/j.bbamcr.2015.01.021. [DOI] [PubMed] [Google Scholar]
- 57.Blaiseau P., Seguin A., Camadro J.-M., Lesuisse E. Iron Uptake and Homeostasis in Microorganisms. Caister Academic Press; Poole, UK: 2011. Iron uptake in yeasts. [Google Scholar]
- 58.Anderson G.J., Vulpe C.D. Mammalian iron transport. Cell. Mol. Life Sci. 2009;66:3241–3261. doi: 10.1007/s00018-009-0051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen C., Paw B.H. Cellular and mitochondrial iron homeostasis in vertebrates. Biochim. Biophys. Acta (BBA) Bioenerg. 2012;1823:1459–1467. doi: 10.1016/j.bbamcr.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Philpott C.C., Ryu M.-S., Frey A., Patel S. Cytosolic iron chaperones: Proteins delivering iron cofactors in the cytosol of mammalian cells. J. Biol. Chem. 2017;292:12764–12771. doi: 10.1074/jbc.R117.791962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vogt A.-C., Arsiwala T., Mohsen M., Vogel M., Manolova V., Bachmann M. On Iron Metabolism and Its Regulation. Int. J. Mol. Sci. 2021;22:4591. doi: 10.3390/ijms22094591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Muckenthaler M., Galy B., Hentze M. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu. Rev. Nutr. 2008;28:197–213. doi: 10.1146/annurev.nutr.28.061807.155521. [DOI] [PubMed] [Google Scholar]
- 63.Rauen U., Springer A., Weisheit D., Petrat F., Korth H.-G., De Groot H., Sustmann R. Assessment of chelatable mitochondrial iron by using mitochondrion-selective fluorescent iron indicators with different iron-binding affinities. ChemBioChem. 2007;8:341–352. doi: 10.1002/cbic.200600311. [DOI] [PubMed] [Google Scholar]
- 64.Nie G., Sheftel A.D., Kim S.F., Ponka P., Brown P., Levis M., Shurtleff S., Campana D., Downing J., Small D. Overexpression of mitochondrial ferritin causes cytosolic iron depletion and changes cellular iron homeostasis. Blood. 2005;105:2161–2167. doi: 10.1182/blood-2004-07-2722. [DOI] [PubMed] [Google Scholar]
- 65.Haag S., Sloan K.E., Ranjan N., Warda A.S., Kretschmer J., Blessing C., Hübner B., Seikowski J., Dennerlein S., Rehling P., et al. NSUN3 and ABH1 modify the wobble position of mt-tRNA Met to expand codon recognition in mitochondrial translation. EMBO J. 2016;35:2104–2119. doi: 10.15252/embj.201694885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fu D., Jordan J.J., Samson L.D. Human ALKBH7 is required for alkylation and oxidation-induced programmed necrosis. Genes Dev. 2013;27:1089–1100. doi: 10.1101/gad.215533.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roemhild K., von Maltzahn F., Weiskirchen R., Knüchel R., von Stillfried S., Lammers T. Iron metabolism: Pathophysiology and pharmacology. Trends Pharmacol. Sci. 2021;42:650–656. doi: 10.1016/j.tips.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bogdan A.R., Miyazawa M., Hashimoto K., Tsuji Y. Regulators of iron homeostasis: New players in metabolism, cell death, and disease. Trends Biochem. Sci. 2015;41:274–286. doi: 10.1016/j.tibs.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muckenthaler M., Rivella S., Hentze M.W., Galy B. A Red Carpet for Iron Metabolism. Cell. 2017;168:344–361. doi: 10.1016/j.cell.2016.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mims M.P., Guan Y., Pospisilova D., Horvathova M., Indrak K., Ponka P., Divoky V., Prchal J.T. Identification of a human mutation of DMT1 in a patient with microcytic anemia and iron overload. Blood. 2005;105:1337–1342. doi: 10.1182/blood-2004-07-2966. [DOI] [PubMed] [Google Scholar]
- 71.Iolascon A., D’Apolito M., Servedio V., Cimmino F., Piga A., Camaschella C. Microcytic anemia and hepatic iron overload in a child with compound heterozygous mutations in DMT1 (SCL11A2) Blood. 2006;107:349–354. doi: 10.1182/blood-2005-06-2477. [DOI] [PubMed] [Google Scholar]
- 72.Beaumont C., Delaunay J., Hetet G., Grandchamp B., De Montalembert M., Tchernia G. Two new human DMT1 gene mutations in a patient with microcytic anemia, low ferritinemia, and liver iron overload. Blood. 2006;107:4168–4170. doi: 10.1182/blood-2005-10-4269. [DOI] [PubMed] [Google Scholar]
- 73.Hildick-Smith G.J., Cooney J.D., Garone C., Kremer L.S., Haack T.B., Thon J.N., Miyata N., Lieber D.S., Calvo S.E., Akman H.O., et al. Macrocytic anemia and mitochondriopathy resulting from a defect in sideroflexin 4. Am. J. Hum. Genet. 2013;93:906–914. doi: 10.1016/j.ajhg.2013.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Farhan S.M.K., Wang J., Robinson J.F., Lahiry P., Siu V.M., Prasad C., Kronick J.B., Ramsay D.A., Rupar C.A., Hegele R.A. Exome sequencing identifies NFS1 deficiency in a novel Fe-S cluster disease, infantile mitochondrial complex II/III deficiency. Mol. Genet. Genom. Med. 2014;2:73–80. doi: 10.1002/mgg3.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hershkovitz T., Kurolap A., Tal G., Paperna T., Mory A., Staples J., Brigatti K.W., Gonzaga-Jauregui C., Dumin E., Saada A., et al. A recurring NFS1 pathogenic variant causes a mitochondrial disorder with variable intra-familial patient outcomes. Mol. Genet. Metab. Rep. 2020;26:100699. doi: 10.1016/j.ymgmr.2020.100699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lim S.C., Friemel M., Marum J.E., Tucker E., Bruno D.L., Riley L.G., Christodoulou J., Kirk E., Boneh A., DeGennaro C.M., et al. Mutations in LYRM4, encoding iron–sulfur cluster biogenesis factor ISD11, cause deficiency of multiple respiratory chain complexes. Hum. Mol. Genet. 2013;22:4460–4473. doi: 10.1093/hmg/ddt295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Campuzano V., Montermini L., Molto M.D., Pianese L., Cossée M., Cavalcanti F., Monros E., Rodius F., Duclos F., Monticelli A., et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–1427. doi: 10.1126/science.271.5254.1423. [DOI] [PubMed] [Google Scholar]
- 78.Coppola G., De Michele G., Cavalcanti F., Painese L., Perretti A., Santoro L., Vita G., Toscano A., Amboni M., Grimaldi G., et al. Why do some Friedreich’s ataxia patients retain tendon reflexes? J. Neurol. 1999;246:353–357. doi: 10.1007/s004150050362. [DOI] [PubMed] [Google Scholar]
- 79.Bidichandani I.S., Ashizawa T., Patel P. Atypical Friedreich ataxia caused by compound heterozygosity for a novel missense mutation and the GAA triplet-repeat expansion. Am. J. Hum. Genet. 1997;60:1251–1256. [PMC free article] [PubMed] [Google Scholar]
- 80.Zühlke C., Laccone F., Cossée M., Kohlschütter A., Koenig M., Schwinger E. Mutation of the start codon in the FRDA1 gene: Linkage analysis of three pedigrees with the ATG to ATT transversion points to a unique common ancestor. Qual. Life Res. 1998;103:102–105. doi: 10.1007/s004390050791. [DOI] [PubMed] [Google Scholar]
- 81.Cossee M., Dürr A., Schmitt M., Dahl N., Trouillas P., Kostrzewa M., Nivelon-Chevallier A., Gustavson K.H., Kohlschütter A., Müller U., et al. Friedreich’s ataxia: Point mutations and clinical presentation of compound heterozygotes. Ann. Neurol. 1999;45:200–206. doi: 10.1002/1531-8249(199902)45:2<200::AID-ANA10>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 82.Gellera C., Castellotti B., Mariotti C., Mineri R., Seveso V., DiDonato S., Taroni F. Frataxin gene point mutations in Italian Friedreich ataxia patients. Neurogenetics. 2007;8:289–299. doi: 10.1007/s10048-007-0101-5. [DOI] [PubMed] [Google Scholar]
- 83.Evans-Galea M.V., Corben L.A., Hasell J., Galea C.A., Fahey M.C., Du Sart D., Delatycki M.B. A novel deletion–insertion mutation identified in exon 3 of FXN in two siblings with a severe Friedreich ataxia phenotype. Neurogenetics. 2011;12:307–313. doi: 10.1007/s10048-011-0296-3. [DOI] [PubMed] [Google Scholar]
- 84.Mochel F., Knight M.A., Tong W.-H., Hernandez D., Ayyad K., Taivassalo T., Andersen P.M., Singleton A., Rouault T.A., Fischbeck K.H., et al. Splice Mutation in the iron-sulfur cluster scaffold protein ISCU causes myopathy with exercise intolerance. Am. J. Hum. Genet. 2008;82:652–660. doi: 10.1016/j.ajhg.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Olsson A., Lind L., Thornell L.-E., Holmberg M. Myopathy with lactic acidosis is linked to chromosome 12q23.3-24.11 and caused by an intron mutation in the ISCU gene resulting in a splicing defect. Hum. Mol. Genet. 2008;17:1666–1672. doi: 10.1093/hmg/ddn057. [DOI] [PubMed] [Google Scholar]
- 86.Sanaker P.S., Toompuu M., Hogan V.E., He L., Tzoulis C., Chrzanowska-Lightowlers Z.M., Taylor R.W., Bindoff L.A. Differences in RNA processing underlie the tissue specific phenotype of ISCU myopathy. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2010;1802:539–544. doi: 10.1016/j.bbadis.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 87.Kollberg G., Tulinius M., Melberg A., Darin N., Andersen O., Holmgren D., Oldfors A., Holme E. Clinical manifestation and a new ISCU mutation in iron–sulphur cluster deficiency myopathy. Brain. 2009;132:2170–2179. doi: 10.1093/brain/awp152. [DOI] [PubMed] [Google Scholar]
- 88.Spiegal R., Saada A., Halvardson J., Soiferman D., Shaag A., Edvardson S., Horovitz Y., Khayat M., Shalev S.A., Feuk L., et al. Deleterious mutation in FDX1L gene is associated with a novel mitochondrial muscle myopathy. Eur. J. Hum. Genet. 2014;22:902–906. doi: 10.1038/ejhg.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gurgel-Giannetti J., Lynch D.S., De Paiva A.R.B., Lucato L., Yamamoto G., Thomsen C., Basu S., Freua F., Giannetti A.V., Assis B.D.R.D., et al. A novel complex neurological phenotype due to a homozygous mutation in FDX2. Brain. 2018;141:2289–2298. doi: 10.1093/brain/awy172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Paul A., Drecourt A., Petit F., Deguine D.D., Vasnier C., Oufadem M., Masson C., Bonnet C., Masmoudi S., Mosnier I., et al. FDXR Mutations cause sensorial neuropathies and expand the spectrum of mitochondrial Fe-S-synthesis diseases. Am. J. Hum. Genet. 2017;101:630–637. doi: 10.1016/j.ajhg.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Van Waveren H.G.D., van Roermund H.P., Snijders P.J. Hereditary sideroblastic anaemia and autosomal inheritance of erythrocyte dimorphism in a Dutch family. Eur. J. Haemat. 1987;38:405–409. doi: 10.1111/j.1600-0609.1987.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 92.Schmitz-Abe K., Ciesielski S., Schmidt P.J., Campagna D.R., Rahimov F., Schilke B.A., Cuijpers M., Rieneck K., Lausen B., Linenberger M.L., et al. Congenital sideroblastic anemia due to mutations in the mitochondrial HSP70 homologue HSPA9. Blood. 2015;126:2734–2738. doi: 10.1182/blood-2015-09-659854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Camaschella C., Campanella A., De Falco L., Boschetto L., Merlini R., Silvestri L., Levi S., Iolascon A. The human counterpart of zebrafish shiraz shows sideroblastic-like microcytic anemia and iron overload. Blood. 2007;110:1353–1358. doi: 10.1182/blood-2007-02-072520. [DOI] [PubMed] [Google Scholar]
- 94.Ye H., Jeong S.Y., Ghosh M.C., Kovtunovych G., Silvestri L., Ortillo D., Uchida N., Tisdale J., Camaschella C., Rouault T.A. Glutaredoxin 5 deficiency causes sideroblastic anemia by specifically impairing heme biosynthesis and depleting cytosolic iron in human erythroblasts. J. Clin. Investig. 2010;120:1749–1761. doi: 10.1172/JCI40372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu G., Guo S., Anderson G.J., Camaschella C., Han B., Nie G. Heterozygous missense mutations in the GLXR5 gene cause sideroblastic anemia in a Chinese patient. Blood. 2014;124:2750–2751. doi: 10.1182/blood-2014-08-598508. [DOI] [PubMed] [Google Scholar]
- 96.Shukla A., Hebbar M., Srivastava A., Kadavigere R., Upadhyai P., Kanthi A., Brandau O., Bielas S., Girisha K.M. Homozygous p. (Glu87Lys) variant in ISCA1 is associated with a multiple mitochondrial dysfunctions syndrome. J. Hum. Genet. 2017;62:723–727. doi: 10.1038/jhg.2017.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Torraco A., Stehling O., Stümpfig C., Rösser R., De Rasmo D., Fiermonte G., Verrigni D., Rizza T., Vozza A., Di Nottia M., et al. ISCA1 mutation in a patient with infantile-onset leukodystrophy causes defects in mitochondrial [4Fe-4S] proteins. Hum. Mol. Genet. 2018;27:2739–2754. doi: 10.1093/hmg/ddy183. [DOI] [PubMed] [Google Scholar]
- 98.Al-Hassan Z.N., Al-Dosary M., Alfadhel M., Faqeih E.A., Alsagob M., Kenana R., Almass R., Al-Harazi O.S., Al-Hindi H., Malibari O.I., et al. ISCA2 mutation causes infantile neurodegenerative mitochondrial disorder. J. Med. Genet. 2015;52:186–195. doi: 10.1136/jmedgenet-2014-102592. [DOI] [PubMed] [Google Scholar]
- 99.Alaimo J.T., Besse A., Alston C.L., Pang K., Appadurai V., Samanta M., Smpokou P., McFarland R., Taylor R.W., Bonnen P.E. Loss-of-function mutations in ISCA2 disrupt 4Fe-4S cluster machinery and cause a fatal leukodystrophy with hyperglycinemia and mtDNA depletion. Hum. Mutat. 2018;39:537–549. doi: 10.1002/humu.23396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Alfadhel M., Nashabat M., Alrifai M.T., Alshaalan H., Al Mutairi F., Al-Shahrani S.A., Plecko B., Almass R., Alsagob M., Almutairi F.B., et al. Further delineation of the phenotypic spectrum of ISCA2 defect: A report of ten new cases. Eur. J. Paediatr. Neurol. 2018;22:46–55. doi: 10.1016/j.ejpn.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 101.Toldo I., Nosadini M., Boscardin C., Talenti G., Manara R., Lamantea E., Legati A., Ghezzi D., Perilongo G., Sartori S. Neonatal mitochondrial leukoencephalopathy with brain and spinal involvement and high lactate: Expanding the phenotype of ISCA2 gene mutations. Metab. Brain Dis. 2018;33:805–812. doi: 10.1007/s11011-017-0181-3. [DOI] [PubMed] [Google Scholar]
- 102.Bolar N.A., Vanlander A.V., Wilbrecht C., Van Der Aa N., Smet J., De Paepe B., Vandeweyer G., Kooy F., Eyskens F., De Latter E., et al. Mutation of the iron-sulfur cluster assembly gene IBA57 causes severe myopathy and encephalopathy. Hum. Mol. Genet. 2013;22:2590–2602. doi: 10.1093/hmg/ddt107. [DOI] [PubMed] [Google Scholar]
- 103.Lossos A., Stümpfig C., Stevanin G., Gaussen M., Zimmerman B.-E., Mundwiller E., Asulin M., Chamma L., Sheffer R., Misk A., et al. Fe/S protein assembly gene IBA57 mutation causes hereditary spastic paraplegia. Neurology. 2015;84:659–667. doi: 10.1212/WNL.0000000000001270. [DOI] [PubMed] [Google Scholar]
- 104.Debray F.-G., Stümpfig C., Vanlander A.V., Dideberg V., Josse C., Caberg J.-H., Boemer F., Bours V., Stevens R., Seneca S., et al. Mutation of the iron-sulfur cluster assembly gene IBA57 causes fatal infantile leukodystrophy. J. Inherit. Metab. Dis. 2015;38:1147–1153. doi: 10.1007/s10545-015-9857-1. [DOI] [PubMed] [Google Scholar]
- 105.Torraco A., Ardissone A., Invernizzi F., Rizza T., Fiermonte G., Niceta M., Zanetti N., Martinelli D., Vozza A., Verrigni D., et al. Novel mutations in IBA57 are associated with leukodystrophy and variable clinical phenotypes. J. Neurol. 2016;264:102–111. doi: 10.1007/s00415-016-8312-z. [DOI] [PubMed] [Google Scholar]
- 106.Liu M., Zhang J., Zhang Z., Zhou L., Jiang Y., Wang J., Xiao J., Wu Y. Phenotypic spectrum of mutations in IBA57, a candidate gene for cavitating leukoencephalopathy. Clin. Genet. 2017;93:235–241. doi: 10.1111/cge.13090. [DOI] [PubMed] [Google Scholar]
- 107.Ishiyama A., Sakai C., Matsushima Y., Noguchi S., Mitsuhashi S., Endo Y., Hayashi Y.K., Saito Y., Nakagawa E., Komaki H., et al. IBA57 mutations abrogate iron-sulfur cluster assembly leading to cavitating leukoencephalopathy. Neurol. Genet. 2017;3:e184. doi: 10.1212/NXG.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Seyda A., Newbold R.F., Hudson T., Verner A., MacKay N., Winter S., Feigenbaum A., Malaney S., Gonzalez-Halphen D., Cuthbert A.P., et al. A novel syndrome affecting multiple mitochondrial functions, located by microcell-mediated transfer to chromosome 2p14-2p13. Am. J. Hum. Genet. 2001;68:386–396. doi: 10.1086/318196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Navarro-Sastre A., Tort F., Stehling O., Uzarska M.A., Arranz J.A., del Toro M., Labayru M.T., Landa J., Font A., Garcia-Villoria J., et al. A fatal mitochondrial disease is associated with defective NFU1 Function in the Maturation of a Subset of mitochondrial Fe-S proteins. Am. J. Hum. Genet. 2011;89:656–667. doi: 10.1016/j.ajhg.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Calvo S.E., Tucker E., Compton A., Kirby D.M., Crawford G., Burtt N.P., Rivas M., Guiducci C., Bruno D.L., Goldberger O.A., et al. High-throughput, pooled sequencing identifies mutations in NUBPL and FOXRED1 in human complex I deficiency. Nat. Genet. 2010;42:851–858. doi: 10.1038/ng.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kevelam S.H., Rodenburg R.J., Wolf N.I., Ferreira P., Lunsing R.J., Nijtmans L.G., Mitchell A., Arroyo H.A., Rating D., Vanderver A., et al. NUBPL mutations in patients with complex I deficiency and a distinct MRI pattern. Neurology. 2013;80:1577–1583. doi: 10.1212/WNL.0b013e31828f1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kimonis V., al Dubaisi R., Maclean A., Hall K., Weiss L., Stover A.E., Schwartz P.H., Berg B., Cheng C., Parikh S., et al. NUBPL mitochondrial disease: New patients and review of the genetic and clinical spectrum. J. Med. Genet. 2020;58:314–325. doi: 10.1136/jmedgenet-2020-106846. [DOI] [PubMed] [Google Scholar]
- 113.Friederich M.W., Perez F.A., Knight K.M., Van Hove R.A., Yang S.P., Saneto R.P., Van Hove J.L. Pathogenic variants in NUBPL result in failure to assemble the matrix arm of complex I and cause a complex leukoencephalopathy with thalamic involvement. Mol. Genet. Metab. 2019;129:236–242. doi: 10.1016/j.ymgme.2019.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Baker P.R., Friederich M.W., Swanson M.A., Shaikh T., Bhattacharya K., Scharer G.H., Aicher J., Creadon-Swindell G., Geiger E., MacLean K.N., et al. Variant non ketotic hyperglycinemia is caused by mutations in LIAS, BOLA3 and the novel gene GLRX5. Brain. 2013;137:366–379. doi: 10.1093/brain/awt328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Haack T.B., Rolinski B., Haberberger B., Zimmermann F., Schum J., Strecker V., Graf E., Athing U., Hoppen T., Wittig I., et al. Homozygous missense mutation in BOLA3 causes multiple mitochondrial dysfunctions syndrome in two siblings. J. Inherit. Metab. Dis. 2012;36:55–62. doi: 10.1007/s10545-012-9489-7. [DOI] [PubMed] [Google Scholar]
- 116.Pagon A.R., Bird T.D., Detter J.C., Pierce I. Hereditary sideroblastic anaemia and ataxia: An X linked recessive disorder. J. Med. Genet. 1985;22:267–273. doi: 10.1136/jmg.22.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bekri S., Kispal G., Lange H., Fitzsimons E., Tolmie J., Lill R., Bishop D.F. Human ABC7 transporter: Gene structure and mutation causing X-linked sideroblastic anemia with ataxia with disruption of cytosolic iron-sulfur protein maturation. Blood. 2000;96:3256–3264. doi: 10.1182/blood.V96.9.3256. [DOI] [PubMed] [Google Scholar]
- 118.Maguire A., Hellier K., Hammans S., May A. X-linked cerebellar ataxia and sideroblastic anaemia associated with a missense mutation in the ABC7 gene predicting V411L. Br. J. Haematol. 2001;115:910–917. doi: 10.1046/j.1365-2141.2001.03015.x. [DOI] [PubMed] [Google Scholar]
- 119.Lamoril J., Boulechfar S., de Verneuil H., Grandchamp B., Nordmann Y., Deybach J.-C. Human Erythropoietic Protoporphyria: Two point mutations in the ferrochelatase gene. Biochem. Biophys. Res. Commun. 1991;181:594–599. doi: 10.1016/0006-291X(91)91231-Z. [DOI] [PubMed] [Google Scholar]
- 120.Nakahashi Y., Fujita H., Taketani S., Ishida N., Kappas A., Sassa S. The molecular defect of ferrochelatase in a patient with erythropoietic protoporphyria. Proc. Natl. Acad. Sci. USA. 1992;89:281–285. doi: 10.1073/pnas.89.1.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Brenner D., Didier J.M., Frasier F., Christensen S.R., Evans G.A., Dailey H.A. A molecular defect in human protoporphyria. Am. J. Hum. Genet. 1992;50:1203–1210. [PMC free article] [PubMed] [Google Scholar]
- 122.Sarkany R.P.E., Alexander G.J.M.A., Cox T.M. Recessive inheritance of erythropoietic protoporphyria with liver failure. Lancet. 1994;343:1394–1396. doi: 10.1016/S0140-6736(94)92525-9. [DOI] [PubMed] [Google Scholar]
- 123.Bloomer J., Bruzzone C., Zhu L., Scarlett Y., Magness S., Brenner D. Molecular defects in ferrochelatase in patients with protoporphyria requiring liver transplantation. J. Clin. Investig. 1998;102:107–114. doi: 10.1172/JCI1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Schneider-Yin X., Gouya L., Dorsey M., Rüfenacht U., Deybach J.C., Ferreira G.C. Mutations in the iron-sulfur cluster ligands of the human ferrochelatase lead to erythropoietic protoporphyria. Blood. 2000;96:1545–1549. doi: 10.1182/blood.V96.4.1545. [DOI] [PubMed] [Google Scholar]
- 125.Herrerro C., To-Figueras J., Badenas C. Clinical, biochemical, and genetic study of 11 patients with erythropoietic protoporphyria including one with homozygous disease. Arch. Dermatol. 2007;143:1125–1129. doi: 10.1001/archderm.143.9.1125. [DOI] [PubMed] [Google Scholar]
- 126.Valnot I., Von Kleist-Retzow J.-C., Barrientos A., Gorbatyuk M., Taanman J.-W., Mehaye B., Rustin P., Tzagoloff A., Munnich A., Rotig A. A mutation in the human heme A: Farnesyltransferase gene (COX10) causes cytochrome c oxidase deficiency. Hum. Mol. Genet. 2000;9:1245–1249. doi: 10.1093/hmg/9.8.1245. [DOI] [PubMed] [Google Scholar]
- 127.Antonicka H., Pankratz N., Nichols W.C., Uniacke S.K., Halter C., Murrell J., Rudolph A., Shults C.W., Conneally P.M., Foroud T. Mutations in COX10 result in a defect in mitochondrial heme A biosynthesis and account for multiple, early-onset clinical phenotypes associated with isolated COX deficiency. Hum. Mol. Genet. 2003;12:2693–2702. doi: 10.1093/hmg/ddg284. [DOI] [PubMed] [Google Scholar]
- 128.Coenen M.J.H., van den Heuvel L.P., Ugalde C., Brinke M.T., Nijtmans L.G.J., Trijbels F.J.M., Beblo S., Maier E.M., Muntau A.C., Smeitink J.A.M. Cytochrome c oxidase biogenesis in a patient with a mutation in COX10 gene. Ann. Neurol. 2004;56:560–564. doi: 10.1002/ana.20229. [DOI] [PubMed] [Google Scholar]
- 129.Kennaway N.G., Carerro-Valenzuela R.D., Ewart G., Balan V.K., Lightowlers R., Zhang Y.Z., Powell B.R., Capaldi R.A., Buist N.R. Isoforms of mammalian cytochrome c oxidase: Correlation with human cytochrome c oxidase deficiency. Pediat. Res. 1990;28:529–535. doi: 10.1203/00006450-199011000-00024. [DOI] [PubMed] [Google Scholar]
- 130.Antonicka H., Mattman A., Carlson C.G., Glerum D.M., Hoffbuhr K.C., Leary S.C., Kennaway N.G., Shoubridge E.A. Mutations in COX15 produce a defect in mitochondrial heme biosynthetic pathway, causing early onset fatal hypertrophic cardiomyopathy. Am. J. Hum. Genet. 2003;72:101–114. doi: 10.1086/345489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Alfadhel M., Lillquist Y.P., Waters P.J., Sinclair G., Struys E., McFadden D., Hendson G., Hyams L., Shoffner J., Vallance H.D. Infantile cardioencephalopathy due to a COX15 gene defect: Report and review. Am. J. Med. Genet. Part A. 2011;155:840–844. doi: 10.1002/ajmg.a.33881. [DOI] [PubMed] [Google Scholar]
- 132.Bugiani M., Tiranti V., Farina L., Uziel G., Zeviani M. Novel mutations in COX15 in a long surviving Leigh syndrome patient with cytochrome c oxidase deficiency. J. Med. Genet. 2005;42:e28. doi: 10.1136/jmg.2004.029926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sheftel A.D., Zhang A.-S., Brown C., Shirihai O.S., Ponka P. Direct interorganellar transfer of iron from endosome to mitochondrion. Blood. 2007;110:125–132. doi: 10.1182/blood-2007-01-068148. [DOI] [PubMed] [Google Scholar]
- 134.Hamdi A., Roshan T.M., Kahawita T.M., Mason A.B., Sheftel A.D., Ponka P. Erythroid cell mitochondria receive endosomal iron by a “kiss-and-run” mechanism. Biochim. Biophys. Acta Mol. Cell Res. 2016;1863:2859–2867. doi: 10.1016/j.bbamcr.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 135.Das A., Nag S., Mason A.B., Barroso M.M. Endosome–mitochondria interactions are modulated by iron release from transferrin. J. Cell Biol. 2016;214:831–845. doi: 10.1083/jcb.201602069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shvartsman M., Kikkeri R., Shanzer A., Cabantchik Z.I. Non-transferrin-bound iron reaches mitochondria by a chelator-inaccessible mechanism: Biological and clinical implications. Am. J. Physiol. Cell Physiol. 2007;293:C1383–C1394. doi: 10.1152/ajpcell.00054.2007. [DOI] [PubMed] [Google Scholar]
- 137.Shvartsman M., Fibach E., Cabantchik Z.I. Transferrin-iron routing to the cytosol and mitochondria as studied by live and real-time fluorescence. Biochem. J. 2010;429:185–193. doi: 10.1042/BJ20100213. [DOI] [PubMed] [Google Scholar]
- 138.Shvartsman M., Cabantchik Z.I. Intracellular iron trafficking: Role of cytosolic ligands. BioMetals. 2012;25:711–723. doi: 10.1007/s10534-012-9529-7. [DOI] [PubMed] [Google Scholar]
- 139.Khalil S., Holy M., Grado S., Fleming R., Kurita R., Nakamura Y., Goldfarb A. A specialized pathway for erythroid iron delivery through lysosomal trafficking of transferrin receptor 2. Blood Adv. 2017;1:1181–1194. doi: 10.1182/bloodadvances.2016003772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hughes C.E., Coody T., Jeong M.-Y., Berg J., Winge D.R., Hughes A.L. Cysteine toxicity drives age-related mitochondrial decline by altering iron homeostasis. Cell. 2020;180:296–310.e18. doi: 10.1016/j.cell.2019.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Weber R.A., Yen F., Nicholson S.P., Alwaseem H., Bayraktar E., Alam M., Timson R.C., La K., Abu-Remaileh M., Molina H., et al. maintaining iron homeostasis is the key role of lysosomal acidity for cell proliferation. Mol. Cell. 2020;77:645–655.e7. doi: 10.1016/j.molcel.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kim J.E., Vali S.W., Nguyen T.Q., Dancis A., Lindahl P.A. Mössbauer and LC-ICP-MS investigation of iron trafficking between vacuoles and mitochondria in vma2Δ Saccharomyces cerevisiae. J. Biol. Chem. 2021;296:100141. doi: 10.1074/jbc.RA120.015907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yambire K.F., Rostosky C., Watanabe T., Pacheu-Grau D., Torres-Odio S., Sanchez-Guerrero A., Senderovich O., Meyron-Holtz E.G., Milosevic I., Frahm J., et al. Author response: Impaired lysosomal acidification triggers iron deficiency and inflammation in vivo. eLife. 2019;8:e51031. doi: 10.7554/eLife.51031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Breuer W., Epsztejn S., Cabantchik Z.I. Iron acquired from transferrin by K562 cells is delivered into a cytoplasmic pool of chelatable iron(II) J. Biol. Chem. 1995;270:24209–24215. doi: 10.1074/jbc.270.41.24209. [DOI] [PubMed] [Google Scholar]
- 145.Jacobs A. Low molecular weight intracellular iron transport compounds. Blood. 1977;50:433–439. doi: 10.1182/blood.V50.3.433.433. [DOI] [PubMed] [Google Scholar]
- 146.Devireddy L.R., Hart D.O., Goetz D.H., Green M.R. A Mammalian siderophore synthesized by an enzyme with a bacterial homolog involved in enterobactin production. Cell. 2010;141:1006–1017. doi: 10.1016/j.cell.2010.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lange H., Kispal G., Lill R. Mechanism of iron transport to the site of heme synthesis inside yeast mitochondria. J. Biol. Chem. 1999;274:18989–18996. doi: 10.1074/jbc.274.27.18989. [DOI] [PubMed] [Google Scholar]
- 148.Flatmark T., Romslo I. Energy dependent accumulation of iron by isolated rat liver mitochondria. J. Biol. Chem. 1975;250:6433–6438. doi: 10.1016/S0021-9258(19)41082-X. [DOI] [PubMed] [Google Scholar]
- 149.Lutsenko S. Human copper homeostasis: A network of interconnected pathways. Curr. Opin. Chem. Biol. 2010;14:211–217. doi: 10.1016/j.cbpa.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Frey A.G., Nandal A., Park J.H., Smith P.M., Yabe T., Ryu M.-S., Ghosh M.C., Lee J., Rouault T.A., Park M.H., et al. Iron chaperones PCBP1 and PCBP2 mediate the metallation of the dinuclear iron enzyme deoxyhypusine hydroxylase. Proc. Natl. Acad. Sci. USA. 2014;111:8031–8036. doi: 10.1073/pnas.1402732111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yanatori I., Yasui Y., Tabuchi M., Kishi F. Chaperone protein involved in transmembrane transport of iron. Biochem. J. 2014;462:25–37. doi: 10.1042/BJ20140225. [DOI] [PubMed] [Google Scholar]
- 152.Li H., Mapolelo D.T., Dingra N.N., Naik A.G., Lees N.S., Hoffman B.M., Riggs-Gelasco P.J., Huynh B.H., Johnson M.K., Outten C.E. The yeast iron regulatory proteins Grx3/4 and Fra2 form heterodimeric complexes containing a [2Fe-2S] cluster with cysteinyl and histidyl ligation. Biochemistry. 2009;48:9569–9581. doi: 10.1021/bi901182w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mühlenhoff U., Molik S., Godoy J.R., Uzarska M.A., Richter N., Seubert A., Zhang Y., Stubbe J., Pierrel F., Herrero E., et al. Cytosolic monothiol glutaredoxins function in intracellular iron sensing and trafficking via their bound iron-sulfur cluster. Cell Metab. 2010;12:373–385. doi: 10.1016/j.cmet.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Shoshan-Barmatz V., Mizrachi D. VDAC1: From structure to cancer therapy. Front. Oncol. 2012;2:164. doi: 10.3389/fonc.2012.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wolff N.A., Ghio A.J., Garrick L.M., Garrick M., Zhao L., Fenton R., Thévenod F. Evidence for mitochondrial localization of divalent metal transporter 1 (DMT1) FASEB J. 2014;28:2134–2145. doi: 10.1096/fj.13-240564. [DOI] [PubMed] [Google Scholar]
- 156.Wolff N.A., Garrick M., Zhao L., Garrick L.M., Ghio A.J., Thévenod F. A role for divalent metal transporter (DMT1) in mitochondrial uptake of iron and manganese. Sci. Rep. 2018;8:2134–2145. doi: 10.1038/s41598-017-18584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Foury F., Roganti T. Deletion of the mitochondrial carrier genes MRS3 and MRS4 suppresses mitochondrial iron accumulation in a yeast frataxin-deficient strain. J. Biol. Chem. 2002;277:24475–24483. doi: 10.1074/jbc.M111789200. [DOI] [PubMed] [Google Scholar]
- 158.Mühlenhoff U., Stadler J.A., Richhardt N., Seubert A., Eickhorst T., Schweyen R.J., Lill R., Wiesenberger G. A specific role of the yeast mitochondrial carriers Mrs3/4p in mitochondrial iron acquisition under iron-limiting conditions. J. Biol. Chem. 2003;278:40612–40620. doi: 10.1074/jbc.M307847200. [DOI] [PubMed] [Google Scholar]
- 159.Nyhus K.J., Ozaki L.S., Jacobson E.S. Role of mitochondrial carrier protein Mrs3/4 in iron acquisition and oxidative stress resistance of Cryptococcus neoformans. Med. Mycol. 2002;40:581–591. doi: 10.1080/mmy.40.6.581.591. [DOI] [PubMed] [Google Scholar]
- 160.Shaw G.C., Cope J.J., Li L., Corson K., Hersey C., Ackermann G.E., Gwynn B., Lambert A.J., Wingert R.A., Traver D., et al. Mitoferrin is essential for erythroid iron assimilation. Nature. 2006;440:96–100. doi: 10.1038/nature04512. [DOI] [PubMed] [Google Scholar]
- 161.Bashir K., Ishimaru Y., Shimo H., Nagasaka S., Fujimoto M., Takanashi H., Tsutsumi N., An G., Nakanishi H., Nishizawa N.K. The rice mitochondrial iron transporter is essential for plant growth. Nat. Commun. 2011;2:322. doi: 10.1038/ncomms1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ren Y., Yang S., Tan G., Ye W., Liu D., Qian X., Ding Z., Zhong Y., Zhang J., Jiang D., et al. Reduction of mitoferrin results in abnormal development and extended lifespan in Caenorhabditis elegans. PLoS ONE. 2012;7:e29666. doi: 10.1371/journal.pone.0029666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Metzendorf C., Wu W., Lind M.I. Overexpression of Drosophila mitoferrin in l(2)mbn cells results in dysregulation of Fer1HCH expression. Biochem. J. 2009;421:463–471. doi: 10.1042/BJ20082231. [DOI] [PubMed] [Google Scholar]
- 164.Paradkar P.N., Zumbrennen K.B., Paw B.H., Ward D.M., Kaplan J. Regulation of mitochondrial iron import through differential turnover of mitoferrin 1 and mitoferrin 2. Mol. Cell. Biol. 2009;29:1007–1016. doi: 10.1128/MCB.01685-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Del Arco A., Satrústegui J. New mitochondrial carriers: An overview. Cell. Mol. Life Sci. 2005;62:2204–2227. doi: 10.1007/s00018-005-5197-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gutiérrez-Aguilar M., Baines C.P. Physiological and pathological roles of mitochondrial SLC25 carriers. Biochem. J. 2013;454:371–386. doi: 10.1042/BJ20121753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kunji E.R., Robinson A.J. The conserved substrate binding site of mitochondrial carriers. Biochim. Biophys. Acta (BBA) Bioenerg. 2006;1757:1237–1248. doi: 10.1016/j.bbabio.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 168.Palmieri F. Diseases caused by defects of mitochondrial carriers: A review. Biochim. Biophys. Acta (BBA) Bioenerg. 2008;1777:564–578. doi: 10.1016/j.bbabio.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 169.Zhang Y., Lyver E.R., Knight S., Lesuisse E., Dancis A. Frataxin and mitochondrial carrier proteins, Mrs3p and Mrs4p, cooperate in providing iron for heme synthesis. J. Biol. Chem. 2005;280:19794–19807. doi: 10.1074/jbc.M500397200. [DOI] [PubMed] [Google Scholar]
- 170.Zhang Y., Lyver E.R., Knight S., Pain D., Lesuisse E., Dancis A. Mrs3p, Mrs4p, and frataxin provide iron for Fe-S cluster synthesis in mitochondria. J. Biol. Chem. 2006;281:22493–22502. doi: 10.1074/jbc.M604246200. [DOI] [PubMed] [Google Scholar]
- 171.Courel M., Lallet S., Camadro J.-M., Blaiseau P.-L. Direct activation of genes involved in intracellular iron use by the yeast iron-responsive transcription factor Aft2 without its paralog Aft1. Mol. Cell. Biol. 2005;25:6760–6771. doi: 10.1128/MCB.25.15.6760-6771.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Rutherford J.C., Jaron S., Winge D.R. Aft1p and Aft2p mediate iron-responsive gene expression in yeast through related promoter elements. J. Biol. Chem. 2003;278:27636–27643. doi: 10.1074/jbc.M300076200. [DOI] [PubMed] [Google Scholar]
- 173.Froschauer E.M., Schweyen R.J., Wiesenberger G. The yeast mitochondrial carrier proteins Mrs3p/Mrs4p mediate iron transport across the inner mitochondrial membrane. Biochim. Biophys. Acta (BBA) Biomembr. 2009;1788:1044–1050. doi: 10.1016/j.bbamem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 174.Vest K.E., Wang J., Gammon M.G., Maynard M.K., White O.L., Cobine J.A., Mahone W.K., Cobine P.A. Overlap of copper and iron uptake systems in mitochondria in Saccharomyces cerevisiae. Open Biol. 2016;6:150223. doi: 10.1098/rsob.150223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Froschauer E.M., Rietzschel N., Hassler M.R., Binder M., Schweyen R.J., Lill R., Mühlenhoff U., Wiesenberger G. The mitochondrial carrier Rim2 co-imports pyrimidine nucleotides and iron. Biochem. J. 2013;455:57–65. doi: 10.1042/BJ20130144. [DOI] [PubMed] [Google Scholar]
- 176.Lin H., Li L., Jia X., Ward D.M., Kaplan J. Genetic and biochemical analysis of high iron toxicity in yeast. J. Biol. Chem. 2011;286:3851–3862. doi: 10.1074/jbc.M110.190959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yoon H., Zhang Y., Pain J., Lyver E.R., Lesuisse E., Pain D., Dancis A. Rim2, a pyrimidine nucleotide exchanger, is needed for iron utilization in mitochondria. Biochem. J. 2011;440:137–146. doi: 10.1042/BJ20111036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Di Noia M.A., Todisco S., Cirigliano A., Rinaldi T., Agrimi G., Iacobazzi V., Palmieri F. The human SLC25A33 and SLC25A36 genes of solute carrier family 25 encode two mitochondrial pyrimidine nucleotide transporters. J. Biol. Chem. 2014;289:33137–33148. doi: 10.1074/jbc.M114.610808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Vozza A., Blanco E., Palmieri L., Palmieri F. Identification of the mitochondrial GTP/GDP transporter in Saccharomyces cerevisiae. J. Biol. Chem. 2004;279:20850–20857. doi: 10.1074/jbc.M313610200. [DOI] [PubMed] [Google Scholar]
- 180.Van Dyck E., Jank B., Ragnini A., Schweyen R.J., Duyckaerts C., Sluse F., Foury F. Overexpression of a novel member of the mitochondrial carrier family rescues defects in both DNA and RNA metabolism in yeast mitochondria. Mol. Genet. Genom. 1995;246:426–436. doi: 10.1007/BF00290446. [DOI] [PubMed] [Google Scholar]
- 181.Traba J., Froschauer E.M., Wiesenberger G., Satrústegui J., Del Arco A. Yeast mitochondria import ATP through the calcium-dependent ATP-Mg/Pi carrier Sal1p, and are ATP consumers during aerobic growth in glucose. Mol. Microbiol. 2008;69:570–585. doi: 10.1111/j.1365-2958.2008.06300.x. [DOI] [PubMed] [Google Scholar]
- 182.Mühlenhoff U., Hoffmann B., Richter N., Rietzschel N., Spantgar F., Stehling O., Uzarska M.A., Lill R. Compartmentalization of iron between mitochondria and the cytosol and its regulation. Eur. J. Cell Biol. 2015;94:292–308. doi: 10.1016/j.ejcb.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 183.Chung J., Anderson S.A., Gwynn B., Deck K.M., Chen M.J., Langer N.B., Shaw G.C., Huston N.C., Boyer L.F., Datta S., et al. Iron regulatory protein-1 protects against mitoferrin1-deficient porphyria. J. Biol. Chem. 2014;289:7835–7843. doi: 10.1074/jbc.M114.547778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wang Y., Langer N.B., Shaw G.C., Yang G., Li L., Kaplan J., Paw B.H., Bloomer J.R. Abnormal mitoferrin-1 expression in patients with erythropoietic protoporphyria. Exp. Hematol. 2011;39:784–794. doi: 10.1016/j.exphem.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Chen W., Paradkar P.N., Li L., Pierce E.L., Langer N.B., Takahashi-Makise N., Hyde B.B., Shirihai O.S., Ward D.M., Kaplan J., et al. Abcb10 physically interacts with mitoferrin-1 (Slc25a37) to enhance its stability and function in the erythroid mitochondria. Proc. Natl. Acad. Sci. USA. 2009;106:16263–16268. doi: 10.1073/pnas.0904519106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen W., Dailey H.A., Paw B.H. Ferrochelatase forms an oligomeric complex with mitoferrin-1 and Abcb10 for erythroid heme biosynthesis. Blood. 2010;116:628–630. doi: 10.1182/blood-2009-12-259614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Shum M., Shintre C.A., Althoff T., Gutierrez V., Segawa M., Saxberg A.D., Martinez M., Adamson R., Young M.R., Faust B., et al. ABCB10 exports mitochondrial biliverdin, driving metabolic maladaptation in obesity. Sci. Transl. Med. 2021;13:eabd1869. doi: 10.1126/scitranslmed.abd1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Huang M.L.-H., Becker E.M., Whitnall M., Rahmanto Y.S., Ponka P., Richardson D.R. Elucidation of the mechanism of mitochondrial iron loading in Friedreich’s ataxia by analysis of a mouse mutant. Proc. Natl. Acad. Sci. USA. 2009;106:16381–16386. doi: 10.1073/pnas.0906784106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Martelli A., Puccio H. Dysregulation of cellular iron metabolism in Friedreich ataxia: From primary iron-sulfur cluster deficit to mitochondrial iron accumulation. Front. Pharmacol. 2014;5:130. doi: 10.3389/fphar.2014.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Martelli A., Schmucker S., Reutenauer L., Mathieu J.R., Peyssonnaux C., Karim Z., Puy H., Galy B., Hentze M., Puccio H. Iron regulatory protein 1 sustains mitochondrial iron loading and function in frataxin deficiency. Cell Metab. 2015;21:311–323. doi: 10.1016/j.cmet.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 191.Crooks D.R., Natarajan T.G., Jeong S.Y., Chen C., Park S.Y., Huang H., Ghosh M.C., Tong W.-H., Haller R.G., Wu C., et al. Elevated FGF21 secretion, PGC-1α and ketogenic enzyme expression are hallmarks of iron-sulfur cluster depletion in human skeletal muscle. Hum. Mol. Gen. 2014;23:24–39. doi: 10.1093/hmg/ddt393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Delatycki M.B., Camakaris J., Brooks H., Evans-Whipp T., Thorburn D.R., Williamson R., Forrest S.M. Direct evidence that mitochondrial iron accumulation occurs in Friedreich ataxia. Ann. Neurol. 1999;45:673–675. doi: 10.1002/1531-8249(199905)45:5<673::AID-ANA20>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 193.Puccio H., Simon D., Cossée M., Criqui-Filipe P., Tiziano F.D., Melki J., Hindelang C., Matyas R., Rustin P., Koenig M. Mouse models for Friedreich ataxia exhibit cardiomyopathy, sensory nerve defect and Fe-S enzyme deficiency followed by intramitochondrial iron deposits. Nat. Genet. 2001;27:181–186. doi: 10.1038/84818. [DOI] [PubMed] [Google Scholar]
- 194.Uchiyama A., Kim J.-S., Kon K., Jaeschke H., Ikejima K., Watanabe S., Lemasters J.J. Translocatoin of iron from lysosomes into mitochondria is a key event during oxidative stress-induced hepatocellular injury. Hepatology. 2008;48:1644–1654. doi: 10.1002/hep.22498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lockhart P., Holtom B., Lincoln S., Hussey J., Zimprich A., Gasser T., Wszolek Z.K., Hardy J., Farrer M. The human sideroflexin 5 (SFXN5) gene: Sequence, expression analysis and exclusion as a candidate for PARK3. Gene. 2002;285:229–237. doi: 10.1016/S0378-1119(02)00402-X. [DOI] [PubMed] [Google Scholar]
- 196.Fleming M.D., Campagna D.R., Haslett J.N., Trenor III C.C., Andrews N.C. A mutation in a mitochondrial transmembrane protein is responsibe for the pleiotropic hematological and skeletal phenotype of flexed-tail (f/f) mice. Genes Dev. 2001;15:652–657. doi: 10.1101/gad.873001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kory N., Wyant G.A., Prakash G., de Bos J.U., Bottanelli F., Pacold M.E., Chan S.H., Lewis C.A., Wang T., Keys H.R., et al. SFXN1 is a mitochondrial serine transporter required for one-carbon metabolism. Science. 2018;362:eaat9528. doi: 10.1126/science.aat9528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Acoba M.G., Alpergin E.S.S., Renuse S., Fernández-Del-Río L., Lu Y.-W., Khalimonchuk O., Clarke C.F., Pandey A., Wolfgang M.J., Claypool S.M. The mitochondrial carrier SFXN1 is critical for complex III integrity and cellular metabolism. Cell Rep. 2021;34:108869. doi: 10.1016/j.celrep.2021.108869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Paul B.T., Tesfay L., Winkler C.R., Torti F.M., Torti S.V. Sideroflexin 4 affects Fe-S cluster biogenesis, iron metabolism, mitochondrial respiration and heme biosynthetic enzymes. Sci. Rep. 2019;9:19634. doi: 10.1038/s41598-019-55907-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Levi S., Corsi B., Bosisio M., Invernizzi R., Volz A., Sanford D., Arosio P., Drysdale J. A Human mitochondrial ferritin encoded by an intronless gene. J. Biol. Chem. 2001;276:24437–24440. doi: 10.1074/jbc.C100141200. [DOI] [PubMed] [Google Scholar]
- 201.Levi S., Arosio P. Mitochondrial ferritin. Int. J. Biochem. Cell Biol. 2004;36:1887–1889. doi: 10.1016/j.biocel.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 202.Cazzola M., Invernizzi R., Bergamaschi G., Levi S., Corsi B., Travaglino E., Rolandi V., Biasiotto G., Drysdale J., Arosio P. Mitochondrial ferritin expression in erythroid cells from patients with sideroblastic anemia. Blood. 2003;101:1996–2000. doi: 10.1182/blood-2002-07-2006. [DOI] [PubMed] [Google Scholar]
- 203.Santambrogio P., Biasiotto G., Sanvito F., Olivieri S., Arosio P., Levi S. Mitochondrial ferritin expression in adult mouse tissues. J. Histochem. Cytochem. 2007;55:1129–1137. doi: 10.1369/jhc.7A7273.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bou-Abdallah F., Santambrogio P., Levi S., Arosio P., Chasteen N.D. Unique iron binding and oxidation properties of human mitochondrial ferritin: A comparative analysis with human H-chain ferritin. J. Mol. Biol. 2005;347:543–554. doi: 10.1016/j.jmb.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 205.Corsi B., Cozzi A., Arosio P., Drysdale J., Santambrogio P., Campanella A., Biasiotto G., Albertini A., Levi S. Human mitochondrial ferritin expressed in HeLa cells incorporates iron and affects cellular iron metabolism. J. Biol. Chem. 2002;277:22430–22437. doi: 10.1074/jbc.M105372200. [DOI] [PubMed] [Google Scholar]
- 206.Campanella A., Rovelli E., Santambrogio P., Cozzi A., Taroni F., Levi S. Mitochondrial ferritin limits oxidative damage regulating mitochondrial iron availability: Hypothesis for a protective role in Friedreich ataxia. Hum. Mol. Genet. 2008;18:1–11. doi: 10.1093/hmg/ddn308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Mari M., Morales A., Colell A., García-Ruiz C., Fernández-Checa J.C. Mitochondrial glutathione, a key survival antioxidant. ARS. 2009;11:2685–2700. doi: 10.1089/ars.2009.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Lindahl P.A., Moore M.J. Labile low-molecular-mass metal complexes in mitochondria: Trials and tribulations of a burgeoning field. Biochemistry. 2016;55:4140–4153. doi: 10.1021/acs.biochem.6b00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Qi W., Cowan J. Mechanism of glutaredoxin—ISU [2Fe-2S] cluster exchange. Chem. Commun. 2011;47:4989–4991. doi: 10.1039/c0cc05079b. [DOI] [PubMed] [Google Scholar]
- 210.Hider R.C., Kong X. Iron speciation in the cytosol: An overview. Dalton Trans. 2013;42:3220–3229. doi: 10.1039/C2DT32149A. [DOI] [PubMed] [Google Scholar]
- 211.Srinivasan V., Pierik A.J., Lill R. Crystal structures of nucleotide-free and glutathione-bound mitochondrial ABC transporter Atm1. Science. 2014;343:1137–1140. doi: 10.1126/science.1246729. [DOI] [PubMed] [Google Scholar]
- 212.Schaedler T., Thornton J.D., Kruse I., Schwarzländer M., Meyer A.J., van Veen H.W., Balk J. A conserved mitochondrial ATP-binding cassette transporter exports glutathione polysulfide for cytosolic metal cofactor assembly. J. Biol. Chem. 2014;289:23264–23274. doi: 10.1074/jbc.M114.553438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Silva A.M.N., Kong X., Parkin M.C., Cammack R., Hider R.C. Iron(iii) citrate speciation in aqueous solution. Dalton Trans. 2009:8616–8625. doi: 10.1039/b910970f. [DOI] [PubMed] [Google Scholar]
- 214.Maio N., Rouault T.A. Iron–sulfur cluster biogenesis in mammalian cells: New insights into the molecular mechanisms of cluster delivery. Biochim. Biophys. Acta (BBA) Bioenerg. 2014;1853:1493–1512. doi: 10.1016/j.bbamcr.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Hinchliffe P., Sazanov L. Organization of iron-sulfur clusters in respiratory complex I. Science. 2005;309:771–774. doi: 10.1126/science.1113988. [DOI] [PubMed] [Google Scholar]
- 216.Sazanov L., Hinchliffe P. Structure of the hydrophilic domain of respiratory complex I from Thermus thermophilus. Science. 2006;311:1430–1436. doi: 10.1126/science.1123809. [DOI] [PubMed] [Google Scholar]
- 217.Rudolf J., Makrantoni V., Ingledew W.J., Stark M., White M.F. The DNA repair helicases XPD and FancJ have essential iron-sulfur domains. Mol. Cell. 2006;23:801–808. doi: 10.1016/j.molcel.2006.07.019. [DOI] [PubMed] [Google Scholar]
- 218.Netz D., Stith C.M., Stümpfig M., Köpf G., Vogel D., Genau H.M., Stodola J.L., Lill R., Burgers P.M.J., Pierik A.J. Eukaryotic DNA polymerases require an iron-sulfur cluster for the formation of active complexes. Nat. Chem. Biol. 2012;8:125–132. doi: 10.1038/nchembio.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yarunin A., Panse V.G., Petfalski E., Dez C., Tollervey D., Hurt E.C. Functional link between ribosome formation and biogenesis of iron–sulfur proteins. EMBO J. 2005;24:580–588. doi: 10.1038/sj.emboj.7600540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Rouault T.A. Biogenesis of iron-sulfur clusters in mammalian cells: New insights and relevance to human disease. Dis. Model. Mech. 2012;5:155–164. doi: 10.1242/dmm.009019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Braymer J.J., Freibert S.A., Rakwalska-Bange M., Lill R. Mechanistic concepts of iron-sulfur protein biogenesis in Biology. Biochim. Biophys. Acta (BBA) Bioenerg. 2020;1868:118863. doi: 10.1016/j.bbamcr.2020.118863. [DOI] [PubMed] [Google Scholar]
- 222.Paul V.D., Lill R. Biogenesis of cytosolic and nuclear iron–sulfur proteins and their role in genome stability. Biochim. Biophys. Acta (BBA) Bioenerg. 2015;1853:1528–1539. doi: 10.1016/j.bbamcr.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 223.Lill R. From the discovery to molecular understanding of cellular iron-sulfur protein biogenesis. Biol. Chem. 2020;401:855–876. doi: 10.1515/hsz-2020-0117. [DOI] [PubMed] [Google Scholar]
- 224.Rawat S., Stemmler T.L. Key Players and Their Role During Mitochondrial Iron-Sulfur Cluster Biosynthesis. Chemistry. 2011;17:746–753. doi: 10.1002/chem.201002143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ye H., Rouault T. Human iron-sulfur cluster assembly, cellular iron homeostasis, and disease. Biochemistry. 2010;49:4945–4956. doi: 10.1021/bi1004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Adam A.C., Bornhövd C., Prokisch H., Neupert W., Hell K. The Nfs1 interacting protein Isd11 has an essential role in Fe/S cluster biogenesis in mitochondria. EMBO J. 2005;25:174–183. doi: 10.1038/sj.emboj.7600905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pandey A., Golla R., Yoon H., Dancis A., Pain D. Persulfide formation on mitochondrial cysteine desulfurase: Enzyme activation by a eukaryote-specific interacting protein and Fe–S cluster synthesis. Biochem. J. 2012;448:171–187. doi: 10.1042/BJ20120951. [DOI] [PubMed] [Google Scholar]
- 228.Van Vranken J.G., Jeong M.-Y., Wei P., Chen Y.-C., Gygi S.P., Winge D.R., Rutter J. The mitochondrial acyl carrier protein (ACP) coordinates mitochondrial fatty acid synthesis with iron sulfur cluster biogenesis. eLife. 2016;5:e17828. doi: 10.7554/eLife.17828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Huttlin E.L., Ting L., Bruckner R.J., Gebreab F., Gygi M.P., Szpyt J., Tam S., Zarraga G., Colby G., Baltier K., et al. The bioplex network: A systemic exploration of the human interactome. Cell. 2015;162:425–440. doi: 10.1016/j.cell.2015.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Sheftel A.D., Stehling O., Pierik A.J., Elsasser H.-P., Muhlenhoff U., Webert H., Hobler A., Hannemann F., Bernhardt R., Lill R. Humans possess two mitochondrial ferredoxins, Fdx1 and Fdx2, with distinct roles in steroidogenesis, heme, and Fe/S cluster biosynthesis. Proc. Natl. Acad. Sci. USA. 2010;107:11775–11780. doi: 10.1073/pnas.1004250107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Shi Y., Ghosh M., Kovtunovych G., Crooks D.R., Rouault T.A. Both human ferredoxins 1 and 2 and ferredoxin reductase are important for iron-sulfur cluster biogenesis. Biochim. Biophys. Acta (BBA) Bioenerg. 2012;1823:484–492. doi: 10.1016/j.bbamcr.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Webert H., Freibert S.-A., Gallo A., Heidenreich T., Linne U., Amlacher S., Hurt E., Mühlenhoff U., Banci L., Lill R. Functional reconstitution of mitochondrial Fe/S cluster synthesis on Isu1 reveals the involvement of ferredoxin. Nat. Commun. 2014;5:5013. doi: 10.1038/ncomms6013. [DOI] [PubMed] [Google Scholar]
- 233.Shi R., Proteau A., Villarroya M.M., Moukadiri I., Zhang L., Trempe J.-F., Matte A., Armengod M.E., Cygler M. Structural basis for Fe–S cluster assembly and tRNA thiolation mediated by IscS protein–protein interactions. PLoS Biol. 2010;8:e1000354. doi: 10.1371/journal.pbio.1000354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Lin C.-W., McCabe J.W., Russell D.H., Barondeau D.P. Molecular mechanism of ISC iron–sulfur cluster biogenesis revealed by high-resolution native mass spectrometry. J. Am. Chem. Soc. 2020;142:6018–6029. doi: 10.1021/jacs.9b11454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Gervason S., Larkem D., Ben Mansour A., Botzanowski T., Müller C.S., Pecqueur L., Le Pavec G., Delaunay-Moisan A., Brun O., Agramunt J., et al. Physiologically relevant reconstitution of iron-sulfur cluster biosynthesis uncovers persulfide-processing functions of ferredoxin-2 and frataxin. Nat. Commun. 2019;10:3566. doi: 10.1038/s41467-019-11470-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Gerber J., Mühlenhoff U., Lill R. An interaction between frataxin and Isu1/Nfs1 that is crucial for Fe/S cluster synthesis on Isu1. EMBO Rep. 2003;4:906–911. doi: 10.1038/sj.embor.embor918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Colin F., Martelli A., Clémancey M., Latour J.-M., Gambarelli S., Zeppieri L., Birck C., Page A., Puccio H., de Choudens S.O. Mammalian frataxin controls sulfur production and iron entry during de novo Fe4S4 cluster assembly. J. Am. Chem. Soc. 2013;135:733–740. doi: 10.1021/ja308736e. [DOI] [PubMed] [Google Scholar]
- 238.Parent A., Elduque X., Cornu D., Belot L., Le Caer J.-P., Grandas A., Toledano M.B., D’Autréaux B. Mammalian frataxin directly enhances sulfur transfer of NFS1 persulfide to both ISCU and free thiols. Nat. Commun. 2015;6:5686. doi: 10.1038/ncomms6686. [DOI] [PubMed] [Google Scholar]
- 239.Fox N.G., Das D., Chakrabarti M., Lindahl P.A., Barondeau D.P. Frataxin accelerates [2Fe-2S] cluster formation on the human Fe–S assembly complex. Biochemistry. 2015;54:3880–3889. doi: 10.1021/bi5014497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Fox N.G., Chakrabarti M., McCormick S.P., Lindahl P.A., Barondeau D.P. The human iron–sulfur assembly complex catalyzes the synthesis of [2Fe-2S] clusters on ISCU2 that can be transferred to acceptor molecules. Biochemistry. 2015;54:3871–3879. doi: 10.1021/bi5014485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Patra S., Barondeau D.P. Mechanism of activation of the human cysteine desulfurase complex by frataxin. Proc. Natl. Acad. Sci. USA. 2019;116:19421–19430. doi: 10.1073/pnas.1909535116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Das D., Patra S., Bridwell-Rabb J., Barondeau D.P. Mechanism of frataxin “bypass” in human iron-sulfur cluster biosynthesis with implications for Friedreich’s ataxia. J. Biol. Chem. 2019;294:9276–9284. doi: 10.1074/jbc.RA119.007716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Schmucker S., Martelli A., Colin F., Page A., Wattenhofer-Donzé M., Reutenauer L., Puccio H. Mammalian frataxin: An essential function for cellular viability through an interaction with a preformed ISCU/NFS1/ISD11 iron-sulfur assembly complex. PLoS ONE. 2011;6:e16199. doi: 10.1371/journal.pone.0016199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Schmucker S., Puccio H. Understanding the molecular mechanisms of Friedreich’s ataxia to develop therapeutic approaches. Hum. Mol. Genet. 2010;19:R103–R110. doi: 10.1093/hmg/ddq165. [DOI] [PubMed] [Google Scholar]
- 245.Pastore A., Puccio H. Frataxin: A protein in search for a function. J. Neurochem. 2013;126:43–52. doi: 10.1111/jnc.12220. [DOI] [PubMed] [Google Scholar]
- 246.Adinolfi S., Iannuzzi C., Prischi F., Pastore C., Iametti S., Martin S.R., Bonomi F., Pastore A. Bacterial frataxin CyaY is the gatekeeper of iron-sulfur cluster formation catalyzed by IscS. Nat. Struct. Mol. Biol. 2009;16:390–396. doi: 10.1038/nsmb.1579. [DOI] [PubMed] [Google Scholar]
- 247.Prischi F., Konarev P., Iannuzzi C., Pastore C., Adinolfi S., Martin S.R., Svergun D.I., Pastore A. Structural bases for the interaction of frataxin with the central components of iron–sulphur cluster assembly. Nat. Commun. 2010;1:95. doi: 10.1038/ncomms1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Gakh O., Bedekovics T., Duncan S.F., Smith IV D.Y., Berkholz D.S., Isaya G. Normal and Friedreich ataxia cells express different isoforms of frataxin with complementary roles in iron-sulfur cluster assembly. J. Biol. Chem. 2010;285:38486–38501. doi: 10.1074/jbc.M110.145144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Tsai C.-L., Barondeau D. Human frataxin is an allosteric switch that activates the Fe−S cluster biosynthetic complex. Biochemistry. 2010;49:9132–9139. doi: 10.1021/bi1013062. [DOI] [PubMed] [Google Scholar]
- 250.Bridwell-Rabb J., Fox N.G., Tsai C.-L., Winn A.M., Barondeau D.P. Human frataxin activates Fe–S cluster biosynthesis by facilitating sulfur transfer chemistry. Biochemistry. 2014;53:4904–4913. doi: 10.1021/bi500532e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Yoon T., Cowan J.A. Frataxin-mediated iron delivery to ferrochelatase in the final step of heme biosynthesis. J. Biol. Chem. 2004;279:25943–25946. doi: 10.1074/jbc.C400107200. [DOI] [PubMed] [Google Scholar]
- 252.Bencze K.Z., Yoon T., Millan-Pacheco C., Bradley P.B., Pastor N., Cowan J.A., Stemmler T. Human frataxin: Iron and ferrochelatase binding surface. Chem. Commun. 2007:1798–1800. doi: 10.1039/B703195E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Cai K., Frederick R.O., Kim J.H., Reinen N.M., Tonelli M., Markley J.L. Human mitochondrial chaperone (mtHSP70) and cysteine desulfurase (NFS1) bind preferentially to the disordered conformation, whereas co-chaperone (HSC20) binds to the structured conformation of the iron-sulfur cluster scaffold protein (ISCU) J. Biol. Chem. 2013;288:28755–28770. doi: 10.1074/jbc.M113.482042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Uhrigshardt H., Singh A., Kovtunovych G., Ghosh M., Rouault T.A. Characterization of the human HSC20, an unusual DnaJ type III protein, involved in iron-sulfur cluster biogenesis. Hum. Mol. Gen. 2010;19:3816–3834. doi: 10.1093/hmg/ddq301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Angerer H., Radermacher M., Mańkowska M., Steger M., Zwicker K., Heide H., Wittig I., Brandt U., Zickermann V. The LYR protein subunit NB4M/NDUFA6 of mitochondrial complex I anchors an acyl carrier protein and is essential for catalytic activity. Proc. Natl. Acad. Sci. USA. 2014;111:5207–5212. doi: 10.1073/pnas.1322438111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Uzarska M.A., Dutkiewicz R., Freibert S.-A., Lill R., Mühlenhoff U. The mitochondrial Hsp70 chaperone Ssq1 facilitates Fe/S cluster transfer from Isu1 to Grx5 by complex formation. Mol. Biol. Cell. 2013;24:1830–1841. doi: 10.1091/mbc.e12-09-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Maio N., Singh A., Uhrigshardt H., Saxena N., Tong W.-H., Rouault T.A. Cochaperone binding to LYR motifs confers specificity of iron sulfur cluster delivery. Cell Metab. 2014;19:445–457. doi: 10.1016/j.cmet.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Sánchez E., Lobo T., Fox J.L., Zeviani M., Winge D.R., Fernández-Vizarra E. LYRM7/MZM1L is a UQCRFS1 chaperone involved in the last steps of mitochondrial Complex III assembly in human cells. Biochim. Biophys. Acta (BBA) Bioenerg. 2013;1827:285–293. doi: 10.1016/j.bbabio.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Shan Y., Cortopassi G. HSC20 interacts with frataxin and is involved in iron–sulfur cluster biogenesis and iron homeostasis. Hum. Mol. Genet. 2011;21:1457–1469. doi: 10.1093/hmg/ddr582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Weiler B.D., Brück M.-C., Kothe I., Bill E., Lill R., Mühlenhoff U. Mitochondrial [4Fe-4S] protein assembly involves reductive [2Fe-2S] cluster fusion on ISCA1–ISCA2 by electron flow from ferredoxin FDX2. Proc. Natl. Acad. Sci. USA. 2020;117:20555–20565. doi: 10.1073/pnas.2003982117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Gelling C., Dawes I.W., Richhardt N., Lill R., Mühlenhoff U. Mitochondrial Iba57p is required for Fe/S cluster formation on aconitase and activation of radical SAM enzymes. Mol. Cell. Biol. 2008;28:1851–1861. doi: 10.1128/MCB.01963-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Mühlenhoff U., Richter N., Pines O., Pierik A.J., Lill R. Specialized function of yeast Isa1 and Isa2 proteins in the maturation of mitochondrial [4Fe-4S] proteins. J. Biol. Chem. 2017;292:17979. doi: 10.1074/jbc.AAC117.000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Sheftel A.D., Wilbrecht C., Stehling O., Niggemeyer B., Elsässer H.-P., Mühlenhoff U., Lill R. The human mitochondrial ISCA1, ISCA2, and IBA57 proteins are required for [4Fe-4S] protein maturation. Mol. Biol. Cell. 2012;23:1157–1166. doi: 10.1091/mbc.e11-09-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kim K.-D., Chung W.-H., Kim H.-J., Lee K.-C., Roe J.-H. Monothiol glutaredoxin Grx5 interacts with Fe–S scaffold proteins Isa1 and Isa2 and supports Fe–S assembly and DNA integrity in mitochondria of fission yeast. Biochem. Biophys. Res. Commun. 2010;392:467–472. doi: 10.1016/j.bbrc.2010.01.051. [DOI] [PubMed] [Google Scholar]
- 265.Sheftel A.D., Stehling O., Pierik A.J., Netz D.J.A., Kerscher S., Elsässer H.-P., Wittig I., Balk J., Brandt U., Lill R. Human Ind1, an iron-sulfur cluster assembly factor for respiratory complex I. Mol. Cell. Biol. 2009;29:6059–6073. doi: 10.1128/MCB.00817-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Beilschmidt L.K., Puccio H.M. Mammalian Fe–S cluster biogenesis and its implication in disease. Biochimie. 2014;100:48–60. doi: 10.1016/j.biochi.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 267.Cameron J., Janer A., Levandovskiy V., Mackay N., Rouault T.A., Tong W.-H., Ogilvie I., Shoubridge E.A., Robinson B.H. Mutations in iron-sulfur cluster scaffold genes NFU1 and BOLA3 cause a fatal deficiency of mutliple respiratory chain and 2-oxoacid dehydrogenase enzymes. Am. J. Hum. Gen. 2011;89:486–495. doi: 10.1016/j.ajhg.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Uzarska M.A., Nasta V., Weiler B.D., Spantgar F., Ciofi-Baffoni S., Saviello M.R., Gonnelli L., Mühlenhoff U., Banci L., Lill R. Author response: Mitochondrial Bol1 and Bol3 function as assembly factors for specific iron-sulfur proteins. eLife. 2016;5:e16673. doi: 10.7554/eLife.16673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Melber A., Na U., Vashisht A., Weiler B.D., Lill R., Wohlschlegel J.A., Winge D.R. Author response: Role of Nfu1 and Bol3 in iron-sulfur cluster transfer to mitochondrial clients. eLife. 2016;5:e15991. doi: 10.7554/eLife.15991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Pandey A.K., Pain J., Dancis A., Pain D. Mitochondria export iron–sulfur and sulfur intermediates to the cytoplasm for iron–sulfur cluster assembly and tRNA thiolation in yeast. J. Biol. Chem. 2019;294:9489–9502. doi: 10.1074/jbc.RA119.008600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Mesecke N., Terziyska N., Kozany C., Baumann F., Neupert W., Hell K., Herrmann J.M. A disulfide relay system in the intermembrane space of mitochondria that mediates protein import. Cell. 2005;121:1059–1069. doi: 10.1016/j.cell.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 272.Qi W., Li J., Cowan J.A. A structural model for glutathione-complexed iron–sulfur cluster as a substrate for ABCB7-type transporters. Chem. Commun. 2014;50:3795–3798. doi: 10.1039/C3CC48239A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Kispal G., Csere P., Guiard B., Lill R. The ABC transporter Atm1p is required for mitochondrial iron homeostasis. FEBS Lett. 1997;418:346–350. doi: 10.1016/S0014-5793(97)01414-2. [DOI] [PubMed] [Google Scholar]
- 274.Pondarre C., Campagna D.R., Antiochos B., Sikorski L., Mulhern H., Fleming M. Abcb7, the gene responsible for X-linked sideroblastic anemia with ataxia, is essential for hematopoiesis. Blood. 2006;109:3567–3569. doi: 10.1182/blood-2006-04-015768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Boultwood J., Pellagatti A., Nikpour M., Pushkaran B., Fidler C., Cattan H., Littlewood T.J., Malcovati L., Della Porta M.G., Jädersten M., et al. The role of the iron transporter ABCB7 in refractory anemia with ring sideroblasts. PLoS ONE. 2008;3:e1970. doi: 10.1371/journal.pone.0001970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Cavadini P., Biasiotto G., Poli M., Levi S., Verardi R., Zanella I., Derosas M., Ingrassia R., Corrado M., Arosio P. RNA silencing of the mitochondrial ABCB7 transporter in HeLa cells causes an iron-deficient phenotype with mitochondrial iron overload. Blood. 2006;109:3552–3559. doi: 10.1182/blood-2006-08-041632. [DOI] [PubMed] [Google Scholar]
- 277.Pondarré C., Antiochos B.B., Campagna D.R., Clarke S.L., Greer E., Deck K.M., McDonald A., Han A.-P., Medlock A., Kutok J.L., et al. The mitochondrial ATP-binding cassette transporter Abcb7 is essential in mice and participates in cytosolic iron–sulfur cluster biogenesis. Hum. Mol. Genet. 2006;15:953–964. doi: 10.1093/hmg/ddl012. [DOI] [PubMed] [Google Scholar]
- 278.Galluhn D., Langer T. Reversible assembly of the ATP-binding cassette transporter Mdl1 with the F1F0-ATP synthase in mitochondria. J. Biol. Chem. 2004;279:38338–38345. doi: 10.1074/jbc.M405871200. [DOI] [PubMed] [Google Scholar]
- 279.Young L., Leonhard K., Tatsuta T., Trowsdale J., Langer T. Role of the ABC Transporter Mdl1 in peptide export from mitochondria. Science. 2001;291:2135–2138. doi: 10.1126/science.1056957. [DOI] [PubMed] [Google Scholar]
- 280.Chloupková M., LeBard L.S., Koeller D.M. MDL1 is a high copy suppressor of ATM1: Evidence for a role in resistance to oxidative stress. J. Mol. Biol. 2003;331:155–165. doi: 10.1016/S0022-2836(03)00666-1. [DOI] [PubMed] [Google Scholar]
- 281.Poulos T. Heme enzyme structure and function. Chem. Rev. 2014;114:3919–3962. doi: 10.1021/cr400415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Mosure S.A., Strutzenberg T.S., Shang J., Munoz-Tello P., Solt L.A., Griffin P.R., Kojetin D.J. Structural basis for heme-dependent NCoR binding to the transcriptional repressor REV-ERBβ. Sci. Adv. 2021;7:eabc6479. doi: 10.1126/sciadv.abc6479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Piel R., III, Dailey H.A., Jr., Medlock A.E. The mitochondrial heme metabolon: Insights into the complex(ity) of heme synthesis and distribution. Mol. Gen. Metab. 2019;128:198–203. doi: 10.1016/j.ymgme.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Celis A., DuBois J.L. Making and breaking heme. Curr. Opin. Struct. Biol. 2019;59:19–28. doi: 10.1016/j.sbi.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Hamza I., Dailey H.A. One ring to rule them all: Trafficking of heme and heme synthesis intermediates in the metazoans. Biochim. Biophys. Acta (BBA) Bioenerg. 2012;1823:1617–1632. doi: 10.1016/j.bbamcr.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Phillips J.D. Heme biosynthesis and the porphyrias. Mol. Genet. Metab. 2019;128:164–177. doi: 10.1016/j.ymgme.2019.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Medlock A.E., Shiferaw M.T., Marcero J.R., Vashisht A.A., Wohlschlegel J.A., Phillips J.D., Dailey H.A. Identification of the mitochondrial heme metabolism complex. PLoS ONE. 2015;10:e0135896. doi: 10.1371/journal.pone.0135896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Martinez-Guzman O., Willoughby M.M., Saini A., Dietz J.V., Bohovych I., Medlock A.E., Khalimonchuk O., Reddi A.R. Mitochondrial-nuclear heme trafficking in budding yeast is regulated by GTPases that control mitochondrial dynamics and ER contact sites. J. Cell Sci. 2020;133:jcs237917. doi: 10.1242/jcs.237917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Kranz R.G., Richard-Fogal C., Taylor J.-S., Frawley E.R. Cytochrome c biogenesis: Mechanisms for covalent modifications and trafficking of heme and for heme-iron redox control. Microbiol. Mol. Biol. Rev. 2009;73:510–528. doi: 10.1128/MMBR.00001-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Babbitt S.E., Francisco B.S., Mendez D.L., Lukat-Rodgers G.S., Rodgers K.R., Bretsnyder E.C., Kranz R.G. Mechanisms of mitochondrial holocytochrome c synthase and the key roles played by cysteines and histidine of the heme attachment site, Cys-XX-Cys-His. J. Biol. Chem. 2014;289:28795–28807. doi: 10.1074/jbc.M114.593509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Babbitt S.E., Sutherland M., Francisco B.S., Mendez D.L., Kranz R.G. Mitochondrial cytochrome c biogenesis: No longer an enigma. Trends Biochem. Sci. 2015;40:446–455. doi: 10.1016/j.tibs.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Bernard D.G., Gabilly S.T., Dujardin G., Merchant S., Hamel P.P. Overlapping specificities of the mitochondrial cytochrome c and c1 heme lyases. J. Biol. Chem. 2003;278:49732–49742. doi: 10.1074/jbc.M308881200. [DOI] [PubMed] [Google Scholar]
- 293.Khalimonchuk O., Bestwick M., Meunier B., Watts T.C., Winge D.R. Formation of the redox cofactor centers during Cox1 maturation in yeast cytochrome oxidase. Mol. Cell. Biol. 2010;30:1004–1017. doi: 10.1128/MCB.00640-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Khalimonchuk O., Kim H., Watts T., Perez-Martinez X., Winge D.R. Oligomerization of heme o Synthase in Cytochrome Oxidase Biogenesis Is Mediated by Cytochrome Oxidase Assembly Factor Coa2. J. Biol. Chem. 2012;287:26715–26726. doi: 10.1074/jbc.M112.377200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Timón-Gómez A., Nývltová E., Abriata L.A., Vila A., Hosler J., Barrientos A. Mitochondrial cytochrome c oxidase biogenesis: Recent developments. Semin. Cell Dev. Biol. 2018;76:163–178. doi: 10.1016/j.semcdb.2017.08.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Bareth B., Dennerlein S., Mick D., Nikolov M., Urlaub H., Rehling P. The heme a synthase Cox15 associates with cytochrome c oxidase assembly intermediates during Cox1 maturation. Mol. Cell. Biol. 2013;33:4128–4137. doi: 10.1128/MCB.00747-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Bundschuh F.A., Hannappel A., Anderka O., Ludwig B. Surf1, associated with leigh syndrome in humans, is a heme-binding protein in bacterial oxidase biogenesis. J. Biol. Chem. 2009;284:25735–25741. doi: 10.1074/jbc.M109.040295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Bestwick M., Khalimonchuk O., Pierrel F., Winge D.R. The role of Coa2 in hemylation of yeast Cox1 revealed by its genetic interaction with Cox10. Mol. Cell. Biol. 2010;30:172–185. doi: 10.1128/MCB.00869-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Bestwick M., Jeong M.-Y., Khalimonchuk O., Kim H., Winge D.R. Analysis of leigh syndrome mutations in the yeast SURF1 homolog reveals a new member of the cytochrome oxidase assembly factor family. Mol. Cell. Biol. 2010;30:4480–4491. doi: 10.1128/MCB.00228-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Zhu Z., Yao J., Johns T., Fu K., De Bie I., Macmillan C., Cuthbert A.P., Newbold R.F., Wang J.-C., Chevrette M., et al. SURF1, encoding a factor involved in the biogenesis of cytochrome c oxidase, is mutated in Leigh syndrome. Nat. Genet. 1998;20:337–343. doi: 10.1038/3804. [DOI] [PubMed] [Google Scholar]
- 301.Pierrel F., Khalimonchuk O., Cobine P., Bestwick M., Winge D.R. Coa2 is an assembly factor for yeast cytochrome c oxidase biogenesis that facilitates the maturation of Cox1. Mol. Cell. Biol. 2008;28:4927–4939. doi: 10.1128/MCB.00057-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Hannappel A., Bundschuh F.A., Ludwig B. Role of Surf1 in heme recruitment for bacterial COX biogenesis. Biochim. Biophys. Acta (BBA) Bioenerg. 2012;1817:928–937. doi: 10.1016/j.bbabio.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 303.Li L., Kaplan J. Characterization of two homologous yeast genes that encode mitochondrial iron transporters. J. Biol. Chem. 1997;272:28485–28493. doi: 10.1074/jbc.272.45.28485. [DOI] [PubMed] [Google Scholar]
- 304.Li L., Miao R., Jia X., Ward D.M., Kaplan J. Expression of the yeast cation diffusion facilitators Mmt1 and Mmt2 affects mitochondrial and cellular iron homeostasis: Evidence for mitochondrial iron export. J. Biol. Chem. 2014;289:17132–17141. doi: 10.1074/jbc.M114.574723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Luk E., Carroll M., Baker M., Culotta V.C. Manganese activation of superoxide dismutase 2 in Saccharomyces cerevisiae requires MTM1, a member of the mitochondrial carrier family. Proc. Natl. Acad. Sci. USA. 2003;100:10353–10357. doi: 10.1073/pnas.1632471100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Naranuntarat A., Jensen A., Pazicni S., Penner-Hahn J.E., Culotta V.C. The interaction of mitochondrial iron with manganese superoxide dismutase. J. Biol. Chem. 2009;284:22633–22640. doi: 10.1074/jbc.M109.026773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Yang M., Cobine P., Molik S., Naranuntarat A., Lill R., Winge D.R., Culotta V.C. The effects of mitochondrial iron homeostasis on cofactor specificity of superoxide dismutase 2. EMBO J. 2006;25:1775–1783. doi: 10.1038/sj.emboj.7601064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Nilsson R., Schultz I.J., Pierce E.L., Soltis K.A., Naranuntarat A., Ward D.M., Baughman J.M., Paradkar P.N., Kingsley P.D., Culotta V.C., et al. Discovery of genes essential for heme biosynthesis through large-scale gene expression analysis. Cell Metab. 2009;10:119–130. doi: 10.1016/j.cmet.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Galmozzi A., Kok B., Kim A., Montenegro-Burke J.R., Lee J., Spreafico R., Mosure S., Albert V., Cintron-Colon R., Godio C., et al. PGRMC2 is an intracellular haem chaperone critical for adipocyte function. Nature. 2019;576:138–142. doi: 10.1038/s41586-019-1774-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Poston C.N., Duong E., Cao Y., Bazemore-Walker C.R. Proteomic analysis of lipid raft-enriched membranes isolated from internal organelles. Biochem. Biophys. Res. Commun. 2011;415:355–360. doi: 10.1016/j.bbrc.2011.10.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Cho I., Adelmant G., Lim Y., Marto J.A., Cho G., Golden J.A. Ascorbate peroxidase proximity labeling coupled with biochemical fractionation identifies promoters of ER-mitochondrial contacts. J. Biol. Chem. 2017;292:16382–16392. doi: 10.1074/jbc.M117.795286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Schumann U., Subramani S. Special delivery from mitochondria to peroxisomes. Trends Cell Biol. 2008;18:253–256. doi: 10.1016/j.tcb.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Sugiura A., McLelland G.-L., Fon E.A., McBride H.M. A new pathway for mitochondrial quality control: Mitochondrial-derived vesicles. EMBO J. 2014;33:2142–2156. doi: 10.15252/embj.201488104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Hughes A.L., Hughes C.E., Henderson K.A., Yazvenko N., Gottschling D.E. Author response: Selective sorting and destruction of mitochondrial membrane proteins in aged yeast. eLife. 2016;5:e13943. doi: 10.7554/eLife.13943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Neuspiel M., Schauss A.C., Braschi E., Zunino R., Rippstein P., Rachubinski R.A., Andrade M., McBride H.M. Cargo-selected transport from the mitochondria to peroxisomes is mediated by vesicular carriers. Curr. Biol. 2008;18:102–108. doi: 10.1016/j.cub.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 316.Vasam G., Nadeau R., Cadete V.J.J., Lavallée-Adam M., Menzies K.J., Burelle Y. Proteomics characterization of mitochondrial-derived vesicles under oxidative stress. FASEB J. 2021;35:e21278. doi: 10.1096/fj.202002151R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Chiabrando D., Marro S., Mercurio S., Giorgi C., Petrillo S., Vinchi F., Fiorito V., Fagoonee S., Camporeale A., Turco E., et al. The mitochondrial heme exporter FLVCR1b mediates erythroid differentiation. J. Clin. Investig. 2012;122:4569–4579. doi: 10.1172/JCI62422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Khan A.A., Quigley J.G. Heme and FLVCR-related transporter families SLC48 and SLC49. Mol. Asp. Med. 2013;34:669–682. doi: 10.1016/j.mam.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Korolnek T., Zhang J., Beardsley S., Scheffer G.L., Hamza I. Control of metazoan heme homeostasis by a conserved multidrug resistance protein. Cell Metab. 2014;19:1008–1019. doi: 10.1016/j.cmet.2014.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Taylor E.B., Rutter J. Mitochondrial quality control by the ubiquitin–proteasome system. Biochem. Soc. Trans. 2011;39:1509–1513. doi: 10.1042/BST0391509. [DOI] [PubMed] [Google Scholar]
- 321.Keel S.B., Doty R.T., Yang Z., Quigley J.G., Chen J., Knoblaugh S., Kingsley P.D., De Domenico I., Vaughn M.B., Kaplan J., et al. A heme export protein is required for red blood cell differentiation and iron homeostasis. Science. 2008;319:825–828. doi: 10.1126/science.1151133. [DOI] [PubMed] [Google Scholar]
- 322.Quigley J., Yang Z., Worthington M.T., Phillips J.D., Sabo K.M., Sabath D.E., Berg C.L., Sassa S., Wood B.L., Abkowitz J.L. Identification of a human heme exporter that is essential for erythropoiesis. Cell. 2004;118:757–766. doi: 10.1016/j.cell.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 323.Rajagopal A., Rao A.U., Amigo J., Tian M., Upadhyay S.K., Hall C., Uhm S., Mathew M.K., Fleming M., Paw B., et al. Haem homeostasis is regulated by the conserved and concerted functions of HRG-1 proteins. Nature. 2008;453:1127–1131. doi: 10.1038/nature06934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.White C., Yuan X., Schmidt P.J., Bresciani E., Samuel T.K., Campagna D., Hall C., Bishop K., Calicchio M.L., Lapierre A., et al. HRG1 is essential for heme transport from the phagolysosome of macrophages during erythrophagocytosis. Cell Metab. 2013;17:261–270. doi: 10.1016/j.cmet.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Lill R., Freibert S.A. Mechanisms of mitochondrial iron-sulfur protein biogenesis. Ann. Rev. Biochem. 2020;89:471–499. doi: 10.1146/annurev-biochem-013118-111540. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.