Abstract
Canine hepatozoonosis caused by Hepatozoon canis is an emerging disease in Europe. Clinical pictures vary from subclinical to life-threatening and non-specific clinical signs are predominantly reported. A 2-month-old female puppy originating from Southern Italy was adopted and moved to Northern Italy. Then, the dog was brought to a local veterinary practice for gastrointestinal signs, migrating lameness and pruritic dermatitis, and then tested positive for Hepatozoon spp. gamonts at the blood smear. After treatment with imidocarb dipropionate and doxycycline, the dog showed an initial clinical improvement. However, gastrointestinal signs recurred, and diffuse superficial pyoderma appeared on the thoracolumbar region, along with fever, lethargy, and weight loss. Eight months from the first onset of clinical signs, the dog was referred to a veterinary clinic and subjected to complete blood count, urine and fecal analysis, along with abdominal ultrasonography, whole-body CT and gastroduodenal endoscopy. Skin biopsies and blood samples were subjected to a PCR-coupled sequencing protocol, which scored both positive for H. canis. Alterations were consistent with a pre-existing cholangiohepatitis and multiple acquired extrahepatic shunts secondary to portal hypertension. The dog was euthanatized due to a clinical worsening two months later. The potential role of H. canis in the systemic disease observed, clinic-pathological findings and epizootiological implications are discussed.
Keywords: Hepatozoon canis, dog, skin, liver
1. Introduction
Hepatozoonosis is an emerging vector borne disease (VBD) of both dogs and cats, caused by different species belonging to the genus Hepatozoon [1,2]. Canine hepatozoonosis is caused by Hepatozoon canis that infects dogs worldwide, and Hepatozoon americanum that has been reported, to date, only in the Americas [1,3,4,5]. Dogs are intermediate hosts of Hepatozoon spp. and become infected via the ingestion of infected ticks (definitive hosts) harboring mature oocysts. The sporozoites released in the intestine penetrate the gut wall and reach, via lymphatic and blood circulation the target organs, i.e., bone marrow, spleen, lymph nodes, liver, kidney and lungs, where the merogony occurs [1]. The micromerozoites released from mature meronts invade the neutrophils and monocytes, where they mature into gamonts. Ticks become then infected ingesting gamonts contained in the leukocytes during a blood meal on a parasitaemic vertebrate [1].
In Europe, the main vector of H. canis is the brown dog tick Rhipicephalus sanguineus in which it is transmitted transstadially [5,6,7]. Although the ingestion of an infected tick is the most common source of infection, transplacental transmission and carnivorism have been reported as alternative routes [1,8].
Clinical pictures range from subclinical to severe signs, and non-specific clinical signs, e.g., lethargy, anorexia, weight loss, lymphadenopathy and fever are predominant, while life-threatening conditions may occur in (i) dogs co-infected by other vector-borne pathogens (e.g., Ehrlichia spp., Anaplasma spp., Leishmania infantum, Babesia canis), (ii) immunocompromised animals and (iii) puppies [1,9,10,11]. Skeletal pain, sub-acute periostitis, gastrointestinal and respiratory signs, oral, skin and ocular lesions (i.e., glaucoma and uveitis) have been associated with H. canis [1,12,13,14,15]. The most common hematobiochemical alterations are non-specific, i.e., anemia, thrombocytopenia, leukocytosis, hyperproteinaemia with polyclonal hyperglobulinaemia and hypoalbuminaemia, increased creatine kinase, and alkaline phosphatase activities [1,16]. Post-mortem findings include pneumonia, hepatitis, and glomerulonephritis [1].
Given the emergence of canine hepatozoonosis in European regions [5,17], knowledge on its epidemiology and clinical features should be implemented. The present report describes a fatal systemic disease in a young dog infected with H. canis. Epizootiological and clinic-pathological implications are discussed.
2. Case Details
2.1. Clinical Case
2.1.1. Visit 1 (2 Months Old)
A 2 month old female mixed-breed puppy originating from Southern Italy was adopted and moved to Northern Italy. The dog received prophylactic treatment for ectoparasites with afoxolaner 5 mg/kg PO and it was regularly vaccinated. Then, the puppy was brought to visit to a local veterinary practice for the onset of diarrhea, vomiting, migrating lameness, and skin lesions that appeared as crusted lesion. The latter were localized mainly in the dorsal portions of the neck and thorax. The animal was initially subjected to complete blood count (CBC), to the evaluation of basal cortisol concentration and to abdominal ultrasonography, along with a fine needle aspiration of the spleen. The dog was also tested for antibodies towards Ehrlichia canis/Ehrlichia ewingii, Anaplasma phagocytophilum/Anaplasma platys, Borrelia burgdorferi and antigens of Dirofilaria immitis using SNAP 4Dx® (IDEXX) and for L. infantum antibodies (IFAT). Hepatozoon spp. gamonts were detected at the blood smear and the dog was treated with doxycycline (10 mg/kg SID PO) and imidocarb dipropionate (6 mg/kg) every two weeks, until negativization of the blood smear [18].
2.1.2. Visit 2 (5 Months Old)
After an initial improvement, diarrhea and vomiting recurred 3 months later and diffuse superficial pyoderma appeared on the thoracolumbar region, along with fever, lethargy, and weight loss. The dog was subjected to complete haemato-biochemical examination, to copromicroscopic analyses (i.e., Baermann test, floatation, and SNAP Giardia®-IDEXX), and to cutaneous biopsies. The dog was then treated with cefazoline (20 mg/kg q8 EV) for skin lesions and subjected to several diet trials.
2.1.3. Visit 3 (10 Months Old)
After a new initial improvement, 4 months later the clinical pictures worsened again with the onset of anorexia, diarrhea, and vomiting. Then, the animal was referred to a veterinary clinic in Bologna, Italy, and it was again subjected to complete haemato-biochemical examination, urine analysis, coagulation test, pre-/post-prandial bile acids test, leptospirosis MAP test, to a further L. infantum IFAT, abdominal ultrasonography, whole-body CT, gastrointestinal endoscopy with hepatic, gastric, duodenal, and cutaneous biopsies. Skin biopsies and blood samples were subjected to a PCR-coupled sequencing protocol for Hepatozoon spp. [19,20]. The dog was treated with maropitant (1 mg/kg) SID orally, S-adenosil methionine 200 mg SID orally, co-amoxiclav 20 mg/kg BID orally, Ursodeoxycholic acid 10 mg/kg SID orally, Vitamin B12 500 mcg SC once every 7 days. The clinical conditions of the dog continued to worsen (i.e., lethargy, anorexia, and ascites) and it was euthanized 2 months later.
2.2. Findings of the Exams Performed at 2 Months Old
The haemato-biochemical exam showed a mild neutrophilic leukocytosis, mild microcytic normochromic anemia, the basal cortisol was mildly increased (Table 1). The dog tested negative to SNAP 4Dx® and to L. infantum antibodies. The fine needle aspiration of the spleen showed an extramedullary hemopoiesis with occasionally neutrophils phagocyting parasite stage compatible with Hepatozoon spp.
Table 1.
Altered values of the haemato-biochemical, urine and coagulation analyses performed on Visit 1 (2 months old), Visit 2 (5 months old) and Visit 3 (10 months old).
| Analyte | Value | Normal Range | Units |
|---|---|---|---|
| Visit 1 | |||
| HCT | 34 | 37–55 | % |
| WBC | 17.75 | 6–17 | 109/L |
| Neutrophils | 14.60 | 3–12 | 109/L |
| Basal cortisol | 9.76 | 1–5 | mcg/dL |
| Visit 2 | |||
| HCT | 36.9 | 37–55 | % |
| WBC | 14.68 | 6–17 | 109/L |
| Neutrophils | 12.61 | 3–12 | 109/L |
| Total protein | 5.3 | 5.5–7.6 | g/dL |
| Visit 3 | |||
| HCT | 41.2 | 37–55 | % |
| Platelets | 489 × 109 | 103–395 | mcL |
| Albumin | 2.01 | 2.4–3.8 | g/dL |
| Total protein | 5.3 | 5.5–7.6 | g/dL |
| Cobalamin | <150 | 251–908 | ng/L |
| Folates | 6.60 | 7.7–24 | mcg/L |
| ALP | 875 | 20–120 | IU/L |
| ALT | 475 | 15–64 | IU/L |
| AST | 166 | 12–54 | IU/L |
| TLI | >50 | 5.2–35 | mcg/L |
| Total iron | 69 | 76–173 | mcg/dL |
| Pre-prandial bile acids | 53.55 | 0–22 | μmol/L |
| Post-prandial bile acids | 97.47 | 0–30 | μmol/L |
| Bilirubinuria | 1 | <1 | mg/dL |
| Urobilinogen | 4 | <1 | mg/dL |
| aPTT | 108 | 75–105 | sec |
2.3. Findings of the Exams Performed at 5 Months Old
The haemato-biochemical showed a mild microcytic normochromic anemia, mild hypoproteinemia (Table 1), while the remaining chemistry was unremarkable, copromicroscopic exams and SNAP Giardia® were negative. Biopsy of the skin showed a perivascular dermatitis and pyoderma with intralesional bacteria.
2.4. Findings of the Exams Performed at 10 Months Old
The results of the exams repeated 5 months later showed moderate thrombocytosis, moderate hypoalbuminemia, mild hypoproteinemia, severe hypocobalaminaemia, mildly decreased folates, severely increased ALT and ALP, moderately increased AST, markedly increased canine TLI, and moderately increased pre- and post-prandial bile acids. Bilirubinuria and urobilinogen were detected in the urine analysis. Mildly increased aPTT was found at the coagulation test (Table 1). The leptospirosis MAP test was negative. The dog was still negative for L. infantum antibodies at IFAT.
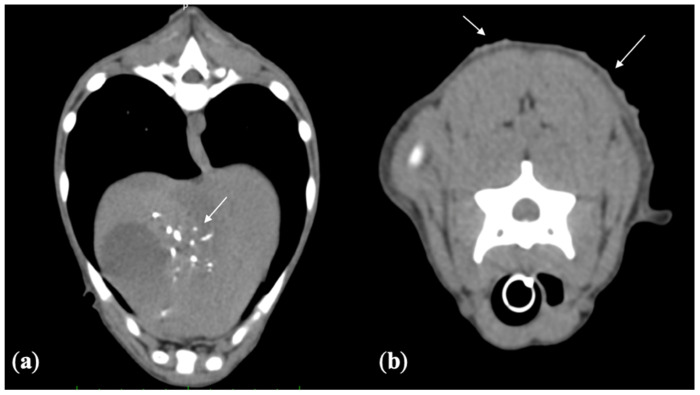
2.4.1. Computed Tomography
The whole-body CT examination was taken with a multidetector CT (Optima 540 GE, Milwaukee; WI, USA), and showed multiple mineralizations at the level of the intrahepatic ducts with concurrent dilation of the common bile duct. A severe thickening of the duodenum, most likely consistent with a pre-existing cholangiohepatitis, was detected. Diffuse irregularity and hyperdense areas on the skin were compatible with diffuse dermatitis (Figure 1). Multiple acquired extra hepatic shunts secondary to portal hypertension were also observed.
Figure 1.
(a) Pre-contrast transverse CT image. Multiple mineralization in the biliary ducts (white arrow). (b) Pre-contrast transverse CT image. In the dorsal portion of the skin a diffuse irregularity and hyperdense areas (white arrows) are evident.
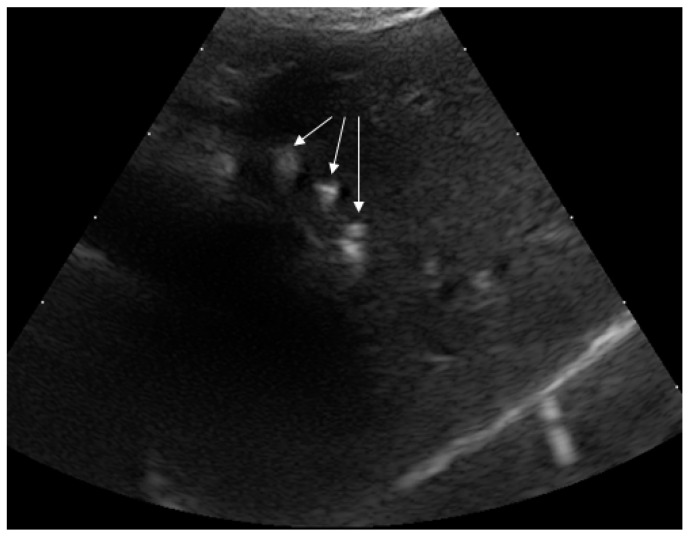
2.4.2. Ultrasound (US)
After the CT study an US-guided biopsy of the liver was carried out (MyLab Eight, Esaote SpA, Genoa, Italy) with no complications. The US examination, despite not complete, showed mineralization (Figure 2) of the liver lobes, as well as other findings seen in CT.
Figure 2.
The US examination taken as a guide for the liver biopsy showed mineralizations within the liver parenchyma, most likely quadrate lobe (white arrows).
2.4.3. Endoscopy
Gastroduodenoscopy showed gastric mucosal hyperemia and irregular mucosa of the duodenum, with squat and fused villi alternating with normal areas. Biopsies from the stomach and duodenum were taken for histopathological examination.
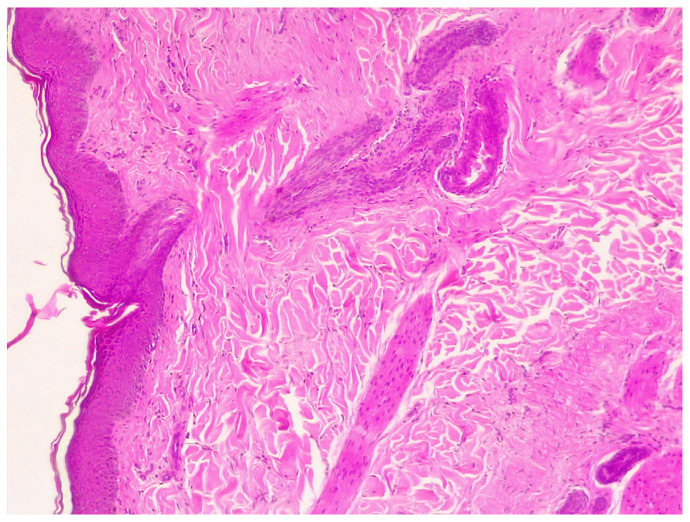
2.4.4. Histopathology
Liver histopathology revealed hypoplasia and hyperplasia of hepatic veins and arterioles, respectively. Gastric biopsy showed a mild lympho-plasmacellular gastritis while in the duodenum biopsy a mild lympho-plasmacellular duodenitis with fibrosis was observed. Skin biopsy revealed hyperplastic dermatitis. The epidermis had moderate acanthosis and small numbers of inflammatory cells in the superficial dermis, composed of neutrophils, lymphocytes, and few plasma cells (Figure 3). In one biopsy a fragmented intracorneal pustule was observed, with large numbers of degenerate neutrophils surrounded by lamellar keratin. The process was interpreted as superficial pyoderma.
Figure 3.
Skin histopathology: the epidermis showed moderate acanthosis and small numbers of inflammatory cells in the superficial dermis, composed by neutrophils, lymphocytes, and few plasma cells.
2.4.5. Molecular Analysis
Skin biopsy and blood samples were subjected to DNA extraction using commercial kits, i.e., Exgene Blood extraction kit and Exgene Tissue extraction kit (GeneAll Biotech, Seoul, South Korea), respectively, following the manufacturer’s instructions. A fragment of ~373 bp of the18S rRNA gene of Hepatozoon spp. was amplified using specific primers [19]. PCR reactions were carried out carried out in a 25 μL reaction mixture containing 2 μL of genomic DNA, 12.5 μL of Ready Mix REDTaq (Sigma, St. Louis, MO, USA), and 0.25 μL of each corresponding primer (50 μM). PCRs were performed in a thermal cycler (2700; Applied Biosystems, Foster City, CA, USA,) as previously described [21].
PCR Amplicons were sequenced for a species diagnosis. A convenient dataset (i.e., around 50% of the amplicons, with high quality and quantity of the PCR products) was purified using a QIAquick® Gel Extraction Kit (Qiagen, GmbH, Hilden, Germany) and sequenced by a commercial laboratory (BMR-Genomics, Padova, Italy). Sequences were determined in both strands, aligned, and compared with those available in GenBank using the Basic Local Alignment Search Tool (BLAST: https://blast.ncbi.nlm.nih.gov/Blast, accessed on 5 April 2021), confirming the identity of H. canis both in the skin and blood samples.
3. Discussion
The present case report suggests a potential role of H. canis in a systemic disease in a puppy, adding possible new clinical knowledge on canine hepatozoonosis. To date, mostly subclinical H. canis infections have been reported in dogs and the severity of the disease has been correlated with the degree of the parasitaemia [22,23,24]. Most clinical signs herein detected fit with those previously reported, i.e., lethargy, fever, anorexia, weight loss, and gastrointestinal signs [1,12]. Though lameness is usually associated with H. americanum infection, this study and other findings suggest that a skeletal involvement could be more frequent than thought in dogs infected with H. canis [1,13].
Skin alterations are an uncommon finding in canine hepatozoonosis due to H. canis, as they have been reported only in few case reports [15,16,25]. In the one reported in New Jersey, the dog showed a raised, pruritic, alopecic, subcutaneous fluctuant swelling (2 cm in diameter) containing H. canis gamonts as the only alteration [15]. In this report, the skin lesions of the dog cannot be ultimately correlated to H. canis, as intralesional gamonts were not microscopically observed. Nevertheless, the exclusion of other causes (e.g., ectoparasites infestation, food/environment allergies, hepatocutaneous syndrome) and the detection of H. canis DNA in situ suggest the involvement of this protozoan in the pathogenesis of the skin lesions.
The laboratory findings were similar to those reported in previous H. canis infections. Mild normochromic anaemia is the most common laboratory finding [1,11,16] while higher leukocyte counts usually correspond to a higher parasitemia [1]. However, the lack of specificity of these alterations does not allow to attribute them unequivocally to H. canis.
The increased pre- and post-prandial bile acids level were consistent with portal systemic shunts, highlighted via the CT exam. Liver abnormalities were attributed to a pre-existing hepatic disease, as no parasitic stages were detected at the liver histopathological examination. Portal hypertension associated with H. canis has never been reported, though the merogony of H. canis occurs in the liver, and chronic hepatitis related to the presence of schizonts has been reported [18,26]. Thus, the role of H. canis in contributing to a pre-existing cholangiohepatitis, the portal hypertension, and/or its role in the worsening of a non-related hepatic disease cannot be definitively excluded.
With all likelihood, the 2-month-old dog of the present case acquired the infection via transplacental transmission, given the early onset of clinical signs. To date, no data is available on the possible effects of H. canis on the fetal development and in the pathogenesis of possible acquired hepatic disorders; thus, knowledge on vertically transmitted infections should be implemented.
Relapsing of clinical signs and/or failure of the therapeutic treatment have been frequently described in dogs with hepatozoonosis [27]. The negativization of the blood smear may be an inefficient criterion for the evaluation of treatment response and the follow up should be performed using molecular techniques [27,28]. The therapeutic management of canine hepatozoonisis is challenging as no drug is labelled for the treatment of canine hepatozoonosis in Europe and a lack of negativization has been observed also after prolonged off-label treatments [18]. New studies aiming at setting up adequate therapeutic guidelines are here advocated.
The relocation of dogs is one main driver fostering the emergence of vector-borne diseases, including hepatozoonosis, in previously free areas [17,29,30]. Accordingly, the dog of the present report was adopted from southern Italy, i.e., an endemic area for H. canis [5,28,31], and moved to an area of Northern Italy where this protozoan had never been described thus far. The uncontrolled movement of potentially infected dogs can be dangerous as R. sanguineus, the main vector of H. canis, is widespread in Northern Italy and in general in Europe, and present all year around [32,33]. Thus, improving the awareness on VBDs, including hepatozoonosis and the establishment of appropriate control programs (e.g., for animals moving from or to endemic areas) are pivotal to appropriately manage and control the spreading of the disease [34]. Regular and adequate prophylactic treatments are, in fact, often overlooked by owners. Thus, veterinarians should educate them on the correct management of dogs in terms of adequate timing, schedule and spectrum of action of products available on the market [34].
4. Conclusions
The role of H. canis in the systemic disease herein described is plausible as (i) skin lesions have been previously described in canine hepatozoonosis, (ii) pre-natal hepatic alterations due to a vertical transmission of H. canis can be considered and call for purposed investigations, and (iii) H. canis might have contributed to the worsening of a pre-existing hepatic disease not related to the infection. The pathogenic mechanisms elicited by H. canis should be further studied, with a particular focus on the vertical transmission route and its potential implications on the health of young animals, in which the infection is often more severe than in adult dogs.
Author Contributions
Conceptualization, M.V.; methodology, A.D.B., R.T., B.B.; validation, M.V.; investigation A.D.B., R.T., B.B., M.C., S.M., M.G.; formal analysis, M.C., S.M., M.G.; data curation, A.D.B., R.T., B.B.; writing—original draft preparation, A.D.B., M.C.; writing—review and editing, M.V.; visualization, M.V.; supervision, M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The dog of the present case report was sampled in the framework of clinical procedures performed by his examining veterinarian for health reasons. No additional samples were taken for mere research scopes.
Informed Consent Statement
No samples were taken from the dog of this study for mere research scopes. A written consent to publish the study was signed by the owner of the dog.
Data Availability Statement
All the data generated are described in the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baneth G. Perspectives on canine and feline hepatozoonosis. Vet. Parasitol. 2011;181:3–11. doi: 10.1016/j.vetpar.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Morelli S., Diakou A., Traversa D., Di Gennaro E., Simonato G., Colombo M., Dimzas D., Grillini M., Frangipane di Regalbono A., Beugnet F., et al. First record of Hepatozoon spp. in domestic cats in Greece. Ticks Tick-Borne Dis. 2021;12:101580. doi: 10.1016/j.ttbdis.2020.101580. [DOI] [PubMed] [Google Scholar]
- 3.Amoli A.R., Khoshnegah J., Razmi G. A preliminary parasitological survey of Hepatozoon spp. infection in dogs in Mashhad, Iran. Iran. J. Parasitol. 2012;7:99. [PMC free article] [PubMed] [Google Scholar]
- 4.Guo W.P., Xie G.C., Xue Z.Q., Yu J.J., Jian R., Du L.Y., Li Y.N. Molecular detection of Hepatozoon canis in dogs and ticks in Shaanxi province, China. Comp. Immunol. Microbiol. Infect. Dis. 2020;72:101514. doi: 10.1016/j.cimid.2020.101514. [DOI] [PubMed] [Google Scholar]
- 5.Pacifico L., Braff J., Buono F., Beall M., Neola B., Buch J., Sgroi G., Piantedosi D., Santoro M., Tyrrell P., et al. Hepatozoon canis in hunting dogs from Southern Italy: Distribution and risk factors. Parasitol. Res. 2020;119:3023–3031. doi: 10.1007/s00436-020-06820-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giannelli A., Ramos R.A., Di Paola G., Mencke N., Dantas-Torres F., Baneth G., Otranto D. Transstadial transmission of Hepatozoon canis from larvae to nymphs of Rhipicephalus sanguineus. Vet. Parasitol. 2013;196:1–5. doi: 10.1016/j.vetpar.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Aktas M., Özübek S. Transstadial Transmission of Hepatozoon canis by Rhipicephalus sanguineus (Acari: Ixodidae) in Field Conditions. J. Med. Entomol. 2017;54:1044–1048. doi: 10.1093/jme/tjx050. [DOI] [PubMed] [Google Scholar]
- 8.Murata T., Inoue M., Tateyama S., Taura Y., Nakama S. Vertical transmission of Hepatozoon canis in dogs. J. Vet. Med. Sci. 1993;55:867–868. doi: 10.1292/jvms.55.867. [DOI] [PubMed] [Google Scholar]
- 9.Sasanelli M., Paradies P., Lubas G., Otranto D., de Caprariis D. Atypical clinical presentation of coinfection with Ehrlichia, Babesia and Hepatozoon species in a dog. Vet. Rec. 2009;164:22–23. doi: 10.1136/vr.164.1.22. [DOI] [PubMed] [Google Scholar]
- 10.Kruzeniski S.J., Tam F.M., Burgess H.J. Pathology in Practice. J. Am. Vet. Med. Assoc. 2013;243:1705–1707. doi: 10.2460/javma.243.12.1705. [DOI] [PubMed] [Google Scholar]
- 11.Kwon S.J., Kim Y.H., Oh H.H., Choi U.S. First Case of Canine Infection with Hepatozoon canis (Apicomplexa: Haemogregarinidae) in the Republic of Korea. Korean J. Parasitol. 2017;55:561–564. doi: 10.3347/kjp.2017.55.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker J.L., Craig T.M., Barton C.L., Scott D.W. Hepatozoon canis in a dog with oral pyogranulomas and neurologic disease. Cornell Vet. 1988;7:179–183. [PubMed] [Google Scholar]
- 13.Marchetti V., Lubas G., Baneth G., Modenato M., Mancianti F. Hepatozoonosis in a dog with skeletal involvement and meningoencephalomyelitis. Vet. Clin. Pathol. 2009;38:121–125. doi: 10.1111/j.1939-165X.2008.00080.x. [DOI] [PubMed] [Google Scholar]
- 14.Acevedo T.S.P., Ramírez L.M., Restrepo R.L.G. Uveitis and glaucoma associated with Hepatozoon canis infection: A case report. Rev. Colomb. Cienc. Pecu. 2010;23:485–491. [Google Scholar]
- 15.Little L., Baneth G. Cutaneous Hepatozoon canis infection in a dog from New Jersey. J. Vet. Diagn. Investig. 2011;23:585–588. doi: 10.1177/1040638711404156. [DOI] [PubMed] [Google Scholar]
- 16.Voyvoda H., Pasa S., Uner A. Clinical Hepatozoon canis infection in a dog in Turkey. J. Small Anim. Pract. 2004;45:613–617. doi: 10.1111/j.1748-5827.2004.tb00184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Attipa C., Maguire D., Solano-Gallego L., Szladovits B., Barker E.N., Farr A., Baneth G., Tasker S. Hepatozoon canis in three imported dogs: A new tickborne disease reaching the United Kingdom. Vet. Rec. 2018;183:716. doi: 10.1136/vr.105087. [DOI] [PubMed] [Google Scholar]
- 18.Baneth G., Weigler B. Retrospective case-control study of hepatozoonosis in dogs in Israel. J. Vet. Int. Med. 1997;11:365–376. doi: 10.1111/j.1939-1676.1997.tb00482.x. [DOI] [PubMed] [Google Scholar]
- 19.Tabar M.D., Altet L., Francino O., Sánchez A., Ferrer L., Roura X. Vector-borne infections in cats: Molecular study in Barcelona area (Spain) Vet. Parasitol. 2008;15:332–336. doi: 10.1016/j.vetpar.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 20.Prakash B.K., Low V.L., Tan T.K., Vinnie-Siow W.Y., Lim Y.A.L., Morvarid A.R., Azman A.S., Yeong Y.S., AbuBakar S., Sofian-Azirun M. Detection of Hepatozoon canis in the brown dog tick and domestic dogs in Peninsular Malaysia. J. Med. Entomol. 2018;55:1346–1348. doi: 10.1093/jme/tjy081. [DOI] [PubMed] [Google Scholar]
- 21.Díaz-Regañón D., Villaescusa A., Ayllón T., Rodríguez-Franco F., Baneth G., Calleja-Bueno L., García-Sancho M., Agulla B., Sainz Á. Molecular detection of Hepatozoon spp. and Cytauxzoon sp. in domestic and stray cats from Madrid, Spain. Parasites Vectors. 2017;10:1–9. doi: 10.1186/s13071-017-2056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gavazza A., Bizzeti M., Papini R. Observations on dogs found naturally infected with Hepatozoon canis in Italy. Rev. Méd. Vét. 2003;154:565–571. [Google Scholar]
- 23.Karagenc T.I., Pasa S., Kirli G., Hosgor M., Bilgic H.B., Ozon Y.H., Atasoy A., Eren H. A parasitological, molecular and serological survey of Hepatozoon canis infection in dogs around the Aegean coast of Turkey. Vet. Parasitol. 2006;135:113–119. doi: 10.1016/j.vetpar.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Skeldon N., Klaassen J., Hinds M. Diagnosis of Hepatozoon canis. Vet. Rec. 2017;180:124. doi: 10.1136/vr.j549. [DOI] [PubMed] [Google Scholar]
- 25.Hubert B., Beaufils J.P., Fabbrini F., Magnol J.P. Hepatozoon canis, a fortuitous or pathogenic agent in canine dermatology: A review of three cases. Vet. Dermatol. 2002;13:211–229. doi: 10.1046/j.1365-3164.2002.00298_24.x. [DOI] [Google Scholar]
- 26.Duscher G.G., Kübber-Heiss A., Richter B., Suchentrunk F. A golden jackal (Canis aureus) from Austria bearing Hepatozoon canis-import due to immigration into a non-endemic area? Ticks Tick-Borne Dis. 2013;4:133–137. doi: 10.1016/j.ttbdis.2012.10.040. [DOI] [PubMed] [Google Scholar]
- 27.Sasanelli M., Paradies P., Greco B., Eyal O., Zaza V., Baneth G. Failure of imidocarb dipropionate to eliminate Hepatozoon canis in naturally infected dogs based on parasitological and molecular evaluation methods. Vet. Parasitol. 2010;171:194–199. doi: 10.1016/j.vetpar.2010.03.042. [DOI] [PubMed] [Google Scholar]
- 28.Otranto D., Dantas-Torres F., Weigl S., Latrofa M.S., Stanneck D., Decaprariis D., Capelli G., Baneth G. Diagnosis of Hepatozoon canis in young dogs by cytology and PCR. Parasites Vectors. 2011;4:55. doi: 10.1186/1756-3305-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson N. Hepatozoon canis: Another unwelcome parasitic visitor to the UK. Vet. Rec. 2018;183:714. doi: 10.1136/vr.k5215. [DOI] [PubMed] [Google Scholar]
- 30.Wright I., Jongejan F., Marcondes M., Peregrine A., Baneth G., Bourdeau P., Bowman D.D., Breitschwerdt E.B., Capelli G., Carodo L., et al. Parasites and vector-borne diseases disseminated by rehomed dogs. Parasites Vectors. 2020;13:546. doi: 10.1186/s13071-020-04407-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dantas-Torres F., Latrofa M.S., Weigl S., Tarallo V.D., Lia R.P., Otranto D. Hepatozoon canis infection in ticks during spring and summer in Italy. Parasitol. Res. 2012;110:695–698. doi: 10.1007/s00436-011-2544-8. [DOI] [PubMed] [Google Scholar]
- 32.Maurelli M.P., Pepe P., Colombo L., Armstrong R., Battisti E., Morgoglione M.E., Counturis D., Rinaldi L., Cringoli G., Ferroglio E., et al. A national survey of Ixodidae ticks on privately owned dogs in Italy. Parasites Vectors. 2018;11:420. doi: 10.1186/s13071-018-2994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.European Center for Disease Prevention and Control. [(accessed on 1 August 2021)]. Available online: https://www.ecdc.europa.eu/en/publications-data/rhipicephalus-sanguineus-current-known-distribution-january-2018.
- 34.Colombo M., Morelli S., Simonato G., Di Cesare A., Veronesi F., Frangipane di Regalbono A., Grassi L., Russi I., Tiscar P.G., Morganti G., et al. Exposure to Major Vector-Borne Diseases in Dogs Subjected to Different Preventative Regimens in Endemic Areas of Italy. Pathogens. 2021;10:507. doi: 10.3390/pathogens10050507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data generated are described in the paper.