Abstract
Purpose
Dementia is an important health issue in Korea due to its associated medical costs. Our study aimed to estimate the prevalence of dementia in Korea by analyzing hospital utilization rates.
Materials and Methods
We examined National Health Insurance data from 2008 to 2016 and identified all dementia cases. Crude and ageand sex-standardized prevalence were calculated. A generalized linear mixed model was used to estimate prevalence ratios.
Results
We identified 176746 and 530269 dementia cases in 2008 and 2016, respectively. Alzheimer's disease was the most common dementia subtype (65.4% and 86.1% in 2008 and 2016, respectively). Across all age groups, the prevalence of dementia increased consistently: the increase was prominent among patients ≥85 years of age. Among patients ≥65 years of age, crude prevalence was estimated at 31.3 and 72.2 per 1000 population in 2008 and 2016, respectively. Age- and sex-standardized prevalence increased from 31.3 to 62.0 per 1000 population between 2008 and 2016, respectively. The prevalence ratio for dementia in 2016 was 2.02 times (95% confidence interval, 2.01–2.03) higher than that in 2008. When adjusted for age, dementia was more prevalent among females. The most common comorbidity was hypertension, followed by diabetes and stroke.
Conclusion
Our results demonstrated that hospital utilization for dementia increased significantly from 2008 to 2016, reflecting a proportional increase in the prevalence of dementia. Korean healthcare policy must prioritize dementia treatment.
Keywords: Dementia prevalence, National Health Insurance, claims data, standardized prevalence
INTRODUCTION
Dementia is defined as a loss of memory and cognitive function that results in a decline in the activities of daily living and is a social and economic burden on patients, families, and the government.1,2,3 Dementia is commonly attributed to Alzheimer's disease (AD) (25%–75%), vascular dementia (20%–30%), frontotemporal dementia, and dementia with Lewy bodies (<5%).4 Patients with dementia commonly have more than one comorbidity, which significantly impacts the treatment for dementia itself and overall quality of life.5 According to the World Alzheimer Report 2018, dementia affects as many as 50 million people worldwide. This number is estimated to increase to 82 million by 2030 and to almost triple to 152 million by 2050.1,6 However, individual studies on the prevalence of this condition have reported conflicting results; the prevalence of dementia is stable in some studies and increasing or decreasing in others.7,8,9,10,11,12,13
The burden of dementia on daily life and financial costs is well-known. The average year lived with disability is 7.4 years, which ranks dementia as the second most difficult chronic disease.14 Caregivers spend an average of 3.6 and 2.6 hours per day assisting patients with activities of daily living and caring for the patient, respectively.15 As such, dementia represents a significant health burden and should be a high priority in health policy.
Korea will become an aged society (20.8% of the population ≥65 years) by 2026.16 It has taken Korea 17 years for the proportion of the population >65 years of age to increase from 7% to 14%, whereas the same increase took France and Japan 115 and 24 years, respectively.17 The Korean Ministry of Health and Welfare estimated that the prevalence of dementia will be 15% in 2050.18 The Nationwide Survey on Dementia Epidemiology of Korea (NaSDEK) was conducted in 2008, 2012, and 2016 to investigate the epidemiologic characteristics of dementia and to estimate its prevalence. These cross-sectional studies determined that the prevalence of dementia was 8.1% and 9.5% in 2008 and 2016, respectively, and showed an increasing trend.19,20,21 Until recently, only a few studies have examined the prevalence of and hospital utilization for dementia.22,23,24,25 It can, however, be difficult to conduct interview or questionnaire-based cross-sectional studies on dementia, because cognitive functional decline and/or memory impairment in these patients may influence the quality of the data on epidemiologic characteristics, comorbidities, and medication utilized.
The National Health Insurance System (NHIS) of Korea requires data on the admitting diagnosis and comorbidities of patients who make insurance claims. In this study, we analyzed the prevalence of dementia between 2008 and 2016 based on NHIS claims data for dementia.
MATERIALS AND METHODS
Study design and population
We collected 2008–2016 hospital utilization data from the Health Insurance Review & Assessment (HIRA) database. The claims database contains information on the date of visit; demographic characteristics; main and sub-diagnosis codes during out-patient, admission, or emergency care; medication history; and patient expenditures. All patients who visited a hospital for dementia were included in our study.
Using the International Classification of Diseases 10th Revision (ICD-10) code, patients with dementia were classified as follows: 1) AD (F00, G30.0, G30.1, G30.8, G30.9), 2) vascular dementia (F01), 3) other (F02, G31.0, A81.0) and unclassified dementia (F03, G31.82). Comorbidities were identified based on hospital utilization for hypertension (I10–15), cardiovascular disease (I20–25), diabetes (E10–14), and stroke (G45–46, I60–64, I67–69). Patients who visited an out-patient clinic or were admitted for dementia and/or a comorbidity more than once each calendar year were defined as dementia cases and dementia cases with comorbidity, respectively. Patients were classified according to their main and sub-diagnostic codes.
This study was approved by the Institutional Review Boards of Yonsei University Health System (2018-0418-001) and HIRA Service, which waived the requirement for informed consent.
Statistical analysis
Dementia cases were stratified by age (< 60, 60–64, 65–69, 70–74, 75–79, 80–84, ≥85) and sex. Crude prevalence was estimated using the mid-year populations for each year, which were derived from population census data. Age- and/or sex-standardized prevalence from 2008 to 2016 was estimated using midyear population data for 2008. Prevalence and 95% confidence interval (CI) were estimated using Proc STDRATE in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). A log normal distribution was used to estimate 95% CIs. Subgroup analyses were performed for age and sex.
Differences in the prevalence of dementia during the study period were estimated using a generalized linear model with log binomial distribution. We analyzed de-identified claims data from the HIRA system. All statistical analyses were performed with SAS version 9.4 (SAS Institute Inc.).
RESULTS
We identified 176746 dementia cases in 2008; this number increased continuously over the course of the study period (Table 1). Hospital utilization for dementia was more prevalent among female patients, especially among those who were 70–79 years of age, particularly between 2008 and 2012. Female patients ≥85 years of age comprised a significant majority of the insurance claims after 2013. Among patients ≥85 years of age, hospital utilization for dementia was 4.3 times higher in 2016 than that in 2008. The most common dementia subtype was AD, and the most common comorbidity was hypertension. The proportion of patients with diabetes increased continuously from 31.6% to 37.0% from 2008 to 2016, respectively, whereas the proportion of patients with stroke followed a decreasing trend (Table 2).
Table 1. General Characteristics of Dementia Cases from 2008 to 2016.
| 2008 (n=176746) |
2009 (n=217323) |
2010 (n=262271) |
2011 (n=309893) |
2012 (n=353179) |
2013 (n=395858) |
2014 (n=436149) |
2015 (n=481609) |
2016 (n=530269) |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | ||||||||||
| <60 years | 9244 (5.2) | 10476 (4.8) | 11621 (4.4) | 12170 (3.9) | 12719 (3.6) | 12929 (3.3) | 13263 (3.0) | 13429 (2.8) | 13904 (2.6) | |
| 60–64 years | 8419 (4.8) | 9832 (4.5) | 11574 (4.4) | 12911 (4.2) | 13193 (3.7) | 13592 (3.4) | 13557 (3.1) | 14210 (3.0) | 15422 (2.9) | |
| 65–69 years | 19564 (11.1) | 22681 (10.4) | 25258 (9.6) | 27060 (8.7) | 27511 (7.8) | 26829 (6.8) | 27896 (6.4) | 29642 (6.2) | 31593 (6.0) | |
| 70–74 years | 31879 (18.0) | 38772 (17.8) | 44967 (17.1) | 51427 (16.6) | 56993 (16.1) | 62570 (15.8) | 64850 (14.9) | 66328 (13.8) | 66858 (12.6) | |
| 75–79 years | 39734 (22.5) | 48824 (22.5) | 59289 (22.6) | 71008 (22.9) | 82389 (23.3) | 92554 (23.4) | 101426 (23.3) | 110303 (22.9) | 117293 (22.1) | |
| 80–84 years | 35447 (20.1) | 44855 (20.6) | 56476 (21.5) | 68958 (22.3) | 80926 (22.9) | 92883 (23.5) | 104707 (24.0) | 119019 (24.7) | 136354 (25.7) | |
| ≥85 years | 32459 (18.4) | 41883 (19.3) | 53086 (20.2) | 66359 (21.4) | 79448 (22.5) | 94501 (23.9) | 110450 (25.3) | 128678 (26.7) | 148845 (28.1) | |
| Sex | ||||||||||
| Male | 54318 (30.7) | 65998 (30.4) | 78872 (30.1) | 90938 (29.3) | 101865 (28.8) | 113071 (28.6) | 123992 (28.4) | 136920 (28.4) | 150785 (28.4) | |
| Female | 122428 (69.3) | 151325 (69.6) | 183399 (69.9) | 218955 (70.7) | 251314 (71.2) | 282787 (71.4) | 312157 (71.6) | 344689 (71.6) | 379484 (71.6) | |
| Dementia subtype* | ||||||||||
| Alzheimer's | 115521 (65.4) | 147305 (67.8) | 179155 (68.3) | 217067 (70.0) | 263177 (74.5) | 306563 (77.4) | 346117 (79.4) | 401925 (83.5) | 456358 (86.1) | |
| Vascular | 26623 (15.1) | 32304 (14.9) | 37724 (14.4) | 43667 (14.1) | 46071 (13.0) | 46699 (11.8) | 49225 (11.3) | 52660 (10.9) | 56306 (10.6) | |
| Others | 59680 (33.8) | 65853 (30.3) | 80576 (30.7) | 93406 (30.1) | 96542 (27.3) | 94169 (23.8) | 96014 (22.0) | 91179 (18.9) | 70422 (13.3) | |
The values in parentheses are percentages.
*Percentages may add up to more than 100% due to multiple diagnoses in the same patient.
Table 2. Comorbidities of Dementia Cases from 2008 to 2016.
| Comorbidity | 2008 (n=176746) |
2009 (n=217323) |
2010 (n=262271) |
2011 (n=309893) |
2012 (n=353179) |
2013 (n=395858) |
2014 (n=436149) |
2015 (n=481609) |
2016 (n=530269) |
|---|---|---|---|---|---|---|---|---|---|
| Hypertension | 112593 (63.7) | 139248 (64.1) | 169363 (64.6) | 200241 (64.6) | 232515 (65.8) | 263157 (66.5) | 291584 (66.9) | 323178 (67.1) | 358281 (67.6) |
| Cardiovascular disease | 30102 (17.0) | 37298 (17.2) | 44397 (16.9) | 50914 (16.4) | 59002 (16.7) | 67236 (17.0) | 77468 (17.8) | 86417 (17.9) | 95076 (17.9) |
| Diabetes | 55914 (31.6) | 69766 (32.1) | 85240 (32.5) | 102307 (33.0) | 120258 (34.1) | 137512 (34.7) | 154158 (35.3) | 174583 (36.2) | 196158 (37.0) |
| Stroke | 79807 (45.2) | 96071 (44.2) | 114005 (43.5) | 129124 (41.7) | 142456 (40.3) | 155665 (39.3) | 168241 (38.6) | 182436 (37.9) | 198687 (37.5) |
The values in parentheses are percentages. Percentages may add up to more than 100% due to multiple diagnoses in the same patient.
Age- and sex-standardized prevalence increased statistically significantly by 1.34 times (0.39 vs. 0.54 per 1000 population in 2008 and 2016, respectively) and 2.02 times (31.28 vs. 61.98 per 1000 population in 2008 and 2016, respectively) in patients under <65 years and ≥65 years of age, respectively (Table 3). After stratifying the cases according to sex, the age-standardized prevalence increased across all age groups. Among males ≥65 years of age, the age-standardized prevalence increased from 22.1 to 39.8 per 1000 population from 2008 to 2016, respectively (Table 4). Among females ≥65 years of age, the agestandardized prevalence increased from 37.4 to 77.0 per 1000 population from 2008 to 2016, respectively. Among males <65 years of age, the age-standardized prevalence increased from 0.39 to 0.52 per 1000 population from 2008 to 2016, respectively, whereas females <65 years of age showed a similar increase from 0.40 to 0.56 per 1000 population from 2008 to 2016, respectively. After 2011, the prevalence of dementia was significantly higher in females (Supplementary Table 1, only online).
Table 3. Crude and Standardized Prevalence of Dementia per 1000 Population from 2008 to 2016.
| Year | <65 years | ≥65 years | ||||
|---|---|---|---|---|---|---|
| Crude | Standardized* | Prevalence ratio† | Crude | Standardized* | Prevalence ratio† | |
| 2008 | 0.39 (0.39–0.4) | 0.39 (0.39–0.4) | Reference | 31.28 (31.12–31.43) | 31.28 (61.81–62.15) | Reference |
| 2009 | 0.45 (0.45–0.46) | 0.44 (0.44–0.45) | 1.13 (1.1–1.15) | 37.27 (37.1–37.43) | 36.52 (59.2–59.55) | 1.17 (1.16–1.17) |
| 2010 | 0.52 (0.51–0.52) | 0.49 (0.49–0.5) | 1.26 (1.23–1.28) | 43.88 (43.7–44.05) | 42.01 (56.39–56.74) | 1.34 (1.33–1.35) |
| 2011 | 0.55 (0.55–0.56) | 0.53 (0.52–0.53) | 1.34 (1.32–1.37) | 50.46 (50.27–50.64) | 47.38 (54.06–54.41) | 1.51 (1.5–1.52) |
| 2012 | 0.57 (0.57–0.58) | 0.53 (0.53–0.54) | 1.36 (1.33–1.38) | 55.26 (55.07–55.45) | 51.05 (50.88–51.23) | 1.64 (1.63–1.65) |
| 2013 | 0.59 (0.58–0.59) | 0.54 (0.53–0.55) | 1.37 (1.34–1.40) | 59.64 (59.45–59.83) | 54.23 (54.06–54.41) | 1.75 (1.74–1.76) |
| 2014 | 0.59 (0.59–0.6) | 0.53 (0.53–0.54) | 1.35 (1.32–1.37) | 63.34 (63.14–63.53) | 56.56 (56.39–56.74) | 1.83 (1.82–1.84) |
| 2015 | 0.61 (0.6–0.62) | 0.53 (0.52–0.53) | 1.32 (1.30–1.35) | 67.56 (67.37–67.76) | 59.38 (59.2–59.55) | 1.93 (1.92–1.94) |
| 2016 | 0.65 (0.64–0.65) | 0.54 (0.53–0.54) | 1.34 (1.32–1.37) | 72.18 (71.98–72.38) | 61.98 (61.81–62.15) | 2.02 (2.01–2.03) |
The values in parentheses are the 95% confidence intervals.
*For estimation of age- and sex-standardized prevalence, the mid-year population number of 2008 was used, †Age- and sex-standardized prevalence ratios used a log binomial linear mixed model.
Table 4. Age-Standardized Prevalence of Dementia per 1000 Population from 2008 to 2016 Analyzed according to Sex among Patients ≥65 Years of Age.
| Year | Male | Female | Female-to-male prevalence ratio† | ||||
|---|---|---|---|---|---|---|---|
| Crude | Standardized* | Prevalence ratio† | Crude | Standardized* | Prevalence ratio† | ||
| 2008 | 22.1 (21.94–22.35) | 22.1 (21.9–22.35) | Reference | 37.4 (37.22–37.65) | 37.4 (37.22–37.65) | Reference | 1.37 (1.35–1.38) |
| 2009 | 26.1 (25.89–26.33) | 25.5 (25.32–25.75) | 1.15 (1.14–1.17) | 44.9 (44.62–45.09) | 43.9 (43.71–44.17) | 1.17 (1.16–1.18) | 1.39 (1.37–1.40) |
| 2010 | 30.4 (30.17–30.63) | 29.1 (28.87–29.31) | 1.31 (1.30–1.33) | 53.1 (52.86–53.36) | 50.7 (50.48–50.96) | 1.35 (1.34–1.36) | 1.40 (1.38–1.41) |
| 2011 | 34.1 (33.82–34.29) | 32.0 (31.76–32.21) | 1.44 (1.43–1.46) | 61.8 (61.55–62.08) | 57.8 (57.52–58.02) | 1.54 (1.53–1.55) | 1.44 (1.43–1.45) |
| 2012 | 36.7 (36.43–36.91) | 33.8 (33.58–34.02) | 1.53 (1.51–1.55) | 68.3 (68.03–68.58) | 62.7 (62.43–62.94) | 1.68 (1.67–1.69) | 1.46 (1.45–1.48) |
| 2013 | 39.0 (38.79–39.27) | 35.4 (35.15–35.59) | 1.61 (1.59–1.63) | 74.3 (74.01–74.57) | 67.0 (66.7–67.21) | 1.80 (1.79–1.81) | 1.48 (1.47–1.49) |
| 2014 | 41.0 (40.80–41.29) | 36.5 (36.31–36.75) | 1.66 (1.64–1.68) | 79.4 (79.08–79.65) | 70.1 (69.82–70.33) | 1.89 (1.88–1.91) | 1.50 (1.49–1.51) |
| 2015 | 43.7 (43.48–43.96) | 38.3 (38.11–38.54) | 1.75 (1.73–1.76) | 84.9 (84.59–85.17) | 73.6 (73.32–73.83) | 2.00 (1.98–2.01) | 1.50 (1.49–1.51) |
| 2016 | 46.5 (46.23–46.72) | 39.8 (39.56–39.99) | 1.81 (1.80–1.83) | 91.0 (90.71–91.3) | 77.0 (76.71–77.21) | 2.11 (2.09–2.12) | 1.50 (1.49–1.51) |
The values in parentheses are the 95% confidence intervals.
*For estimation of age-standardized prevalence, the mid-year population of 2008 was used, †Age-adjusted prevalence ratio.
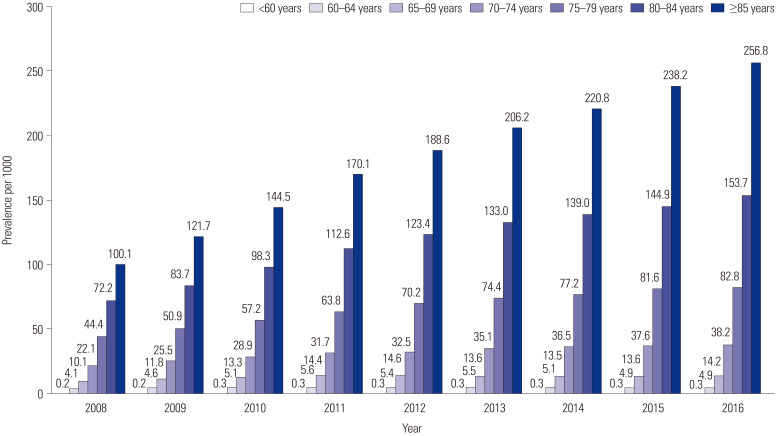
Fig. 1 shows the sex-standardized prevalence according to age group. Although sex-standardized prevalence increased across all age groups, a prominent increase in prevalence was observed in patients ≥70 years of age. In both male and female patients, the prevalence of dementia increased across all age groups over time. The highest increase was observed in the group ≥85 years of age (Supplementary Table 2, only online). Across age groups, females showed a higher prevalence of dementia, except among patients <60 years of age.
Fig. 1. Sex-standardized prevalence of dementia per 1000 population from 2008 to 2016 analyzed according to age group.
DISCUSSION
Our study demonstrated that the number of patients with dementia in Korea tripled from 176746 to 530269 from 2008 to 2016. The age- and sex-standardized prevalence of dementia among patients ≥65 years of age increased from 3.13% to 6.2% from 2008 to 2016, respectively.
According to the World Alzheimer Report 2018, North Africa/Middle East and Latin America had the highest prevalence of standardized dementia among patients ≥60 years of age at 8.7% and 8.4%, respectively. In contrast, Central Europe had the lowest prevalence at 4.7%. All other regions had prevalence rates between 5.6%–7.6%.26 Further, while the data from these studies show mixed results,27 data from high-income countries like Germany, the United States, Spain, and England have high-lighted stable10 or declining 11,12,13 rates, respectively.
Although age plays a role in the prevalence of dementia, our findings showed that the prevalence of dementia in Korea was lower than that in other countries. Both our data and the NaSDEK data demonstrated an increasing trend in the prevalence of dementia in Korea. However, when we compared study findings, our prevalence were lower than those in the NaSDEK study, especially for the year 2008.18,21 Interestingly, while there was a difference in the prevalence of dementia between our study and the NaSDEK (e.g., 2008: 1.0% vs. 3.6% among patients 65–69 years of age and 2.2% vs. 5.2% among patients 70–74 years of age), the prevalence estimates for these same age groups among <75 years of age were exactly the same in 2016 (1.4% and 3.8% among patients 65–69 and 70–74 years of age, respectively). Nevertheless, the difference in prevalence persisted among patients ≥75 years of age in 2016 (8.3% vs. 11.9%, 15.4% vs. 21.1%, and 25.7% vs. 38.4% among patients aged 75–79, 80–84, ≥85 years of age, respectively). Overall, our study demonstrated a lower prevalence of dementia than NaSDEK.21
Because we used health insurance claims data, patients with dementia who did not visit a hospital may have been excluded from our prevalence estimation. The prevalence of dementia may be underestimated in situations where there is a low social interest in dementia screening and treatment. In our study, the rapid increase in prevalence (14% average annual increase) and discrepancies in dementia prevalence between the NaSDEK study and our study may be caused by hospital underutilization, especially during the early study period. While there is a strong push towards improving dementia coverage and improving the quality of life of patients with dementia, our study strongly suggests that hospital underutilization for dementia still exists, particularly among patients ≥75 years of age.
In our study, the most common dementia subtype was AD, followed by vascular dementia and other dementias. Consistent with other studies,18,28 the proportion of AD continuously increased from 65.4% to 86.1% from 2008 to 2016, whereas the proportion of vascular dementia decreased from 15.1% to 10.6%. Throughout the study period, dementia was also more prevalent in females. This corroborates other studies that have reported that the prevalence of dementia is 19–29% higher in females than in males.6,26,29
Dementia commonly occurs with other comorbidities. Comorbidities, such as hypertension, diabetes, and cerebrovascular disease, can exacerbate the progression of dementia, particularly in terms of cognitive decline. Dementia also adversely affects the quality of care, treatment, and prognosis of these comorbidities.30,31 As such, it is necessary to actively screen for and manage comorbidities to delay the progression of disability from dementia. A previous study in Korea that used hospital-based registry data also demonstrated that 48.9% and 22.3% of 1786 patients with AD had hypertension and diabetes, respectively.32 A recent study in Taiwan reported that the proportion of subjects with at least three comorbidities was higher in individuals with cognitive impairment (mild cognitive impairement 20.9%, dementia 27.2%) than in those with normal cognition (15.6%).33 The same study also identified hypertension and diabetes as the most common comorbidities of dementia. Our results agreed with their data in that hypertension was the most common comorbidity (63.7% and 67.6% in 2008 and 2016, respectively), followed by diabetes and stroke. The prevalence of diabetes increased from 31.6% to 37.0% from 2008 to 2016, respectively, whereas the prevalence of stroke decreased over the same period. This finding coincides with a decreasing trend in stroke in Korea.34
Our study is the first to estimate the prevalence of dementia and its comorbidities using NIH claims data; however, our study has some limitations. First, the prevalence estimated in this study may be underestimated because claims data are collected for cost calculation and reimbursement rather than disease surveillance. As such, patients who did not visit medical institutions to seek care for dementia were not included in our calculations. This is especially important for the earlier time periods of our study, when hospital utilization for dementia was likely lower. However, our data eventually matched the data published in a national epidemiological survey, which may be due to active screening and treatment of dementia in later years. In 2011, the Korean government passed a dementia management law, established dementia centers in all communities, and launched a mandatory dementia screening program. These might have affected the hospital utilization for dementia. In the future, longitudinal claims data may allow for more accurate prevalence estimates. Second, our study may have misclassified dementia cases and their subtypes.35 We defined dementia cases as patients who visited medical institutions more than once each calendar year. Thus, classification of dementia and its subtype was likely to be inaccurate, and the results might be biased.
In conclusion, our study demonstrated that the prevalence of dementia in Korea increased significantly from 2008 to 2016. Enhanced programs that screen and treat dementia and its associated comorbidities are necessary to prevent dementia progression and to improve the overall quality of care. In addition, although limitations exist, our study suggested that claims data may be utilized to estimate the prevalence of dementia. Because claims data cover the entire population of Korea, the data may be a valuable research tool for tracking trends in dementia prevalence and its subtypes.
ACKNOWLEDGEMENTS
This study was performed in collaboration with the Big Data Research division at the Health Insurance Review & Assessment Service.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yoon Jung Choi, Young Jae Hwang, and Changsoo Kim.
- Data curation: Yoon Jung Choi, Sanghyun Kim, and Changsoo Kim.
- Formal analysis: Yoon Jung Choi, Sanghyun Kim, and Changsoo Kim.
- Funding acquisition: Changsoo Kim.
- Investigation: Yoon Jung Choi and Changsoo Kim.
- Methodology: Yoon Jung Choi, Young Jae Hwang, and Changsoo Kim.
- Project administration: Sanghyun Kim and Changsoo Kim.
- Resources: Yoon Jung Choi, Sanghyun Kim, and Changsoo Kim.
- Software: Sanghyun Kim and Changsoo Kim.
- Supervision: Young Jae Hwang and Changsoo Kim.
- Validation: Young Jae Hwang and Changsoo Kim.
- Visualization: Yoon Jung Choi, Young Jae Hwang, and Changsoo Kim.
- Writing—original draft: Yoon Jung Choi, Young Jae Hwang, and Changsoo Kim.
- Writing—review & editing: Yoon Jung Choi, Young Jae Hwang, and Changsoo Kim.
- Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIALS
Age-Standardized Prevalence of Dementia per 1000 Population from 2008 to 2016 Analyzed according to Sex among Patients <65 Years of Age
Prevalence of Dementia per 1000 Population from 2008 to 2016 according to Age and Sex
References
- 1.Alzheimer's Disease International. World Alzheimer report 2018. The state of the art of dementia research: new frontiers. [accessed on 2021 May 20]. Available at: https://www.alzint.org/resource/world-alzheimer-report-2018/
- 2.Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 3.Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, Huang Y, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. doi: 10.1016/S0140-6736(09)61829-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer's disease: an analysis of population-based data. Lancet Neurol. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- 5.Savva GM, Stephan BC Alzheimer's Society Vascular Dementia Systematic Review Group. Epidemiological studies of the effect of stroke on incident dementia: a systematic review. Stroke. 2010;41:e41–e46. doi: 10.1161/STROKEAHA.109.559880. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Dementia [Internet] [accessed on 2021 May 20]. Available at: https://www.who.int/news-room/fact-sheets/detail/dementia.
- 7.Sekita A, Ninomiya T, Tanizaki Y, Doi Y, Hata J, Yonemoto K, et al. Trends in prevalence of Alzheimer's disease and vascular dementia in a Japanese community: the Hisayama Study. Acta Psychiatr Scand. 2010;122:319–325. doi: 10.1111/j.1600-0447.2010.01587.x. [DOI] [PubMed] [Google Scholar]
- 8.Jacklin KM, Walker JD, Shawande M. The emergence of dementia as a health concern among First Nations populations in Alberta, Canada. Can J Public Health. 2013;104:e39–e44. doi: 10.1007/BF03405652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertrand M, Tzourio C, Alpérovitch A. Trends in recognition and treatment of dementia in france analysis of the 2004 to 2010 database of the national health insurance plan. Alzheimer Dis Assoc Disord. 2013;27:213–217. doi: 10.1097/WAD.0b013e3182695a3b. [DOI] [PubMed] [Google Scholar]
- 10.Doblhammer G, Fink A, Fritze T. Short-term trends in dementia prevalence in Germany between the years 2007 and 2009. Alzheimers Dement. 2015;11:291–299. doi: 10.1016/j.jalz.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Langa KM, Larson EB, Karlawish JH, Cutler DM, Kabeto MU, Kim SY, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4:134–144. doi: 10.1016/j.jalz.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lobo A, Saz P, Marcos G, Dia JL, De-la-Camara C, Ventura T, et al. Prevalence of dementia in a southern European population in two different time periods: the ZARADEMP Project. Acta Psychiatr Scand. 2007;116:299–307. doi: 10.1111/j.1600-0447.2007.01006.x. [DOI] [PubMed] [Google Scholar]
- 13.Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2013;382:1405–1412. doi: 10.1016/S0140-6736(13)61570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alzheimer's Disease International. World Alzheimer report 2009. [accessed on 2021 May 20]. Available at: https://www.alz.org/national/documents/report_full_2009worldalzheimerreport.pdf.
- 15.Alzheimer's Disease International. World Alzheimer report 2010. The global economic impact of dementia. [accessed on 2021 May 20]. Available at: https://www.alzint.org/resource/world-alzheimer-report-2010/
- 16.Statistics Korea. Population projection: 2017-2067. [accessed on 2021 May 20]. Available at: https://kostat.go.kr/portal/korea/kor_nw/1/2/6/index.board.
- 17.Kang L, Lee BH, Choi KS. A study on innovation system approach to national R&D in the aged society: focusing on GT in Korea. International Information Institute (Tokyo) 2017;20:8381–8392. [Google Scholar]
- 18.Ministry of Health and Welfare. 2012 study on the prevalence of dementia. [accessed on 2021 May 20]. Available at: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=286138.
- 19.Jhoo JH, Kim KW, Huh Y, Lee SB, Park JH, Lee JJ, et al. Prevalence of dementia and its subtypes in an elderly urban Korean population: results from the Korean Longitudinal Study on Health And Aging (KLoSHA) Dement Geriatr Cogn Disord. 2008;26:270–276. doi: 10.1159/000160960. [DOI] [PubMed] [Google Scholar]
- 20.Kim KW, Park JH, Kim MH, Kim MD, Kim BJ, Kim SK, et al. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea. J Alzheimers Dis. 2011;23:281–291. doi: 10.3233/JAD-2010-101221. [DOI] [PubMed] [Google Scholar]
- 21.Ministry of Health and Welfare. 2016 National dementia epidemiological survey. Sejong: Ministry of Health and Welfare; 2017. [Google Scholar]
- 22.Park J, Ko HJ, Park YN, Jung CH. Dementia among the elderly in a rural Korean community. Br J Psychiatry. 1994;164:796–801. doi: 10.1192/bjp.164.6.796. [DOI] [PubMed] [Google Scholar]
- 23.Lee DY, Lee JH, Ju YS, Lee KU, Kim KW, Jhoo JH, et al. The prevalence of dementia in older people in an urban population of Korea: the Seoul study. J Am Geriatr Soc. 2002;50:1233–1239. doi: 10.1046/j.1532-5415.2002.50310.x. [DOI] [PubMed] [Google Scholar]
- 24.Kim J, Jeong I, Chun JH, Lee S. The prevalence of dementia in a metropolitan city of South Korea. Int J Geriatr Psychiatry. 2003;18:617–622. doi: 10.1002/gps.897. [DOI] [PubMed] [Google Scholar]
- 25.Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in Korea: a systematic review and meta-analysis. J Korean Med Sci. 2014;29:903–912. doi: 10.3346/jkms.2014.29.7.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alzheimer's Disease International. World Alzheimer report 2015. The global impact of dementia: an analysis of prevalence, incidence, cost and trends. [accessed on 2021 May 20]. Available at: https://www.alzint.org/resource/world-alzheimer-report-2015/
- 27.Kosteniuk JG, Morgan DG, O'Connell ME, Kirk A, Crossley M, Teare GF, et al. Simultaneous temporal trends in dementia incidence and prevalence, 2005-2013: a population-based retrospective cohort study in Saskatchewan, Canada. Int Psychogeriatr. 2016;28:1643–1658. doi: 10.1017/S1041610216000818. [DOI] [PubMed] [Google Scholar]
- 28.Goodman RA, Lochner KA, Thambisetty M, Wingo TS, Posner SF, Ling SM. Prevalence of dementia subtypes in United States Medicare fee-for-service beneficiaries, 2011-2013. Alzheimers Dement. 2017;13:28–37. doi: 10.1016/j.jalz.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Schubert CC, Boustani M, Callahan CM, Perkins AJ, Carney CP, Fox C, et al. Comorbidity profile of dementia patients in primary care: are they sicker? J Am Geriatr Soc. 2006;54:104–109. doi: 10.1111/j.1532-5415.2005.00543.x. [DOI] [PubMed] [Google Scholar]
- 31.Sanderson M, Wang J, Davis DR, Lane MJ, Cornman CB, Fadden MK. Co-morbidity associated with dementia. Am J Alzheimers Dis Other Demen. 2002;17:73–78. doi: 10.1177/153331750201700210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park HK, Na DL, Han SH, Kim JY, Cheong HK, Kim SY, et al. Clinical characteristics of a nationwide hospital-based registry of mild-to-moderate Alzheimer's disease patients in Korea: a CREDOS (Clinical Research Center for Dementia of South Korea) study. J Korean Med Sci. 2011;26:1219–1226. doi: 10.3346/jkms.2011.26.9.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen TB, Yiao SY, Sun Y, Lee HJ, Yang SC, Chiu MJ, et al. Comorbidity and dementia: a nationwide survey in Taiwan. PLoS One. 2017;12:e0175475. doi: 10.1371/journal.pone.0175475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the epidemiology research council of the Korean Stroke Society. J Stroke. 2019;21:42–59. doi: 10.5853/jos.2018.03125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corrada M, Brookmeyer R, Kawas C. Sources of variability in prevalence rates of Alzheimer's disease. Int J Epidemiol. 1995;24:1000–1005. doi: 10.1093/ije/24.5.1000. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Age-Standardized Prevalence of Dementia per 1000 Population from 2008 to 2016 Analyzed according to Sex among Patients <65 Years of Age
Prevalence of Dementia per 1000 Population from 2008 to 2016 according to Age and Sex