Abstract
The COVID-19 pandemic has hugely impacted global public health and economy. The COVID-19 has also shown potential impacts on maternal perinatal and neonatal outcomes. This systematic review aimed to summarize the evidence from existing systematic reviews about the effects of SARS-CoV-2 infections on maternal perinatal and neonatal outcomes. We searched PubMed, MEDLINE, Embase, and Web of Science in accordance with PRISMA guidelines, from 1 December 2019 to 7 July 2021, for published review studies that included case reports, primary studies, clinical practice guidelines, overviews, case-control studies, and observational studies. Systematic reviews that reported the plausibility of mother-to-child transmission of COVID-19 (also known as vertical transmission), maternal perinatal and neonatal outcomes, and review studies that addressed the effect of SARS-CoV-2 infection during pregnancy were also included. We identified 947 citations, of which 69 studies were included for further analysis. Most (>70%) of the mother-to-child infection was likely due to environmental exposure, although a significant proportion (about 20%) was attributable to potential vertical transmission of SARS-CoV-2. Further results of the review indicated that the mode of delivery of pregnant women infected with SARS-CoV-2 could not increase or decrease the risk of infection for the newborns (outcomes), thereby emphasizing the significance of breastfeeding. The issue of maternal perinatal and neonatal outcomes with SARS-CoV-2 infection continues to worsen during the ongoing COVID-19 pandemic, increasing maternal and neonatal mortality, stillbirth, ruptured ectopic pregnancies, and maternal depression. Based on this study, we observed increasing rates of cesarean delivery from mothers with SARS-CoV-2 infection. We also found that SARS-CoV-2 could be potentially transmitted vertically during the gestation period. However, more data are needed to further investigate and follow-up, especially with reports of newborns infected with SARS-CoV-2, in order to examine a possible long-term adverse effect.
Keywords: COVID-19, pandemic, vertical transmission, pregnancy, systematic review
1. Introduction
COVID-19, a disease caused by SARS-CoV-2, is a member of the Coronaviridae family which is mainly transmitted through air droplets [1,2], but other routes of transmission have been reported [3]. These include maternal perinatal transmission (which could be due to biological or social factors) [4,5,6,7,8,9], vertical transmission (direct transmission between mother-to-child during pregnancy) [10,11,12,13], and environmental transmission [14,15].
Maternal physiological changes during pregnancy predispose pregnant women to infectious diseases [3,4,16,17,18]. Most early systematic reviews that reported mother-to-child transmission during pregnancy highlighted that vertical transmission of SARS-CoV-2 is plausible, even though there was insufficient evidence at the early stage of the pandemic, due to scarcity or inconsistencies in the reported data. Thus, emphasis should be placed towards further investigating and monitoring possible infection in the neonates, born to COVID-19-infected mothers [16,19,20]. Moreover, the studies that reported the possibility of mother-to-child transmission of COVID-19 during pregnancy highlighted the need for additional data to ascertain if the transmission occurs via the transplacental route, transcervical route, or environmental exposure [3,4,5,13,18,21]. It is therefore imperative to investigate the mechanism(s) through which SARS-CoV-2 reaches the fetus, to proffer ways to prevent neonatal infection, optimize pregnancy management, and eventually better understand SARS-CoV-2 epidemiology.
Several reports have shown that vertical transmission of SARS-CoV-2 is possible and likely happens in a minority of cases of maternal SARS-CoV-2 infection, especially during the third trimester of pregnancy [13,20,22,23,24]. The rates of mother-to-child infection are similar to those of other pathogens that cause congenital infections [13,25]. Notwithstanding, given the paucity of early-trimester data, it is challenging to further assess such data regarding mother-to-child transmission in early pregnancy and the potential risk for consequent fetal morbidity and mortality [13]. Thus, this indicates an urgent need to investigate the possibility of SARS-CoV-2 vertical transmission during pregnancy, and to design a strategic public health response to this scenario.
Here, we present a comprehensive systematic review of the existing literature to demonstrate the effect of COVID-19 on transplacental transmission with clinical manifestation in the neonates that resembles neurological signs and symptoms of COVID-19. In particular, this systematic review of systematic reviews intended to report the possibility of vertical transmission related to SARS-CoV-2 during pregnancy. The study consisted of a large collection of systematic reviews that included studies recruiting many pregnant women infected with SARS-CoV-2 and neonatal outcomes. We believe our findings will have significant contributions to the current literature and provide more suggestions for clinical and preventive practice guidelines against SARS-CoV-2 worldwide.
Objectives of the Study
This study aimed to answer the following questions: (i) Are the current evidence supporting the possibility of vertical transmission of SARS-CoV-2 adequate? (ii) Are there enough evidence to ascertain the possibility of mother-to-child transmission of SARS-CoV-2 during pregnancy?
2. Methods
2.1. Search Strategy and Study Screening Processes
This study adopted the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) guidelines [26]. We conducted a systematic review of systematic reviews of the literature to report an important scenario of mother-to-child transmission of SARS-CoV-2, via vertical transmission route, during pregnancy that covered published peer-reviewed articles from 1 December 2019 to 7 July 2021. A comprehensive literature search was conducted via the following medical databases: PubMed, MEDLINE, Embase, and Web of Science, for papers published in English, on human participants. Search terms used across all databases included: (COVID-19 OR SARS-CoV-2) AND (antenatal OR prenatal OR vertical transmission OR pregnancy OR pregnant OR delivery OR infant OR neonate OR newborn) AND (systematic review). Further, relevant references were manually searched via the reference lists of included studies to ensure robust literature coverage. Citations were independently managed by two authors (S.S.M. and U.M.B.) using EndNote X9.0. All duplicates were removed using the ENDNOTE built-in ‘Find Duplicates’ feature. The two authors (S.S.M. and U.M.B.) independently screened the titles, abstracts, and full text of the non-duplicate generated citations and identified the full texts that met the eligibility criteria of the study.
2.2. Study Selection and Eligibility Criteria
Systematic reviews (SR) that assessed vertical transmission of COVID-19 were included in this study if the: (i) SR reported an explicit search strategy in popular databases; (ii) SR examined SARS-CoV-2 vertical transmission during pregnancy; (iii) SR aimed to assess maternal perinatal SARS-CoV-2 infection with neonatal outcomes, and; (iv) SR was published in the English language or with at least an abstract in the English language [26]. To ensure adequate coverage of the literature, we included SRs that reported the possibility of vertical transmission of severe acute respiratory illnesses, which include SARS-CoV-2, Middle East Respiratory Syndrome coronavirus (MERS-CoV), and Severe Acute Respiratory Syndrome coronavirus (SARS-CoV).
Non-SR studies, such as primary studies, clinical practice guidelines, overviews, case reports, and other types of studies aimed at synthesizing evidence of vertical transmission of SARS-CoV-2, were excluded. Studies with irrelevant topics, or lack of relevant information (data), or ineligible article types were also excluded. Furthermore, we excluded studies that reported plausibility of SARS-CoV-2 vertical transmission published in a non-English language. The searching and screening processes of the literature were independently conducted by the two authors (S.S.M. and U.M.B.), and discrepancies were resolved via discussions amongst the authors.
2.3. Quality Assessment
We adopted the modified version of the quality assessment tool for systematic reviews and meta-analyses, entitled “Overview Quality Assessment Questionnaire (OQAQ; Supplementary Materials Table S2) [27], for assessing the methodological quality of the included SRs. The OQAQ tool is flexible for evaluating the quality of studies with multiple study designs. This tool is widely used in public health studies [28,29,30,31,32]. The scoring ranges from 0 to 18 points, with higher scores indicating better methodological quality. SRs scoring 14 points or above are regarded as having higher quality, whereas scores of less than 14 points are rated as low quality [27,28]. Two authors (S.S.M. and U.M.B.) independently assessed methodological quality of the included SRs. Discrepancies in the outcome of the independent quality ratings were resolved via discussions between the authors. For details, see Supplementary Materials Table S3.
2.4. Data Extraction and Synthesis
To meet the standard criteria of the review, two authors (S.S.M. and U.M.B.) independently extracted all the relevant data using a pre-designed excel sheet. The data extracted included: authors details; database(s) where SR was located; date of publication; number of included primary studies in the SR; numbers of pregnant women, newborns, infected newborns, maternal deaths, and newborn deaths; mode of delivery, remark on vertical transmission reported in the SR, and; sensitivity analysis in studies with meta-analysis. The data extracted were compared, and any inconsistency in the data was rectified by further deliberations among the authors. Furthermore, the data obtained were synthesized to report issues of SARS-CoV-2 vertical transmission during pregnancy. The data synthesis included all the systematic reviews reports on the incidence of SARS-Cov-2 vertical transmission during pregnancy, i.e., direct mother-to-child transmission of SARS-CoV-2 during pregnancy.
3. Results
3.1. Literature Search Findings and Study Characteristics
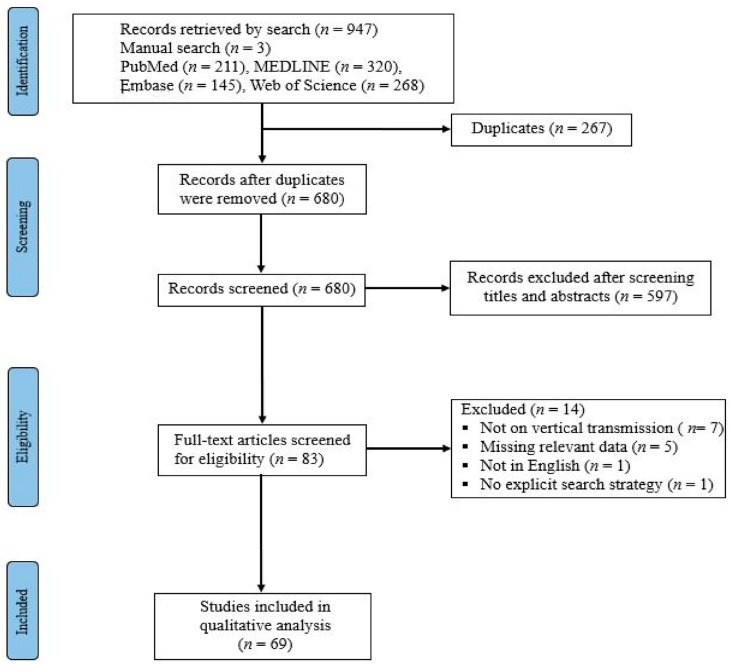
In total, 947 articles were identified through the electronic search of the databases (211, PubMed; 320, MEDLINE; 145, Embase; 268 Web of Science; and 3, from other sources). There were 680 studies left after duplicates were removed. After 597 articles were excluded by titles and abstracts screening, we retrieved 83 articles eligible for the full-text screening. We excluded 13 articles due to irrelevant or missing data on one or more variables of interest (based on the exclusion criteria mentioned earlier). Eventually, 69 studies that satisfied the eligibility criteria were included in this systematic review of systematic reviews for further synthesis and analysis. Figure 1 presents the flowchart of the study search and screening processes. The included studies were all systematic reviews on varieties of primary studies, with different study designs, including case reports, clinical practice guidelines, overviews, and observational studies. Overall, the included studies recruited over 54,413 pregnant women infected with SARS-CoV-2 consisting of more than 30,840 newborns delivered by the infected mothers. Among the neonates born from infected mothers, more than 800 neonates were reported as COVID-19 positive, out of which a majority of them likely acquired SARS-CoV-2 infection through environmental exposures, whereas a significant proportion likely acquired SARS-CoV-2 infection via vertical transmission. Table 1 presents the characteristics of the included studies.
Figure 1.
PRISMA diagram for the search and selection processes of the articles.
Table 1.
Features of the included studies.
| Study | Database(s) | Date of Publication | Number of Included Studies | Number of Pregnant Women | Number of Newborns | Number of Infected Newborns | Maternal Deaths | Newborns Deaths | Cesarean Delivery | Remark (Vertical Transmission) | Sensitivity Analysis in Studies with Meta-Analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AbdelMassih et al. [19] | Embase, MEDLINE, Cochrane | April, 2021 | 64 | 1787 | 1787 | 45 (2.5) | NA | 19 | NA | Unlikely | Y |
| Abdollahpour et al. [33] | PubMed, Scopus, Embase, Science direct, ClinicalKey, PsycINFO, manual searches of other relevant papers |
May, 2020 | 29 | NA | 2 | NA | NA | NA | NA | No direct evidence | NM |
| Abou Ghayda et al. [16] | PubMed, Scopus, MEDLINE, Google Scholar, Embase | October, 2020 | 11 | 104 | NA | NA | NA | 6 (5.8) | 52 | Vertical infection was not found | NM |
| Akhtar et al. [20] | MEDLINE, PubMed, Scopus, Google Scholar | July, 2020 | 22 | 156 | 108 | 7 | 8 | 3 | 66 | No evidence to support vertical transmission | NM |
| Allotey et al. [22] | MEDLINE, Embase, Cochrane database, WHO COVID-19 database, CNKI, Wanfang, L·OVE |
September, 2020 | 77 | 11432 | NA | NA | <1% | <1% | 1060 (65% (57–73%) 95% CI) | Not reported | Y |
| Amaral et al. [34] | Embase, PubMed database | November, 2020 | 70 | 1457 | 1042 | 39 (3.7%) | 15 (1%) | 16 (1.5%) | 15% | Low evidence to support vertical transmission | NM |
| Arroyo-Sanchez et al. [34] | MEDLINE/PubMed, ScienceDirect, ClinicalKey, LILACS, SciELO, Google Scholar, medRxiv, and SciELO Preprints. |
2020 | 30 | 476 | 476 | 9 (1.9%) | Probable | NM | |||
| Ashraf et al. [35] | PubMed, Scopus, WoS, Embase, Google Scholar | July–September, 2020 | 21 | 90 | 92 | 4 | 1 | 1 | 81 | Possible but rare | NM |
| Banaei et al. [36] | MEDLINE, Embase, Scopus, WoS, ProQuest, Google Scholar |
2020 | 16 | 123 | 124 | 5 | 0 | 1 | 99 | Probable | NM |
| Barcelos et al. [37] | PubMed, Scopus, Embase | Accepted November, 2020 | 27 | NA | NA | 9 | NA | NA | NA | Possible, with low risk | NM |
| Bwire et al. [38] | PubMed/MEDLINE, Google Scholar | Accepted October, 2020 | 33 | 205 | 205 | 13 (6.3%) | NA | NA | 71.9% | Low possibility of vertical transmission | NM |
| Cai et al. [39] | PubMed, Embase, Cochrane Library, Web of Science, Google Scholar, CBM | February, 2021 | 68 | 1019 | 1035 | 34 (3.29%) | 14 | 6 | 59.71% | Possible | NM |
| Capobianco et al. [40] | PubMed, Scopus | Accepted July, 2020 | 13 | 114 | 108 | 5 | 0 | 2 | 95 | Low probability of vertical transmission | N |
| Chamseddine et al. [41] | PubMed, medRxiv | October, 2020 | 48 | 245 | 201 | 6.45% | 8 (3.2%) | 2.5% | 89% | Possible | NM |
| Chi et al. [42] | PubMed/MEDLINE, Embase, Cumulative Index to Nursing and Allied Health Literature, National Digital Library of Theses and Dissertations in Taiwan, Art Image Indexing Service on the Internet, Cochrane | February, 2021 | 14 | 107 | 105 | 8 (8.8%) | NA | NA | 87.6% | Possible | NM |
| Della Gatta et al. [43] | PubMed, Scopus, CINAHL | July, 2020 | 6 | 51 | 48 | 1 | NA | 1 | 46 | No evidence of vertical transmission | NM |
| Deniz & Tezer [44] | medRxiv, PubMed | July, 2020 | 50 | 714 | 606 | 20 | NA | NA | NA | Potentially vertically transmit-ted | NM |
| Dhir et al. [45] | MEDLINE, Embase, Web of Science | August, 2020 | 86 | 1992 | 1141 | 58 | NA | 0 | 66% | Possible, with low risk | NM |
| Di Mascio et al. [46] | MEDLINE, Embase, CINAHL, ClinicalTrials.gov | May, 2020 | 6 | 41 | 42 | 0 | 0 | 2.4% | 38 | None has been reported | N |
| Di Toro et al. [25] | PubMed, Embase, medRxiv, Scholar, Scopus, Web of Science | January, 2021 | 24 | 588 | 444 | 19 | 5 | 3 | 85% | No evidence of vertical transmission | N |
| Diriba et al. [47] | PubMed, Web of Science, Embase, Google Scholar, Cochrane | September, 2020 | 23 | 1271 | NA | 0 | 1.5% | 1.2% | 57% | No evidence of vertical transmission | Y |
| Amaral et al. [34] | PubMed, Embase | November, 2020 | 70 | 1457 | 1112 | 39 | 15 | 16 | 597 (57.3%) | Possible | NM |
| Dube et al. [48] | PubMed, Embase, LitCovid, medRxiv, bioRxiv, Google Scholar, EBSCO MEDLINE, CINAHL, Scopus | November, 2020 | 72 | NA | 1408 | 51 (3.67%) | NA | NA | 59.9% | Possible but low | NM |
| Dubey et al. [49] | PubMed | September, 2020 | 61 | 790 | 548 | NA | NA | NA | 72% | None reported | Y |
| Duran et al. [50] | Google Scholar, LILACS, PubMed | May, 2020 | 20 | 195 | 222 | 13 | NA | 1 | 48 | Probable | NM |
| Elshafeey et al. [51] | LitCovid, EBSCO MEDLINE, CENTRAL, CINAHL, Web of Science, Scopus | May, 2020 | 33 | 385 | 256 | 4 | 1 | 1 | 175 (69.4) | Probable | NM |
| Galang et al. [52] | MEDLINE, ClinicalTrials.gov | August, 2020 | 31 | 98 | 94 | 8 | 1 | 1 | 72 | Probable | NM |
| Gao et al. [53] | PubMed, Web of Science, Embase, MEDLINE | August, 2020 | 14 | 236 | NA | 1.8% | NA | 1 | 69% | No evidence available | Y |
| Ghayda et al. [16] | PubMed, Scopus, MEDLINE, Google Scholar, Embase | October, 2020 | 11 | 104 | NA | 0 | 7 | 5 fetal + 1 neonatal | 50% | No vertical transmission reported | N |
| Gordon et al. [54] | CINAHL, Embase, MEDLINEMEDLINE, PubMed | May, 2020 | 8 | NA | 46 | 7 | NA | 0 | 86% | Likely | NM |
| Han et al. [55] | MEDLINE, PubMed, Web of Science, Cochrane, CNKI, Wanfang Data, VIP, SinoMed, ClinicalTrials.gov | October, 2020 | 36 | 1103 | NA | <0.01% | <0.01% | <0.01% | 28.59% | Unlikely | NM |
| Hassanipour et al. [56] | PubMed, Embase, Scopus, Web of Science, Google Scholar | December, 2020 | 10 | 135 | NA | 1 | NA | 1 | 84% | Low evidence for vertical transmission | N |
| Huntley et al. [57] | MEDLINE, Ovid, ClinicalTrials.gov, medRxiv, Scopus |
August, 2020 | 13 | 538 | 435 | 0 | 0 | 1 | 85% | None reported | NM |
| Islam et al. [58] | PubMed, Embase, Scopus, Google Scholar, Web of Science |
December, 2020 | 13 | 235 | NA | 0 | NA | NA | 156 (66.38%) | Not reported | N |
| Jafari et al. [59] | Embase, Scopus, PubMed, Web of Science, Cochrane | January, 2021 | 121 | NA | 8% | NA | NA | 2.5% | 48% | Possible | N |
| Juan et al. [60] | PubMed, Embase, Cochrane, CNKI, Wanfang Data | May, 2020 | 24 | 324 | 240 | 3 | 7 | 1 | 78.1% | Possible | NM |
| Karabay et al. [61] | MEDLINE, Web of Science, PubMed, ScienceDirect, CINAHL, Scopus, Cochrane, TUBiTAK | November, 2020 | 35 | NA | NA | 68 | NA | 0 | NA | Possible | NM |
| Kasraeian et al. [62] | PubMed, Google Scholar, medRxiv, UpToDate search engines | May, 2020 | 9 | 87 | 86 | 0 | 0 | 0.2% | 92.2% | Not reported | Y |
| Khalil et al. [63] | MEDLINE, Embase, ClinicalTrials.gov, Cochrane | August, 2020 | 86 | 2567 | NA | 1.4% | 0.9% | 0.6% | 48.3% | Possible | N |
| Kotlyar et al. [13] | PubMed, Embase, medRxiv, bioRxiv | Jan, 2021 | 69 | 1566 | 936 | 27 (3.2%) | NA | NA | 73% | Possible | Y |
| Lopes de Sousa et al. [64] | PubMed, Scopus, Embase, ScienceDirect, WoS, Google Scholar, bioRxiv, medRxiv |
June, 2020 | 49 | 755 | 598 | 1.8% | 8 | 10 | 64.7% | No concrete evidence of vertical transmission | NM |
| Matar et al. [65] | Ovid MEDLINE and Epub Ahead of Print, In-Process and Other Nonindexed Citations, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, Scopus |
June, 2020 | 24 | 136 | 94 | 2 | 1 | 3 | 76.3% | Probable | N |
| Melo et al. [66] | PubMed, Scopus, LILACS, Web of Science, Google Scholar, Preprints, bioRxiv, medRxiv | July, 2020 | 38 | 520 | NA | 16 | NA | NA | NA | Possible | Y |
| Mirbeyk et al. [67] | PubMed, Web of Science, Google Scholar, Scopus, WHO COVID-19 database | April, 2021 | 37 | 386 | 302 | 5% | 2 | 3 | 86% | Possible, with low evidence | NM |
| Muhidin et al. [68] | PubMed, Scopus, Embase, ProQuest, ScienceDirect | April, 2020 | 9 | 89 | 89 | 0 | 0 | 2.2% | 91.9% | No evidence | NM |
| Najafi et al. [69] | PubMed, Scopus, Google Scholar | December, 2020 | 20 | NA | 145 | 7 | NA | 10% | NA | Low risk of vertical transmission | NM |
| Neef et al. [70] | PubMed, Google Scholar, Web of Science | October, 2020 | 32 | 258 | 261 | 12 | NA | 3 | NA | The risk of vertical transmission is low | N |
| Novoa et al. [21] | MEDLINE, Embase, Cochrane Library, LILACS, CNKI, VIP, Wanfang Data | January–February, 2021 | 37 | 322 | 195 | 16 | 1 | 1 | 99 (50.8%) | No concrete evidence to support vertical transmission | N |
| Oltean et al. [71] | MEDLINE, Embase, Google Scholar, WHO database on COVID-19, Disaster Lit: Database, medRxiv, and OSF Preprints | March, 2021 | 41 | 315 | 262 | 3.1% | NA | 1 | NA | Vertical transmission has yet to be confirmed | NM |
| Oshay et al. [72] | PubMed, Embase, World Health Organization, Google Scholar | July, 2021 | 67 | 427 | 304 | 3.2% | 8 | NA | NA | Low risk of vertical transmission | NM |
| Papapanou et al. [17] | PubMed, Scopus, Cochrane | January, 2021 | 39 | NA | NA | 1.6–10% | <2% | <3% | 52.3–95.8% | Probable | NM |
| Pastick et al. [73] | PubMed/MEDLINE | August, 2020 | 126 | 11308 | 10597 | NA | 33 | 0.7% | 70% | Not reported | NM |
| Pettirosso et al. [74] | MEDLINE, Embase, WHO COVID-19 database, Cochrane | August, 2020 | 60 | 1287 | NA | 19 | 8 | 6 | NA | Possible | NM |
| Raschetti et al. [75] | PubMed, Cochrane, Web of Science, bioRxiv, and medRxiv | October, 2020 | 74 | NA | NA | 53 | NA | NA | NA | Confirmed/possible | N |
| Rodrigues et al. [76] | PubMed, Scopus, Web of Science, medRxiv | November, 2020 | 161 | 3985 | 2015 | 61 | 28 | 10 | 53.92% | Possible | NM |
| Smith et al. [23] | PubMed, MEDLINE, Embase | June, 2020 | 9 | 92 | 60 | 1 | 0 | 1 | 80% | Probable | NM |
| Thomas et al. [77] | Ovid MEDLINE, Embase, CENTRAL | July, 2020 | 18 | 157 | 160 | 5 | 1 | 1 | 115 (73%) | No conclusive evidence to support vertical transmission | NM |
| Tolu et al. [24] | PubMed, CINAHL, Web of Science, Scopus, CENTRAL | April, 2021 | 51 | NA | 336 | 15 | NA | NA | 265 (78.8%) | Not enough evidence on vertical transmission | NM |
| Trippella et al. [78] | MEDLINE, Embase, Google Scholar, medRxiv | June, 2020 | 37 | 275 | 248 | 16 | 1 | 1 | 74.9% | Possible | NM |
| Trocado et al. [79] | PubMed, Scopus database, and WHO database | July, 2020 | 8 | 95 | 51 | 1 | 0 | 1 | 94% | Probable | NM |
| Turan et al. [80] | PubMed, Ovid MEDLINE, WoS, China Academic Literature Database |
July, 2020 | 63 | 637 | 479 | 8 | 10 | 5 | 83% | Probable | NM |
| Vergara-Merino et al. [18] | PubMed/MEDLINE, Embase, other electronic databases, clinical trials registries, and preprint repositories, among other sources relevant to COVID-19 | February, 2021 | 52 | NA | NA | 0–11.5% | 0–11.1% | 0–11.7% | 48.3–100% | Possible | NM |
| Walker et al. [81] | MEDLINE, Embase, Maternity and Infant Care Database | June, 2020 | 49 | 655 | 666 | 28 | NA | NA | 5.3% | Probable | NM |
| Yang et al. (a) [82] | PubMed, Google Scholar, CNKI, Wanfang Data, VIP, CBMdisc |
April, 2020 | 18 | 114 | NA | 7 | NA | 1 | 90.8% | No direct evidence | NM |
| Yang et al. (b) [83] | PubMed, CNKI, CBMdisc, Wanfang Data | 2020 | 22 | NA | 83 | 9 | NA | NA | 88% | No direct evidence | NM |
| Yee et al. [84] | PubMed, Embase, WoS | October, 2020 | 9 | 93 | 103 | 4 | NA | 0 | NA | No direct evidence | N |
| Yoon et al. [85] | PubMed/MEDLINE, Embase | 2020 | 28 | 223 | 201 | 4 | NA | 1 | 88.1% | Probable | NM |
| Yuan et al. [86] | PubMed, MEDLINE, CBM, Wanfang | 2021 | 29 | 564 | 555 | 18 | NA | NA | 62.8% | No sufficient evidence to exclude the possibility of vertical transmission | NM |
| Zaigham et al. [87] | MEDLINE, Embase, Google Scholar | April, 2020 | 18 | 108 | 87 | 1 | 0 | 1 | 92% | Probable | NM |
Abbreviation: NA: Not available; Remark: Conclusion remarks drawn from the included systematic reviews studies on vertical transmission of SARS-CoV-2; Y: Yes; N: No; NM: No Meta-analysis.
3.2. Methodological Quality of the Included Studies
A majority of the included studies (92.75% (n = 64)) were of higher methodological quality, with 13.54% (n = 13) scoring the maximum obtainable score (18 points) on the quality-rating tool. All the included studies provided adequate details regarding “search method used to find evidence on the primary question(s) stated” (Item 1 on the OQAQ). Item 6 (were study quality assessment criteria used to inform the review analysis) scored the highest number for limited reporting (with 5 studies not reporting the details on the item and another 28 reporting the details partially). Avoidance of selection bias (Item 4) was partially reported in many of the included studies (48%, n = 33). The findings of the methodological quality are reported in Supplementary Materials Table S3.
3.3. SARS-CoV-2 Vertical Transmission
In the current systematic review, we identified 69 studies that satisfied all the inclusion criteria, reporting over 54,413 pregnancies infected with SARS-CoV-2 resulting in more than 30,840 newborns delivered by the infected mothers. Subsequently, the newborns were screened for COVID-19 using throat-swab SARS-CoV-2 RT-PCR testing or other standard diagnostic procedures for testing for COVID-19 infection from exposed individuals. Results from the samples tested revealed that there were over 800 neonates with positive SARS-CoV-2 results, indicating the plausibility of SARS-CoV-2 vertical transmission from COVID-19-infected mothers.
Furthermore, our analysis also showed that, although most of the reports during the early epidemic period suggested the plausibility of vertical transmission of SARS-CoV-2 [23,34,35,36,44,50,51,52,54,60,63,65,66,79,80,81,88], most of these reports hinted that more data were needed to confirm whether the mother-to-child transmission during pregnancy resulted from a vertical transmission or due to environmental exposure, such as during breastfeeding, hospital contamination by health workers, among others. Therefore, caution should be taken in making the conclusion that SARS-CoV-2 pathogens can be potentially transmitted vertically. In their systematic review, Smith et al. [23] identified one scenario of mother-to-child infection (neonatal infection) of COVID-19. They highlighted that, although SARS-CoV-2 could probably be transmitted vertically, there is still no concrete evidence to support the claim, likely due to the scarcity of the data at the moment. The neonatal infection could be during the post-delivery period, because the RT-PCR assay was performed when the infant was 36 h old. Moreover, none of the previous coronaviruses were reported to have been transmitted vertically [23]. However, that would not rule out the possibility of vertical transmission for SARS-CoV-2 [25].
Morevier, as the COVID-19 pandemic continues, many clinical and epidemiological features keep unfolding, and new knowledge is being discovered regarding SARS-CoV-2 transmission. Recently, several reports published in decent journals revealed that SARS-CoV-2 can be transmitted vertically and provided some clinical and epidemiological evidence to support the claim. Raschetti et al. [75] reported that the majority of mother-to-child infections (about 70%) of SARS-CoV-2 during pregnancy were likely transmitted due to environmental exposure (postpartum transmission). However, about 30% of the infections were likely due to vertical transmission, intrapartum or congenital. A reasonable number (i.e., about 9%) of the infections were confirmed to be potentially transmitted vertically.
3.4. Maternal and Newborn Death Rates
Maternal mortality was reported in 39 SRs, [16,17,18,20,21,22,23,25,34,35,36,39,40,41,46,47,51,52,54,55,57,60,62,63,64,65,67,68,72,73,74,76,77,78,79,80,87,88] and varied from 0% to 11.1% among the included reviews.
Newborns mortality was reported in 50 SRs, [16,17,18,19,20,21,22,23,25,34,35,36,39,40,41,43,45,46,47,49,50,51,52,53,54,56,57,59,60,62,63,64,65,67,68,69,70,71,73,74,76,77,78,79,80,82,84,85,87] and varied from 0% to 11.7% among the included reviews.
Our results are consistent with previous reports, including that of Vergara-Merino et al. [18]. Table 1 presents a summary of the results of maternal and newborns death rates.
3.5. Cesarean Delivery
A cesarean delivery (C-section) can be defined as a clinical surgical method used to deliver a an unborn child through incisions in the abdomen and uterus [89]. Our results show that a majority of the neonates who tested positive for SARS-CoV-2 were either delivered via C-section (cesarean delivery) [21], or had not been breastfed by the infected mothers [24]. For instance, according to Novoa et al. [21], there was more cesarean delivery (about 50.8%) than vaginal delivery (approximately 38.8%). Tolu et al. [24] reported that among the neonates with positive SARS-CoV-2 results, 54% were separated from their mother, and obviously, there was no breastfeeding during the separation period. Several reports also highlighted that high or low risk of mother-to-child transmission did not depend on the mode of delivery (i.e., either via C-section or virginal delivery) ([22,38,39,41,42], and the references therein).
4. Discussion
The connection between maternal with neonatal outcomes infected with SARS-CoV-2 during pregnancy has recently been reported and revealed some silent (and one of the most important) features of COVID-19. The transmission of COVID-19 directly from mother to child, or vertical transmission, has been an essential topic of discussion among researchers and public health experts, which raised concerns recently. Therefore, it needs urgent attention, from researchers and public health in order to protect an unborn vulnerable child from being infected with SARS-CoV-2. In this work, we conducted a systematic review of systematic reviews, based on available literature, focusing on the plausibility of vertical transmission of SARS-CoV-2 based on clinical evidence and scientific reports. Our results also included systematic review results that reported the issue of vertical transmission in pregnant women with other comorbid conditions, such as hypertensive disorders of pregnancy, maternal gestational diabetes, preterm birth (before the birth period of at least 37 weeks), labor induction, and post-partum hemorrhage.
Based on available evidence regarding SARS-CoV-2 transmission from mother to child through a placenta, we found that among all the 69 systematic reviews studies, most of them have hinted that vertical transmission of SARS-CoV-2 occurs postnatally due to environmental exposure during the pregnancy period. However, a significant percentage reported that SARS-CoV-2 could be transmitted vertically. Thus, our results highlighted that most early review reports suggested the plausibility of SARS-CoV-2 vertical transmission. Our findings are in line with previous reports [3,24,75]. In particular, Raschetti et al. [75] conducted a systematic review and meta-analysis based on 176 published cases of maternal outcomes infected with SARS-CoV-2. They found that 70% and 30% of neonates infected with SARS-CoV-2 were due to environmental exposures and vertical transmission, respectively. Moreover, according to more recent reports with availability of more relevant data or information on maternal perinatal and neonatal outcomes infected with SARS-CoV-2 during pregnancy, we found that SARS-CoV-2 can be potentially transmitted vertically. However, there is still a need for more adequate data to guide clinical recommendations with the required certainty of the evidence.
As SARS-CoV-2 continues to unfold, its biological system, especially in pregnant women infected with the disease, is still ambiguous. For vertical transmission to occur via the transplacental route, the SARS-CoV-2 infection should initially circle within the contaminated pregnant woman [90]. Previous works [90,91] reported that the virus attacks the uterine arterioles, then passes through the placenta’s fetal side, and reaches the chorionic villus and then continues to circulate in the fetus. Vis-a-vis catalytic feature, SARS-CoV-2 contamination can happen via enactment of the angiotensin-converting catalyst receptor on the outer layer of cells inside the fetus.
It is conjectured that SARS-CoV-2 vertical transmission during pregnancy through a transplacental route is likely to be higher when there is an increment in gestational age. This is thus thought to be added to the inexorably communicated angiotensin-converting protein 2 (ACE-2) receptors on the placenta nearer to the furthest limit of incubation [92]. Moreover, some proposed animal models highlighted that ACE-2 receptor articulation attains maximum, which is closer to the furthest limit of the gestational period [91,93]. In addition, some previous reports revealed that the identification of ACE-2 receptors on the human placenta differs amongst pregnant women. This could uphold the debate regarding why vertical transmission is uncommon and variable between COVID-19-infected pregnant women [94]. Fenizia et al. [12] reported that the two common receptors for SARS-CoV-2, that is, angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2, broadly spread in particular cell types of the maternal–fetal interface [12,91]. Thus, the effect of the SARS-CoV-2 on the placenta and the potential for vertical transmission need further investigation.
Furthermore, recent reports showed that the vertical transmission of COVID-19 during pregnancy likely occurs when there is a high viral burden and duplication level in the maternal blood [95]. However, SARS-CoV-2 viremia is uncommon amongst contaminated pregnant women. However, a few studies highlighted that a high viral load coupled with general inflammation could lead to viremia [96]. It has been recommended that there may likewise be a connection between the time/length of viral openness in utero and neonatal SARS-CoV-2 status. A lengthier size of viral openness might prompt increased probability of neonatal infection [91,97]. Nevertheless, solid proof is scarce for this issue, and future works are required to shed more light on mother-to-child transmission during pregnancy. Moreover, previous investigations divulged that various comorbidities might influence the probability of vertical transmission [91]. We also observed that the severity of disease progression did not increase the risk of vertical transmission [91,98].
Most of the previous works failed to address the issues bedeviling potential infection complications to both COVID-19-infected pregnant women and the outcomes. However, some included studies reported and discussed the plausibility of infection complications which could fuel the vertical transmission of SARS-CoV-2 during pregnancy. Based on previous studies, SARS-CoV-2 infection complications in pregnant women infected with COVID-19 and their newborns included maternal and neonatal mortality, preterm delivery, ruptured ectopic pregnancies, maternal depression, prematurity, abnormalities in amniotic fluid and the umbilical cord, placental abruption, gestational diabetes mellitus, fetal distress, abortion, vaginal bleeding, and fetal death (and stillbirth) [16,99]. These infection complications likely increase the possibility of the fact that there could be vertical transmission of SARS-CoV-2.
In summary, we conducted a systematic review of systematic reviews that provided evidence supporting the mother-to-child transmission of SARS-CoV-2 during pregnancy. We found that SARS-CoV-2 could be potentially transmitted vertically and could be likely due to the detection of SARS-CoV-2 RNA in placental tissue, which might lead to perinatal outcomes of infection with SARS-CoV-2. However, further investigation and analysis are needed, especially on amniotic fluid, a cord blood sample, and breast milk, to confirm/ascertain the possibility of SARS-CoCV-2 vertical transmission during pregnancy. Our results are consistent with recent studies [12,13,23], which revealed that, although evidence is still low, SARS-CoV-2 can be transmitted from a COVID-19-infected mother to the child via a vertical route.
Furthermore, several reports highlighted that most of the neonates infected with SARS-CoV-2 were delivered through a cesarean mode, indicating that the risk of vertical transmission does not solely depend on the delivery mode [21,24]. However, the long-term or short-term impact of SARS-CoV-2 vertical transmission should be investigated to protect vulnerable children from the adverse effect of SARS-CoV-2 mother-to-child infection during pregnancy. Also, more time is needed to follow up on the children infected with COVID-19 or other comorbid conditions of new babies born from infected mothers.
4.1. Strengths
The current systematic review study was conducted following an extensive literature search of well-known databases, including PubMed, MEDLINE, Embase, and Web of Science. Furthermore, relevant citations were extracted using the reference lists of the included studies to ensure robust coverage of the existing literature. The primary studies included a large number of pregnant women (in the first, second, and third trimesters of the pregnancy) and their diagnostic outcomes of SARS-CoV-2 for data from different countries across the globe. In addition, the justification for conducting the current study was the need to timely find and discuss the availability of the existing evidence on SARS-CoV-2 vertical transmission. It is also imperative to note that this study gathered all the relevant evidence available in the literature up to 7 July 2021, which is crucial in guiding public health authorities and policymakers on the association between maternal perinatal and neonatal outcomes infected with SARS-CoV-2 during pregnancy.
4.2. Limitations
The current study was not free from limitations. First, some of the included studies have poor quality, likely due to the potential risk of bias, small sample size, missing data, or lack of standard methodological approach. Secondly, heterogeneity among the included primary studies in terms of design could also serve a limiting factor. As such, interpretation of the findings should be done cautiously. Thirdly, due to the study period and the urgent need to investigate the issue of maternal perinatal with neonatal outcomes infected with SARS-CoV-2, and the fact that new reports related to COVID-19 are being published every day, we were unable to register our study with PROSPERO. However, as for the future, we plan to extend the current research when new information/relevant data become publicly available, which could help interpret the issue of vertical transmission of SARS-CoV-2 during pregnancy much better. We plan to have a proper registration of a review protocol before commencing the future update research. Furthermore, due to the inability of many previous works to address potential infection complications, which likely occurs to both COVID-19-infected mothers and their newborns, we did not provide an in-depth analysis regarding infection complications in the current work. Nevertheless, this issue would be given considerable effort in our future research. Therefore, it is imperative to emphasize that, as the COVID-19 pandemic is still in progress and many epidemiological features are unfolding, it is difficult to conclude how COVID-19 is transmitted vertically during pregnancy. Furthermore, it is plausible that some additional relevant information might have been published during this manuscript’s submission or publication process.
5. Conclusions
This systematic review of systematic reviews provides a general overview of maternal perinatal and neonatal outcomes infected with SARS-CoV-2. We found that SARS-CoV-2 could be potentially transmitted vertically. The results also indicated that the mode of delivery for women infected with SARS-CoV-2 did not increase or decrease the risk of COVID-19 infection for newborns but likely increased the risk for direct and indirect adverse health outcomes. Moreover, the maternal death rates were significantly higher in pregnant woman infected with COVID-19 than those without the disease [12,16]. However, prospective studies are needed to clarify the actual risk of SARS-CoV-2 mother-to-child infection and identify the optimal prevention and control strategies.
Acknowledgments
The authors are grateful to the handling editor and anonymous reviewers for their helpful comments and suggestions, which were used to improve the manuscript from its initial draft.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/v13091877/s1, Table S1: Search Strategy, Table S2: OQAQ: Overview Quality Assessment Tool for Systematic Reviews and Meta-Analyses, Table S3: Quality rating using OQAQ.
Author Contributions
Conceptualization, data curation, formal analysis, formal analysis, investigation, methodology, project administration, resources, validation, visualization, writing—original draft, writing—review and editing: S.S.M.; conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, validation, visualization, writing—original draft, writing—review and editing: U.M.B.; conceptualization, formal analysis, investigation, methodology, validation, visualization, writing—original draft, writing—review and editing: S.Z.; investigation, methodology, project administration, validation, visualization, writing—review and editing: Z.U.A.; conceptualization, investigation, methodology, supervision, validation, visualization, writing—original draft, writing—review and editing: M.A.L.; conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, visualization, writing—original draft, writing—review and editing: D.H. All authors have read and agreed to the published version of the manuscript.
Funding
The work described in this paper was partially supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (HKU C7123-20G).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data used in this work were publicly available.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jayaweera M., Perera H., Gunawardana B., Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020;188:109819. doi: 10.1016/j.envres.2020.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vivanti A.J., Vauloup-Fellous C., Prevot S., Zupan V., Suffee C., Do Cao J., Benachi A., De Luca D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020;11:1–7. doi: 10.1038/s41467-020-17436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angelidou A., Sullivan K., Melvin P.R., Shui J.E., Goldfarb I.T., Bartolome R., Chaudhary N., Vaidya R., Culic I., Singh R. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw. Open. 2021;4:e217523. doi: 10.1001/jamanetworkopen.2021.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong L., Tian J., He S., Zhu C., Wang J., Liu C., Yang J. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846–1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu N., Li W., Kang Q., Xiong Z., Wang S., Lin X., Liu Y., Xiao J., Liu H., Deng D. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020;20:559–564. doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng H., Xu C., Fan J., Tang Y., Deng Q., Zhang W., Long X. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848–1849. doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeng L., Xia S., Yuan W., Yan K., Xiao F., Shao J., Zhou W. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020;174:722–725. doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu H., Wang L., Fang C., Peng S., Zhang L., Chang G., Xia S., Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020;9:51. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alzamora M.C., Paredes T., Caceres D., Webb C.M., Valdez L.M., La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am. J. Perinatol. 2020;37:861–865. doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fenizia C., Biasin M., Cetin I., Vergani P., Mileto D., Spinillo A., Gismondo M.R., Perotti F., Callegari C., Mancon A. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020;11:1–10. doi: 10.1038/s41467-020-18933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotlyar A.M., Grechukhina O., Chen A., Popkhadze S., Grimshaw A., Tal O., Taylor H.S., Tal R. Vertical transmission of coronavirus disease 2019: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2021;224:35–53. doi: 10.1016/j.ajog.2020.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poirier C., Luo W., Majumder M.S., Liu D., Mandl K.D., Mooring T.A., Santillana M. The role of environmental factors on transmission rates of the COVID-19 outbreak: An initial assessment in two spatial scales. Sci. Rep. 2020;10:1–11. doi: 10.1038/s41598-020-74089-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vardoulakis S., Sheel M., Lal A., Gray D. COVID-19 environmental transmission and preventive public health measures. Aust. N. Z. J. Public Health. 2020;44:333–335. doi: 10.1111/1753-6405.13033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abou Ghayda R., Li H., Lee K.H., Lee H.W., Hong S.H., Kwak M., Lee M., Kwon M., Koyanagi A., Kronbichler A., et al. COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases. J. Clin. Med. 2020;9:3441. doi: 10.3390/jcm9113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Papapanou M., Papaioannou M., Petta A., Routsi E., Farmaki M., Vlahos N., Siristatidis C. Maternal and Neonatal Characteristics and Outcomes of COVID-19 in Pregnancy: An Overview of Systematic Reviews. Int. J. Environ. Res. Public Health. 2021;18:596. doi: 10.3390/ijerph18020596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vergara-Merino L., Meza N., Couve-Perez C., Carrasco C., Ortiz-Munoz L., Madrid E., Bohorquez-Blanco S., Perez-Bracchiglione J. Maternal and perinatal outcomes related to COVID-19 and pregnancy: An overview of systematic reviews. Acta Obstet. Gynecol. Scand. 2021;100:1200–1218. doi: 10.1111/aogs.14118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.AbdelMassih A., Fouda R., Essam R., Negm A., Khalil D., Habib D., Afdal G., Ismail H.A., Aly H., Genedy I., et al. COVID-19 during pregnancy should we really worry from vertical transmission or rather from fetal hypoxia and placental insufficiency? A systematic review. Egypt. Pediatr. Assoc. Gaz. 2021;69:1386. doi: 10.1186/s43054-021-00056-0. [DOI] [Google Scholar]
- 20.Akhtar H., Patel C., Abuelgasim E., Harky A. COVID-19 (SARS-CoV-2) Infection in Pregnancy: A Systematic Review. Gynecol. Obstet. Investig. 2020;85:295–306. doi: 10.1159/000509290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Novoa R.H., Quintana W., Llancarí P., Urbina-Quispe K., Guevara-Ríos E., Ventura W. Maternal clinical characteristics and perinatal outcomes among pregnant women with coronavirus disease 2019. A systematic review. Travel Med. Infect. Dis. 2021;39:101919. doi: 10.1016/j.tmaid.2020.101919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T., Debenham L., Llavall A.C., Dixit A., Zhou D., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. Bmj. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith V., Seo D., Warty R., Payne O., Salih M., Chin K.L., Ofori-Asenso R., Krishnan S., Costa F.D., Vollenhoven B., et al. Maternal and neonatal outcomes associated with COVID-19 infection: A systematic review. PLoS ONE. 2020;15:e0234187. doi: 10.1371/journal.pone.0234187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tolu L.B., Ezeh A., Feyissa G.T. Vertical transmission of Severe Acute Respiratory Syndrome Coronavirus 2: A scoping review. PLoS ONE. 2021;16:e0250196. doi: 10.1371/journal.pone.0250196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Toro F., Gjoka M., Di Lorenzo G., De Santo D., De Seta F., Maso G., Risso F.M., Romano F., Wiesenfeld U., Levi-D’Ancona R., et al. Impact of COVID-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021;27:36–46. doi: 10.1016/j.cmi.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Moher D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021;134:103–112. doi: 10.1016/j.jclinepi.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Oxman A.D., Guyatt G.H. Validation of an index of the quality of review articles. J. Clin. Epidemiol. 1991;44:1271–1278. doi: 10.1016/0895-4356(91)90160-B. [DOI] [PubMed] [Google Scholar]
- 28.Greaves C.J., Sheppard K.E., Abraham C., Hardeman W., Roden M., Evans P.H., Schwarz P. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:1–12. doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Biddle S.J., Mutrie N., Gorely T., Faulkner G. Psychology of Physical Activity: Determinants, Well-Being and Interventions. Volume 502. Routledge, Taylor & Francis Group; London, UK: 2021. [Google Scholar]
- 30.Colberg S.R., Sigal R.J., Yardley J.E., Riddell M.C., Dunstan D.W., Dempsey P.C., Horton E.S., Castorino K., Tate D.F. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–2079. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landsberg L., Aronne L.J., Beilin L.J., Burke V., Igel L.I., Lloyd-Jones D., Sowers J. Obesity-related hypertension: Pathogenesis, cardiovascular risk, and treatment—A position paper of the The Obesity Society and the American Society of Hypertension. Obesity. 2013;21:8–24. doi: 10.1002/oby.20181. [DOI] [PubMed] [Google Scholar]
- 32.Wu Y., Ding Y., Tanaka Y., Zhang W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int. J. Med. Sci. 2014;11:1185. doi: 10.7150/ijms.10001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdollahpour S., Khadivzadeh T. Improving the quality of care in pregnancy and childbirth with coronavirus (COVID-19): A systematic review. J. Matern. Fetal Neonatal Med. 2020:1–9. doi: 10.1080/14767058.2020.1759540. [DOI] [PubMed] [Google Scholar]
- 34.Amaral W.N.D., Moraes C.L.D., Rodrigues A.P.D.S., Noll M., Arruda J.T., Mendonça C.R. Maternal Coronavirus Infections and Neonates Born to Mothers with SARS-CoV-2: A Systematic Review. Healthcare. 2020;8:511. doi: 10.3390/healthcare8040511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ashraf M.A., Keshavarz P., Hosseinpour P., Erfani A., Roshanshad A., Pourdast A., Nowrouzi-Sohrabi P., Chaichian S., Poordast T. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Pregnancy and the Possibility of Vertical Transmission. J. Reprod. Infertil. 2020;21:157–168. [PMC free article] [PubMed] [Google Scholar]
- 36.Banaei M., Ghasemi V., Saei M., Naz M.S.G., Kiani Z., Rashidi-Fakari F., Banaei S., Souri B.M., Rokni M. Obstetrics and Neonatal Outcomes in Pregnant Women with COVID-19: A Systematic Review. Iran. J. Public Health. 2020;49:38–47. doi: 10.18502/ijph.v49iS1.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barcelos I., Penna I.A.A., Soligo A.G., Costa Z.B., Martins W.P. Vertical Transmission of SARS-CoV-2: A Systematic Review. Rev. Bras. Ginecol. Obstet. 2021;43:207–215. doi: 10.1055/s-0040-1722256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bwire G.M., Njiro B.J., Mwakawanga D.L., Sabas D., Sunguya B.F. Possible vertical transmission and antibodies against SARS-CoV-2 among infants born to mothers with COVID-19: A living systematic review. J. Med. Virol. 2021;93:1361–1369. doi: 10.1002/jmv.26622. [DOI] [PubMed] [Google Scholar]
- 39.Cai J., Tang M., Gao Y., Zhang H., Yang Y., Zhang D., Wang H., Liang H., Zhang R., Wu B. Cesarean Section or Vaginal Delivery to Prevent Possible Vertical Transmission From a Pregnant Mother Confirmed With COVID-19 to a Neonate: A Systematic Review. Front. Med. 2021;8:634949. doi: 10.3389/fmed.2021.634949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Capobianco G., Saderi L., Aliberti S., Mondoni M., Piana A., Dessole F., Dessole M., Cherchi P.L., Dessole S., Sotgiu G. COVID-19 in pregnant women: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;252:543–558. doi: 10.1016/j.ejogrb.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chamseddine R.S., Wahbeh F., Chervenak F., Salomon L.J., Ahmed B., Rafii A. Pregnancy and Neonatal Outcomes in SARS-CoV-2 Infection: A Systematic Review. J. Pregnancy. 2020;2020:4592450. doi: 10.1155/2020/4592450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chi H., Chiu N.C., Tai Y.L., Chang H.Y., Lin C.H., Sung Y.H., Tseng C.Y., Liu L.Y., Lin C.Y. Clinical features of neonates born to mothers with coronavirus disease-2019: A systematic review of 105 neonates. J. Microbiol. Immunol. Infect. 2021;54:69–76. doi: 10.1016/j.jmii.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Della Gatta A.N., Rizzo R., Pilu G., Simonazzi G. Coronavirus disease 2019 during pregnancy: A systematic review of reported cases. Am. J. Obstet. Gynecol. 2020;223:36–41. doi: 10.1016/j.ajog.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deniz M., Tezer H. Vertical transmission of SARS CoV-2: A systematic review. J. Matern. Fetal Neonatal Med. 2020:1–8. doi: 10.1080/14767058.2020.1793322. [DOI] [PubMed] [Google Scholar]
- 45.Dhir S.K., Kumar J., Meena J., Kumar P. Clinical Features and Outcome of SARS-CoV-2 Infection in Neonates: A Systematic Review. J. Trop. Pediatr. 2020 doi: 10.1093/tropej/fmaa059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Di Mascio D., Khalil A., Saccone G., Rizzo G., Buca D., Liberati M., Vecchiet J., Nappi L., Scambia G., Berghella V., et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2020;2:100107. doi: 10.1016/j.ajogmf.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diriba K., Awulachew E., Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: A systematic review and meta-analysis. Eur. J. Med. Res. 2020;25:39. doi: 10.1186/s40001-020-00439-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dube R., Kar S.S. COVID-19 in pregnancy: The foetal perspective-a systematic review. BMJ Paediatr. Open. 2020;4:e000859. doi: 10.1136/bmjpo-2020-000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dubey P., Reddy S.Y., Manuel S., Dwivedi A.K. Maternal and neonatal characteristics and outcomes among COVID-19 infected women: An updated systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;252:490–501. doi: 10.1016/j.ejogrb.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duran P., Berman S., Niermeyer S., Jaenisch T., Forster T., de Leon R.G.P., De Mucio B., Serruya S. COVID-19 and newborn health: Systematic review. Rev. Panam. Salud Publica. 2020;44:e54. doi: 10.26633/RPSP.2020.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elshafeey F., Magdi R., Hindi N., Elshebiny M., Farrag N., Mahdy S., Sabbour M., Gebril S., Nasser M., Kamel M., et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int. J. Gynecol. Obstet. 2020;150:47–52. doi: 10.1002/ijgo.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Galang R.R., Chang K., Strid P., Snead M.C., Woodworth K.R., House L.D., Perez M., Barfield W.D., Meaney-Delman D., Jamieson D.J., et al. Severe Coronavirus Infections in Pregnancy: A Systematic Review. Obstet Gynecol. 2020;136:262–272. doi: 10.1097/AOG.0000000000004011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gao Y.-J., Ye L., Zhang J.-S., Yin Y.-X., Liu M., Yu H.-B., Zhou R. Clinical features and outcomes of pregnant women with COVID-19: A systematic review and meta-analysis. BMC Infect. Dis. 2020;20:564. doi: 10.1186/s12879-020-05274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gordon M., Kagalwala T., Rezk K., Rawlingson C., Ahmed M.I., Guleri A. Rapid systematic review of neonatal COVID-19 including a case of presumed vertical transmission. BMJ Paediatr. Open. 2020;4:e000718. doi: 10.1136/bmjpo-2020-000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Han Y., Ma H., Suo M., Han F., Wang F., Ji J., Ji J., Yang H. Clinical manifestation, outcomes in pregnant women with COVID-19 and the possibility of vertical transmission: A systematic review of the current data. J. Perinat. Med. 2020;48:912–924. doi: 10.1515/jpm-2020-0431. [DOI] [PubMed] [Google Scholar]
- 56.Hassanipour S., Faradonbeh S.B., Momeni K., Heidarifard Z., Khosousi M.-J., Khosousi L., Ameri H., Arab-Zozani M. A systematic review and meta-analysis of pregnancy and COVID-19: Signs and symptoms, laboratory tests, and perinatal outcomes. Int. J. Reprod. Biomed. 2020;18:1005–1018. doi: 10.18502/ijrm.v18i12.8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huntley B.J.F., Huntley E.S., Di Mascio D., Chen T., Berghella V., Chauhan S.P. Rates of Maternal and Perinatal Mortality and Vertical Transmission in Pregnancies Complicated by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Co-V-2) Infection: A Systematic Review. Obstet. Gynecol. 2020;136:303–312. doi: 10.1097/AOG.0000000000004010. [DOI] [PubMed] [Google Scholar]
- 58.Islam M.M., Poly T.N., Walther B.A., Yang H.C., Wang C.-W., Hsieh W.-S., Atique S., Salmani H., Alsinglawi B., Lin M.C., et al. Clinical Characteristics and Neonatal Outcomes of Pregnant Patients With COVID-19: A Systematic Review. Front. Med. 2020;7:909. doi: 10.3389/fmed.2020.573468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jafari M., Pormohammad A., Neshin S.A.S., Ghorbani S., Bose D., Alimohammadi S., Basirjafari S., Mohammadi M., Rasmussen-Ivey C., Razizadeh M.H., et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2020:e2208. doi: 10.1002/rmv.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Juan J., Gil M.M., Rong Z., Zhang Y., Yang H., Poon L.C. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: Systematic review. Ultrasound Obstet. Gynecol. 2020;56:15–27. doi: 10.1002/uog.22088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karabay M., Cinar N., Suzan O.K., Caka S.Y., Karabay O. Clinical characteristics of confirmed COVID-19 in newborns: A systematic review. J. Matern. Fetal Neonatal Med. 2020 doi: 10.1080/14767058.2020.1849124. [DOI] [PubMed] [Google Scholar]
- 62.Kasraeian M., Zare M., Vafaei H., Asadi N., Faraji A., Bazrafshan K., Roozmeh S. COVID-19 pneumonia and pregnancy; a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2020 doi: 10.1080/14767058.2020.1763952. [DOI] [PubMed] [Google Scholar]
- 63.Khalil A., Kalafat E., Benlioglu C., O’Brien P., Morris E., Draycott T., Thangaratinam S., Le Doare K., Heath P., Ladhani S., et al. SARS-CoV-2 infection in pregnancy: A systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinicalMedicine. 2020;25:100446. doi: 10.1016/j.eclinm.2020.100446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lopes de Sousa Á.F., Carvalho H.E.F.D., Oliveira L.B.D., Schneider G., Camargo E.L.S., Watanabe E., de Andrade D., Fernandes A.F.C., Mendes I.A.C., Fronteira I. Effects of COVID-19 Infection during Pregnancy and Neonatal Prognosis: What Is the Evidence? Int. J. Environ. Res. Public Health. 2020;17:4176. doi: 10.3390/ijerph17114176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matar R., Alrahmani L., Monzer N., Debiane L.G., Berbari E., Fares J., Fitzpatrick F., Murad M.H. Clinical presentation and outcomes of pregnant women with coronavirus disease 2019: A systematic review and meta-analysis. Clin. Infect. Dis. 2021;72:521–533. doi: 10.1093/cid/ciaa828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Melo G.C., Araújo K. COVID-19 infection in pregnant women, preterm delivery, birth weight, and vertical transmission: A systematic review and meta-analysis. Cad. Saude Publica. 2020;36:e00087320. doi: 10.1590/0102-311x00087320. [DOI] [PubMed] [Google Scholar]
- 67.Mirbeyk M., Saghazadeh A., Rezaei N. A systematic review of pregnant women with COVID-19 and their neonates. Arch. Gynecol. Obstet. 2021;304:5–38. doi: 10.1007/s00404-021-06049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Muhidin S., Behboodi Moghadam Z., Vizheh M. Analysis of Maternal Coronavirus Infections and Neonates Born to Mothers with 2019-nCoV; a Systematic Review. Arch. Acad. Emerg. Med. 2020;8:e49. [PMC free article] [PubMed] [Google Scholar]
- 69.Najafi T.F., Dashti S., Bahri N. Vertical Transmission of COVID-19: A Systematic Review. Arch. Pediatr. Infect. Dis. 2021;9:e108769. doi: 10.5812/pedinfect.108769. [DOI] [Google Scholar]
- 70.Neef V., Buxmann H., Rabenau H.F., Zacharowski K., Raimann F.J. Characterization of neonates born to mothers with SARS-CoV-2 infection: Review and meta-analysis. Pediatr. Neonatol. 2021;62:11–20. doi: 10.1016/j.pedneo.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Oltean I., Tran J., Lawrence S., Ruschkowski B.A., Zeng N., Bardwell C., Nasr Y., de Nanassy J., El Demellawy D. Impact of SARS-CoV-2 on the clinical outcomes and placental pathology of pregnant women and their infants: A systematic review. Heliyon. 2021;7:e06393. doi: 10.1016/j.heliyon.2021.e06393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Oshay R.R., Chen M.Y.C., Fields B.K.K., Demirjian N.L., Lee R.S., Mosallaei D., Gholamrezanezhad A. COVID-19 in pregnancy: A systematic review of chest CT findings and associated clinical features in 427 patients. Clin. Imaging. 2021;75:75–82. doi: 10.1016/j.clinimag.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pastick K.A., Nicol M.R., Smyth E., Zash R., Boulware D.R., Rajasingham R., McDonald E.G. A Systematic Review of Treatment and Outcomes of Pregnant Women With COVID-19-A Call for Clinical Trials. Open Forum Infect. Dis. 2020;7:ofaa350. doi: 10.1093/ofid/ofaa350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pettirosso E., Giles M., Cole S., Rees M. COVID-19 and pregnancy: A review of clinical characteristics, obstetric outcomes and vertical transmission. Aust. N. Z. J. Obstet. Gynaecol. 2020;60:640–659. doi: 10.1111/ajo.13204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Raschetti R., Vivanti A.J., Vauloup-Fellous C., Loi B., Benachi A., De Luca D. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat. Commun. 2020;11:5164. doi: 10.1038/s41467-020-18982-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rodrigues C., Baía I., Domingues R., Barros H. Pregnancy and Breastfeeding During COVID-19 Pandemic: A Systematic Review of Published Pregnancy Cases. Front. Public Health. 2020;8:558144. doi: 10.3389/fpubh.2020.558144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thomas P., Alexander P.E., Ahmed U., Elderhorst E., El-Khechen H., Mammen M.J., Debono V.B., Aponte Torres Z., Aryal K., Brocard E., et al. Vertical transmission risk of SARS-CoV-2 infection in the third trimester: A systematic scoping review. J. Matern. Fetal Neonatal Med. 2020:1–8. doi: 10.1080/14767058.2020.1786055. [DOI] [PubMed] [Google Scholar]
- 78.Trippella G., Ciarcià M., Ferrari M., Buzzatti C., Maccora I., Azzari C., Dani C., Galli L., Chiappini E. COVID-19 in Pregnant Women and Neonates: A Systematic Review of the Literature with Quality Assessment of the Studies. Pathogens. 2020;9:485. doi: 10.3390/pathogens9060485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trocado V., Silvestre-Machado J., Azevedo L., Miranda A., Nogueira-Silva C. Pregnancy and COVID-19: A systematic review of maternal, obstetric and neonatal outcomes. J. Matern. Fetal Neonatal Med. 2020 doi: 10.1080/14767058.2020.1781809. [DOI] [PubMed] [Google Scholar]
- 80.Turan O., Hakim A., Dashraath P., Jeslyn W.J.L., Wright A., Abdul-Kadir R. Clinical characteristics, prognostic factors, and maternal and neonatal outcomes of SARS-CoV-2 infection among hospitalized pregnant women: A systematic review. Int. J. Gynaecol. Obstet. 2020;151:7–16. doi: 10.1002/ijgo.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Walker K.F., O’Donoghue K., Grace N., Dorling J., Comeau J.L., Li W., Thornton J.G. Maternal transmission of SARS-COV-2 to the neonate, and possible routes for such transmission: A systematic review and critical analysis. BJOG Int. J. Obstet. Gynaecol. 2020;127:1324–1336. doi: 10.1111/1471-0528.16362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang Z., Wang M., Zhu Z., Liu Y. Coronavirus disease 2019 (COVID-19) and pregnancy: A systematic review. J. Matern. Fetal Neonatal Med. 2020:1–4. doi: 10.1080/14767058.2020.1759541. [DOI] [PubMed] [Google Scholar]
- 83.Yang Z.Y., Liu Y. Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2: A Systematic Review. Am. J. Perinatol. 2020;37:1055–1060. doi: 10.1055/s-0040-1712161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yee J., Kim W., Han J.M., Yoon H.Y., Lee N., Lee K.E., Gwak H.S. Clinical manifestations and perinatal outcomes of pregnant women with COVID-19: A systematic review and meta-analysis. Sci. Rep. 2020;10:18126. doi: 10.1038/s41598-020-75096-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yoon S.H., Kang J.M., Ahn J.G. Clinical outcomes of 201 neonates born to mothers with COVID-19: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2020;24:7804–7815. doi: 10.26355/eurrev_202007_22285. [DOI] [PubMed] [Google Scholar]
- 86.Yuan J., Qian H., Cao S., Dong B., Yan X., Luo S., Zhou M., Zhou S., Ning B., Zhao L. Is there possibility of vertical transmission of COVID-19: A systematic review. Transl. Pediatr. 2021;10:423–434. doi: 10.21037/tp-20-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zaigham M., Andersson O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020;99:823–829. doi: 10.1111/aogs.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Arroyo-Sanchez A.S., Chirinos M.F.M., Egusquiza T.M., Rodriguez B.P., Arroyo-Sanchez A.S. Pregnant women with coronavirus disease 2019 and intrauterine vertical transmission: A systematic review. Rev. Peru. Ginecol. Obstet. 2020;66 doi: 10.31403/rpgo.v66i2277. [DOI] [Google Scholar]
- 89.Mayo Clinic C-Section. [(accessed on 1 July 2021)]. Available online: https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655.
- 90.Egloff C., Vauloup-Fellous C., Picone O., Mandelbrot L., Roques P. Evidence and possible mechanisms of rare maternal-fetal transmission of SARS-CoV-2. J. Clin. Virol. 2020;128:104447. doi: 10.1016/j.jcv.2020.104447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jeganathan K., Paul A.B. Vertical transmission of SARS-CoV-2: A systematic review. Obstet. Med. 2021:1753495X211038157. doi: 10.1177/1753495X211038157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Valdes G., Neves L., Anton L., Corthorn J., Chacon C., Germain A., Merrill D., Ferrario C., Sarao R., Penninger J. Distribution of angiotensin-(1-7) and ACE2 in human placentas of normal and pathological pregnancies. Placenta. 2006;27:200–207. doi: 10.1016/j.placenta.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 93.Li Y., Zhao R., Zheng S., Chen X., Wang J., Sheng X., Zhou J., Cai H., Fang Q., Yu F. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg. Infect. Dis. 2020;26:1335. doi: 10.3201/eid2606.200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020 doi: 10.1101/2020.01.26.919985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Xiong X., Wei H., Zhang Z., Chang J., Ma X., Gao X., Chen Q., Pang Q. Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19. J. Med. Virol. 2020;92:1657–1659. doi: 10.1002/jmv.25857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Demirjian A., Singh C., Tebruegge M., Herbert R., Draz N., Mirfenderesky M., Jones V., Hinstridge P., Seneviratne R., Myers R. Probable vertical transmission of SARS-CoV-2 infection. Pediatr. Infect. Dis. J. 2020;39:e257–e260. doi: 10.1097/INF.0000000000002821. [DOI] [PubMed] [Google Scholar]
- 97.Oncel M.Y., Akın I.M., Kanburoglu M.K., Tayman C., Coskun S., Narter F., Er I., Oncan T.G., Memisoglu A., Cetinkaya M. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with COVID-19 by Turkish Neonatal Society. Eur. J. Pediatr. 2021;180:733–742. doi: 10.1007/s00431-020-03767-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cao D., Yin H., Chen J., Tang F., Peng M., Li R., Xie H., Wei X., Zhao Y., Sun G. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: A retrospective study. Int. J. Infect. Dis. 2020;95:294–300. doi: 10.1016/j.ijid.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Leung J.S. Impact of COVID-19 as a vertical infection in late pregnancy. Hong Kong Med. J. 2020;26:271–272. doi: 10.12809/hkmj208655. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in this work were publicly available.