Abstract
Calcium phosphate cement (CPC) is a promising material used in the treatment of bone defects due to its profitable features of self-setting capability, osteoconductivity, injectability, mouldability, and biocompatibility. However, the major limitations of CPC, such as the brittleness, lack of osteogenic property, and poor washout resistance, remain to be resolved. Thus, significant research effort has been committed to modify and reinforce CPC. The mixture of CPC with various biological materials, defined as the materials produced by living organisms, have been fabricated by researchers and their characteristics have been investigated in vitro and in vivo. This present review aimed to provide a comprehensive overview enabling the readers to compare the physical, mechanical, and biological properties of CPC upon the incorporation of different biological materials. By mixing the bone-related transcription factors, proteins, and/or polysaccharides with CPC, researchers have demonstrated that these combinations not only resolved the lack of mechanical strength and osteogenic effects of CPC but also further improve its own functional properties. However, exceptions were seen in CPC incorporated with certain proteins (such as elastin-like polypeptide and calcitonin gene-related peptide) as well as blood components. In conclusion, the addition of biological materials potentially improves CPC features, which vary depending on the types of materials embedded into it. The significant enhancement of CPC seen in vitro and in vivo requires further verification in human trials for its clinical application.
Keywords: biomaterials, hydroxyapatite, polysaccharide, protein, transcription factor, platelet-rich plasma
1. Introduction
Bone defect refers to the absence of bone tissue at specific anatomical positions where it is typically present, often as sequelae of trauma, infection, or removal of bone tumours [1,2]. Our skeletal system can self-repair bone defects by undergoing five main healing processes, including hematoma, inflammation, tissue granulation, callus formation, and bone remodelling. A blood clot is formed immediately after an injury providing a provisional matrix. Platelet degranulation releases inflammatory cells and mediators to activate the inflammatory stage, attracting a large number of immune, mesenchymal, and endothelial cells. The tissue granulation phase ensues, whereby the aggregated cells stimulate angiogenesis, osteoprogenitor cell proliferation, and extracellular matrix production. Subsequently, the formation of soft and hard callus improves the stability of the defect. Finally, bone remodelling occurs whereby osteoclasts resorb primary bone followed by re-establishment of bone shape and structure [3]. Typically, a bone defect has an average recovery period of six to eight weeks [4].
Autologous or artificial bone grafting is the surgical method predominantly used to rectify bone defects. The lack of readily available grafts and donor site complications often limit the clinical application of autologous bone grafts even though it is the gold standard [2]. The use of natural bone substitutes has shifted towards synthetic bone substitutes as alternatives, such as calcium phosphate-based biomaterials, to fulfil the application demands. Calcium phosphate cement (CPC) is commonly used to repair bone defects as its chemical composition is identical to the bone mineral [5]. CPC offers attractive features such as good self-setting ability, injectability, mouldability, biocompatibility, osteoconductivity, resorbability, and feasibility in controlled drug delivery [6,7]. Hence, it is the most promising and convenient injectable filler material to be used at the bone defect site. However, the critical limitations of CPC include poor mechanical strength, high brittleness, poor anti-washout behaviour, and lack of osteogenic property [8,9] (Table 1). Researchers have invested much effort to enhance their physical, mechanical, and biological performance by adding biological materials into the composition of CPC. In this context, biological materials refer to materials that are derived from living organisms. The enhancement of CPC using naturally derived materials such as bone-related transcription factors, proteins, polysaccharides, blood components, and their combinations has been demonstrated in previous scientific studies.
Table 1.
The characteristics of ideal bone cement.
| Characteristics | Criteria for an Ideal Bone Cement |
|---|---|
| Self-setting ability | The bone cement should harden in situ, forming solid hydroxyapatite. |
| Injectability | The bone cement could be pushed out through a syringe without separation of the liquid and powder that composed it. |
| Mouldability | The bone cement could be moulded according to the shape of a bone cavity |
| Biocompatibility | The bone cement should not cause any local or systemic adverse response. |
| Osteoconductivity | The bone cement should encourage host bone cells, capillaries, and tissue to move into it to facilitate bone repair. |
| Resorbability | The bone cement should be resorbable by the body. |
| Feasibility in controlled drug delivery | The bone cement could be designed to deliver a drug at a predetermined rate. |
| Mechanical strength | The bone cement could withstand application of force without failure and deformation. |
| Brittleness | The bone cement should not be fractured easily when subjected to stress. |
| Anti-washout | The bone cement should be resistant to segregation under washing action. |
| Osteogenic property | The bone cement should encourage new bone formation by osteoblasts. |
Herein, the reinforcement of CPC using various biological materials was summarised. The shortcomings of the current research methodology, potential research gap, and future direction have also been addressed. This review aims to discuss the broad prospects of CPC in bone tissue repair and engineering by focusing on the advantages of different biological materials in overcoming the drawbacks of CPC.
2. Literature Search
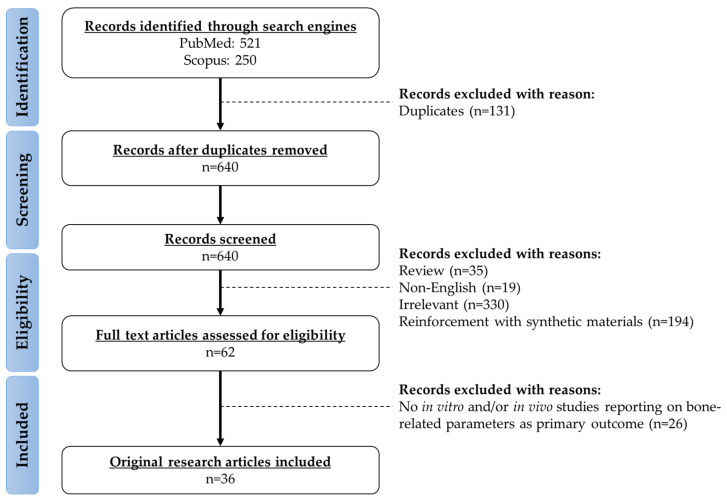
A customised literature search was performed using the PubMed/MEDLINE and Scopus search engines with keywords: “(enhancement OR improvement OR reinforcement) AND (calcium phosphate cement) AND (bone OR osteoporosis OR fracture OR osteoblast OR osteoclast OR osteocyte)”. The search resulted in 521 and 250 items from the search engines respectively from inception till 15 July 2021. Duplicate articles were excluded. The titles and abstracts were initially screened based on the inclusion and exclusion criteria. The main focus of this review was to summarise the characteristics of CPC upon the incorporation of biological materials originated from living organisms. The exclusion criteria were: (a) non-English articles; (b) books, book chapters, commentaries, conference papers, letters to the editor, meta-analysis, reviews, and theses; (c) CPC reinforced with synthetic materials (such as chemicals, drugs, synthetic polymers, carbon fibres, carbon nanotubes, and metals/transition metals). Subsequently, full-text articles were screened. Original research articles reporting the effects of biological materials-enhanced CPC on bone parameters as the primary outcomes using in vitro and in vivo experimental approaches were retrieved. For example, studies that used the biological material-enhanced CPC as a scaffold for bone cells/bone progenitor cells seeding or as implant material being filled at the bone defect site of animals were included. A total of 36 related original research articles was included in this review. The framework of evidence acquisition has been summarised in Figure 1.
Figure 1.
The framework for the selection of relevant studies.
3. The Enhancement of CPC
3.1. Bone-Related Transcription Factors
Bone morphogenetic protein (BMP) is a group of growth factors that belong to the transforming growth factor-beta (TGF-β) superfamily. Signal transduction through the interaction between BMP and TGF-β with their receptors, i.e., bone morphogenetic protein receptor (BMPR) and transforming growth factor-beta receptor (TGF-βR), results in the phosphorylation of SMAD proteins and transcription of Runx-2 (a master regulator of osteoblastogenesis). Apart from the potent osteoinductive properties, BMP and TGF-β have other non-skeletal actions. For example, they enhance the development of new blood vessels and restoration of microcirculation by promoting the synthesis of pro-angiogenic factors that provide oxygen and nutrients to the injured site, stimulate the formation of tip cells and sprouting, as well as migration and proliferation of endothelial cells [10,11]. Hence, BMP and TGF-β have been potentially used as a new adjunct to graft materials for bone regeneration (Table 2).
Table 2.
The bone protecting effects of CPC enhanced by BMP-2 and TGF-β.
| Enhancer | Characteristics of Enhanced CPC | Type of Study | Type of Cell, Sample, and Animal Model | Outcomes Observed in Animals | Reference |
|---|---|---|---|---|---|
| rhTGF-β1 | - | In vitro | Pre-osteoblastic and osteoblastic cells obtained from collagenase-treated fragments of adult rat long bones | Cell differentiation: ↑, ALP: ↑ | [12] |
| rhBMP-2 | - | In vitro | Myoblastic precursor cells | ALP: ↑, COL1: ↑, OCN: ↑, Runx-2: ↑ | [13] |
| In vivo | Bone defect at femur of female New Zealand rabbits | BV/TV: ↑, residue of material: ↓, newly formed bone area: ↑ | |||
| rhBMP-2 | Maximum compressive strength: ↑ | In vivo | Critical defect at the middle of the radius of male New Zealand rabbits | BMC: ↑, BMD: ↑, bone formation: ↑, bone regeneration: ↑, maximum load: ↑ | [14] |
| BMP-2 | - | In vivo | Bone defect at femoral metaphysis of ovariectomised rats | BV/TV: ↑, Tb.N: ↑, Tb.Th: ↑, Tb.Sp: ↓, newly formed bone: ↑, percentage of remaining biomaterial: ↓, ultimate load: ↑ | [15] |
Abbreviations: ALP, alkaline phosphatase; BMC, bone mineral content; BMD, bone mineral density; BV/TV: bone volume/total volume; COL1, type I collagen; CPC, calcium phosphate cement; OCN: osteocalcin; rhBMP-2, recombinant human bone morphogenetic protein-2; rhTGF-β1, recombinant human transforming growth factor-beta 1; Runx-2, runt-related transcription factor 2; Tb.N, trabecular number; Tb.Sp, trabecular separation; Tb.Th, trabecular thickness; ↑: increase/improve, ↓: decrease/inhibit.
An earlier in vitro study pointed out that the addition of recombinant human TGF-β1 (rhTGF-β1) to CPC increased ALP activity in two cell populations, the pre-osteoblastic and osteoblastic cells isolated from adult rat long bones [12]. The incorporation of recombinant human BMP-2 (rhBMP-2) increased the compressive strength of the CPC scaffold [14]. A study by Zhang et al. demonstrated that the viability of myoblastic precursor cells was promoted and the expression of osteogenic genes (including alkaline phosphatase (ALP), type I collagen (COL1), osteocalcin (OCN), and Runt-related transcription factor 2 (Runx-2)) were elevated when seeded on CPC/rhBMP-2 scaffold. Using New Zealand white rabbits as an animal model of femoral bone defect, the same group of investigators reported that the residue of material (CPC scaffold with rhBMP-2) was decreased while bone ingrowth and newly formed bone area were increased at the defect site after eight weeks of implantation [13]. Another group of researchers implanted a CPC scaffold loaded with rhBMP-2 at the defect area in the middle radius of white rabbits. Qualitative assessment of bone defect using radiograph and micro-computed tomography indicated that the defect area was filled by the implanted material and callus formation was observable as early as two weeks after implantation. The animals with defect areas implanted with CPC and rhBMP-2 also had higher bone mineral content (BMC), bone mineral density (BMD), and maximum load compared to those animals without any implants [14]. Recently, Tao et al. investigated the effects of strontium-modified CPC dripped with a single-dose local administration of BMP-2 on healing bone defects in osteoporotic rats induced by ovariectomy. The improvement of bone defect healing was noted in animals eight weeks after implantation with strontium-modified CPC in the presence of BMP-2 local administration, evidenced by denser bone microstructure, greater newly formed bone, decreased percentage of remaining biomaterials, and higher ultimate load [15].
Overall, the scientific evidence showed that BMP-2 enhanced the maximum compressive strength of CPC. Several in vitro and in vivo studies consistently supported that BMP-2 stimulated osteogenic differentiation leading to enhanced bone formation and regeneration in animals with cavity defects.
3.2. Proteins
Proteins, such as silk fibroin and amino acids, have been used as enhancers to improve the mechanical properties of CPC (Table 3). Silk fibroin is a natural protein biopolymer found abundantly in silkworms, Bombyx mori. Silk has been traditionally used as a luxury raw material in the textile industry. The advancement in technology revealed that silk fibroin is a biomaterial with excellent biocompatibility and natural strength, suggesting its wide application for drug delivery, vascular tissue regeneration, wound treatment, and bone tissue scaffold [16]. The reinforcement of CPC by alkaline-treated silk fibroin was developed by Hu et al. and the features were evaluated. The compressive strength was improved, setting time was shorter, no collapse was observed, and injectability was increased in cement after adding silk fibroin solution. Ex vivo analysis on sheep vertebrae implanted with CPC containing silk fibroin showed increased mechanical strength and stiffness. The MC3T3-E1 cells seeded on silk fibroin/CPC showed increased proliferation and normal cell morphology [17].
Table 3.
The bone protecting effects of CPC enhanced by proteins.
| Enhancer | Characteristics of Enhanced CPC |
Type of Study | Type of Cell, Sample, and Animal Model | Outcomes Observed in Animals | Reference |
|---|---|---|---|---|---|
| Alkaline-treated silk fibroin | Compressive strength: ↑, setting time: ↓, anti-washout: ↑, injectability: ↑ | Ex vivo | Sheep vertebra | Compressive strength: ↑, stiffness: ↑ | [17] |
| In vitro | MC3T3-E1 cells | No cytotoxicity, good cell morphology | |||
| Lysine | Compressive strength: ↑, apparent porosity: ↑ | In vitro | Bone mesenchymal stem cells | ALP: ↑, Runx-2: ↑, COL1: ↑, OCN: ↑ | [18] |
| Arginine-glycine-aspartate | Flexural strength: ↔, elastic modulus: ↔, work of fracture: ↔ | In vitro | Human umbilical cord mesenchymal stem cells | Viable cells: ↑, ALP: ↑, COL1: ↑, OCN: ↑, Runx-2: ↑, mineralisation: ↑ | [19] |
| Arginine-glycine-aspartate | Setting time: ↔, flexural strength: ↔, elastic modulus: ↔ | In vitro | Human umbilical cord mesenchymal stem cells | Cell density: ↑, ALP: ↑, OCN: ↑, COL1: ↑, mineralisation: ↑ | [20] |
| N-acetyl cysteine loaded silk fibroin | - | Ex vivo | Sheep vertebra | Compressive strength: ↑, stiffness: ↑ | [21] |
| In vivo | Bone defect at distal femoral metaphysis of male Sprague-Dawley rats | Maximum force: ↑, BV/TV: ↑, remaining material in bone: ↓ | |||
| In vitro | Rat bone marrow mesenchymal stromal cells | ALP: ↑, mineralisation: ↑, Runx-2: ↑, OSX: ↑, OCN: ↑, β-catenin: ↑ | |||
| Collagen | Flexural strength: ↑ | In vitro | Human umbilical cord mesenchymal stem cells | Mineral nodules: ↑, extracellular matrix formation: ↑, cell number: ↑, ALP: ↑, OCN: ↑, COL1: ↑, Runx-2: ↑, mineralisation: ↑ | [22] |
| Collagen microsphere | - | In vivo | Bone defect at femoral condyles of female New Zealand rabbits | New bone formation: ↑ | [23] |
| Gelatine | Initial and final setting time: ↓, compressive strength: ↑, elastic displacement: ↑ | In vitro | Human osteosarcoma (G-292) cells | Cell number: ↑, ALP: ↑ | [24] |
| Gelatine | Setting time: ↓, compressive strength: ↑ | In vitro | Human osteoblast-like (MG63) cells | Cell proliferation: ↑, ALP: ↑, type 1 pro-collagen: ↑, TGF-β1: ↑ | [25] |
| Elastin-like polypeptide | Micro-hardness: ↑, compressive strength: ↑, initial and final setting time: ↑, anti-washout, denser microstructure with fewer pores, crystallite formation: ↑ | In vitro | NIH3T3 cells | Viable cells, normal cell morphology, normal spreading pattern, normal cell distribution, no nuclear condensation in cells | [26] |
| CGRP | Pore size distribution: ↔, compressive strength: ↔ | In vitro | Rat bone marrow mesenchymal stromal cells | Cell proliferation: ↑, ALP: ↑, BMP-2: ↑, osteonectin: ↑, Runx-2: ↑ | [27] |
| Bone sialoprotein | - | In vitro | Human primary osteoblasts | Cell number: ↑, ALP: ↔, OPN: ↔, OSX: ↑, Runx-2: ↔, osteonectin: ↑ | [28] |
| Bone sialoprotein | - | In vivo | Bone defect at femoral condyles of male Wistar rats | BV/TV: ↔, bone ingrowth: ↔ | [29] |
Abbreviations: ALP, alkaline phosphatase; BMP-2, bone morphogenetic protein-2; BV/TV, bone volume/total volume; CGRP, calcitonin gene-related peptide; COL1, type I collagen; CPC, calcium phosphate cement; OCN, osteocalcin; OPN, osteopontin; OSX, osterix; Runx-2, runt-related transcription factor 2; ↑, increase/improve; ↓, decrease/inhibit; ↔, no change.
Amino acids are organic compounds consisting of two functional groups (amino (–NH2) and carboxyl (–COOH)) and a side chain. Lysine is an essential amino acid that must be obtained from the diet. It is important for the synthesis of protein, hormone, enzyme, collagen, elastin, and absorption of intestinal calcium, suggesting its role in maintaining skeletal homeostasis [30]. Thus, lysine has been incorporated into CPC to promote osteogenic activity. A recent study examined the characteristics of CPC with lysine as well as the expression of osteogenic markers in bone mesenchymal stem cells seeded on lysine-incorporated CPC. Results showed that the presence of lysine in CPC improved mechanical strength and apparent porosity in a lysine-content-dependent manner [18]. The pore size of a scaffold regulates osteogenesis as it affects bone cell adhesion, proliferation, and distribution. Scaffold with high porosity allows adequate diffusion of nutrients, bone cell migration, and provides sufficient surface area for cell-biomaterial interactions [31]. In this context, the scaffold porosity should be balanced with the mechanical needs for bone tissue at the defect site as mechanical strength decreases with increasing porosity. The in vitro findings from a study by Shi et al. showed that the ALP activity and osteogenic protein expression were increased after seven days of culturing bone mesenchymal stem cells on CPC incorporated with lysine [18].
A tripeptide motif, consisting of amino acids arginine, glycine, and aspartate, is initially identified as an amino acid sequence that facilitates cell attachment. It is present in various proteins of the extracellular matrix, including fibronectin, vitronectin, and fibrinogen. This tripeptide motif has a strong affinity towards integrins, the transmembrane glycoproteins involved in anchoring cells to the extracellular matrix [32]. It is known that integrins are expressed in various types of cells including leukocytes [33], macrophages [34], endothelial cells [35], and bone cells [36,37]. Recruitment of these cells through recognition of the arginine-glycine-aspartate motif on biomaterial surface is important for tissue regeneration, including the regeneration of bone defects. It is worth mentioning that the addition of peptide sequences arginine-glycine-aspartate motif into CPC did not compromise the setting time, flexural strength, elastic modulus, and work to fracture of CPC [19,20]. The adding of arginine-glycine-aspartate improved human umbilical cord mesenchymal stem cell attachment. Faster cell proliferation, increased cell number, higher osteogenic gene expression as well as higher mineral concentration were noted, indicating osteogenic differentiation of human umbilical cord mesenchymal stem cells [19,20].
N-acetyl cysteine (NAC) is an acetylated product of cysteine, a semi-essential amino acid naturally found in the human body. It is a known medication used to treat overdose of paracetamol through its action as the precursor of glutathione to conjugate and deactivate toxic N-acetyl-p-benzoquinone imine metabolised from paracetamol [38]. The anti-oxidative ability of NAC suggests its potential in promoting bone health and osteoinduction. Recently, Feng et al. prepared a CPC composite by mixing NAC loaded silk fibroin solution with α-tricalcium phosphate (α-TCP) and tested the osteogenic properties ex vivo, in vivo, and in vitro. In the ex vivo experiment, a bone defect (6 mm) was created by surgical drilling through the vertebral body perpendicular to the sagittal plane of the excised sheep lumbar vertebra and filled with silk fibroin-NAC/α-TCP. Higher compressive strength and stiffness were detected in the lumbar vertebra after being filled with silk fibroin-NAC/α-TCP. Maximum force, BV/TV, and rate of material degradation were increased in the rats subjected to surgical drill to create a critical-size bone defect at femoral condyle which was filled with silk fibroin-NAC/α-TCP. An in vitro study using rat bone marrow mesenchymal stromal cells showed higher ALP activity, mineralisation, and osteogenic genes expression after being seeded onto cement with the addition of silk fibroin and NAC. These osteogenic actions were inhibited after the addition of Dickkopf-related protein-1 (DKK-1, a known Wnt inhibitor) in the culture, thus suggesting the postulated signalling pathway involved in the osteogenic enhancement was mediated through the activation of Wnt/β-catenin [21].
Collagen consists of amino acids that are bound together to form a triple collagen helix, which has a main structural function in connective tissues, such as bone, cartilage, tendon, ligament, and skin. Collagen has been primarily used for cosmetic, nutraceutical, pharmaceutical, and medical applications. Previous investigations indicated that dietary hydrolysed collagen increased osteoblast activity, leading to improved bone architecture and biomechanical resistance in osteoporotic mice [39]. In view of the potential skeletal-promoting effects of collagen, its combination with CPC had better bone repair effects mainly due to the biomimetic properties of CPC that resembled the composition of natural bone. Collagen had been added into composite scaffolds to enhance osteoblast proliferation and load-bearing capacity [22]. The cell attachment, proliferation, and osteogenic differentiation of human umbilical cord mesenchymal stem cells on the collagen-CPC scaffold were investigated. Collagen fibres in CPC improved the mechanical properties. The presence of mineral nodules, increase in an extracellular matrix formation, cell numbers, and higher osteogenic expression were noted in human umbilical cord mesenchymal stem cells cultured on CPC with collagen than those on CPC without collagen [22]. Likewise, the presence of collagen microsphere in injectable cement paste facilitated new bone formation after it was implanted at a defect site in the femoral condyles of female New Zealand rabbits [23].
Gelatine is a colourless, tasteless, odourless, and translucent protein product from animal-derived collagen. It dissolves in warm water and forms a jelly-like texture at lower temperatures, providing a binding force [40]. Gelatine has been used in food and cosmetic applications, acting as stabiliser and thickener in foods or texturiser in conditioners and moisturisers. Gelatine is less antigenic than collagen and binds well to tricalcium phosphate, suggesting that it is an excellent material for bone replacement [41]. Two groups of researchers synthesised an injectable homogeneous paste comprising of CPC with or without gelatine. The initial and final setting time was decreased whereas the mechanical strength was increased by adding gelatine into CPC. In vitro experiment showed that the cell number, proliferation, ALP activity, type 1 procollagen, and TGF-β1 level were induced in G-292 and MG63 osteoblastic cells when seeded on gelatine-containing CPC as compared to those without gelatine additives [24,25].
The elastin-like polypeptide is a protein-based polypeptide that consists of valine-proline-glycine-Xaa-glycine (Val-Pro-Gly-Xaa-Gly) pentapeptide repeats, in which Xaa can be a variable naturally occurring amino acid, except for proline [42]. It has been developed using genetic engineering technology with excellent properties of biocompatibility, non-immunogenic, non-toxic, and controllable degradation [26]. The addition of elastin-like polypeptide into CPC increased micro-hardness, compressive strength, washout resistance as well as initial and final setting time. The microstructure of the biomaterial was denser with fewer pores, larger crystallites, and fewer sharp edges, indicating the ability of the elastin-like polypeptide to stabilise CPC. Mouse embryonic fibroblast (NIH3T3) cells remained viable and displayed normal cell morphology, spreading pattern, cell distribution, and no nuclear condensation after being cultured on CPC supplemented with elastin-like polypeptide [26].
Calcitonin gene-related peptide (CGRP) is an amino acid peptide mainly produced in both central and peripheral neurons. It is primarily released from innervating sensory fibres and possesses potent vasodilator activity. Thus, it is implicated in the pathophysiological conditions involving the cardiovascular system, wound healing, and nociception [43]. The role of CGRP on bone remodelling and regeneration has also been reported within in vivo studies. CGRP enhanced blood vessel formation and bone regeneration in a rat model of distraction osteogenesis [44]. Mice with CGRP deficiency subjected to a femoral osteotomy had reduced bone-forming osteoblast number, higher rate of incomplete callus bridging, and fracture non-union [45]. The enrichment of CPC with CGRP did not alter pore size distribution and compressive strength of CPC, but this material increased cell proliferation, ALP activity, expression of BMP-2, osteonectin, and Runx-2 in rat bone marrow mesenchymal stem cells [27].
Bone sialoprotein is a non-collagenous protein synthesised by mineralising connective tissues, such as bone, dentin, cementum, and calcified cartilage tissues [46]. It regulates hydroxyapatite crystal formation in bones and teeth as well as contains an arginine-glycine-aspartate sequence to attract cells and support cell adherence [47,48]. As a result, higher numbers of osteoblast cells grew on the bone sialoprotein-functionalised CPC scaffolds compared to the untreated CPC scaffolds. However, significant changes in the expression of osteogenic genes were not detected among the scaffolds coated with and without bone sialoprotein [28]. Subsequently, the same group of investigators investigated the effects of bone sialoprotein-coated CPC on bone formation in a femoral defect rat model. Their findings indicated that the implantation of the bone sialoprotein-CPC scaffold into the defect site caused minimal changes in bone regeneration and ingrowth after 8 weeks [29].
In general, most of the proteins improved washout resistance, injectability, compressive strength, and reduced the setting time of CPC. Exceptions were seen in the arginine-glycine-aspartate motif, elastin-like polypeptide, and CGRP. The tripeptide motif was insufficient in enhancing the biomechanical strength of CPC. Elastin-like polypeptide delayed the setting reaction of CPC, mainly attributed to their interaction which decreased the hydration of CPC. Meanwhile, the enrichment of CGRP did not affect the compressive strength and pore size distribution of CPC. These characteristics might be the challenges for its clinical applications. Furthermore, different types of proteins have different effects on pore size distribution. For instance, lysine increased the apparent porosity of CPC whereas elastin-like polypeptide-supplemented CPC had a smaller pore size indicating denser microstructure. In terms of biological performance, favourable improvements were noted by supplementing proteins into CPC with increased cell viability and osteogenic activity. However, the coating of bone sialoprotein on CPC supported cell attachment, but a lesser tendency towards osteogenic gene upregulation and bone formation.
3.3. Polysaccharides
Polysaccharides, including cellulose, chitosan, hyaluronic acid, and alginate, have received much attention as biomaterials for bone regeneration (Table 4). Cellulose is the most abundant organic biopolymer with the formula of (C6H10O5)n. It is a polysaccharide that consists of linear chains of repeated β-D-glucopyranose units linked by β-1,4-glycosidic bonds. Cellulose can be derived from plants, algae, and bacteria. Cellulose secreted by gram-negative bacteria has a similar molecular structure but exhibits several advantages over plant-derived cellulose, such as high purity, tensile strength, and large surface area. These intrinsic characteristics make it an ideal biomaterial in various medical applications, such as wound dressings, drug delivery, skeletal and cartilage substitutes [49]. A study by Zhang et al. reported that the bacterial cellulose-reinforced CPC composite had higher thermal stability and compressive strength than CPC. The composite also promoted cell growth, cell proliferation and displayed higher cell survival than CPC when seeded with MC3T3-E1 cells, indicating improved biocompatibility [50].
Table 4.
The bone protecting effects of CPC enhanced by polysaccharides.
| Enhancer | Characteristics of Enhanced CPC |
Type of Study | Type of Cell, Sample, and Animal Model | Outcomes Observed in Animals | Reference |
|---|---|---|---|---|---|
| Bacterial cellulose | Thermal stability: ↑, compressive strength: ↑ | In vitro | MC3T3-E1 cells | Cell growth and proliferation: ↑ | [50] |
| Chitosan | - | In vitro | Osteoblastic cells | ALP: ↑ | [51] |
| Chitosan | Flexural strength: ↑, elastic modulus: ↑ | In vitro | Rat bone marrow mesenchymal stem cells | ALP: ↑ | [52] |
| Chitosan | Compressive strength: ↑ | In vivo | Bone defect at radius of mature dogs | Amount of implant debris: ↓, new bone callus formation: ↑ | [53] |
| Hyaluronic acid | - | In vitro | Osteoblastic cells | ALP: ↑ | [51] |
| Hyaluronic acid | Compressive strength: ↑ | In vitro | Human bone marrow mesenchymal stromal cells | ALP: ↑, OPN: ↑, Runx-2: ↑ | [54] |
| In vivo | Bone defect at metaphyseal region of medial tibia in female Sprague-Dawley rats | BV/TV: ↑, Tb.Pf: ↑, BMD: ↑, bone and vessel formation: ↑, mineralisation: ↑, OCN: ↑, COL1: ↑, BMP-2: ↑ | |||
| Alginate | Injectability: ↑, cohesion: ↑, compressive strength: ↑, Young’s modulus: ↑, setting time: ↔ | In vitro | Human osteoblast-like cells | Viable cells: ↑ | [55] |
| Alginate hydrogel microbeads | Flexural strength: ↑, work of failure: ↑ | In vitro | Human umbilical cord mesenchymal stem cells | ALP: ↑, OCN: ↑, COL1: ↑, OSX: ↑ | [56] |
Abbreviations: ALP, alkaline phosphatase; BMD, bone mineral density; BMP-2, bone morphogenetic protein-2; BV/TV, bone volume/total volume; COL1, type I collagen; CPC, calcium phosphate cement; OCN, osteocalcin; OPN, osteopontin; OSX, osterix; Runx-2, Runt-related transcription factor 2; Tb.Pf, trabecular pattern factor; ↑, increase/improve; ↓, decrease/inhibit; ↔, no change.
Chitosan is a natural linear polysaccharide derived from chitin, the second most abundant polysaccharide after cellulose. It can be extracted from the exoskeleton of insects, the hard outer skeleton of shellfish (including crab, lobster, and shrimp), and the fungi cell wall. Chitosan is a versatile biomaterial due to non-antigenicity, biocompatibility, biodegradability, non-toxicity, good adsorption, and anti-bacterial potency [57]. However, its application is limited by its insolubility in neutral and aqueous solutions [58]. The addition of chitosan into other materials, such as ceramics, composites, and hydrogels, broadens its application as a scaffold component with new functional properties. The differences in elastic modulus, compressive and flexural strength between CPC reinforced with chitosan and those without chitosan were significant, with the former group higher than the latter group [52,53]. In vitro, the ALP activity was higher in rat bone marrow mesenchymal stem cells or osteoblastic cells cultured on CPC-chitosan than in CPC alone [51,52]. Radiographic examination detected the increase in new bone callus formation and reduction in material debris after the filling of chitosan-reinforced CPC into periosteum bone defect at the left canine radius for 20 weeks compared to those filled with CPC without chitosan [53].
Hyaluronic acid, also known as hyaluronan, is a naturally occurring linear glycosaminoglycan that is widely distributed in the connective tissues including skin, synovial fluid, vitreous, and cartilage. It exhibits properties of high viscosity, elasticity, negative charge, biocompatibility, biodegradability, and non-immunogenicity [59]. Hyaluronic acid has been widely employed in the applications of drug delivery [60], cosmetics [61], cancer diagnosis [62], wound healing [63], orthopaedics [64], tissue engineering [65], and tissue regeneration [66]. The addition of hyaluronic acid into CPC significantly increased the compressive strength [54]. Better ALP activity was observed in osteoblastic cells cultured on CPC with hyaluronic acid than CPC alone [51]. Cui et al. reported higher protein expression of ALP, OCN, and BMP-2 in human bone marrow mesenchymal stromal cells after being cultured with hyaluronic acid-containing CPC relative to those without hyaluronic acid. The material has also been tested by implanting it into adult female rats with a bone defect (2 mm diameter × 2 mm depth) at the metaphyseal region of the medial tibia. The findings of this study indicated denser calcified new bone, higher mineralisation, improved bone microarchitecture, and stronger positive expression of osteogenic markers in animals receiving hyaluronic acid-CPC implant than those receiving only CPC implant [54].
Another natural water-soluble polysaccharide, alginate, can be isolated from the cell wall of brown seaweed or algae. It has multifaceted roles in the biomedical and pharmaceutical fields due to its biocompatibility, non-immunogenicity, non-toxicity, low cost, and mild gelation. Alginate is commonly used in hydrogel form, providing a three-dimensional cross-linked network for migration of cells, delivery of bioactive agents, and stability of structure [67]. Several reports supported the role of alginate in improving the injectability, cohesion, strength, and elasticity of CPC without affecting the hardening rate. For instance, in vitro cell tests demonstrated that alginate-added CPC did not harm the viability of human osteoblast-like cells and human umbilical cord mesenchymal stem cells [55,56]. The differentiation capability of human umbilical cord mesenchymal stem cells into osteogenic lineage was enhanced with elevated ALP, OCN, COL1, and OSX expression [56].
Based on the collated evidence, polysaccharides enhanced CPC physically, mechanically, and biologically. The injectability, thermal stability, cohesion, mechanical strength, osteogenic activity, and bone formation were promoted without affecting the setting time of CPC.
3.4. Blood Components
Whole blood is a specialised body fluid with four main components, namely plasma, red blood cells, white blood cells, and platelets. Blood has multiple functions, including transporting oxygen and nutrients, forming blood clots to prevent excessive blood loss, carrying cells and antibodies to fight infection, bringing waste products to kidneys and livers for excretion, and maintaining the body’s pH and temperature. Considering that hematoma formation occurs as the first stage of bone healing after trauma, the addition of blood components might enhance the osteoinductive properties of CPC (Table 5). In the study conducted by Mellier et al., autologous whole blood stabilised by sodium citrate was used as the liquid phase for CPC paste formation. The CPC-blood composite was implanted into a cylindrical osseous critical-sized defect at the distal femoral end of female New Zealand white rabbits. The animals receiving CPC/blood composite exhibited higher material degradation and new bone formation 12 weeks after implantation than those receiving CPC only. The physical characteristics of CPC after incorporation with whole blood showed an increase in setting time, decrease in stiffness, and no change in compressive strength [68].
Table 5.
The bone protecting effects of CPC enhanced by blood components.
| Enhancer | Characteristics of Enhanced CPC | Type of Study | Type of Cell, Sample, and Animal Model | Outcomes Observed in Animals | Reference |
|---|---|---|---|---|---|
| Blood composite | Initial setting time: ↑, compressive strength: ↔, stiffness: ↓ | In vivo | Bone defect at distal femoral end of adult female New Zealand white rabbits | Degradation rate: ↑, new bone formation: ↑ | [68] |
| Platelet-rich plasma | No disintegration of paste consistency, setting time: ↓, compressive strength: ↔ | In vitro | MC3T3-E1 cells | No cytotoxic effect, cell proliferation: ↑, cell-to-cement interaction: ↑ | [69] |
| In vivo | Bone defect at femoral head of male New Zealand white rabbits | Residuary material: ↓, BV/TV: ↑ | |||
| Platelet-rich plasma | - | In vivo | Bone defect at distal 1/3 of the caudal vertebra body in ovariectomised female Sprague-Dawley rats | BV/TV: ↑, Tb.Th: ↑, Tb.N: ↑, Tb.Sp: ↓, BMD: ↑, new bone formation: ↑, osteogenesis grade: ↑ | [1] |
| Platelet-rich plasma | - | In vitro | Progenitor bone cells | ALP: ↑, diametral tensile strength: ↔ | [70] |
| In vivo | Bone defect at femur of rabbits | New trabecular bone formation: ↑, breakdown of bulk dense implants into pieces was observed. | |||
| Fibrin glue | - | In vivo | Bone defect at femoral condyles of male New Zealand white rabbits | Compressive strength: ↑, elastic modulus: ↑, new bone formation: ↑ | [71] |
Abbreviations: ALP, alkaline phosphatase; BMD, bone mineral density; BV/TV, bone volume/total volume; CPC, calcium phosphate cement; Tb.N, trabecular number; Tb.Sp, trabecular separation; Tb.Th, trabecular thickness; ↑, increase/improve; ↓, decrease/inhibit; ↔, no change.
Platelet-rich plasma, also known as autologous conditioned plasma, is plasma with concentrated platelets obtained from centrifugation or gravity filtration of autologous blood. It receives much attention in recent years for its application in different medical fields. The widespread clinical uses of platelet-rich plasma are mainly attributed to several factors: (a) the large amount of growth factors and various proteins stimulates the tissue healing process; (b) the neovascularisation ability provides blood supply and nutrients essential for cell proliferation, differentiation, and tissue regeneration; (c) the autologous characteristic prevents the risk of crossed contamination, disease transmission, and immune reactions [72]. The performance of CPC was enhanced by platelet-rich plasma additives, with enhanced viscosity, no disintegration of paste consistency, and decreased setting time. MC3T3-E1 cells seeded on the brushite-based CPC in the presence of platelet-rich plasma demonstrated increased cell density, homogenous cellular distribution, and higher cell-to-cement interaction. New Zealand white rabbits implanted with platelet-rich plasma-enhanced CPC had higher BV/TV and degradation rate after four weeks. Histological findings showed the recruitment of fibrous tissues at the early stage of implantation, which later disappeared to facilitate bone formation [69]. In female ovariectomised rats with a cavity-like defect at the distal 1/3 of the caudal vertebral body, the augmentation of CPC with platelet-rich plasma as filler material improved trabecular bone microstructure, BMD, new bone formation, and osteogenesis grade as compared to those implanted with CPC only [1]. Likewise, the enhancement of osteogenic properties of CPC after the addition of platelet-rich plasma was reported by another group of researchers. The ALP production of bone marrow mesenchymal stem cells from BALB/c mice grown on CPC containing platelet-rich plasma composite surface was higher than CPC only. The in vivo rabbit model of bone defects also indicated a breakdown of bulk dense CPC/platelet-rich plasma implants into pieces with higher trabecular bone tissues around the implant site over time [70].
Fibrin glue (or sealant) is a blood-derived biological tissue adhesive product consisting of a fibrinogen component and a thrombin component, which induces the coagulation cascade. It can be prepared from the plasma of individual volunteers with a low yield of fibrinogen or produced commercially using pools of plasma with a high concentration of fibrinogen [73]. Fibrin glue has been widely used in surgical procedures for wound closure, tissue repair, wound healing, and prevention of leakage or bleeding [74]. Dong et al. introduced fibrin glue purified from the blood into CPC powder to be inserted into the rabbit femoral defect model. The compressive strength and elastic modulus of the rabbit femur filled with CPC-fibrin glue were higher than those filled with CPC only. Analyses from micro-computed tomography and histological examination showed a greater amount of newly formed bone in the group provided with CPC-fibrin glue implants compared to the animals with CPC implants [71]. However, the application of human-derived fibrin glue is limited by the possibility of blood-borne disease transmission [75] and antibodies development [76]. Recently, researchers have attempted to establish fibrin glue extracted from snake venom attributed to its favourable properties for not causing adverse side effects, not having human blood components, not transmitting diseases, and has the good adhesive ability [77]. Thus, the use of heterologous snake venom fibrin glue as a potential candidate to enhance the physical, mechanical, and biological characteristics of CPC should be tested. The effects of snake venom fibrin glue in promoting bone regeneration in cancellous bone defects requires investigation from scientific studies.
The combination of CPC with blood components can influence the biological properties of the composites, particularly the increases in osteogenic proliferation and cell-to-cement interaction with no cytotoxic effect. In terms of physical performance, although the whole blood prolonged the setting time of the composite, the authors claimed that it did not limit its practical use in bone surgery as the cohesiveness was higher than the blood-free analogue. The ability of blood clot formation caused by whole blood prevented disaggregation of the composite by body fluids at the defect site [68]. Newer advancements in using platelet-rich plasma may be a better option as there was no disintegration and faster setting reaction during implantation, which can withstand segregation and stabilise the defect site, followed by its ability to degrade after a period of time to allow the growth of new bone tissue. On the other hand, fibrin glue may be superior in enhancing the mechanical properties of CPC as compared to other blood components. Improvements are warranted to enhance the biomechanical strength of CPC incorporated with blood composite and platelet-rich plasma.
3.5. Combination of Biological Enhancers
The blend of two different enhancers could be an idea to improve the features of CPC further. BMP-2 combined with other enhancers (such as collagen, gelatine, and silk fibroin) has also been previously utilised to reinforce the CPC scaffold (Table 6A). Based on the above discussion, supplementing the individual enhancer (either BMP-2 or collagen) into CPC conferred better biomechanical strength [14,22]. Lee et al. developed an injectable CPC with collagen and BMP-2 loading, which displayed the characteristics of decreased setting time with no disintegration apart from increased mechanical strength relative to the CPC without enhancement [78]. Findings from this study suggested that the combination of BMP-2 and collagen was superior in reinforcing CPC than its individual component. Mouse pre-osteoblast (MC3T3-E1) cells cultured on the combined material displayed rapid cell viability, cell proliferation, and cell spreading. In addition, qualitative micro-computed tomography scanning images showed defect integration, new bone tissue formation, and material degradation of CPC loaded with BMP-2 and collagen after 4 weeks of implantation at the cylindrical defect created on the parietal part of the femur of New Zealand white rabbits [78]. Using bigger animals as models, female goats were subjected to ovariectomy to induce osteoporosis and bone defect at the lumbar vertebrae, which was filled with CPC containing BMP-2 loaded gelatine microspheres. The implanted vertebral bone of the animals had greater mechanical strength and bone mineralisation rate after 45 days than the untreated group [79]. In the ovine model of interbody defect created at the midpoint of disc space, the site filled with CPC/silk fibroin/rhBMP-2 composite exhibited higher stiffness and bone volume, which were on par with those implanted with autograft. Lower material residue volume was also detected in CPC reinforced with silk fibroin and rhBMP-2 compared to the material without rhBMP-2 [80].
Table 6.
The bone protecting effects of CPC enhanced by the combination of biological enhancers.
| Enhancer | Characteristics of Enhanced CPC |
Type of Study | Type of Cell, Sample, and Animal Model |
Outcomes Observed in Animals | Reference |
|---|---|---|---|---|---|
| (A) Combination of BMP-2 and other enhancers | |||||
| BMP-2-loaded collagen | Setting time: ↓, compressive strength: ↑, disintegration or degree of cohesion: ↔ | In vitro | MC3T3-E1 cells | Cell viability: ↑, cell density: ↑ | [78] |
| In vivo | Bone defect at the parietal part of femur of New Zealand white rabbits | New bone tissue formation: ↑, degradation of material: ↑ | |||
| BMP-2 loaded gelatine microsphere | - | In vivo | Bone defect at lumbar vertebrae of female ovariectomised goats | Pushout value: ↑, bone mineralisation: ↑ | [79] |
| rhBMP-2 loaded silk fibroin | - | In vivo | Interbody defect at midpoint of disc space of mature sheep | Stiffness: ↑, BV/TV: ↑, ceramic residue volume: ↓ | [80] |
| (B) Combination of protein and polysaccharide | |||||
| Chitosan with arginine-glycine-aspartate motif | Setting time: ↔, flexural strength: ↑, elastic modulus: ↔, work of fracture: ↑ | In vitro | Human embryonic stem cell-derived mesenchymal stem cells | Percentage of live cells: ↑, cell density: ↑, OCN: ↑, COL1: ↑, mineralisation: ↑ | [81] |
| Chitosan with arginine-glycine-aspartate motif | Flexural strength: ↑ | In vitro | Mouse pluripotent C3H10T1/2(C3) cells | Cell number: ↑, cell proliferation: ↑, ALP: ↑, | [82] |
| In vivo | Bone defect at femoral condyles of New Zealand white rabbits | New bone volume: ↑ | |||
| (C) Combination of two different polysaccharides | |||||
| Chitosan-alginate complex | Initial and final setting time: ↓, no disintegration, compressive strength: ↑ | In vivo | Bone defect at femoral head of male New Zealand white rabbits | New bone formation: ↑, implant remaining: ↓ | [83] |
| Alginate-chitosan microencapsulated MC3T3-E1 cells | Setting time: ↔, compressive strength: ↓ | In vivo | BALB/c nude mice | Scaffold remaining: ↓, lamellar-bone-like mineral structure: ↑, newly formed collagen: ↑, mineralisation rate: ↑ | [84] |
Abbreviations: ALP, alkaline phosphatase; BMP-2, bone morphogenetic protein-2; BV/TV, bone volume/total volume; COL1, type I collagen; CPC, calcium phosphate cement; OCN, osteocalcin; rhBMP-2, recombinant human bone morphogenetic protein-2; Runx-2, Runt-related transcription factor 2; ↑, increase/improve; ↓, decrease/inhibit; ↔, no change.
Proteins and polysaccharides have been combined and incorporated into CPC to enhance osteogenic effects and mechanical properties (Table 6B). The addition of peptide sequences arginine-glycine-aspartate motif into chitosan-containing CPC enhanced flexural strength and work of fracture but did not have any effect on elastic modulus [81,82]. Compared to CPC reinforced with arginine-glycine-aspartate motif alone, which did not cause any change in biomechanical strength [19,20], the addition of chitosan further improved the mechanical strength of CPC incorporated with the arginine-glycine-aspartate motif. Two groups of researchers investigated the osteogenic proliferation and differentiation of human embryonic stem cell-derived mesenchymal stem cells and mouse pluripotent C3H10T1/2(C3) cells on CPC with the addition of chitosan immobilised with peptide sequences arginine-glycine-aspartate motif. Their results demonstrated higher cell number, proliferation, differentiation, and mineralisation [81,82]. A similar biomaterial was also used as a filler for a 3 mm diameter and 6 mm depth bone cavity at femoral condyles of New Zealand white rabbits. The implanted material underwent degradation in the femur cavity with lesser residual found in animals receiving CPC-chitosan with arginine-glycine-aspartate compared to those receiving CPC-chitosan [82].
Two different types of polysaccharides were also combined and introduced into CPC, in which the bone regeneration properties have been tested in vivo (Table 6C). The mixture of chitosan-alginate complex and CPC produced a gel-like matrix, with reduced setting time, no disintegration, and increased compressive strength [83]. This combination reduced the time for CPC to harden, which was not seen in CPC supplemented with alginate alone. Following implantation of the chitosan-alginate complex in vivo to a cylindrical defect at the femoral head of male New Zealand white rabbits, an increased amount of newly formed bone with less implant remaining and denser mineralisation were noted [83]. A similar biomaterial was created by another group of researchers, consisting of CPC and alginate-chitosan microencapsulated with mouse osteoblast MC3T3-E1 cells. They researched the osteogenic potential of this complex by injecting it into the dorsal subcutaneous area of BALB/c nude mice. The results revealed higher lamellar bone-like mineral structure, newly formed collagen, mineralisation rate, and less scaffold material remaining in the animals implanted with CPC containing alginate-chitosan and MC3T3-E1 cells compared to those implanted with CPC alone [84].
Taken together, different combinations of biological enhancers may not necessarily improve the limitations of CPC. Positive improvements of CPC were seen in the composites with the presence of BMP-2 and other biological enhancers as well as two types of polysaccharides, but not in the mixture of protein and polysaccharides. However, there is only a paucity of studies available to support these findings. Further studies are recommended to validate this hypothesis.
4. Perspectives
Calcium phosphate cement can self-harden and incorporate various components (such as drugs and biological materials) owing to its intrinsic porosity without affecting its functions. In this review, the scientific evidence pointed out that the incorporation of biological materials has great potential to resolve the limitations and further enhance the characteristics of CPC. Although some biological materials may be insufficient to reinforce CPC, their incorporation did not cause any deterioration on the beneficial features of CPC. Most of these biological materials increased the physical, mechanical, and biological performance resolving the brittleness, lack of osteogenic properties, and poor anti-washout of CPC, except for incorporating the elastin-like polypeptide, CGRP, bone sialoprotein, and blood components. A summary of the effects of biological materials in improving the characteristics of CPC has been provided (Table 7).
Table 7.
Summary on the characteristics of CPC after incorporation of biological enhancers.
| Bone-Related Transcription Factors |
Proteins | Polysaccharides | Blood Components |
Bone-Related Transcription Factors + Proteins |
Proteins + Polysaccharide |
Polysaccharide + Polysaccharide | |
|---|---|---|---|---|---|---|---|
| Physical properties | - | ↑ injectability ↑ anti-washout ↓ setting time (except for elastin-like polypeptide) Pore size: lysine increased, elastin-like polypeptide reduced but CGRP has no change in porosity |
↑ injectability ↑ thermal stability ↑ cohesion No change in setting time |
Whole blood increased but PRP reduced setting time | ↓ setting time No change in disintegration or cohesion |
No change in setting time | ↓ setting time No disintegration |
| Mechanical properties | ↑ compressive strength | ↑ compressive strength (except for CGRP) ↑ flexural strength ↑ elasticity ↑ work of fracture ↑ micro-hardness |
↑ compressive strength ↑ flexural strength ↑ elasticity ↑ work of fracture |
No improvement in compressive strength ↓ stiffness |
↑ compressive strength | ↑ flexural strength No change in elasticity ↑ work of fracture |
↑ compressive strength |
| Biological properties | ↑ osteogenesis ↑ bone density, microstructure, and strength |
No cytotoxicity ↑ osteogenesis (except bone sialoprotein) ↑ bone microstructure and strength |
No cytotoxicity ↑ osteogenesis ↑ bone density and microstructure |
No cytotoxicity ↑ osteogenesis ↑ bone density and microstructure |
No cytotoxicity ↑ osteogenesis ↑ bone microstructure and strength |
No cytotoxicity ↑ osteogenesis ↑ bone microstructure |
↑ bone formation and mineralisation |
Abbreviations: CGRP, calcitonin gene-related peptide; CPC, calcium phosphate cement; PRP, ↑, increase/improve; ↓, decrease/inhibit.
The limitation of current evidence has been acknowledged. The evaluation of biological materials-enhanced CPC in most in vivo bone defect animal models was performed radiologically and histologically with qualitative but not quantitative analysis. The quantifications of bone microstructural parameters and bone cells at multiple time points allow the observation of dynamic bone tissue healing and regeneration process at the defect site. Apart from that, paucity in the number of original studies needs to be addressed. The characteristics of CPC enhanced with single materials and those enhanced with multiple materials could not be compared directly due to the lack of original studies. Therefore, the comparison was drawn from different studies with possible different experiment conditions and the readers should read with caution.
Several recommendations for future studies are suggested. Firstly, various plant extracts and their isolated bioactive compounds have been extensively demonstrated by researchers to exert potent bone-protecting properties [85,86,87,88,89,90], which could be introduced into CPC to improve its physical, mechanical, and osteogenic effects. Secondly, a three-dimensional osteoblast-osteoclast co-culture system mimicking the skeletal microenvironment in humans could be used to investigate the properties of CPC after the reinforcement using biological materials [91,92]. The positive outcomes of biological material-enhanced CPC in promoting bone healing and tissue regeneration observed in the in vitro and in vivo evidence await further validation on its performance for clinical applications.
5. Conclusions
In summary, the current evidence demonstrated the potential enhancement of CPC properties by introducing biological materials. However, the addition of different materials may result in different degrees of improvement in CPC. The desired bone graft substitutes should display the characteristics of injectable, cohesive, resorbable, self-hardening, and high mechanical strength that allows rapid cell invasion, cell proliferation, and osteogenic activity, which may be a major challenge to designing a single bone graft substitute that fulfils all the criteria. From the articles reviewed here, polysaccharides are the best biological additives for CPC as they fulfil most of the criteria of an excellent bone graft. With the advancement of new technology, the development of tailor-made bone substitutes by incorporation of bioactive substances into CPC is the way forward to meet the demands for use in research and in the clinical setting.
Author Contributions
Conceptualization, S.K.W.; writing—original draft preparation, S.K.W.; writing—review and editing, Y.H.W., K.-Y.C. and S.I.-N.; visualization, S.K.W., Y.H.W., K.-Y.C. and S.I.-N.; funding acquisition, S.K.W., K.-Y.C. and S.I.-N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Universiti Kebangsaan Malaysia, grant number FF-2020-366.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Smrke D., Rožman P., Veselko M., Gubina B. Treatment of Bone Defects—Allogenic Platelet Gel and Autologous Bone Technique. IntechOpen; London, UK: 2013. [Google Scholar]
- 2.Wang W., Yeung K. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017;2:224–247. doi: 10.1016/j.bioactmat.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahney C.S., Zondervan R., Allison P., Theologis A., Ashley J., Ahn J., Miclau T., Marcucio R.S., Hankenson K.D. Cellular biology of fracture healing. J. Orthop. Res. 2018;37:35–50. doi: 10.1002/jor.24170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pountos I., Giannoudis P.V. Fracture Reduction and Fixation Techniques. Springer; Cham, Switzerland: 2018. Fracture Healing: Back to Basics and Latest Advances; pp. 3–17. [DOI] [Google Scholar]
- 5.Yousefi A.-M. A review of calcium phosphate cements and acrylic bone cements as injectable materials for bone repair and implant fixation. J. Appl. Biomater. Funct. Mater. 2019;17:2280800019872594. doi: 10.1177/2280800019872594. [DOI] [PubMed] [Google Scholar]
- 6.Ginebra M.-P., Canal C., Espanol M., Pastorino D., Montufar E.B. Calcium phosphate cements as drug delivery materials. Adv. Drug Deliv. Rev. 2012;64:1090–1110. doi: 10.1016/j.addr.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Xu H.H., Wang P., Wang L., Bao C., Chen Q., Weir M.D., Chow L.C., Zhao L., Zhou X., Reynolds M.A. Calcium phosphate cements for bone engineering and their biological properties. Bone Res. 2017;5:17056. doi: 10.1038/boneres.2017.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li X., He F., Ye J. Preparation, characterization and in vitro cell performance of anti-washout calcium phosphate cement modified by sodium polyacrylate. RSC Adv. 2017;7:32842–32849. doi: 10.1039/C7RA03221H. [DOI] [Google Scholar]
- 9.Wu T., Shi H., Liang Y., Lu T., Lin Z., Ye J. Improving osteogenesis of calcium phosphate bone cement by incorporating with manganese doped β-tricalcium phosphate. Mater. Sci. Eng. C. 2019;109:110481. doi: 10.1016/j.msec.2019.110481. [DOI] [PubMed] [Google Scholar]
- 10.Pearson H.B., Mason D.E., Kegelman C.D., Zhao L., Dawahare J.H., Kacena M.A., Boerckel J.D. Effects of Bone Morphogenetic Protein-2 on Neovascularization During Large Bone Defect Regeneration. Tissue Eng. Part A. 2019;25:1623–1634. doi: 10.1089/ten.tea.2018.0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poniatowski L.A., Wojdasiewicz P., Gasik R., Szukiewicz D. Transforming Growth Factor Beta Family: Insight into the Role of Growth Factors in Regulation of Fracture Healing Biology and Potential Clinical Applications. Mediat. Inflamm. 2015;2015:137823. doi: 10.1155/2015/137823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blom E.J., Klein-Nulend J., Klein C.P., Kurashina K., van Waas M.A., Burger E.H. Transforming growth factorbeta1 incorporated during setting in calcium phosphate cement stimulates bone cell differentiation in vitro. J. Biomed. Mater. Res. 2000;50:67–74. doi: 10.1002/(SICI)1097-4636(200004)50:1<67::AID-JBM10>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 13.Zhang J., Zhou H., Yang K., Yuan Y., Liu C. RhBMP-2-loaded calcium silicate/calcium phosphate cement scaffold with hierarchically porous structure for enhanced bone tissue regeneration. Biomaterials. 2013;34:9381–9392. doi: 10.1016/j.biomaterials.2013.08.059. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y., Hou J., Yin M., Wang J., Liu C. Enhanced healing of rabbit segmental radius defects with surfacecoated calcium phosphate cement/bone morphogenetic protein-2 scaffolds. Mater. Sci. Eng. C. 2014;44:326–335. doi: 10.1016/j.msec.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 15.Tao Z., Zhou W., Jiang Y., Wu X., Xu Z., Yang M., Xie J. Effects of strontiummodified calcium phosphate cement combined with bone morphogenetic protein-2 on osteoporotic bone defects healing in rats. J. Biomater. Appl. 2018;33:3–10. doi: 10.1177/0885328218765847. [DOI] [PubMed] [Google Scholar]
- 16.Qi Y., Wang H., Wei K., Yang Y., Zheng R.-Y., Kim I.S., Zhang K.-Q. A Review of Structure Construction of Silk Fibroin Biomaterials from Single Structures to Multi-Level Structures. Int. J. Mol. Sci. 2017;18:237. doi: 10.3390/ijms18030237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu M., He Z., Han F., Shi C., Zhou P., Ling F., Zhu X., Yang H., Li B. Reinforcement of calcium phosphate cement using alkaline-treated silk fibroin. Int. J. Nanomed. 2018;13:7183–7193. doi: 10.2147/IJN.S172881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi H., Ye X., He F., Ye J. Improving osteogenesis of calcium phosphate bone cement by incorporating with lysine: An in vitro study. Colloids Surf. B Biointerfaces. 2019;177:462–469. doi: 10.1016/j.colsurfb.2019.02.034. [DOI] [PubMed] [Google Scholar]
- 19.Zhou H., Chen W., Weir M.D., Xu H.H. Biofunctionalized calcium phosphate cement to enhance the attachment and os-teodifferentiation of stem cells released from fast-degradable alginate-fibrin microbeads. Tissue Eng. Part A. 2012;18:1583–1595. doi: 10.1089/ten.tea.2011.0604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen W., Zhou H., Weir M.D., Bao C., Xu H.H. Umbilical cord stem cells released from alginate–fibrin microbeads inside macroporous and biofunctionalized calcium phosphate cement for bone regeneration. Acta Biomater. 2012;8:2297–2306. doi: 10.1016/j.actbio.2012.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feng T., Niu J., Pi B., Lu Y., Wang J., Zhang W., Li B., Yang H., Zhu X. Osteogenesis enhancement of silk fibroin/α-TCP cement by N-acetyl cysteine through Wnt/β-catenin signaling pathway in vivo and vitro. J. Mech. Behav. Biomed. Mater. 2019;101:103451. doi: 10.1016/j.jmbbm.2019.103451. [DOI] [PubMed] [Google Scholar]
- 22.Thein-Han W., Xu H.H. Collagen-Calcium Phosphate Cement Scaffolds Seeded with Umbilical Cord Stem Cells for Bone Tissue Engineering. Tissue Eng. Part A. 2011;17:2943–2954. doi: 10.1089/ten.tea.2010.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuzmar E., Perez R.A., Manzanares M.C., Ginebra M.P., Franch J. In Vivo Osteogenic Potential of Biomimetic Hydroxy-apatite/Collagen Microspheres: Comparison with Injectable Cement Pastes. PLoS ONE. 2015;10:e0131188. doi: 10.1371/journal.pone.0131188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orshesh Z., Hesaraki S., Khanlarkhani A. Blooming gelatin: An individual additive for enhancing nanoapatite precipitation, physical properties, and osteoblastic responses of nanostructured macroporous calcium phosphate bone cements. Int. J. Nanomed. 2017;2017:745–758. doi: 10.2147/IJN.S128368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bigi A., Torricelli P., Fini M., Bracci B., Panzavolta S., Sturba L., Giardino R. A Biomimetic Gelatin-Calcium Phosphate Bone Cement. Int. J. Artif. Organs. 2004;27:664–673. doi: 10.1177/039139880402700804. [DOI] [PubMed] [Google Scholar]
- 26.Jang J.H., Shin S., Kim H.J., Jeong J., Jin H.E., Desai M.S., Lee S.W., Kim S.Y. Improvement of physical properties of cal-cium phosphate cement by elastin-like polypeptide supplementation. Sci. Rep. 2018;8:5216. doi: 10.1038/s41598-018-23577-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liang W., Li L., Cui X., Tang Z., Wei X., Pan H., Li B. Enhanced Proliferation and Differentiation Effects of a CGRP- and Sr-Enriched Calcium Phosphate Cement on Bone Mesenchymal Stem Cells. J. Appl. Biomater. Funct. Mater. 2016;14:431–440. doi: 10.5301/jabfm.5000295. [DOI] [PubMed] [Google Scholar]
- 28.Klein A., Baranowski A., Ritz U., Götz H., Heinemann S., Mattyasovszky S., Rommens P.M., Hofmann A. Effect of bone sialoprotein coated three-dimensional printed calcium phosphate scaffolds on primary human osteoblasts. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018;106:2565–2575. doi: 10.1002/jbm.b.34073. [DOI] [PubMed] [Google Scholar]
- 29.Klein A., Baranowski A., Ritz U., Mack C., Götz H., Langendorf E., Al-Nawas B., Drees P., Rommens P.M., Hofmann A. Effect of bone sialoprotein coating on progression of bone formation in a femoral defect model in rats. Eur. J. Trauma Emerg. Surg. 2019;46:277–286. doi: 10.1007/s00068-019-01159-5. [DOI] [PubMed] [Google Scholar]
- 30.Bihuniak J.D., Insogna K.L. The effects of dietary protein and amino acids on skeletal metabolism. Mol. Cell. Endocrinol. 2015;410:78–86. doi: 10.1016/j.mce.2015.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polo-Corrales L., Latorre-Esteves M., Ramirez-Vick J. Scaffold Design for Bone Regeneration. J. Nanosci. Nanotechnol. 2014;14:15–56. doi: 10.1166/jnn.2014.9127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zapp C., Minsky B.B., Boehm H. Tuning RGD Motif and Hyaluronan Density to Study Integrin Binding. Front. Physiol. 2018;9:1022. doi: 10.3389/fphys.2018.01022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitroulis I., Alexaki V.I., Kourtzelis I., Ziogas A., Hajishengallis G., Chavakis T. Leukocyte integrins: Role in leukocyte recruitment and as therapeutic targets in inflammatory disease. Pharmacol. Ther. 2014;147:123–135. doi: 10.1016/j.pharmthera.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zaveri T., Lewis J.S., Dolgova N.V., Clare-Salzler M.J., Keselowsky B.G. Integrindirected modulation of macrophage responses to biomaterials. Biomaterials. 2014;35:3504–3515. doi: 10.1016/j.biomaterials.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malinin N., Pluskota E., Byzova T.V. Integrin signaling in vascular function. Curr. Opin. Hematol. 2012;19:206–211. doi: 10.1097/MOH.0b013e3283523df0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duong L.T., Lakkakorpi P., Nakamura I., Rodan G.A. Integrins and signaling in osteoclast function. Matrix Biol. 2000;19:97–105. doi: 10.1016/S0945-053X(00)00051-2. [DOI] [PubMed] [Google Scholar]
- 37.Hendesi H., Barbe M., Safadi F.F., Monroy M.A., Popoff S.N. Integrin Mediated Adhesion of Osteoblasts to Connective Tissue Growth Factor (CTGF/CCN2) Induces Cytoskeleton Reorganization and Cell Differentiation. PLoS ONE. 2015;10:e0115325. doi: 10.1371/journal.pone.0115325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Green J.L., Heard K.J., Reynolds K.M., Albert D. Oral and Intravenous Acetylcysteine for Treatment of Acetaminophen Toxicity: A Systematic Review and Meta-analysis. West. J. Emerg. Med. 2013;14:218–226. doi: 10.5811/westjem.2012.4.6885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guillerminet F., Beaupied H., Fabien-Soulé V., Tomé D., Benhamou C.-L., Roux C., Blais A. Hydrolyzed collagen improves bone metabolism and biomechanical parameters in ovariectomized mice: An in vitro and in vivo study. Bone. 2010;46:827–834. doi: 10.1016/j.bone.2009.10.035. [DOI] [PubMed] [Google Scholar]
- 40.Alipal J., Mohd Pu’ad N.A.S., Lee T.C., Nayan N.H.M., Sahari N., Basri H., Idris M.I., Abdullah H.Z. A review of gelatin: Properties, sources, process, applications, and commercialisation. Mater. Today Proc. 2021;42:240–250. [Google Scholar]
- 41.Chen K.-Y., Yao C.-H. Repair of bone defects with gelatin-based composites: A review. BioMedicine. 2011;1:29–32. doi: 10.1016/j.biomed.2011.10.005. [DOI] [Google Scholar]
- 42.Kowalczyk T., Hnatuszko-Konka K., Gerszberg A., Kononowicz A.K. Elastinlike polypeptides as a promising family of genetically-engineered protein based polymers. World J. Microbiol. Biotechnol. 2014;30:2141–2152. doi: 10.1007/s11274-014-1649-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Russell F.A., King R., Smillie S.-J., Kodji X., Brain S.D. Calcitonin Gene-Related Peptide: Physiology and Pathophysiology. Physiol. Rev. 2014;94:1099–1142. doi: 10.1152/physrev.00034.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mi J., Xu J., Yao H., Li X., Tong W., Li Y., Dai B., He X., Chow D.H.K., Li G., et al. Calcitonin Gene-Related Peptide Enhances Distraction Osteogenesis by Increasing Angiogenesis. Tissue Eng. Part A. 2021;27:87–102. doi: 10.1089/ten.tea.2020.0009. [DOI] [PubMed] [Google Scholar]
- 45.Appelt J., Baranowsky A., Jahn D., Yorgan T., Köhli P., Otto E., Farahani S.K., Graef F., Fuchs M., Herrera A., et al. The neuropeptide calcitonin gene-related peptide alpha is essential for bone healing. EBioMedicine. 2020;59:102970. doi: 10.1016/j.ebiom.2020.102970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ganss B., Kim R.H., Sodek J. Bone sialoprotein. Crit. Rev. Oral Biol. Med. 1999;10:79–98. doi: 10.1177/10454411990100010401. [DOI] [PubMed] [Google Scholar]
- 47.Hunter G.K., Goldberg H.A. Nucleation of hydroxyapatite by bone sialoprotein. Proc. Natl. Acad. Sci. USA. 1993;90:8562–8565. doi: 10.1073/pnas.90.18.8562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mintz K.P., Midura R.J., Fisher L.W. Purification of bone sialoprotein from the medium of the rat osteoblast-like cell line UMR 106-01 BSP. J. Tissue Cult. Methods. 1994;16:205–209. doi: 10.1007/BF01540652. [DOI] [Google Scholar]
- 49.Portela R., Leal C.R., Almeida P.L., Sobral R.G. Bacterial cellulose: A versatile biopolymer for wound dressing applications. Microb. Biotechnol. 2019;12:586–610. doi: 10.1111/1751-7915.13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Q., Lei Z., Peng M., Zhong M., Wan Y., Luo H. Enhancement of mechanical and biological properties of calcium phosphate bone cement by incorporating bacterial cellulose. Mater. Technol. 2019;34:800–806. doi: 10.1080/10667857.2019.1630951. [DOI] [Google Scholar]
- 51.Hesaraki S., Nezafati N. In vitro biocompatibility of chitosan/hyaluronic acid-containing calcium phosphate bone cements. Bioprocess Biosyst. Eng. 2014;37:1507–1516. doi: 10.1007/s00449-013-1122-0. [DOI] [PubMed] [Google Scholar]
- 52.Moreau J.L., Xu H.H. Mesenchymal stem cell proliferation and differentiation on an injectable calcium phosphate—Chitosan composite scaffold. Biomaterials. 2009;30:2675–2682. doi: 10.1016/j.biomaterials.2009.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lian Q., Li D.-C., He J.-K., Wang Z. Mechanical properties and in-vivo performance of calcium phosphate cement—Chitosan fibre composite. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2008;222:347–353. doi: 10.1243/09544119JEIM340. [DOI] [PubMed] [Google Scholar]
- 54.Cui X., Huang C., Chen Z., Zhang M., Liu C., Su K., Wang J., Li L., Wang R., Li B., et al. Hyaluronic acid facilitates bone repair effects of calcium phosphate cement by accelerating osteogenic expression. Bioact. Mater. 2021;6:3801–3811. doi: 10.1016/j.bioactmat.2021.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sprio S., Dapporto M., Montesi M., Panseri S., Lattanzi W., Pola E., Logroscino G., Tampieri A. Novel Osteointegrative Sr-Substituted Apatitic Cements Enriched with Alginate. Materials. 2016;9:763. doi: 10.3390/ma9090763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhao L., Weir M.D., Xu H.H. An injectable calcium phosphate-alginate hydrogel-umbilical cord mesenchymal stem cell paste for bone tissue engineering. Biomaterials. 2010;31:6502–6510. doi: 10.1016/j.biomaterials.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheung R.C., Ng T.B., Wong J.H., Chan W.Y. Chitosan: An Update on Potential Biomedical and Pharmaceutical Applica-tions. Mar. Drugs. 2015;13:5156–5186. doi: 10.3390/md13085156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roy J.C., Salaün F., Giraud S., Ferri G.C.A., Chen G., Guan J. Solubility of Chitin: Solvents, Solution Behaviors and Their Related Mechanisms. Volume 10. IntechOpen; London, UK: 2017. [DOI] [Google Scholar]
- 59.Zhao N., Wang X., Qin L., Zhai M., Yuan J., Chen J., Li D. Effect of hyaluronic acid in bone formation and its applications in dentistry. J. Biomed. Mater. Res. A. 2016;104:1560–1569. doi: 10.1002/jbm.a.35681. [DOI] [PubMed] [Google Scholar]
- 60.Huang G., Huang H. Application of hyaluronic acid as carriers in drug delivery. Drug Deliv. 2018;25:766–772. doi: 10.1080/10717544.2018.1450910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bukhari S.N.A., Roswandi N.L., Waqas M., Habib H., Hussain F., Khan S., Sohail M., Ramli N.A., Thu H.E., Hussain Z. Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int J. Biol. Macromol. 2018;120:1682–1695. doi: 10.1016/j.ijbiomac.2018.09.188. [DOI] [PubMed] [Google Scholar]
- 62.Liang Z., Zhang Q., Wang C., Shi F., Cao H., Yu Y., Zhang M., Liu X. Hyaluronic acid/Hyaluronidase as biomarkers for bladder cancer: A diagnostic meta-analysis. Neoplasma. 2017;64:901–908. doi: 10.4149/neo_2017_612. [DOI] [PubMed] [Google Scholar]
- 63.Kawano Y., Patrulea V., Sublet E., Borchard G., Iyoda T., Kageyama R., Morita A., Seino S., Yoshida H., Jordan O., et al. Wound Healing Promotion by Hyaluronic Acid: Effect of Molecular Weight on Gene Expression and In Vivo Wound Closure. Pharmaceuticals. 2021;14:301. doi: 10.3390/ph14040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bowman S., Awad M.E., Hamrick M.W., Hunter M., Fulzele S. Recent advances in hyaluronic acid based therapy for os-teoarthritis. Clin. Transl. Med. 2018;7:6. doi: 10.1186/s40169-017-0180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Park S.H., Seo J.Y., Park J.Y., Ji Y.B., Kim K., Choi H.S., Choi S., Kim J.H., Min B.H., Kim M.S. An injectable, clickcrosslinked, cytomodulin-modified hyaluronic acid hydrogel for cartilage tissue engineering. NPG Asia Mater. 2019;11:30. doi: 10.1038/s41427-019-0130-1. [DOI] [Google Scholar]
- 66.Dovedytis M., Liu Z.J., Bartlett S. Hyaluronic acid and its biomedical applications: A review. Eng. Regen. 2020;1:102–113. doi: 10.1016/j.engreg.2020.10.001. [DOI] [Google Scholar]
- 67.Lee K.Y., Mooney D.J. Alginate: Properties and biomedical applications. Prog. Polym. Sci. 2012;37:106–126. doi: 10.1016/j.progpolymsci.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mellier C., Lefevre F.X., Fayon F., Montouillout V., Despas C., Le Ferrec M., Boukhechba F., Walcarius A., Janvier P., Dutilleul M., et al. A straightforward approach to enhance the textural, mechanical and biological properties of injectable calcium phosphate apatitic cements (CPCs): CPC/blood composites, a comprehensive study. Acta Biomater. 2017;62:328–339. doi: 10.1016/j.actbio.2017.08.040. [DOI] [PubMed] [Google Scholar]
- 69.Hasan L., Taz M., Lee B.-T. Effects of platelet-rich plasma on biological activity and bone regeneration of brushite-based calcium phosphate cement. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017;106:2316–2326. doi: 10.1002/jbm.b.34036. [DOI] [PubMed] [Google Scholar]
- 70.Cho A.-R., Kim H.-K., Kwon J.-Y., Kim T.-K., Choi Y.-M., Kim K.-H. The incorporation of platelet-rich plasma into calcium phosphate cement enhances bone regeneration in osteoporosis. Pain Physician. 2014;17:E737–E745. [PubMed] [Google Scholar]
- 71.Ko C.-L., Chen W.-C., Chen J.-C., Wang Y.H., Shih C.-J., Tyan Y.-C., Hung C.-C., Wang J.-C. Properties of osteoconductive biomaterials: Calcium phosphate cement with different ratios of platelet-rich plasma as identifiers. Mater. Sci. Eng. C. 2013;33:3537–3544. doi: 10.1016/j.msec.2013.04.042. [DOI] [PubMed] [Google Scholar]
- 72.Lei W., Dong J., Cui G., Bi L., Li J. The mechanical and biological stud ies of calcium phosphate cement-fibrin glue for bone reconstruction of rabbit femoral defects. Int. J. Nanomed. 2013;8:1317–1324. doi: 10.2147/IJN.S42862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pavlovic V., Ciric M., Jovanovic V., Stojanovic P. Platelet Rich Plasma: A short overview of certain bioactive components. Open Med. 2016;11:242–247. doi: 10.1515/med-2016-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Panda A., Kumar S., Kumar A., Bansal R., Bhartiya S. Fibrin glue in ophthalmology. Indian J. Ophthalmol. 2009;57:371–379. doi: 10.4103/0301-4738.55079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nan A. Miscellaneous Drugs, Materials, Medical Devices and Techniques. In: Ray S.D., editor. Side Effects of Drugs Annual. Elsevier; Amsterdam, The Netherlands: 2016. pp. 523–532. [Google Scholar]
- 76.Joch C. The safety of fibrin sealants. Cardiovasc. Surg. 2003;11:23–28. doi: 10.1016/S0967-2109(03)00068-1. [DOI] [PubMed] [Google Scholar]
- 77.Seifert J., Klause N., Stobbe J., Egbers H.J. Antibodies formed against fibrin glue components and their circulatory relevance. J. Invest. Surg. 1994;7:167–171. doi: 10.3109/08941939409015361. [DOI] [PubMed] [Google Scholar]
- 78.Cunha M.R.d., Menezes F.A., Santos G.R.d., Pinto C.A.L., Barraviera B., Martins V.d.C.A., Plepis A.M.d.G., Ferreira R.S. Hydroxyapatite and a new fibrin sealant derived from snake venom as scaffold to treatment of cranial defects in rats. Mater. Res. 2015;18:196–203. doi: 10.1590/1516-1439.316014. [DOI] [Google Scholar]
- 79.Lee G.H., Makkar P., Paul K., Lee B. Incorporation of BMP-2 loaded collagen conjugated BCP granules in calcium phosphate cement based injectable bone substitutes for improved bone regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2017;77:713–724. doi: 10.1016/j.msec.2017.03.296. [DOI] [PubMed] [Google Scholar]
- 80.Li M., Liu X., Liu X., Ge B. Calcium phosphate cement with BMP-2-loaded gelatin microspheres enhances bone healing in osteoporosis: A pilot study. Clin Orthop Relat Res. 2010;468:1978–1985. doi: 10.1007/s11999-010-1321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gu Y., Chen L., Yang H.L., Luo Z.P., Tang T.S. Evaluation of an injectable silk fibroin enhanced calcium phosphate cement loaded with human recombinant bone morphogenetic protein-2 in ovine lumbar interbody fusion. J. Biomed. Mater. Res. A. 2011;97:177–185. doi: 10.1002/jbm.a.33018. [DOI] [PubMed] [Google Scholar]
- 82.Chen W., Zhou H., Weir M.D., Tang M., Bao C., Xu H.H. Human Embryonic Stem Cell-Derived Mesenchymal Stem Cell Seeding on Calcium Phosphate Cement-Chitosan-RGD Scaffold for Bone Repair. Tissue Eng. Part A. 2013;19:915–927. doi: 10.1089/ten.tea.2012.0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu T.-Y., Zhou Z.-B., He Z.-W., Ren W.-P., Yu X.-W., Huang Y. Reinforcement of a new calcium phosphate cement with RGD-chitosan-fiber. J. Biomed. Mater. Res. Part A. 2013;102:68–75. doi: 10.1002/jbm.a.34669. [DOI] [PubMed] [Google Scholar]
- 84.Lee H.J., Kim B., Padalhin A.R., Lee B.T. Incorporation of chitosan-alginate complex into injectable calcium phosphate ce-ment system as a bone graft material. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;94:385–392. doi: 10.1016/j.msec.2018.09.039. [DOI] [PubMed] [Google Scholar]
- 85.Qiao P., Wang J., Xie Q., Li F., Dong L., Xu T. Injectable calcium phosphate–alginate–chitosan microencapsulated MC3T3-E1 cell paste for bone tissue engineering in vivo. Mater. Sci. Eng. C. 2013;33:4633–4639. doi: 10.1016/j.msec.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 86.Ekeuku S., Pang K.-L., Chin K.-Y. The Skeletal Effects of Tanshinones: A Review. Molecules. 2021;26:2319. doi: 10.3390/molecules26082319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kamaruzzaman M.A., Chin K.-Y., Ramli E.S.M. A Review of Potential Beneficial Effects of Honey on Bone Health. Evid. Based Complement. Altern. Med. 2019;2019:8543618. doi: 10.1155/2019/8543618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wong S.K., Chin K.-Y., Ima-Nirwana S. Quercetin as an Agent for Protecting the Bone: A Review of the Current Evidence. Int. J. Mol. Sci. 2020;21:6448. doi: 10.3390/ijms21176448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wong S.K., Chin K.-Y., Ima-Nirwana S. Berberine and musculoskeletal disorders: The therapeutic potential and underlying molecular mechanisms. Phytomedicine. 2019;73:152892. doi: 10.1016/j.phymed.2019.152892. [DOI] [PubMed] [Google Scholar]
- 90.Wong S.K., Chin K.-Y., Ima-Nirwana S. The Osteoprotective Effects of Kaempferol: The Evidence From In Vivo and In Vitro Studies. Drug Des. Dev. Ther. 2019;13:3497–3514. doi: 10.2147/DDDT.S227738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wong S.K., Mohamad N.-V., Ibrahim N., Chin K.-Y., Shuid A.N., Ima-Nirwana S. The Molecular Mechanism of Vitamin E as a Bone-Protecting Agent: A Review on Current Evidence. Int. J. Mol. Sci. 2019;20:1453. doi: 10.3390/ijms20061453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jolly J.J., Mohd Fozi N.F., Chin K.Y., Wong S.K., Chua K.H., Alias E., Adnan N.S., Ima-Nirwana S. Skeletal microenvi-ronment system utilising bovine bone scaffold co-cultured with human osteoblasts and osteoclast-like cells. Exp. Ther Med. 2021;22:680. doi: 10.3892/etm.2021.10112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.