Abstract
Objectives: Ventricular septal rupture (VSR) is a rare but lethal complication of acute myocardial infarction (AMI). We conducted a retrospective analysis of the clinical characteristics of VSR patients and explored the risk factors for long-term mortality.
Methods: In this single-center cohort study, 127 patients diagnosed with post-AMI VSR between May 2012 and April 2019 were included. Demographic, clinical, operative, and outcome data were collected. The 30-day and long-term mortality were outcomes of interest. Cox proportional hazard regression analysis was used to explore the predictors of long-term mortality.
Results: The mean age of the VSR cohort was 66.6 ± 8.7 years, 67 (52.8%) were males. Among the 127 patients, 78 patients (61.4%) were medically managed, 31 (24.4%) patients underwent percutaneous transcatheter closure (TCC), and 18 (14.2%) patients received surgical repair. The median follow-up time was 1129 days [interquartile range: 802–2019 days]. The 30-day mortality of the medically managed group, percutaneous TCC group, and surgical management group was 93.6, 22.6, and 11.1%, respectively; and the long-term mortality was 96.2, 25.8, and 22.2%, respectively. VSR repair treatment including surgical management (HR 0.01, 95% CI 0.001–0.09, p < 0.001) and percutaneous TCC (HR 0.09, 95% CI 0.03–0.26, p < 0.001) was associated with a better prognosis, and cardiogenic shock (CS) (HR 9.30, 95% CI 3.38–25.62, p < 0.001) was an independent risk factor of long-term mortality.
Conclusions: The prognosis of VSR patients without operative management remains poor, especially in those complicated with CS. Timely and improved surgery treatment is needed for better outcomes in VSR patients.
Keywords: acute myocardial infarction, percutaneous transcatheter closure, surgery, prognosis, ventricular septal rupture (VSR)
Introduction
Ventricular septal rupture (VSR), a rare complication of acute myocardial infarction (AMI), remains one of the most challenging clinical problems to treat (1). Though the incidence of VSR has decreased to 0.2–0.5% with the advent of reperfusion strategies nowadays, (2, 3) the outcome of patients who develop VSR remains poor and appears almost unchanged over the last few decades (4). The mortality rates of patients with medical management alone were extremely high; therefore, a surgical closure is recommended to be the standard therapy by the current ST-elevation MI (STEMI) guidelines of the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) and the European Society of Cardiology (ESC) (5, 6). In the real-world clinical practice, surgery procedures were often performed during the subacute and chronic periods (≥2 weeks after the initial detection of VSR) (7). However, the better outcome observed with delayed repair operation is also criticized as a representation of survival bias, as many patients were too sick to wait for delayed surgery and died during the waiting period (8). Recently, percutaneous transcatheter closure (TCC) has emerged as an alternative to surgical closure of VSR but is mainly restricted to selected cases in which patients have small VSR in the subacute or chronic phase (9–11). Besides, some surgical modifications have been proposed but appear less promising due to the lack of the repeatability and effectiveness confirmed by other researchers (12–15). Current treatments for VSR vary greatly, but the results remain disappointing.
Data on VSR complicating AMI are limited in China. This study aimed to review the treatment of VSR complicating AMI in our single-center. We attempted to identify the current status, compare the treatment outcomes, explore the prognostic risk factors of VSR, and provide some information regarding the management of such patients.
Methods
The present study was a single-center analysis of post-AMI VSR patients at the First Affiliated Hospital of Zhengzhou University, Henan, China. Patients who were admitted because of VSR complicating AMI were retrospectively enrolled between May 2012 and April 2019. The VSR was defined as a disruption in the ventricular septum with evidence of left-to-right shunt and was confirmed by transthoracic echocardiography (TTE) examination. The enrolled cases, which exclude VSR secondary to the presence of congenital heart disease or resulting from a previous surgical procedure or by trauma or other reasons. The study was approved by the Human Research Ethics Committee of the First Affiliated Hospital of Zhengzhou University and was performed in accordance with the Declaration of Helsinki (Approved No. of ethic committee SS-2019-001). Written informed consent was obtained from each participant at their enrollment.
To assess the baseline clinical characteristics of the study cohort, we retrospectively collected data concerning patients' demographics information, hemodynamic conditions, morbidities, echocardiographic features, coronary angiography (CAG) findings, physiological data, laboratory tests. The definition of each variable was in line with the cardiovascular data standards (16). The location of the rupture was defined as apical, anterior, or posterior. Cardiogenic shock (CS) definition was according to clinical and hemodynamic criteria, including hypotension [systolic blood pressure (SBP) <90 mm Hg for 30 min or need for supportive measures to maintain the systolic blood pressure of >90 mm Hg) and evidence of end-organ hypoperfusion (17). Information on postoperative complications in patients who received VSR repair was also recorded, including low cardiac output syndrome (LCOS), renal failure requiring renal replacement therapy (CRRT), residual shunt, hemolysis requiring blood transfusion, and the length of stay in the intensive care unit.
Patient Treatment and Operation Management
All patients received standard therapy of AMI as clinically indicated. Once VSR diagnosis was established, patients were under close monitoring of hemodynamic status, consistent urine output, creatinine level, liver enzymes, and blood lactate concentration. At the same time, they were administered volume expansion, vasopressors, and inotropes, with additional therapy for preventing or treating multi-organ dysfunction syndrome. If the diagnosis of VSR is made prior to revascularization therapy, including the primary percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), prompt restoration coronary flow would be recommended for all patients. In our experience with the management of VSR patients, the surgical repair would be performed in the following cases: evidence of CS, patients with poor perfusion and cardiac output, signs of congestive heart failure, maximum use of vasopressors or intra-aortic balloon pumping (IABP) could not maintain the SBP, and evidence of end-organ hypoperfusion. However, there were a considerable number of VSR patients deteriorated rapidly in the study, which making them unable to receive surgical/percutaneous intervention and leading to high mortality among medically treated patients.
Since there is no consensus on the optimal timing for surgery nowadays, the first 2 weeks of VSR onset were defined as the acute phase. Thus, the acute or early VSR closure means that the VSR repair operation, including the percutaneous TCC and surgery, was performed in the first 2 weeks after VSR onset. A delayed elective repair approach 3–4 weeks later may be considered in patients who respond well to aggressive heart failure therapy, including medication treatment or IABP. Besides, hemodynamically stable patients with a size <15 mm apical located VSR or with residual VSR after the initial surgical approach might be suited to receive percutaneous TCC repair procedure after the acute phase (9). If a delayed elective repair strategy were chosen, the coronary flow would be restored in the infarct-related artery with aspiration thrombectomy and/or balloon angioplasty, or PCI procedure with bare-metal stent placement, or preparations made for VSR repair with CABG. The use of mechanical circulatory or ventilatory support, as well as the proper VSR repair strategy, and the choice of revascularization therapy, were left to the consensus of experienced cardiologists and cardiac surgeons, and the final decision was made by the patient and his/her family.
Follow-Up and Outcomes
The outcomes were the 30-day mortality and the long-term mortality. The Long-term mortality was defined as overall mortality during the follow-up period. The long-term outcomes were obtained by contacting each patient individually with monthly telephone interviews by trained staff.
Statistical Analysis
Continuous variables were presented as the mean and standard deviation or median [Interquartile range (IQR)] and compared with one-way analysis of variance (ANOVA) or the Mann-Whitney or Kruskal-Wallis test. Categorical variables were expressed as frequency (percentage) and assessed by the Chi-square test or Fisher's exact test (when at least an expected value in a cell is <5). Cumulative incidence rates of unadjusted long-term mortality in patients with different management were estimated by the Kaplan-Meier method and compared with the log-rank test. Cox proportional hazard regression was performed to evaluate the HR and 95% CI for the association between risk factors and long-term mortality. The factors entered into the regression analysis were as follows: management of VSR, revascularization therapy, age, sex, CS, VSR type, size of main VSR, VSR location, complicated with ventricular arrhythmia, IABP support, previous histories of MI, hypertension, diabetes, heart rate, SBP, left ventricular eject fraction, white blood cell, estimated glomerular filtration rate, N-terminal pro b-type natriuretic peptide (NT-proBNP), cardiac troponin I (CTNI), creatine kinase MB (CK-MB), lactate dehydrogenase (LDH), and aspartate transaminase (AST). Levels of NT-proBNP, CTNI, CK-MB, LDH, and AST were normalized by log10 transformation. The assumption of proportional hazards was assessed with time-dependent covariate test methods, and none of the covariates was time-dependent (P > 0.05) (Online source 2). All analyses were performed using R (The R version 4.0.3; http://www.r-project.org). A 2-sided p < 0.05 was considered to be statistically significant.
Results
Between May 2012 and April 2019, a total of 127 patients with a diagnosis of VSR complicating AMI were consecutively enrolled in this analysis. The present VSR cohort had a mean age of 66.6 ± 8.7 years, 67 (52.8%) were males. Among the 127 VSR patients, 78 (61.4%) patients were medically managed which meant treated conservatively, 31 (24.4%) patients went through percutaneous TCC, and 18 (14.2%) patients underwent surgical repair. Baseline characteristics according to patients' management strategies were detailed in Table 1. Patients in the conservatively treated group were more likely to be older, have acute VSR type, have a higher prevalence of CS (63/78, 80.8%), and a higher level of NT-proBNP and CK-MB, but more likely to have a smaller VSR size.
Table 1.
Characteristics of VSR patients stratified by different managements.
| Characteristics | Medical management (without VSR repair) (n = 78) | Percutaneous TCC management (n = 31) | Surgical management (n = 18) | P value |
|---|---|---|---|---|
| Age, (years) | 68.5 ± 8.7 | 64.0 ± 8.96 | 63.1 ± 5.53 | 0.008 |
| Male sex, n (%) | 36 (46.2) | 19 (61.3) | 12 (66.7) | 0.162 |
| Cardiogenic shock, n (%) | 63 (80.8) | 4 (12.9) | 9 (50.0) | <0.001 |
| AMI to VSR time, (days) | 3.2 ± 2.4 | 3.8 ± 2.8 | 3.5 ± 2.6 | 0.448 |
| *VSR Type, n (%) | 0.400 | |||
| Acute | 28 (36.4) | 8 (25.8) | 5 (27.8) | |
| Subacute | 22 (28.6) | 8 (25.8) | 6 (33.3) | |
| Late presentation | 27 (35.1) | 15 (48.4) | 7 (38.9) | |
| Size of main VSR, (mm) | 9.3 ± 5.3 | 10.9 ± 5.01 | 15.7 ± 6.16 | <0.001 |
| Single VSR, n (%) | 56 (82.4) | 26 (83.9) | 17 (94.4) | 0.449 |
| VSR location, n (%) | 0.332 | |||
| Apical | 62 (79.5) | 20 (64.5) | 11 (66.7) | |
| Anterior | 9 (11.5) | 6 (19.4) | 3 (16.7) | |
| Posterior | 7 (9.0) | 5 (16.1) | 4 (22.2) | |
| VSR to operation time (days) | – | 20.0 [14.0–27.0] | 14.0 [11.75–20.25] | 0.018 |
| Acute phase repair, n (%) | – | 8 (25.8) | 10 (55.6) | |
| Elective repair, n (%) | 23 (74.2) | 8 (44.4) | ||
| MI information | – | |||
| Infarct territory, n (%) | 0.953 | |||
| Anterior | 63 (81.8) | 25 (80.6) | 14 (77.8) | |
| Inferior | 11 (14.3) | 5 (16.1) | 4 (22.2) | |
| Others | 3 (3.9) | 1 (3.2) | – | |
| Prior Fibrinolysis therapy, n (%) | 13 (16.7) | 2 (6.5) | 3 (16.7) | 0.369 |
| CAG data, n (%) | <0.001 | |||
| Negative | 1 (5.3) | 3 (9.7) | 1 (5.6) | |
| LAD | 16 (84.2) | 20 (64.5) | 10 (55.6) | |
| RCA | 2 (10.5) | 4 (12.9) | 3 (16.7) | |
| LCX | – | 1 (3.2) | – | |
| Triple vessel disease | – | 2 (6.5) | 2 (11.1) | |
| Culprit artery treatment, n (%) | <0.001 | |||
| PCI | 16 (79.5) | 15 (48.4) | 4 (22.2) | |
| CABG | – | 1 (3.2) | 9 (50.0) | |
| PCI+CABG | – | 1 (3.2) | 2 (11.1) | |
| In-hospital stays, (days) | 5.0 [2.0–11.0] | 27.0 [19.0–32.0] | 31.5 [22.7–40.3] | <0.001 |
| Comorbidities, n(%) | ||||
| Current smoker | 16 (20.5) | 11 (35.5) | 5 (27.8) | 0.260 |
| Current drinker | 11 (14.1) | 5 (16.1) | 3 (16.7) | 0.942 |
| Hypertension | 42 (53.8) | 16 (51.6) | 11 (61.1) | 0.807 |
| Diabetes mellitus | 25 (32.1) | 7 (22.6) | 7 (38.9) | 0.453 |
| History of MI | 5 (6.4) | 1 (3.2) | 2 (11.1) | 0.550 |
| History of stroke/TIA | 16 (20.5) | 1 (3.2) | 4 (22.2) | 0.072 |
| Hyperlipidemia | 8 (10.3) | 2 (6.5) | 3 (16.7) | 0.526 |
| Examinations | ||||
| Heart rate, (b.p.m.) | 92.6 ± 19.6 | 92.1 ± 15.4 | 93.2 ± 15.3 | 0.977 |
| SBP, (mmHg) | 105.9 ± 18.3 | 108.5 ± 14.7 | 114.3 ± 16.5 | 0.176 |
| DBP, (mmHg) | 68.9 ± 15.7 | 71.1 ± 9.8 | 74.1 ± 11.4 | 0.344 |
| LVEF, (%) | 49.6 ± 10.1 | 52.7 ± 9.3 | 52.2 ± 8.9 | 0.299 |
| NT-pro BNP, (pg/mL) | 9517.5 [4613.8–18367.7] | 5160.0 [2610.5–10032.9] | 5861.0 [2593.8–8693.8] | 0.013 |
| CK-MB, (mmol/L) | 35.0 [15.5–74.9] | 16.0 [9.5–24.1] | 19.0 [15.5–29.6] | 0.003 |
| CTnI, (mmol/L) | 2.0 [0.96–5.24] | 0.74 [0.22–3.99] | 0.22 [0.05–8.79] | 0.134 |
| LDH, (U/L) | 737.0 [399.0–1229.0] | 604.0 [361.0–745.0] | 460.5 [288.8–915.5] | 0.248 |
| AST, (mmol/L) | 84.0 [33.5–328.5] | 37.0 [21.0–58.5] | 31.0 [20.0–278.0] | 0.191 |
| Hemoglobin, (g/L) | 121.4 ± 15.8 | 129.1 ± 47.3 | 126.3 ± 19.8 | 0.413 |
| WBC, (103/μL) | 13.0 ± 6.43 | 10.9 ± 6.18 | 11.8 ± 4.26 | 0.277 |
| Creatinine, (μmol/L) | 101.5 [74.7–159.2] | 88.4 [78.5–100.4] | 94.7 [78.3–137.5] | 0.328 |
| Blood urea nitrogen, (mmol/L) | 12.2 ± 8.74 | 9.40 ± 4.58 | 12.0 ± 8.19 | 0.252 |
| eGFR, (mL/min/1.73 m2) | 73.6 ± 34.2 | 68.5 ± 18.9 | 61.8 ± 27.2 | 0.208 |
| Total bilirubin, (mmol/L) | 20.6 ± 16.8 | 16.4 ± 9.45 | 21.3 ± 18.0 | 0.426 |
| Albumin, (mmol/L) | 36.9 ± 9.75 | 37.1 ± 7.74 | 37.5 ± 6.82 | 0.965 |
| LDL-C, (mmol/L) | 2.25 ± 0.74 | 2.35 ± 0.96 | 2.32 ± 0.80 | 0.857 |
| 30-day mortality, n (%) | 73 (93.6) | 7 (22.6) | 2 (11.1) | <0.001 |
| Long-term mortality, n (%) | 75 (96.2) | 8 (25.8) | 4 (22.2) | <0.001 |
| Survival time (days) | 5.0 [2.0–12.0] | 892.0 [45.0–1698.0] | 1059.0 [529.75–1323.25] | <0.001 |
VSR, ventricular septal rupture; TCC, Percutaneous transcatheter closure;
VSR Type: Acute (Within 24 hours Post AMI), Subacute (Within 24–72 h Post AMI), Late presentation (More than 72 h Post AMI); SD, Standard Deviation; AMI, acute myocardial infarction; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation; STEMI, ST segment elevate myocardial infarction; CAG, coronary angiography; LAD, left anterior descending; RCA, right coronary artery; LCX, left circumflex coronary artery; PCI, percutaneous coronary intervention; CABG, coronary artery bypass surgery; TIA, transient ischemic attack; SBP, systolic blood pressure; DBP, diastolic blood pressure; LVEF, left ventricular eject fraction; NT-pro BNP, N-terminal pro b-type natriuretic peptide; CK-MB, creatine kinase MB; CTNI, cardiac troponin I; LDH, lactate dehydrogenase; WBC, white blood cell; eGFR, estimated glomerular filtration rate; AST, aspartate transaminase; LDL-C, low-density lipoprotein cholesterol. P values in bold meant significantly different (P < 0.05).
The 30-day mortality rate of the conservatively treated group, percutaneous TCC group, and surgical management group was 93.6% (73/78), 22.6% (7/31), and 11.1% (2/11), respectively. The median duration of follow-up was 1129 days [Interquartile range (IQR): 802–2019 days]. During the follow-up period, another five patients (2 in the medical management group, 1 in the percutaneous TCC group, and 2 in the surgical management group) died, and no patient was lost to follow-up. The main complications included CS (76, 59.8%), ventricular arrhythmia (16, 12.6%), ventricular aneurysm (75, 59.5%), and use of IABP (21, 16.5%). Causes of death included LCOS (32, 25.2%), refractory heart failure (46, 36.2%), multiple-system organ failure (5, 3.14%), hemorrhage event (2, 1.57%), and unknown reasons (2, 1.57%) (Table 2).
Table 2.
Clinical complications, causes of death, and outcomes of patients with VSR.
| Clinical complications/outcomes | Patients N = 127 |
|---|---|
| 30-day mortality, n (%) | 82 (64.6) |
| Overall mortality, n (%) | 87 (68.5) |
| Survival time (days) | 15.0 [3.0–784.0] |
| Cardiogenic shock, n (%) | 76 (59.8) |
| Ventricular arrhythmia, n (%) | 16 (12.6) |
| Ventricular aneurysm, n (%) | 75 (59.5) |
| IABP support, n (%) | 21 (16.5) |
| Causes of death | Patients N = 127 |
| Low cardiac output syndrome, n (%) | 32 (25.2) |
| Refractory heart failure, n (%) | 46 (36.2) |
| Multiple-system organ failure, n (%) | 5 (3.14) |
| Hemorrhage event, n (%) | 2 (1.57) |
| Unknown reasons, n (%) | 2 (1.57) |
| Peri-operative complications | Patients N = 49 |
| Surgical management, n (%) | 31 (63.3) |
| Percutaneous TCC, n (%) | 18 (36.7) |
| Operation failure, n (%) | 3 (6.12) |
| Postoperative IABP, n (%) | 8 (16.3) |
| Postoperative ECMO, n (%) | 2 (4.08) |
| Postoperative CRRT, n (%) | 4 (8.16) |
| Residual VSR, n (%) | 15 (30.6) |
| Postoperative hemolysis, n (%) | 3 (6.12) |
VSR, ventricular septal rupture; TCC, Percutaneous transcatheter closure; IABP, intra-aortic balloon pump; ECMO, Extracorporeal membrane oxygenation; CRRT, continuous renal replacement therapy.
As for the 31 patients who received percutaneous TCC repair procedures, two operations failed. The first failure resulted from an appropriate position that could not be found for releasing the closure device. In another patient, the failure was due to the inability to fix the closure device. Among patients with surgical repair operations, ten patients were repaired with David's infarction exclusion technique (18). One of ten cases failed for the rupture was too large to be closed, and the patient died one day after the surgery procedure. The remaining eight patients received a modified surgery method named SurCOP (Surgical repair Combining an Occluder and a Patch) with a 100% success rate. SurCOP repair technique upgraded the VSR repair material from a simple patch to a patch combined with an arterial catheter occluder which was first performed in our institution and associated with promising results for prognosis (19). The postoperative complications were: use of IABP (8, 16.53%), use of ECMO (2, 4.08%), use of CRRT (4, 8.16%), residual VSR (15, 30.6%), and hemolysis (3, 6.12%). Patients with VSR repair management according to operation timing were also compared, and patients who receive an early VSR repair operation had higher mortality than those who underwent the delayed surgery. Detailed individual patient data and outcomes with operative management were shown in Supplementary Tables 1–3.
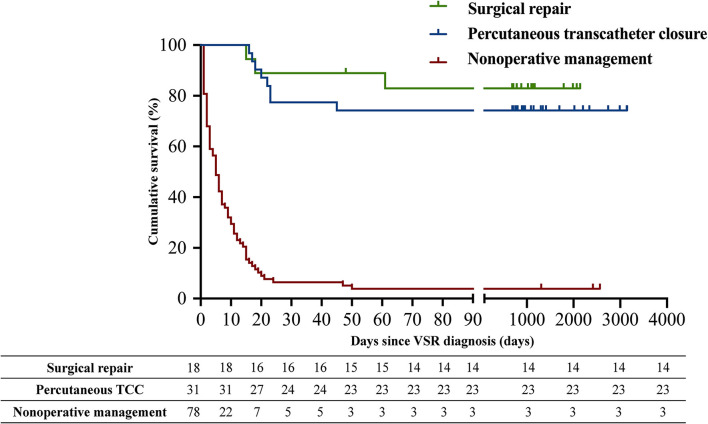
Figure 1 showed the difference in the cumulative long-term survival rates of patients with different management strategies. Patients with medical management had a significantly higher long-term mortality compared with those received percutaneous TCC and surgical management [Medical management (96.2%, 75/78) vs. percutaneous TCC (25.8%, 8/31), p < 0.001; Medical management vs. surgery (22.2%, 4/18), p < 0.001]. There was no significant survival difference between the percutaneous TCC and surgical management group (p = 0.742). Survival analysis using the Cox regression model showed that VSR medical management, non-revascularization therapy, advanced age, concomitant CS, acute VSR type, complicated with ventricular arrhythmia, lower systolic blood pressure and left ventricular eject fraction, higher level of log NT-proBNP, log CTNI, log CK-MB, log LDH, log AST, white blood cell count, and estimated glomerular filtration rate <60 mL/min/1.73 m2 were univariate predictors of the long-term mortality. Moreover, the multivariate Cox regression analysis revealed that VSR repair treatment including percutaneous TCC (HR 0.09, 95% CI 0.03–0.26, p < 0.001) and surgical management (HR 0.01, 95% CI 0.001–0.09, p < 0.001) was associated with a better long-term prognosis, and CS (HR 9.30, 95% CI 3.38–25.62, p < 0.001) was associated with a poor future outcome (Table 3).
Figure 1.
Kaplan-Meier estimates of cumulative event-free survival for long-term mortality.
Table 3.
Independent risk factors of long-term mortality.
| Predictors | Long-term mortality | |||||
|---|---|---|---|---|---|---|
| Unadjusted HR | 95% CI | P value | Adjusted HR | 95% CI | P value | |
| Management of VSR (Medical management as reference) | <0.001 | <0.001 | ||||
| Percutaneous transcatheter closure | 0.078 | 0.037–0.167 | <0.001 | 0.09 | 0.03–0.26 | <0.001 |
| Surgery | 0.066 | 0.023–0.183 | <0.001 | 0.01 | 0.001–0.09 | <0.001 |
| Revascularization therapy (Medical management as reference) | 0.001 | 0.90 | 0.40–2.04 | 0.802 | ||
| PCI | 0.46 | 0.28–0.76 | 0.002 | |||
| CABG | 0.11 | 0.03–0.47 | 0.003 | |||
| Age (year) | 1.03 | 1.01–1.06 | 0.008 | 0.99 | 0.95–1.03 | 0.588 |
| Male sex | 0.67 | 0.44–1.02 | 0.064 | 1.07 | 0.46–2.51 | 0.873 |
| Cardiogenic shock | 5.39 | 3.23–8.99 | <0.001 | 9.30 | 3.38–25.62 | <0.001 |
| VSR type (Acute VSR as reference) | 0.048 | 0.277 | ||||
| Subacute | 0.77 | 0.46–1.29 | 0.322 | 0.64 | 0.26–1.56 | 0.326 |
| Late presentation | 0.53 | 0.32–0.88 | 0.014 | 0.47 | 0.19–1.20 | 0.115 |
| Size of main VSR | 0.97 | 0.93–1.01 | 0.188 | 1.02 | 0.95–1.09 | 0.687 |
| VSR Location (Apical as reference) | 0.201 | 0.866 | ||||
| Anterior | 0.77 | 0.42–1.43 | 0.410 | 0.71 | 0.20–2.51 | 0.597 |
| Posterior | 0.53 | 0.26–1.11 | 0.092 | 0.91 | 0.21–3.95 | 0.897 |
| Complicated with ventricular arrhythmia | 1.85 | 1.05–3.26 | 0.032 | 0.43 | 0.13–1.47 | 0.179 |
| IABP support | 1.05 | 0.65–1.71 | 0.843 | 0.67 | 0.28–1.57 | 0.353 |
| Previous history of MI | 0.79 | 0.32–1.94 | 0.603 | 1.36 | 0.24–7.64 | 0.727 |
| Hypertension | 0.98 | 0.65–1.50 | 0.933 | 1.03 | 0.45–2.35 | 0.954 |
| Diabetes | 1.20 | 0.77–1.87 | 0.419 | 1.15 | 0.53–2.50 | 0.725 |
| Heart rate | 1.01 | 0.99–1.02 | 0.081 | 1.01 | 0.98–1.03 | 0.600 |
| Systolic blood pressure | 0.98 | 0.97–0.99 | 0.015 | 0.99 | 0.97–1.01 | 0.363 |
| Left ventricular eject fraction | 0.98 | 0.95–0.99 | 0.033 | 0.99 | 0.96–1.04 | 0.959 |
| Log NT-pro BNP | 4.26 | 2.30–7.88 | <0.001 | 1.74 | 0.47–6.39 | 0.406 |
| Log CTNI | 3.12 | 1.95–5.01 | <0.001 | 1.27 | 0.70–2.31 | 0.472 |
| Log CK-MB | 1.51 | 1.19–1.91 | 0.001 | 1.75 | 0.47–6.39 | 0.436 |
| Log LDH | 2.58 | 1.30–5.09 | 0.006 | 1.54 | 0.21–11.1 | 0.667 |
| Log AST | 2.37 | 1.69–3.30 | <0.001 | 0.67 | 0.26–1.70 | 0.397 |
| WBC | 1.05 | 1.02–1.08 | 0.002 | 1.04 | 0.98–1.11 | 0.228 |
| eGFR (>90 mL/min/1.73 m2 as reference) | 0.009 | 0.664 | ||||
| 60–90 mL/min/1.73 m2 | 1.20 | 0.70–2.05 | 0.516 | 1.52 | 0.52–4.72 | 0.427 |
| <60 mL/min/1.73 m2 | 2.22 | 1.30–3.80 | 0.004 | 1.57 | 0.57–4.04 | 0.401 |
HR, hazard ratios; CI, confidence intervals; VSR, ventricular septal rupture; NT-pro BNP, N-terminal pro b-type natriuretic peptide; CTNI, cardiac troponin I; CK-MB, creatine kinase MB; LDH, lactate dehydrogenase; AST, aspartate transaminase; WBC, white blood cell; eGFR, estimated glomerular filtration rate.
Discussion
Despite improvements in medical treatment and revascularization techniques during the last two decades, the prognosis of post-AMI VSR remained disappointing. In this single-center retrospective cohort study, we found that the mortality of patients treated conservatively was extremely high, with a 30-day mortality rate of 93.6% (73/78) and a long-term mortality rate of 96.2% (75/78), which was consistent with previous studies (3, 4). Patients who survived the early stage and underwent VSR repair surgery showed a good long-term prognosis, either they received percutaneous TCC operation (25.8%, 8/31) or surgical repair (22.2%, 4/18). However, whether VSR is repaired or not, CS was found to be the independent predictor of poor prognosis, which multiplied the long-term mortality rate by nearly 9.3 times.
VSR results from full-thickness MI of the interventricular septum, leading to acute left-to-right shunting and superseding biventricular failure, CS, and finally, death (20). Previous studies have found that advanced age, (21) the shorter time between AMI and surgery, (22) posterior septal rupture, (23) incomplete coronary revascularization, (24) and right ventricular dysfunction (25) were independent predictors of mortality. However, this study found that all the above factors were pale and powerless if adjusted with CS. Compared to those without CS, patients with CS at the initial onset of VSR were 2–5 times more likely to die (26–28). In this study, CS was the main cause of death, and the high mortality rate of patients with conservative treatment was mainly due to the high prevalence rate of CS (80.8%, 63/78). Therefore, it is significant to stabilize patients' hemodynamics status in the early stage to improve their survival chances. Nowadays, in addition to the optimal use of afterload reducing agents, early use of mechanical circulatory support including IABP and ECMO can rapidly improve the hemodynamic status and provide a better condition for patients with CS to receive delayed surgery (29, 30). In the presented study, the application rate of preoperative IABP and ECMO was low, which might be part of the reason for the high early mortality rate. Directly closes the rupture site by surgery is the definitive treatment for patients with VSR, and it is associated with a promising prognosis (20). Our study found that VSR repair treatment, including surgical management (HR 0.01) and percutaneous TCC (HR 0.09), was associated with an improved long-term prognosis.
Although a surgical repair is highly recommended for patients with VSR, the appropriate timing of repair surgery remains elusive. Previous studies showed that the operative mortality was extremely high when the surgery was done urgently and decreased dramatically when it was intentionally delayed (31). The 2013 American College of Cardiology and American Heart Association guidelines recommended emergency surgical repair once the VSR was diagnosed, regardless of the hemodynamic status (5). Whereas, the 2017 European Society of Cardiology guidelines prefer delaying VSR repair operation in patients who respond well to aggressive medication therapy (6). Unfortunately, the better outcome of an elective surgery might be a manifestation of survival bias. After a waiting period of 4–6 weeks, the necrotic myocardium could undergo fibrotic remodeling, and the tensile strength is high enough to sustain the defect interpolation (32). This will definitely improve the prognosis of those patients who can survive the waiting period. However, those patients with hemodynamic instability could not survive long enough to receive the surgical intervention (7). Our research was no exception to this bias. In the present study, the median survival time of medically treated patients was 5 days, and more than 75% of patients died within 12 days of VSR symptom onset, but the median time from onset of VSR to the repair procedure was about 18.0 [13.0–24.5] days. As an early surgery intervention offers the only realistic chance of survival and each survivor is something to treasure, we cannot help thinking that these patients might derive the maximal benefit from much earlier and aggressive surgical therapy. Though surgical mortality of VSR patients with CS in the early phase remains very high, non-surgical mortality is undoubtedly higher. Thus, we clinicians should weigh the risk of the extended indications of repair surgery against the risk of postponing surgery and developing further clinical deterioration.
Nowadays, the David infarct exclusion (IE) strategy has been widely used in surgical procedures (18). In fact, insertion of a large patch that bears strong tension might tear off the friable myocardium from the suture line, resulting in the significant operative complication of concern, postoperative residual shunt, which has been considered the most crucial risk factor for poor outcomes (33). Percutaneous TCC has recently emerged as a potential strategy; however, it is mainly restricted to patients with a small VSR in the subacute or chronic phase. When operated in the acute phase, TCC is associated with high operative mortality (34). An improved technique of both surgical and percutaneous repairs was urgently needed. Recently, numerous modifications of the surgical techniques have been proposed: two patches with or without gelatin-resorcin-formalin, three-patch technique, local applications of adhesives, etc. (12–15). Regrettably, these techniques tend to be more complicated, and the reproducibility issue is of utmost concern. Based on our experience with the management of VSR, we also proposed a modified surgical repair technique, named SurCOP (Surgical repair Combining an Occluder and a Patch), which combines the use of a patent ductus arteriosus occluder with a slightly larger bovine pericardial patch to close the rupture site and the preliminary results have been reported (19). Till April 2019, the SurCOP was performed on eight patients, and our experience has shown that the SurCOP technique is a safe, easy-to-manipulate, and effective method that can be used in patients with hemodynamic instability.
The present study increased our knowledge of the current status of this rare complication and demonstrated the mortality risk factors of VSR. There are several other limitations to this investigation. First, the better results of a VSR repair surgery might be a manifestation of survival bias, as it is usually performed in relatively stable patients with VSR who are expected to have a better prognosis than those patients with hemodynamic instability in the early stage. Our research was no exception to this bias. Second, this study was retrospective, and patient selection could not be randomized. Although all data were collected retrospectively, selection and recall bias could not be completely prevented. Another consideration is that all patients in the research were enrolled from a single center; thus, their prognoses might be the results of more specialized teams with sufficient expertise instead of more general facilities.
Conclusion
VSR is relatively rare but highly lethal in clinical practice. The outcomes of patients with VSR are still disappointing. The patient's survival chance depends on the intervention closure of the VSR. Thus, the coordination of surgical expertise and the application of novel treatment methods are required to improve the clinical outcomes of patients with VSR.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the First Affiliated Hospital of Zhengzhou University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LW, X-FW, and J-ZD: study planning, study analysis, and responsible for the overall content as guarantors. CL, Y-ZZ, X-YZ, and LL: conducted the study and performed the examinations. LW and L-LX: performed the statistical analysis and wrote the manuscript. All authors have read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.679148/full#supplementary-material
References
- 1.Crenshaw BS, Granger CB, Birnbaum Y, Pieper KS, Morris DC, Kleiman NS, et al. Risk factors, angiographic patterns, and outcomes in patients with ventricular septal defect complicating acute myocardial infarction. Circulation. (2000) 101:27–32. 10.1161/01.CIR.101.1.27 [DOI] [PubMed] [Google Scholar]
- 2.Moreyra AE, Huang MS, Wilson AC, Deng Y, Cosgrove NM, Kostis JB, MIDAS Study Group (MIDAS 13) . Trends in incidence and mortality rates of ventricular septal rupture during acute myocardial infarction. Am J Cardiol. (2010) 106:1095–100. 10.1016/j.amjcard.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 3.Goldsweig AM, Wang Y, Forrest JK, Cleman MW, Minges KE, Mangi AA, et al. Ventricular septal rupture complicating acute myocardial infarction: incidence, treatment, and outcomes among medicare beneficiaries 1999–2014. Catheter Cardiovasc Interv. (2018) 92:1104–15. 10.1002/ccd.27576 [DOI] [PubMed] [Google Scholar]
- 4.Birnbaum Y, Fishbein MC, Blanche C, Siegel RJ. Ventricular septal rupture after acute myocardial infarction. New Eng J Med. (2002) 347:1426–32. 10.1056/NEJMra020228 [DOI] [PubMed] [Google Scholar]
- 5.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation. (2013) 127:e362–425. 10.1161/CIR.0b013e3182742cf6 [DOI] [PubMed] [Google Scholar]
- 6.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. (2018) 39:119–77. 10.5603/KP.2018.0041 [DOI] [PubMed] [Google Scholar]
- 7.Jones BM, Kapadia SR, Smedira NG, Robich M, Tuzcu EM, Menon V, et al. Ventricular septal rupture complicating acute myocardial infarction: a contemporary review. Eur Heart J. (2014) 35:2060–8. 10.1093/eurheartj/ehu248 [DOI] [PubMed] [Google Scholar]
- 8.Omar S, Morgan GL, Panchal HB, Thourani V, Rihal CS, Patel R, et al. Management of post-myocardial infarction ventricular septal defects: a critical assessment. J Interven Cardiol. (2018) 31:939–48. 10.1111/joic.12556 [DOI] [PubMed] [Google Scholar]
- 9.Attia R, Blauth C. Which patients might be suitable for a septal occluder device closure of postinfarction ventricular septal rupture rather than immediate surgery? Interact Cardiovasc Thorac Surg. (2010) 11:626–9. 10.1510/icvts.2010.233981 [DOI] [PubMed] [Google Scholar]
- 10.Calvert PA, Cockburn J, Wynne D, Ludman P, Rana BS, Northridge D, et al. Percutaneous closure of postinfarction ventricular septal defect: in-hospital outcomes and long-term follow-up of UK experience. Circulation. (2014) 129:2395–402. 10.1161/CIRCULATIONAHA.113.005839 [DOI] [PubMed] [Google Scholar]
- 11.Ari H, Melek M, Ari S, Doganay K, Coşar Öztaş S. Percutaneous closure of post-myocardial infarction ventricular septal rupture in patients with ventricular septal rupture and apical thrombus: first case in literature. Int J Cardiol. (2015) 182:487–90. 10.1016/j.ijcard.2014.12.164 [DOI] [PubMed] [Google Scholar]
- 12.Gerola LR, Kim HC, Filho AP, Araújo W, Santos PC, Buffolo E, et al. New surgical technique for ventricular septal rupture closure after myocardial infarction. J Thorac Cardiovasc Surg. (2007) 134:1073–6. 10.1016/j.jtcvs.2007.05.063 [DOI] [PubMed] [Google Scholar]
- 13.Yamasaki T, Matsuzaki Y, Hohri Y, Hiramatsu T. Modified double patch repair for septal rupture with ventricular wall dissection. Ann Thorac Surg. (2018) 106:e289–91. 10.1016/j.athoracsur.2018.05.008 [DOI] [PubMed] [Google Scholar]
- 14.Parachuri VR, Tripathy AK, Gaikwad NM, Singh AP, Mahajan V, Niranjan S. Modified infarct exclusion technique for repair of postinfarction ventricular septal rupture. Ann Thorac Surg. (2019) 107:e219–21. 10.1016/j.athoracsur.2018.09.045 [DOI] [PubMed] [Google Scholar]
- 15.Ranocchi F, Lio A, Fiorani B, Musumeci F. A modified transatrial approach for repair of postinfarction ventricular septal defect. Ann Thorac Surg. (2019) 107:e147–9. 10.1016/j.athoracsur.2018.08.077 [DOI] [PubMed] [Google Scholar]
- 16.Anderson HV, Weintraub WS, Radford MJ, Kremers MS, Roe MT, Shaw RE, et al. Standardized cardiovascular data for clinical research, registries, and patient care. J Am Coll Cardiol. (2013) 61:1835–46. 10.1016/j.jacc.2012.12.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hochman JS, Buller CE, Sleeper LA, Boland J, Dzavik V, Sanborn TA, et al. Cardiogenic shock complicating acute myocardial infarction—etiologies, management and outcome: a report from the SHOCK trial registry. J Am Coll Cardiol. (2000) 36:1063–70. 10.1016/S0735-1097(00)00879-2 [DOI] [PubMed] [Google Scholar]
- 18.David TE, Dale L, Sun Z. Postinfarction ventricular septal rupture: repair by endocardial patch with infarct exclusion. J Thorac Cardiovasc Surg. (1995) 110:1315–22. 10.1016/S0022-5223(95)70054-4 [DOI] [PubMed] [Google Scholar]
- 19.Liu C, Xiao L-L, Wang L, Sun F-Q, Yao X-X, Zhang Y-Z, et al. New surgical technique for post-myocardial infarction ventricular septal rupture with hemodynamic instability. Chin Med J. (2021) 134:981–3. 10.1097/CM9.0000000000001442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murday A. Optimal management of acute ventricular septal rupture. Heart. (2003) 89:1462–6. 10.1136/heart.89.12.1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pojar M, Harrer J, Omran N, Turek Z, Striteska J, Vojacek J. Surgical treatment of postinfarction ventricular septal defect: risk factors and outcome analysis. Interact Cardiovasc Thorac Surg. (2018) 26:41–6. 10.1093/icvts/ivx230 [DOI] [PubMed] [Google Scholar]
- 22.Cinq-Mars A, Voisine P, Dagenais F, Charbonneau É, Jacques F, Kalavrouziotis D, et al. Risk factors of mortality after surgical correction of ventricular septal defect following myocardial infarction: Retrospective analysis and review of the literature. Int J Cardiol. (2016) 206:27–36. 10.1016/j.ijcard.2015.12.011 [DOI] [PubMed] [Google Scholar]
- 23.Jeppsson A, Liden H, Johnsson P, Hartford M, Rådegran K. Surgical repair of post infarction ventricular septal defects: a national experience Eur J Cardiothorac Surg. (2005) 27:216–21. 10.1016/j.ejcts.2004.10.037 [DOI] [PubMed] [Google Scholar]
- 24.Takahashi H, Arif R, Almashhoor A, Ruhparwar A, Karck M, Kallenbach K. Long-term results after surgical treatment of postinfarction ventricular septal rupture. Eur J Cardiothorac Surg. (2015) 47:720–4. 10.1093/ejcts/ezu248 [DOI] [PubMed] [Google Scholar]
- 25.Pang PY, Sin YK, Lim CH, Tan TE, Lim SL, Chao VT, et al. Outcome and survival analysis of surgical repair of post-infarction ventricular septal rupture. J Cardiothorac Surg. (2013) 8:44. 10.1186/1749-8090-8-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menon V, Webb JG, Hillis LD, Sleeper LA, Abboud R, Dzavik V, et al. Outcome and profile of ventricular septal rupture with cardiogenic shock after myocardial infarction: a report from the SHOCK trial registry. J Am Coll Cardiol. (2000) 36:1110–6. 10.1016/S0735-1097(00)00878-0 [DOI] [PubMed] [Google Scholar]
- 27.Lundblad R, Abdelnoor M, Geiran OR, Svennevig JL. Surgical repair of postinfarction ventricular septal rupture: risk factors of early and late death. J Thorac Cardiovasc Surg. (2009) 137:862–8. 10.1016/j.jtcvs.2008.09.008 [DOI] [PubMed] [Google Scholar]
- 28.Singh V, Rodriguez AP, Bhatt P, Alfonso CE, Sakhuja R, Palacios IF, et al. Ventricular septal defect complicating ST-elevation myocardial infarctions: a call for action. Am J Med. (2017) 130:863.e1–e12. 10.1016/j.amjmed.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 29.Rob D, Špunda R, Lindner J, Rohn V, Kunstýr J, Balík M, et al. A rationale for early extracorporeal membrane oxygenation in patients with postinfarction ventricular septal rupture complicated by cardiogenic shock: ECMO in patients with ventricular septal rupture. Eur J Heart Fail. (2017) 19:97–103. 10.1002/ejhf.852 [DOI] [PubMed] [Google Scholar]
- 30.Ariza-Solé A, Sánchez-Salado JC, Sbraga F, Ortiz D, González-Costello J, Blasco-Lucas A, et al. The role of perioperative cardiorespiratory support in post infarction ventricular septal rupture-related cardiogenic shock. Eur Heart J Acute Cardiovasc Care. (2020) 9:128–37. 10.1177/2048872618817485 [DOI] [PubMed] [Google Scholar]
- 31.Papalexopoulou N, Young CP, Attia RQ. What is the best timing of surgery in patients with post-infarct ventricular septal rupture? Int Cardiovasc Thorac Surg. (2013) 16:193–6. 10.1093/icvts/ivs444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Furui M, Yoshida T, Kakii B, Uchino G, Nishioka H. Strategy of delayed surgery for ventricular septal perforation after acute myocardial infarction. J Cardiol. (2018) 71:488–93. 10.1016/j.jjcc.2017.10.016 [DOI] [PubMed] [Google Scholar]
- 33.Arnaoutakis GJ, Zhao Y, George TJ, Sciortino CM, McCarthy PM, Conte JV. Surgical Repair of ventricular septal defect after myocardial infarction: outcomes from the society of thoracic surgeons national database. Ann Thorac Surg. (2012) 94:436–44. 10.1016/j.athoracsur.2012.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thiele H, Kaulfersch C, Daehnert I, Schoenauer M, Eitel I, Borger M, et al. Immediate primary transcatheter closure of postinfarction ventricular septal defects. Eur Heart J. (2008) 30:81–8. 10.1093/eurheartj/ehn524 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.