Abstract
Introduction and importance
This case report details the first use of Axial 3D printing technology in Northern Ireland for surgical planning and decision making in ENT skull base surgery.
Case presentation
39 year old male seen at ENT clinic with nasal congestion. CT showed multi-sinus mucosal thickening. Histology reported inverted papilloma polyp. The surgical options were modified Lothrops endoscopic sinus surgery or an open approach of frontal sinuses with osteoplastic flap and septorhinoplasty. A model 3D skull was created by Axial 3D using stereolithography 3D printing technology with photopolymer resin. The tumour was printed in a contrasting colour, which allowed clear visualisation and appreciation of tumour borders and relations to surrounding structures. The patient underwent FESS with modified Lothrops approach, achieving good clearance of polyp.
Clinical discussion
The use of a 3D model allowed for visualisation of tumour size and relation to surrounding anatomy, particularly the absence of dural involvement within the fontal sinus. It assisted in surgical planning. The use of the 3D skull was beneficial for patient as it allowed less invasive surgery and therefore shorter recovery. It was beneficial for the hospital organisation as it lowered resource requirements of theatre time, hospital bed days and staff resources. One limitation of the 3D printed skull was that the fine lamellae ethmoid air cells were not shown due to the manufacturing process.
Conclusion
The use of 3D printing is becoming increasingly popular as a surgical aid. We found the use of the 3D skull to be useful in individualised surgical planning for endoscopic sinus surgery.
Keywords: 3D printing technology, Skull base surgery, ENT, Case report
Highlights
-
•
The use of 3D printed skull model informed choice of intervention.
-
•
The skull model allowed clear visualisation and appreciation of tumour borders and relations to surrounding structures.
-
•
One limitation of the model skull was that the fine lamellae ethmoid air cells were not shown.
-
•
The use of 3D printing is becoming increasingly popular as a surgical aid.
-
•
The skull model can be used as a teaching aid.
1. Introduction
This case report details the first use of Axial 3D printing technology in Northern Ireland for surgical planning and decision making in ENT skull base surgery. The use of 3D printed skull model informed our choice of intervention. This case report has been reported in line with the SCARE 2020 criteria [1].
2. Clinical details
39 year old caucasian male referred by his GP to ENT outpatient clinic with poor airflow through his nose. He was a non-smoker and had no significant past medical history, family history or regular medications. Over the counter decongestants (xylometazoline hydrochloride nasal spray, one spray in each nostril t.d.s) had not alleviated his symptoms. On examination there was a large left sided nasal polyp and grossly deviated septum to the right side. Biopsy of the polyp was carried out and showed inverted papilloma (Schneiderian). CT sinuses showed marked mucosal thickening in the frontal, ethmoidal, sphenoidal and both maxillary sinuses. Both osteomeatal complexes were occluded. There was nasal congestion, mainly on the left side, which was in-keeping with polyposis. Soft tissue extension was seen to oropharyngeal space. The case was discussed at the regional radiology meeting and the patient was referred to a rhinology specialist for surgical planning. The surgical options discussed with the patient were to proceed with either modified Lothrops functional endoscopic sinus surgery (FESS) or an open approach of frontal sinuses with osteoplastic flap and septorhinoplasty. Pre-operatively the patient was prescribed 2 months of betamethasone sodium phosphate 0.1% w/v nose drops (two drops in each nostril t.d.s).
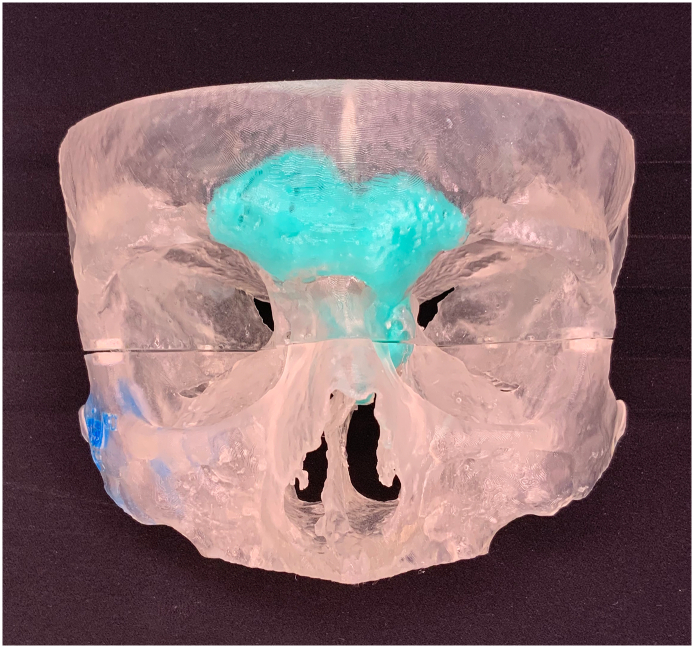
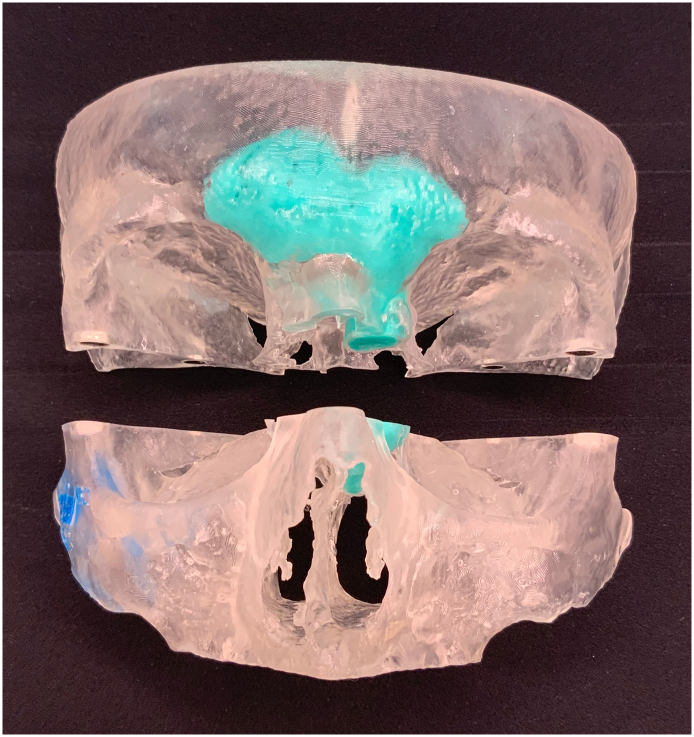
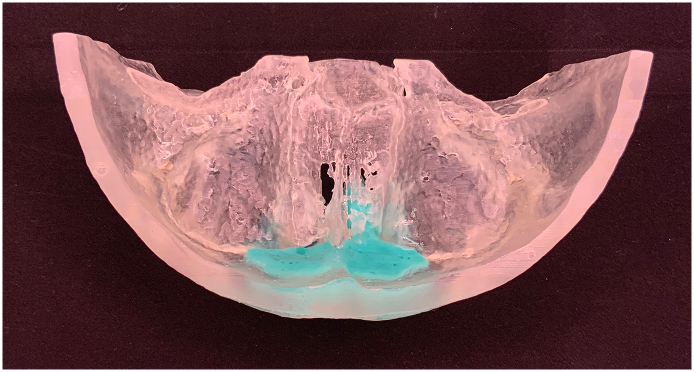
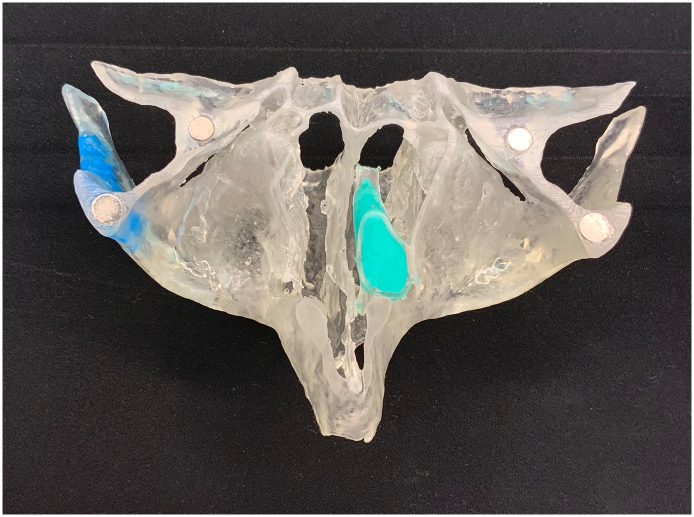
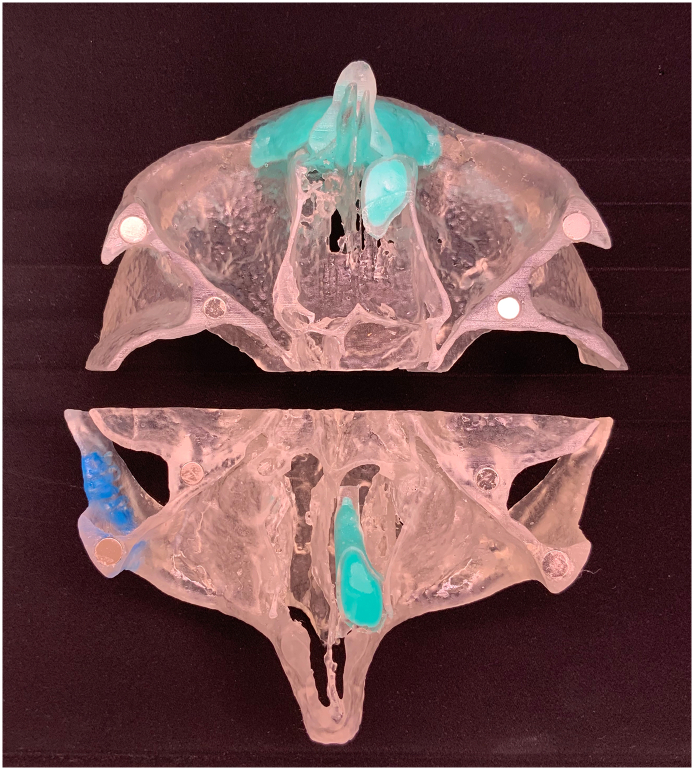
A model 3D skull was created by Axial 3D using stereolithography 3D printing technology with photopolymer resin. The skull was made in 1:1 scale with tolerance of 0.2 mm. The tumour was printed in a contrasting colour to the colour of the skull, which allowed clear visualisation and appreciation of tumour borders and relations to surrounding structures. Normal pricing for the skull would be £750 (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6).
Fig. 1.
Frontal view of 3D skull. Tumour represented by teal section.
Fig. 2.
Frontal view of skull model showing two adjoining halves.
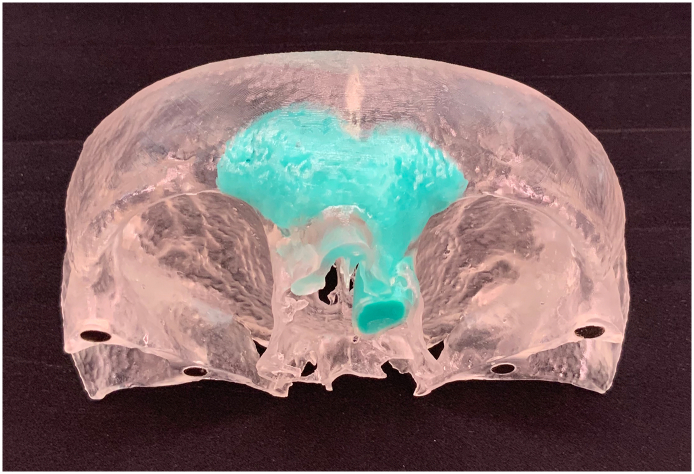
Fig. 3.
Model tumour within frontal sinuses.
Fig. 4.
Tumour borders demonstrating no invasion into dura.
Fig. 5.
Axial view of nasal cavity- large polyp.
Fig. 6.
Skull model splits through maxillary sinuses. Internal view of sinuses and relation of tumour of each.
The patient underwent functional endoscopic sinus surgery with modified Lothrops approach, by a consultant ENT surgeon in a District General Hospital, without complication. Good clearance of polyp mass was achieved. The patient recovered well and was discharged the following day. Discharge medication included saline nasal douche to be used twice daily for two months, xylometazoline hydrochloride nasal spray (one spray in each nostril t.d.s) for two weeks and he was advised to continue use of the betamethasone nasal drops for two months. Biopsies of the left sided polyp showed inverted papilloma with partial squamous metaplasia. Biopsies from right nasal airway and right frontal recess showed inflammatory type polyp with no dysplasia or malignancy.
When the patient was reviewed face to face in clinic 2 months after his operation there was residual inflammation from surgery but already his nasal congestion had improved. He was reviewed again 6 months after his operation. All nasal symptoms had settled and there was no evidence of recurrence on rigid nasal endoscopy. The patient was pleased with his management, and grateful for the less invasive approach.
3. Discussion
Use of 3D printed models is becoming increasingly popular as an aid to surgical planning. We found that the 3D printed skull presented both benefits and limitations.
The use of a 3D model allowed for clear visualisation of tumour size and relation to surrounding anatomy, particularly the absence of dural involvement within the fontal sinus. The 3D skull assisted in making the decision to carry out less invasive surgery and ultimately provided the confidence to attempt a more conservative surgical approach. Both patient and surgeon were happy with the outcome of the surgery.
The 3D skull had particular benefits for the patent; less invasive surgery meant a shorter recovery time, less potential for complications, and less risk of post-operative scaring or deformity.
The use of 3D skull also had benefits for the hospital; the less invasive approach took less time in theatre which allowed for more cases to be performed on the theatre list that day. The patient was fit for discharge the following day which meant less hospital bed days and fewer hours of healthcare staff care were required in the post-operative period. There was no need for an oestoplastic flap template to be created which was another cost that was avoided with the conservative approach.
One limitation of the 3D printed skull was that the fine lamellae ethmoid air cells were not shown due to the manufacturing process. The skull cost is £750 for this one piece, however when balanced against theatre time, hospital bed days, staff resources, osteoplastic flap it could be considered finically beneficial.
4. Other examples of 3D printing technology used in skull base surgery
Muelleman et al. studied the utility of 3D printed models in individualised petroclival tumour resection planning. They found that individualised 3D models were useful for pre-operative planning and that any limitations of individual surgical approach which were not identified through pre-operative imaging were apparent after 3D models were evaluated. However they did note that one drawback was that the printing process did not replicate mastoid air cells [2].
The 3D skull also lends itself to learning opportunities after it has completed it's role in surgical planning. Narayanan et el studied the role of 3D printed models in endoscopic skull base training. They held a sinus surgery workshop using 3D printed skulls. They found that the 3D models were suitable for learning key endoscopic skills and that anatomical structures were accurately represented by the models [3].
5. Conclusion
The use of 3D printing is becoming increasingly popular as a surgical aid. In this case we found the use of the 3D skull to be useful in individualised surgical planning for endoscopic sinus surgery. In summary we found it to be beneficial for the patient as it allowed less invasive surgery and therefore shorter recovery time. It is also beneficial for the organisation as it lowered resource requirements. The skull can be used for teaching opportunities once it's original purpose has been fulfilled. Development to allow for replication of fine lamella ethmoid air cells would enhance this product. We recommend a case series to further evaluate the use of 3D printing within the field of ENT surgery.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
None.
Ethical approval
N/A.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
N/A.
Guarantor
Miss Aoife Mallon
Presentations
This case report has been presented as a poster presentation at the ASIT Annual conference 2021.
Credit authorship contribution statement
Ms. Aoife Mallon- data collection, writing the paper, submitting the paper.
Mr. Turlough Farnan- data collection, editing the paper, provided images.
Declaration of competing interest
None declared.
Contributor Information
Aoife Mallon, Email: aoife.mallon@doctors.org.uk.
Turlough Farnan, Email: turlough.farnan@southerntrust.hscni.net.
References
- 1.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Muelleman Thomas John, Peterson Jeremy, Chowdhury Naweed Iffat, Jason Group Naweed Iffat, Camarata Paul, Lin James. Individuali`ed surgical approach planning for petroclival Tumours using a 3D printer. J. Neural Surg. B Skull Base. 2016;77(3):243–248. doi: 10.1055/s-0035-1566253. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Narayanan Variravan, Narayanan Prepageran, Waran Vicknes. European Archives of too-rhino-laryngology. Vol. 272. 2015. Endoscopic skull base training using 3D printed models with pre-existing pathology; pp. 753–757. [DOI] [PubMed] [Google Scholar]