Abstract
Objective:
This study was conducted to determine the clinical practice and barriers of ventilatory support management in COVID-19 patients in Saudi Arabia among respiratory therapists.
Methods:
A validated questionnaire comprising three parts was distributed to all critical care respiratory therapists registered with the Saudi Society for Respiratory Care through the official social networks.
Results:
A total of 74 respiratory therapists completed the survey. The mean (±standard deviation) of intensive care unit beds was 67 ± 79. Clinical presentation (54%) and arterial blood gas (38%) were the two main diagnostic tools used to initiate ventilatory support. While protocols for the initiation of invasive mechanical ventilation (IMV; 81%) were widely available, participants had limited availability of protocols for the use of non-invasive ventilation (NIV; 34%) and high-flow nasal cannula (HFNC; 34%). In mild cases of COVID-19, most respondents used HFNC (57%), while IMV was mostly used in moderate (43%) and severe (93%) cases. Regular ventilator check was mostly done every 4 h (57%). BiPAP (47.3%) and full-face masks (45.9%) were the most used mode and interface, respectively, while pressure-regulated volume control (55.4%) and pressure control (27%) were the most used mechanical ventilation modes for COVID-19 patients. In terms of use of proning, 62% used it on IMV, while 26% reported using awake proning. Staff shortage (51.4%), personal protective equipment (PPE) shortage (51.4%), increased workload (45.9%), inadequate training (43.2%) and lack of available protocols and policies (37.8%) were the main barriers.
Conclusion:
Ventilatory support management of COVID-19 in Saudi Arabia was inconsistent with the global practice, lacked uniformity, and there was limited use of standard protocols/treatment guidelines. Shortage of staff and PPE, increased workload and insufficient training were the most prevalent barriers.
Keywords: COVID-19, intensive care units, mechanical ventilation, noninvasive ventilation, respiratory, Saudi Arabia
INTRODUCTION
The coronavirus disease-2019 (COVID-19) pandemic continues to overwhelm health-care services around the world.[1] It is estimated that 5%–8% of individuals diagnosed with COVID-19 become critically ill and may develop acute respiratory failure that necessitates ventilatory support initiation.[2] Individuals diagnosed with COVID-19 may require either noninvasive respiratory support and/or invasive mechanical ventilation (IMV) to aid breathing and improve gas exchange.[3]
Noninvasive respiratory support includes high-flow nasal cannula (HFNC), and noninvasive ventilation (NIV) is often used to reduce the rate of tracheal intubation and associated complications.[4,5] Although their efficacy and safety remain unclear, HFNC and NIV are commonly used in critically ill patients diagnosed with COVID-19 to reduce respiratory symptoms, improve prognosis and ultimately reduce tracheal intubation.[6,7] With regard to IMV, two large epidemiological studies have indicated that the rate of tracheal intubation among COVID-19 patients admitted to intensive care unit ranges from 29% to 89%.[8,9]
Ventilatory support managements in critically ill patients diagnosed with COVID-19 are derived mainly from evidence on standard intensive care management and/or direct experience.[3] Alqahtani et al.,[10] in their recent international study of current techniques of ventilatory support management in COVID-19, reported significant variability and heterogeneity with minimal usage of specific protocols and most of the ventilatory support practices being based on isolated and varied guidelines. The researchers also concluded that major restricting factors affecting global COVID-19 ventilatory support managements are increased workload, shortage of skilled staff and lack of personal protective equipment (PPE).
Current literature lacks unified global protocols for ventilatory support that guide critical care providers in the battle against COVID-19. Challenges and barriers related to ventilatory support management vary from country to country. While Saudi Arabia is one of the leading countries in the global fight against COVID-19, it is important to understand the general practices of ventilatory support management within the country. Therefore, this study explores and assesses the clinical practice and barriers regarding ventilatory support management of COVID-19 patients among respiratory therapists in Saudi Arabia.
METHODS
Study design and participants
This cross-sectional survey used a convenience sampling method, as it was the most feasible option for recruiting participants during the pandemic. To ensure a countrywide sample representativeness, the Saudi Society for Respiratory Care (SSRC) was contacted to distribute the survey to registered members using their official platforms. The period of the survey was during the peak of the first wave of COVID-19 infection in the country (i.e., April 25 to June 15, 2020).
Data collection
A web-based survey was hosted at SurveyMonkey (www.surveymonkey.com, Portland, Oregon, USA) that was developed according to current literature and validated by 10 international experts.[10] The link of the survey was openly available on the SSRC platforms. This adaptive survey included 32 questions distributed across three sections. Part one elicits the demographic information of the participants, including hospital characteristics, training, and experience. Part two explores the clinical practices of ventilatory support management in COVID-19 patients that includes diagnosis strategies, mechanical ventilation (MV) types used and other unconventional ventilation strategies. Part three determines the limitations and barriers faced by respiratory therapists during the ventilatory support management of COVID-19 patients. We conducted face and content validity after piloting this to 10 critical care respiratory therapists. The approximate estimated time for completing the questionnaire based on the pilot testing was 10 min. Formal training in MV was defined as theoretical and practical sessions for not less than 6 weeks. In addition, disease severity was defined according to the 2012 Berlin definition of acute respiratory distress syndrome.[11]
SSRC distributed the survey to registered members using official platforms. The participants were informed about the purpose of the study, the estimated time for completing the survey, data confidentiality and participation being voluntary. No incentive (monetary or nonmonetary) was offered. The respondents were able to review all responses before submitting the survey. No duplication in responses was ensured through the use of IP address.
Data analysis
The data were automatically captured through the hosting platform and then exported to an Excel Sheet. To mimimize the likeliness of errors, the exported data were verified and proofchecked by one of the authors and cross-verified by another. Descriptive analysis (i.e., absolute values and proportions) were used to analyze responses and summarize respondents' characteristics. Chi-square and Fisher's exact tests were applied to draw comparisons between groups. The Statistical Package for the Social Sciences (SPSS) version 25 (IBM Corp., Armonk, NY, USA) was used to analyze the collected responses. P ≤ 0.05 was considered statistically significant. As our survey was an online web survey, only the completion rate could be calculated. Completion of the survey was defined as those who answered all questions that were considered mandatory in each section for eliciting information necessary for achieving the objective of this study.
Ethical considerations
Ethical approval was obtained from the Institutional Review Board of the Armed Forces Hospital, Eastern Region, Saudi Arabia. Response to the survey was considered as consent for participation. The personal information was converted to anonymized data that were to be deleted as soon as it was processed.
RESULTS
A total of 79 critical care respiratory therapists from across Saudi Arabia completed the survey; the completion rate was 82%. Of these, five responses were excluded from the final analysis due to incomplete responses. The demographic data and characteristics of all respondents are presented in Table 1.
Table 1.
Characteristics of respiratory therapists (n=74)
| Characteristics | Values, n (%) |
|---|---|
| Qualification | |
| Diploma | 5 (6.8) |
| Bachelor | 48 (64.9) |
| Master | 19 (25.7) |
| PhD | 2 (2.7) |
| Type of hospital | |
| Secondary care | 22 (29.7) |
| Tertiary care | 52 (70.3) |
| Number of beds in hospital | |
| <200 | 20 (27.8) |
| 200–499 | 28 (38.9) |
| 500–1000 | 16 (22.2) |
| >1000 | 8 (11.1) |
| ICU beds | |
| Total number | 4883 |
| Mean±SD | 67±79 |
| Previous training in MV use | 71 (95.9) |
| Experience and training in MV use | |
| >20-year experience | 4 (5.4) |
| 11–20-year experience | 12 (16.2) |
| 6–10-year experience | 25 (33.8) |
| ≤5-year experience | 33 (44.6) |
| >20-year experience and trained | 4 (5.6) |
| 11–20-year experience and trained | 10 (14.1) |
| 6–10-year experience and trained | 25 (35.2) |
| ≤5-year experience and trained | 32 (45.1) |
ICU – Intensive care unit; SD – Standard deviation; MV – Mechanical ventilation
Qualifications, experience and formal training of respondents
Bachelor's degree was the most common academic qualification among the respondents (64.9%). Most respondents were from tertiary care hospitals (70.3%). While 71 (95.9%) of the respondents had training in the use of mechanical ventilators, the tendency to be trained was not related to the years of experience (P = 0.1) and qualifications (P = 0.4). Most of the respiratory therapists (32; 45.1%) with training in MV had a ≤5-year experience [Table 1]. Moreover, no significant difference was found in formal training (P = 0.9), years of experience (P = 0.7) and qualifications (P = 0.7) between the secondary and tertiary care hospital types.
Factors for the initiation of therapy
Clinical presentation (40/74, 54%) and arterial blood gas (28/74, 38%) were the two diagnostic tools most commonly used in deciding the mode of ventilator support needed by COVID-19 patients [Table 2]. While protocols for the initiation of IMV were widely available (81%), the protocols for the use of NIV and HFNC were not readily available (34% for both). The general management of COVID-19 patients was mainly based on the guidelines of the World Health Organization (62%), followed by national guidelines (54%). For clinical management of mild cases of COVID-19, most respondents used HFNC (57%), while IMV was mostly used in both moderate (43%) and severe (93%) cases. The decision regarding the method of ventilatory management in mild, moderate or severe cases was mostly validated by using existing protocols and results from diagnostic tools. Ventilator check was mostly done every 4 h (57%), followed by “As needed” (32%).
Table 2.
Factors considered in the clinical management of COVID-19 patients and the maintenance of ventilators
| Characteristics | Values, n (%) |
|---|---|
| Diagnostic tool used to initiate treatment | |
| Arterial blood gas | 28 (38) |
| Chest imaging | 4 (5) |
| Clinical presentation | 40 (54) |
| All of the above | 2 (3) |
| Available protocols | |
| HFNC | 25 (34) |
| NIV | 32 (43) |
| IMV | 60 (81) |
| COVID-19 guidelines used | |
| Local guideline | 34 (46) |
| National guideline | 40 (54) |
| WHO | 46 (62) |
| AARC | 36 (49) |
| NICE | 7 (10) |
| ANZICS | 5 (7) |
| SCCM | 19 (26) |
| Initial ventilation strategy based on severity | |
| Mild | |
| HFNC | 42 (57) |
| NIV | 15 (20) |
| IMV | 8 (11) |
| Moderate | |
| HFNC | 13 (18) |
| NIV | 23 (31) |
| IMV | 32 (43) |
| Severe | |
| HFNC | 1 (1) |
| NIV | 0 |
| IMV | 69 (93) |
| Ventilator management | |
| Suctioning system used | |
| Open | 2 (3) |
| Closed | 72 (97) |
| Ventilator system check | |
| As needed | 24 (32) |
| Every 1–2 h | 2 (3) |
| Every 2 h | 6 (8) |
| Every 4 h | 42 (57) |
HFNC – High-flow nasal cannula; NIV – Noninvasive ventilation; IMV – Invasive mechanical ventilation; WHO – World Health Organization; AARC – American Association for Respiratory Care; ANZICS – The Australian and New Zealand Intensive Care Society; SCCM – The Society of Critical Care Medicine; NICE – National Institute for Health & Care Excellence
Clinical management of ventilatory support in COVID-19 patients
HFNC initial flow of 30 to 45 L/m was the most used technique (41.9%), and this was combined with humidification in most cases (73%). For NIV, BiPAP (47.3%) and full-face masks (45.9%) were the most used mode and interface, respectively [Table 3]. Pressure-regulated volume control (PRVC; 55.4%) and pressure control (PC) (27%) were the most used MV modes for COVID-19 patients. The most popular humidifier used in MV was heat and moisture exchanger (75.7%) [Table 3]. Higher positive end-expiratory pressure (PEEP) strategy and low tidal volume ventilation were the most used techniques in the management of severe COVID-19 patients. A total of 46 (62%) respondents used proning, with the most common duration being 12 to 16 h/day (38% of all participants). Lack of training (39%) was the main obstacle to the use of proning in COVID-19 management. The use of awake proning was reported by 19 (26%) respondents. There was limited use of both nitric oxide (20%) and extracorporeal membrane oxygenation (20%) in the ventilatory management of COVID-19 patients.
Table 3.
Management of COVID-19 patients using ventilatory support
| Variable | Values, n (%) |
|---|---|
| Initial flow setting of HFNC | |
| Below 30 L/m | 9 (12) |
| From 30–45 L/m | 31 (42) |
| >45 L/m | 6 (8) |
| Use of humidification with HFNC | 54 (73) |
| NIV modes | |
| BiPAP | 35 (47) |
| CPAP/PS | 18 (24) |
| PC | 10 (14) |
| VC | 5 (7) |
| NIV interfaces frequently used | |
| Full face mask | 34 (46) |
| Helmet | 5 (7) |
| Nasal mask | 7 (10) |
| Oronasal mask | 22 (30) |
| IMV modes | |
| APRV | 4 (5) |
| PC | 20 (27) |
| PRVC | 41 (55) |
| VC | 9 (12) |
| Humidifier type used with IMV | |
| Heated circuit | 17 (23) |
| Heat and moisture exchanger | 56 (76) |
| Ventilation strategy used in IMV | |
| Low VT ventilation (VT: 4–8 ml/kg of predicted body weight) | 71 (96) |
| High VT ventilation (VT>8 ml/kg of predicted body weight) | 3 (4) |
| PEEP strategy | |
| Lower PEEP | 9 (12) |
| Higher PEEP | 65 (88) |
| Use of prone with IMV | 46 (62) |
| Prone duration (h/day) | |
| <12 | 14 (19) |
| 12–16 | 28 (38) |
| >16 | 5 (7) |
| Reasons for not proning | |
| Limited resources | 14 (19) |
| Lack of training | 29 (39) |
| Complications | 15 (20) |
| Not indicated | 10 (14) |
| Tried awake prone positioning | 19 (26) |
| Frequent use of nitric oxide | 15 (20) |
| Use inhaled pulmonary vasodilator | 40 (54) |
| Use of recruitment maneuvers | |
| Recruitment maneuvers used | 50 (68) |
| Stepwise PEEP adjustment | 24 (32) |
| Inspiratory hold | 31 (42) |
| Use of VV-ECMO | 15 (20) |
| Use of systemic corticosteroids | 30 (41) |
HFNC – High-flow nasal cannula; NIV – Noninvasive ventilation; BiPAP – Bilevel positive airway pressure; CPAP – Continuous positive airway pressure; PS – Pressure support; PC – Pressure control; IMV – Invasive mechanical ventilation; APRV – Airway pressure release ventilation; PRVC – Pressure-regulated volume control; VT – tidal volume; PEEP – Positive end-expiratory pressure; VC – volume control; VV-ECMO – Veno-venous extracorporeal membrane oxygenation
Barriers and limitations of COVID-19 clinical management
The most reported barriers and limitations in COVID-19 clinical management faced by respiratory therapists in Saudi Arabia were staff shortage (51.4%), PPE shortage (51.4%) and increased workload (45.9%). In addition, poor training (43.2%) and lack of available protocols and policies (37.8%) were the main limitations affecting the ventilatory management of COVID-19 patients in Saudi Arabia. Figure 1 shows the other barriers that include patient- and system-related factors. Notably, lack of ventilators and hospital beds were not reported as major barriers in the management of COVID-19 patients. Relatively few responders considered governmental measures as a potential barrier (8.1%).
Figure 1.
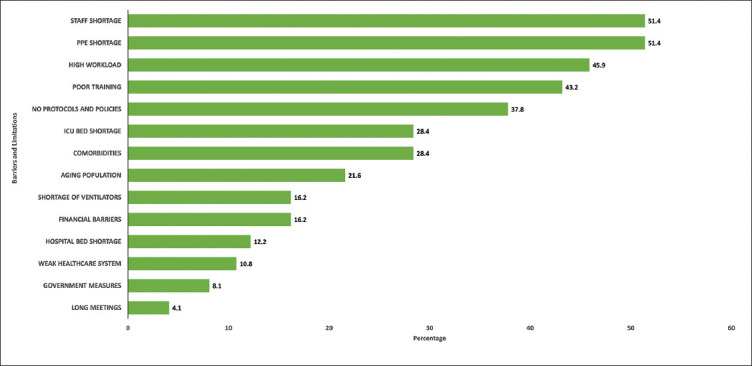
Barriers and limitations of ventilatory support management of COVID-19 patients
DISCUSSION
To the best of the author's knowledge, this is the first study to report practices and barriers of ventilatory support management of COVID-19 patients in Saudi Arabia. Our data showed that the practice of ventilatory support management of COVID-19 patients in Saudi Arabia was inconsistent with the global practice, whereby most frontline clinicians followed isolated and varied guidelines with limited use of standardized protocols.[10] The key finding of the current study was that staff and PPE shortage, followed by increased workload, poor training and lack of protocols and polices were barriers to effective clinical management of COVID-19 by respiratory therapists. Similarly, a global study found that the most common reported limitations were increased workload, lack of trained staff, shortage of PPE and staff,[10] which was also reported by other international studies.[12,13] Consistent with a previous study,[10] we purport that unavailability or inappropriate national ventilatory support management protocols and/or standards at the time of this survey may be critical reasons for our findings. Indeed, the establishment of standardized protocols and guidelines for patients' management has been previously associated with increased effectiveness and lower cost.[14]
Interestingly, respiratory therapists with the least number of years of professional experience (<5 years) have the highest percentage of training (45.1%). This finding suggests that the tendency to be trained was not directly related to the years of experience. Although a relatively high percentage [46 (62%)] of critical care respiratory therapists in Saudi Arabia adhere to the World Health Organization and national guidelines, there is a striking lack of nationally accepted clinical guidelines for the management of COVID-19 patients when this survey was performed. However, the Saudi Critical Care Society has recently released clinical practice guidelines on the management of COVID-19 patients who need ventilatory support.[15] There is a need for national inter-professional collaboration to overcome the lack of adherence to a single guideline/protocol nationally. Our findings are in alignment with other reports regarding the lack of universally accepted clinical guidelines for the management of adult COVID-19 patients.[10]
One notable difference can be found in the reported percentages for the initial diagnostic tool used for treatment initiation. Arterial blood gas and clinical presentation were the main diagnostic tools utilized for decision-making regarding the treatment course. However, as opposed to the global preference for arterial blood gas, in Saudi Arabia, there appears to be more inclination on deciding the management plan based on the patient's clinical presentation.[10] This survey also found that access to protocols for HFNC and NIV was notably limited compared to IMV. Thus, IMV was more widely accessible and utilized for both moderate and severe cases, while NIV, mostly BiPAP (47%), was used for mild cases of COVID-19. Despite the lack of HFNC protocol, 57% of respondents reported it as the preferred method to treat mild cases of COVID-19. These findings are compatible with the report by Winck and Ambrosino,[16] whereby HFNC was the first line of respiratory management, followed by NIV and IMV.
Surprisingly, 43% of providers used MV as an initial management strategy for moderate cases and 11% used IMV for mild cases. This may be due to the shortfall of PPE, isolation rooms in the face of rising infection rate and hospital admission similar to those that have been previously observed.[17,18] Suctioning plays a key role in maintaining airway patency during MV by removing secretions. Most of the respondents (97%) used a closed suction system in COVID-19 patients. A closed system drastically reduces aerosol/droplet generation, essential for patients who require high PEEP.[19] However, 3% reported utilization of an open suction system, which increases the risk of atelectasis and infection.[19,20] Interestingly, respiratory therapists in Saudi Arabia most commonly monitored ventilators every 4 h (57%) followed by “as needed,” while globally respondents most commonly reported monitoring ventilators as needed.[10] Close and consistent monitoring can support early detection of patient-ventilator asynchrony and other invasive and noninvasive complications.[21,22,23] These findings are compatible with the current evidence regarding ventilator check frequency.[24,25]
Nearly 42% of the respiratory care providers in Saudi Arabia reported using a full-face mask (46%), followed by the use of an oronasal mask (30%) and helmet (7%) with NIV. However, the current evidence recommends using helmets over full-face masks to prevent viral infection and to reduce intubation.[16,26] These findings further emphasize the importance of standardized protocols and we encourage inter-professional collaboration to develop a national management guideline that aligns with internationally accepted standards.[17]
BiPAP (47%) was used nearly two times more often than continuous positive airway pressure (CPAP) (24%) compared to globally, where CPAP was more widely utilized.[10] Further, although the majority (36.1%) of respiratory critical care providers globally used volume control (VC), only 12% of respiratory therapists in Saudi Arabia used it. It should be noted that VC could cause barotrauma if not monitored carefully.[19] On the other hand, over half of the respondents (55%) used PRVC, which delivers a set volume within a safe range and limits the settings adjustments.[10,27] Alvarez et al. compared VC ventilation to PRVC and reported lower peak airway pressure.[28] The airway pressure release ventilation was used least often (5%) despite being a viable option. In addition, respiratory therapists in Saudi Arabia use PC mode as their second preferred mode, which aligns with what has been reported globally.[10] PC mode pressure offers the option of pressure adjustment to align with varied mung mechanics.[19]
Clinicians in Saudi Arabia and internationally use low tidal volume, which aligns with the current guidelines.[10,25] On the other hand, respiratory therapists in Saudi Arabia report the use of “high PEEP low fraction of inspired oxygen (FiO2),” despite evidence that there is no difference between FiO2/low PEEP or low FIO2/high PEEP in ARDS patients.[29] Hence, there is a great need for further research to develop an evidence-based protocol for the management of COVID-19 through MV.[8]
Mortality prevention can be aided by proning intubated patients with severely hypoxemic respiratory failure.[30,31] Interestingly, only 26% of respondents in Saudi Arabia attempted awake pronation of COVID-19 patients, whereas 46% of respondents globally attempted it.[10] It should be noted that a great percentage (39%) of the respondents in the current study reported a lack of training in proning. Given that this approach is more widely used internationally which is indicative of the feasibility of this technique, but further studies are required to determine the effectiveness of the technique.[28] As a positive aspect regarding stepwise PEEP adjustment, the majority (42%) of the respondents in this study used inspiratory hold instead. These findings agree with previously published evidence concerning an increase in mortality with stepwise PEEP adjustment.[21,32]
The results of this study have important implications for both clinical and research purposes. They highlight the current strengths and limitations facing a key subset of frontline health-care professionals in Saudi Arabia managing COVID-19 patients needing ventilatory support. These findings will help improve clinical management in future, which could be of considerable benefit to both health-care providers and COVID-19 patients. Further research should focus on charting out clear, integrated and consistent guidance for the management of ventilatory support for COVID-19 patients, while simultaneously providing solutions to the major barriers and limitations outlined in this survey. This survey is limited by the sample size and reduced disciplinary diversity of the respondents. In addition, although the survey has a degree of randomness, it may not necessarily represent the experiences of the overall critical care respiratory therapists in Saudi Arabia. Thus, interpretation of this finding should be carried out with these in mind.
CONCLUSION
This study shows that the practice of ventilatory support management of COVID-19 patients in Saudi Arabia was inconsistent with the global current practice, and lacked uniformity, with limited use of standard protocols and treatment guidelines. Shortage of staff and PPE, increased workload and poor training were found to be the most prevalent limiting factors affecting COVID-19 ventilatory support management within Saudi Arabia.
Ethical considerations
The Institutional Review Board of the Armed Forces Hospital, Eastern Region, Saudi Arabia, provided ethical approval for this study on April 20, 2020. Response to the survey was considered as consent for participation. The study was conducted in accordance with the Declaration of Helsinki, 2013.
Peer review
This article was peer-reviewed by two independent and anonymous reviewers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pelkonen M, Notkola IL, Nissinen A, Tukiainen H, Koskela H. Thirty-year cumulative incidence of chronic bronchitis and COPD in relation to 30-year pulmonary function and 40-year mortality: A follow-up in middle-aged rural men. Chest. 2006;130:1129–37. doi: 10.1378/chest.130.4.1129. [DOI] [PubMed] [Google Scholar]
- 2.Anesi GL, Bloom A. Coronavirus Disease 2019 (COVID-19): Critical Care Issues UptoDate. 2020:24. [Google Scholar]
- 3.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–87. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hill NS, Brennan J, Garpestad E, Nava S. Noninvasive ventilation in acute respiratory failure. Crit Care Med. 2007;35:2402–7. doi: 10.1097/01.CCM.0000284587.36541.7F. [DOI] [PubMed] [Google Scholar]
- 5.Yam LY, Chen RC, Zhong NS. SARS: Ventilatory and intensive care. Respirology. 2003;8(Suppl):S31–5. doi: 10.1046/j.1440-1843.2003.00521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Esquinas AM, Egbert Pravinkumar S, Scala R, Gay P, Soroksky A, Girault C, et al. Noninvasive mechanical ventilation in high-risk pulmonary infections: A clinical review. Eur Respir Rev. 2014;23:427–38. doi: 10.1183/09059180.00009413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xia JG, Zhao JP, Cheng ZS, Hu Y, Duan J, Zhan QY. Non-invasive respiratory support for patients with novel coronavirus pneumonia: Clinical efficacy and reduction in risk of infection transmission. Chin Med J (Engl) 2020;133:1109–11. doi: 10.1097/CM9.0000000000000761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430–4. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alqahtani JS, Mendes RG, Aldhahir A, Rowley D, AlAhmari MD, Ntoumenopoulos G, et al. Global current practices of ventilatory support management in COVID-19 patients: An international survey. J Multidiscip Healthc. 2020;13:1635–48. doi: 10.2147/JMDH.S279031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: An expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38:1573–82. doi: 10.1007/s00134-012-2682-1. [DOI] [PubMed] [Google Scholar]
- 12.Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers' adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4:CD013582. doi: 10.1002/14651858.CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir Med. 2020;8:506–17. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marx WH, DeMaintenon NL, Mooney KF, Mascia ML, Medicis J, Franklin PD, et al. Cost reduction and outcome improvement in the intensive care unit. J Trauma Acute Care Surg. 1999;46:625–30. doi: 10.1097/00005373-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Alhazzani W, Al-Suwaidan F, Al Aseri Z, Al Mutair A, Alghamdi G, Rabaan A, et al. The Saudi critical care society clinical practice guidelines on the management of COVID-19 patients in the intensive care unit. Saudi Crit Care J. 2020;4:27–44. [Google Scholar]
- 16.Winck JC, Ambrosino N. COVID-19 pandemic and non invasive respiratory management: Every Goliath needs a David.An evidence-based evaluation of problems. Pulmonology. 2020;26:213–20. doi: 10.1016/j.pulmoe.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health O. Geneva: World Health Organization; 2020. Clinical Management of Severe Acute Respiratory Infection when Novel Coronavirus (2019-nCoV) Infection Is Suspected: Interim Guidance, 28 January 2020. Contract No.: WHO/nCoV/Clinical/2020.3. [Google Scholar]
- 18.Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020;46:837–40. doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haas CF. Mechanical ventilation with lung protective strategies: What works? Crit Care Clin. 2011;27:469–86. doi: 10.1016/j.ccc.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 20.World Health O. Geneva: World Health Organization; 2020. Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID-19 Disease Is Suspected: Interim Guidance, 13 March 2020. Contract No.: WHO/2019-nCoV/clinical/2020.4. [Google Scholar]
- 21.Sreedharan J, Alqahtani J. Driving pressure: Clinical applications and implications in the intensive care units. Indian J Respir Care. 2018;7:62–6. [Google Scholar]
- 22.Alqahtani JS, AlAhmari MD, Alshamrani KH, Alshehri AM, Althumayri MA, Ghazwani AA, et al. Patient-ventilator asynchrony in critical care settings: National outcomes of ventilator waveform analysis. Heart Lung. 2020;49:630–6. doi: 10.1016/j.hrtlng.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Karim HM, Burns KE, Ciobanu LD, El-Khatib M, Nicolini A, Vargas N, et al. Noninvasive ventilation: Education and training.A narrative analysis and an international consensus document. Adv Respir Med. 2019;87:36–45. doi: 10.5603/ARM.a2019.0006. [DOI] [PubMed] [Google Scholar]
- 24.AARC clinical practice guideline. Patient-ventilator system checks.American Association for Respiratory Care. Respir Care. 1992;37:882–6. [PubMed] [Google Scholar]
- 25.Guidelines for standards of care for patients with acute respiratory failure on mechanical ventilatory support. Task Force on Guidelines; Society of Critical Care Medicine. Crit Care Med. 1991;19:275–8. doi: 10.1097/00003246-199102000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Hui DS, Chow BK, Lo T, Ng SS, Ko FW, Gin T, et al. Exhaled air dispersion during noninvasive ventilation via helmets and a total facemask. Chest. 2015;147:1336–43. doi: 10.1378/chest.14-1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal A, Basmaji J, Muttalib F, Granton D, Chaudhuri D, Chetan D, et al. High-flow nasal cannula for acute hypoxemic respiratory failure in patients with COVID-19: Systematic reviews of effectiveness and its risks of aerosolization, dispersion, and infection transmission. Can J Anaesth. 2020;67:1217–48. doi: 10.1007/s12630-020-01740-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alvarez A, Subirana M, Benito S. Decelerating flow ventilation effects in acute respiratory failure. J Crit Care. 1998;13:21–5. doi: 10.1016/s0883-9441(98)90025-9. [DOI] [PubMed] [Google Scholar]
- 29.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 30.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–43. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, Mason DM, et al. Increased incidence of barotrauma in patients with COVID-19 on invasive mechanical ventilation. Radiology. 2020;297:E252–62. doi: 10.1148/radiol.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–87. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


