Abstract
Introduction
Fatigue is a prevalent and potentially debilitating symptom that impacts the health-related quality-of-life of individuals diagnosed with acute and chronic medical conditions. Yet, its etiologic mechanism is not fully understood. Additionally, the assessment and determination of the clinical meaning of fatigue and its multidimensionality may vary by medical condition.
Methods
A scoping literature review was conducted to investigate how fatigue is defined and measured, including its dimensions, in non-oncologic medical conditions. The PubMed database was searched using keywords.
Results
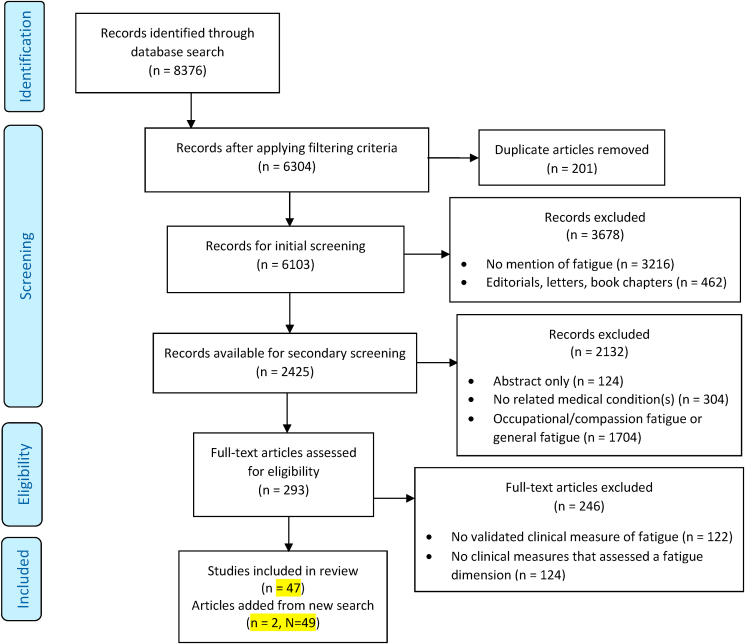
Overall, 8376 articles were screened at the title/abstract levels, where 293 articles were chosen for full-text review that mentioned fatigue or included fatigue measures. The review of the full text excluded 246 articles that did not assess at least one fatigue dimension using validated questionnaires and clinical tests. The final set included 47 articles. Physical fatigue was the most assessed fatigue dimension and the Multidimensional Fatigue Inventory was the most widely used questionnaire to assess fatigue in this review.
Limitations
This review was limited by including only English-language publications and using PubMed as the sole database for the search.
Conclusions
This review affirms that fatigue is a multidimensional construct, agnostic of medical condition, and that individual fatigue dimensions can be measured by validated clinical measures. Future research should focus on expanding the repertoire of clinical measures to assess specific fatigue dimensions.
Keywords: Fatigue, Fatigue dimension, Fatigue assessment, Clinical measure
Highlights
-
•
The 27 different validated clinical measures used to assess fatigue and its dimensions; 20 instruments assessed the physical, 8 for mental, 7 cognitive, 5 for motivational, 2 for emotional, 1 peripheral, 1 for central, 1 psychosocial.
-
•
Physical was the most measured dimension, as assessed in 42 of 47 included articles.
-
•
This review affirms that fatigue is a multidimensional construct, agnostic of medical condition, and that individual fatigue dimensions can be measured by validate clinical measures.
1. Introduction
Fatigue is a common, yet complex symptom experience that is reported by both healthy individuals and individuals with acute and chronic medical conditions and/or diseases (e.g., post-viral infection, cancer, depression, multiple sclerosis, and fibromyalgia) (Saligan et al., 2015). Usually, fatigue is described within the context of specific medical conditions. It can co-occur with other clinical symptoms such as depression, pain, sleep impairment, and cognitive dysfunction (Kinsinger et al., 2010).
The negative effects of fatigue range from losses of productivity at work due to medical disability, occupational hazards, deaths from medication errors, and suicidal ideation (Fan and Smith, 2017; Kapur and Webb, 2016). These negative effects cut across disciplines, sectors, and populations. For example, fatigue among medical residents, physicians, and nurses contributes to the deaths of approximately 100,000 Americans annually secondary to potentially avoidable injurious events (Salen and Norman, 2017). In a comparative study sample of 3442 working United States (US) adults, physicians were significantly more likely to have symptoms of emotional, physical, and mental exhaustion (37.9% vs 27.8%), with certain specialists at relative greater risk for burnout (Shanafelt et al., 2012). Fatigue-related drowsiness in the US contributes to more than 1500 fatalities, 100,000 motor vehicle accidents, and 76,000 injuries annually (Ziwu et al., 2021; Caldwell et al., 2008). Furthermore, fatigue has a strong adverse impact on the performance, health, and safety of individuals in the workplace (Volker et al., 2016). In the US army, 12.2% of mishaps are related to fatigue (Caldwell et al., 2008).
While there is a lack of unanimity in the definition and assessment of fatigue (Ericsson et al., 2013), there is an apparent acceptance of the idea that fatigue is a multidimensional construct as demonstrated by the use of multiple definitions of fatigue across different studies (Pattyn et al., 2018). For the purposes of this review, the term multidimensional means having more than one dimension, of which either may be present at the same time. For example, researchers Norton et al. (2010) described fatigue in patients with inflammatory bowel syndrome as a “multifactorial and multifaceted symptom that is strongly associated with depression and poor quality of life.” Hernandez-Ronquillo et al. (2011), whose research team studies epilepsy, described fatigue as, “extreme and persistent tiredness, weakness or exhaustion that could be mental, physical or both,” which concurs to the idea that fatigue can have multiple dimensions. Therefore, published fatigue dimensions, including physical fatigue, mental fatigue, cognitive fatigue, emotional fatigue, and motivational fatigue, will be assessed in this scoping literature review.
There has been a gradual improvement in the identification and measurement of fatigue as a clinical symptom, but much is still being discovered about its ability to manifest as more than one dimension. Thus, a scoping literature review was performed to answer the following research questions: How is fatigue and its dimensions being described and measured in various non-oncologic medical conditions? Whether these descriptions and methods of measurements are similar or not, identifying the research gap that exist in the consistency of how fatigue is described and how it is measured? The objective of conducting this review then is focused on identifying the different published fatigue definitions across medical conditions not related to cancer (non-oncologic medical conditions) and identifying validated measures used that captured the multidimensional nature of fatigue.
2. Methods
2.1. Search
Using the PRISMA guidelines, the search strategies were initially drafted by an informationist from the National Institutes of Health library and completed in May 2018 using the PubMed (National Library of Medicine) database. The search strategy included the following key words:
fatigue[majr] OR fatigue[ti] AND phenotype[tiab] OR phenotypes[tiab]) OR (questionnaire[tiab] OR questionnaires[tiab] OR instrument[tiab] OR instruments[tiab] OR measure[tiab] OR measures [tiab] OR scale[tiab] OR scales[tiab] OR "patient reported outcome"[tiab] OR "patient reported outcomes"[tiab]) OR (chronic[tiab] OR subjective[tiab] OR physical[tiab] OR cognitive[tiab] OR affective[tiab] OR emotional[tiab] OR motivational[tiab] OR actional[tiab] OR actionable[tiab]) AND (manage[tiab] OR managed[tiab] OR managing[tiab] OR management[tiab] OR intervention[tiab] OR interventions[tiab])
The PubMed filters for Publication Date (10 years), Language (English), Species (Human), and Ages (Adult: 19+ years) were used to limit articles to those published from 2008 to 2018, written in English, and human adult studies. The final search results were exported into EndNote X9, which was the software tool utilized to manage, collect, and identify duplicate references from the database searches, as well as to cite included articles in this review. Using the same search criteria, a new search was conducted to extract articles published after May 2018 to 2021.
2.2. Selection of sources of evidence
Two reviewers (R.B. and J.L.) screened independently and in parallel the titles and abstracts of all retrieved articles using established eligibility criteria. The inclusion criteria for the title and abstract screening were human adult (19+) populations, article is on fatigue, any non-oncologic medical condition or disease, and publication type (original research or reviews (scoping, systematic, meta-analysis) only). The exclusion criteria for the title and abstract screening were pediatric or adolescent populations, compassion fatigue, occupational fatigue, oncologic medical conditions and diseases (a separate review for oncologic conditions is underway), animal studies, publication types (editorials, letters, commentary, books/book chapters, dissertations, white papers, conference proceedings/abstracts), and articles with no abstract. Any disagreements between the reviewers was resolved by a separate third reviewer (L.S.).
Four reviewers (R.B., J.L., S.A., J.R.) worked in pairs to retrieve and examine the full text of articles for potentially relevant publications. The inclusion criterion specific for the full-text review was ensuring validated clinical outcome measures (questionnaires, instruments, etc.) was used to assess the fatigue dimensions. Any ambiguity or disagreements on study selection were discussed between reviewers in a peer discussion group.
2.3. Data extraction and synthesis of results
A data charting form in Microsoft Excel was jointly developed by two reviewers (R.B. and J.L) to determine which variables to extract from the included articles. Four reviewers (R.B., J.L., K.B., L.G.) working in pairs extracted the data, charted the data, discussed the results in peer discussion groups, and continuously updated the data-charting form. Disagreements between reviewers and any unclear data were resolved by a separate fifth reviewer (L.S.).
The following data items were extracted from each included study: the non-oncologic medical condition or disease being studied, population characteristics (e.g., sample size of both control and experimental groups), demographic data, the professional fields of study for the authors of the reviewed articles (e.g., country of origin, departmental affiliation), study design (e.g., cross-sectional vs. longitudinal), published definitions of fatigue, fatigue dimensions being assessed (e.g. total number, descriptions of each fatigue dimension), and validated clinical measures to assess the fatigue dimensions. The published definitions of fatigue were grouped together and organized by non-oncologic medical condition (Table 1). Included articles were then categorized by the non-oncologic medical condition they shared, the clinical measures used, and the fatigue dimensions assessed (Table 2a).
Table 1.
Definitions of fatigue from non-oncologic medical conditions.
| Medical Condition | Definition of Fatigue | References |
|---|---|---|
| Autoimmune Rheumatic Disease | “.. persistent, and severity is similar to the chronic fatigue syndrome … fatigue generally is subscribed to disease-related factors, especially inflammation, anemia and pain.” | van Hoogmoed et al. (2010) |
| Chronic Obstructive Pulmonary Disorder (COPD) | “… described mostly in relationship with muscular force exhaustion as if following a strenuous exercise period and with no malaise.” | Antoniu & Ungureanu (2015) |
| Cushing's Syndrome | “Mental fatigue is characterized by a mental exhaustion which appears especially during sensory stimulation or following mentally strenuous tasks. Other typical features are the long recovery time that is needed for restoration of mental energy, irritability, impaired memory, and concentration as well as stress, sound, and light hypersensitivity.” | Papakokkinou et al. (2015) |
| Epilepsy | “… extreme and persistent tiredness, weakness or exhaustion that could be mental, physical or both.” | Hernandez-Ronquillo et al. (2011) |
| Fibromyalgia | “… disruptive or extremely disruptive” to health-related quality of life. | Li et al. (2017) |
| “… profound and overwhelming, more severe, constant, and unpredictable than normal tiredness, not relieved by resting or sleep, not proportional to effort exerted, and disruptive in terms of motivation, activities, and cognition.” | Kratz et al. (2016) | |
| Inflammatory Bowel Disease | “… unpleasant, multifactorial and multifaceted symptom that is strongly associated with depression and poor quality of life (QoL). … a sense of continuing tiredness, with periods of sudden and overwhelming lack of energy or feeling of exhaustion that is not relieved, or fully relieved following rest or sleep.” | Norton et al. (2015) |
| Multiple Sclerosis | “… most common, debilitating and life altering symptoms.” | Learmonth et al. (2013) |
| Myasthenia Gravis | “… a complex phenomenon and includes both physiological and psychological factors, a distinction has recently been made between fatigue as a subjective feeling of tiredness, lack of energy, and difficulty concentrating, and muscle fatigability defined as the difficulty initiating or sustaining muscle activities.” | Elsais et al. (2013) |
| Parkinson's Disease | “… an important and frequent non-motor symptom. It is difficult to describe, there are no biological markers, being always a subjective definition. It is described with a wide range of terms, which is dependent on the education of the people and cultural background.” | Falup-Pecurariu (2013) |
| Rheumatoid Arthritis | “… subscribed to disease-related factors, especially inflammation, anemia and pain. … fatigue may incorporate cognitive and emotional elements. | van Hoogmoed et al. (2010) |
| Sjogren's Syndrome | “… somatic and mental exhaustion that interferes with a person's ability to carry out physical and cognitive activities and can be persistent and overwhelming … differs from normal fatigue, when healthy, which is ‘earned’ by being physically and/or cognitively active.” | Goodchild et al. (2008) |
| “… complex and subjective phenomenon. Its origins are multifactorial. It is an intimate, universal and extremely frequent experience that cannot be objectively measured.” | Belmont et al. (2006) | |
| Traumatic Brain Injury | “… one of the most challenging and distressing long-term symptoms, interfering considerably with their ability to work and lead a normal life, including social activities with family and friends.” | Palm et al. (2017) |
| Chronic Fatigue Syndrome (CFS) | “… is a multi-system complex disorder, characterized by extreme mental and physical fatigue with array of physical symptoms not relieved by rest.. | Slomoko et al. (2020) |
Note. A – Z column sorting order for “Medical Condition.”
Table 2a.
Clinical measures for fatigue dimensions in non-oncologic medical conditions.
| Clinical Measure | Fatigue Dimension(s) | Medical Condition(s) | Statistical Findings |
|---|---|---|---|
| Multidimensional Fatigue Inventory (MFI or MFI-20) |
|
||
|
|||
| Physical |
|
||
| Mental |
|
||
| Cognitive |
|
|
|
| Motivational |
|
|
|
| Emotional |
|
|
|
|
|
||
|
|
||
|
|
||
| Multidimensional Assessment of Fatigue (MAF) | Emotional Cognitive |
|
|
| Mental |
|
|
|
| Motivational |
|
|
|
| Physical |
|
|
|
| The Revised Piper Fatigue Scale (PFS) | Emotional |
|
|
| Cognitive |
|
||
| Physical |
|
||
| Checklist of Individual Strength (CIS) | Mental |
|
|
| Motivational |
|
||
| Physical |
|
||
| Isometric Muscle Strength Test - physiological test of fatigue | Central |
|
|
| Peripheral | |||
| Physical | |||
| Manchester COPD Fatigue Scale | Cognitive |
|
|
| Physical | |||
| Psycho-social | |||
| Modified Fatigue Impact Scale (MFIS) | Cognitive |
|
|
| Mental |
|
|
|
| Physical |
|
|
|
| Multidimensional Daily Diary of Fatigue-Fibromyalgia-17 (MDF-Fibro-17) instrument | Cognitive |
|
|
| Motivational | |||
| Physical | |||
| PROMIS Fatigue Fibromyalgia (FM) Profile | Cognitive |
|
|
| Motivational | |||
| Physical | |||
| Brugmann Fatigue Scale (BFS) | Mental |
|
|
| Physical | |||
| Chalder Fatigue Scale | Mental |
|
|
| Physical |
|
||
| Fatigue Assessment Scale (FAS) | Physical |
|
|
| Fatigue Impact Scale | Physical |
|
|
|
|
||
|
|
||
| Fatigue Symptom Inventory (FSI) | Physical |
|
|
| Health Assessment Questionnaire (HAQ) | Physical |
|
|
| MG Fatigue Scale (MGFS) | Physical |
|
|
| Modified Fatigue Impact Scale for Spinal Cord Injury (MFIS-SCI) | Physical |
|
|
| Visual Analogue Scale (VAS) | Physical |
|
|
| |||
| |||
| |||
| Mental Fatigue Scale (MFS) | Mental |
|
|
| |||
| Wood Mental Fatigue Inventory (WMFI) | Mental |
|
|
Note. Column sorting order: For “Clinical Measure,” the most frequently used clinical measure was listed first with the others based on descending frequency. Columns for “Fatigue Dimension(s)” and “Medical Condition(s)” have an A – Z sorting order. “Statistical Findings” column has a randomized sorting.
N/A = no statistical findings for domain differentiation reported in included articles.
3. Results
The PubMed search yielded 8376 articles (Fig. 1), where 6304 articles remained after initial application of filtering criteria. Then, 201 duplicate articles were removed, leaving 6103 articles for initial screening. So, 2425 articles remained after 3216 articles that did not mention fatigue and 462 studies that were editorials, letters, commentaries, dissertations, or book chapters were removed. A secondary level screening of titles and abstracts was conducted to select studies that regarded fatigue as a symptom of a non-oncologic medical condition. Another 1704 articles were excluded because they studied general fatigue, overall quality of life, or compassion/occupational fatigue, 304 studies were excluded because they investigated fatigue that was not related to or in a context of a disease or any medical condition, and 124 articles were removed because they only published an abstract. Finally, 293 were subjected for full text review to further apply the inclusion and exclusion criteria.
Fig. 1.
PRISMA diagram for literature search and review.
A discussion-based peer review among all the authors was conducted to determine which full-text studies were going to be included in the final paper. After reviewing the full texts of all 293 studies, 122 articles were excluded because they had no validated clinical measure for fatigue. Another 124 articles were excluded because none of the clinical outcome measures directly assessed a dimension of fatigue. There were two additional articles added after May 2018–2021 that met the eligibility criteria. A final 49 articles were selected by the group for this scoping review. All references included in this review have been organized by fatigue dimensions and the medical condition/disease investigated (Table 2a).
Cumulatively, a total of 10787 subjects were enrolled in the studies described in the 49 articles. About 68% of those subjects were female. Twenty-nine medical non-oncologic conditions assessed, traumatic brain injury (TBI; 11% of studies), fibromyalgia (11% of studies), and multiple sclerosis (11% of studies) were the most studied, followed by chronic fatigue syndrome (CFS; 9% of studies) and rheumatoid arthritis (9% of studies). Twenty-nine articles used a cross-sectional design, 9 used a longitudinal design, and 16 were clinical trials. Three articles utilized interviews to assess fatigue and unidimensional clinical measures were used in 30 articles.
There were 29 articles where the institutional affiliations of the authors were from North America (US, Canada); 22 authors from Europe (Denmark, Germany, Poland, Romania, Sweden, and Switzerland, and 4 authors from Asia (Mainland China, Hong Kong, and the Middle East) (8%). The professional affiliations of the authors were in psychology (n = 16), rehab medicine (n = 12), rheumatology (n = 11), neurology (n = 8), neuroscience (n = 7), nursing (n = 3), psychiatry (n = 3), gastroenterology (n = 3), pharmacology (n = 2), somatic medicine (n = 3), pneumonology (n = 1), and allergy (n = 1).
3.1. Definition of fatigue
Each fatigue definition listed in Table 1 came from the 47 included articles. In 26 of the 49 articles (55%), fatigue was defined as multidimensional. The most common keywords and phrases used to define fatigue included: “disruptive,” “subjective,” “distressing,” “debilitating,” “exhaustion,” “persistent,” “overwhelming,” “lack of energy,” and “not relieved by rest or sleep” (Table 1).
3.2. Measuring the fatigue dimensions
The included articles used synonymous terms for dimensions, including: dimension (53%), domain (42%), and component (34%). This review used, dimension, to capture the multidimensional nature of the fatigue construct. Eight fatigue dimensions were identified in the included articles: physical, cognitive, mental, central, peripheral, emotional, motivational, and psychosocial dimensions of fatigue. Many of the articles assessed multiple dimensions of fatigue at once (83%), while 17% assessed a single dimension of fatigue.
Table 2a lists the validated clinical measures used in the reviewed articles to assess fatigue and its dimensions. Twenty instruments assessed the physical fatigue dimension, 8 for mental fatigue, 7 for cognitive fatigue, 5 for motivational fatigue, 2 for emotional fatigue, 1 for peripheral fatigue, 1 for central fatigue, and 1 for psychosocial fatigue. During the data extraction process, 4 clinical measures did not specifically assess a fatigue dimension but measured general fatigue (see Table 2b.
Table 2b.
Clinical measures for general fatigue in non-oncologic medical conditions.
|
Clinical Measure |
Fatigue Dimension(s) | Medical Condition(s) | Statistical Findings |
|---|---|---|---|
| Fibromyalgia Impact Questionnaire (FIQ) | General Fatigue | Fibromyalgia (Ablin et al., 2010; Ericsson et al., 2013) | N/A |
| Numerical Rating Scales (NRS) | General Fatigue | Primary Biliary Cirrhosis (Zangi et al., 2012) | N/A |
| Fatigue Catastrophizing Scale | General Fatigue | Crohn's Disease (van Erp et al., 2017) | N/A |
| Fatigue Severity Scale (FSS) | General Fatigue | Myotonic Dystrophy (Baldanzi et al., 2017) | Total FSS score (mean ± sd) was 43.6 ± 12.4 and was significantly associated to: total muscle impairment as assessed by the Medical Research Council (r = −0.496; p = 0.01); handgrip maximal voluntary contractions (MVC) at baseline (r = −0.583; p < 0.01); MVC_60% (r = −0.534; p < 0.05). |
Note. Column sorting order: For “Clinical Measure,” the most frequently used clinical measure was listed first with the others based on descending frequency. Columns for “Fatigue Dimension(s),” “Medical Condition(s),” and “Statistical Findings” have an A – Z sorting order.N/A = no statistical findings for domain differentiation reported in included articles.
3.3. Clinical measures for general fatigue in non-oncologic medical conditions
3.3.1. Fatigue dimension: physical fatigue
Physical fatigue was the most measured dimension, as assessed in 42 of 49 included articles. Using an example taken from an included article, physical fatigue was described as a “debilitating physical exhaustion or a distressing lack of energy not relieved by sleep or rest” (Norton et al., 2015). Physical fatigue was also “characterized by muscle fatigability, which was defined as the difficulty to initiate or sustain muscle activities” (Elsais et al., 2013).
The three most widely used questionnaires to measure physical fatigue were the Multidimensional Fatigue Inventory (MFI, 14/42 articles), the Modified Fatigue Impact Scale (MFIS, 7/42 articles), and the Multidimensional Assessment of Fatigue (MAF, 4/42 articles). See Table 2a for a list of all clinical measures identified.
3.3.2. Fatigue dimension: mental fatigue
Mental fatigue was the second-most measured fatigue dimension, as assessed in 32 included articles. An example of a description of mental fatigue was “mental exhaustion that appears especially during sensory stimulation or following mentally strenuous tasks” (Papakokkinou et al., 2015). Another description of mental fatigue was “the subjective perception of feeling fatigued after performing intense or demanding cognitive activities that involve concentration” (Falup-Pecurariu, 2013). Sample phrases that commonly described mental fatigue included: “reduced sustained mental effort,” “quickly becoming fatigued after reading or watching television or conversing with others,” “prolonged rest to recover after a mentally-strenuous activity,” and “forgetting things easily” (Berginstrom et al., 2017). In the 32 included articles, mental fatigue was mainly assessed in study subjects with TBI, rheumatoid arthritis, fibromyalgia, irritable bowel disease (IBD), multiple sclerosis, and myasthenia gravis.
From the 32 included articles in which mental fatigue was measured, two measures were most commonly used: the MFI (14/32 articles) and the MFIS (7/32 articles). In addition, one unidimensional mental fatigue assessment was used, the Wood Mental Fatigue Inventory (WMFI, 1/32 articles).
3.3.3. Fatigue dimension: cognitive fatigue
Cognitive fatigue was assessed in 24 included articles and an article defined it as “a symptom interfering with a person's ability to carry out cognitive activities and can be persistent and overwhelming, which differs from normal fatigue” (Goodchild et al., 2008). Another article described cognitive fatigue as “decreased performance over a period of sustained mental exertion” (DeLuca et al., 2008). “Having impaired memory and difficulty with concentration” were additional descriptors used for cognitive fatigue (Elsais et al., 2013; Papakokkinou et al., 2015). The cognitive dimension of fatigue was mainly assessed in subjects with TBI, chronic obstructive pulmonary disorder (COPD), IBD, multiple sclerosis, and fibromyalgia. Across all 29 non-oncologic medical conditions identified in the included articles, the MFI was the most widely used measure to assess cognitive fatigue (14/24 articles) followed by the MFIS (7/24 articles), and finally the MAF (4/27 articles).
3.3.4. Fatigue dimension: motivational fatigue
Motivational fatigue was assessed in 21 included articles. Examples of its definition included, “a symptom that is disruptive in terms of motivation and in initiating activities” (Kratz et al., 2016), and “having capabilities to considerably interfere with patients’ ability to work and lead a normal life, including social activities with family and friends” (Palm et al., 2017). This dimension of fatigue was assessed in subjects with fibromyalgia, rheumatoid arthritis, CFS, TBI, and spinal cord injury.
Five clinical measures were used to assess motivational fatigue (see Table 2a). The measures commonly used to assess motivational fatigue were the MFI (14/21 articles), the MFIS (7/21 articles), and the Checklist of Individual Strength (CIS, 3/21 articles). Additionally, two of the five clinical measures were specifically used with fibromyalgia patients: the Multidimensional Daily Diary of Fatigue-Fibromyalgia-17 (Li et al., 2017) and the Patient-Reported Outcomes Measurement Information System (PROMIS) Fatigue Fibromyalgia Profile (Kratz et al., 2016).
3.3.5. Fatigue dimension: emotional fatigue
Emotional fatigue was measured in 16 included articles. It was defined by a couple of articles as “an unpleasant symptom that is strongly associated with depression and is extremely disruptive to health-related quality of life” (Norton et al., 2015; Li et al., 2017). Another article incorporated both cognitive and emotional elements to define emotional fatigue (van Hoogmoed et al., 2010). Emotional fatigue was assessed in subjects with CFS, TBI, COPD, systemic lupus erythematosus (SLE), and fibromyalgia. Two instruments were commonly used in the 16 included articles to assess emotional fatigue: the MAF (4/16 articles) and the revised Piper Fatigue Scale (PFS; 2/16 articles).
3.3.6. Objective measure of central and peripheral fatigue
Only one included article assessed central and peripheral fatigue, but it did not define these fatigue dimensions (Kent-Braun and Miller, 2000). So, the following definitions were taken from other literature sources as points of reference. Central fatigue was attributed to factors in the central nervous system (CNS), which consists of the brain and spinal cord. Enhanced perception of effort and limited endurance of sustained physical and mental activities are its main characteristics (Chaudhuri and Behan, 2004). Whereas, peripheral fatigue was defined as dysfunction in the peripheral nervous system and neuromuscular system manifested as muscle fatigability induced by repetitive contractions (Falup-Pecurariu, 2013).
Kent-Braun and Miller (2000) explored central and peripheral fatigue in subjects with amyotrophic lateral sclerosis (ALS). An isometric muscle strength test was used to assess muscle fatigue by measuring the decrease in maximal voluntary contractions (MVC) from an initial pre-test MVC. To assess peripheral fatigue, the fall of tetanic force was quantified during the exercise period. To assess central fatigue, the subjects were asked to “add force” after the final MVC during the exercise period to promote central muscle activation. When subjects failed to rapidly generate force during a submaximal contraction, central activation failure was the cause for central fatigue (Kent-Braun and Miller, 2000).
Other objective measure of physical function and performance, such as the 6-Minute Walk Test (6MWT) was also used in several studies (Ericsson et al., 2013; Jordan et al., 2017, & Tseng et al., 2009). This objective measure was used to measure fatigue in conjunction with subjective fatigue questionnaires such as the MFI and FIQ (Ericson et al., 2013) that assessed the level of fatigue after physical activity. Ericsson et al. (2013) study, investigators found a negative correlation between the distance walked during the 6MWT and the participants’ fatigue levels as assessed by the MFI.
3.3.7. Fatigue dimension: psychosocial fatigue
Psychosocial fatigue was assessed in only one included article. It was defined as a “complex syndrome with both physical and psychological features” (Antoniu and Ungureanu, 2015). This fatigue dimension was assessed using the Manchester COPD Fatigue Scale. Scores from this measure correlated well with scores from other instruments such as the Borg scale and the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) questionnaire (Antoniu and Ungureanu, 2015).
4. Discussion
Fatigue is a multi-faceted, multi-factorial, and multidimensional construct, as defined in the included articles of this scoping review. A key theme identified in this review was there were many ways in which fatigue was defined, assessed, and measured. Eight fatigue dimensions were identified and measured. The most commonly assessed dimensions of fatigue were the physical, cognitive, and mental dimensions of fatigue. This finding suggests that these three dimensions represent a core set of dimensions to use in order to characterize the construct of fatigue.
4.1. On defining fatigue construct and its dimensions
Based on the findings of this review, there is no one common definition of fatigue that was identified from the included articles. Of the multiple non-oncologic conditions included in the reviewed articles, each had their own medical condition-specific definition of fatigue. However, there were common terms and phrases used to describe this fatiguing experience. Examples of these terms and phrases used in the reviewed articles included, “increased rest propensity” (Brugmann Fatigue Scale; Mairesse et al., 2017), “tiredness and lack of energy for more than 3 h,” “lack of energy or reduction related to motivation,” and “lack of energy related to enjoyment” (Chalder Fatigue Scale (CFS); Chalder et al., 1993, 2017; Vercoulen et al., 1994). Other terms to describe fatigue included, “no desire to do anything”, “reduction in concentration” (Vercoulen et al., 1994), “wandering thoughts”, “avoidant behavior from physical activity, disturbed sleep; depressed mood” (Vercoulen et al., 1994), “feeling bothered by fatigue,” “not enough energy for the day,” “feeling exhausted,” “problems starting things,” “problems thinking clearly,” “mentally exhausted,” “lack of concentration” (Fatigue Impact Scale (FIS); Michielsen et al., 2003), “lack of attention on any activity,” and “spending most of the day lying down to rest” (Fatigue Impact Scale; Fisk et al., 1994).
The use of these common terms to describe the fatigue experience suggest that the reporting of fatigue symptoms is sensitive to context, and that meaning is driven by individual subjective experiences. Part of that context was the medical condition their clinician diagnosed them on. This type of reporting within specific medical conditions may have implications that can explain the wide variability of the interpretation of fatigue scores and dimensions observed in the clinical setting.
The reviewed articles confirm that to define fatigue must be described multidimensionally. Moreover, some fatigue dimensions may be more explored and/or reported in one medical non-oncologic condition than in others. Patient reports of their fatigue experiences may highlight a specific fatigue dimension within the context of their medical condition or as side effects of their treatments. For instance in our review, emotional and motivational fatigue were investigated more in individuals with schizophrenia, fibromyalgia, Sjogren's syndrome, COPD, and HIV/AIDS.
Additionally, specific medical conditions tend to explore or report one or more dominant dimensions of fatigue. From our review, patients with schizophrenia tended to have more reported mental and motivational fatigue dimensions as compared to the general population (Hedlund et al., 2015). There also appeared to be a greater focus on physical and mental fatigue in patients with multiple sclerosis, TBI, CFS, and rheumatoid arthritis. The fatigue experience reported by patients greatly influences the type of fatigue dimension assessed by clinicians (Alsén et al., 2010).
4.2. Fatigue dimensions
Overall, the physical dimension of fatigue was the most measured, as identified in our review. The primary reason why physical fatigue is the most commonly measured dimension may stem from the way fatigue is generally understood, in that the lack of physical energy is an anchor construct and becomes the evident starting point to describing the fatigue experience. In fibromyalgia patients for example, the experience of fatigue is defined as not relieved by physical rest or sleep (Li et al., 2017). In TBI patients, fatigue is related to the inability to work linked to the increased requirement of physical energy (Belmont et al., 2006, Palm et al., 2017). For IBD patients, fatigue is described around the lack of muscular strength exertion (Falup-Pecurariu et al., 2013). Additionally, the somatization of fatigue symptoms is prevalent in Sjogren's syndrome, physical weakness in epilepsy (Hernandez-Ronquillo, Moien-Afshari, Knox, Britz and Tellez- Zenteno, 2011), and an incapacity to sustain activities requiring muscle strength in myasthenia gravis (Elsais et al., 2013).
Although some included articles did mention the study specific fatigue dimensions, there were fatigue measures used by the included studies that did not measure a specific dimension. For example, the Fatigue Severity Scale (FSS) was the most commonly used clinical measures across various medical conditions. However, the FSS measures general fatigue and not the fatigue dimensions, whereas, the Multidimensional Fatigue Inventory (commonly used in our included articles) is a clinical measure that assesses general fatigue, as well as, physical, motivational, cognitive, and mental fatigue. Several other clinical measures were used in the included articles including the Multidimensional Assessment of Fatigue (MAF), Checklist of Individual Strength (CIS), Mental Fatigue Scale (MFS), and the Modified Fatigue Impact Scale (MFIS), which measure specific fatigue dimensions. Clinical measures such as the FSS, Fatigue Catastrophizing Scale (FCS), and the Numerical Rating Scale, were used only to measure general fatigue (Table 2b).
Studies which used multidimensional assessments performed more statistical tests, such as Cronbach's alpha and interclass correlation coefficient, to elucidate statistically significant differences between experimental and control groups. Whereas, studies that utilized unidimensional assessments more commonly calculated differences between groups by the total score of questionnaires. Equally important, the use of either types of instruments (unidimensional vs multidimension assessments), was dependent on the researcher and the non-oncologic medical condition studied. For instance, it may be more prudent to utilize unidimensional assessments when exploring a medical condition that produces complaints of a specific fatigue dimension (Berginström et al., 2017; Palm et al., 2017; Zeng et al., 2016). Although, it may be more effective to utilize a multidimensional assessment when studying medical conditions, such as CFS, that may cause participants to suffer from various dimensions of debilitating fatigue (Jason et al., 2011; Rowe et al., 2016).
The use of objective measures in conjunction with subjective fatigue questionnaires, such as the 6-Minute Walk Test (6MWT), is an interesting idea to explore for future research several studies (Ericsson et al., 2013; Jordan et al., 2017, & Tseng et al., 2009). So far, there has been inconsistencies in finding significant correlations between objective measures with subjective fatigue questionnaire data. For instance, in the Ericsson et al. (2013) study, investigators found a negative correlation between the distance walked during the 6MWT and the participants’ fatigue levels as assessed by the MFI. This relationship was not often observed, as patient-reported general fatigue did not correlate with objective measures in several medical conditions (e.g., healthy, Multiple Sclerosis, Traumatic Brain Injury, stroke, heart disease) (DeLuca et al., 2008). Perhaps, using innovative statistical approaches or exploring novel variables extracted from the objective data may provide some link between these objective outcomes with the complex, dynamic, multidimensional subjective experiences.
Cognitive and mental fatigue were frequently used interchangeably (DeLuca et al., 2008), while other included studies delineated the components that encompass these constructs. For example, Pattyn et al. (2018) suggested that the term “mental fatigue” may evoke the roles of emotion and motivation in fatigue, rather than just cognition. However, in other included studies, cognitive fatigue was used as a component of mental fatigue (Palm et al., 2017; Falup-Pecurariu et al., 2013; Chaudhuri et al., 2004). While in other studies, mental fatigue can be provoked and captured by cognitive tests combined with a self-report questionnaire, such as the MFS (Johansson et al., 2010). It was also observed that mental fatigue was influenced by pre-existing symptoms of depressed mood, sleep disturbances, and anxious feelings (Zeng et al., 2016, Da Costa et al., 2011; Kilsinger et al., 2010). Central fatigue, however, is a form of fatigue caused by diseases that affect the central, peripheral and autonomic nervous systems. (Chaudhuri et al., 2004). Further research and discussion is needed in order to come to a consensus on the appropriate terms to use for these specific dimensions of fatigue.
4.3. Limitations
As only one database was searched (i.e., PubMed) for this initial attempt to build evidence related to this topic, other relevant articles were possibly missed from our literature search and results. There are a number of specialized databases (ie. PsycINFO or Web of Science) that could have unique references where the topic of fatigue may be represented. Additionally, the inclusion of only English-language publications may have led to omission of relevant validated measures in different languages.
The use of multiple published definitions of fatigue from various medical conditions and diseases poses another limitation for this scoping review and for the topic, in general. In this scoping review, fatigue was defined differently among the included articles and different diagnostic criteria and clinical measures were used. This variability limited the ability to compare findings across studies. Further, ambiguity was increased when subjective assessments of each criterion with nominal (present vs. absent) scaling and no gradation for symptom severity of the fatiguing experience were used. Additionally, there is no consensus in the literature on an epidemiologically derived variable that unifies a single underlying pathophysiological process as to why fatigue exists.
Another limiting factor is that some of the included articles targeted their enrollment towards a specific demographic factor (e.g., sex). For example, 9 out of 10 patients with systemic lupus erythematosus (SLE) and over 80% of patients with Sjogren's syndrome were females (Goodchild et al., 2008). This non-mention of the specificity of gender-specific measures could possibly impact the testing and validation of certain measures across other disease populations.
4.4. Recommendations
Few articles differentiated fatigue using subscales that focused on differences in physical, mental, cognitive, emotional, and motivational functionality. This generalized approach could impact the reliability in measuring the various dimensions of fatigue. For example, physical fatigue will be measured differently than emotional fatigue, but this dimension-specific assessment will also differ between medical conditions. The impact of this variability is critical for both the research and clinical communities. Barriers in assessment consistency impede translation and ultimately delay appropriate patient-centered treatment.
More validation of these measures in various populations with different demographics is highly recommended. This can be done by administering the clinical measures to assess fatigue and its dimensions to a larger number of individuals to increase sample size and by enrolling participants from a diversified pool of individuals (e.g., age, sociocultural background, races/ethnicities, etc.) with a specific medical condition and from a specific clinical population.
5. Conclusion
Fatigue is a common but complex symptom. Having validated medical condition-specific clinical measures that measure fatigue and its dimensions is valuable, but psychometrics should reflect a common conceptualization of fatigue along with the use of subscales that allow for recognition of its multidimensional nature. Future research should examine if all or a core set of dimensions of fatigue (e.g., physical, cognitive, mental, motivational, emotional) should be included when measuring fatigue. Lastly, this scoping literature review examined non-oncologic related fatigue, thus a parallel investigation of fatigue in oncologic medical conditions should also be examined to compare these initial findings.
Declaration of competing interest
There are no conflicts of interest to report.
References
- Ablin J.N., Odes L., Neumann L., Buskila D. The Hebrew version of the FibroFatigue scale: validation of a questionnaire for assessment of fibromyalgia and chronic fatigue syndrome. Rheumatol. Int. 2010;30(9):1173–1176. doi: 10.1007/s00296-009-1122-1. [DOI] [PubMed] [Google Scholar]
- Abraham A., Drory V.E. Fatigue in motor neuron diseases. Neuromuscul. Disord. 2012;22(Suppl. 3):S198–S202. doi: 10.1016/j.nmd.2012.10.013. [DOI] [PubMed] [Google Scholar]
- Ali S., Matcham F., Irving K., Chalder T. Fatigue and psychosocial variables in autoimmune rheumatic disease and chronic fatigue syndrome: a cross-sectional comparison. J. Psychosom. Res. 2017;92:1–8. doi: 10.1016/j.jpsychores.2016.11.002. [DOI] [PubMed] [Google Scholar]
- Alsén P., Brink E., Brändström Y., Karlsson B., Persson L.-O. Fatigue after myocardial infarction: relationships with indices of emotional distress and sociodemographic and clinical variables. Int. J. Nurs. Pract. 2010;16:326–334. doi: 10.1111/j.1440-172X.2010.01848.x. [DOI] [PubMed] [Google Scholar]
- Anton H.A., Miller W.C., Townson A.F., Imam B., Silverberg N., Forwell S. The course of fatigue after acute spinal cord injury. Spinal Cord. 2017;55(1):94–97. doi: 10.1038/sc.2016.102. [DOI] [PubMed] [Google Scholar]
- Antoniu S.A., Ungureanu D. Measuring fatigue as a symptom in COPD: from descriptors and questionnaires to the importance of the problem. Chron. Respir. Dis. 2015;12(3):179–188. doi: 10.1177/1479972315575716. [DOI] [PubMed] [Google Scholar]
- Baldanzi S., Ricci G., Bottari M., Chico L., Simoncini C., Siciliano G. The proposal of a clinical protocol to assess central and peripheral fatigue in myotonic dystrophy type 1. Arch. Ital. Biol. 2017;155(1–2):43–53. doi: 10.12871/000398292017125. [DOI] [PubMed] [Google Scholar]
- Balsamo S., Diniz L.R., dos Santos-Neto L.L., da Mota L.M. Exercise and fatigue in rheumatoid arthritis. Isr. Med. Assoc. J. 2014;16(1):57–60. [PubMed] [Google Scholar]
- Belmont A., Agar N., Hugeron C., Gallais B., Azouvi P. Annales de réadaptation et de médecine physique. Vol. 49, No. 6. Elsevier Masson; 2006, July. Fatigue and traumatic brain injury; pp. 370–374. [DOI] [PubMed] [Google Scholar]
- Berginström N., Nordström P., Schuit R., Nordström A. The effects of (-)-OSU6162 on chronic fatigue in patients with traumatic brain injury: a randomized controlled trial. J. Head Trauma Rehabil. 2017;32(2):E46–E54. doi: 10.1097/HTR.0000000000000236. [DOI] [PubMed] [Google Scholar]
- Boehm N., Muehlberg H., Stube J.E. Managing poststroke fatigue using telehealth: a case report. Am. J. Occup. Ther. 2015;69(6) doi: 10.5014/ajot.2015.016170. 6906350020p1–6906350020p7. [DOI] [PubMed] [Google Scholar]
- Boehm K., Ostermann T., Milazzo S., Büssing A. Effects of yoga interventions on fatigue: a meta-analysis. Evid. base Compl. Alternative Med. 2012;2012 doi: 10.1155/2012/124703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell J.A., Caldwell J.L., Schmidt R.M. Alertness management strategies for operational contexts. Sleep Med. Rev. 2008;12(4):257–273. doi: 10.1016/j.smrv.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Castillo-Cejas M.D., Robles V., Borruel N., Torrejon A., Navarro E., Pelaez A., Casellas F. Questionnaries for measuring fatigue and its impact on health perception in inflammatory bowel disease. Rev. Esp. Enferm. Dig. 2013;105(3):144–153. doi: 10.4321/s1130-01082013000300005. [DOI] [PubMed] [Google Scholar]
- Chalder T., Berelowitz G., Pawlikowska T., Watts L., Wessely S., Wright D., Wallace E.P. Development of a fatigue scale. J. Psychosom. Res. 1993;37(2):147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- Chaudhuri A., Behan P.O. Fatigue in neurological disorders. Lancet. 2004;363(9413):978–988. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- Da Costa D., Zummer M., Fitzcharles M.A. Biopsychosocial determinants of physical and mental fatigue in patients with spondyloarthropathy. Rheumatol. Int. 2011;31(4):473–480. doi: 10.1007/s00296-009-1250-7. [DOI] [PubMed] [Google Scholar]
- DeLuca J., Genova H.M., Hillary F.G., Wylie G. Neural correlates of cognitive fatigue in multiple sclerosis using functional MRI. J. Neurol. Sci. 2008;270(1–2):28–39. doi: 10.1016/j.jns.2008.01.018. [DOI] [PubMed] [Google Scholar]
- Dencker A., Sunnerhagen K.S., Taft C., Lundgren-Nilsson A. Multidimensional fatigue inventory and post-polio syndrome - a Rasch analysis. Health Qual. Life Outcome. 2015;13:20. doi: 10.1186/s12955-015-0213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsais A., Wyller V.B., Loge J.H., Kerty E. Fatigue in myasthenia gravis: is it more than muscular weakness? BMC Neurol. 2013;13:132. doi: 10.1186/1471-2377-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ericsson A., Bremell T., Mannerkorpi K. Usefulness of multiple dimensions of fatigue in fibromyalgia. J. Rehabil. Med. 2013;45(7):685–693. doi: 10.2340/16501977-1161. [DOI] [PubMed] [Google Scholar]
- Falup-Pecurariu C. Fatigue assessment of Parkinson's disease patient in clinic: specific versus holistic. J. Neural. Transm. 2013;120(4):577–581. doi: 10.1007/s00702-013-0969-1. [DOI] [PubMed] [Google Scholar]
- Fan J., Smith A.P. In: Longo L., Leva M., editors. vol. 726. Springer; Cham: 2017. The impact of workload and fatigue on performance. (Human Mental Workload: Models and Applications. H-WORKLOAD 2017. Communications in Computer and Information Science). [Google Scholar]
- Fisk J.D., Ritvo P.G., Ross L., Haase D.A., Marrie T.J., Schlech W.F. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin. Infect. Dis. 1994;18(Supplement_1):S79–S83. doi: 10.1093/clinids/18.supplement_1.s79. [DOI] [PubMed] [Google Scholar]
- Goligher E.C., Pouchot J., Brant R., Kherani R.B., Avina-Zubieta J.A., Lacaille D.…Liang M.H. Minimal clinically important difference for 7 measures of fatigue in patients with systemic lupus erythematosus. J. Rheumatol. 2008;35(4):635–642. [PubMed] [Google Scholar]
- Goodchild C.E., Treharne G.J., Booth D.A., Kitas G.D., Bowman S.J. Measuring fatigue among women with Sjogren's syndrome or rheumatoid arthritis: a comparison of the Profile of Fatigue (ProF) and the Multidimensional Fatigue Inventory (MFI) Muscoskel. Care. 2008;6(1):31–48. doi: 10.1002/msc.124. [DOI] [PubMed] [Google Scholar]
- Gorski W., Mokros L., Kumor-Kisielewska A., Pietras T., Piotrowski W.J. The utility of selected questionnaires in the assessment of fatigue, depression and health quality in post-sarcoidosis fatigue syndrome. Adv Respir Med. 2017;85(6):313–321. doi: 10.5603/arm.2017.0054. [DOI] [PubMed] [Google Scholar]
- Hedlund L., Gyllensten A.L., Hansson L. A psychometric study of the multidimensional fatigue inventory to assess fatigue in patients with schizophrenia spectrum disorders. Community Ment. Health J. 2015;51(3):377–382. doi: 10.1007/s10597-014-9746-3. [DOI] [PubMed] [Google Scholar]
- Hernandez-Ronquillo L., Moien-Afshari F., Knox K., Britz J., Tellez-Zenteno J.F. How to measure fatigue in epilepsy? The validation of three scales for clinical use. Epilepsy Res. 2011;95(1–2):119–129. doi: 10.1016/j.eplepsyres.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Hester K.L., Macfarlane J.G., Tedd H., Jary H., McAlinden P., Rostron L., De Soyza A. Fatigue in bronchiectasis. QJM. 2012;105(3):235–240. doi: 10.1093/qjmed/hcr184. [DOI] [PubMed] [Google Scholar]
- Huang L.L., Guo D.H., Jing M.J., Wang X.X., Liu N., Wang P.X. A correlation between sickness or injury within two weeks, chronic diseases and fatigue among adults aged 18-45 years. Psychol. Health Med. 2017:1–8. doi: 10.1080/13548506.2017.1371313. [DOI] [PubMed] [Google Scholar]
- Husted J.A., Tom B.D., Farewell V.T., Gladman D.D. Longitudinal analysis of fatigue in psoriatic arthritis. J. Rheumatol. 2010;37(9):1878–1884. doi: 10.3899/jrheum.100179. [DOI] [PubMed] [Google Scholar]
- Jason L.A., Evans M., Brown M., Porter N., Brown A., Hunnell J.…Lerch A. Fatigue scales and chronic fatigue syndrome: issues of sensitivity and specificity. Disabil. Stud. Q. 2011;31(1) [PMC free article] [PubMed] [Google Scholar]
- Johansson B., Starmark A., Berglund P., Rödholm M., Rönnbäck L. A self-assessment questionnaire for mental fatigue and related symptoms after neurological disorders and injuries. Brain Inj. 2009;24(1):2–12. doi: 10.3109/02699050903452961. [DOI] [PubMed] [Google Scholar]
- Jordan B., Mehl T., Schweden T.L.K., Menge U., Zierz S. Assessment of physical fatigability and fatigue perception in myasthenia gravis. Muscle Nerve. 2017;55(5):657–663. doi: 10.1002/mus.25386. [DOI] [PubMed] [Google Scholar]
- Kapur N., Webb R. Suicide risk in people with chronic fatigue syndrome. Lancet. 2016;387(10028):1596–1597. doi: 10.1016/s0140-6736(16)00270-1. [DOI] [PubMed] [Google Scholar]
- Kent-Braun J.A., Miller R.G. Central fatigue during isometric exercise in amyotrophic lateral sclerosis. Muscle Nerve. 2000;23(6):909–914. doi: 10.1002/(sici)1097-4598(200006)23:6<909::aid-mus10>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Kinsinger S.W., Lattie E., Mohr D.C. Relationship between depression, fatigue, subjective cognitive impairment, and objective neuropsychological functioning in patients with multiple sclerosis. Neuropsychology. 2010;24(5):573–580. doi: 10.1037/a0019222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratz A.L., Schilling S., Goesling J., Williams D.A. The PROMIS FatigueFM Profile: a self-report measure of fatigue for use in fibromyalgia. Qual. Life Res. 2016;25(7):1803–1813. doi: 10.1007/s11136-016-1230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Learmonth Y.C., Dlugonski D., Pilutti L.A., Sandroff B.M., Klaren R., Motl R.W. Psychometric properties of the fatigue severity scale and the modified fatigue impact scale. J. Neurol. Sci. 2013;331(1–2):102–107. doi: 10.1016/j.jns.2013.05.023. [DOI] [PubMed] [Google Scholar]
- Lequerica A., Bushnik T., Wright J., Kolakowsky-Hayner S.A., Hammond F.M., Dijkers M.P., Cantor J. Psychometric properties of the multidimensional assessment of fatigue scale in traumatic brain injury: an NIDRR traumatic brain injury model systems study. J. Head Trauma Rehabil. 2012;27(6):E28–E35. doi: 10.1097/HTR.0b013e31826fe574. [DOI] [PubMed] [Google Scholar]
- Lewko A., Bidgood P.L., Jewell A., Garrod R. Evaluation of multidimensional COPD-related subjective fatigue following a pulmonary rehabilitation programme. Respir. Med. 2014;108(1):95–102. doi: 10.1016/j.rmed.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Li Y., Morris S., Cole J., Dube S., Smith J.A.M., Burbridge C., Wang W. Multidimensional daily diary of fatigue-fibromyalgia-17 items (MDF-fibro-17): part 2 psychometric evaluation in fibromyalgia patients. BMC Muscoskel. Disord. 2017;18(1):198. doi: 10.1186/s12891-017-1545-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukkahatai N., Walitt B., Espina A., Gelio A., Saligan L.N. Understanding the association of fatigue with other symptoms of fibromyalgia: development of a cluster model. Arthritis Care Res. 2016;68(1):99–107. doi: 10.1002/acr.22626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mairesse O., Damen V., Newell J., Kornreich C., Verbanck P., Neu D. The brugmann fatigue scale: an analogue to the epworth sleepiness scale to measure behavioral rest propensity. Behav. Sleep Med. 2017:1–22. doi: 10.1080/15402002.2017.1395336. [DOI] [PubMed] [Google Scholar]
- Michielsen H.J., De Vries J., Van Heck G.L. Psychometric qualities of a brief self-rated fatigue measure: The Fatigue Assessment Scale. J. Psychosom. Res. 2003;54(4):345–352. doi: 10.1016/s0022-3999(02)00392-6. [DOI] [PubMed] [Google Scholar]
- Norton C., Czuber-Dochan W., Bassett P., Berliner S., Bredin F., Darvell M.…Terry H. Assessing fatigue in inflammatory bowel disease: comparison of three fatigue scales. Aliment. Pharmacol. Ther. 2015;42(2):203–211. doi: 10.1111/apt.13255. [DOI] [PubMed] [Google Scholar]
- Palm S., Ronnback L., Johansson B. Long-term mental fatigue after traumatic brain injury and impact on employment status. J. Rehabil. Med. 2017;49(3):228–233. doi: 10.2340/16501977-2190. [DOI] [PubMed] [Google Scholar]
- Papakokkinou E., Johansson B., Berglund P., Ragnarsson O. Mental fatigue and executive dysfunction in patients with cushing's syndrome in remission. Behav. Neurol. 2015:173653. doi: 10.1155/2015/173653. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattyn N., Cutsem J.V., Dessy E., Mairesse O. Bridging exercise science, cognitive psychology, and medical practice: is “cognitive fatigue” a remake of “the emperor's new clothes”? Front. Psychol. 2018;9 doi: 10.3389/fpsyg.2018.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner I.K., Raselli C., Stocklin M., Opwis K., Kappos L., Calabrese P. The Fatigue Scale for Motor and Cognitive Functions (FSMC): validation of a new instrument to assess multiple sclerosis-related fatigue. Mult. Scler. 2009;15(12):1509–1517. doi: 10.1177/1352458509348519. [DOI] [PubMed] [Google Scholar]
- Rowe P.C., Fontaine K.R., Lauver M., Jasion S.E., Marden C.L., Moni M., Violand R.L. Neuromuscular strain increases symptom intensity in chronic fatigue syndrome. PloS One. 2016;11(7) doi: 10.1371/journal.pone.0159386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabre L., Westerberg E., Liik M., Punga A.R. Diversity in mental fatigue and social profile of patients with myasthenia gravis in two different Northern European countries. Brain Behav. 2017;7(4) doi: 10.1002/brb3.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saligan L.N., Olson K., Filler K., Larkin D., Cramp F., Yennurajalingam S., Mustian K. The biology of cancer-related fatigue: a review of the literature. Support. Care Canc. 2015;23(8):2461–2478. doi: 10.1007/s00520-015-2763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T.D., Boone S., Tan L., Dyrbye L.N., Sotile W., Satele D., Oreskovich M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- Slomko J., Estevez-Lopez F., Kujawski Slawomir K., Zawadka-Kuiskowska M., Tafil-Klaw T., Kwale J., Zalewski P. Autonomic phenotypes in Chronic Fatigue syndrome (CFS) are associated with illnes severity: a cluster analyis. J. Clin. Med. 2020;9:2531. doi: 10.3390/jmc9082531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng B.Y., Kluding P. The relationship between fatigue, aerobic fitness, and motor control in people with chronic stroke: a pilot study. J. Geriatr. Phys. Ther. 2009;32(3):97–102. doi: 10.1519/00139143-200932030-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Diemen T., van Lankveld W., van Leeuwen C., Post M., van Nes I. Multidimensional fatigue during rehabilitation in persons with recently acquired spinal cord injury. J. Rehabil. Med. 2016;48(1):27–32. doi: 10.2340/16501977-2018. [DOI] [PubMed] [Google Scholar]
- van Erp S., Ercan E., Breedveld P., Brakenhoff L., Ghariq E., Schmid S., van der Meulen-de Jong A. Cerebral magnetic resonance imaging in quiescent Crohn's disease patients with fatigue. World J. Gastroenterol. 2017;23(6):1018–1029. doi: 10.3748/wjg.v23.i6.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hoogmoed D., Fransen J., Bleijenberg G., van Riel P. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology. 2010;49(7):1294–1302. doi: 10.1093/rheumatology/keq043. [DOI] [PubMed] [Google Scholar]
- van Leeuwen N., Bossema E.R., Knoop H., Kruize A.A., Bootsma H., Bijlsma J.W., Geenen R. Psychological profiles in patients with Sjogren's syndrome related to fatigue: a cluster analysis. Rheumatology. 2015;54(5):776–783. doi: 10.1093/rheumatology/keu387. [DOI] [PubMed] [Google Scholar]
- Vercoulen J.H., Swanink C.M., Fennis J.F., Galama J.M., van der Meer, Bleijenberg G. Dimensional assessment of chronic fatigue syndrome. J. Psychosom. Res. 1994;38(5):383–392. doi: 10.1016/0022-3999(94)90099-x. [DOI] [PubMed] [Google Scholar]
- Voermans N.C., Knoop H., Bleijenberg G., van Engelen B.G. Fatigue is associated with muscle weakness in Ehlers-Danlos syndrome: an explorative study. Physiotherapy. 2011;97(2):170–174. doi: 10.1016/j.physio.2010.06.001. [DOI] [PubMed] [Google Scholar]
- Voermans N.C., Knoop H., van de Kamp N., Hamel B.C., Bleijenberg G., van Engelen B.G. Seminars in Arthritis and Rheumatism. 3. Vol. 40. Vol. 40. WB Saunders; 2010. 2010. Fatigue is a frequent and clinically relevant problem in Ehlers-Danlos syndrome; pp. 267–274.pp. 267–274. (Seminars in Arthritis and Rheumatism). [DOI] [PubMed] [Google Scholar]
- Volker I., Kirchner C., Bock O.L. Relation between multiple markers of work-related fatigue. Saf Health Work. 2016;7(2):124–129. doi: 10.1016/j.shaw.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolkorte R., Heersema D.J., Zijdewind I. Reduced dual-task performance in MS patients is further decreased by muscle fatigue. Neurorehabilitation Neural Repair. 2015;29(5):424–435. doi: 10.1177/1545968314552529. [DOI] [PubMed] [Google Scholar]
- Zangi H.A., Mowinckel P., Finset A., Eriksson L.R., Hoystad T.O., Lunde A.K., Hagen K.B. A mindfulness-based group intervention to reduce psychological distress and fatigue in patients with inflammatory rheumatic joint diseases: a randomised controlled trial. Ann. Rheum. Dis. 2012;71(6):911–917. doi: 10.1136/annrheumdis-2011-200351. [DOI] [PubMed] [Google Scholar]
- Zeng E.Q., Zeng B.Q., Tian J.L., Du B., Tian X.B., Chen H. Perceived social support and its impact on mental fatigue in patients with mild traumatic brain injury. Balkan Med. J. 2016;33(2):152–157. doi: 10.5152/balkanmedj.2016.15701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziwu R., Rihui L., Zhang Y. EEG-based fatigue detection using a two-level learning hierarchy radial basis function. Front. Neurorob. 2021;15:618408. doi: 10.3389/fnbot.2021.618408. [DOI] [PMC free article] [PubMed] [Google Scholar]