Abstract
Psychoneuroimmunology, the area of research dedicated to understanding the fundamental interactions between the central nervous system and the immune system, has given rise to the development of Immunopsychiatry, a new discipline which harnesses the immune system to produce beneficial outcomes for mental health problems. Immunopsychiatry has the potential to become a clinically relevant specialty area in psychiatric practice, but has not yet been adopted by the wider mental health community. This paper aims to map out the future trajectory of Immunopsychiatry on its road towards science-to-policy knowledge translation and clinical implementation. Three critical milestones which will need to be reached in order for Immunopsychiatry to fulfil its promise for clinical innovation are discussed: a clear definition of patients who fall within the immunopsychiatric continuum; demonstration of well-defined clinical benefit and incorporation in clinical guidelines; and convergence with other paradigms in biological psychiatry.
Keywords: Immunopsychiatry, Psychoneuroimmunology, Translational, Policy, Psychiatry, Innovation, Mental health
1. From psychoneuroimmunology to immunopsychiatry
A functional link between mental states and immunological processes has been hypothesized since long before the founding of psychoneuroimmunology (PNI) as the area of basic research dedicated to understanding these fundamental interactions (Solomon, 1985). As previously examined by other authors, in the last decade the field has undergone a translational shift into an area of research that harnesses the immune system to deliver real-world positive outcomes for psychiatric patients under the new flag of “Immunopsychiatry” (IP) (Leboyer, 2015; Leboyer et al., 2016a, 2016b; Pariante, 2015, 2019) (see Fig. 1).
Fig. 1.

Livia J. De Picker (°1988) MD PhD received her summa cum laude medical degree from the University of Antwerp (Belgium) in 2012, after which she concurrently undertook her PhD and psychiatry residency programs. She worked abroad at the University of Southampton (UK) and UMC Leiden (NL), and won several scholarships and awards, including the ADS Science Communication Contest. In 2013 she joined the board of the European Federation of Psychiatric Trainees, an independent federation of psychiatric trainee organisations representing trainees from 37 countries. She led the organization as president in 2015–2016, and hosted the 24th European Forum of Psychiatric Trainees. After graduating as psychiatrist in 2019, and defending her PhD thesis ‘State-associated Inflammatory Changes in Psychotic Illness’’ in 2020, she started her new position as clinical psychiatrist and postdoctoral researcher at the University Psychiatric Hospital Duffel (Belgium). Dr. De Picker's current work convenes at the interface of research, clinical care, education and health policy – focusing on synergies and strategies for knowledge translation in psychiatric care. With eight years of Immunopsychiatry research experience, she has become an influential early career clinician-scientist who consistently promotes her field in Belgium and Europe. As board member of the European Psychiatric Association and president-elect of the Belgian College for Neuropsychopharmacology and Biological Psychiatry, she organized several successful scientific events and launched initiatives for junior clinician-researchers. Her track record as member of the European College of Neuropsychopharmacology (ECNP) Early Career Advisory Panel (2015–2019) and Educational Committee (2017–2019) includes the creation of new educational initiatives aimed to bridge the translational gap between preclinical and clinical research. In 2021, she led several international collaborative research projects on COVID-19 for the ECNP Immuno-NeuroPsychiatry Network and coordinated an international advocacy campaign for priority vaccination of patients with severe mental illness, which received endorsements from five major psychiatric organisations and resulted in policy changes in several countries.
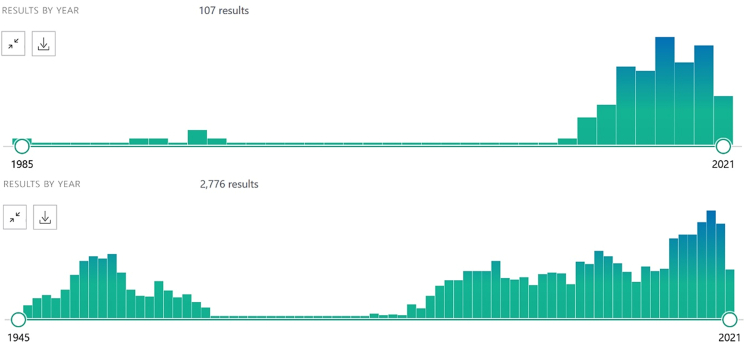
While Immunopsychiatry has the potential to become a clinically relevant specialty area in psychiatric practice, to the larger field of mental health care research and practice, Immunopsychiatry is still considered a “niche” area with little actual impact. A scoping PubMed search quickly reveals that the term has not yet been adopted by the larger scientific community (Fig. 2). One of the main challenges that will need to be overcome is explaining and convincing clinicians, service users, and other stakeholders of the significance of this discipline.
Fig. 2.
Evolution of scientific publications including the terms “Immunopsychiatry” (top) and “Psychoneuroimmunology” (bottom). Immunopsychiatry is a younger discipline, and the term featured only 100 times in scientific literature over the last decade (2010–2021), compared to 857 results for Psychoneuroimmunology in the same time period. Source: PubMed (accessed May 13th, 2021).
In his 2019 editorial for a special issue of Psychoneuroendocrinology, Prof. C. Pariante writes that Immunopsychiatry has now been recognised “as an essential aspect of mainstream psychiatry research and clinical practice” (Pariante, 2019). As someone active in both fields and directly involved in the major European psychiatric associations, I cannot yet concur with this optimistic stance. Despite the major efforts and achievements of many PNI/IP research groups, the discipline still operates largely within its own corner. If it were truly an essential aspect of mainstream psychiatry research, the COVID-19 pandemic and its abundantly clear impact on mental health should have resulted in an eruption of scientific literature on the role of immunopsychiatric mechanisms in the pandemic. Although the term “Immunopsychiatry” has gained some attention during the pandemic, it still represents less than 1% of all psychiatric COVID-related preprints (SSRN 6 out of 767 preprints; bioRxiv/medRxiv 14 out of 1435 preprints, see Table 1). An estimated 34% of COVID-19 survivors are diagnosed with a new neurological or psychiatric diagnosis within six months after the acute infection (Taquet et al., 2021), and we have recently demonstrated that patients with pre-existent mental illness are at significantly increased risk of mortality (crude odds ratio 2·00, 95% CI 1·58-2·54) and hospitalization (crude odds ratio 2·24, 95% CI 1·70-2·94) following COVID-19 infection (Vai et al., 2021). Yet in the discussion about priority vaccination of patients with severe mental illness, immunopsychiatric arguments remained largely disregarded until we have pointed them out in a collaborative Viewpoint paper published in Brain, Behavior, and Immunity upon the initiative of the COVID-19 working group of the ECNP Immuno-NeuroPsychiatry Network (De Picker et al., 2021). Indeed the COVID-19 pandemic may offer our discipline a unique opportunity for progress by serving as a catalyst event for generating, validating and disseminating immunopsychiatric hypotheses – but only if we are ready to take this next leap forward.
Table 1.
Scoping search of two main biomedical preprint servers SSRN (https://www.ssrn.com/index.cfm/en/) and bioRxiv and/or medRxiv (https://www.biorxiv.org/); search window January 1st, 2020 to May 13th, 2021.
| Search term | SSRN | bioRxiv and/or MedRxiv |
|---|---|---|
| Immunopsychiatry | 6 (of which 6 COVID-related) | 20 (of which 14 COVID-related) |
| Psychoneuroimmunology | 16 (of which 2 COVID-related) | 29 (of which 5 COVID-related) |
| Psychiatry | 3407 | 8437 |
| Psychiatry AND COVID∗ | 767 | 1435 |
This paper aims to map out the future trajectory of Immunopsychiatry on its road towards science-to-policy knowledge translation and clinical implementation. Three critical milestones will be discussed. They represent targets which will need to be reached in order for Immunopsychiatry to fulfil its promise for clinical innovation:
-
(1)
a clear definition of patients who fall within the immunopsychiatric continuum;
-
(2)
demonstration of well-defined clinical benefit and incorporation in clinical guidelines;
-
(3)
convergence with other paradigms in biological psychiatry.
2. Cui bono? The immunopsychiatric continuum
Engaging in a discussion with important stakeholders requires a clear definition of which patients and which problems our discipline is trying to formulate an answer for. Interestingly, this is a remarkably difficult question to answer, as Immunopsychiatry encompasses a large spectrum of immune mechanisms which may to varying degrees and in various constellations contribute to mental health issues.
A classical, categorical way to define the target patient population has been to differentiate between two different sets of patients. A first group are persons presenting with what are commonly referred to as “organic” immunopsychiatric syndromes. These are patients who demonstrate psychiatric complaints, caused by an underlying, identifiable, and diagnosable inflammatory or immunological process with or without direct impact in the central nervous system (CNS). Distinct examples include tertiary syphilis, NMDA-receptor encephalitis or interferon-gamma treatment-induced depression. Such patients would be categorised as “[Psychiatric Disorder] Due to Another Medical Condition” under the DSM-5 (American Psychiatric Association, 2013). As knowledge about CNS-immune interactions has now broadened and deepened, this concept could also encompass patients within a wider and unbounded spectrum of comorbid (un)diagnosed multisystem inflammatory conditions (e.g. rheumatoid arthritis, psoriasis, diabetes mellitus type I, auto-immune thyroid conditions, paraneoplastic syndromes etc.) (Leboyer et al., 2012). During my active clinical career, I have personally witnessed a few such presentations (Masrori et al., 2021; van Ham et al., 2014)). Notwithstanding the interesting case presentations which they may give rise to, most psychiatrists will consider these clinical syndromes at the outer boundary of their discipline and field of expertise. This is contrasted against a second group of patients: those with “true” or “primary” psychiatric illness. In these patients, immune disturbances may be part of a multifactorial pathophysiology, either through increasing vulnerability for illness onset or by mediating illness progression (De Picker et al., 2017). It is currently still unknown if immune mechanisms exclusively or differentially affect: (1) specific psychiatric disorders; (2) specific subpopulations within a psychiatric disorder, or (3) specific clinical states within a patient with a psychiatric disorder. Based on our own work in psychotic and mood disorders, there seems to be more support for the notion of state-specific rather than diagnosis-specific inflammatory changes in psychotic and mood disorders (De Picker et al., 2019a, 2019b; Hebbrecht et al., 2021; Morrens et al., 2020).
Because of this dualistic dichotomy between “organic” and “primary” (immuno)psychiatric syndromes, most mental health professionals have received little to no training on how to screen and diagnose immunological abnormalities or comorbidities, while negative bias or insufficient experience may get in the way of the clinical management of psychiatric patients by somatic specialists. Clinical guidance on how immunological disturbances may interact with the clinical presentation and treatment of a psychiatric disorder is still crucially lacking. The result is that many immunological problems may remain underdiagnosed and undertreated among psychiatric patients, in particular in patients with subclinical, polymorphic or atypical somatic presentations. Furthermore, patients with severe mental illness have been demonstrated to have reduced access to appropriate somatic care, while also being disproportionally often affected by somatic health problems, including comorbid autoimmune disease, chronic infections and other types of inflammatory disorders (De Hert et al., 2011; Fleischhacker et al., 2008; Lawrence and Kisely, 2010). Bidirectional longitudinal associations have been found for a personal and family history of several autoimmune diseases and increased risks for psychotic and bipolar disorders (Chen et al., 2021; Jeppesen and Benros, 2019). A recent meta-analysis comprising data for >25 million individuals estimated that patients diagnosed with a non-neurological autoimmune disease (NNAI) had a 43% increased chance to subsequently receive a diagnosis of psychotic disorder, while patients with psychotic disorders were 50% more likely to be diagnosed with NNAI disease (Cullen et al., 2019).
Growing evidence of the important overlap between these two patient groups challenges us to reconceptualize them as representing two extremes on a clinical continuum, rather than two or more distinct clinical groups who each need to be treated by different specialists in different settings (Fig. 3). Much in the same way as we now understand the role of genetics in most medical conditions, we can conceive of a clinical continuum based upon the proportional attribution of the immune mechanism in the pathophysiology of the psychiatric presentation. On the one extreme, there are some distinct, often rare, conditions for which we can identify one specific causal immunological mechanism (i.e. rare auto-immune conditions with neuropsychiatric presentation – similar to rare monogenetic syndromes). On the other extreme, many “common” conditions require a complex interplay of multiple immunological and non-immunological pathways (similar to polygenic risk scores and gene-environment interactions). This concept would validate the observed clinical heterogeneity and add structure to the ongoing shift from categorical to dimensional or personalized diagnostic approaches in psychiatry (Leboyer and Schurhoff, 2014).
Fig. 3.
Proposal for an “Immunopsychiatry continuum”: Different patient groups are dimensionally defined depending on the proportional attribution of immune mechanism in the pathophysiology of their psychiatric presentation, i.e. from ‘single-cause and direct’ to ‘multifactorial and indirect’.
The conception of an immunopsychiatric continuum should be accompanied by targeted educational, policy and clinical strategies covering all patients on the spectrum. Dedicated multidisciplinary expert clinics should be established for systematic screening of immunological disturbances of all newly diagnosed and/or treatment-resistant major psychiatric disorders, and for expert evaluation of specific mental changes accompanying immunological causes. Close collaboration and knowledge exchange, including joint consultations (e.g. joint immunopsychiatry consultations at the University Hospital Henri Mondor, Paris, France) should be fostered between psychiatrists, immunologists and other appropriate specialties (e.g. neurologists, internal medicine specialists, geriatric medicine specialists etc.) both in research groups and the clinical level. Interestingly, patients who fall towards the middle of the continuum, with diagnosed comorbid psychiatric ánd immunological disorders are often excluded from psychiatric, immunological ánd immunopsychiatric clinical trials, perpetuating the knowledge gap. Ultimately, these synergistic efforts should provide the foundation to generate sufficient evidence to develop multidisiciplinary clinical immunopsychiatry guidelines.
3. Science-to-policy transformation
Following the clear definition of the spectrum of patients who can benefit from Immunopsychiatry, we will need a strategy to push the discipline from bench to bedside, by focusing on the most promising clinical innovations our discipline may produce: i.e. (1) novel treatment options and (2) biomarkers for prediction of illness onset and/or progression (Table 2).
Table 2.
Strategic priorities for clinical translation of Immunopsychiatry research.
| Opportunities | Challenges | |
|---|---|---|
| Multidisciplinary management of comorbid auto-immune/ inflammatory conditions |
|
|
| Immunopsychiatric treatments for ‘primary’ psychiatric conditions |
|
|
| Immune biomarkers for prediction of illness onset |
|
|
| Immune biomarkers for prediction of illness progression or treatment response |
|
|
The study of immune-modulating treatments for psychiatric disorders has definitely gained traction in the last two decades, and meta-analyses demonstrating the benefit of celecoxib and/or minocycline are now available for schizophrenia, bipolar disorder and major depressive disorder (Bavaresco et al., 2019; Cakici et al., 2019; Jeppesen et al., 2020; Na et al., 2014; Rosenblat et al., 2016; Rosenblat and McIntyre, 2018; Xiang et al., 2017). Yet none of these treatment options have been included in official clinical guidelines. While evidence keeps on accumulating, it is unclear at which point we will surpass the critical level needed to use this knowledge in clinical practice. Part of the problem is that the research on immunological compounds of psychiatric disorders is seen as generating conflicting results, with unpredictable expected benefit for an individual patient (De Picker et al., 2017). In many countries, clinicians cannot prescribe off-label compounds unless they are incorporated in national and/or international treatment guidelines. This step will not be taken until our field can provide an answer to the questions: which disorder, which patients, which phase of the illness, which compound(s). Stratified and adapted trial designs, including multi-arm and multi-stage trials in which patients are stratified by their baseline immunological profile, can help answer these important questions within the next decade (Table 2).
Despite the urgent unmet need for good clinical biomarkers for psychiatric illness, their development has been hindered by a lack of methodological standardization and clinical heterogeneity (De Picker and Haarman, 2021). Confounding through methodological variability is a major problem which needs to be eliminated through consensus guidelines for standardized immunopsychiatric assessments, a priority issue on the agenda of the ECNP's Immuno-NeuroPsychiatry Network (https://www.ecnp.eu/research-innovation/ECNP-networks/List-ECNP-Networks/Immuno-NeuroPsychiatry). Beyond the standardization of laboratory measurements, patients also need to be adequately characterized, with differentiation of trait and state effects. Longitudinal, transdiagnostic designs including multiple markers and biological compartments (e.g. plasma proteins, blood messenger RNA, peripheral blood mononuclear cells, cerebrospinal fluid, …) are preferred. Large cohorts with standardized comprehensive assessments are needed to test and validate predictive models which can help clinicians to (1) determine treatment response to regular psychiatric or immunomodulating treatments (Attwells et al., 2020), (2) forecast the most likely clinical course or (3) provide a meaningful differentiation between phenotypically similar clinical presentations (Poletti et al., 2021). In addition, multidisciplinary and translational research projects, integrating both preclinical and clinical models, are required to tackle fundamental pathophysiological questions, such as how immunogenetic vulnerabilities interact with early-life immunological stressors to produce a specific illness phenotype, and which preventive actions can counteract these effects. Research projects of this scale can only be accomplished through the establishment of large consortia which are willing to share datasets to create sufficient predictive power. For all the strategic priorities outlined above, international organisations such as the PsychoNeuroImmunology Research Society (PNIRS) and ECNP Immuno-NeuroPsychiatry Network will need to step up as key actors and pave the way forward.
4. Integration within the psychiatric paradigm
A final priority towards the integration of our discipline in mainstream psychiatry is obtaining a higher level of convergence between PNI/IP research and other research paradigms of biological psychiatry (e.g. gut-brain axis; early-life stress/HPA axis; mono-aminergic and other neurotransmitter systems; (epi)genetics; chronobiology; neuroplasticity; ageing etc.). Immunopsychiatry needs to be incorporated into psychiatric textbooks, not just as a separate section or subdiscipline, but at the core of psychiatric pathophysiology, integrated with the other dominant theories. In one of my earlier works, I strived to do this by using the approach of a meta-review, linking the literature of immune dysregulation and neuroplasticity in psychotic disorders (De Picker et al., 2017). While Immunopsychiatry research has started venturing out to explore such links, more work is clearly still needed before we can present an integrated overarching theory of vulnerability which explains how immune disturbances lead to dopaminergic/serotonergic malfunctioning and ultimately specific clinical presentations. Such an endeavour crucially depends on close interactions and collaboration between researchers working in different fields. A scoping PubMed search with combined search terms from five major paradigms [(psychiatr∗ AND immun∗ AND neurotransmitter AND (plasticity OR neuroplasticity) AND stress AND (genetic OR epigenetic) (accessed May 15th 2021)] generated only 17 results published between 2012 and 2021, 11 of which were preclinical (cell line or animal) studies. Only three review papers were found which reconceptualized schizophrenia (Howes and McCutcheon, 2017; van Winkel et al., 2013) and bipolar (Sigitova et al., 2017) pathophysiology with integrated findings from different research paradigms.
Finally, integration within the mainstream psychiatric paradigm will be both a prerequisite to and a consequence of the incorporation of clinically relevant immunopsychiatric insights into pre- and postgraduate medical education curricula. Amendments to medical education move at a notoriously slow pace, and thus need to be planned and prepared well in advance. In Europe in particular, we have recently demonstrated that psychiatric training curricula are highly heterogeneous and difficult to influence or harmonize, as each country determines the content and structure of its own postgraduate psychiatric training program (Baessler et al., 2021). Training the Immunopsychiatrists of the future therefore calls for unrelenting and coordinated action by stakeholder organisations, starting today.
In conclusion, after delineating the Immunopsychiatry continuum and demonstrating clear therapeutic benefit for the patients it encompasses, we need to embrace the notion that immune responses are intricately linked with other biological processes. Immunopsychiatry will only be useful as part of a systemic or holistic approach. Reiterating earlier words, convergence was at the origin of our discipline, and we now need it again to make it succeed (Hutchinson, 2018).
Role of funding
There was no funding source for this study. LDP is funded by the University Psychiatric Hospital Duffel. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Ethics approval
No human subject participants were involved. The study was exempt from ethics approval.
Contribution
LDP conceptualized and wrote the manuscript as single author.
Declaration of competing interest
LDP reports grants from Boehringer-Ingelheim and Janssen R&D, outside the submitted work. LDP is a member of the ECNP Immuno-NeuroPsychiatry Network.
Acknowledgment
The author would like to thank the University Psychiatric Hospital Duffel for their support, as well as Prof. dr. Marion Leboyer and the members of the ECNP Immuno- NeuroPsychiatry Network for the many interesting discussions and meetings which served as inspiration for this manuscript.
References
- American Psychiatric Association . fifth ed. 2013. Diagnostic and Statistical Manual of Mental Disorders. Arlington, vol. A. [Google Scholar]
- Attwells S., Setiawan E., Rusjan P.M., Xu C., Hutton C., Rafiei D., Varughese B., Kahn A., Kish S.J., Vasdev N., Houle S., Meyer J.H. Translocator protein distribution volume predicts reduction of symptoms during open-label trial of celecoxib in major depressive disorder. Biol. Psychiatr. 2020;88:649–656. doi: 10.1016/j.biopsych.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baessler F., Zafar A., Gargot T., da Costa M.P., Biskup E.M., De Picker L., Koelkebeck K., Riese F., Ryland H., Kazakova O., Birkle S., Kanellopoulos T., Grassl R., Braicu A., Schultz J.H., Casanova Dias M. Psychiatry training in 42 European countries: a comparative analysis. Eur. Neuropsychopharmacol. 2021;46:68–82. doi: 10.1016/j.euroneuro.2021.02.003. [DOI] [PubMed] [Google Scholar]
- Bavaresco D.V., Colonetti T., Grande A.J., Colom F., Valvassori S.S., Quevedo J., da Rosa M.I. Efficacy of celecoxib adjunct treatment on bipolar disorder: systematic review and meta-analysis. CNS Neurol. Disord. - Drug Targets. 2019;18:19–28. doi: 10.2174/1871527317666181105162347. [DOI] [PubMed] [Google Scholar]
- Cakici N., van Beveren N.J.M., Judge-Hundal G., Koola M.M., Sommer I.E.C. An update on the efficacy of anti-inflammatory agents for patients with schizophrenia: a meta-analysis. Psychol. Med. 2019;49:2307–2319. doi: 10.1017/S0033291719001995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M., Jiang Q., Zhang L. The prevalence of bipolar disorder in autoimmune disease: a systematic review and meta-analysis. Ann. Palliat. Med. 2021;10:350–361. doi: 10.21037/apm-20-2293. [DOI] [PubMed] [Google Scholar]
- Cullen A.E., Holmes S., Pollak T.A., Blackman G., Joyce D.W., Kempton M.J., Murray R.M., McGuire P., Mondelli V. Associations between non-neurological autoimmune disorders and psychosis: a meta-analysis. Biol. Psychiatr. 2019;85:35–48. doi: 10.1016/j.biopsych.2018.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Hert M., Cohen D., Bobes J., Cetkovich-Bakmas M., Leucht S., Ndetei D.M., Newcomer J.W., Uwakwe R., Asai I., Moller H.J., Gautam S., Detraux J., Correll C.U. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatr. 2011;10:138–151. doi: 10.1002/j.2051-5545.2011.tb00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Picker L., Fransen E., Coppens V., Timmers M., de Boer P., Oberacher H., Fuchs D., Verkerk R., Sabbe B., Morrens M. Immune and neuroendocrine trait and state markers in psychotic illness: decreased kynurenines marking psychotic exacerbations. Front. Immunol. 2019;10:2971. doi: 10.3389/fimmu.2019.02971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Picker L., Ottoy J., Verhaeghe J., Deleye S., Wyffels L., Fransen E., Kosten L., Sabbe B., Coppens V., Timmers M., de Boer P., Van Nueten L., Op De Beeck K., Oberacher H., Vanhoenacker F., Ceyssens S., Stroobants S., Staelens S., Morrens M. State-associated changes in longitudinal [(18)F]-PBR111 TSPO PET imaging of psychosis patients: evidence for the accelerated ageing hypothesis? Brain Behav. Immun. 2019;77:46–54. doi: 10.1016/j.bbi.2018.11.318. [DOI] [PubMed] [Google Scholar]
- De Picker L.J., Haarman B.C.M. Applicability, potential and limitations of TSPO PET imaging as a clinical immunopsychiatry biomarker. Eur. J. Nucl. Med. Mol. Imag. 2021 doi: 10.1007/s00259-021-05308-0. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- De Picker L.J., Morrens M., Chance S.A., Boche D. Microglia and brain plasticity in acute psychosis and schizophrenia illness course: a meta-review. Front. Psychiatr. 2017;8:238. doi: 10.3389/fpsyt.2017.00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Picker L.J., Yolken R., Benedetti F., Borsini A., Branchi I., Fusar-Poli P., Carlos Leza J., Pariante C., Pollak T., Tamouza R., Vai B., Vernon A.C., Benros M.E., Leboyer M. Viewpoint | European COVID-19 exit strategy for people with severe mental disorders: too little, but not yet too late. Brain Behav. Immun. 2021 doi: 10.1016/j.bbi.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischhacker W.W., Cetkovich-Bakmas M., De Hert M., Hennekens C.H., Lambert M., Leucht S., Maj M., McIntyre R.S., Naber D., Newcomer J.W., Olfson M., Osby U., Sartorius N., Lieberman J.A. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J. Clin. Psychiatr. 2008;69:514–519. doi: 10.4088/jcp.v69n0401. [DOI] [PubMed] [Google Scholar]
- Hebbrecht K., Skorobogatov K., Giltay E.J., Coppens V., De Picker L., Morrens M. Tryptophan catabolites in bipolar disorder: a meta-analysis. Front. Immunol. 2021 doi: 10.3389/fimmu.2021.667179. (accepted for publication April 13, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howes O.D., McCutcheon R. Inflammation and the neural diathesis-stress hypothesis of schizophrenia: a reconceptualization. Transl. Psychiatry. 2017;7:e1024. doi: 10.1038/tp.2016.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain M.I., Chaudhry I.B., Khoso A.B., Husain M.O., Hodsoll J., Ansari M.A., Naqvi H.A., Minhas F.A., Carvalho A.F., Meyer J.H., Deakin B., Mulsant B.H., Husain N., Young A.H. Minocycline and celecoxib as adjunctive treatments for bipolar depression: a multicentre, factorial design randomised controlled trial. Lancet Psychiatry. 2020;7:515–527. doi: 10.1016/S2215-0366(20)30138-3. [DOI] [PubMed] [Google Scholar]
- Hutchinson M.R. 'Convergence' created psychoneuroimmunology, and is needed again to secure the future of the field. Brain Behav. Immun. 2018;71:1–2. doi: 10.1016/j.bbi.2018.05.011. [DOI] [PubMed] [Google Scholar]
- Jeppesen R., Benros M.E. Autoimmune diseases and psychotic disorders. Front. Psychiatr. 2019;10:131. doi: 10.3389/fpsyt.2019.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeppesen R., Christensen R.H.B., Pedersen E.M.J., Nordentoft M., Hjorthoj C., Kohler-Forsberg O., Benros M.E. Efficacy and safety of anti-inflammatory agents in treatment of psychotic disorders - a comprehensive systematic review and meta-analysis. Brain Behav. Immun. 2020;90:364–380. doi: 10.1016/j.bbi.2020.08.028. [DOI] [PubMed] [Google Scholar]
- Lawrence D., Kisely S. Inequalities in healthcare provision for people with severe mental illness. J. Psychopharmacol. 2010;24:61–68. doi: 10.1177/1359786810382058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leboyer M. Is it time for immuno-psychiatry in bipolar disorder and suicidal behaviour? Acta Psychiatr. Scand. 2015;132:159–160. doi: 10.1111/acps.12456. [DOI] [PubMed] [Google Scholar]
- Leboyer M., Berk M., Yolken R.H., Tamouza R., Kupfer D., Groc L. Immuno-psychiatry: an agenda for clinical practice and innovative research. BMC Med. 2016;14:173. doi: 10.1186/s12916-016-0712-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leboyer M., Oliveira J., Tamouza R., Groc L. Is it time for immunopsychiatry in psychotic disorders? Psychopharmacology (Berlin) 2016;233:1651–1660. doi: 10.1007/s00213-016-4266-1. [DOI] [PubMed] [Google Scholar]
- Leboyer M., Schurhoff F. Searching across diagnostic boundaries. Schizophr. Bull. 2014;40:946–948. doi: 10.1093/schbul/sbu112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leboyer M., Soreca I., Scott J., Frye M., Henry C., Tamouza R., Kupfer D.J. Can bipolar disorder be viewed as a multi-system inflammatory disease? J. Affect. Disord. 2012;141:1–10. doi: 10.1016/j.jad.2011.12.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masrori P., Vaesen Bentein H., Raskin J., Montagna M., De Picker L., De Volder I., Van Schil P.E., Janssens A., Mercelis R. Caspr2 autoantibody-associated Morvan syndrome predating thymoma relapse by 30 months. Lung Canc. 2021;153:117–119. doi: 10.1016/j.lungcan.2021.01.012. [DOI] [PubMed] [Google Scholar]
- Morrens M., De Picker L., Kampen J.K., Coppens V. Blood-based kynurenine pathway alterations in schizophrenia spectrum disorders: a meta-analysis. Schizophr. Res. 2020;223:43–52. doi: 10.1016/j.schres.2020.09.007. [DOI] [PubMed] [Google Scholar]
- Na K.S., Lee K.J., Lee J.S., Cho Y.S., Jung H.Y. Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2014;48:79–85. doi: 10.1016/j.pnpbp.2013.09.006. [DOI] [PubMed] [Google Scholar]
- Nettis M.A., Lombardo G., Hastings C., Zajkowska Z., Mariani N., Nikkheslat N., Worrell C., Enache D., McLaughlin A., Kose M., Sforzini L., Bogdanova A., Cleare A., Young A.H., Pariante C.M., Mondelli V. Augmentation therapy with minocycline in treatment-resistant depression patients with low-grade peripheral inflammation: results from a double-blind randomised clinical trial. Neuropsychopharmacology. 2021;46:939–948. doi: 10.1038/s41386-020-00948-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariante C.M. Psychoneuroimmunology or immunopsychiatry? Lancet Psychiatry. 2015;2:197–199. doi: 10.1016/S2215-0366(15)00042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariante C.M. The year of immunopsychiatry: a special issue that foresaw the future. Psychoneuroendocrinology. 2019;103:49–51. doi: 10.1016/j.psyneuen.2019.01.002. [DOI] [PubMed] [Google Scholar]
- Poletti S., Vai B., Mazza M.G., Zanardi R., Lorenzi C., Calesella F., Cazzetta S., Branchi I., Colombo C., Furlan R., Benedetti F. A peripheral inflammatory signature discriminates bipolar from unipolar depression: a machine learning approach. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;105:110136. doi: 10.1016/j.pnpbp.2020.110136. [DOI] [PubMed] [Google Scholar]
- Rosenblat J.D., Kakar R., Berk M., Kessing L.V., Vinberg M., Baune B.T., Mansur R.B., Brietzke E., Goldstein B.I., McIntyre R.S. Anti-inflammatory agents in the treatment of bipolar depression: a systematic review and meta-analysis. Bipolar Disord. 2016;18:89–101. doi: 10.1111/bdi.12373. [DOI] [PubMed] [Google Scholar]
- Rosenblat J.D., McIntyre R.S. Efficacy and tolerability of minocycline for depression: a systematic review and meta-analysis of clinical trials. J. Affect. Disord. 2018;227:219–225. doi: 10.1016/j.jad.2017.10.042. [DOI] [PubMed] [Google Scholar]
- Sigitova E., Fisar Z., Hroudova J., Cikankova T., Raboch J. Biological hypotheses and biomarkers of bipolar disorder. Psychiatr. Clin. Neurosci. 2017;71:77–103. doi: 10.1111/pcn.12476. [DOI] [PubMed] [Google Scholar]
- Solomon G. The emerging field of psychoneuroimmunology. Behav. Brain Sci. 1985;8:411. [Google Scholar]
- Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vai B., Mazza M.G., Delli Colli C., Foiselle M., Allen B., Benedetti F., Borsini A., Casanova Dias M., Tamouza R., Leboyer M., Benros M.E., Branchi I., Fusar-Poli P., De Picker L.J. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry [online ahead of print] 2021 doi: 10.1016/S2215-0366(21)00232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ham C., Schrijvers D., De Picker L., Vandendriessche F., Sabbe B. Neuropsychiatric features in Behcet's disease: a case report. Clin. Neurol. Neurosurg. 2014;127:13–14. doi: 10.1016/j.clineuro.2014.09.010. [DOI] [PubMed] [Google Scholar]
- van Winkel R., van Nierop M., Myin-Germeys I., van Os J. Childhood trauma as a cause of psychosis: linking genes, psychology, and biology. Can. J. Psychiatr. 2013;58:44–51. doi: 10.1177/070674371305800109. [DOI] [PubMed] [Google Scholar]
- Xiang Y.Q., Zheng W., Wang S.B., Yang X.H., Cai D.B., Ng C.H., Ungvari G.S., Kelly D.L., Xu W.Y., Xiang Y.T. Adjunctive minocycline for schizophrenia: a meta-analysis of randomized controlled trials. Eur. Neuropsychopharmacol. 2017;27:8–18. doi: 10.1016/j.euroneuro.2016.11.012. [DOI] [PubMed] [Google Scholar]