Amyloidosis is a disorder resulting from the abnormal extracellular accumulation of amyloid in various tissues and organs.1 Tracheobronchial and pulmonary amyloidosis may be part of a systemic process or confined only to the respiratory organs.2 Although rare, nodular pulmonary amyloidosis can mimic other diseases that manifest as multiple pulmonary lesions, including neoplastic and granulomatous conditions.3 Therefore, pulmonary amyloidosis should be included in the differential diagnosis of single or multiple pulmonary nodules.
An 82-year-old asymptomatic nonsmoking woman with a history of breast cancer was seen at our hospital because of an irregular shadow on her chest radiograph. High-resolution computed tomography (CT) revealed four solid nodules: a dominant 27-mm spiculated lesion corresponding to the shadow on the chest radiograph, a lesion in the right middle lobe, and two smaller lesions (mean, 8 mm) located in the right lower and left upper lobes (Fig. 1A–C). The CT also noted partial tracheobronchial wall thickening (Fig. 2A). Positron emission tomography revealed focal fluorodeoxyglucose uptake in the 27-mm nodule only (Fig. 1D). Bronchoscopy was performed given these tracheobronchial findings, which revealed several polypoid nodules on the tracheobronchial wall; biopsy was then performed, which revealed amyloidosis (Fig. 2B and C). Thoracoscopic wedge resection of the right lower lobe was performed, and the frozen section diagnosis indicated suspicion of amyloidosis. Right middle lobectomy with lymph node dissection was performed to obtain a definitive diagnosis of the pulmonary nodules. The nodule with fluorodeoxyglucose accumulation was diagnosed as stage IA invasive adenocarcinoma (Fig. 3A). Pathologic examination of the two other nodules in the right lung specimen revealed an anucleate eosinophilic material (Fig. 3B). No malignant cells were present. Direct fast scarlet staining confirmed amyloid deposition (Fig. 3C). Lambda light-chain–predominant amyloidosis was diagnosed (Fig. 3D and E). After systemic evaluation for potential amyloidosis in other organs, the patient was diagnosed to have a stage IA lung adenocarcinoma with tracheobronchial and pulmonary amyloidosis. To the best of our knowledge, this is the first report of co-existing lung cancer and amyloid nodules.
Figure 1.
(A–C) Computed tomography revealed bilateral lung nodules. (D) Positron emission tomography revealed increased fluorodeoxyglucose uptake only in the right middle lobe nodule.
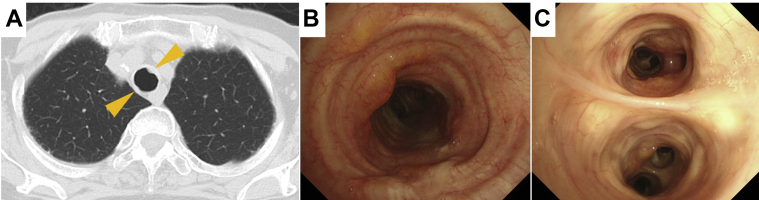
Figure 2.
(A) Computed tomography revealed partial tracheobronchial wall thickening. (B, C) Bronchoscopy revealed polypoid nodules along the tracheobronchial wall.
Figure 3.
Histologic images of the resected right lung. (A) The nodule that revealed fluorodeoxyglucose accumulation was found to be an adenocarcinoma (hematoxylin and eosin stain). The other nodules were found to contain (B) anucleate eosinophilic material (hematoxylin and eosin stain) and (C) amyloid deposition (direct fast scarlet). (D, E) Light-chain staining revealed a lambda light-chain restriction (kappa and lambda stain).
Solitary pulmonary amyloidosis is known to mimic malignancy on chest CT and positron emission tomography imaging.4 The differential diagnoses of these nodules include synchronous primary lung cancer and also extrathoracic malignancies with pulmonary metastases such as breast cancer. In this patient, curative resection of early-stage lung cancer and definitive diagnosis of amyloidosis in other nodules was made possible through surgical biopsy. The remaining nodule in the left lung and the other small lesions were similar in appearance on chest CT. The left nodule may be amyloidosis, and careful follow-up is required. Pathologic confirmation would be needed whether a new lung nodule develops.
Acknowledgments
No author received funds regarding this work.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Baker K.R., Rice L. The amyloidoses: clinical features, diagnosis and treatment. Methodist Debakey Cardiovasc J. 2012;8:3–7. doi: 10.14797/mdcj-8-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Czeyda-Pommersheim F., Hwang M., Chen S.S., Strollo D., Fuhrman C., Bhalla S. Amyloidosis: modern cross-sectional imaging. Radiographics. 2015;35:1381–1392. doi: 10.1148/rg.2015140179. [DOI] [PubMed] [Google Scholar]
- 3.Fisch A.S., Fintelmann F.J., Garcia-Moliner M.L. Systemic amyloidosis mimicking lung cancer. Am J Respir Crit Care Med. 2020;201:107–108. doi: 10.1164/rccm.201812-2261IM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baresic M., Sreter K.B., Brcic L., Hećimović A., Janevski Z., Anić B. Solitary pulmonary amyloidoma mimicking lung cancer on 18F-FDG PET-CT scan in systemic lupus erythematosus patient. Lupus. 2015;24:1546–1551. doi: 10.1177/0961203315591025. [DOI] [PubMed] [Google Scholar]