Abstract
We present a 48-year-old female patient with history of methamphetamine use who developed ataxia, gait difficulty, slurred speech, left Cranial Nerve 7 palsy and mild alteration in mental status. MRI findings suggest that the cause of her newly developed neurological problems is central pontine myelinolysis (CPM).
Keywords: Central pontine myelinolysis, Methamphetamine, Neurological effects of methamphetamines
Highlights
-
•
Based on clinical findings and imaging we propose that our patient developed CPM secondary to methamphetamine use.
-
•
Central pontine myelinolysis is caused by disruption of BBB which results in BBB demyelination of the pons.
-
•
Methamphetamines disrupt the BBB by disrupting tight junctions and destroying the extracellualr matrix.
-
•
Disruption of BBB by methamphetamines resulted in demyelination of the pons in our patient.
1. Introduction
Central pontine myelinolysis (CPM) is a neurological disorder caused by damage to the myelin sheath of brain cells resulting in demyelination of the pons (Hurley et al., 2011; Singh et al., 2014; Lambeck et al., 2019; NINDS, 2019; Khan and Dagur, 2015). The most commonly known cause of CPM is a rapid correction of chronic hyponatremia (development of hyponatremia during more than 48 h). Chronic hyponatremia is a result of conditions that cause nutritional deficiencies and electrolyte imbalances such as alcoholism, cirrhosis, renal failure, cancer, syndrome of inappropriate ADH secretion (SIADH) and liver transplants (Hurley et al., 2011; Singh et al., 2014).
CPM initially presents clinically with delirium, seizures or encephalopathy followed by either a stable or symptomless interval (Hurley et al., 2011; Singh et al., 2014; Lambeck et al., 2019). Afterwards patients experience neurological deterioration with the development of dysarthria, dysphagia weakness or paralysis and gait instability (Hurley et al., 2011; Singh et al., 2014; Lambeck et al., 2019; NINDS, 2019). They also develop neuropsychiatric deficits with impaired cognition, bizarre behaviors and emotional liability (Hurley et al., 2011; Lambeck et al., 2019; NINDS, 2019). CPM can also result in locked-in syndrome or death (Hurley et al., 2011; Singh et al., 2014; NINDS, 2019).
The diagnosis of CPM involves identifying patients with the clinical features and risk factors, followed by confirmation with T2-FLAIR MRI imaging of the brain (Lambeck et al., 2019). The typical MRI findings are hyperdense lesions in the central pons (Singh et al., 2014; Lambeck et al., 2019).
According to the United Nations Office on Drugs and Crime (UNODC), amphetamines account for the most health disorders attributed to drug use, with methamphetamines being the most wildly used type of amphetamines. As of 2016, methamphetamines have been perceived the second largest drug threat with an annual prevalence growing from 0.5% in 2012 to 0.8% in 2015 in individuals between 15 and 64 years old in the United States (United Nations Office on Drugs and Crime, 2017). Methamphetamine is a highly addictive drug, well known for developing tolerance in its abusers (NIDA, 2020). Long term methamphetamine use has been shown to cause drastic structural and functional changes in the brain resulting in deficits in thinking, motor skills, memory, changes in mood, aggressive behavior and psychosis (NIDA, 2020).
1.1. Case
A 48-year-old female with a past medical history of diabetes (DM), hypertension (HTN) and known methamphetamine use presented to the hospital for headache, left facial weakness and repeated falls for the past few days. She was oriented to name, place, time and situation. She had an isolated left CN 7 palsy. Extraocular movements were intact, no gaze preference or palsy. No neglect, no visual field deficit. No hearing loss and no tinnitus. There was mild dysarthria associated with the facial weakness. No aphasia and no dysphagia noted. Motor exam revealed normal tone and bulk, strength was 5/5 in all extremities. Sensation was mildly decreased to light touch, pin prick and temperature on the left side. No proprioceptive loss. On cerebellar exam, there was mild dysmetria and moderate dysdiadochokinesia, but all appeared to be symmetrical. She was having difficulty with balance and gait, requiring minimal to moderate assistance to ambulate.
Vitals during this visit were Tmax of 99 F, BP 163/99 (range 110–189/60–100), HR 74 (range 60–102). Her laboratory findings included HgbA1c of 12.2, chemistry panel showed Na of 138, there was no major fluctuation in Na level throughout the whole hospitalization (ranging 130–138). Hematology was normal. Her toxicology screen was positive for methamphetamine. Patient admitted to chronic and current methamphetamine use. Her cerebral spinal fluid (CSF) analysis showed zero WBC, 20 RBC, protein of 54, glucose of 183. Her multiple sclerosis panel revealed negative oligoclonal band and normal IgG synthesis rate, but the Myelin Basic Protein (MBP) was elevated at 7.88. She had normal copper, ceruloplasmin, B12 levels, TSH, CK and GFR. Her ganglioside antibodies panel was negative. Her imaging during that admission included a head CT and head MRI. She had a negative CT scan. On MRI (Fig. 2), DWI was negative with no evidence of acute ischemia. On FLAIR sequence, we saw symmetrical signal abnormalities affecting both sides of central pons as well as bilateral middle cerebellar peduncle.
Fig. 2.

MRI FLAIR sequence from current admission.
During that admission the patient was treated with steroids and was given a course of IVIG. Patient’s deficits remained the same without significant improvement, she was discharged to rehab unit and eventually went home. She was able to ambulate with a walker.
We are able to see the changes of the demyelination over time due to multiple admissions. Four months prior to that admission she had come in for a headache and malaise, so her imaging included a head MRI, which was negative (Fig. 1). At that time she was found to have a UTI and medical issues only, chart review noted no neurological findings and a toxicology screen positive for methamphetamine. Afterwards she returned to the hospital twice, three months and then eight months later, complaining of fluctuation and subjective worsening of symptoms. Examination did not reveal any new findings and repeat MRIs show no DWI abnormalities. The existing lesion on FLAIR sequence appears to have evolved and became more pronounced, but the extent remained the same (Fig. 3, Fig. 4).
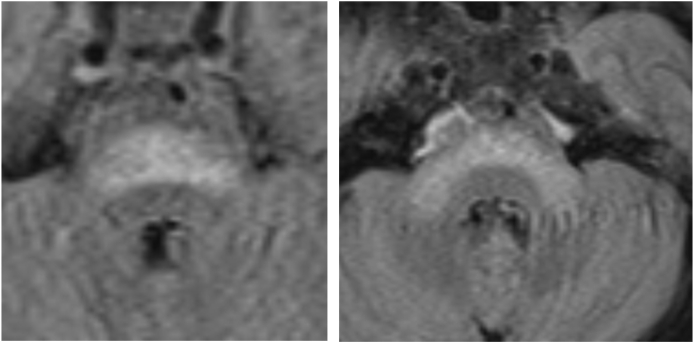
Fig. 1.

MRI FLAIR sequence from 3 months prior to current admission.
Fig. 3.
MRI FLAIR sequence from 3 months after current admission.
Fig. 4.
MRI FLAIR sequence from 8 months after current admission.
2. Discussion
When evaluating the patient some of the things on our differential diagnosis were multiple sclerosis (MS), stroke, vasculitis, CPM, infection, pan-pontine posterior reversible encephalopathy syndrome or a tumor. We have evidence that it was not a preexisting lesion as seen by the first MRI. We can say that it is not MS due to the timeline; the neurological symptoms are not separated by time and space. Also, symptoms were not improved with steroids. The imaging helped us rule out stroke or tumor as DWI-MRI images were negative for stroke and there was no change in size and no enhancement on MRI imaging. A vasculitis is unlikely, since she presented with focal neurological symptoms instead of global neurological symptoms, and steroids and IVIG would have resulted in symptom improvement. The CSF analysis did not support an infectious process.
The main diagnoses left were CPM and pan pontine PRES. Pan pontine PRES, which was described by Liu and Gowan had strong evidence due to the patient’s history of HTN, DM and the hyperdense signaling in the pons seen on MRI (Gowan and Liu, 2019). We know that her diagnosis can not be pan pontine PRES because her symptoms did not resolve. Based on the neurological findings, MRI imaging and an elevated CSF MBP (demonstrating a demyelination episode) we decided on CPM as a diagnosis. Normally for CPM we would have expected a sodium abnormality with a rapid correction or fluctuation, but our patient had a normal sodium level throughout the different visits. The only abnormality that remained consistent in her labs was a positive result for methamphetamines on UDS.
The overall mechanism for the demyelination in CPM is via osmotic stress that results in destruction of oligodendrocytes, the cells responsible for myelination. The most common cause of CPM is rapid correction of chronic hyponatremia. Sodium is the most effective osmole, so changes in sodium concentration cause osmotic stress leading to cellular shrinkage or swelling. When hyponatremia develops over time, as the sodium levels decrease, water travels into glial cells via aquaporins, and there is movement of electrolytes and organic osmoles to keep the osmotic balance between the brain and blood (Hurley et al., 2011; Khan and Dagur, 2015). The rapid correction of hyponatremia results in loss of electrolytes and organic osmoles from the extra cellular space, a swift movement of water out of glial cells causing glial cell dehydration and osmotic shrinkage (Hurley et al., 2011; Khan and Dagur, 2015). The osmotic cell shrinkage pulls apart the tight junctions from endothelial vascular cells, opening the blood brain barrier (Hurley et al., 2011; Khan and Dagur, 2015). With the opening of the blood brain barrier endothelial vascular cells release a plethora of substances such as compliment protease, cytokines, plasminogen activator, immunoglobulins and neural proteases that destroy the newly exposed oligodendrocytes (Hurley et al., 2011; Khan and Dagur, 2015). The degeneration of oligodendrocytes results in the destruction of myelin (Hurley et al., 2011; Khan and Dagur, 2015).
Methamphetamines are well known to cause structural changes in the brain, they affect dopamine pathways and increase the number of microglial cells (NIDA, 2020). Due to the different well known ways methamphetamines change the brain, we propose that in our patient, methamphetamine use caused CPM via BBB disruption, which ultimately could have resulted in myelin destruction. There have been multiple studies that have shown that methamphetamine use disrupts the BBB as evidenced by IgG extravasion and Evans Blue leakage (O’Shea et al., 2014, Urrutia et al., 2013). O’Shea and colleagues propose that BBB destruction secondary to methamphetamine exposure can be attributed to the breakdown of extra cellular matrix (ECM) proteins and tight junction disassembly which results in the increased permeability of the BBB. In methamphetamine-injected mice there is an increase in metalloproteinase-9, a protein that degrades components of the extra cellular matrix (ECM) such as laminin which results in an increase of BBB permeability O’Shea et al., 2014, Urrutia et al., 2013. Muneer and colleagues, during in vitro studies with human brain endothelial cells, show that exposure to methamphetamines decreases glucose transport protein-1 (GLUT-1) expression which leads to decreased glucose uptake and energy-associated destruction of tight junction assembly (Muneer, 2011). Regardless of cause, BBB destruction leads to the release of substances that ultimately sets the stage for brain cell destruction that can lead to the degeneration of oligodendrocytes and demyelination.
3. Conclusion
In conclusion, our patient presented with a clinical picture that matches CPM, MRI images show hyperdense signaling on the pons which is diagnostic for CPM and CSF MBP levels support a demylination process. Thoughout her different hospitalizations the only recurrent lab abnormality was a positive UDS for methamphetamines, making methamphetamine use the cause for the development of CPM. CPM develops as a result of demyelination and demylination is the end result of the disruption of the BBB. In the typical etiology of CPM its osmotic stress due to rapid correction of hyponatremia that destroys the BBB. Methamphetamines have been reported to cause the disruption of the BBB due to the disruption of ECM proteins or tight junctions which could have caused demylination in our patient’s pons.
Acknowledgements
Published with written consent of the patent.
References
- Gowan J.M., Liu A. Isolated pan-pontine posterior reversible encephalopathy syndrome in a patient with uncontrolled hypertension. Clin Case Rep. 2019;7:32–36. doi: 10.1002/ccr3.1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley R.A., Filley C.M., Taber K.H. Central pontine myelinolysis: a metabolic disorder of myelin. J. Neuropsychiatry Clin. Neurosci. 2011;23(4):369–374. doi: 10.1176/jnp.23.4.jnp369. [DOI] [PubMed] [Google Scholar]
- Khan S.A., Dagur G. Current concepts in pontine myelinolysis: review of literature. Transl. Biomed. 2015;6:4. doi: 10.21767/2172-0479.100038. [DOI] [Google Scholar]
- Lambeck J., Hieber M., Dreßing A., Niesen W.D. Central pontine myelinosis and osmotic demyelination syndrome. Dtsch Arztebl Int. 2019;116:600–606. doi: 10.3238/arztebl.2019.0600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muneer Abdul. Impairment of brain endothelial glucose transporter by methamphetamine causes blood-brain barrier dysfunction. Molecular Neurodegeneration. 2011;6(23) doi: 10.1186/1750-1326-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIDA What are the long-term effects of methamphetamine misuse? National Institute on Drug Abuse. 3 Jun. 2020 https://www.drugabuse.gov/publications/research-reports/methamphetamine/what-are-long-term-effects-methamphetamine-misuse [Google Scholar]
- NINDS . 2019. Central Pontine Myelinolysis Information Page. National Institute on Neurological Disorders and Stroke.https://www.ninds.nih.gov/Disorders/All-Disorders/Central-Pontine-Myelinolysis-Information- [Google Scholar]
- O’Shea E., Urrutia A., Green A.R., Colado M.I. Current preclinical studies on neuroinflammation and changes in blood brain barrier integrity by MDMA and methamphetamine. Neuropharmacology. 2014;78:125–134. doi: 10.1016/j.neuropharm.2014.02.015. [DOI] [PubMed] [Google Scholar]
- Singh T.D., Fugate J.E., Rabinstein A.A. Central pontine and extrapontine myelinolysis: a systematic review. Eur. J. Neurol. 2014;21:1443–1450. doi: 10.1111/ene.12571. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime, reportWorld Drug Report 2017 (ISBN: 978-92-1-148291-1, eISBN: 978-92-1-060623-3, United Nations publication, Sales No. E.17.XI.6).
- Urrutia A., Rubio-Araiz A., Gutierrez-Lopez M.D., ElAli A., Herman D.M., O’Shea E., Colado M.I. A study on the effect of JNK inhibitor, SP600125, on the disruption of blood–brain barrier induced by methamphetamine. Neurobiol. Dis. 2013;50:49–58. doi: 10.1016/j.nbd.2012.10.006. https://0-doi-org.catalog.llu.edu/10.1016/j.nbd.2012.10.006 [DOI] [PubMed] [Google Scholar]