Abstract
Objective
This study aims to investigate the utilization of acute ischemic stroke (AIS) services during the Corona Virus Disease 2019 (COVID-19) pandemic. Based on early observations among healthcare utilization on stroke and other healthcare services, we hypothesized that there would be a persistent significant decline in AIS patients presenting to hospitals as the pandemic has progressed for over a year.
Method
TriNetX, a large research network, is used to collect real-time electronic medical data. Data on utilization of acute ischemic stroke service was collected for the years 2018, 2019, and 2020 for variables including overall stroke volume and the number of patients that received intravenous tissue plasminogen activator (tPA) and mechanical thrombectomy (MT).
Result
We found a 13.2–15.4% decrease in total number of AIS patients in 2020 (n 77231) compared with the years 2018 and 2019 (n 88948 and 91270 respectively, p < 0.001). In the year 2020 Stroke volume was significantly lower in Q4 comparing to Q1 (Q1 vs Q4, p < 0.01, while there were no significant differences in stroke volume between Quarters 2, 3, and 4 in 2020 (Q2 vs Q3, p = 0.39, Q2 vs Q4, p = 0.61, Q3 vs Q4, p = 0.18). The Proportion of patients receiving tPA in 2020 was significantly lower compared to prior years (5.4% in 2020 vs 6.4% in 2018 and 6.0% in 2019, p < 0.01), however, the proportion of patients receiving MT was significantly higher in 2020 than in 2018 (0.024 vs 0.022, p < 0.01).
Conclusion
Despite significant alteration in practices to optimize healthcare delivery and mitigate the collateral impact of the pandemic on care for other conditions, a persistent decline in AIS volumes remains. Delayed presentation, fear-of-contagion, reallocation, and poor availability of health care resources are potential contributors. Prospective evaluation and further investigation for these trends is needed.
Keywords: COVID-19, Acute ischemic stroke, Healthcare utilization, Tissue plasminogen activator (tPA), Mechanical thrombectomy (MT)
1. Introduction
Corona Virus Disease 2019 (COVID-19) emerged in China in December 2019 and rapidly caused a global health pandemic. Currently, there are more than 32 million confirmed COVID-19 cases in the United States (Trends in Number ofD, 2021). The management of pandemic is an international priority as it overburdens hospital resources and requires drastic changes in the allocation of resources. Delivery of acute ischemic stroke (AIS) care was affected by the pandemic as noted by several prior observational studies conducted in the initial phase of this pandemic (Baracchini et al., 2020; Onteddu et al., 2020; Wira et al., 2020; Nogueira et al., 2021). On the other hand, neurological diseases, in particular ischemic strokes have been increasingly reported since the onset of COVID-19 infection potentially secondary to prothrombotic state (Onteddu et al., 2020; Elkhider et al., 2020). Hospitals have evolved practices to limit the collateral impact of pandemic on various disease-states. There is limited updated literature on healthcare utilization among AIS patients as the pandemic has progressed. We hypothesized that there would be a persistent profound decline in AIS patients presenting to hospitals even after one year into the pandemic.
2. Methods
2.1. Data source
We retrospectively collected data using de-identified patient information extracted from the TriNetX database. TriNetX is a global collaborative clinical research platform utilizing electronic medical record (EMR) data longitudinally and retrospectively in a real-time fashion from a network of health care organizations (HCO) in the U.S and U.S territories. The TriNetX platform is described in detail elsewhere, and several similar studies on COVID-19 using TriNetX have been published to date (Shah et al., 2020; Turk et al., 2020; Taquet et al., 2021; Nalleballe et al., 2020; Kovvuru et al., 2021). Arkansas Clinical Data Repository (AR-CDR) at the University of Arkansas for Medical Sciences manages TriNetX.
2.2. Analytic methods
Two physicians using TriNetX performed cross-sectional analysis independently. Using the ICD-10 code for ischemic stroke (I63), we identified AIS patients who presented between January and December 2020. Employing identical criteria, two comparison cohorts were identified for the years 2018 and 2019. Total number of adult patients (>18 years) with AIS, as well as the number of patients that received intravenous tissue plasminogen activator (tPA) and mechanical thrombectomy (MT) were extracted for each month in these three cohorts. Proportion of patients receiving tPA and MT relative to total number of AIS patients were then calculated. To better visualize the trends, cohort for each year was divided into four groups based on the quarter of presentation (Quarter 1, Jan–Mar; Quarter 2, Apr–Jun; Quarter 3 July–Sep; and Quarter 4 Oct–Dec). Between yearly-cohorts and between quarterly-groups comparisons were then drawn for the total number of AIS patients, proportion of patients receiving tPA, and proportion of patients undergoing MT patients, using a general linear model (SAS University Studio version 9). An alpha of ≤0.01 was considered statistically significant.
3. Results
3.1. Total stroke volume
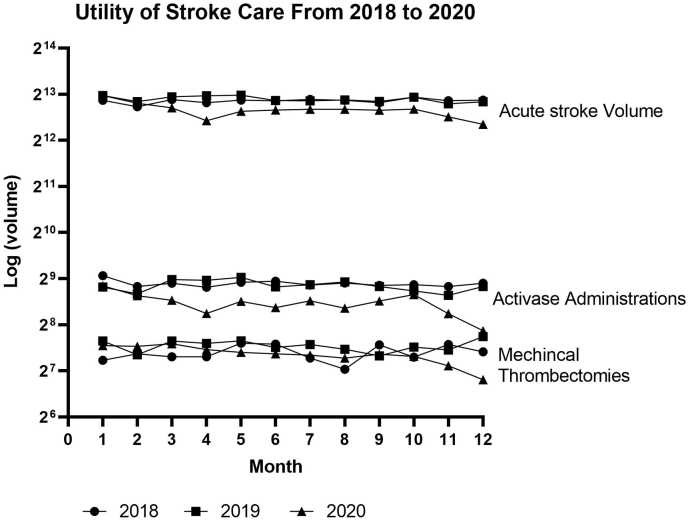
Total stroke volumes in 2018 and 2019 were 88948 and 91270 respectively, while there were only 77231 AIS cases in 2020. This constituted a 13.2–15.4% decrease in total number of AIS patients in 2020 compared to the years 2018 and 2019 (p < 0.001). Further analysis demonstrated that for the year 2020, total stroke volume for Q4 was significantly lower than Q1 (Q4 vs Q1, p = 0.01); however, there was no significant difference between the total stroke volumes for Q2, Q3, and Q4. ((Q2 vs Q3, p = 0.39, Q2 vs Q4, p = 0.61, Q3 vs Q4, p = 0.18) see details in Fig. 1 and Table 1).
Fig. 1.
Total number of AIS patients, number of patients receiving tPA, and number of patients undergoing mechanical Thrombectomy for each month of the years 2018, 2019, and 2020 in US hospitals.
Table 1.
Stroke volume, tPA ratio and MT ratio in quarters from 2018 to 2020.
| Stroke volume | tPA ratio | MT ratio | |
|---|---|---|---|
| 2018 Q1 | 21832 | 6.72% | 2.1% |
| 2018 Q2 | 22110 | 6.51% | 2.4% |
| 2018 Q3 | 22241 | 6.3% | 2.1% |
| 2018 Q4 | 22765 | 6.14% | 2.3% |
| 2019 Q1 | 23242 | 5.9% | 2.4% |
| 2019 Q2 | 23529 | 6.2% | 2.5% |
| 2019 Q3 | 22689 | 6.2% | 2.3% |
| 2019 Q4 | 22223 | 5.7% | 2.6% |
| 2020 Q1 | 21857b | 5.6%e | 2.6% |
| 2020 Q2 | 18292b | 5.4%e | 2.9% |
| 2020 Q3 | 19503b | 5.4%e | 2.5% |
| 2020 Q4 | 17579b | 5.3%e | 2.3% |
| 2018 total | 88948a | 6.4%c | 2.3%d |
| 2019 total | 91270a | 6.0%c | 2.5% |
| 2020 total | 77231a | 5.5%c | 2.4%d |
Stroke volume in 2020 decreases significantly comparing volumes in 2018 and 2019.
Stroke volume decreased in Q2, Q3, Q4 compared with Q1, but no significant difference between Q2, Q3, and Q4 in 2020.
The proportion of patients receiving tPA was significantly lower in 2020 compared to prior years (p < 0.0001) (p < 0.01).
The proportion of thrombectomy was significantly higher in 2020 than in 2018 (0.024 vs 0.022, p < 0.01.
No difference in tPA r0061tio between Q1, Q2, Q3 and Q4 in 2020.
3.2. Proportion of AIS patients’ receiving tPA (tPA ratio)
The tPA ratio showed a gradual decrease over time (2018, 6.4%; 2019, 6.0%; and 2020 5.4%. Reduction in tPA ratio for the year 2020 was statistically significant when compared to prior years (p < 0.01). For the year 2020, there was no significant difference in tPA ratio amongst Q1, Q2, Q3, and Q4 (p > 0.05) (see details in Table 1).
3.3. Proportion of AIS patients’ receiving mechanical thrombectomy (MT ratio)
The proportion of AIS patients’ receiving MT in 2020 was significantly higher for the year 2020, compared with 2018 (0.025 vs 0.022, p < 0.01). No significant difference was noticed in the MT ratio between 2020 and 2019 (p = 0.07). For the year 2020, no statistical significant difference between quarterly MT ratio was found between quarters. (Q1 vs Q2, p = 0.3, Q1 vs Q3, p = 0.5, Q1 vs Q4, p = 0.18, Q2 vs Q3, p = 0.11, Q2 vs Q4, p = 0.18, Q3 vs Q4, p = 0.45. (see details in Table 1)).
4. Discussion
Reduction in the utilization of medical care among AIS patients during the first wave of COVID-19 pandemic has been previously reported 3. Although re-allocation of healthcare resources is believed to modify the impact of this pandemic on utilization of essential clinical services, our study showed a persistent significant reduction (13.2–15.4%) in AIS volumes in 2020 compared with previous years 2018 and 2019. Within year 2020 also, stroke volumes in Q2 and Q4 were significantly lower than Q1 – this quarterly reduction in AIS volumes appears to be persistent and somewhat stable given no significant differences were noticed amongst Q2, Q3, and Q4 of 2020. Precise reasons for this persistent declining trend remain unknown, however, an under-utilization of healthcare services rather than a reduction in the incidence of AIS is considered more plausible (Zhao et al., 2020; Shah et al., 2021).
Another important finding of this work is a reduction in AIS patients qualifying for thrombolysis, which may be related to delayed presentation. Conversely, compared with earlier years, we noted a slight increase in the proportion of patients receiving MT during 2020. This could possibly be related to a more severe presentation of AIS secondary to large vessel occlusions and the extended time window available for intervention. These hypotheses need further confirmation in prospective studies.
As the COVID-19 pandemic continues, “at-home” telemedicine services have become more popular and widely available. However, care for medical emergencies such as AIS cannot be replaced by these telemedicine services. Despite significant alteration in inpatient practices to optimize healthcare delivery (Zhao et al., 2020; Shah et al., 2021) and mitigate the collateral impact of the pandemic on care for other conditions, the decline in AIS volumes remains. This may be due to fear-of-contagion, reallocation, and poor availability of health care resources.
5. Conclusion
There has been a significant and persistent reduction in hospitalization and utilization of acute ischemic stroke services throughout the COVID-19 pandemic in the U.S. Innovative solutions along with public education will play a vital role in reducing morbidity and mortality due to AIS.
5.1. Limitations
There are several limitations in our study, including: retrospective nature, reporting bias associated with ICD-10 codes, and the regional heterogeneity in the COVID-19 pandemic and public stroke education.
Declaration of competing interest
Sen Sheng, on behalf of all authors, has no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work.
References
- Baracchini C., Pieroni A., Viaro F. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol. Sci. 2020;41(5):1003–1005. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkhider H., Ibrahim F., Sharma R. COVID-19 and stroke, a case series and review of literature. Brain Behav Immun Health. 2020;9 doi: 10.1016/j.bbih.2020.100172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovvuru S., Nalleballe K., Onteddu S.R. Immunosuppression in chronic autoimmune neurological disorders during the COVID-19 pandemic. J. Neurol. Sci. 2021;420 doi: 10.1016/j.jns.2020.117230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalleballe K., Reddy Onteddu S., Sharma R. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav. Immun. 2020;88:71–74. doi: 10.1016/j.bbi.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogueira R.G., Qureshi M.M., Abdalkader M. Global impact of COVID-19 on stroke care and intravenous thrombolysis. Neurology. 2021;10:1212. doi: 10.1212/WNL.0000000000011885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onteddu S.R., Nalleballe K., Sharma R., Brown A.T. Underutilization of health care for strokes during the COVID-19 outbreak. Int. J. Stroke. 2020;15(5):NP9–NP10. doi: 10.1177/1747493020934362. [DOI] [PubMed] [Google Scholar]
- Shah V.A., Nalleballe K., Zaghlouleh M.E., Onteddu S. Acute encephalopathy is associated with worse outcomes in COVID-19 patients. Brain Behav Immun Health. 2020;8 doi: 10.1016/j.bbih.2020.100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah V.A., Nalleballe K., Onteddu S.R. Critically ill neurologic patients during the COVID-19 pandemic: a short communication. Brain Behav Immun Health. 2021;12 doi: 10.1016/j.bbih.2021.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trends in number of COVID-19 cases and deaths in the US reported to CDC. https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases by State/Territory. 2021 May 3rd.
- Turk M.A., Landes S.D., Formica M.K., Goss K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disabil Health J. 2020;13(3) doi: 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wira C.R., Goyal M., Southerland A.M. Pandemic guidance for stroke centers aiding COVID-19 treatment teams. Stroke. 2020;51(8):2587–2592. doi: 10.1161/STROKEAHA.120.030749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Li H., Kung D., Fisher M., Shen Y., Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]