Abstract
Despite marriage's health benefits, all couples experience stress that can increase morbidity and mortality risks. Marital stress can alter endocrine, cardiovascular, and immune function—key pathways from troubled relationships to poor health. This review discusses how partners “get under each other's skin” to influence psychological, behavioral, and biological health. Then, I offer a comprehensive Dyadic Biobehavioral Stress Model to build on this foundational work and inspire transdisciplinary research integrating psychoneuroimmunological and relational lenses. This conceptual and empirically driven model provides promising new directions to investigate mechanisms linking individuals' relationships behaviors to their own and their partners' health, with particular emphasis on biological pathways. These mechanisms may impact each partner's physical health outcomes, such as disease development, illness severity, and accelerated biological aging. Risk and protective factors across developmental stages and diverse contexts are also discussed to help explain how, and under what conditions, partners influence each other's health. Research applying this model can push the boundaries of our current understanding on dyadic stress its far-reaching health effects on self-report and biological markers across the lifespan.
Keywords: Dyadic coping, Inflammation, Interdependence, Marriage, Psychoneuroimmunology, Stress reactivity
Highlights
-
•
Marital stress can alter morbidity and mortality risks.
-
•
This review discusses how partners “get under the skin” to influence health.
-
•
The Dyadic Biobehavioral Stress Model connects stress to each partner’s health.
-
•
Risk and protective factors across developmental and diverse contexts are discussed.
-
•
This model shows dyadic effects on psychological, behavioral, and biological health.
1. Introduction
Married people live longer, healthier lives than those who are unmarried, divorced, or widowed (Kiecolt-Glaser and Newton, 2001; Robles et al., 2014). Marriage's health impact is similar to if not greater than that of well-known factors, such as how often people exercise, drink alcohol, and smoke cigarettes (Holt-Lunstad et al., 2010, 2017). Despite these health benefits, all couples, even happy couples, experience stress that can increase morbidity and mortality risks. Some couples navigate life's inevitable ups and downs, while stress takes a toll on other couples' health. Indeed, marital stress can alter endocrine, cardiovascular, and immune function—key pathways from troubled relationships to poor health (Pietromonaco and Collins, 2017a; Kiecolt-Glaser and Lovesick, 2017). Accordingly, the way couples manage stress—rather than the stress itself—may confer health risks or benefits across the lifespan (Kiecolt-Glaser and Lovesick, 2017).
Researchers across fields—including but not limited to psychoneuroimmunology (PNI), family studies, psychology, and public health—have contributed to a growing literature on marriage's health impact. Yet, work is still uncovering exactly how partners influence each other's health, particularly during stress. Why do some couples become closer and healthier through hardship, while others experience relationship conflict and health problems? Research using individual, dyadic, and biobehavioral stress perspectives have helped address this question and identify pathways through which relationships improve or impair health, from momentary physiological stress responses to clinical disease outcomes (Kiecolt-Glaser et al., 2020; Shrout, 2019; Shrout et al., 2020a). This review will first discuss connections between close relationships and health more broadly, and then identify key findings linking stress to health in romantic relationships. Then, I offer a comprehensive Dyadic Biobehavioral Stress Model that illustrates how partners shape one another's health through psychological, behavioral, and biological pathways (Fig. 1).
Fig. 1.

M. Rosie Shrout, PhD. Dr. Shrout is an Assistant Professor in Purdue University's Human Development and Family Studies Department, as well as a Faculty Associate of Purdue University's Center on Aging and the Life Course. She earned her PhD in Interdisciplinary Social Psychology from the University of Nevada, Reno in 2019 where she worked with Dr. Daniel Weigel. Then she received a Presidential Postdoctoral Fellowship with Dr. Janice Kiecolt-Glaser in the Ohio State University's Institute for Behavioral Medicine Research. As a social-health psychologist with specialized training in psychoneuroimmunology, Dr. Shrout studies how couples' stress affects their relationships and health using dyadic, biobehavioral, and longitudinal methods. Her work focuses on the underlying psychological, behavioral, and biological pathways connecting stress to people's own and their partners' relational and physical health across adulthood. Though relationships often provide health benefits, all couples experience stress that poses risks to partners' relationship quality, emotional and physical well-being, and longevity. Through transdisciplinary and collaborative work, Dr. Shrout's research addresses why some couples grow stronger and healthier through hardship, while others experience relationship and health problems. With an emphasis on three common and yet challenging stressors—infidelity, conflict, and chronic illness—she considers how sociodemographic and developmental-contextual factors affect how people perceive stress, use their resources, and experience relationship and health problems. Dr. Shrout's goal is to identify factors that put couples' relationships and health at risk and to inform interventions on how couples can grow closer and stronger during turbulent times. Dr. Shrout has received several grants, fellowships, and awards supporting her research. Most notable among these honors include a prestigious Bilinski Dissertation Fellowship, the University of Nevada, Reno's most Outstanding Graduate Student Researcher, and Ohio State University's Presidential Postdoctoral Fellowship.
2. Close relationships and health
Marriage's potent health effects have inspired calls for treating relationships as a public health priority of equal importance to lifestyle factors (Holt-Lunstad et al., 2017; Smith, 2019). Indeed, mounting evidence suggests that the quality and quantity of close relationships more broadly are linked to all-cause mortality and disease development and severity (Holt-Lunstad et al., 2010, 2017). For example, individuals with greater social support have better cardiovascular, neuroendocrine, and immune function than less supported individuals, decreasing disease risks and promoting long-term health (Uchino, 2006). However, these health benefits often come with a tradeoff because social stress carries greater health threats than general stress (Cohen, 2004; Shields et al., 2020). Several studies have shown individuals who experienced laboratory social stressors or reported frequent interpersonal stress had greater depressive symptoms, cortisol responses, and inflammatory reactivity than those who experienced general, non-interpersonal laboratory stressors or reported non-interpersonal stress (Cohen, 2004; Madison et al., et al.; Dickerson et al., 2008; Slavich and Irwin, 2014).
Romantic relationships in particular carry strong health consequences (Graham et al., 2006, 2007). For example, happily married spouses had better psychological, cardiovascular, and immune health than their unhappily married, divorced, or single counterparts (Graham et al., 2007; Holt-Lunstad et al., 2008). Though single individuals fared better than those in unhappy marriages, having a supportive network of family and friends did not improve their health (Holt-Lunstad et al., 2008). These results suggest that romantic relationships provide both health benefits and risks that are unique and distinct from other close relationships. Moreover, these findings fit within the broader literature illustrating that romantic partners are typically a person's closest and most central relationship (Pietromonaco and Collins, 2017b). Partners provide support, security, intimacy, and a sense of belongingness—fundamental needs for emotional and physical health, particularly during stress (Pietromonaco and Overall, 2020).
3. Health consequence of stress in couples: Actor effects
Research has been shifting toward a dyadic stress lens to demonstrate how stress affects each couple member. Stress is dyadic when the situation or event concerns both partners (Bodenmann, 2005). For example, an internal dyadic stressor like relationship conflict directly affects each partner, whereas an external dyadic stressor like job loss typically occurs to one partner and can spill over into the relationship and affect the other partner (Bodenmann, 2005). Statistical modeling advancements, such as the Actor-Partner Interdependence Model, have allowed researchers to examine dyadic stress and how partners influence one another. APIMs includes cross-partner effects that can estimate how people's stress relate to their own outcomes (“actor” effects) and to their partners' outcomes (“partner” effects) (Kenny et al., 2006). The actor effects have been most extensively examined; accordingly, this paper will first review key findings connecting people's relationship experiences to their own health.
3.1. Psychological and subjective health pathways
Relationships have been linked to self-reported psychological and subjective health across several stressors (Choi and Marks, 2008; Umberson et al., 2006; Wright and Loving, 2011). These links are important because subjective health—the self-reported evaluation of one's overall health (Monden and Michalos, 2014)—is a robust predictor of objective health indicators like morbidity and mortality (Idler, Benyamini; Jylhä, 2009). A stressor that nearly all partners experience is conflict, which can be detrimental to their health and relationships if navigated poorly. Conflict has been associated with heightened depressive and anxiety symptoms, poorer subjective health, and increased functional impairment cross-sectionally and over time (Wright and Loving, 2011; Loving and Slatcher, 2013). Using longitudinal data from a diverse sample of Black and White American couples over the first 16 years of marriage, my colleagues and I showed conflict impacted wives' and husbands' subjective health in different ways (Shrout et al., 2019). Husbands had worse subjective health in the years the couples argued more often than usual, whereas disagreeing about several topics over 16 years predicted wives' poorer health. Our work has also shown individuals with greater depressive symptoms blamed themselves more for their relationship conflict and experienced greater relationship disillusionment than those with fewer depressive symptoms (Weigel and Shrout, 2020a). Depressed individuals may therefore see conflict as more damaging, a potential pathway to poor health.
Relationships become even more important when managing a serious illness like breast cancer—a group with increased morbidity and mortality risks. Breast cancer survivors whose psychological and physical symptoms remain elevated after completing treatment are more likely to experience chronic inflammation and inflammaging, or biological aging of the immune system (Ferrucci and Fabbri, 2018; Aggarwal et al., 2006). Previous work has shown spouses can help navigate a cancer diagnosis and treatment, reducing stress and promoting health (Kayser et al., 2007; Kayser and Scott, 2008). My colleagues and I extended these findings and showed married survivors—both those in satisfying and dissatisfying marriages—experienced improvements in their stress, depressive symptoms, and fatigue after treatment, with satisfied survivors reporting greater improvements (Shrout et al., 2021). In contrast, unmarried survivors’ stress, depressive symptoms, and fatigue remained elevated years after treatment ended. Although marriage was associated with improved health, the gains were most notable when their marriages were satisfying.
3.2. Behavioral pathways
Though less studied than psychological mechanisms, relationships have important implications for behavioral health. Partners inherently influence each other's health behaviors, such as sleep, exercise, diet, substance use, and health care utilization, each of which is tied to disease development, longevity, and quality of life (Pietromonaco et al., 2013). For example, my colleagues and I have shown that poor emotional and psychological health following a partner's infidelity was linked to increased risky behaviors like drug and alcohol use (Shrout and Weigel, 2018). Moreover, the mere suspicion of a partner's infidelity was associated with poorer psychological, physical, and behavioral health (Weigel and Shrout, 2020b). In other work, a daily study showed wives slept better on days they talked openly with their spouses (Kane et al., 2014). Additionally, middle-aged and older adults were more likely to exercise, smoke less, and lose weight if their partners did the same (Jackson et al., 2015). Couples' heath behaviors also become more similar over time, altering health risks as people age (Kiecolt-Glaser and Lovesick, 2017).
3.3. Biological pathways
3.3.1. Endocrine function
Dyadic stress can alter the hypothalamic-pituitary-adrenal axis and its end-product, cortisol (Gunnar and Vazquez, 2001). Although cortisol secretion is a key part of the body's stress response, dysregulated diurnal rhythms like blunted peaks and flattened slopes affect autonomic, immune, and metabolic systems, posing additional health threats (Adam et al., 2017; Kumari et al., 2009, 2011). Indeed, flatter cortisol slopes have been linked to atherosclerosis (Hajat et al., 2013) and Type II diabetes (Hackett et al., 2014).
Laboratory research has shown partners who used more negative and less positive behaviors during conflict, such as criticizing each other or withdrawing from the conversation, had higher cortisol levels than their less negative and more positive counterparts (Shrout et al., 2020a). In another study, wives had higher cortisol, adrenocorticotropic hormone, and norepinephrine levels when their negative behaviors escalated during conflict, amplifying immune risks (Glaser and Kiecolt-Glaser, 2005; Kiecolt-Glaser et al., 1997). Positive relationship interactions can also promote healthier cortisol patterns. A daily study showed on days partners reported more physical intimacy, such as hugging and holding hands, they also reported greater positive affect and, in turn, had lower cortisol secretion (Ditzen et al., 2008). A longitudinal study found that feeling cared for and understood by a partner was associated with lower negative affect, which in turn was linked to healthier diurnal cortisol profiles 10 years later (Slatcher et al., 2015). Those who felt less cared for and understood over time, however, were more reactive emotionally to daily stressors and reported poorer well-being, contributing to higher mortality rates another 10 years later (Stanton et al., 2019; Selcuk et al., 2016).
3.3.2. Cardiovascular function
Relationship stress is also connected to the autonomic nervous system and particularly heart rate variability (HRV). Higher HRV generally indicates greater cardiac flexibility and that the body's sympathetic and parasympathetic systems are balanced (Kim et al., 2018). However, chronic stress can interfere with the body's ability to keep these systems balanced, leading to low HRV that affects multiple regulatory systems. For example, low HRV is a marker of cardiovascular risk and is associated with heightened inflammation (Frasure-Smith et al., 2009). HRV is particularly important among older adults because it decreases with age, posing additional age-related health consequences (Antelmi et al., 2004).
Cross-sectional and longitudinal research over 10 years showed individuals in higher quality and more satisfying relationships had higher resting HRV than those in lower quality and less satisfying relationships (Smith et al., 2011; Donoho et al., 2015); increases in marital strain, however, predicted lower HRV 10 years later. Marital conflict has also been linked to other cardiovascular reactivity and disease markers. More hostile partners had greater blood pressure and heart rate reactivity during conflict than their less hostile counterparts (Robles et al., 2014; Robles and Kiecolt-Glaser, 2003). In another conflict study, hostile partners had greater coronary artery calcification than those who were less hostile (Smith et al., 2009). Daily studies showed more frequent positive relationship interactions were associated with lower carotid artery intima-medial thickness (Joseph et al., 2014); in contrast, more frequent negative relationship interactions were linked to greater cardiovascular risk.
3.3.3. Immune function
Troubled marriages pose proinflammatory threats that underlie cardiovascular disease, arthritis, diabetes, and cancer (Kiecolt-Glaser et al., 2010; Michaud et al., 2013; Kiecolt-Glaser, 2018). These associations become even stronger across the lifespan because age-related immune system weakening can heighten inflammatory responses (Ferrucci and Fabbri, 2018). This physiological cascade can lead to changes in health status and biological aging, suggesting that inflammation is an important biological marker underlying morbidity and mortality.
Individuals in more satisfying relationships showed better immune and antibody responses to vaccination compared to those in dissatisfying relationships (Phillips et al., 2006). Likewise, partners who were more hostile during support and conflict discussions showed slower wound healing and higher inflammation than their less hostile counterparts (Kiecolt-Glaser et al., 2005). Partners who were more engaged during the discussions had lower inflammation the next day (Graham et al., 2009). Longitudinal research showed less distressed and satisfied partners had better cellular immune function than those in more distressing and dissatisfying relationships two years later (Jaremka et al., 2013). My research on breast cancer survivors—a group with particularly elevated immune risks—showed when survivors were more satisfied with their relationships than usual, their own stress and, in turn, inflammation were lower than usual (Shrout et al., 2020b). These findings provide mechanistic evidence that relationships can impact health through several biological pathways.
4. Health consequence of stress in couples: Partner effects
The field has begun to examine both actor and partner effects to understand marriage's health impact and the health consequences of stress. These actor and partner effects stem from interdependence theory, which suggests partners mutually influence each other's outcomes (Kelley and Thibaut, 1978). Key, albeit limited, data provide promising evidence that people's stress is linked to their own and their partners' health and well-being across self-report and biological health markers.
4.1. Psychological and behavioral pathways
Partner effects have been more widely examined on psychological and behavioral health than on biological health, particularly among couples with chronic illness (Berg and Upchurch, 2007). My research conceptualized and tested an integrated model of dyadic coping using interdependence theory and an actor-partner lens (Shrout, 2019). When individuals with chronic illnesses saw the illness as more shared—meaning they could work together to manage the illness—their partners were more likely to talk openly and honestly about the illness. Likewise, when one partner saw their relationship as stronger and more resilient, the other partner was more likely to feel comfortable talking about the illness. These findings show how seeing stress as dyadic, or shared, can promote adaptive coping among both partners.
4.2. Biological pathways
4.2.1. Endocrine function
Extending these self-report findings to the biological level, my colleagues and I integrated dyadic and biobehavioral stress perspectives showing how a partner's stress can alter a person's own cortisol on a day the couple experienced conflict (Shrout et al., 2020a). At the beginning of the day, cortisol levels were similar regardless of a partner's stress, but differences emerged after the conflict. Spouses with stressed partners had slower, less healthy cortisol declines across the day and even 4 h after the conflict than those with less stressed partners. Also, spouses' average cortisol that day was higher when they argued with a stressed partner and used more negative behaviors during the conflict. In contrast, couples who used positive behaviors had similar average cortisol levels regardless of their partners' stress. These findings suggest couples' relationship-promoting behaviors helped protect people from their partners' higher stress.
4.2.2. Cardiovascular and immune function
Additional work has focused on links between partners' stress, cardiovascular, and immune health. A study on middle age and older couples showed husbands had higher blood pressure when their wives reported greater stress (Birditt et al., 2016). Husbands' and wives' blood pressure also was higher when both couple members rated their relationships as lower quality compared to those in higher quality relationships. A growing literature has also examined synchrony and coregulation in their physiological stress levels and reactivity. For instance, couples' moment-to-moment HRV synchronized across a series of laboratory tasks (Helm et al., 2012, 2014) and during conflict (Wilson et al., 2018), which predicted greater negative affect reactivity and higher inflammation. Adding the actor-partner effects, people's HRV at one occasion predicted their own and their partners' HRV at the next occasion, and this effect was stronger for those in highly satisfying relationships (Helm et al., 2014); accordingly, a partner's HRV was more strongly associated with a person's own subsequent HRV when that person was highly satisfied. These findings show how partners' physiological stress responses rise and fall together and mutually influence one another over time (Butler and Randall, 2013). These studies provide initial evidence that a partner can heighten or dampen a person's own physiological and biological stress response, altering both partners' health consequences.
5. Actor and Partner effects: A comprehensive Dyadic Biobehavioral Stress Model
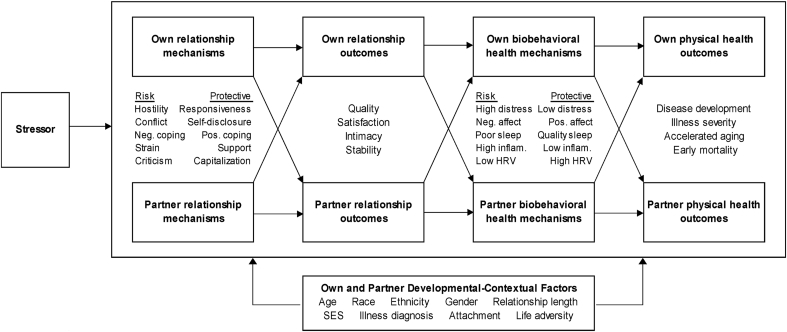
Individual, dyadic, and biobehavioral stress perspectives show how relationships impact partners' health (Kiecolt-Glaser et al., 2020; Berg and Upchurch, 2007; Slatcher, 2010; Farrell and Simpson, 2017). A unifying theory capturing partners' interdependent nature could help explain how partners influence their own and each other's health across several stressful contexts. Accordingly, the comprehensive Dyadic Biobehavioral Stress Model identifies the underlying psychological, behavioral, and biological health mechanisms connecting stress to people's own and their partners' health (see Fig. 2).
Fig. 2.
An illustration of the Dyadic Biobehavioral Stress Model showing how relational and health mechanisms connect stress to people's own and their partners' health across diverse developmental and contextual factors. Biobehavioral health mechanisms span psychological, behavioral, and biological factors. Neg. = negative; pos. = positive; inflam. = inflammation; HRV = heart rate variability.
The research discussed in this review provides conceptual and empirical evidence for paths throughout the Dyadic Biobehavioral Stress Model. As shown in Fig. 2, when experiencing a stressor, such as chronic illness, partners influence how each other see and react emotionally and physiologically to the stressor. People's own and their partners' effects can help or hinder their relationships and health, often referred to as risk and protective factors. Hostility, conflict, negative coping, strain, and criticism are linked to lower relationship satisfaction and poorer health; in contrast, responsiveness, self-disclosure, positive coping and support, and capitalization are associated with better relationship and health outcomes (Kiecolt-Glaser et al., 2020; Farrell and Simpson, 2017; Slatcher and Selcuk, 2016). For example, when both couple members saw their relationships as strong, they each felt comfortable talking about a partner's chronic illness (Shrout, 2019). In turn, their dyadic communication and coping strategies promoted both partners' relationship outcomes, like satisfaction and intimacy (Shrout, 2019; Manne et al., 2014). These relationship outcomes can then inform both partners' psychological, behavioral, and biological health. For instance, when one partner was satisfied and used relationship-promoting behaviors, the other partner had lower stress, cortisol, and HRV (Shrout et al., 2020a; Helm et al., 2014; Ditzen et al., 2007; Jakubiak and Feeney, 2019). These health mechanisms can then promote or impair each partner's physical health outcomes. High distress, poor sleep, heightened inflammation, and low HRV are linked to increases in disease development, illness severity, and accelerated biological aging; conversely, low distress, high quality sleep, low inflammation, and high HRV are associated with better health outcomes (Kiecolt-Glaser and Lovesick, 2017; Berg and Upchurch, 2007; Slatcher and Schoebi, 2016). Though not exhaustive, these relationship and health mechanisms may connect a stressor to each partner's health.
Developmental-contextual aspects, such as age, gender, and culture, can alter how partners shape each other's relationships and health during stress. Because women tend to think about their relationships more than men do, they are generally more reactive to relational stress than men (Kiecolt-Glaser and Newton, 2001). Recent research has shown more nuanced gender differences: more frequent conflict from year-to-year was related to husbands' poorer subjective health, whereas the pile up of conflict over 16 years was linked to wives' poorer subjective health (Shrout et al., 2019).
Individual differences in attachment and life adversity across developmental stages also have relationship and health implications. Partners with insecure attachment styles and those who experienced intimate partner violence reported sleep problems (Newton et al., 2016; Adams et al., 2014) and showed blunted cortisol reactivity to relationship conflict (Jarnecke et al., 2018; Powers et al., 2006). Early life adversity also can prime greater emotional and physiological reactivity to later stress, promoting chronic disease development across the lifespan (Miller et al., 2011). Work led by my colleague showed individuals with childhood emotional, physical, or sexual abuse histories had steeper inflammatory trajectories across adulthood than those without such histories (Renna et al., 2021). These age-related inflammation increases may contribute to accelerated aging, morbidity, and early mortality.
The chance of developing a chronic health condition also increases with advancing age, and many older adults are managing their own and their partners' chronic illnesses. Couples managing multiple health conditions, particularly in older adulthood, may rely on each other more often, perhaps intensifying links between partners' relationship behaviors and health. For instance, unsatisfied older couples experience heightened reactivity to marital stress (Wilson et al., 2021). In addition to age-related differences, partners' relationship and health effects may vary across relationship stages. Newly formed couples may be less comfortable discussing personal issues and have less experience navigating stress together compared to longer-term couples (Berg and Upchurch, 2007). However, stress can accumulate over time, particularly among more hostile and less supportive couples, straining partners' relationships and health (Bodenmann, 2005; Shrout et al., 2019). Addressing partners' connections across these developmental and contextual features is important to understand how, when, and under what conditions partners improve or impair each other's health. Identifying key risk and protective factors also may help inform interventions and initiatives to promote healthy aging and well-being across the lifespan and diverse relationship stages.
5.1. Future directions applying the Dyadic Biobehavioral Stress Model
The model can spur new research addressing links between partners' stress and health. This conceptual and empirically driven framework offers promising new directions as we push the boundaries of our current understanding of dyadic stress and its far-reaching health effects. Of notable importance, work is needed examining actor-partner effects across biological health markers. Key candidates for further investigation include effects of partners' stress perceptions, coping strategies, and relationship behaviors on each other's endocrine function, inflammatory reactivity, chronic inflammation, and resting and task specific HRV.
The gut environment also is a new promising candidate for understanding a relationship's health impact (Kiecolt-Glaser and Lovesick, 2017). Breast cancer survivors' and healthy middle-aged adults' satisfying relationships were linked to lower intestinal permeability and greater microbiota diversity and richness over time (Shrout et al., ; Kiecolt-Glaser et al., 2021). Older survivors, but not younger survivors, had greater inflammation when their intestinal permeability was higher than usual. This physiological cascade might indicate accelerated aging because their weakened immune systems primed stronger inflammatory responses, posing morbidity and mortality risks. In addition, couples' convergent health behaviors may compound health consequences. Partners often have similar diets and substance use, both of which have notable effects on gut microbiota composition (Kiecolt-Glaser and Lovesick, 2017). Likewise, couples shared social and structural stressors, such as changes in their income, employment, and socioeconomic status (SES), can worsen health behaviors. Additional research is needed to address how couples' shared experiences and health behaviors implicate the gut environment.
Psychological and behavioral mechanisms may connect relationship interactions to biological health. Previous work showed non-significant direct effects of relationship satisfaction on inflammation, potentially due to the healthy sample (Uchino et al., 2018). An additional possibility is that a partner's biological health effects may be transmitted through psychological mechanisms, such as perceived stress or depressive symptoms (Shrout et al., 2020b; Kiecolt-Glaser et al., 2021). A partner's effects might also be strongest in high stress situations, such as conflict or managing chronic illness, relative to more global, unbound experiences. For example, our paper showed cortisol differences based on a partner's stress level only emerged after experiencing conflict. These findings underscore the importance of assessing the couple's and the stressor's context, including the type of stressor, when the couples experience it, and how long lasting it is. Future research may consider addressing the context and designing studies that capture stressors in the lab or in everyday life through experimental, daily, and ecological momentary assessments. Couples' daily stressors provide many opportunities to identify key factors that protect or worsen health.
The current understanding of ties between relationships and health does not reflect our cultural or relational diversity. Most studies have focused on married couples, but research should investigate dating and marital-like relationships, along with consensual non-monogamous relationships. Likewise, same-gender couples report more similar behaviors than different-gender couples, altering long-term health consequences (Holway et al., 2018). A couple's SES can also influence their relationship quality and health in nuanced ways. Higher SES couples' withdrawal during conflict was associated with lower relationship satisfaction, but lower SES-couples withdrawal predicted greater satisfaction (Ross et al., 2019). Black and White couples also experience stress and its relational and health consequences in different ways. We found stress caused by a spouse's friends was associated with poorer marital well-being among Black spouses and wives (Trotter et al., 2019). Black spouses' and women's marital perceptions, therefore, may be more susceptible to external stress spillover. Though not an exhaustive list, these developmental-contextual features can enrich our understanding of how couples influence each other's health within their broader social contexts.
5.2. Conclusion
Our field has provided rich data and theoretical perspectives spanning individual, dyadic, and biobehavioral stress. This review was written to build on this foundational work and inspire transdisciplinary research integrating dyadic and biobehavioral lenses. The Dyadic Biobehavioral Stress Model offers a new way to conceptualize and investigate interdependent links among couples' relationships and health. Research applying this model can provide a deeper understanding of how partners influence their own and each other's health through psychological, behavioral, and biological pathways across developmental stages and diverse contexts.
Funding
This work was partially supported by a President's Postdoctoral Scholars Program Fellowship from the Ohio State University.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The author wishes to thank Dr. Megan E. Renna and the anonymous reviewers for their helpful comments on the manuscript.
References
- Adam E.K., Quinn M.E., Tavernier R., McQuillan M.T., Dahlke K.A., Gilbert K.E. Diurnal cortisol slopes and mental and physical health outcomes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;83(May):25–41. doi: 10.1016/j.psyneuen.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams G.C., Stoops M.A., Skomro R.P. Sleep tight: exploring the relationship between sleep and attachment style across the life span. Sleep Med. Rev. 2014;18(6):495–507. doi: 10.1016/j.smrv.2014.03.002. [DOI] [PubMed] [Google Scholar]
- Aggarwal B.B., Shishodia S., Sandur S.K., Pandey M.K., Sethi G. Inflammation and cancer: how hot is the link? Biochem. Pharmacol. 2006;72(11):1605–1621. doi: 10.1016/j.bcp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- Antelmi I., De Paula R.S., Shinzato A.R., Peres C.A., Mansur A.J., Grupi C.J. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am. J. Cardiol. 2004;93(3):381–385. doi: 10.1016/j.amjcard.2003.09.065. [DOI] [PubMed] [Google Scholar]
- Berg C.A., Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol. Bull. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Birditt K.S., Newton N.J., Cranford J.A., Ryan L.H. Stress and negative relationship quality among older couples: implications for blood pressure. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016;71(5):775–785. doi: 10.1093/geronb/gbv023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenmann G. 2005. Dyadic Coping and its Significance for Marital Functioning. [Google Scholar]
- Butler E.A., Randall A.K. Emotional coregulation in close relationships. Emot Rev. 2013;5(2):202–210. doi: 10.1177/1754073912451630. [DOI] [Google Scholar]
- Choi H., Marks N.F. Marital conflict, depressive symptoms, and functional impairment. J. Marriage Fam. 2008;70(2):377–390. doi: 10.1111/j.1741-3737.2008.00488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59(November):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Dickerson S.S., Mycek P.J., Zaldivar F. Negative social evaluation, but not mere social presence, elicits cortisol responses to a laboratory stressor task. Health Psychol. 2008;27(1):116–121. doi: 10.1037/0278-6133.27.1.116. [DOI] [PubMed] [Google Scholar]
- Ditzen B., Neumann I.D., Bodenmann G. Effects of different kinds of couple interaction on cortisol and heart rate responses to stress in women. Psychoneuroendocrinology. 2007;32(5):565–574. doi: 10.1016/j.psyneuen.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Ditzen B., Hoppmann C., Klumb P. Positive couple interactions and daily cortisol: on the stress-protecting role of intimacy. Psychosom. Med. 2008;70(8):883–889. doi: 10.1097/PSY.0b013e318185c4fc. [DOI] [PubMed] [Google Scholar]
- Donoho C.J., Seeman T.E., Sloan R.P., Crimmins E.M. Marital status, marital quality, and heart rate variability in the MIDUS cohort. J. Fam. Psychol. 2015;29(2):290–295. doi: 10.1037/fam0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell A.K., Simpson J.A. Effects of relationship functioning on the biological experience of stress and physical health. Curr Opin Psychol. 2017;13:49–53. doi: 10.1016/j.copsyc.2016.04.014. [DOI] [PubMed] [Google Scholar]
- Ferrucci L., Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018;15(9):505–522. doi: 10.1038/s41569-018-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasure-Smith N., Lespérance F., Irwin M.R., Talajic M., Pollock B.G. The relationships among heart rate variability, inflammatory markers and depression in coronary heart disease patients. Brain Behav. Immun. 2009;23(8):1140–1147. doi: 10.1016/j.bbi.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Glaser R., Kiecolt-Glaser J.K. Stress-induced immune dysfunction: implications for health. Nat. Rev. Immunol. 2005;5(March):243–251. doi: 10.3390/nu5041241. [DOI] [PubMed] [Google Scholar]
- Graham J.E., Christian L.M., Kiecolt-Glaser J.K. Marriage, health, and immune function. Relational Process DSM-V Neurosci assessment, Prev Treat. 2006:61–76. [Google Scholar]
- Graham J.E., Christian L.M., Kiecolt-glaser J.K. vol. 2. 2007. Close relationships and immunity; pp. 781–798. (Psychoneuroimmunology, Two-Volume Set). [DOI] [Google Scholar]
- Graham J.E., Glaser R., Loving T.J., Malarkey W.B., Stowell J.R., Kiecolt-Glaser J.K. Cognitive word use during marital conflict and increases in proinflammatory cytokines. Health Psychol. 2009;28(5):621–630. doi: 10.1037/a0015208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M.R., Vazquez D.M. Low cortisol and a flattening of expected daytime rhythm: potential indices of risk in human development. Dev. Psychopathol. 2001;13(3):515–538. doi: 10.1017/S0954579401003066. [DOI] [PubMed] [Google Scholar]
- Hackett R.A., Steptoe A., Kumari M. Association of diurnal patterns in salivary cortisol with type 2 diabetes in the Whitehall II study. J. Clin. Endocrinol. Metab. 2014;99(12):4625–4631. doi: 10.1210/jc.2014-2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A., Diez-Roux A.V., Sánchez B.N. Examining the association between salivary cortisol levels and subclinical measures of atherosclerosis: the Multi-Ethnic Study of Atherosclerosis. Psychoneuroendocrinology. 2013;38(7):1036–1046. doi: 10.1016/j.psyneuen.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helm J.L., Sbarra D., Ferrer E. Assessing cross-partner associations in physiological responses via coupled oscillator models. Emotion. 2012;12(4):748–762. doi: 10.1037/a0025036. [DOI] [PubMed] [Google Scholar]
- Helm J.L., Sbarra D.A., Ferrer E. Coregulation of respiratory sinus arrhythmia in adult romantic partners. Emotion. 2014;14(3):522–531. doi: 10.1037/a0035960. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Birmingham W., Jones B.Q. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Ann. Behav. Med. 2008;35(2):239–244. doi: 10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7) doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Robles T.F., Sbarra D.A. Advancing social connection as a public health priority in the United States. Am. Psychol. 2017;72(6):517–530. doi: 10.1037/amp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holway G.V., Umberson D., Donnelly R. Health and health behavior concordance between spouses in same-sex and different-sex marriages. Soc Curr. 2018;5(4):319–327. doi: 10.1177/2329496517734570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E.L., Benyamini Y. Self-rated health and Mortality : a review of twenty-seven community studies author (s): ellen L . Idler and Yael Benyamini Source. J. Health Soc. Behav. Mar, 1997;38(1):21–37. Published by : American Sociologic. J Health Soc Behav. 1997;38(1):21-37. [PubMed] [Google Scholar]
- Jackson S.E., Steptoe A., Wardle J. The influence of Partner's behavior on health behavior change: the English longitudinal study of Ageing. JAMA Intern Med. 2015;175(3):385–392. doi: 10.1001/jamainternmed.2014.7554. [DOI] [PubMed] [Google Scholar]
- Jakubiak B.K., Feeney B.C. Interpersonal touch as a resource to facilitate positive personal and relational outcomes during stress discussions. J. Soc. Pers. Relat. 2019;36(9):2918–2936. doi: 10.1177/0265407518804666. [DOI] [Google Scholar]
- Jaremka L.M., Glaser R., Malarkey W.B., Kiecolt-Glaser J.K. Marital distress prospectively predicts poorer cellular immune function. Psychoneuroendocrinology. 2013;38(11):2713–2719. doi: 10.1016/j.psyneuen.2013.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarnecke A.M., Barden E., Back S.E., Brady K.T., Flanagan J.C. Intimate partner violence moderates the association between oxytocin and reactivity to dyadic conflict among couples. Psychiatr. Res. 2018;270(May):404–411. doi: 10.1016/j.psychres.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph N.T., Kamarck T.W., Muldoon M.F., Manuck S.B. Daily marital interaction quality and carotid artery intima-medial thickness in healthy middle-aged adults. Psychosom. Med. 2014;76(5):347–354. doi: 10.1097/PSY.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kane H.S., Slatcher R.B., Reynolds B.M., Repetti R.L., Robles T.F. Daily self-disclosure and sleep in couples. Health Psychol. 2014;33(8):813–822. doi: 10.1037/hea0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser K., Scott J.L. Springer Science+Business Media; New York: 2008. Helping Couples Cope with Women's Cancers: an Evidence-Based Approach for Practitioners. [Google Scholar]
- Kayser K., Watson L.E., Andrade J.T. Cancer as a “we-disease”: examining the process of coping from a relational perspective. Fam. Syst. Health. 2007;25(4):404–418. doi: 10.1037/1091-7527.25.4.404. [DOI] [Google Scholar]
- Kelley H.H., Thibaut J.W. Wiley; New York, NY: 1978. Interpersonal Relations: A Theory of Interdependence. [Google Scholar]
- Kenny D.A., Kashy D.A., Cook W.L. Guilford Press; New York, NY, US: 2006. Dyadic Data Analysis. [Google Scholar]
- Kiecolt-Glaser J.K. Marriage, divorce, and the immune system. Am. Psychol. 2018;73(9):1098–1108. doi: 10.1037/amp0000388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Lovesick Wilson S. How couples' relationships influence health. Annu Rev ofClinical Psychol. 2017 doi: 10.1146/annurev-clinpsy-032816-045111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Newton T.L. Marriage and health: his and hers. Psychol. Bull. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Glaser R., Cacioppo J.T. Marital conflict in older adults: endocrinological and immunological correlates. Psychosom. Med. 1997;59(4):339–351. doi: 10.1097/00006842-199707000-00001. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Loving T.J., Stowell J.R. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Arch. Gen. Psychiatr. 2005;62(12):1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Gouin J.P., Hantsoo L. Close relationships, inflammation, and health. Neurosci. Biobehav. Rev. 2010;35(1):33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Renna M.E., Shrout M.R., Madison A.A. Stress reactivity: what pushes us higher, faster, and longer—and why it matters. Curr. Dir. Psychol. Sci. 2020;29(5):492–498. doi: 10.1177/0963721420949521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Wilson S.J., Shrout M.R. The gut reaction to couples' relationship troubles: a route to gut dysbiosis through changes in depressive symptoms. Psychoneuroendocrinology. 2021;125(January):105132. doi: 10.1016/j.psyneuen.2021.105132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.G., Cheon E.J., Bai D.S., Lee Y.H., Koo B.H. Stress and heart rate variability: a meta-analysis and review of the literature. Psychiatry Investig. 2018;15(3):235–245. doi: 10.30773/pi.2017.08.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari M., Badrick E., Chandola T. Cortisol secretion and fatigue: associations in a community based cohort. Psychoneuroendocrinology. 2009;34(10):1476–1485. doi: 10.1016/j.psyneuen.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Kumari M., Shipley M., Stafford M., Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. J. Clin. Endocrinol. Metab. 2011;96(5):1478–1485. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loving T.J., Slatcher R. oxford Handb close relationships; 2013. Romantic Relationships and Health. [Google Scholar]
- Madison AA, Andridge R, Shrout MR, et al. Chronic interpersonal stress and inflammatory reactivity predict depressive symptom increases: two tests of the social signal transduction theory of depression. Psychol. Sci. in press. [DOI] [PMC free article] [PubMed]
- Manne S.L., Siegel S., Kashy D., Heckman C.J. Cancer-specific relationship awareness, relationship communication, and intimacy among couples coping with early stage breast cancer. J. Soc. Pers. Relat. 2014;31(3):314–334. doi: 10.1177/0265407513494950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaud M., Balardy L., Moulis G. Proinflammatory cytokines, aging, and age-related diseases. J. Am. Med. Dir. Assoc. 2013;14(12):877–882. doi: 10.1016/j.jamda.2013.05.009. [DOI] [PubMed] [Google Scholar]
- Miller G.E., Chen E., Parker K.J. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol. Bull. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monden C. In: Encyclopedia of Quality of Life and Well-Being Research. Michalos A.C., editor. Springer Netherlands; Dordrecht: 2014. Subjective health and subjective well-being; pp. 6423–6426. [DOI] [Google Scholar]
- Newton T.L., Burns V.E., Miller J.J., Fernandez-Botran G.R. Subjective sleep quality in women with divorce histories: the role of intimate partner victimization. J. Interpers Violence. 2016;31(8):1430–1452. doi: 10.1177/0886260514567961. [DOI] [PubMed] [Google Scholar]
- Phillips A.C., Carroll D., Burns V.E., Ring C., Macleod J., Drayson M. Bereavement and marriage are associated with antibody response to influenza vaccination in the elderly. Brain Behav. Immun. 2006;20(3):279–289. doi: 10.1016/j.bbi.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Pietromonaco P.R., Collins N.L. Interpersonal mechanisms linking close relationships to health. Am. Psychol. 2017;72(6):531–542. doi: 10.1037/amp0000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietromonaco P.R., Collins N.L. Interpersonal mechanisms linking close relationships to health. Am. Psychol. 2017;72(6):531–542. doi: 10.1037/amp0000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietromonaco P.R., Overall N.C. Applying relationship science to evaluate how the COVID-19 pandemic may impact couples' relationships. Am. Psychol. 2020 doi: 10.1037/amp0000714. [DOI] [PubMed] [Google Scholar]
- Pietromonaco P.R., Uchino B.N., Schetter C.D. Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. 2013;32(5):499–513. doi: 10.1037/a0029349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers S.I., Pietromonaco P.R., Gunlicks M., Sayer A. Dating couples' attachment styles and patterns of cortisol reactivity and recovery in response to a relationship conflict. J. Pers. Soc. Psychol. 2006;90(4):613–628. doi: 10.1037/0022-3514.90.4.613. [DOI] [PubMed] [Google Scholar]
- Renna M.E., Peng J., Shrout M.R. Childhood abuse histories predict steeper inflammatory trajectories across time. Brain Behav. Immun. 2021;91(November):541–545. doi: 10.1016/j.bbi.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles T.F., Kiecolt-Glaser J.K. The physiology of marriage: pathways to health. Physiol. Behav. 2003;79(3):409–416. doi: 10.1016/S0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Robles T.F., Slatcher R.B., Trombello J.M., McGinn M.M. Marital quality and health: a meta-analytic review. Psychol. Bull. 2014;140(1):140–187. doi: 10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J.M., Karney B.R., Nguyen T.P., Bradbury T.N. Communication that is maladaptive for middle-class couples is adaptive for socioeconomically disadvantaged couples. J. Pers. Soc. Psychol. 2019;116(4):582–597. doi: 10.1037/pspi0000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selcuk E., Gunaydin G., Ong A.D., Almeida D.M. Does partner responsiveness predict hedonic and eudaimonic well-being? A 10-year longitudinal study. J. Marriage Fam. 2016;78(2):311–325. doi: 10.1111/jomf.12272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields G.S., Spahr C.M., Slavich G.M. Psychosocial interventions and immune system function: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2020;77(10):1031–1043. doi: 10.1001/jamapsychiatry.2020.0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout M.R. Couples and nonvisible chronic illness: an integrated model of dyadic Coping. Dissertation. 2019;23(3):2019. [Google Scholar]
- Shrout M.R., Weigel D.J. Infidelity's aftermath: appraisals, mental health, and health-compromising behaviors following a partner's infidelity. J. Soc. Pers. Relat. 2018;35(8):1067–1091. doi: 10.1177/0265407517704091. [DOI] [Google Scholar]
- Shrout M.R., Brown R.D., Orbuch T.L., Weigel D.J. A multidimensional examination of marital conflict and subjective health over 16 years. Pers. Relat. 2019;26(3):490–506. doi: 10.1111/pere.12292. [DOI] [Google Scholar]
- Shrout M.R., Renna M.E., Madison A.A. Cortisol slopes and conflict: a spouse's perceived stress matters. Psychoneuroendocrinology. 2020;121:104839. doi: 10.1016/j.psyneuen.2020.104839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout M.R., Renna M.E., Madison A.A. Relationship satisfaction predicts lower stress and inflammation in breast cancer survivors: a longitudinal study of within-person and between-person effects. Psychoneuroendocrinology. 2020;118:104708. doi: 10.1016/j.psyneuen.2020.104708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout M.R., Renna M., Madison A.A. Breast cancer survivors' satisfying marriages predict better psychological and physical health: a longitudinal comparison of satisfied, dissatisfied, and unmarried women. Psycho Oncol. 2021;30(5):699–707. doi: 10.1002/pon.5615. [DOI] [PubMed] [Google Scholar]
- Shrout MR, Madison AA, Renna ME, et al. The Gut Connection: Gut Leakiness as a Pathway from Breast Cancer Survivors' Relationship Satisfaction to Inflammation across Treatment.. [DOI] [PMC free article] [PubMed]
- Slatcher R.B. Marital functioning and physical health: implications for social and personality psychology. Soc Personal Psychol Compass. 2010;4(7):455–469. doi: 10.1111/j.1751-9004.2010.00273.x. [DOI] [Google Scholar]
- Slatcher R.B., Schoebi D. Protective processes underlying the links between marital quality and physical health. Curr Opin Psychol. 2016;13:148–152. doi: 10.1016/j.copsyc.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher R.B., Selcuk E. A social psychological perspective on the links between close relationships and health. Curr. Dir. Psychol. Sci. 2016;26(1):16–21. doi: 10.1177/0963721416667444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher R.B., Selcuk E., Ong A.D. Perceived partner responsiveness predicts diurnal cortisol profiles 10 years later. Psychol. Sci. 2015;26(7):972–982. doi: 10.1177/0956797615575022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich G.M., Irwin M.R. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol. Bull. 2014;140(3):774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T.W. Relationships matter: progress and challenges in research on the health effects of intimate relationships. Psychosom. Med. 2019;81(1):2–6. doi: 10.1097/PSY.0000000000000660. [DOI] [PubMed] [Google Scholar]
- Smith T.W., Uchino B.N., Berg C.A. Conflict and collaboration in middle-aged and older couples: II. Cardiovascular reactivity during marital interaction. Psychol. Aging. 2009;24(2):274–286. doi: 10.1037/a0016067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T.W., Cribbet M.R., Nealey-Moore J.B. Matters of the variable heart: respiratory sinus arrhythmia response to marital interaction and associations with marital quality. J. Pers. Soc. Psychol. 2011;100(1):103–119. doi: 10.1037/a0021136. [DOI] [PubMed] [Google Scholar]
- Stanton S.C.E., Selcuk E., Farrell A.K., Slatcher R.B., Ong A.D. Perceived partner responsiveness, daily negative affect reactivity, and all-cause mortality: a 20-year longitudinal study. Psychosom. Med. 2019;81(1):7–15. doi: 10.1097/PSY.0000000000000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotter P.B., Orbuch T.L., Shrout M.R. Spouses' perceptions of network interference in the early years of marriage. Interpersona. 2019;13(2):220–236. doi: 10.5964/ijpr.v13i2.362. [DOI] [Google Scholar]
- Uchino B.N. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Uchino B.N., de Grey R.G.K., Cronan S. Life satisfaction and inflammation in couples: an actor–partner analysis. J. Behav. Med. 2018;41(1):22–30. doi: 10.1007/s10865-017-9880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D., Williams K., Powers D.A., Liu H., Needham B. You make me sick: marital quality and health over the life course. J. Health Soc. Behav. 2006;47(1):1–16. doi: 10.2307/30040295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigel D.J., Shrout M.R. Relationship conflict, appraisals, and disillusionment: the moderating role of depression. Pers. Indiv. Differ. 2020;(October):110494. doi: 10.1016/j.paid.2020.110494. [DOI] [Google Scholar]
- Weigel D.J., Shrout M.R. Suspicious minds: the psychological, physical and behavioral consequences of suspecting a partner's infidelity. J. Soc. Pers. Relat. 2020;38(3):865–887. doi: 10.1177/0265407520975851. [DOI] [Google Scholar]
- Wilson S.J., Bailey B.E., Jaremka L.M. When couples' hearts beat together: synchrony in heart rate variability during conflict predicts heightened inflammation throughout the day. Psychoneuroendocrinology. 2018;93(September 2017):107–116. doi: 10.1016/j.psyneuen.2018.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S.J., Bailey B.E., Malarkey W.B., Kiecolt-Glaser J.K. Linking marital support to aging-related biomarkers: both age and marital quality matter. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76(2):273–282. doi: 10.1093/geronb/gbz106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright B.L., Loving T.J. Health implications of conflict in close relationships. Soc Personal Psychol Compass. 2011;5(8):552–562. doi: 10.1111/j.1751-9004.2011.00371.x. [DOI] [Google Scholar]