Introduction
Non-muscle invasive bladder cancer (NMIBC) exhibits a high recurrence rate and tumor multifocality, placing significant financial and psychological burden on patients. Extracellular vesicles (EVs) are membrane-bound nano-particles containing bioactive molecules critical for intercellular communication. Recent studies provide evidence that bladder cancer EVs (BCEVs) promote the malignant transformation of predisposed cells by activating the oncogenic ER stress response. We sought to identify responsible cargo proteins and underlying mechanisms that drive tumorigenesis.
Methods
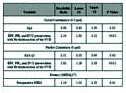
Mass spectrometry was used to identify the candidate EV protein: protein disulfide isomerase (PDI). Loss/gain-of-function approaches were applied to define the functional roles of EV-borne PDI. Various assays including Western blot, DCFDA, immunofluorescence staining, and colony-forming assay were performed to characterize cellular molecular alterations during transformation. Whole-genome sequencing (WGS) analysis was performed to assess the mutations in the transformed cells. Urinary EVs isolated from NMIBC patients were analyzed for the presence of PDI.
Results
EV-borne PDI, a redox chaperone of ER, was identified for its exclusive and abundant presence in BCEVs. Treating normal urothelial SV-HUC cells with PDI-enriched BCEVs increased cellular oxidative stress and DNA damage. Knock down of PDI in BCEVs reduced cellular ROS and DNA damage, suppressing tumorigenesis in SV-HUC recipient cells. Restoring PDI by extrusion rescues tumorigenic phenotypes. In transformed cells, WGS identified 114,978 unique variants and 875 genes harboring mutations in coding regions. Importantly, several of these genes are tumor suppressors, negative regulators of cell proliferation, and regulators of apoptosis-essential alterations described as seminal hallmarks of cancer. PDI was detectable in urinary EVs derived from NMIBC patients, making PDI a viable candidate marker for liquid biopsy.
Conclusions
This supports a model wherein PDI-enriched EVs induce cellular stress responses in recipient normal urothelial cells and promote mutational events. Accumulation of somatic mutations facilitates the selection for cells that gain a survival advantage and eventually evolve into fully transformed malignant cells. This study offers a potential therapeutic target in BCEVs to prevent BC recurrence. PDI detection in urinary EVs may provide a novel noninvasive biomarker for NMIBC recurrence.
Footnotes
Funding: NCI R01 CA173986.