Abstract
Objective
This research addresses the following questions: what is the prevalence and severity of first-rank symptoms (FRS) during an extended period of time in patients with schizophrenia and bipolar disorder with psychosis? Are the specific FRS listed in Diagnostic and Statistical Manual of Mental Disorders DSM, Third Edition, Revised/Fourth Edition Criterion A for schizophrenia diagnosis (a voice keeping a running commentary or voices conversing) more prevalent and severe in patients with schizophrenia than bipolar disorder with psychosis? Lastly, do FRS at index hospitalization in patients with schizophrenia predict the absence of later recovery?
Methods
This research follows a sample of patients with psychotic disorders who were evaluated at index hospitalization and then prospectively followed-up at 6 evaluations during next 20 years (n = 86). All patients were evaluated as part of a prospective research study designed to measure multiple factors of phenomenology, severity of illness, course of illness, prognosis, and global outcome.
Results
First-rank symptoms are not exclusive to schizophrenia; they also occur in some bipolar patients. However, they are more frequent and more severe in patients with schizophrenia than bipolar disorder. Schizophrenia patients with FRS during the acute phase are more likely to have poorer long-term outcome than schizophrenia patients who do not have FRS during the acute phase.
Conclusions
Our results indicate FRS at the acute phase are not a clinicopathologic correlate specific to schizophrenia. However, the presence and severity of any FRS and specifically of the 2 FRS associated with Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised/Fourth Edition Criterion A are more prevalent and more severe in patients with schizophrenia than patients with bipolar disorder.
1. Introduction
Since the early 19th century, several models of schizophrenia as a disease entity have been proposed. One of the most prominent models was introduced by Kurt Schneider, who identified first-rank symptoms (FRS) that he considered to be pathognomonic of schizophrenia. These symptoms include delusional perceptions; auditory hallucinations experienced as voices speaking one’s thoughts, voices arguing, and voices commenting on one’s actions; and 7 types of delusions: somatic passivity, thought withdrawal, thought broadcasting, thought insertion, belief that one’s emotions are not one’s own, and belief that impulses and/or actions are controlled by an outside force [1,2]. First-rank symptoms have been considered primary characteristics of schizophrenia in current diagnostic conceptualization in both Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-IIIR) and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). According to Criterion A of DSM-IIIR/IV, unlike other psychotic symptoms, the presence of only one of the following FRS, a bizarre delusion, hallucination consisting of a voice keeping a running commentary on the person’s behavior or thoughts (FRS), or 2 or more voices conversing with each other, is needed for the schizophrenia diagnosis [3].
Throughout the years, researchers have argued about the diagnostic specificity and prognostic validity of FRS. A literature review indicated that FRS were specific to schizophrenia [4]. Other studies have shown that FRS occur more frequently, but not exclusively in schizophrenia, and that FRS are also found in patients with affective disorders [5]. Most studies conclude that FRS are not unique to schizophrenia [6-9].
Regarding the prognostic validity of FRS, the International Pilot Study of Schizophrenia, prospective research sponsored by the World Health Organization, and other studies have suggested that the presence of FRS does not predict poor outcome [10-13]. However, some studies have found that FRS predict poor outcome in individuals with psychotic illnesses other than schizophrenia, even while failing to predict poor outcome for schizophrenia [14]. A number of studies have suggested that schizophrenia and affective disorders are not discrete entities but rather constitute a continuum of psychotic symptoms that cross diagnostic boundaries [15-17].
Longitudinal studies examining outcome in patients with schizophrenia and bipolar disorder with psychosis who experienced FRS at index hospitalization may be valuable in the understanding of recovery and relapse in psychosis [18,19]. The current prospective 20-year multi–follow-up longitudinal research studied the course, outcome, and potential recovery in patients with schizophrenia and bipolar with psychosis who experienced FRS during the acute phase of illness at index hospitalization. With a focus on the underlying issue of whether FRS constitute a more important type of psychotic symptom than other types, this article addresses the following:
What is the prevalence and severity of FRS during an extended period of time in patients with schizophrenia and bipolar disorder with psychosis?
Are the specific FRS listed in DSM III-R/IV Criterion A for schizophrenia diagnosis more prevalent and severe in patients with schizophrenia than bipolar disorder with psychosis?
Do FRS at index hospitalization predict the absence of recovery years later in patients with schizophrenia?
2. Method
The sample consisted of a total of 86 participants studied longitudinally for 20 years: 59 patients diagnosed with schizophrenia and 27 patients with bipolar disorder with psychosis. Patients were evaluated relatively early in their disorder (between 17 and 32 years old at index) in that 64% of the total sample had one or fewer previous hospitalizations. There was no significant difference between patients with schizophrenia and bipolar disorder in the number of previous admissions. Of the 59 patients with schizophrenia, 39% were first admission and 61% were not first admission. Of the 27 patients with bipolar disorder, 34% were first admission and 66% were not first admission.
In addition, when we looked at outcome measures in schizophrenia, there was no significant difference between first-admission and not first-admission patients in predicting future FRS, chronic psychosis, or recovery. The same pattern held true for patients with bipolar disorder.
All patients were evaluated as part of the Harrow Chicago Follow-up study, a prospective research program designed to study major symptoms including psychosis, negative symptoms, thought disorders, outcome, and factors in psychopathology and recovery in schizophrenia and major mood disorders [20-22].
Data on FRS at the 20-year follow-up were available for 73% of the original sample assessed. The 59 schizophrenia patients were compared with a subsample of schizophrenia patients who were assessed at index hospitalization, but not at the 20-year follow-up. These 2 groups did not differ significantly on major demographic and other key variables.
This research follows a sample of patients with psychotic and mood disorders who were evaluated at index hospitalization and then prospectively followed at 6 evaluations subsequently for 20 years [23,24]. Follow-up evaluations occurred at 2, 4.5, 7.5, 10, 15, and 20 after index hospitalization.
All 86 patients were assessed at the 20-year follow-up. Fifty patients (58%) were studied at all 6 follow-ups for 20 years. Another 26 patients were studied at 5 of the 6 follow-ups, including the 20-year follow-up. Overall, 76 patients (88%) were studied at 5 or 6 of the follow-ups.
Research Diagnostic Criteria (RDC) diagnoses at index hospitalization were based on structured clinical interviews including the Schedule for Affective Disorders and Schizophrenia, and/or the Schizophrenia State Inventory and collateral information. The RDC were used for diagnosis because they provide diagnostic criteria that are independent of FRS, allowing diagnostic analyses that have not been confounded by the use of FRS as an inclusion criterion for schizophrenia. The RDC diagnosis was further supported by the construct validity of the symptom presentation by diagnosis over time. For example, (a) all the patients with bipolar disorder had a manic syndrome at index hospitalization, whereas none of the schizophrenia patients had such a syndrome, and (b) later at follow-up, 38% of patients with schizophrenia showed more vulnerability to chronic FRS (FRS at 3 or more follow-ups) compared with 14% of patients with bipolar disorder (χ2 = 4.1, df = 1, P < .05). Diagnostic interrater reliability was κ = 0.88. Interviewers performing follow-up evaluations were not informed of diagnosis or the results of previous follow-up evaluations. All research was approved by the institutional review board, and informed written consent was obtained.
Table 1 presents the demographic characteristics for the sample at index hospitalization. There were no significant diagnostic differences for age, sex, race, percentage of 1 or fewer previous hospitalizations, parental socioeconomic class [25], or level of education.
Table 1.
Demographic characteristics
| Demographic characteristics | Schizophrenia (n = 59) |
Bipolar/manic (n = 27) |
P | ||
|---|---|---|---|---|---|
| M | (SD) | M | (SD) | ||
| Age at testing (y) | 23 | (3.4) | 24 | (6.3) | NS |
| % Male | 61% | – | 52% | – | NS |
| % White | 59% | – | 65% | – | NS |
| One or fewer previous hospitalizations | 68% | – | 56% | – | NS |
| Social Class | 3.3 | (1.5) | 3.2 | (1.5) | NS |
| Education | 12.7 | (2.2) | 13.6 | (2.3) | NS |
NS indicates not significant.
At the 20-year follow-up, 65% (n = 38) of schizophrenia patients were on psychiatric medications as were 58% (n = 15) bipolar patients. Of these, 55% (n = 32) of schizophrenia patients were on antipsychotic medications compared with 23% (n = 6) of bipolar patients.
2.1. Measures used to assess Schneiderian FRS
First-rank symptoms were individually evaluated at index hospitalization and at each subsequent follow-up. The assessment of FRS was based on the Schedule for Affective Disorders and Schizophrenia and determined by a system of assessment used successfully in previous research [21]. First-rank symptoms were scored as absent (score of “1”), weak or equivocal (“2”), and definitely present (“3”). Patients were considered to have FRS if they received a score of “2” or “3” on this variable.
At index hospitalization, the following FRS were assessed: thought broadcasting, thought insertion, thought withdrawal, delusions of control, a voice keeping a running commentary, and voices conversing. We evaluated at index and at all 6 follow-ups the 2 FRS in DSM-IIIR/IV criterion A for schizophrenia, auditory hallucinations that consist of a voice keeping a running commentary and voices conversing. In addition, at each follow-up, all 12 FRS were assessed.
The 20 years of assessments allowed us to obtain for each patient a cumulative index based on whether the patient ever experienced an FRS at any of the 6 follow-ups. Our longitudinal design also allowed us to evaluate the presence of chronic FRS, assessing how many patients experienced FRS at 3 or more of the 6 follow-ups.
2.2. Operational definition of recovery
Psychiatric research has yet to define a unified or set criterion for recovery; thus, multiple definitions of recovery exist. However, many researchers agree that recovery includes the absence of major symptoms and adequate instrumental work and psychosocial functioning [24,26-28].
The operational criteria for recovery, which we have used successfully in the past [18], required the following: the absence of psychosis and negative symptoms for 12 months before evaluation, adequate instrumental work functioning (working half-time or more), adequate psychosocial functioning, and no psychiatric hospitalization during the past year.
To assess recovery and global outcome, we used the 8-point Levenstein-Klein-Pollack scale and the 5-point Strauss-Carpenter Scales [18,22,29,30].
The Levenstein-Klein-Pollack, our major index of global functioning at each follow-up, has been used successfully by our research team and others [31]. This scale takes into account work and social functioning, life adjustment, level of self-support, major symptoms, relapses, and rehospitalization. Psychosocial and work functioning were measured by the Strauss-Carpenter scales denoting adequacy of social contacts and work status. The operational definition of recovery has been consistently applied to multiple reports by the Harrow Chicago Follow-up study and provides data on the cumulative percentage of participants who have experienced a period of recovery at any time during the 20 years of follow-ups. Recovery at any follow-up does not necessarily predict future recovery, which, for patients with psychotic disorders, may be a function of many factors. These include the natural course of illness, patients’ resilience, environment, level of stress, biological factors, and treatment.
3. Results
3.1. Diagnostic differences in prevalence of FRS at 6 follow-ups over 20 years
We compared the number and percentage of patients with schizophrenia and bipolar disorder who exhibited FRS at each of the 6 follow-ups during the 20-year study period. First-rank symptoms at each follow-up were subjected to 2-way mixed-design analyses of variance with one repeated-measure factor. The 2 main effects were diagnosis and time of assessment (the repeated-measure factor). Schizophrenia patients were significantly more likely to exhibit FRS during the course of illness than bipolar patients (F1, 23 = 5.16, P = .03).
Fig. 1 presents the percentage of patients who experienced at least one FRS, at each follow-up. Schizophrenia patients and some bipolar patients were vulnerable to FRS, although schizophrenia patients exhibited FRS at increased prevalence compared with bipolar patients at the acute phase and in subsequent follow-ups. At all 6 follow-ups, the percentage of schizophrenia patients with FRS was higher than that of bipolar patients. The differences were significant at 2-year (χ2 = 5.45, df = 1, P = .02), 4.5-year (χ2 = 5.03, df = 1, P = .03), and 20-year evaluations (χ2 = 5.03, df = 1, P = .04).
Fig. 1.
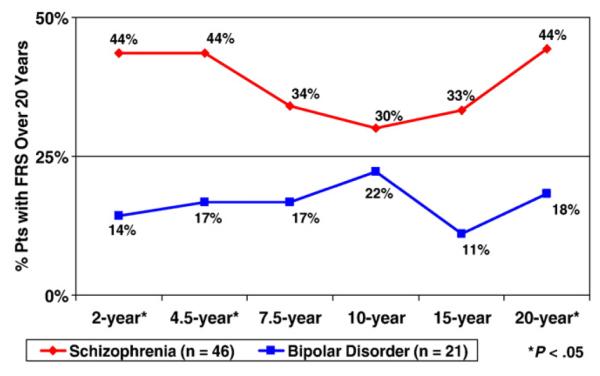
Prevalence of FRS over 20 years in schizophrenia and bipolar disorder.
We compared the number of schizophrenia and bipolar patients who ever exhibited a FRS during the 20-year period. Data indicated that 75% of schizophrenia patients experienced a FRS at some point from index hospitalization through the 20-year follow-up, compared with 44% of bipolar patients (χ2 = 7.4, df = 1, P = .007).
3.2. DSMIII/IV diagnostic differences in prevalence and severity of FRS of a voice keeping a running commentary or voices conversing
Using this criterion for schizophrenia (auditory hallucinations consisting of a voice keeping a running commentary or voices conversing with each other), our data indicate that these 2 FRS are not unique to schizophrenia, although a larger percentage of schizophrenia patients had these FRS at index hospitalization and at each of the 6 follow-ups (see Fig. 2). The diagnostic differences in the percentage with these 2 symptoms over time were significant at the 2-year follow-up (χ2 = 6.1, df = 1, P < .02), 4.5-year follow-up (χ2 = 5.8, df = 1, P < .02), 7.5-year follow-up (χ2 = 4.2, df = 1, P < .05), and 20-year follow-up (χ2 = 4.0, df = 1, P < .05). In addition, either one or both of these FRS were present at 3 or more follow-ups in 25% of schizophrenia patients compared with 0% with bipolar disorder (χ2 = 5.9, df = 1, P < .015) from the 2-year follow-up through the 20-year follow-up. One or both FRS occurred in 55% of patients with schizophrenia at some point during the 20-year follow-up as compared with only 27% with bipolar disorder. Thus, schizophrenia patients are more vulnerable to the chronicity of these 2 FRS.
Fig. 2.
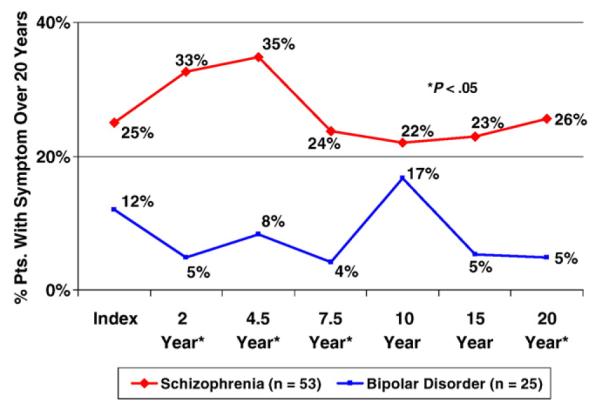
Twenty-year assessment of the prevalence of “voices keeping a running commentary” or “voices conversing.”
These 2 FRS were also more severe in schizophrenia than bipolar disorder and showed a significant difference over time on a 3-point scale of severity of symptoms (F1, 21 = 11.5, P = .003). Fig. 3 shows that these differences were significant at the 2-year follow-up (F1, 65 = 6.1, P < .02), 4.5-year follow-up (F1, 68 = 5.8, P < .02), 7.5-year follow-up (F1, 64 = 4.1, P < .05), and 20-year follow-up (F1, 62 = 4.1, P < .05).
Fig. 3.
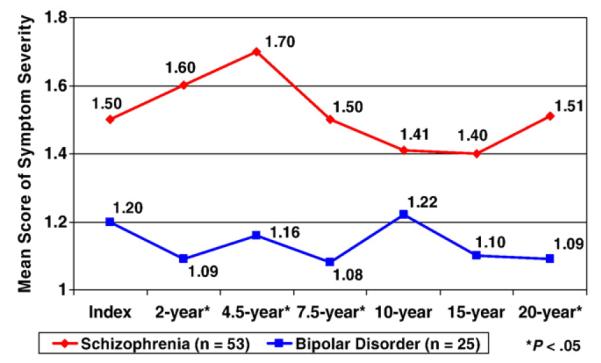
Twenty-year assessment of the severity of “voices keeping a running commentary” or “voices conversing.”
3.3. The predictive value of FRS on recovery in schizophrenia
We studied whether the presence of FRS at the acute phase predicts the absence of later periods of recovery in schizophrenia. Of the 23 schizophrenia patients who had FRS at the acute phase, 70% (n = 16) had no year-long periods of recovery during the 20-year follow-up.
We also studied whether FRS at the 2-year follow-up predicted later periods of recovery. Fig. 4 compares recovery data for schizophrenia patients with FRS at the 2-year follow-up, showing that FRS at the 2-year follow-up, predicted the absence of later periods of recovery (χ2 = 11.3, df = 1, P < .001). The 2 DSM-IIIR/IV-specific FRS did not predict the absence of later periods of recovery when measured at index hospitalization. However, they did predict the absence of later periods of recovery when measured at the 2-year follow-up (χ2 = 4.5, df = 1, P < .03).
Fig. 4.
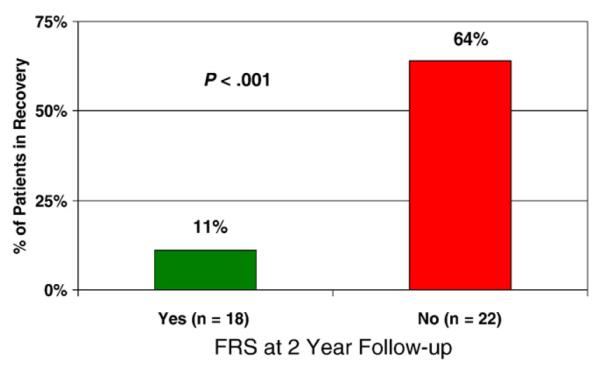
Predictive value of FRS in schizophrenia.
4. Discussion
This research compared the prevalence and severity of FRS studied longitudinally during an extended period of time in schizophrenia and bipolar patients. It also examined the prevalence and severity of the 2 specific FRS given special emphasis in DSM-IIIR/IV Criterion A for schizophrenia diagnosis (voices keeping a running commentary and voices conversing). We also examined the prognostic power of FRS in general as well as that of the 2 specific FRS, during the acute phase and at the 2-year follow-up as a predictor of the absence of later periods of recovery in patients with schizophrenia. Twenty-year longitudinal prospective multi–follow-up data on the prevalence and severity of FRS and cumulative data on recovery have not previously been available to the field. These issues have become more important because of the recent questions regarding diagnostic specificity in schizophrenia and bipolar disorders [32,33].
4.1. What is the prevalence and severity of FRS during an extended period of time in patients with schizophrenia and bipolar disorder?
The current longitudinal data support findings by others indicating that although FRS also occur in some patients with psychotic disorders other than schizophrenia, FRS are more prevalent and severe in patients with schizophrenia [8,9,34-36]. At the acute phase of index hospitalization and at each of the 6 follow-ups throughout the 20-year period, the percentage of schizophrenia patients reporting at least one FRS was significantly higher than that of bipolar patients.
Although previous studies have reported that some schizophrenia patients experience periods of recovery during the course of their illness, greater chronicity of symptoms has always been one of the main factors separating schizophrenia from bipolar disorder [24,26].
The current longitudinal data on patients with schizophrenia and bipolar disorder with FRS at 3 or more follow-ups indicate greater vulnerability to FRS in schizophrenia. The data on the relation of FRS to a lower rate of recovery in schizophrenia suggest FRS as one indicator of a more severe schizophrenic disorder. In addition, the finding of FRS in some bipolar patients is consistent with the conclusions of others who report that FRS are not unique to schizophrenia and do not identify an empirically homogeneous diagnostic group [8,37].
4.2. Are the specific FRS listed in DSMIII-R and DSM-IV Criterion A for schizophrenia more prevalent and severe in patients with schizophrenia than bipolar disorder?
The 2 specific auditory hallucinations listed in DSMIIIR/IV Criterion A for schizophrenia have been identified as symptoms that offer diagnostic specificity [9]. Our data show that both these FRS symptoms, though not found exclusively in schizophrenia patients, were more prevalent and severe in patients with schizophrenia compared with bipolar disorder. Our results indicate that FRS at the acute phase are not a clinicopathologic correlate specific to schizophrenia. However, the presence and severity of any FRS and specifically 1 of the 2 FRS associated with DSM-IIIR/IV Criterion A are more prevalent and more severe in patients with schizophrenia than bipolar disorder.
4.3. Do FRS at the acute phase in schizophrenia patients predict the absence of later periods of global recovery?
Previous studies assessing the predictive value of FRS at index hospitalization on later recovery have produced mixed results [12,35]. Thus, some studies reported that FRS do not predict outcome [6,11,38]. Other studies found that FRS at the acute phase have high specificity and predictive value of global recovery in both schizophrenia and bipolar disorder [39,40]. Most of this research only studies outcome during a 2- to 5-year period. Our longitudinal study, using a longer period of assessment of both FRS and recovery, found that FRS at the acute phase significantly predict the absence of later recovery in schizophrenia. These specific DSMIIIR/IV FRS do not predict later recovery when measured at the acute phase. However, they successfully predict later recovery when measured at the 2-year follow-up. These data fit with other data suggesting that the presence of FRS at the acute phase represents more severe type of psychotic symptoms [41]. If true, future research might profitably study which characteristics of FRS render them more severe.
In conclusion, FRS are not exclusive to schizophrenia but are more frequent and severe in schizophrenia than in bipolar disorder. Most other psychotic symptoms are also more severe in schizophrenia and more frequent during the longitudinal course of illness. The data indicate that FRS may have prognostic significance regarding later periods of global recovery, suggesting that FRS are especially severe psychotic symptoms. These results paint a less optimistic picture for schizophrenia patients with FRS during the acute phase, indicating that these patients are more likely to have poorer long-term outcome. Our data support further investigation of the phenomenologic aspects, either dimensional or categorical, of symptoms and other phenotypic characteristics. Such research may lead to greater understanding of the biologic underpinnings of homogenous dimensions of psychosis. An alternative to categorical diagnosis opens the possibility of “spectrum” or “dimensional” illness, in which specific traits exist within a continuum from normal to pathologic. Within this model, vulnerability to psychosis or a specific type of psychosis such as FRS becomes a critical dimension, perhaps even more important than diagnosis. Data indicating that antipsychotic medication can be used to treat psychosis regardless of patients’ diagnosis are consistent with the dimensional approach. Given that certain FRS are used in the DSM-IIIR/IV diagnosis of schizophrenia, it is important to understand the etiologic similarities among psychotic disorders, both at onset and throughout the course of illness. Thus, this research contributes results that have not been previously available consisting of the cumulative percentage of patients with schizophrenia and bipolar disorder who experience FRS during a 20-year period. The current findings may serve to guide diagnostic determination in DSM-V.
Acknowledgments
Funding for this study was provided by National Institute of Mental Health (NIMH) Grant grants MH-26341 and MH-068688 (Dr Harrow); the NIMH had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
The authors have no conflict of interest or financial relationships to disclose.
Cherise Rosen contributed ideas on first rank symptoms, wrote a major part of the paper, and undertook statistical analysis. Linda S. Grossman contributed ideas and wrote major parts of manuscript. Martin Harrow directed the collection of the data, wrote parts of the paper, and contributed ideas on first rank symptoms and psychosis. Aaron Bonner-Jackson contributed in the literature search and analysis. Robert Faull undertook the statistical analysis.
References
- [1].Schneider K. Clinical psychopathology. Stratton; New York: Grune: 1959. [Google Scholar]
- [2].Carpenter WT. The schizophrenia paradigm; a hundred-year challenge. J Nerv Ment Dis. 2006;194(9):639–43. doi: 10.1097/01.nmd.0000235484.45810.df. [DOI] [PubMed] [Google Scholar]
- [3].American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Ed., Text Rev. American Psychiatric Association; Washington (DC): 2000. [Google Scholar]
- [4].Tandon R, Greden JF. Schneiderian first rank symptoms: reconfirmation of high specificity for schizophrenia. Acta Psychiatr Scand. 1987;75:392–6. doi: 10.1111/j.1600-0447.1987.tb02807.x. [DOI] [PubMed] [Google Scholar]
- [5].Kendell RE, Brockington IF, Leff JP. Prognostic implications of six alternative definitions of schizophrenia. Arch Gen Psychiatry. 1979;36:25–31. doi: 10.1001/archpsyc.1979.01780010031002. [DOI] [PubMed] [Google Scholar]
- [6].Carpenter WT, Jr, Strauss JS, Muleh S. Are there pathognomonic symptoms in schizophrenia? An empiric investigation of Schneider’s first-rank symptoms. Arch Gen Psychiatry. 1973;28:847–52. doi: 10.1001/archpsyc.1973.01750360069010. [DOI] [PubMed] [Google Scholar]
- [7].Taylor MA, Abrams R. The phenomenology of mania. A new look at some old patients. Arch Gen Psychiatry. 1973;29:520–2. doi: 10.1001/archpsyc.1973.04200040066011. [DOI] [PubMed] [Google Scholar]
- [8].Carpenter WT, Strauss JS. Cross-cultural evaluation of Schneider’s first rank symptoms of schizophrenia: a report from the International Pilot Study of schizophrenia. Am J Psychiatry. 1974;131:682–7. doi: 10.1176/ajp.131.6.682. [DOI] [PubMed] [Google Scholar]
- [9].Peralta V, Cuesta MJ. Diagnostic significance of Schneider’s first rank symptoms in schizophrenia: comparative study between schizophrenic and non-schizophrenic psychotic disorders. Br J Psychiatry. 1999;174:243–8. doi: 10.1192/bjp.174.3.243. [DOI] [PubMed] [Google Scholar]
- [10].World Health Organization . The international pilot study of schizophrenia. Vol. 1. World Health Organization Press; Geneva: 1973. [Google Scholar]
- [11].Hawk AB, Carpenter WT, Jr, Strauss JS. Diagnostic criteria and five-year outcome in schizophrenia. A report from the International Pilot Study of Schizophrenia. Arch Gen Psychiatry. 1975;32:343–7. doi: 10.1001/archpsyc.1975.01760210077005. [DOI] [PubMed] [Google Scholar]
- [12].Silverstein ML, Harrow M. Schneiderian first-rank symptoms in schizophrenia. Arch Gen Psychiatry. 1981;38:288–93. doi: 10.1001/archpsyc.1981.01780280056006. [DOI] [PubMed] [Google Scholar]
- [13].Stephens JH, Astrup C, Carpenter WT, Jr, Shaffer JW, Goldberg J. A comparison of nine systems to diagnose schizophrenia. Psychiatry Res. 1982;6:127–43. doi: 10.1016/0165-1781(82)90001-4. [DOI] [PubMed] [Google Scholar]
- [14].Conus P, Abdel-Baki A, Harrigan S, Lambert M, McGorry PD. Schneiderian first rank symptoms predict poor outcome within first episode manic psychosis. J Affect Disord. 2004;81:259–68. doi: 10.1016/j.jad.2003.09.003. P. [DOI] [PubMed] [Google Scholar]
- [15].Crow TJ. The continuum of psychosis and its genetic origins: the sixty-fifth Maudsley lecture. Br J Psychiatry. 1990;156:788–97. doi: 10.1192/bjp.156.6.788. [DOI] [PubMed] [Google Scholar]
- [16].Maj M. Critique of the DSM-IV operational diagnostic criteria for schizophrenia. Br J Psychiatry. 1998;172:458–60. doi: 10.1192/bjp.172.6.458. [DOI] [PubMed] [Google Scholar]
- [17].Pierre J. Deconstructing schizophrenia for DSM-IV: challenges for clinical and research agendas. Clin Schizophr Relat Psychoses. 2008:166–74. [Google Scholar]
- [18].Harrow M, Grossman LS, Jobe TH, Herbener ES. Do patients with schizophrenia ever show periods of recovery? A 15 year multi-follow-up Study. Schizophr Bull. 2005;31(3):723–34. doi: 10.1093/schbul/sbi026. [DOI] [PubMed] [Google Scholar]
- [19].Rosen K, Garety P. Predicting recovery for schizophrenia: a retrospective comparison of characteristics at onset of people with single and multiple episodes. Schizophr Bull. 2005;31(3):735–50. doi: 10.1093/schbul/sbi017. [DOI] [PubMed] [Google Scholar]
- [20].Grossman LS, Harrow M, Goldberg JF, Fichtner CG. Outcome of schizoaffective disorder at two long-term follow-ups: comparisons with outcome of schizophrenia and affective disorders. Am J Psychiatry. 1991;148:1359–65. doi: 10.1176/ajp.148.10.1359. [DOI] [PubMed] [Google Scholar]
- [21].Harrow M, Herbener ES, Shanklin A, Jobe TH, Rattenbury F, Kaplan KJ. Follow-up of psychotic outpatients: dimensions of delusions and work functioning in schizophrenia. Schizophr Bull. 2004;30:147–61. doi: 10.1093/oxfordjournals.schbul.a007059. [DOI] [PubMed] [Google Scholar]
- [22].Grossman LS, Harrow M, Rosen C, Faull R. Sex differences in outcome and recovery for schizophrenia and other psychotic disorders: 5 follow-ups over 15-years. Psychiatr Serv. 2006;57:844–50. doi: 10.1176/ps.2006.57.6.844. [DOI] [PubMed] [Google Scholar]
- [23].Harrow M, Grossman LS, Silverstein M, Meltzer ML, Kettering RLA. A longitudinal study of thought disorder in manic patients. Arch Gen Psychiatry. 1986;43:781–5. doi: 10.1001/archpsyc.1986.01800080067009. [DOI] [PubMed] [Google Scholar]
- [24].Harrow M, Jobe TH. How frequent is chronic multiyear delusional activity and recovery in schizophrenia: a 20-year multi–follow-up. Schizophr Bull. 2008 doi: 10.1093/schbul/sbn074. doi:10.1093/schbul/sbn074. Advance Access published on July 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hollingshead AB, Redlich FC. Social class and mental illness: a community study. John Wiley and Sons; New York: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Liberman R, Kopelowicz A. Recovery from schizophrenia: a challenge for the 21st century. Int Rev Psychiatry. 2002;14:245–55. [Google Scholar]
- [27].Noordsy D, Torrey W, Mueser K, Mead S, O’Keefe C, Fox L. Recovery from severe mental illness: an intrapersonal and functional outcome definition. Int Rev Psychiatry. 2002;14:318–26. [Google Scholar]
- [28].Andreasen N, Carpenter W, Kane J, Lasser R, Marder S, Weinberger M. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441–9. doi: 10.1176/appi.ajp.162.3.441. [DOI] [PubMed] [Google Scholar]
- [29].Levenstein DSW, Klein DF, Pollack M, et al. Follow-up study of formerly hospitalized voluntary psychiatric patients: the first two years. Am J Psychiatry. 1966;122:1102–9. doi: 10.1176/ajp.122.10.1102. [DOI] [PubMed] [Google Scholar]
- [30].Strauss J, Carpenter W. The prediction of outcome in schizophrenia: I. Characteristics of outcome. Arch Gen Psychiatry. 1972;17:739–46. doi: 10.1001/archpsyc.1972.01750300011002. [DOI] [PubMed] [Google Scholar]
- [31].Carone BJ, Harrow M, Westermeyer JF. Posthospital course and outcome in schizophrenia. Arch Gen Psychiatry. 1991;48(3):247–53. doi: 10.1001/archpsyc.1991.01810270059008. [DOI] [PubMed] [Google Scholar]
- [32].Andreasen N. DSM and the death of phenomenology in America: an example of unintended consequences. Schizophr Bull. 2006;33(1):108–12. doi: 10.1093/schbul/sbl054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Van Os J, Tamminga C. Deconstructing psychosis. Schizophr Bull. 2007;33:861–2. doi: 10.1093/schbul/sbm066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Abrams R, Taylor M. First-rank symptoms, severity of illness, and treatment response in schizophrenia. Compr Psychiatry. 1973;14:353–5. doi: 10.1016/0010-440x(73)90027-8. [DOI] [PubMed] [Google Scholar]
- [35].Silverstein ML, Harrow M. First-rank symptoms in the postacute schizophrenic: a follow-up study. Am J Psychiatry. 1978;135:1481–6. doi: 10.1176/ajp.135.12.1481. [DOI] [PubMed] [Google Scholar]
- [36].Carpenter WT. Commentaries on “First-Rank symptoms or rank-and-file- symptoms?”. Br J Psychiatry. 1996;169(5):541–2. doi: 10.1192/bjp.169.5.537. [DOI] [PubMed] [Google Scholar]
- [37].Nordgaard J, Arnfred SM, Handest P, Parnas J. The diagnostic status of first-rank symptoms. Schizophr Bull. 2008;34(1):137–54. doi: 10.1093/schbul/sbm044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Mason P, Harrison G, Croudace T, Glazebrook C, Medley I. The predictive validity of a diagnosis of schizophrenia (ISoS0 coordinated by the World Health Organization and the Department of Psychiatry, University of Nottingham. Br J Psychiatry Boulme. 1977;170(4):321–7. doi: 10.1192/bjp.170.4.321. [DOI] [PubMed] [Google Scholar]
- [39].Wing J, Nixon J. Discriminating symptoms in schizophrenia. A report from the international pilot study of schizophrenia. Arch Gen Psychiatry. 1975;32:853–9. doi: 10.1001/archpsyc.1975.01760250045004. [DOI] [PubMed] [Google Scholar]
- [40].Bertelsen A. Schizophrenia and related disorders: experience with current diagnostic systems. Psychopathology. 2002;35:89–93. doi: 10.1159/000065125. [DOI] [PubMed] [Google Scholar]
- [41].Tanenberg-Karant M, Fennig S, Ram R, Krishna J, Jandorf L, Bromet EJ. Bizarre delusions and first-rank symptoms in a first-admission sample: a preliminary analysis of prevalence and correlates. Compr Psychiatry. 1995;36:428–34. doi: 10.1016/s0010-440x(95)90250-3. [DOI] [PubMed] [Google Scholar]


