Arterial hypertension is the most important modifiable risk factor for cardiovascular morbidity and mortality.1 Safe and effective antihypertensive drugs are widely available but the prevalence of uncontrolled hypertension has recently increased.2 Moreover, because of the unacceptably high rates of patients with blood pressures (BPs) above the recommended targets, several device‐based hypertension treatments have been developed and are under clinical investigation.3 These device‐based therapies, among which renal denervation is the most extensively studied, predominantly target the autonomic nervous system.3
In this issue of the Journal of the American Heart Association (JAHA), a novel approach to treat high BP is presented. The Moderato system (BackBeat Medical) is a dual‐chamber, rate‐responsive, implantable pulse generator that takes advantage of the fact that left ventricular (LV) filling and thereby cardiac output can be reduced by shortening the atrioventricular coupling interval.4 This is pathophysiologically relevant since BP is determined by cardiac output and peripheral vascular resistance. To prevent a compensatory activation of the sympathetic nervous system after short‐interval atrioventricular pacing with subsequent reductions in cardiac output, the device intermittently and asymmetrically introduces short sequences of 1 to 3 beats of longer atrioventricular delay (eg, alternating 20–80 ms and 100–180 ms intervals).4 After the results of the prospective, single‐group MODERATO I study,4 the results of the sham‐controlled MODERATO II trial were presented as late‐breaking science at the Transcatheter Cardiovascular Therapeutics 2019 annual conference and are now reported in this issue by Kalarus and colleagues.5
In the double‐blind, randomized MODERATO II trial, 68 patients (43% of whom were women) with uncontrolled hypertension (daytime ambulatory systolic BP [SBP] ≥130 mm Hg and office SBP ≥140 mm Hg) despite treatment with at least 1 antihypertensive medication and an indication for the implantation (68% of the patients) or replacement (32% of the patients) of a dual‐chamber pacemaker underwent Moderato device implantation at 13 European centers. Of note, the BP inclusion criteria are somewhat uncommon for hypertension trials as an average daytime ambulatory SBP >130 mm Hg would not be considered elevated by most guidelines6 and inclusion of patients with a 24‐hour SBP <125 mm Hg is not supported by current consensus documents.7 Patients with permanent atrial fibrillation or a history of significant paroxysmal atrial fibrillation/flutter burden, reduced LV ejection fraction <50%, and advanced chronic kidney disease (estimated glomerular filtration rate <30 mL/min per 1.73 m2) were excluded. If uncontrolled hypertension was confirmed after the 1‐month run‐in period (daytime ambulatory SBP ≥125 mm Hg), the patients were randomized in a 1:1 ratio to treatment (cardiac neuromodulation therapy [CNT]‐on) or control (CNT‐off). A total of 21 patients (31%) fell below the BP inclusion criterion during the run‐in period and were consequently excluded. The primary efficacy end point, between‐group difference of the change in 24‐hour ambulatory SBP, for which the trial was powered, was met. In the treatment group, 24‐hour ambulatory SBP immediately dropped after the activation of CNT and the BP‐lowering effect was maintained through 6 months of follow‐up (between‐group difference at 6 months: −8.1 mm Hg; 95% CI, −14.2 to −1.9 [P=0.012]). Although the baseline BP was lower, the relative change in 24‐hour ambulatory SBP in the treatment group was larger than in other sham‐controlled trials in device‐based hypertension treatment (Figure). Trials for device‐based therapies have taught us that nonadherence is a major confounder in hypertension trials.8 The current study, however, did not objectively assess drug adherence. A total of 29 medication changes (17 increases and 12 decreases) were documented between baseline and 6 months. As there were more dose increases reported in the control group, the true treatment effect may not have been fully estimated.
Figure 1. Absolute and relative change in 24‐hour ambulatory systolic blood pressure (SBP) in sham‐controlled trials of device‐based therapies for the treatment of hypertension.
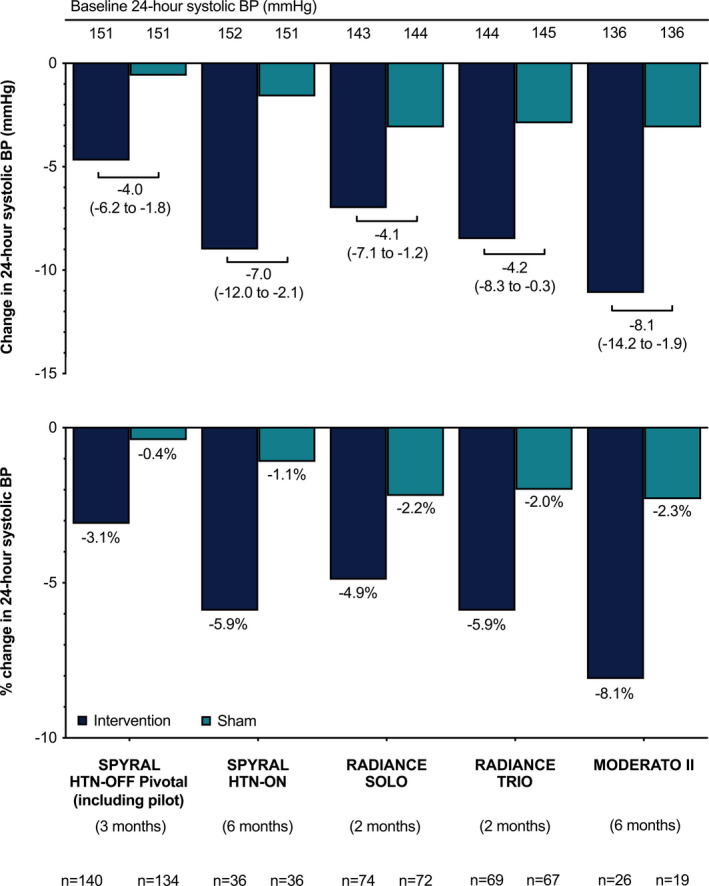
Data are presented as mean (mm Hg) and 95% CIs.
Effective in Isolated Systolic Hypertension
Compared with patients included in the sham‐controlled renal denervation trials,9, 10, 11, 12 the patients herein were older and had more comorbidities but had substantially lower baseline ambulatory BP values (Table). Importantly, the BP‐lowering effects were shown in a population in which 81% of the patients had isolated systolic hypertension (office SBP ≥140 mm Hg and diastolic BP <90 mm Hg). Elderly patients predominantly have isolated systolic hypertension (65% of patients aged >60 years with hypertension)13; however, these patients were purposely excluded from the most recent sham‐controlled trials investigating other device‐based therapies, such as renal denervation and baroreceptor stimulation. The reason for this is that patients with isolated systolic hypertension, characterized by high aortic stiffness and the subsequent inability to dilate and decrease vascular resistance, appear to respond less to neuromodulation with renal denervation.14 In the MODERATO II trial, possibly because of the high proportion of patients with isolated systolic hypertension (mean 24‐hour diastolic BP at baseline was normal: 74.9±7.1 mm Hg), there was no significant change in 24‐hour diastolic BP between baseline and 6 months (between‐group difference, +2.5 mm Hg; P=0.178).
Table 1.
Key Characteristics of Placebo‐Controlled Trials
| RADIANCE‐HTN SOLO (2018) | RADIANCE‐HTN TRIO (2021) | SPYRAL HTN‐OFF MED Pivotal (2020) | SPYRAL HTN‐ON MED (2018) | MODERATO II (2021) | |
|---|---|---|---|---|---|
| Mean age, y | 54 | 53 | 53 | 53 | 74 |
| Women, % | 42 | 20 | 34 | 16 | 36 |
| Number of antihypertensive drugs (inclusion criterion) | 0 | 3 | 0 | 1–3 | ≥1 |
| Mean number of antihypertensive drugs at randomization | 0 | 3 | 0 | 2.2 | 3.3 |
| BP inclusion criterion, mm Hg | Daytime ambulatory BP: 135–164/85–104 | Daytime ambulatory SBP: ≥135/85 |
24 h‐SBP: 140–169 OBP: 150–179/≥90 |
24 h‐SBP: 140–169 OBP: 150–179/≥90 |
Daytime SBP: ≥130 (≥125 after run‐in) Office SBP ≥140 |
| Mean office SBP at baseline, mm Hg | 154 | 155 | 163 | 164 | 154 |
| Mean office DBP at baseline, mm Hg | 100 | 100 | 101 | 101 | 82 |
| Mean 24‐h SBP at baseline, mm Hg | 150 | 144 | 151 | 152 | 136 |
| Mean 24‐h DBP at baseline, mm Hg | 93 | 89 | 99 | 97 | 73 |
| Follow‐up duration, mo | 2 | 2 | 3 | 6 | 6 |
BP indicates blood pressure; DBP, diastolic blood pressure; OBP, office blood pressure; and SBP, systolic blood pressure.
Strengths of the Study Design
The 1‐month run‐in period was particularly important to reduce the Hawthorne effect8 but also to ensure stabilization of BP and normalization of daily life activities since some patients may have been limited by the underlying bradycardic arrhythmias requiring pacemaker implantation (43% of the patients had atrioventricular block grade II or III, and 34% had sick sinus syndrome). Although 21 patients with a marked BP reduction during the run‐in period (mean decrease in ambulatory SBP of 15 mm Hg) were excluded, which possibly reduced the variability in BP response, 37% of the patients in the control group (compared with 54% of the patients in the treatment group) had a decrease of >10 mm Hg in ambulatory SBP between baseline and 6 months.
Device implantation without activation of the CNT can be regarded as an appropriate sham treatment to reduce placebo effects, as patients did not experience any specific symptoms associated with the short atrioventricular delay beats.8 Unfortunately, the blinding of patients and investigators was not systematically assessed.
Open Questions
Is the Device Safe in the Long Term?
Importantly, serious adverse events (7 events in 4 patients) and protocol‐prespecified primary safety end point events (3 events in 2 patients) occurred only in the control group. Compared with the control group, there was a trend to a drop in LV ejection fraction at 6 months in the treatment group (−1.3%±5.4% versus −5.4%±7.5%; P=0.09). The reduction is, in part, expected and caused by the mechanism of action (reduction in LV preload). However, larger studies with longer follow‐up must be performed to assess whether right ventricular pacing (essential for BP‐lowering efficacy) increases the risk of heart failure development. Especially in heart failure with reduced ejection fraction, right ventricular pacing causing electrical and mechanical LV dyssynchrony has been shown to increase the risk of atrial fibrillation, heart failure events, and death.15, 16 Moreover, there is growing evidence that right ventricular pacing may also be detrimental in patients with normal LV ejection fraction.17, 18 In addition, short atrioventricular coupling intervals might result in myocardial remodeling because the atria contract against partially closed atrioventricular valves, with unknown long‐term consequences on atrial anatomy and function. All of these potential adverse effects need to be investigated in future studies with appropriate an sample size and longer follow‐up.
Can We Expect Pacemakers to Be Implanted in Patients Without Arrhythmias?
In contrast to previous trials investigating device‐based therapy,3 the patients included in the MODERATO II trial had an indication for the implantation (68% of the patients) or replacement (32% of the patients) of a dual‐chamber pacemaker. Hence, the patients had not undergone a dedicated invasive procedure for their hypertension treatment. However, if further trials confirm the immediate BP‐lowering effect, one might speculate whether CNT is reasonable as an antihypertensive standalone treatment in patients without bradycardic arrhythmia. Unlike other device‐based procedures, such as renal denervation, in which no implant remains in the body, pacemaker and cardioverter‐defibrillator implantations are more frequently complicated by severe (incidence of perforation: 0.1%–1.5%; infection: 0.6%–3.4%; lead dislodgement: 1.2%–3.3%) and also fatal (incidence of 30‐day mortality: 0.6%–1.4%) complications.19 Even if the BP‐lowering effect of CNT is sustained over the long term, the effect requires a functioning battery; therefore, battery replacements may become necessary especially in young patients.
The authors should be commended for conducting and completing another randomized, sham‐controlled device‐based hypertension trial, which undoubtedly represents the gold standard to assess the efficacy and safety of novel invasive BP‐lowering technologies.7 The placebo‐controlled MODERATO II trial has shown that CNT is feasible and acceptably safe in the short term in patients with hypertension and an indication for pacemaker implantation. Particularly, the clinically relevant and immediate drop in ambulatory SBP, as well as its efficacy in patients with isolated systolic hypertension, are to be highlighted. However, larger studies with longer follow‐up are needed to confirm the long‐term safety before any thought can be given to the device's role in clinical practice.
Disclosures
Mahfoud is supported by Deutsche Gesellschaft für Kardiologie, and Deutsche Forschungsgemeinschaft (SFB TRR219) and has received scientific support and speaker honoraria from Bayer, Boehringer Ingelheim, Medtronic, and ReCor Medical. Lauder has no disclosures to report.
(J Am Heart Assoc. 2021;10:e022622. DOI: 10.1161/JAHA.121.022622.)
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
For Disclosures, see page 4.
See Article by Kalarus et al.
References
- 1.Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, Brauer M, Burnett R, Cercy K, Charlson FJ, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1724. DOI: 10.1016/S0140-6736(16)31679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324:1190. DOI: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahfoud F, Schlaich MP, Lobo MD. Device therapy of hypertension. Circ Res. 2021;128:1080–1099. DOI: 10.1161/CIRCRESAHA.121.318091 [DOI] [PubMed] [Google Scholar]
- 4.Neuzil P, Merkely B, Erglis A, Marinskis G, de Groot JR, Schmidinger H, Rodriguez Venegas M, Voskuil M, Sturmberger T, Petru J, et al. Pacemaker‐mediated programmable hypertension control therapy. J Am Heart Assoc. 2017;6:e006974. DOI: 10.1161/JAHA.117.006974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalarus Z, Merkely B, Neužil P, Grabowski M, Mitkowski P, Marinskis G, Erglis A, Kazmierczak J, Sturmberger T, Sokal A, et al. A pacemaker‐based cardiac neuromodulation therapy in hypertensive patients: a pilot study. J Am Heart Assoc. 2021;10:e020492. DOI: 10.1161/JAHA.120.020492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. DOI: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 7.Mahfoud F, Azizi M, Ewen S, Pathak A, Ukena C, Blankestijn PJ, Böhm M, Burnier M, Chatellier G, Durand Zaleski I, et al. Proceedings from the 3rd European Clinical Consensus Conference for clinical trials in device‐based hypertension therapies. Eur Heart J. 2020;41:1588–1599. DOI: 10.1093/eurheartj/ehaa121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lauder L, da Costa BR, Ewen S, Scholz SS, Wijns W, Lüscher TF, Serruys PW, Edelman ER, Capodanno D, Böhm M, et al. Randomized trials of invasive cardiovascular interventions that include a placebo control: a systematic review and meta‐analysis. Eur Heart J. 2020;41:2556–2569. DOI: 10.1093/eurheartj/ehaa495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Townsend RR, Mahfoud F, Kandzari DE, Kario K, Pocock S, Weber MA, Ewen S, Tsioufis K, Tousoulis D, Sharp AS, et al. Catheter‐based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN‐OFF MED): a randomised, sham‐controlled, proof‐of‐concept trial. Lancet. 2017;390:2160–2170. DOI: 10.1016/S0140-6736(17)32281-X [DOI] [PubMed] [Google Scholar]
- 10.Böhm M, Kario K, Kandzari DE, Mahfoud F, Weber MA, Schmieder RE, Tsioufis K, Pocock S, Konstantinidis D, Choi JW, et al. Efficacy of catheter‐based renal denervation in the absence of antihypertensive medications (SPYRAL HTN‐OFF MED Pivotal): a multicentre, randomised, sham‐controlled trial. Lancet. 2020;395:1444–1451. DOI: 10.1016/S0140-6736(20)30554-7 [DOI] [PubMed] [Google Scholar]
- 11.Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Davies J, Basile J, Kirtane AJ, Wang Y, Lobo MD, et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE‐HTN SOLO): a multicentre, international, single‐blind, randomised, sham‐controlled trial. Lancet. 2018;391:2335–2345. DOI: 10.1016/S0140-6736(18)31082-1 [DOI] [PubMed] [Google Scholar]
- 12.Azizi M, Sanghvi K, Saxena M, Gosse P, Reilly JP, Levy T, Rump LC, Persu A, Basile J, Bloch MJ, et al. Ultrasound renal denervation for hypertension resistant to a triple medication pill (RADIANCE‐HTN TRIO): a randomised, multicentre, single‐blind, sham‐controlled trial. Lancet. 2021;397:2476–2486. DOI: 10.1016/S0140-6736(21)00788-1 [DOI] [PubMed] [Google Scholar]
- 13.Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D. Prevalence of hypertension in the US adult population. Hypertension. 1995;25:305–313. DOI: 10.1161/01.HYP.25.3.305 [DOI] [PubMed] [Google Scholar]
- 14.Mahfoud F, Bakris G, Bhatt DL, Esler M, Ewen S, Fahy M, Kandzari D, Kario K, Mancia G, Weber M, et al. Reduced blood pressure‐lowering effect of catheter‐based renal denervation in patients with isolated systolic hypertension: data from SYMPLICITY HTN‐3 and the Global SYMPLICITY Registry. Eur Heart J. 2017;38:93–100. DOI: 10.1093/eurheartj/ehw325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The DAVID Trial Investigators *. Dual‐chamber pacing or ventricular backup pacing in patients with an implantable defibrillator. JAMA. 2002;288:3115. DOI: 10.1001/jama.288.24.3115 [DOI] [PubMed] [Google Scholar]
- 16.Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, Shinn T, St. John Sutton M. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368:1585–1593. DOI: 10.1056/NEJMoa1210356 [DOI] [PubMed] [Google Scholar]
- 17.Shen LI, Jhund PS, Docherty KF, Petrie MC, Anand IS, Carson PE, Desai AS, Granger CB, Komajda M, McKelvie RS, et al. Prior pacemaker implantation and clinical outcomes in patients with heart failure and preserved ejection fraction. JACC Heart Fail. 2019;7:418–427. DOI: 10.1016/j.jchf.2018.12.006 [DOI] [PubMed] [Google Scholar]
- 18.Zhang XH, Chen H, Siu CW, Yiu KH, Chan WS, Lee KL, Chan HW, Lee SW, Fu GS, Lau CP, et al. New‐onset heart failure after permanent right ventricular apical pacing in patients with acquired high‐grade atrioventricular block and normal left ventricular function. J Cardiovasc Electrophysiol. 2008;19:136–141. DOI: 10.1111/j.1540-8167.2007.01014.x [DOI] [PubMed] [Google Scholar]
- 19.Burri H, Starck C, Auricchio A, Biffi M, Burri M, D’Avila A, Deharo JC, Glikson M, Israel C, Lau CP, et al. EHRA expert consensus statement and practical guide on optimal implantation technique for conventional pacemakers and implantable cardioverter‐defibrillators: endorsed by the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), and the Latin‐American Heart Rhythm Society (LAHRS). Europace. 2021:23:983–1008. DOI: 10.1093/europace/euaa367 [DOI] [PMC free article] [PubMed] [Google Scholar]


