ABSTRACT
Background: Misophonia is a disorder in which patients suffer from anger or disgust when confronted with specific sounds such as loud chewing or breathing, causing avoidance of cue-related situations resulting in significant functional impairment. Though the first treatment studies with cognitive behavioural therapy (CBT) showed promising results, an average of 50% of the patients has not improved much clinically.
Objective: The aim of this pilot study was to assess the effectiveness of eye movement desensitization and reprocessing (EMDR) therapy as a trauma-focused approach in treating misophonia symptoms.
Method: A sample of 10 adult participants with misophonia was studied at the outpatient clinic of the Academic Medical Center in Amsterdam. Participants were either on the waiting list for CBT or non-responders to CBT. EMDR was focused on misophonia-related emotionally disturbing memories and delivered in a mean of 2.6 sessions of 60–90 minutes. Pre- and post-treatment self-assessed ratings of misophonia symptoms (AMISOS-R, primary outcome), of general psychopathology (SCL-90-R) and of quality of life (SDS) were administered. The co-primary outcome was the Clinical Global Impression Improvement scale (CGI-I).
Results: A paired t-test (n = 8) showed improvement on the primary outcome (−6.14 [MD], 5.34 [SD]) on the AMISOS-R (P = .023). Three of the eight patients showed clinically significant improvement measured with the CGI-I. No significant effect on secondary outcomes was found.
Conclusions: These preliminary results suggest that EMDR therapy focused on emotionally disturbing misophonia-related memories can reduce misophonia symptoms. RCTs with sufficient sample sizes are required to firmly establish the value of EMDR therapy for misophonia.
KEYWORDS: Misophonia, eye movement desensitization and reprocessing, trauma-focused psychotherapy, feasibility, preliminary effect, case series
HIGHLIGHTS
This pilot study investigated the potential benefits of EMDR for 10 patients with misophonia.
Three of the seven completers showed clinical improvement in misophonia symptoms within a mean of 2.6 sessions.
The exploratory nature of this study makes further research necessary.
Short abstract
Antecedentes: La misofonía es un trastorno en el que los pacientes sufren de rabia o desagrado cuando se enfrentan a sonidos específicos como la masticación o la respiración ruidosa, lo que provoca la evitación de las situaciones relacionadas con el estímulo y da lugar a un deterioro funcional significativo. Aunque los primeros estudios de tratamiento con terapia cognitivo-conductual (TCC) mostraron resultados prometedores, una media del 50% de los pacientes no ha mejorado mucho clínicamente.
Objetivo: El objetivo de este estudio piloto fue evaluar la eficacia de la terapia de desensibilización y reprocesamiento por movimientos oculares (EMDR) como enfoque centrado en el trauma para tratar los síntomas de la misofonía.
Método: Se estudió una muestra de 10 participantes adultos con misofonía en la clínica ambulatoria del Centro Médico Académico de Ámsterdam. Los participantes estaban en lista de espera para la TCC o no respondían a la TCC. La EMDR se centró en los recuerdos emocionalmente perturbadores relacionados con la misofonía y se aplicó en una media de 2,6 sesiones de 60–90 minutos. Se administraron calificaciones autoevaluadas antes y después del tratamiento de los síntomas de misofonía (AMISOS-R, resultado primario), de psicopatología general (SCL-90-R) y de calidad de vida (SDS). El resultado co-primario fue la escala de Mejora de la Impresión Clínica Global (CGI-I).
Resultados: Una prueba t pareada (n=8) mostró una mejora en el resultado primario (−6,14 [DM]), 5,34 [DE] en la AMISOS-R (P= .023). Tres de los ocho pacientes mostraron una mejora clínicamente significativa medida con la CGI-I. No se encontró ningún efecto significativo en los resultados secundarios.
EMDR para la misofonía Estos resultados preliminares sugieren que la terapia EMDR centrada en los recuerdos emocionalmente perturbadores relacionados con la misofonía puede reducir los síntomas de ésta. Se requieren ECAs con tamaños de muestra suficientes para establecer firmemente el valour de la terapia EMDR para la misofonía.
PALABRAS CLAVE: Misofonía, desensibilización y reprocesamiento por movimientos oculares, psicoterapia centrada en el trauma, viabilidad, efecto preliminar, serie de casos
Short abstract
背景:恐音症是一种疾病, 患者在面对如大声咀嚼或呼吸等特定声音时会感到愤怒或厌恶, 从而回避与相关情况提示物, 导致显著的功能障碍。尽管认知行为疗法 (CBT) 的首批治疗研究显示出有希望的结果, 平均 50% 的患者无明显临床改善。
目的:本试点研究旨在评估眼动脱敏和再加个 (EMDR) 疗法作为一种治疗恐音症症状的聚焦创伤方法的有效性。
方法:在阿姆斯特丹学术医疗中心门诊对一个10 名患有恐音症的成年参与者样本进行了研究。参与者要么在 CBT 等候名单上, 要么对 CBT 没有反应。 EMDR专注于与恐音症相关的情绪不安记忆, 以平均 2.6 次, 每次 60–90 分钟进行。治疗前, 后对恐音症症状 (AMIOSS-R, 主要结果), 一般精神病 (SCL-90-R) 和生活质量 (SDS) 进行自我评估。共同主要结果是临床总体印象改善量表 (CGI-I)。
结果:配对 t检验 (n=8) 显示主要结果的改善 (AMISOS-R: −6.14 [MD], 5.34 [SD] (P= .023)) 。8 名患者中有 3 名表现出临床上CGI-I的显著改善。未发现次要结果的显著效应。
结论:这些初步结果表明 EMDR 治疗专注于情绪不安的恐音症相关记忆可以减少恐音症症状。需要具有足够样本量的 RCT 来确定 EMDR 治疗恐音症的价值。
关键词: 恐音症, 眼动脱敏和再加工, 聚焦创伤心理治疗, 可行性, 初步效果, 病例系列, EMDR
1. Background
Misophonia is a disorder in which patients suffer from anger or disgust when confronted with specific sounds such as loud chewing or breathing, causing avoidance of cue-related situations resulting in significant functional impairments (Jager et al., 2020a; Schröder, Vulink, & Denys, 2013). Misophonia patients can often not eat, sleep or work in company and most social and family relations are negatively affected. Since the onset of symptoms is around the age of 13 (Jager et al, 2020a; Schröder et al., 2013), misophonia patients develop a lifelong coping behaviour of avoidance, like walking away or using music or earplugs to camouflage trigger sounds. There is debate about the nature of the disorder, other research groups emphasize its audiological or neurological nature. Recently, a Delphi Process study led to an agreement of experts of at least 80% on the consensus definition of misophonia (Swedo et al., 2021).
Estimates of the incidence of misophonia in adults vary (Naylor, Caimino, Scutt, Hoare, & Baguley, 2020; Zhou, Wu, & Storch, 2017). Solid epidemiological studies are missing, also as a consequence of the ongoing debate about the definition of misophonia. Comorbidity is relatively low: 40% (Erfanian, Kartsonaki, & Keshavarz, 2019) to 72% (Jager et al., 2020a) of subjects diagnosed with misophonia do not report another Axis I psychiatric disorder. Hence, misophonia is an impairing and common disorder for which effective treatment is urgently needed, given the huge impact on family and social relations.
The Amsterdam University Medical Center of Psychiatry, location AMC (Amsterdam UMC) has developed the first protocoled treatment with cognitive behavioural therapy (CBT) for misophonia (Van Loon et al., 2019). CBT consists of four main components: task concentration exercises, positive affect labelling, stimulus manipulation, and arousal reduction. The first treatment studies with CBT showed promising results, respectively, 48% (Schröder, Vulink, Van Loon, & Denys, 2017) and 37% of the patients (Jager et al., 2020b) showed significant clinical improvement with CBT post treatment. However, CBT is ineffective for more than half of misophonia patients, who therefore require alternative treatments. Except for CBT, some data suggest Tinnitus Retraining Therapy offers an 83% success rate for misophonia (Jastreboff & Jastreboff, 2014).
EMDR therapy is an evidence-based psychological treatment that is effective for post-traumatic stress disorder (PTSD) and its comorbid symptoms (De Jongh, Amann, Hofmann, Farrell, & Lee, 2019; International Society of Traumatic Stress Studies [ISTSS], 2019; National Institute for Health and Care Excellence, 2018). In the last decades, the insight that unprocessed traumatic memories (not only criterion A events) play an important role in the development and maintenance of a variety of mental health conditions led to the use of EMDR therapy as a trauma-focused treatment for a broader spectrum of disorders (Shapiro, 2018). Evidence for its effectiveness for disorders beyond PTSD is growing, such as for major depressive disorder, bipolar disorder, psychosis, anxiety disorders, obsessive compulsive disorder, substance use disorder, and pain (Matthijssen et al., 2020; Maxfield, 2019). In a recent meta-analysis of RCTs (Cuijpers, Veen, Sijbrandij, Yoder, & Cristea, 2020), significant results were found for EMDR in phobias and test anxiety, but with a high risk of bias. Overall, the authors concluded that there is not enough evidence for the use of EMDR for mental health problems other than PTSD (Cuijpers et al., 2020). More research on EMDR and larger RCTs with clear-cut results are needed, as in the majority of the RCTs EMDR is merely used for comorbid PTSD or as an add-on to treatment-as-usual (Meyerbröker, Emmelkamp, & Merkx, 2019).
The theoretical model behind EMDR, the adaptive information processing model (AIP), suggests that ‘dysfunctionally stored’ memories may have an atiological and maintaining role for a broad spectrum of symptoms and problems, not limited to PTSD (Hase, Balmaceda, Ostacoli, Liebermann, & Hofmann, 2017; Shapiro, 2018). Desensitization and reprocessing of these disturbing memories and images with EMDR will result in reduction of the vividness and emotionality of unpleasant mental representations (Gunter & Bodner, 2008).
Up to date it is unknown if there might be a connection between misophonia symptoms and related disturbing experiences or memories. Only one case description found a decrease in misophonia symptoms after EMDR treatment (Vollbehr & ten Broeke, 2017). When relevant memories are found a trauma-focused approach such as EMDR therapy could reduce misophonia symptoms. This pilot study aimed first to identify relevant experiences related to misophonia symptoms and secondly to reduce misophonia symptoms with EMDR therapy for reprocessing maladaptive implicit memories. Therefore, with this pilot study we assess the feasibility and preliminary effectiveness of EMDR in reducing misophonia symptoms and improving general mental functioning and quality of life.
2. Methods
The study site was the outpatient clinic of the department of psychiatry of the Amsterdam University Medical Center (Amsterdam UMC, location AMC, the Netherlands). All patients gave written informed consent. The study was approved by the AMC medical ethics committee and carried out in accordance with the Declaration of Helsinki.
2.1. Participant selection, recruitment, and enrolment
A total of 14 patients were selected from September 2015 to July 2017 from the outpatient clinic at the Amsterdam UMC (see Figure 1). All patients were referred by their General Practitioners for treatment of invalidating misophonia symptoms. All had received a psychiatric assessment at our clinic. Presence of comorbid Axis I disorders according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) diagnostic criteria was validated at baseline by the MINI-International Neuropsychiatric Interview Plus (MINI-plus) (Sheehan et al., 1997; Sheehan et al., 1998; Van Vliet & De Beurs, 2007).
Figure 1.
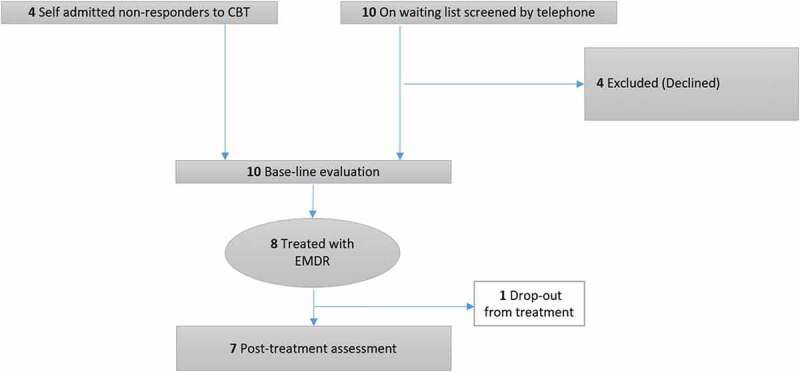
Consort diagram
Recruited patients were either on the waiting list for treatment or non-responders to CBT. Ten subsequently referred patients, who were most recently added to the waiting list, were approached in order of registration. Six were included, four patients were not willing to participate. We also included four non-responders; patients who completed CBT without positive results at the AMC in the period of this study and searched for help and further treatment.
Inclusion criteria were diagnosis of misophonia (Schröder et al., 2013) and aged between 18 and 65 years. Exclusion criteria were: previous EMDR treatment for misophonia, the presence of depression and anxiety disorder as a primary diagnosis, bipolar disorder, autism spectrum disorders, schizophrenia or any other psychotic disorder, substance-related disorder during the past 6 months, any structural central nervous system disorder or stroke within the last year, currently taking benzodiazepines or stimulants, patients at risk for suicide and patients with language barriers or illiteracy.
2.2. EMDR therapy
The EMDR therapy was conducted according to the standard eight-phase protocol by Shapiro using the Dutch translation of the EMDR protocol (De Jongh & ten Broeke, 2019; Shapiro, 2001). The standard EMDR treatment protocol (Shapiro, 2018) consists of the following phases: 1. History Taking (including discussion of the rationale for therapy and case conceptualization/idiographic formulation of the patient’s difficulties); 2. Preparation (preparation for reprocessing of target trauma memories and equipping patients with strategies to better self-regulate during trauma reprocessing work); 3. Assessment (the identification of a specific target memory/image as well as associated negative cognitions, disturbing emotions or bodily sensations; a positive cognition that is preferable to the negative one is also identified); 4. Desensitization and reprocessing (involving the repetitive use of bilateral stimulation, for example, the tracking of a moving object, while the patient is asked to simultaneously focus on the image, the negative cognition, and the disturbing emotion or body sensation until he/she reports a marked reduction in distress associated with these experiences); 5. Installation (in which the patient is encouraged to associate the trauma memory with the positive cognition previously identified, or a new more adaptive positive cognition); 6. Body scan (designed to target any residual negative/uncomfortable physical sensation or bodily tension associated with the trauma memory); 7. Closure (generally involving the use of distress management and tolerance strategies before the end of the session); 8. Re-evaluation (where the patient and therapist reassess the previous target to evaluate whether additional work is necessary before proceeding further with the intervention).
The memories EMDR focused on were identified (phase 1) following a standardized search strategy called time-line path in the first session (first method; de Jongh et al., 2010). This strategy is used for a broad spectrum of symptoms beyond PTSD and helps to develop a case conceptualization in terms of a relationship between memories of significant events, on one hand, and clients' current symptoms, on the other hand. It is also suggested for the case conceptualization for EMDR for misophonia (Vollbehr & ten Broeke, 2017). The time-line path deals with symptoms whereby memories of the aetiological and aggravating events can be specified on a time line. For this pilot study, the main questions of the therapist were: ‘When did your misophonia symptoms start and when did they get worse?’. The events or experiences found were target memories for EMDR and processed with EMDR. The order of targets was set; starting with targets that were related to the onset of the misophonia symptoms and subsequently, the memories of the events after which symptoms worsened. For all identified events a Subjective Units of Distress Scale (SUD) score was given between 0 and 10 (0 meaning no distress to 10 meaning highest distress) that was felt when the memory was kept in mind. Hereafter, the standard protocol was first applied to the first target memory in time. A substantial reduction in SUD was required to move to the next memory. In all the following sessions, memories were processed. Eye movements were applied as a dual-attention stimulus. Each EMDR session lasted 60–90 minutes. Treatment was ended when the Subjective Units of Distress Scale (SUD) score was zero for all indexed misophonia-related memories identified on the time-line. All patients were equally involved in the eight phases of the standard protocol. The total number of sessions varied across patients depending on the number of targets and the speed of desensitization.
The therapist was a licenced clinical psychologist (IJ) with appropriate training (level II trained) in EMDR and extensive experience in CBT for obsessive-compulsive and related disorders and misophonia in particular.
2.3. Assessments
Patients were assessed at baseline (T1), and post treatment (T2). At T2 an independent assessor rated all patients in a clinical interview. This independent assessor was a cognitive behavioural worker with extensive experience in CBT for misophonia.
2.4. Measures
2.4.1. Primary outcomes
Misophonia symptoms were measured using the revised Amsterdam Misophonia Scale (AMISOS-R) (Schröder & Spape, 2014). It consists of 10 items with scores ranging from 0 to 40. Higher scores indicate more severe misophonia; 0–10: normal to subclinical misophonia; 11–20: mild misophonia; 21–30: moderate severe misophonia; 31–40: severe to extreme misophonia. (see supplementary appendix). This improved version of the A-MISO-S (Schröder et al., 2013) is in the process of validation; Preliminary results of the validation show reliability of the scale was good (α = .84), as well as its validity (r = .87, p < .01).
The co-primary outcome was CGI-Improvement (CGI-I) (Guy, 1976) as objective observer ratings. The CGI-I consists of one question: ‘Compared to the patient’s condition at admission to the project this patient’s condition is: 1 = very much improved since the initiation of treatment; 2 = much improved; 3 = minimally improved; 4 = no change from baseline (the initiation of treatment); 5 = minimally worse; 6 = much worse; 7 = very much worse since the initiation of treatment.’
Responses are defined by a CGI-I scale score <3, usually used to define response (Bandelow, Baldwin, Dolberg, Andersen, & Stein, 2006). Full response was defined by 25% reduction (or more) in the AMISOS-R and a CGI-I score <3. Partial response was defined by either a 25% reduction (or more) on the AMISOS-R or a CGI-I score <3.
2.4.2. Secondary outcomes
General mental dysfunction was assessed with the Symptom Checklist-90-R (SCL-90-R; Arrindell & Ettema, 1986; Derogatis, Lipman, & Covi, 1973). The total score is 90 to 450, with higher scores indicating more general psychopathology. Quality of life was assessed with the Sheehan Disability Scale (SDS; Sheehan, 1983). The SDS has three domains; Work, Social and Family, and the range per domain is 0 to 10. The total score was 0 to 30, with higher scores indicating more impairment.
2.4.3. Qualitative outcome
The perceived intensity of disturbance or distress of an image or an emotional memory being recalled is measured with the Subjective Units of Distress (SUD) scale. This score is indexed on an 11-point Likert scale, ranging from 0 (‘no disturbance at all’) to 10 (‘greatest level of disturbance’) (Shapiro, 2018). Participants were requested to indicate the SUD score verbally to the therapist for all identified events at the start, during and after EMDR therapy. The SUD scores are displayed at Table 4.
Table 4.
EMDR treatment information of the 10 included patients with misophonia
| Patient | Included | Number of EMDR sessions | Target memories | SUD scores PRE |
AMISOS-R PRE | AMISOS-R POST | CGI-I |
|---|---|---|---|---|---|---|---|
| 1 | No | 0 | - | - | 28 | - | - |
| 2 | Yes | 2 | Misophonia related panic attack on holiday (onset) Suicidal ideations following a misophonia related fight (increase) |
7 4 |
32 | 33 | 4 |
| 3 | Yes | 4 | Tension during meal caused by aggressive father (onset) Misophonia symptoms during the silence following death of caring grandmother (onset) Fight with friend about binge eating as coping (increase) |
10 8 8 |
23 | 9 | 2 |
| 4 | Yes | 1 | Misophonia related fight in school and being punished by teacher (onset) | 5 | 27 | 17 | 4 |
| 5 | No | 0 | - | - | 36 | - | - |
| 6 | Yes | 2 | Misophonia related fight on holiday (onset) | 9 | 32 | 30 | 4 |
| 7 | Yes | 3 | Misophonia related fight at dining table followed by pulling hair and snacking (onset) 8-hour drive to a holiday destination with snacking family (increase) |
10 7 |
36 | 31 | 3 |
| 8 | Yes | 3 | Misophonia related fight with father (prototypical situation) Overhearing parents judgemental comments on misophonia (increase) |
8 7 |
33 | 30 | 4 |
| 9 | Yes | 3 | Misophonia triggered by a disabled child who sniffed in class (onset) Misophonia-related snapping at sibling during grandmothers’ funeral (increase) |
9 9 |
30 | 20 | 2 |
| 10 | Yes | 1 | Almost choking on a candy on holiday (onset) | 7 | 31 | - | - |
The severity of posttraumatic stress symptoms was measured on indication (if the presence of these symptoms was assumed) with the Impact of Events Scale (IES; Brom & Kleber, 1985; Horowitz, Wilner, & Alvarez, 1979; van der Ploeg, Mooren, Kleber, van der Velden, & Brom, 2004). The Impact of Events Scale has two subscales (avoidance and intrusions) and a total score ranging from 15 to 60, with higher scores indicating more PTSD symptoms and a cut-off score of 33 or more (Creamer, Bell, & Failla, 2003).
2.4.4. Statistical analysis
Since this is a pilot study no formal sample size calculations were performed. We tested the decrease in symptom severity with a paired t-test; the dependent variable was AMISOS-R total score, and independent factors were assessments (T1, T2). An additional intention-to-treat analysis was performed, including all patients who received EMDR therapy, irrespective of whether they completed the therapy. Missing values were hereby imputed by the last observation carried forward (LOCF).
All analyses were all based on 2-tailed t-tests. For both co-primary and secondary outcomes P < .05 was considered to be statistically significant. All results should be considered as exploratory. In all analyses for normal distribution was controlled by Shapiro–Wilk and a visual check of the histogram. Data were analysed using IBM SPSS Statistics version 25.
3. Results
3.1. Participant flow and characteristics
A total of 10 patients (9 [90%] female; mean [SD] age, 35 [14,53] years) were included (Table 1). Mean (SD) age of onset was 13.10 (9.75). Fifty percent of the patients fulfiled criteria (measured with the MINI-plus) for comorbidity on Axis I, none of patients suffered from comorbid PTSD, and AXIS II personality traits were found in 60% of the patients.
Table 1.
Demographic and clinical characteristics of the 10 patients with misophonia
| Patient | Sex | Age (years) | Age onset (years) | Family history | Previous CBT | Comorbidity Axis I | Comorbidity Axis II |
|---|---|---|---|---|---|---|---|
| 1 | F | 49 | 6 | Misophonia | No | Specific phobia | No diagnosis |
| 2 | F | 19 | 11 | Clear | No | Anxiety disorder NOS | No diagnosis |
| 3 | F | 55 | 39 | Misophonia | No | No diagnosis | No diagnosis |
| 4 | F | 23 | 7 | Clear | No | No diagnosis | Avoidant traits |
| 5 | F | 26 | 15 | Misophonia | No | No diagnosis | OCPD traits |
| 6 | M | 56 | 6 | Misophonia | No | No diagnosis | No diagnosis |
| 7 | F | 40 | 13 | Clear | Yes | Trichotillomania | Borderline traits |
| 8 | F | 27 | 14 | Misophonia | Yes | No diagnosis | OCPD traits |
| 9 | F | 37 | 7 | Clear | Yes | Eating disorder NOS | OCPD |
| 10 | F | 18 | 13 | Clear | Yes | Social phobia | Avoidant traits |
In eight of the 10 patients, misophonia-related emotionally disturbing memories were identified; the other two patients were excluded from the study. Seven patients completed EMDR-therapy and the post-treatment measures. Only one patient dropped out after the first EMDR session. Despite several attempts to approach the patient, she declined to attend treatment appointments and post-treatment measures were missing.
3.2. Primary outcomes
On average, 2.6 sessions of EMDR were provided to each participant (n = 7). A paired t-test for the completers showed significant improvement on the primary outcome (−6.14 [MD], 5.34 [SD]) on the AMISOS-R (P = .023) (Tables 2 and 3). On average, the AMISOS-R total scores were reduced by 20%. In Figure 2 the decrease in AMISOS-R is shown for the completers. An additional intention-to-treat analysis showed the same significant difference and direction of the effect on the AMISOS-R (−5.37 [MD], 5.40 [SD], P = .026).
Table 2.
Paired samples t-test statistics for the mean changes between baseline and end-of-treatment in completers (n = 7)
| Pre treatment means (sd) | Post treatment means (sd) | N | t | Sig. | |
|---|---|---|---|---|---|
| AMISOS-R | 30.43 (4.28) | 24.29 (9.05) | 7 | 3.046 | .023 |
| SCL-90 | 172.83 (22.09) | 154.83 (32.32) | 6 | 1.402 | .220 |
| SDS work | 4.57 (2.99) | 3.14 (2.91) | 7 | 1.369 | .220 |
| SDS social | 5.00 (2.38) | 4.00 (1.63) | 7 | .882 | .412 |
| SDSfamily | 6.29 (3.04) | 4.86 (2.48) | 7 | .946 | .381 |
| SDS total | 15.86 (3.81) | 12.00 (5.89) | 7 | 1.218 | .269 |
Table 3.
Paired samples t-test statistics for the mean changes between baseline and end-of-treatment. Intention-to-treat analysis with the last observation carried forwards (n = 8)
| Pre treatment means (sd) | Post treatment means (sd) | N | t | Sig. | |
|---|---|---|---|---|---|
| AMISOS-R | 30.50 (3.96) | 25.13 (8.71) | 8 | 2.817 | .026 |
| SCL-90 | 181.57 (30.68) | 166.14 (42.02) | 7 | 1.383 | .216 |
| SDS work | 4.38 (2.83) | 3.13 (2.70) | 8 | 1.357 | .217 |
| SDS social | 5.38 (2.45) | 4.50 (2.07) | 8 | .884 | .406 |
| SDSfamily | 6.50 (2.88) | 5.25 (2.55) | 8 | .947 | .375 |
| SDS total | 16.25 (3.69) | 12.88 (5.99) | 8 | 1.213 | .265 |
Figure 2.
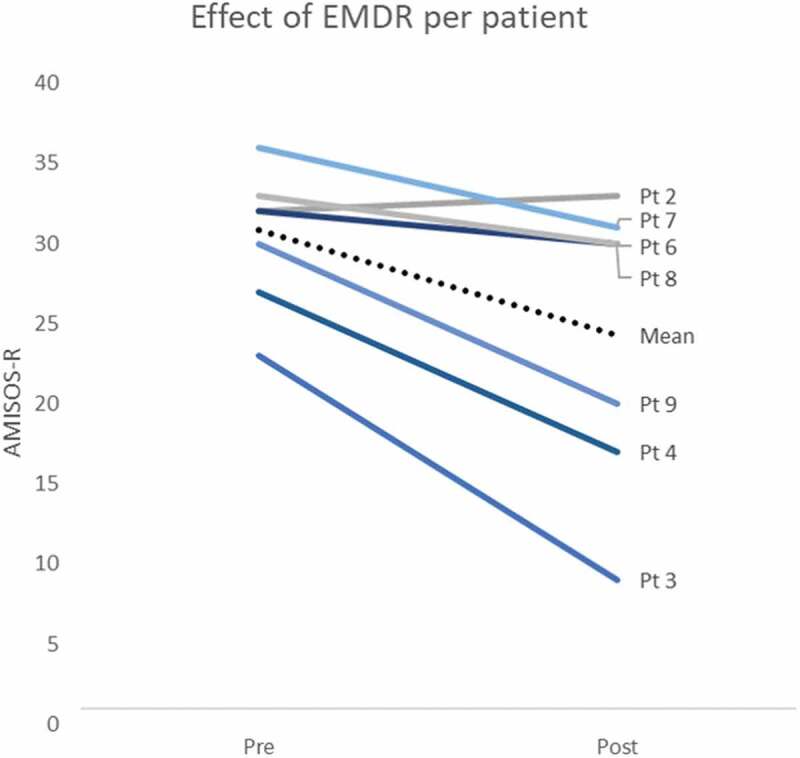
Effect of EMDR therapy on misophonia symptoms per treatment completer (n = 7)
Three patients (#3, #7, #9) were found to be clinically improved, two of them with much improvement (CGI-I < 3). One patient (#4), who showed large improvement on the AMISOS-R, was not considered clinically improved, since the improvement seemed to be related to temporary reduction of specific misophonia triggers.
In conclusion, the full response rate was 25%; two of the eight included patients had both 25% symptom reduction and a maximum CGI-I score of 2 (‘much improved’ (2) or ‘very much improved’ (1)). Two other patients were considered as partial responders with at least 25% symptom reduction on the AMISOS-R or a maximum CGI-I score of 2 (see Table 4).
3.3. Secondary outcomes
No significant effect was found on secondary outcomes (see Tables 2 and 3). However, SCL-90 mean scores decreased with 33% and patients reported fewer disabilities in all SDS subscales (work, family and social functioning) after EMDR-therapy.
In one patient who experienced neglect and aggression as negative childhood experiences, the IES was administered pre- and post-treatment. The scores of 23 (pre) to 3 (post) were mild and not indicative for PTSD. The difference in total score between pre and post was large, but IES was not used as an outcome measure in this study.
3.4. Qualitative outcomes: misophonia-related memories
In total 14 target misophonia-related memories were identified in eight patients, of which seven reported one or two targets and one patient reported three targets (for an overview of the targets, see Table 4). The number of EMDR sessions varied from 1 to 4 sessions of 60–90 minutes. Subjective Units of Distress (SUD) Scale scores at the start of the EMDR therapy varied from 5 to 10 and at the end of the therapy all SUD scores were decreased to 0. Two examples of target memories are: firstly, as an 11-year-old girl on holiday sharing a tent with her father, she had a panic attack after hyper focusing on his snoring with the experience she could not escape from the tent in the middle of the night (negative cognition: ‘I am powerless’). Secondly, as a 10-year-old girl who could not grieve at her grandmother’s funeral, because she was so bothered by the breathing sound of her crying brother that she snubbed him and felt terrible about herself (negative cognition: ‘I am a bad person’).
3.5. Adverse events and side effects
No adverse events were reported. Three patients showed misophonia symptoms during EMDR (e.g. expressing anger in reaction to the ticking of the clock or to breathing sounds of the therapist). Other mild side effects included fatigue or headaches in three patients, lasting for two days maximum. One patient suffered from suicidal ideations with intrusions of suicide during EMDR treatment after the first session. After the second EMDR session, the suicidal ideations disappeared. In the end, this patient (#3) profited most of all patients from EMDR.
4. Discussion
This is the first clinical sample study which examines the feasibility and effectiveness of EMDR for misophonia in eight patients. The results showed that EMDR focused on desensitizing emotionally disturbing memories related to the onset or worsening of misophonia symptoms and significantly reduced these symptoms.
Our positive outcome is in line with the results of the case report of Vollbehr and ten Broeke (2017). However, comparisons with their findings is difficult, because pre- and post-treatment assessments were missing and extra targets were used during EMDR therapy. Nevertheless, though no questionnaires were administered, Vollbehr and ten Broeke observed alleviation of symptoms of misophonia without full remission. Their patient was still sensitive to misophonia triggers, but his/her emotional reaction and avoidance behaviour diminished substantially. Apart from desensitization of the identified misophonia-related target memories, their patient was also instructed to create an extremely inflated image of present triggers in imagination, after which desensitization of this image took place (Shapiro, 2018). In our study, no present triggers, nor an inflated image of present triggers were targeted. However, after having treated all misophonia-related target memories, the ‘future template’ procedure was used (Shapiro, 2018) to help patients visualizing successfully managing an anticipated future event with misophonia triggers.
In our trial, for two out of 10 patients, no explicit disturbing misophonia-related memories could be identified. For the remaining patients, their memories of the first (onset) misophonic experience and/or aggravating experiences were treated. The nature of these experiences were not evidently traumatic (corresponding to Criterion A of the DSM 5 PTSD criteria; American Psychiatric Association, 2013). They may be classified as unpleasant and disturbing, as is described in previous clinical case series (Ferreira, Harrison, & Fontenelle, 2013; Johnson et al., 2013). Target memories related to the onset or worsening of misophonia in childhood consisted in our pilot of situations of fierce arguments caused by their misophonia, maladaptive coping incidents such as bulimic outrage, suicidal ideations, or panic attacks when misophonia triggers could not be avoided (feeling overwhelmed and powerless). Target memories of the two full responders were easier to identify with the time-line method and had a higher level of observed distress than in the other patients. This could be one of the reasons why EMDR was more successful in these cases, as it is known that EMDR is more effective when the level of disturbance at the start of the session is high (Littel, Remijn, Tinga, Engelhard, & van den Hout, 2017). We did not examine predictors of treatment outcomes because of the small sample, but we hypothesize that the nature of target memories, participant characteristics or type of misophonia symptoms such as disgust, might predict treatment outcomes. Hypothesizing about a treatment mechanism is beyond the scope of this article.
Since we used only the time-line procedure to identify the target-memories for EMDR therapy, it remains unclear whether the two patients without target memories could have benefitted from EMDR. It would be interesting to add more explicit desensitization of ‘present triggers’ following desensitization of misophonia-related target memories, or use the creation of an extremely inflated image of present triggers (Rijkeboer, ten Broeke, & Koekbakker, 2016). We advise clinicians working with patients with misophonia to select and desensitize different types of targets, such as past traumatic or disturbing events, present triggers (e.g. inflated image), and future targets as well.
Treatment options are still limited for misophonia. So far, the only well-studied intervention for misophonia is G-CBT (Jager et al., 2020b; Schröder et al., 2017). Compared to the results of the recent RCT of G-CBT, EMDR was less effective with a decrease of −6.14 vs −9.7 points (G-CBT) on the AMISOS-R post treatment, respectively, though an equal percentage of patients clinically improved, 38% with EMDR vs 37% with G-CBT on the CGI-I post treatment (Jager et al., 2020b).
G-CBT and EMDR both have pros and cons. G-CBT as a multicomponent intervention offers more techniques from which patients can profit, extensive psychoeducation, more opportunity to practice under guidance, peer support, and support of loved ones. The empirical level of evidence is higher for G-CBT including a RCT with one 1-year follow-up, no adverse events were reported and patient’s acceptability is high (Jager et al., 2020b; Schröder et al., 2017). In this pilot study, EMDR therapy time was limited by a mean of 2.6 sessions of 1 to 1.5 hours (mean total of 3.9 hours) versus 8 (group) sessions of CBT of 3 hours (mean total of 24 hours) and could therefore be more cost-effective. As a con, apart from this case study, there is no empirical evidence for its effectivity. So far, indication to use EMDR was conditional, depending on the presence of emotionally disturbing target memories related to the onset or worsening of the symptoms.
Our results suggest as well that EMDR is an attractive alternative for non-responders to G-CBT. In this pilot study, patients on the waiting list for G-CBT (n = 6) and non-responders to G-CBT (n = 4) were included. Patients from both groups profited from EMDR (one patient waiting for CBT and 2 non-responders), but no post-hoc analyses could be performed because of the small sample size. We might speculate in which cases EMDR or G-CBT should be considered. First, EMDR might be preferred in cases where clear and emotionally disturbing target memories for EMDR can be identified. Secondly, when therapists can not provide (G-)CBT or patients are reluctant to participate in group therapy. Finally, if patients are in need of a quick fix for example, when a final exam in 2 weeks is hindered by misophonia symptoms.
4.1. Limitations and strengths
This is a small case series without a control group and therefore our study suffers from several important limitations. The lack of a control group prevents us from assessing the effects of time and of non-specific factors on misophonia symptoms. The small sample warrants caution in the generalization of the results. There was no follow-up assessment since half of the patients were on the waiting list for CBT and received CBT following EMDR, making it impossible to determine whether treatment gain was maintained over time. The inclusion of two subpopulations can be considered a limitation in this small sample. However, this does resemble clinical practice. All participants received EMDR from one therapist, the evaluator was not blind to treatment and treatment fidelity measures were not carried out, possibly leading to bias. More and larger studies are needed to confirm the effectiveness of EMDR therapy and to determine the average number of EMDR sessions needed to significantly reduce misophonia symptoms. Finally, because of the small sample size, some tantalizing questions regarding prediction or comparative efficacy with CBT could not be answered.
On the other hand, our study is innovative, and the use of a case series was considered appropriate given the exploratory nature of the study. The sample had baseline characteristics comparable to larger misophonia samples (Jager et al., 2020a; Rouw & Erfanian, 2018), leading to adequate external validity. We used a diagnostic clinical interview to assess the presence of disorders, an objective diagnostic assessment (CGI) and a manualized treatment. Data were also analysed under restrictions of intention-to-treat analysis and missing values were imputed by LOCF, resulting in a conservative estimation of the effect.
4.2. Conclusions
In conclusion, the results of this study suggest that EMDR therapy is a promising and time-limited intervention in reducing misophonia symptoms, also in patients who were previously unable to benefit from evidence-based treatment (G-CBT). No adverse events were reported. Given the limitations due to the study design, the results should be considered preliminary. The next step would therefore be replication of the results in a larger RCT comparing EMDR therapy (with an extended target selection) with CBT and a waiting list or EMDR therapy as an add-on intervention to CBT, with a long-term follow-up.
Acknowledgments
We are very grateful to the 10 participating misophonia patients who relied on our expertise to try an innovative treatment. We thank Steven Meijer for his advice on the EMDR techniques at the beginning of this study. We thank Annemieke Polling for conducting the clinical interviews. Finally, we thank Isidoor Bergfeld for his advice on the statistics.
Funding Statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. For privacy reasons the research cannot be made publicly available.
Ethics statement
The study was approved by the Amsterdam UMC, location AMC medical ethics committee (approval number NL62982.018.17) and carried out in accordance with the Declaration of Helsinki. All patients gave written informed consent.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Arrindell, W. A., & Ettema, J. H. M. (1986). SCL-90: Handleiding bij een multidimensionele psychopathologie-indicator. Lisse: Swets test publishers. [Google Scholar]
- Bandelow, B., Baldwin, D. S., Dolberg, O. T., Andersen, H. F., & Stein, D. J. (2006). What is the threshold for symptomatic response and remission for major depressive disorder, panic disorder, social anxiety disorder, and generalized anxiety disorder? The Journal of Clinical Psychiatry, 67(9), 1428–10. doi: 10.4088/jcp.v67n0914 [DOI] [PubMed] [Google Scholar]
- Brom, D., & Kleber, R. J. (1985). De Schok Verwerkings Lijst [The Dutch version of the impact of event scale]. Nederlands Tijdschrift voor de Psychologie, 40, 164–168. [Google Scholar]
- Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the impact of event scale –revised. Behaviour Research and Therapy, 41(12), 1489–1496. doi: 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- Cuijpers, P., Veen, S. C. V., Sijbrandij, M., Yoder, W., & Cristea, I. A. (2020). Eye movement desensitization and reprocessing for mental health problems: A systematic review and meta-analysis. Cognitive Behaviour Therapy, 49(3), 165–180. doi: 10.1080/16506073.2019.1703801 [DOI] [PubMed] [Google Scholar]
- De Jongh, A., Amann, B. L., Hofmann, A., Farrell, D., & Lee, C. W. (2019). The status of EMDR therapy in the treatment of posttraumatic stress disorder 30 years after its introduction. Journal of EMDR Practice and Research, 13(4), 261–269. doi: 10.1891/1933-3196.13.4.261 [DOI] [Google Scholar]
- De Jongh, A., ten Broeke, E., & Meijer, S. (2010). Two method approach: A case conceptualization model in the context of EMDR. Journal of EMDR Practice and Research, 4(1), 12. doi: 10.1891/1933-3196.4.1.12 [DOI] [Google Scholar]
- De Jongh, A. J. C. M., & ten Broeke, E. (2019). Handboek EMDR: Een geprotocolleerde behandelmethode voor de gevolgen van psychotrauma. [Handbook of EMDR: A standardized treatment for the consequences of psychotrauma]. Amsterdam: Pearson. [Google Scholar]
- Derogatis, L. R., Lipman, R. S., & Covi, L. (1973). The SCL-90: An outpatient psychiatric rating scale – preliminary report. Psychopharmacology Bulletin, 9, 13–18. [PubMed] [Google Scholar]
- Erfanian, M., Kartsonaki, C., & Keshavarz, A. (2019). Misophonia and comorbid psychiatric symptoms: A preliminary study of clinical findings. Nordic Journal of Psychiatry, 73(4–5), 219–228. doi: 10.1080/08039488.2019.1609086 [DOI] [PubMed] [Google Scholar]
- Ferreira, G. M., Harrison, B. J., & Fontenelle, L. F. (2013). Hatred of sounds: Misophonic disorder or just an underreported psychiatric symptom? Annals of Clinical Psychiatry, 25(4), 271–274. [PubMed] [Google Scholar]
- Gunter, R. W., & Bodner, G. E. (2008). How eye movements affect unpleasant memories: Support for a working-memory account. Behaviour Research and Therapy, 46(8), 913–931. doi: 10.1016/j.brat.2008.04.006 [DOI] [PubMed] [Google Scholar]
- Guy,W. C. G. I. (1976). Clinical global impression. Assessment manual for Psychopharmacology, 217–222. [Google Scholar]
- Hase, M., Balmaceda, U. M., Ostacoli, L., Liebermann, P., & Hofmann, A. (2017). The AIP model of EMDR therapy and pathogenic memories. Frontiers in Psychology, 8, 1578. doi: 10.3389/fpsyg.2017.01578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. doi: 10.1097/00006842-197905000-00004 [DOI] [PubMed] [Google Scholar]
- International Society of Traumatic Stress Studies (ISTSS) . (2019). Post-traumatic stress disorder: Prevention and treatment guidelines. Retrieved from http://www.istss.org/treating-trauma/new-istss-prevention-and-treatment-guidelines.aspx [DOI] [PubMed]
- Jager, I., de Koning, P., Bost, T., Denys, D., & Vulink, N. (2020a). Misophonia: Phenomenology, comorbidity and demographics in a large sample. PloS One, 15(4), e0231390. doi: 10.1371/journal.pone.0231390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager, I. J., Vulink, N. C., Bergfeld, I. O., van Loon, A. J., & Denys, D. A. (2020b). Cognitive behavioral therapy for misophonia: A randomized clinical trial. Depression and Anxiety. doi: 10.1002/da.23127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jastreboff, P. J., & Jastreboff, M. M. (2014, May). Treatments for decreased sound tolerance (hyperacusis and misophonia). Seminars in Hearing, 35(2), 105–120. Thieme Medical Publishers. doi: 10.1055/s-0034-1372527 [DOI] [Google Scholar]
- Johnson, P. L., Webber, T. A., Wu, M. S., Lewin, A. B., Murphy, T. K., & Storch, E. A. (2013). When selective audiovisual stimuli become unbearable: A case series on pediatric misophonia. Neuropsychiatry, 3(6), 569–575. doi: 10.2217/npy.13.70 [DOI] [Google Scholar]
- Littel, M., Remijn, M., Tinga, A. M., Engelhard, I. M., & van den Hout, M. A. (2017). Stress enhances the memory-degrading effects of eye movements on emotionally neutral memories. Clinical Psychological Science, 5(2), 316–324. doi: 10.1177/2167702616687292 [DOI] [Google Scholar]
- Matthijssen, S. J., Lee, C. W., de Roos, C., Barron, I. G., Jarero, I., Shapiro, E., … Moreno-Alcázar, A. (2020). The current status of EMDR therapy, specific target areas, and goals for the future. Journal of EMDR Practice and Research, 14(4), 241–284. doi: 10.1891/EMDR-D-20-00039 [DOI] [Google Scholar]
- Maxfield, L. (2019). A clinician’s guide to the efficacy of EMDR therapy. Journal of EMDR Practice and Research, 13(4), 239–246. doi: 10.1891/1933-3196.13.4.239 [DOI] [Google Scholar]
- Meyerbröker, K., Emmelkamp, P. M. G., & Merkx, M. (2019). Effectiviteit van EMDR bij andere stoornissen en problemen dan PTSS: Een literatuuroverzicht. Gedragstherapie, 52(3), 225. [Google Scholar]
- National Institute for Health and Care Excellence . (2018). Post-traumatic stress disorder. NG116. Management of PTSD in children, young people and adults (1.6.13). Retrieved from https://www.nice.org.uk/guidance/ng116/chapter/Recommendations#management-of-ptsd-in-children-young-people-and-adults [PubMed]
- Naylor, J., Caimino, C., Scutt, P., Hoare, D. J., & Baguley, D. M. (2020). The prevalence and severity of misophonia in a UK undergraduate medical student population and validation of the Amsterdam misophonia scale. Psychiatric Quarterly, 1–11. doi: 10.1007/s11126-020-09825-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rijkeboer, M., ten Broeke, E., & Koekbakker, J. (2016). EMDR bij obsessieve compulsieve stoornis: Back tot he future. In Oppenhiem H., Hornsveld H., ten Broeke E., & de Jongh A. (Eds.), Praktijkboek EMDR deel ll (pp. 337–366). Amsterdam: Pearson Assessment and Information B.V. [Google Scholar]
- Rouw, R., & Erfanian, M. (2018). A large‐scale study of misophonia. Journal of Clinical Psychology, 74(3), 453–479. doi: 10.1002/jclp.22500 [DOI] [PubMed] [Google Scholar]
- Schröder, A., & Spape, M. (2014). Amsterdam misophonia scale – revised (AMISOS-R) [Measurement instrument]. Retrieved from https://journals.plos.org/plosone/article/file?type=supplementary&id=info
- Schröder, A., Vulink, N., & Denys, D. (2013). Misophonia: Diagnostic criteria for a new psychiatric disorder. PLoS One, 8(1), e54706. doi: 10.1371/journal.pone.0054706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schröder, A. E., Vulink, N. C., van Loon, A. J., & Denys, D. A. (2017). Cognitive behavioral therapy is effective in misophonia: An open trial. Journal of Affective Disorders, 217, 289–294. doi: 10.1016/j.jad.2017.04.017 [DOI] [PubMed] [Google Scholar]
- Shapiro, F. (2001). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures. New York: Guilford Publications. [Google Scholar]
- Shapiro, F. (2018). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures, third edition. New York: Guilford Press. [Google Scholar]
- Sheehan, D. V. (1983). Sheehan disability scale. Handbook of Psychiatric Measures, 2, 100–102. [Google Scholar]
- Sheehan, D. V., Lecrubier, Y., Harnett Sheehan, K., Janavs, J., Weiller, E., Keskiner, A., … Dunbar, G. C. (1997). The validity of the mini international neuropsychiatric interview (MINI) according to the SCID-P and its reliability. European Psychiatry, 12(5), 232–241. doi: 10.1016/S0924-9338(97)83297-X [DOI] [Google Scholar]
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., & Dunbar, G. C. (1998). the mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. quiz 34-57. [PubMed] [Google Scholar]
- Swedo, S., Baguley, D. M., Denys, D., Dixon, L. J., Erfanian, M., Fioretti, A., … Raver, S. M. (2021). A consensus definition of misophonia: Using a delphi process to reach expert agreement. medRxiv. doi: 10.1101/2021.04.05.21254951 [DOI] [Google Scholar]
- van der Ploeg, E., Mooren, T., Kleber, R. J., van der Velden, P. G., & Brom, D. (2004). Construct validation of the Dutch version of the impact of event scale. Psychology Assessment, 16(1), 16–26. doi: 10.1037/1040-3590.16.1.16 [DOI] [PubMed] [Google Scholar]
- Van Loon, A., Van der Pol, M., Slaghekke, S., Van der Meer, C., Schekman, E., Nieuwendijk, E., De Wit, I., & Jager, J. (2019). Misofonie: Behandelprotocol in 8 sessies [Misophonia: Treatment protocol of 8 sessions]. Boom Publishers.
- Van Vliet, I. M., & De Beurs, E. (2007). The MINI-international neuropsychiatric interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders. Tijdschrift voor psychiatrie, 49(6), 393–397. [PubMed] [Google Scholar]
- Vollbehr, A., & ten Broeke, E. (2017). EMDR bij misofonie [EMDR for misophonia]. Tijdschrift voor Gedragstherapie, 2017(3), 190–206. [Google Scholar]
- Zhou, X., Wu, M. S., & Storch, E. A. (2017). Misophonia symptoms among Chinese university students: Incidence, associated impairment, and clinical correlates. Journal of Obsessive-Compulsive and Related Disorders, 14, 7–12. doi: 10.1016/j.jocrd.2017.05.001 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. For privacy reasons the research cannot be made publicly available.


