Abstract
Purpose
This study aimed to investigate cross-sectional associations between physical activity, sleep health, and depression symptoms using mediation models.
Methods
Participants (N = 1576, MAge = 39.3 years, 40% female) were recruited online from Amazon’s Mechanical Turk crowd-sourcing service. Physical activity was measured using a single-item self-report measure and depression symptoms were reported using the Hospital Anxiety and Depression Scale. Sleep health was measured using the 6-question RUSATED Sleep Health survey V2.0.
Results
Good sleep health (direct effect: β = − .273, t = − 13.87, p < .0001) and high levels of physical activity (direct effect: β = − .092, t = − 4.73, p < .0001) were both individually associated with fewer depression symptoms. Sleep health significantly mediated 19% of the association between physical activity and depression symptoms (indirect effect: β = − .022, 95% CI [− .036 to − .008]), while physical activity significantly mediated 3% of the relationship between sleep health and depression symptoms (indirect effect: β = − .008, 95% CI [− .014 to − .003]).
Conclusion
Physical activity and sleep health act as predictors and mediators of depression symptoms.
Keywords: Sleep health, Physical activity, Depression, Epidemiology, Public health
Introduction
Sleep and physical activity are both behaviors that strongly relate to depression. Short and long sleep duration, decreased sleep continuity (e.g., low sleep efficiency, long sleep latency, and more nighttime awakening), decreased sleep depth (e.g., less time in stage 2 and slow-wave sleep), and insomnia have been associated with depression [1]. High levels of physical activity prospectively predict lower rates of incident depression in children, adolescents, and adults and in randomized controlled trials of clinically depressed individuals, physical activity intervention has been shown to significantly reduce depression symptoms to the same or to a larger extent than medication and other non-pharmacological therapies [2].
While many biological, psychological, and behavioral mechanisms have been proposed to be responsible for the associations that sleep and physical activity have with depression [2–4], it remains unknown whether sleep may mediate the relationship between physical activity and depression or vice versa. Physical activity and sleep are reciprocally related. A meta-analysis of physical activity interventions showed that higher levels of physical activity were associated with increased sleep duration, sleep efficiency, slow-wave sleep, and subjective quality, as well as decreased sleep latency and wake after sleep onset [5]. In the other direction, emerging research suggests that poor sleep may contribute to lower physical activity levels [6]. Daily diary and actigraphy studies have shown that within-person variation in sleep quality and efficiency predicts physical activity the next day [7] and experimental sleep restriction has been shown to reduce physical activity levels and increase sedentary time in freely living participants [8].
Despite evidence of strong reciprocal ties, it remains unclear if sleep mediates the relationship between physical activity and depression or vice versa, although emerging evidence supports a role for sleep as a potential mediator [9]. As such, we tested sleep as a mediator of the relationship between physical activity and depression and physical activity as a mediator of the relationship between sleep and depression. We hypothesized that both sleep and physical activity would individually predict depression and that each would be a significant mediator in a population-based, cross-sectional sample.
Participants and methods
Study sample
Participants were recruited online using Amazon’s Mechanical Turk (MTurk) crowd-sourcing service from January to March 2020, prior to the COVID-19 pandemic in the USA. To be eligible, participants had to be at least 18 years of age and be in the USA at the time of participation. Participant demographics are summarized in Table 1. This study was approved by the University IRB, and all participants provided informed consent.
Table 1.
Participant characteristics (N = 1576)
| Study sample | American Community Survey Dataa | |
|---|---|---|
| Variable | Mean (SD), [range] | %, (Margin error) |
| Age, years | 39.3 (13.7), [18–78] | |
| Smoking: n, % yes | 537, 34% | |
| Sex: n, % female | 627, 40% | 51%a |
| Race: n, % of total | ||
| White | 1103, 70% | 60%, ± .01% |
| Black | 264, 17% | 12%, ± .2% |
| Hispanic | 103, 7% | 18%, ± .02% |
| Asian | 64, 4% | 6%, ± .2% |
| Native American | 33, 2% | 1%, ± 1% |
| Pacific Islander | 1, < 0.1% | 0.2%, ± 3% |
| Other, mixed | 33, 2% | 3% ± 1% |
| Subjective social status: | 6.1 (2.1), [1–10] | |
| Neuroticism: | 22.7 (6.5), [8–40] | |
| Morningness-eveningness score: | 55.5 (9.5), [18–85] | |
| Evening-type: n, % | 139, 9% | |
| Intermediate-type: n, % | 824, 52% | |
| Morning-type: n, % | 613, 39% | |
| Cardiometabolic disease: n, % yes | 679, 43% | |
| Physical activity: n, % | ||
| Level 1 | 366, 23% | |
| Level 2 | 437, 28% | |
| Level 3 | 424, 27% | |
| Level 4 | 220, 14% | |
| Level 5 | 129, 8% | |
| Sleep health | 7.9 (2.3), [0–12] | |
| Depression symptoms | 6.6 (3.9), [0–19] | |
aData from American Community Survey 2020, US Census Bureau
MTurk is an online crowd-sourcing service where employees (called workers) are recruited by employers (called requesters) to execute batches of discrete tasks (called HITs, acronym for Human Intel) [10]. In a research context, workers are participants, requesters are researchers, and HITs represent study survey completion opportunities. In the present study, a total of 1704 HITs were released to participants for completion. The total number of HITs was divided across smaller batches that were released around the clock at varying 3- and 6-h intervals in order to enroll respondents of different chronotypes in each of the four time zones of the continental USA. A total of 1652 HITs were completed (97% completion). Our analytical sample comprised 1576 participants after removal of duplicate participants using unique Amazon IDs, participants with < 75% survey completion, and participants with missing data. Age, sex, and race data for the sample approximated 2020 census data from the American Community Survey [11] (Table 1).
Data collection procedure
After participants accepted a HIT on MTurk, they were directed to the study survey via URL (Qualtrics, Provo, UT, USA). Participants provided informed consent before viewing instructions for satisfactory completion of the survey. Participants were then tested on their comprehension of the goals, timeline, and expectations of the survey prior to proceeding to the survey itself (e.g., “This survey is concerned with my sleep over the… (last night, last week, last month”; answer: last month)). The survey comprised individual questionnaires presented in random order.
Several data quality checks were integrated into the survey. In order to identify potential computer bots (i.e., fake participants), participants were asked to free-hand draw the word “mouse” on their keypad and successfully pass a CAPTCHA V2 bot check. In addition, a free response sentence-style question at the end of the survey was used. A response resembling a coherent sentence was required to pass this bot check. Attention to the survey was also assessed via embedded questions in a matrix-style question (prompt stated: “Select option ‘3’ for this question”). Satisfactory completion of comprehension questions, bot checks, and attention checks was requisite for inclusion in statistical analyses.
Study surveys
Sleep health
Sleep health is a descriptive multidimensional paradigm comprising six sleep dimensions including regularity, satisfaction, alertness, timing, efficiency, and duration [12]. These six sleep health dimensions load onto a single latent sleep health construct [13] and relate to various health outcomes such as body mass index [14], self-reported health [15], cardiometabolic morbidity [16], and depression [17]. Questions were formatted on a 3-point Likert scale: never/seldom (0), sometimes (1), and always/almost always (2). The scale has a scoring range of 0–12, with higher scores indicating better sleep health.
Hospital Anxiety and Depression Scale
The 14-item Hospital Anxiety and Depression Scale (HADS) was used to assess depression symptoms using the depression subscale (HADS-D) [18]. This subscale consists of seven Likert-style questions ranging from 0 to 3. Higher scores indicate a higher prevalence of depression symptoms. Scores ≥ 8 on the HADS-D indicate clinically significant depression symptoms; 776 participants in the current sample (49%) met this threshold. The HADS has been validated across a range of clinical and epidemiological samples. Cronbach’s α = 0.77 in the present study.
Physical activity
Physical activity was assessed using a single-item measure designed to capture habitual physical activity patterns [19, 20]. The scale consists of 5 categories, of which participants endorsed 1 of 5 potential physical activity levels ranging from “little activity other than walking for pleasure” (level 1) to “aerobic exercise such as running/walking for greater than 3 h per week” (level 5). Levels 4 and 5 approach or meet US Department of Health and Human Services physical activity guidelines [21].
Covariates
Covariates were chosen based on previously demonstrated associations with depression. The following covariates were included in the analyses: sex, age, subjective social status, race, neuroticism, smoking status, chronotype, and self-reported cardiometabolic diagnoses or medication use. Participants self-reported sex (male, female), race (White, Black, other), current smoking status (yes, no), and age (years). Subjective social status was self-reported using the social status ladder [22]. Neuroticism was recorded using the neuroticism subscale of the 44-item Big Five Personality Inventory [23]. Chronotype was measured using the MEQ [24] and continuous scores were used in analyses. Participants self-reported if they had ever received a cardiometabolic diagnosis (e.g., stroke, hypertension, coronary artery disease, obesity, and type 2 diabetes) from a physician or if they were prescribed medications from a physician to treat any of these conditions. Individuals endorsing a diagnosis and/or prescription were considered positive for cardiometabolic disease and coded accordingly in a dichotomous cardiometabolic disease variable.
Statistical analysis
Descriptive analyses were conducted on all covariates. Pearson’s bivariate correlations were conducted to assess the associations between physical activity, sleep health, and depression symptoms, all treated as continuous variables. Two subsequent models of interest were tested, both with depression symptoms as an outcome. Model 1 tested physical activity as a predictor of depression symptoms and sleep health as a mediator while model 2 tested sleep health as a predictor of depression symptoms and physical activity as a mediator. To test these two models of interest, ordinary least squares (OLS) regression was used. All assumptions of OLS were tested and satisfied. Analyses of statistical mediation were conducted using the PROCESS macro [25] in SPSS (IBM, V25, Armonk, NY, USA) controlling for all covariates. Confidence intervals for model effects were constructed using percentile bootstrapping (5,000 bootstrapped samples). According to simulations, a sample of 558 participants is needed to have acceptable power (0.80) for detecting small mediation effects (β for pathways a and b equal to 0.14). Given the current sample size (N = 1576), this study was sufficiently powered to detect small effects [26]. Both standardized and partially standardized coefficients were used to quantify total, direct, and indirect effects [25].
Several sets of additional analyses were conducted. First, in both models of interest, sleep health was replaced with the scores of each individual sleep health dimension to determine if individual sleep health dimensions acted as mediators of the relationship between physical activity and depression symptoms or as predictors of depression symptoms. These analyses were carried out in the whole sample. Second, the two models of interest were separately tested in subgroups of individuals displaying clinical or subclinical levels of depression symptoms. Such analyses were conducted to assess whether results obtained from the whole sample generalized to each subsample. Finally, given the cross-sectional nature of our data, a set of exploratory (i.e., no a priori hypotheses) mediation analyses were conducted testing the other four possible permutations of the three study variables.
Results
Study variables
Participant characteristics are included in Table 1. The most commonly endorsed physical activity category was level 2, which indicated some regular participation in modest physical activity involving sports and recreational activities. The mean sleep health score was 7.9 (range: 0–12). Depression scores ranged from 0 to 9 with a mean score of 6.6. Depression, physical activity, and sleep health scores all significantly correlated with each other with small-moderate r-values (all p ≤ 0.001; Table 2).
Table 2.
Pearson correlational analyses of mediation model variables
| Variable | Physical activity | Sleep health |
|---|---|---|
| Depressions | − .139 | − .338 |
| Physical activity | – | .082 |
all p-values ≤ .001
Main analysis: physical activity, sleep health, and depression symptoms
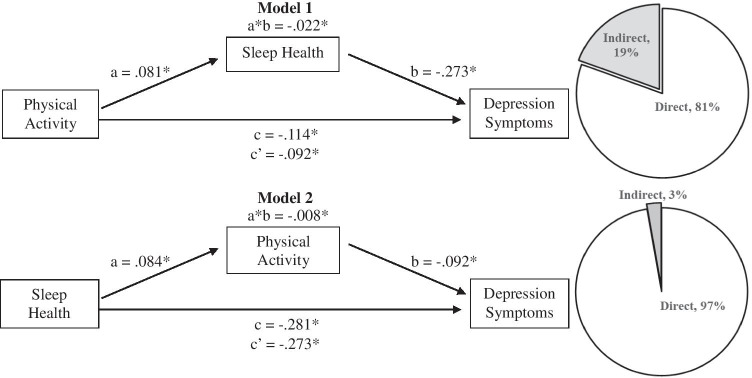
In adjusted analyses of model 1 (Fig. 1), higher levels of self-reported physical activity significantly predicted fewer depression symptoms (total effect: β = − 0.114, t = − 5.56, p < 0.0001) and greater sleep health (path a: β = 0.081, t = 3.27, p = 0.0001). Greater sleep health predicted fewer depression symptoms (pathway b: β = − 0.273, t = − 13.87, p < 0.0001). Sleep health significantly mediated the relationship between physical activity and depression symptoms (indirect effect: β = − 0.022, 95% CI [− 0.036 to − 0.008], p < 0.05) and reduced the total effect of physical activity on depression symptoms, β = − 0.092, t = − 4.73, p < 0.0001 (direct effect). Inspection of partially standardized effect sizes revealed that every increasing level of physical activity score was associated with a 0.36-point lower score in depression symptoms, of which 0.29 points were due to the direct effect of physical activity and 0.07 points (19%) due to the mediating effect of sleep.
Fig. 1.
Adjusted mediation models predicting depression symptoms in full sample (N = 1576) with A physical activity as a predictor and sleep health as a mediator and B sleep health as a predictor and physical activity as a mediator. Values represent standardized coefficients. *indicates p < .05
In adjusted analyses of model 2 (Fig. 1), greater sleep health significantly predicted fewer depression symptoms (total effect: β = − 0.281, t = − 14.21, p < 0.0001) and higher levels of self-reported physical activity (path a: β = 0.084, t = 3.27, p = 0.0001). Physical activity significantly predicted fewer depression symptoms (pathway b: β = − 0.092, t = − 4.73, p < 0.0001). Physical activity significantly mediated the relationship between sleep health and depression symptoms (indirect effect: β = − 0.008, 95% CI [− 0.014 to − 0.003], p < 0.05) and reduced the total effect of sleep health on depression symptoms, β = − 0.273, t = − 13.87, p < 0.0001 (direct effect). Every single point increase in sleep health (e.g., going from rarely/never to sometimes or sometimes to usually/always on one sleep health dimension) was associated with a 0.47-point lower score in depression symptoms, of which 0.46 points were due to the direct effect of sleep health and 0.01 points (3%) due to the mediating effect of physical activity.
Sensitivity analyses: individual sleep health dimensions
For model 1, analyses of individual sleep health dimensions revealed that sleep regularity, satisfaction, timing, and duration each significantly mediated the relationship between physical activity and depression symptoms. These dimensions mediated between 6 and 10% of the total effect of physical activity on depression symptoms. Daytime alertness and sleep efficiency did not statistically mediate the relationship between physical activity and depression symptoms (Table 3). For model 2, each individual sleep health dimension was significantly associated with depression scores (range βtotal effect = − 0.203 to − 0.050). Physical activity significantly mediated the relationships between depression symptoms and sleep regularity, satisfaction, timing, and duration. In cases where there was significant mediation, physical activity mediated 3 to 4% of the total effect of sleep health on depression scores.
Table 3.
Sensitivity analyses of individual sleep health dimensions
| Sleep health dimension | Total effect (β) | Direct effect (β) | Indirect effect (β) | % of total effect due to direct effect | % of total effect due to indirect effect |
|---|---|---|---|---|---|
| Model 1: physical activity–sleep health–depression symptoms | |||||
| Regularity | − .114* | − .102* | − .012* | 90 | 1 |
| Satisfaction | − .114* | − .104* | − .010* | 91 | 9 |
| Alertness | − .114* | − .109* | − .004 | 9 | 4 |
| Timing | − .114* | − .107* | − .007* | 94 | 6 |
| Efficiency | − .114* | − .113* | − .001 | 9 | 1 |
| Duration | − .114* | − .104* | − .010* | 91 | 9 |
| Model 2: sleep health–physical activity–depression symptoms | |||||
| Regularity | − .203* | − .197* | − .006* | 97 | 3 |
| Satisfaction | − .192* | − .186* | − .006* | 97 | 3 |
| Alertness | − .149* | − .146* | − .003 | 98 | 2 |
| Timing | − .130* | − .125* | − .005* | 96 | 4 |
| Efficiency | − .050* | − .048* | − .003 | 95 | 5 |
| Duration | − .187* | − .182* | − .006* | 97 | 3 |
*indicates p < .05
Sensitivity analyses: participant subgroups
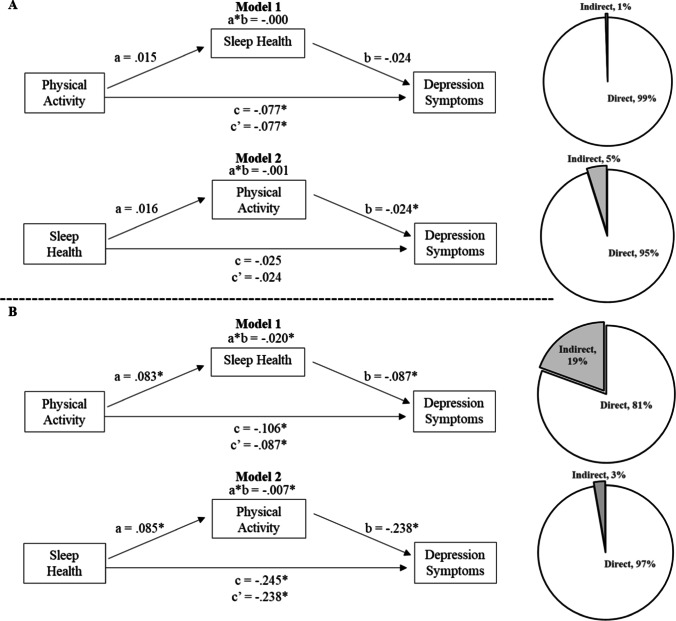
In a subsample of individuals indicating a least mild depression symptoms (n = 776), adjusted analyses for model 1 revealed that higher levels of self-reported physical activity significantly predicted fewer depression symptoms (total effect: β = − 0.077, t = − 2.21, p = 0.028). However, the associations of sleep health with physical activity and depression were non-significant. Sleep health did not significantly mediate the relationship between physical activity and depression symptoms (Fig. 2A, model 1). Testing of model 2 with covariates showed that sleep health did not predict depression symptoms (total effect: β = − 0.025, t = − 0.69, p = 0.49) and that there was no statistically significant mediation by physical activity (Fig. 2A, model 2).
Fig. 2.
Adjusted mediation models predicting depression symptoms in A a participant subsample with at least mild depression symptoms (n = 776) and in B a participant subsample with low/no symptoms of depression (n = 800). Values represent standardized coefficients. *indicates p < .05
Among individuals with few or no depression symptoms (n = 800), assessment of model 1 with covariates showed that higher levels of physical activity significantly predicted fewer depression symptoms (total effect: β = − 0.106, t = − 3.53, p = 0.0004) and better sleep health (path a: β = 0.083, t = 2.36, p = 0.018). Better sleep health predicted fewer depression symptoms (pathway b: β = − 0.087, t = − 8.07, p < 0.0001) and significantly mediated the relationship between physical activity and depression symptoms (indirect effect: β = − 0.020, 95% CI [− 0.037 to − 0.004], p < 0.05). For each increasing level of physical activity, depression symptoms were lower by 0.31 points, of which 0.25 points (81%) were attributed to the direct effect of physical activity and 0.06 points (19%) were due to the mediating effect of sleep health (Fig. 2B, model 1). In adjusted model 2, better sleep health predicted fewer depression symptoms (total effect: β = − 0.245, t = − 8.31, p < 0.0001) and higher levels of physical activity (path a: β = 0.085, t = 2.36, p = 0.018). Higher levels of physical activity significantly predicted fewer depression symptoms (pathway b: β = − 0.238, t = − 2.98, p = 0.003) and significantly mediated the relationship between sleep health and depression symptoms (indirect effect: β = − 0.007, 95% CI [− 0.017 to − 0.001], p < 0.05). Each point scored higher on sleep health coincided with a 0.43 point lower score on depression symptoms. The direct effect of sleep health accounted for 0.42 points (97%), while the mediating effect of physical activity accounted for almost 0.01 points (3%) (Fig. 2B, model 2).
Exploratory analyses: alternative mediation models
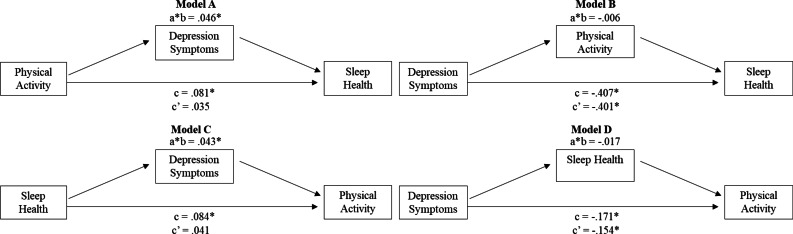
Figure 3 outlines the results of four exploratory mediation models that were tested, controlling for covariates. As a predictor, depression was significantly associated with poor sleep health and low physical activity. In each case (Fig. 3B, D), neither sleep health nor physical activity was found to be a significant mediator. Depression was found to be a significant mediator in both models accounting for approximately 50% of the total effect of sleep health on physical activity and vice versa (Fig. 3A, C).
Fig. 3.
Adjusted exploratory mediation models in full sample (N = 1576). Values represent standardized coefficients. *indicates p < .05
Discussion
The current study examined the roles of sleep health and physical activity as statistical mediators and predictors of depression symptoms in a cross-sectional US population-based sample. Sleep health was a significant predictor of depression symptoms and significantly mediated 19% of the association between physical activity scores and depression symptoms, even after controlling for sociodemographic, behavioral, and health-related covariates. By comparison, physical activity also significantly predicted depression symptoms, but only mediated about 3% of the relationship between sleep health and depression symptoms after controlling for covariates. Together, these findings demonstrate that physical activity and sleep health both are individually associated with depression symptoms, and may mediate the other’s effect, to some extent.
The current results accord with reports demonstrating that sleep health predicts depression symptoms in both cross-sectional and longitudinal analyses [17]. Sleep health significantly predicted the depression score and the current results showed that a two-point difference in a single dimension of sleep health (e.g., from rarely/never to usually/always) was associated with almost a full-point difference in depression scores. In a recent longitudinal analysis from the Cardiovascular Risk in Young Finns Study, higher self-reported physical activity was significantly and prospectively associated with fewer sleep problems and depression symptoms. In unadjusted analyses, fewer sleep problems significantly mediated the relationship between physical activity and depressive symptoms [9]; the mediation effect, however, did not withstand adjustment for baseline depression symptoms. Our cross-sectional results broadly map onto these findings as sleep health significantly mediated approximately 20% of the effect of physical activity on depression symptoms in the whole sample. However, in a subsample of participants with at least clinically mild depression symptoms, sleep health failed to mediate the relationship. Together, these findings suggest that while sleep may be a mediator of the relationship between physical activity and depression symptoms, a history of depression or at least a mild level of prevailing symptoms significantly mitigate the effect of sleep as a mediating mechanism. It is important to note that physical activity continued to significantly predict depression symptoms in this subgroup, suggesting that other mechanisms may be operational in those with at least mild depression symptoms including psychological, behavioral, and neurobiological pathways [2, 4].
These findings also align with other studies that have examined the relationship between physical activity and depression [2, 4]. Physical activity acted both as a predictor of depression (associated with a 0.36-point lower depression score) and a partial mediator (approximately 3%) of sleep health’s effect on depression. To contextualize the magnitude of this effect, consider the case of two individuals who differ on physical activity by 4 categories (e.g., one is physically inactive and the other meets current physical activity guidelines). According to these results, these individuals would differ by 1.44 points in their HADS-D scores, with the individual who reports greater physical activity having a lower depression score. For context, the minimal clinically important difference for depression measured using the HADS in patients with cardiovascular disease and chronic obstructive pulmonary disorder ranges from 1.4 to 1.7 [27]. As a mediator, physical activity seemed to play only a small, albeit statistically significant, role in the relationship between sleep health and depression scores. It may be that the effects of sleep health on depression scores are mediated, in large part, by other mechanisms (e.g., impaired emotional regulation or abnormal dopaminergic/serotonergic signaling) [3].
These findings also add to the growing body of literature supporting the use of the sleep health construct and, more generally, the consideration of sleep as a multidimensional process. As a predictor and mediator, sleep health produced larger effects than any one of the six individual dimensions. This finding may not be surprising, given the overlap in sleep dimensions impacted by physical activity and depression. For example, low levels of physical activity and high levels of depressive symptoms have both been shown to relate to poor sleep duration, efficiency, latency, and slow-wave sleep [1, 4]. In addition, high levels of physical activity [28] and depression symptoms [17] have been individually associated with better and worse composite sleep health, respectively.
These results need to be interpreted within the context of study strengths and weaknesses. Strengths of the study include the use of a novel online crowd-sourcing service to capture a diverse and geographically representative sample of participants in the USA [29], as well as the extensive use of data quality measures. On the other hand, cross-sectional design precludes conclusions regarding causality. However, analyses from a similarly designed, yet longitudinal, study [9] reported results that align with the present study. In addition, the exclusive use of self-report measures leaves open the question as to whether these results will generalize to other measures of physical activity and sleep. Given that self-reported physical activity has been shown to moderately correlate with objective measures of physical activity [30] and self-reported sleep health performs similarly to actigraphy-based sleep health [16], it is reasonable to think that these results may generalize to other methods of physical activity and sleep assessment.
In conclusion, higher levels of physical activity and greater sleep health were associated with lower levels of depression symptoms. Both individually predicted depression symptoms, and each acted as a statistically significant mediator of the other’s overall effect. This study highlights the close association of sleep health and physical activity.
Author contribution
Conceptualization: William T. Barham, Ryan C. Brindle; methodology: William T. Barham, Ryan C. Brindle; formal analysis and investigation: William T. Barham, Ryan C. Brindle; writing—original draft preparation: William T. Barham, Ryan C. Brindle; writing—review and editing: William T. Barham, Ryan C. Brindle, Christopher E. Kline, Andrew G. Kubala, Daniel J. Buysse; funding acquisition: Ryan C. Brindle; resources: Ryan C. Brindle; supervision: Ryan C. Brindle.
Funding
This study was funded by Washington and Lee University.
Data availability
Upon request to author.
Code availability
Not applicable.
Declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Washington and Lee University (1/23/2020, IRB.201920.009).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors have approved submission of the manuscript.
Conflict of interest
Dr. Buysse has served as a paid consultant to Bayer, BeHealth Solutions, Cereve/Ebb Therapeutics, Emmi Solutions, National Cancer Institute, Pear Therapeutics, Philips Respironics, Sleep Number, and Weight Watchers International. He has served as a paid consultant for professional educational programs developed by the American Academy of Physician Assistants and CME Institute, and received payment for a professional education program sponsored by Eisai (content developed exclusively by Dr. Buysse). Dr. Buysse is an author of the Pittsburgh Sleep Quality Index, Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A), Brief Pittsburgh Sleep Quality Index (B-PSQI), Daytime Insomnia Symptoms Scale, Pittsburgh Sleep Diary, Insomnia Symptom Questionnaire, and RU_SATED (copyright held by University of Pittsburgh). These instruments have been licensed to commercial entities for fees. He is also co-author of the Consensus Sleep Diary (copyright held by Ryerson University), which is licensed to commercial entities for a fee. All other authors report no conflict of interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, Reynolds CF, Riemann D. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–990. doi: 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rethorst CD, Wipfli BM, Landers DM. The antidepressant effects of exercise: a meta-analysis of randomized trials. Sports Med. 2009;39:491–511. doi: 10.2165/00007256-200939060-00004. [DOI] [PubMed] [Google Scholar]
- 3.Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. 2011;31:225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38:427–449. doi: 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- 6.Kline CE. The bidirectional relationship between exercise and sleep: implications for exercise adherence and sleep improvement. Am J Lifestyle Med. 2014;8:375–379. doi: 10.1177/1559827614544437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dzierzewski JM, Buman MP, Giacobbi PR, Jr, Roberts BL, Aiken-Morgan AT, Marsiske M, McCrae CS. Exercise and sleep in community-dwelling older adults: evidence for a reciprocal relationship. J Sleep Res. 2014;23:61–68. doi: 10.1111/jsr.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bromley LE, Booth JN, 3rd, Kilkus JM, Imperial JG, Penev PD. Sleep restriction decreases the physical activity of adults at risk for type 2 diabetes. Sleep. 2012;35:977–984. doi: 10.5665/sleep.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaseva K, Dobewall H, Yang X, Pulkki-Råback L, Lipsanen J, Hintsa T, Hintsanen M, Puttonen S, Hirvensalo M, Elovainio M, Raitakari O, Tammelin T. Physical activity, sleep, and symptoms of depression in adults-testing for mediation. Med Sci Sports Exerc. 2019;51:1162–1168. doi: 10.1249/MSS.0000000000001896. [DOI] [PubMed] [Google Scholar]
- 10.Mortensen K, Hughes TL. Comparing Amazon’s Mechanical Turk platform to conventional data collection methods in the health and medical research literature. J Gen Intern Med. 2018;33:533–538. doi: 10.1007/s11606-017-4246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Census Bureau. (2020) American community survey (ACS). https://data.census.gov/cedsci/table?q=Hispanic%20or%20Latino&tid=ACSDT1Y2019.B03002&hidePreview=false. Accessed 8 Mar 2021
- 12.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brandolim-Becker N, Martins R, Jesus SN, Chiodelli R, Rieber M. Sleep health assessment: a scale validation. Psychiatry Res. 2018;259:51–55. doi: 10.1016/j.psychres.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 14.DeSantis AS, Dubowitz T, Ghosh-Dastidar B, Hunter GP, Buman M, Buysse DJ, Hale L, Troxel WM. A preliminary study of a composite sleep health score: associations with psychological distress, body mass index, and physical functioning in a low-income African American community. Sleep Health. 2019;5:514–520. doi: 10.1016/j.sleh.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalmases M, Benítez ID, Mas A, Garcia-Codina O, Medina-Bustos A, Escarrabill J, Saltó E, Buysse DJ, Roure N, Sánchez-de-la-Torre M, Rué M, Barbé F, de Batlle J. Assessing sleep health in a European population: results of the Catalan Health Survey 2015. PLoS ONE. 2018;13:e0194495. doi: 10.1371/journal.pone.0194495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brindle RC, Yu L, Buysse DJ, Hall MH. Empirical derivation of cutoff values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the midlife in the United States (MIDUS) study. Sleep. 2019;42:zsz116. doi: 10.1093/sleep/zsz116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Furihata R, Hall MH, Stone KL, Ancoli-Israel S, Smagula SF, Cauley JA, Kaneita Y, Uchiyama M, Buysse DJ, Study of Osteoporotic Fractures (SOF) Research Group An aggregate measure of sleep health is associated with prevalent and incident clinically significant depression symptoms among community-dwelling older women. Sleep. 2017;40:075. doi: 10.1093/sleep/zsw075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 19.Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22:863–870. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Jurca R, Jackson AS, LaMonte MJ, Morrow JR, Jr, Blair SN, Wareham NJ, Haskell WL, van Mechelen W, Church TS, Jakicic JM, Laukkanen R. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29:185–193. doi: 10.1016/j.amepre.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 21.President’s Council on Sports, Fitness & Nutrition (2018) Physical activity guidelines for Americans. Office of Disease Prevention and Health Promotion. https://www.hhs.gov/fitness/be-active/physical-activity-guidelines-for-americans/index.html#:~:text=For%20substantial%20health%20benefits%2C%20adults,or%20an%20equivalent%20combination%20of. Accessed 20 May 2021
- 22.Adler NE, Stewart J (2007) MacArthur research network on SES and health: research psychosocial notebook. The Regents of the University of California. https://macses.ucsf.edu/research/psychosocial/subjective.php. Accessed 21 Oct 2019
- 23.Costa PT Jr, McCrae RR (2008) The revised NEO personality inventory (NEO-PI-R). In G. J. Boyle, G. Matthews, & D. H. Saklofske (Eds.), The SAGE handbook of personality theory and assessment: Vol. 2. Personality measurement and testing (pp. 179–198). Sage Publications, Inc
- 24.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 25.Hayes AF (2017) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach 2nd ed. Guilford Publications, Inc
- 26.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lemay KR, Tulloch HE, Pipe AL, Reed JL. Establishing the minimal clinically important difference for the hospital anxiety and depression scale in patients with cardiovascular disease. J Cardiopulm Rehabil Prev. 2019;39:E6–E11. doi: 10.1097/HCR.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 28.Kubala AG, Buysse DJ, Brindle RC, Krafty RT, Thayer JF, Hall MH, Kline CE. The association between physical activity and a composite measure of sleep health. Sleep Breath. 2020;24:1207–1214. doi: 10.1007/s11325-019-02007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strickland JC, Stoops WW. The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Exp Clin Psychopharmacol. 2019;27:1–18. doi: 10.1037/pha0000235. [DOI] [PubMed] [Google Scholar]
- 30.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phy Act. 2008;5:56. doi: 10.1186/1479-5868-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon request to author.
Not applicable.