Abstract
Substance use disorder is on the rise; it has increased massively during the COVID-19 lockdown and has been found as a risk factor for depressive symptoms and major depressive disorder. Less is known about the hypothetical moderating effect of social support in that association. Three thousand five hundred Spanish adults were interviewed by phone during the COVID-19 lockdown (May–June 2020). The 8-item Patient Health Questionnaire Depression Scale (PHQ-8) was used to measure the symptoms of depression. The CAGE Adapted to Include Drugs (CAGE-AID) questionnaire was used to assess substance use disorder during the previous month. Social support was measured through the Oslo Social Support Scale (OSSS-3). Regression models were constructed to assess factors related to depressive symptoms. People with substance use disorder (alcohol and drugs) showed considerable high levels of depressive symptoms, particularly among those with low levels of social support, which reported levels above major depressive disorder cut-off.
Keywords: Depressive symptoms, Major depressive disorder, COVID-19 lockdown, Social support, Substance use disorder, Spain
The COVID-19 pandemic, social restriction measures, and associated socioeconomic consequences have all had a detrimental effect on mental health. In particular, the development of anxiety, depressive symptoms, and psychological distress has increased in the COVID-19 pandemic context (Rajkumar, 2020; Vindegaard & Benros, 2020). In addition, increases in substance use disorder have also been reported during the pandemic (Czeisler et al., 2020). For instance, previous research found increases in alcohol use by 23% and drug use by 16% (Taylor et al., 2021). Moreover, the social restriction measures have been associated with social disconnectedness (e.g., decrease in social support and increase in feelings of loneliness) (Hwang et al., 2020).
Among mental health problems, depression is one the most prevalent disorders, and it has a great impact on the global burden of disease. The prevalence of depression in Spain was estimated at 5.2% by the WHO (World Health Organization, 2017). And it has been shown to occur more frequently among women, middle-aged people, in poor health, and with low educational levels (Haro et al., 2006).
Substance use disorder is more frequent among males and those with low education levels. Whereas young people between 16 and 35 years of age report a higher percentage of cocaine and cannabis use, older adults report more frequent daily consumption of alcoholic beverages. In Spain, the prevalence of substance use disorder ranges from 11 for alcohol to 2% for cocaine among the active population (Spanish Drug Observatory, 2015).
Several researchers have reported that substance use disorder is related to depressive symptoms (Alsheikh et al., 2020; Esmaeelzadeh et al., 2018), and the directionality of substance use-depression comorbidity varies depending on the substance used (Boden & Fergusson, 2011).
People with major depressive disorder and comorbid substance use disorder suffer from greater depression severity, worse illness course, poorer recovery rates from both disorders (Blanco et al., 2012; Hasin et al., 2002), and increased frequency of suicide attempts (Davis et al., 2005). According to a recent systematic review and meta-analysis, the prevalence of any substance use disorder in individuals with MDD was 0.250. Maximum prevalence was found with alcohol use disorder, followed by illicit drug disorder and cannabis use disorder. The pooled prevalence in men was significantly higher than in women (Hunt et al., 2020).
It is widely recognized that social support is a protective factor for mental health (Gariépy et al., 2016), and particularly for depression (Li et al., 2021). Previous studies have also detected a moderating effect of social support on the association of several risk factors such as feelings of loneliness (Domènech-Abella et al., 2017), economic stress factors (Viseu et al., 2018), and physical health (Liu et al., 2021) with depression. Moreover, social support may reduce internalized stigma and improve mental health among people with substance use disorder problems (Birtel et al., 2017). However, information concerning the moderating effect of social support on the association between substance use disorder and depression is lacking.
The study was conducted just after the first COVID-19 lockdown in Spain that started in March 2020. The objectives of the present study were first to test whether substance use disorder is a risk factor for depressive symptoms, secondly, to determine if social support is a protective factor for depressive symptoms, and finally, to examine the moderating effect of social support on the association between substance use disorder and depressive symptomatology.
Material and Methods
Study Design
The data come from a cross-sectional survey of a random sample of the adult non-institutionalized population in Spain, as part of the MIND/COVID project (www.mindcovid.org). Survey’s target population included people who were at least 18 years old, had access to a mobile or landline telephone, and spoke Spanish fluently. The sample was drawn using a dual-frame random digit dialing (DFRDD) telephone survey, including both landlines and mobile telephones. First, a sample of Spanish mobile telephone numbers was generated through an automated system. Subsequently, landline numbers were selected from an internal database developed and maintained by the survey company to ensure that all geographical areas were represented in the required proportion. Up to 7 calls at different times of day were attempted to each number. The distribution of the interviews was planned according to quotas proportional to the Spanish population in terms of age group, sex, and region of residence (INE, 2019). A total of 138,656 numbers were sampled, with a final split of 71% mobile and 29% landline telephones; 45,002 numbers were non-eligible, and 72,428 had unknown eligibility. In the end, 3,500 people were interviewed during the COVID-19 lockdown in Spain.
Ethics Statement
The Parc Sanitari Sant Joan de Déu (PIC 86–20) and Parc de Salut Mar Clinical Research (protocol 2020/9203/I) ethics committees approved this study. Participants were made completely aware of the study’s objectives, and oral consent was obtained prior to proceeding with the interview.
Measurements
Depressive Symptoms and Health-Related Variables
Symptoms of depression were measured using the 8-item Patient Health Questionnaire Depression Scale (PHQ-8) (Kroenke et al., 2009). The PHQ-8 contains 8 items, with a total score ranging from 0 to 24, where each item is scored from 0 to 3 (0: Not at all; 1: Several days; 2: More than half of the days; 3: Nearly every day). A PHQ-8 score of ≥ 10 is the established cut-off for detecting major depression (Kroenke et al., 2009). Participants were also asked about their perception of their physical health (no discomfort, light discomfort, strong discomfort, moderate discomfort, and extreme discomfort).
Social Support
To assess and evaluate social support, the Oslo Social Support Scale (OSSS-3) was used. It contains three items ranging from 1 to 4 or 5. The total score range is from 3 to 14, with low scores defining poor levels of social support and high scores characterizing high levels of social support (Kocalevent et al., 2018).
Substance Use Disorder During the Last Month
The CAGE-AID was used to assess substance use disorder during the previous month. It consists of 4 questions with “yes” or “no” answers: (1) “Have you ever felt you ought to cut down on your drinking or drug use?”; (2) “Have people annoyed you by criticizing your drinking or drug use?”; (3) “Have you ever felt bad or guilty about your drinking or drug use?”; and (4) “Have you ever had a drink or used drugs first thing in the morning to steady your nerves or get rid of a hangover?” Answering “yes” to one or more questions determines substance use disorder (Brown & Rounds, 1995).
Sociodemographic Variables
Sociodemographic information such as gender, age (classified into five age groups: 18–34 years, 35–49 years, 50–64 years, 65–79 years, and 80 years or more), and education level (primary, secondary, professional training, and tertiary) was obtained.
Statistical Analysis
To compensate for survey non-response and ensure the representativeness of the sample, post-stratification weighting was used to restore the distribution of the adult general population of Spain by age group, sex, and geographic region.
A single imputation was performed because the median value of individuals with missing values around the analyzed variables was less than 1%, and all variables had less than 5% missing values (van Buuren, 2018).
Descriptive analyses included weighted proportions and unweighted frequencies for categorical variables and mean with standard deviation (SD) for scales. Groups made according to depressive symptoms (PHQ-8 < 10 vs. PHQ-8 ≥ 10) were compared using Chi square test for categorical variables and Student’s t-test for scales.
To assess whether sex, age, education level, physical health, social support, and substance use disorder (covariates) were variables with a statistically significant association with depressive symptoms (dependent variable), bivariate and multivariate Tobit regression models were fitted.
Regarding dependent variables with a wide cluster of responses at the lowest value, Tobit models are appropriate. Since the assessed categories are not precise enough to reveal latent values in the depression scale, this method assumes that many responses are censored at the lowest value. Approximately 25% of the sample accumulates at the dependent variable’s lowest value (0) and around 50% at the three smallest values (0, 1, and 2). The rest of the sample is distributed among the remaining values, with percentages decreasing as they get further from the lower values. Tobit models produce theoretically continuous values with a normal distribution using the highest possible estimates for censored values and a standard linear model for the rest of the values (Long, 1997).
Interaction of social support with substance use disorder was included in the multivariate Tobit regression model to determine whether social support had a moderating effect on the association between substance use disorder and depressive symptoms. The multivariate model included all covariates. Unstandardized coefficients and 95 percent confidence intervals (95% CI) were reported.
Tobit regression coefficients show the effect on the uncensored latent dependent variables. To assess the interaction effect for expected censored value, estimated means of depression were calculated through margins (Cong, 2001) based on the Tobit regression model with censured dependent variable values. To estimate these means, covariables were centered, taking the real proportion in the sample into account. Figure 1 depicts the expected depression means associated with the relationship of social support and substance use disorder. The major depression cut-off limit was used to display the interaction values with a mean estimated above the cut-off.
Fig. 1.
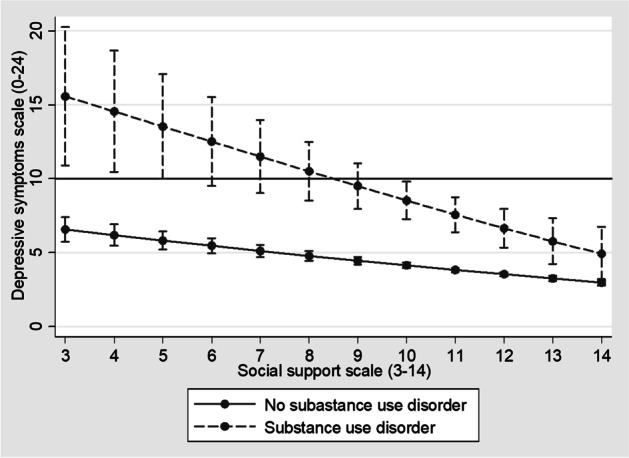
Predicted mean for depressive symptoms according to substance use disorder and social support level. Note: a cut-off point of 10 was used as screening for major depressive disorder (MDD)
All observed p-values were calculated using a two-sided test with a statistical significance level of p < 0.05. The survey data were analyzed using Stata SE 13 (StataCorp, 2013).
Results
Table 1 shows the sociodemographic features of the study participants. Percentages of population by age group, 18–34, 35–49, 50–64, 65–79, and 80 + , were 22%, 28%, 26%, 20%, and 3%, respectively. Some 43.9% of the participants were male. The mean of depression scale (PHQ-8) was 3.95, and the prevalence of substance use disorder scale was 2.8%. Individuals with major depressive disorder (PHQ-8 ≥ 10) were more frequently females, from 18 to 34 years old; had a lower educational level, less social support, and poorer physical health; as well as reporting a higher proportion of substance use disorder (7.9%).
Table 1.
Characteristics of the study sample
| Characteristic | Overall (N = 3,500) | Depressive symptoms ≥ 10 (N = 407 (11.2)) | p-valuea |
|---|---|---|---|
| Sex | |||
| • Male | 1538 (48.5) | 126 (36.0) | < 0.001 |
| • Female | 1962 (51.5) | 281 (64.0) | |
| Age group | |||
| • 18–34 | 697 (22.1) | 116 (31.8) | < 0.001 |
| • 35–49 | 1054 (28.4) | 119 (28.3) | |
| • 50–64 | 1127 (25.8) | 129 (25.3) | |
| • 65–79 | 534 (20.3) | 35 (11.9) | |
| • 80 + | 88 (3.4) | 8 (2.7) | |
| Education level | |||
| • Primary | 237 (7.7) | 40 (10.8) | < 0.001 |
| • Secondary | 1193 (34.2) | 179 (43.6) | |
| • Professional training | 663 (18.6) | 64 (15.2) | |
| • Tertiary | 1407 (39.6) | 124 (30.4) | |
| Physical health | |||
| • No discomfort | 2272 (65.0) | 189 (47.7) | < 0.001 |
| • Slight discomfort | 684 (19.4) | 93 (22.6) | |
| • Moderate discomfort | 388 (11.1) | 74 (17.2) | |
| • Strong discomfort | 131 (3.7) | 39 (9.4) | |
| • Extreme discomfort | 25 (0.8) | 12 (3.1) | |
| Social support scale (3–14) | 11.13 (1.89)* | 10.39 (0.12)* | < 0.001 |
| Depressive symptoms scale (0–24) | 3.96 (0.08)* | 14.09 (0.19)* | < 0.001 |
| Substance use disorder | |||
| • Scale (0–4) | 0.10 (0.01)* | 0.31 (0.05)* | < 0.001 |
| • No (< 2) | 3406 (97.2) | 376 (92.1) | < 0.001 |
| • Yes (≥ 2) | 94 (2.8) | 31 (7.9) | |
Weighted proportions and unweighted frequencies are displayed for categorical variables, and mean with standard deviation (SD) is displayed for scales (*)
aGroups according to depressive symptoms (< 10 vs. ≥ 10) were compared using Chi square test for categorical variables and Student’s t-test for scales
Table 2 shows coefficients of unadjusted and adjusted Tobit regressions models of variables associated with depressive symptoms. Being female, with poor physical health, younger age, and presenting substance use disorder and low levels of social support were significantly associated with depressive symptoms in unadjusted and adjusted models. Nevertheless, lower educational levels were significantly associated with depression as well in adjusted models. According to the interaction included in the adjusted model, the association between substance use disorder and depressive symptoms was stronger for those with lower levels of social support.
Table 2.
Tobit regression models of factors related to depressive symptoms
| Bivariate Coef. [95% CI] |
Multivariate Coef. [95% CI] |
|
|---|---|---|
| Intercept | - | 9.18 [7.56; 10.79] |
| Sex | ||
| • Male | Ref | Ref |
| • Female | 1.61 [1.20; 2.03]*** | 1.60 [1.22; 1.98]*** |
| Age group | ||
| • 18–34 | Ref | Ref |
| • 35–49 | − 1.55 [− 2.1; − 0.99]*** | − 1.41 [− 1.94; − 0.88]*** |
| • 50–64 | − 2.39 [− 2.95; − 1.83]*** | − 2.89 [− 3.42; − 2.35]*** |
| • 65–79 | − 3.95 [− 4.62; − 3.28]*** | − 4.81 [− 5.46; − 4.15]*** |
| • 80 + | − 2.58 [− 3.83; − 1.33]*** | − 4.53 [− 5.77; − 3.30]*** |
| Education level | ||
| • Primary | Ref | Ref |
| • Secondary | 0.09 [− 0.88; 1.05] | − 0.72 [− 1.63; 0.18] |
| • Professional training | − 0.73 [− 1.74; 0.27] | − 1.45 [− 2.40; − 0.50]** |
| • Tertiary | − 0.93 [− 1.88; 0.02] | − 1.41 [− 2.31; − 0.50]** |
| Physical health | ||
| • No discomfort | Ref | Ref |
| • Slight discomfort | 1.24 [0.73; 1.76]*** | 1.69 [1.21; 2.16]*** |
| • Moderate discomfort | 2.51 [1.83; 3.19]*** | 3.17 [2.50; 3.84]*** |
| • Strong discomfort | 3.95 [2.83; 5.07]*** | 4.45 [3.31; 5.58]*** |
| • Extreme discomfort | 6.33 [3.18; 9.47]*** | 6.95 [3.97; 9.92]*** |
| Social support scale | ||
| • Social support | − 0.57 [− 0.69; − 0.45]*** | − 0.42 [− 0.54: − 0.31]*** |
| Substance use disorder | ||
| • No | Ref | Ref |
| • Yes | 5.46 [4; 6.92]*** | 10.42 [3.92; 16.93]** |
| Interaction: social support × substance use disorder | ||
| • No–No | - | Ref |
| • Yes–Yes | - | − 0.59 [− 1.19; − 0.01]* |
*p < 0.05, **p < 0.01, ***p < 0.001
Figure 1 depicts the approximate PHQ-8 depression scale mean scores stratified by social support level and drug abuse status. The graph shows that the impact of substance use disorder on depressive symptoms was higher when the social support was low. Participants with lower levels of social support (3–8) and with substance use disorder had depressive symptoms above the major depressive disorder cut-off score (PHQ8 = 10.5, CI 95% 8.5, 12.5 at social support = 8).
Discussion
To the best of our knowledge, this is one of the first studies to examine the moderating role of social support in the association between substance use disorder and depressive symptoms in the context of the COVID-19 outbreak. Substantial differences concerning the effect of substance use disorder on depression were found in terms of social support levels. The link between substance use disorder and depression was indeed stronger among participants reporting low social support levels, leading to a reported level of depressive symptoms above the limit for major depressive disorder.
These results are consistent with those of previous studies indicating a correlation between substance use disorder (Anand et al., 2019) and low levels of social support (Guntzviller et al., 2020), with greater depression. Moreover, according to our results, interventions based on providing social support to people with substance use disorder could lower the risk of developing depressive symptoms. In turn, higher levels of social support may help lower substance use disorder since mental well-being has been found to be a factor facilitating this (Birtel et al., 2017).
In addition to social support and substance use disorder, we found that depression was associated with being female, with physical health problems, and with lower levels of education, which is consistent with previous studies (Haro et al., 2006). Moreover, the present results suggest that being younger is associated with higher levels of depressive symptoms, which is also in line with previous studies conducted in the context of the COVID-19 lockdown (Solomou & Constantinidou, 2020). The lockdown seems to have affected younger adults in particular, probably because their psychosocial well-being depends on frequent social interactions to a greater extent than it does for older adults (Carstensen, 1993).
A systematic review has shown that the protective effect of distinct social support providers varies depending on age. Parental support was most important among children and adolescents, whereas adults and older adults relied more on spouses, followed by family and then friends (Gariépy et al., 2016).
We found a substance use disorder prevalence of 7.9% in people with major depressive disorder. This prevalence was higher than in the general population (2.8%) but lower than that reported by a recent systematic review about substance use disorder in major depressive disorder, which was 25% (Hunt et al., 2020). However, because of the varying instruments used to measure substance use disorder in the studies included in this systematic review, there is a wide range in the prevalence reported, from 7 to 51% (Currie et al., 2005; Mueser et al., 2000). Our study has a range of strengths, including the use of a large community-representative sample of Spanish adults from various socioeconomic backgrounds and the ability to control for confounding factors. Nevertheless, we must note several limitations. The cross-sectional design hinders the interpretation of the described associations as causal. Our data are based on self-reports, which could result in recall or reporting bias. Despite this, to minimize recall bias, we kept recall periods short and well-defined in our research. Finally, since the study was focused on depressive symptoms, we used a screening measure for major depressive disorder. Future studies should replicate our results using a structured psychiatric interview for diagnosis, as this is a more accurate tool.
Conclusion
The findings of this study highlight the importance of objective social support in the relationship between substance use disorder and depression, especially in stressful and unprecedented situations, such as the COVID-19 outbreak in Spain. It appears that maintaining social communication during lockdowns and improving social relationships can minimize the effect of substance use disorder on mental health and facilitate the ceasing of substance use disorder.
Author Contribution
The study was designed by LHF, JD-A, AG–P, MF-N, PM, GV, BO, JA, RLC, and JMH. JD-A conducted the data analyses. LHF and AG–P drafted the article. JD-A supervised the data analyses and development of the paper. The paper was edited and reviewed by all the authors.
Funding
This work was supported by the Instituto de Salud Carlos III, Ministerio de Ciencia, e Innovación (grant number COV20/00711). Philippe Mortier has a Sara Borrell research contract awarded by the ISCIII (CD18/00049). Joan Domènech-Abella has a Juan de la Cierva research contract awarded by the Ministry of Science and Innovation (FJC2019-038955-I).
Declarations
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alsheikh, A. M., Elemam, M. O., & El-bahnasawi, M. (2020). Treatment of depression with alcohol and substance dependence: A systematic review. Cureus, 12(10), e11168. 10.7759/cureus.11168 [DOI] [PMC free article] [PubMed]
- Anand D, Paquette C, Bartuska A, Daughters SB. Substance type moderates the longitudinal association between depression and substance use from pre-treatment through a 1-year follow-up. Drug and Alcohol Dependence. 2019;197:87–94. doi: 10.1016/j.drugalcdep.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birtel MD, Wood L, Kempa NJ. Stigma and social support in substance use disorder: Implications for mental health and well-being. Psychiatry Research. 2017;252:1–8. doi: 10.1016/j.psychres.2017.01.097. [DOI] [PubMed] [Google Scholar]
- Blanco C, Alegría AA, Liu SM, Secades-Villa R, Sugaya L, Davies C, Nunes EV. Differences among major depressive disorder with and without co-occurring substance use disorders and substance-induced depressive disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry. 2012;73(6):865–873. doi: 10.4088/JCP.10m06673. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106(5):906–914. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- Brown, R. L., & Rounds, L. A. (1995). Conjoint screening questionnaires for alcohol and other drug abuse: Criterion validity in a primary care practice. Wisconsin Medical Journal, 94(3), 135–140. [PubMed]
- Carstensen, L. L. (1993). Motivation for social contact across the life span: A theory of socioemotional selectivity. In J. E. Jacobs (Ed.), Current theory and research in motivation, Vol. 40. Nebraska Symposium on Motivation, 1992: Developmental perspectives on motivation (p. 209–254). University of Nebraska Press. [PubMed]
- Cong, R. (2001). Marginal effects of the tobit model. Stata Technical Bulletin, 10(56).
- Currie SR, Patten SB, Williams JV, Wang J, Beck CA, El-Guebaly N, Maxwell C. Comorbidity of major depression with substance use disorders. The Canadian Journal of Psychiatry. 2005;50(10):660–666. doi: 10.1177/070674370505001013. [DOI] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, Rajaratnam SMW. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, L. L., Rush, J. A., Wisniewski, S. R., Rice, K., Cassano, P., Jewell, M. E., ... & McGrath, P. J. (2005). Substance use disorder comorbidity in major depressive disorder: An exploratory analysis of the Sequenced Treatment Alternatives to Relieve Depression cohort. Comprehensive psychiatry, 46(2), 81-89. [DOI] [PubMed]
- Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, Ayuso-Mateos JL, Mundó J, Haro JM. Loneliness and depression in the elderly: The role of social network. Social Psychiatry and Psychiatric Epidemiology. 2017;52(4):381–390. doi: 10.1007/s00127-017-1339-3. [DOI] [PubMed] [Google Scholar]
- Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the U.S. and Canada—A systematic review and meta-analysis. Journal of Clinical Medicine. 2018;7(12):543. doi: 10.3390/jcm7120543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: Systematic review of current findings in western countries. British Journal of Psychiatry. 2016;209(4):284–293. doi: 10.1192/bjp.bp.115.169094. [DOI] [PubMed] [Google Scholar]
- Guntzviller LM, Williamson LD, Ratcliff CL. Stress, social support, and mental health among young adult Hispanics. Family and Community Health. 2020;43(1):82–91. doi: 10.1097/FCH.0000000000000224. [DOI] [PubMed] [Google Scholar]
- Haro JM, Palacín C, Vilagut G, Martínez M, Bernal M, Luque I, Codony M, Dolz M, Alonso J. Prevalence of mental disorders and associated factors: Results from the ESEMeD-Spain study. Medicina Clinica. 2006;126(12):445–451. doi: 10.1157/13086324. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59(4):375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Hunt GE, Malhi GS, Lai HMX, Cleary M. Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: Systematic review and meta-analysis. Journal of Affective Disorders. 2020;266:288–304. doi: 10.1016/j.jad.2020.01.141. [DOI] [PubMed] [Google Scholar]
- Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics. 2020;32(10):1217–1220. doi: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INE, Instituto Nacional de Estadística (National Statistics Institute). (2019). Retrieved August 21, 2021, from https://www.ine.es/dynt3/inebase/es/index.htm?padre=517&capsel=522.
- Kocalevent RD, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, Nater U, Brähler E. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3) BMC Psychology. 2018;6(1):31. doi: 10.1186/s40359-018-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Li, F., Luo, S., Mu, W., Li, Y., Ye, L., Zheng, X., ... & Chen, X. (2021). Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry, 21(1), 1–14. 10.1186/s12888-020-03012-1. [DOI] [PMC free article] [PubMed]
- Liu J, Wei W, Peng Q, Guo Y. How does perceived health status affect depression in older adults? Roles of attitude toward aging and social support. Clinical Gerontologist. 2021;44(2):169–180. doi: 10.1080/07317115.2019.1655123. [DOI] [PubMed] [Google Scholar]
- Long, J. S. (1997). Regression models for categorical and limited dependent variables | SAGE Publications Inc (Vol. 7). Retrieved August 21, 2021, from https://us.sagepub.com/en-us/nam/regression-models-for-categorical-and-limited-dependent-variables/book6071.
- Mueser KT, Yarnold PR, Rosenberg SD, Swett C, Jr, Miles KM, Hill D. Substance use disorder in hospitalized severely mentally ill psychiatric patients: Prevalence, correlates, and subgroups. Schizophrenia Bulletin. 2000;26(1):179–192. doi: 10.1093/oxfordjournals.schbul.a033438. [DOI] [PubMed] [Google Scholar]
- Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed]
- Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. International Journal of Environmental Research and Public Health. 2020;17(14):1–19. doi: 10.3390/ijerph17144924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanish Drug Observatory (2015). [2013–2014 Survey on the use of psychoactive substances in the workplace in Spain]. Madrid: Ministry of Health and Social Policy. Retrieved August 21, 2021, from https://pnsd.sanidad.gob.es/en/noticiasEventos/dossier/pdf/EncuestaLaboral2013.pdf.
- StataCorp. (2013). Stata Statistical Software: Release 13. Statacorp LP, College Station, TX
- Taylor, S., Paluszek, M. M., Rachor, G. S., McKay, D., & Asmundson, G. J. (2021). Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addictive Behaviors, 114, 106754. 10.1016/j.addbeh.2020.106754 [DOI] [PMC free article] [PubMed]
- Van Buuren, S. (2018). Flexible imputation of missing data. CRC press. 10.1201/9780429492259
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viseu J, Leal R, de Jesus SN, Pinto P, Pechorro P, Greenglass E. Relationship between economic stress factors and stress, anxiety, and depression: Moderating role of social support. Psychiatry Research. 2018;268:102–107. doi: 10.1016/j.psychres.2018.07.008. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: global health estimates (No. WHO/MSD/MER/2017.2). World Health Organization.


