ABSTRACT
Developing an effective and safe vaccine against Covid-19 will facilitate return to normal. Due to hesitation toward the vaccine, it is crucial to explore the acceptability of the COVID-19 vaccine to the public and healthcare workers. In this cross-sectional survey, we invited 2251 pediatricians and 506 (22%) of them responded survey and 424 (84%) gave either nasopharyngeal swap or antibody assay for COVID-19 and 71 (14%) of them got diagnosis of COVID-19. If the effective and safe COVID-19 vaccine was launched on market, 420 (83%) of pediatrician accepted to get vaccine shot, 422 (83%) of them recommended vaccination to their family members, 380 (75%) of them accepted to vaccine their children and 445 (85%) of them offered vaccination to their pediatric patients. Among the participated pediatricians 304 (60%) of them thought COVID-19 vaccine should be mandatory. We found that there are high COVID-19 vaccine willingness rates for pediatricians for themselves, their own children, family members and their pediatric patients. We also found that being a pediatric subspecialist, believing in achieving an effective vaccine, willingness to participate in the phase 1–2 clinical vaccine trial, willingness to get an influenza shot this season, believing a vaccine and vaccine passport should be mandatory were significant factors in accepting the vaccine. It is important to share all information about COVID-19 vaccines, especially effectiveness and safety, with the public in a clear communication and transparency. The opposite will contribute to vaccine hesitancy and anti-vaccine movement.
KEYWORDS: COVID-19, healthcare workers, pediatricians, vaccine acceptance, vaccine hesitancy, Turkey
Introduction
Over 100 million confirmed infections and over 2 million deaths of coronavirus disease (COVID-19) have been reported globally since the start of the COVID-19 pandemic to December 3, 2020.1 The disease has spread to all countries in the world and caused social and economic destruction in some countries. In Turkey, the first confirmed COVID-19 case was reported by Turkish Ministry of Health on March 11, 2020, and up to December 16, 2020, a total of 1.928.165 confirmed cases and 17.121 deaths have been reported, despite strict pandemic control measures declared by the Turkish government.2 Since December 2019, nearly one hundred thousand of healthcare workers (HCWs) worldwide were infected with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).3 In December 2020, the Ministry of Health announced that the number of infected HCWs exceeded 120.000, and 216 HCWs died due to COVID-19 in Turkey. There is a rising concern that patients who recover from COVID-19 may be at risk of re-infection. Recently, articles about the recurrence of positive SARS-CoV-2 cases among recovered COVID-19 patients have been published.4–6 Increased rates of infection and recurrence in HCWs could cause the healthcare system collapse and a further worsening of the COVID-19 pandemic; if there are too few HCWs it will be even more difficult to manage.
Until now, there is neither a specific effective medication nor vaccinations for treatment and prevention of COVID-19. To date, over 160 COVID-19 vaccine candidates are under development, with 26 in human trials.7 Three vaccines have been shown to be efficacious and are being distributed and two more (J&J, Novavax) have been shown to be efficacious and are expected to be distributed. Vaccination will be one of the most effective strategies in stopping the spread of the SARS-CoV-2. It is currently thought that developing some effective vaccines for SARS-CoV-2 will be relatively straightforward and attainable since the virus seems to be fairly stable.8 Therefore, acceptance of COVID-19 vaccinations is important in preventing spread of COVID-19. Many factors could affect acceptance of newly developed vaccines, especially among HCWs, who have a higher risk of being infected with COVID-19. Specifically, during a viral pandemic, like H1N1 pandemic, if the HCWs perceived the developed vaccine is safe and effective in preventing infection of self and others, and if they perceived the viral pandemic severe, their acceptance of vaccination increases.9 For example, during the 2009/2010 H1N1 pandemic season, influenza vaccination increased in population in Beijing, China but decreased in the pre-pandemic season in 2010/2011 season.10 Even with the presence of strong recommendations about influenza vaccination for HCWs, the acceptance and coverage of vaccination among HCWs varies between 12 and 76% in non-pandemic normal seasons.11–13 Since influenza and COVID-19 shared similar mode of transmission and clinical characteristics, COVID-19 pandemic may affect the uptake of seasonal influenza vaccine.
To the best of our knowledge, the HCWs’, especially pediatricians’ views on the willingness to receive COVID-19 vaccine are not clearly known and there are no data on COVID-19 vaccines acceptance or hesitancy rates during the COVID-19 pandemic. Thus, in this study, we aimed to examine the effect of COVID-19 pandemic on the acceptance of influenza vaccine and to explore the factors associated with willingness to receive COVID-19 vaccination among the pediatricians.
Materials and methods
Sample and procedures
The Turkish Pediatric Workshop group was established by authors AS, EG, ET, TT and MK on Telegram application on October 31, 2018 for the first time. The group consists mainly of pediatricians, pediatric subspecialists, pediatric surgeons, child psychiatry specialists, and physicians serving for pediatric population including pediatric dermatology, pediatric ENT, pediatric radiology, pediatric urology and finally an advocate – pediatrics specialist for issues about pediatric malpractice and other medico legal cases. Group members were included by invitation and memberships were confirmed by telegram group directors. The Turkish Pediatric Workshop group works in a way that all members can ask any questions related with pediatrics, radiological images, dermatologic conditions in patients, laboratory results, drug dosages, etc.14
Questionnaire information
Online questionnaires organized using Google Forms were sent to pediatric workshop members between 1 and 15 November 2020. The questionnaire consisted of questions that measured the participants’ basic demographic data, the usage of the workshop and the overall impact of the workshop on their professional behavior, which province and in which specialty (pediatrician and/or pediatric subspecialist) they work, questions about themselves or family members suffering from Covid-19, knowledge and factors affecting the acceptance of COVID-19 and influenza vaccination. The pediatricians provided consent for participation in the online survey. The survey is available in the end of the article. This study was ethically approved by the Istanbul Memorial Şişli Hospital ethics committee.
Data analysis
Data were analyzed using Stata 10.0 Statistics/Data Analysis (StataCorp, College Station, TX, USA). For the univariate analysis, Student’s t-test, Pearson χ2 test and Fisher–Freeman–Halton exact test were used for categorical and continuous variables. When appropriate, categorical variables were further tested in a multivariate analysis by using logistic regression analysis. Significance was set at p < .05.
Results
Since the establishment of the Turkish Pediatric Atelier, 2251 pediatric specialists, subspecialists and specialists related to pediatrics have been involved in this network. The response rate was 22% (n = 506) for the survey among all active members of Turkish Pediatric Atelier.
In all, 297 (58%) of these responders were women, 209 were men, 66% were 45 years and under. Mean age of responded pediatricians was 41 ± 8 years (range 26–66 years). For health status, 89 (18%) of them reported to have chronic diseases and 70 (14%) of them reported tobacco usage. Participants included 458 (90%) pediatrician, and 48 (10%) pediatric subspecialists (Table 1). At least pediatricians working in 64 (%79) out of a total of 81 cities of Turkey were involved in the survey. Out of the 506 respondents, 224 (44%) were working in Istanbul, 27 (5%) in Ankara, 17 (3%) in Bursa, 16 (3%) Kocaeli, 15 (%3) in Tekirdağ, and 14 (3%) in Izmir, and others are shown in Table 1. Among the responders, 225 (44%) were working in private hospitals, 136 (27%) were working in state hospitals, 110 (23%) were working in University or Teaching hospitals and 35 (7%) in a doctor’s office (Table 1). 424 (%84) of pediatricians had treated or followed-up children with COVID-19. Moreover, among the 506 pediatricians, 362 (72%) of them either from a nasopharyngeal swap PCR or an antibody assay were suspected to have COVID-19, and unfortunately, 71 (14%) of them were diagnosed with SARS-CoV-2 infection. Moreover, 105 (20%) pediatricians reported one of their family members diagnosed with COVID-19, and 395 (78%) of them reported one of their close friends/relatives diagnosed with COVID-19. Besides, 115 (23%) pediatricians also revealed that at least one of their friend’s/family members has died because of COVID-19. During their daily life, 98% (n = 505) of the pediatricians were wearing masks, 96% (n = 488) obeying social distancing rules, 96% (n = 487) using hand-hygiene products, 56% (n = 282) avoiding crowded places and 25% (n = 128) using face shields. Moreover, when pediatricians were asked what they were doing during their daily pediatric clinical practice regarding healthcare settings, 100% reported (n = 506) using a mask, 31% (n = 160) using gloves, 26% (n = 130) wearing glasses, 24% (n = 120) using face shields and 14% (n = 160) wearing gowns.
Table 1.
Demographic characteristics of pediatricians
| Characteristics | Data n (%) |
|---|---|
| Survey response rate | 506/2251 (22%) |
| Gender | |
| Male | 209 (42%) |
| Female | 297 (58%) |
| Age (years) | |
| 26–35 | 169 (33%) |
| 36–44 | 168 (33) |
| 45–60 | 153 (30%) |
| >60 | 16 (4%) |
| Presence of chronic diseases | 89 (18%) |
| Having a child | 379 (75%) |
| Tobacco use | 70 (14%) |
| Specialty area | |
| Pediatrician | 190 (49%) |
| Pediatric subspecialist | 82 (21) |
| Instutition | |
| Private hospitals | 225 (44%) |
| University and teaching hospitals | 110 (22%) |
| State hospitals | 136 (27%) |
| Doctor office | 32 (6%) |
| City | |
| Istanbul | 224 |
| Ankara | 27 |
| Bursa | 17 |
| Kocaeli | 16 |
| Tekirdağ | 15 |
| İzmir | 14 |
| Sakarya | 11 |
| Diyarbakır | 11 |
| Tokat | 11 |
| Konya | 10 |
| Antalya | 10 |
| Gaziantep | 9 |
| Batman | 9 |
| Others | 122 |
Knowledge of COVID-19 vaccine and factors affecting the acceptance of COVID-19 vaccination
In Table 2, we summarized responses of pediatricians about COVID-19-related questions. When the pediatricians were asked where they were getting the information related to COVID-19, 373 (74%) of them reported they regularly read scientific literature, 39 (8%) of them reported following the Ministry of Health COVID-19-related announcements and 94 (18%) of them got their information from social, written or visual media. Among the responding pediatricians, 350 (69%) of them knew that phase 2 and 3 vaccine research studies have been going on, 91 (17%) of them following social and other media were up-to-date regarding COVID-19 vaccines, 40 (7%) of them regularly read scientific articles related to COVID-19 vaccines and 25 (%4) of them had no idea about COVID-19 vaccines. Among all participants, 214 (42%) of them had no idea what types of COVID-19 vaccines were undergoing research, 113 (22%) of them stated that mRNA-based vaccines will be a success, 72 (14%) stated that live vaccines will be a success, 65 (12%) of them thought inactive virus vaccine will be a success, 28 (5%) Adenovector vaccines will be a success and 14 (3%) of them thought the same about DNA vaccines. As stated in the responses, 67% (n = 340) of pediatricians believe that an effective COVID-19 vaccine will be launched onto the market and 285 (56%) of them thought that vaccination will be repeated every year, 152 (30%) thought vaccination will be repeated every 6 months and only 24 (4%) thought the vaccine will offer a life-long protection. Only 79 (16%) pediatricians accepted to participate in a phase 2 clinical COVID-19 vaccine trial as a subject. When the pediatricians were asked what the most important aspect of COVID-19 vaccine for them was, 293 (57%) of them reported that the vaccine should be safe, 206 (40%) reported it should have enough protection, only 6 of them reported that the country origin of the vaccine manufacturer is important and only one pediatrician reported the price of vaccine to be the most important. If an effective and safe COVID-19 vaccine was launched onto the market, 420 (83%) of pediatricians would accept to get vaccine shot, 422 (83%) of them would recommend vaccination to their family members, 380 (75%) of them would accept to vaccinate their children and 445 (85%) of them would offer vaccination to their pediatric patients (Figure 1). While the rate of pediatricians who received the seasonal influenza vaccine last year was 39.1%, this year the rate of those who wanted to get this vaccine was found to be 69.9% (Figure 1). When pediatricians were asked which group should be vaccinated first in case of access to a limited number of vaccines, 232 (45%) of the participants replied HCWs, 173 (34%) replied people with chronic diseases, and 76 (15%) replied elderly people (age >65 years). Among the participating pediatricians, 304 (60%) of them thought that if an effective vaccine is to be available, it should be mandatory and 303 (60%) of them thought that for travel, attending school and public activities, a COVID-19 vaccine passport should be mandatory.
Table 2.
Responses of pediatricians to COVID-19-related questions
| Quotes | Total (n) | Yes n,% | No n,% |
|---|---|---|---|
| Serve for COVID-19 suspected or infected children | 506 | 424 (84%) | 82 (16%) |
| History of a having a COVID-19 test (either PCR or antibody assay) | 506 | 362 (72%) | 144 (28%) |
| History of infection with SARS-CoV2 during the pandemic | 506 | 71 (14%) | 435 (86%) |
| Any of family members infected with SARS-CoV-2 | 506 | 105 (20%) | 401 (80%) |
| Any of close circle friends infected with SARS-CoV-2 | 506 | 395 (78%) | 111 (22%) |
| Any of your close friends or family member death due to COVID-19 | 506 | 115 (23%) | 391 (77%) |
| Source of COVID-19 related information | |||
| (a) Regularly following literature | 506 | 373 (73%) | - |
| (b) Ministry of Health announces | 506 | 39 (8%) | - |
| (c) Social media and newspapers | 506 | 94 (19%) | - |
| Believe that effective COVID-19 vaccine will be developed | 506 | 340 (67%) | 166 (33%) |
| Most important factor for COVID-19 vaccine acceptance | |||
| (a) Safety of vaccine | 506 | 293 (57%) | - |
| (b) Protectivity of vaccine | 506 | 206 (41%) | |
| (c) Country of vaccine manufacturer | 506 | 6 (1%) | |
| (d) Price of vaccine | 506 | 1 (1%) | |
| Willing to participate as a subject in phase 2 COVID-19 vaccine research | 506 | 79 (16%) | 427 (84%) |
| Willing to get vaccinated if effective COVID-19 vaccine available | 506 | 420 (83%) | 86 (17%) |
| Willing to vaccinate their family member if effective COVID-19 vaccine available | 506 | 422 (83%) | 84 (17%) |
| Willing to vaccinate their children member if effective COVID-19 vaccine available | 506 | 380 (75) | 126 (25%) |
| Willing to vaccinate their children member if effective COVID-19 vaccine available | 506 | 445 (86%) | 61 (14%) |
| COVID-19 vaccine knowledge level | 506 | ||
| (a) No idea | 25 (4%) | - | |
| (b) Got information from social media and newspaper | 91 (17%) | ||
| (c) Reading regularly scientific articles | 40 (7%) | ||
| (d) Just know phase 2 and 3 studies continued | 350 (72%) | ||
| COVID-19 vaccine should be mandatory | 506 | 303 (59%) | 203 (41%) |
| COVID-19 vaccine passport should be mandatory for school entrance or travel | 506 | 303 (59%) | 203 (41%) |
| Which of the people should receive firstly COVID-19 vaccine in population if doses is limited | 506 | ||
| Healthcare workers | 232(46%) | ||
| People with chronic diseases | 173(34%) | ||
| People age over 65 years | 76 (15%) | ||
| Children | 82 | ||
| Health adult | 173 | ||
| Which of the COVID-19 vaccine will be effective? | 506 | ||
| No idea | 214(42%) | ||
| mRNA-based vaccines | 113(22%) | ||
| Inactive whole viral vaccines | 65(12%) | ||
| Attenuated live viral vaccines | 72(14%) | ||
| Adenoviral vector-based vaccines | 28(6%) | ||
| DNA vaccines | 14(45) | ||
| What do you think about vaccination schedule of probable covid19 vaccine | |||
| Annual vaccination | 285(57%) | ||
| Biannual period vaccination | 7 (1%) | ||
| 6 months interval vaccination | 152(28%) | ||
| No idea | 38 (9%) | ||
| Single dose for lifelong | 24 (5%) | ||
| Which is the most effective strategy for stopping covid19 pandemic | |||
| Vaccination | 342(68%) | ||
| Herd immunity | 102(20%) | ||
| Total closure for 14 days | 37 (7%) | ||
| Social distance | 20 (5%) |
Figure 1.
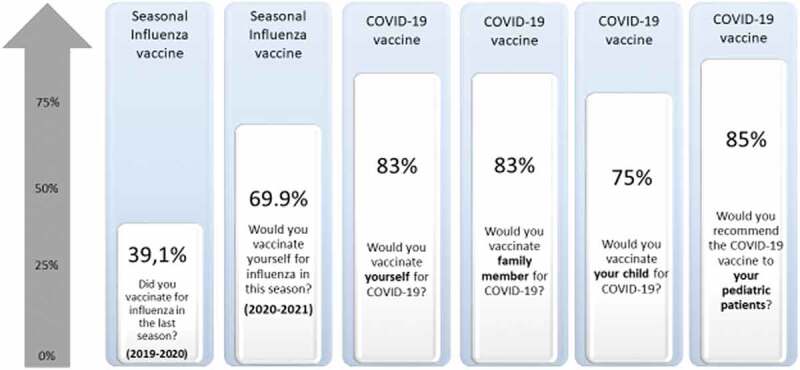
Pediatricians’ willingness for influenza and COVID-19 vaccines upon themselves, family members, their child/children and their pediatric patients
In the univariate analysis, we revealed that pediatricians of male gender, pediatricians believing that an effective COVID-19 vaccine will be developed, pediatricians accepted to be enrolled as a subject in phase 2 clinical COVID-19 vaccine trial, pediatricians who thought that COVID-19 vaccine should be mandatory, pediatricians who thought that COVID-19 vaccine passport should be used in entrance to school and travel, pediatricians who were vaccinated with influenza vaccine in year 2019 and pediatricians who wanted to get influenza vaccine shot in year 2020 had a higher rate of COVID-19 vaccination willingness (Table 3).
Table 3.
Factors associated with acceptance of COVID-19 vaccination in pediatricians
| Features of pediatricians | Total number (n=) | COVID-19 vaccine acceptant n = (%) | COVID-19 vaccine non-acceptant n = (%) | P value |
|---|---|---|---|---|
| Age | ||||
| < 45 years | 337 | 282 (83%) | 55 (17%) | 0.32 |
| ≥ 45 years | 169 | 138 (81%) | 31 (19%) | |
| Gender | ||||
| Female | 297 | 236 (79%) | 61 (21%) | 0.01 |
| Male | 209 | 184 (88%) | 25 (12%) | |
| Specialty | ||||
| Pediatrician | 458 | 374 (82%) | 84 (18%) | |
| Pediatric subspecialist | 48 | 46 (96%) | 2(4) | |
| Chronic Diseases | <0.01 | |||
| Not present | 417 | 345 (83%) | 72 (17%) | 0.12 |
| Present | 89 | 75 (84%) | 14 (16%) | |
| Tobacco Usage | ||||
| No | 436 | 362 (83%) | 74 (17%) | 0.79 |
| Yes | 70 | 59 (84%) | 11 (16%) | |
| Having a child | ||||
| No | 127 | 107 (84%) | 20 (16%) | 0.7 |
| Yes | 379 | 314 (82%) | 65 (18%) | |
| Covid-19 test (PCR or Ab) | ||||
| Not done | 144 | 121 (84%) | 23 (16%) | 0.69 |
| Done | 362 | 299 (83%) | 63 (17%) | |
| History of SARS-CoV2 infection | ||||
| Not-infected | 435 | 363 (83%) | 72 (17%) | 0.51 |
| Infected | 71 | 57 (80%) | 14 (20%) | |
| History of SARS-CoV2 infection in family | ||||
| Not-infected | 401 | 337 (84%) | 64 (16%) | 0.22 |
| Infected | 105 | 83 (79%) | 22 (21%) | |
| History of SARS-CoV2 infection in close friends | ||||
| Not-infected | 111 | 90 (81%) | 21 (19%) | 0.54 |
| Infected | 395 | 330 (83%) | 65 (17%) | |
| Dead due to COVID-19 in close friends/family | ||||
| No | 391 | 324 (82%) | 67 (18%) | 0.87 |
| Yes | 115 | 96 (83%) | 19 (17%) | |
| Serve for COVID-19 patients | ||||
| No | 82 | 68 (82%) | 14 (18%) | 0.98 |
| Yes | 424 | 352 (83%) | 72 (17%) | |
| Effective vaccine will be developed | ||||
| No | 166 | 110 (65%) | 56 (35%) | <0.0001 |
| Yes | 340 | 310 (91%) | 110 (9%) | |
| Intent to be enrolled in phase 2 vaccine study | ||||
| No | 427 | 340 (73%) | 85 (27%) | 0.00004 |
| Yes | 79 | 78 (99%) | 1 (1%) | |
| COVID-19 vaccine should be mandatory | ||||
| No | 203 | 133 | 70 | <0.00001 |
| Yes | 303 | 287 | 16 | |
| COVID-19 vaccine passport should be mandatory | ||||
| No | 203 | 135 | 68 | <0.0001 |
| Yes | 303 | 285 | 18 | |
| Influenza vaccination in 2019 season | <0.0001 | |||
| No | 308 | 240 (77%) | 68 (23%) | |
| Yes | 198 | 180 (90%) | 18 (10%) | |
| Willing to influenza vaccination in 2020 | ||||
| No | 152 | 104 (68%) | 48 (32%) | <0.0001 |
| Yes | 354 | 316 (89%) | 38 (11%) |
The multivariate logistic regression analysis showed that being a pediatric subspecialist (p = .02), participants believing an effective vaccine will be achieved (p < .01), pediatricians willing to participate in phase 1–2 clinical vaccine trial (p = .039), and participants believing the vaccine should be mandatory (p < .001) and vaccine passport (p = .05) and participants want to get influenza shot in this season (p = .013).
Discussion
Effectiveness of the vaccines developed against COVID-19 will have positive effects on the education sector, the tourism sector and the country’s economy by reducing the morbidity and mortality of the disease, and will facilitate return to normal. While numerous clinical vaccine trials are in progress, some countries, such as Turkey, began to explain the immunization plan. The timeline for public distribution of an effective and safe vaccine in many countries is estimated to be between late 2020 and 2022.15 Due to vaccine hesitation, the availability of a safe and effective vaccine and the vaccine supply of countries sufficient population vaccination cannot be guaranteed. Indeed, the concept of ‘vaccine hesitancy’ has been considered by the World Health Organization (WHO) as “one of the top-ten threats to global health”.16 In planning for the near-future, availability of a COVID-19 vaccine, as well as focusing on how to deliver COVID-19 vaccine programs and ensure equitable vaccine allocation globally, it is crucial to explore the acceptability of a COVID-19 vaccine to the public. The success of any COVID-19 vaccination will depend on public willingness to receive the vaccination.17 Little is known today about the factors affecting the willingness of the COVID-19 vaccine for HCWs or the general population. Positive or negative factors to be identified can guide future strategies to improve vaccine acceptability. In this respect, analysis studies on vaccine willingness or hesitancy with various groups in the population are important to evaluate vaccine compliance rates. Due to the fact that the issue is current, articles on the willingness of COVID-19 vaccines in the general population have started to be published recently.18–22 In this cross-sectional survey study, we aimed to analyze the views of pediatricians, a specific group of HCWs, on the COVID-19 pandemic and the vaccines, and discuss the data in the light of current literature.
In our study, the high willingness of the male gender to be vaccinated is consistent with the studies in the literature, 20 and may be influenced by a number of factors, including courage and risk-taking tendencies toward the newly developed vaccine. The prevailing view is that although the number of male cases is not dissimilar to the number of female cases, men have about twice the risk of death from COVID-19, leading to a range of hypotheses, from lifestyles to differences in chromosomal structure.23 Children account for about 11.5% of total COVID-19 cases, about 1.7% of hospitalizations and 0.06% of deaths according to the reports.24 Pediatricians have to be closely related to the disease-related developments such as the vaccination studies. 424 (84%) of the pediatricians who participated in this study had treated or followed-up pediatric patients with COVID-19. 373 (74%) of the participants stated that they have updated their information with scientific publications about COVID-19. The rate of those who only got the information from social, written or visual media was 18% (n = 94). In survey studies conducted with different groups, it was observed that these rates were reversed in the literature. For example, in a survey study conducted with medical students, more than half of the participants (59.3%) stated that they followed the COVID-19 vaccine studies from social media, while the rate of those who followed scientific studies was reported as 26.7%.25 The rates of non-HCWs to follow studies on COVID-19 and its vaccine via media may be higher.26 HCWs especially clinicians such as pediatricians must do their best to disseminate up-to-date information on the vaccines in the light of scientific studies to the public and to correct the mistakes about vaccine hesitancy by using all media facilities. Fighting on this front is as important as fighting on the clinical front where COVID-19 patients are followed.
In our study, the willingness rates about a COVID-19 vaccine for pediatricians themselves, for their own children, for family members and for their pediatric patients were found to be 83%, 75%, 83%, 85%, respectively (Figure 1). In the survey study conducted by Dror et al. with both HCWs and the general population, they reported the willingness rate of the COVID 19 vaccine to be 78% in medical doctors, 61% in nurses and 75% in the general population. In the same study, vaccination willingness rates for their own children were found to be 60%, 55% and 70% in these groups.27 While the medical doctors participating in the study had a high COVID-19 vaccine willingness which was similar to our study, the willingness to receive the vaccine for their own children was found to be lower which was inconsistent with our study. In a survey with 1541 caregivers from six countries, 65% of caregivers reported that they intend to vaccinate their children against COVID-19, once a vaccine is available.18 In another study conducted by Palamenghi et al. with Italian citizens, it was reported that 59% of the respondents to be likely to receive a vaccine for COVID-19.28 In another survey study conducted with 735 students in Italy, 633 of the students (86.1%) were reported to be willing to get the COVID-19 vaccine.19 In another English study conducted with parents and caregivers, the rate of those who would definitely accept the COVID-19 vaccine for themselves and their children was found to be 55.8% and 48.2%, respectively. These rates rose to 79.5% and 82.9%, respectively, with those who stated they were unsure but leaning toward accepting a COVID-19 vaccine.17 In a survey study conducted with 1359 participants in Indonesia, 93% of the participants were willing to be vaccinated with a 95% effective COVID-19 vaccine, while the rate of those willing to be vaccinated for the 50% effective COVID-19 vaccine had fell to 67%.22 In the studies with different groups from different countries in the current literature, the COVID-19 vaccine willingness rates for the participants themselves ranged from 55.8% to 93%, and the COVID-19 vaccine willingness rate for their children ranged from 48.2% to 82.9%.17–22,27,28 The vaccine willingness rates of the pediatricians for both their own children and pediatric patients are higher than the average rates in studies conducted with other occupational groups in the literature, which may be related to the fact that pediatricians have the opportunity to observe more closely the contribution of vaccines to child health.
Many governments are looking for paths out of restrictive physical distancing measures imposed to control the COVID-19 pandemic. Some of them have suggested the use of COVID-19 immunity passports. Although the introduction of a vaccination passport provides some advantages for returning to work, school or normal life, it can also create disadvantages in terms of equitable and legal challenges.29 In our survey study, 60% of pediatricians thought that both the COVID-19 vaccine and the vaccine passport should be mandatory. The WHO explained that there is insufficient evidence on the effectiveness of antibody-mediated immunity to guarantee the reliability of the immunity passport.30 The same applies to the vaccine passport. Until it is clear at what rate and for how long the vaccines will provide protection, it may be a risky practice to start the vaccine passport application.
Even if the COVID-19 vaccines have high-efficacy rates, the public should accept the vaccine and most of the population must be vaccinated to control the pandemic. To increase the acceptability of the COVID-19 vaccine, there needs to be clear communication and transparency as to how COVID-19 vaccines are developed and tested, as well as safety and efficacy information.17 In addition, it is important to identify and analyze the factors affecting vaccine acceptability in order to effectively fight vaccine hesitancy. As a result of the analysis performed in our study, it was found that being a pediatric subspecialist, believing effective vaccine will be achieved, being willing to be participate in phase 1–2 clinical vaccine trial, wanting to get an influenza shot in this season, believing the vaccine should be mandatory and vaccine passport were factors that increase the willingness to get COVID-19 vaccine. According to our survey, the willingness for the COVID-19 vaccine of the participants who had the influenza vaccine in 2019 and who are considering getting it this year was significantly high. In an article by Dror et al., it was found that vaccination against seasonal influenza is the most important positive predictive factor in the tendency to accept a future COVID-19 vaccine which was consistent with our study.27 Similar results were reported in the survey study with HCWs from Malta conducted by Grech et al.20 In addition, they reported that concerns were related to insufficient knowledge about such a novel vaccine and especially the lack of information of its long-term side effects.20 In an international cross-sectional study with caregivers, greater willingness for COVID-19 vaccine was found to be associated with older children, children that were up-to-date with their vaccines, children with no chronic illness, cases where fathers were the ones to complete the survey, if the caregiver was older cases where the child or the caregiver reported they were immunized against influenza in the last year.18 While age was not an important factor in our study, it was found to be a significant factor in the willingness to be vaccinated in a study conducted in Italy. In particular, post hoc tests showed that the middle-age group had a reduced willingness to be vaccinated for Covid-19 in the study. They also found that willingness to be vaccinated was positively correlated with both trust in scientific research and general attitude toward vaccines’ efficacy.27 These findings are consistent with our findings that believe in obtaining an effective vaccine and willingness to participate in the phase 1–2 clinical vaccine trial as significant factors in our study.
Conducting the study only with pediatricians is one of the limitations of this study. The rates found may not match the vaccine willingness or hesitation rates of other occupational groups or the general population. Another limitation of the study is that it consists of local data. The second limitation of this study is that although the Turkish Pediatric Atelier has 2251 members, most of them do not actively follow the survey or posts on the network. This technical problem is the biggest reason for the low response rate (22%). There was no situation that could create a bias and change willingess or hesitation of the vaccination rates. Although the results of the study do not reflect the global situation, the data are important in terms of being a reference to research in the other countries.
In conclusion, there is an urgent need for safe and effective vaccines to protect people from SARS-CoV-2 infection. In order to control the pandemic, it is not enough just to implement COVID-19 vaccines but to have the needed wide acceptability and willingness in the populations. Therefore, identifying data on the acceptance or hesitancy of the novel vaccine and developing strategies in the light of this information play a key role in the pandemic control. In our study, we found that there are high COVID-19 vaccine willingness rates for pediatricians for themselves, their own children, family members and their pediatric patients, even though there is still vaccine hesitation among HCWs. We also found that being a pediatric subspecialist, believing in achieving an effective vaccine, willingness to participate in the phase 1–2 clinical vaccine trial, willingness to get an influenza shot this season, believing a vaccine and vaccine passport should be mandatory were significant factors in accepting the vaccine. When we analyzed other COVID-19 vaccine willingness studies in the literature, we observed that it is important to share all information about COVID-19 vaccines, especially effectiveness and safety, with the public in a clear communication and transparency. The opposite will contribute to vaccine hesitancy and anti-vaccine movement.
Appendix.
The members of the PedCovidVaC Study Group are as follows: Veli Korkmaz (Nusaybin State Hospital, Clinic of Pediatrics, Mardin, Turkey), Aslı Hasçelik (Bilgi Hospital, Clinic of Pediatrics, Ankara, Turkey), Şeyda Doğantan (Erciyes University Department of Pediatric Rehumatology, Kayseri, Turkey), Alper Özkılıç (Medicana International Hospital, Clinic of Pediatrics, Istanbul, Turkey), Fatma Mahsereci (Medical Park Gaziantep hospital, Clinic of pediatrics, Gaziantep), Şenay Acar Karaarslan (Ozel 2000 Medical Center, Clinic of Pediatrics, İstanbul, Turkey), Büşra Sultan Kibar (Yalova State Hospital Clinic of Pediatrics, Yalova, Turkey), Serdar Pop (Tokat Erbaa State Hospital, Clinic of Pediatrics, Tokat, Turkey), Gözde Nur Yurttaş (Tokat State Hospital, Clinic of Pediatrics, Tokat, Turkey) Gülberat İnce (Kuşadası State Hospital, Clinic of Pediatrics, Aydin, turkey), Can Polat (Memorial Şişli Hospital, Clinic of Pediatrics, İstanbul, Turkey).
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.WHO Coronavirus Disease (COVID-19) Dashboard . [accessed2020Dec3]. https://covid19.who.int/.
- 2.Turkish ministry of Health Covid19 information page . [accessed2020Dec3]. https://covid19.saglik.gov.tr/.
- 3.World Health Organization . Coronavirus disease (COVID-19) situation report. [accessed 2020 Dec 3]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200914-weekly-epi-update-5.pdf?sfvrsn=cf929d04_2.
- 4.Lafaie L, Célarier T, Goethals L, Pozzetto B, Grange S, Ojardias E, Annweiler C, Botelho‐Nevers E.. Recurrence or relapse of COVID-19 in older patients: a description of three cases. J Am Geriatr Soc. 2020;7. Online ahead of print. doi: 10.1111/jgs.16728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edridge AWD, Kaczorowska J, Hoste ACR, Bakker M, Klein M, Loens K, Jebbink MF, Matser A, Kinsella CM, Rueda P, et al. Seasonal coronavirus protective immunity is short-lasting. Nat Med. 2020;14. Online ahead of print. doi: 10.1038/s41591-020-1083-1. [DOI] [PubMed] [Google Scholar]
- 6.Long QX, Tang XJ, Shi QL, Li Q, Deng HJ, Yuan J, Hu J-L, Xu W, Zhang Y, Lv F-J, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020Aug;26(8):1200–04. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . The push for a COVID-19 vaccine; 2020. [cited 2020 Sept 21; accessed 2020 Dec 3]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines?gclid=EAIaIQobChMI48KIyeT56wIVzuntCh2nsggFEAAYASAAEgL46vD_BwE.
- 8.Mahase E. Covid-19: what do we know so far about a vaccine? BMJ. 2020Apr27;369:m1679. doi: 10.1136/bmj.m1679. [DOI] [PubMed] [Google Scholar]
- 9.Prematunge C, Corace K, McCarthy A, Nair RC, Pugsley R, Garber G. Factors influencing pandemic influenza vaccination of healthcare workers–a systematic review. Vaccine. 2012Jul6;30(32):4733–43. doi: 10.1016/j.vaccine.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 10.Wu S, Yang P, Li H, Ma C, Zhang Y, Wang Q. Influenza vaccination coverage rates among adults before and after the 2009 influenza pandemic and the reasons for non-vaccination in Beijing, China: a cross-sectional study. BMC Public Health. 2013;13(1):636. doi: 10.1186/1471-2458-13-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polat HH, Yalcin AN, Oncel S. Influenza vaccination. Rates, knowledge and the attitudes of physicians in a university hospital. Turk Klin J Med Sci. 2010;30:48–53. doi: 10.5336/medsci.2008-8117. [DOI] [Google Scholar]
- 12.Mistik S, Balci E, Elmali F. Primary healthcare professionals’ knowledge, attitude and behavior regarding influenza immunization; 2006–2007 season adverse effect profile. Bratisl Lek Listy. 2012;113:384–88. doi: 10.4149/bll_2012_088. [DOI] [PubMed] [Google Scholar]
- 13.Savas E, Tanriverdi D. Knowledge, attitudes and anxiety towards influenza A/H1N1 vaccination of healthcare workers in Turkey. BMC Infect Dis. 2010;10:281. doi: 10.1186/1471-2334-10-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gönüllü E, Soysal A, Can İ, Tutak E, Tunç T, Yıldız İ, Yeşilbaş O, Öner N, Anarat A, Soysal FG, et al. The use of social network in daily pediatric practice and education: Turkish Pediatric Atelier. Int J Pediatr. 2020:1–7. doi: 10.1155/2020/7301309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580:576–77. doi: 10.1038/d41586-020-01221-y. [DOI] [PubMed] [Google Scholar]
- 16.WHO Ten threats to global health in 2019. [accessed 2020 Dec 6]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 17.Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020Nov17;38(49):7789–98. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldman RD, Yan TD, Seiler M, Parra Cotanda C, Brown JC, Klein EJ, Hoeffe J, Gelernter R, Hall JE, Davis AL, et al. Caregiver willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine. 2020Nov10;38(48):7668–73. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020Aug;35(8):781–83. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grech V, Gauci C, Agius S. Vaccine hesitancy among Maltese healthcare workers toward influenza and novel COVID-19 vaccination. Early Hum Dev. 2020Oct1; 105213. doi: 10.1016/j.earlhumdev.2020.105213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020Sep29;38(42):6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Mudatsir M, et al. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020Jul14;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396(10250):532–33. doi: 10.1016/S0140-6736(20)31748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.AAP news . Pediatric COVID-19 cases surpass ‘tragic’ 1 million mark. [accessed 2020 Dec 6]. https://www.aappublications.org/news/2020/11/16/covid19children111620.
- 25.Çifcibaşı HS, Elibol A, Kef B, Gür B, Kolsuz S, Kurtoğlu B, Ipsalali, HO, Kükürtcü, N, Şenyiğit, E, Altinbaş, E, et al. Thoughts and awareness of medical students about the COVID-19 pandemic. Turk Med Stud J. 2020;7(2):44–64. [Google Scholar]
- 26.Liu M, Zhang H, Huang H. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health. 2020Nov4;20(1):1649. doi: 10.1186/s12889-020-09761-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020Aug;35(8):775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020Aug;35(8):785–88. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phelan AL. COVID-19 immunity passports and vaccination certificates: scientific, equitable, and legal challenges. Lancet. 2020May23;395(10237):1595–98. doi: 10.1016/S0140-6736(20)31034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO . “Immunity passports” in the context of COVID-19 scientific brief. [accessed2020 Dec 12]. https://www.who.int/publications-detail/immunity-passports-in-the-context-of-covid-19.


