Abstract
Purpose:
Cancer caregivers experience health challenges related to their caregiving role, and self-efficacy can contribute to health outcomes through behavioral, environmental, and personal factors. The purpose of this integrative review was to examine self-efficacy in caregivers of adults diagnosed with cancer, including its association with health factors.
Method:
A systematic search of PubMed, CINAHL, and PsychInfo yielded 560 articles. Following duplicate removal, 232 articles were screened for inclusion criteria with 71 articles remaining for final review.
Results:
Studies were generally quantitative (n=67), with predominantly female (n=55) non-Hispanic White (n=36) caregivers between the ages of 45-60 (n=48). Self-efficacy was significantly associated with quality of life, caregiver function, social support, hope, depression, anxiety, and burden as a predictor, mediator, and outcome. Physical health and social determinants of health (social support and financial well-being) were addressed among fewer studies than mental and emotional health outcomes.
Conclusions:
Addressing self-efficacy in diverse populations and physical, mental, social health contexts will enhance understanding of how self-efficacy impacts caregivers of adults diagnosed with cancer. Nurses and other health care professionals can then more effectively address supportive needs of caregivers in the personal, behavioral, and environmental domains.
Keywords: cancer, caregiver, caregiving, self-efficacy, health outcomes, social determinants of health, integrative review
Introduction
Cancer burden will continue to grow globally with a projected 27.5 million new cancer cases in 2040, although global cancer caregiver numbers are less well understood (American Cancer Society, 2018). Informal caregivers, herein referred to as family caregivers, are foundational to health care delivery (National Cancer Institute, 2019), with caregivers described as the hidden patient (Roche, 2009). Family caregivers of individuals diagnosed with cancer may provide physical, mental, emotional, spiritual, and financial support, and they may be asked to provide care for which they feel unprepared to deliver (National Cancer Institute, 2019). Caregivers may also suffer consequences from their caregiving role including unintentional weight changes, sleep deprivation, depressive symptoms, anxiety, social isolation, and an increased risk of mortality (Adelman et al., 2014, Perkins et al., 2013).
Cancer caregiving has unique challenges related to the disease course and patient supportive needs. Caregivers are often tasked with managing complicated medication regimens, assessing for signs of cancer recurrence or medication toxicity, addressing symptoms related to cancer and its treatment, and navigating complex and costly testing and treatments, all while still caring for themselves and maintaining personal and professional responsibilities (National Cancer Institute, 2019). Similar to the broader caregiving population, caregivers for individuals with cancer are generally women and most often family members (National Alliance for Caregiving, 2016, 2020). Many are still working part- or full-time, and may have existing health issues of their own. Finally, the care they provide is intensive and complex, yet their role in the care team and their own health and personal needs often go unacknowledged (Dębska et al., 2017; NAC, 2016, 2020). This is in direct conflict with the tenets of palliative care, which emphasize the fundamental role of family caregivers in serious and life-limiting illness (National Concensus Project, 2018)
Self-efficacy has been described in health care research as a factor contributing to health outcomes (Bandura, 1977). This has been posited to occur through the stress response and behavior change, both of which are relevant to caregiving in cancer (O’Leary, 1992). Goren and colleagues (2014) reported health impairments experienced by caregivers of individuals with cancer including stress-related illnesses, work challenges, increased healthcare utilization, and poorer health-related quality of life. Researchers have described the interdependence of individuals with cancer and their caregivers, with partner effects related to psychological and physical distress in one individual affecting the distress and quality of life in the other (Segrin et al., 2018, Segrin et al., 2020). With the effects of self-efficacy on stress and well-being and the partner effects between caregivers and individuals with cancer for well-being, self-efficacy is a relevant factor to understand in these caregivers (O’Leary, 1992). In addition to these known effects, the social context and environment are fundamental to self-efficacy and health outcomes in caregivers (Bandura, 1998, Burke et al., 2009). Therefore, the purpose of this integrative review is to present the state of the science on the concept of self-efficacy in caregivers of adults with cancer by both understanding how self-efficacy is being measured, tested, and described in the literature and addressing its association with health factors in the behavioral, personal, and environmental domains.
Theoretical Framework: Self-Efficacy
Self-efficacy, the belief in one’s ability to achieve a desired outcome, is a fundamental factor in behavior and behavioral change (Bandura, 1977). With this theoretical perspective, individuals are self-agents whose behaviors are impacted by both internal and external processes. Self-efficacy is influenced by mastery and vicarious experiences, physiologic states, and verbal persuasion (Bandura, 2001). It is grounded in the context of social cognitive theory, where environmental, behavioral, and personal factors reciprocally interact to impact behavior (Bandura, 1977). Bandura (2006) described the importance of assessing self-efficacy within specific domains rather than the global level, because individuals can vary in their self-efficacy based on circumstance and experience.
Self-efficacy affects human behavior through cognition, motivation, mental and emotional well-being, and goals and decisions (Bandura, 1994). In caregivers of adults with cancer, self-efficacy has the potential to influence caregivers’ perceptions and behaviors related to themselves as well as care recipients in areas such as self-care, symptom management, and navigation of the health care system (Bandura, 2006). Recognition of the role of caregivers in health care and life-limiting illness has been growing in the United States since 2001 with the publication of Crossing the Quality Chasm: A New Health System for the 21st Century (Institute of Medicine, 2001) and founding of the National Coalition for Hospice and Palliative Care (NCHPC, 2020). Additionally, Bandura (2001) acknowledged the impact of self-efficacy at the individual and social systems level during this same time, which is relevant to caregiving as an individual and family system experience.
Methods
Search Strategy
For this integrative review, a systematic approach was used to search and identify articles relevant to self-efficacy in caregivers of individuals diagnosed with cancer. In the month of October 2019, a literature search was conducted through PubMed using the following MeSH terms: Neoplasm AND Caregiver AND Self-Efficacy AND Health; Neoplasm AND Caregiver AND Self-Efficacy. Additional searches were conducted in CINAHL, and PsychInfo using the following combinations of search terms: Cancer Caregiver AND Self-Efficacy AND Well-Being; Cancer Caregiver AND Self-Efficacy. The search yielded a total of 560 articles (See Figure 1).
Figure 1:
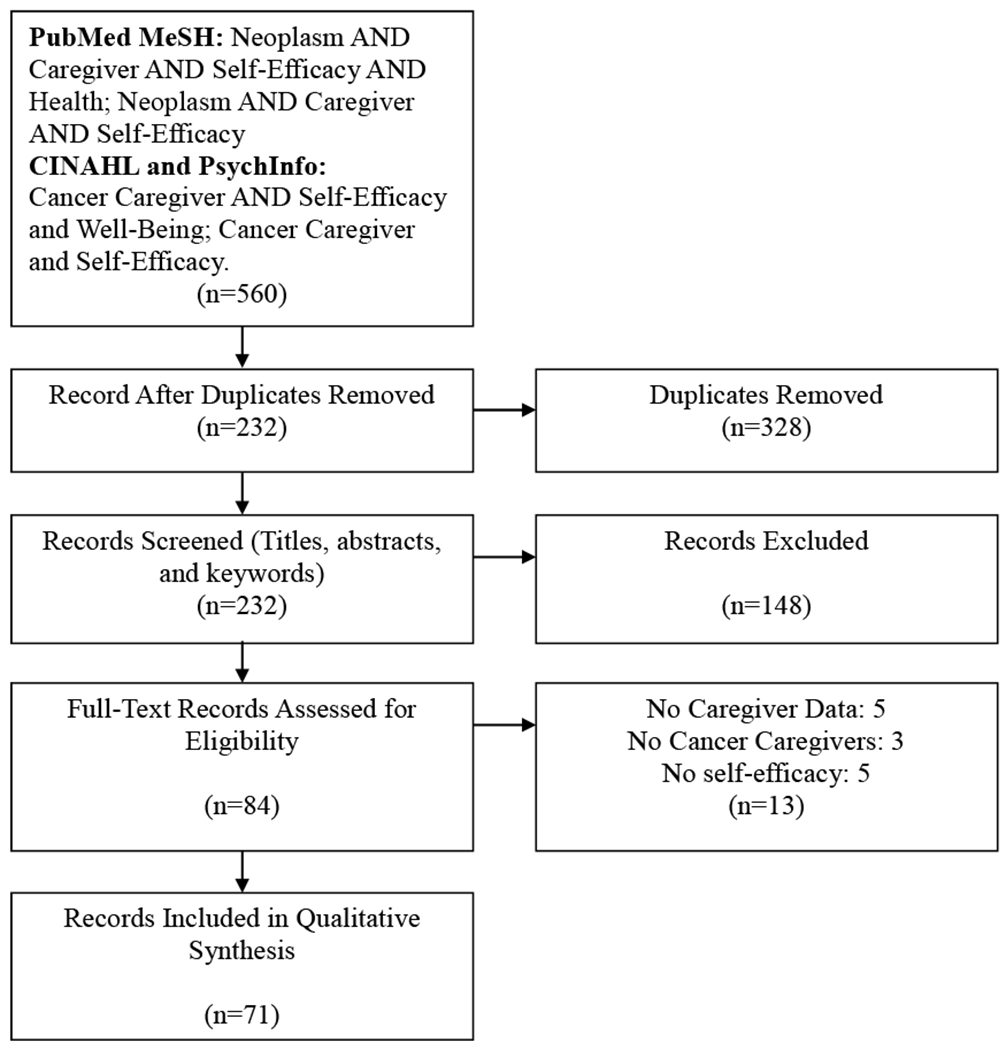
Modified PRISMA Diagram
Article Selection
After duplicates were removed, article titles, abstracts, and key words of 232 records were initially reviewed for relevance to this integrative review, then 84 full-text records were screened. This process was conducted with two authors using a worksheet with inclusion and exclusion criteria. Any disagreements between the authors were examined and discussed until full agreement was reached. Articles were included if they met the following criteria: caregivers of adults with a diagnosis of cancer as participants, assessment of self-efficacy, written in English, and published from January 1, 2001 to October 1, 2019. Articles were excluded if they did not have caregiver-specific data related to self-efficacy. Articles combining caregiver and care recipient findings, making caregiver findings indistinguishable, were excluded. Opinion pieces, non-systematic literature reviews, and research protocols were not included, although dissertations, systematic literature reviews, metasyntheses, and meta-analyses were included. Seventy-one articles remained after completion of the screening process. See Figure 1 for a modified PRISMA diagram of the article selection process.
Article Review
Data extraction focused on the types of studies, participant characteristics reported in the data-based manuscripts, representation of self-efficacy through measurement or themes, self-efficacy measurement differences based on cancer stage, application of concepts and theories, and associations of physical, mental, social, and emotional health outcomes with caregiver self-efficacy. Some studies included measurement of self-efficacy in both caregivers and individuals with cancer, but only the caregiver-related self-efficacy measurement and outcomes were addressed for this review (see Table 1 for detailed study information).
Results
Overall, more studies have been published between 2010 and 2019 (n= 54) that address self-efficacy in caregivers of individuals diagnosed with cancer than studies published between 2001 to 2009 (n=17). In this review, no qualitative studies addressing self-efficacy were published after 2010, and all review articles were published after 2010. The review articles will be discussed first, followed by the studies with primary research.
Review Studies
Two systematic reviews (Latter et al., 2016, Li and Loke, 2013), one metasynthesis (Duggleby et al., 2017b), and one metaanalysis (Northouse et al., 2010) were included in this review. Self-efficacy was described as a positive outcome in the Redefining Normal conceptual Framework outlined in the metasynthesis by Duggleby et al. (2017b), and this was influenced by coming to terms, connecting, and redefining normal. In two reviews and one meta-analysis, self-efficacy improved with pain management interventions (Latter et al., 2016), higher self-efficacy was associated with positive feelings about caregiving (Li and Loke, 2013) and eight interventions examined self-efficacy as an outcome with an overall effect size of g=0.25 and intervention effect persisting up to three to six months (Northouse et al., 2010).
Study Design and Participants in Primary Research
Study design among the 67 articles with primary research was mostly quantitative with 23 cross-sectional, 13 randomized controlled or randomized pilot trials 13 quasi-experimental studies, six longitudinal analyses, and nine secondary data analyses (see Table 1 for details). There were two studies using mixed-methods (Duggleby et al., 2015, Duggleby et al., 2013), and one grounded theory qualitative study (Kazanowski, 2005). Dyads were the participants in 38, caregivers alone were the participants in 23, caregivers and care recipients (not designated as dyads) were the participants in five (Barber, 2012, Barber, 2013, Morse, 2013, Mystakidou et al., 2013, Porter et al., 2011), and one study focused on the care recipient and up to three caregivers (Bevans et al., 2014) (see Table 1 for details).
Caregiver Characteristics in Primary Research
Among the 67 studies with primary research, most studies had larger proportions of caregivers who were female, White, and with a mean age or age range between 45–60. Six studies had primarily male or only male participants (Collinge et al., 2007, Dockham et al., 2016, Duggleby et al., 2014a, Duggleby et al., 2017a, Duggleby et al., 2015, Lewis et al., 2019). Five studies were focused on a care recipient of one gender, yet did not specifically describe caregiver gender (Badger et al., 2020, Campbell et al., 2004, Kershaw et al., 2008, Knoll et al., 2009, Northouse et al., 2002). One study was evenly split between male and female caregivers (Hendrix et al., 2016). The mean caregiver age ranged from 36-70 years among the studies, with most (n=48) studies reporting caregivers with mean ages or higher frequency ages between 45-60 years. Only five studies had participants’ mean or median age less than 45 years (Badger et al., 2020, Kizza and Maritz, 2019, Kizza and Muliira, 2019, Kizza and Muliira, 2020, Marshall et al., 2013). Finally, participants were predominantly spousal caregivers (≥50%) in 50 of 67 studies with primary research, and there were seven studies that did not describe caregiver relationships to care recipients (Bachner et al., 2014, Barber, 2013, Hudson et al., 2005, Morse, 2013, Oh, 2017, Titler et al., 2017, Yildiz et al., 2017). None of the studies specifically identified or focused on sexual and gender minority caregivers.
Thirty-six studies reported participants as primarily White caregivers (54%). DeSanto-Madeya and colleagues (DeSanto-Madeya et al., 2009) examined end-of-life treatment factors and acculturation with a split of White (47%) and Hispanic (43%) caregivers. Four studies focused on specific ethnic groups for the care recipient or caregivers: Latina breast cancer survivors (Badger et al., 2020), African-Americans with prostate cancer (Campbell et al., 2004), Hispanic caregivers (Marshall et al., 2013), and Ashkenazi and Sephardi Jews (Bachner et al., 2014) . In eleven of the 67 studies with primary research there was no description of caregiver race/ethnicity (Badr et al., 2015, Cameron et al., 2004, Duggleby et al., 2017a, Hudson et al., 2006, Johansen et al., 2017, Kazanowski, 2005, Knoll et al., 2009, Mori et al., 2013, Porter et al., 2012, Ugalde et al., 2013, Ugalde and Krishnasamy, 2014). Twenty-four data-based studies were conducted in countries outside of the United States including: Canada (Duggleby et al., 2014a, Duggleby et al., 2017a, Duggleby et al., 2015, Duggleby et al., 2013, Duggleby et al., 2014b), Australia (Hudson et al., 2005, Hudson et al., 2006, Hyde et al., 2017, Ugalde and Krishnasamy, 2014, Ugalde et al., 2013), Israel (Bachner and Carmel, 2009, Bachner et al., 2014), Taiwan (Lee et al., 2016, Lee et al., 2013, Lee et al., 2018), Japan (Ito and Tadaka, 2017), Greece (Mystakidou et al., 2013), Turkey (Yildiz et al., 2017), China (Li et al., 2015, Li et al., 2018), Singapore (Leow et al., 2015), and Uganda (Kizza and Maritz, 2019, Kizza and Muliira, 2019, Kizza and Muliira, 2020).
Self-Efficacy Representation by Measures and Description
Self-efficacy was represented in general and specific ways among the quantitative and qualitative articles (Tables 2 and 3). In a qualitative study, Kazanowski (2005) described caregiver expressions of self-efficacy in medication management, including feeling more confident with more nursing support, having a system for medications, and managing medications for longer periods of time. Caregivers measured their self-efficacy through patient comfort, symptom control, following instructions, and keeping the patient home as long as possible. Various measures were used among the 66 quantitative studies. There were three widely used and adapted measures, including the General Self-Efficacy Scale in 18 studies, the Lorig Self-Efficacy Scale in 11 studies, and the Lewis Cancer Self-Efficacy Scale in 10 studies. In 49 of 66 studies, the measures were situation specific (see Table 3 for more details).
Self-Efficacy in Advanced Cancer
Self-efficacy was addressed in 27 studies where the individual with cancer was diagnosed with advanced cancer or at the end-of-life. The emphases of these studies included family and patient-caregiver communication (Bachner & Carmel, 2009; Bachner et al., 2014), in-advance end-of-life discussions (Mori et al., 2013), and culture and end-of-life decision-making (DeSanto-Madeya et al., 2009). Other studies examined psychosocial functioning (Hudson et al., 2006), symptom distress and threat appraisals (Ellis et al., 2017), quality of life (Ito & Tadaka, 2017), personal and interpersonal effects of health and self-efficacy between caregivers and individuals with cancer (Kershaw et al., 2015), prevalence of anxiety and depression (Lee et al, 2013), symptom burden trajectories (Lee et al., 2018), and development of a self-efficacy measure and assessment of the measure in relationship to anxiety and distress (Ugalde et al., 2013, 2014). There were intervention studies examining the effect of psychosocial, integrative, hope-based, coping skills, problem-solving, or psychoeducational interventions (Badr et al., 2015; Cameron et al., 2004; Duggleby et al., 2013; Hudson et al., 2005; Lee et al., 2016; Leow et al., 2015; Mosher et al., 2018) and a cross-sectional survey to understand self-care practices of caregivers (Dionne-Odom et al., 2017). Both hope (Duggleby et al., 2014) and religious coping (Pearce et al., 2006) were examined in cross-sectional and longitudinal studies, respectively. Finally, medication management (Kazanowski, 2005) and pain management (Keefe et al., 2003, 2005) were addressed in advanced cancer and at the end-of-life.
There were 27 studies where the stage of cancer was unclear for the care recipient, eight where care recipients could have any stage of cancer, and nine where care recipients were not diagnosed with advanced cancer or at the end life. In those nine studies, there were similar trends to those studies in advanced cancer and end-of-life with self-efficacy examined in the context of psychosocial interventions (Badger et al., 2019; Duggleby et al., 2017), marital communication and interpersonal support intervention (Lewis et al., 2019), coping skills training (Porter et al., 2011), quality of life (Duggleby et al., 2014; Duggleby et al., 2015), and pain and symptom management (Porter et al., 2008). Uniquely, caregiver activation (Mazanec et al., 2016) and attachment styles (Porter et al., 2012) were examined in longitudinal and secondary analyses that were focused on earlier stage cancers, respectively. End-of-life decision making was not addressed in studies where care recipients did not have advanced cancer or were at the end-of-life, nor were any of these studies overtly focused on hope or caregiver burden.
Theory or Concepts
Self-efficacy was embedded directly or indirectly in the studies through theoretical or conceptual connections. As a primary concept, it was addressed by Campbell et al. (2004) in examining the relationship between patient and partner self-efficacy, symptom control, and quality of life. Havyer et al. (2017) and Hendrix et al. (2009, 2013, 2016) tested self-efficacy in the context of caregiver training in cross-sectional and interventional studies, respectively. Keefe et al. (2003) and Porter et al. (2008) studied caregiver self-efficacy in managing cancer pain and other symptoms at the end-of-life. An interventional study tested a culturally adapted intervention for caregivers and individuals with cancer with self-efficacy as the primary concept (Marshall et al., 2013). The relationship between anxiety and self-efficacy were addressed by Mystakidou et al. (2013) with self-efficacy as the main concept. In two studies, Ugalde et al. (2013, 2014) directly addressed self-efficacy in advanced cancer, while Yildiz et al. (2017) examined self-efficacy conceptually along with caregiver burden. Other studies examined self-efficacy indirectly in relation to concepts such as problem-solving, end-of-life decision-making, culture, communication, quality of life, social support, psychological functioning and distress, hope, transitions, threat appraisals, caregiver burden, pain and symptom management, caregiving training, activation, benefit finding and positive aspects of caregiving, living with love, attachment and meaning in life.
Theoretically, self-efficacy was examined directly as Self-Efficacy Theory in Morse (2014), where the goal was to understand group support topics endorsed by caregivers and individuals living with cancer. Self-efficacy was addressed under the umbrella of Social Cognitive Theory in the context of physical activity and (Barber, 2012), a symptom management intervention (Mosher et al., 2016), and individual and interpersonal influences on health and self-efficacy for caregivers and individuals living with cancer. Self-efficacy was described in connection to other theories including Self-Determination Theory (Badr et al., 2015), Stress-Coping Theory or Stress Appraisal Model (Cameron et al., 2004; Dockham et al., 2016; Hudson et al., 2005; Kershaw et al., 2008; Northouse et al., 2002, 2014; Oh, 2017; Pearce et al., 2006), Pender’s Health Promotion Model, Riegel’s Middle-Range Theory of Self-Care in of Chronic Illness (Dionne-Odom et al., 2017), and Transitions Theory (Duggleby et al., 2017). Tate (2018) discussed the intersection of Stress-Coping Theory, the Pearlin Caregiving Model and Self-Efficacy Theory in examining caregiving strain.
Association of Self-Efficacy with Health Outcomes in Quantitative Studies
Self-efficacy as a predictor.
Self-efficacy was examined as a primary predictor, mediator, primary and secondary outcome variable, and a variable in a non-directional correlational relationship (see Table 4 for details). As a primary predictor it was a significant predictor of psychosocial phenomena such as open communication at the end of life (Bachner and Carmel, 2009, Bachner et al., 2014), mental and emotional health (Campbell et al., 2004, Kershaw et al., 2015, Kim et al., 2005, Lee et al., 2013, Mystakidou et al., 2013, Porter et al., 2008, Posluszny et al., 2019), and hope (Duggleby et al., 2013, Duggleby et al., 2014b). Outcome variables related to caregiver perceptions that were influenced by self-efficacy included threat appraisals (Ellis et al., 2017), caregiver burden (Hu et al., 2018, Kizza and Muliira, 2020, Lee et al., 2018), strain (Tate, 2018), uncertainty (Kershaw et al., 2008), benefit finding (Li et al., 2018), and appraisals of caregiving (Northouse et al., 2002). Caregiver outcomes such as quality of life (Campbell et al., 2004, Duggleby et al., 2014a, Ito and Tadaka, 2017, Northouse et al., 2002), higher caregiver functioning (Hudson et al., 2006), coping (Kershaw et al., 2008), physical health (Kershaw et al., 2015) , and adaptation (Kizza and Muliira, 2020) were significantly positively associated with caregiver self-efficacy. Environmental issues impacting the caregiving experience such as social support (Kim et al., 2005, Kizza and Muliira, 2020) and financial well-being (Kizza and Muliira, 2020) were also significant outcomes related to self-efficacy. Conversely, a few studies noted no relationship between self-efficacy and caregiver outcomes including quality of life (Duggleby et al., 2015, Duggleby et al., 2017a), caregiver burden (Johansen et al., 2017), or caregiver activation (Mazanec et al., 2015).
Self-efficacy as a primary intervention outcome.
Self-efficacy was a primary outcome in multiple intervention and observational studies (see Table 4). Self-efficacy improved significantly in interventions focused on problem-solving (Bevans et al., 2014), therapeutic massage (Collinge et al., 2007), hope in rural female caregivers (Duggleby et al., 2013), enhanced experiential caregiver training before hospital discharge and during in-home care (Hendrix et al., 2009, Hendrix et al., 2016, Hendrix et al., 2013), home education program (Kizza and Muliira, 2019), marital communication (Lewis et al., 2019), and psychoeducation with simulation (Mazanec et al., 2019). Self-efficacy did not improve significantly in three studies focused on informational (Cameron et al., 2004), or psychoeducational interventions (Hudson et al., 2005, Leow et al., 2015).
Self-efficacy as a primary observational outcome.
In the observational studies, self-efficacy as an outcome was influenced significantly by health responsibility and stress management (Dionne-Odom et al., 2017), caregiver training, end-of-life discussions, and communication with health professionals (Havyer et al., 2017, Mori et al., 2013, Oh, 2017), and caregiver, patient, and family distress (Ellis et al., 2017). In one study, perceived impact of caregiving role on physical well-being, hours of caregiving, presence of a chronic illness, and receiving organizational support were significant factors related to caregiver self-efficacy for pain management in regression analysis (Kizza and Maritz, 2019).
Self-efficacy as a secondary intervention outcome.
As a secondary outcome, self-efficacy was primarily examined in intervention studies. In an intervention study comparing supportive health education versus telephone interpersonal counseling (TIP-C) in caregivers and Latinas with breast cancer, self-efficacy for symptom management was higher at follow-up for the TIP-C intervention (Badger et al., 2020.) Other intervention studies with significant self-efficacy outcomes between groups or within groups included a psychosocial dyadic intervention (Badr et al., 2015), the FOCUS (family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management) psychoeducational program (Dockham et al., 2016, Northouse et al., 2014, Titler et al., 2017), partner-guided pain management (Keefe et al., 2005), integrative caregiver support (Lee et al., 2016), Caring for Couples Coping with Cancer (Li et al., 2015), Un Abrazo Para la Familia (A Hug for the Family—use of skills training and promotoras) (Marshall et al., 2013), and a peer-helping and coping skills program (Mosher et al., 2018). In one study focused on caregiver-assisted coping skills, caregiver self-efficacy significantly improved over time for treatment and control groups, but there were no significant differences between treatment and control groups immediately following the coping skills intervention (Porter et al., 2011). Self-efficacy for managing one’s own emotions increased significantly over time in a telephone intervention study, but there was no time by group effect for self-efficacy on managing patient’s symptoms (Mosher et al., 2016).
Self-efficacy as a secondary observational outcome.
Three studies examined self-efficacy as a secondary observational outcome with non-significant changes in self-efficacy. Porter and colleagues (2012) found that caregiver self-efficacy was not a significant factor for dyad attachment, there was no change over time in self-efficacy for caregivers of colorectal cancer patients (Mazanec et al., 2015), and a study comparing self-efficacy in individuals with cancer versus caregivers showed higher levels in individuals with cancer (Morse, 2013).
Self-efficacy as a mediator variable.
Self-efficacy was examined as a mediator variable in three studies. Caregiver symptom distress had an indirect effect on caregiver threat appraisals through individual self-efficacy (Ellis et al., 2017). Self-efficacy mediated the relationship between negative religious coping and quality of life and satisfaction (Pearce et al., 2006). Self-efficacy was a partial mediator between communication with health professionals and psychological distress and a full mediator between trust in health professionals and psychological distress (Oh, 2017).
Self-efficacy in non-directional correlations.
Significant non-directional correlational relationships were reported in sixteen studies. In a study examining a physical activity intervention, self-efficacy sticking to it and self-efficacy making time for physical activity had a significant positive association (Barber, 2012, Barber, 2013). Other studies noted significant inverse relationships between self-efficacy and acculturation (DeSanto-Madeya et al., 2009), caregiver burden and strain (Keefe et al., 2003, Yildiz et al., 2017), and anxiety and depression (Lee et al., 2013, Mystakidou et al., 2013, Perz et al., 2011, Ugalde and Krishnasamy, 2014). Positive correlations between self-efficacy and other variables among the studies included quality of life and well-being (Ito and Tadaka, 2017, Keefe et al., 2003) and religious coping (Pearce et al., 2006), among others. Interestingly, lower caregiver self-efficacy was significantly related to younger age and patient chemotherapy and radiation treatment in one study (Porter et al., 2008), and baseline caregiver self-efficacy was associated with longitudinal self-efficacy in another study (Kershaw et al., 2015). In contrast, Knoll and colleagues (2009) found that caregiver self-efficacy was not related to long-term patient mobilized support.
Discussion
This integrative review provides a holistic overview of self-efficacy and its role use in research examining caregivers of individuals with cancer, a gap in current caregiver literature. Several patterns emerged in this integrative review including primarily quantitative studies addressing the construct of self-efficacy, caregiver homogeneity in the self-efficacy literature, emotional and mental health outcomes, lack of inclusion of environmental factors, and measurement of self-efficacy which can guide future self-efficacy research. First, the number of qualitative studies was limited in this review to one grounded theory study (Kazanowski, 2005). The mixed-methods studies in this review did not highlight issues related to self-efficacy within the qualitative thematic analyses (Duggleby et al., 2015, Duggleby et al., 2013). Second, over one-third of the studies in this review were interventional in nature, which is an important step in the research process, but may be premature if self-efficacy in cancer caregiving is not fully understood. Third, findings from this review suggest that self-efficacy is most often studied as a predictor for mental and emotional health outcomes and the most frequently identified significant relationships included anxiety, depression, caregiver burden, and quality of life. Thus far, theoretically, self-efficacy was supported directly through Self-Efficacy Theory or Social Cognitive Theory in four studies, while the remaining studies addressed it conceptually or indirectly through other theoretical frameworks or models (Kershaw et al., 2015; Morse, 2013; Mosher et al., 2016; Tate, 2018).
Caregiver characteristics were relatively homogeneous among the studies. Only three studies focused specifically on racial/ethnic minority groups in the United States (Badger et al., 2020, Campbell et al., 2004, Marshall et al., 2013), while over one-third were focused on populations outside of the United States. In addition, there were no studies specifically addressing sexual and gender minorities. Finally, only six studies specifically addressed male caregivers or had predominantly male participants (Collinge et al., 2007; Dockham et al., 2016; Duggleby et al., 2014; Duggleby et al., 2017; Duggleby et al., 2015; Lewis et al., 2019). Overall, there continues to be a greater proportion of female caregivers of individuals with cancer (NAC, 2016) in the United States, but this distribution is shifting with the Millennial generation (Flinn, 2018, AARP, 2020).
Additionally, self-efficacy was an outcome for observational and interventional studies that focused primarily on communication with family or providers, caregiver support, and educational training. These findings are consistent with the factors that influence self-efficacy such as verbal persuasion and mastery experiences (Bandura, 1994). Over half of the studies (n=38) included in this analysis focused on dyads. The emphasis of this analysis was specific to caregiver outcomes, therefore a full picture of self-efficacy within the dyads was beyond the scope of this article.
Twenty-one instruments were used to measure self-efficacy among the studies. Most researchers aligned with Bandura’s (2006) recommendation for situation specific self-efficacy measures, while 18 studies used the General Self-Efficacy Scale. With the push for standardized patient reported outcomes measurement, there is a tension between Bandura’s recommendation (2006) for situation specific self-efficacy measurement and standardization with rigorous testing to promote consistency in measurement (National Institutes of Health, 2020).
Implications for Research and Practice
Self-efficacy continues to be an important facet of behavioral and cancer caregiving research, with over fifty of the articles in this review being published in the last ten years. Future research on self-efficacy in caregivers of individuals with cancer should be conducted with both attention to accurate and standardized measurement of self-efficacy and Bandura’s (2006) recommendation for situation specificity. In addition to refinement of quantitative approaches in future research, qualitative research is needed with its value in highlighting the multiple realities and experiences of caregivers of adults with cancer (Rahman, 2016).
Self-regulatory mechanisms, such as self-efficacy, have little benefit if the environment perpetuates poor health (Young et al., 2020, Bandura, 1998). Issues such as healthcare provider bias, service accessibility, and structural racism embedded in health policy and the built environment may all influence caregiver self-efficacy. Future research should also address the potentially different self-efficacy needs and experiences of female versus male caregivers due to generational and social differences (Pajares, 2002), so interventions can be appropriately tailored. In addition, cultural experiences and service delivery in different countries or regions of countries may inform mastery and vicarious experiences and verbal persuasion. Thus, it is important that a diverse pool of caregivers of individuals with cancer are represented in the literature when addressing self-efficacy (Bandura, 2001).
Future cancer caregiving research should also examine other aspects of self-efficacy reinforcement including vicarious experiences through peer support groups and networks (Friedman et al., 2018), physiologic states through mindfulness or mind-body interventions (Oken et al., 2010), and social policy and systems that affect social capital, the built environment, and health care affordability and access (Bandura, 1998, Burke et al., 2009). Based on the potential for changes in behavior with self-efficacy (Bandura, 1994), there may be a greater role for self-efficacy and physical health outcomes including ratings of physical health or physical health behaviors such as exercise in caregivers of adults with cancer (Pekmezi et al., 2009). There is also a vital connection between self-efficacy and social capital and social systems that serve to support health (Bandura, 1998, Burke et al., 2009).
There are known reciprocal effects of physical and mental distress between caregivers and adults diagnosed with cancer (Segrin and Badger, 2014, Segrin et al., 2018, Segrin et al., 2020), illustrating the importance of addressing the caregiver and care recipient as a family unit (National Consensus Project, 2018). This is an opportunity for further evaluation of self-efficacy in dyadic studies, consistent with Bandura’s assertion of collective self-efficacy (Bandura, 2001).
In sum, ensuring theoretical connections between study design and measurement of self-efficacy will contribute to a more comprehensive understanding of this concept in cancer caregiving. Results from this review indicate important additional factors to include in research, and suggest the need for refining various middle range theories, rather than one comprehensive and complex theory, to guide future caregiver self-efficacy research. In Bandura’s theory, mastery and vicarious experiences, verbal persuasion, and physiological states all influence self-efficacy, while self-efficacy itself can affect cognition, motivation, emotional well-being, and decision-making (Bandura, 1994).
Nurses are key communicators and educators for individuals with cancer and their caregivers. There is a need for understanding the importance of education, practice with caregiving tasks, encouragement, and additional support for caregivers. Future research in areas identified through this review will help refine the theoretical foundations for guiding development of interventions that support nurses’ efforts to enhance self-efficacy in cancer caregiving.
Limitations
This review has several limitations that should be considered before applying findings broadly to caregivers of adults with cancer. First, articles were excluded if they were not written in English. This could potentially exclude more diverse populations that would add insight to self-efficacy and cancer caregiving. Given that self-efficacy is grounded contextually in experience and behavior, further exploration of self-efficacy among diverse groups is needed. Second, findings from this review cannot be generalized beyond caregivers of adults diagnosed with cancer, although many articles in this review were dyadic studies. Future reviews should include self-efficacy in cancer caregiving dyads to provide a family systems perspective.
Conclusion
Caregivers of individuals diagnosed with cancer are vital team members, and they are vulnerable to adverse outcomes related to their caregiving responsibilities. Self-efficacy is a construct that readily applies to these caregivers due to the experiences and stress-related processes that contribute to emotional, mental, social, and physical outcomes affected by self-efficacy. Nurses and other health professionals can support self-efficacy in caregivers through educational, behavioral, and psychosocial interventions that address mastery, verbal persuasion, vicarious experiences, and physiologic states. Additionally, nurses can advocate for policies that address environmental factors affecting self-efficacy and health, such as social determinants of health. Through an understanding of the current state of research related to self-efficacy in caregivers of adults diagnosed with cancer, future research can intentionally target areas of need such as qualitative studies, more diverse representation of caregivers, social and environmental health factors, and examination of self-efficacy in physical health.
Supplementary Material
Highlights.
Cancer caregivers provide complex care and are at risk for poor health.
Self-efficacy may influence cancer caregiver well-being.
Cancer caregiver self-efficacy and physical/environmental health are understudied.
Cancer caregiver self-efficacy improved with interventions for education, training, and support.
More research is needed to examine self-efficacy and cancer caregiver intersectionality.
Acknowledgements:
Funding:
Dr. Hebdon is supported by the National Institute of Nursing Research (T32NR013456)
Appendix A: Tables
Table 1:
Study Characteristics
| Author | Purpose/Caregiver Characteristics | Study Type/Participants | Theory/Concept | Caregiver of Individual at End-of-Life or with Advanced Cancer |
|---|---|---|---|---|
| Bachner & Carmel, 2009 | Examine open communication about end-of-life and caregiver/situational variables related to open communication; participants from south and Central Israel, mean age 55, 77% female, 48% child and 45% spouse/partner | Cross-sectional; Descriptive, correlational Caregivers | Concept: Family communication | Yes, individuals with terminal cancer |
| Bachner, Yosef-Sela, & Carmel, 2014 | Compare level of open communication between Ashkenazi and Sephardi Jews and examine caregiver/situational variables affecting open communication; Ashkenazi (36) and Sephardi (41); mean age 70.35; 62.3% female | Cross-sectional; Descriptive, correlational Caregivers | Concept: Caregiver-patient communication | Yes, individuals with terminal cancer |
| Badger et al., 2020 | Test two 2-month psychosocial interventions for Latinas with breast cancer and informal caregivers; caregivers of Latina breast cancer survivors, mean age (44), spouses (30%), child (30%) | RCT Dyads | Concept: Quality of life | No, individual in active treatment or completed treatment within 1 year |
| Badr, Smith, Goldstein, Gomez, & Redd, 2015 | Examine feasibility, acceptability, and preliminary efficacy of psychosocial intervention in lung cancer dyads; Mostly female (69%); mean age 51, 51% spouse/partner | Randomized Pilot Trial Dyads | Theory: Self-Determination Theory | Yes, individuals with advanced cancer |
| Barber, 2013 | Explore relationships between social support, self-efficacy for physical activity, physical activity behavior, and quality of life in survivors and caregivers; Mean age 65, mostly female (74%), mostly white (83%) | Quasiexperimental, mixed methods Cancer survivors and caregivers | Concept: Social Support | Mixed, individuals with cancer stage I-IV |
| Barber, 2012 | Explore differences and relationships between survivor and caregiver social support, self-efficacy for physical activity, physical activity, and quality of life; Mean age 62, 74% female, 77% white, 54% spouse | Quasiexperimental, mixed methods (Dissertation) Cancer survivors and caregivers | Theory: Social Cognitive Theory | Mixed, individuals with cancer stage I-IV |
| Bevans et al., 2014 | Determine effect of problem-solving education on self-efficacy and distress; 72% female, 78% white, mean age of 53, 47% spouse, 44% family member nonspouse | Quasiexperimental: Longitudinal, repeated measures design Care recipient and caregiver teams | Concept: Problem-solving | Unclear, individuals receiving stem-cell transplant, but prognosis not specified |
| Cameron, Shin, Williams, & Stewart, 2004 | Evaluate a brief problem-solving intervention for family caregivers; 68% female, mean age 54, 74% spouse | Quasiexperimental: one-sample pretest/post-test Dyads | Theory: Stress Appraisal and Coping theory | Yes, individuals with advanced cancer |
| Campbell et al., 2004 | Examine relationship between patient and partner ratings of self-efficacy, symptom control and quality of life; mean age 58, all spouse/partner, all partners to African American with prostate cancer, but no caregiver race included | Cross-sectional, comparison study Dyads | Concept: Self-efficacy | Unclear, individuals with prostate cancer who have completed treatment |
| Collinge, Kahn, Yarnold, Bauer-Wu, & McCorkle, 2007 | Examine feasibility of brief massage instruction and touch therapy for caregivers; mean age 53, 66% male, 86% white, all spouse/partner | Quasiexperimental: feasibility, longitudinal within-subjects, repeated measures, control and intervention phases Dyads | Concept: Distress | Unclear, individuals receiving or had received conventional cancer treatment |
| DeSanto-Madeya et al., 2009 | To examine how EOL treatment factors and psychosocial factors differ based on acculturation; 74% female, 47% white and Hispanic 43%, mean age 50, 51% spouse | Cross-sectional Caregivers | Concept: Culture and End-of-Life Decision-Making | Yes, individuals at end-of-life |
| Dionne-Odom et al., 2017 | To explore differences in caregivers’ self-care practices associated with varying level of well-being, preparedness, and decision-making self-efficacy; average age 66 years, 73% female, 91% white, 60% spouse | Cross-sectional survey Caregivers | Theory: Pender’s Health Promotion Model and Riegel’s Middle-Range Theory of Self-Care of Chronic Illness | Yes, individuals with stage IV cancer |
| Dockham et al., 2016 | Examine effectiveness of FOCUS program on cancer survivor and caregiver outcomes; mean age 53, 65% male, 86% white, 92% spouse | Preintervention, postintervention feasibility study Dyads | Theory: Stress Coping Theory | Mixed, individuals with any stage of cancer |
| Duggleby et al., 2013 | Examine effects of Living with Hope on self-efficacy, loss and grief, hope, and quality of life in rural female caregivers; mean age 59 and 86% were spouses, 92% white | Mixed methods, time series design Caregivers | Concept: Hope | Yes, individuals with advanced cancer |
| Duggleby et al., 2014 | To determine factors influencing hope of rural female caregivers; mean age 59, 66% spouses, 83% white, all female | Cross-sectional correlational design Caregivers | Concept: Hope | Yes, individuals with advanced cancer |
| Duggleby et al., 2017 | To explore the transition experience of family caregivers, triggers for transitions, and develop a conceptual framework; mean age 59, 71% female, and 49% spouses | Metasynthesis Caregivers | Concept: Transitions | Yes, individuals with advanced cancer |
| Duggleby et al., 2015 | To describe types of transitions of male caregivers of women with breast cancer and examine factors related to their quality of life; 85% white, all male, all spouses, mean age 61 | Cross-sectional, mixed methods Dyads | Concept: Transitions | No, individuals with cancer stage I-III |
| Duggleby, Doell, Cooper, Thomas, & Ghosh, 2014 | To examine the relationship of quality of life of male spouses of partners with breast cancer; mean age 59, 84% white, all male, all spouse/partner | Cross-sectional correlational design Caregiver | Concept: Quality of life | No, individuals with breast cancer stages I-III |
| Duggleby et al., 2017 | To evaluate feasibility of a web-based psychosocial support intervention; all male, all spouse/partner, mean age 55, 90% male | RCT, mixed methods, concurrent feasibility Dyads | Theory: Transitions Theory | No, individuals with breast cancer stages I-III |
| Ellis et al., 2017 | Examine influence of patient and caregiver symptom distress on threat appraisals and self-efficacy; mean age 57, 57% female, 80% white, and 70% spouse | Secondary analysis of baseline data from RCT Dyads | Concepts: Threat appraisals and self-efficacy | Yes, individuals with advanced cancer |
| Havyer et al., 2017 | Examine relationship between training during routine cancer care and self-efficacy among caregivers of colorectal cancer patients; 90% female, 68% spouse/partner, mean age 61, 77% white | Cross-sectional Caregivers | Concept: Self-efficacy | Unclear, individuals diagnosed with colorectal cancer |
| Hendrix et al., 2016 | Examine effects of enhanced informal caregiver training in cancer symptom and caregiver stress management on caregivers; mean age 55, 77% white, 83% female, 67% spouse | 2-armed RCT Dyads | Concept: Self-efficacy | Unclear, individuals admitted to oncology unit for treatment or cancer-related complications |
| Hendrix, Abernethy, Sloane, Misuraca, & Moore, 2009 | Investigate if an individualized and experiential training can promote family caregiver self-efficacy in home care and symptom management; mean age of 62, 85% female, 85% white, and 65% spouse | Pilot study, quasi-experimental, one group repeated measures Caregivers | Concept: Self-efficacy | Unclear, no cancer stage indicated, individuals actively dying were excluded |
| Hendrix, Landerman, & Abernethy, 2013 | Investigate effects of individualized caregiver training program on self-efficacy in home care and symptom management; 50% female, mostly 46-54 years of age (41.7%-53.3%), mostly white (81.7%-86.7%), mostly spouses (70%-83%) | RCT Dyads | Concept: Self-efficacy | Unclear, individuals with hematological malignancy and admitted to hospital for cancer-related treatment or complications |
| Hu, Peng, Su, & Huang, 2018 | Investigate caregiver burden and factors relating to burden in Chinese caregivers of individuals with lung cancer; 58% female, less than or equal to 50 years of age (39%), Chinese caregivers, 60% spouse | Cross-sectional Dyads | Concept: Caregiver burden | Unclear, no cancer stage indicated for individuals |
| Hudson, Hayman-White, Aranda, & Kristjanson, 2006 | Determine if it is possible to predict psychosocial functioning of family caregivers; 66% female, mean age 60, 62% spouse | Secondary analysis of baseline data from RCT Caregivers | Concept: Caregiver psychosocial functioning | Yes, individuals with advanced cancer |
| Hudson, Aranda, & Hayman-White, 2005 | Evaluate psychoeducational program for family caregivers of patients dying at home; 65% female, mean age of 61, 74% Australian born | RCT Caregivers | Concept: Stress and Coping Framework | Yes, individuals with advanced cancer |
| Ito & Tadaka, 2017 | Identify factors associated with quality of life among family caregivers of patients with terminal cancer at home; mean age 64, 80% female, 54% spouse, Japanese | Epidemiological cross-sectional study Caregivers | Concept: Quality of life | Yes, individuals with terminal cancer |
| Johansen, Cvancarova, & Ruland, 2018 | Examine effect of cancer patients’ and caregiver symptoms and demographic characteristics on caregiver burden at initiation of patient radiation treatment; mean age 56, 81% spouse, 53% female | Cross-sectional Dyads | Concept: Caregiver burden | Unclear, individuals with recent diagnosis or new recurrence |
| Kazanowski, 2005 | Understand process of medication management in terminal patients from the perspective of caregivers; all female, mean age of 54, 70% spouse | Qualitative, grounded theory Caregivers | Concept: Symptom management | Yes, individuals at end-of-life |
| Keefe et al., 2003 | Examine self-efficacy of family caregivers in managing cancer patients’ pain at the end of life; 90% spouse/partner, mean age 58, 81% white, 67% female | Secondary analysis of baseline data from RCT Dyads | Concept: Self-efficacy | Yes, individuals who are hospice eligible |
| Keefe et al., 2005 | Test efficacy of partner-guided cancer pain management protocol for patients at the end of life; mean age 59, 62% female, 79% white and 20% African American, 76% spouses | RCT Dyads | Concept: Caregiver training | Yes, individuals at end-of-life |
| Kershaw et al., 2008 | Examine stress-coping model to assess whether baseline variables predict subsequent appraisal and how appraisal predicts coping and quality of life for prostate cancer patients and their spouses; all spouses, 86% white and 13% African American, mean age 59 | Secondary analysis from larger RCT Dyads | Theory: Stress-Coping Model | Mixed, individuals with all stages of prostate cancer |
| Kershaw et al., 2015 | Use SCT to investigate individual and interpersonal influences on patients’ and family caregivers’ mental health, physical health, and self-efficacy; mean age 57, 57% female, 83% white and 14% African American, 74% spouse | Longitudinal secondary analysis from RCT Dyads | Theory: Social-Cognitive Theory | Yes, individuals with advanced cancer |
| Kim, Duberstein, Sorensen, & Larson, 2005 | Identify personality correlates of depressive symptoms in spouses of people with lung cancer; 66% female, all spouses, mean age 63, 97% white | Cross-sectional Caregivers | Concepts: Personality, Social Support, and Burden | Unclear, individuals diagnosed with cancer in the past 5 years |
| Kizza & Maritz, 2019 | Assess caregivers’ knowledge and self-efficacy levels for pain management for advanced cancer patients while at home; mean age 36, 73% female, 20% spouse, 39% child, participants from Uganda | Descriptive, cross-sectional Dyads | Concept: Pain management | Unclear, no cancer stage indicated for individuals |
| Kizza & Muliira, 2018 | Evaluate the influence of a home education intervention on caregivers’ knowledge and self-efficacy for pain management in advanced cancer patients; 43% aged 18-30, 65% female, 39% child and 20% spouse, participants from Uganda | Quasiexperimental, single group pre/post-test design Dyads | Concept: Pain management | Unclear, no cancer stage indicated for individuals |
| Kizza & Muliira, 2019 | Explore the determinants of quality of life among caregivers of advanced cancer patients in Uganda; mean age 36, participants from Uganda, 73% female, 80% non-spouse | Cross-sectional Dyads | Concept: Auality of life | Unclear, no cancer stage indicated for individuals |
| Knoll, Scholz, Burkert, Roigas, & Gralla, 2009 | Investigate patient mobilized and received support as predictors of their own and spouses’ self-efficacy beliefs 1 year after prostatectomy; mean age 58, all spouse | Longitudinal Dyads | Concepts: Social support and self-efficacy | Unclear, no cancer stage indicated for individuals |
| Latter et al., 2016 | To identify and review studies of interventions to help carers manage medicines for pain in advanced cancer | Systematic Review Mixed | Concept: Pain management | Yes, individuals with advanced cancer |
| Lee et al., 2013 | Explore the prevalence of anxiety and depression in family caregivers of patients newly diagnosed with advanced lung cancer and identify factors related to caregiver anxiety and depression; 42% spouse, 67% female, mean age 47, participants from Taiwan | Cross-sectional Dyads | Concept: Psychological distress | Yes, individuals advanced cancer |
| Lee, Yiin, & Chao, 2016 | Test ability of an integrative intervention for caregivers of advanced cancer patients to lower caregiving burden at end-of-life; mean age 51 and 50, 64% and 62% female, 61% and 55% spouse, participants from Taiwan | Quasiexperimental, 2 group comparative repeated measures design Dyads | Concept: Caregiver burden | Yes, individuals with advanced cancer |
| Lee et al., 2018 | Identify changes of 5 domains of family caregiver burden, overall burden, and subtrajectories when caring for newly diagnosed advanced lung cancer patients and identify caregiver and patient-related factors associated with burden; mean age 48, 70% female, 50% spouse, participants from Taiwan | Longitudinal Dyads | Concept: Caregiver burden | Yes, individuals with advanced cancer |
| Leow, Chan, & Moon Fai, 2015 | Evaluate effectiveness of a psychoeducational intervention, Caring for the Caregiver; participants from Singapore; mean age 47, 68% female, 85% Chinese, 58% child, 25% spouse | Pilot RCT, two group pretest and repeated post-test Caregiver | Concept: Quality of life | Yes, individuals with advanced cancer |
| Lewis et al., 2019 | Test short-term efficacy of a brief marital communication and interpersonal support intervention for couples facing a recent diagnosis of breast cancer; 89% white, mean age of 55, all male, all spouse | RCT Dyads | Concept: Distress | No, individuals with stage 0-III breast cancer |
| Li et al., 2018 | Examine benefit finding relationship between cancer patients and family caregivers and investigate factors that modify these relationships; mean age 48, 53% female, 61% spouse, Chinese participants | Secondary analysis of large cross-sectional study Dyads | Concept: Benefit finding | Unclear, no cancer stage indicated for individuals |
| Li, Xu, Zhou, & Loke, 2015 | Examine acceptability, feasibility and preliminary effect of a Caring for Couples Coping with Cancer program; all Chinese, all spouse, mean age 57, 67% female | Quasiexperimental pre and post-intervention design Dyads | Concept: Live with Love Conceptual Framework | Unclear, no cancer stage indicated for individuals |
| Li & Loke, 2013 | Summarize and appraise positive aspects of spousal caregiving and identify directions for future research | Critical Review Mixed | Concept: Positive Aspects of Caregiving Framework (includes caregiver self-efficacy) | Unclear, no cancer stage indicated for individuals |
| Marshall et al., 2013 | Explore effectiveness of Un Abrazo Para La Familia in increasing cancer knowledge and self-efficacy in caregivers; 97% female, all Hispanic, median age 38, 18% child | Pre- and post-intervention quasiexperimental pilot study Caregivers | Concept: Self-efficacy | Unclear, no cancer stage indicated for individuals |
| Mazanec, Sattar, Delaney, & Daly, 2016 | Describe activation in patients with colorectal cancer and family caregivers and examine the relationship between patient and caregiver action, and determine factors related to activation; mean age 55, 71% spouse, 88% white, 79% female | Longitudinal, correlational design Dyads | Concept: Activation | No, individuals with Stage I-III cancer |
| Mazanec et al., 2019 | Evaluate feasibility, acceptability, safety and fidelity of a psychoeducational intervention to improve family caregiver technical and communication skills using simulations; mean age 58, 67% female, 83% white, 78% spouse | Pilot RCT Caregivers | Concepts: Communication skills and caregiver distress | Mixed, individuals with Stages II-IV cancer |
| Mori et al., 2013 | Examine whether in-advance end-of-life discussions and DNR status would affect quality of inpatient end-of-life care; 52% spouse, 76% female, no age listed | Post-mortality survey Dyads | Concept: End-of-life discussion | Yes, individuals with advanced cancer |
| Morse, 2013 | Investigate group support topics endorsed by people living with cancer and caregivers and whether satisfaction with groups can be predicted by cancer status and demographics; mean age 54, 77% females, 91% white | Cross-sectional (Dissertation) Caregivers and People Living with Cancer | Theory: Self-Efficacy Theory | Unclear, no cancer stage indicated for individuals |
| Mosher et al., 2018 | Examine whether a peer helping component to a coping sills intervention leads to improved meaning in life and peace for advanced gastrointestinal cancer patients and their caregivers; 68% and 64% female, mean age 52 and 55, 88% white for both, and 68% and 84 % spouse | RCT Dyads | Concept: Meaning in life | Yes, individuals with Stage IV cancer |
| Mosher et al., 2016 | Examine the preliminary efficacy of telephone-based symptom management for symptomatic lung cancer patients and their family caregivers; 73% female, mean age 56 and 57, 86% and 93% white, 63% and 62% spouse/partner | Randomized pilot trial Dyads | Theory: Social Cognitive Theory | Unclear, no cancer stage indicated for individuals |
| Mystakidou et al., 2013 | Examine relationship between caregivers’ anxiety supporting a patient with advanced cancer and self-efficacy and sociodemographic characteristics; 49% child and 29% spouse, 64% female, mean age 48, Greek study participants | Cross-sectional Caregiver and care recipient | Concept: Self-efficacy | Unclear, no cancer stage indicated for individuals but 65% with metastases |
| Northouse et al., 2002 | Assess patient and family member quality of life within month after cancer recurrence and effects of multiple factors on quality of life; mean age 52, 59% spouse, 73% white and 23% African American | Secondary analysis of baseline data from larger prospective intervention study Dyads | Theory: Stress-Appraisal Model | Unclear, individuals with recurrent breast cancer |
| Northouse et al., 2010 | Analyze types of interventions offered to family caregivers of cancer patients and determine effect on caregiver outcomes; 64% female, 84% white, mean age of 55, 84% spouse | Meta-analysis Mixed | Concept: Well-being | Unclear, no cancer stage indicated for individuals |
| Northouse et al., 2014 | Examine feasibility of translating the FOCUS program for patients and caregivers to a tailored, dyadic web-based intervention; mean age 51, 61% female, 92% white, 68% spouse | Phase 2 feasibility study Dyads | Theory: Stress-Coping Theory | Mixed, individuals with early or advanced |
| Oh, 2017 | Investigate relationship between communication with health professionals and psychological distress in family caregivers and the mediating effects of self-efficacy in this model; mean age 52, 63% female, 70% white, | Secondary analysis of a large national study Caregivers | Theory: Stress-Coping Theory | Unclear, no cancer stage indicated for individuals |
| Pearce, Singer, & Prigerson, 2006 | Investigate the association between religious coping, mental health and the caring experience, and potential explanatory mechanisms in caregivers of terminally ill cancer patients; mean age 51, 74% white, 61% spouse, 73% female | Secondary analysis of a larger, longitudinal study Dyads | Theory: Stress-Coping Theory | Yes, individuals with advanced cancer |
| Perz, Ussher, Butow, & Wain, 2011 | Examine mediating roles of burden, unmet needs, self-silencing, self-efficacy and optimism and moderating influence of social support, cancer stage, patient gender, time spent caring and other responsibilities on gender differences in caregiver distress; 67% female, mean age 54 for women and 57 for men, 81% white for women and 83% white for men, 65% spouse for women and 91% spouse for men | Secondary analysis from larger mixed-methods study Caregivers | Concept: Distress | Mixed, individuals with different stages of cancer |
| Porter et al., 2012 | Examine attachment styles in patients with lung cancer and their spouses and associations between attachment styles and patient/spouse adjustment; all spouse, 62% female, mean age 63 | Secondary analysis from larger treatment outcome study Dyads | Concept: Attachment | No, individuals with early stage cancer |
| Porter et al., 2011 | Test efficacy of caregiver-assisted coping skills training protocol in patients with lung cancer; mean age 59, 92% white, 76% spouse, 69% female | RCT Lung cancer patients and caregivers (caregivers secondary participant) | Concept: Coping skills training | No, individuals diagnosed with early stage cancer |
| Porter, Keefe, Garst, McBride, & Baucom, 2008 | Examine self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their caregivers and associations between self-efficacy and patient and caregiver adjustment; Mean age 60, 66% female, 86% white, 76% spouse | Cross-sectional Dyads | Concept: Self-efficacy | No, individuals diagnosed with early stage cancer |
| Posluszny, Bovbjerg, Syrjala, Agha, & Dew, 2019 | Identify clinical, psychosocial, and sociodemographic factors related to pre-transplant distress; Mean age 53, 71% female, 95% European American, 77% spouse | Cross-sectional Dyads | Concepts: Anxiety and depression | Unclear, individuals involved in curative treatment for hematological malignancy |
| Tate, 2018 | Examine role of self-efficacy and coping skills in caregiver strain; mostly 45-54 years of age (31%), 40% spouse, 88% female, 88% white | Cross-sectional (Dissertation) Caregivers | Theory: Stress-Coping Theory and Pearlin Caregiving Model, Self-Efficacy Theory | Unclear, no cancer stage indicated for individuals |
| Titler et al., 2017 | Examine effectiveness, feasibility, and satisfaction with FOCUS program; mean age 56, 78% white, 56% female | Pre- and post-intervention design Dyads | Concepts: Distress and quality of life | Mixed, individuals with different stages of cancer |
| Ugalde, Krishnasamy, & Schofield, 2013 | To develop a new self-efficacy measure in caregivers of people with advanced cancer; 70% female, mean age 55, 75% spouse/partner | Measure development—pilot and field testing Caregivers | Concept: Self-efficacy | Yes, individuals with advanced cancer |
| Ugalde, Krishnasamy, & Schofield, 2014 | Describe prevalence of anxiety and distress in caregivers and explore relationships with self-efficacy; mean age of 55, 70% female; 75% spouse/partner | Cross-sectional study Caregivers | Concepts: Self-efficacy and distress | Yes, individuals with advanced cancer |
| Yildiz, Karakaş, Güngörmüş, & Cengiz, 2017 | Determine levels of self-efficacy and caregiver burden for cancer caregivers; Turkish caregivers, 38% between ages 24-34, 70% female, 52% parent (caregiver is the child) | Descriptive Study Caregivers | Concepts: Self-efficacy and burden | Unclear, No cancer stage indicated for individuals |
Table 2:
Self-Efficacy Description in Qualitative and Review Articles
| Author | Study Type | Self-Efficacy Description |
|---|---|---|
| Duggleby et al., 2017 | Metasynthesis | Self-efficacy was a positive outcome in the Redefining Normal Conceptual Framework that was affected by coming to terms, connecting, and redefining normal. |
| Kazanowski, 2005 | Grounded Theory Qualitative | In taking on the role of medication management, caregivers described feelings of uncertainty and greater confidence with ongoing nurse assessments and having a system to manage medications After death, caregivers reflected on self-efficacy through patient comfort, symptom control, following nurse’s instructions, and keeping the patient home as long as possible. Caregivers had more self-efficacy if they managed medications longer |
| Latter et al., 2016 | Systematic Review | Two studies with significant improvement in self-efficacy outcomes with pain management interventions. |
| Li & Loke, 2013 | Critical Review | High caregiver self-efficacy was associated with positive feelings about caregiving such as positive mood |
| Northouse et al., 2010 | Meta-Analysis | Eight studies evaluated the effect of interventions on self-efficacy, and the overall effect size was small but significant g=0.25 and they varied between −0.13 to 0.93. The positive significant effect persisted up to 3 to 6 months. |
Table 3:
Self-Efficacy Measurement in Quantitative Articles
Table 4:
Quantitative Study Outcomes
| Type of Variable | Outcomes |
|---|---|
| Primary Predictor |
Significant relationship with self-efficacy: Open communication (Bachner and Carmel, 2009, Bachner et al., 2014) Caregiver depression, anxiety, fatigue, and strain (Campbell et al., 2004, Tate, 2018, Posluszny et al., 2019, Kim et al., 2005, Mystakidou et al., 2013, Lee et al., 2013) Hope (Duggleby et al., 2013, Duggleby et al., 2014b) Quality of life (Duggleby et al., 2014a, Ito and Tadaka, 2017, Kizza and Muliira, 2020, Northouse et al., 2002) Threat appraisals (Ellis et al., 2017) Burden (Hu et al., 2018, Kim et al., 2005, Kizza and Muliira, 2020, Lee et al., 2018) Higher caregiver function (Hudson et al., 2006) Mood disturbance (Porter et al., 2008) Negative appraisal of caregiving (Kershaw et al., 2008, Northouse et al., 2002) Uncertainty (Kershaw et al., 2008) Avoidant coping (Kershaw et al., 2008) Present mental health and subsequent mental and physical health (Kershaw et al., 2015) Social support (Kim et al., 2005) Positive adaptation, financial concerns, and perceived support (Kizza and Muliira, 2020) Benefit (Li et al., 2018) Non-significant relationship with self-efficacy: Quality of life (Duggleby et al., 2015, Duggleby et al., 2017a) Burden (Hu et al., 2018, Johansen et al., 2017) Caregiver activation (Mazanec et al., 2015) |
| Primary Outcome |
Significant change in self-efficacy with intervention: Problem-solving intervention, and baseline SE predictive of post-intervention SE (Bevans et al., 2014) Partner massage training intervention, SE improved at 3 months (Collinge et al., 2007) SE scores higher at 7 days, 2 weeks, 3 months, 6 months and 12 months with Living With Hope intervention (Duggleby et al., 2013) Enhanced caregiver training had higher SE than those in education only group, differences not sustained at 2 and 4 weeks (Hendrix et al., 2016) After in-hospital training, SE levels increased immediately and 1 week after hospital discharge (Hendrix et al., 2009) SE increased after individualized caregiver training at 4 weeks post-discharge (Hendrix et al., 2013) SE improved in marital communication and support treatment group at 3, 6, and 9 months (Lewis et al., 2019) SE improved with simulation intervention for technical and communication skills (Mazanec et al., 2019) Non-significant change or no change in self-efficacy with intervention: Brief problem-solving intervention, no change post-intervention (Cameron et al., 2004) No difference after psychoeducational intervention for caregivers by time or group (Hudson et al., 2005) SE improved post- home education intervention (Kizza and Muliira, 2019) No difference in SE by time or group with psychoeducational intervention (Leow et al., 2015) Significant relationship with self-efficacy: Health responsibility and stress management (Dionne-Odom et al., 2017) caregiver, patient, and family distress (Ellis et al., 2017) Caregiver training (Havyer et al., 2017) Communication with health professionals, partially mediated by trust in health professionals (Oh, 2017) Impact of caregiving role on physical well-being, hours of caregiving, having a chronic illness, and receiving organizational support (Kizza and Maritz, 2019) Receipt of in-advance end-of-life discussions (Mori et al., 2013) Non-significant change in or relationship with self-efficacy: 1 year after patient prostatectomy (Knoll et al., 2009) |
| Secondary Outcome |
Significant change in self-efficacy with intervention: Higher in supportive health education versus telephone interpersonal counseling (Badger et al., 2020) Higher in psychosocial dyadic intervention group than usual care (Badr et al., 2015) Increased post-psychoeducational intervention for the dyad, greater effect size for dyad total versus caregiver alone (Dockham et al., 2016) Increased with FOCUS intervention (Titler et al., 2017, Northouse et al., 2014) Higher with partner-guided pain management intervention (Keefe et al., 2005) Significant by time and group with integrative caregiver support intervention (Lee et al., 2016) Greater for caregivers than patients following the Caring for Couples Coping with Cancer (Li et al., 2015) Increased after Un Abrazo Para la Familia (Marshall et al., 2013) Increase over time with telephone intervention group, small effect for SE managing emotions (Mosher et al., 2016) No significant change in self-efficacy with intervention: Improved with time for both groups, no differences between coping skills intervention group and control (Porter et al., 2011) Time by group effect for dyads self-efficacy following peer-helping intervention with peer helping, but not for caregivers alone (Mosher et al., 2018) Non-significant relationship with or change in self-efficacy: Dyad attachment (Porter et al., 2012) No change over time for caregivers of colorectal patients (Mazanec et al., 2015) People with cancer had higher levels than caregivers of people with cancer (Morse, 2013) |
| Mediator | Indirect effect of symptom distress on caregiver threat appraisals through individual self-efficacy (Ellis et al., 2017) Mediated the relationship between negative religious coping and quality of life and satisfaction (Pearce et al., 2006) Partial mediator between communication with health professionals and psychological distress and a full mediator between trust in health professionals and psychological distress (Oh, 2017) |
| Variable in simple correlation |
Significant relationship with self-efficacy: SE sticking to it and SE making time for physical activity (Barber, 2013, Barber, 2012) Acculturation (DeSanto-Madeya et al., 2009) Quality of life of female survivors with male partners’ self-efficacy (Duggleby et al., 2015) Caregiver burden (Yildiz et al., 2017, Kizza and Muliira, 2020) Anxiety (Ugalde and Krishnasamy, 2014, Perz et al., 2011, Lee et al., 2013, Mystakidou et al., 2013) Depression (Perz et al., 2011, Lee et al., 2013) Distress (Ugalde and Krishnasamy, 2014) Emotional support (Ito and Tadaka, 2017) Caregiver strain (Ito and Tadaka, 2017, Keefe et al., 2003) Caregiving appraisals (Ito and Tadaka, 2017) Acceptance (Ito and Tadaka, 2017) Quality of life (Ito and Tadaka, 2017) Younger age (Porter et al., 2008) Patient chemotherapy and radiation treatment (Porter et al., 2008) Religious coping (Pearce et al., 2006) Positive and negative mood (Keefe et al., 2003) Baseline and longitudinal SE (Kershaw et al., 2015) Support and disruptiveness (Kizza and Muliira, 2020) Non-significant relationship with self-efficacy: Long-term patient mobilized support (Knoll et al., 2009) |
all significant relationships in expected directions (ex: low self-efficacy, high depression), SE: self-efficacy
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
Conflict of Interest Statement
The authors declare no conflict of interest.
References
- American Cancer Society. 2018. Global Cancer Facts & Figures. 4th ed.Atlanta, GA: American Cancer Society. [Google Scholar]
- Adelman RD, Tmanova LL, Delgado D, Dion S, & Lachs MS 2014. Caregiver burden: a clinical review. JAMA, 311, 1052–1060. 10.1001/jama.2014.304 [DOI] [PubMed] [Google Scholar]
- Bachner YG & Carmel S 2009. Open communication between caregivers and terminally ill cancer patients: the role of caregivers’ characteristics and situational variables. Health Commun, 24, 524–531. 10.1080/10410230903104913 [DOI] [PubMed] [Google Scholar]
- Backner YG, Yosef-Sela N, & Carmel S 2014. Open communication with terminally ill cancer patients about illness and death: a comparison between spouses of Ashkenazi and Sephardi ethnic origins. Cancer Nurs, 37, 50–8. 10.1097/NCC.0b013e31827b5c7a [DOI] [PubMed] [Google Scholar]
- Badger TA, Segrin C, Sikorskii A, Pasvogel A, Weihs K, Lopez AM, & Chalasani P 2020. Randomized controlled trial of supportive care interventions to manage psychological distress and symptoms in Latinas with breast cancer and their informal caregivers. Psychol Health, 35, 87–106. 10.1080/08870446.2019.1626395 [DOI] [PubMed] [Google Scholar]
- Badr H, Smith CB, Goldstein NE, Gomez JE, & Reed WH 2015. Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer, 121, 150–158. 10.1002/cncr.29009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A 1977. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev, 84, 191–215. https://psycnet.apa.org/doi/10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Bandura A 1994. Self-efficacy. In: Ramachaudran VS (ed.) Encyclopedia of Human Behavior. New York, NY: Academic Press. [Google Scholar]
- Bandura A 1998. Health promotion from the perspective of social cognitive theory. PsycholHealth, 13, 623–649. 10.1080/08870449808407422 [DOI] [Google Scholar]
- Bandura A 2001. Social cognitive theory: an agentic perspective. Ann Review Psychol, 52, 1–26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- Bandura A 2006. Guide for constructing self-efficacy scales. In: Bandura A (ed.)Self-Efficacy Beliefes of Adolescents. Greenwich, Connecticut: Information Age Publishing. [Google Scholar]
- Barber FD 2012. Exploring the differences between adult cancer survivors and their caregivers’ social support, self-efficacy for physical activity, physicaly activity behavior, and qulaity of life. PhD, University of Texas at Tyler. [Google Scholar]
- Barber FD 2013. Effects of social support on physical activity, self-efficacy, and quality of life in adult cancer survivors and their caregivers. Oncol Nurs Forum, 40, 481–9. 10.1188/13.ONF.481-489. [DOI] [PubMed] [Google Scholar]
- Bevans M, Wehrlen L, Castro K, Prince P, Shelburne N, Soeken K, Zabora J & Wallen GR 2014. A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. J Health Psychol, 19, 602–17. 10.1177/1359105313475902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NJ, Bird JA, Clark MA, Rakowski W, Guerra C, Barker JC & Pasick RJ 2009. Social and cultural meanings of self-efficacy. Health Educ Behav, 36, 111S–28S. https://dx.doi.org/10.1177%2F1090198109338916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron JI, Shin JL, Williams D & Stewart DE 2004. A brief problem-solving intervention for family caregivers to individuals with advanced cancer. J Psychosom Res, 57, 137–143. 10.1016/S0022-3999(03)00609-3 [DOI] [PubMed] [Google Scholar]
- Campbell LC, Keefe FJ, Mckee DC, Edwards CL, Herman SH, Johnson LE, Colvin OM, Mcbride CM & Donattuci CF 2004. Prostate cancer in African Americans: relationship of patient and partner self-efficacy to quality of life. J Pain Symptom Manage, 28, 433–44. 10.1016/j.jpainsymman.2004.02.020 [DOI] [PubMed] [Google Scholar]
- Collinge W, Kahn J, Yarnold P, Bauer-Wu S & Mccorkle R 2007. Couples and cancer: feasibility of brief instruction in massage and touch therapy to build caregiver efficacy. J Soc Integr Oncol, 5, 147–54. 10.2310/7200.2007.013 [DOI] [PubMed] [Google Scholar]
- Debska G, Pasek M & Wojtyna E 2017. Does anybody support the supporters? social support in the cancer patient-caregiver dyad. Fam Med Prim Care Rev, 2, 110–113. 10.5114/fmpcr.2017.67863 [DOI] [Google Scholar]
- Desanto-Madeya S, Nilsson M, Loggers ET, Paulk E, Stieglitz H, Kupersztoch YM & Prigerson HG 2009. Associations between United States acculturation and the end-of-life experience of caregivers of patients with advanced cancer. J Palliat Med, 12, 1143–1149. 10.1089/jpm.2009.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionne-Odom JN, Demark-Wahnefried W, Taylor RA, Rocque GB, Azuero A, Acemgil A, Martin MY, Astin M, Ejem D, Kvale E, Heaton K, Pisu M, Partridge EE & Bakitas MA 2017. The self-care practices of family caregivers of persons with poor prognosis cancer: differences by varying levels of caregiver well-being and preparedness. Support Care Cancer, 25, 2437–2444. 10.1007/s00520-017-3650-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockham B, Sschafenacker A, Yoon H, Ronis DL, Kershaw T, Titler M & Northouse L 2016. Implementation of a psychoeducational program for cancer survivors and family caregivers at a cancer support community affiliate: a pilot effectiveness study. Cancer Nurs, 39, 169–80. 10.1097/NCC.0000000000000311 [DOI] [PubMed] [Google Scholar]
- Duggleby W, Doell H, Cooper D, Thomas R & Ghosh S 2014a. The quality of life of male spouses of women with breast cancer: hope, self-efficacy, and perceptions of guilt. Cancer Nurs, 37, E28–35. 10.1097/NCC.0b013e31827ca807 [DOI] [PubMed] [Google Scholar]
- Duggleby W, Ghosh S, Struthers Montford K, Nekolaichuk C, Cumming C, Thomas R, Tonkin K & Swindle J 2017a. Feasibility study of an online intervention to support male spouses of women with breast cancer. Oncol Nurs Forum, 44, 765–775. 10.1188/17.ONF.765-775 [DOI] [PubMed] [Google Scholar]
- Duggleby W, Thomas J, Montford K, Thomas R, Nekolaichuk C, Ghosh S, Cumming C & Tonkin K 2015. Transitions of male partners of women with breast cancer: hope, guilt, and quality of life. Oncol Nurs Forum, 42, 134–41. 10.1188/15.ONF.134-141 [DOI] [PubMed] [Google Scholar]
- Duggleby W, Tycholiz J, Holtslander L, Hudson P, Nekolaichuk C, Mirhosseini M, Parmar J, Chambers T, Alook A & Swindle J 2017b. A metasynthesis study of family caregivers’ transition experiences caring for community-dwelling persons with advanced cancer at the end of life. Palliat Med, 31, 602–616. 10.1177/0269216316673548 [DOI] [PubMed] [Google Scholar]
- Duggleby W, Williams A, Holtslander L, Cooper D, Ghosh S, Hallstrom L, Mclean R & Hampton M 2013. Evaluation of the Living with Hope Program for rural women caregivers of persons with advanced cancer. BMC Palliat Care, 12, 36. 10.1186/1472-684X-12-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggleby W, Williams A, Holtslander L, Thomas R, Cooper D, Hallstrom L, Ghosh S & O’Rourke H 2014b. Hope of rural women caregivers of persons with advanced cancer: guilt, self-efficacy and mental health. Rural Remote Health, 14, 2561. [PubMed] [Google Scholar]
- Ellis KR, Janevic MR, Kershaw T, Caldwell CH, Janz NK & Northouse L 2017. The influence of dyadic symptom distress on threat appraisals and self-efficacy in advanced cancer and caregiving. Support Care Cancer, 25, 185–194. 10.1007/s00520-016-3385-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flinn B 2018. Millennials: The emerging generation of family caregivers. Washington D. C.: AARP Public Policy Institute. [Google Scholar]
- Friedman EM, Trail TE, Vaughan CA & Tanielian T 2018. Online peer support groups for family caregivers: are they reaching the caregivers with the greatest needs? J Am Med Inform Assoc, 25, 1130–1136. 10.1093/jamia/ocy086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goren A, Gilloteau I, Lees M & Dacosta Dibonaventura M 2014. Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer, 22, 1637–46. 10.1007/s00520-014-2122-6 [DOI] [PubMed] [Google Scholar]
- Havyer RD, Van Ryn M, Wilson PM & Griffin JM 2017. The effect of routine training on the self-efficacy of informal caregivers of colorectal cancer patients. Support Care Cancer, 25, 1071–1077. 10.1007/s00520-016-3494-6 [DOI] [PubMed] [Google Scholar]
- Hendrix CC, Abernethy A, Sloane R, Misuraca J & Moore J 2009. A pilot study on the influence of an individualized and experiential training on cancer caregiver’s self-efficacy in home care and symptom management. Home Health Nurs, 27, 271–8. 10.1097/01.nhh.0000356777.70503.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrix CC, Bailey DE JR., Steinhauser KE, Olsen MK, Stechuchak KM, Lowman SG, Schwartz AJ, Riedel RF, Keefe FJ, Porter LS & Tulsky JA 2016. Effects of enhanced caregiver training program on cancer caregiver’s self-efficacy, preparedness, and psychological well-being. Support Care Cancer, 24, 327–336. 10.1007/s00520-015-2797-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrix CC, Landerman R & Abernethy AP 2013. Effects of an individualized caregiver training intervention on self-efficacy of cancer caregivers. West J Nurs Res, 35, 590–610. 10.1177/0193945911420742 [DOI] [PubMed] [Google Scholar]
- Hu X, Peng X, Su Y & Huang W 2018. Caregiver burden among Chinese family caregivers of patients with lung cancer: A cross-sectional survey. Eur J Oncol Nurs, 37, 74–80. 10.1016/j.ejon.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Hudson PL, Aranda S & Hayman-White K 2005. A psycho-educational intervention for family caregivers of patients receiving palliative care: a randomized controlled trial. J Pain Symptom Manage, 30, 329–41. 10.1016/j.jpainsymman.2005.04.006 [DOI] [PubMed] [Google Scholar]
- Hudson PL, Hayman-White K, Aranda S & Kristjanson LJ 2006. Predicting family caregiver psychosocial functioning in palliative care. J Palliat Care, 22, 133–40. [PubMed] [Google Scholar]
- Hyde M, Legg M, Occhipinti S, Lepore S, Ugalde A, Zajdlewicz L, Laurie K, Dunn J & Chambers S 2017. Predictors of long-term distress in female partners of men diagnosed with prostate cancer. Psychooncology, 27. 10.1002/pon.4617 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US). [PubMed] [Google Scholar]
- Ito E & Tadaka E 2017. Quality of life among the family caregivers of patients with terminal cancer at home in Japan. Jpn J Nurs Sci, 14, 341–352. 10.1111/jjns.12164 [DOI] [PubMed] [Google Scholar]
- Johansen S, Cvancarova M & Ruland C 2017. The effect of cancer patients’ and their family caregivers’ physical and emotional symptoms on caregiver burden. Cancer Nurs, 41, 1. 10.1097/NCC.0000000000000493 [DOI] [PubMed] [Google Scholar]
- Kazanowski M 2005. Family caregivers’ medication management of symptoms in patients with cancer near death. J Hosp Palliat Nurs, 7, 174–181. [Google Scholar]
- Keefe FJ, Ahles TA, Porter LS, Sutton LM, Mcbride CM, Pope MS, Mckinstry ET, Furstenberg CP, Dalton J & Baucom DH 2003. The self-efficacy of family caregivers for helping cancer patients manage pain at end-of-life. Pain, 103, 157–62. 10.1016/s0304-3959(02)00448-7 [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Ahles TA, Sutton L, Dalton J, Baucom D, Pope MS, Knowles V, McKinstry E, Furstenberg C, Syrjala K, Waters SJ, McKee D, McBride C, Rumble M & Scipio C 2005. Partner-guided cancer pain management at the end of life: a preliminary study. J Pain Symptom Manage, 29, 263–72. 10.1016/j.jpainsymman.2004.06.014 [DOI] [PubMed] [Google Scholar]
- Kershaw T, Ellis KR, Yoon H, Schafenacker A, Katapodi M & Northouse L 2015. The interdependence of advanced cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Ann Behav Med, 49, 901–11. 10.1007/s12160-015-9743-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw TS, Mood DW, Newth G, Ronis DL, Sanda MG, Vaishampayan U & Northouse LL 2008. Longitudinal analysis of a model to predict quality of life in prostate cancer patients and their spouses. Ann Behav Med, 36, 117–28. 10.1007/s12160-008-9058-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Duberstein PR, Sorsensen S & Larson MR 2005. Levels of depressive symptoms in spouses of people with lung cancer: effects of personality, social support, and caregiving burden. Psychosomatics, 46, 123–30. 10.1176/appi.psy.46.2.123 [DOI] [PubMed] [Google Scholar]
- Kizza IB & Maritz J 2019. Family caregivers for adult cancer patients: knowledge and self-efficacy for pain management in a resource-limited setting. Support Care Cancer, 27, 2265–2274. 10.1007/s00520-018-4504-7 [DOI] [PubMed] [Google Scholar]
- Kizza IB & Muliira JK 2019. The influence of a home-based education intervention on family caregivers’ knowledge and self-efficacy for cancer pain management in adult patients within a resource-limited setting. J Cancer Educ, 34, 1150–1159. 10.1007/s13187-018-1421-x [DOI] [PubMed] [Google Scholar]
- Kizza IB & Muliira JK 2020. Determinants of quality of life among family caregivers of adult cancer patients in a resource-limited setting. Support Care Cancer, 28, 1295–1304. 10.1007/s00520-019-04947-2 [DOI] [PubMed] [Google Scholar]
- Knoll N, Scholz U, Burkert S, Roigas J & Gralla O 2009. Effects of received and mobilized support on recipients’ and providers’ self-efficacy beliefs: a 1-year follow-up study with patients receiving radical prostatectomy and their spouses. Int J Psychol, 44, 129–37. 10.1080/00207590701607930 [DOI] [PubMed] [Google Scholar]
- Latter S, Hopkinson JB, Richardson A, Hughes JA, Lowson E & Edwards D 2016. How can we help family carers manage pain medicines for patients with advanced cancer? A systematic review of intervention studies. BMJ Support Palliat Care, 6, 263–75. 10.1136/bmjspcare-2015-000958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KC, Yiin JJ & Chao YF 2016. Effect of integrated caregiver support on caregiver burden for people taking care of people with cancer at the end of life: A cohort and quasi-experimental clinical trial. Int J Nurs Stud, 56, 17–26. 10.1016/j.ijnurstu.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Lee YH, Liao YC, Liao WY, Shun SC, Liu YC, Chan JC, Yu CJ, Yang PC & Lai YH 2013. Anxiety, depression and related factors in family caregivers of newly diagnosed lung cancer patients before first treatment. Psychooncology, 22, 2617–23. 10.1002/pon.3328 [DOI] [PubMed] [Google Scholar]
- Lee YH, Liao YC, Shun SC, Lin KC, Liao WY, Chang PH, Jhang SY, Yu CJ, Yang PC, Hsieh PY & Lai YH 2018. Trajectories of caregiver burden and related factors in family caregivers of patients with lung cancer. Psychooncology, 27, 1493–1500. https://doi.org/0.1002/pon.4678 [DOI] [PubMed] [Google Scholar]
- Leow M, Chan S & Chan M 2015. A pilot randomized, controlled trial of the effectiveness of a psychoeducational intervention on family caregivers of patients with advanced cancer. Oncol Nurs Forum, 42, E63–72. 10.1188/15.ONF.E63-E72 [DOI] [PubMed] [Google Scholar]
- Lewis FM, Griffith KA, Alzawad Z, Dawson PL, Zahlis EH & Shands ME 2019. Helping Her Heal: randomized clinical trial to enhance dyadic outcomes in couples. Psychooncology, 28, 430–438. 10.1002/pon.4966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Lin Y, Zhou H, Xu Y, Yang L & Xu Y 2018. Factors moderating the mutual impact of benefit finding between Chinese patients with cancer and their family caregivers: A cross-sectional study. Psychooncology, 27, 2363–2373. 10.1002/pon.4833 [DOI] [PubMed] [Google Scholar]
- Li Q & Loke AY 2013. The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology, 22, 2399–407. 10.1002/pon.3311 [DOI] [PubMed] [Google Scholar]
- Li Q, Xu Y, Zhou H & Loke AY 2015. A couple-based complex intervention for Chinese spousal caregivers and their partners with advanced cancer: an intervention study. Psychooncology, 24, 1423–1431. 10.1002/pon.3809 [DOI] [PubMed] [Google Scholar]
- Marshall CA, Badger TA, Curran MA, Koerner SS, Larkey LK, Weihs KL, Verdugo L & Garcia FA 2013. Un Abrazo Para La Familia: providing low-income Hispanics with education and skills in coping with breast cancer and caregiving. Psychooncology, 22, 470–4. 10.1002/pon.2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazanec S, Sattar A, Delaney C & Daly B 2015. Activation for health management in colorectal cancer survivors and their family caregivers. West J Nurs Res, 38. 10.1177/0193945915604055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazanec SR, Sandstrom K, Coletta D, Dorth J, Zender C, Alfes CM & Daly BJ 2019. Building family caregiver skills using a simulation-based intervention: a randomized pilot trial. Oncol Nurs Forum, 46, 419–427. 10.1188/19.ONF.419-427 [DOI] [PubMed] [Google Scholar]
- Mori M, Ellison D, Ashikaga T, McVeigh U, Ramsay A & Ades S 2013. In-advance end-of-life discussions and the quality of inpatient end-of-life care: a pilot study in bereaved primary caregivers of advanced cancer patients. Support Care Cancer, 21, 629–36. 10.1007/s00520-012-1581-x [DOI] [PubMed] [Google Scholar]
- Morse KD 2013. Predictors of preferences for cancer support group topic and group satisfaction among people living with cancer and caregivers of people living with cancer. PhD. [Google Scholar]
- Mosher CE, Secinti E, Johns SA, O’Neil BH, Helft PR, Shahda S, Jalal SI & Champion VL 2018. Examining the effect of peer helping in a coping skills intervention: a randomized controlled trial for advanced gastrointestinal cancer patients and their family caregivers. Qual Life Res, 27, 515–528. 10.1007/s11136-017-1620-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher CE, Winger JG, Hanna N, Jalal SI, Einhorn LH, Birdas TJ, Ceppa DP, Kesler KA, Schmitt J, Kashy DA & Champion VL 2016. Randomized pilot trial of a telephone symptom management intervention for symptomatic lung cancer patients and their family caregivers. J Pain Symptom Manage, 52, 469–482. 10.1016/j.jpainsymman.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mystakidou K, Parpa E, Panagiotou I, Tsilika E, Galanos A & Gouliamos A 2013. Caregivers’ anxiety and self-efficacy in palliative care. Eur J Cancer Care, 22, 188–195. 10.1111/ecc.12012 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving. 2016. Cancer Caregiving in the U.S.: An Intense, Episodic, & Challenging Care Experience. Washington D.C.: National Alliance for Caregiving, National Cancer Institute, and Cancer Support Community. [Google Scholar]
- National Alliance for Caregiving. 2020. Caregiving in the U.S Washington D.C.: National Alliance for Caregiving. [Google Scholar]
- National Cancer Institute. 2019. PDQ Informal Caregivers in Cancer. Bethesda, MD: National Cancer Institute. [Google Scholar]
- National Coalition for Hospice and Palliative Care. 2020. Who we are [Online]. Available: https://www.nationalcoalitionhpc.org/about/ [Accessed 2020].
- National Consensus Projet. 2018. Clinical Practice Guidelines for Quality Palliative Care. 4th ed.Richmond, VA: National Consensus Project. [Google Scholar]
- National Institutes of Health. 2020. Patient-Reported Outcomes Measurement Information System (PROMIS) [Online]. Available: https://commonfund.nih.gov/promis/index [Accessed 2020].
- Northouse L, Schafenackera A, Barr KL, Katapodi M, Yoon H, Brittain K, Song L, Ronis DL & An L 2014. A tailored web-based psychoeducational intervention for cancer patients and their family caregivers. Cancer Nurs, 37, 321–30. 10.1097/NCC.0000000000000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L & Mood DW 2010. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin, 60, 317–39. 10.3322/caac.20081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, Galvin E & Decker V 2002. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol, 20, 4050–64. 10.1200/JCO.2002.02.054 [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, Lorusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL & Kershaw T 2013. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology, 22, 555–63. 10.1002/pon.3036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary A 1992. Self-efficacy and health: behavioral and stress-physiological mediation. Cognit Ther Res, 16, 229–245. https://psycnet.apa.org/doi/10.1007/BF01173490 [Google Scholar]
- Oh YS 2017. Communications with health professionals and psychological distress in family caregivers to cancer patients: A model based on stress-coping theory. Appl Nurs Res, 33, 5–9. 10.1016/j.apnr.2016.09.008 [DOI] [PubMed] [Google Scholar]
- Oken BS, Fonareva I, Haas M, Wahbeh H, Lane JB, Zajdel D & Amen A 2010. Pilot controlled trial of mindfulness meditation and education for dementia caregivers. J Alternat Complement Med, 16, 1031–1038. 10.108/acm.2009.0733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajares F 2002. Gender and perceived self-efficacy in self-regulated learning. Theory Pract, 41, 116–125. https://www.jstor.org/stable/1477463 [Google Scholar]
- Pearce MJ, Singer JL & Prigerson HG 2006. Religious coping among caregivers of terminally ill cancer patients: main effects and psychosocial mediators. J Health Psychol, 11, 743–59. 10.1177/1359105306066629 [DOI] [PubMed] [Google Scholar]
- Pekmezi D, Jennings E & Marcus BH 2009. Evaluating and enhancing self-efficacy for physical activity. ACSM’s Health Fit J, 13. 10.1249/FFIT.0b013e3181996571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins M, Howard VJ, Wadley VG, Crowe M, Safford MM, Haley WE, Howard G & Roth DL 2013. Caregiving strain and all-cause mortality: evidence from the REGARDS study. J Gerontol B Psychol Sci Soc Sci, 68, 504–12. 10.1093/geronb/gbs084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perz J, Ussher JM, Butow P & Wain G 2011. Gender differences in cancer carer psychological distress: an analysis of moderators and mediators. Eur J Cancer Care, 20, 610–9. 10.1111/j.1365-2354.2011.01257.x [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Davis D, Rumble M, Scipio C & Garst J 2012. Attachment styles in patients with lung cancer and their spouses: associations with patient and spouse adjustment. Support Care Cancer, 20, 2459–2466. 10.1007/s00520-011-1367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Garst J, Baucom DH, Mcbride CM, Mckee DC, Suttom L, Carson K, Knowles V, Rumble M & Scipio C 2011. Caregiver-assisted coping skills training for lung cancer: results of a randomized clinical trial. J Pain Symptom Manage, 41, 1–13. 10.1016/j.jpainsymman.2010.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Garst J, Mcbride CM & Baucon D 2008. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: associations with symptoms and distress. Pain, 137, 306–15. 10.1016/j.pain.2007.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posluszny DM, Bovbjerg DH, Syrjala KL, Agha M & Dew MA 2019. Correlates of anxiety and depression symptoms among patients and their family caregivers prior to allogeneic hematopoietic cell transplant for hematological malignancies. Support Care Cancer, 27, 591–600. 10.1007/s00520-018-4346-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M 2016. The advantages and disadvantages of using qualitative and quantitative approaches and methods in language “testing and assessment” research: a literature review. J Educ Learn, 6, 102. [Google Scholar]
- Roche V 2009. The hidden patient: addressing the caregiver. Am J Med Sci, 337, 199–204. 10.1097/MAJ.0b013e31818b114d [DOI] [PubMed] [Google Scholar]
- Segrin C & Badger TA 2014. Psychological and physical distress are interdependent in breast cancer survivors and their partners. Psychol Health Med, 19, 716–23. 10.1080/13548506.2013.871304 [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger TA, Sikorskii A, Crane TE & Pace TWW 2018. A dyadic analysis of stress processes in Latinas with breast cancer and their family caregivers. Psychooncology, 27, 838–846. 10.1002/pon.4580 [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger TA, Sikorskii A, Pasvogel A, Weihs K, Lopez AM & Chalasani P 2020. Longitudinal dyadic interdependence in psychological distress among Latinas with breast cancer and their caregivers. Support Care Cancer, 28, 2735–2743. 10.1007/s00520-019-05121-4 [DOI] [PubMed] [Google Scholar]
- Tate RH 2018. Learning to be a cancer caregiver: The role of self-efficacy in caregivers strain. PhD, The Pennsylvania State University. [Google Scholar]
- Titler MG, Visovatti MA, Shuman C, Ellis KR, Banerjee T, Dockham B, Yakusheva O & Northouse L 2017. Effectiveness of implementing a dyadic psychoeducational intervention for cancer patients and family caregivers. Support Care Cancer, 25, 3395–3406. 10.1007/s00520-017-3758-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ugalde A & Krishnasamy M 2014. The relationship between self-efficacy and anxiety and general distress in caregivers of people with advanced cancer. J Palliat Med, 17. 10.1089/jpm.2013.0338 [DOI] [PubMed] [Google Scholar]
- Ugalde A, Krishnasamy M & Schofield P 2013. Development of an instrument to measure self-efficacy in caregivers of people with advanced cancer. Psychooncology, 22, 1428–34. 10.1002/pon.3160 [DOI] [PubMed] [Google Scholar]
- Yildiz E, Asi Karakas S, Gungormus Z & Cengiz M 2017. Levels of care burden and self-efficacy for informal caregiver of patients with cancer. Holist Nurs Pract, 31, 7–15. 10.1097/HNP.0000000000000185 [DOI] [PubMed] [Google Scholar]
- Young HM, Bell JF, Whitney RL, Ridberg RA, Reed SC & Vitaliano PP 2020. Social determinants of health: underreported heterogeneity in systematic reviews of caregiver interventions. Gerontologist, 60, S14–S28. 10.1093/geront/gnz148 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


