ABSTRACT
Introduction: Vaccination coverage among undernourished children often associated with higher risk of contracting infectious diseases due to lowered immunity is a critical public health concern. The vaccination coverage is low and the child mortality rate is high in Nigeria. This study investigates the association between selected vaccines uptake and undernutrition among Nigerian children.
Methods: The 2018 Nigeria Demographic and Health Survey dataset was used for this study. Children aged 0–36 months were included in the study. Stunting and wasting were the main outcome variables to define undernutrition outcomes. The effect of BCG, first dose of DPT/Pentavalent (DPT/Penta1), third dose of DPT/Pentavalent (DPT/Penta3) and measles vaccines on nutrition outcomes were individually examined using logistic regression at 5% significance level.
Results: Among 6,928 children aged 0 to 36 months old, 34.4% were stunted and 8.7% were wasted, while the vaccination rate was 70.0% (BCG), 65.0% (DPT/Penta1), 48.2% (DPT/Penta1), and 43.6% (measles). Vaccination uptake was consistently associated with less likelihood of stunting, while it was not associated with wasting. We also found that some vaccination uptake was negatively associated with stunting particularly among older children.
Discussions/Conclusion: The finding that vaccination is associated with less likelihood of stunting implies that the vaccination can be important to enhance the long-term nutrition outcomes. Targeting children with disadvantageous sociodemographic characteristics for vaccination can further enhance the overall nutrition outcomes among them.
KEYWORDS: Vaccination, undernutrition, stunting, wasting, Nigeria
Introduction
Vaccination saves lives.1 Vaccination can be even more important among malnourished children as they have higher risk of contracting infectious diseases due to lowered immunity.2–4 Vaccination can improve children’s nutritional status through lowering infection incidences.5,6
Nigeria has high child mortality: the under-5 mortality rate is 132 deaths per 1,000 live births.7 Nutrition-related factors contribute to 45% of deaths in children aged 5 or below.8 Nigeria also has one of the highest burden of stunted children in the world: the prevalence of stunting was 32.0%.9
The vaccination coverage in Nigeria is low as compared to other countries. For example, in Nigeria’s neighboring country Ghana, the vaccination rate for third dose of the diphtheria, tetanus and pertussis vaccine (DTP3) reached 97% in 2019,10 while it was only 57% in Nigeria.11 The global coverage of the DTP3 was 85% in 2019.10
Because vaccination coverage among undernourished children often associated with higher risk of contracting infectious diseases due to lowered immunity is a critical public health concern,12,13,14,1516 this study investigates the association between selected vaccination uptake and undernutrition among Nigerian children in Nigeria. In addition, we also analyze how sociodemographic characteristics are associated with nutrition outcomes as well as with vaccine uptake.
Through these analyses, this study intends to identify who are exposed to disease risks and to malnutrition, and to inform the policy on which population to target to improve people’s health outcomes in efficient ways.
Methods
Data source
The dataset we used in the analysis is the Nigeria Demographic and Health Survey (DHS) conducted in 2018, which contains various pieces of information on respondents and their children. From the DHS data, vaccination records of respondents’ children for each vaccine are used. The data contain information whether each dose of vaccine was received by children aged between 0 and 36 months old within 5 years prior to the survey. We focus on the uptake of BCG, first dose of DPT/Pentavalent (DPT/Penta1), third dose of DPT/Pentavalent (DPT/Penta3), and measles vaccine. These vaccines are recommended to be received at the age of 0 week (BCG), 6 weeks (DPT/Penta1), 14 weeks (DPT/Penta3), and at 9 months (measles).13 We focus on these four vaccines because they either have the distinct vaccine schedule, such as BCG at birth, or are usually used as a benchmark for the vaccination coverage such as DPT/Penta3 or measles.8 Other researchers have previously investigated the effect of these vaccines on malnutrition.14 From the same dataset, two nutrition outcome variables are used: stunting and wasting, among children aged between 0 and 36 months old. Stunting is measured in terms of height-for-age, which is an indication of chronic (long-term) undernutrition, while wasting is measured in terms of weight-for-height, which is an indication of acute (short-term) undernutrition.7
Statistical analysis
To evaluate the association between vaccination uptake and nutrition outcomes, logistic regression is employed, because the nutrition outcome is a dummy variable, in the following regression framework:
| (1) |
where is a nutrition outcome, in this case either stunted or wasted, of a respondent’s child i in cluster j; indicates if a child i in cluster j received a vaccine (BCG, DPT/Penta1, DPT/Penta3, or measles). Because we use four vaccines, there are four different regression specifications, corresponding to each type of vaccine: BCG, DPT/Penta1, DPT/Penta3, or measles, to evaluate the association between each vaccine uptake and nutrition outcome. In this main regression, a set of sociodemographic characteristics of women, their households, and their children, such as women’s education level, child’s age, wealth level, place of residence (urban/rural), are controlled for. Cluster fixed effects (v) are also controlled for. The cluster fixed effect controls for any observable and unobservable characteristics at the cluster level that is correlated with nutrition outcomes within the cluster.
To evaluate the potential differential pattern according to children’s age, we also evaluate the association between vaccination uptake and nutrition outcome according to children’s age. For this analysis, the sample was divided by their age: under 12 months, 12 to 24 months, and 24 to 36 months. We control for the same set of controls as above, including the child’s age because there might be differential effect of age even within a certain age range.
Results
Analyses were based on a total of 6,928 children aged 0 to 36 months old, with no missing information on important characteristics such as nutrition outcomes, vaccination uptake, and sociodemographic characteristics. Table A1 presents the summary statistics. Among all the children, 2,382 children (34.4%) were stunted, while 601 children (8.7%) were wasted. The vaccination uptake was 70.0% for BCG, 65.0% for DPT/Penta1, 48.2% for DPT/Penta3, and 43.6% for measles vaccine.
More than one-thirds (36.9%) of children’s mothers did not receive any form of education, while less than 10% of them (9.6%) received higher education than high school. Children’s households were almost equally distributed across five wealth levels (poorest, poorer, middle, richer, and richest). More than half of children (60.4%) reside in rural area. The average age of children was 16.8 months.
Figure 1 presents the vaccination rate by nutrition status. Panel A shows that stunted children had lower rate of vaccination than children who were not stunted, and Panel B shows that wasted children had lower rate of vaccination than children who are wasted.
Figure 1.
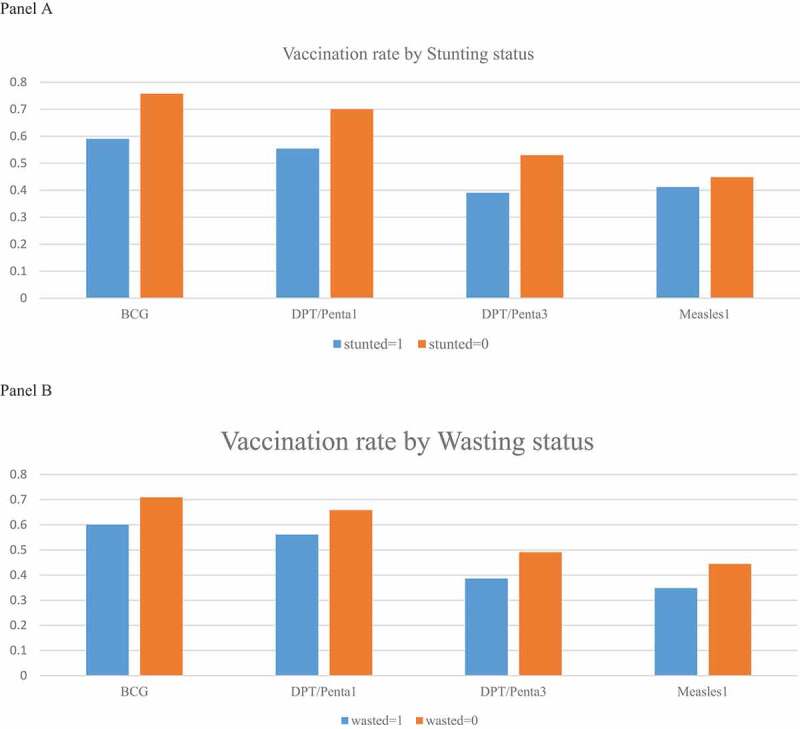
Vaccination rate by nutrition status. Panel A: By stunting status. Panel B: Wasting status
Table 1 presents the main result: the association between the vaccination uptake and nutrition outcomes. After controlling for sociodemographic characteristics, vaccination uptake for all the vaccine types were negatively correlated with stunting (Columns 1 to 4), although DPT/Penta1 is only insignificantly correlated with stunting (Column 2). On the other hand, they were not significantly correlated with wasting (Column 5 to 8). Odds ratio on stunting is similar for each vaccination; vaccination was associated with lower odds of being stunted by 17.2 to 24.2%. Vaccination uptake was rather positively associated with wasting, although insignificant.
Table 1.
Association between malnutrition and vaccination
| Stunted |
Wasted |
|||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| BCG | 0.758* | 1.033 | ||||||
| [0.621,0.926] | [0.767,1.390] | |||||||
| DPT/Penta1 | 0.828 | 1.252 | ||||||
| [0.682,1.006] | [0.954,1.642] | |||||||
| DPT/Penta3 | 0.770* | 1.184 | ||||||
| [0.630,0.941] | [0.885,1.583] | |||||||
| Measles | 0.780* | 1.087 | ||||||
| [0.641,0.950] | [0.801,1.476] | |||||||
| Education (comparison: No education) | ||||||||
| Incomplete primary | 0.954 | 0.941 | 0.936 | 0.936 | 0.975 | 0.960 | 0.971 | 0.970 |
| [0.659,1.383] | [0.650,1.361] | [0.647,1.353] | [0.646,1.355] | [0.535,1.778] | [0.527,1.751] | [0.533,1.767] | [0.534,1.761] | |
| Complete primary | 0.774 | 0.765 | 0.766 | 0.757 | 0.674 | 0.662 | 0.666 | 0.673 |
| [0.580,1.034] | [0.572,1.022] | [0.573,1.024] | [0.566,1.013] | [0.426,1.066] | [0.418,1.048] | [0.419,1.056] | [0.426,1.066] | |
| Incomplete secondary | 0.670* | 0.665* | 0.671* | 0.657* | 0.722 | 0.700 | 0.705 | 0.721 |
| [0.489,0.919] | [0.485,0.911] | [0.489,0.921] | [0.480,0.901] | [0.431,1.209] | [0.418,1.173] | [0.419,1.184] | [0.431,1.208] | |
| Complete secondary | 0.608* | 0.597* | 0.611* | 0.595* | 0.797 | 0.774 | 0.777 | 0.794 |
| [0.451,0.820] | [0.444,0.805] | [0.453,0.823] | [0.442,0.802] | [0.488,1.302] | [0.474,1.263] | [0.474,1.274] | [0.486,1.298] | |
| Higher | 0.339* | 0.334* | 0.343* | 0.334* | 0.605 | 0.576 | 0.580 | 0.603 |
| [0.209,0.549] | [0.206,0.541] | [0.211,0.557] | [0.206,0.542] | [0.311,1.176] | [0.296,1.119] | [0.296,1.137] | [0.311,1.171] | |
| Child’s age in months | 1.079* | 1.080* | 1.081* | 1.084* | 0.971* | 0.970* | 0.970* | 0.970* |
| [1.070,1.088] | [1.071,1.089] | [1.072,1.090] | [1.074,1.093] | [0.960,0.982] | [0.959,0.981] | [0.959,0.981] | [0.957,0.982] | |
| Wealth (comparison: poorest) | ||||||||
| Poorer | 0.968 | 0.968 | 0.960 | 0.971 | 0.742 | 0.743 | 0.744 | 0.741 |
| [0.745,1.257] | [0.745,1.258] | [0.738,1.249] | [0.747,1.262] | [0.498,1.107] | [0.499,1.109] | [0.499,1.109] | [0.497,1.105] | |
| Middle | 0.982 | 0.981 | 0.978 | 0.987 | 0.742 | 0.736 | 0.741 | 0.742 |
| [0.703,1.372] | [0.701,1.372] | [0.699,1.370] | [0.705,1.382] | [0.445,1.235] | [0.442,1.228] | [0.444,1.237] | [0.446,1.235] | |
| Richer | 0.735 | 0.731 | 0.733 | 0.742 | 0.672 | 0.664 | 0.667 | 0.669 |
| [0.494,1.093] | [0.491,1.087] | [0.493,1.092] | [0.498,1.105] | [0.362,1.246] | [0.357,1.234] | [0.359,1.241] | [0.360,1.241] | |
| Richest | 0.558* | 0.552* | 0.560* | 0.569* | 0.450* | 0.439* | 0.444* | 0.448* |
| [0.339,0.918] | [0.335,0.910] | [0.339,0.923] | [0.345,0.938] | [0.208,0.976] | [0.202,0.953] | [0.204,0.965] | [0.206,0.973] | |
| Residence (comparison: urban) | ||||||||
| Rural | 0.541* | 0.576* | 0.602 | 0.560* | 0.767* | 0.796 | 0.710* | 0.782 |
| [0.314,0.930] | [0.335,0.990] | [0.358,1.013] | [0.330,0.952] | [0.594,0.991] | [0.614,1.030] | [0.534,0.944] | [0.598,1.023] | |
| N | 5373 | 5373 | 5373 | 5373 | 2788 | 2788 | 2788 | 2788 |
| Cluster FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
*Significant at 5%.
Table 2 repeats the same exercise on the association between vaccination and stunting, according to children’s age. The vaccination uptake was not statistically correlated with stunting among children under 12 months. Measles vaccination was negatively associated with stunting among children between 12 and 24 months old, while BCG and DPT/Penta1 were negatively correlated with stunting among children between 24 and 36 months old.
Table 2.
Association between stunting and vaccination, by children’s age
| |
Stunted |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
<12 months |
12–24 months |
24–36 months |
|||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | |
| BCG | 0.975 | 0.826 | 0.494* | |||||||||
| [0.601,1.581] | [0.494,1.381] | [0.248,0.985] | ||||||||||
| DPT/Penta1 | 1.004 | 0.858 | 0.488* | |||||||||
| [0.611,1.649] | [0.517,1.425] | [0.261,0.915] | ||||||||||
| DPT/Penta3 | 0.662 | 0.971 | 0.734 | |||||||||
| [0.391,1.122] | [0.594,1.589] | [0.418,1.288] | ||||||||||
| Measles | 0.802 | 0.629* | 0.760 | |||||||||
| [0.430,1.498] | [0.402,0.985] | [0.446,1.293] | ||||||||||
| Education (comparison: No education) | ||||||||||||
| Incomplete primary | 0.796 | 0.795 | 0.797 | 0.797 | 1.561 | 1.574 | 1.558 | 1.590 | 1.073 | 0.989 | 0.988 | 0.960 |
| [0.370,1.714] | [0.370,1.707] | [0.373,1.705] | [0.370,1.713] | [0.584,4.176] | [0.587,4.226] | [0.579,4.194] | [0.588,4.298] | [0.342,3.363] | [0.315,3.108] | [0.330,2.961] | [0.321,2.869] | |
| Complete primary | 0.963 | 0.960 | 0.998 | 0.968 | 0.522 | 0.521 | 0.511 | 0.544 | 0.514 | 0.501 | 0.500 | 0.497 |
| [0.466,1.990] | [0.464,1.986] | [0.482,2.066] | [0.467,2.004] | [0.215,1.263] | [0.214,1.267] | [0.209,1.249] | [0.225,1.315] | [0.212,1.246] | [0.209,1.203] | [0.210,1.189] | [0.207,1.193] | |
| Incomplete secondary | 0.887 | 0.885 | 0.916 | 0.883 | 0.492 | 0.490 | 0.482 | 0.486 | 0.320* | 0.328* | 0.312* | 0.301* |
| [0.421,1.868] | [0.420,1.866] | [0.433,1.935] | [0.419,1.861] | [0.212,1.141] | [0.212,1.134] | [0.206,1.128] | [0.211,1.121] | [0.129,0.792] | [0.133,0.808] | [0.126,0.777] | [0.123,0.739] | |
| Complete secondary | 0.762 | 0.757 | 0.816 | 0.757 | 0.333* | 0.331* | 0.324* | 0.351* | 0.315* | 0.321* | 0.308* | 0.303* |
| [0.346,1.676] | [0.343,1.668] | [0.372,1.790] | [0.345,1.665] | [0.136,0.815] | [0.135,0.810] | [0.131,0.803] | [0.143,0.860] | [0.138,0.715] | [0.142,0.726] | [0.137,0.693] | [0.134,0.688] | |
| Higher | 1.221 | 1.211 | 1.267 | 1.231 | 0.363 | 0.359 | 0.349 | 0.374 | 0.131* | 0.130* | 0.126* | 0.128* |
| [0.400,3.726] | [0.395,3.718] | [0.413,3.888] | [0.402,3.773] | [0.106,1.246] | [0.104,1.234] | [0.100,1.214] | [0.108,1.296] | [0.040,0.430] | [0.040,0.424] | [0.039,0.409] | [0.039,0.418] | |
| Child’s age in months | 1.111* | 1.110* | 1.131* | 1.121* | 1.128* | 1.129* | 1.128* | 1.132* | 0.969 | 0.967 | 0.964 | 0.965 |
| [1.053,1.172] | [1.050,1.174] | [1.067,1.199] | [1.055,1.192] | [1.063,1.197] | [1.064,1.198] | [1.063,1.197] | [1.067,1.202] | [0.896,1.049] | [0.894,1.046] | [0.893,1.042] | [0.893,1.042] | |
| Wealth (comparison: poorest) | ||||||||||||
| Poorer | 0.727 | 0.727 | 0.735 | 0.728 | 1.364 | 1.351 | 1.358 | 1.367 | 1.312 | 1.261 | 1.226 | 1.226 |
| [0.387,1.366] | [0.387,1.367] | [0.390,1.389] | [0.386,1.372] | [0.683,2.724] | [0.678,2.690] | [0.680,2.711] | [0.681,2.743] | [0.512,3.362] | [0.495,3.214] | [0.487,3.082] | [0.490,3.066] | |
| Middle | 1.002 | 1.001 | 0.998 | 1.023 | 1.223 | 1.218 | 1.210 | 1.269 | 1.007 | 0.968 | 0.946 | 0.957 |
| [0.430,2.334] | [0.430,2.331] | [0.428,2.328] | [0.439,2.383] | [0.536,2.790] | [0.533,2.783] | [0.530,2.764] | [0.548,2.937] | [0.355,2.855] | [0.340,2.757] | [0.336,2.668] | [0.340,2.694] | |
| Richer | 0.499 | 0.498 | 0.488 | 0.513 | 1.110 | 1.106 | 1.098 | 1.146 | 1.089 | 1.083 | 1.001 | 0.985 |
| [0.179,1.390] | [0.179,1.383] | [0.176,1.352] | [0.185,1.421] | [0.408,3.014] | [0.406,3.013] | [0.401,3.004] | [0.416,3.154] | [0.324,3.666] | [0.322,3.642] | [0.301,3.334] | [0.295,3.283] | |
| Richest | 0.409 | 0.408 | 0.399 | 0.424 | 0.438 | 0.436 | 0.433 | 0.464 | 0.707 | 0.713 | 0.649 | 0.646 |
| [0.115,1.455] | [0.115,1.449] | [0.112,1.423] | [0.120,1.505] | [0.132,1.456] | [0.131,1.454] | [0.129,1.458] | [0.138,1.558] | [0.171,2.921] | [0.173,2.929] | [0.159,2.646] | [0.159,2.624] | |
| Residence (comparison: urban) | ||||||||||||
| Rural | 1.802 | 1.815 | 1.677 | 1.715 | 0.082* | 0.083* | 0.087* | 0.072* | 1.004 | 1.422 | 1.242 | 0.989 |
| [0.707,4.589] | [0.657,5.012] | [0.642,4.383] | [0.667,4.410] | [0.032,0.208] | [0.033,0.213] | [0.035,0.221] | [0.028,0.187] | [0.380,2.649] | [0.506,3.997] | [0.434,3.556] | [0.380,2.575] | |
| N | 1069 | 1069 | 1069 | 1069 | 1078 | 1078 | 1078 | 1078 | 814 | 814 | 814 | 814 |
| Cluster FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
*Significant at 5%.
Table 3 repeats the same exercise on wasting, according to children’s age. There was no statistically significant association between vaccination uptake and wasting, except that measles vaccination was positively associated with wasting among children aged between 24 and 36 months.
Table 3.
Association between wasting and vaccination, by children’s age
| Wasted |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <12 months |
12–24 months |
24–36 months |
||||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | |
| BCG | 0.698 | 1.305 | 0.736 | |||||||||
| [0.357,1.363] | [0.564,3.019] | [0.201,2.690] | ||||||||||
| DPT/Penta1 | 1.003 | 1.649 | 0.523 | |||||||||
| [0.523,1.923] | [0.819,3.318] | [0.153,1.787] | ||||||||||
| DPT/Penta3 | 0.827 | 1.733 | 0.939 | |||||||||
| [0.409,1.676] | [0.868,3.459] | [0.205,4.296] | ||||||||||
| Measles | 0.557 | 3.071* | 0.617 | |||||||||
| [0.241,1.290] | [1.490,6.331] | [0.180,2.116] | ||||||||||
| Education (comparison: No education) | ||||||||||||
| Incomplete primary | 0.608 | 0.603 | 0.610 | 0.625 | 2.469 | 2.502 | 2.457 | 2.301 | 0.229 | 0.191 | 0.238 | 0.260 |
| [0.168,2.198] | [0.166,2.194] | [0.168,2.215] | [0.172,2.272] | [0.484,12.588] | [0.485,12.901] | [0.480,12.568] | [0.446,11.872] | [0.009,5.721] | [0.007,5.468] | [0.010,5.859] | [0.011,6.267] | |
| Complete primary | 0.631 | 0.613 | 0.634 | 0.640 | 0.653 | 0.652 | 0.635 | 0.692 | 0.449 | 0.452 | 0.428 | 0.452 |
| [0.237,1.675] | [0.233,1.617] | [0.238,1.693] | [0.244,1.680] | [0.198,2.152] | [0.201,2.122] | [0.193,2.093] | [0.213,2.255] | [0.048,4.189] | [0.043,4.715] | [0.048,3.841] | [0.047,4.309] | |
| Incomplete secondary | 0.598 | 0.600 | 0.598 | 0.581 | 0.576 | 0.572 | 0.579 | 0.711 | 0.618 | 0.631 | 0.617 | 0.631 |
| [0.188,1.898] | [0.189,1.907] | [0.191,1.875] | [0.181,1.858] | [0.145,2.293] | [0.145,2.266] | [0.149,2.256] | [0.185,2.740] | [0.066,5.786] | [0.065,6.163] | [0.070,5.464] | [0.068,5.844] | |
| Complete secondary | 0.769 | 0.718 | 0.742 | 0.733 | 0.941 | 0.935 | 0.950 | 0.971 | 0.924 | 0.930 | 0.864 | 0.908 |
| [0.269,2.199] | [0.254,2.031] | [0.261,2.113] | [0.256,2.097] | [0.232,3.811] | [0.235,3.727] | [0.236,3.829] | [0.231,4.094] | [0.057,14.943] | [0.055,15.664] | [0.053,13.982] | [0.060,13.633] | |
| Higher | 1.432 | 1.252 | 1.346 | 1.336 | 0.312 | 0.301 | 0.314 | 0.273 | 0.963 | 0.974 | 0.887 | 0.913 |
| [0.278,7.372] | [0.240,6.527] | [0.263,6.882] | [0.257,6.946] | [0.030,3.296] | [0.029,3.134] | [0.031,3.186] | [0.027,2.780] | [0.061,15.237] | [0.060,15.829] | [0.057,13.892] | [0.064,13.033] | |
| Child’s age in months | 1.166* | 1.154* | 1.163* | 1.181* | 0.883* | 0.882* | 0.884* | 0.877* | 1.056 | 1.065 | 1.053 | 1.055 |
| [1.077,1.263] | [1.064,1.251] | [1.071,1.264] | [1.083,1.287] | [0.806,0.967] | [0.805,0.968] | [0.807,0.969] | [0.797,0.964] | [0.866,1.286] | [0.876,1.294] | [0.864,1.283] | [0.864,1.288] | |
| Wealth (comparison: poorest) | ||||||||||||
| Poorer | 0.918 | 0.939 | 0.943 | 0.908 | 0.560 | 0.586 | 0.593 | 0.534 | 0.706 | 0.751 | 0.675 | 0.733 |
| [0.395,2.132] | [0.403,2.192] | [0.402,2.213] | [0.389,2.122] | [0.217,1.441] | [0.229,1.500] | [0.225,1.564] | [0.200,1.430] | [0.153,3.254] | [0.165,3.425] | [0.147,3.102] | [0.158,3.408] | |
| Middle | 0.768 | 0.737 | 0.734 | 0.724 | 0.735 | 0.763 | 0.711 | 0.574 | 1.334 | 1.319 | 1.346 | 1.438 |
| [0.235,2.511] | [0.222,2.445] | [0.223,2.412] | [0.219,2.390] | [0.199,2.712] | [0.210,2.774] | [0.194,2.607] | [0.156,2.114] | [0.151,11.769] | [0.140,12.467] | [0.151,12.031] | [0.145,14.271] | |
| Richer | 0.735 | 0.712 | 0.703 | 0.707 | 1.387 | 1.421 | 1.274 | 1.137 | 0.221 | 0.253 | 0.209 | 0.266 |
| [0.197,2.740] | [0.191,2.652] | [0.189,2.622] | [0.192,2.606] | [0.230,8.373] | [0.239,8.436] | [0.210,7.707] | [0.178,7.275] | [0.011,4.382] | [0.013,5.062] | [0.009,4.598] | [0.012,5.833] | |
| Richest | 0.557 | 0.565 | 0.560 | 0.555 | 0.468 | 0.505 | 0.457 | 0.381 | 0.546 | 0.610 | 0.516 | 0.586 |
| [0.110,2.821] | [0.111,2.886] | [0.109,2.866] | [0.110,2.791] | [0.055,3.999] | [0.060,4.243] | [0.054,3.877] | [0.042,3.458] | [0.013,22.551] | [0.015,24.203] | [0.011,23.810] | [0.016,21.688] | |
| Residence (comparison: urban) | ||||||||||||
| Rural | 0.419* | 0.423* | 0.460* | 0.399* | 1.044 | 1.123 | 1.024 | 0.852 | 2.253 | 2.487 | 2.168 | 2.384 |
| [0.210,0.834] | [0.212,0.844] | [0.213,0.994] | [0.203,0.783] | [0.235,4.631] | [0.259,4.872] | [0.250,4.191] | [0.204,3.568] | [0.077,65.649] | [0.082,75.047] | [0.075,62.593] | [0.088,64.444] | |
| N | 648 | 648 | 648 | 648 | 482 | 482 | 482 | 482 | 188 | 188 | 188 | 188 |
| Cluster FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
*Significant at 5%.
Table A2 presents the association between nutrition outcomes and sociodemographic characteristics. Odds of being stunted was less as mothers’ education attainment got higher (column 1). As children got older, odds of them being stunted got higher. The wealth level was mostly not significantly correlated with the odds of being stunted, except that children in the richest households were less likely to be stunted. Mothers’ educational attainment was mostly uncorrelated with wasting, except that primary completion was associated with less odds of wasting (column 2). Children’s age was negatively associated with wasting. Being in the richest quintile of the wealth index was associated with lower odds of wasting, and so is residing in rural area.
Table A3 presents the association between vaccination uptake and sociodemographic characteristics. Generally, we observed the similar correlation between sociodemographic characteristics and vaccination uptake for any type of vaccines. Mothers’ higher education was strongly and positively correlated with vaccination. The wealth level was weakly but positively correlated with BCG and DPT/Penta3 vaccination, while it was significantly correlated with DPT/Penta1 and measles vaccination. Residing in rural area was positively correlated with DPT/Penta1 and DPT/Penta3 vaccination, but it was negatively correlated with measles vaccination.
Discussion
This paper evaluates the association between vaccination uptake and nutrition outcomes; long-term and short-term separately, among children aged under 36 months in Nigeria. Among 6,928 representative Nigerian children, 34.4% were stunted and 8.7% were wasted. The stunting prevalence in Nigeria is high; the world average of stunting prevalence is 21.3%, while it is 30.9% among African countries.8 The vaccination rate remains low in Nigeria; for example, 43.6% for measles vaccine, while the world average is over 85%.15
Vaccination uptake was negatively and significantly correlated with stunting, while it was not associated with wasting. Given that stunting is a measurement for the long-term malnutrition and wasting is the measurement for the short-term malnutrition, this clear distinction in the correlation between stunting and wasting is important. After controlling for sociodemographic characteristics, vaccination is associated with less likelihood of long-term malnutrition while it is not associated with short-term malnutrition.
This result is consistent with previous studies. For example,14 found that the take-up of BCG, DPT1, and measles vaccination is negatively correlated with stunting prevalence if children receive these vaccination early in life in Africa,4 also found the similar negative correlation between vaccination uptake and stunting prevalence in developing countries. However, they also found the significant correlation between vaccination uptake and wasting. This difference on wasting between our analysis and the analysis from Solis-Soto et al. might be due to the data coverage. Their results are based on data from 16 developing countries, 10 of which are from Africa but Nigeria was not one of them.
Vaccination is considered to protect children from diseases by building immune system, which can prevent them from falling malnourished. This process takes time. Thus, it makes logical sense that the vaccination uptake was not associated with wasting, the short-term malnutrition. On the other hand, the positive association between vaccination and nutrition outcomes is reassuring that vaccination enhances the health outcomes in the long run.
The vaccination uptake was mostly negatively correlated with stunting among children of older age. This finding is consistent with the main result described above that the vaccination uptake is associated with long-term nutrition outcomes. It takes time for vaccination to take effect on nutritional outcomes among children.
On the other hand, the vaccination uptake was mostly not correlated with wasting among children of any age. This finding is also consistent with the main result that the process through which the vaccination takes effect in children’s nutrition takes time. In other words, vaccination does not affect short-term nutrition status, regardless of children’s age.
Through this study, some correlations between nutrition outcomes and sociodemographic characteristics are also identified. Stunting were concentrated among children of less educated mothers and of less wealthy households. Wasting had the similar correlation with sociodemographic characteristics as stunting did, but weaker. Children’s age was positively correlated with stunting, while it was negatively correlated with wasting. Generally, vaccination uptake was positively correlated with mothers’ education, children’s age, and wealth level of households. Residing in rural area was positively correlated with DPT/Penta vaccination, while it was negatively correlated with measles vaccination. This opposite correlation pattern between residential area and DPT/Penta vaccination might indicate that DPT/Penta vaccine series are more available in rural areas, while measles vaccination was rather scarce in rural areas. However, the exact reason for this pattern is unknown.
Overall, vaccination can be important to enhance the long-term nutrition outcomes. Because both vaccination uptake and nutrition outcomes are associated with mothers’ education and wealth level of households, targeting children with poor sociodemographic characteristics for policy interventions to enhance vaccination uptake can also improve their nutrition outcomes in the long run.
Limitations
One limitation of the study is the lack of causal interpretation. Because the vaccination uptake is endogenous, as shown in Tables A2 and Tables A3, the results can be interpreted only as an association. The same limitation is discussed in, Berendsen, et al.14 and in Solis-Soto, et al.4
Conclusion
This study evaluates the association between vaccination uptake and nutrition outcomes, both long-term and short-term, among Nigerian children. The vaccination uptake is negatively associated with stunting, the long-term malnutrition indicator, while it is not associated with wasting, the short-term indicator. The result has an important policy implication. Targeting children with disadvantageous sociodemographic characteristics for vaccination can further enhance the overall nutrition outcomes among them.
Appendices.
Table A1.
Summary statistics (N = 6,928)
| N | % | |||
|---|---|---|---|---|
| Nutrition status | ||||
| Not Stunted | 4546 | 65.62 | ||
| Stunted | 2382 | 34.38 | ||
| Not wasted | 6327 | 91.33 | ||
| Wasted | 601 | 8.67 | ||
| Vaccination | ||||
| No BCG | 2080 | 30.02 | ||
| BCG | 4848 | 69.98 | ||
| No DPT/Penta1 | 2426 | 35.02 | ||
| DPT/Penta1 | 4502 | 64.98 | ||
| No DPT/Penta3 | 3591 | 51.83 | ||
| DPT/Penta3 | 3337 | 48.17 | ||
| No measles1 | 3910 | 56.44 | ||
| Measles1 | 3018 | 43.56 | ||
| Sociodemographic characteristics | ||||
| Mother’s education | ||||
| No education | 2553 | 36.85 | ||
| Incomplete primary | 299 | 4.32 | ||
| Complete primary | 812 | 11.72 | ||
| Incomplete secondary | 924 | 13.34 | ||
| Complete secondary | 1676 | 24.19 | ||
| Higher | 664 | 9.58 | ||
| Wealth | ||||
| Poorest | 1337 | 19.3 | ||
| Poorer | 1391 | 20.08 | ||
| Middle | 1529 | 22.07 | ||
| Richer | 1481 | 21.38 | ||
| Richest | 1190 | 17.18 | ||
| Residence | ||||
| Urban | 2742 | 39.58 | ||
| Rural | 4186 | 60.42 | ||
| Mean | Std Dev | min | max | |
| Child’s age in months | 16.82 | 10.09 | 0 | 36 |
Table A2.
Association between malnutrition and sociodemographic characteristics
| |
Stunted |
Wasted |
|---|---|---|
| (1) | (2) | |
| Education (comparison: No education) | ||
| Incomplete primary | 0.926 | 0.980 |
| [0.640,1.341] | [0.539,1.780] | |
| Complete primary | 0.749 | 0.677 |
| [0.561,1.000] | [0.427,1.072] | |
| Incomplete secondary | 0.646* | 0.725 |
| [0.471,0.886] | [0.433,1.214] | |
| Complete secondary | 0.577* | 0.802 |
| [0.428,0.777] | [0.491,1.309] | |
| Higher | 0.320* | 0.610 |
| [0.198,0.518] | [0.314,1.184] | |
| Child’s age in months | 1.079* | 0.971* |
| [1.070,1.088] | [0.960,0.982] | |
| Wealth (comparison: poorest) | ||
| Poorer | 0.970 | 0.742 |
| [0.747,1.259] | [0.497,1.106] | |
| Middle | 0.982 | 0.743 |
| [0.703,1.372] | [0.446,1.237] | |
| Richer | 0.729 | 0.673 |
| [0.490,1.083] | [0.363,1.249] | |
| Richest | 0.547* | 0.451* |
| [0.333,0.901] | [0.208,0.978] | |
| Residence (comparison: urban) | ||
| Rural | 0.663 | 0.766* |
| [0.395,1.113] | [0.592,0.989] | |
| N | 5373 | 2788 |
| Cluster FE | Yes | Yes |
*Significant at 5%
Table A3.
Association between vaccination and sociodemographic characteristics
| |
BCG |
DPT/Penta1 |
DPT/Penta3 |
Measles1 |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Education (comparison: No education) | ||||
| Incomplete primary | 1.566* | 1.367 | 1.115 | 1.327 |
| [1.021,2.401] | [0.864,2.162] | [0.741,1.678] | [0.789,2.234] | |
| Complete primary | 1.874* | 1.736* | 1.581* | 1.434 |
| [1.335,2.630] | [1.269,2.376] | [1.149,2.177] | [1.000,2.058] | |
| Incomplete secondary | 2.294* | 2.435* | 2.385* | 1.913* |
| [1.574,3.344] | [1.724,3.440] | [1.739,3.270] | [1.326,2.759] | |
| Complete secondary | 4.065* | 2.896* | 3.291* | 2.367* |
| [2.786,5.931] | [2.075,4.043] | [2.408,4.498] | [1.669,3.357] | |
| Higher | 10.721* | 6.363* | 5.066* | 3.122* |
| [5.246,21.912] | [3.787,10.691] | [3.265,7.860] | [2.058,4.736] | |
| Child’s age in months | 1.015* | 1.046* | 1.066* | 1.164* |
| [1.006,1.024] | [1.036,1.055] | [1.057,1.075] | [1.151,1.177] | |
| Wealth (comparison: poorest) | ||||
| Poorer | 0.924 | 0.999 | 0.769 | 1.044 |
| [0.676,1.261] | [0.725,1.379] | [0.540,1.097] | [0.734,1.486] | |
| Middle | 1.102 | 1.131 | 0.940 | 1.109 |
| [0.720,1.685] | [0.757,1.689] | [0.627,1.410] | [0.733,1.679] | |
| Richer | 1.602 | 1.391 | 1.301 | 1.570 |
| [0.973,2.637] | [0.880,2.199] | [0.827,2.048] | [0.980,2.515] | |
| Richest | 1.787 | 1.804* | 1.520 | 2.406* |
| [0.887,3.597] | [1.014,3.207] | [0.903,2.559] | [1.394,4.153] | |
| Residence (comparison: urban) | ||||
| Rural | 1.082 | 2.241* | 1.633* | 0.707* |
| [0.714,1.639] | [1.776,2.827] | [1.212,2.202] | [0.605,0.827] | |
| N | 3834 | 4490 | 4953 | 5601 |
| Cluster FE | Yes | Yes | Yes | Yes |
*Significant at 5%.
Disclosure statement
The author declares no conflict of interest.
References
- 1.Orenstein WA, Ahmed R.. Simply put: vaccination saves lives. Proceedings of the National Academy of Sciences of the United States of America. 2017;114(16):4031–33. 10.1073/pnas.1704507114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katona P, Katona-Apte J. The interaction between nutrition and infection. Clin Infect Dis. 2008;46(10):1582–88. doi: 10.1086/587658. [DOI] [PubMed] [Google Scholar]
- 3.Prendergast AJ. Malnutrition and vaccination in developing countries. Philosophical Trans Royal Soc B: Biol Sci. 2015;370(1671):20140141. doi: 10.1098/rstb.2014.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solis-Soto MT, Paudel D, Nicoli F. Relationship between vaccination and nutritional status in children: analysis of recent demographic and health surveys. Demogr Res. 2020;42:1–14. doi: 10.4054/DemRes.2020.42.1. [DOI] [Google Scholar]
- 5.Rodrigues A, Fischer TK, Valentiner-Branth P, Nielsen J, Steinsland H, Perch M, Garly ML, Molbak K, Aaby P. Community cohort study of rotavirus and other enteropathogens: are routine vaccinations associated with sex-differential incidence rates? Vaccine. 2006;24(22):4737‒4746. doi: 10.1016/j.vaccine.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 6.Sorup S, Benn CS, Poulsen A, Krause TG, Aaby P, Ravn H. Live vaccine against measles, mumps, and rubella and the risk of hospital admissions for nontargeted infections. JAMA. 2014;311(8):826‒835. doi: 10.1001/jama.2014.470. [DOI] [PubMed] [Google Scholar]
- 7.National Population Commission (NPC) [Nigeria] and ICF . Nigeria demographic and health survey 2018. Abuja (Nigeria, and Rockville, Maryland, USA): NPC and ICF; 2019. [Google Scholar]
- 8.World Health Organization . Immunization coverage. [accessed 10 Dec 2020]. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage#:~:text=During%202019%2C%20about%2085%25%20of,90%25%20coverage%20of%20DTP3%20vaccine
- 9.Nigeria National Bureau of Statistics. National Nutrition and Health Survey (NNHA) 2018: Report on the Nutrition and Health Situation of Nigeria; 2018.
- 10.UNICEF . Immunization; 2019. [accessed 10 Dec 2020]. https://data.unicef.org/topic/child-health/immunization/
- 11.WHO and UNICEF estimates of national immunization coverage . Revision; [accessed 10 Dec 2020]. https://www.who.int/immunization/monitoring_surveillance/data/nga.pdf
- 12.Schaible UE, Stefan HE. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4(5):e115. 320 doi: 10.1371/journal.pmed.0040115. [DOI] [PMC free article] [PubMed]
- 13.Ophori EA, Tula MY, Azih AV, Okojie R, Ikpo PE. Current trends of immunization in Nigeria: prospect and challenges. Trop Med Health. 2014;42(2):67–75. doi: 10.2149/tmh.2013-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berendsen MLT, Smits J, Netea MG, van der Ven A. Non-specific effects of vaccines and stunting: timing may be essential. EBioMedicine. 2016;8:341–48. doi: 10.1016/j.ebiom.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Bank. Immunization, measles (% of children aged 12-23 months); 2018. [accessed 10 Dec 2020]. https://data.worldbank.org/indicator/SH.IMM.MEAS


