Abstract
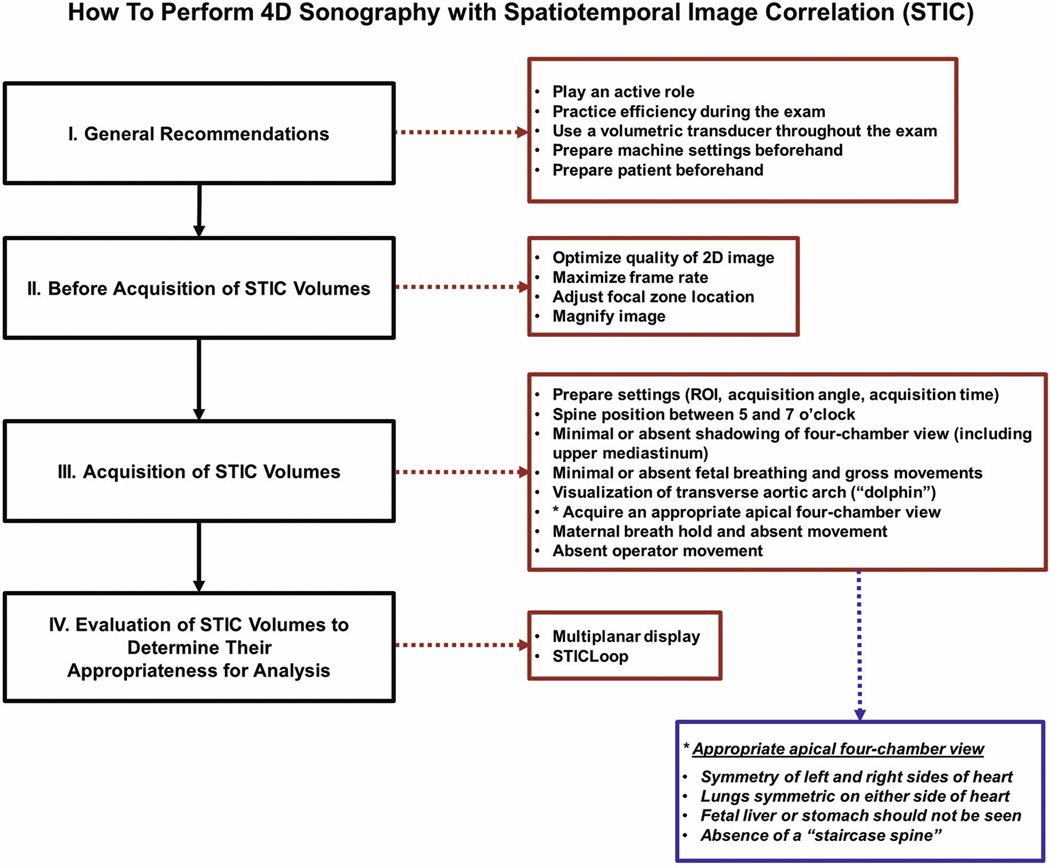
The effective performance of fetal cardiac examination using spatiotemporal image correlation (STIC) technology requires two essential steps – volume acquisition and post-processing. An important prerequisite is training sonologists to acquire high-quality volume datasets so that, when analyzed, such volumes are informative. This article is Part 2 of a series on four-dimensional (4D) sonography with STIC. Part 1 focused on STIC technology and its features, the importance of operator training/experience, and acquisition of high-quality STIC volumes, factors that affect STIC volume acquisition rates, and general recommendations on performing 4D sonography with STIC. In Part 2, we discuss a detailed and practical step-wise approach for STIC volume acquisition, along with methods to determine whether such volumes are appropriate for analysis.
Keywords: fetal echocardiography, fetus, four-dimensional (4D), spatiotemporal image correlation (STIC), STICLoop, ultrasound
Introduction/Summary
The effective performance of fetal cardiac examination using spatiotemporal image correlation (STIC) technology requires two essential steps – volume acquisition and post-processing. An important prerequisite is training sonologists to acquire high-quality volume datasets so that, when analyzed, such volumes are informative (e.g. allow the successful display of cardiac views and anatomic structures).
This article is Part 2 of a two-part series on four-dimensional (4D) sonography with STIC. Part 1 focused on STIC technology and its features, the importance of operator training/experience, and acquisition of high-quality STIC volumes, factors that affect STIC volume acquisition rates, and general recommendations on performing 4D sonography with STIC.1 In Part 2 herein, we discuss a detailed and practical step-wise approach for STIC volume acquisition, along with methods to determine whether such volumes are appropriate for analysis.
How to Perform 4D Sonography with STIC
Four-dimensional sonography with STIC technology allows the acquisition of a fetal cardiac volume dataset and visualization of cardiac structures as a cine loop of a complete single cardiac cycle in motion.2–5 Such technology is readily available across many ultrasound platforms and is integrated into the system’s basic software option. Once STIC has been activated, the array within the transducer housing begins an automatic single sweep over the region of interest (ROI).3,6 The STIC volume display is thus composed of thousands of two-dimensional (2D) images acquired through this area of interest during the sweep. Once the image data have been analyzed according to their spatial and temporal domains (hence, the term spatiotemporal image correlation), the dynamic image sequence can be displayed as a multiplanar view, single plane, and/or rendered image.3 The end result is that STIC volume datasets contain all the necessary information for an adequate examination of the fetal heart, having an unlimited number of cardiac images available for review in any plane and orientation. This fact is relevant, since the standard fetal cardiac views recommended by professional organizations7–10 for prenatal diagnosis can be generated.
A solid body of evidence suggests that 4D sonography with STIC facilitates examination of the fetal heart,3,4,5,11–37 and may also be used to evaluate fetal cardiac function.18,22,27,30,31,33,38–46 This modality has also been used in the prenatal evaluation and diagnosis of congenital heart disease (CHD),2,20,47–71 because it improves the ability to identify complex intracardiac relationships and can shorten the examination time.3,17,72 These facts are important, since evaluation of the normal and abnormal fetal heart73–75 using 2D ultrasound is one of the most challenging tasks in prenatal diagnosis. Indeed, structural cardiac abnormalities are among the major malformations that are most frequently missed on prenatal sonographic examinations.76–78 STIC technology also has the potential to reduce the operator dependency associated with 2D sonography. This aspect is relevant, since the most important factor affecting the prenatal detection of CHD is operator skill and expertise,79–85 in which mental reconstruction of a sequence of individual cross-sectional images is required.86
Three main time points deserve focus when acquiring STIC volume datasets and determining their appropriateness for analysis:1 1) before acquisition of STIC volumes; 2) acquisition of STIC volumes; and 3) immediately after acquisition of STIC volumes (i.e. multiplanar display and/or STICLoop87).
Before obtaining STIC volume datasets, it is essential to enhance the overall sonographic image. This can be accomplished through the following steps.
Before the Acquisition of STIC Volumes
1. Optimize the quality of the 2D image:
An important concept is that the image quality of STIC volume datasets depends primarily on the original quality of the 2D image, along with prior adjustments in grayscale (and color Doppler, if used) parameters.88 Thus, if the 2D image quality is suboptimal (e.g. poor resolution due to maternal habitus or acoustic shadowing), it will also generally be the case for the STIC volume dataset.89 The goal is to enhance the temporal and spatial resolution of the volume by highly optimizing 2D images prior to the acquisition. Settings should be adjusted to obtain clear visualization of the fetal heart, an image that is neither too bright nor dark, and one that is characterized by increased contrast and high resolution.9 Ultrasound platforms frequently have settings specifically designed for fetal cardiac examination. Thus, the operator can choose this setting initially and then make adjustments based on preference. Some have reported that highly optimized 2D image resolution (required to obtain proper STIC volume reconstruction) improves with sonographer experience.90
2. Maximize the frame rate:
A high frame rate leads to a STIC volume dataset with improved quality, since there will be more frames within such volume. This goal can be accomplished by decreasing three parameters: 1) depth, so that there is less depth below the fetal heart in the imaging window; 2) sector width (or viewing angle) around the heart, so that other irrelevant structures are not in the field of view; and 3) number of focal zones, so that there is a single zone. How does imaging depth affect temporal resolution? Shallow imaging increases the frame rate and improves temporal resolution, whereas deeper imaging decreases the frame rate and degrades temporal resolution.91 Thus, an inverse relationship exists between imaging depth and frame rate. When the sector width is narrowed, the number of pulses required to make an image decreases, and there is increased temporal resolution along with a higher frame rate.91 The number of focal zones also influences the frame rate. The focal zone is a region around the focus where the beam is relatively narrow and where image detail is superior.91 With single-focus imaging, only one sound pulse is transmitted down each scan line, which results in superior temporal resolution and a higher frame rate.
3. Adjust the focal zone location:
Besides the number of focal zones, the location also influences the sonographic image. Reflections that arise from the focal zone create images that are more accurate than those from other depths. 19 Thus, the single focal zone should be placed at, or below, the level of the fetal heart in the imaging window.
4. Magnify the image:
Magnification of the fetal heart should be performed before STIC volume acquisition to improve visualization of cardiac anatomy. However, it is noteworthy that the image should not be magnified so much, that the entire four-chamber view and fetal chest are not visualized fully on the monitor screen.
Acquisition of STIC Volumes
When obtaining STIC volume datasets, it is important to: 1) prepare the acquisition settings (e.g. acquisition angle); 2) follow pre-set criteria; 3) obtain an appropriate apical four-chamber view; and 4) recognize when to discard volumes and when volumes should not be obtained. We will now review each of these steps in detail.
1. Prepare the acquisition settings (i.e. ROI, acquisition angle, acquisition time):
Besides frame rate, the quality of a STIC volume dataset also depends on the acquisition angle and acquisition time.5 The more images that are stored per acquisition period, the greater the number available for volume reconstruction, and the better the image resolution. In other words, the longer the sweep or acquisition time, the greater the number of frames collected for the STIC volume dataset, and the better the spatial resolution. Acquisition settings that should be adjusted include the ROI, acquisition angle, and acquisition time.
a. Region of interest:
The ROI box determines the height (y-plane) and width (x-plane) of the STIC volume dataset (Figure 1, Video clip 1). Contrary to what one may think, a large and/or wide ROI is associated with lower frame rates that may negatively impact the temporal resolution and quality of the volume. Thus, adjusting the ROI box size to be as small as possible will maximize the frame rate during acquisition and also improve the temporal resolution of the volume dataset.88 The box should be adjusted to encompass the entire fetal chest circumference so that it contains all the anatomical information of the fetal heart (Figure 1, Video clip 1). Moreover, the heart should occupy the maximum proportion of the image to be acquired. It is important during the actual sweep by the transducer array to observe on the monitor screen the sequential images within the ROI box. By doing so, it will be apparent whether either the size or location of the ROI box is inappropriate.
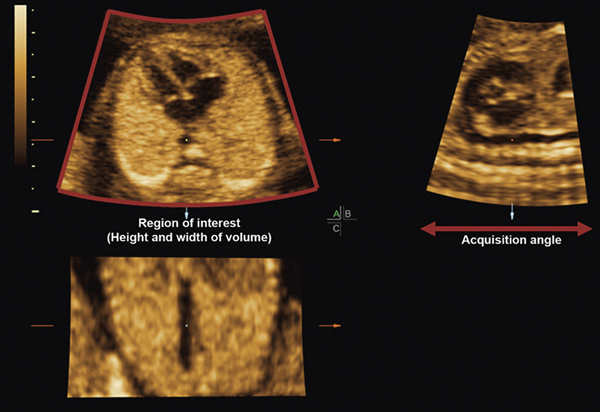
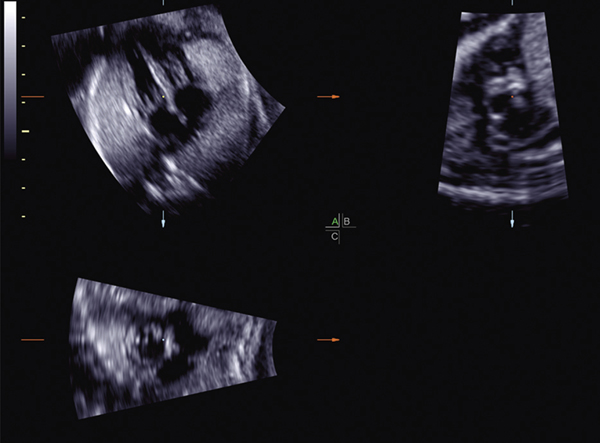
Figure 1:
Multiplanar display of a STIC volume (normal fetal heart). The ROI box around the acquisition plane (apical four-chamber view) determines the height (y-plane) and width (x-plane) of the volume. Note that the box encompasses the entire fetal chest circumference. The B plane (sagittal image; upper right corner) demonstrates the acquisition angle of the volume, which determines the acquisition depth. Since the reference dot has been placed in the cross-section of the descending aorta in the A plane, the longitudinal descending aorta is visible in both the B and C planes.
ROI, region of interest; STIC, spatiotemporal image correlation.
b. Acquisition angle:
The acquisition angle (e.g. 15°– 60°) determines the acquisition depth (i.e. amount of information acquired in the z-plane) (Figure 1, Video clip 1). Thus, a smaller acquisition angle is equivalent to a shorter distance covered during the sweep. The angle should be selected by the sonologist before STIC volume acquisition, and the goal is to encompass all the anatomical structures of interest. For example, when volume acquisitions are performed in the transverse plane of the fetal heart, the upper mediastinum through the upper abdomen/stomach of the fetus should ideally be included in the volume dataset.2 This process ensures that all standard transverse planes (e.g. three-vessel view) are available for assessment.
The acquisition plane is defined as the starting 2D plane for a volume acquisition (Figure 1, Video clip 1). Once the acquisition plane (e.g. apical four-chamber view) has been obtained and the acquisition angle is selected by the sonologist (e.g. 15°), the STIC volume dataset is initially created by a mechanical sweeping of the beam 7.5° from such acquisition plane. The acquisition process then begins, coming back toward the acquisition plane and then continuing for another 7.5° to create a total volume of information of 15°. Therefore, a total sweep of 15° cranial and caudal to the apical four-chamber view is obtained, in which the acquisition plane is located in the middle of the sweep box.
How does one determine the appropriate acquisition angle for the STIC volume dataset? The angle should always be adjusted, depending on whether there is a smaller or larger fetal size. A useful rule of thumb is to set the acquisition angle at least 5° more than the gestational age (e.g. at 30 weeks of gestation, the angle could be set at 35°). An earlier gestational age will therefore require a narrower angle. It is also essential that one not obtain too wide of an acquisition angle, believing that “more is better,” because for a selected acquisition time, the image resolution of the B and C planes in the multiplanar display (see description of these planes later) will actually be lower when the angle is 40° (vs. 15°).92 Moreover, when the volume sweep angle is larger than the structure(s) being examined, this leads to: 1) redundant information being included within the volume; 2) decreased volume resolution; and 3) an increased chance of artifacts being introduced (e.g. fetal movements). Therefore, it is desirable to set the minimum acquisition angle that will include only the area(s) of interest. Doing so will reduce artifacts and optimize volume quality.26 On the other hand, if an acquisition angle is too narrow, the anatomical structures(s) may not be included within the volume dataset at all, and it becomes uninformative. Viñals et al.2 obtained standard fetal cardiac planes by scrolling through STIC volume datasets from the upper abdomen to the mediastinum. However, low visualization rates were observed for structures located in the mediastinal or abdominal areas. These results were attributed to a lack of operator experience, for which the acquisition angle was not set wide enough to include such structures.2
How can one determine whether the appropriate acquisition angle for the STIC volume has been set? During the actual volume sweep, it is necessary to observe the images on the monitor screen to determine whether the structure(s) of interest have been included. For a four-chamber view acquisition plane, the sonologist should evaluate whether the fetal upper mediastinum (start of the sweep), and the stomach (end of the sweep) are visible on the screen (Video clip 2). If neither of the views have been included (i.e. angle of acquisition too narrow), the STIC volume can be immediately discarded, and for subsequent acquisitions, the acquisition angle should be increased. On the other hand, if one observes planes that are inferior to the stomach during the acquisition sweep, the acquisition angle is probably too wide, and it should be decreased for future acquisitions. Once the STIC volume has been obtained, one can also evaluate the multiplanar display to determine whether the acquisition angle was appropriate (also see “Acquisition angle in B plane” later) (Figure 1, Video clip 1).
c. Acquisition time:
The acquisition time (or duration of acquisition) determines the speed at which the transducer sweeps the ROI. An inverse relationship exists between the acquisition time and sweep speed. Therefore, the shorter the acquisition time (e.g. 7.5 seconds), the faster is the sweep speed of the transducer. All ultrasound platforms allow the operator to select the volume acquisition speed, and the acquisition times generally range from 5 to 15 seconds in duration.
For a fixed acquisition angle (e.g. 30°), the number of acquired frames will increase as the duration of the acquisition time goes up.92 Thus, the quality of a STIC volume acquisition is essentially reflected by the acquisition time.26 It is desirable to obtain volumes containing the greatest possible number of 2D images from which the dataset will be constructed. With increasing STIC acquisition times (e.g. 15 seconds) or a slower sweep speed, the image resolution of the B and C planes in the multiplanar display will be higher. Conversely, with decreasing acquisition times (e.g. 7 seconds) or a faster sweep speed, the image resolution in the B and C planes will be lower.
Therefore, STIC volumes should be obtained using the longest possible acquisition time. Some women, however, may have difficulty holding their breath for 15 seconds. Moreover, there is a higher likelihood that artifacts related to fetal motion or breathing may be introduced into the volume dataset, thus compromising quality.40 In our experience, since most women can hold their breath without difficulty for a duration of 10 to 12.5 seconds during the STIC acquisition, we recommend setting the acquisition time for at least 10 seconds. However, when fetuses are very active (e.g. movements), there may be no choice but to set the shortest possible acquisition time to minimize motion artifacts, recognizing that this set time will be at the expense of optimal spatial resolution.
Taken together, the goal is to identify an acquisition time (or sweep speed) that will optimize image resolution but not allow the introduction of artifacts (e.g. fetal breathing or movements) into the B and C planes, which can occur if the sweep speed is too slow. Typically, we preset the time for 10 to 12.5 seconds, and then adjust it according to the presence/absence of fetal breathing or movements.
A recent development is the introduction of an electronic matrix 4D probe that allows up to a 75% reduction in STIC acquisition time, along with improved resolution in the B and C planes.93 High-resolution sub-volumes are acquired, in which each sub-volume contains a portion of the fetal heart. The system analyzes each sub-volume and combines them to display the entire fetal heart for a full cardiac cycle. With sub-volume acquisitions, the A and B plane line densities are tuned pair-wise to have similar image quality.93 Therefore, due to the marked reduction in the acquisition time and improved image resolution in the B and C planes, the electronic matrix probe may prove to be useful when performing 4D sonography with STIC.
2. Spine position between 5 and 7 o’clock:
To assess cardiac views from a STIC volume dataset, the fetal spine ideally should be positioned between 5 and 7 o’clock (i.e. an apical four-chamber view) (Figure 2) because this reduces the possibility of acoustic shadowing from the ribs or spine. Such shadowing can obscure visualization of cardiac structures (Video clip 3) and is more likely to occur if the fetal spine is located at other clock “times” (e.g. between 11 and 1 o’clock). Indeed, a fetus with the spine located in an anterior position (i.e. “back up”) has been associated with a significantly lower probability (by 72%) that cardiac views (four chamber and left and right ventricular outflow tracts) would be regarded as satisfactory for screening.25 It should be noted, however, that high-quality STIC volumes can still be obtained when the fetal spine position is outside the recommended 5-to-7 o’clock times (e.g. 4 o’clock).
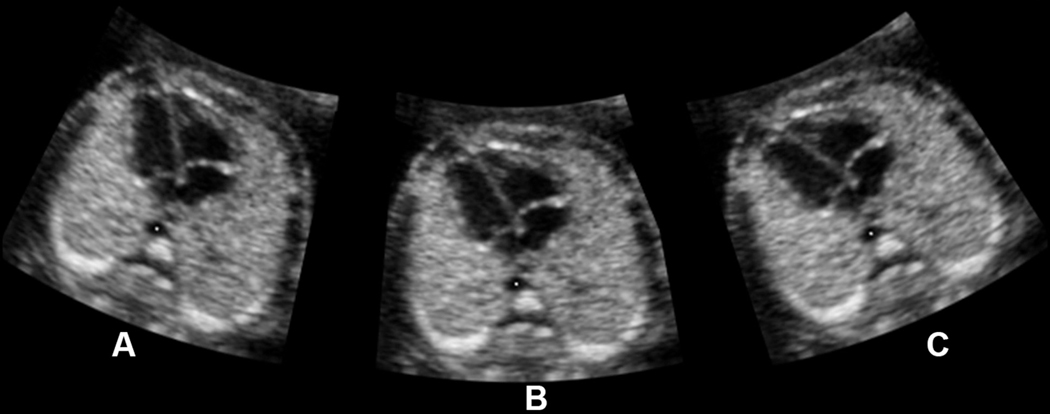
Figure 2:
Apical four-chamber view with the fetal spine positioned at different locations: A) 7 o’clock; B) 6 o’clock; C) 5 o’clock. Such positions reduce the possibility of acoustic shadowing from the fetal ribs or spine.
An interesting concept is whether it is possible to “change” the fetal spine position so that the location appears more optimal on the monitor screen. Effective methods that can actually alter the true fetal spine position include asking the supine mother to turn (or roll) laterally onto her side (e.g. “clockwise roll”) in the same direction that you desire the fetal cardiac apex to turn (see Part 1 of this series for further explanation1). Other options include gently “moving” the fetus into the desired position by placing one’s hands on the maternal abdomen or having the patient sit up/ambulate for a brief period. Extra time can also be allowed during the sonographic examination so that the fetus changes to a more optimal position.
a. Driving the Transducer:
A technique that we have found to be effective in “converting” the fetal spine to a posterior position on the monitor screen is what we term “driving the transducer” (Figures 3 and 4, Video clips 4 and 5). The fetus itself does not change position but, rather, the transducer (and, thus, its beam) is “driven” on the maternal abdomen so that it comes to lie above the anterior (vs. lateral) fetal chest.
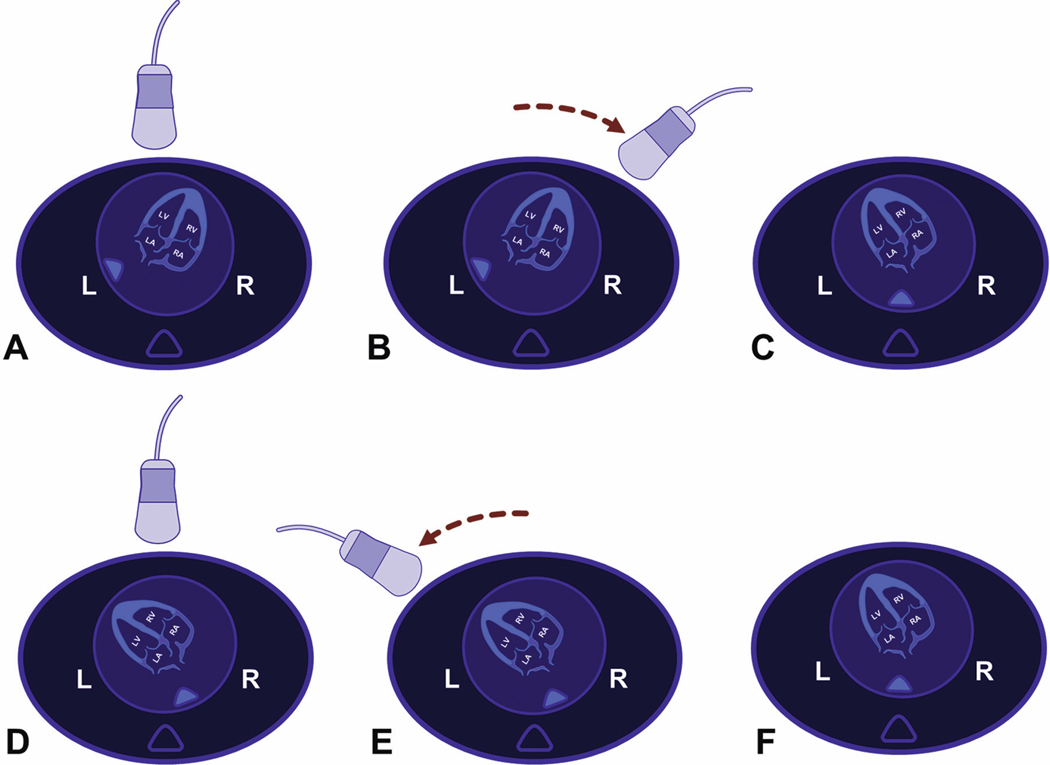
Figure 3:
“Driving the transducer” technique in a vertex fetus. A) Spine originally located at 8 o’clock in the apical four-chamber view; B) the transducer is driven on the maternal abdomen (toward the fetal right side) in a fixed arc until it lies above the cardiac apex; C) on the monitor screen, the fetal spine has “converted” to a more posterior position (6 o’clock), and the cardiac apex is now “up”; D) spine located at 5 o’clock in the apical four-chamber view; E) the transducer is driven leftward on the maternal abdomen (toward the fetal left side) in a fixed arc until it lies above the cardiac apex; F) on the monitor screen, the fetal spine has “converted” to a more posterior position (6 o’clock), and the cardiac apex is now “up.”
L, fetal left; R, fetal right.
Figure 4:
“Driving the transducer” technique in a breech fetus: A) Spine originally located at 8 o’clock in the subcostal four-chamber view. The transducer is driven on the maternal abdomen (to operator’s right, toward the fetal left side) in a fixed arc until it lies above the cardiac apex; B) on the monitor screen, the fetal spine has “converted” to a 6 o’clock position, and the apical four-chamber view is visible.
To accomplish this technique, one should take advantage of the entire maternal abdominal field by moving the transducer in different locations on the abdomen, even near the flanks. Such a technique is based on the following principle: when steering a car with one hand, the driver fixes his or her hand on the steering wheel and can only rotate the wheel to the right or left direction in a fixed arc. Even if one twists the hand while on the steering wheel, this action cannot change the fixed arc, since steering wheels are rigid and stationary in place. Similarly, one can “drive” or steer the transducer in a fixed arc around the transverse fetal chest (from one side to the other) by moving the transducer across the maternal abdomen (typically from one flank to the other). In this technique, the four-chamber view can be thought of as the center of a steering wheel. Essentially, the objective is to always move the probe on the maternal abdomen so that it comes to lie above the anterior fetal chest, leading the spine to be more posteriorly located on the screen and the cardiac apex to be “up” (Figures 3 and 4).
The steps to be performed are the following. Once the four-chamber view has been identified on the monitor screen, the sonologist should hold the transducer (i.e. steering wheel) in a fixed manner without twisting the hand. Next, one should “drive” the probe in a fixed arc either to the operator’s right or left (maternal left or right, respectively, if the patient faces the operator) until it lies above the anterior fetal chest, always keeping the four-chamber view on the screen. If one “drives” with the probe but twists the hand at the same time, the four-chamber view will no longer be visualized on the screen but, rather, a different cardiac plane (e.g. left ventricular outflow tract). Therefore, it is essential that the “driving” movements of the transducer should simulate that of rotating a steering wheel in a fixed arc to the operator’s right or left side. If such technique is done correctly, often the fetal spine in the four-chamber view will “convert” to a more posterior position on the monitor screen, and the cardiac apex will be “up” (Figures 3 and 4, Video clips 4 and 5).
Although the method is not complicated, we have found that it may be difficult for beginners to learn how to “drive” with the transducer because: 1) random (vs. targeted) scanning movements are made with the probe; 2) the entire maternal abdominal field is not scanned; and 3) twisting of the hand occurs during the sonographic examination. Therefore, driving the transducer initially requires some practice.
Since complete rotation of a STIC volume dataset around a 360° axis is manually possible using software,1 a question often asked is why a given STIC volume cannot just be rotated so that the fetal spine location is between 5 and 7 o’clock. There are two issues that arise from this action. First, simply rotating a STIC volume on the z-axis (i.e. rotating clockwise or counter-clockwise) can never “erase” acoustic shadowing, dropout, or artifacts already contained within the dataset. It is not possible to do this once a STIC volume has been acquired. The second issue is that when the acquisition plane is rotated on the z-axis (e.g. four-chamber view with the spine located at 4 o’clock now rotated to 6 o’clock), it alters the normal aspect of the image in terms of ultrasound-wave reflection and refraction.94 As a result, the B-plane image in the multiplanar view becomes more blurred or “waxy,” and the image clarity/quality diminishes (Figure 5, Video clip 6). It is worth repeating that any movement or rotational changes to the acquisition plane image will also lead to respective changes in the images of the B and C planes.1
Figure 5:
STIC volume acquired from the subcostal four-chamber view, in which the spine was originally located at 4 o’clock. The acquisition plane (A plane) has been manually rotated on the z-axis so that the spine location is at 6 o’clock. As a result, the B plane image (ductal arch) becomes more blurred or “waxy” in appearance with diminished image clarity.
STIC, spatiotemporal image correlation.
3. Minimal or absent shadowing of four-chamber view (including the upper mediastinum):
Acoustic shadowing is defined as signal loss in the sound path secondary to echogenic structures, while acoustic dropout is defined as signal loss in the sound path without intervening structures.30 When acquiring STIC volume datasets, it is important that there is minimal or absent acoustic shadowing/dropout in the ROI. In addition to clear visualization of the four-chamber view acquisition plane within the ROI, the same applies to the upper fetal mediastinum (Video clip 7). If acoustic shadowing or dropout is present, it may obscure visualization of the cardiac anatomy and structures in STIC reconstruction.
Even when the fetal spine is ideally positioned between 5 and 7 o’clock, acoustic shadowing or dropout may still occur secondary to the fetal extremities, fetal ribs or sternum, an anterior placenta, co-twin, maternal umbilicus, and maternal abdominal scarring. Therefore, to avoid these issues, it may be necessary to move the transducer to different locations on the maternal abdomen, adjust the rotational position or tilt of the transducer, or wait for fetal parts to move out of the field of view.
4. Minimal or absent fetal breathing and gross movements:
Ideally, there should be minimal-to-absent fetal breathing and gross movements during the STIC acquisition. All such conditions can lead to motion artifacts within the volume dataset, with distortion of images and anatomical structures (Figure 6, Video clip 8) (also see “wavy lasagna wall” later). Indeed, STIC motion artifacts have interfered with the evaluation of anatomic relationships between great vessels and cardiac chambers, leading to an incorrect diagnosis.95 Therefore, it is prudent to acquire multiple STIC volumes when CHD is suspected to avoid misdiagnosis.89 The presence of fetal hiccups (regular or irregular) will also lead to motion artifacts within the STIC volume dataset (see “piano keys” later).
Figure 6:
During the STIC volume acquisition, fetal breathing occurred at the beginning, leading to a motion artifact in the area of the upper mediastinum. As a result, there is distortion of the 3-vessel and trachea view, as evidenced in the acquisition plane (upper left corner). Note that the pulmonary artery and ductus arteriosus (ductal arch view, B plane) appears distorted, and the anatomy cannot be assessed with confidence.
STIC, spatiotemporal image correlation.
Thus, one should attempt to obtain STIC volumes when fetal breathing and gross movements are absent or have subsided. In a few cases, it will be impossible, and the following points are noteworthy. When fetal breathing/movements occur during the acquisition, their degree (mild or intense), frequency (regular or irregular), and location (relative to fetal anatomy) will cause orthogonal planes to range from being minimally altered to completely uninterpretable. Specifically: 1) minimal and occasional fetal breathing/gross movements may not affect image resolution; 2) regular and intense fetal breathing/movements throughout the STIC volume acquisition will lead to an uninterpretable and distorted image (see “wavy lasagna wall” later). Moreover, the fetal heart rate depicted on the monitor screen immediately after the acquisition is completed will usually be abnormal; and 3) if fetal breathing/movements occur in certain anatomical areas of interest (e.g. upper mediastinum; Figure 6 and Video clip 8), the volume will be uninformative and, thus, unacceptable. However, if such movements occur only in the area of the fetal abdomen (Video clip 9), the cardiac planes may still be very informative.
Taken together, it seems that a major limitation of STIC technology is the requirement to obtain volumes in a quiescent fetus lying supine. However, multiple investigators have shown how this condition can easily be met during routine sonographic examinations.5,17,19
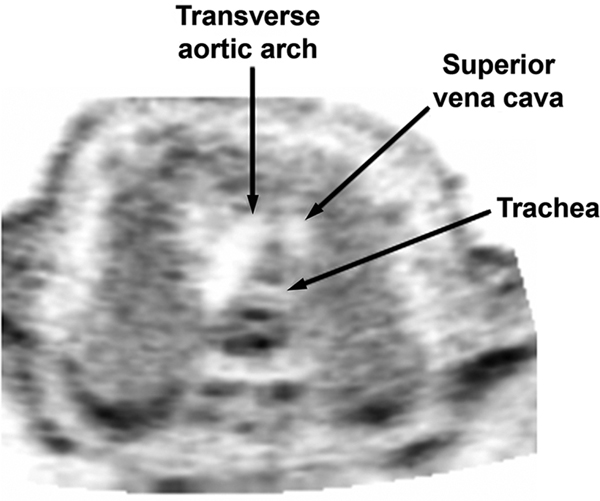
5. Visualization of transverse aortic arch (“dolphin”):
Just immediately before beginning a STIC acquisition of the four-chamber view, the transducer should be tilted or rocked slightly to ensure that the transverse aortic arch (“dolphin”) is clearly visible in the upper fetal mediastinum (Figure 7, Video clip 10). Confirming visibility of the transverse aortic arch maximizes the chances that it will also be discernible in later volume reconstruction. If the transverse aortic arch is not evident, the transducer should be repositioned and/or tilted on the maternal abdomen until the four-chamber view and “dolphin” are clearly visualized. This process may require “driving” the transducer in a fixed arc around the transverse fetal chest (see above). The transverse aortic arch may not be clearly visible due to acoustic shadowing from the fetal sternum or extremities or because there is a cardiac abnormality (e.g. coarctation of the aorta).
Figure 7:
Transverse view of the fetal upper mediastinum, demonstrating the transverse aortic arch (“dolphin”), cross-section of the superior vena cava, and cross-section of the trachea. Just immediately before beginning a STIC volume acquisition of the four-chamber view, one should tilt the transducer to ensure that the transverse aortic arch is also clearly visualized.
STIC, spatiotemporal image correlation.
6. Four-chamber view as the acquisition plane:
In most cases, the starting 2D plane for the STIC volume acquisition (i.e. acquisition plane) will be the four-chamber view (vs. the five-chamber view, for example) for several reasons. First, the four-chamber view is best suited as the reference plane to evaluate transverse cardiac views, which include the cardiac chambers, origin of the great vessels, three-vessel view, and three-vessel and trachea view (3VT).26 Although optimal evaluation of the aortic arch, ductal arch, and venous connections is best achieved through a sagittal STIC volume acquisition of the fetal chest,4,35 such structures can also be successfully obtained from a transverse sweep through the fetal chest.16,29,34,87,96–98 Second, the sonographic plane most easily obtained in the fetal heart is the four-chamber view.99 Indeed, such a view can be obtained in 95% to 98% of fetuses in a non-selected population during the second trimester.100–102 Moreover, in a study of three-dimensional (3D) sonographic evaluation of the fetal heart, the four-chamber view acquisition plane was most-often obtained (93%) and was also the most valuable, since it yielded the maximum number of cardiac views.103 Finally, Turan et al.90 reported that optimal imaging of the four-chamber view in the first trimester (e.g. at STIC volume acquisition) was the cornerstone for identifying CHD.
Through proper training, all sonologists should be able to obtain an appropriate STIC volume dataset, which is acquired from the four-chamber view. Yet, it is noteworthy that acquiring an apical four-chamber view per se is not enough – it should also be the correct (or appropriate) four-chamber view (i.e. true cross-section of the thorax with proper alignment in the axial plane).29 We will now review how this view can be achieved.
7. How to acquire an appropriate apical four-chamber view:
The four-chamber view is imaged through a transverse section of the fetal thorax. Once a true axial plane of the apical four-chamber view is achieved (Figure 8, Video clip 11), a STIC volume can be obtained. This process may seem like fairly straightforward (i.e. depicting four cardiac chambers is not difficult); however, the key is insonating the fetal heart so that the correct four-chamber view appears. It is well known that the appearance of the four cardiac chambers can vary, depending on the orientation of the ultrasound beam to the heart.104 Therefore, proper orientation of the transducer is essential. Indeed, investigators have noted that it is easy to obtain an improper plane of the four-chamber view since the ultrasound beam may be tilted, resulting in asymmetry of both sides of the fetal heart.105 Thus, many sonologists technically obtain a “four-chamber view,” but one that is characterized by improper alignment in the axial plane as well as the azimuth. In this situation, for example, the size of the fetal lungs will appear asymmetric on either side of the heart, or a portion of the liver may be visualized in the four-chamber view plane. In our experience, sonologists tend to foreshorten the left (vs. right) side of the fetal heart when imaging the apical four-chamber view and, as a result, the left atrium and ventricle will appear “cut-off” compared to the right side (Video clip 12).
Figure 8:
Transverse section of the fetal thorax demonstrating a true axial plane of the apical four-chamber view (vertex presentation). Note that the size of the fetal lungs is symmetrical, and the left atrium and ventricle are not foreshortened in this insonation.
Why is obtaining the appropriate apical four-chamber view important in STIC volume acquisition? There are several reasons. First, if there is improper alignment in the axial plane and the presence of azimuth, the operator will need to manually navigate and manipulate the STIC volume dataset to “correct” the four-chamber view. Manual navigation106 is accomplished by using controls to interrogate the three orthogonal planes in the multiplanar display, which can be challenging, cumbersome, and time-consuming. An inexperienced sonologist may have difficulty manipulating the STIC volume dataset to obtain the proper acquisition plane (in this case, the apical four-chamber view). Therefore, it is likely to be easier obtaining the appropriate apical four-chamber view at the time of STIC acquisition (i.e. real-time sonography) than via manual navigation of the multiplanar display.
Second, failing to begin the STIC acquisition from the correct transverse plane of the four-chamber view leads to incomplete acquisition of fetal cardiac structures and/or views toward the far ends of the automatic sweep.55 This situation occurs because the acquisition axis does not coincide with the fetal body axis.55 Others also recommend that sonologists identify a perfect four-chamber view at the time of STIC volume acquisition.107 The reason is that when the exact four-chamber view is the initial plane before scrolling inside the STIC volume (“cardiac-based technique”), there are higher success rates of obtaining transverse cardiac views (i.e. four chamber, five chamber, three vessel, three-vessel and trachea, and transverse aortic arch views) than if one uses a “body-based technique” (i.e. placing the fetus in an exact dorsal supine position as the initial plane before scrolling inside the STIC volume).107
Our recommendation is that once an apical four-chamber view has been obtained on 2D sonography, transducer movements should be minimal and focused to fine tune the apical four-chamber view plane to the correct one. Since the size of the fetal heart is small, anatomical structures are therefore close to each other within a small area. Thus, broad, random, and abrupt movements while using the transducer may change the cardiac plane completely (e.g. from a four-chamber view to an outflow tract). The following section describes guidelines for obtaining an appropriate apical four-chamber view of the fetal heart when the fetus is in a vertex presentation, as well as frequent errors that are made.
a. Obtain a four-chamber view:
We have observed sonologists to be slightly “off” plane when capturing STIC volumes. Specifically, a five-chamber view is obtained and on the monitor screen at the exact moment the sonologist presses the button to activate the STIC volume sweep. It is essential that the acquisition plane is not the five-chamber view with the aortic root or the left ventricular outflow tract. If either view is being obtained, the transducer may have been rotated rightward on the y-axis. To correct this situation, the operator should rotate the transducer in the opposite manner (i.e. leftward on the y-axis) to obtain the actual four-chamber view.
b. Symmetry of the left and right sides of the heart:
There is often a tendency to foreshorten the left (vs. right) side of the fetal heart when imaging the apical four-chamber view (Video clip 12). If this situation occurs, the transducer should be tilted and readjusted so that there is symmetry of both the left and right sides of the heart (the atria and ventricle comprise one side). Of course, asymmetry between the left and right sides of the fetal heart may represent CHD, and this possibility should be ruled out.
c. Lungs symmetric on either side of the heart:
In the apical four-chamber view, each fetal lung should be similar in size to each other. If one side is smaller (i.e. foreshortened) or larger than the other, it could indicate an azimuthal issue in which the probe has been tilted. The sonologist should readjust the probe so that both lungs appear symmetrical in size.
d. Fetal liver or stomach should not be visualized:
If any portion of the fetal liver or stomach is seen within the plane of the four-chamber view of a normal fetus (Video clip 13), it means that the transverse plane of the fetal chest is actually oblique and should be corrected by tilting/readjusting the probe. On the other hand, congenital anomalies (e.g. diaphragmatic hernia) may give this appearance. Thus, before acquiring a STIC volume, the fetal liver or stomach should never be visible in the same plane as the four-chamber view.
e. Absence of a “staircase spine:”
Visualizing a fetal “staircase spine” indicates that a true transverse plane of the fetal chest has not been obtained. Let us assume that a normal fetus is lying completely supine (i.e. 0°) in a longitudinal lie and vertex presentation, similar to a loaf of bread. If the transducer is positioned horizontally on the maternal abdomen, and the beam is exactly perpendicular (vs. oblique) to the fetus, a single plane will depict the fetal spine location at 6 o’clock, with its three ossification centers. An analogy would be visualizing a single “slice” from the loaf of bread. During a volume acquisition sweep of this fetus, the three spinal ossification centers will be visible in each serial transverse plane and located at the same area or point on the screen (i.e. 6 o’clock) (Video clip S14). However, if the same probe has now been tilted forward or backward on the maternal abdomen so that the insonation beam is oblique (vs. perpendicular) to the fetus, a “staircase spine” will be visualized on the screen.
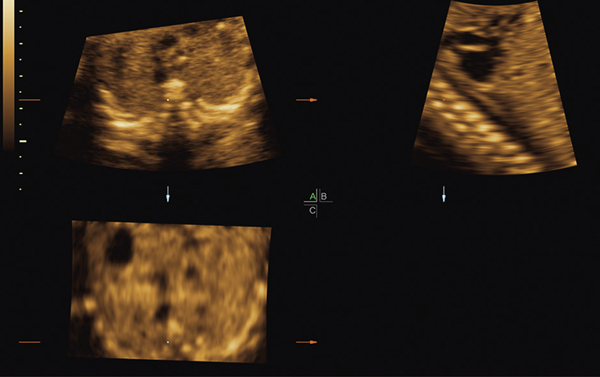
Therefore, we have coined the term “staircase spine” (or “caterpillar spine”) to refer to a fetus in which the transverse view on sonography shows spinal ossification centers “stacked” on each other like a staircase or caterpillar (Figure 9, Video clips 15 and 16). In addition, a coronal view of the curved ribs may also be seen. Therefore, the fetal spine appears to look like a staircase, in that the ossification centers are imaged obliquely and appear to be “moving” in a vertical direction on the monitor screen, as the STIC volume is being acquired. There are two situations that can lead to visualization of a staircase spine: 1) the fetus itself is inclined vertically at an angle to the floor (e.g. like a see-saw) with the top of the fetus tilted either downward or upward, but with the transducer beam perpendicular to the floor; or 2) the fetus is lying completely flat (i.e. 0°), but the transducer beam insonates the fetus in an oblique or tilted manner. When a staircase spine is apparent on the monitor screen, STIC volume acquisitions should be avoided, unless there is only a mild degree of incline.
Figure 9:
Staircase spine (downstairs type). In the A plane (transverse view) of the STIC volume, note that the ossification centers of the spine appear “stacked” upon each other like a staircase or a caterpillar, and a coronal view of the curved ribs can be seen because the ossification centers are being imaged obliquely. The staircase spine is confirmed in the B plane, which shows the fetus inclined vertically downward. During a STIC volume acquisition, the ossification centers will appear to be “moving” in a vertical direction on the monitor screen.
STIC, spatiotemporal image correlation.
The staircase spine can also be further subdivided into either an “upstairs spine” or a “downstairs spine.” With an upstairs spine (Figure 10, Video clip 16), the fetus is tilted upward (feet raised higher than the head), and an exaggerated view of the ventricles will be evident in the apical four-chamber view. Specifically, the ventricles will appear more prominent in size than usual, and their trabeculations may be seen. Additionally, the pulmonary valve and a portion of the liver may be noticeable when moving through serial transverse planes. To correct this situation (i.e. obtain an appropriate apical four-chamber view), one should move the transducer inferiorly on the maternal abdomen (toward the bladder) and tilt the transducer backward (operator’s wrist bending backward).
Figure 10:
Staircase spine (upstairs type). With the fetus tilted upward (feet raised higher than the head), this position leads to an upstairs spine. In this image, the fetal head is located on the right side (not in view). The fetal bladder is visualized on the left side.
With a downstairs spine (Figure 9, Video clip 15), the fetus is tilted downward (head raised higher than the feet), and the left atria may appear foreshortened in the apical four-chamber view. The Eustachian valve (or valve of the inferior vena cava) may be visible as well. To correct this situation (i.e. obtain an appropriate apical four-chamber view), one should move the transducer superiorly on the maternal abdomen (toward her head) and tilt the transducer forward (operator’s wrist bending forward). One of the possible issues with a downstairs spine is that the longitudinal pulmonary artery with its valve may not be visualized in its entirety when moving through serial transverse planes. In our experience, downstairs spines occur more frequently than upstairs spines.
It is noteworthy that the characteristics described above for a fetal staircase spine and how to correct it pertain to fetuses in a vertex presentation. When a fetus is in a breech presentation, the adjustment in transducer movements and tilting to obtain an appropriate apical four-chamber view will be the opposite of that described above. We have also observed that, generally, sonologists have more difficulty in obtaining an appropriate apical four-chamber view when the fetus is in a breech presentation (vs. vertex).
After an appropriate apical four-chamber view has been obtained, the sonologist should next quickly tilt or rock the probe slightly to ensure that the transverse aortic arch is clearly visible in the upper fetal mediastinum (Figure 7, Video clip 10) and then return back to the four-chamber view. While keeping this view on the monitor screen, the STIC volume acquisition is begun by pressing a button on the console. A key point is that when this action occurs, the fetal anatomical plane on the monitor screen will become the acquisition plane of the STIC volume. Therefore, it is crucial that the sonologist precisely coordinate pressing of the button to start the volume acquisition with attaining the correct apical four-chamber view on the screen. For example, if the five-chamber view instead is depicted on the screen, the transducer should be readjusted to obtain the four-chamber view before pressing the button for STIC acquisition.
8. Maternal breath holding and movement:
Maternal breathing or movements during the STIC acquisition may also lead to motion artifacts within the volume. Therefore, women should be asked to take a deep breath and to hold it for the entire duration of the STIC acquisition. We have found that it is very helpful to verbally support and encourage patients throughout the breath hold. Patients should be informed when the sweep has been completed, so that breathing can resume immediately. As a useful gauge, sonographic monitor screens usually have a small trapezoid-shaped icon that fills in with color as the STIC volume acquisition is occurring. Thus, the sonologist can determine what proportion of the acquisition has been completed and how much remains. If a television monitor is available that simultaneously depicts the images on the sonographic monitor screen, it is useful for patients to also observe the STIC acquisition, since it focuses their attention. Since maternal movements may lead to motion artifacts in the volume, women should be asked to momentarily suspend any body movements in addition to breathing.
Occasionally, patients are unable to perform a breath hold. In this situation, they should then be asked to minimize the intensity and frequency of abdominal movements that occur during breathing as much as possible. On the flip side, some women are so eager to cooperate that they inspire deeply enough to actually shift the fetal heart location on the screen. Specifically, the four-chamber view will either shift outside the ROI box or move inferiorly off the monitor screen. To address this situation, minor adjustments should be made with the transducer or to the image depth, ROI box, etc., so that the four-chamber view is again visible on the screen and the ROI box encompasses the entire fetal chest circumference. An alternative is to repeat another maternal breath hold but with more shallow breaths to diminish the maternal abdominal excursion.
9. Operator movement:
During the STIC volume acquisition, it is also important for sonologists to remain motionless (not move their hand on the transducer) while maintaining the transducer fixed and in good contact with the maternal abdomen.
10. When to discard STIC volumes and when not to obtain them:
In general, it is important to practice efficiency1 during the sonographic examination to be successful in STIC volume acquisition, especially because the sonologist may have only a single and limited window of opportunity to capture volumes. Efficiency, however, implies more than just procedurally performing the acquisition process. This concept also refers to an immediate awareness of when a volume will be uninformative and needs to be discarded. Such evaluation can occur: 1) after STIC volumes are displayed in the multiplanar view or through STICLoop (see later); or 2) during the actual acquisition process itself. For example, if there is obvious fetal movement and/or breathing during the acquisition, such a process can be terminated immediately (Video clip 17). If the fetus was initially motionless during the volume capture, but 1) suddenly changes position or moves; 2) the fetal heart shifts outside the ROI box; 3) an extremity moves into the field of view (leading to acoustic shadowing of the cardiac structures); or 4) the acquisition angle is insufficient, the STIC acquisition should be ended immediately or the volume discarded. Therefore, the goal is to capture and save as many volumes as possible in rapid succession when the environment is appropriate while discarding those that are obviously inappropriate. Even so, it may not always be clearly evident which STIC volume(s) will later turn out to be good. In such cases, it is prudent to be cautious by capturing and saving volumes anyway, since they can always be discarded later, if necessary. Moreover, protocols that include the acquisition of more than a single volume increase the chances that relevant information can be obtained.108 If the initial STIC volumes are unsatisfactory or inappropriate, additional volumes should be obtained when possible.
If the sonologist has already captured appropriate and informative STIC volumes, this becomes advantageous when an optimal fetal position suddenly changes during the course of a sonographic examination. Thus, one clinical approach is to acquire several STIC volumes while the fetal position is optimal and then continue with 2D sonography. If the latter does not allow one to successfully obtain cardiac views, the STIC volume datasets are still available for analysis.87
Besides fetal motion or breathing leading to artifacts within the STIC volume, they can also occur with changes in the fetal heart rate.109 Moreover, in the presence of an abnormal fetal heart rate (e.g. tachycardia or bradycardia), sudden changes in the fetal heart rate, or cardiac rhythm disturbances/arrhythmias, a STIC volume acquisition may not be feasible. When there are severe changes in the fetal heart rate during the STIC capture, the algorithm has difficulties in calculating the average heart rate correctly, which can lead to artifacts secondary to rearrangement of non-corresponding images.3 In other words, there is significant misregistration of the information required for precise reconstruction of moving cardiac structures.4
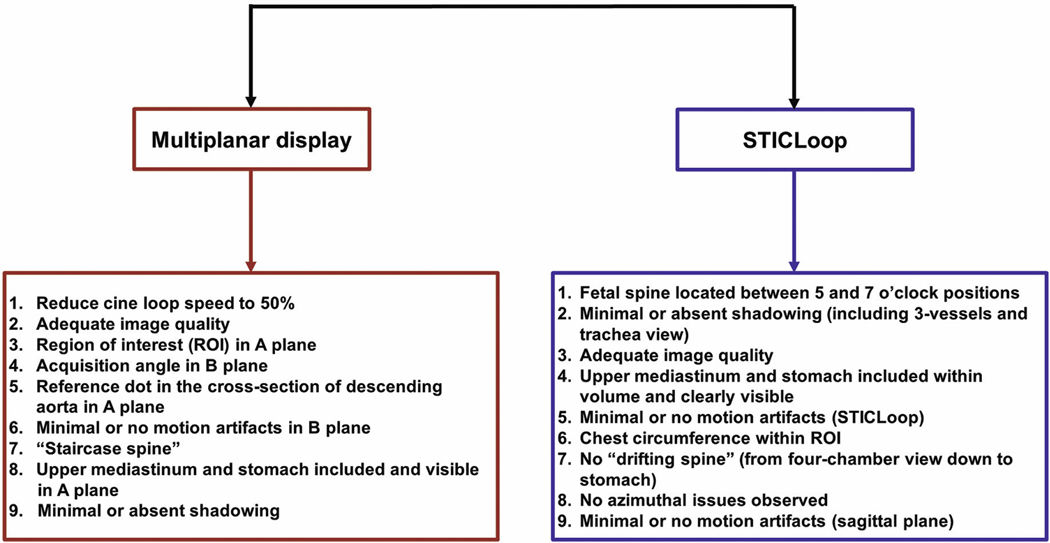
Evaluation of STIC Volumes to Determine their Appropriateness for Analysis
Immediately after a STIC volume acquisition, the volume may be displayed in the multiplanar view or automatically converted into a 2D cine loop (STICLoop).87 These methods of STIC volume display are useful to promptly determine whether the volume is appropriate for further analysis (e.g. to obtain fetal cardiac views). This process is an important and necessary next step because STIC volumes must also be informative.98 In this article, we will not describe the initial adjustment of STIC volume datasets for standardization purposes, which is done before navigation is performed. Such adjustment has been suggested to simplify the STIC orientation and enable reproducible planes for analysis; the interested reader is referred elsewhere for this information.94,110
Various factors influence the success of a protocol for STIC volume acquisition, including whether there is a standardized acquisition technique along with feedback regarding technical errors.108 Indeed, some have recommended that before introducing STIC technology into the screening setting, one requirement is that sonologists must be able to acquire clinically valid (i.e. acceptable diagnostic quality) volume datasets daily, while also learning how to immediately assess volume quality to discard those inappropriate for diagnostic use.57 It is clear that for STIC volumes to be informative (i.e. ability to display fetal cardiac planes and structures), they should be of high quality.88,97,98 Thus, methods to determine whether such volumes are appropriate for further analysis are essential.
When STIC volumes are assessed at the patient’s bedside (via either the multiplanar display or STICLoop), there are two methods of practice: 1) one method is to assess each volume sequentially and then decide whether saving that volume is appropriate. Although this process takes seconds to perform, a disadvantage is that an optimal window of opportunity to collect more volumes may be lost (e.g. fetus changes position or begins breathing movements). On the other hand, an advantage of this approach is that appropriate STIC volume(s) may be found, such that it may not be necessary to continue capturing more volumes; 2) the other method is to take advantage of the optimal window of opportunity by capturing and saving as many STIC volumes as possible in rapid succession but without assessing them until the session is finished. The main advantage of this method is that a larger number of volumes may be collected for analysis. However, the disadvantage is that both appropriate and inappropriate STIC volumes will have been saved, and the operator will be assessing this entire group of volumes at the bedside. It is worth noting, however, that both methods (i.e. multiplanar display or STICLoop) to evaluate STIC volume datasets can be performed rather quickly and are detailed below. The choice of which method to implement should be based on user preference and the clinical environment. In general, we prefer the second method of capturing and saving as many STIC volumes as possible, with evaluation after the session is completed.
STIC volumes may also be evaluated offline (using the multiplanar display or STICLoop) to determine whether the datasets are appropriate. This process is accomplished through software on desktop or laptop computers, which duplicates the on-line environment. We will now review the two methods of STIC volume display, as well as how to evaluate STIC volumes to determine their appropriateness for analysis.
1. What is the multiplanar display?
The dynamic image sequence of a STIC volume dataset can be displayed in various formats: 1) multiplanar view; 2) single-plane view; and 3) rendered image. When a volume is displayed in three orthogonal planes (representing the transverse, sagittal, and coronal planes of a reference 2D plane within this volume), it is known as the “multiplanar display” or “multiplanar view” (Figure 1, Video clip 1). Through STIC technology, dynamic images of the fetal heart in motion can be visualized simultaneously in all three orthogonal planes.
a. Characteristics of three planes:
The starting reference plane from which the STIC volume is acquired is referred to as the A plane and is located in the upper left corner (Figure 1, Video clip 1). The plane orthogonal to the A plane, but parallel to the ultrasound beam, is termed the B plane (upper right corner). The plane perpendicular to both the A plane and the ultrasound beam is termed the C plane (lower left corner), and is commonly referred to as the coronal plane. Both the B and C planes are perpendicular planes corresponding to the location of the reference dot within the STIC volume.1
The multiplanar display of a STIC volume dataset provides information on the ROI, as well as the acquisition angle of the volume. Specifically, the A plane displays the size of the ROI box (selected height and width) of the volume, while the B plane demonstrates the acquisition angle of the volume (Figure 1 and Video clip 1).
It should be noted that when a STIC volume has been acquired from a fetus in a vertex presentation, the heart will be displayed with its left side in the left part of the A plane. At the same time, the fetal head will be on the left side of the screen in the B plane. For a breech presentation, however, the opposite is the case. The left ventricle will appear in the right part of the A plane, while the fetal head will be on the right side of the screen in the B plane.
b. Image resolution in the planes:
The A-plane image consists of pixels that have the properties of axial and lateral resolution.92 Accordingly, this plane has the highest resolution and best image quality and is equivalent to a 2D image displayed during sonographic examination. The B and C planes also have axial and lateral resolution. Yet, the resolution in these planes is a function of the transducer beam, as well as the size of the “voxel” (or volume of pixels) that is created from the original STIC volume dataset. Both B and C planes have been reconstructed by the system. Therefore, these images are characterized by lower resolution than that of the A plane.92 The coronal reconstructed plane generally has the lowest resolution of all three planes in the multiplanar display. Since the quality of a STIC volume dataset can be estimated by directly analyzing the B plane, this step is included when evaluating volumes to determine their appropriateness for further analysis.
c. Rendered image:
The panel in the right lower corner of the multiplanar display of the STIC volume dataset demonstrates the rendered image, which can provide additional information not available from thin 2D image slices.3 Volume rendering describes the display of either external or internal surfaces of organs with data derived from multiple 2D sections.86 STIC volumes can be rendered in various display modes (e.g. surface rendering,4,111 minimum mode,13,15 glass body,15,53 and inversion52,54). Such rendering techniques can be used to visualize any fetal cardiac structure (and provide a depth perspective to structures) as well as optimize the contrast of myocardial borders, septa, and valves.4,111,112 Realistic 4D images of the structure(s) of interest may also be obtained.15
2. How to evaluate STIC volumes to determine their appropriateness for analysis using the multiplanar display:
Immediately after the STIC acquisition has been completed, the estimated fetal heart rate will appear on the sonographic monitor screen, and the operator should decide whether to cancel/discard or to accept/save the volume. In general, the fetal heart rate should be within normal limits to accept the volume. Next, the ultrasound machine can be programmed such that the multiplanar display will appear on the monitor screen. The following steps are recommended:
a. Reduce cine loop speed to 50%:
The operator can adjust the speed of the STIC cine loop according to his or her preference. We recommend reducing the speed down to 50% because when the cine speed is 100% or higher, detection of true motion artifacts within the STIC volume may become more difficult to discern. Moreover, inherent cardiac motion will appear more pronounced. As a result, one may misinterpret a motion artifact to be present, when the “motion” is actually due to the dynamic image sequence.
b. Adequate image quality:
The planes of the multiplanar display should demonstrate images of adequate quality (e.g. clear visualization of the fetal heart and an image neither too bright nor too dark). If the image quality is suboptimal, the STIC volume will most likely be uninformative.
c. Region of interest in A plane:
The A plane displays the size of the ROI box (selected height and width) of the STIC volume that should be evaluated to ensure the size is adequate and encompasses the entire fetal chest circumference (Figure 1, Video clip 1).
d. Acquisition angle in B plane:
When an apical four-chamber view is the acquisition plane, the B plane will depict a sagittal view of the fetal heart (e.g. ductal arch) (Figure 1, Video clip 1). To determine whether the acquisition angle is wide enough, the fetal heart and upper abdomen should be visualized in the B plane (this task can also be accomplished by scrolling through serial parallel frames in the A plane). In theory, for a four-chamber view acquisition plane, if the operator observed the upper fetal mediastinum and stomach on the monitor screen while the STIC volume sweep was occurring (Video clip 2), the acquisition angle should be adequate. If the volume demonstrates an acquisition angle that is too narrow, it should be discarded.
e. Reference dot in cross-section of descending aorta in A plane:
The reference dot imaging tool is used to localize the same anatomic structure in all three orthogonal planes.1 As the reference dot is moved around, the corresponding planes will change respectively.3 The dot should be placed in the cross-section of the descending aorta in the A plane, so that the longitudinal descending aorta becomes visible in both the B and C planes (Figure 1, Video clip 1). Next, the sagittal view of the fetal heart (B plane) should be evaluated for the presence of: 1) wavy lasagna wall; 2) water dive; 3) piano keys; and 4) staircase spine. The first three signs indicate the presence of motion artifact(s) within the STIC volume dataset.
f. Minimal or no motion artifacts observed in B plane:
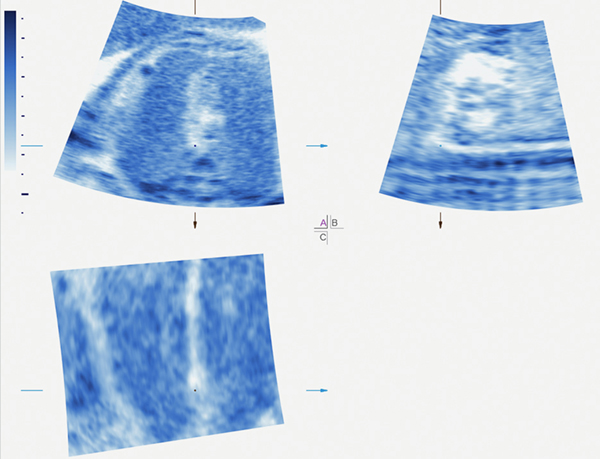
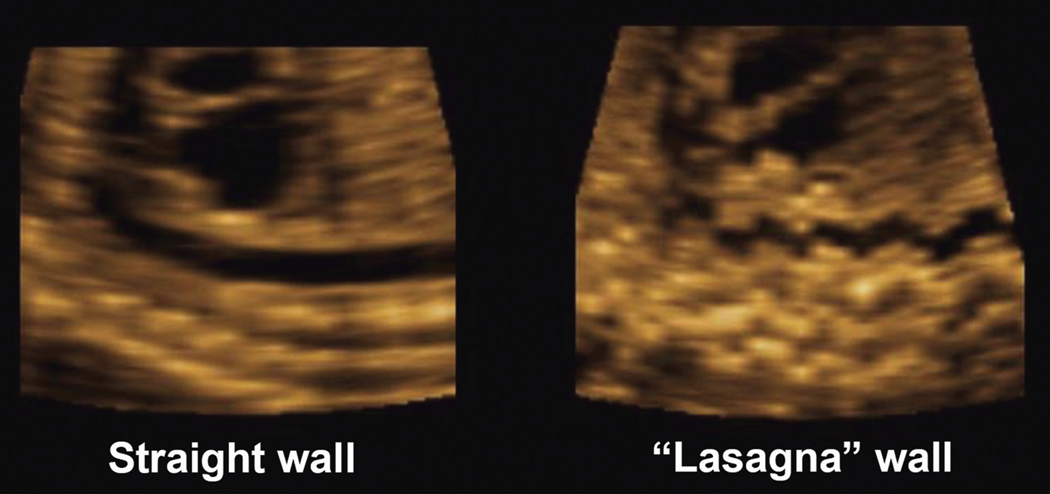
Any type of motion artifacts or errors in STIC assembly can modify fetal anatomical structure representation87 and, therefore, are relevant issues when performing 4D sonography with STIC. Indeed, artifacts during STIC acquisition will produce artifacts in the reconstructed planes, with erroneous information contained in the multiplanar display.26 Specifically, motion artifacts secondary to fetal breathing or gross body movements may be observed in the B plane (sagittal plane) of the multiplanar view. Although much of the fetal anatomy may be affected (Video clip 8), it is helpful to focus on the wall of the longitudinal descending aorta to evaluate volume quality. In the absence of motion artifact, the wall should appear straight (Figure 11). However, when motion artifact(s) are present, they can affect the characteristics of the longitudinal descending aorta wall in several ways; we have categorized this into 3 types: 1) wavy lasagna wall; 2) water dive; and 3) piano keys. Fetal breathing or gross body movements will also affect the image in the C plane.
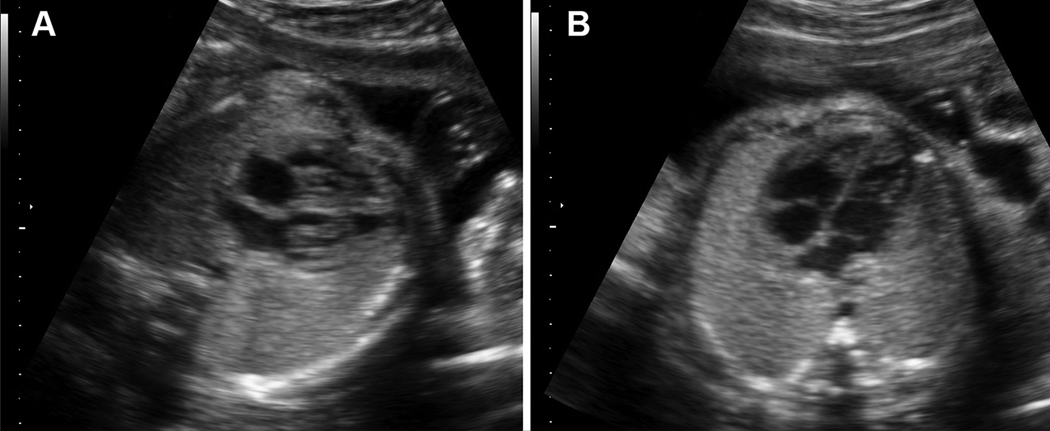
Figure 11:
Example of motion artifacts in the wall of the longitudinal descending aorta in a STIC volume dataset. The left image shows a straight wall, consistent with absence of fetal breathing during the STIC acquisition. However, the right image shows a “wavy lasagna wall,” indicating regular fetal breathing during the STIC acquisition. Thus, this volume is not appropriate and should be discarded.
STIC, spatiotemporal image correlation.
Lasagna pasta is a long, broad noodle, which is ideally suited to layering in a baking dish. Although such noodles have a flat shape in Italy, American lasagna noodles tend to be ruffled or wavy along the edges. Similarly, in the presence of regular breathing motion (fetal or maternal), the fetal longitudinal descending aorta wall often appears undulated or wavy at regular intervals. Therefore, we refer to this type of artifact as a wavy lasagna wall (Figure 11, Video clips 18 and 19). On the other hand, when there are discrete area(s) of motion artifact seen in the sagittal plane of the multiplanar view, we term this a water dive (Video clip 20). This term refers to the discrete underwater turbulence/motion that develops only in the specific location where a diver enters the water. A water dive artifact usually occurs when there is isolated breathing or gross body movements during the STIC acquisition. Depending upon the area(s) of interest, this type of motion artifact may not be an issue. For example, if one is interested in assessing the 3-vessel and trachea view, a water dive motion artifact in the fetal upper abdomen will not pose a problem. The third type of motion artifact occurs in the presence of fetal hiccups. The sagittal plane of the multiplanar view has a very distinctive appearance, similar to that of a pianist sharply pressing and releasing multiple piano keys at fixed intervals apart on the keyboard (i.e. corresponding to the regular and episodic nature of hiccups). Therefore, we refer to this appearance as piano keys (Video clip 21). Such a regular pattern may be visualized in an isolated portion of the B-plane image (i.e. regular fetal hiccups occurring at a single time point during the volume acquisition), or the pattern may be seen throughout the B-plane image (i.e. regular fetal hiccups during the entire volume acquisition, which is more common).
In contrast to most fetal breathing movements which are regular in nature, gross body movements typically occur at sporadic time points. Yet, because the intensity of body movements tends to be greater than that of fetal breathing movements, the B-plane image is usually non-interpretable in such cases. Although any type of excessive fetal movement will make interpretation of the B-plane image difficult, minimal movement(s) may still preserve the anatomical relationships which are required for diagnosis (Video clip 9).3
Can motion artifacts be identified in the A-plane image of the multiplanar display? In our experience, when a motion artifact is present within the STIC volume dataset, it is much easier to identify this in the B plane rather than in the A plane. Fetal breathing or movement will not alter the A-plane image unless it is excessive3 because the A plane contains the original, acquired B-mode images used to construct the B- and C-plane images. Therefore, although fetal breathing will alter the images in the B and C planes, the A-plane image will still be interpretable if the sonologist: 1) evaluates the heart using only this image; and 2) moves through the STIC volume from the beginning to end of the acquisition without rotating the image.3
In the presence of excessive fetal breathing or movement, however, the A-plane image may appear to “jump” out of place, or one may observe what we term a “double-vision” image or “ghost” image in a specific frame(s). A double-vision image (Video clip 22) occurs when a single object looks like two images simultaneously or when two images of the same object overlap.113 In contrast, a ghost image (Video clip 23) occurs when two images are only very slightly separated but are not two distinct images.113 In the A plane, the presence of a ghost image, a double-vision image, or an image “jumping” out of place will render the STIC volume unacceptable and uninformative.
g. Staircase spine:
It is optimal to acquire STIC volumes such that the fetal spine appears horizontal (i.e. 0°) on the monitor screen, rather than inclined [“upstairs spine” with the feet raised higher than the head (Figure 10, Video clip 16), or “downstairs spine” with the head raised higher than the feet (Figure 9, Video clip 15)]. When the acquisition plane is the four-chamber view, the orientation of the fetal spine can be evaluated easily in the B plane of the multiplanar display (Figure 9, Video clip 15). If there is a mild staircase spine, the STIC volume may still be acceptable. However, a STIC volume with a steep staircase spine should be discarded for the reasons discussed previously. The A plane (transverse plane) in the multiplanar display can also depict a staircase or a caterpillar spine. This appearance is recognized when the spinal ossification centers appear “stacked” on each other like a staircase or a caterpillar. Additionally, a coronal view of the curved ribs may also be seen (see “Absence of a staircase spine” above for further explanation) (Figure 9, Video clips 15 and 16).
h. Upper mediastinum and stomach:
Next, the sonologist should scroll through the A plane of the multiplanar display so that one is moving through serial transverse planes from front to back and vice versa. For this action, the location of the reference dot is irrelevant since a parallel shift movement through transverse planes is occurring. While scrolling through the A plane, both the fetal upper mediastinum (including the transverse aortic arch) and stomach should be included and clearly visible.
i. Minimal or absent shadowing:
In general, shadowing artifacts should not be observed in either the A or B planes of the multiplanar display. Although it may seem that acoustic shadowing or dropout is not present in the 2D image plane (which is a single slice) during real-time scanning, it may actually be present within the STIC volume because the volume dataset comprises thousands of 2D images acquired through the area of interest during the sweep. Therefore, acoustic shadowing or dropout can occur in any of these 2D frames. This issue should be apparent to the sonologist by careful observation during the actual STIC volume sweep. Yet, if acoustic shadowing or dropout has been included within the volume dataset, its location influences whether such volume will be informative. For example, if shadowing or dropout occurs in the fetal abdominal area, it may not be as crucial if it occurs in the upper mediastinum.
3. What is STICLoop?
This is a 2D cine loop tool developed to aid the user in determining the appropriateness of STIC volume datasets before applying the Fetal Intelligent Navigation Echocardiography (FINE) method to such volumes.87 Once a STIC volume has been obtained, it is automatically converted into a 2D cine loop that scrolls in a continuous fashion (Video clip 24).87 With STICLoop, the image on the screen begins with the initial frame that was obtained by the transducer, and automatic scrolling through all the frames occurs until the last frame acquired in the sweep is reached. Thus, when the acquisition plane is the apical four-chamber view, serial fetal transverse planes will be depicted in the STICLoop (Video clip 24). This tool was developed to facilitate detection of 1) discontinuity or undulating movements that could modify anatomical structure representation that are due to motion artifacts or errors in STIC assembly (Video clip 25); 2) azimuthal issues (tilted acquisitions); and 3) “drifting spines,” in which the spine location “migrates” on the screen during the automatic STICLoop scroll (Video clip 26).87
How does STICLoop compare to manual navigation through the multiplanar display when evaluating for motion artifacts? With manual navigation, motion artifacts may be hidden or underestimated in the A plane due to speed variability generated when the user operates the mouse.87 For example, if a fetus has moved quickly during the STIC volume acquisition, a few frames could be displaced from the rest. Yet, we have found that this may not be as noticeable when manually navigating through the A plane and is more likely to be detected by using STICLoop.87 Observation of the 2D cine loop allows improved detection of issues (e.g. undulating movements) compared to the multiplanar display because it is operator-independent and runs automatically at a constant speed.87 Moreover, as previously discussed, fetal breathing or movements will not alter the A-plane image in the multiplanar display unless it is excessive.3
4. How to evaluate STIC volumes to determine their appropriateness for analysis using STICLoop:
To determine whether STIC volumes are appropriate before applying the FINE method,87 the operator should observe that the following criteria are met using STICLoop (Video clip 24)87: 1) fetal spine located between the 5- and 7-o’clock positions (reducing the possibility of shadowing from the ribs or spine) (Figure 2); 2) minimal or absent shadowing (including the three-vessel and trachea view), which could obscure visualization of cardiac anatomy; 3) adequate image quality; 4) upper mediastinum and stomach included within the volume and clearly visible; 5) minimal or no motion artifacts observed in the STICLoop (i.e. smooth sweep without evidence of abrupt jumps or discontinuous movements) (Video clip 25); 6) chest circumference contained within the ROI; 7) sequential axial planes parallel to each other, similar to a sliced loaf of bread (i.e. no “drifting spine” from the four-chamber view down to the stomach) (Video clip 26); 8) no azimuthal issues observed (i.e. atria/ventricles do not appear foreshortened in the four-chamber view); and 9) minimal or no motion artifacts observed in the sagittal plane. Similar to evaluation of the B plane (sagittal plane) in the multiplanar display, the sonologist should also evaluate for motion artifact(s) in the sagittal plane of STICLoop [e.g. presence/absence of a wavy lasagna wall (Figure 11, Video clips 18 and 19), water dive (Video clip 20), and piano keys (Video clip 21)]. In the absence of motion artifacts, the wall of the longitudinal descending aorta should appear straight (Figure 11). It should be noted that the sagittal plane image of STICLoop was designed only to evaluate for motion artifact(s) and not to evaluate cardiac anatomy itself.
In summary, herein we have 1) described a practical and step-wise approach to performing 4D sonography with STIC (Figure 12); and 2) reviewed the evaluation of STIC volumes to determine their appropriate for analysis, through use of the multiplanar display or STICLoop (Figure 13). For the readers’ convenience, Table 1 lists terms and definitions related to 4D sonography with STIC, and Table 2 summarizes important points and tips to remember when performing 4D sonography with STIC.
Figure 12:
Overall practical and step-wise approach to performing 4D sonography with spatiotemporal image correlation (STIC). See text for further details.
Figure 13:
Two methods to evaluate STIC volumes and determine their appropriateness for analysis (using multiplanar display and STICLoop). See text for further details.
ROI, region of interest; STIC, spatiotemporal image correlation.
Table 1.
Terms and definitions related to 4D sonography with STIC
| Term | Definition |
|---|---|
| Acoustic dropout | Signal loss in the sound path without intervening structures |
| Acoustic shadowing | Signal loss in the sound path secondary to echogenic structures |
| Acquisition angle (degrees) | Determines the acquisition depth (amount of information acquired in the z-plane) |
| Acquisition plane | • Starting 2D plane for the volume acquisition • Known as the A plane in the multiplanar display |
| Acquisition time (seconds) | • Equivalent to the duration of volume acquisition • Determines the speed at which the transducer sweeps the region of interest • An inverse relationship exists between acquisition time and sweep speed of transducer |
| Dolphin | Refers to fetal transverse aortic arch (appears like a dolphin on ultrasound) |
| Double vision image | • Observed in the A plane (multiplanar display) in the presence of excessive fetal breathing or movement • When a single object looks like two images simultaneously, or when two images of the same object overlap |
| Drifting spine | • Fetal spine location “migrates” on the monitor screen during the automatic STICLoop™ scroll • When sequential axial planes are parallel to each other (similar to a loaf of bread), there is no drifting spine |
| Driving the transducer | Sonographic technique to “convert” the fetal spine to a posterior position on the monitor screen |
| Four-dimensional or 4D | Volume datasets that incorporate information about the three spatial dimensions plus the temporal dimension |
| Ghost image | • Observed in the A plane (multiplanar display) in the presence of excessive fetal breathing or movement • When two images are only very slightly separated and not two distinct images |
| Multiplanar display or view | • Display format of sonographic volumes (e.g. STIC) in which there are three orthogonal planes (transverse, sagittal, coronal) • Allows correlation between image planes that are perpendicular to the main acquisition plane • Can be used to determine whether a STIC volume is appropriate for further analysis |
| a. A plane | • Acquisition plane • Displays the size of the region of interest box (selected height and width) of volume • Located in upper left corner of multiplanar display |
| b. B plane | • Plane orthogonal to A plane, but parallel to ultrasound beam • Demonstrates the acquisition angle of volume • Located in upper right corner of multiplanar display |
| c. C plane | • Plane perpendicular to both A plane and ultrasound beam • Commonly referred to as the coronal plane • Located in lower left corner of multiplanar display |
| Piano keys artifact | • Characterized by a distinctive appearance in the B plane of multiplanar display • Similar to a pianist sharply pressing and releasing multiple piano keys at fixed intervals apart on the keyboard • Occurs in presence of fetal hiccups |
| Reference point or dot | • Intersection of three planes in the multiplanar display • Tool can be used to manually navigate through the STIC volume and localize the same anatomic structure in all three orthogonal planes |
| Region of interest (ROI) | Box determines the height (y-plane) and width (x-plane) of the volume dataset |
| Rendered image or display | • Contains depth in the z-plane, and provides additional information not available from thin 2D image slices • Volumes can be rendered in various display modes (e.g. surface rendering, inversion) • Located in right lower corner of multiplanar display |
| Spatiotemporal Image Correlation (STIC) technology | Allows acquisition of a fetal cardiac volume dataset, and displays a cine loop of a complete single cardiac cycle in motion |
| Staircase (or caterpillar) spine | • Fetus in which the transverse view of fetal spine on ultrasound shows ossification centers “stacked” upon each other like a staircase or caterpillar; coronal view of curved ribs may also be seen • Ossification centers are imaged obliquely and appear to “move” vertically on the monitor screen as the volume is being acquired |
| a. Upstairs spine | • Fetus is tilted upwards (feet raised higher than the head) • Exaggerated view of ventricles will be evident in apical four-chamber view |
| b. Downstairs spine | • Fetus is tilted downward (head raised higher than the feet) • Left atria may appear foreshortened in apical four-chamber view and Eustachian valve may be visible |
| STICLoop™ | • 2D cine loop to aid the user in determining the appropriateness of STIC volume datasets before applying the FINE method to such volumes • Facilitates detection of: 1) discontinuity or undulating movements that could modify anatomical structure representation and are due to motion artifacts or errors in STIC assembly; 2) azimuthal issues (tilted acquisitions); and 3) drifting spines • Operator independent and runs automatically at a constant speed |
| Voxel | Volume of pixels |
| Water dive artifact | • Discrete area(s) of motion artifact seen in the B plane of multiplanar display • Occurs when there is isolated breathing or gross body movements during volume acquisition |
| Wavy lasagna wall artifact | • Wall of the fetal longitudinal descending aorta (B plane of multiplanar display) appears undulated or wavy at regular intervals • Occurs in presence of regular breathing motion (fetal or maternal) |
2D, two-dimensional; 3D, three-dimensional; FINE, Fetal Intelligent Navigation Echocardiography
Table 2.
Performing 4D sonography with STIC: important points and tips
| • Many factors which affect the acquisition and quality of STIC volume datasets also pertain to 2D sonography |
| • Success rates of volume acquisition in fetuses with normal hearts range widely (26–100%) and depend on many factors (e.g. operator skill), preset criteria/requirements for acquisition, and the purpose of study |
| • Four essential steps in performing 4D sonography with STIC include: volume acquisition, display, manipulation / post-processing, and storage of volumes and images |
| • When acquiring volumes and determining whether they are appropriate for further analysis, there are three main time points: before acquisition, acquisition, and immediately after acquisition |
| • Volumes may be obtained in each trimester (recommend 19–30 gestational weeks for optimal assessment of fetal cardiac anatomy) |
| • Ask the mother who is lying supine to turn (or roll) laterally onto her side in the same direction that you wish the fetal cardiac apex to turn |
| • Constantly adapt to the fetal “situation” throughout the ultrasound examination and take advantage of any proper moments to obtain volumes |
| • If the fetal heart is in an optimal position and conditions are appropriate, immediately acquire multiple volumes in rapid succession |
| • Image quality of volume datasets depends primarily on the original quality of the 2D image |
| • A high frame rate can be achieved by decreasing depth, sector width, and the number of focal zones |
| • Adjust the region of interest (ROI) box size to be as small as possible to maximize the frame rate during acquisition and improve the temporal resolution of the volume dataset |
| • Set the acquisition angle at least 5 degrees more than the gestational age; however, the angle should not be too wide either |
| • The quality of a volume acquisition is reflected by the acquisition time, and volumes should be obtained using the longest possible time (higher image resolution). Recommend an acquisition time of at least 10 seconds, with adjustment based upon presence/absence of fetal breathing or movements |
| • When the fetal spine location is between 5 and 7 o’clock, this reduces the possibility of acoustic shadowing from ribs or spine |
| • Use the technique of driving the transducer to “convert” the fetal spine to a posterior position on the monitor screen |
| • Fetal breathing and gross body movements during the volume acquisition can lead to motion artifact(s) within the volume dataset, with distortion of images and anatomical structures |
| • In most cases, the acquisition plane will be the four-chamber view |
| • A correct (or appropriate) four-chamber view should be obtained (i.e. true cross-section of the thorax with proper alignment in the axial plane) |
| • Sonologists tend to foreshorten the left (vs. right) side of the heart when imaging the apical four-chamber view |
| • Visualizing a fetal staircase spine indicates that a true transverse plane of the fetal chest has not been obtained, and therefore should be avoided |
| • In general, sonologists have more difficulty in obtaining an appropriate apical four-chamber view when the fetus is in breech presentation (vs. vertex) |
| • At the time a volume acquisition begins by pressing a button, the fetal anatomical plane on the monitor screen at that moment will become the acquisition plane |
| • It is very helpful to verbally support and encourage patients throughout the breath hold which occurs during the acquisition |
| • During the actual volume sweep, observe the sequential images within the ROI box on the monitor screen to evaluate for satisfactory or unsatisfactory (e.g. fetal movement) conditions |
| • Practicing efficiency during the sonographic examination is immediate awareness of when a volume will be uninformative and needs to be discarded (e.g. fetal heart shifts outside the ROI box during the acquisition) |
| • In the presence of an abnormal fetal heart rate (e.g. tachycardia, bradycardia), sudden changes in fetal heart rate, or cardiac rhythm disturbances/arrhythmias, volume acquisitions may not be feasible |
| • Two methods of STIC volume display (multiplanar view or STICLoop™) are useful to immediately determine whether the volume is appropriate for further analysis (e.g. to obtain fetal cardiac views) |
| • The multiplanar display of a volume dataset provides information on the ROI box size (A plane) and the acquisition angle (B plane) |
| • The A plane image (multiplanar display) has the highest resolution, best image quality, and is equivalent to a 2D image displayed during sonographic examination |
| • Both B and C planes (multiplanar display) are reconstructed planes, and therefore these images are characterized by lower resolution than that of the A plane |
| • The B plane of multiplanar display may be evaluated for motion artifact(s), such as wavy lasagna wall, water dive, or piano keys |
| • Fetal breathing or movement will not alter the A plane image unless it is excessive. In this case, the A plane image may appear to “jump” out of place, or one may observe a ghost image or double vision image in a specific frame(s) |
| • Although acoustic shadowing or dropout may seem absent in the 2D image plane during real-time scanning, this may actually be present within the volume |
| • STICLoop™ is a 2D cine loop tool that aids the user in determining the appropriateness of STIC volume datasets before applying the FINE method to such volumes |
| • STICLoop™ allows improved detection of issues (e.g. undulating movements) vs. manual navigation through the A plane |
2D, two-dimensional; FINE, Fetal Intelligent Navigation Echocardiography; ROI, region of interest; STIC, spatiotemporal image correlation
Conclusions
STIC technology has been a major technological advance in the field of obstetric sonography. Since volumetric sonography of the fetal heart allows the review of all cardiac planes at any time during the cardiac cycle, it could be helpful in cardiac screening and has the potential to increase the detection rate of CHD. Indeed, a large body of evidence suggests that 4D sonography with STIC facilitates examination of the fetal heart and also has the potential to reduce operator dependency that is associated with conventional 2D sonography. Compared to the latter, 4D sonography with STIC is also characterized by unique features and advantages.
It is our hope that by having reviewed here a pragmatic and step-wise approach to performing STIC, sonologists will find such information useful in clinical practice and, as a result, will more widely embrace STIC technology as a valuable tool in the armamentarium of fetal cardiac evaluation.
Supplementary Material
Acknowledgements
Dr. Roberto Romero has contributed to this work as part of his official duties as an employee of the United States Federal Government. This article is a U.S. Government work and is in the public domain in the USA.
This research was supported, in part, by the Perinatology Research Branch, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, U.S. Department of Health and Human Services (NICHD/NIH/DHHS); and, in part, with Federal funds from NICHD/NIH/DHHS under Contract No. HHSN275201300006C.
REFERENCES:
- 1.Yeo L, Romero R. How to acquire cardiac volumes for sonographic examination of the fetal heart (Part 1). J Ultrasound Med 2016;35:1021–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viñals F, Poblete P, Giuliano A. Spatio-temporal image correlation (STIC): a new tool for the prenatal screening of congenital heart defects. Ultrasound Obstet Gynecol 2003; 22: 388–394. [DOI] [PubMed] [Google Scholar]
- 3.DeVore GR, Falkensammer P, Sklansky MS, Platt LD. Spatiotemporal image correlation (STIC): new technology for evaluation of the fetal heart. Ultrasound Obstet Gynecol 2003; 22: 380–387. [DOI] [PubMed] [Google Scholar]
- 4.Gonçalves LF, Lee W, Chaiworapongsa T, et al. Four-dimensional ultrasonography of the fetal heart with spatiotemporal image correlation. Am J Obstet Gynecol 2003; 189: 1792–1802. [DOI] [PubMed] [Google Scholar]
- 5.Chaoui R, Hoffmann J, Heling KS. Three-dimensional (3D) and 4D color Doppler fetal echocardiography using spatio-temporal image correlation (STIC). Ultrasound Obstet Gynecol 2004; 23: 535–545. [DOI] [PubMed] [Google Scholar]
- 6.Bhat AH, Corbett VN, Liu R, et al. Validation of volume and mass assessments for human fetal heart imaging by 4-dimensional spatiotemporal image correlation echocardiography: in vitro balloon model experiments. J Ultrasound Med 2004; 23: 1151–1159. [DOI] [PubMed] [Google Scholar]
- 7.American Institute of Ultrasound in Medicine. AIUM practice guideline for the performance of fetal echocardiography. J Ultrasound Med. 2013; 32:1067–1082. [DOI] [PubMed] [Google Scholar]
- 8.Lee W, Allan L, Carvalho JS, et al. ; ISUOG Fetal Echocardiography Task Force. ISUOG consensus statement: what constitutes a fetal echocardiogram? Ultrasound Obstet Gynecol. 2008; 32:239–242. [DOI] [PubMed] [Google Scholar]
- 9.International Society of Ultrasound in Obstetrics and Gynecology; Carvalho JS, Allan LD, Chaoui R, et al. ISUOG Practice Guidelines (updated): sonographic screening examination of the fetal heart. Ultrasound Obstet Gynecol. 2013; 41:348–359. [DOI] [PubMed] [Google Scholar]
- 10.Donofrio MT, Moon-Grady AJ, Hornberger LK, et al. ; American Heart Association Adults with Congenital Heart Disease Joint Committee of the Council on Cardiovascular Disease in the Young and Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Council on Cardiovascular and Stroke Nursing. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation. 2014; 129:2183–2242. [DOI] [PubMed] [Google Scholar]
- 11.Tudorache S, Cara M, Iliescu DG, Novac L, Cernea N. First trimester two- and four-dimensional cardiac scan: intra- and interobserver agreement, comparison between methods and benefits of color Doppler technique. Ultrasound Obstet Gynecol 2013; 42: 659–668. [DOI] [PubMed] [Google Scholar]
- 12.DeVore GR, Polanco B, Sklansky MS, Platt LD. The ‘spin’ technique: a new method for examination of the fetal outflow tracts using three-dimensional ultrasound. Ultrasound Obstet Gynecol 2004; 24: 72–82. [DOI] [PubMed] [Google Scholar]
- 13.Espinoza J, Gonçalves LF, Lee W, et al. The use of the minimum projection mode in 4-dimensional examination of the fetal heart with spatiotemporal image correlation. J Ultrasound Med 2004; 23: 1337–1348. [DOI] [PubMed] [Google Scholar]
- 14.Gonçalves LF, Romero R, Espinoza J, et al. Four-dimensional ultrasonography ofthe fetal heart using color Doppler spatiotemporal image correlation. J Ultrasound Med 2004; 23: 473–481. [DOI] [PubMed] [Google Scholar]
- 15.Chaoui R, Heling KS. New developments in fetal heart scanning: three- and four-dimensional fetal echocardiography. Semin Fetal Neonatal Med 2005; 10: 567–577. [DOI] [PubMed] [Google Scholar]
- 16.Espinoza J, Kusanovic JP, Gonçalves LF, et al. A novel algorithm for comprehensive fetal echocardiography using 4-dimensional ultrasonography and tomographic imaging. J Ultrasound Med 2006; 25: 947–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yagel S, Cohen SM, Shapiro I, Valsky DV. 3D and 4D ultrasound in fetal cardiac scanning: a new look at the fetal heart. Ultrasound Obstet Gynecol 2007; 29: 81–95. [DOI] [PubMed] [Google Scholar]
- 18.Molina FS, Faro C, Sotiriadis A, Dagklis T, Nicolaides KH. Heart stroke volume and cardiac output by four-dimensional ultrasound in normal fetuses. Ultrasound Obstet Gynecol 2008; 32: 181–187. [DOI] [PubMed] [Google Scholar]
- 19.Rizzo G, Capponi A, Muscatello A, Cavicchioni O, Vendola M, Arduini D. Examination of the fetal heart by four-dimensional ultrasound with spatiotemporal image correlation during routine second-trimester examination: the ‘three-steps technique’. Fetal Diagn Ther 2008; 24:126–131. [DOI] [PubMed] [Google Scholar]
- 20.Tutschek B, Sahn DJ. Semi-automatic segmentation of fetal cardiac cavities: progress towards an automated fetal echocardiogram. Ultrasound Obstet Gynecol 2008; 32: 176–180. [DOI] [PubMed] [Google Scholar]
- 21.Bennasar M, Martínez JM, Olivella A, et al. Feasibility and accuracy of fetal echocardiography using four-dimensional spatiotemporal image correlation technology before 16 weeks’ gestation. Ultrasound Obstet Gynecol 2009; 33: 645–651. [DOI] [PubMed] [Google Scholar]
- 22.Uittenbogaard LB, Haak MC, Spreeuwenberg MD, van Vugt JM. Fetal cardiac function assessed with four-dimensional ultrasound imaging using spatiotemporal image correlation. Ultrasound Obstet Gynecol 2009; 33: 272–281. [DOI] [PubMed] [Google Scholar]
- 23.Turan S, Turan OM, Ty-Torredes K, Harman CR, Baschat AA. Standardization of the first-trimester fetal cardiac examination using spatiotemporal image correlation with tomographic ultrasound and color Doppler imaging. Ultrasound Obstet Gynecol 2009; 33: 652–656. [DOI] [PubMed] [Google Scholar]
- 24.Gonçalves LF, Espinoza J, Romero R, et al. Four-dimensional ultrasonography of the fetal heart using a novel Tomographic Ultrasound Imaging display. J Perinat Med 2006; 34: 39–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen L, Mangers K, Grobman WA, Platt LD. Satisfactory visualization rates of standard cardiac views at 18 to 22 weeks’ gestation using spatiotemporal image correlation. J Ultrasound Med 2009; 28: 1645–1650. [DOI] [PubMed] [Google Scholar]
- 26.Abuhamad A, Chaoui R (eds). A Practical Guide to Fetal Echocardiography: Normal and Abnormal Hearts. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 27.Rizzo G, Capponi A, Pietrolucci ME, Arduini D. Role of sonographic automatic volume calculation in measuring fetal cardiac ventricular volumes using 4-dimensional sonography: comparison with virtual organ computer-aided analysis. J Ultrasound Med 2010; 29: 261–270. [DOI] [PubMed] [Google Scholar]
- 28.Jantarasaengaram S, Vairojanavong K. Eleven fetal echocardiographic planes using 4-dimensional ultrasound with spatio-temporal image correlation (STIC): a logical approach to fetal heart volume analysis. Cardiovasc Ultrasound 2010; 8: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yeo L, Romero R, Jodicke C, et al. Four-chamber view and ‘swing technique’ (FAST) echo: a novel and simple algorithm to visualize standard fetal echocardiographic planes. Ultrasound Obstet Gynecol 2011; 37: 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamill N, Yeo L, Romero R, et al. Fetal cardiac ventricular volume, cardiac output, and ejection fraction determined with 4-dimensional ultrasound using spatiotemporal image correlation and virtual organ computer-aided analysis. Am J Obstet Gynecol 2011; 205: 76.e1-e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luewan S, Yanase Y, Tongprasert F, Srisupundit K, Tongsong T. Fetal cardiac dimensions at 14–40 weeks’ gestation obtained using cardio-STIC-M. Ultrasound Obstet Gynecol 2011; 37: 416–422. [DOI] [PubMed] [Google Scholar]
- 32.Wang N, Xie HN, Peng R, Zheng J, Zhu YX. Accuracy, agreement, and reliability of fetal cardiac measurements using 4-dimensional spatiotemporal image correlation. J Ultrasound Med 2012; 31: 1719–1726. [DOI] [PubMed] [Google Scholar]
- 33.Messing B, Gilboa Y, Lipschuetz M, Valsky DV, Cohen SM, Yagel S. Fetal tricuspid annular plane systolic excursion (f-TAPSE): evaluation of fetal right heart systolic function with conventional M-mode ultrasound and spatiotemporal image correlation (STIC) M-mode. Ultrasound Obstet Gynecol 2013; 42:182–188. [DOI] [PubMed] [Google Scholar]
- 34.Yeo L, Romero R, Jodicke C, et al. Simple targeted arterial rendering (STAR) technique: a novel and simple method to visualize the fetal cardiac outflow tracts. Ultrasound Obstet Gynecol 2011; 37: 549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Espinoza J Contemporary clinical applications of spatio-temporal image correlation in prenatal diagnosis. Curr Opin Obstet Gynecol 2011; 23: 94–102. [DOI] [PubMed] [Google Scholar]
- 36.Espinoza J, Lee W, Viñals F, Martinez JM, Bennasar M, Rizzo G, Belfort M. Collaborative study of 4-dimensional fetal echocardiography in the first trimester of pregnancy. J Ultrasound Med 2014; 33:1079–1084. [DOI] [PubMed] [Google Scholar]
- 37.Avnet H, Mazaaki E, Shen O, Cohen S, Yagel S. Evaluating spatiotemporal image correlation technology as a tool for training nonexpert sonographers to perform examinations of the fetal heart. J Ultrasound Med. 2016; 35:111–119. [DOI] [PubMed] [Google Scholar]
- 38.Koestenberger M, Raith W, Ravekes W. Importance of quantifiable right heart systolic function evaluation using tricuspid annular plane systolic excursion (TAPSE) in fetuses and neonates. Ultrasound Obstet Gynecol 2013; 42: 367. [DOI] [PubMed] [Google Scholar]
- 39.Acharya G Measurement of atrioventricular annular plane displacement has been revived: will it prove to be useful in assessing fetal cardiac function? Ultrasound Obstet Gynecol 2013; 42: 125–129. [DOI] [PubMed] [Google Scholar]
- 40.Messing B, Cohen SM, Valsky DV, et al. Fetal cardiac ventricle volumetry in the second half of gestation assessed by 4D ultrasound using STIC combined with inversion mode. Ultrasound Obstet Gynecol 2007; 30: 142–151. [DOI] [PubMed] [Google Scholar]
- 41.Rizzo G, Capponi A, Cavicchioni O, Vendola M, Arduini D. Fetal cardiac stroke volume determination by four-dimensional ultrasound with spatio-temporal image correlation compared with two-dimensional and Doppler ultrasonography. Prenat Diagn 2007; 27: 1147–1150. [DOI] [PubMed] [Google Scholar]
- 42.Schoonderwaldt EM, Groenenberg IA, Hop WC, Wladimiroff JW, Steegers EA. Reproducibility of echocardiographic measurements of human fetal left ventricular volumes and ejection fractions using four-dimensional ultrasound with the spatio-temporal image correlation modality. Eur J Obstet Gynecol Reprod Biol 2012; 160: 22–29. [DOI] [PubMed] [Google Scholar]
- 43.Messing B, Cohen SM, Valsky DV, et al. Fetal heart ventricular mass obtained by STIC acquisition combined with inversion mode and VOCAL. Ultrasound Obstet Gynecol 2011; 38: 191–197. [DOI] [PubMed] [Google Scholar]
- 44.Simioni C, Nardozza LM, Araujo Júnior E, et al. Heart stroke volume, cardiac output, and ejection fraction in 265 normal fetus in the second half of gestation assessed by 4D ultrasound using spatio-temporal image correlation. J Matern Fetal Neonatal Med 2011; 24: 1159–1167. [DOI] [PubMed] [Google Scholar]
- 45.Uittenbogaard LB, Haak MC, Tromp CH, Terwee CB, Van Vugt JM. Reliability of fetal cardiac volumetry using spatiotemporal image correlation: assessment of in-vivo and in-vitro measurements. Ultrasound Obstet Gynecol 2010; 36: 308–314. [DOI] [PubMed] [Google Scholar]
- 46.Hamill N, Romero R, Hassan S, et al. The fetal cardiovascular response to increased placental vascular impedance to flow determined with 4-dimensional ultrasound using spatiotemporal image correlation and virtual organ computer-aided analysis. Am J Obstet Gynecol 2013; 208: 153.e1-e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Votino C, Cos T, Abu-Rustum R, et al. Use of spatiotemporal image correlation at 11–14 weeks’ gestation. Ultrasound Obstet Gynecol 2013; 42: 669–678. [DOI] [PubMed] [Google Scholar]
- 48.Zidere V, Pushparajah K, Allan LD, Simpson JM. Three-dimensional fetal echocardiography for prediction of postnatal surgical approach in double outlet right ventricle: a pilot study. Ultrasound Obstet Gynecol 2013; 42: 421–425. [DOI] [PubMed] [Google Scholar]
- 49.Pinto NM, Nelson R, Puchalski M, Metz TD, Smith KJ. Cost-effectiveness of prenatal screening strategies for congenital heart disease. Ultrasound Obstet Gynecol 2014; 44: 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu LH, Wang N, Xie HN, Du L, Peng R. Cardiovascular Z-scores in fetuses with tetralogy of Fallot. Ultrasound Obstet Gynecol 2014; 44: 674–681. [DOI] [PubMed] [Google Scholar]
- 51.Adriaanse BM, Bartelings MM, van Vugt JM, Chaoui R, Gittenberger-de Groot AC, Haak MC. Differential and linear insertion of atrioventricular valves: a useful tool? Ultrasound Obstet Gynecol 2014; 44: 568–574. [DOI] [PubMed] [Google Scholar]
- 52.Gonçalves LF, Espinoza J, Lee W, Mazor M, Romero R. Three- and four-dimensional reconstruction of the aortic and ductal arches using inversion mode: a new rendering algorithm for visualization of fluid-filled anatomical structures. Ultrasound Obstet Gynecol 2004; 24: 696–698. [DOI] [PubMed] [Google Scholar]
- 53.Gonçalves LF, Espinoza J, Romero R, et al. A systematic approach to prenatal diagnosis of transposition of the great arteries using 4-dimensional ultrasonography with spatiotemporal image correlation. J Ultrasound Med 2004; 23: 1225–1231. [DOI] [PubMed] [Google Scholar]
- 54.Gonçalves LF, Espinoza J, Lee W, et al. A new approach to fetal echocardiography: digital casts of the fetal cardiac chambers and great vessels for detection of congenital heart disease. J Ultrasound Med 2005; 24: 415–424. [DOI] [PubMed] [Google Scholar]
- 55.Viñals F, Mandujano L, Vargas G, Giuliano A. Prenatal diagnosis of congenital heart disease using four-dimensional spatio-temporal image correlation (STIC) telemedicine via an Internet link: a pilot study. Ultrasound Obstet Gynecol 2005; 25: 25–31. [DOI] [PubMed] [Google Scholar]
- 56.Ghi T, Cera E, Segata M, Michelacci L, Pilu G, Pelusi G. Inversion mode spatio-temporal image correlation (STIC) echocardiography in three-dimensional rendering of fetal ventricular septal defects. Ultrasound Obstet Gynecol 2005; 26: 679–680. [DOI] [PubMed] [Google Scholar]
- 57.Paladini D, Sglavo G, Greco E, Nappi C. Cardiac screening by STIC: cansonologists performing the 20-week anomaly scan pick up outflow tract abnormalities by scrolling the A-plane of STIC volumes? Ultrasound Obstet Gynecol 2008; 32: 865–870. [DOI] [PubMed] [Google Scholar]
- 58.Gindes L, Hegesh J, Weisz B, Gilboa Y, Achiron R. Three and four dimensional ultrasound: a novel method for evaluating fetal cardiac anomalies. Prenat Diagn 2009; 29: 645–653. [DOI] [PubMed] [Google Scholar]
- 59.Hata T, Mashima M, Ito M, Uketa E, Mori N, Ishimura M. Three-dimensional HDlive rendering images of the fetal heart. Ultrasound Med Biol 2013; 39: 1513–1517. [DOI] [PubMed] [Google Scholar]
- 60.Bennasar M, Martínez JM, Gómez O, et al. Accuracy of four-dimensional spatiotemporal image correlation echocardiography in the prenatal diagnosis of congenital heart defects. Ultrasound Obstet Gynecol 2010; 36: 458–464. [DOI] [PubMed] [Google Scholar]
- 61.Xiong Y, Liu T, Wu Y, et al. Comparison of real-time three-dimensional echocardiography and spatiotemporal image correlation in assessment of fetal interventricular septum. J Matern Fetal Neonatal Med 2012; 25: 2333–2338. [DOI] [PubMed] [Google Scholar]
- 62.Espinoza J, Lee W, Comstock C, et al. Collaborative study on 4-dimensional echocardiography for the diagnosis of fetal heart defects: the COFEHD study. J Ultrasound Med 2010; 29: 1573–1580. [DOI] [PubMed] [Google Scholar]
- 63.Zhang M, Pu DR, Zhou QC, Peng QH, Tian LQ. Four-dimensional echocardiography with B-flow imaging and spatiotemporal image correlation in the assessment of congenital heart defects. Prenat Diagn 2010; 30: 443–448. [DOI] [PubMed] [Google Scholar]
- 64.Hata T, Tanaka H, Noguchi J, Dai SY, Yamaguchi M, Yanagihara T. Four-dimensional volume-rendered imaging of the fetal ventricular outflow tracts and great arteries using inversion mode for detection of congenital heart disease. J Obstet Gynaecol Res 2010; 36: 513–518. [DOI] [PubMed] [Google Scholar]
- 65.Adriaanse BM, Tromp CH, Simpson JM, et al. Interobserver agreement in detailedprenatal diagnosis of congenital heart disease by telemedicine using four-dimensional ultrasound with spatiotemporal image correlation. Ultrasound Obstet Gynecol 2012; 39: 203–209. [DOI] [PubMed] [Google Scholar]
- 66.Hongmei W, Ying Z, Ailu C, Wei S. Novel application of four-dimensional sonography with B-flow imaging and spatiotemporal image correlation in the assessment of fetal congenital heart defects. Echocardiography 2012; 29: 614–619. [DOI] [PubMed] [Google Scholar]
- 67.He Y, Wang J, Gu X, et al. Application of spatio-temporal image correlation technology in the diagnosis of fetal cardiac abnormalities. Exp Ther Med 2013; 5: 1637–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Qin Y, Zhang Y, Zhou X, et al. Four-dimensional echocardiography with spatiotemporal image correlation and inversion mode for detection of congenital heart disease. Ultrasound Med Biol 2014; 40: 1434–1441. [DOI] [PubMed] [Google Scholar]
- 69.Volpe P, Tuo G, De Robertis V, et al. Fetal interrupted aortic arch: 2D-4D echocardiography, associations and outcome. Ultrasound Obstet Gynecol 2010; 35: 302–309. [DOI] [PubMed] [Google Scholar]
- 70.Myers SA, Fresquez M, Hamill N. Four-dimensional sonography of the fetal heart with spatiotemporal image correlation directed at the interventricular septum. J Ultrasound Med 2007; 26: 1071–1075. [DOI] [PubMed] [Google Scholar]
- 71.Yagel S, Cohen SM, Rosenak D, et al. Added value of three-/four-dimensional ultrasound in offline analysis and diagnosis of congenital heart disease. Ultrasound Obstet Gynecol. 2011; 37:432–437. [DOI] [PubMed] [Google Scholar]
- 72.Espinoza J, Hassan SS, Gotsch F, et al. A systematic approach to the use of the multiplanar display in evaluation of abnormal vascular connections to the fetal heart using 4-dimensional ultrasonography. J Ultrasound Med 2007; 26: 1461–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gómez-Montes E, Herraiz I, Mendoza A, Escribano D, Galindo A. Prediction of coarctation of the aorta in the second half of pregnancy. Ultrasound Obstet Gynecol 2013; 41: 298–305. [DOI] [PubMed] [Google Scholar]
- 74.Ganesan S, Brook MM, Silverman NH, Moon-Grady AJ. Prenatal findings in total anomalous pulmonary venous return: a diagnostic road map starts with obstetric screening views. J Ultrasound Med 2014; 33:1193–1207. [DOI] [PubMed] [Google Scholar]
- 75.Menahem S, Rotstein A, Meagher S. Rightward convexity of the great vessel arising from the anterior ventricle: a novel fetal marker for transposition of the great arteries. Ultrasound Obstet Gynecol 2013; 41: 168–171. [DOI] [PubMed] [Google Scholar]
- 76.D’Alton ME, DeCherney AH. Prenatal diagnosis. N Engl J Med 1993; 328: 114–120. [DOI] [PubMed] [Google Scholar]
- 77.Crane JP, LeFevre ML, Winborn RC, et al. A randomized trial of prenatal ultrasonographic screening: impact on the detection, management, and outcome of anomalous fetuses. The RADIUS Study Group. Am J Obstet Gynecol 1994; 171: 392–399. [DOI] [PubMed] [Google Scholar]
- 78.Abu-Harb M, Hey E, Wren C. Death in infancy from unrecognised congenital heart disease. Arch Dis Child 1994; 71: 3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Allan L, Benacerraf B, Copel JA, et al. Isolated major congenital heart disease. Ultrasound Obstet Gynecol 2001; 17: 370–379. [DOI] [PubMed] [Google Scholar]
- 80.Carvalho JS, Mavrides E, Shinebourne EA, Campbell S, Thilaganathan B. Improving the effectiveness of routine prenatal screening for major congenital heart defects. Heart 2002; 88: 387–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hunter S, Heads A, Wyllie J, Robson S. Prenatal diagnosis of congenital heart disease in the northern region of England: benefits of a training programme for obstetric ultrasonographers. Heart 2000; 84: 294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rustico MA, Benettoni A, D’Ottavio G, et al. Early screening for fetal cardiac anomalies by transvaginal echocardiography in an unselected population: the role of operator experience. Ultrasound Obstet Gynecol 2000; 16: 614–619. [DOI] [PubMed] [Google Scholar]
- 83.Tegnander E, Eik-Nes SH. The examiner’s ultrasound experience has a significant impact on the detection rate of congenital heart defects at the second-trimester fetal examination. Ultrasound Obstet Gynecol 2006; 28: 8–14. [DOI] [PubMed] [Google Scholar]
- 84.Wong SF, Chan FY, Cincotta RB, Lee-Tannock A, Ward C. Factors influencing the prenatal detection of structural congenital heart diseases. Ultrasound Obstet Gynecol 2003; 21: 19–25. [DOI] [PubMed] [Google Scholar]
- 85.Baardman ME, du Marchie Sarvaas GJ, de Walle HE, et al. Impact of introduction of 20-week ultrasound scan on prevalence and fetal and neonatal outcomes in cases of selected severe congenital heart defects in The Netherlands. Ultrasound Obstet Gynecol 2014; 44: 58–63. [DOI] [PubMed] [Google Scholar]
- 86.Tutschek B, Sahn DJ. Three-dimensional echocardiography for studies of the fetal heart: present status and future perspectives. Cardiol Clin 2007; 25: 341–355. [DOI] [PubMed] [Google Scholar]
- 87.Yeo L, Romero R. Fetal Intelligent Navigation Echocardiography (FINE): a novel method for rapid, simple, and automatic examination of the fetal heart. Ultrasound Obstet Gynecol 2013; 42:268–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gonçalves LF, Lee W, Espinoza J, Romero R. Examination of the fetal heart by four-dimensional (4D) ultrasound with spatio-temporal image correlation (STIC). Ultrasound Obstet Gynecol 2006; 27: 336–348. [DOI] [PubMed] [Google Scholar]
- 89.Bega G Volume sonography: core concepts for clinical practice. In Sonography in Obstetrics & Gynecology: Principles & Practice, Seventh Edition, Fleischer AC, Toy EC, Lee W, Manning FA, Romero R (eds). The McGraw-Hill Companies, Inc: Columbus, 2011; 1134–1169. [Google Scholar]
- 90.Turan S, Turan OM, Desai A, Harman CR, Baschat AA. First-trimester fetal cardiac examination using spatiotemporal image correlation, tomographic ultrasound and color Doppler imaging for the diagnosis of complex congenital heart disease in high-risk patients. Ultrasound Obstet Gynecol 2014; 44: 562–567. [DOI] [PubMed] [Google Scholar]
- 91.Edelman SK. Understanding Ultrasound Physics, Third Edition, Edelman SK (ed). Vertex Communications: China, 2007. [Google Scholar]
- 92.DeVore GR, Sklansky MS. Three-dimensional imaging of the fetal heart: current applications and future directions. Prog Pediatr Cardiol 2006; 22: 9–29. [Google Scholar]
- 93.Angiulli A, Tai A, Easterbrook S. Voluson. Electronic 4D Imaging – Designed for Women’s Health. September2014. [Google Scholar]
- 94.Paladini D Standardization of on-screen fetal heart orientation prior to storage of spatio temporal image correlation (STIC) volume datasets. Ultrasound Obstet Gynecol 2007; 29: 605–611. [DOI] [PubMed] [Google Scholar]
- 95.Gonçalves LF, Nien JK, Espinoza J, et al. What does 2-dimensional imaging add to 3- and 4-dimensional obstetric ultrasonography? J Ultrasound Med 2006; 25: 691–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Espinoza J, Romero R, Kusanovic JP, et al. The role of the sagittal view of the ductal arch in identification of fetuses with conotruncal anomalies using 4-dimensional ultrasonography. J Ultrasound Med 2007; 26: 1181–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Uittenbogaard LB, Haak MC, Spreeuwenberg MD, Van Vugt JM. A systematic analysis of the feasibility of four-dimensional ultrasound imaging using spatiotemporal image correlation in routine fetal echocardiography. Ultrasound Obstet Gynecol 2008; 31: 625–632. [DOI] [PubMed] [Google Scholar]
- 98.Garcia M, Yeo L, Romero R, et al. Prospective evaluation of the fetal heart using Fetal Intelligent Navigation Echocardiography (FINE). Ultrasound Obstet Gynecol 2016; 47:450–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Allan LD, Tynan MJ, Campbell S, Wilkinson JL, Anderson RH. Echocardiographic and anatomical correlates in the fetus. Br Heart J 1980; 44: 444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tegnander E, Eik-Nes SH, Linker DT. Incorporating the four-chamber view of the fetal heart into the second-trimester routine fetal examination. Ultrasound Obstet Gynecol 1994; 4: 24–28. [DOI] [PubMed] [Google Scholar]
- 101.Vergani P, Mariani S, Ghidini A, et al. Screening for congenital heart disease with the four-chamber view of the fetal heart. Am J Obstet Gynecol 1992; 167: 1000–1003. [DOI] [PubMed] [Google Scholar]
- 102.Achiron R, Glaser J, Gelernter I, Hegesh J, Yagel S. Extended fetal echocardiographic examination for detecting cardiac malformations in low risk pregnancies. BMJ 1992; 304: 671–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bega G, Kuhlman K, Lev-Toaff A, Kurtz A, Wapner R. Application of three-dimensional ultrasonography in the evaluation of the fetal heart. J Ultrasound Med 2001; 20: 307–313. [DOI] [PubMed] [Google Scholar]
- 104.Sharland GK, Allan LD. Screening for congenital heart disease prenatally. Results of a 2 1/2-year study in the South East Thames Region. Br J Obstet Gynaecol 1992; 99: 220–225. [DOI] [PubMed] [Google Scholar]
- 105.Tongsong T, Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K. Cardio-STIC (spatio-temporal image correlation) as genetic ultrasound of fetal Down syndrome. J Matern Fetal Neonatal Med 2015; 28:1843–1949. [DOI] [PubMed] [Google Scholar]
- 106.Yeo L, Romero R. Intelligent navigation to improve obstetrical sonography. Ultrasound Obstet Gynecol 2016; 47:403–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jatavan T, Tongsong T. Comparison of fetal cardiac spatiotemporal image correlation segmental analysis between cardiac- and body-based scrolling. J Ultrasound Med 2013; 32: 2125–2129. [DOI] [PubMed] [Google Scholar]
- 108.Viñals F Current experience and prospect of internet consultation in fetal cardiac ultrasound. Fetal Diagn Ther 2011; 30: 83–87. [DOI] [PubMed] [Google Scholar]
- 109.Zhang Y, Ding C, Fan M, et al. Evaluation of normal fetal pulmonary veins using B-flow imaging with spatiotemporal image correlation and by traditional color Doppler echocardiography. Prenat Diagn 2012; 32: 1186–1191. [DOI] [PubMed] [Google Scholar]
- 110.Abuhamad AZ. Standardization of 3-dimensional volumes in obstetric sonography: a required step for training and automation. J Ultrasound Med 2005; 24: 397–401. [DOI] [PubMed] [Google Scholar]
- 111.Yagel S, Benachi A, Bonnet D, et al. Rendering in fetal cardiac scanning: the intracardiac septa and the coronal atrioventricular valve planes. Ultrasound Obstet Gynecol 2006; 28: 266–274. [DOI] [PubMed] [Google Scholar]
- 112.Viñals F, Pacheco V, Giuliano A. Fetal atrioventricular valve junction in normal fetuses and in fetuses with complete atrioventricular septal defect assessed by 4D volume rendering. Ultrasound Obstet Gynecol 2006; 28: 26–31. [DOI] [PubMed] [Google Scholar]
- 113.ImproveEyesightHQ.com. Double vision: causes, symptoms and treatment. Web site: http://www.improveeyesighthq.com/double-vision.html.Accessed January 23, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.