Supplemental Digital Content is available in the text.
Problem
The most effective way to train clinicians to safely don and doff personal protective equipment (PPE) and perform aerosol-generating procedures (AGPs), such as intubations, is unknown when clinician educators are unavailable, as they have been during the COVID-19 pandemic. Proper PPE and airway management techniques are critical to prevent the transmission of respiratory illnesses such as COVID-19.
Approach
In March 2020, the authors implemented a structured train-the-trainers curriculum to teach PPE techniques and a modified airway management algorithm for suspected COVID-19 patients. A single emergency medicine physician trainer taught 17 subsequent emergency medicine and critical care physician trainers the proper PPE and airway management techniques. The initial trainer and 7 of the subsequent trainers then instructed 99 other emergency medicine resident and attending physicians using in situ simulation. Trainers and learners completed retrospective pre–post surveys to assess their comfort teaching the material and performing the techniques, respectively.
Outcomes
The surveys demonstrated a significant increase in the trainers’ comfort in teaching simulation-based education, from 4.00 to 4.53 on a 5-point Likert scale (P < .005), and in teaching the airway management techniques through simulation, from 2.47 to 4.47 (P < .001). There was no difference in the change in comfort level between those learners who were taught by the initial trainer and those who were taught by the subsequent trainers. These results suggest that the subsequent trainers were as effective in teaching the simulation material as the initial trainer.
Next Steps
Work is ongoing to investigate clinician- and patient-specific outcomes, including PPE adherence, appropriate AGP performance, complication rate, and learners’ skill retention. Future work will focus on implementing similar train-the-trainers strategies for other health professions, specialties, and high-risk or rare procedures.
Problem
In a pandemic, especially one that is as severe as COVID-19, safety precautions and attention to personal protective equipment (PPE) are paramount. 1 Clinicians must correctly don and doff PPE and perform aerosol-generating procedures (AGPs), such as intubations, in a modified manner to minimize disease transmission. For example, intubations can be customized to maximize safety using techniques such as video laryngoscopy, addition of a viral filter, and modification of preoxygenation strategies to limit aerosol generation. In situ simulation training, or simulation that is integrated into the clinical environment, provides a valuable opportunity for clinicians to practice PPE and airway management techniques in situations where failure to perform properly has significant consequences. 2,3
The availability of traditional clinical educators became limited during the COVID-19 pandemic as these educators were needed to provide patient care. To train clinicians to safely don and doff PPE and perform proper airway management techniques, an effective instructional strategy was needed to rapidly disseminate this important knowledge. The train-the-trainers model was an attractive and sustainable option. 4 To our knowledge, although a train-the-trainers curriculum has previously been implemented to teach clinical skills, such as point-of-care ultrasound, emergency care, and PPE adherence, 5–7 it has never been used to teach in situ simulation training for airway management during a pandemic.
In this report, we describe the rapid and effective dissemination of a PPE and airway management in situ simulation training using a structured train-the-trainers curriculum. We demonstrate that a single trainer was able to quickly train additional trainers who had no specialized education background to then teach frontline clinicians appropriate PPE and airway management techniques, all during the COVID-19 pandemic. Furthermore, we developed assessment tools to quantitatively measure trainer and learner outcomes. We propose that other specialties and institutions can implement similar strategies to disseminate and sustain essential clinical knowledge during future pandemics or in other resource-limited settings.
Approach
We developed a structured curriculum to teach appropriate donning and doffing of PPE and a modified airway management algorithm for suspected COVID-19 patients using in situ simulation. 8,9 The modified airway management algorithm and simulation scenario were developed by institutional leaders, including our initial trainer (C.H.H.), who had experience in health care operations, education, and critical care. 8,9 The algorithm was tested and revised multiples times using the plan–do–study–act process and feedback from its use in both the simulated and clinical environments. 8,9 Our prior work had demonstrated that learners achieved significant improvement in comfort with donning and doffing PPE, role identification, and AGP management for suspected COVID-19 patients after the in situ simulation. 8 The work we describe in this report focuses on the implementation of a structured train-the-trainers curriculum to disseminate material to multiple clinicians with consistent outcomes.
The initial trainer used a structured curriculum to teach other clinicians to become trainers (see the Outcomes section for a timeline of curriculum implementation and evaluation). This curriculum was based on prior work on objective structured teaching exercises that emphasize the following steps 10: (1) clarification of the goal, (2) clarification of the target audience, (3) identification of teaching skills to be addressed, (4) preparation of a scenario, (5) assessment of the new teacher, (6) identification of the learner, and (7) evaluation of the activity.
The primary educational goal was to train trainers to effectively teach appropriate PPE and airway management techniques for suspected COVID-19 patients using in situ simulation. To assess the teaching skills of the trainers, we developed and piloted a skills assessment checklist that evaluated critical actions including: adherence to the algorithm, assessment of learner understanding, and management of multiple learners of different skill levels (see Supplemental Digital Appendix 1 at http://links.lww.com/ACADMED/B95). This tool was developed by education and critical care faculty (W.J.P., C.H.H.) and reviewed by education faculty (B.W.M., E.D.L., C.Harvey) to assess for clarity and completeness and to contribute to content and face validity. The checklist was piloted with a group of emergency medicine physicians performing the in situ simulation training.
The curriculum lasted 60 minutes, during which the initial trainer first prebriefed the subsequent trainers on the learning objectives of the airway management algorithm and in situ simulation. The initial trainer then summarized in detail the airway management algorithm and simulation script. Anticipated questions and potential learner errors were also discussed, and strategies to answer these questions and correct these errors were highlighted. Next, the initial trainer provided the subsequent trainers with the opportunity to practice and ask questions. Finally, videos of the simulation scenario and appropriate donning and doffing of PPE were available to the subsequent trainers to review asynchronously. 9
Our target trainers were emergency medicine and critical care physicians. Through this approach, the initial trainer (a dual-boarded emergency medicine and critical care physician) taught 14 emergency medicine and 3 critical care trainers. Seven of the 14 emergency medicine trainers along with the initial trainer then taught 99 additional emergency medicine learners using in situ simulation.
All 17 subsequent trainers completed a retrospective pre–post 5-point Likert scale survey (1 = extremely uncomfortable, 2 = somewhat uncomfortable, 3 = neither comfortable nor uncomfortable, 4 = somewhat comfortable, 5 = extremely comfortable) to assess their comfort level in teaching the simulation training and airway management algorithm before and following the train-the-trainers curriculum. In addition, the learners completed a separate retrospective pre–post 5-point Likert scale survey (same scale as above) to assess their comfort with the PPE and airway management techniques. These surveys were developed by education and critical care faculty (W.J.P., B.W.M., C.H.H.) and reviewed by education faculty (R.V.T., E.D.L., C.Harvey) to ensure content and criterion validity. The surveys were created using the Qualtrics online platform (Provo, Utah) and were piloted among the author group to assess clarity.
Two-tailed paired t tests were performed to compare the subsequent trainers’ responses before and after attending the train-the-trainers curriculum and to compare responses from learners in the sessions taught by the initial trainer to those from learners in the sessions taught by the subsequent trainers. We considered P < .05 to be statistically significant, and we used SAS 9.4 (SAS, Cary, North Carolina) to perform the statistical analysis.
The University of Michigan Medical School Institutional Review Board deemed this study exempt.
Outcomes
To demonstrate rapid dissemination of COVID-19 airway management knowledge, we measured the following outcomes: number of learners and timing of teaching sessions, trainer evaluations of the train-the-trainers curriculum, and comparison of learner evaluations from sessions taught by the subsequent trainers and from those taught by the initial trainer. The primary focus of our evaluation was the emergency medicine trainers, and further work is ongoing to assess outcomes from the critical care trainers.
Development of the airway management algorithm and simulation training began in early March 2020. On March 16, the initial trainer trained 14 emergency medicine and 3 critical care trainers to teach PPE techniques and a modified airway management algorithm for suspected COVID-19 patients. Over the next week (March 16–22), the initial trainer and 7 of the emergency medicine trainers taught 71 resident and attending emergency medicine physicians (57% of all emergency medicine physicians at our institution) the PPE techniques and modified airway management algorithm by holding 45-minute just-in-time in situ simulation sessions 3 times a day, before the standard shift change. The number of sessions decreased to 2 times a day after that first week. These 8 trainers reached 99 learners (80% of all emergency medicine physicians) in 23 days, with sessions ending on April 7 (see Supplemental Digital Appendix 2 at http://links.lww.com/ACADMED/B95 for the number of simulation learners by date).
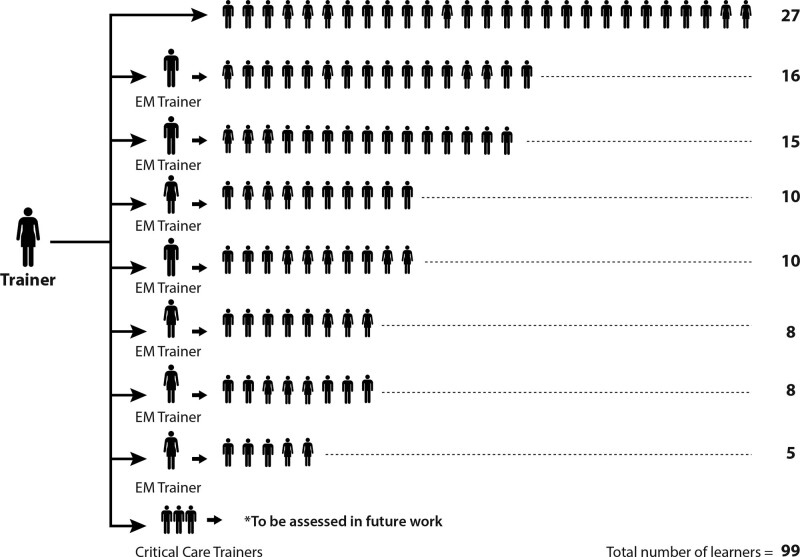
The initial trainer taught 27 learners, while the 7 subsequent emergency medicine trainers taught 72 learners (see Figure 1). The remaining 7 emergency medicine trainers were taught the PPE techniques and modified airway management algorithm in anticipation of expanding the curriculum to other clinicians, including nurses, respiratory therapists, and technicians.
Figure 1.
Flowchart for a train-the-trainers curriculum focused on teaching appropriate personal protective equipment (PPE) and airway management techniques for suspected COVID-19 patients, University of Michigan Medical School, 2020. The initial trainer trained 14 emergency medicine (EM) and 3 critical care physicians as subsequent trainers. The initial trainer and 7 of the EM subsequent trainers then taught 99 EM physicians the PPE and airway management content using in situ simulation.
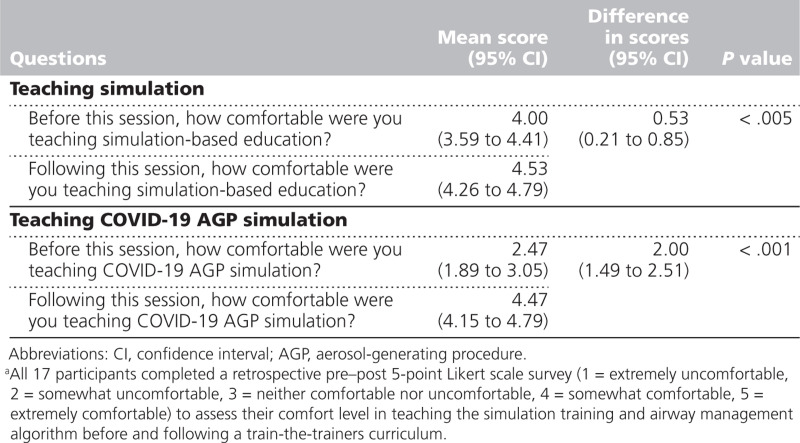
Evaluations of the train-the-trainers curriculum revealed statistically significant increases in trainers’ comfort teaching both simulation-based education and airway management simulation. All 17 trainers (100% response rate) completed the survey, which demonstrated an increase from 4.00 to 4.53 in comfort teaching simulation-based education (P < .005) and an increase from 2.47 to 4.47 in comfort teaching COVID-19 airway management simulation (P < .001; see Table 1).
Table 1.
Trainer Evaluations of a Train-the-Trainers Curriculum, University of Michigan Medical School, 2020a
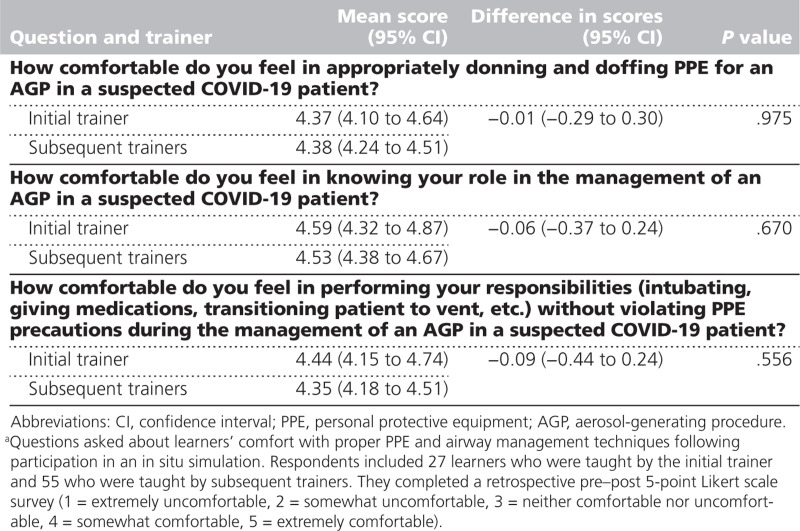
The emergency medicine learners completed their evaluations at the end of each session (82/99, 83% response rate). Overall, their comfort level in donning and doffing PPE and in airway management techniques significantly increased from 2.93 to 4.35 (P < .01, n = 82) after the in situ simulation. 8 Notably, there was no significant difference in learners’ comfort levels with donning and doffing PPE (4.37 and 4.38, P = .975), knowing their role in AGP management of suspected COVID-19 patients (4.59 and 4.53, P = .670), or AGP performance for suspected COVID-19 patients (4.44 and 4.35, P = .556) between learners taught by the initial trainer and those taught by the subsequent trainers (see Table 2).
Table 2.
Learner Evaluations of Sessions Taught by the Initial Trainer Compared With Those Taught by Subsequent Trainers, University of Michigan Medical School, 2020a
Learners did not differ in their baseline comfort levels in donning and doffing PPE, knowing their role in AGP management, or AGP performance before participating in the in situ simulation sessions (2.95 and 3.00, P = .831; 3.65 and 3.26, P = .155; and 2.98 and 3.26, P = .350, respectively). Importantly, these data demonstrate that the subsequent emergency medicine trainers were just as effective in teaching COVID-19 airway management as the initial trainer.
Next Steps
In a pandemic, new clinical knowledge often needs to be disseminated rapidly in resource-limited settings. Maximizing clinician safety and prioritizing patient care are paramount, necessitating expeditious innovation of policies and approaches. Here, we demonstrated the rapid and effective dissemination of a train-the-trainers curriculum to teach the appropriate use of PPE and a modified airway management algorithm via in situ simulation. In these sessions, a single trainer was able to quickly train additional trainers to then exponentially scale up the dissemination of these techniques for suspected COVID-19 patients.
While we focused on emergency medicine physicians in the work described in this report, the train-the-trainers curriculum was also taught to clinicians from other disciplines, including anesthesia critical care, pulmonary critical care, and neurocritical care, and it could be expanded further to include other specialties.
Work is ongoing to investigate clinician- and patient-specific outcomes, including PPE adherence, appropriate AGP performance, complication rate, and learners’ skill retention. Future work will focus on implementing similar train-the-trainers strategies for other specialties, such as critical care physicians; health professions, such as nurses, technicians, and respiratory therapists; and high-risk or rare procedures, such as cardiac arrest management for COVID-19 patients.
Acknowledgments:
The authors acknowledge Katelyn Murphy for her assistance in graphic design for this project and the University of Michigan Department of Emergency Medicine faculty, residents, nurses, and staff for their dedication to patients and each other during the COVID-19 pandemic.
Supplementary Material
Footnotes
Supplemental digital content for this article is available at http://links.lww.com/ACADMED/B95.
Funding/Support: Cindy H. Hsu was supported by a National Institutes of Health grant (K12HL133304-01).
Other disclosures: None reported.
Ethical approval: The University of Michigan Medical School Institutional Review Board deemed this study exempt (4/3/2020; HUM00179824).
Previous presentations: This work was presented as an oral presentation at the 2020 Michigan Medicine Barsan Research Forum in Ann Arbor, Michigan, on April 8, 2020.
Contributor Information
Brendan W. Munzer, Email: bmunzer@med.umich.edu.
Ryan V. Tucker, Email: rytucker@med.umich.edu.
Eve D. Losman, Email: losman@med.umich.edu.
Carrie Harvey, Email: hcarrie@med.umich.edu.
Colman Hatton, Email: colman.j.hatton@hitchcock.org.
Nana Sefa, Email: nanas@med.umich.edu.
Ben S. Bassin, Email: bsbassin@med.umich.edu.
Cindy H. Hsu, Email: hcindy@med.umich.edu.
References
- 1.Wiyor HD, Coburn JC, Siegel KL. Impact of clinician personal protective equipment on medical device use during public health emergency: A review. Disaster Med Public Health Prep. 2020; 14:273–283 [DOI] [PubMed] [Google Scholar]
- 2.Nagoshi Y, Cooper LA, Meyer L, et al. Application of an objective structured clinical examination to evaluate and monitor intern’s proficiency of hand hygiene and personal protective equipment use in the United States. J Educ Eval Health Prof. 2019; 16:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braga MS, Tyler MD, Rhoads JM, et al. Effect of just-in-time simulation training on provider performance and patient outcomes for clinical procedures: A systematic review. BMJ Simul Technol Enhanc Learn. 2015; 1:94–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearce J, Mann MK, Jones C, van Buschbach S, Olff M, Bisson JI. The most effective way of delivering a train-the-trainers program: A systematic review. J Contin Educ Health Prof. 2012; 32:215–226 [DOI] [PubMed] [Google Scholar]
- 5.Henwood PC, Mackenzie DC, Rempell JS, et al. A practical guide to self-sustaining point-of-care ultrasound education programs in resource-limited settings. Ann Emerg Med. 2014; 64:277–285.e2 [DOI] [PubMed] [Google Scholar]
- 6.Martel J, Oteng R, Mould-Millman NK, et al. The development of sustainable emergency care in Ghana: Physician, nursing and prehospital care training initiatives. J Emerg Med. 2014; 47:462–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abualenain JT, Al-Alawi MM. Simulation-based training in Ebola personal protective equipment for healthcare workers: Experience from King Abdulaziz University Hospital in Saudi Arabia. J Infect Public Health. 2018; 11:796–800 [DOI] [PubMed] [Google Scholar]
- 8.Munzer BW, Bassin BS, Peterson WJ, et al. In-situ simulation use for rapid implementation and process improvement of COVID-19 airway management. West J Emerg Med. 2020; 21:99–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu CH, Munzer BW, Bassin BS. Preparation and Practice Make Perfect for COVID-19 Airway Management [blog post]. https://web.archive.org/web/20200424151734/https://mcircc.umich.edu/latest-news/preparation-and-practice-make-perfect-for-covid-19-airway-management. Published April 6, 2020 Accessed March 24, 2021
- 10.Boillat M, Bethune C, Ohle E, Razack S, Steinert Y. Twelve tips for using the objective structured teaching exercise for faculty development. Med Teach. 2012; 34:269–273 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.