Abstract
Background
It is unclear whether the recent increase in the number of heart transplants performed annually in the United States is only because of higher availability of donors and if it affected recipients’ survival.
Methods and Results
We examined characteristics of donors and recipients from 2008 to 2012 (n=11 654) and 2013 to 2017 (n=14 556) and compared them with 2003 to 2007 (n=10 869). Cox models examined 30‐day and 1‐year risk of recipients’ death post transplant. From 2013 to 2017, there was an increase in the number of transplanted hearts and number of donor offers but an overall decline in the ratio of hearts transplanted to available donors. Donors between 2013 and 2017 were older, heavier, more hypertensive, diabetic, and likely to have abused illicit drugs compared with previous years. Drug overdose and hepatitis C positive donors were additional contributors to donor risk in recent years. In Cox models, risk of death post transplant between 2013 and 2017 was 15% lower at 30 days (hazard ratio [HR] 0.85; 95% CI, 0.74–0.98) and 21% lower at 1 year (HR, 0.79; 95% CI, 0.73–0.87) and between 2008 and 2012 was 9% lower at 30 days (HR, 0.91; 95% CI, 0.79–1.05) and 14% lower at 1 year (HR, 0.86; 95% CI, 0.79–0.94) compared with 2003 to 2007.
Conclusions
Despite a substantial increase in heart donor offers in recent years, the ratio of transplants performed to available donors has decreased. Even though hearts from donors who are older, more hypertensive, and have diabetes mellitus are being used, overall recipient survival continues to improve. Broader acceptance of drug overdose and hepatitis C positive donors may increase the number and percentage of heart transplants further without jeopardizing short‐term outcomes.
Keywords: cardiac failure, cardiac transplantation, donor exclusion, donor screening
Subject Categories: Cardiomyopathy, Heart Failure, Transplantation
Nonstandard Abbreviations and Acronyms
- NAT
nucleic acid amplification test
- ODD
overdose death donor
- UNOS
United Network for Organ Sharing
Clinical Perspective
What Is New?
Over the past 5 years, the number of donor hearts offered for transplant has increased; however, the actual donor to transplant ratio has declined.
The recent increase in the number of hearts is because of the higher availability of organs from donors who have died from drug overdose or have hepatitis C. Recent donors also have more comorbid illnesses (hypertension, diabetes mellitus, obesity, etc)
What Are the Clinical Implications?
Despite the increase in usage of hearts from donors with higher comorbidities, short‐term survival of recipients of heart transplants continues to improve.
Broader acceptance and usage of hepatitis C virus positive and overdose death donor hearts should alleviate the strain on the current waitlist pool without compromising recipient outcomes.
In the past 5 years, the number of total heart transplants performed annually in the United States has been increasing. In fact, more than 3000 hearts were transplanted in 2016, the first time this was achieved.1 Despite the increasing number of heart transplants performed, the list of patients waiting for heart transplant continues to grow at a higher pace.2 Although interventions such as increased use and durability of mechanical circulatory support devices may have led to a decrease in pretransplant mortality from 14.6 deaths per 100 years in 2005 to 9.7 deaths per 100 years in 2015 to 2016, the absolute number of waitlist deaths remains high.2 Reportedly, 20% of candidates for heart transplant die on the waiting list or have been removed from the list as they are deemed “too sick” to benefit from a heart transplant.3
Given the continued donor shortage and high waitlist mortality rate, efforts are being undertaken to improve use of donor hearts and specifically to consider transplanting hepatitis C virus (HCV) positive or opioid overdose death donor (ODD) hearts.4 The current opioid epidemic has led to a substantial increase in donor offers for transplant, with anoxia from drug overdose as the increasing cause of death. Although cocaine use has increased from 11% in 2000 to 27% in 2018, usage of other drugs (nonintravenous street drugs such as crack, marijuana, prescription narcotics, sedatives, hypnotics, or stimulants) has doubled from 25% to 57% from 2000 to 2018.5 In 2015, over 33 000 individuals died from an opioid overdose, a number that has quadrupled since 1999.6 Recent reports have shown that the mortality rate in recipients of heart transplant who received organs from donors who died from drug overdose are comparable to those who received organs from donors who died from other causes.7 With the advent of the opioid epidemic, the availability of donor hearts with hepatitis C has also increased.8 However, not all centers or patients are still willing to accept donors who are hepatitis C positive, and separate consents and sometimes approvals from healthcare insurance carriers are needed for each patient. It is unclear whether the increase in heart transplant volume in relation to total donor offers is real and whether such an increase is only a reflection of donors with drug overdoses and hepatitis C infection. Moreover, the question of whether overall changes in the donor pool composition has adversely affected early posttransplant outcomes in the contemporary era has yet to be addressed.
Therefore, we undertook the present study to examine the national donor usage trends since 1995 and in particular the use of donors who died from overdose or are HCV positive. Additionally, we determined the influence of donor characteristics on 30‐day or 1‐year posttransplant survival in recent times (2008–2012 and 2013–2017) compared with the years 2003 to 2007.
Methods
Because of the sensitive nature of the data collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the United Network for Organ Sharing at https://optn.transplant.hrsa.gov/data/request‐data/.
Study Sample
In the present study, we evaluated the number and percentage of hearts accepted for transplant, declined for transplant, or used for alternative purposes (eg, research) and the trends in heart donor characteristics, specifically donor hepatitis C antibody and hepatitis C nucleic acid amplification test (NAT) statuses and drug ODD from 1995 through 2018. The donor characteristics for organs used for heart transplant and their influence on 30‐day and 1‐year posttransplant survival rates were assessed across 3 different time periods. Information regarding donors was acquired from the Organ Procurement and Transplantation Network database.
Demographics and Database
In early 2019 we received the UNOS data set, which had complete information regarding follow‐ups until December 31, 2018. Hence, to allow for at least 1‐year follow‐up after transplant and to compare times within reasonable intervals, we a priori divided the data into 3 five‐year periods (2003–2007 [referent], 2008–2012, and 2013–2017) and compared all baseline and demographic characteristics of donors among the 3 groups. The donor characteristics that were evaluated for this study included the following: sex, age, height, weight, race, cause of death, hypertension, diabetes mellitus, prior myocardial infarction, cancer, cigarette use, cocaine use, intravenous drug use, other drug use, and HIV risk. We also examined the recipient’s characteristics such as age, sex, donor to recipient sex match, ischemic time, total bilirubin, and serum creatinine at time of transplant.
Statistical Analysis
We first analyzed all donor trends from 1995 through 2018 by evaluating the number of total donor offers and the absolute number and percentages of donor offers that were transplanted, declined or were used for “other” reasons (eg, research).9 In a similar fashion, donor trends were examined for donors who were HCV infected and drug ODD (total number of offers and offers accepted, declined, or used for other purposes) between 1995 through 2018, presented separately in figures. To examine trends statistically over time we employed Poisson regression for the counts and logistic regression for the percentages. In both cases, a Pearson overdispersion parameter with robust standard errors were used in a Wald‐type test of the potential linear trend over time. These models were extended as a supplementary analysis to include and assess regional differences as per UNOS regions and organ procurement organization center size (examined by quartiles) in trends over time.
Second, for all donor hearts that were used for transplants, we then compared the baseline characteristics of donors and recipients using chi‐square tests for categorical variables and Kruskal‐Wallis tests for continuous measures across the 3 different time frames as designated previously. Thereafter, we constructed Kaplan‐Meier curves examining the risk of death on follow‐up according to 3 different eras and compared them using log‐rank test. Then, using a multivariable Cox regression model, we compared 30‐day and 1‐year risk of death for heart transplant recipients from 2008 to 2012 and 2013 to 2017 to that of 2003 to 2007 (reference group). All models were adjusted for donor characteristics of age (0–17, 18–55, ≥56), height (cm), weight (kg), sex, race/ethnicity (White, Asian, Black, Hispanic, or American Indian or Alaska native), cause of death (anoxia, central nervous system tumor, cerebrovascular, head trauma, or Native Hawaiian or Other Pacific islander), hypertension, diabetes mellitus, prior myocardial infarction, cancer, cigarette use, cocaine use, intravenous drug use, other drug use, and HIV risk in addition to recipient and perioperative characteristics as recipient’s age, sex mismatch, size mismatch (defined as >14% of predicted heart mass10), ischemic time, baseline serum creatinine, and serum bilirubin. Additionally, we created a Forest plot to examine the effect of each donor variable on recipient’s posttransplant outcome according to different time periods by comparing donors from the years 2013 to 2017 and 2008 to 2012 to the donors from 2003 to 2007 across various population subgroups.
A P value of <0.05 was considered statistically significant. All analyses were performed using SAS software (SAS Institute, Cary, NC) version 9.4. Our study involved the use of a de‐identified registry database and after review, the study protocol was approved by our institutional review board at University of Wisconsin‐Madison.
Results
As shown elsewhere1 and as seen in Figure 1, the total number of hearts offered for transplant has steadily increased, particularly since 2011, and the total number of transplants has also increased. More specifically, the total number of potential donors increased from ≈8000 in 2010 to nearly 10 000 in 2016 and ≈11 000 in 2018 (Figure 1). Overdispersed Poisson and logistic regression models comparing time periods showed a statistically significant increase over time in the total donor numbers, and though the number of transplanted hearts continued to increase, the percentage of transplanted hearts has decreased over time (P value for all <0.01). Specifically, percentages of donor offers accepted for heart transplant decreased from a peak of 45% in 1995 to 28% in 2008 and thereafter has remained lower between 28 and 32% until 2018. Conversely, the percentage of donor offers declined for transplant increased from a nadir of 35% in 1995 to a peak of 55% in 2005 and then decreased to 53% in 2018. Importantly, the absolute number of donors declined for transplant has increased substantially over time and percentage of donor offers “declined” for transplants also increased. Lastly, the number of patients waitlisted for heart transplant continues to rise each year in the recent era (purple line, Figure 1A), at a similar rate as the increase in transplants performed each year, hence unfortunately it has not improved the current demand to supply ratio.
Figure 1. Trends in all heart donor allocation by year.
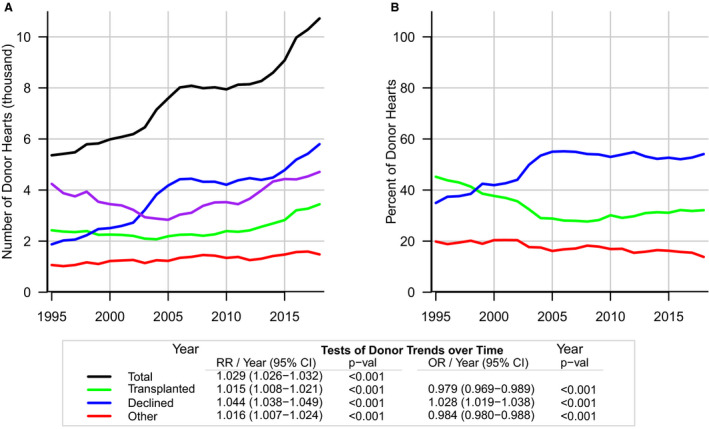
A, counts over time. B, percentages over time. Results are differentiated based on total donors (black line), transplanted donors (green line), denied donors (blue line), or “other” (eg, used for research; red line) and total number of waitlisted patients (purple line) during the years 1995 to 2018. RR in the trend test represents the relative risk per year from the Poisson regression of counts and the odds ratio per year was calculated from the logistic regression model. OR indicates odds ratio.
Significant differences were observed between UNOS regions in both number and percentage of total donors and transplanted and declined hearts over time (P value for all <0.001, Figure S1). When these donor trends were examined according to organ procurement organization size (separated by quartiles) the overall trends in transplanted hearts and percentages of transplanted hearts remained similar overtime (Figure S2).
There has been a significant rise in availability of donors with HCV infection (relative risk [RR]/year of 1.08, P‐ value 0.001) and those who die of drug overdose since 1995 (RR/year of 1.18, P value <0.001), and particularly since 2011 to 2012, as displayed in Figures 2 and 3 respectively. From 1995 through 2006, very few HCV‐positive donor hearts were transplanted. Specifically, between 2006 and 2014, donors from individuals who were HCV infected were not accepted for transplant. Since 2015, because of novel and effective antiviral therapy, hearts from donors who were HCV infected are being transplanted with increasing frequency (Figure 2B, RR/year of 1.07, P value 0.02). When delineated between donor HCV antibody status and donor HCV NAT status for the years 1995 to 2018, there are 977 donors who were antibody positive but NAT negative and 88 donors who were antibody negative but NAT positive. Additionally, there were 1793 donors who were antibody positive and NAT positive. Historically, number of overdose deaths have markedly increased, specifically since 2010 (Figure 3A) and fortunately, there appears to be a proportionate increase in the number of heart transplants performed using ODD (Figure 3B, RR/year 1.18, P value <0.001). Indeed, since 2015, there has been an increase in the use of ODD hearts (Figure 3B). Finally, overdose deaths continued to rise with 64 070 deaths in 2016 alone and perhaps leveled off thereafter.11
Figure 2. Trends in use of HCV‐positive donor hearts by year.
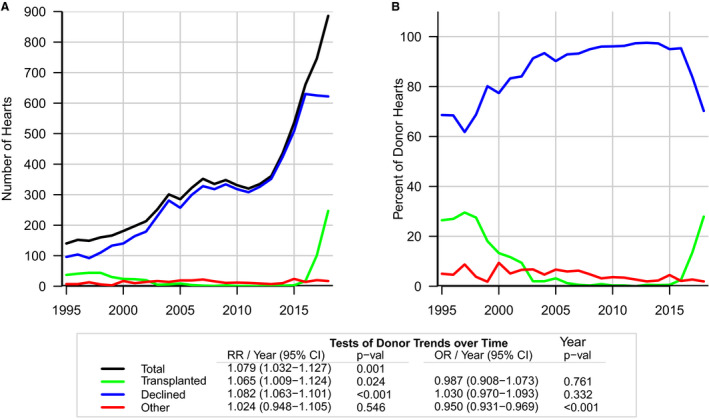
Graphs examining use of total HCV‐positive donor hearts from the years 1995 to 2018. A, the total number of donors who were HCV positive (black line), and number of HCV‐positive hearts transplanted (green line) have increased whereas HCV‐positive hearts declined for transplant (blue line) has leveled off since 2015. B, the percentage of donor hearts accepted for transplant (green line) and declined for transplant (blue line), and since 2015, the percentage of HCV‐positive hearts accepted for transplant has increased. RR represents the relative risk per year from the linear trend parameter of the Poisson model. OR indicates odds ratio.
Figure 3. Trends in use of overdose‐death donors by year.
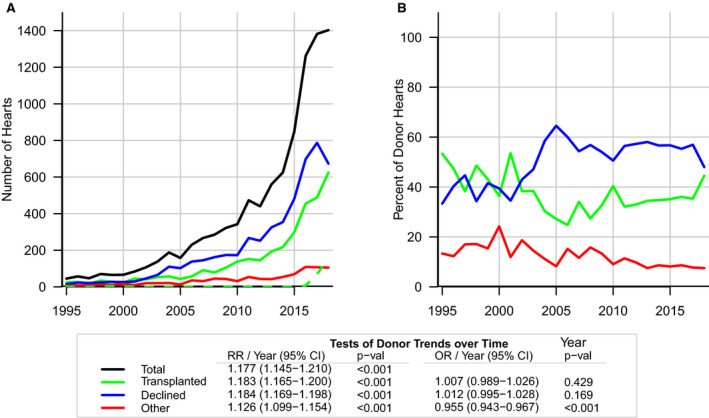
Graphs examining use of overdose‐death donors (ODD) from the years 1995 to 2018. A, total drug overdose (black line) donors, transplanted donors (green line), and those declined from transplant (blue line). Out of all ODD, number of HCV‐positive hearts transplanted (dotted green line) have increased as well since 2015. B, the percentage of transplanted ODD hearts (green line), ODD hearts declined for transplant (blue line), and in recent years, the percentage of accepted ODD hearts has increased. RR represents the relative risk per year from the linear trend parameter of the Poisson model. OR indicates odds ratio.
Donor characteristics of 37 079 that were accepted for heart transplants across all 3 periods (2003–2007, 2008–2012, and 2013–2017) are displayed in Table 1. As compared with donors from 2003 to 2007, donors from 2008 to 2012 or 2013 to 2017 were heavier and more likely to be women. Whereas White donors remained predominant in all eras, the percentage of Black and Hispanic donors increased in the recent eras. Compared with the reference period (2003–2007), donors between 2008 to 2012 and 2013 to 2017 were likely to have more hypertension and diabetes mellitus and less likely to have a prior myocardial infarction and cancer. These differences were minor although statistically significant. Head trauma remained the most common cause of death in the donor pool, though the percentage of donors dying from anoxia increased dramatically (33% of the donors in 2013–2017 versus 21% of the donors in 2008–2012 versus 13% of the donors in 2003–2007). Moreover, we also see the percentage of donors dying from drug overdose increasing in the more recent years (3% in 2003–2007, 5% in 2008–2012, and 11% in 2013–2018). Notably, the number and percentage of donors who have abused cocaine, intravenous drugs, “other” drugs, and those who are at risk for HIV have significantly increased through the years. On the contrary, the number and percentage of donors with history of cigarette smoking have steadily declined. In regard to the recipients, patients in the recent era (2013–2017) were older and had more female recipients, lower total bilirubin, and serum creatinine baseline levels when compared with the reference era (2003–2007). Ischemic time during transplant was also slightly shorter in the recent time periods (2013–2017) compared with previous times. Additionally, there were fewer donor–recipient sex mismatches in the more contemporary eras (Table 1). Specifically, female donor to male recipient mismatch steadily decreased in more recent years (17% in 2003–2007, 16% in 2008–2012, 15% in 2013–2017). As analyzed in Table 1, the proportion of undersized donor heart use for transplant has largely remained the same over the past 3 eras (18% in 2003–2007, 18% in 2008–2012, 17% in 2013–2017). Of note, undersizing was defined as donor size ≤86% of the recipient size calculated by predicted heart mass.
Table 1.
Baseline Characteristics of Donors and Recipients According to Different Time Periods
| Variable | 2003–2007 (N=10 869) | 2008–2012 (N=11 654) | 2013–2017 (N=14 556) | P Value* | ||||
|---|---|---|---|---|---|---|---|---|
| Transplanted Heart Donor Characteristics | ||||||||
| Female sex, n (%) | 3278 (30%) | 3683 (32%) | 4601 (32%) | 0.024 | ||||
| Height (cm) | 166.5±27.4 | 164.6±29.0 | 165.6±27.0 | <0.001 | ||||
| Weight (kg) | 73.9±25.7 | 73.9±27.1 | 75.7±27.2 | <0.001 | ||||
| Age, y, n (%) | <0.001 | |||||||
| 0–17 | 2292 (21%) | 2360 (20%) | 2625 (18%) | |||||
| 18–55 | 8313 (76%) | 9053 (78%) | 11 635 (80%) | |||||
| 56 + | 264 (2%) | 241 (2%) | 296 (2%) | |||||
| Race/Ethnicity, n (%) | <0.001 | |||||||
| Asian | 159 (1%) | 204 (2%) | 270 (2%) | |||||
| Black | 1524 (14%) | 2051 (18%) | 2499 (17%) | |||||
| Hispanic | 1864 (17%) | 2001 (17%) | 2463 (17%) | |||||
| Other‡ | 165 (2%) | 1 35 (1%) | 250 (2%) | |||||
| White | 7157 (66%) | 7263 (62%) | 9074 (62%) | |||||
| Cause of death, n (%) | <0.001 | |||||||
| Anoxia | 1388 (13%) | 2500 (21%) | 4766 (33%) | |||||
| Central nervous system tumor | 110 (1%) | 86 (1%) | 69 (0%) | |||||
| Cerebrovascular | 2347 (22%) | 2340 (20%) | 2328 (16%) | |||||
| Head trauma | 6819 (63%) | 6430 (55%) | 7055 (48%) | |||||
| Other | 205 (2%) | 298 (3%) | 338 (2%) | |||||
| Overdose death, n (%) | 303 (3%) | 620 (5%) | 1656 (11%) | <0.001 | ||||
| Hypertension, n (%) | 1143 (11%) | 1459 (13%) | 1909 (13%) | <0.001 | ||||
| Diabetes mellitus, n (%) | 228 (2%) | 340 (3%) | 449 (3%) | <0.001 | ||||
| Prior myocardial infarction, n (%) | 107 (1%) | 45 (0%) | 52 (0%) | <0.001 | ||||
| Cancer, n (%) | 178 (2%) | 165 (1%) | 170 (1%) | <0.001 | ||||
| Cigarette use, n (%) | 2239 (21%) | 1429 (12%) | 1320 (9%) | <0.001 | ||||
| Cocaine, n (%) | 1285 (12%) | 1427 (12%) | 2476 (17%) | <0.001 | ||||
| Intravenous drugs, n (%) | 55 (1%) | 411 (4%) | 1355 (9%) | <0.001 | ||||
| Other drug, n (%) | 3228 (30%) | 4171 (36%) | 6758 (46%) | <0.001 | ||||
| HIV risk, n (%) | 596 (5%) | 1067 (9%) | 3255 (22%) | <0.001 | ||||
| Heart Transplant Recipients’ Characteristics | ||||||||
| Age, y | 44.9±19.6 | 45.2±20.7 | 46.5±20.5 | <0.001 | ||||
| Female sex, n (%) | 2828 (27%) | 3281 (29%) | 4163 (29%) | <0.001 | ||||
| Sex match, n (%) | 7351 (69%) | 7998 (70%) | 10 558 (73%) | <0.001 | ||||
| Female donor to male recipient, n (%) | 1776 (17%) | 1835 (16%) | 2102 (15%) | <0.001 | ||||
| Ischemic time (hours) | 3.3±1.1 | 3.3±1.1 | 3.2±1.1 | <0.001 | ||||
| Total bilirubin mg/dL | 1.3±2.5 | 1.1±1.9 | 1.0±1.8 | <0.001 | ||||
| Serum creatinine, mg/dL | 1.3±1.0 | 1.2±1.0 | 1.2±1.0 | <0.001 | ||||
| Undersized,† n (%) | 1867 (18%) | 2038 (18%) | 2497 (17%) | 0.51 | ||||
All numbers are displayed as mean±SD or percentages as indicated.
The P values were calculated using chi‐square tests for categorical variables or Kruskal‐Wallis tests for continuous measures and correspond to a nontrend analysis signifying any difference among the eras.
Undersizing was calculated using predicted heart mass and noted when donor size was <86% of the recipient.
Other indicates American Indian or Alaska native, Native Hawaiian or Other Pacific Islander.
Survival Analyses
There were 1375 deaths within 30 days and 3222 deaths within 1 year post transplant. Kaplan‐Meier curves showed significantly improved 1‐year survival in the more recent eras (log‐rank P<0.01; Figure 4). In multivariable Cox models, the 30‐day risk of death (HR, 0.85; 95% CI, 0.74–0.98) and 1‐year risk of death (HR, 0.79; 95% CI, 0.73–0.87; Table 2) were significantly lower among posttransplant recipients in the 2013 to 2017 era compared with those undergoing transplant from 2003 to 2007. Additionally, 30‐day risk of death in the 2008 to 2012 era (HR, 0.91; 95% CI, 0.791–1.05) was lower although it did not reach statistical significance, but the 1‐year risk of death (HR, 0.86; 95% CI, 0.79–0.94; Table 2) was significantly lower compared with those undergoing transplant from 2003 to 2007.
Figure 4. Kaplan‐Meier curve examining the different eras.
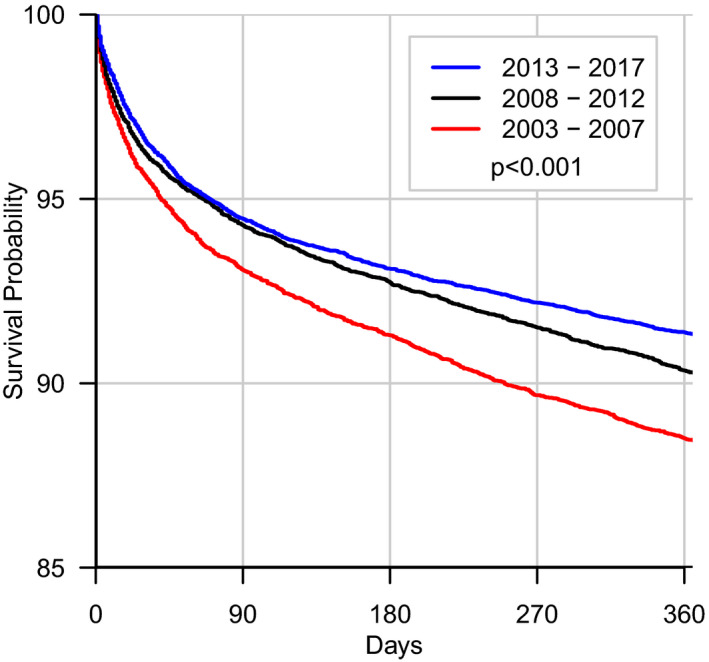
Kaplan‐Meier curves examining 1‐year all‐cause mortality across the different eras. The referent era (2003–2007) was found to have the worst mortality with the more recent eras having significantly lower 1‐year mortality in comparison.
Table 2.
Cox Proportional Models Examining the Risk of Early (30‐day) and Short‐term (1‐year) Death among Heart Transplant Recipients across Three Different Periods
| Models |
2003–2007 HR (95% CI) |
2008–2012 HR (95% CI) |
2013–2017 HR (95% CI) |
P Value |
|---|---|---|---|---|
| 30‐d risk of death | ||||
| Multivariable* | Reference | 0.91 (0.79–1.05) | 0.85 (0.74–0.98) | 0.006 |
| 1‐y risk of death | ||||
| Multivariable* | Reference | 0.86 (0.79–0.94) | 0.79 (0.73–0.87) | <0.0001 |
HR indicates hazard ratio.
Multivariable models were adjusted for sex, age (0–17, 18–55, ≥56), height (cm), weight (kg), race/ethnicity (White, Asian, Black, Hispanic, or others [American Indian or Alaska native, Native Hawaiian or Other Pacific Islander]), cause of death (anoxia, central nervous system tumor, cerebrovascular, head trauma, or other), hypertension, diabetes mellitus, prior myocardial infarction, cancer, cigarette use, cocaine use, intravenous drug use, other drug use, tuberculosis, HIV risk, recipient age, sex match, size mismatch, ischemic time, total bilirubin at time of transplant, and serum creatinine at time of transplant.
To examine the predictors of posttransplant mortality across 3 different periods, the recent eras (2008–2012 and 2013–2017) were compared with the oldest era (2003–2007). Overall mortality rates of transplant recipients were lower in the 2 most recent eras, independent of whether the donor was male or female, age <18 or 18 to 55, or cause of death was cerebrovascular accident or non‐cerebrovascular accident (Figure 5). Similarly, survival improved following transplant in the 2 more recent time periods when hearts from donors without diabetes mellitus, hypertension, or cocaine use were transplanted. In contrast, no survival benefit was observed among transplant recipients in the 2 most recent time periods compared with the referent group (years 2003–2007) if the donors had diabetes mellitus, hypertension, or were cocaine users. Recipients who received organs from older donors (≥56 years) in the periods 2008 to 2012 and 2013 to 2017 had similar survival rates when compared with those who received organs from older donors in 2003 to 2007, though this analysis is limited by the small number of patients in this cohort. Moreover, recipients survival improved despite the use of ODD hearts between 2013 to 2017 and 2008 to 2012 (statistically borderline significance) when compared with 2003–2007; Figure 5). It is also important to note that the number of overdose deaths in the most recent era are significantly higher than the prior 2 periods combined (1636 in 2013–2017, 609 in 2008–2012, 290 in 2003–2007).
Figure 5. Risk of death among heart transplant recipient according to donor characteristics and by different time periods.
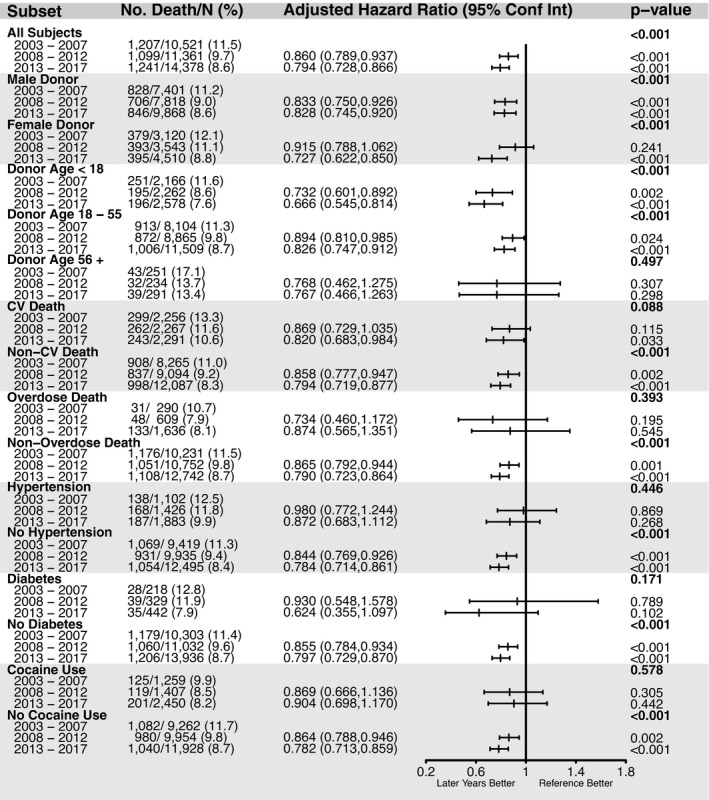
Forest plot examining the risk of death for recipient associated with each individual donor characteristic in 2008 to 2012 and 2013 to 2017 comparing with 2003 to 2007 is displayed. All models were adjusted with the same covariates used primary adjusted models. Bold P values assess the omnibus 3‐era comparison. Other P values asses the relevant era to the 2003 to 2007 reference era. CV indicates cardiovascular.
Discussion
The present study has 3 principal findings. First, even though overall number of heart transplants performed in the United States has steadily increased, the percentage of donor offers accepted for transplant have decreased. Thus, the recent increase in number of actual heart transplants in any given year is not proportionate to available donor offers. Specifically, we also observed that the increase in the number of heart transplants is in large part because of the availability and acceptance of ODD and more recently also because of donors who were hepatitis C positive. Second, despite the greater use of hearts from donors with risk factors as defined by cocaine use, intravenous drug use, other drug use risk for HIV including donors with overdose death and hepatitis C, overall posttransplant 30‐day and 1‐year recipient survival has been improving in the recent 2 periods (2007–2012 and 2013–2017) as compared with the oldest period (2003–2007). Lastly, separate examination of donor variables in the recent 2 periods compared with the oldest period (2003–2007), demonstrated improved posttransplant survival independent of donor age (<18 or 18–55), mode of death (cerebrovascular accident or non‐cerebrovascular accident) or ODD.
Increase in Heart Transplant Numbers in the Recent Era
In 2015, Khush and colleagues studied the regional variability of donor use between 1995 and 2010, and observed an increase in probability of transplants for most UNOS regions between 2008 and 2010.9 Our study extended those results from 2010 to 2018 and examined the reasons for recent increase in transplant numbers and the overall increase in donor offers. UNOS and other organizations such as Dow Take Initiative Program and policies like the National Organ Transplant Act have been at the forefront to increase donor awareness and perhaps these results are a reflection of those efforts.12
As discussed previously, donors from overdose death have increased in the recent period compared with the oldest era13 (Figure 3A) and several of these donors are hepatitis C infected. Heart transplant recipients of donors with hepatitis C, treated with antiviral therapy for the first month post transplant, have had comparable early (6‐month) mortality and graft function to those who have received organs from donors without hepatitis C.14 Moreover, 2 recent single‐center studies15, 16 and a study using UNOS database17 have also shown that when patients who are HCV naïve underwent cardiac transplantation from donor infected with HCV, there were no detrimental effects on graft function or 1‐year mortality. In the present study, we observed a significant increase in hepatitis C infected donor hearts being accepted for transplant only since 2016. Assuming the current trend in the availability and use of donors who are HCV infected (Figure 2) and acceptable posttransplant outcomes, the greater use of these donors will likely lead to a sizable increase in the total number of transplanted hearts in the near future. Additionally, given the shortage of donor organs, recent efforts have evaluated the use of donation after circulatory death donors in order to expand the donor pool.5 Open‐label clinical trials and case series have thus far demonstrated successful use of hearts from donation after circulatory death donors,18 which is an ongoing area of research and is likely going to affect donor availability and risk factors in the long run. Lastly, with recent changes to the heart allocation system in the United States that included broader geographic sharing of donors, ischemic times have increased again. Nonetheless, the comprehensive impact of these allocation changes with sicker recipient profiles, increasing ischemic times, and the use of donation after circulatory death donors is yet to be understood fully.
Improved Survival in Recent Era
Despite the increased use of high‐risk donors, 30‐day and 1‐year posttransplant survival has improved in the contemporary era with 1‐year mortality summarized in Figure 4. As summarized in Table 1, heart transplant recipients were more likely to be sex matched, have a lower serum creatinine, lower ischemic time, and lower total bilirubin in the more recent years when compared with 2003 to 2007. We surmise that the reduction in early posttransplant mortality may be likely related to better recipient selection, immunosuppressive regimens, updated surgical techniques, better posttransplant follow‐up, and the use of pretransplant mechanical circulatory support devices in the recent 2 time periods. Indeed, we have noted in Table 1 that in the contemporary era, there have been fewer sex mismatches in the contemporary eras. Given that it has been shown that female donors to male recipients confer a >2.5‐fold increase in risk for rejections and >3‐fold increase in risk for major events during follow up,19 fewer sex mismatches among donors and recipients in the contemporary eras could be contributing to the decrease in mortality in more recent eras. Also, Kransdorf et al have noted that undersized predicted heart mass (defined as being less than or equal to 86% of recipient size) as higher predictor of mortality. In the present study, prevalence of undersized donors usage based on predicted heart mass has remained the same across all eras.10 Although immunosuppressive strategies and surgical techniques have certainly evolved over time, it is difficult to control for these variables as they were noted to be a gradual shift that was dependent on the individual transplant center’s expertise. Therefore, the overall summation of these efforts was taken within the context of improved mortality in recent times. The incidence of graft rejection has been steadily decreasing over time, attributable to the development of new immunosuppressive drugs and treatment regimens.20 International Society of Heart and Lung Transplant guidelines currently recommend a corticosteroid, a calcineurin inhibitor, and an antiproliferative agent.21 When compared with those treated with cyclosporine, recipients of heart transplants treated with tacrolimus had a decreased incidence of severe rejection at 1 year, with an associated decrease in the development of conditions such as posttransplant hypertension and dyslipidemia.22 As noted in the annual 2018 International Society of Heart and Lung Transplant report, >80% of transplant centers now use tacrolimus as opposed to cyclosporine.23 During the early 2000s, the use of an implantable left ventricular assist device as a bridge to transplant was thought to possibly increase the risk of posttransplant mortality; however, in the recent era, pretransplant use of continuous flow left ventricular assist devices has not been shown to affect posttransplant survival, regardless of the duration of mechanical circulatory support.22, 24
Nonetheless, our study results show that even though posttransplant mortality as a whole has improved through the eras, this improvement has not been conferred onto those who have received a heart from a donor with history of hypertension and diabetes mellitus, an observation that is consistent with prior literature.25 Additionally, improvement in the recipient mortality was also not evident when donors with cocaine use were compared from contemporary era to oldest era. Note, that 1 prior study has indicated that nonintravenous cocaine use has not been associated with inferior posttransplant mortality.26 Our study database did not have the information to draw any conclusions about nonintravenous versus intravenous cocaine use.
Strengths and Limitations
Strengths of this study include using the UNOS database, which allowed us to study national trends, to individually examine donor characteristics over time and perform subgroup analyses based on these donor characteristics. Because our study focused on donor characteristics and donor use trends over the years in the United States and usage of HCV‐infected donor organs, we did not examine all recipient risk factors. Conceivably, some of these increased risk donors were used for very sick patients who had been at critical risk of death within days. If so, early posttransplant survival using these high‐risk organs may have been compromised, not enhanced. Unfortunately, the UNOS heart allocation strategy executed until October 2018 did not allow us to decipher such assumptions in depth. Additionally, because of the retrospective nature of our study, causality cannot be inferred from the associations we show.
Conclusions
Over the past decade, the number of donor hearts offered for transplant has increased significantly, largely because of the increased availability of organ donors who have died from drug overdose. However, the overall percentage of donor offers accepted for heart transplant have not increased proportionally, in part because of the lack of use of organs from donors infected with HCV and donors who died from drug overdose up until 2016. Overall, early (30‐day) and short‐term (1‐year) survival of heart transplant recipients has improved in the recent decade compared with the era from 2003 to 2007. Given our findings, we believe that greater use of HCV‐positive and ODD hearts should alleviate the strain on the current waitlist pool without compromising long‐term mortality outcomes.
Sources of Funding
Authors received no financial support for research, authorship, or publication of this article. OPTN database is in part supported by Human Resources and Services Administration contract 234‐2005‐370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. This investigation was supported by the National Institutes of Health, under Ruth L. Kirschstein National Research Service Award T32 HL 007936 from the National Heart, Lung, and Blood Institute to the University of Wisconsin‐Madison Cardiovascular Research Center.
Disclosures
None.
Supporting information
Figure S1–S2
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.019655
For Sources of Funding and Disclosures, see page 10.
References
- 1.Ahmad T, Schroder JN, Januzzi JL Jr. Breaking bad: the heartbreak of drug abuse. JACC Heart Fail. 2017;5:446–448. DOI: 10.1016/j.jchf.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Colvin M, Smith JM, Hadley N, Skeans MA, Carrico R, Uccellini K, Lehman R, Robinson A, Israni AK, Snyder JJ, et al. OPTN/SRTR 2016 annual data report: heart. Am J Transplant. 2018;18:1291–1362. DOI: 10.1111/ajt.14561. [DOI] [PubMed] [Google Scholar]
- 3.Colvin M, Smith JM, Skeans MA, Edwards LB, Uccellini K, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2015 annual data report: heart. Am J Transplant. 2017;17:286–356. DOI: 10.1111/ajt.14128. [DOI] [PubMed] [Google Scholar]
- 4.Kobashigawa J, Khush K, Colvin M, Acker M, Van Bakel A, Eisen H, Naka Y, Patel J, Baran DA, Daun T, et al. Report from the American Society of Transplantation conference on donor heart selection in adult cardiac transplantation in the United States. Am J Transplant. 2017;17:2559–2566. DOI: 10.1111/ajt.14354. [DOI] [PubMed] [Google Scholar]
- 5.Chambers DC, Zuckermann A, Cherikh WS, Harhay MO, Hayes D Jr, Hsich E, Khush KK, Potena L, Sadavarte A, Singh TP, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: 37th adult lung transplantation report 2014; 2020; focus on deceased donor characteristics. J Heart Lung Transplant. 2020;39:1016–1027. DOI: 10.1016/j.healun.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glazier AK, Delmonico FL, Koh HK. Organ donation in the era of the opioid crisis: a clinical strategy to maximize transplantation. Transplantation. 2017;101:2652–2654. DOI: 10.1097/TP.0000000000001878. [DOI] [PubMed] [Google Scholar]
- 7.Mehra MR, Jarcho JA, Cherikh W, Vaduganathan M, Lehman RR, Smits J, Stehlik J. The drug‐intoxication epidemic and solid‐organ transplantation. N Engl J Med. 2018;378:1943–1945. DOI: 10.1056/NEJMc1802706. [DOI] [PubMed] [Google Scholar]
- 8.Zibbell JE, Asher AK, Patel RC, Kupronis B, Iqbal K, Ward JW, Holtzman D. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health. 2018;108:175–181. DOI: 10.2105/ajph.2017.304132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khush KK, Zaroff JG, Nguyen J, Menza R, Goldstein BA. National decline in donor heart utilization with regional variability: 1995–2010. Am J Transplant. 2015;15:642–649. DOI: 10.1111/ajt.13055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kransdorf EP, Kittleson MM, Benck LR, Patel JK, Chung JS, Esmailian F, Kearney BL, Chang DH, Ramzy D, Czer LSC, et al. Predicted heart mass is the optimal metric for size match in heart transplantation. J Heart Lung Transplant. 2019;38:156–165. DOI: 10.1016/j.healun.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Dowell D, Noonan RK, Houry D. Underlying factors in drug overdose deaths. JAMA. 2017;318:2295–2296. DOI: 10.1001/jama.2017.15971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsich EM. Matching the market for heart transplantation. Circ Heart Fail. 2016;9:e002679. DOI: 10.1161/CIRCHEARTFAILURE.115.002679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Durand CM, Bowring MG, Thomas AG, Kucirka LM, Massie AB, Cameron A, Desai NM, Sulkowski M, Segev DL. The drug overdose epidemic and deceased‐donor transplantation in the United States: a national registry study. Ann Intern Med. 2018;168:702–711. DOI: 10.7326/M17-2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blumberg EA. Organs from hepatitis C virus‐positive donors. N Engl J Med. 2019;380:1669–1670. DOI: 10.1056/NEJMe1901957. [DOI] [PubMed] [Google Scholar]
- 15.Woolley AE, Singh SK, Goldberg HJ, Mallidi HR, Givertz MM, Mehra MR, Coppolino A, Kusztos AE, Johnson ME, Chen K, et al. Heart and lung transplants from HCV‐infected donors to uninfected recipients. N Engl J Med. 2019;380:1606–1617. DOI: 10.1056/NEJMoa1812406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schlendorf KH, Zalawadiya S, Shah AS, Wigger M, Chung CY, Smith S, Danter M, Choi CW, Keebler ME, Brinkley DM, et al. Early outcomes using hepatitis C‐positive donors for cardiac transplantation in the era of effective direct‐acting anti‐viral therapies. J Heart Lung Transplant. 2018;37:763–769. DOI: 10.1016/j.healun.2018.01.1293. [DOI] [PubMed] [Google Scholar]
- 17.Madan S, Patel SR, Rahgozar K, Saeed O, Murthy S, Vukelic S, Sims DB, Shin JJ, Goldstein DJ, Jorde UP. Utilization rates and clinical outcomes of hepatitis C positive donor hearts in the contemporary era. J Heart Lung Transplant. 2019;38:907–917. DOI: 10.1016/j.healun.2019.06.023. [DOI] [PubMed] [Google Scholar]
- 18.Dhital KK, Iyer A, Connellan M, Chew HC, Gao L, Doyle A, Hicks M, Kumarasinghe G, Soto C, Dinale A, et al. Adult heart transplantation with distant procurement and ex‐vivo preservation of donor hearts after circulatory death: a case series. Lancet. 2015;385:2585–2591. DOI: 10.1016/S0140-6736(15)60038-1. [DOI] [PubMed] [Google Scholar]
- 19.Peled Y, Lavee J, Arad M, Shemesh Y, Katz M, Kassif Y, Asher E, Elian D, Har‐Zahav Y, Goldenberg I, et al. The impact of gender mismatching on early and late outcomes following heart transplantation. ESC Heart Fail. 2017;4:31–39. DOI: 10.1002/ehf2.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costanzo MR, Costanzo MR, Dipchand A, Starling R, Anderson A, Chan M, Desai S, Fedson S, Fisher P, Gonzales‐Stawinski G, et al. The international society of heart and lung transplantation guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29:914–956. DOI: 10.1016/j.healun.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 21.Nativi JN, Drakos SG, Kucheryavaya AY, Edwards LB, Selzman CH, Taylor DO, Hertz MI, Kfoury AG, Stehlik J. Changing outcomes in patients bridged to heart transplantation with continuous‐ versus pulsatile‐flow ventricular assist devices: an analysis of the registry of the international society for heart and lung transplantation. J Heart Lung Transplant. 2011;30:854–861. DOI: 10.1016/j.healun.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Kamdar F, John R, Eckman P, Colvin‐Adams M, Shumway SJ, Liao K. Postcardiac transplant survival in the current era in patients receiving continuous‐flow left ventricular assist devices. J Thorac Cardiovasc Surg. 2013;145:575–581. DOI: 10.1016/j.jtcvs.2012.09.095. [DOI] [PubMed] [Google Scholar]
- 23.Magliato KE, Trento A. Heart transplantation–surgical results. Heart Fail Rev. 2001;6:213–219. [DOI] [PubMed] [Google Scholar]
- 24.John R, Pagani FD, Naka Y, Boyle A, Conte JV, Russell SD, Klodell CT, Milano CA, Rogers J, Farrar DJ, et al. Post‐cardiac transplant survival after support with a continuous‐flow left ventricular assist device: impact of duration of left ventricular assist device support and other variables. J Thorac Cardiovasc Surg. 2010;140:174–181. DOI: 10.1016/j.jtcvs.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 25.Stehlik J, Feldman DS, Brown RN, VanBakel AB, Russel SD, Ewald GA, Hagan ME, Folsom J, Kirklin JK, Cardiac Transplant Research Database G . Interactions among donor characteristics influence post‐transplant survival: a multi‐institutional analysis. J Heart Lung Transplant. 2010;29:291–298. DOI: 10.1016/j.healun.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Freimark D, Czer LS, Admon D, Aleksic I, Valenza M, Barath P, Harasty D, Queral C, Azen CG, Blanche C, et al. Donors with a history of cocaine use: effect on survival and rejection frequency after heart transplantation. J Heart Lung Transplant. 1994;13:1138–1144. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1–S2


