Abstract
Late life depression (LLD), a familiar syndrome, is not differentiated in the DSM-5. LLD can resemble depressive syndromes in younger adults but it differs in demographic characteristics, phenomenology, prognosis, treatment, suicide risk, relationship to other disorders, and etiology. Older depressed adults often present with fewer major depressive symptoms, less emphasis on mood disturbance, greater preoccupation with somatic or psychotic symptoms, and misleading cognitive deficits. LLD’s relationships with medical and neurocognitive symptoms and with inflammatory and immune factors are complex. Formal screening tools and biopsychosocial assessment informs diagnosis and treatment. Evidence supports the effectiveness of lifestyle interventions, several psychotherapies, and a variety of somatic treatment approaches. Comorbid medical disorders must be taken into account when planning treatment. In this article, the authors describe the characteristics of LLD, present an approach to assessment and management, and recommend that future DSM editions include a new specifier to differentiate LLD from other depressive syndromes.
Keywords: Depression, Geriatric psychiatry
In the extended family of DSM-5 diagnoses, late life depression (LLD) is the unacknowledged relative who awaits a formal invitation to the party. The DSM-5 states that “there are no clear effects of current age on the course or treatment response of major depressive disorder” (1); however, evidence suggests that there are multiple differentiated presentations of depression more characteristic of its appearance in later years. LLD shares features with depressive syndromes found among younger adults, but it also differs in many ways, not only in demographic characteristics but also in etiology, phenomenology, prognosis, acute treatment, maintenance treatment, suicide risk, and relationship to other medical and psychiatric disorders. Because of its differences from depression among younger adults, LLD risks going undetected or being mismanaged. In this overview, we highlight the essential characteristics of LLD and emphasize the most important differences between late life and earlier depression with the objectives of improving recognition and treatment of this common and debilitating disorder.
Demographic Characteristics
Depression is one of the more common psychiatric syndromes among older adults, and it presents in many guises. No official set of diagnostic criteria defines the diagnosis of LLD. By convention, this term typically denotes the presence of a depressive syndrome consistent with DSM criteria in an adult age 65 or older. The prevalence of major depressive disorder among community-dwelling older adults is estimated at 1%–4% (2). Taking various settings into consideration, another 10%–50% of older adults manifest clinically significant depressive symptoms below the threshold of major depressive disorder (3, 4). In primary care settings, higher rates of major depressive disorder are seen, an estimated 6%–9% (5). The highest rates of late life major depressive disorder are seen in long-term care facilities, where up to 25% of residents warrant that diagnosis; moreover, another estimated 30%–50% of residents manifest clinically significant depressive symptoms (6). Notably, LLD is an important antecedent to suicide in later life, which occurs at a higher rate than among the young. Depression is known to be the strongest risk factor for suicide among older adults (7). In 2000, the World Health Organization estimated suicide rates of men and women, age 75 and older, to be 50 and 16 per 100,000, respectively (8).
Although the prevalence of major depressive disorder is lower among older adults than among younger adults, milder depressive symptoms are more highly prevalent among older adults (2, 9). These clinically significant depressive symptoms, sometimes referred to as “minor depression,” can be a debilitating contributor to the psychiatric morbidity of the aging population (10).
Symptoms and Syndromes of LLD
The DSM-5 diagnosis of major depressive disorder provides a useful basic framework for detection of depression through the life cycle; however, the sensitivity and specificity of DSM-5 mood states and neurovegetative features differ between younger and older adults. Although the presentation of depressive episodes is heterogeneous at all ages, the “background noise” of symptoms reflecting age-associated medical burden and the frequent focus of older adults on somatic symptoms or psychotic concerns rather than depressed mood require clinicians to think beyond DSM-5 vegetative symptoms in diagnosing LLD. Disturbed sleep, energy, concentration, appetite, or activity among older adults can reflect various physiologic changes or medical disorders common to later life. As a result, the use of these symptoms in diagnosing LLD may lead to an overly inclusive approach that results in too many false positive diagnoses. However, when people with LLD fail to report mood changes characteristic of depression, which can occur for a variety of reasons, the diagnosis of LLD may be prematurely dismissed and a potential treatment opportunity lost.
An additional diagnostic consideration with LLD concerns the broad range of ages that make up “late life.” Older adults range from ages 65 to 100. Although the effects of age are individualized, increasing age amplifies the diversity of the older population and the symptoms, medical conditions, and functional status of individuals. The “young-old” group contains many individuals who perform at a high level in social and occupational domains, whereas the “old-old” group contains a much higher proportion of individuals who are retired, socially isolated, or compromised by impaired health and diminished function. Given the interactions between these variables and the phenomenology of mood disorders, LLD is not surprisingly a heterogeneous disorder with various presentations and disparate treatment needs.
Notably, these presentations include at least the following entities: recurrence of earlier onset major depressive disorder (9); the syndrome of subsyndromal depression, with symptoms too few for major depression; depression lacking a prominent low mood (i.e., depression without sadness) (11); depression with emphasis on somatization, including concern about pain, bodily dysfunction, or cognition; depression with psychotic features; depressive symptoms secondary to general medical conditions; depressive symptoms secondary to substance or medication use; and depressive symptoms associated with neurocognitive disorders. Episodes of depression that represent a late life recurrence of a longstanding mood disorder are grouped with other LLD depressive syndromes; however, these episodes may represent a significantly different condition because most LLD episodes are not preceded by earlier episodes (12). One study reported that as many as 71% of the older adults with depression enrolled in a home health care program were experiencing their first episode of depression (13). LLD in the context of bipolar disorder, which is less frequent than unipolar LLD, is beyond the scope of this article and has been recently reviewed elsewhere (14).
Etiologic Theories
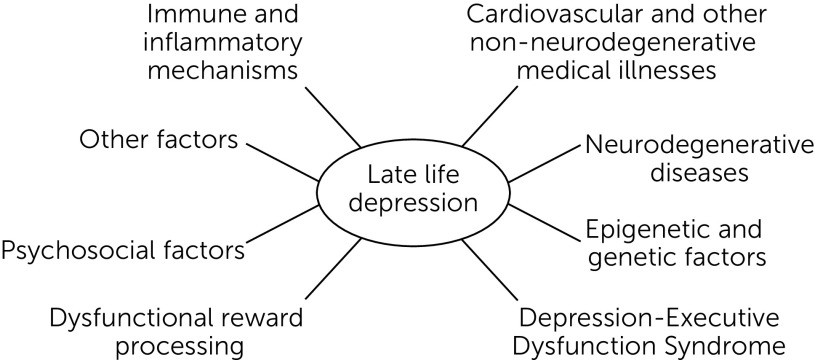
Multiple factors can contribute to LLD. In any affected individual, one or more of these might be the most critical to recognize or address. The most prominent of the proposed contributors to LLD are illustrated in Figure 1 and discussed in the subsequent text.
FIGURE 1.
Factors that contribute to late life depression
Immune and Inflammatory Mechanisms
Dysregulation of the immune system, as a consequence of age or disease, appears to be an important factor in LLD (15). The multiple mechanisms by which aging alters immune function are referred to collectively as “immunosenescence” (16). Increased levels of proinflammatory mediators with aging have been demonstrated in several cross-sectional studies (17). Evidence also suggests that a muted or inhibited immune response contributes to the maladies associated with an aging immune system. Proinflammatory changes in particular can alter communication between the peripheral and central nervous system immune systems (18), dampened the normal anti-inflammatory response, and facilitate a chronic proinflammatory state in the brain which leads to production of proinflammatory cytokines and harmful reactive oxygen and nitrogen species (18).
Immunosenescence can be further exacerbated by adverse psychosocial factors. In particular, evidence is increasing that psychosocial stressors can stimulate proinflammatory molecules such as elevated interleukin‐6 (IL‐6), tumor necrosis factor-alpha (TNF-α), and interferon-gamma (IFN-γ) (19). A proinflammatory milieu is also promoted by adverse lifestyle factors such as a diet high in sugar or saturated fat content, smoking, or increased body mass index. The proinflammatory cytokine, IL-6, has been consistently found to be increased in depressive disorders, and treatment with antidepressants significantly decreases peripheral levels of IL-6 (20). Elevated IL-6 levels in the cerebrospinal fluid have been correlated with increased suicide risk and with attempt severity (21). Meta-analysis has shown that peripheral levels of other inflammatory molecules such as TNF-α, IL‐13, IL‐18, IL‐12, soluble IL‐2 receptor, IL‐1 receptor antagonist, and soluble TNF receptor 2 were elevated in individuals with major depression compared with control groups.
Besides looking at peripheral markers, a cross-sectional positron emission tomography study used F-FEPPA ligand to measure the association of translocator protein total distribution volume (TSPO VT), a marker of microglial activation, with the duration of untreated major depressive disorder. A positive association between the duration of illness and TSPO VT was found (22). Alternatively, studies of healthy participants demonstrate that classic depressive symptoms can be induced by infusing endotoxin, which triggers cytokine release (23). Although the exact role of each of these inflammatory molecules and processes is still not fully understood, clear evidence exists to show that these immune mediators are dysregulated and sometimes correlated to disease severity in depressive disorders.
Cardiovascular Mechanisms
Aging is associated with increased vascular dysfunction (24). As people age, two major changes affect the arteries: large artery stiffening and endothelial dysfunction. Stiffening of the large arteries diminishes elasticity and compliance (25). Endothelial dysfunction is associated with a significant increase in the production of a wide range of cytokines, exacerbating the heightened inflammatory state of the aging vasculature (26). The vascular hypothesis of depression proposes “cerebrovascular disease may predispose, precipitate, or perpetuate some geriatric depressive syndromes” (27). Vascular depression, named for this hypothesis, is characterized by executive dysfunction, psychomotor retardation, disability disproportional to the severity of depression, and greater relapse risk (28). Presence of moderate to severe white matter hyperintensities on neuroimaging studies, interpreted as corresponding to cerebral small vessel disease, is a typical feature of vascular depression (29). These white matter changes are also associated with a slower response to citalopram treatment (30), a finding suggestive of slower antidepressant responsiveness in general.
Cerebrovascular Disease
In individuals with disrupted cerebrovascular function as a result of cerebrovascular accident (CVA or stroke), depression is common and described as “poststroke depression” (PSD). Every year, more than 795,000 CVAs occur in the United States (31), and about one-third of affected individuals develop PSD (32). In contrast to vascular depression, PSD is a disorder of larger blood vessels. It develops in the weeks and months following a CVA and can continue for many years (33). The correlation of PSD with CVA lesion location is controversial, but left hemispheric location or proximity to the frontal pole have been proposed as probable PSD risk factors (34). Bilateral basal ganglia damage appears to be associated with apathetic depression (32). Current research approaches are moving beyond a focus on lesion location to consider the effect of CVA on larger brain networks using techniques such as diffusion tensor imaging. Along these lines, one study has linked poststroke apathy to damage to the genu and splenium of the corpus callosum, left anterior corona radiata, and white matter of the frontal gyrus, thereby interconnecting brain regions involved in tasks such as decision making, emotional regulation, and reward-processing (35).
Non-Neurodegenerative Medical Illnesses
The bidirectional relationship between LLD and medical illness is an especially important consideration because of the high medical burden among older adults and the frequent ambiguity of symptom etiology. Research has shown that many medical diseases induce or mimic depressive symptoms. Conversely, depression can manifest itself in somatic symptoms or exacerbation of medical illness. Among the medical conditions associated with depressive symptoms, the most frequent are cardiopulmonary disorders, cerebrovascular disease, endocrine conditions, autoimmune disorders, neoplasms, and neurological conditions.
Some 80% of older individuals live with at least one chronic health condition, and 50% have two or more. Therefore, the co-occurrence of depressive and medical symptoms is not unexpected. The frequency of co-occurrence, however, suggests more than coincidence. The prevalence of major depressive disorder among patients with coronary heart disease is estimated to be between 15% and 23% (36). Among people with diabetes mellitus, the prevalence of major depressive disorder is estimated to be 12%; moreover, subsyndromal depressive symptoms are reported to be present in 15%–35% (37). One meta-analysis found the mean prevalence of meaningful depressive symptoms to be 8%–24% in patients with cancer and the prevalence of major depressive disorder to be 13% (38). Among patients with multiple sclerosis, the estimated prevalence of major depression is reported to be between 19% and 54% (39). Although major depressive disorder is common in individuals with medical illness, the prevalence of subsyndromal symptoms is even higher. Milder depressive symptoms contribute to a self-perception of poorer health and can affect self-care and the course of a patient’s medical illness.
The evaluation of depression in an individual with comorbid medical illness requires considerable clinical judgment when deciding which symptoms might best be attributed to one or the other etiology. Excess disability related to depression or depressive disturbances of mood, energy, appetite, sleep, and interest can be falsely attributed to a medical disorder, obscuring the presence of a potentially treatable mood disorder contribution.
Neurodegenerative Disorders
The neurocognitive disorders deserve special attention in a discussion of medical disorders associated with depressive symptoms. Here, again, the relationship is bidirectional and can be ambiguous. Some evidence supports the idea that depression is a risk factor for the development of dementia, or major neurocognitive disorder as it is now termed. Depression can also be a consequence of cognitive decline, both as a psychological reaction to self-observed diminished function and also as a physiological consequence of neurodegenerative changes. In some cases, the onset of depressive symptoms reflects a prodromal phase of dementia (40). Cognitive symptoms attributed to a primary mood disorder have been labeled “pseudodementia,” a term that is appropriately giving way to a more accurate designation, the “dementia syndrome of depression.” This newer term validates cognitive symptoms in depression as genuine dysfunction rather than purely psychodynamic or factitious. Controversy exists as to whether depression-related cognitive symptoms represent unmasking of a latent cognitive decline, because some longitudinal studies have reported a high rate of subsequent dementia among patients whose depressive episodes included acutely reversible cognitive symptoms (41).
In contrast to the treatment of depressive symptoms associated with the dementia syndrome of depression, the treatment outcome for depressive symptoms accompanying a primary dementia is often disappointing. Despite some positive studies, the preponderance of evidence, including a large recent study, suggests that antidepressants have limited value in this endeavor (14, 42). For clinicians, a general consideration is to evaluate the response to treatment and avoid prolonging an ineffective antidepressant trial when the target of treatment, depressive symptoms in a person with dementia, is failing to respond despite a reasonable trial.
Epigenetic and Genetic Factors
The contribution of epigenetic and genetic factors to the risk for LLD is an area of current growing interest. A sizable French investigation (the European/Australasian Stroke Prevention in Reversible Ischaemia Trial [ESPRIT]) of neuropsychiatric disorders in 302 participants age 65 and older suggested that a decrease in methylation of a specific serotonin transporter gene (SLC6A4) might increase the risk for LLD (43). Another meta-analysis has linked two additional genes that affect hippocampal plasticity and stress reactivity, apolipoprotein E (APOE) and brain-derived neurotrophic factor (BDNF), with LLD (44). Although the number of genetic studies is limited at present, current evidence suggests that the genetic associations of LLD may differ from those in younger adults (45).
Depression-Executive Dysfunction Syndrome
The depression-executive dysfunction syndrome (DEDS) attributes a characteristic depressive syndrome (with specific cognitive and mood manifestations and a poorer response to antidepressant treatment) to the disruption of frontostriatal-limbic pathways among older adults (15, 46, 47). The etiology of this condition can be vascular but can also include other causes. The clinical profile of DEDS is characterized by apathy; anhedonia; trouble with planning, initiating, and completing goal-directed activities; lack of insight; suspiciousness; and pronounced disability (15). Apathy, in this syndrome, has been associated with damage to cortical-subcortical networks associated with emotion regulation, reward, and goal-directed behavior (48).
A meta-analysis concluded that among the domains of executive functions, planning and organization were the ones significantly associated with poor response to antidepressant treatment (46). In addition to executive dysfunction predicting poorer response to antidepressants, a marker of executive dysfunction (decreased brain activation measured by functional magnetic resonance imaging during the Wisconsin Card Sorting Task) predicted poor outcome to a psychotherapeutic intervention (cognitive-behavioral psychotherapy) among individuals with LLD (49).
Dysfunctional Reward Processing
Abnormalities in the reward processing system characterized by a reduction in reward responsiveness have also been suggested as a contributing factor (50); this finding is further discussed in the Psychotherapy section in relationship to the role of Engage therapy.
Psychosocial Factors
Adverse life events, lack of social support, loneliness, and lower income are among the psychosocial risk factors associated with LLD (51). Loneliness, even in prepandemic times, has been identified as an important stressor in later life. In a large longitudinal cohort study of older adults, 43% reported feeling lonely (52). In another study, the long-term trajectory of depression was affected by loneliness in a cohort of elderly Finnish adults (53). The mechanisms underlying the association between loneliness and LLD are not entirely clear, but various theories have been proposed. Perceived isolation or loneliness results in increased sympathetic tone, increased systemic inflammation, and decreased sleep (54), which, in turn, exacerbate depressive symptoms. During the later years of life, when social interactions may be restricted, disruption of the dyadic relationship takes on a particular importance in exacerbating depression; this relationship must also be taken into account when implementing treatment interventions. Complex persistent bereavement disorder overlaps symptomatically with LLD, or can co-occur, and both disorders have been associated with increased morbidity and mortality. Following the loss of a spouse, the period of greatest relative mortality risk occurs between 7 and 12 months after the event (55).
Bereavement is one of the psychosocial stressors that increases suicide risk. Assessment of suicide risk, which is an essential component in the evaluation on an individual with LLD, is therefore very important when bereavement has occurred. Suicide risk can be reduced by recognizing reduced social support, by screening for suicidal ideation or behavior, and by enrolling high-risk individuals in appropriate follow-up (such as that described in the innovative Prevention of Suicide in Primary Care Elderly: Collaborative Trial [PROSPECT], which evaluated suicide risk in a primary care setting to prevent adverse outcomes) (7).
Other Factors
Prescribed medications, sometimes helpful for a medical condition or believed to reduce symptoms such as insomnia, may inadvertently contribute to the symptoms of LLD. Angiotensin-converting enzyme (ACE) inhibitors, beta blockers, corticosteroids, and other medications used by many older adults have been linked with initiation or exacerbation of depressive symptoms (56). The effect of aging on the hormonal internal milieu is also significant. Postmenopausal loss of normal estradiol cycling has been proposed to increase depressive symptoms in LLD via effects on neurotransmitter and mood regulatory systems. Specific estrogen receptor polymorphisms have been associated with heightened depression risk among older women, and maintenance of normal estrogen levels is important for several brain regions vulnerable to age-related changes (e.g., the prefrontal cortex and hippocampus) (57).
One review has called attention to the possibility that this hormonal change is growing in importance as increased life expectancy prolongs the duration of postmenopausal life (58). Testosterone, too, may play a role in mood regulation, and testosterone levels appear to be of significance in both men and women. Augmentation with low-dose testosterone, in one trial, improved depressive symptoms among women (59), although the association between depression and low testosterone in other studies has been inconsistent (60, 61). Among hypogonadal men with depression, exogenous supplementation of testosterone has been reported to be beneficial (62, 63).
Assessment
Comprehensive biopsychosocial assessment is warranted when an older adult presents with depressive symptoms. Evaluation begins with a careful history of prior episodes and risk factors, delineation of symptoms, exclusion of symptom-inducing or treatment-complicating medical diseases or toxins (including medications and recreational substances), and identification of acute suicide risk. Laboratory evaluation, to rule out treatable medical disorders that mimic depression, routinely includes the complete blood count (CBC), comprehensive metabolic panel, and thyroid-stimulating hormone (TSH). When clinically indicated, additional tests such as estradiol and testosterone levels as well as vitamin D (64), vitamin B12 (65, 66), or folate (67, 68) levels are also checked. C-reactive protein levels can assess the presence of an ongoing inflammatory process. On the basis of the history and physical examination, one may also consider neuroimaging and sleep assessment for selected patients.
Objective assessment of depressive symptoms using an appropriate rating scale can help to guide and monitor effective treatment. Table 1 provides a list of instruments that can be used to screen and track treatment outcomes among older individuals. Providers are encouraged to use the tools that are best suited to their patients and practice settings. Each instrument has a relatively high and comparable degree of sensitivity and specificity, but these measures vary depending on the studied populations; a detailed summary of these variations is beyond the scope of this article. In addition, a cognitive screening test such as the Saint Louis University Mental Status Examination (69) or the Montreal Cognitive Assessment (70) should be part of the routine assessment of LLD because of the frequent co-occurence of cognitive symptoms among people with LLD. The presence of these symptoms may indicate the prodrome of a neurocognitive disorder (71). Regardless of whether these symptoms are prodromal to neurocognitive decline, their presence may be clinically significant, and their response to treatment may be important to measure.
TABLE 1.
Instruments used to screen for late life depressiona
| Instrument | Who administers? | No. of items | Time required for administration (minutes) | In public domain? |
|---|---|---|---|---|
| SELFCARE (D) | Self | 12 | 5–7 | Yes |
| Center for Epidemiological Studies Depression Scale | Self | 20 | 20 | Yes |
| Center for Epidemiological Studies Depression Scale-10 | Self | 10 | 10 | Yes |
| Geriatric Depression Scale-Long Form | Self | 30 | 5–7 | Yes |
| Geriatric Depression Scale-Short Form | Self | 15 | 5–7 | Yes |
| Patient Health Questionnaire-2 | Self | 2 | 5 | Yes |
| Patient Health Questionnaire-9 | Self | 9 | 5 | Yes |
| Cornell Scale for Depression in Dementia | Provider | 19 + 19 | 20 | Yes |
| Beck Depression Inventory | Self | 21 | 10 | No |
| Hamilton Depression Rating Scale | Provider | 21 | 20 | Yes |
| Montgomery-Åsberg Depression Rating Scale | Provider | 10 | 20–30 | Yes |
More information and links to instruments are available at https://www.apa.org/depression-guideline/assessment.
Treatment Approach
Psychosocial and somatic treatment interventions have each been shown to be effective in treating LLD. Nonpharmacological strategies, alone or with somatic therapies, should be strongly considered and discussed when planning initial treatment because they can be highly effective and are preferred by many patients.
Physical Activity
Encouraging appropriate physical activity is both preventive and therapeutic with respect to LLD. Physical inactivity among older adults is associated with depression and cognitive deficits, whereas greater midlife physical activity is linked with lower depressive symptomatology in later life. A study of 140 patients showed that engagement in physical activity was associated with lower levels of depression and anxiety (72). Exercise has been shown to reduce inflammation and oxidative stress (73). Evidence indicates that physical exercise can be comparable with antidepressant medication in achieving therapeutic response rates (74, 75); moreover, the addition of exercise to pharmacological treatment is linked to higher and faster remission rates in LLD (76). Although aerobic activity has been consistently shown to be effective in LLD (77), the dose-response relationship has yet to be fully established (78).
Restful Sleep
Reduced ability to initiate and maintain sleep, especially after age 50, is part of the normal aging process (79). Disturbed sleep, however, is also a characteristic feature of depression that may even anticipate mood symptoms during a depressive episode. When both sleep disturbance and mood symptoms are present, the trajectory of depression is likely to include longer and more severe episodes as well as higher relapse rates (80). In addition, incomplete resolution of insomnia portends relapse of other depressive symptoms (81). Consequently, addressing insomnia, discussing sleep hygiene, and incorporating sleep measures into follow-up care are crucial ingredients of LLD care. In pilot studies, newer nonpharmacologic modalities such as brief behavioral treatment for insomnia show promise in effectively treating insomnia among older adults (82).
Appropriate Nutrition and Microbiome Health
A growing body of research supports and characterizes the clinical significance of a gut-brain axis and elucidates a possible contribution of gut microbiome dysfunction to depressive symptoms. This relationship may reflect the association between inflammatory states and gut barrier health (83). Additional evidence suggests that alterations in the gut microbiome affect serotonin levels in the central and peripheral nervous system. Probiotics have been shown to improve depressive symptoms, decrease levels of inflammatory markers, and increase serotonin availability (84). These compelling data suggest the value of additional research among patient populations.
Additional Lifestyle Factors
Smoking is associated with higher rates of depression among older adults compared with those who have never smoked (85). For this and other health reasons, smoking cessation should be encouraged and assisted. At-risk and problem drinking of alcohol also elevate the potential for depressive symptoms. The co-occurrence of alcohol use disorders and depression increases the potential for poor mental and general health outcomes among older adults. Alcohol dependence is both a risk factor for LLD and an obstacle to effective treatment (70). Addressing alcohol misuse in late life is important. Targeted screening that takes into account alcohol consumption and life context can help to identify older adults at higher risk for excessive or problematic drinking (86), which is a problem in its own right that also undermines treatment of LLD.
Psychotherapy and Somatic Treatment Interventions
Psychotherapy
Evidence-based psychotherapies, alone or with pharmacotherapy, are recommended for older individuals with mild to moderate depression (70); they are also recommended for individuals with inadequate or adverse response to therapeutic doses of antidepressants or who are at risk for drug interactions secondary to polypharmacy, which is a particularly important concern among older adults. However, cognitive and sensory impairments as well as access issues such as therapist unavailability, impaired patient mobility, and limited transportation options can interfere with this form of treatment. Randomized controlled trials have provided support for the efficacy of several psychotherapeutic approaches, which can be chosen and customized on the basis of individual needs and resources. Cognitive-behavioral therapy (CBT), problem-solving therapy (PST), interpersonal therapy (IPT), and Engage therapy (87) have been shown effective in treating LLD (88). Each of these approaches is amenable to delivery within a time frame that is customized for the individual, in briefer sessions if necessary and in a problem-focused manner.
CBT, which is based on the premise that inaccurate beliefs lead to maladaptive thoughts and behaviors, is an established and effective approach to treating LLD. In CBT, the therapist is an interactive coach and teacher, helping a patient to identify and alter dysfunctional cognitions while also encouraging behavioral activation and the scheduling of pleasant events. A recent multicenter study showed CBT, with modifications, to be effective in treating LLD (89). These modifications concern both the delivery of treatment and the content of sessions (90). Older adults sometimes find it easier to participate in shorter but more numerous sessions. Engagement with the issues can be enhanced through use of summarization and symptom assessment. Behavioral interventions should target the concerns most relevant to older adults, such as counteracting loneliness through an increase in social engagement.
PST conceptualizes depression as a consequence of a skill deficit. Acting as a sort of project manager and coach, the PST therapist helps a patient with depression to learn and apply new skills or to utilize abilities that were not learned or have fallen into disuse (91). The PST therapist teaches effective problem-solving techniques by providing a structured approach for defining a goal, planning a strategic solution, and monitoring progress toward success, which can be used in diverse populations (92). In one studied cohort, PST was significantly more efficacious than supportive therapy in reducing suicidality among older adults with major depressive disorder and significant executive dysfunction (93). This and other evidence suggest that PST may even have a role in treating older adults with depression and mild degrees of cognitive impairment (94).
IPT was designed to address depression arising from alterations in one’s interpersonal environment. It focuses on one or two of four areas frequently encountered in LLD: role transitions (significant life change), role disputes (conflict with a partner or another person), death of a loved one (complicated grief), and interpersonal deficits (isolation and loneliness or lack of a purpose) (95). Individuals with LLD often blame themselves inaccurately, and an IPT therapist can help the individual reframe the reactions to life changes as treatable life disruptions rather than moral failures. Redefining problems in this way reduces self-blame and clarifies the relationship between depressive symptoms and life events. Identifying and processing the precipitating circumstances with IPT can counteract depressive symptoms.
Engage therapy claims to differ from other psychotherapies as a result of its grounding in the principles of the Research Domain Criteria (RDoC) initiative, an effort to integrate multiple levels of evidence (genetics, molecules, cells, circuitry, behavior, physiology, and self-report) to explore basic elements of functioning to better understand and treat mental illness. Engage therapy postulates that depression reflects dysfunction of the positive valence (reward) system, and it uses reward exposure as its principal intervention to depressive symptoms (96). In RDoC terms, the commonly encountered barriers to treatment response are negativity bias (negative valence system dysfunction), apathy (arousal system), or emotional dysregulation (cognitive control dysfunction). Strategies targeting these dysfunctions are added when needed. For example, methods for addressing negativity bias can include discussing or writing alternative positive explanations to negative thoughts. Strategies for addressing apathy can consist of prompts to initiate action plans or even reminders from others. Emotional dysregulation can be countered by mindfulness activities such as meditation or deep breathing (96).
An additional promising related nonpharmacologic approach, computerized cognitive remediation, uses computer software designed to provide training in cognitive control and to enhance responsiveness of the reward system (97). This type of approach is personalized and continuously adapts its level of difficulty on the basis of the individual’s aptitude, both at baseline and through the course of treatment; this approach also provides consistent supportive feedback to avoid frustration or discouragement (15).
Pharmacotherapy
Despite research demonstrating the importance of psychosocial factors, the treatment of LLD in specialty settings or primary care very often relies upon the use of pharmacotherapy. Studies have shown that among older individuals with moderate to severe depression, antidepressants are more efficacious when compared with placebo (81). Any of the FDA-indicated antidepressants may be used, with a reported response rate of 50%–65% in randomized controlled trials with intention to treat compared with a 25%–30% response to placebo treatment. The intention to treat remission rate with treatment is lower: 30%–40% versus 15% for placebo (98). Individual risks and benefits are likely to vary as a result of pharmacokinetic and pharmacodynamic differences that affect the interaction between patient and medication. In cases of treatment resistance, augmentation strategies and coprescribing have successfully been used. Table 2 lists some of the commonly used antidepressants and augmenters in LLD with typical dosing ranges (99–106).
TABLE 2.
Antidepressants and augmenters commonly used in the pharmacotherapy of late life depressiona
| Antidepressant class and medication | Typical dose (mg/day) |
|---|---|
| SSRI | |
| Citalopram | 10–20 |
| Escitalopram | 5–20 |
| Fluoxetine | 10–40 |
| Sertraline | 50–200 |
| Vortioxetine | 10–20 |
| Vilazodone | 10–40 |
| Paroxetine | 10–30 |
| SNRI | |
| Venlafaxine | 75–225 |
| Desvenlafaxine | 25–50 |
| Duloxetine | 30–120 |
| Levomilnacipran | 20–120 |
| TCA | |
| Nortriptyline | 20–150 |
| Desipramine | 50–200 |
| MAOI | |
| Tranylcypromine | 30–60 |
| Phenelzine | 60–90 |
| Selegiline (Emsam)b | 3–6c |
| Miscellaneous antidepressants | |
| Bupropion | 100–300 |
| Mirtazapine | 15–45 |
| Esketamine | 84d |
| Agomelatinee (104) | 25–50 |
| Antipsychotic-antidepressant | |
| Quetiapine | 100–600 |
| Antidepressant combinations | |
| SRI+mirtazapinef | |
| SRI+bupropionf | |
| Bupropion+mirtazapinef | |
| Augmenters | |
| Lithium carbonate (105)g | |
| Triidothyronine (106) | 25–50h |
| Methylphenidate (107) | 2.5–5i |
| Aripiprazole (108) | 10–15 |
| Brexpiprazole (109) | 1–3 |
| Testosteroneb (110) | 100–200j |
SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor; TCA, tricyclic antidepressant; MAOI, monoamine oxidase inhibitor; SRI, serotonin reuptake inhibitor.
Available for transdermal administration.
Per 24 hours.
Twice per week.
Not available in the United States.
In combination, doses up to individual agent maximum levels can be used with caution and appropriate monitoring.
Dosed to target ≥0.5 mmol/L.
Dosed in micrograms.
Twice per day.
Intramuscular/weekly.
It is not our goal here to offer specific guidance regarding choice of antidepressant, an exhaustive list of antidepressants, or the procedure for dosing and monitoring treatment, all of which have been reviewed extensively elsewhere (107). General pharmacotherapy principles in LLD include choosing a medication with an eye to potential adverse effects, starting at a low dose, increasing gradually to optimal benefit, and discontinuing after nonresponse or appropriate response and maintenance.
Treatment-resistant depression often requires the use of an augmenter or combination intervention, whereas depression with psychotic features usually requires the combination of an antidepressant with an antipsychotic medication. After remission is achieved, relapse and recurrence rates are diminished by maintenance pharmacotherapy. The focus in successful treatment of LLD must reach beyond treatment of the individual episode and take into account the long-term view, which includes maintenance therapy for prevention of future episodes. In the context of recurrent LLD episodes, extended maintenance pharmacotherapy has been suggested, and limited evidence is available to help the clinician assess the optimal time for antidepressant discontinuation (108).
As in the adult population, careful management of adverse effects is an essential element of successful pharmacotherapy. Selective serotonin reuptake inhibitors are commonly associated with gastrointestinal side effects, changes in weight, hyponatremia, sexual dysfunction, and bruising; they are much less frequently associated with some more serious adverse effects, including gastrointestinal bleeding and cardiac arrhythmias. Tricyclic antidepressant (TCA) use has been associated with sedation, postural hypotension, and anticholinergic side effects such as blurred vision, constipation, urinary retention, and confusion. Less frequent but more severe events include delirium and cardiac conduction disturbances, including ventricular arrhythmias that account for the lethality of TCA overdose.
Broadly, antidepressant side effects can be anticipated on the basis of the medications’ pharmacokinetic characteristics and the pharmacodynamic properties of the medications listed in Table 3; practitioners can anticipate and monitor parameters accordingly. In general, our recommendation is that for older individuals with LL D whose symptoms are managed with antidepressants, providers should consider obtaining a baseline electrocardiogram, CBC, and basic metabolic panel before initiating medications. These parameters can be reviewed after dose titration or as clinically indicated.
TABLE 3.
Pharmacologic basis of adverse medication effects in the pharmacotherapy of late life depressiona
| Medication property | Possible clinical consequences |
|---|---|
| NE reuptake blockade | Tremors, tachycardia, erectile and ejaculatory dysfunction, elevated blood pressure |
| Serotonin reuptake blockade | GI symptoms, sexual dysfunction, EPS, bruising and bleeding, bone mass density loss |
| Dopamine reuptake blockade | Activation, aggravation of psychosis |
| Histamine H1 receptor antagonism | CNS depressant potentiation, sedation, weight gain, hypotension |
| Muscarinic receptor antagonism | Blurred vision, dry mouth, constipation, urinary retention, cognitive dysfunction |
| NE α1 receptor antagonism | Some antihypertensive potentiation, postural hypotension, dizziness, reflex tachycardia |
NE, norepinephrine; GI, gastrointestinal; EPS, extrapyramidal symptoms; CNS, central nervous system.
Neuromodulation
Electroconvulsive therapy (ECT) remains an effective but underused treatment option for LLD (109, 110). ECT is especially useful among individuals with antidepressant intolerance or nonresponse; it is also beneficial when treating LLD associated with delusions, catatonia, and mania (87). The acute antidepressant efficacy of ECT has repeatedly been shown superior to other antidepressant treatment modalities, including pharmacotherapy and psychotherapy. Because of its rapid effect, ECT is the treatment of choice for patients who are urgently ill, including those with psychosis and strong suicidal ideation from depression. ECT treatment of LLD can be associated with transient memory disturbance and significant posttreatment relapse rates; however, the procedure is considered relatively safe for older adults and has been demonstrated to be one of the most effective treatment options for LLD (111). No definitive guideline has identified the optimal number of ECT treatments for patients with LLD. One influential suggestion, from the 2009 Prolonging Remission In Depressed Elderly (PRIDE) study, is to provide at least four additional maintenance ECT treatments following a successful course of ECT, with further treatments as clinically indicated (112).
Repetitive transcranial magnetic stimulation (rTMS) is an additional neuromodulatory approach that has consistently been reported as safe and well tolerated with minimal cognitive adverse effects and a low dropout rate. Evidence of efficacy of rTMS in treating patients with LLD who have failed antidepressant treatments, including patients with treatment-resistant vascular depression (113), has generated interest in its use as a first line treatment. Many clinicians and patients see it as an alternative to medications suitable for individuals hesitant to undergo or unable to tolerate ECT. Older individuals require some modifications of rTMS administration, such as adjustment of the treatment schedule and the use individualized treatment protocols. Identification of factors predictive of rTMS response will further improve its therapeutic potential (114). Deep rTMS is a technical refinement that compensates for age-associated brain atrophy, which increases the distance of the brain from the applied magnetic field. A recent study showed that delivery of deep rTMS using an H1 coil over the dorsolateral and ventrolateral prefrontal cortex achieved a higher remission rate than sham rTMS (40.0% vs. 14.8%) and may be especially suitable for use among patients with treatment-resistant LLD (115).
Collaborative Care
Given the shortage of geriatric psychiatrists and the prevalence of LLD, researchers have explored methods for improving the recognition and management of LLD in primary care settings. The IMPACT study, which is one of the larger treatment trials for LLD, showed that a collaborative care model can increase the effectiveness of treating LLD in primary care settings. Older adults are more likely to seek depression treatment from a primary care provider than from a mental health specialist; however, treatment as usual in primary care may is less efficacious than collaborative treatment in the primary setting that incorporates guidance from a depression care specialist.
Results from the IMPACT study showed that at 12 months, about half of the primary care patients receiving collaborative care for depression reported at least a 50% reduction in depressive symptoms compared with only 19% of those in usual care. Surveys conducted 1 year after the study showed that the benefits of the IMPACT intervention persisted at follow-up assessment (116). Other collaborative care models, some of which engage community health workers, have also been successful. These models present an effective and affordable approach that can improve engagement of different racial-ethnic minority groups within the LLD population (117).
Concluding Comments
Depression is not a normative aspect of the aging process, but it is an often overlooked or undertreated psychiatric disorder among older adults. The consequences of failing to recognize and adequately treat LLD include impaired functional capacity and diminished quality of life. In later life, the most frequent psychiatric antecedent of suicide is depression. People with LLD are most often identified and treated in primary care settings. Whether in primary care or specialized settings, attentive and comprehensive assessment is required to avoid a missed diagnosis or ineffective treatment plan. Early detection and management are both desirable and challenging.
Older adults are especially vulnerable to suboptimal outcome because of age-associated variant presentations, medical comorbid conditions, cognitive impairment, and social determinants that interfere with treatment. LLD is amenable to lifestyle interventions, psychotherapy, or somatic approaches, including antidepressant therapy and neurotherapeutic approaches. Appropriate management is associated with reasonably high rates of response and remission, although maximal improvement may be more limited or require a longer duration of treatment. Individuals with vascular depression or the depression-executive dysfunction syndrome, for example, have been shown to respond less fully and more slowly to conventional antidepressant pharmacotherapy (15, 30).
Given the common presentation of treatment resistance among patients with LLD, further research is needed to guide clinicians who treat older adults with depression who fail to respond well to typical initial approaches. Psychotherapy plays a valuable role and can be modified to target the special needs of older adults. Antidepressants have been shown effective, but side effects require attentive management. Augmentation and coprescribing strategies effective in younger adults are used in treating people with resistant LLD, but further evaluation among older adults is needed to propose evidence-based pathways for management. Additional areas for investigation include the potential preventive value of lifestyle interventions such as physical and mental activity, nutrition, social engagement, and management of sleep disturbances.
As primary care practitioners increase their competence in treating LLD, the psychiatrist’s role is often consultative. Psychiatrists are in a unique position to assist and educate primary care colleagues in recognizing and treating LLD in its various manifestations. A psychiatric perspective can be valuable in identifying important medical and psychosocial determinants that are less amenable to pharmacotherapy but must be addressed to achieve an optimal outcome.
Because LLD can vary from the depressive syndromes seen among younger adults with respect to detection and management, it may be valuable to call attention to its distinct characteristics in the classification of mood disorders. Currently, several variants of major depressive disorder with differential presentations or treatment requirements are highlighted through the use of specifiers such as “with anxious distress,” “with mixed features,” “with melancholic features,” “with atypical features,” “with mood-congruent psychotic features,” “with mood-incongruent psychotic features,” or “with peripartum onset.” Inclusion of a specifier for “with late life onset” in future DSM editions would emphasize the uniqueness of LLD and remind clinicians that this particular mood disorder syndrome may be associated with different approaches to prognosis, risk assessment, evaluation, acute treatment, and follow-up care.
Footnotes
The authors report no financial relationships with commercial interests.
References
- 1. Diagnostic and Statistical Manual of Mental Disorders , 5th ed . Arlington, VA: , American Psychiatric Publishing; , 2013. [Google Scholar]
- 2. Blazer DG : Depression in late life: review and commentary . J Gerontol A Biol Sci Med Sci 2003. ; 58 : 249 – 265 [DOI] [PubMed] [Google Scholar]
- 3. Meeks TW , Vahia IV , Lavretsky H , et al. : A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults . J Affect Disord 2011. ; 129 : 126 – 142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Haigh EAP , Bogucki OE , Sigmon ST , et al. : Depression among older adults: a 20-year update on five common myths and misconceptions . Am J Geriatr Psychiatry 2018. ; 26 : 107 – 122 [DOI] [PubMed] [Google Scholar]
- 5. Hall CA , Reynolds CF 3rd : Late-life depression in the primary care setting: challenges, collaborative care, and prevention . Maturitas 2014. ; 79 : 147 – 152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Luppa M , Sikorski C , Luck T , et al. : Age- and gender-specific prevalence of depression in latest-life—systematic review and meta-analysis . J Affect Disord 2012. ; 136 : 212 – 221 [DOI] [PubMed] [Google Scholar]
- 7. Bruce ML , Ten Have TR , Reynolds CF 3rd , et al. : Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial . JAMA 2004. ; 291 : 1081 – 1091 [DOI] [PubMed] [Google Scholar]
- 8. Lapierre S , Erlangsen A , Waern M , et al. : A systematic review of elderly suicide prevention programs . Crisis 2011. ; 32 : 88 – 98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fiske A , Wetherell JL , Gatz M : Depression in older adults . Annu Rev Clin Psychol 2009. ; 5 : 363 – 389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barry LC , Abou JJ , Simen AA , et al. : Under-treatment of depression in older persons . J Affect Disord 2012. ; 136 : 789 – 796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gallo JJ , Rabins PV : Depression without sadness: alternative presentations of depression in late life . Am Fam Physician 1999. ; 60 : 820 – 826 [PubMed] [Google Scholar]
- 12. Brodaty H , Luscombe G , Parker G , et al. : Early and late onset depression in old age: different aetiologies, same phenomenology . J Affect Disord 2001. ; 66 : 225 – 236 [DOI] [PubMed] [Google Scholar]
- 13. Bruce ML , McAvay GJ , Raue PJ , et al. : Major depression in elderly home health care patients . Am J Psychiatry 2002. ; 159 : 1367 – 1374 [DOI] [PubMed] [Google Scholar]
- 14. Sajatovic M , Strejilevich SA , Gildengers AG , et al. : A report on older-age bipolar disorder from the International Society for Bipolar Disorders Task Force . Bipolar Disord 2015. ; 17 : 689 – 704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alexopoulos GS : Mechanisms and treatment of late-life depression . Transl Psychiatry 2019. ; 9 : 188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pawelec G : Age and immunity: What is “immunosenescence”? Exp Gerontol 2018. ; 105 : 4 – 9 [DOI] [PubMed] [Google Scholar]
- 17. Chung HY , Kim DH , Lee EK , et al. : Redefining chronic inflammation in aging and age-related diseases: proposal of the senoinflammation concept . Aging Dis 2019. ; 10 : 367 – 382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sochocka M , Diniz BS , Leszek J : Inflammatory response in the CNS: friend or foe? Mol Neurobiol 2017. ; 54 : 8071 – 8089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Berk M , Williams LJ , Jacka FN , et al. : So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 2013. ; 11 : 200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Köhler CA , Freitas TH , Stubbs B , et al. : Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis . Mol Neurobiol 2018. ; 55 : 4195 – 4206 [DOI] [PubMed] [Google Scholar]
- 21. Lindqvist D , Janelidze S , Hagell P , et al. : Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity . Biol Psychiatry 2009. ; 66 : 287 – 292 [DOI] [PubMed] [Google Scholar]
- 22. Setiawan E , Attwells S , Wilson AA , et al. : Association of translocator protein total distribution volume with duration of untreated major depressive disorder: a cross-sectional study . Lancet Psychiatry 2018. ; 5 : 339 – 347 [DOI] [PubMed] [Google Scholar]
- 23. Lasselin J , Lekander M , Benson S , et al. : Sick for science: experimental endotoxemia as a translational tool to develop and test new therapies for inflammation-associated depression . Mol Psychiatry (Epub Sep 1, 2020). doi: 10.1038/s41380-020-00869-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Xu X , Wang B , Ren C , et al. : Age-related impairment of vascular structure and functions . Aging Dis 2017. ; 8 : 590 – 610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Donato AJ , Machin DR , Lesniewski LA : Mechanisms of dysfunction in the aging vasculature and role in age-related disease . Circ Res 2018. ; 123 : 825 – 848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ungvari Z , Tarantini S , Donato AJ , et al. : Mechanisms of vascular aging . Circ Res 2018. ; 123 : 849 – 867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alexopoulos GS , Meyers BS , Young RC , et al. : ‘Vascular depression’ hypothesis . Arch Gen Psychiatry 1997. ; 54 : 915 – 922 [DOI] [PubMed] [Google Scholar]
- 28. Taylor WD , Aizenstein HJ , Alexopoulos GS : The vascular depression hypothesis: mechanisms linking vascular disease with depression . Mol Psychiatry 2013. ; 18 : 963 – 974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Krishnan KR , Hays JC , Blazer DG : MRI-defined vascular depression . Am J Psychiatry 1997. ; 154 : 497 – 501 [DOI] [PubMed] [Google Scholar]
- 30. Manning KJ , Alexopoulos GS , Banerjee S , et al. : Executive functioning complaints and escitalopram treatment response in late-life depression . Am J Geriatr Psychiatry 2015. ; 23 : 440 – 445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Benjamin EJ , Blaha MJ , Chiuve SE , et al. : Heart disease and stroke statistics—2017 update: a report from the American Heart Association . Circulation 2017. ; 135 : e146 – e603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nickel A , Thomalla G : Post-stroke depression: impact of lesion location and methodological limitations—a topical review . Front Neurol 2017. ; 8 : 498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ayerbe L , Ayis S , Wolfe CD , et al. : Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis . Br J Psychiatry 2013. ; 202 : 14 – 21 [DOI] [PubMed] [Google Scholar]
- 34. Shi YZ , Xiang YT , Wu SL , et al. : The relationship between frontal lobe lesions, course of post-stroke depression, and 1-year prognosis in patients with first-ever ischemic stroke . PLoS One 2014. ; 9 : e100456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yang SR , Shang XY , Tao J , et al. : Voxel-based analysis of fractional anisotropy in post-stroke apathy . PLoS One 2015. ; 10 : e116168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Forrester AW , Lipsey JR , Teitelbaum ML , et al. : Depression following myocardial infarction . Int J Psychiatry Med 1992. ; 22 : 33 – 46 [DOI] [PubMed] [Google Scholar]
- 37. Andreoulakis E , Hyphantis T , Kandylis D , et al. : Depression in diabetes mellitus: a comprehensive review . Hippokratia 2012. ; 16 : 205 – 214 [PMC free article] [PubMed] [Google Scholar]
- 38. Krebber AM , Buffart LM , Kleijn G , et al. : Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments . Psychooncology 2014. ; 23 : 121 – 130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Skokou M , Soubasi E , Gourzis P : Depression in multiple sclerosis: a review of assessment and treatment approaches in adult and pediatric populations . ISRN Neurol 2012. ; 2012 : 427102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hsiao JJ , Teng E : Depressive symptoms in clinical and incipient Alzheimer’s disease . Neurodegener Dis Manag 2013. ; 3 : 147 – 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brodaty H , Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression . Alzheimers Dement (Amst) 2020. ; 12 : e12027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Drye LT , Martin BK , Frangakis CE , et al. : Do treatment effects vary among differing baseline depression criteria in depression in Alzheimer’s disease study ± 2 (DIADS-2)? Int J Geriatr Psychiatry 2011. ; 26 : 573 – 583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lam D , Ancelin ML , Ritchie K , et al. : Genotype-dependent associations between serotonin transporter gene (SLC6A4) DNA methylation and late-life depression . BMC Psychiatry 2018. ; 18 : 282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tsang RS , Mather KA , Sachdev PS , et al. : Systematic review and meta-analysis of genetic studies of late-life depression . Neurosci Biobehav Rev 2017. ; 75 : 129 – 139 [DOI] [PubMed] [Google Scholar]
- 45. Goldman N , Glei DA , Lin YH , et al. : The serotonin transporter polymorphism (5-HTTLPR): allelic variation and links with depressive symptoms . Depress Anxiety 2010. ; 27 : 260 – 269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pimontel MA , Rindskopf D , Rutherford BR , et al. : A meta-analysis of executive dysfunction and antidepressant treatment response in late-life depression . Am J Geriatr Psychiatry 2016. ; 24 : 31 – 41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alexopoulos GS : Role of executive function in late-life depression . J Clin Psychiatry 2003. ; 64 ( Suppl 14 ): 18 – 23 [PubMed] [Google Scholar]
- 48. Hollocks MJ , Lawrence AJ , Brookes RL , et al. : Differential relationships between apathy and depression with white matter microstructural changes and functional outcomes . Brain 2015. ; 138 : 3803 – 3815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thompson DG , Kesler SR , Sudheimer K , et al. : FMRI activation during executive function predicts response to cognitive behavioral therapy in older, depressed adults . Am J Geriatr Psychiatry 2015. ; 23 : 13 – 22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Admon R , Pizzagalli DA : Dysfunctional reward processing in depression . Curr Opin Psychol 2015. ; 4 : 114 – 118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rafnsson SB , Orrell M , d’Orsi E , et al. : Loneliness, social integration, and incident dementia over 6 years: prospective findings from the English Longitudinal Study of Ageing . J Gerontol B Psychol Sci Soc Sci 2020. ; 75 : 114 – 124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Perissinotto CM , Stijacic Cenzer I , Covinsky KE : Loneliness in older persons: a predictor of functional decline and death . Arch Intern Med 2012. ; 172 : 1078 – 1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Heikkinen RL , Kauppinen M : Depressive symptoms in late life: a 10-year follow-up . Arch Gerontol Geriatr 2004. ; 38 : 239 – 250 [DOI] [PubMed] [Google Scholar]
- 54. Cacioppo JT , Hawkley LC , Thisted RA : Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study . Psychol Aging 2010. ; 25 : 453 – 463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Rozenzweig A , Prigerson H , Miller MD , et al. : Bereavement and late-life depression: grief and its complications in the elderly . Annu Rev Med 1997. ; 48 : 421 – 428 [DOI] [PubMed] [Google Scholar]
- 56. Rogers D , Pies R. General medical with depression drugs associated . Psychiatry (Edgmont) 2008. ; 5 : 28 – 41 [PMC free article] [PubMed] [Google Scholar]
- 57. Laird KT , Krause B , Funes C , et al. : Psychobiological factors of resilience and depression in late life . Transl Psychiatry 2019. ; 9 : 88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Daan NM , Fauser BC : Menopause prediction and potential implications . Maturitas 2015. ; 82 : 257 – 265 [DOI] [PubMed] [Google Scholar]
- 59. Miller KK , Perlis RH , Papakostas GI , et al. : Low-dose transdermal testosterone augmentation therapy improves depression severity in women . CNS Spectr 2009. ; 14 : 688 – 694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Giltay EJ , van der Mast RC , Lauwen E , et al. : Plasma testosterone and the course of major depressive disorder in older men and women . Am J Geriatr Psychiatry 2017. ; 25 : 425 – 437 [DOI] [PubMed] [Google Scholar]
- 61. Rohr UD : The impact of testosterone imbalance on depression and women’s health . Maturitas 2002. ; 41 ( Suppl 1 ): S25 – S46 [DOI] [PubMed] [Google Scholar]
- 62. Carnahan RM , Perry PJ : Depression in aging men: the role of testosterone . Drugs Aging 2004. ; 21 : 361 – 376 [DOI] [PubMed] [Google Scholar]
- 63. Walther A , Breidenstein J , Miller R : Association of testosterone treatment with alleviation of depressive symptoms in men: a systematic review and meta-analysis . JAMA Psychiatry 2019. ; 76 : 31 – 40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Parker GB , Brotchie H , Graham RK : Vitamin D and depression . J Affect Disord 2017. ; 208 : 56 – 61 [DOI] [PubMed] [Google Scholar]
- 65. Coppen A , Bolander-Gouaille C : Treatment of depression: time to consider folic acid and vitamin B12 . J Psychopharmacol 2005. ; 19 : 59 – 65 [DOI] [PubMed] [Google Scholar]
- 66. Sangle P , Sandhu O , Aftab Z , et al. : Vitamin B12 supplementation: preventing onset and improving prognosis of depression . Cureus 2020. ; 12 : e11169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fava M , Mischoulon D : Folate in depression: efficacy, safety, differences in formulations, and clinical issues . J Clin Psychiatry 2009. ; 70 ( Suppl 5 ): 12 – 17 [DOI] [PubMed] [Google Scholar]
- 68. Bender A , Hagan KE , Kingston N : The association of folate and depression: a meta-analysis . J Psychiatr Res 2017. ; 95 : 9 – 18 [DOI] [PubMed] [Google Scholar]
- 69. Tariq SH , Tumosa N , Chibnall JT , et al. : Comparison of the Saint Louis University Mental Status Examination and the Mini-Mental State Examination for detecting dementia and mild neurocognitive disorder—a pilot study . Am J Geriatr Psychiatry 2006. ; 14 : 900 – 910 [DOI] [PubMed] [Google Scholar]
- 70. Nasreddine ZS , Phillips NA , Bédirian V , et al. : The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment . J Am Geriatr Soc 2005. ; 53 : 695 – 699 [DOI] [PubMed] [Google Scholar]
- 71. Singh-Manoux A , Dugravot A , Fournier A , et al. : Trajectories of depressive symptoms before diagnosis of dementia: a 28-year follow-up study . JAMA Psychiatry 2017. ; 74 : 712 – 718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Teixeira CM , Vasconcelos-Raposo J , Fernandes HM , et al. : Physical activity, depression and anxiety among the elderly . Social Indicators Research 2013. ; 113 : 307 – 318 [Google Scholar]
- 73. Eyre H , Baune BT : Neuroimmunological effects of physical exercise in depression . Brain Behav Immun 2012. ; 26 : 251 – 266 [DOI] [PubMed] [Google Scholar]
- 74. Sherwood A , Blumenthal JA , Smith PJ , et al. : Effects of exercise and sertraline on measures of coronary heart disease risk in patients with major depression: results from the SMILE-II randomized clinical trial . Psychosom Med 2016. ; 78 : 602 – 609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Blumenthal JA , Babyak MA , Doraiswamy PM , et al. : Exercise and pharmacotherapy in the treatment of major depressive disorder . Psychosom Med 2007. ; 69 : 587 – 596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Belvederi Murri M , Amore M , Menchetti M , et al. : Physical exercise for late-life major depression . Br J Psychiatry 2015. ; 207 : 235 – 242 [DOI] [PubMed] [Google Scholar]
- 77. Blumenthal JA , Babyak MA , Moore KA , et al. : Effects of exercise training on older patients with major depression . Arch Intern Med 1999. ; 159 : 2349 – 2356 [DOI] [PubMed] [Google Scholar]
- 78. Mura G , Carta MG : Physical activity in depressed elderly. A systematic review . Clin Pract Epidemiol Ment Health 2013. ; 9 : 125 – 135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mander BA , Winer JR , Walker MP : Sleep and human aging . Neuron 2017. ; 94 : 19 – 36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Franzen PL , Buysse DJ : Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications . Dialogues Clin Neurosci 2008. ; 10 : 473 – 481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Pigeon WR , Hegel M , Unützer J , et al. : Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep 2008. ; 31 : 481 – 488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Gebara MA , DiNapoli EA , Lederer LG , et al. : Brief behavioral treatment for insomnia in older adults with late-life treatment-resistant depression and insomnia: a pilot study . Sleep Biol Rhythms 2019. ; 17 : 287 – 295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Cheung SG , Goldenthal AR , Uhlemann AC , et al. : Systematic review of gut microbiota and major depression . Front Psychiatry 2019. ; 10 : 34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wallace CJK , Milev R : The effects of probiotics on depressive symptoms in humans: a systematic review . Ann Gen Psychiatry 2017. ; 16 : 14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Choi NG , DiNitto DM : Role of new diagnosis, social isolation, and depression in older adults’ smoking cessation . Gerontologist 2015. ; 55 : 793 – 801 [DOI] [PubMed] [Google Scholar]
- 86. Moos RH , Schutte KK , Brennan PL , et al. : Late-life and life history predictors of older adults’ high-risk alcohol consumption and drinking problems . Drug Alcohol Depend 2010. ; 108 : 13 – 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Alexopoulos GS , Raue PJ , Gunning F , et al. : “Engage” therapy: behavioral activation and improvement of late-life major depression . Am J Geriatr Psychiatry 2016. ; 24 : 320 – 326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ellison JM , Kyomen HH , Harper DG : Depression in later life: an overview with treatment recommendations . Psychiatr Clin North Am 2012. ; 35 : 203 – 229 [DOI] [PubMed] [Google Scholar]
- 89. Dafsari FS , Bewernick B , Biewer M , et al. : Cognitive behavioural therapy for the treatment of late life depression: study protocol of a multicentre, randomized, observer-blinded, controlled trial (CBTlate) . BMC Psychiatry 2019. ; 19 : 423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Evans C : Cognitive–behavioural therapy with older people . Adv Psychiatr Treat 2007. ; 13 : 111 – 118 [Google Scholar]
- 91. Alexopoulos GS , Raue PJ , Banerjee S , et al. : Comparing the streamlined psychotherapy “Engage” with problem-solving therapy in late-life major depression. A randomized clinical trial . Mol Psychiatry (Epub July 1, 2020). doi: 10.1038/s41380-020-0832-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Dias A , Azariah F , Anderson SJ , et al. : Effect of a lay counselor intervention on prevention of major depression in older adults living in low- and middle-income countries: a randomized clinical trial . JAMA Psychiatry 2019. ; 76 : 13 – 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Gustavson KA , Alexopoulos GS , Niu GC , et al. : Problem-solving therapy reduces suicidal ideation in depressed older adults with executive dysfunction . Am J Geriatr Psychiatry 2016. ; 24 : 11 – 17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Alexopoulos GS , Raue PJ , Kanellopoulos D , et al. : Problem solving therapy for the depression-executive dysfunction syndrome of late life . Int J Geriatr Psychiatry 2008. ; 23 : 782 – 788 [DOI] [PubMed] [Google Scholar]
- 95. Markowitz JC , Weissman MM : Interpersonal psychotherapy: principles and applications . World Psychiatry 2004. ; 3 : 136 – 139 [PMC free article] [PubMed] [Google Scholar]
- 96. Alexopoulos GS , O’Neil R , Banerjee S , et al. : “Engage” therapy: prediction of change of late-life major depression . J Affect Disord 2017. ; 221 : 192 – 197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Morimoto SS , Wexler BE , Liu J , et al. : Neuroplasticity-based computerized cognitive remediation for treatment-resistant geriatric depression . Nat Commun 2014. ; 5 : 4579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Shanmugham B , Karp J , Drayer R , et al. : Evidence-based pharmacologic interventions for geriatric depression . Psychiatr Clin North Am 2005. ; 28 : 821 – 835 [DOI] [PubMed] [Google Scholar]
- 99. Salzman C (ed): Clinical Geriatric Psychopharmacology , 4th ed . Philadelphia: , Lippincott Williams & Wilkins; , 2004. [Google Scholar]
- 100. Heun R , Ahokas A , Boyer P , et al. : The efficacy of agomelatine in elderly patients with recurrent major depressive disorder: a placebo-controlled study . J Clin Psychiatry 2013. ; 74 : 587 – 594 [DOI] [PubMed] [Google Scholar]
- 101. Buspavanich P , Behr J , Stamm T , et al. : Treatment response of lithium augmentation in geriatric compared to non-geriatric patients with treatment-resistant depression . J Affect Disord 2019. ; 251 : 136 – 140 [DOI] [PubMed] [Google Scholar]
- 102. Goodwin FK , Prange AJ Jr , Post RM , et al. : Potentiation of antidepressant effects by L-triiodothyronine in tricyclic nonresponders . Am J Psychiatry 1982. ; 139 : 34 – 38 [DOI] [PubMed] [Google Scholar]
- 103. Lavretsky H , Park S , Siddarth P , et al. : Methylphenidate-enhanced antidepressant response to citalopram in the elderly: a double-blind, placebo-controlled pilot trial . Am J Geriatr Psychiatry 2006. ; 14 : 181 – 185 [DOI] [PubMed] [Google Scholar]
- 104. Lenze EJ , Mulsant BH , Blumberger DM , et al. : Efficacy, safety, and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised, double-blind, placebo-controlled trial . Lancet 2015. ; 386 : 2404 – 2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lepola U , Hefting N , Zhang D , et al. : Adjunctive brexpiprazole for elderly patients with major depressive disorder: an open-label, long-term safety and tolerability study . Int J Geriatr Psychiatry 2018. ; 33 : 1403 – 1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Perry PJ , Yates WR , Williams RD , et al. : Testosterone therapy in late-life major depression in males . J Clin Psychiatry 2002. ; 63 : 1096 – 1101 [DOI] [PubMed] [Google Scholar]
- 107. Ellison JM , Sivrioglu EY , Salzman C : Pharmacotherapy of late-life depression: evidence-based recommendations ; in Mood Disorders in Later Life , 2nd ed . Edited by Ellison JM , Kyomen , HH , Verma , S. New York: , Informa Healthcare; , 2008. [Google Scholar]
- 108. Reynolds CF 3rd , Frank E , Perel JM , et al. : Maintenance therapies for late-life recurrent major depression: research and review circa 1995 . Int Psychogeriatr 1995. ; 7 ( Suppl ): 27 – 39 [DOI] [PubMed] [Google Scholar]
- 109. Jones KC , Salemi JL , Dongarwar D , et al. : Racial/ethnic disparities in receipt of electroconvulsive therapy for elderly patients with a principal diagnosis of depression in inpatient settings . Am J Geriatr Psychiatry 2019. ; 27 : 266 – 278 [DOI] [PubMed] [Google Scholar]
- 110. Geduldig ET , Kellner CH : Electroconvulsive therapy in the elderly: new findings in geriatric depression . Curr Psychiatry Rep 2016. ; 18 : 40 [DOI] [PubMed] [Google Scholar]
- 111. Kerner N , Prudic J : Current electroconvulsive therapy practice and research in the geriatric population . Neuropsychiatry (London) 2014. ; 4 : 33 – 54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Kellner CH , Husain MM , Knapp RG , et al. : A novel strategy for continuation ECT in geriatric depression: phase 2 of the PRIDE study . Am J Psychiatry 2016. ; 173 : 1110 – 1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Sabesan P , Lankappa S , Khalifa N , et al. : Transcranial magnetic stimulation for geriatric depression: promises and pitfalls . World J Psychiatry 2015. ; 5 : 170 – 181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Baeken C , Brem AK , Arns M , et al. : Repetitive transcranial magnetic stimulation treatment for depressive disorders: current knowledge and future directions . Curr Opin Psychiatry 2019. ; 32 : 409 – 415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Kaster TS , Daskalakis ZJ , Noda Y , et al. : Efficacy, tolerability, and cognitive effects of deep transcranial magnetic stimulation for late-life depression: a prospective randomized controlled trial . Neuropsychopharmacology 2018. ; 43 : 2231 – 2238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Unützer J , Katon W , Callahan CM , et al. : Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial . JAMA 2002. ; 288 : 2836 – 2845 [DOI] [PubMed] [Google Scholar]
- 117. Scazufca M , Nakamura CA , Peters TJ , et al. : A collaborative care psychosocial intervention to improve late life depression in socioeconomically deprived areas of Guarulhos, Brazil: the PROACTIVE cluster randomised controlled trial protocol . Trials 2020. ; 21 : 914 [DOI] [PMC free article] [PubMed] [Google Scholar]