Maintenance dialysis is the most commonly chosen treatment for kidney failure in older patients. Current guidelines recommend presenting conservative care (CC) as a valid alternative to older patients who do not want to start dialysis [1]. While the survival benefit of dialysis is distinct, it appears to be reduced for the oldest patients and those with multiple comorbid conditions [2]. Also, the risk of treatment burden and the impact on daily life increase after dialysis initiation [2, 3]. In terms of health-related quality of life (HRQoL) and symptom burden, both treatment pathways have the potential to achieve similar outcomes [3].
Determining the most appropriate treatment pathway—often a difficult process—results from a dialogue between healthcare professionals, patients and their relatives on the goals of care, possible treatment options and risks and patients’ values and preferences. This process of shared decision making (SDM) may start as early as from an estimated glomerular filtration rate (eGFR) of 20–30 mL/min/1.73 m2, allowing time for dialogue, education and preparation for kidney replacement therapy. Reasons for choosing either dialysis or CC are based on aspects other than mortality and HRQoL and are likely to differ between patients, their relatives and physicians [4]. Furthermore, as patients’ circumstances and preferences may change over time, the choice of therapy might also be subject to change.
When kidney function declines, clinical condition often deteriorates and symptoms increase. Intuitively, one may think that increasing uraemic complaints may result in more patients changing their initial choice from CC to dialysis than vice versa. However, no studies have been published presenting aggregated numbers of patients switching their treatment choice. Therefore we aim to assess the number of patients with chronic kidney disease (CKD) who made an explicit choice for dialysis or CC and switched their decision afterwards, either from dialysis to CC or from CC to dialysis.
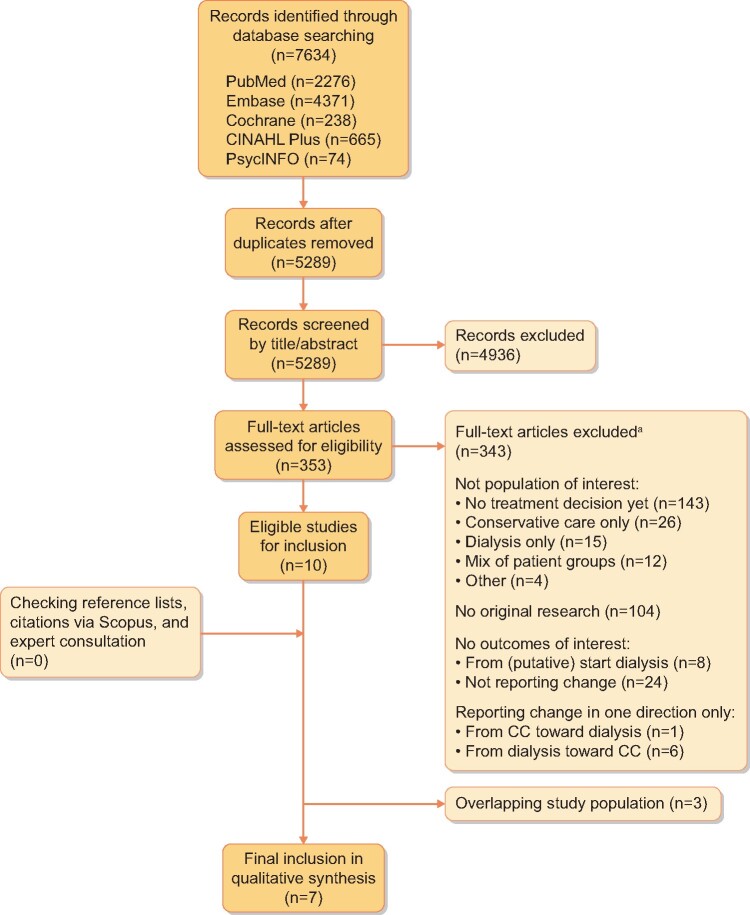
We systematically searched five databases from inception to 25 February 2021 for studies in patients with severely reduced eGFR or kidney failure (CKD stage G4–G5) and choosing either dialysis or CC that compared patient-reported outcomes (HRQoL and symptoms) [3], survival and treatment burden [5]. Detailed methods on search strategy and predefined selection criteria are described elsewhere [3, 5]. For the present analysis we included studies reporting the number of patients switching their (initial) treatment choice in either direction. Studies that started their observations at the (putative) start of dialysis were excluded. Screening of 7634 records resulted in 10 studies [2, 6–14] that reported the number of patients changing their treatment choice from dialysis to CC or vice versa (Figure 1). (Sub)groups where the decision to withhold dialysis was based on medical grounds only were excluded from the analysis; e.g. patients who started acute dialysis or when their nephrologist decided that dialysis was not appropriate [9]. This was done to ensure that our results reflected a patient group that was allowed to make a treatment choice. Three studies were omitted because of (partly) overlapping study populations; we excluded the studies first published and with the lowest number of CC patients [10, 11] or shortest follow-up duration [12].
FIGURE 1.
Study inclusion and exclusion flow diagram.
aExplanation of reasons for exclusion: No treatment decision yet includes patients with advanced CKD who did not or did not yet have to decide on a preferred treatment (commonly referred to as ‘non-dialysis dependent CKD patients’), including four studies discussed with the authors to clarify their CC-like patient group (Verberne et al. [3]); mix of patient groups means mix of different patient categories into one patient group without subgroup analyses (e.g. mix of patients who have not made a treatment decision yet and patients who chose CC); no original research, e.g. reviews, opinion papers or study protocols; no outcomes of interest for the initial systematic reviews, i.e. on HRQoL, symptoms, hospitalization and/or mortality.
Seven observational cohort studies were included, mostly single centre and with a retrospective design. The sample size varied from 269 to 1216 patients per study (3527 patients overall: 2217 with an initial treatment plan for dialysis and 1310 for CC). Within these highly heterogeneous study populations, treatment plans changed among 0.0–8.9% of the patients. Table 1 shows that 0.0–12.1% (weighted mean 5.3%) of patients changed their choice from dialysis to CC, whereas 0.0–3.9% (weighted mean 2.7%) of patients changed their choice from CC to dialysis. Reported reasons to change from dialysis to CC were based on a change in personal preference or due to deterioration of their clinical condition [7, 10]. Reported reasons to change from CC to dialysis were physical complaints after a sudden decline in kidney function [10] or secondary to intercurrent illness for which urgent dialysis was offered [7].
Table 1.
Studies reporting a change in initial choice for either dialysis or CC pathway
| Country | Design | Inclusion criteria |
Dialysis choice |
CC choice |
||||
|---|---|---|---|---|---|---|---|---|
| Study | CKD | Age | Initial, | Changed, | Initial, | Changed, | ||
| stage | (years) | n | n (%) | n | n (%) | |||
| Brown et al. [6] | Australia | P, S | G4–G5 | – | 273 | 33 (12.1) | 122 | 2 (1.6) |
| Hussain et al. [7] | UK | R, S | eGFR <20 mL/min/1.73 m2 | >70 | 269 | 19 (7.1) | 172 | 3 (1.7) |
| Kwok et al. [8] | Hong Kong | R, S | eGFR <15 mL/min/1.73 m2 | >65 | 126 | 7 (5.6) | 432 | 17 (3.9) |
| Moranne et al. [9] | France | P, M | eGFR <20 mL/min/1.73 m2 | >75 | 215a | 14 (6.5) | 54a | 1 (1.9) |
| Pyart et al. [14] | UK | R, S | eGFR <20 mL/min/1.73 m2 | >70 | 841 | 29 (3.4) | 375 | 8 (2.1) |
| Verberne et al. [2] | Netherlands | R, S | G4–G5 | >70 | 240 | 15 (6.3) | 126 | 4 (3.2) |
| Salat et al. [13] | USA | P, S | G4–G5 | >60 | 253b | 0 (0.0) | 29b | 0 (0.0) |
| Total | 2217 | 117 (5.3) | 1310 | 35 (2.7) | ||||
G4, severely reduced eGFR of 15–29 mL/min/1.73 m2); G5, kidney failure, eGFR <15 mL/min/1.73 m2; M, multicentre; n, number of patients; P, prospective study; R, retrospective study; S, single centre.
Excluding patients with nephrologist’s decision that dialysis is not appropriate and patients postponing the decision about dialysis because of stable clinical condition.
Estimation of the number of patients; due to rounding differences, no exact number could be derived from the percentages given.
Within the few studies that reported a change in (initial) treatment choice, older patients more often switched from a choice of dialysis to CC than vice versa. The studies did not specify any difference in change between patients with an initial choice for haemodialysis versus peritoneal dialysis in switching to CC. One study [14] found that all eight patients changed their choice from CC to haemodialysis (instead of peritoneal dialysis, home haemodialysis or pre-emptive transplant). The data do not describe the patient characteristics of switchers, i.e. whether patients with more advanced disease and comorbid conditions switched back to CC, while patients with better clinical conditions and faster disease progression decided to initiate dialysis. When foregoing dialysis, this most likely is a more well-informed decision, well-discussed between the patient, the medical team and the patient’s relatives, compared with a choice for dialysis, which might be the default option. Previous studies have reported that doubts are more apparent in older patients who choose dialysis rather than CC [4], and substantial numbers of patients report decisional regret after starting dialysis [15, 16]. Education programmes have been reported to reduce changes in treatment decisions [17]. We hypothesize that the smaller number of switches from CC to dialysis reflects a more thorough consideration of the treatment decision for CC.
Our review has several major limitations. First, only a small number of studies reported a change in treatment decision in both directions, suggesting that results may be biased by publication. Second, studies were heterogeneous and had a high risk of confounding and selection bias, e.g. for heterogeneity between treatment groups, incomplete outcome data and missing information [3], which warrants careful interpretation. Third, data are based on practices of nephrologists who are experienced and have a special interest in the CC pathway and may not reflect SDM practices elsewhere. Fourth, this study does not account for patients who withdraw from dialysis early in favour of CC, which may potentially lead to a greater number of patients ultimately switching from dialysis to CC. Fifth, as our systematic data search was primarily focused on survival, HRQoL and treatment burden, other research articles on therapy choice switches [17] may have been missed.
In conclusion, little attention has been paid to the topic of older patients switching their choice of therapy between dialysis and CC. The few studies that have been conducted show that older patients with CKD stage G4–G5 more often change their decision from dialysis to CC than vice versa, although treatment groups are heterogeneous and outcomes are highly susceptible to bias and confounding. Our findings underline that SDM is a continuous process rather than a static point in time. Patients may benefit from an exhaustive education process on all treatment options, including centre and home haemodialysis, peritoneal dialysis, incremental dialysis and CC, in the management of advanced CKD. This management should include active and ongoing evaluation of treatment decisions and the patient’s goals for care. Prospective studies should pay more attention to changing treatment choices for kidney failure by reporting controlled clinical observations. Both characterizing the group of patients who switch their treatment choice and gaining insights into reasons for decision changes may help nephrologists to better inform older patients with CKD in future SDM processes.
FUNDING
The study was funded by an unrestricted grant from Nephrosearch Foundation to C.G.N.V. The funder played no role in study design, collection, analysis and interpretation of data, writing of the report or the decision to submit the report for publication.
AUTHORS’ CONTRIBUTIONS
C.G.N.V., W.R.V., M.v.B. and W.J.W.B. were responsible for the research idea and study design. C.G.N.V. and W.R.V. were responsible for data acquisition. C.G.N.V., W.R.V., M.v.O., Y.M. and W.J.W.B. were responsible for data analysis/interpretation. M.v.B. and W.J.W.B. were responsible for supervision or mentorship. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author’s own contributions and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST STATEMENT
W.R.V. and W.J.W.B. reported grant support from Zilveren Kruis Healthcare Insurance Company during the conduct of the study. The remaining authors declare that they have no potential conflicts of interest.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article. No new data were generated or analysed in support of this research.
REFERENCES
- 1.Farrington K, Covic A, Nistor I. et al. Clinical practice guideline on management of older patients with chronic kidney disease stage 3b or higher (eGFR < 45 mL/min/1.73 m2): a summary document from the European Renal Best Practice Group. Nephrol Dial Transplant 2017; 32: 9–16 [DOI] [PubMed] [Google Scholar]
- 2.Verberne WR, Dijkers J, Kelder JC. et al. Value-based evaluation of dialysis versus conservative care in older patients with advanced chronic kidney disease: a cohort study. BMC Nephrol 2018; 19: 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verberne WR, van den Wittenboer ID, Voorend CGN. et al. Health-related quality of life and symptoms of conservative care versus dialysis in patients with end-stage kidney disease: a systematic review. Nephrol Dial Transplant 2020; doi: 10.1093/ndt/gfaa078 [DOI] [PubMed] [Google Scholar]
- 4.Verberne WR, Konijn WS, Prantl K. et al. Older patients’ experiences with a shared decision-making process on choosing dialysis or conservative care for advanced chronic kidney disease: a survey study. BMC Nephrol 2019; 20: 264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van den Wittenboer ID, Bos WJ. Patient-relevant outcomes of dialysis treatment versus conservative care in older patients with advanced chronic kidney disease: a systematic review. PROSPERO 2018, CRD42018103379
- 6.Brown MA, Collett GK, Josland EA. et al. CKD in elderly patients managed without dialysis: survival, symptoms, and quality of life. Clin J Am Soc Nephrol 2015; 10: 260–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussain JA, Mooney A, Russon L.. Comparison of survival analysis and palliative care involvement in patients aged over 70 years choosing conservative management or renal replacement therapy in advanced chronic kidney disease. Palliat Med 2013; 27: 829–839 [DOI] [PubMed] [Google Scholar]
- 8.Kwok W-H, Yong S-P, Kwok O-L.. Outcomes in elderly patients with end-stage renal disease: comparison of renal replacement therapy and conservative management. Hong Kong J Nephrol 2016; 19: 42–56 [Google Scholar]
- 9.Moranne O, Fafin C, Roche S. et al. Treatment plans and outcomes in elderly patients reaching advanced chronic kidney disease. Nephrol Dial Transplant 2018; 33: 2182–2191 [DOI] [PubMed] [Google Scholar]
- 10.Verberne WR, Geers AB, Jellema WT. et al. Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol 2016; 11: 633–640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuen S-K, Suen HP, Kwok O-L. et al. Advance care planning for 600 Chinese patients with end-stage renal disease. Hong Kong J Nephrol 2016; 19: 19–27 [Google Scholar]
- 12.Tse D.Experience of a renal palliative care program in a Hong Kong center: characteristics of patients who prefer palliative care to dialysis. Hong Kong J Nephrol 2009; 11: 50–58 [Google Scholar]
- 13.Salat H, Javier A, Siew ED. et al. Nephrology provider prognostic perceptions and care delivered to older adults with advanced kidney disease. Clin J Am Soc Nephrol 2017; 12: 1762–1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pyart R, Aggett J, Goodland A. et al. Exploring the choices and outcomes of older patients with advanced kidney disease. PLoS One 2020; 15: e0234309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davison SN.End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 2010; 5: 195–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkhout-Byrne N, Gaasbeek A, Mallat MJK. et al. Regret about the decision to start dialysis: a cross-sectional Dutch national survey. Neth J Med 2017; 75: 225–234 [PubMed] [Google Scholar]
- 17.Prieto-Velasco M, Quiros P, Remon C, Spanish Group for the Implementation of a Shared Decision Making Process for RRT Choice with Patient Decision Aid Tools. The concordance between patients’ renal replacement therapy choice and definitive modality: is it a utopia? PLoS One 2015; 10: e0138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article. No new data were generated or analysed in support of this research.