Abstract
Purpose
To explore how adult patients perceive deprescribing in a country with developing pharmaceutical care.
Patients and Methods
This was a multicenter cross-sectional study conducted in ten community pharmacies across Croatia. Community-dwelling adults 40 years and older, taking at least one prescription medication long term, were invited to participate. The revised and validated Patients’ Attitude Towards Deprescribing Questionnaire was used to investigate community-dwelling adults’ opinions on potential medication discontinuation. Questions regarding the patients’ perception of pharmacist competences and involvement as well as patients’ preferences in deprescribing were added. Collected data were analyzed using IBM SPSS Statistics using descriptive and inferential statistical analysis. Binary logistic regression was used to explore potential predictive factors of willingness to have medication deprescribed. All tests were performed as two-tailed and a p < 0.05 was considered statistically significant.
Results
A total of 315 adults aged 40 years and older completed the questionnaire. Majority of participants, 83.81% (95% CI, 79.72% to 87.90%) stated that they were satisfied with their medications, and 83.81% (95% CI, 79.72% to 87.90%) would be willing to deprescribe one or more medications. Participants expressed a positive attitude toward pharmacists’ competences (68.89%, 95% CI, 63.75% to 74.03%) and involvement in deprescribing (71.11%, 95% CI, 66.08% to 76.14%). Participants who stated specific medication as deprescribing preference were more likely show dissatisfaction with current medication and show greater willingness to have medication deprescribed. Three factors were found to be associated with a positive attitude towards deprescribing: low concerns about stopping factor score (aOR 0.54, 95% CU=0.35–0.84; p=0.006), low appropriateness factor score (aOR 0.62, 95% CI=0.39–0.98; p=0.039), and a positive opinion on pharmacist involvement (aOR 2.35, 95% CI=1.18–4.70; p= 0.016).
Conclusion
This study showed the patient’s willingness for deprescription as well as their positive attitude towards pharmacists being involved in the process. Results favour transition to a patient-centred care and shared-decision making model.
Keywords: stopping medications, patient preference, pharmacist, transition
Introduction
It is reported that the prevalence of polypharmacy in European’s community-dwelling older population ranges from 26.3 to 39.9% and it is expected to rise as the population continues to age.1,2 There are many definitions of polypharmacy (ie use of five or more medication) and many distinguish between appropriate and inappropriate polypharmacy. Appropriate polypharmacy typically indicates use of many medications, all of which may be needed or whose use outweighs the potential risks. Inappropriate polypharmacy represents the use of too many medications and is associated with increased risk of unwanted health outcomes.2,3 Several factors have been identified to be connected with an increased risk of polypharmacy, such as female sex, lower socioeconomic status, and lower educational attainment.4,5 Deprescribing can be used as an important and appropriate tool to combat inappropriate polypharmacy. Deprescribing has been described as a process of reducing the dose or withdrawing an inappropriate medication with the aim of reducing polypharmacy and improving health outcomes.6–9 It is a patient-focused process led by a healthcare provider. As patients are taking up a more active role in healthcare, it is becoming more evident that their opinions, beliefs, and attitudes play a key role in ensuring that the newly introduced aspects of care are beneficial. Community pharmacists are a valuable part of the healthcare team and have specific competences useful for implementing deprescribing in the primary care setting. Pharmacists’ competences in deprescribing include performing medicating review and identifying deprescribing possibilities (determining risks and benefits of medications, making evidence-based recommendations), approaching, educating, and monitoring patients during and after deprescribing and collaborating with prescribers. For instance, pharmacist-led educational interventions have proven to be effective in reducing inappropriate prescriptions.10,11 Patients at risk of polypharmacy might benefit from early familiarization to the concept of deprescribing, and community pharmacist alongside primary care physician could be an ideal healthcare provider to initiate such an important conversation.
Pharmacists from countries with less developed pharmaceutical care in central and eastern Europe (referred to as transition European countries) often find themselves encountering a paradoxical situation. Their desire to keep up to date with current trends in pharmaceutical care as presented by pharmacists from well-developed healthcare systems conflicts with the lack of policy, practice guidelines, and recognition from their own society.12–14 In Croatia pharmacist-led medication reviews, comprehensive medication management or deprescribing are still seldom used in everyday practice. Currently, comprehensive medication management is available as a pilot project in one primary health care facility,15 and one university hospital is conducting a project on pharmacist-led medication reconciliation.16,17 These services are still not supported by health policy nor reimbursed. There are no official reports, studies, or research data on deprescribing in Croatia. A recently published systematic review on community pharmacists’ role in deprescribing shows lack of deprescribing research within community pharmacies in central and eastern European countries and reports only one cohort study from Slovenia whose outcomes resulted in deprescribing.11
Patients and health care providers from lower income central and eastern Europe are accustomed to a paternalistic decision-making relationship and are making a slow transition to a shared-decision-making model. In everyday practice, it is still evident that when new aspects of care are being introduced, patients tend to escape into the protection of a paternalistic relationship rather than seek information.18,19 Pharmacists should recognize such patients and lead them towards adapting a patient-centered, shared decision-making attitude. Successful deprescribing requires patient participation and shared-decision making. Patients active involvement in decision-making improves both physical and mental health, and patients with higher decision-making preferences experienced greater increase in treatment satisfaction.20–22 Research emphasizes the importance of patients’ perspective and involvement in deprescribing, and calls for future research to focus on patient perspectives, increasing patient education, engagement and shared-decision making.23–25 Pharmacists are one potential health care provider who can initiate a conversation about deprescribing. Each health care provider contributes to deprescribing, and the final decision to proceed with deprescribing should include all stakeholders’ input. Obtaining insight into patients’ attitudes toward deprescribing and their opinion of pharmacist involvement in that process will enable pharmacists to gain momentum to take up deprescribing as part of routine pharmaceutical care. Research on all stakeholders’ opinions on new aspects of pharmaceutical care, such as deprescribing, will be useful for future policy making as well.
The objectives of this study are to explore the attitudes and opinions of Croatian patients regarding deprescribing and their perception of pharmacist involvement.
Methods
Ethics approval for this study was granted by the Ethics Committee of City Pharmacies Zagreb (1-7EP/2020 granted on 6th of February 2020). During the research, the principles of the Helsinki Declaration were followed. Written informed consent was obtained from participants.
Study Setting and Sample Size Determination
A multicenter cross-sectional study was conducted in community pharmacies across Croatia. To collect a representative sample of participants, pharmacies from different geographic areas were recruited, including four inner city urban pharmacies located in Zagreb, two suburban pharmacies in Mošćenica near the town of Sisak and Sukošan near Zadar, two rural area pharmacies (in Bedekovčina in Krapina-Zagorje County and Brodski Stupnik in Brod-Posavina County), and two pharmacies located on islands (island of Krk and island of Ugljan).
The sample size was calculated using a single population proportion formula with a 95% confidence level, relative precision of 5%, and the proportion of patients willing to have medicines deprescribed 50% since there were no previous studies in Croatia on this topic. The calculated sample size was 385. Based on available information on Croatian population spatial distribution, the selected ten pharmacies were stratified to collect the following number of participants: 60% for inner city pharmacies (around 230 participants), 30% for suburban pharmacies (around 115 participants) and 5% each for rural and island pharmacies (around 20 participants each).
Participants and Data Collection
Data collection was performed from 15th December 2019 to 15th March 2020. Community pharmacists recruited potential participants while dispensing prescriptions or counseling on the use of prescription medications. All adults 40 years and older who were using at least one prescription medication long term were approached by pharmacist with an inquiry to participate in the study. The choice to include adults 40 years and older was made due to the fact that the most prescriptions for chronic disease medications in the country of study conduction are dispensed to middle-aged and older adults. Involved pharmacist selected the participants using a simple random sampling technique. Informed consent and questionnaires (in paper form) were handed out to interested participants, who were then given the option to complete the questionnaire at home or at the pharmacy, with or without pharmacist assistance (reading questions or filling out the questionnaire for participants with poor eyesight). Participants using medication “as needed”, suffering from dementia or unwilling to participate or sign the informed consent were excluded from recruitment.
Survey
The questionnaire was composed of three sections (Supplementary file 1). The first section included personal information (age, sex, list of prescription and over-the-counter medications). The second section employed the revised Patients’ Attitude towards Deprescribing Questionnaire (rPATD) developed by Reeve et al which asked participants to answer questions on a 5-point Likert scale.26 The questionnaire has 22 items; two representing global question on willingness to have medications deprescribed and satisfaction with current pharmacotherapy. Other twenty items explore four factors (five items for each): the perceived appropriateness of medications, burden of medications, concerns about stopping, and involvement in treatment. Questions pertaining to the burden, concerns about stopping, involvement in treatment, and global questions were scored such that a higher total score indicates a greater burden, concern, involvement, or agreement with global questions (5= strongly agree, 4= agree, 3= unsure, 2=disagree, 1= strongly disagree). Questions regarding the appropriateness factor were scored in reverse. In that case, a higher score indicates participants’ belief in the appropriateness of their medications. The permission to use and translate the rPATD questionnaire was given in writing by the author. This information was stated in a footnote on the questionnaire given to participants. Following the Brislin translation model, the questionnaire was translated into Croatian and then back-translated to English to ensure no loss of meaning in translation. Two researchers independently translated the questionnaire into Croatian, while two other researchers translated it back into English.
The third section included additional questions, which explored patients’ opinions of pharmacists’ competences and involvement in potential deprescribing as well as questions regarding personal preferences toward deprescribing medication, as shown in Table 1. These questions were deemed necessary since this is the first research on deprescribing in Croatia and the study intended to explore specific opinions regarding pharmacist involvement. Similar questions were used in research in the original PATD questionnaire used in Australia, Denmark, Italy, and Malaysia.27–30 A pilot study of the pre-final version of the questionnaire was conducted on 10 participants, whose results were not included in the final analysis, and minor adjustments were made to ensure the ease of use of the final questionnaire.31
Table 1.
Questions in the Third Section of the Questionnaire
| Question | Type of Answer/Possible Answers |
|---|---|
| How would you feel if a pharmacist was involved in the process of stopping the use of one or more of your regular medications, and provided follow up? (in collaboration with your physician) | 5-point Likert scale: very comfortable, comfortable, unsure, uncomfortable, very uncomfortable |
| If you were to stop using one or more of your regular medication in collaboration with your pharmacist and physician, what follow-up method would you prefer? | Telephone call, pharmacy visit, mail (including e-mail, text message, social media), no follow-up, other |
| Do you believe your pharmacist has enough knowledge, skills, and information about your medications to suggest deprescribing to you and your physician? | 3-point Likert scale: yes, unsure, no |
| What medication/s would you LIKE to stop taking (that you believe you no longer need, or feel is causing you harm) | Text space to fill |
| What medication/s you would NOT LIKE to stop taking? | Text space to fill |
Statistical Analysis
Collected data were analyzed using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY, USA). Frequencies, percentages, medians, and interquartile ranges were used to describe the data. A chi-squared test was used to analyze differences in frequencies between groups. Groups were formed for gender (male or female), age (younger or older than 65 years), and number of medicines (less than five or five and more medications). For analysis purposes, answers to global questions were combined as following: “strongly agree” and “agree” to form “agree”, and “unsure”, “disagree” and “strongly disagree” to form “disagree”. Factor score was calculated by summing the score of each item and dividing by the number of items within the factor. Based on median factor score, two ranks were computed for each factor (low or high). Spearman’s rank-order correlation analysis was employed to explore the relationship between factor scores and global questions (using ordinal data for five-point Likert scale data for global questions and continuous data for calculated factor scores). Binary logistic regression was used to explore potential predictive factors of willingness to have medication deprescribed. All tests were performed as two-tailed, and a p < 0.05 was considered statistically significant. Internal consistency of all factors was satisfactory, with Cronbach’s alpha values as follows: 0.88 for burden factor, 0.81 for appropriateness factor, 0.63 for concerns about stopping factor and 0.83 for involvement factor. The intraclass correlation coefficient (ICC) was used to assess the test–retest reliability of the questionnaire for all items scored with Likert scale. The ICC of each item ranged from 0.69 to 0.96 indicating a good to excellent inter-rater reliability.
Results
Pharmacists distributed 385 questionnaires and received 315 completely answered questionnaires (return rate 82%). Eight returned questionnaires did not have correctly signed informed consent and were thus excluded from the analysis, and 62 questionnaires were not returned. Of the 315 participants, 61.60% were female (194 participants), and the median age was 68 years (IQR: 57–77). Participants were taking a median of four (IQR: 2–6) medications daily and the most commonly prescribed medications included those for the treatment of the cardiovascular system, alimentary tract and metabolism, nervous system, and blood forming organs (Table 2).
Table 2.
Participants’ Characteristics
| Participants’ characteristics (n=315) | |
| Age (years) | |
| Median (IQR) | 68 (57–77) |
| < 65 years (n, % of participants) | 121 (38.40%) |
| > 65 years (n, % of participants) | 194 (61.60%) |
| Gender (n, %) | |
| Male | 121 (38.40%) |
| Female | 194 (61.60%) |
| Pharmacotherapy characteristics | |
| Number of medications | |
| Median (IQR) | 4 (2–6) |
| < 5 medication (n, % of participants) | 219 (69.50%) |
| ≥ 5 medication (n, % of participants) | 96 (30.50%) |
| ATC classification (% of participants with prescribed medication) | |
| Alimentary tract and metabolism | 45.40% |
| Blood and blood forming organs | 26.98% |
| Cardiovascular system | 81.27% |
| Dermatologics | 1.59% |
| Genitourinary system and sex hormones | 11.75% |
| Systemic hormonal preparations | 18.10% |
| Antineoplastic and immunomodulating agents | 5.40% |
| Musculoskeletal system | 20.00% |
| Nervous system | 38.10% |
| Respiratory system | 12.38% |
| Sensory organs | 6.35% |
| Various | 0.63% |
Abbreviation: IQR, interquartile range.
About 62% of the participants were elderly (over 65 years of age) and 30.50% were taking five or more medications.
Patients Attitude Towards Deprescribing
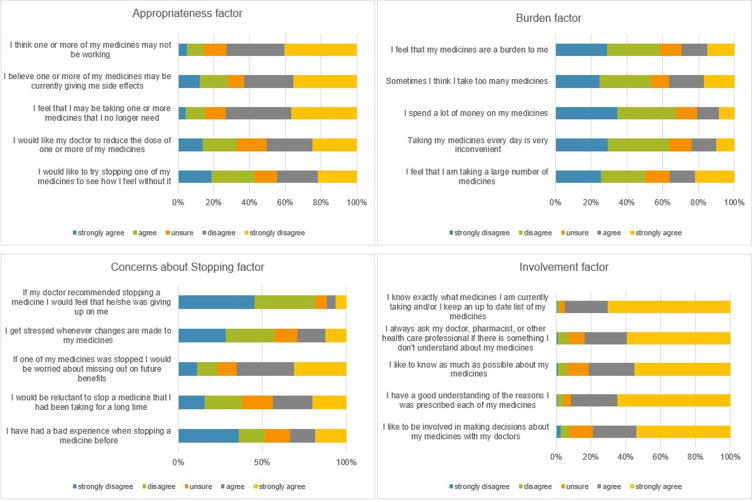
Most of the participants reported that they were satisfied with their current medications (n=264, 83.81%, 95% CI, 79.72% to 87.90%). A similar percentage of participants would be willing to stop one or more of their regular medications if their doctor said it was possible (83.81%, 95% CI, 79.72% to 87.90%). Responses to all rPATD questions are represented in Figure 1.
Figure 1.
Responses to rPATD questions.
An association between gender and overall satisfaction was observed (χ2 (1) =6.99; p= 0.008), with women being more satisfied with their current medications than men. There was no statistically significant difference in the willingness toward deprescribing medication between gender.
Participants over the age of 65 years were more willing to have their medications deprescribed (χ2 (1) =4.06; p= 0.044) than their younger counterparts, but there was no statistically significant difference in overall satisfaction with medications between age groups.
There was no statistically significant difference in patients’ willingness to have medications deprescribed or in overall satisfaction with medication between patients currently taking >5 or <5 medications.
Assessed factor scores show that participants experience a moderate medication burden and have moderate concerns about stopping medication. Higher median scores for the involvement and appropriateness factors indicate that participants want to be involved in the management of their medications and find their pharmacotherapy somewhat appropriate (Table 3).
Table 3.
Factor Scores
| Factor Scores (N=315) | Burden Factor Score | Appropriateness Factor Score | Concerns About Stopping Score | Involvement Factor Score |
|---|---|---|---|---|
| Median | 2.60 | 3.60 | 2.80 | 4.60 |
| Percentiles | 1.60 | 2.80 | 2.20 | 4.00 |
| 2.60 | 3.60 | 2.80 | 4.60 | |
| 3.40 | 4.20 | 3.40 | 5.00 |
Participants under the age of 65 years were more likely to have the appropriateness factor score below the median (χ2 (1) =5.96; p= 0.015) than their older counterparts. There were no statistically significant differences in concerns about stopping factor score, burden factor score, involvement factor score, opinion on pharmacist involvement and knowledge, or specific preferences to deprescribing between age groups.
The strongest positive correlation was found between overall satisfaction with medications and belief in appropriateness (rs = 0.488; p < 0.001). A positive correlation was found between the involvement factor and global questions (rs = 0.273; p < 0.001 and rs = 0.243; p < 0.001, respectively), meaning greater involvement in treatment was associated with greater overall satisfaction with medications and greater willingness to have medications deprescribed. There was a weak positive correlation between the involvement factor and the appropriateness factor, and a moderate positive correlation between the burden factor and the concerns about stopping medication factor. A moderate strength negative correlation was found between burden and appropriateness, and burden and overall satisfaction (rs = −0.556; p < 0.001 and rs = −0.406; p < 0.001, respectively), indicating that an increased burden correlated with decreased satisfaction and belief in the appropriateness of medications. A weak negative correlation was found between willingness to have medication deprescribed and the concerns about stopping factor.
Perception of Pharmacists’ Involvement, Knowledge, and Skills
The majority of participants (71.11%, 95% CI, 66.08% to 76.14%) would feel comfortable if a pharmacist was involved in the deprescribing process, 17.46% were unsure, and 11.43% felt uncomfortable When asked: “Do you believe your pharmacist has enough knowledge, skills, and information about your medications to suggest deprescribing to you and your physician?”, 68.89% (95% CI, 63.75% to 74.03%) of participants answered positively, 22.54% were unsure, and 8.57% answered negatively. No difference was found among groups of different ages, sex, and number of medications with regard to their perception of pharmacist competences or involvement.
Regarding the follow-up method, 44.12% of participants preferred a pharmacy visit (appointment with a pharmacist), 34.28% preferred telephone calls, 0.97% preferred mail of any kind, 11.11% would prefer other methods of follow-up (eg, doctor’s appointment), and 9.52% would prefer no follow-up. A statistically significant difference was observed in the patients’ preference of follow-up method, with participants aged <65 years preferring telephone calls to pharmacy visits. Younger participants also chose “no follow-up” more frequently than older participants (χ2(4) = 13.05; p= 0.011).
Patients’ Personal Preference to Deprescribing
Two final questions in the questionnaire aimed to gather information on participants’ preference on which medication they would or would not like to have deprescribed. When asked which medication they would like to have deprescribed, 31.75% participants gave no answer, 32.69% stated that they would not have any medication deprescribed, and 2.85% stated wanting to have all their medication deprescribed. A small percentage of participants stated the exact medication they would be willing to have deprescribed, with almost 7% of participants wanting to have anti-hypertensive medication deprescribed, 3.50% wanting benzodiazepines or hypnotics and statins deprescribed, while 2.88% wanted NSAIDs deprescribed. Interestingly, four participants (1.27%) stated that they stopped taking medication of their own accord.
Participants gave a more diverse array of responses to the question of which medication they would not like to have deprescribed. About 28.25% did not give an answer, 24.44% stated “all medication”, 15.87% stated anti-hypertensive medication, 8.57% stated “no medication”, 4.76% stated antidiabetic medication, and 3.50% of participants stated not wanting benzodiazepines or hypnotics and thyroid medication deprescribed.
Participants who stated specific medication as deprescribing preference were more likely to answer negative to the question of overall satisfaction with current medicines (χ2 (1) = 40.38; p < 0.001). Likewise, patients who answered positively to the global question of willingness to have medication deprescribed were more likely to state a specific medication they would be willing to stop taking (χ2 (1) = 9.07; p = 0.003).
Predictors of the Willingness to Have Medication Deprescribed
A binary logistic regression model was used to analyze potential predictors of the willingness to have medication deprescribed. Participants’ age, sex, number of medications, factor scores, and opinions on pharmacist involvement and pharmacist knowledge in deprescribing were included in the model. The results showed that those having a positive opinion about pharmacist’s involvement had the odds of 2.35 times greater willingness to participate in deprescription (aOR=2.35; 95% CI=1.18–4.70). The odds ratio for appropriateness factor scores (aOR= 0.62; 95% CI=0.39–0.98) and concerns about stopping factor scores (aOR= 0.542; 95% CI=0.35–0.84) indicates that higher the scores, the less likely the patient will want to have medication deprescribed. (Table 4).
Table 4.
Willingness to Have Medication Deprescribed Binary Logistic Regression Analysis
| Independent Variable | aOR | 95% CI | p value | |
|---|---|---|---|---|
| Appropriateness factora | 0.619 | 0.392 | 0.976 | 0.039 |
| Burden factor scorea | 1.466 | 0.954 | 2.253 | 0.081 |
| Concerns about stopping factor scorea | 0.542 | 0.351 | 0.839 | 0.006 |
| Involvement factor scorea | 1.443 | 0.885 | 2.352 | 0.142 |
| Positive opinion on pharmacist competencesb | 1.370 | 0.677 | 2.776 | 0.381 |
| Positive opinion on pharmacist involvementb | 2.351 | 1.176 | 4.699 | 0.016 |
| Age | 0.973 | 0.924 | 1.024 | 0.292 |
| Number of medications | 0.945 | 0.804 | 1.111 | 0.496 |
| Female gender | 1.307 | 0.667 | 2.561 | 0.436 |
Notes: The logistic regression model was significant (p < 0.001) with a good model fit (Hosmer–Lemeshow test χ2 (8) =7.894; p= 0.444). It correctly predicted 84.80% of the results and explained 20.00% of the variance. Variables which are significant for this model are labeled in italics and their values in bold. aPossible score range 1–5, bparticipants could have a positive or negative opinion.
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
Discussion
This cross-sectional study reported the first data on patients’ attitudes on deprescribing in transitioning European country. The results showed that Croatian patients are satisfied with their pharmacotherapy but have nevertheless expressed their willingness to have medication deprescribed. Majority of participants were comfortable with pharmacists’ potential involvement in deprescribing and had a positive opinion on pharmacists’ competencies regarding deprescribing.
This study is among few to have an accentuated focus on patients’ opinions of the role of community pharmacists in deprescribing. The emphasis on community pharmacists’ potential involvement in deprescribing stems from research demonstrating that a multidisciplinary approach (including a pharmacist) is essential for successful deprescribing.10,32–35 A study by Ng et al reported that half of the participants were comfortable with pharmacist involvement.36 In this study, a larger percentage of participants were identified as having a positive attitude toward the pharmacists’ role in deprescribing. Seventy-one percent had a positive opinion on pharmacists’ involvement, and 69% believed that pharmacists had appropriate competences for deprescribing Another positive aspect of pharmacist involvement is that majority of patients reported that they preferred face-to-face meetings with a pharmacist as a follow-up method. Schiøtz et al reported comparable results in their study in Denmark.27
Patients with multiple chronic comorbidities and repeat prescriptions often visit their community pharmacist more often than their physician. Community pharmacists are well positioned to be physicians’ partner in improving patient outcomes. Successful collaboration requires not only mutual trustworthiness,37,38 but exchange and access to information as well. Studies have proven that pharmacist-led collaborative deprescribing interventions are feasible and effective.39,40 The accessibility of a community pharmacist should invoke building a trustworthy relationship, and pharmacists could provide the encouragement a patient needs to consider deprescribing.
An association between age and willingness to have medication deprescribed was identified; patients aged 65 years and older were more willing to have medication deprescribed. Other studies have investigated the opinions of older adults in various settings; selecting adults 40 years and older to participate in this study seemed reasonable. With Europeans aging population and rise of inappropriate polypharmacy, deprescribing research in younger patients is limited. Many younger adults with comorbidities will most likely be adding medication to their pharmacotherapy and could benefit from early familiarization with deprescribing. Nevertheless, opinions of older participants from this study are comparable to opinions of older adults worldwide.26,29,30,36,41–46 While younger participants might not have expressed their willingness to have medication deprescribed through the global question, they were more likely to have lower appropriateness factor score. Low appropriateness factor score was found to be a predictive factor for willingness to have medication discontinued and could indicate younger participants require additional attention and conversation regarding their pharmacotherapy. Middle-aged adults could become an important group for future deprescribing interventions.
Patients from this study have similar appropriateness, burden, and concerns about stopping factor scores as patients from well-developed countries.44,47 The slight difference in scores could be due to the proportion of younger participants or differences in the healthcare system and participants’ healthcare literacy.48,49 In contrast to patients from the UK and the Netherlands participants from this study expressed greater desire to be involved in management of their treatment.50,51 We identified patients’ readiness for the deprescribing service, which is an important element for the initiation of the deprescribing process. However, the preparedness of the health-care system is equally important for successful implementation with an emphasis on collaboration of different healthcare providers and the availability and sharing of the information. For example, Croatian community pharmacists are in a disadvantageous position with regard to access to patients’ healthcare information, where only the currently prescribed and previously dispensed electronic prescriptions in particular pharmacy are accessible. Lack of information for pharmacist could be a missed opportunity to review medication from a different perspective, recognize deprescribing opportunities, and initiate conversation about deprescribing. Participants' desire for involvement in decision-making is an important stepping stone in providing shared-decision-making care. For countries with developing pharmaceutical care high level of patients’ involvement could be an indicator of readiness to accept new forms of patient-centered services, such as deprescribing. This finding could be used as a part of implementation strategy. One potential strategy could include initiating conversation between patient interest groups and primary care providers including pharmacist on the topic of inappropriate medicines use and deprescribing.
Many participants did not clearly state which medication they would prefer to stop taking. These results are contradictory to the results to one of the global questions, to which a majority of participants answered positively. Moreover, some participants mentioned that they want all their medications deprescribed, which is not the goal of deprescribing. This could indicate patients’ misunderstanding of the deprescribing process, which is not surprising in the country where it is not implemented. Patients’ perception of deprescribing could be based on knowledge they gained from a questionnaire but also on their desire to stop all the therapy. In practice, this could be an important finding and allows for the identification of patients who need consultation on their therapy in order to ensure the adherence to the necessary therapy. Overall, patients answers on the question which specific medication they want to be deprescribed could suggest lack of knowledge about their therapy, disguised non-adherence, or uncertainty about the possibilities of informed shared-decision making, and indicate pharmacist educator role is very important. Two recent conceptual deprescribing frameworks emphasize the importance of patients factors when discussing deprescribing, especially attitudes about medications, medication literacy, and experience with medication.24,25 The final decision to start the deprescribing process should be made equally by all involved parties, pharmacist, physician, and patient. Patients should view deprescribing as a positive intervention in their therapy and their familiarity and opinion on pharmacotherapy is an important factor to consider. For pharmacists, this finding could represent a challenge in deprescribing, and indicates the need for additional time invested in counseling patients. This challenge pharmacists for providing better, more holistic pharmaceutical care; thus, this should be addressed.52 It is the healthcare providers’ role to use their expertise and evaluate the suitability and need for a certain medication, and they should not expect patients to know which medication is no longer necessary. Nevertheless, for patients who have stated specific medication they would want to have deprescribed it would be prudent to further investigate the deprescribing potential as well as other important patient factors, such as medication adherence or potential adverse reactions. Even though a small number of participants stated the exact medication they would be willing to stop taking, benzodiazepines, NSAID and antihypertensives, for most medication there are available deprescribing guidelines. Knowing which specific medication patients are willing to have deprescribed would allow pharmacist and physician an easier planning of interventions. The diversity of answers could suggest the realistic number of patients who would actually participate in a deprescribing attempt.
Three factors were found to be predictive of a positive attitude toward deprescribing: low concerns about stopping medication factor score, low appropriateness factor score, and a positive opinion on pharmacist involvement. In comparison to other studies, in this study, positive opinion on pharmacist involvement is indicative of the patient’s willingness to have medications deprescribed. Pharmacists could take advantage of this information and identify potential candidates who are more willing to deprescribe. A study by Martinez et al investigated the attitudes of middle-aged women and came to a similar conclusion.53
This study has limitations. Sociodemographic information may be a predictor of willingness to deprescribe; however, the information provided was limited in this study. This approach was chosen because Croatian patients are not accustomed to participating in research and are often unwilling to participate if personal information is collected or if data collection is time-consuming. For this reason, investigators deemed it more important to focus on the rPATD and added questions to avoid potential participant fatigue. Community pharmacists collecting data could have been prone to selection bias, which may have influenced how questions about pharmacists’ involvement and knowledge were answered. Adults who were able to visit the pharmacy were selected to participate; therefore, our results could not be generalized to other community-dwelling patient populations such as frailer adults or patients with disabilities. The majority of participants completed the questionnaire in the pharmacy with the pharmacists’ help, and as such, their answers might be prone to bias. Nevertheless, the results could be viewed as the patients trusting the pharmacist and as a good foundation for the successful implementation of deprescribing. The fact that some participants mentioned that they want all their medications deprescribe could indicate their misunderstanding in deprescribing concept and may result in biased responses. However, it also provides additional information on patients’ understanding of their therapy and the concept of deprescribing. As intended, this open question gets deeper understanding of patients’ attitudes towards the deprescribing and added to the rPADT could inform the health-providers on the needed interventions besides the deprescribing. Further analysis of patient’s answers did not show any statistically significant differences between patients’ opinion on pharmacist knowledge or involvement in deprescribing and their answers to which medication they would want to stop taking.
It could be helpful to introduce the rPATD questionnaire as standard practice in pharmaceutical care for patients with chronic pharmacotherapy and to have them revisit and retake the survey from time to time as patients’ beliefs might change with their age and the appropriateness of their pharmacotherapy. In everyday practice, where pharmacist experience time constraints, it might prove to be useful to ask selected items from the rPATD questionnaire (ie appropriateness factor items) to quickly identify patients who could benefit from additional conversation about deprescribing.
While deprescribing has become a significant research topic, with new and interesting evidence emerging, there is no agreement on the most efficient approach to successful deprescribing. For countries that lack funding for pharmaceutical development, this could be even harder. It is pertinent to explore deprescribing “globally” within such healthcare systems and to include all stakeholders so that the inevitable introduction and acceptance of deprescribing is as seamless as possible. Further research should focus on exploring opinions, barriers, and factors, which enable pharmacists and primary care physicians to fulfill their role in deprescribing, as they might differ from providers in different healthcare systems. Characteristics specific to this country and its healthcare include a relatively small population with little social or racial diversity, predominantly universal (social) healthcare insurance, universally used centralized healthcare information system on the primary healthcare level, and the specific positions of community pharmacists could be important factors that influence deprescribing. Information gained from future research, including planned interventional studies, could help countries with similar characteristics to experience an easier transition into implementing deprescribing in everyday practice. Future interventional studies could be community pharmacist-led, directed at patients with low appropriateness factor score, patients with higher involvement factor score, or those who state dissatisfaction with certain medication as they are more likely to want to have medicines deprescribed.
Conclusion
Implementation of new aspects of patient-centered care in transition health care systems should be based on research, not only including opinions and capabilities of healthcare professionals, but also the attitudes and expectations of those who are intended to receive the most benefits from those actions. Patients from a country with developing pharmaceutical care would be comfortable with pharmacists’ involvement in deprescribing, and this finding should be used in introducing deprescribing and promoting the pharmacists’ competences. While transitioning to a shared decision-making mindset may take time, these patients show similar attitudes towards deprescribing as patients from countries with well-developed pharmaceutical care.
Potentially, those with decreased opinion on medication appropriateness could be the first candidates to benefit from deprescribing. Additional interventional studies in transition healthcare systems are necessary.
Acknowledgments
Tena Tarade, MPharm, Kristina Grgić Petrović, MPharm, Marina Šekerija, MPharm, and Magdalena Mašić, MPharm helped distribute and collect surveys across Croatia.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sector.
Abbreviations
rPATD, revised Patients’ Attitude towards Deprescribing Questionnaire; NSAID, nonsteroidal anti-inflammatory drug.
Author Contributions
Iva Bužančić: Conceptualization, Methodology, Software, Formal analysis, Investigation, Data Curation, Writing – Original Draft, Writing – Review & Editing, Visualization, Project administration. Patricia Dragović: Conceptualization, Investigation, Data Curation, Writing – Original Draft, Formal analysis. Tajana Iva Pejaković: Investigation, Data Curation, Writing – Original Draft. Luka Markulin: Investigation, Data Curation, Writing – Original Draft. Maja Ortner-Hadžiabdić: Conceptualization, Methodology, Resources, Writing – Original Draft, Writing – Review & Editing, Visualization, Supervision, Project administration. All authors contributed to data analysis, drafting, or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Midão L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr. 2018;78:213–220. doi: 10.1016/j.archger.2018.06.018 [DOI] [PubMed] [Google Scholar]
- 2.Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:204209862093374. doi: 10.1177/2042098620933741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1). doi: 10.1186/s12877-017-0621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Assari B. Race/Ethnicity, socioeconomic status, and polypharmacy among older Americans. Pharmacy. 2019;7(2):41. doi: 10.3390/pharmacy7020041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang N, Sundquist J, Sundquist K, Ji J. An increasing trend in the prevalence of polypharmacy in Sweden: a nationwide register-based study. Front Pharmacol. 2020;11:326. doi: 10.3389/fphar.2020.00326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. J Pharm Pract Res. 2003;33(4):323–328. doi: 10.1002/jppr2003334323 [DOI] [Google Scholar]
- 7.Alldred DP. Deprescribing: a brave new word? Int J Pharm Pract. 2014;22(1):2–3. doi: 10.1111/ijpp.12093 [DOI] [PubMed] [Google Scholar]
- 8.Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of “deprescribing” with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol. 2015;80(6):1254–1268. doi: 10.1111/bcp.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Potter K, Page A, Clifford R, Etherton-Beer C. Deprescribing: a guide for medication reviews. J Pharm Pract Res. 2016;46(4):358–367. doi: 10.1002/jppr.1298 [DOI] [Google Scholar]
- 10.Martin P, Tamblyn R, Benedetti A, Ahmed S, Tannenbaum C. Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: the D-PRESCRIBE randomized clinical trial. J Am Med Assoc. 2018;320(18):1889–1898. doi: 10.1001/jama.2018.16131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bužančić I, Kummer I, Držaić M, Ortner‐Hadžiabdić M. Community‐based pharmacists’ role in deprescribing: a systematic review. Br J Clin Pharmacol. 2021;bcp14947. doi: 10.1111/bcp.14947 [DOI] [PubMed] [Google Scholar]
- 12.Świeczkowski D, Merks P, Cwalina N, Jaguszewski M. Development of pharmacy practice in European Countries—The polish perspective. Pharmacy. 2017;5(4):43. doi: 10.3390/pharmacy5030043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Medication safety in transitions of care. WHO; 2019:52. [Google Scholar]
- 14.Bulajeva A, Labberton L, Leikola S, et al. Medication review practices in European countries. Res Soc Adm Pharm. 2014;10(5):731–740. doi: 10.1016/j.sapharm.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 15.Brajković A, Mucalo I, De Oliveira DR. Implementation of medication management services at the primary healthcare level - a pilot study. Acta Pharm. 2019;69(4):585–606. doi: 10.2478/acph-2019-0055 [DOI] [PubMed] [Google Scholar]
- 16.Marinović I, Marušić S, Mucalo I, Mesarić J, Vrca VB. Clinical pharmacist-led program on medication reconciliation implementation at hospital admission: experience of a single university hospital in Croatia. Croat Med J. 2016;57(6):572–581. doi: 10.3325/cmj.2016.57.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marinović I, Bačić Vrca V, Samardžić I, et al. Impact of an integrated medication reconciliation model led by a hospital clinical pharmacist on the reduction of post-discharge unintentional discrepancies. J Clin Pharm Ther. 2021. doi: 10.1111/jcpt.13431 [DOI] [PubMed] [Google Scholar]
- 18.Murgic L, Hébert PC, Sovic S, Pavlekovic G. Paternalism and autonomy: views of patients and providers in a transitional (post-communist) country. BMC Med Ethics. 2015;16(1):65. doi: 10.1186/s12910-015-0059-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vučemilo L, Ćurković M, Milošević M, Mustajbegović J, Borovečki A. Are physician-patient communication practices slowly changing in Croatia? - A cross-sectional questionnaire study. Croat Med J. 2013;54(2):185–191. doi: 10.3325/cmj.2013.54.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kayyali R, Gebara SN, Hesso I, et al. Shared decision making and experiences of patients with long-term conditions: Has anything changed? BMC Health Serv Res. 2018;18(1):1–10. doi: 10.1186/s12913-018-3575-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes TM, Merath K, Chen Q, et al. Association of shared decision-making on patient-reported health outcomes and healthcare utilization. Am J Surg. 2018;216(1):7–12. doi: 10.1016/J.AMJSURG.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 22.Aljumah K. Impact of pharmacist intervention using shared decision making on adherence and measurable depressed patient outcomes. Value Health. 2016;19(3):A19. doi: 10.1016/J.JVAL.2016.03.410 [DOI] [Google Scholar]
- 23.Thompson W, Reeve E, Moriarty F, et al. Deprescribing: future directions for research. Res Soc Adm Pharm. 2019;15(6):801–805. doi: 10.1016/j.sapharm.2018.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Linsky A, Gellad W, Linder JA, Friedberg MW. Advancing the science of deprescribing: a novel comprehensive conceptual framework. J Am Geriatr Soc. 2019;67(10):2018–2022. doi: 10.1111/jgs.16136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Todd A, Jansen J, Colvin J, McLachlan AJ. The deprescribing rainbow: a conceptual framework highlighting the importance of patient context when stopping medication in older people. BMC Geriatr. 2018;18(1):1–8. doi: 10.1186/s12877-018-0978-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reeve E, Low LF, Shakib S, Hilmer SN. Development and validation of the revised Patients’ Attitudes Towards Deprescribing (rPATD) questionnaire: versions for older adults and caregivers. Drugs Aging. 2016;33(12):913–928. doi: 10.1007/s40266-016-0410-1 [DOI] [PubMed] [Google Scholar]
- 27.Schiøtz ML, Frølich A, Jensen AK, et al. Polypharmacy and medication deprescribing: a survey among multimorbid older adults in Denmark. Pharmacol Res Perspect. 2018;6(6):e00431. doi: 10.1002/prp2.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reeve E, Wiese MD, Hendrix I, Roberts MS, Shakib S. People’s attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc. 2013;61(9):1508–1514. doi: 10.1111/jgs.12418 [DOI] [PubMed] [Google Scholar]
- 29.Jia Hao L, Omar MS, Tohit N. Polypharmacy and willingness to deprescribe among elderly with chronic diseases. Int J Gerontol. 2018;12(4):340–343. doi: 10.1016/j.ijge.2018.05.006 [DOI] [Google Scholar]
- 30.Galazzi A, Lusignani M, Chiarelli MT, et al. Attitudes towards polypharmacy and medication withdrawal among older inpatients in Italy. Int J Clin Pharm. 2016;38(2):454–461. doi: 10.1007/s11096-016-0279-4 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. Process of translation and adaptation of instruments. WHO; 2010. [Google Scholar]
- 32.Ailabouni N, Mangin D, Nishtala PS. DEFEAT-polypharmacy: deprescribing anticholinergic and sedative medicines feasibility trial in residential aged care facilities. Int J Clin Pharm. 2019;41(1):167–178. doi: 10.1007/s11096-019-00784-9 [DOI] [PubMed] [Google Scholar]
- 33.Martin P, Tamblyn R, Ahmed S, Tannenbaum C. An educational intervention to reduce the use of potentially inappropriate medications among older adults (EMPOWER study): protocol for a cluster randomized trial. Trials. 2013;14(1):80. doi: 10.1186/1745-6215-14-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med. 2014;174(6):890–898. doi: 10.1001/jamainternmed.2014.949 [DOI] [PubMed] [Google Scholar]
- 35.Elbeddini A, Zhang CXY. The pharmacist’s role in successful deprescribing through hospital medication reconciliation. Can Pharm J. 2019;152(3):177–179. doi: 10.1177/1715163519836136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ng WL, Tan MZW, Koh EYL, Tan NC. Deprescribing: what are the views and factors influencing this concept among patients with chronic diseases in a developed Asian community? Proc Singapore Healthc. 2017;26(3):172–179. doi: 10.1177/2010105817699633 [DOI] [Google Scholar]
- 37.Matzke GR, Moczygemba LR, Williams KJ, Czar MJ, Lee WT. Impact of a pharmacist–physician collaborative care model on patient outcomes and health services utilization. Am J Heal Pharm. 2018;75(14):1039–1047. doi: 10.2146/AJHP170789 [DOI] [PubMed] [Google Scholar]
- 38.Snyder ME, Zillich AJ, Primack BA, et al. Exploring successful community pharmacist-physician collaborative working relationships using mixed methods. Res Soc Adm Pharm. 2010;6(4):307–323. doi: 10.1016/J.SAPHARM.2009.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Potter EL, Lew TE, Sooriyakumaran M, Edwards AM, Tong E, Aung AK. Evaluation of pharmacist-led physician-supported inpatient deprescribing model in older patients admitted to an acute general medical unit. Australas J Ageing. 2019;38(3):206–210. doi: 10.1111/AJAG.12643 [DOI] [PubMed] [Google Scholar]
- 40.Cheong ST, Ng TM, Tan KT. Pharmacist-initiated deprescribing in hospitalised elderly: prevalence and acceptance by physicians. Eur J Hosp Pharm. 2018;25(e1):e35–e39. doi: 10.1136/EJHPHARM-2017-001251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nusair MB, Arabyat R, Al-Azzam S, El-Hajji FD, Nusir AT, Al-Batineh M. Translation and psychometric properties of the Arabic version of the revised patients’ attitudes towards deprescribing questionnaire. J Pharm Health Serv Res. 2020;11(2):173–181. doi: 10.1111/jphs.12340 [DOI] [Google Scholar]
- 42.Edelman M, Jellema P, Hak E, Denig P, Blanker MH. Patients’ attitudes towards deprescribing alpha-blockers and their willingness to participate in a discontinuation trial. Drugs Aging. 2019;36(12):1133–1139. doi: 10.1007/s40266-019-00712-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Soc Adm Pharm. 2017;13(4):864–870. doi: 10.1016/j.sapharm.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 44.Aoki T, Yamamoto Y, Ikenoue T, Fukuhara S. Factors associated with patient preferences towards deprescribing: a survey of adult patients on prescribed medications. Int J Clin Pharm. 2019;41(2):531–537. doi: 10.1007/s11096-019-00797-4 [DOI] [PubMed] [Google Scholar]
- 45.Tegegn HG, Tefera YG, Erku DA, et al. Older patients’ perception of deprescribing in resource-limited settings: a cross-sectional study in an Ethiopia university hospital. BMJ Open. 2018;8(4):e020590. doi: 10.1136/bmjopen-2017-020590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kua KP, Saw PS, Lee SWH. Attitudes towards deprescribing among multi-ethnic community-dwelling older patients and caregivers in Malaysia: a cross-sectional questionnaire study. A comment. Int J Clin Pharm. 2019;41(5):1131–1132. doi: 10.1007/s11096-019-00891-7 [DOI] [PubMed] [Google Scholar]
- 47.Reeve E, Low LF, Hilmer SN. Attitudes of older adults and caregivers in Australia toward deprescribing. J Am Geriatr Soc. 2019;67(6):1204–1210. doi: 10.1111/jgs.15804 [DOI] [PubMed] [Google Scholar]
- 48.Australian Institute of Health and Welfare 2018. Australia's health 2018. Cat. no. AUS 221. Canberra: AIHW. doi: 10.25816/5ec1e56f25480 Available from: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/indicators-of-australias-health/health-literacy. Accessed May 2, 2021. [DOI]
- 49.Brangan S, Ivanišić M, Rafaj G, Rowlands G. Health literacy of hospital patients using a linguistically validated Croatian version of the Newest Vital Sign screening test (NVS-HR). PLoS One. 2018;13(2):e0193079. doi: 10.1371/journal.pone.0193079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scott S, Clark A, Farrow C, et al. Attitudinal predictors of older peoples’ and caregivers’ desire to deprescribe in hospital. BMC Geriatr. 2019;19(1):1–11. doi: 10.1186/s12877-019-1127-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crutzen S, Abou J, Smits SE, et al. Older people’s attitudes towards deprescribing cardiometabolic medication. BMC Geriatr. 2021;21(1):366. doi: 10.1186/s12877-021-02249-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wolters M, van Hulten R, Blom L, Bouvy ML. Exploring the concept of patient centred communication for the pharmacy practice. Int J Clin Pharm. 2017;39(6):1145–1156. doi: 10.1007/s11096-017-0508-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martinez AI, Spencer J, Moloney M, Badour C, Reeve E, Moga DC. Attitudes toward deprescribing in a middle-aged health disparities population. Res Soc Adm Pharm. 2020;16(10):1502–1507. doi: 10.1016/j.sapharm.2020.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]